User login
FDA grants drug orphan designation for PNH

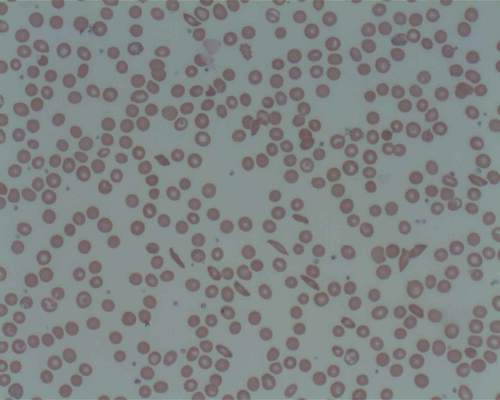
The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Bevacizumab no better than placebo for epistaxis in HHT

of nasal spray
Bevacizumab nasal spray is no more effective than a placebo for reducing epistaxis caused by hereditary hemorrhagic telangiectasia (HHT), according to a study published in JAMA.
Researchers compared 3 different doses of bevacizumab to a sodium chloride placebo and found no significant difference between the treatment groups in the frequency or duration of epistaxis, the need for transfusion, or hemoglobin/ferritin levels.
Sophie Dupuis-Girod, MD, PhD, of the Hopital Femme-Mere-Enfants in Bron, France, and her colleagues conducted this trial, enrolling 80 patients with HHT and a history of epistaxis.
The patients were randomized to receive placebo (0.9% sodium chloride, n=21) or 1 of 3 doses of bevacizumab nasal spray.
Patients in the bevacizumab groups received 25 mg (n=20), 50 mg (n=20), or 75 mg (n=19) in 3 doses, 14 days apart, for a total treatment duration of 4 weeks, resulting in a total dose of 75 mg, 150 mg, or 225 mg.
Epistaxis duration
The researchers measured the mean monthly epistaxis duration at 3 months and found no significant difference between the placebo group and the bevacizumab groups (P=0.57). Likewise, there were no significant differences between the bevacizumab groups.
However, most of the groups experienced improvements in epistaxis duration after treatment.
The mean monthly epistaxis duration (in minutes) before treatment (from day −90 to day −1) and after treatment (from day 29 to day 118), respectively, was:
- 262.8 and 200.4 in the placebo group
- 285.5 and 259.2 in the 25 mg group
- 229.0 and 244.0 in the 50 mg group
- 272.9 and 215.0 in the 75 mg group.
Epistaxis frequency
There was no significant difference between the bevacizumab groups and the placebo group when it came to the number of epistaxis episodes (P=0.55). However, patients in all of the groups saw a reduction in episodes after treatment.
The mean number of epistaxis episodes before treatment (from day −90 to day −1) and after (from day 29 to day 118), respectively, were:
- 31.37 and 24.27 in the placebo group
- 30.99 and 23.13 in the 25 mg bevacizumab group
- 25.06 and 20.01 in the 50 mg bevacizumab group
- 27.84 and 24.35 in the 75 mg bevacizumab group.
Other outcomes
There was no significant difference between the bevacizumab groups and the placebo group regarding the number of red blood cell transfusions at 3 months (P=0.35) and 6 months (P=0.39), mean hemoglobin levels (P=0.66), and mean ferritin levels (P=0.86).
There were no adverse events (AEs) thought to be treatment-related. There were 161 AEs overall and no significant differences between the groups—47 AEs in the 25 mg bevacizumab group, 33 in the 50 mg bevacizumab group, 38 in the 75 mg bevacizumab group, and 43 in the placebo group.
After an interim analysis, an independent data monitoring committee recommended terminating this study early due to treatment futility. So the study was stopped before entering phase 3.
![]()

of nasal spray
Bevacizumab nasal spray is no more effective than a placebo for reducing epistaxis caused by hereditary hemorrhagic telangiectasia (HHT), according to a study published in JAMA.
Researchers compared 3 different doses of bevacizumab to a sodium chloride placebo and found no significant difference between the treatment groups in the frequency or duration of epistaxis, the need for transfusion, or hemoglobin/ferritin levels.
Sophie Dupuis-Girod, MD, PhD, of the Hopital Femme-Mere-Enfants in Bron, France, and her colleagues conducted this trial, enrolling 80 patients with HHT and a history of epistaxis.
The patients were randomized to receive placebo (0.9% sodium chloride, n=21) or 1 of 3 doses of bevacizumab nasal spray.
Patients in the bevacizumab groups received 25 mg (n=20), 50 mg (n=20), or 75 mg (n=19) in 3 doses, 14 days apart, for a total treatment duration of 4 weeks, resulting in a total dose of 75 mg, 150 mg, or 225 mg.
Epistaxis duration
The researchers measured the mean monthly epistaxis duration at 3 months and found no significant difference between the placebo group and the bevacizumab groups (P=0.57). Likewise, there were no significant differences between the bevacizumab groups.
However, most of the groups experienced improvements in epistaxis duration after treatment.
The mean monthly epistaxis duration (in minutes) before treatment (from day −90 to day −1) and after treatment (from day 29 to day 118), respectively, was:
- 262.8 and 200.4 in the placebo group
- 285.5 and 259.2 in the 25 mg group
- 229.0 and 244.0 in the 50 mg group
- 272.9 and 215.0 in the 75 mg group.
Epistaxis frequency
There was no significant difference between the bevacizumab groups and the placebo group when it came to the number of epistaxis episodes (P=0.55). However, patients in all of the groups saw a reduction in episodes after treatment.
The mean number of epistaxis episodes before treatment (from day −90 to day −1) and after (from day 29 to day 118), respectively, were:
- 31.37 and 24.27 in the placebo group
- 30.99 and 23.13 in the 25 mg bevacizumab group
- 25.06 and 20.01 in the 50 mg bevacizumab group
- 27.84 and 24.35 in the 75 mg bevacizumab group.
Other outcomes
There was no significant difference between the bevacizumab groups and the placebo group regarding the number of red blood cell transfusions at 3 months (P=0.35) and 6 months (P=0.39), mean hemoglobin levels (P=0.66), and mean ferritin levels (P=0.86).
There were no adverse events (AEs) thought to be treatment-related. There were 161 AEs overall and no significant differences between the groups—47 AEs in the 25 mg bevacizumab group, 33 in the 50 mg bevacizumab group, 38 in the 75 mg bevacizumab group, and 43 in the placebo group.
After an interim analysis, an independent data monitoring committee recommended terminating this study early due to treatment futility. So the study was stopped before entering phase 3.
![]()

of nasal spray
Bevacizumab nasal spray is no more effective than a placebo for reducing epistaxis caused by hereditary hemorrhagic telangiectasia (HHT), according to a study published in JAMA.
Researchers compared 3 different doses of bevacizumab to a sodium chloride placebo and found no significant difference between the treatment groups in the frequency or duration of epistaxis, the need for transfusion, or hemoglobin/ferritin levels.
Sophie Dupuis-Girod, MD, PhD, of the Hopital Femme-Mere-Enfants in Bron, France, and her colleagues conducted this trial, enrolling 80 patients with HHT and a history of epistaxis.
The patients were randomized to receive placebo (0.9% sodium chloride, n=21) or 1 of 3 doses of bevacizumab nasal spray.
Patients in the bevacizumab groups received 25 mg (n=20), 50 mg (n=20), or 75 mg (n=19) in 3 doses, 14 days apart, for a total treatment duration of 4 weeks, resulting in a total dose of 75 mg, 150 mg, or 225 mg.
Epistaxis duration
The researchers measured the mean monthly epistaxis duration at 3 months and found no significant difference between the placebo group and the bevacizumab groups (P=0.57). Likewise, there were no significant differences between the bevacizumab groups.
However, most of the groups experienced improvements in epistaxis duration after treatment.
The mean monthly epistaxis duration (in minutes) before treatment (from day −90 to day −1) and after treatment (from day 29 to day 118), respectively, was:
- 262.8 and 200.4 in the placebo group
- 285.5 and 259.2 in the 25 mg group
- 229.0 and 244.0 in the 50 mg group
- 272.9 and 215.0 in the 75 mg group.
Epistaxis frequency
There was no significant difference between the bevacizumab groups and the placebo group when it came to the number of epistaxis episodes (P=0.55). However, patients in all of the groups saw a reduction in episodes after treatment.
The mean number of epistaxis episodes before treatment (from day −90 to day −1) and after (from day 29 to day 118), respectively, were:
- 31.37 and 24.27 in the placebo group
- 30.99 and 23.13 in the 25 mg bevacizumab group
- 25.06 and 20.01 in the 50 mg bevacizumab group
- 27.84 and 24.35 in the 75 mg bevacizumab group.
Other outcomes
There was no significant difference between the bevacizumab groups and the placebo group regarding the number of red blood cell transfusions at 3 months (P=0.35) and 6 months (P=0.39), mean hemoglobin levels (P=0.66), and mean ferritin levels (P=0.86).
There were no adverse events (AEs) thought to be treatment-related. There were 161 AEs overall and no significant differences between the groups—47 AEs in the 25 mg bevacizumab group, 33 in the 50 mg bevacizumab group, 38 in the 75 mg bevacizumab group, and 43 in the placebo group.
After an interim analysis, an independent data monitoring committee recommended terminating this study early due to treatment futility. So the study was stopped before entering phase 3.
![]()
Saline comparable to drug therapy for epistaxis in HHT

Photo courtesy of the
University of Utah
Health Sciences Center
Results of a phase 2 study suggest a saline nose spray may be as effective as 3 different medicated sprays for preventing epistaxis in patients with hemorrhagic telangiectasia (HHT).
The study was a comparison of bevacizumab, estriol, tranexamic acid, and saline.
The results showed no significant differences in the frequency or duration of epistaxis, and patients in all 4 groups reported improvements in Epistaxis Severity Scores (ESS).
“This research highlights that there could be a benefit even in the simplest of interventions,” said study author Kevin Whitehead, MD, of the University of Utah School of Medicine in Salt Lake City.
“No drug proved to be any better than the saline placebo, but the majority of patients improved over the course of treatment—even those using saline.”
Dr Whitehead and his colleagues reported these results in JAMA.
The study included 121 HHT patients who had experienced HHT-related epistaxis. They were randomized to twice-daily nose sprays with bevacizumab 1% (4 mg/day), estriol 0.1% (0.4 mg/day), tranexamic acid 10% (40 mg/day), or placebo (0.9% saline) for 12 weeks.
Safety
The investigators said nasal symptoms were the most common adverse events, and they occurred in all 4 treatment groups.
Gastrointestinal symptoms, including abdominal pain, nausea, and vomiting, were most common among patients receiving tranexamic acid.
There were no thrombotic complications, episodes of severe hypertension, serious drug-related adverse events, or deaths in any treatment group.
Efficacy
There was no significant difference in epistaxis frequency between the placebo group and the other treatment groups (P=0.97).
After 12 weeks of treatment, the median weekly number of bleeding episodes was 7.0 for patients in the bevacizumab group, 8.0 for the estriol group, 7.5 for the tranexamic acid group, and 8.0 for the placebo group. At baseline, the median weekly number of bleeding episodes was 10.0, 7.0, 7.8, and 7.0, respectively.
After 12 weeks of treatment, there was no significant difference in epistaxis duration between the placebo group and the other treatment groups (P=0.09).
The median duration of epistaxis per bleeding episode was 3.0 minutes for the bevacizumab group, 4.0 minutes for the estriol group, 6.2 minutes for the tranexamic acid group, and 5.0 minutes for the placebo group. (Bleeding duration was not recorded at baseline.)
After 12 weeks of treatment, there were no significant differences between the treatment groups when it came to hemoglobin levels (P=0.43), ferritin levels (P=0.10), treatment failure (P=0.08), the need for transfusion (P=0.42), or emergency department visits (P=0.72).
Patients in all 4 treatment groups experienced a significant decline in ESS from baseline to week 12 (P<0.001 for time effect).
The median ESS decreased from 5.71 to 3.74 in the placebo group, 5.16 to 3.54 in the bevacizumab group, 5.19 to 3.56 in the estriol group, and 5.43 to 4.06 in the tranexamic acid group. The investigators said the improvement in ESS was clinically significant.
However, the team also said they cannot completely rule out the possibility that symptoms may have improved because of a placebo effect.
What’s more, it could be that some of the drugs tested would work better if taken at a higher dose, or if applied as a gel or polymer that adheres better to the inside of the nasal cavity.
Nevertheless, the results from this trial were enough to convince Dr Whitehead and his colleagues to routinely recommend saline nasal spray to their patients with HHT.
“We stress the importance of hydration,” Dr Whitehead said. “We tell them that something as simple as a morning and night saline spray could offer them some benefit.” ![]()

Photo courtesy of the
University of Utah
Health Sciences Center
Results of a phase 2 study suggest a saline nose spray may be as effective as 3 different medicated sprays for preventing epistaxis in patients with hemorrhagic telangiectasia (HHT).
The study was a comparison of bevacizumab, estriol, tranexamic acid, and saline.
The results showed no significant differences in the frequency or duration of epistaxis, and patients in all 4 groups reported improvements in Epistaxis Severity Scores (ESS).
“This research highlights that there could be a benefit even in the simplest of interventions,” said study author Kevin Whitehead, MD, of the University of Utah School of Medicine in Salt Lake City.
“No drug proved to be any better than the saline placebo, but the majority of patients improved over the course of treatment—even those using saline.”
Dr Whitehead and his colleagues reported these results in JAMA.
The study included 121 HHT patients who had experienced HHT-related epistaxis. They were randomized to twice-daily nose sprays with bevacizumab 1% (4 mg/day), estriol 0.1% (0.4 mg/day), tranexamic acid 10% (40 mg/day), or placebo (0.9% saline) for 12 weeks.
Safety
The investigators said nasal symptoms were the most common adverse events, and they occurred in all 4 treatment groups.
Gastrointestinal symptoms, including abdominal pain, nausea, and vomiting, were most common among patients receiving tranexamic acid.
There were no thrombotic complications, episodes of severe hypertension, serious drug-related adverse events, or deaths in any treatment group.
Efficacy
There was no significant difference in epistaxis frequency between the placebo group and the other treatment groups (P=0.97).
After 12 weeks of treatment, the median weekly number of bleeding episodes was 7.0 for patients in the bevacizumab group, 8.0 for the estriol group, 7.5 for the tranexamic acid group, and 8.0 for the placebo group. At baseline, the median weekly number of bleeding episodes was 10.0, 7.0, 7.8, and 7.0, respectively.
After 12 weeks of treatment, there was no significant difference in epistaxis duration between the placebo group and the other treatment groups (P=0.09).
The median duration of epistaxis per bleeding episode was 3.0 minutes for the bevacizumab group, 4.0 minutes for the estriol group, 6.2 minutes for the tranexamic acid group, and 5.0 minutes for the placebo group. (Bleeding duration was not recorded at baseline.)
After 12 weeks of treatment, there were no significant differences between the treatment groups when it came to hemoglobin levels (P=0.43), ferritin levels (P=0.10), treatment failure (P=0.08), the need for transfusion (P=0.42), or emergency department visits (P=0.72).
Patients in all 4 treatment groups experienced a significant decline in ESS from baseline to week 12 (P<0.001 for time effect).
The median ESS decreased from 5.71 to 3.74 in the placebo group, 5.16 to 3.54 in the bevacizumab group, 5.19 to 3.56 in the estriol group, and 5.43 to 4.06 in the tranexamic acid group. The investigators said the improvement in ESS was clinically significant.
However, the team also said they cannot completely rule out the possibility that symptoms may have improved because of a placebo effect.
What’s more, it could be that some of the drugs tested would work better if taken at a higher dose, or if applied as a gel or polymer that adheres better to the inside of the nasal cavity.
Nevertheless, the results from this trial were enough to convince Dr Whitehead and his colleagues to routinely recommend saline nasal spray to their patients with HHT.
“We stress the importance of hydration,” Dr Whitehead said. “We tell them that something as simple as a morning and night saline spray could offer them some benefit.” ![]()

Photo courtesy of the
University of Utah
Health Sciences Center
Results of a phase 2 study suggest a saline nose spray may be as effective as 3 different medicated sprays for preventing epistaxis in patients with hemorrhagic telangiectasia (HHT).
The study was a comparison of bevacizumab, estriol, tranexamic acid, and saline.
The results showed no significant differences in the frequency or duration of epistaxis, and patients in all 4 groups reported improvements in Epistaxis Severity Scores (ESS).
“This research highlights that there could be a benefit even in the simplest of interventions,” said study author Kevin Whitehead, MD, of the University of Utah School of Medicine in Salt Lake City.
“No drug proved to be any better than the saline placebo, but the majority of patients improved over the course of treatment—even those using saline.”
Dr Whitehead and his colleagues reported these results in JAMA.
The study included 121 HHT patients who had experienced HHT-related epistaxis. They were randomized to twice-daily nose sprays with bevacizumab 1% (4 mg/day), estriol 0.1% (0.4 mg/day), tranexamic acid 10% (40 mg/day), or placebo (0.9% saline) for 12 weeks.
Safety
The investigators said nasal symptoms were the most common adverse events, and they occurred in all 4 treatment groups.
Gastrointestinal symptoms, including abdominal pain, nausea, and vomiting, were most common among patients receiving tranexamic acid.
There were no thrombotic complications, episodes of severe hypertension, serious drug-related adverse events, or deaths in any treatment group.
Efficacy
There was no significant difference in epistaxis frequency between the placebo group and the other treatment groups (P=0.97).
After 12 weeks of treatment, the median weekly number of bleeding episodes was 7.0 for patients in the bevacizumab group, 8.0 for the estriol group, 7.5 for the tranexamic acid group, and 8.0 for the placebo group. At baseline, the median weekly number of bleeding episodes was 10.0, 7.0, 7.8, and 7.0, respectively.
After 12 weeks of treatment, there was no significant difference in epistaxis duration between the placebo group and the other treatment groups (P=0.09).
The median duration of epistaxis per bleeding episode was 3.0 minutes for the bevacizumab group, 4.0 minutes for the estriol group, 6.2 minutes for the tranexamic acid group, and 5.0 minutes for the placebo group. (Bleeding duration was not recorded at baseline.)
After 12 weeks of treatment, there were no significant differences between the treatment groups when it came to hemoglobin levels (P=0.43), ferritin levels (P=0.10), treatment failure (P=0.08), the need for transfusion (P=0.42), or emergency department visits (P=0.72).
Patients in all 4 treatment groups experienced a significant decline in ESS from baseline to week 12 (P<0.001 for time effect).
The median ESS decreased from 5.71 to 3.74 in the placebo group, 5.16 to 3.54 in the bevacizumab group, 5.19 to 3.56 in the estriol group, and 5.43 to 4.06 in the tranexamic acid group. The investigators said the improvement in ESS was clinically significant.
However, the team also said they cannot completely rule out the possibility that symptoms may have improved because of a placebo effect.
What’s more, it could be that some of the drugs tested would work better if taken at a higher dose, or if applied as a gel or polymer that adheres better to the inside of the nasal cavity.
Nevertheless, the results from this trial were enough to convince Dr Whitehead and his colleagues to routinely recommend saline nasal spray to their patients with HHT.
“We stress the importance of hydration,” Dr Whitehead said. “We tell them that something as simple as a morning and night saline spray could offer them some benefit.” ![]()
ASH launches sickle cell coalition
To improve the lives of individuals with sickle cell disease, the American Society of Hematology has launched the Sickle Cell Disease Coalition (SCDC). Creation of the coalition with 20 other organizations coincides with the release of “State of Sickle Cell Disease: 2016” – a report detailing the status of access to care for patients with sickle cell disease, gaps in the training and education of health care professionals, areas of interest for research and clinical trials, and the global state of the disease. All four of these areas need improvement, ASH officials said in a statement.
“Not only are individuals with [sickle cell disease] burdened by the pain and disability that comes with a chronic condition, but they also have very few accessible treatment options due to our fragmented health care system,” Dr. Charles S. Abrams, president of ASH, said in the statement. Sickle cell disease affects approximately 100,000 Americans and remains a growing global health concern, according to the statement.
The coalition’s goals include development of evidence-based treatment guidelines to improve quality of care, education of clinicians to increase the number of health care providers available to treat sickle cell disease, investment in research and clinical trials to improve existing treatments and develop new ones, and expansion of early intervention programs to help ease the global burden of sickle cell disease.
For more information regarding the coalition, click here.
To improve the lives of individuals with sickle cell disease, the American Society of Hematology has launched the Sickle Cell Disease Coalition (SCDC). Creation of the coalition with 20 other organizations coincides with the release of “State of Sickle Cell Disease: 2016” – a report detailing the status of access to care for patients with sickle cell disease, gaps in the training and education of health care professionals, areas of interest for research and clinical trials, and the global state of the disease. All four of these areas need improvement, ASH officials said in a statement.
“Not only are individuals with [sickle cell disease] burdened by the pain and disability that comes with a chronic condition, but they also have very few accessible treatment options due to our fragmented health care system,” Dr. Charles S. Abrams, president of ASH, said in the statement. Sickle cell disease affects approximately 100,000 Americans and remains a growing global health concern, according to the statement.
The coalition’s goals include development of evidence-based treatment guidelines to improve quality of care, education of clinicians to increase the number of health care providers available to treat sickle cell disease, investment in research and clinical trials to improve existing treatments and develop new ones, and expansion of early intervention programs to help ease the global burden of sickle cell disease.
For more information regarding the coalition, click here.
To improve the lives of individuals with sickle cell disease, the American Society of Hematology has launched the Sickle Cell Disease Coalition (SCDC). Creation of the coalition with 20 other organizations coincides with the release of “State of Sickle Cell Disease: 2016” – a report detailing the status of access to care for patients with sickle cell disease, gaps in the training and education of health care professionals, areas of interest for research and clinical trials, and the global state of the disease. All four of these areas need improvement, ASH officials said in a statement.
“Not only are individuals with [sickle cell disease] burdened by the pain and disability that comes with a chronic condition, but they also have very few accessible treatment options due to our fragmented health care system,” Dr. Charles S. Abrams, president of ASH, said in the statement. Sickle cell disease affects approximately 100,000 Americans and remains a growing global health concern, according to the statement.
The coalition’s goals include development of evidence-based treatment guidelines to improve quality of care, education of clinicians to increase the number of health care providers available to treat sickle cell disease, investment in research and clinical trials to improve existing treatments and develop new ones, and expansion of early intervention programs to help ease the global burden of sickle cell disease.
For more information regarding the coalition, click here.
Andexanet controlled factor Xa inhibitor–related bleeding
The factor Xa antidote andexanet achieved effective hemostasis 12 hours after infusion in 79% of patients who had developed serious acute bleeding on factor Xa inhibitor therapy, according to a preliminary analysis of an ongoing study of how reducing anti–factor Xa activity affects clinical hemostatic outcomes.
“The site of bleeding was most often gastrointestinal or intracranial; anti–factor Xa activity was considerably elevated in most patients and, as such, was likely to be a major impediment to clinical hemostasis. The administration of an andexanet bolus and infusion resulted in rapid and substantial reversal of anti–factor Xa activity,” Stuart Connolly, MD, of McMaster University, Hamilton, Ont., and his associates reported at the ESC Congress and in a simultaneously published study (N Engl J Med. 2016 Aug 30. doi: 10.1056/NEJMoa1607887).
Andexanet alfa is a recombinant modified human factor Xa decoy protein that “sharply” reduced plasma levels of unbound factor Xa inhibitors as well as anti-factor Xa activity in healthy older volunteers receiving apixaban or rivaroxaban, the researchers noted. Based on those findings, they designed a prospective, multicenter, single-group, open-label study (Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of FXA Inhibitors; ANNEXA-4) of andexanet in patients with potentially life-threatening acute major bleeding related to anticoagulation with a factor Xa inhibitor.
This interim report from the ongoing study included 67 patients with data available by June 17, 2016. Participants averaged 77 years of age and were receiving a factor Xa inhibtor because of atrial fibrillation, venous thromboembolism, or both. All patients received a bolus of andexanet for 15 to 30 minutes followed by a 2-hour infusion. Based on previous studies, the researchers used a 400-mg bolus of andexanet followed by a 480-mg infusion when patients had last taken their factor Xa inhibitor more than 7 hours before, and a higher 800-mg bolus followed by a 960-mg infusion when patients had taken their anticoagulant more recently. Bleeding and hemostasis were evaluated based on serial CT or MRI scans of patients with intracranial hemorrhage and corrected hemoglobin and hematocrit levels at 12 hours for patients with gastrointestinal and other nonvisible bleeding.
Among 47 patients in the primary efficacy analysis, 37 (79%) achieved excellent or good hemostasis (95% confidence interval, 64% to 89%), including 81% of patients on rivaroxaban and 75% of patients on enoxaparin, the researchers reported. “The rates of excellent or good efficacy were 84% for gastrointestinal bleeding and 80% for intracranial bleeding, rates that were consistent for other subgroups that were examined,” they said. Among the five patients (10%) with the most residual anti–factor Xa activity, all had received the lower andexanet dose. Four had received rivaroxaban while one had received apixaban.
The safety population included all 67 patients, none of whom developed infusion reactions or antibodies to factors X, Xa, or andexanet. After 30 days of follow-up, 12 patients (18%) had experienced one or more thrombotic events, including deep vein thrombosis (seven patients), stroke (five patients), myocardial infarction (one patient), and pulmonary embolism (one patient). One-third of these events occurred within 3 days of receiving andexanet, while the rest occurred by day 30. A total of 10 patients (15%) died, and six deaths were from cardiovascular causes. “A controlled study would be required to assess whether the frequency of these events exceeded that expected in patients at increased risk for thrombotic events,” the researchers commented.
Portola Pharmaceuticals makes andexanet alfa and funded the study. Dr. Connolly disclosed ties to Bayer, Bristol-Myers Squibb/Pfizer, Daiichi-Sankyo, CSL Behring, Octapharma, and Boehringer Ingelheim outside the submitted work.
The factor Xa antidote andexanet achieved effective hemostasis 12 hours after infusion in 79% of patients who had developed serious acute bleeding on factor Xa inhibitor therapy, according to a preliminary analysis of an ongoing study of how reducing anti–factor Xa activity affects clinical hemostatic outcomes.
“The site of bleeding was most often gastrointestinal or intracranial; anti–factor Xa activity was considerably elevated in most patients and, as such, was likely to be a major impediment to clinical hemostasis. The administration of an andexanet bolus and infusion resulted in rapid and substantial reversal of anti–factor Xa activity,” Stuart Connolly, MD, of McMaster University, Hamilton, Ont., and his associates reported at the ESC Congress and in a simultaneously published study (N Engl J Med. 2016 Aug 30. doi: 10.1056/NEJMoa1607887).
Andexanet alfa is a recombinant modified human factor Xa decoy protein that “sharply” reduced plasma levels of unbound factor Xa inhibitors as well as anti-factor Xa activity in healthy older volunteers receiving apixaban or rivaroxaban, the researchers noted. Based on those findings, they designed a prospective, multicenter, single-group, open-label study (Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of FXA Inhibitors; ANNEXA-4) of andexanet in patients with potentially life-threatening acute major bleeding related to anticoagulation with a factor Xa inhibitor.
This interim report from the ongoing study included 67 patients with data available by June 17, 2016. Participants averaged 77 years of age and were receiving a factor Xa inhibtor because of atrial fibrillation, venous thromboembolism, or both. All patients received a bolus of andexanet for 15 to 30 minutes followed by a 2-hour infusion. Based on previous studies, the researchers used a 400-mg bolus of andexanet followed by a 480-mg infusion when patients had last taken their factor Xa inhibitor more than 7 hours before, and a higher 800-mg bolus followed by a 960-mg infusion when patients had taken their anticoagulant more recently. Bleeding and hemostasis were evaluated based on serial CT or MRI scans of patients with intracranial hemorrhage and corrected hemoglobin and hematocrit levels at 12 hours for patients with gastrointestinal and other nonvisible bleeding.
Among 47 patients in the primary efficacy analysis, 37 (79%) achieved excellent or good hemostasis (95% confidence interval, 64% to 89%), including 81% of patients on rivaroxaban and 75% of patients on enoxaparin, the researchers reported. “The rates of excellent or good efficacy were 84% for gastrointestinal bleeding and 80% for intracranial bleeding, rates that were consistent for other subgroups that were examined,” they said. Among the five patients (10%) with the most residual anti–factor Xa activity, all had received the lower andexanet dose. Four had received rivaroxaban while one had received apixaban.
The safety population included all 67 patients, none of whom developed infusion reactions or antibodies to factors X, Xa, or andexanet. After 30 days of follow-up, 12 patients (18%) had experienced one or more thrombotic events, including deep vein thrombosis (seven patients), stroke (five patients), myocardial infarction (one patient), and pulmonary embolism (one patient). One-third of these events occurred within 3 days of receiving andexanet, while the rest occurred by day 30. A total of 10 patients (15%) died, and six deaths were from cardiovascular causes. “A controlled study would be required to assess whether the frequency of these events exceeded that expected in patients at increased risk for thrombotic events,” the researchers commented.
Portola Pharmaceuticals makes andexanet alfa and funded the study. Dr. Connolly disclosed ties to Bayer, Bristol-Myers Squibb/Pfizer, Daiichi-Sankyo, CSL Behring, Octapharma, and Boehringer Ingelheim outside the submitted work.
The factor Xa antidote andexanet achieved effective hemostasis 12 hours after infusion in 79% of patients who had developed serious acute bleeding on factor Xa inhibitor therapy, according to a preliminary analysis of an ongoing study of how reducing anti–factor Xa activity affects clinical hemostatic outcomes.
“The site of bleeding was most often gastrointestinal or intracranial; anti–factor Xa activity was considerably elevated in most patients and, as such, was likely to be a major impediment to clinical hemostasis. The administration of an andexanet bolus and infusion resulted in rapid and substantial reversal of anti–factor Xa activity,” Stuart Connolly, MD, of McMaster University, Hamilton, Ont., and his associates reported at the ESC Congress and in a simultaneously published study (N Engl J Med. 2016 Aug 30. doi: 10.1056/NEJMoa1607887).
Andexanet alfa is a recombinant modified human factor Xa decoy protein that “sharply” reduced plasma levels of unbound factor Xa inhibitors as well as anti-factor Xa activity in healthy older volunteers receiving apixaban or rivaroxaban, the researchers noted. Based on those findings, they designed a prospective, multicenter, single-group, open-label study (Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of FXA Inhibitors; ANNEXA-4) of andexanet in patients with potentially life-threatening acute major bleeding related to anticoagulation with a factor Xa inhibitor.
This interim report from the ongoing study included 67 patients with data available by June 17, 2016. Participants averaged 77 years of age and were receiving a factor Xa inhibtor because of atrial fibrillation, venous thromboembolism, or both. All patients received a bolus of andexanet for 15 to 30 minutes followed by a 2-hour infusion. Based on previous studies, the researchers used a 400-mg bolus of andexanet followed by a 480-mg infusion when patients had last taken their factor Xa inhibitor more than 7 hours before, and a higher 800-mg bolus followed by a 960-mg infusion when patients had taken their anticoagulant more recently. Bleeding and hemostasis were evaluated based on serial CT or MRI scans of patients with intracranial hemorrhage and corrected hemoglobin and hematocrit levels at 12 hours for patients with gastrointestinal and other nonvisible bleeding.
Among 47 patients in the primary efficacy analysis, 37 (79%) achieved excellent or good hemostasis (95% confidence interval, 64% to 89%), including 81% of patients on rivaroxaban and 75% of patients on enoxaparin, the researchers reported. “The rates of excellent or good efficacy were 84% for gastrointestinal bleeding and 80% for intracranial bleeding, rates that were consistent for other subgroups that were examined,” they said. Among the five patients (10%) with the most residual anti–factor Xa activity, all had received the lower andexanet dose. Four had received rivaroxaban while one had received apixaban.
The safety population included all 67 patients, none of whom developed infusion reactions or antibodies to factors X, Xa, or andexanet. After 30 days of follow-up, 12 patients (18%) had experienced one or more thrombotic events, including deep vein thrombosis (seven patients), stroke (five patients), myocardial infarction (one patient), and pulmonary embolism (one patient). One-third of these events occurred within 3 days of receiving andexanet, while the rest occurred by day 30. A total of 10 patients (15%) died, and six deaths were from cardiovascular causes. “A controlled study would be required to assess whether the frequency of these events exceeded that expected in patients at increased risk for thrombotic events,” the researchers commented.
Portola Pharmaceuticals makes andexanet alfa and funded the study. Dr. Connolly disclosed ties to Bayer, Bristol-Myers Squibb/Pfizer, Daiichi-Sankyo, CSL Behring, Octapharma, and Boehringer Ingelheim outside the submitted work.
FROM ESC CONGRESS 2016
Key clinical point: Andexanet alfa achieved effective hemostasis in most patients with acute major bleeding on factor Xa inhibitors.
Major finding: At 12 hours after infusion, 37 of 47 patients in the efficacy analysis achieved excellent or good hemostasis (79%; 95% confidence interval, 64% to 89%).
Data source: A prospective, multicenter, single-group, open-label study of 67 adults, most of whom had substantial cardiovascular disease.
Disclosures: Portola Pharmaceuticals makes andexanet alfa and funded the study. Dr. Connolly disclosed ties to Bayer, Bristol-Myers Squibb/Pfizer, Daiichi-Sankyo, CSL Behring, Octapharma, and Boehringer Ingelheim outside the submitted work.
Hemophilia carriers are at risk for abnormal bleeding
ORLANDO – The traditional view that women who are hemophilia carriers are unaffected by the disease may not be accurate, because many hemophilia carriers experience abnormal bleeding, a hemophilia specialist contends.
“We do know that hemophilia carriers have increased bleeding scores compared to controls,” said Michelle Sholzberg, MD, a hematologist and medical director of the coagulation laboratory at St. Michael’s Hospital in Toronto.
Bleeding in carriers is predominantly mucocutaneous bleeding, and may include epistaxis, heavy menstrual bleeding, bleeding with interventional procedures, and postpartum hemorrhage, she said at the World Federation of Hemophilia World Congress.
The majority of women who carry a factor VIII or factor IX mutation on one X chromosome have factor levels ranging from 0.40 to 0.60 IU/mL, which are generally considered to be adequate for hemostasis.
Yet, “we know that many carriers bleed, and in fact there are carriers who bleed with higher factor levels that are truly in the normal range,” Dr. Sholzberg said.
Normal coagulation factor levels in the general population range from about 0.50 to 1.50 IU/mL. By this standard, approximately 30% of hemophilia carriers have low factor levels, she said.
Joint damage
In addition, 14%-19% of hemophilia A carriers report hemarthrosis, and there is an association in factor VIII or IX deficiencies among hemophilia carriers and reduced joint range of motion. In one study, this decreased range of motion was evident as early as the preteen years, and was suggestive of subclinical musculoskeletal bleeding among carriers. In a separate study, investigators found evidence that hemophilia A carriers have pathologic and radiologic evidence of structural joint damage.
Variability in factor levels among carriers may be caused by lyonization (the inactivation of one of the X-chromosomes), ABO blood type, the presence of mutations in genes encoding for von Willebrand factor, compound heterozygosity or homozygosity, or Turner’s mosaicism.
Clotting factor levels can also change with pregnancy, with hemophilia A carriers experiencing an increase in mean factor VIII levels from 0.46 IU/mL prepregnancy to 1.21 IU/mL in the third trimester, and hemophilia B carriers having a corresponding rise in factor IX levels from 0.31 IU/mL to 0.48 IU/mL, and many carriers still have suboptimal factor levels at pregnancy, Dr. Sholzberg said.
Postpartum hemorrhagic complications among carriers can lead to iron-deficiency anemia. The Centers for Disease Control and Prevention recommends testing all nonpregnant women for anemia every 5-10 years throughout their childbearing years, and annual objective testing for women with risk factors, she noted.
“I think we can all appreciate now that the multidisciplinary approach is important for women with bleeding disorders, and carriers of hemophilia can be safely cared for at HTCs [hemophilia treatment centers],” she said.
Carriers should be treated with a multimodal approach that enhances patient education and awareness, with an emphasis on self-report of symptoms and communication with health care providers.
“It’s also critical never to start a conversation with a woman who has a bleeding disorder with ‘Do you have heavy menstrual bleeding?’ I think we all know that the answer is almost always ‘No, I don’t,’ and that’s because if she has bled heavily for her entire life, she doesn’t know what normal is,” Dr. Sholzberg said.
She described a typical comprehensive care plan for a pregnant hemophilia A carrier. The plan will include information about the diagnosis, recommendations to the obstetricians to avoid the use of invasive instrumentation, anesthesia recommendations, recommendations for care of the mother regarding hemostatic agents, postpartum tranexamic acid, and factor levels, and hematology recommendations for the newborn.
Dr. Sholzberg disclosed research support and/or honoraria from Shire (previously Baxter, Baxalta), Octapharma, CSL Behring, Pfizer, and Novo Nordisk, and advisory committee activity for Shire.
ORLANDO – The traditional view that women who are hemophilia carriers are unaffected by the disease may not be accurate, because many hemophilia carriers experience abnormal bleeding, a hemophilia specialist contends.
“We do know that hemophilia carriers have increased bleeding scores compared to controls,” said Michelle Sholzberg, MD, a hematologist and medical director of the coagulation laboratory at St. Michael’s Hospital in Toronto.
Bleeding in carriers is predominantly mucocutaneous bleeding, and may include epistaxis, heavy menstrual bleeding, bleeding with interventional procedures, and postpartum hemorrhage, she said at the World Federation of Hemophilia World Congress.
The majority of women who carry a factor VIII or factor IX mutation on one X chromosome have factor levels ranging from 0.40 to 0.60 IU/mL, which are generally considered to be adequate for hemostasis.
Yet, “we know that many carriers bleed, and in fact there are carriers who bleed with higher factor levels that are truly in the normal range,” Dr. Sholzberg said.
Normal coagulation factor levels in the general population range from about 0.50 to 1.50 IU/mL. By this standard, approximately 30% of hemophilia carriers have low factor levels, she said.
Joint damage
In addition, 14%-19% of hemophilia A carriers report hemarthrosis, and there is an association in factor VIII or IX deficiencies among hemophilia carriers and reduced joint range of motion. In one study, this decreased range of motion was evident as early as the preteen years, and was suggestive of subclinical musculoskeletal bleeding among carriers. In a separate study, investigators found evidence that hemophilia A carriers have pathologic and radiologic evidence of structural joint damage.
Variability in factor levels among carriers may be caused by lyonization (the inactivation of one of the X-chromosomes), ABO blood type, the presence of mutations in genes encoding for von Willebrand factor, compound heterozygosity or homozygosity, or Turner’s mosaicism.
Clotting factor levels can also change with pregnancy, with hemophilia A carriers experiencing an increase in mean factor VIII levels from 0.46 IU/mL prepregnancy to 1.21 IU/mL in the third trimester, and hemophilia B carriers having a corresponding rise in factor IX levels from 0.31 IU/mL to 0.48 IU/mL, and many carriers still have suboptimal factor levels at pregnancy, Dr. Sholzberg said.
Postpartum hemorrhagic complications among carriers can lead to iron-deficiency anemia. The Centers for Disease Control and Prevention recommends testing all nonpregnant women for anemia every 5-10 years throughout their childbearing years, and annual objective testing for women with risk factors, she noted.
“I think we can all appreciate now that the multidisciplinary approach is important for women with bleeding disorders, and carriers of hemophilia can be safely cared for at HTCs [hemophilia treatment centers],” she said.
Carriers should be treated with a multimodal approach that enhances patient education and awareness, with an emphasis on self-report of symptoms and communication with health care providers.
“It’s also critical never to start a conversation with a woman who has a bleeding disorder with ‘Do you have heavy menstrual bleeding?’ I think we all know that the answer is almost always ‘No, I don’t,’ and that’s because if she has bled heavily for her entire life, she doesn’t know what normal is,” Dr. Sholzberg said.
She described a typical comprehensive care plan for a pregnant hemophilia A carrier. The plan will include information about the diagnosis, recommendations to the obstetricians to avoid the use of invasive instrumentation, anesthesia recommendations, recommendations for care of the mother regarding hemostatic agents, postpartum tranexamic acid, and factor levels, and hematology recommendations for the newborn.
Dr. Sholzberg disclosed research support and/or honoraria from Shire (previously Baxter, Baxalta), Octapharma, CSL Behring, Pfizer, and Novo Nordisk, and advisory committee activity for Shire.
ORLANDO – The traditional view that women who are hemophilia carriers are unaffected by the disease may not be accurate, because many hemophilia carriers experience abnormal bleeding, a hemophilia specialist contends.
“We do know that hemophilia carriers have increased bleeding scores compared to controls,” said Michelle Sholzberg, MD, a hematologist and medical director of the coagulation laboratory at St. Michael’s Hospital in Toronto.
Bleeding in carriers is predominantly mucocutaneous bleeding, and may include epistaxis, heavy menstrual bleeding, bleeding with interventional procedures, and postpartum hemorrhage, she said at the World Federation of Hemophilia World Congress.
The majority of women who carry a factor VIII or factor IX mutation on one X chromosome have factor levels ranging from 0.40 to 0.60 IU/mL, which are generally considered to be adequate for hemostasis.
Yet, “we know that many carriers bleed, and in fact there are carriers who bleed with higher factor levels that are truly in the normal range,” Dr. Sholzberg said.
Normal coagulation factor levels in the general population range from about 0.50 to 1.50 IU/mL. By this standard, approximately 30% of hemophilia carriers have low factor levels, she said.
Joint damage
In addition, 14%-19% of hemophilia A carriers report hemarthrosis, and there is an association in factor VIII or IX deficiencies among hemophilia carriers and reduced joint range of motion. In one study, this decreased range of motion was evident as early as the preteen years, and was suggestive of subclinical musculoskeletal bleeding among carriers. In a separate study, investigators found evidence that hemophilia A carriers have pathologic and radiologic evidence of structural joint damage.
Variability in factor levels among carriers may be caused by lyonization (the inactivation of one of the X-chromosomes), ABO blood type, the presence of mutations in genes encoding for von Willebrand factor, compound heterozygosity or homozygosity, or Turner’s mosaicism.
Clotting factor levels can also change with pregnancy, with hemophilia A carriers experiencing an increase in mean factor VIII levels from 0.46 IU/mL prepregnancy to 1.21 IU/mL in the third trimester, and hemophilia B carriers having a corresponding rise in factor IX levels from 0.31 IU/mL to 0.48 IU/mL, and many carriers still have suboptimal factor levels at pregnancy, Dr. Sholzberg said.
Postpartum hemorrhagic complications among carriers can lead to iron-deficiency anemia. The Centers for Disease Control and Prevention recommends testing all nonpregnant women for anemia every 5-10 years throughout their childbearing years, and annual objective testing for women with risk factors, she noted.
“I think we can all appreciate now that the multidisciplinary approach is important for women with bleeding disorders, and carriers of hemophilia can be safely cared for at HTCs [hemophilia treatment centers],” she said.
Carriers should be treated with a multimodal approach that enhances patient education and awareness, with an emphasis on self-report of symptoms and communication with health care providers.
“It’s also critical never to start a conversation with a woman who has a bleeding disorder with ‘Do you have heavy menstrual bleeding?’ I think we all know that the answer is almost always ‘No, I don’t,’ and that’s because if she has bled heavily for her entire life, she doesn’t know what normal is,” Dr. Sholzberg said.
She described a typical comprehensive care plan for a pregnant hemophilia A carrier. The plan will include information about the diagnosis, recommendations to the obstetricians to avoid the use of invasive instrumentation, anesthesia recommendations, recommendations for care of the mother regarding hemostatic agents, postpartum tranexamic acid, and factor levels, and hematology recommendations for the newborn.
Dr. Sholzberg disclosed research support and/or honoraria from Shire (previously Baxter, Baxalta), Octapharma, CSL Behring, Pfizer, and Novo Nordisk, and advisory committee activity for Shire.
EXPERT ANALYSIS FROM WFH 2016 WORLD CONGRESS
No VTE prophylaxis needed after joint surgery in patients with hemophilia
ORLANDO – In patients with hemophilia who have therapeutic factor levels at the time of joint replacement surgery, prophylaxis against venous thromboembolism (VTE) may be unnecessary.
In a cohort study of patients with hemophilia A or B who underwent total joint replacement surgery while being in proper hemostasis with therapeutic factor levels, there were no clinically evident episodes of venous thromboembolism, even though none of the patients had received perioperative anticoagulant prophylaxis, reported investigators from the National Hemophilia Center and Institute of Thrombosis and Hemostasis at the Sheba Medical Center in Tel Hashomer, Israel.
The data should be reassuring to clinicians whose patients with hemophilia require major orthopedic procedures, said lead author Dr. Anna Seltser, an orthopedic resident at Sheba Medical Center, in an interview.
“We have a lot of hemophilia patients who are not well treated because they live in the desert or distant communities, and we also sometimes treat patients from the Palestinian side of the Gaza Strip who don’t have access to care and need this type of surgery,” she said.
“We collected what I think is the biggest series of patients until now, we didn’t give any of them VTE prophylaxis, and none of them had any DVT [deep vein thrombosis], PE [pulmonary embolism], or similar complication,” she said.
Skip the heparin?
VTE prophylaxis with low-molecular-weight heparin, warfarin, or other anticoagulant agents is a common practice following orthopedic surgery in patients without bleeding disorders. But for patients with severe hemophilia, who often require major joint replacement surgery following years of bleeding-induced arthropathy, it’s unclear whether perioperative anticoagulation is beneficial, the investigators noted in a scientific poster at the World Federation of Hemophilia World Congress.
Dr. Seltser and colleagues therefore conducted a prospective cohort study of 50 patients with hemophilia A or B treated with major joint surgery and subsequent revisions from 1988 through 2015 at their center. In all, 47 patients had severe hemophilia A, 2 had mild hemophilia A, and 1 had hemophilia B.
The authors analyzed data on demographics, comorbidities, type of surgery, use of factor concentrates therapy around the time of surgery, and complications during follow-up, including massive hemorrhage, infections, implant loosening, DVT, and PE.
The patients underwent a total of 74 primary joint replacements (16 hips, 52 knees, and 6 ankles) and 23 revision surgeries.
As noted, there were no episodes of either DVT or PE among any of the patients. All but one complication occurred among patients undergoing total knee replacement. These included three cases of hemarthrosis, three limited-range-of-motion cases requiring closed manipulations, four soft-tissue hematomas, and one case each of superficial wound infection, urinary tract infection, pneumonia, and Candida infection of the tongue.
The only other complication was a case of disseminated intravascular coagulation, sepsis, and hemorrhagic shock in a patient who had undergone a revision (original procedure unspecified).
“Despite the concern that proper replacement factor therapy, applied before and after the surgery, may increase the risk for thromboembolic complications in patients with hemophilia undergoing joint replacement, our data show that prophylactic anticoagulation in this group of patients is not necessary,” the investigators concluded.
The study was internally funded. The investigators reported no conflicts of interest.
ORLANDO – In patients with hemophilia who have therapeutic factor levels at the time of joint replacement surgery, prophylaxis against venous thromboembolism (VTE) may be unnecessary.
In a cohort study of patients with hemophilia A or B who underwent total joint replacement surgery while being in proper hemostasis with therapeutic factor levels, there were no clinically evident episodes of venous thromboembolism, even though none of the patients had received perioperative anticoagulant prophylaxis, reported investigators from the National Hemophilia Center and Institute of Thrombosis and Hemostasis at the Sheba Medical Center in Tel Hashomer, Israel.
The data should be reassuring to clinicians whose patients with hemophilia require major orthopedic procedures, said lead author Dr. Anna Seltser, an orthopedic resident at Sheba Medical Center, in an interview.
“We have a lot of hemophilia patients who are not well treated because they live in the desert or distant communities, and we also sometimes treat patients from the Palestinian side of the Gaza Strip who don’t have access to care and need this type of surgery,” she said.
“We collected what I think is the biggest series of patients until now, we didn’t give any of them VTE prophylaxis, and none of them had any DVT [deep vein thrombosis], PE [pulmonary embolism], or similar complication,” she said.
Skip the heparin?
VTE prophylaxis with low-molecular-weight heparin, warfarin, or other anticoagulant agents is a common practice following orthopedic surgery in patients without bleeding disorders. But for patients with severe hemophilia, who often require major joint replacement surgery following years of bleeding-induced arthropathy, it’s unclear whether perioperative anticoagulation is beneficial, the investigators noted in a scientific poster at the World Federation of Hemophilia World Congress.
Dr. Seltser and colleagues therefore conducted a prospective cohort study of 50 patients with hemophilia A or B treated with major joint surgery and subsequent revisions from 1988 through 2015 at their center. In all, 47 patients had severe hemophilia A, 2 had mild hemophilia A, and 1 had hemophilia B.
The authors analyzed data on demographics, comorbidities, type of surgery, use of factor concentrates therapy around the time of surgery, and complications during follow-up, including massive hemorrhage, infections, implant loosening, DVT, and PE.
The patients underwent a total of 74 primary joint replacements (16 hips, 52 knees, and 6 ankles) and 23 revision surgeries.
As noted, there were no episodes of either DVT or PE among any of the patients. All but one complication occurred among patients undergoing total knee replacement. These included three cases of hemarthrosis, three limited-range-of-motion cases requiring closed manipulations, four soft-tissue hematomas, and one case each of superficial wound infection, urinary tract infection, pneumonia, and Candida infection of the tongue.
The only other complication was a case of disseminated intravascular coagulation, sepsis, and hemorrhagic shock in a patient who had undergone a revision (original procedure unspecified).
“Despite the concern that proper replacement factor therapy, applied before and after the surgery, may increase the risk for thromboembolic complications in patients with hemophilia undergoing joint replacement, our data show that prophylactic anticoagulation in this group of patients is not necessary,” the investigators concluded.
The study was internally funded. The investigators reported no conflicts of interest.
ORLANDO – In patients with hemophilia who have therapeutic factor levels at the time of joint replacement surgery, prophylaxis against venous thromboembolism (VTE) may be unnecessary.
In a cohort study of patients with hemophilia A or B who underwent total joint replacement surgery while being in proper hemostasis with therapeutic factor levels, there were no clinically evident episodes of venous thromboembolism, even though none of the patients had received perioperative anticoagulant prophylaxis, reported investigators from the National Hemophilia Center and Institute of Thrombosis and Hemostasis at the Sheba Medical Center in Tel Hashomer, Israel.
The data should be reassuring to clinicians whose patients with hemophilia require major orthopedic procedures, said lead author Dr. Anna Seltser, an orthopedic resident at Sheba Medical Center, in an interview.
“We have a lot of hemophilia patients who are not well treated because they live in the desert or distant communities, and we also sometimes treat patients from the Palestinian side of the Gaza Strip who don’t have access to care and need this type of surgery,” she said.
“We collected what I think is the biggest series of patients until now, we didn’t give any of them VTE prophylaxis, and none of them had any DVT [deep vein thrombosis], PE [pulmonary embolism], or similar complication,” she said.
Skip the heparin?
VTE prophylaxis with low-molecular-weight heparin, warfarin, or other anticoagulant agents is a common practice following orthopedic surgery in patients without bleeding disorders. But for patients with severe hemophilia, who often require major joint replacement surgery following years of bleeding-induced arthropathy, it’s unclear whether perioperative anticoagulation is beneficial, the investigators noted in a scientific poster at the World Federation of Hemophilia World Congress.
Dr. Seltser and colleagues therefore conducted a prospective cohort study of 50 patients with hemophilia A or B treated with major joint surgery and subsequent revisions from 1988 through 2015 at their center. In all, 47 patients had severe hemophilia A, 2 had mild hemophilia A, and 1 had hemophilia B.
The authors analyzed data on demographics, comorbidities, type of surgery, use of factor concentrates therapy around the time of surgery, and complications during follow-up, including massive hemorrhage, infections, implant loosening, DVT, and PE.
The patients underwent a total of 74 primary joint replacements (16 hips, 52 knees, and 6 ankles) and 23 revision surgeries.
As noted, there were no episodes of either DVT or PE among any of the patients. All but one complication occurred among patients undergoing total knee replacement. These included three cases of hemarthrosis, three limited-range-of-motion cases requiring closed manipulations, four soft-tissue hematomas, and one case each of superficial wound infection, urinary tract infection, pneumonia, and Candida infection of the tongue.
The only other complication was a case of disseminated intravascular coagulation, sepsis, and hemorrhagic shock in a patient who had undergone a revision (original procedure unspecified).
“Despite the concern that proper replacement factor therapy, applied before and after the surgery, may increase the risk for thromboembolic complications in patients with hemophilia undergoing joint replacement, our data show that prophylactic anticoagulation in this group of patients is not necessary,” the investigators concluded.
The study was internally funded. The investigators reported no conflicts of interest.
AT WFH 2016 WORLD CONGRESS
Key clinical point: Prophylaxis against thromboembolic events after orthopedic surgery in patients with hemophilia may not be necessary.
Major finding: There were no thromboembolic events after joint surgery without anticoagulant prophylaxis in patients with hemophilia A or B.
Data source: Cohort study of 50 patients with hemophilia A or B undergoing major joint replacement surgery.
Disclosures: The study was internally funded. The investigators reported no conflicts of interest.
Hematuria a common finding in pediatric hemophilia
ORLANDO – Screening urinalysis should be a part of routine care for children and young adults with hemophilia, although the clinical significance of the finding is still unclear, investigators say.
Among 93 boys and young men with hemophilia A or B followed at a hemophilia treatment center, nearly half were found to have hematuria on routine screening, a possible indicator for future renal problems, said Kyle Davis, MD, and Amy Dunn, MD, from the division of hematology at Nationwide Children’s Hospital in Columbus, Ohio.
“It’s not routine for all centers to screen for hematuria, so there is likely a large number of patients that are underrecognized, who have hematuria but we don’t even know it,” Dr. Davis said in an interview at the World Federation of Hemophilia World Congress.
Hematuria is a recognized complication in patients with hemophilia A and B, second only to joint damage in frequency. In addition, adults with hemophilia have been shown to have a higher prevalence of renal disease than the general population, suggesting that hematuria might be a marker or harbinger of later renal disease, the authors proposed in a scientific poster.
The investigators conducted their study as part of a quality improvement program at their center aimed at increasing the frequency of urine screening in patients with hemophilia during annual comprehensive visits.
They looked at urinalysis results collected from all male patients older than 2 years with hemophilia A or B seen at their center from August 2011 through September 2015. They defined hematuria as the presence of three or more red blood cells on at least one urinalysis sample.
They also performed univariate logistic regression to evaluate the association of hematuria with patient age, race, hemophilia type and severity, treatment regimen, and history of inhibitory antibodies.
A total of 93 patients, 67 with hemophilia A and 26 with hemophilia B, were included. In all, 43 patients (47%) were identified as having hematuria, with a median of seven red cells. Hematuria was seen in 37 patients with hemophilia A (55%), and in 6 patients with hemophilia B (23%).
Characteristics associated with risk for hematuria included older age and hemophilia A.
Imaging studies available on 24 of the 93 patients showed renal calculi in 3 patients, minor pelviectasis in 1, and congenital dysplastic left kidney, ureterocele, and right hydroureter in 1 patient.
Dr. Davis and Dr. Dunn said that while screening urinalysis could be considered as a part of routine hemophilia, additional studies are needed to replicate the finding in other treatment centers and to determine whether urinalysis results can be predictive of future renal disease, and if so, whether interventions might help.
“For example, there is the potential that if you recognize hematuria in a patient and that patient is currently on an on-demand treatment process, should we switch to prophylaxis?” Dr Davis said.
Dr. Dunn noted that “certainly there are high-risk populations who should be screened, like our patients who have an active inhibitor or even a tolerized inhibitor. Our data suggest that we ought to be looking a bit more closely at those patients, and perhaps that will help us tease out the cause of this. Can we blame it all on hemophilia, or is there something else going on?”
The study was internally funded. Dr. Davis and Dr. Dunn reported no relevant disclosures.
ORLANDO – Screening urinalysis should be a part of routine care for children and young adults with hemophilia, although the clinical significance of the finding is still unclear, investigators say.
Among 93 boys and young men with hemophilia A or B followed at a hemophilia treatment center, nearly half were found to have hematuria on routine screening, a possible indicator for future renal problems, said Kyle Davis, MD, and Amy Dunn, MD, from the division of hematology at Nationwide Children’s Hospital in Columbus, Ohio.
“It’s not routine for all centers to screen for hematuria, so there is likely a large number of patients that are underrecognized, who have hematuria but we don’t even know it,” Dr. Davis said in an interview at the World Federation of Hemophilia World Congress.
Hematuria is a recognized complication in patients with hemophilia A and B, second only to joint damage in frequency. In addition, adults with hemophilia have been shown to have a higher prevalence of renal disease than the general population, suggesting that hematuria might be a marker or harbinger of later renal disease, the authors proposed in a scientific poster.
The investigators conducted their study as part of a quality improvement program at their center aimed at increasing the frequency of urine screening in patients with hemophilia during annual comprehensive visits.
They looked at urinalysis results collected from all male patients older than 2 years with hemophilia A or B seen at their center from August 2011 through September 2015. They defined hematuria as the presence of three or more red blood cells on at least one urinalysis sample.
They also performed univariate logistic regression to evaluate the association of hematuria with patient age, race, hemophilia type and severity, treatment regimen, and history of inhibitory antibodies.
A total of 93 patients, 67 with hemophilia A and 26 with hemophilia B, were included. In all, 43 patients (47%) were identified as having hematuria, with a median of seven red cells. Hematuria was seen in 37 patients with hemophilia A (55%), and in 6 patients with hemophilia B (23%).
Characteristics associated with risk for hematuria included older age and hemophilia A.
Imaging studies available on 24 of the 93 patients showed renal calculi in 3 patients, minor pelviectasis in 1, and congenital dysplastic left kidney, ureterocele, and right hydroureter in 1 patient.
Dr. Davis and Dr. Dunn said that while screening urinalysis could be considered as a part of routine hemophilia, additional studies are needed to replicate the finding in other treatment centers and to determine whether urinalysis results can be predictive of future renal disease, and if so, whether interventions might help.
“For example, there is the potential that if you recognize hematuria in a patient and that patient is currently on an on-demand treatment process, should we switch to prophylaxis?” Dr Davis said.
Dr. Dunn noted that “certainly there are high-risk populations who should be screened, like our patients who have an active inhibitor or even a tolerized inhibitor. Our data suggest that we ought to be looking a bit more closely at those patients, and perhaps that will help us tease out the cause of this. Can we blame it all on hemophilia, or is there something else going on?”
The study was internally funded. Dr. Davis and Dr. Dunn reported no relevant disclosures.
ORLANDO – Screening urinalysis should be a part of routine care for children and young adults with hemophilia, although the clinical significance of the finding is still unclear, investigators say.
Among 93 boys and young men with hemophilia A or B followed at a hemophilia treatment center, nearly half were found to have hematuria on routine screening, a possible indicator for future renal problems, said Kyle Davis, MD, and Amy Dunn, MD, from the division of hematology at Nationwide Children’s Hospital in Columbus, Ohio.
“It’s not routine for all centers to screen for hematuria, so there is likely a large number of patients that are underrecognized, who have hematuria but we don’t even know it,” Dr. Davis said in an interview at the World Federation of Hemophilia World Congress.
Hematuria is a recognized complication in patients with hemophilia A and B, second only to joint damage in frequency. In addition, adults with hemophilia have been shown to have a higher prevalence of renal disease than the general population, suggesting that hematuria might be a marker or harbinger of later renal disease, the authors proposed in a scientific poster.
The investigators conducted their study as part of a quality improvement program at their center aimed at increasing the frequency of urine screening in patients with hemophilia during annual comprehensive visits.
They looked at urinalysis results collected from all male patients older than 2 years with hemophilia A or B seen at their center from August 2011 through September 2015. They defined hematuria as the presence of three or more red blood cells on at least one urinalysis sample.
They also performed univariate logistic regression to evaluate the association of hematuria with patient age, race, hemophilia type and severity, treatment regimen, and history of inhibitory antibodies.
A total of 93 patients, 67 with hemophilia A and 26 with hemophilia B, were included. In all, 43 patients (47%) were identified as having hematuria, with a median of seven red cells. Hematuria was seen in 37 patients with hemophilia A (55%), and in 6 patients with hemophilia B (23%).
Characteristics associated with risk for hematuria included older age and hemophilia A.
Imaging studies available on 24 of the 93 patients showed renal calculi in 3 patients, minor pelviectasis in 1, and congenital dysplastic left kidney, ureterocele, and right hydroureter in 1 patient.
Dr. Davis and Dr. Dunn said that while screening urinalysis could be considered as a part of routine hemophilia, additional studies are needed to replicate the finding in other treatment centers and to determine whether urinalysis results can be predictive of future renal disease, and if so, whether interventions might help.
“For example, there is the potential that if you recognize hematuria in a patient and that patient is currently on an on-demand treatment process, should we switch to prophylaxis?” Dr Davis said.
Dr. Dunn noted that “certainly there are high-risk populations who should be screened, like our patients who have an active inhibitor or even a tolerized inhibitor. Our data suggest that we ought to be looking a bit more closely at those patients, and perhaps that will help us tease out the cause of this. Can we blame it all on hemophilia, or is there something else going on?”
The study was internally funded. Dr. Davis and Dr. Dunn reported no relevant disclosures.
AT WFH 2016 WORLD CONGRESS
Key clinical point:. Hematuria is a common finding in children with hemophilia A or B.
Major finding: Of 93 patients with hemophilia, 43 (47%) had hematuria findings on routine urinalysis.
Data source:. Prospective study in 67 patients with hemophilia A and 26 with hemophilia B.
Disclosures: The study was internally funded. Dr. Davis and Dr. Dunn reported no relevant disclosures
Hemophilia may not be protective against CVD
ORLANDO – Conventional wisdom holds that persons with hemophilia are at lower risk for death from cardiovascular events than the general population, but there are conflicting data from studies attempting to confirm or refute this notion.
In a prospective, multicenter European study of more than 500 patients with hemophilia, the predicted cardiovascular disease (CVD) event rate was less than half of what was expected, reported Paul R. van der Valk, MD, from University Medical Center in Utrecht, the Netherlands, and colleagues.
In patients with hemophilia, “the leading cause of death seems to be malignancy related and intracranial hemorrhage. Atrial fibrillation is quite common,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
But a second study of 100 patients with hemophilia showed that the bleeding disorder did not appear to offer protection against cardiovascular or thrombotic adverse events, Beatriz Delgado, MD, and colleagues at the Centro Hospitalar São João in Porto, Portugal, also presented in a poster session.
Risk scores considered
The prospective study by Dr. van der Valk and colleagues was designed to assess the incidence of CVD in patients with hemophilia in the Netherlands and the United Kingdom, compared with the general population. They used the QRISK2 cardiovascular risk score (2011 version). This instrument is used to calculate risk of CVD events in adults from 30 to 84 with no history of CVD or statin use.
Among 557 patients with a calculable QRISK2 score at 2 years of follow-up, there were four CVD events, including two cases of ischemic heart disease, one ischemic stroke, and one intracranial hemorrhage. The median 2-year QRISK2 score was 1.7%, and the 10-year risk was 9.0%, which translated in to an expected 9.5 CVD events during 2 years of follow-up.
Among the additional 104 patients who could not have a QRISK2 score calculated because of age over 84, statin use, or history of CVD, there were four CVD events: ischemic heart disease, transient ischemic attack/carotid artery stenosis, myocardial infarction, and intracranial hemorrhage.
Other CVD events occurring in both groups included atrial fibrillation in eight patients, other arrhythmia in three, and, in one patient each, aortic valve pathology, pericarditis, and carotid artery plaque.
Portuguese experience
Dr, Delgado and colleagues noted that although hemophilia has traditionally been regarded as protective against ischemic heart disease or thrombotic events, modern management “has prolonged life expectancy of people with hemophilia and consequently, an associated increase in incidence and prevalence of conditions that affect the general older population, such as cardiovascular disease and hypertension, are expected.”
They conducted a retrospective analysis of 100 adults (69 with hemophilia A, and 31 with hemophilia B) treated at their center. Overall, 29 patients had severe hemophilia A, 20 moderate hemophilia A, and 20 mild hemophilia A. Among patients with hemophilia B, 11 had severe, 15 moderate, and 5 mild disease.
Two patients (one with moderate and one with severe hemophilia) had angina episodes with coronary artery disease and underwent multiple coronary bypass grafts. The patient with severe disease had a disabling ischemic stroke during recovery from bypass surgery, and the patient with moderate hemophilia had an acute myocardial infarction prior to bypass surgery.
Two other patients had transient ischemic strokes from which they recovered without disability.
The main cardiovascular risk factors identified in this population were hypertension, diabetes mellitus, heavy smoking, obesity, and dyslipidemia. All patients were screened for prothrombotic risk, and all patients had negative test results.
“Hemophilia does not seem to have a protective effect against thrombotic/cardiovascular events, mainly in [patients with] coronary artery disease,” the investigators wrote.
Endothelial function
In a study presented in an oral abstract session, Shannon Jackson, MD, of the University of British Columbia in Vancouver found that men with hemophilia appear to have better macrovascular endothelial function but worse microvascular endothelial function than did men with normal clotting parameters.
“Based on endothelial function, contemporary hemophilia cohorts may have a different profile of cardiovascular risk than healthy controls,” she said.
Although they do not have an obvious mechanistic explanation for the differences in microvascular function among patients with hemophilia vs. healthy controls, there is evidence to show that microvascular function is predictive of cardiovascular events independent of other risk factors in otherwise healthy people. Their findings indicate that further study of the association between endothelial function, cardiovascular risk factors, and atherosclerosis among patients with hemophilia is warranted, she said.
Dr. van der Valk and colleagues and Dr. Delgado and colleagues did not disclose funding or conflicts of interest. The study by Dr. Jackson and colleagues was supported by the Canadian Hemophilia Society and Pfizer. She disclosed honoraria for speaking engagements for Biogen, Baxalta, and Pfizer and for participating in scientific advisory boards for Bayer, Pfizer, Baxalta, CLS Behring, and Novo Nordisk.
ORLANDO – Conventional wisdom holds that persons with hemophilia are at lower risk for death from cardiovascular events than the general population, but there are conflicting data from studies attempting to confirm or refute this notion.
In a prospective, multicenter European study of more than 500 patients with hemophilia, the predicted cardiovascular disease (CVD) event rate was less than half of what was expected, reported Paul R. van der Valk, MD, from University Medical Center in Utrecht, the Netherlands, and colleagues.
In patients with hemophilia, “the leading cause of death seems to be malignancy related and intracranial hemorrhage. Atrial fibrillation is quite common,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
But a second study of 100 patients with hemophilia showed that the bleeding disorder did not appear to offer protection against cardiovascular or thrombotic adverse events, Beatriz Delgado, MD, and colleagues at the Centro Hospitalar São João in Porto, Portugal, also presented in a poster session.
Risk scores considered
The prospective study by Dr. van der Valk and colleagues was designed to assess the incidence of CVD in patients with hemophilia in the Netherlands and the United Kingdom, compared with the general population. They used the QRISK2 cardiovascular risk score (2011 version). This instrument is used to calculate risk of CVD events in adults from 30 to 84 with no history of CVD or statin use.
Among 557 patients with a calculable QRISK2 score at 2 years of follow-up, there were four CVD events, including two cases of ischemic heart disease, one ischemic stroke, and one intracranial hemorrhage. The median 2-year QRISK2 score was 1.7%, and the 10-year risk was 9.0%, which translated in to an expected 9.5 CVD events during 2 years of follow-up.
Among the additional 104 patients who could not have a QRISK2 score calculated because of age over 84, statin use, or history of CVD, there were four CVD events: ischemic heart disease, transient ischemic attack/carotid artery stenosis, myocardial infarction, and intracranial hemorrhage.
Other CVD events occurring in both groups included atrial fibrillation in eight patients, other arrhythmia in three, and, in one patient each, aortic valve pathology, pericarditis, and carotid artery plaque.
Portuguese experience
Dr, Delgado and colleagues noted that although hemophilia has traditionally been regarded as protective against ischemic heart disease or thrombotic events, modern management “has prolonged life expectancy of people with hemophilia and consequently, an associated increase in incidence and prevalence of conditions that affect the general older population, such as cardiovascular disease and hypertension, are expected.”
They conducted a retrospective analysis of 100 adults (69 with hemophilia A, and 31 with hemophilia B) treated at their center. Overall, 29 patients had severe hemophilia A, 20 moderate hemophilia A, and 20 mild hemophilia A. Among patients with hemophilia B, 11 had severe, 15 moderate, and 5 mild disease.
Two patients (one with moderate and one with severe hemophilia) had angina episodes with coronary artery disease and underwent multiple coronary bypass grafts. The patient with severe disease had a disabling ischemic stroke during recovery from bypass surgery, and the patient with moderate hemophilia had an acute myocardial infarction prior to bypass surgery.
Two other patients had transient ischemic strokes from which they recovered without disability.
The main cardiovascular risk factors identified in this population were hypertension, diabetes mellitus, heavy smoking, obesity, and dyslipidemia. All patients were screened for prothrombotic risk, and all patients had negative test results.
“Hemophilia does not seem to have a protective effect against thrombotic/cardiovascular events, mainly in [patients with] coronary artery disease,” the investigators wrote.
Endothelial function
In a study presented in an oral abstract session, Shannon Jackson, MD, of the University of British Columbia in Vancouver found that men with hemophilia appear to have better macrovascular endothelial function but worse microvascular endothelial function than did men with normal clotting parameters.
“Based on endothelial function, contemporary hemophilia cohorts may have a different profile of cardiovascular risk than healthy controls,” she said.
Although they do not have an obvious mechanistic explanation for the differences in microvascular function among patients with hemophilia vs. healthy controls, there is evidence to show that microvascular function is predictive of cardiovascular events independent of other risk factors in otherwise healthy people. Their findings indicate that further study of the association between endothelial function, cardiovascular risk factors, and atherosclerosis among patients with hemophilia is warranted, she said.
Dr. van der Valk and colleagues and Dr. Delgado and colleagues did not disclose funding or conflicts of interest. The study by Dr. Jackson and colleagues was supported by the Canadian Hemophilia Society and Pfizer. She disclosed honoraria for speaking engagements for Biogen, Baxalta, and Pfizer and for participating in scientific advisory boards for Bayer, Pfizer, Baxalta, CLS Behring, and Novo Nordisk.
ORLANDO – Conventional wisdom holds that persons with hemophilia are at lower risk for death from cardiovascular events than the general population, but there are conflicting data from studies attempting to confirm or refute this notion.
In a prospective, multicenter European study of more than 500 patients with hemophilia, the predicted cardiovascular disease (CVD) event rate was less than half of what was expected, reported Paul R. van der Valk, MD, from University Medical Center in Utrecht, the Netherlands, and colleagues.
In patients with hemophilia, “the leading cause of death seems to be malignancy related and intracranial hemorrhage. Atrial fibrillation is quite common,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
But a second study of 100 patients with hemophilia showed that the bleeding disorder did not appear to offer protection against cardiovascular or thrombotic adverse events, Beatriz Delgado, MD, and colleagues at the Centro Hospitalar São João in Porto, Portugal, also presented in a poster session.
Risk scores considered
The prospective study by Dr. van der Valk and colleagues was designed to assess the incidence of CVD in patients with hemophilia in the Netherlands and the United Kingdom, compared with the general population. They used the QRISK2 cardiovascular risk score (2011 version). This instrument is used to calculate risk of CVD events in adults from 30 to 84 with no history of CVD or statin use.
Among 557 patients with a calculable QRISK2 score at 2 years of follow-up, there were four CVD events, including two cases of ischemic heart disease, one ischemic stroke, and one intracranial hemorrhage. The median 2-year QRISK2 score was 1.7%, and the 10-year risk was 9.0%, which translated in to an expected 9.5 CVD events during 2 years of follow-up.
Among the additional 104 patients who could not have a QRISK2 score calculated because of age over 84, statin use, or history of CVD, there were four CVD events: ischemic heart disease, transient ischemic attack/carotid artery stenosis, myocardial infarction, and intracranial hemorrhage.
Other CVD events occurring in both groups included atrial fibrillation in eight patients, other arrhythmia in three, and, in one patient each, aortic valve pathology, pericarditis, and carotid artery plaque.
Portuguese experience
Dr, Delgado and colleagues noted that although hemophilia has traditionally been regarded as protective against ischemic heart disease or thrombotic events, modern management “has prolonged life expectancy of people with hemophilia and consequently, an associated increase in incidence and prevalence of conditions that affect the general older population, such as cardiovascular disease and hypertension, are expected.”
They conducted a retrospective analysis of 100 adults (69 with hemophilia A, and 31 with hemophilia B) treated at their center. Overall, 29 patients had severe hemophilia A, 20 moderate hemophilia A, and 20 mild hemophilia A. Among patients with hemophilia B, 11 had severe, 15 moderate, and 5 mild disease.
Two patients (one with moderate and one with severe hemophilia) had angina episodes with coronary artery disease and underwent multiple coronary bypass grafts. The patient with severe disease had a disabling ischemic stroke during recovery from bypass surgery, and the patient with moderate hemophilia had an acute myocardial infarction prior to bypass surgery.
Two other patients had transient ischemic strokes from which they recovered without disability.
The main cardiovascular risk factors identified in this population were hypertension, diabetes mellitus, heavy smoking, obesity, and dyslipidemia. All patients were screened for prothrombotic risk, and all patients had negative test results.
“Hemophilia does not seem to have a protective effect against thrombotic/cardiovascular events, mainly in [patients with] coronary artery disease,” the investigators wrote.
Endothelial function
In a study presented in an oral abstract session, Shannon Jackson, MD, of the University of British Columbia in Vancouver found that men with hemophilia appear to have better macrovascular endothelial function but worse microvascular endothelial function than did men with normal clotting parameters.
“Based on endothelial function, contemporary hemophilia cohorts may have a different profile of cardiovascular risk than healthy controls,” she said.
Although they do not have an obvious mechanistic explanation for the differences in microvascular function among patients with hemophilia vs. healthy controls, there is evidence to show that microvascular function is predictive of cardiovascular events independent of other risk factors in otherwise healthy people. Their findings indicate that further study of the association between endothelial function, cardiovascular risk factors, and atherosclerosis among patients with hemophilia is warranted, she said.
Dr. van der Valk and colleagues and Dr. Delgado and colleagues did not disclose funding or conflicts of interest. The study by Dr. Jackson and colleagues was supported by the Canadian Hemophilia Society and Pfizer. She disclosed honoraria for speaking engagements for Biogen, Baxalta, and Pfizer and for participating in scientific advisory boards for Bayer, Pfizer, Baxalta, CLS Behring, and Novo Nordisk.
At WFH 2016 World Congress
Key clinical point: Hemophilia has traditionally been considered protective against CVD but data presented at the World Federation of Hemophilia World Congress show conflicting results.Major finding: The CVD event rate in one study was lower than predicted by risk scores, but a separate study showed a higher rate of events. A third study suggests that men with hemophilia have worse microvascular endothelial function than men without bleeding disorders.
Data source: Two prospective and one retrospective study of CVD in patients with hemophilia.
Disclosures: Dr. van der Valk and colleagues and Dr. Delgado and colleagues did not disclose funding or conflicts of interest. The study by Dr. Jackson and colleagues was supported by the Canadian Hemophilia Society and Pfizer. She disclosed honoraria for speaking engagements for Biogen, Baxalta, and Pfizer and for participating in scientific advisory boards for Bayer, Pfizer, Baxalta, CLS Behring, and Novo Nordisk.
Age, not infusion frequency, affects hemophilia prophylaxis adherence
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
AT WFH 2016 WORLD CONGRESS
Key clinical point: Adherence to hemophilia prophylaxis regimens may be influenced by age but not frequency of infusions.
Major finding: Infusion frequency did not make a difference in adherence rates, but young and middle-aged adults reported lower adherence than did children or seniors.
Data source: A study of 23 pediatric hemophilia patients in Canada, and a separate study of 364 children and adults with moderate to severe hemophilia in Germany.
Disclosures: Both studies were internally funded. The authors reported no relevant disclosures.