User login
Leadless dual-chamber pacemaker clears early safety, performance hurdles
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HRS 2023
Cut in AFib burden gains traction as gauge of ablation success: PULSED-AF
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HRS 2023
Earlier anticoagulation safe in stroke with AFib: ELAN
, a new study suggests.
The ELAN trial found that starting DOAC treatment earlier was not associated with an increased risk for intracranial hemorrhage (ICH) but rather was linked to a lower rate of ischemic events.
“We conclude that there is no reason to delay DOAC treatment in these patients. Our results suggest that early DOAC treatment is reasonable; it is unlikely to cause harm, and it is probably better at reducing ischemic events,” lead investigator of the study, Urs Fischer, MD, professor of neurology at University Hospital Basel (Switzerland), commented in an interview.
“This trial will change clinical practice in that we can feel much more reassured that starting DOAC treatment early in these patients will not cause harm,” he said.
Senior investigator Jesse Dawson, MD, professor of stroke medicine at Queen Elizabeth University Hospital, Glasgow, added: “This issue of timing of DOAC treatment causes a lot of anxiety in our daily workload. Clinicians are scared of causing an ICH, so they tend to wait. These results will ease a lot of that anxiety.”
Dr. Fischer presented the results of the ELAN trial at the European Stroke Organisation Conference (ESOC) in Munich. The trial was also simultaneously published online in The New England Journal of Medicine.
He explained that patients presenting with acute ischemic stroke who are found to have atrial fibrillation need to be started on anticoagulation to reduce the risk for a recurrent stroke. But there are no clear guidelines on when to start anticoagulation in these patients at present, with concerns that starting very early may increase the risk for hemorrhagic transformation and ICH.
Based on observations that patients with larger strokes have a higher risk for ICH in the early post-stroke period, some guidelines advise different times for starting anticoagulation for different stroke severities: 1 day for a transient ischemic attack, 3 days for a minor stroke, 6 days for a moderate stroke, and 12 days for a severe stroke – known as the 1-, 3-, 6-, 12-day rule.
“But this is not based on evidence – just on expert opinion,” Dr. Fischer noted. “The ELAN trial was conducted to obtain more solid information on optimal timing for starting anticoagulation and whether we can safely start a DOAC earlier than these guidelines currently advise.”
For the trial, which was conducted in 15 countries, 2,013 patients with an acute ischemic stroke and found to have AFib were randomly selected to start DOAC treatment earlier or later.
The later-treatment strategy followed the current approach of starting treatment at day 3 or 4 after a minor stroke, day 6 or 7 after a moderate stroke, or day 12, 13, or 14 after a major stroke, whereas the earlier-treatment group started DOAC treatment within 48 hours after a minor or moderate stroke or on day 6 or 7 after a major stroke.
In terms of stroke severity, which was defined on imaging-based criteria, 37% of patients had a minor stroke, 40% had a moderate stroke, and 23% had a major stroke.
The primary outcome was a composite of recurrent ischemic stroke, systemic embolism, major extracranial bleeding, symptomatic intracranial hemorrhage, or vascular death within 30 days after randomization.
Results showed that this occurred in 2.9% in the early-treatment group and 4.1% in the later-treatment group (risk difference, –1.18 percentage points; 95% confidence interval, –2.84-0.47) by 30 days.
Recurrent ischemic stroke occurred in 1.4% in the early-treatment group and 2.5% in the later-treatment group (odds ratio, 0.57; 95% CI, 0.29-1.07). Symptomatic intracranial hemorrhage occurred in two participants (0.2%) in both groups by 30 days.
The rates of the outcomes increased only slightly more at 90 days than at 30 days, “findings that suggest there was not an excessive risk associated with early anticoagulation through that period,” the researchers report in the NEJM paper.
“Early treatment initiation can therefore be supported if indicated or if desired,” they conclude.
“The most important finding was that among 2,000 patients randomized, there was a very low rate of bleeding complications and no increase in any bleeding complication in the early DOAC group. This has been a major worry about starting anticoagulation early,” Dr. Fischer commented.
“These are very practical findings in that we can keep things simple,” Dr. Dawson added. “If the patient has a big stroke, anticoagulation with a DOAC can now be started at 6 days. For everyone else, we can start DOAC treatment as soon as possible without fear of causing harm. So, we can now confidently give patients with a minor or moderate stroke, as defined by imaging, a beneficial treatment as soon as we establish they are having an ischemic stroke and have AFib.”
Dr. Dawson pointed out that about 25% of patients with ischemic stroke are found to have AFib on admission ECG, and in another 4%-5%, AFib is found in the first 48 hours. “These are the patients we are targeting in this study.”
The researchers note that the trial did not have a statistical superiority or noninferiority design but rather aimed to estimate the treatment effects of early initiation versus later initiation of DOACs.
“This trial was slightly different in that we weren’t testing a strict statistical hypothesis because we didn’t have any data with which to formulate what sort of effect size to aim for, so we performed a qualitative trial to look at what the event rates were with the two approaches,” Dr. Fischer explained. “Our main findings are that ICH rates were not increased with early DOAC treatment and that ischemic event rates were numerically reduced, but because we didn’t have strict statistical limits, we can only say this is a high probability but not a certainty.”
Dr. Dawson added: “We can say from these results that there is a high level of probability that early DOAC treatment does not cause harm and a reasonable probability that it reduces risks of a recurrent stroke or other ischemic event.”
The researchers give an estimate of the effect size for the primary composite endpoint, which combines the major ischemic and bleeding events, ranging from a 2.8% lower risk to a 0.5% higher risk with early DOAC treatment.
“So, it is very likely that the composite endpoint would be lower,” Dr. Dawson said.
Dr. Fischer noted that a previous study (TIMING) tried to address the issue of earlier versus later anticoagulation in these patients but was stopped early after 880 patients had been enrolled because of slow recruitment.
“Results from this study failed to show superiority of early versus late DOAC treatment but they did suggest noninferiority, and they also found no increase in major bleeding complications, which is an added reassurance,” he commented.
Another trial looking at early versus late anticoagulation in these patients, OPTIMAS, is ongoing in the United Kingdom and is aiming to randomize 3,500 patients.
Imaging-based assessment of stroke severity
In the ELAN trial, the definition of stroke severity was based on imaging rather than on the National Institutes of Health Stroke Scale (NIHSS).
“We took a cautious approach by using imaging to define stroke severity. So, when using these results in clinical practice, it is important that patients are selected for the timing of DOAC treatment based on the imaging results,” Dr. Dawson explained. “This is very straightforward, as the size of the stroke can be seen clearly on the routine CT imaging that all patients receive up front. This is a very pragmatic and simple protocol. And advanced imaging is not required.”
He noted that though clinicians tend to use the NIHSS clinical symptom score to define mild, moderate, and severe stroke, the imaging approach is actually more accurate when determining the risk for bleeding and ICH. And though imaging results often correlate with NIHSS scores, there can be some exceptions.
Commenting on the ELAN trial results at the ESOC meeting, Georgios Tsivgoulis, MD, professor of neurology, University of Athens, said that the trial showed that early administration of DOACs in these patients was safe and did not increase the rate of ICH.
“There was a very low ICH rate with only two events in each group. And then there was above a 1% reduction in the composite outcome including ischemic vascular events and bleeding,” he noted.
“This is important because there are many thousands of patients with acute ischemic stroke and AFib, and now we have a large study showing we can treat them with a DOAC early, and this appears to be safe and it appears also be more effective in terms of outcome events,” Dr. Tsivgoulis said.
But he highlighted one important caveat: The majority of patients had mild or moderate stroke.
A version of this article first appeared on Medscape.com.
, a new study suggests.
The ELAN trial found that starting DOAC treatment earlier was not associated with an increased risk for intracranial hemorrhage (ICH) but rather was linked to a lower rate of ischemic events.
“We conclude that there is no reason to delay DOAC treatment in these patients. Our results suggest that early DOAC treatment is reasonable; it is unlikely to cause harm, and it is probably better at reducing ischemic events,” lead investigator of the study, Urs Fischer, MD, professor of neurology at University Hospital Basel (Switzerland), commented in an interview.
“This trial will change clinical practice in that we can feel much more reassured that starting DOAC treatment early in these patients will not cause harm,” he said.
Senior investigator Jesse Dawson, MD, professor of stroke medicine at Queen Elizabeth University Hospital, Glasgow, added: “This issue of timing of DOAC treatment causes a lot of anxiety in our daily workload. Clinicians are scared of causing an ICH, so they tend to wait. These results will ease a lot of that anxiety.”
Dr. Fischer presented the results of the ELAN trial at the European Stroke Organisation Conference (ESOC) in Munich. The trial was also simultaneously published online in The New England Journal of Medicine.
He explained that patients presenting with acute ischemic stroke who are found to have atrial fibrillation need to be started on anticoagulation to reduce the risk for a recurrent stroke. But there are no clear guidelines on when to start anticoagulation in these patients at present, with concerns that starting very early may increase the risk for hemorrhagic transformation and ICH.
Based on observations that patients with larger strokes have a higher risk for ICH in the early post-stroke period, some guidelines advise different times for starting anticoagulation for different stroke severities: 1 day for a transient ischemic attack, 3 days for a minor stroke, 6 days for a moderate stroke, and 12 days for a severe stroke – known as the 1-, 3-, 6-, 12-day rule.
“But this is not based on evidence – just on expert opinion,” Dr. Fischer noted. “The ELAN trial was conducted to obtain more solid information on optimal timing for starting anticoagulation and whether we can safely start a DOAC earlier than these guidelines currently advise.”
For the trial, which was conducted in 15 countries, 2,013 patients with an acute ischemic stroke and found to have AFib were randomly selected to start DOAC treatment earlier or later.
The later-treatment strategy followed the current approach of starting treatment at day 3 or 4 after a minor stroke, day 6 or 7 after a moderate stroke, or day 12, 13, or 14 after a major stroke, whereas the earlier-treatment group started DOAC treatment within 48 hours after a minor or moderate stroke or on day 6 or 7 after a major stroke.
In terms of stroke severity, which was defined on imaging-based criteria, 37% of patients had a minor stroke, 40% had a moderate stroke, and 23% had a major stroke.
The primary outcome was a composite of recurrent ischemic stroke, systemic embolism, major extracranial bleeding, symptomatic intracranial hemorrhage, or vascular death within 30 days after randomization.
Results showed that this occurred in 2.9% in the early-treatment group and 4.1% in the later-treatment group (risk difference, –1.18 percentage points; 95% confidence interval, –2.84-0.47) by 30 days.
Recurrent ischemic stroke occurred in 1.4% in the early-treatment group and 2.5% in the later-treatment group (odds ratio, 0.57; 95% CI, 0.29-1.07). Symptomatic intracranial hemorrhage occurred in two participants (0.2%) in both groups by 30 days.
The rates of the outcomes increased only slightly more at 90 days than at 30 days, “findings that suggest there was not an excessive risk associated with early anticoagulation through that period,” the researchers report in the NEJM paper.
“Early treatment initiation can therefore be supported if indicated or if desired,” they conclude.
“The most important finding was that among 2,000 patients randomized, there was a very low rate of bleeding complications and no increase in any bleeding complication in the early DOAC group. This has been a major worry about starting anticoagulation early,” Dr. Fischer commented.
“These are very practical findings in that we can keep things simple,” Dr. Dawson added. “If the patient has a big stroke, anticoagulation with a DOAC can now be started at 6 days. For everyone else, we can start DOAC treatment as soon as possible without fear of causing harm. So, we can now confidently give patients with a minor or moderate stroke, as defined by imaging, a beneficial treatment as soon as we establish they are having an ischemic stroke and have AFib.”
Dr. Dawson pointed out that about 25% of patients with ischemic stroke are found to have AFib on admission ECG, and in another 4%-5%, AFib is found in the first 48 hours. “These are the patients we are targeting in this study.”
The researchers note that the trial did not have a statistical superiority or noninferiority design but rather aimed to estimate the treatment effects of early initiation versus later initiation of DOACs.
“This trial was slightly different in that we weren’t testing a strict statistical hypothesis because we didn’t have any data with which to formulate what sort of effect size to aim for, so we performed a qualitative trial to look at what the event rates were with the two approaches,” Dr. Fischer explained. “Our main findings are that ICH rates were not increased with early DOAC treatment and that ischemic event rates were numerically reduced, but because we didn’t have strict statistical limits, we can only say this is a high probability but not a certainty.”
Dr. Dawson added: “We can say from these results that there is a high level of probability that early DOAC treatment does not cause harm and a reasonable probability that it reduces risks of a recurrent stroke or other ischemic event.”
The researchers give an estimate of the effect size for the primary composite endpoint, which combines the major ischemic and bleeding events, ranging from a 2.8% lower risk to a 0.5% higher risk with early DOAC treatment.
“So, it is very likely that the composite endpoint would be lower,” Dr. Dawson said.
Dr. Fischer noted that a previous study (TIMING) tried to address the issue of earlier versus later anticoagulation in these patients but was stopped early after 880 patients had been enrolled because of slow recruitment.
“Results from this study failed to show superiority of early versus late DOAC treatment but they did suggest noninferiority, and they also found no increase in major bleeding complications, which is an added reassurance,” he commented.
Another trial looking at early versus late anticoagulation in these patients, OPTIMAS, is ongoing in the United Kingdom and is aiming to randomize 3,500 patients.
Imaging-based assessment of stroke severity
In the ELAN trial, the definition of stroke severity was based on imaging rather than on the National Institutes of Health Stroke Scale (NIHSS).
“We took a cautious approach by using imaging to define stroke severity. So, when using these results in clinical practice, it is important that patients are selected for the timing of DOAC treatment based on the imaging results,” Dr. Dawson explained. “This is very straightforward, as the size of the stroke can be seen clearly on the routine CT imaging that all patients receive up front. This is a very pragmatic and simple protocol. And advanced imaging is not required.”
He noted that though clinicians tend to use the NIHSS clinical symptom score to define mild, moderate, and severe stroke, the imaging approach is actually more accurate when determining the risk for bleeding and ICH. And though imaging results often correlate with NIHSS scores, there can be some exceptions.
Commenting on the ELAN trial results at the ESOC meeting, Georgios Tsivgoulis, MD, professor of neurology, University of Athens, said that the trial showed that early administration of DOACs in these patients was safe and did not increase the rate of ICH.
“There was a very low ICH rate with only two events in each group. And then there was above a 1% reduction in the composite outcome including ischemic vascular events and bleeding,” he noted.
“This is important because there are many thousands of patients with acute ischemic stroke and AFib, and now we have a large study showing we can treat them with a DOAC early, and this appears to be safe and it appears also be more effective in terms of outcome events,” Dr. Tsivgoulis said.
But he highlighted one important caveat: The majority of patients had mild or moderate stroke.
A version of this article first appeared on Medscape.com.
, a new study suggests.
The ELAN trial found that starting DOAC treatment earlier was not associated with an increased risk for intracranial hemorrhage (ICH) but rather was linked to a lower rate of ischemic events.
“We conclude that there is no reason to delay DOAC treatment in these patients. Our results suggest that early DOAC treatment is reasonable; it is unlikely to cause harm, and it is probably better at reducing ischemic events,” lead investigator of the study, Urs Fischer, MD, professor of neurology at University Hospital Basel (Switzerland), commented in an interview.
“This trial will change clinical practice in that we can feel much more reassured that starting DOAC treatment early in these patients will not cause harm,” he said.
Senior investigator Jesse Dawson, MD, professor of stroke medicine at Queen Elizabeth University Hospital, Glasgow, added: “This issue of timing of DOAC treatment causes a lot of anxiety in our daily workload. Clinicians are scared of causing an ICH, so they tend to wait. These results will ease a lot of that anxiety.”
Dr. Fischer presented the results of the ELAN trial at the European Stroke Organisation Conference (ESOC) in Munich. The trial was also simultaneously published online in The New England Journal of Medicine.
He explained that patients presenting with acute ischemic stroke who are found to have atrial fibrillation need to be started on anticoagulation to reduce the risk for a recurrent stroke. But there are no clear guidelines on when to start anticoagulation in these patients at present, with concerns that starting very early may increase the risk for hemorrhagic transformation and ICH.
Based on observations that patients with larger strokes have a higher risk for ICH in the early post-stroke period, some guidelines advise different times for starting anticoagulation for different stroke severities: 1 day for a transient ischemic attack, 3 days for a minor stroke, 6 days for a moderate stroke, and 12 days for a severe stroke – known as the 1-, 3-, 6-, 12-day rule.
“But this is not based on evidence – just on expert opinion,” Dr. Fischer noted. “The ELAN trial was conducted to obtain more solid information on optimal timing for starting anticoagulation and whether we can safely start a DOAC earlier than these guidelines currently advise.”
For the trial, which was conducted in 15 countries, 2,013 patients with an acute ischemic stroke and found to have AFib were randomly selected to start DOAC treatment earlier or later.
The later-treatment strategy followed the current approach of starting treatment at day 3 or 4 after a minor stroke, day 6 or 7 after a moderate stroke, or day 12, 13, or 14 after a major stroke, whereas the earlier-treatment group started DOAC treatment within 48 hours after a minor or moderate stroke or on day 6 or 7 after a major stroke.
In terms of stroke severity, which was defined on imaging-based criteria, 37% of patients had a minor stroke, 40% had a moderate stroke, and 23% had a major stroke.
The primary outcome was a composite of recurrent ischemic stroke, systemic embolism, major extracranial bleeding, symptomatic intracranial hemorrhage, or vascular death within 30 days after randomization.
Results showed that this occurred in 2.9% in the early-treatment group and 4.1% in the later-treatment group (risk difference, –1.18 percentage points; 95% confidence interval, –2.84-0.47) by 30 days.
Recurrent ischemic stroke occurred in 1.4% in the early-treatment group and 2.5% in the later-treatment group (odds ratio, 0.57; 95% CI, 0.29-1.07). Symptomatic intracranial hemorrhage occurred in two participants (0.2%) in both groups by 30 days.
The rates of the outcomes increased only slightly more at 90 days than at 30 days, “findings that suggest there was not an excessive risk associated with early anticoagulation through that period,” the researchers report in the NEJM paper.
“Early treatment initiation can therefore be supported if indicated or if desired,” they conclude.
“The most important finding was that among 2,000 patients randomized, there was a very low rate of bleeding complications and no increase in any bleeding complication in the early DOAC group. This has been a major worry about starting anticoagulation early,” Dr. Fischer commented.
“These are very practical findings in that we can keep things simple,” Dr. Dawson added. “If the patient has a big stroke, anticoagulation with a DOAC can now be started at 6 days. For everyone else, we can start DOAC treatment as soon as possible without fear of causing harm. So, we can now confidently give patients with a minor or moderate stroke, as defined by imaging, a beneficial treatment as soon as we establish they are having an ischemic stroke and have AFib.”
Dr. Dawson pointed out that about 25% of patients with ischemic stroke are found to have AFib on admission ECG, and in another 4%-5%, AFib is found in the first 48 hours. “These are the patients we are targeting in this study.”
The researchers note that the trial did not have a statistical superiority or noninferiority design but rather aimed to estimate the treatment effects of early initiation versus later initiation of DOACs.
“This trial was slightly different in that we weren’t testing a strict statistical hypothesis because we didn’t have any data with which to formulate what sort of effect size to aim for, so we performed a qualitative trial to look at what the event rates were with the two approaches,” Dr. Fischer explained. “Our main findings are that ICH rates were not increased with early DOAC treatment and that ischemic event rates were numerically reduced, but because we didn’t have strict statistical limits, we can only say this is a high probability but not a certainty.”
Dr. Dawson added: “We can say from these results that there is a high level of probability that early DOAC treatment does not cause harm and a reasonable probability that it reduces risks of a recurrent stroke or other ischemic event.”
The researchers give an estimate of the effect size for the primary composite endpoint, which combines the major ischemic and bleeding events, ranging from a 2.8% lower risk to a 0.5% higher risk with early DOAC treatment.
“So, it is very likely that the composite endpoint would be lower,” Dr. Dawson said.
Dr. Fischer noted that a previous study (TIMING) tried to address the issue of earlier versus later anticoagulation in these patients but was stopped early after 880 patients had been enrolled because of slow recruitment.
“Results from this study failed to show superiority of early versus late DOAC treatment but they did suggest noninferiority, and they also found no increase in major bleeding complications, which is an added reassurance,” he commented.
Another trial looking at early versus late anticoagulation in these patients, OPTIMAS, is ongoing in the United Kingdom and is aiming to randomize 3,500 patients.
Imaging-based assessment of stroke severity
In the ELAN trial, the definition of stroke severity was based on imaging rather than on the National Institutes of Health Stroke Scale (NIHSS).
“We took a cautious approach by using imaging to define stroke severity. So, when using these results in clinical practice, it is important that patients are selected for the timing of DOAC treatment based on the imaging results,” Dr. Dawson explained. “This is very straightforward, as the size of the stroke can be seen clearly on the routine CT imaging that all patients receive up front. This is a very pragmatic and simple protocol. And advanced imaging is not required.”
He noted that though clinicians tend to use the NIHSS clinical symptom score to define mild, moderate, and severe stroke, the imaging approach is actually more accurate when determining the risk for bleeding and ICH. And though imaging results often correlate with NIHSS scores, there can be some exceptions.
Commenting on the ELAN trial results at the ESOC meeting, Georgios Tsivgoulis, MD, professor of neurology, University of Athens, said that the trial showed that early administration of DOACs in these patients was safe and did not increase the rate of ICH.
“There was a very low ICH rate with only two events in each group. And then there was above a 1% reduction in the composite outcome including ischemic vascular events and bleeding,” he noted.
“This is important because there are many thousands of patients with acute ischemic stroke and AFib, and now we have a large study showing we can treat them with a DOAC early, and this appears to be safe and it appears also be more effective in terms of outcome events,” Dr. Tsivgoulis said.
But he highlighted one important caveat: The majority of patients had mild or moderate stroke.
A version of this article first appeared on Medscape.com.
FROM ESOC 2023
Losing weight may bolster AFib ablation’s chances for success: LEAF interim results
, a new analysis suggests.
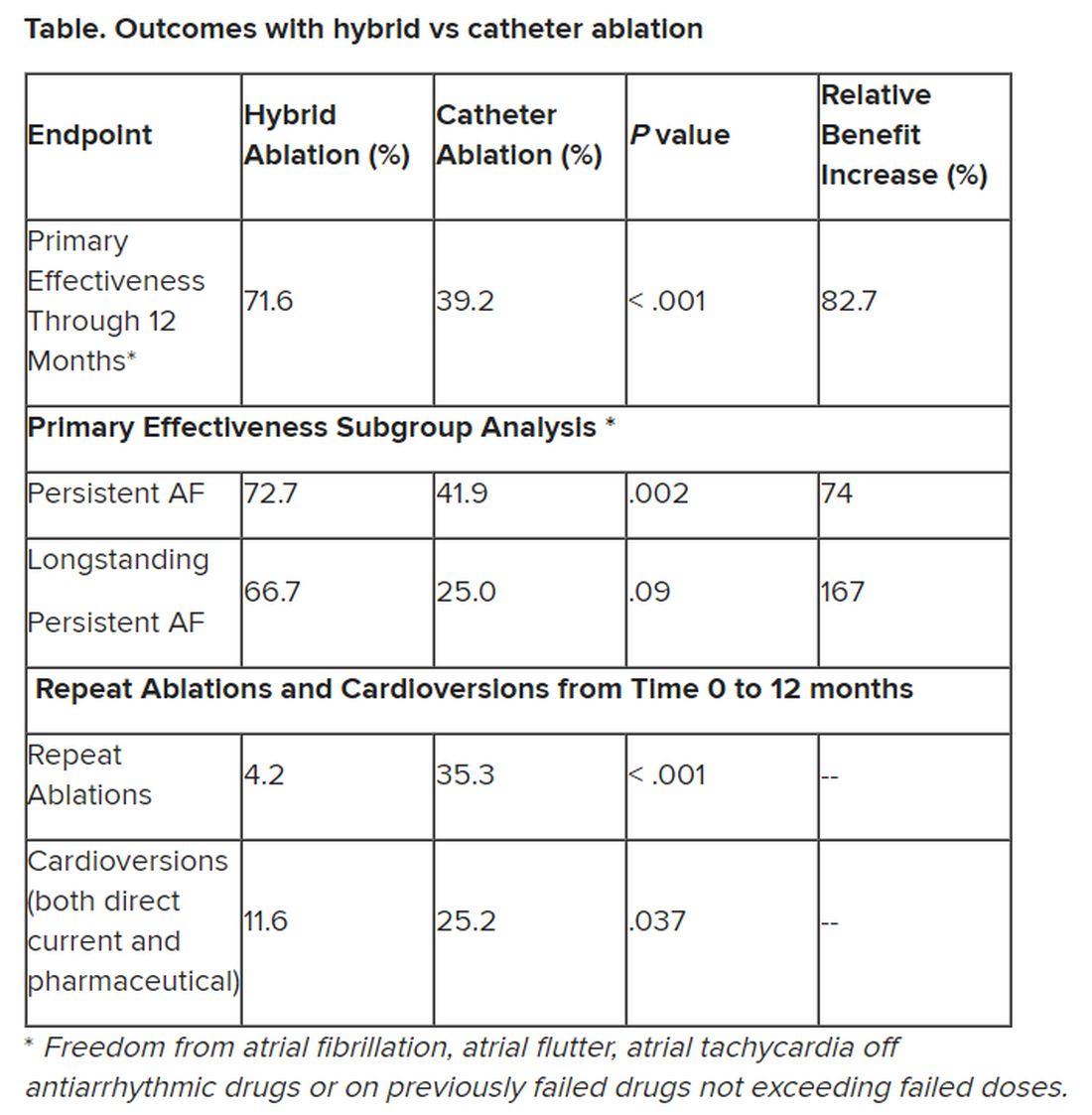
The finding comes from a small study that entered such patients with paroxysmal and especially persistent AFib who were candidates for ablation. Those shedding at least 3% of body weight in the months before the procedure while engaged in a structured risk-factor modification (RFM) program were “dramatically” more likely to be AFib-free 6 months later.
The improved ablation efficacy, compared with results in similar patients who didn’t lose as much weight, was most pronounced among those whose AFib had been the persistent form, reported investigators at the annual scientific sessions of the Heart Rhythm Society, held in New Orleans.
Of note, ablations in the study were consistently limited, as much as possible, to standard pulmonary-vein isolation (PVI).
Associations between AFib and obesity and other behavioral and lifestyle-related risk factors are well recognized, but the limited studies of their effect on AFib ablation success have been inconsistent. The current analysis, the group says, points specifically to preablation weight loss as means to improving AFib-ablation outcomes.
“Adjunctive therapy focused on weight loss should be incorporated in the treatment plan for obese patients undergoing ablation for atrial fibrillation,” Jeffrey J. Goldberger, MD, MBA, of the University of Miami, said when presenting the new results at the HRS sessions.
Such a plan is entirely consistent with recent guidelines and especially a 2020 American Heart Association (AHA) consensus statement, but is inconsistently and perhaps even seldom realized in clinical practice.
Dramatic increase in success
Even modest weight loss before ablation may help, proposed Dr. Goldberger, who directs his institution’s Center for Atrial Fibrillation. Decreases for the greater-weight-loss group actually averaged less than 6% of baseline body weight.
Yet it was apparently enough to improve ablation outcomes significantly: Eighty-eight percent were free of AFib 6 months after the procedure, compared with 61% for patients who lost less than 3% of their preablation weight.
For improving ablation success, he said, “We’re talking about a moderate amount of weight loss. These patients are not going from being obese to being thin. They’re still quite overweight.”
In an analysis limited to the four-fifths of patients with persistent AFib, “we saw the same pattern,” Dr. Goldberger said at a media presentation prior to his formal report at the HRS sessions.
Moreover, that subgroup’s benefit persisted out to 12 months, at which time 42% and 81% of patients with less and greater weight loss, respectively, were free of AFib. That represents, he said, “a really tremendous – dramatic, actually – increase in success of pulmonary vein isolation in those who lost weight.”
“We’ve known for a long time that weight loss is important for preventing atrial fibrillation or increasing the success rates of the different treatments we use,” Cynthia M. Tracy, MD, said in an interview. “Probably in some studies, weight loss has been as effective as antiarrhythmics.”
A loss of 3% body weight “is not a lot,” she said. In the current analysis, “It’s notable that it made that much difference with even a fairly modest amount of weight loss.”
Now when asked, “ ‘How much do I have to lose before you’ll consider doing my ablation?’ we have a bit more concrete data to give patients and doctors as to what amount might be beneficial,” said Dr. Tracy of George Washington University Hospital, Washington, who is not associated with the study.
Evolving view of AFib
The findings are emblematic of the profession’s evolving view of AFib and its management, Dr. Goldberger observed at the press conference. Should clinicians think of AFib as similar to “a disease like Wolff-Parkinson-White syndrome,” in which the patient usually has a successful ablation, and then “we expect that to last in perpetuity with no further interventions?”
Or, he said, “is atrial fibrillation more a disease like coronary artery disease, where even if they have an intervention, the disease process is still ongoing and requires long-term disease management? I think it’s pretty clear that we’re dealing with the latter case.”
Dr. Goldberger’s report was an interim analysis of an ongoing randomized trial called LEAF (Liraglutide Effect on Atrial Fibrillation), which is comparing patients with AFib assigned to “take” vs. “not take” the GLP-1 receptor agonist liraglutide, an antidiabetic (Victoza) and weight-loss (Saxenda) drug. The trial aims to assess the drug’s apparent ability to shrink atrial epicardial adipose tissue which, Dr. Goldberger said, is thought to contribute to AFib development and influence AFib-ablation outcomes.
It’s unknown and a limitation of the current analysis, he said, whether the observed link between improved preablation–weight ablation success “is specifically related to weight loss, liraglutide treatment, or both.”
As the invited discussant for Dr. Goldberger’s presentation, David Frankel, MD, observed that studies have been inconsistent on whether substantial weight loss may improve the results of AFib rhythm-control therapy.
Those finding such an association, including LEAF and the influential LEGACY study, differed from others showing a null effect by including “a comprehensive risk factor management” program, observed Dr. Frankel, of the Hospital of the University of Pennsylvania and Penn Heart and Vascular Center, Philadelphia.
Rather than focusing solely on weight loss or sleep apnea as AFib risk factors, he said, the studies linking weight loss to AFib rhythm control also included “hypertension, diabetes, hyperlipidemia, smoking cessation, and alcohol reduction,” Dr. Frankel said. “So it seems clear that to significantly impact AF recurrence, we need to focus on all these contributors to metabolic syndrome.”
Comprehensive risk-factor management
LEAF entered patients with AFib, 79% of whom had persistent AF and the rest paroxysmal AF, who followed the RFM program and were randomly assigned also to take liraglutide or placebo. The “nurse-practitioner-led” RFM program, conducted both in-clinic and online, featured “established goals for each patient” using AHA diet and lifestyle recommendations, an exercise prescription, dietary counseling, evaluation and treatment of sleep apnea, and measures to control any diabetes, hyperlipidemia, or hypertension, Dr. Goldberger said. And patients “were counseled on alcohol reduction and smoking cessation as necessary.”
After 3 months, 29 and 30 patients – regardless of randomization assignment – had lost < 3% and at least 3% of baseline body weight, respectively.
Catheter ablation achieved PVI in all patients. A 3-month blanking period followed, after which they went off antiarrhythmic meds.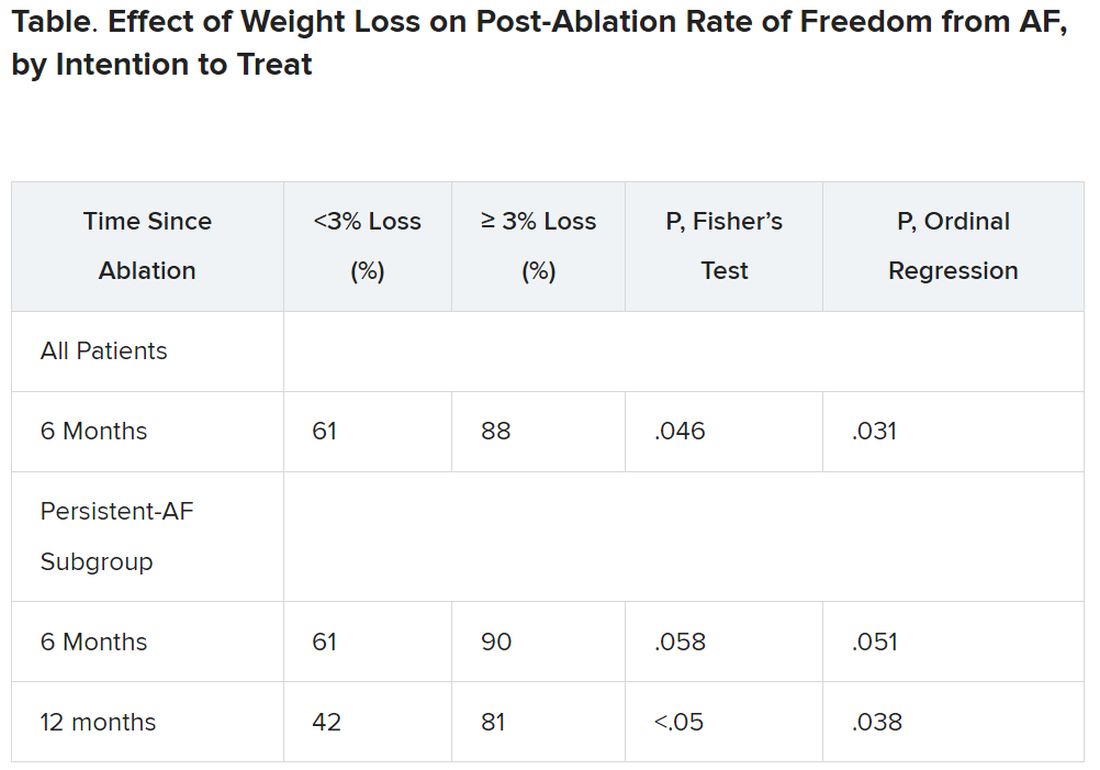
It’s very difficult for patients to lose 10% or more of body weight, “and it would not happen overnight,” Dr. Tracy observed. “These are symptomatic patients, for the most part, if they get referred to an electrophysiologist. So you don’t want to defer them indefinitely.”
The current findings, she said, point to “a more realistic target,” suggesting that weight loss of at least 3% should improve AFib ablation’s chances for success.
Dr. Goldberger disclosed ties to Medtronic. Dr. Frankel disclosed ties to Medtronic, Stryker, Biosense Webster, and Boston Scientific. Dr. Tracy reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new analysis suggests.
The finding comes from a small study that entered such patients with paroxysmal and especially persistent AFib who were candidates for ablation. Those shedding at least 3% of body weight in the months before the procedure while engaged in a structured risk-factor modification (RFM) program were “dramatically” more likely to be AFib-free 6 months later.
The improved ablation efficacy, compared with results in similar patients who didn’t lose as much weight, was most pronounced among those whose AFib had been the persistent form, reported investigators at the annual scientific sessions of the Heart Rhythm Society, held in New Orleans.
Of note, ablations in the study were consistently limited, as much as possible, to standard pulmonary-vein isolation (PVI).
Associations between AFib and obesity and other behavioral and lifestyle-related risk factors are well recognized, but the limited studies of their effect on AFib ablation success have been inconsistent. The current analysis, the group says, points specifically to preablation weight loss as means to improving AFib-ablation outcomes.
“Adjunctive therapy focused on weight loss should be incorporated in the treatment plan for obese patients undergoing ablation for atrial fibrillation,” Jeffrey J. Goldberger, MD, MBA, of the University of Miami, said when presenting the new results at the HRS sessions.
Such a plan is entirely consistent with recent guidelines and especially a 2020 American Heart Association (AHA) consensus statement, but is inconsistently and perhaps even seldom realized in clinical practice.
Dramatic increase in success
Even modest weight loss before ablation may help, proposed Dr. Goldberger, who directs his institution’s Center for Atrial Fibrillation. Decreases for the greater-weight-loss group actually averaged less than 6% of baseline body weight.
Yet it was apparently enough to improve ablation outcomes significantly: Eighty-eight percent were free of AFib 6 months after the procedure, compared with 61% for patients who lost less than 3% of their preablation weight.
For improving ablation success, he said, “We’re talking about a moderate amount of weight loss. These patients are not going from being obese to being thin. They’re still quite overweight.”
In an analysis limited to the four-fifths of patients with persistent AFib, “we saw the same pattern,” Dr. Goldberger said at a media presentation prior to his formal report at the HRS sessions.
Moreover, that subgroup’s benefit persisted out to 12 months, at which time 42% and 81% of patients with less and greater weight loss, respectively, were free of AFib. That represents, he said, “a really tremendous – dramatic, actually – increase in success of pulmonary vein isolation in those who lost weight.”
“We’ve known for a long time that weight loss is important for preventing atrial fibrillation or increasing the success rates of the different treatments we use,” Cynthia M. Tracy, MD, said in an interview. “Probably in some studies, weight loss has been as effective as antiarrhythmics.”
A loss of 3% body weight “is not a lot,” she said. In the current analysis, “It’s notable that it made that much difference with even a fairly modest amount of weight loss.”
Now when asked, “ ‘How much do I have to lose before you’ll consider doing my ablation?’ we have a bit more concrete data to give patients and doctors as to what amount might be beneficial,” said Dr. Tracy of George Washington University Hospital, Washington, who is not associated with the study.
Evolving view of AFib
The findings are emblematic of the profession’s evolving view of AFib and its management, Dr. Goldberger observed at the press conference. Should clinicians think of AFib as similar to “a disease like Wolff-Parkinson-White syndrome,” in which the patient usually has a successful ablation, and then “we expect that to last in perpetuity with no further interventions?”
Or, he said, “is atrial fibrillation more a disease like coronary artery disease, where even if they have an intervention, the disease process is still ongoing and requires long-term disease management? I think it’s pretty clear that we’re dealing with the latter case.”
Dr. Goldberger’s report was an interim analysis of an ongoing randomized trial called LEAF (Liraglutide Effect on Atrial Fibrillation), which is comparing patients with AFib assigned to “take” vs. “not take” the GLP-1 receptor agonist liraglutide, an antidiabetic (Victoza) and weight-loss (Saxenda) drug. The trial aims to assess the drug’s apparent ability to shrink atrial epicardial adipose tissue which, Dr. Goldberger said, is thought to contribute to AFib development and influence AFib-ablation outcomes.
It’s unknown and a limitation of the current analysis, he said, whether the observed link between improved preablation–weight ablation success “is specifically related to weight loss, liraglutide treatment, or both.”
As the invited discussant for Dr. Goldberger’s presentation, David Frankel, MD, observed that studies have been inconsistent on whether substantial weight loss may improve the results of AFib rhythm-control therapy.
Those finding such an association, including LEAF and the influential LEGACY study, differed from others showing a null effect by including “a comprehensive risk factor management” program, observed Dr. Frankel, of the Hospital of the University of Pennsylvania and Penn Heart and Vascular Center, Philadelphia.
Rather than focusing solely on weight loss or sleep apnea as AFib risk factors, he said, the studies linking weight loss to AFib rhythm control also included “hypertension, diabetes, hyperlipidemia, smoking cessation, and alcohol reduction,” Dr. Frankel said. “So it seems clear that to significantly impact AF recurrence, we need to focus on all these contributors to metabolic syndrome.”
Comprehensive risk-factor management
LEAF entered patients with AFib, 79% of whom had persistent AF and the rest paroxysmal AF, who followed the RFM program and were randomly assigned also to take liraglutide or placebo. The “nurse-practitioner-led” RFM program, conducted both in-clinic and online, featured “established goals for each patient” using AHA diet and lifestyle recommendations, an exercise prescription, dietary counseling, evaluation and treatment of sleep apnea, and measures to control any diabetes, hyperlipidemia, or hypertension, Dr. Goldberger said. And patients “were counseled on alcohol reduction and smoking cessation as necessary.”
After 3 months, 29 and 30 patients – regardless of randomization assignment – had lost < 3% and at least 3% of baseline body weight, respectively.
Catheter ablation achieved PVI in all patients. A 3-month blanking period followed, after which they went off antiarrhythmic meds.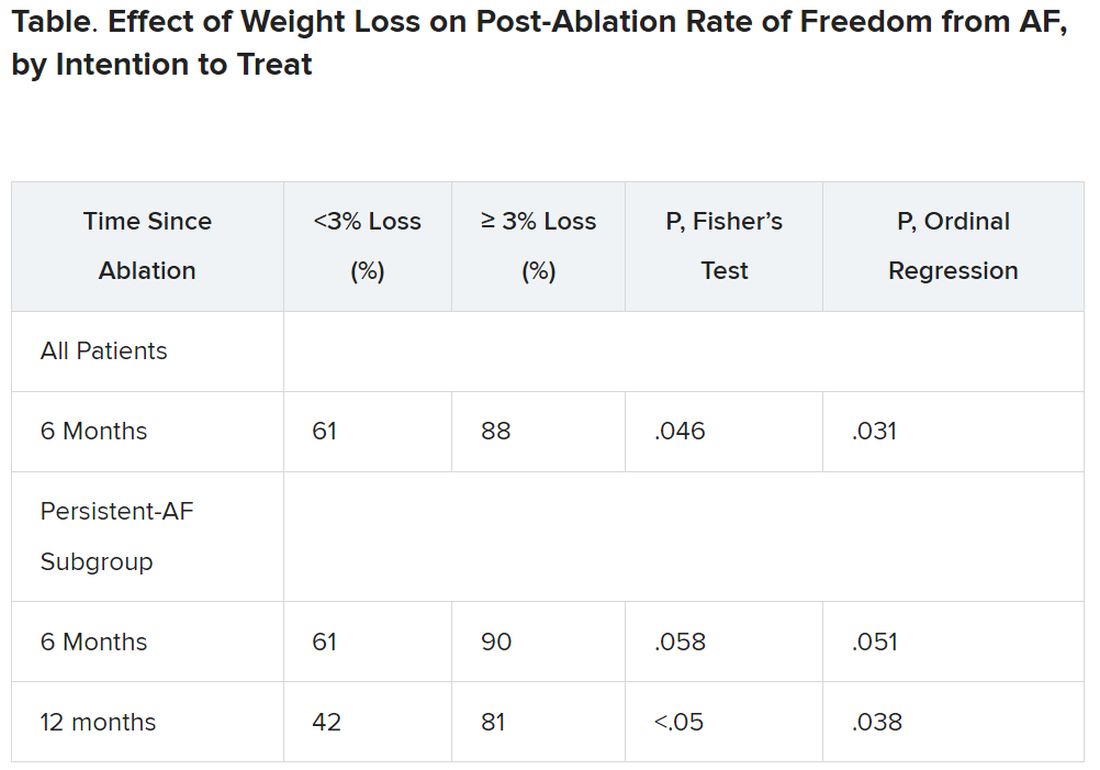
It’s very difficult for patients to lose 10% or more of body weight, “and it would not happen overnight,” Dr. Tracy observed. “These are symptomatic patients, for the most part, if they get referred to an electrophysiologist. So you don’t want to defer them indefinitely.”
The current findings, she said, point to “a more realistic target,” suggesting that weight loss of at least 3% should improve AFib ablation’s chances for success.
Dr. Goldberger disclosed ties to Medtronic. Dr. Frankel disclosed ties to Medtronic, Stryker, Biosense Webster, and Boston Scientific. Dr. Tracy reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new analysis suggests.
The finding comes from a small study that entered such patients with paroxysmal and especially persistent AFib who were candidates for ablation. Those shedding at least 3% of body weight in the months before the procedure while engaged in a structured risk-factor modification (RFM) program were “dramatically” more likely to be AFib-free 6 months later.
The improved ablation efficacy, compared with results in similar patients who didn’t lose as much weight, was most pronounced among those whose AFib had been the persistent form, reported investigators at the annual scientific sessions of the Heart Rhythm Society, held in New Orleans.
Of note, ablations in the study were consistently limited, as much as possible, to standard pulmonary-vein isolation (PVI).
Associations between AFib and obesity and other behavioral and lifestyle-related risk factors are well recognized, but the limited studies of their effect on AFib ablation success have been inconsistent. The current analysis, the group says, points specifically to preablation weight loss as means to improving AFib-ablation outcomes.
“Adjunctive therapy focused on weight loss should be incorporated in the treatment plan for obese patients undergoing ablation for atrial fibrillation,” Jeffrey J. Goldberger, MD, MBA, of the University of Miami, said when presenting the new results at the HRS sessions.
Such a plan is entirely consistent with recent guidelines and especially a 2020 American Heart Association (AHA) consensus statement, but is inconsistently and perhaps even seldom realized in clinical practice.
Dramatic increase in success
Even modest weight loss before ablation may help, proposed Dr. Goldberger, who directs his institution’s Center for Atrial Fibrillation. Decreases for the greater-weight-loss group actually averaged less than 6% of baseline body weight.
Yet it was apparently enough to improve ablation outcomes significantly: Eighty-eight percent were free of AFib 6 months after the procedure, compared with 61% for patients who lost less than 3% of their preablation weight.
For improving ablation success, he said, “We’re talking about a moderate amount of weight loss. These patients are not going from being obese to being thin. They’re still quite overweight.”
In an analysis limited to the four-fifths of patients with persistent AFib, “we saw the same pattern,” Dr. Goldberger said at a media presentation prior to his formal report at the HRS sessions.
Moreover, that subgroup’s benefit persisted out to 12 months, at which time 42% and 81% of patients with less and greater weight loss, respectively, were free of AFib. That represents, he said, “a really tremendous – dramatic, actually – increase in success of pulmonary vein isolation in those who lost weight.”
“We’ve known for a long time that weight loss is important for preventing atrial fibrillation or increasing the success rates of the different treatments we use,” Cynthia M. Tracy, MD, said in an interview. “Probably in some studies, weight loss has been as effective as antiarrhythmics.”
A loss of 3% body weight “is not a lot,” she said. In the current analysis, “It’s notable that it made that much difference with even a fairly modest amount of weight loss.”
Now when asked, “ ‘How much do I have to lose before you’ll consider doing my ablation?’ we have a bit more concrete data to give patients and doctors as to what amount might be beneficial,” said Dr. Tracy of George Washington University Hospital, Washington, who is not associated with the study.
Evolving view of AFib
The findings are emblematic of the profession’s evolving view of AFib and its management, Dr. Goldberger observed at the press conference. Should clinicians think of AFib as similar to “a disease like Wolff-Parkinson-White syndrome,” in which the patient usually has a successful ablation, and then “we expect that to last in perpetuity with no further interventions?”
Or, he said, “is atrial fibrillation more a disease like coronary artery disease, where even if they have an intervention, the disease process is still ongoing and requires long-term disease management? I think it’s pretty clear that we’re dealing with the latter case.”
Dr. Goldberger’s report was an interim analysis of an ongoing randomized trial called LEAF (Liraglutide Effect on Atrial Fibrillation), which is comparing patients with AFib assigned to “take” vs. “not take” the GLP-1 receptor agonist liraglutide, an antidiabetic (Victoza) and weight-loss (Saxenda) drug. The trial aims to assess the drug’s apparent ability to shrink atrial epicardial adipose tissue which, Dr. Goldberger said, is thought to contribute to AFib development and influence AFib-ablation outcomes.
It’s unknown and a limitation of the current analysis, he said, whether the observed link between improved preablation–weight ablation success “is specifically related to weight loss, liraglutide treatment, or both.”
As the invited discussant for Dr. Goldberger’s presentation, David Frankel, MD, observed that studies have been inconsistent on whether substantial weight loss may improve the results of AFib rhythm-control therapy.
Those finding such an association, including LEAF and the influential LEGACY study, differed from others showing a null effect by including “a comprehensive risk factor management” program, observed Dr. Frankel, of the Hospital of the University of Pennsylvania and Penn Heart and Vascular Center, Philadelphia.
Rather than focusing solely on weight loss or sleep apnea as AFib risk factors, he said, the studies linking weight loss to AFib rhythm control also included “hypertension, diabetes, hyperlipidemia, smoking cessation, and alcohol reduction,” Dr. Frankel said. “So it seems clear that to significantly impact AF recurrence, we need to focus on all these contributors to metabolic syndrome.”
Comprehensive risk-factor management
LEAF entered patients with AFib, 79% of whom had persistent AF and the rest paroxysmal AF, who followed the RFM program and were randomly assigned also to take liraglutide or placebo. The “nurse-practitioner-led” RFM program, conducted both in-clinic and online, featured “established goals for each patient” using AHA diet and lifestyle recommendations, an exercise prescription, dietary counseling, evaluation and treatment of sleep apnea, and measures to control any diabetes, hyperlipidemia, or hypertension, Dr. Goldberger said. And patients “were counseled on alcohol reduction and smoking cessation as necessary.”
After 3 months, 29 and 30 patients – regardless of randomization assignment – had lost < 3% and at least 3% of baseline body weight, respectively.
Catheter ablation achieved PVI in all patients. A 3-month blanking period followed, after which they went off antiarrhythmic meds.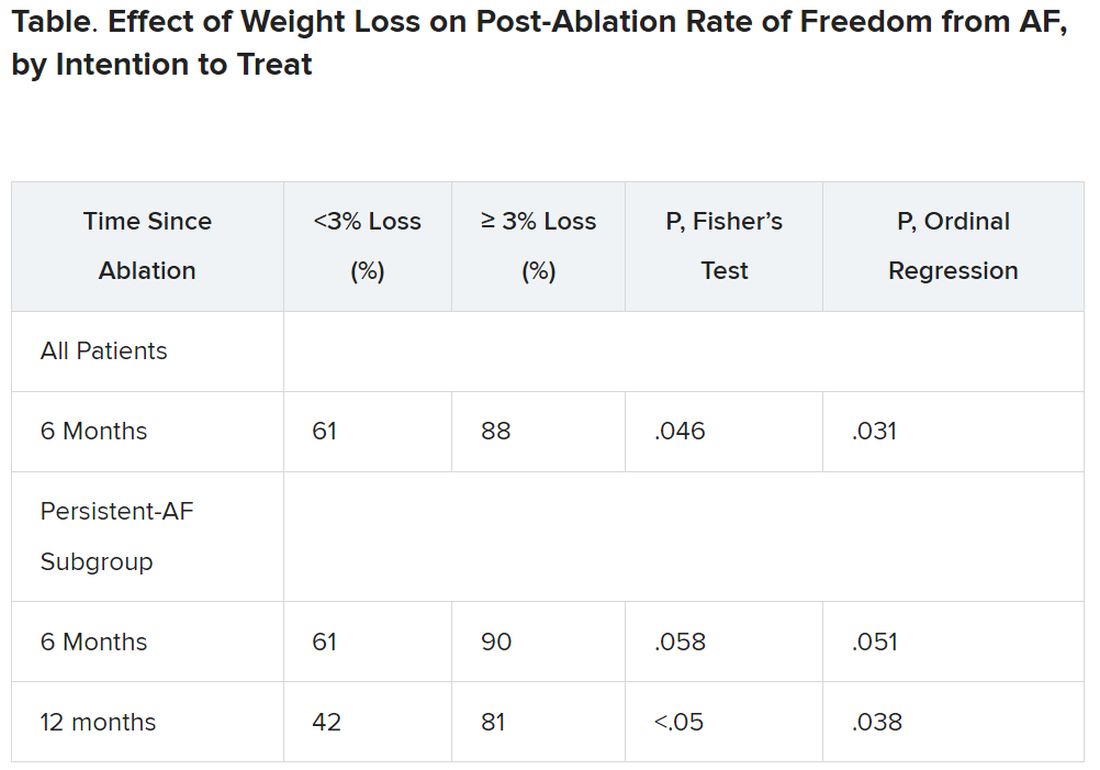
It’s very difficult for patients to lose 10% or more of body weight, “and it would not happen overnight,” Dr. Tracy observed. “These are symptomatic patients, for the most part, if they get referred to an electrophysiologist. So you don’t want to defer them indefinitely.”
The current findings, she said, point to “a more realistic target,” suggesting that weight loss of at least 3% should improve AFib ablation’s chances for success.
Dr. Goldberger disclosed ties to Medtronic. Dr. Frankel disclosed ties to Medtronic, Stryker, Biosense Webster, and Boston Scientific. Dr. Tracy reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HEART RHYTHM 2023
Surprisingly more nonsustained VT shown in HCM using extended ECG monitoring
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EHRA
LAA closure outcomes improve with CCTA: Swiss-Apero subanalysis
The largest multicenter randomized trial to date of CT angiography before left atrial appendage closure (LAAC) to treat atrial fibrillation has added to the evidence that the imaging technique on top of transesophageal echocardiography achieves a higher degree of short- and long-term success than TEE alone.
The results are from a subanalysis of the Swiss-Apero trial, a randomized comparative trial of the Watchman and Amulet devices for LAAC, which published results in Circulation.
“Our observational data support to use of CT for LAAC procedure planning,” senior investigator Lorenz Räber, MD, PhD, said in an interview. “This is not very surprising given the high variability of the LAA anatomy and the associated complexity of the procedure.” Dr. Räber is director of the catheterization laboratory at Inselspital, Bern (Switzerland) University Hospital.
The study, published online in JACC: Cardiovascular Interventions, included 219 LAAC procedures in which the operators performed coronary CT angiography (CTTA) beforehand. When the investigators designed the study, LAAC procedures were typically planned using TEE alone, and so participating operators were blinded to preprocedural CCTA imaging. Soon after the study launch, European cardiology societies issued a consensus statement that included CCTA as an option for procedure planning. So the Swiss-Apero investigators changed the subanalysis protocol to unblind the operators – that is, they were permitted to plan LAAC procedures with CCTA imaging in addition to TEE. In this subanalysis, most patients had implantation with blinding to CCTA (57.9% vs. 41.2%).
Study results
The subanalysis determined that operator unblinding to preprocedural CCTA resulted in better success with LAAC, both in the short term, at 93.5% vs. 81.1% (P = .009; adjusted odds ratio, 2.76; 95% confidence interval, 1.05-7.29; P = .40) and the long term, at 83.7% vs. 72.4% (P = .050; aOR, 2.12; 95% CI, 1.03-4.35; P = .041).
Dr. Räber noted that this is only the third study to date that examined the potential impact of preprocedural CCTA plus TEE. One was a small study of 24 consecutive LAAC procedures with the Watchman device that compared TEE alone and CCTA plus TEE, finding better outcomes in the group that had both imaging modalities . A larger, single-center cohort study of 485 LAAC Watchman procedures found that CCTA resulted in faster operation times and higher successful device implantation rates, but no significant difference in procedural complications.
Dr. Räber explained why his group’s subanalysis may have found a clinical benefit with CCTA on top of TEE. “Our study was much larger, as compared to the randomized clinical trial, and there was no selection bias as in the second study mentioned before, as operators did not have the option to decide whether or not to assess the CCTA prior to the procedure,” he said. “Finally, in the previous studies there was no random allocation of device type” – that is, Amulet versus Watchman.
One study limitation Dr. Räber noted was that significantly more patients in the blinded group were discharged with dual-antiplatelet therapy. “The lower rate of procedure complications observed in unblinded procedures was mostly driven by a lower number of major bleedings and in particular of pericardial tamponade,” he said. “We cannot therefore exclude that the higher percentage of patients under dual-antiplatelet therapy in the CCTA-blinded group might have favored this difference.”
However, he noted the investigators corrected their analysis to account for differences between the groups. “Importantly, the numerical excess in major procedural bleeding was observed within both the single-antiplatelet therapy and dual-antiplatelet therapy subgroups of the TEE-only group.”
In an accompanying editorial, coauthors Brian O’Neill, MD, and Dee Dee Wang, MD, both with the Center for Structural Heard Disease at Henry Ford Hospital in Detroit, noted that the Swiss-Apero subanalysis “reinforced” the benefit of CCTA before LAAC.
“This study demonstrated, for the first time, improved short- and long-term procedural success using CT in addition to TEE for left atrial appendage occlusion,” Dr. O’Neill said in an interview. “This particular study may serve as a guide to an adequately powered randomized trial of CT versus TEE in left atrial appendage occlusion.” Future LAAC trials should incorporate preprocedural CCTA.
Dr. O’Neill noted that, as a subanalysis of a randomized trial, the “results are hypothesis generating.” However, he added, “the results are in line with several previous studies of CT versus TEE in left atrial appendage occlusion.”
Dr Räber disclosed financial relationships with Abbott Vascular, Boston Scientific, Biotronik, Infraredx, Heartflow, Sanofi, Regeneron, Amgen, AstraZeneca, CSL Behring, Canon, Occlutech, and Vifor. Dr. O’Neill disclosed financial relationships with Edwards Lifesciences, Medtronic, and Abbott Vascular.
The largest multicenter randomized trial to date of CT angiography before left atrial appendage closure (LAAC) to treat atrial fibrillation has added to the evidence that the imaging technique on top of transesophageal echocardiography achieves a higher degree of short- and long-term success than TEE alone.
The results are from a subanalysis of the Swiss-Apero trial, a randomized comparative trial of the Watchman and Amulet devices for LAAC, which published results in Circulation.
“Our observational data support to use of CT for LAAC procedure planning,” senior investigator Lorenz Räber, MD, PhD, said in an interview. “This is not very surprising given the high variability of the LAA anatomy and the associated complexity of the procedure.” Dr. Räber is director of the catheterization laboratory at Inselspital, Bern (Switzerland) University Hospital.
The study, published online in JACC: Cardiovascular Interventions, included 219 LAAC procedures in which the operators performed coronary CT angiography (CTTA) beforehand. When the investigators designed the study, LAAC procedures were typically planned using TEE alone, and so participating operators were blinded to preprocedural CCTA imaging. Soon after the study launch, European cardiology societies issued a consensus statement that included CCTA as an option for procedure planning. So the Swiss-Apero investigators changed the subanalysis protocol to unblind the operators – that is, they were permitted to plan LAAC procedures with CCTA imaging in addition to TEE. In this subanalysis, most patients had implantation with blinding to CCTA (57.9% vs. 41.2%).
Study results
The subanalysis determined that operator unblinding to preprocedural CCTA resulted in better success with LAAC, both in the short term, at 93.5% vs. 81.1% (P = .009; adjusted odds ratio, 2.76; 95% confidence interval, 1.05-7.29; P = .40) and the long term, at 83.7% vs. 72.4% (P = .050; aOR, 2.12; 95% CI, 1.03-4.35; P = .041).
Dr. Räber noted that this is only the third study to date that examined the potential impact of preprocedural CCTA plus TEE. One was a small study of 24 consecutive LAAC procedures with the Watchman device that compared TEE alone and CCTA plus TEE, finding better outcomes in the group that had both imaging modalities . A larger, single-center cohort study of 485 LAAC Watchman procedures found that CCTA resulted in faster operation times and higher successful device implantation rates, but no significant difference in procedural complications.
Dr. Räber explained why his group’s subanalysis may have found a clinical benefit with CCTA on top of TEE. “Our study was much larger, as compared to the randomized clinical trial, and there was no selection bias as in the second study mentioned before, as operators did not have the option to decide whether or not to assess the CCTA prior to the procedure,” he said. “Finally, in the previous studies there was no random allocation of device type” – that is, Amulet versus Watchman.
One study limitation Dr. Räber noted was that significantly more patients in the blinded group were discharged with dual-antiplatelet therapy. “The lower rate of procedure complications observed in unblinded procedures was mostly driven by a lower number of major bleedings and in particular of pericardial tamponade,” he said. “We cannot therefore exclude that the higher percentage of patients under dual-antiplatelet therapy in the CCTA-blinded group might have favored this difference.”
However, he noted the investigators corrected their analysis to account for differences between the groups. “Importantly, the numerical excess in major procedural bleeding was observed within both the single-antiplatelet therapy and dual-antiplatelet therapy subgroups of the TEE-only group.”
In an accompanying editorial, coauthors Brian O’Neill, MD, and Dee Dee Wang, MD, both with the Center for Structural Heard Disease at Henry Ford Hospital in Detroit, noted that the Swiss-Apero subanalysis “reinforced” the benefit of CCTA before LAAC.
“This study demonstrated, for the first time, improved short- and long-term procedural success using CT in addition to TEE for left atrial appendage occlusion,” Dr. O’Neill said in an interview. “This particular study may serve as a guide to an adequately powered randomized trial of CT versus TEE in left atrial appendage occlusion.” Future LAAC trials should incorporate preprocedural CCTA.
Dr. O’Neill noted that, as a subanalysis of a randomized trial, the “results are hypothesis generating.” However, he added, “the results are in line with several previous studies of CT versus TEE in left atrial appendage occlusion.”
Dr Räber disclosed financial relationships with Abbott Vascular, Boston Scientific, Biotronik, Infraredx, Heartflow, Sanofi, Regeneron, Amgen, AstraZeneca, CSL Behring, Canon, Occlutech, and Vifor. Dr. O’Neill disclosed financial relationships with Edwards Lifesciences, Medtronic, and Abbott Vascular.
The largest multicenter randomized trial to date of CT angiography before left atrial appendage closure (LAAC) to treat atrial fibrillation has added to the evidence that the imaging technique on top of transesophageal echocardiography achieves a higher degree of short- and long-term success than TEE alone.
The results are from a subanalysis of the Swiss-Apero trial, a randomized comparative trial of the Watchman and Amulet devices for LAAC, which published results in Circulation.
“Our observational data support to use of CT for LAAC procedure planning,” senior investigator Lorenz Räber, MD, PhD, said in an interview. “This is not very surprising given the high variability of the LAA anatomy and the associated complexity of the procedure.” Dr. Räber is director of the catheterization laboratory at Inselspital, Bern (Switzerland) University Hospital.
The study, published online in JACC: Cardiovascular Interventions, included 219 LAAC procedures in which the operators performed coronary CT angiography (CTTA) beforehand. When the investigators designed the study, LAAC procedures were typically planned using TEE alone, and so participating operators were blinded to preprocedural CCTA imaging. Soon after the study launch, European cardiology societies issued a consensus statement that included CCTA as an option for procedure planning. So the Swiss-Apero investigators changed the subanalysis protocol to unblind the operators – that is, they were permitted to plan LAAC procedures with CCTA imaging in addition to TEE. In this subanalysis, most patients had implantation with blinding to CCTA (57.9% vs. 41.2%).
Study results
The subanalysis determined that operator unblinding to preprocedural CCTA resulted in better success with LAAC, both in the short term, at 93.5% vs. 81.1% (P = .009; adjusted odds ratio, 2.76; 95% confidence interval, 1.05-7.29; P = .40) and the long term, at 83.7% vs. 72.4% (P = .050; aOR, 2.12; 95% CI, 1.03-4.35; P = .041).
Dr. Räber noted that this is only the third study to date that examined the potential impact of preprocedural CCTA plus TEE. One was a small study of 24 consecutive LAAC procedures with the Watchman device that compared TEE alone and CCTA plus TEE, finding better outcomes in the group that had both imaging modalities . A larger, single-center cohort study of 485 LAAC Watchman procedures found that CCTA resulted in faster operation times and higher successful device implantation rates, but no significant difference in procedural complications.
Dr. Räber explained why his group’s subanalysis may have found a clinical benefit with CCTA on top of TEE. “Our study was much larger, as compared to the randomized clinical trial, and there was no selection bias as in the second study mentioned before, as operators did not have the option to decide whether or not to assess the CCTA prior to the procedure,” he said. “Finally, in the previous studies there was no random allocation of device type” – that is, Amulet versus Watchman.
One study limitation Dr. Räber noted was that significantly more patients in the blinded group were discharged with dual-antiplatelet therapy. “The lower rate of procedure complications observed in unblinded procedures was mostly driven by a lower number of major bleedings and in particular of pericardial tamponade,” he said. “We cannot therefore exclude that the higher percentage of patients under dual-antiplatelet therapy in the CCTA-blinded group might have favored this difference.”
However, he noted the investigators corrected their analysis to account for differences between the groups. “Importantly, the numerical excess in major procedural bleeding was observed within both the single-antiplatelet therapy and dual-antiplatelet therapy subgroups of the TEE-only group.”
In an accompanying editorial, coauthors Brian O’Neill, MD, and Dee Dee Wang, MD, both with the Center for Structural Heard Disease at Henry Ford Hospital in Detroit, noted that the Swiss-Apero subanalysis “reinforced” the benefit of CCTA before LAAC.
“This study demonstrated, for the first time, improved short- and long-term procedural success using CT in addition to TEE for left atrial appendage occlusion,” Dr. O’Neill said in an interview. “This particular study may serve as a guide to an adequately powered randomized trial of CT versus TEE in left atrial appendage occlusion.” Future LAAC trials should incorporate preprocedural CCTA.
Dr. O’Neill noted that, as a subanalysis of a randomized trial, the “results are hypothesis generating.” However, he added, “the results are in line with several previous studies of CT versus TEE in left atrial appendage occlusion.”
Dr Räber disclosed financial relationships with Abbott Vascular, Boston Scientific, Biotronik, Infraredx, Heartflow, Sanofi, Regeneron, Amgen, AstraZeneca, CSL Behring, Canon, Occlutech, and Vifor. Dr. O’Neill disclosed financial relationships with Edwards Lifesciences, Medtronic, and Abbott Vascular.
FROM JACC: CARDIOVASCULAR INTERVENTIONS
Statins tied to lower stroke risk in atrial fibrillation
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM EHRA 2023
Active older women show heightened AFib risk
Older women with high levels of physical activity showed twice the risk of atrial fibrillation (AFib) over 10 years as they did for cardiac disease or stroke, based on data from 46 cross-country skiers.
Although previous research suggests that women derive greater health benefits from endurance sports, compared with men, women are generally underrepresented in sports cardiology research, and most previous studies have focused on younger women, Marius Myrstad, MD, of Baerum Hospital, Gjettum, Norway, said in a presentation at the annual congress of the European Association of Preventive Cardiology.
Previous research also has shown an increased risk of AFib in male endurance athletes, but similar data on women are lacking, Dr. Myrstad said.
The researchers reviewed data from the Birkebeiner Ageing Study, a study of Norwegian cross-country skiers aged 65 years and older who were followed for 10 years. The participants were competitors in the 2009/2010 Birkebeiner race, a 54-km cross country ski race in Norway.
Participants responded to a questionnaire addressing cardiovascular disease risk factors, exercise habits, and other health issues. The mean age at baseline was 67.5 year. A total of 34 participants (76%) were available for follow-up visits in 2014, and 36 attended a follow-up visit in 2020. Cumulative exposure to exercise was 26 years.
A total of 86% of the women reported moderate to vigorous exercise in the past year at baseline; 61% did so at the 2020 follow-up visit. One of the participants died during the study period.
“The baseline prevalence of cardiovascular conditions was very low,” Dr. Myrstad noted.
However, despite a low prevalence of cardiovascular risk factors, the risk of AFib in the study population was twice as high as for other cardiac diseases and stroke (15.6%, 7.1%, and 7.1%, respectively).
The mechanism of action for the increased AFib remains unclear, but the current study highlights the need for large, prospective studies of female athletes to address not only AFib, but also exercise-induced cardiac remodeling and cardiovascular health in general, said Dr. Myrstad.
The findings were limited by the small sample size and use of self-reports, Dr. Myrstad said, and more research is needed to clarify the association between increased AFib and high-level athletic activity in women.
“We should strive to close the gap between female and male athletes in sports cardiology research,” he added.
Consider the big picture of AFib risk
This study is important because of the growing recognition that atrial fibrillation may be a preventable disease, said Gregory Marcus, MD, a cardiologist at the University of California, San Francisco, said in an interview.
“Various behaviors or exposures that are under the control of the individual patient may reveal especially powerful means to help reduce risk,” he added.
Dr. Marcus said he was not surprised by the current study findings, as they reflect those of other studies suggesting a heightened risk for atrial fibrillation associated with very excessive exercise. However, the study was limited by the relatively small size and lack of a comparison group, he said. In addition, “The study was observational, and therefore the possibility that factors other than the predictor of interest, in this case intensive endurance exercise, were truly causal of atrial fibrillation could not be excluded,” he noted.
“It is very important to place this specialized analysis in the greater context of the full weight of evidence related to physical activity and atrial fibrillation,” said Dr. Marcus. “Specifically, when it comes to the general public and the great majority of patients we see in clinical practice, encouraging more physical activity is generally the best approach to reduce risks of atrial fibrillation,” he said. “It appears to be only in extraordinarily rigorous and prolonged endurance exercise that higher risks of atrial fibrillation may result,” he noted.
However, “Exercise also has many other benefits, related to overall cardiovascular health, brain health, bone health, and even cancer risk reduction, such that, even among the highly trained endurance athletes, the net benefit versus risk remains unknown,” he said.
“While the risk of atrial fibrillation in these highly trained endurance athletes was higher than expected, it still occurred in the minority,” Dr. Marcus said. “Therefore, there are certainly other factors yet to be identified that influence this heightened atrial fibrillation risk, and future research aimed at elucidating these other factors may help identify individuals more or less prone to atrial fibrillation or other behaviors that can help mitigate that risk.”
Dr. Myrstad disclosed lecture fees from Bayer, Boehringer-Ingelheim, Bristol Myers Squibb, MSD, and Pfizer unrelated to the current study. Dr. Marcus disclosed serving as a consultant for Johnson and Johnson and InCarda, and holding equity as a cofounder of InCarda.
Older women with high levels of physical activity showed twice the risk of atrial fibrillation (AFib) over 10 years as they did for cardiac disease or stroke, based on data from 46 cross-country skiers.
Although previous research suggests that women derive greater health benefits from endurance sports, compared with men, women are generally underrepresented in sports cardiology research, and most previous studies have focused on younger women, Marius Myrstad, MD, of Baerum Hospital, Gjettum, Norway, said in a presentation at the annual congress of the European Association of Preventive Cardiology.
Previous research also has shown an increased risk of AFib in male endurance athletes, but similar data on women are lacking, Dr. Myrstad said.
The researchers reviewed data from the Birkebeiner Ageing Study, a study of Norwegian cross-country skiers aged 65 years and older who were followed for 10 years. The participants were competitors in the 2009/2010 Birkebeiner race, a 54-km cross country ski race in Norway.
Participants responded to a questionnaire addressing cardiovascular disease risk factors, exercise habits, and other health issues. The mean age at baseline was 67.5 year. A total of 34 participants (76%) were available for follow-up visits in 2014, and 36 attended a follow-up visit in 2020. Cumulative exposure to exercise was 26 years.
A total of 86% of the women reported moderate to vigorous exercise in the past year at baseline; 61% did so at the 2020 follow-up visit. One of the participants died during the study period.
“The baseline prevalence of cardiovascular conditions was very low,” Dr. Myrstad noted.
However, despite a low prevalence of cardiovascular risk factors, the risk of AFib in the study population was twice as high as for other cardiac diseases and stroke (15.6%, 7.1%, and 7.1%, respectively).
The mechanism of action for the increased AFib remains unclear, but the current study highlights the need for large, prospective studies of female athletes to address not only AFib, but also exercise-induced cardiac remodeling and cardiovascular health in general, said Dr. Myrstad.
The findings were limited by the small sample size and use of self-reports, Dr. Myrstad said, and more research is needed to clarify the association between increased AFib and high-level athletic activity in women.
“We should strive to close the gap between female and male athletes in sports cardiology research,” he added.
Consider the big picture of AFib risk
This study is important because of the growing recognition that atrial fibrillation may be a preventable disease, said Gregory Marcus, MD, a cardiologist at the University of California, San Francisco, said in an interview.
“Various behaviors or exposures that are under the control of the individual patient may reveal especially powerful means to help reduce risk,” he added.
Dr. Marcus said he was not surprised by the current study findings, as they reflect those of other studies suggesting a heightened risk for atrial fibrillation associated with very excessive exercise. However, the study was limited by the relatively small size and lack of a comparison group, he said. In addition, “The study was observational, and therefore the possibility that factors other than the predictor of interest, in this case intensive endurance exercise, were truly causal of atrial fibrillation could not be excluded,” he noted.
“It is very important to place this specialized analysis in the greater context of the full weight of evidence related to physical activity and atrial fibrillation,” said Dr. Marcus. “Specifically, when it comes to the general public and the great majority of patients we see in clinical practice, encouraging more physical activity is generally the best approach to reduce risks of atrial fibrillation,” he said. “It appears to be only in extraordinarily rigorous and prolonged endurance exercise that higher risks of atrial fibrillation may result,” he noted.
However, “Exercise also has many other benefits, related to overall cardiovascular health, brain health, bone health, and even cancer risk reduction, such that, even among the highly trained endurance athletes, the net benefit versus risk remains unknown,” he said.
“While the risk of atrial fibrillation in these highly trained endurance athletes was higher than expected, it still occurred in the minority,” Dr. Marcus said. “Therefore, there are certainly other factors yet to be identified that influence this heightened atrial fibrillation risk, and future research aimed at elucidating these other factors may help identify individuals more or less prone to atrial fibrillation or other behaviors that can help mitigate that risk.”
Dr. Myrstad disclosed lecture fees from Bayer, Boehringer-Ingelheim, Bristol Myers Squibb, MSD, and Pfizer unrelated to the current study. Dr. Marcus disclosed serving as a consultant for Johnson and Johnson and InCarda, and holding equity as a cofounder of InCarda.
Older women with high levels of physical activity showed twice the risk of atrial fibrillation (AFib) over 10 years as they did for cardiac disease or stroke, based on data from 46 cross-country skiers.
Although previous research suggests that women derive greater health benefits from endurance sports, compared with men, women are generally underrepresented in sports cardiology research, and most previous studies have focused on younger women, Marius Myrstad, MD, of Baerum Hospital, Gjettum, Norway, said in a presentation at the annual congress of the European Association of Preventive Cardiology.
Previous research also has shown an increased risk of AFib in male endurance athletes, but similar data on women are lacking, Dr. Myrstad said.
The researchers reviewed data from the Birkebeiner Ageing Study, a study of Norwegian cross-country skiers aged 65 years and older who were followed for 10 years. The participants were competitors in the 2009/2010 Birkebeiner race, a 54-km cross country ski race in Norway.
Participants responded to a questionnaire addressing cardiovascular disease risk factors, exercise habits, and other health issues. The mean age at baseline was 67.5 year. A total of 34 participants (76%) were available for follow-up visits in 2014, and 36 attended a follow-up visit in 2020. Cumulative exposure to exercise was 26 years.
A total of 86% of the women reported moderate to vigorous exercise in the past year at baseline; 61% did so at the 2020 follow-up visit. One of the participants died during the study period.
“The baseline prevalence of cardiovascular conditions was very low,” Dr. Myrstad noted.
However, despite a low prevalence of cardiovascular risk factors, the risk of AFib in the study population was twice as high as for other cardiac diseases and stroke (15.6%, 7.1%, and 7.1%, respectively).
The mechanism of action for the increased AFib remains unclear, but the current study highlights the need for large, prospective studies of female athletes to address not only AFib, but also exercise-induced cardiac remodeling and cardiovascular health in general, said Dr. Myrstad.
The findings were limited by the small sample size and use of self-reports, Dr. Myrstad said, and more research is needed to clarify the association between increased AFib and high-level athletic activity in women.
“We should strive to close the gap between female and male athletes in sports cardiology research,” he added.
Consider the big picture of AFib risk
This study is important because of the growing recognition that atrial fibrillation may be a preventable disease, said Gregory Marcus, MD, a cardiologist at the University of California, San Francisco, said in an interview.
“Various behaviors or exposures that are under the control of the individual patient may reveal especially powerful means to help reduce risk,” he added.
Dr. Marcus said he was not surprised by the current study findings, as they reflect those of other studies suggesting a heightened risk for atrial fibrillation associated with very excessive exercise. However, the study was limited by the relatively small size and lack of a comparison group, he said. In addition, “The study was observational, and therefore the possibility that factors other than the predictor of interest, in this case intensive endurance exercise, were truly causal of atrial fibrillation could not be excluded,” he noted.
“It is very important to place this specialized analysis in the greater context of the full weight of evidence related to physical activity and atrial fibrillation,” said Dr. Marcus. “Specifically, when it comes to the general public and the great majority of patients we see in clinical practice, encouraging more physical activity is generally the best approach to reduce risks of atrial fibrillation,” he said. “It appears to be only in extraordinarily rigorous and prolonged endurance exercise that higher risks of atrial fibrillation may result,” he noted.
However, “Exercise also has many other benefits, related to overall cardiovascular health, brain health, bone health, and even cancer risk reduction, such that, even among the highly trained endurance athletes, the net benefit versus risk remains unknown,” he said.
“While the risk of atrial fibrillation in these highly trained endurance athletes was higher than expected, it still occurred in the minority,” Dr. Marcus said. “Therefore, there are certainly other factors yet to be identified that influence this heightened atrial fibrillation risk, and future research aimed at elucidating these other factors may help identify individuals more or less prone to atrial fibrillation or other behaviors that can help mitigate that risk.”
Dr. Myrstad disclosed lecture fees from Bayer, Boehringer-Ingelheim, Bristol Myers Squibb, MSD, and Pfizer unrelated to the current study. Dr. Marcus disclosed serving as a consultant for Johnson and Johnson and InCarda, and holding equity as a cofounder of InCarda.
FROM ESC PREVENTIVE CARDIOLOGY 2023
Hybrid ablation superior for persistent AFib: CEASE-AF
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT EHRA 2023
Napping and AFib risk: The long and the short of it
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
FROM ESC PREVENTIVE CARDIOLOGY 2023