User login
Medicare Advantage: The good, the bad, and the ugly
As of 2023, most people eligible for Medicare are enrolled in Medicare Advantage plans administered by commercial insurers, rather than traditional Medicare plans sponsored by the federal government. The Kaiser Family Foundation reports that 31 million people are now enrolled in a Medicare Advantage plan, with almost half of them (47%) served by United Healthcare or Humana.
This is 51% of all people eligible for Medicare, compared with 19% in 2007. The Congressional Budget Office projects that 62% of Medicare participants will be in Medicare Advantage plans by 2033.
Given the explosive growth in Medicare Advantage participation, many readers have likely seen patients served by Medicare Advantage or will soon. Below is information about the program’s purpose, strengths, limitations, and effect on physicians.
How does Medicare Advantage differ from traditional Medicare?
A Medicare Advantage plan is approved by the U.S. Centers for Medicare & Medicaid Services and competes for customers by offering lower premiums and/or more benefits. Traditional Medicare plans are unified contracts across the country, with the same fees for the same services paid nationwide.
CMS pays Medicare Advantage plans a per-member rate, which can be increased for people who seem sicker than other plan participants – for example, someone with uncontrolled diabetes and multiple comorbidities. This so-called “risk adjustment” doesn’t exist in traditional Medicare.
CMS also gives incentive payments to Medicare Advantage plans whose members receive better care, measured by such metrics as lower unnecessary hospital admissions. There are some analogues to this in traditional Medicare, such as the Making Care Primary program, but value-based care is a larger component of Medicare Advantage.
“Being paid for outcomes is what we as physicians always thought we went into medicine to do,” said Sarah Candler, MD, an internist in Houston. She most recently worked for One Medical and her experiences with Veterans Affairs and One Medical focused on value-based contracts, including for Medicare Advantage plans.
How do patients benefit from Medicare Advantage?
“Honestly the financial benefits to patients are what’s really driving the rise in Medicare Advantage,” said
Claire Ankuda, MD, MPH, is a geriatrician at the Icahn School of Medicine at Mt. Sinai in New York who has published extensively about Medicare Advantage.
A spokesperson for Highmark Health, which provides Medicare Advantage plans, told us that “Medicare Advantage plans are offered by private health insurers, such as Highmark, and typically offer benefits that support members’ total health, such as low-cost access to doctors and preventive care, and cover things like prescription drugs, vision, and hearing services, dental, and chiropractic care. Medicare Advantage plans also protect members from unforeseen costs like hospitalizations, surgery, or an expensive drug. And unlike traditional Medicare, Medicare Advantage plans can offer set copays for doctor’s visits (rather than coinsurance) to help members budget for their costs.”
Dr. Ankuda said hospitalization costs are sometimes higher for Medicare Advantage but agreed that costs for doctor visits are often lower with Medicare Advantage plans than with traditional Medicare.
So while the overarching goal of Medicare Advantage makes sense, Dr. Candler said, the actual physician experience of working with Medicare Advantage can be challenging.
What challenges might physicians experience when treating patients in a Medicare Advantage plan?
“The plan itself has control over what it will pay for and they’re much more aggressive about it than traditional Medicare,” Dr. Candler said. Medicare Advantage plans are often structured as health maintenance organizations, with narrow provider networks and extensive prior authorization requirements.
Dr. Candler gave an example of a plan that offers transportation to medical appointments – a seemingly great benefit. But what if someone needs to see a cardiologist and the only cardiologist within the plan is 100 miles away? That’s too far for the transportation benefit, it turns out.
Or a Medicare Advantage plan requires a physician to first do a physical exam before ordering an MRI, even though in the physician’s judgment only the MRI will have diagnostic value. Or the plan denies coverage for a service that’s already occurred. These practices aim to weed out unnecessary care but at the cost of patient confusion or physician time in arguing why something should be covered.
“The argument from us as physicians would be, ‘Just trust us to practice good medicine,’” Dr. Candler said.
Beside these concerns at the physician level, the regulations surrounding Medicare Advantage plans may open the door to billing fraud.
How do Medicare Advantage Plans interact with diagnosis codes?
“I just can’t stand when I see fraud in the health care system,” said Nancy Keating, MD, MPH, an internist at Brigham and Women’s Hospital and a health policy professor at Harvard Medical School, both in Boston.
This July, Dr. Keating published a report in the Annals of Internal Medicine about a patient of hers whose health insurer – a Medicare Advantage plan – claimed had diabetes with comorbidities and was morbidly obese. None of this was true. But submitting such diagnoses to CMS would suggest that Dr. Keating’s patient was especially ill, leading to greater reimbursements from CMS for covering her care.
“I’m not averse to paying plans that are taking care of sicker patients more, but we need to figure out who those patients truly are,” Dr. Keating said.
“It is absolutely true and widely proven that Medicare Advantage plans do a lot of clever things” to inflate diagnoses, added Dr. Ankuda. Also, she said that Medicare Advantage plan representatives would say this is legitimate work, as the entire point of Medicare Advantage is to pay more for caring for sicker patients.
“I don’t think anyone here is acting in bad faith. It’s just that [there are] very different incentives,” Dr. Ankuda said.
How can Medicare Advantage be improved?
Dr. Keating believes that CMS should reduce the number of diagnosis codes allowed within Medicare Advantage to thwart the potential for upcoding. Dr. Ankuda thinks the biggest problem is that there is no good way for patients to choose among Medicare Advantage plans.
“I don’t see it as Medicare Advantage is bad or Medicare Advantage is good. MA plans are incredibly diverse,” Dr. Ankuda said. The problem is that it’s very hard for patients to tell which plans are delivering the best care, what their out-of-pocket costs will actually be, or how often a plan denies payment.
Dr. Ankuda argues for much more data transparency around such plan factors.
Dr. Candler and Dr. Ankuda had no relevant conflicts. Dr. Keating is a consultant to the Research Triangle Institute, which advises CMS about Medicare Advantage billing codes.
As of 2023, most people eligible for Medicare are enrolled in Medicare Advantage plans administered by commercial insurers, rather than traditional Medicare plans sponsored by the federal government. The Kaiser Family Foundation reports that 31 million people are now enrolled in a Medicare Advantage plan, with almost half of them (47%) served by United Healthcare or Humana.
This is 51% of all people eligible for Medicare, compared with 19% in 2007. The Congressional Budget Office projects that 62% of Medicare participants will be in Medicare Advantage plans by 2033.
Given the explosive growth in Medicare Advantage participation, many readers have likely seen patients served by Medicare Advantage or will soon. Below is information about the program’s purpose, strengths, limitations, and effect on physicians.
How does Medicare Advantage differ from traditional Medicare?
A Medicare Advantage plan is approved by the U.S. Centers for Medicare & Medicaid Services and competes for customers by offering lower premiums and/or more benefits. Traditional Medicare plans are unified contracts across the country, with the same fees for the same services paid nationwide.
CMS pays Medicare Advantage plans a per-member rate, which can be increased for people who seem sicker than other plan participants – for example, someone with uncontrolled diabetes and multiple comorbidities. This so-called “risk adjustment” doesn’t exist in traditional Medicare.
CMS also gives incentive payments to Medicare Advantage plans whose members receive better care, measured by such metrics as lower unnecessary hospital admissions. There are some analogues to this in traditional Medicare, such as the Making Care Primary program, but value-based care is a larger component of Medicare Advantage.
“Being paid for outcomes is what we as physicians always thought we went into medicine to do,” said Sarah Candler, MD, an internist in Houston. She most recently worked for One Medical and her experiences with Veterans Affairs and One Medical focused on value-based contracts, including for Medicare Advantage plans.
How do patients benefit from Medicare Advantage?
“Honestly the financial benefits to patients are what’s really driving the rise in Medicare Advantage,” said
Claire Ankuda, MD, MPH, is a geriatrician at the Icahn School of Medicine at Mt. Sinai in New York who has published extensively about Medicare Advantage.
A spokesperson for Highmark Health, which provides Medicare Advantage plans, told us that “Medicare Advantage plans are offered by private health insurers, such as Highmark, and typically offer benefits that support members’ total health, such as low-cost access to doctors and preventive care, and cover things like prescription drugs, vision, and hearing services, dental, and chiropractic care. Medicare Advantage plans also protect members from unforeseen costs like hospitalizations, surgery, or an expensive drug. And unlike traditional Medicare, Medicare Advantage plans can offer set copays for doctor’s visits (rather than coinsurance) to help members budget for their costs.”
Dr. Ankuda said hospitalization costs are sometimes higher for Medicare Advantage but agreed that costs for doctor visits are often lower with Medicare Advantage plans than with traditional Medicare.
So while the overarching goal of Medicare Advantage makes sense, Dr. Candler said, the actual physician experience of working with Medicare Advantage can be challenging.
What challenges might physicians experience when treating patients in a Medicare Advantage plan?
“The plan itself has control over what it will pay for and they’re much more aggressive about it than traditional Medicare,” Dr. Candler said. Medicare Advantage plans are often structured as health maintenance organizations, with narrow provider networks and extensive prior authorization requirements.
Dr. Candler gave an example of a plan that offers transportation to medical appointments – a seemingly great benefit. But what if someone needs to see a cardiologist and the only cardiologist within the plan is 100 miles away? That’s too far for the transportation benefit, it turns out.
Or a Medicare Advantage plan requires a physician to first do a physical exam before ordering an MRI, even though in the physician’s judgment only the MRI will have diagnostic value. Or the plan denies coverage for a service that’s already occurred. These practices aim to weed out unnecessary care but at the cost of patient confusion or physician time in arguing why something should be covered.
“The argument from us as physicians would be, ‘Just trust us to practice good medicine,’” Dr. Candler said.
Beside these concerns at the physician level, the regulations surrounding Medicare Advantage plans may open the door to billing fraud.
How do Medicare Advantage Plans interact with diagnosis codes?
“I just can’t stand when I see fraud in the health care system,” said Nancy Keating, MD, MPH, an internist at Brigham and Women’s Hospital and a health policy professor at Harvard Medical School, both in Boston.
This July, Dr. Keating published a report in the Annals of Internal Medicine about a patient of hers whose health insurer – a Medicare Advantage plan – claimed had diabetes with comorbidities and was morbidly obese. None of this was true. But submitting such diagnoses to CMS would suggest that Dr. Keating’s patient was especially ill, leading to greater reimbursements from CMS for covering her care.
“I’m not averse to paying plans that are taking care of sicker patients more, but we need to figure out who those patients truly are,” Dr. Keating said.
“It is absolutely true and widely proven that Medicare Advantage plans do a lot of clever things” to inflate diagnoses, added Dr. Ankuda. Also, she said that Medicare Advantage plan representatives would say this is legitimate work, as the entire point of Medicare Advantage is to pay more for caring for sicker patients.
“I don’t think anyone here is acting in bad faith. It’s just that [there are] very different incentives,” Dr. Ankuda said.
How can Medicare Advantage be improved?
Dr. Keating believes that CMS should reduce the number of diagnosis codes allowed within Medicare Advantage to thwart the potential for upcoding. Dr. Ankuda thinks the biggest problem is that there is no good way for patients to choose among Medicare Advantage plans.
“I don’t see it as Medicare Advantage is bad or Medicare Advantage is good. MA plans are incredibly diverse,” Dr. Ankuda said. The problem is that it’s very hard for patients to tell which plans are delivering the best care, what their out-of-pocket costs will actually be, or how often a plan denies payment.
Dr. Ankuda argues for much more data transparency around such plan factors.
Dr. Candler and Dr. Ankuda had no relevant conflicts. Dr. Keating is a consultant to the Research Triangle Institute, which advises CMS about Medicare Advantage billing codes.
As of 2023, most people eligible for Medicare are enrolled in Medicare Advantage plans administered by commercial insurers, rather than traditional Medicare plans sponsored by the federal government. The Kaiser Family Foundation reports that 31 million people are now enrolled in a Medicare Advantage plan, with almost half of them (47%) served by United Healthcare or Humana.
This is 51% of all people eligible for Medicare, compared with 19% in 2007. The Congressional Budget Office projects that 62% of Medicare participants will be in Medicare Advantage plans by 2033.
Given the explosive growth in Medicare Advantage participation, many readers have likely seen patients served by Medicare Advantage or will soon. Below is information about the program’s purpose, strengths, limitations, and effect on physicians.
How does Medicare Advantage differ from traditional Medicare?
A Medicare Advantage plan is approved by the U.S. Centers for Medicare & Medicaid Services and competes for customers by offering lower premiums and/or more benefits. Traditional Medicare plans are unified contracts across the country, with the same fees for the same services paid nationwide.
CMS pays Medicare Advantage plans a per-member rate, which can be increased for people who seem sicker than other plan participants – for example, someone with uncontrolled diabetes and multiple comorbidities. This so-called “risk adjustment” doesn’t exist in traditional Medicare.
CMS also gives incentive payments to Medicare Advantage plans whose members receive better care, measured by such metrics as lower unnecessary hospital admissions. There are some analogues to this in traditional Medicare, such as the Making Care Primary program, but value-based care is a larger component of Medicare Advantage.
“Being paid for outcomes is what we as physicians always thought we went into medicine to do,” said Sarah Candler, MD, an internist in Houston. She most recently worked for One Medical and her experiences with Veterans Affairs and One Medical focused on value-based contracts, including for Medicare Advantage plans.
How do patients benefit from Medicare Advantage?
“Honestly the financial benefits to patients are what’s really driving the rise in Medicare Advantage,” said
Claire Ankuda, MD, MPH, is a geriatrician at the Icahn School of Medicine at Mt. Sinai in New York who has published extensively about Medicare Advantage.
A spokesperson for Highmark Health, which provides Medicare Advantage plans, told us that “Medicare Advantage plans are offered by private health insurers, such as Highmark, and typically offer benefits that support members’ total health, such as low-cost access to doctors and preventive care, and cover things like prescription drugs, vision, and hearing services, dental, and chiropractic care. Medicare Advantage plans also protect members from unforeseen costs like hospitalizations, surgery, or an expensive drug. And unlike traditional Medicare, Medicare Advantage plans can offer set copays for doctor’s visits (rather than coinsurance) to help members budget for their costs.”
Dr. Ankuda said hospitalization costs are sometimes higher for Medicare Advantage but agreed that costs for doctor visits are often lower with Medicare Advantage plans than with traditional Medicare.
So while the overarching goal of Medicare Advantage makes sense, Dr. Candler said, the actual physician experience of working with Medicare Advantage can be challenging.
What challenges might physicians experience when treating patients in a Medicare Advantage plan?
“The plan itself has control over what it will pay for and they’re much more aggressive about it than traditional Medicare,” Dr. Candler said. Medicare Advantage plans are often structured as health maintenance organizations, with narrow provider networks and extensive prior authorization requirements.
Dr. Candler gave an example of a plan that offers transportation to medical appointments – a seemingly great benefit. But what if someone needs to see a cardiologist and the only cardiologist within the plan is 100 miles away? That’s too far for the transportation benefit, it turns out.
Or a Medicare Advantage plan requires a physician to first do a physical exam before ordering an MRI, even though in the physician’s judgment only the MRI will have diagnostic value. Or the plan denies coverage for a service that’s already occurred. These practices aim to weed out unnecessary care but at the cost of patient confusion or physician time in arguing why something should be covered.
“The argument from us as physicians would be, ‘Just trust us to practice good medicine,’” Dr. Candler said.
Beside these concerns at the physician level, the regulations surrounding Medicare Advantage plans may open the door to billing fraud.
How do Medicare Advantage Plans interact with diagnosis codes?
“I just can’t stand when I see fraud in the health care system,” said Nancy Keating, MD, MPH, an internist at Brigham and Women’s Hospital and a health policy professor at Harvard Medical School, both in Boston.
This July, Dr. Keating published a report in the Annals of Internal Medicine about a patient of hers whose health insurer – a Medicare Advantage plan – claimed had diabetes with comorbidities and was morbidly obese. None of this was true. But submitting such diagnoses to CMS would suggest that Dr. Keating’s patient was especially ill, leading to greater reimbursements from CMS for covering her care.
“I’m not averse to paying plans that are taking care of sicker patients more, but we need to figure out who those patients truly are,” Dr. Keating said.
“It is absolutely true and widely proven that Medicare Advantage plans do a lot of clever things” to inflate diagnoses, added Dr. Ankuda. Also, she said that Medicare Advantage plan representatives would say this is legitimate work, as the entire point of Medicare Advantage is to pay more for caring for sicker patients.
“I don’t think anyone here is acting in bad faith. It’s just that [there are] very different incentives,” Dr. Ankuda said.
How can Medicare Advantage be improved?
Dr. Keating believes that CMS should reduce the number of diagnosis codes allowed within Medicare Advantage to thwart the potential for upcoding. Dr. Ankuda thinks the biggest problem is that there is no good way for patients to choose among Medicare Advantage plans.
“I don’t see it as Medicare Advantage is bad or Medicare Advantage is good. MA plans are incredibly diverse,” Dr. Ankuda said. The problem is that it’s very hard for patients to tell which plans are delivering the best care, what their out-of-pocket costs will actually be, or how often a plan denies payment.
Dr. Ankuda argues for much more data transparency around such plan factors.
Dr. Candler and Dr. Ankuda had no relevant conflicts. Dr. Keating is a consultant to the Research Triangle Institute, which advises CMS about Medicare Advantage billing codes.
Not another emergency
This country faces a broad and frightening rogues’ gallery of challenges to its health. From the recent revelation that gunshots are the leading cause of death in children to the opioid epidemic to the overworked and discouraged health care providers, the crises are so numerous it is hard to choose where we should be investing what little political will we can muster. And, where do these disasters fit against a landscape raked by natural and climate change–triggered catastrophes? How do we even begin to triage our vocabulary as we are trying to label them?
The lead article in October’s journal Pediatrics makes a heroic effort to place pediatric obesity into this pantheon of health disasters. The authors of this Pediatrics Perspective ask a simple question: Should the United States declare pediatric obesity a public health emergency? They have wisely chosen to narrow the question to the pediatric population as being a more realistic target and one that is more likely to pay bigger dividends over time.
While acknowledging that obesity prevention strategies have been largely ineffective to this point, the authors are also concerned that despite the promising development of treatment strategies, the rollout of these therapies is likely to be uneven because of funding and disparities in health care delivery.
After reviewing pros and cons for an emergency declaration, they came to the conclusion that despite the scope of the problem and the fact that health emergencies have been declared for conditions effecting fewer individuals, now is not the time. The authors observed that a declaration may serve only to hype “the problem without offering tangible solutions.” Even when as yet to be discovered effective therapies become available, the time lag before measurable improvement is likely to be so delayed that “catastrophizing” pediatric obesity may be just another exercise in wolf-crying.
A closer look
While I applaud the authors for their courage in addressing this question and their decision to discourage an emergency declaration, a few of their observations deserve a closer look. First, they are legitimately concerned that any health policy must be careful not to further perpetuate the stigmatization of children with obesity. However, they feel the recognition by all stakeholders “that obesity is a genetically and biologically driven disease are essential.” While I have supported the disease designation as a pragmatic strategy to move things forward, I would prefer their statement to read “obesity can be ... “ I don’t think we have mined the data deep enough to determine how many out of a cohort of a million obese children from across a wide span of socioeconomic strata have become obese primarily as a result of decisions made by school departments, parents, and governmental entities – all of which had the resources to make healthier decisions but failed to do so.
While a majority of the population may believe that obesity is a “condition of choice,” I think they would be more likely to support the political will for action if they saw data that acknowledges that yes, obesity can be a condition of choice, but here are the circumstances in which choice can and can’t make a difference. Language must always be chosen carefully to minimize stigmatization. However, remember we are not pointing fingers at victims; we are instead looking for teaching moments in which adults can learn to make better choices for the children under their care who are too young to make their own.
Finally, as the authors of this Pediatric Perspectives considered cons of a declaration of health care emergency, they raised the peculiarly American concern of personal autonomy. As they pointed out, there are unfortunate examples in this country in which efforts to limit personal choice have backfired and well-meaning and potentially effective methods for limiting unhealthy behaviors have been eliminated in the name of personal freedom. I’m not sure how we manage this except to wait and be judicious as we move forward addressing pediatric obesity on a national scale. I urge you to take a few minutes to read this perspective. It is a topic worth considering.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
This country faces a broad and frightening rogues’ gallery of challenges to its health. From the recent revelation that gunshots are the leading cause of death in children to the opioid epidemic to the overworked and discouraged health care providers, the crises are so numerous it is hard to choose where we should be investing what little political will we can muster. And, where do these disasters fit against a landscape raked by natural and climate change–triggered catastrophes? How do we even begin to triage our vocabulary as we are trying to label them?
The lead article in October’s journal Pediatrics makes a heroic effort to place pediatric obesity into this pantheon of health disasters. The authors of this Pediatrics Perspective ask a simple question: Should the United States declare pediatric obesity a public health emergency? They have wisely chosen to narrow the question to the pediatric population as being a more realistic target and one that is more likely to pay bigger dividends over time.
While acknowledging that obesity prevention strategies have been largely ineffective to this point, the authors are also concerned that despite the promising development of treatment strategies, the rollout of these therapies is likely to be uneven because of funding and disparities in health care delivery.
After reviewing pros and cons for an emergency declaration, they came to the conclusion that despite the scope of the problem and the fact that health emergencies have been declared for conditions effecting fewer individuals, now is not the time. The authors observed that a declaration may serve only to hype “the problem without offering tangible solutions.” Even when as yet to be discovered effective therapies become available, the time lag before measurable improvement is likely to be so delayed that “catastrophizing” pediatric obesity may be just another exercise in wolf-crying.
A closer look
While I applaud the authors for their courage in addressing this question and their decision to discourage an emergency declaration, a few of their observations deserve a closer look. First, they are legitimately concerned that any health policy must be careful not to further perpetuate the stigmatization of children with obesity. However, they feel the recognition by all stakeholders “that obesity is a genetically and biologically driven disease are essential.” While I have supported the disease designation as a pragmatic strategy to move things forward, I would prefer their statement to read “obesity can be ... “ I don’t think we have mined the data deep enough to determine how many out of a cohort of a million obese children from across a wide span of socioeconomic strata have become obese primarily as a result of decisions made by school departments, parents, and governmental entities – all of which had the resources to make healthier decisions but failed to do so.
While a majority of the population may believe that obesity is a “condition of choice,” I think they would be more likely to support the political will for action if they saw data that acknowledges that yes, obesity can be a condition of choice, but here are the circumstances in which choice can and can’t make a difference. Language must always be chosen carefully to minimize stigmatization. However, remember we are not pointing fingers at victims; we are instead looking for teaching moments in which adults can learn to make better choices for the children under their care who are too young to make their own.
Finally, as the authors of this Pediatric Perspectives considered cons of a declaration of health care emergency, they raised the peculiarly American concern of personal autonomy. As they pointed out, there are unfortunate examples in this country in which efforts to limit personal choice have backfired and well-meaning and potentially effective methods for limiting unhealthy behaviors have been eliminated in the name of personal freedom. I’m not sure how we manage this except to wait and be judicious as we move forward addressing pediatric obesity on a national scale. I urge you to take a few minutes to read this perspective. It is a topic worth considering.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
This country faces a broad and frightening rogues’ gallery of challenges to its health. From the recent revelation that gunshots are the leading cause of death in children to the opioid epidemic to the overworked and discouraged health care providers, the crises are so numerous it is hard to choose where we should be investing what little political will we can muster. And, where do these disasters fit against a landscape raked by natural and climate change–triggered catastrophes? How do we even begin to triage our vocabulary as we are trying to label them?
The lead article in October’s journal Pediatrics makes a heroic effort to place pediatric obesity into this pantheon of health disasters. The authors of this Pediatrics Perspective ask a simple question: Should the United States declare pediatric obesity a public health emergency? They have wisely chosen to narrow the question to the pediatric population as being a more realistic target and one that is more likely to pay bigger dividends over time.
While acknowledging that obesity prevention strategies have been largely ineffective to this point, the authors are also concerned that despite the promising development of treatment strategies, the rollout of these therapies is likely to be uneven because of funding and disparities in health care delivery.
After reviewing pros and cons for an emergency declaration, they came to the conclusion that despite the scope of the problem and the fact that health emergencies have been declared for conditions effecting fewer individuals, now is not the time. The authors observed that a declaration may serve only to hype “the problem without offering tangible solutions.” Even when as yet to be discovered effective therapies become available, the time lag before measurable improvement is likely to be so delayed that “catastrophizing” pediatric obesity may be just another exercise in wolf-crying.
A closer look
While I applaud the authors for their courage in addressing this question and their decision to discourage an emergency declaration, a few of their observations deserve a closer look. First, they are legitimately concerned that any health policy must be careful not to further perpetuate the stigmatization of children with obesity. However, they feel the recognition by all stakeholders “that obesity is a genetically and biologically driven disease are essential.” While I have supported the disease designation as a pragmatic strategy to move things forward, I would prefer their statement to read “obesity can be ... “ I don’t think we have mined the data deep enough to determine how many out of a cohort of a million obese children from across a wide span of socioeconomic strata have become obese primarily as a result of decisions made by school departments, parents, and governmental entities – all of which had the resources to make healthier decisions but failed to do so.
While a majority of the population may believe that obesity is a “condition of choice,” I think they would be more likely to support the political will for action if they saw data that acknowledges that yes, obesity can be a condition of choice, but here are the circumstances in which choice can and can’t make a difference. Language must always be chosen carefully to minimize stigmatization. However, remember we are not pointing fingers at victims; we are instead looking for teaching moments in which adults can learn to make better choices for the children under their care who are too young to make their own.
Finally, as the authors of this Pediatric Perspectives considered cons of a declaration of health care emergency, they raised the peculiarly American concern of personal autonomy. As they pointed out, there are unfortunate examples in this country in which efforts to limit personal choice have backfired and well-meaning and potentially effective methods for limiting unhealthy behaviors have been eliminated in the name of personal freedom. I’m not sure how we manage this except to wait and be judicious as we move forward addressing pediatric obesity on a national scale. I urge you to take a few minutes to read this perspective. It is a topic worth considering.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
My pet peeves about the current state of primary care
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Employed physicians: A survival guide
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Artificial intelligence in the office: Part 2
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
Prior authorization software: Saves time but hurdles remain
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
Docs weigh in on insurance coverage for obesity medications
You can’t argue with success, unless you are an insurance company faced with covering medications shown to improve obesity.
The ability of drugs originally designed for diabetes management to reduce body weight has spiked demand and taxed supplies, according to the U.S. Food and Drug Administration, which included semaglutide (both Wegovy and Ozempic) on its Drug Shortages List as of May 31, 2023.
Meanwhile, clinicians and patients report that insurance companies are pushing back against coverage of these medications that mimic glucagon-like peptide 1 (GLP-1) because of the costs. A recent study conducted by Prime Therapeutics, a pharmacy benefit management organization, showed that individuals who started GLP-1 drugs for weight loss and who were adherent to the treatment averaged a 59% increase in health care costs after 1 year; for those in a subgroup analysis who were treatment adherent, the increase in health care costs was 98%.
“Insurance coverage for obesity treatment is challenging, particularly regarding medications,” said Scott Kahan, MD, director of the National Center for Weight and Wellness at George Washington University, Washington, in an interview. Employers must opt in for patients to have coverage for these medications; therefore, relatively few patients have had access at reasonable out-of-pocket costs, he said.
For example, the University of Texas stated on its website that its prescription drug plans will no longer cover drugs with the active ingredients semaglutide (Wegovy) or liraglutide (Saxenda) for weight loss as of Sept. 1, 2023. Both products are FDA-approved for weight management, whereas the equally popular Ozempic is currently approved only as a treatment for diabetes. The school’s website noted that the current price of the drugs, which cost the plan more than $5 million per month as of May 2023, outstrips the most expensive cancer agents.
The University of Texas also found that among its patients, the compliance rate for those who began Wegovy or Saxenda for weight loss was only 46%, which was not enough to justify continued coverage. The plan advised patients to approach their insurers directly.
Eventually, more information may prompt more support from insurance across a range of medications, Dr. Kahan noted. “Most insurers are wanting cost-effectiveness data in order to support their investments in broader coverage,” he said.
However, costs do vary with and without insurance; some medications are less expensive than others without significant differences in outcomes, so encourage patients to explore all the options and not just one brand, Dr. Kahan said.
Educate patients on plan details
Clinicians can’t guarantee coverage, but they can offer guidance to their patients, according to said Andrew Kraftson, MD, an endocrinologist and internal medicine physician at the University of Michigan, Ann Arbor, who specializes in the care of people with obesity.
Unfortunately, some of the challenges to obtaining insurance coverage for weight-loss medications lie in the plan details because some insurers have a blanket prohibition against the use of weight-loss medications, he said.
If patients did not look for this particular aspect of coverage at the time of enrollment in their chosen plan, they may not have known about this exclusion, and they are disappointed to find that they are ineligible for weight-loss medications despite medical circumstances, Dr. Kraftson said in an interview.
If weight-loss medications are covered, prior authorization often is required, Dr. Kraftson added.
“Unfortunately, the requirements vary from insurer to insurer, and this can present challenges for the busy clinicians who may not have dedicated staff to assist with these authorizations. Sometimes, the requirements are exactingly particular, and denials can commonly occur,” he said.
Some insurers will cover weight-loss medications for an initial period then require a certain degree of weight loss before renewing the approval, Dr. Kraftson said.
“While this is reasonable, sometimes it is necessary to titrate a medication more slowly to help a patient get used to the medicine, so they may not reach the required weight loss in the time required by the insurer,” he said. “As such, the medical professional is ‘punished’ for trying to be safe and patient-sensitive, and the patient may lose coverage of the medicine.”
Clinicians can help patients increase their chances for insurance coverage by providing a patient instruction guide to walk them through the steps that allow the patient to make inquiries with their own insurer, Dr. Kraftson said.
This guide should instruct patients on how to read their prescription coverage card to correctly contact their insurer, along with a guide to medical coverage terminology.
Lauren Oshman, MD, also of the University of Michigan, heads a collaborative quality initiative in the state known as Michigan Collaborative for Type 2 Diabetes (MCT2D). Dr. Oshman and her colleagues created a user-friendly list of terms to help patients understand their plans and better advocate for coverage (see below). The list was designed to guide patients with diabetes but applies to any medication.
Learn the lingo (common insurance terms and definitions)
- Deductible: Predetermined amount that must be paid annually before insurance pays for anything.
- Copayment: Set amount paid for a prescription.
- Coinsurance: Amount you pay after your deductible is met. Your insurance pays their portion. Coinsurance only applies to prescriptions and services covered under your health plan.
- Medication tier: Levels of insurance medication coverage; you play a smaller amount for a lower tier and a higher amount for a higher tier.
- Out-of-pocket max: Annual limit on what you pay before insurance covers 100% of covered services. Deductibles, copayment, and coinsurance all apply toward your out-of-pocket maximum.
- Prior authorization: Request made by your doctor to insurance company for coverage of a medication.
- Quantity limit: Limitation on the number of pills covered for a period of time.
- Step therapy: Medication you must have tried prior to approval of a nonpreferred medication, typically prior to trying a more expensive medication.
(Source: Learn the Lingo: A Guide to Common Insurance Terms and Definitions, courtesy of Lauren Oshman, MD, and MCT2D)
Also, make sure patients understand that they need to find out whether they have a deductible and if so, how much it is, Dr. Kraftson said.
Pros and cons of compounding
Compounded drugs are not approved by the FDA; however, that does not mean they are not available, and patients may pursue them as an option for weight-loss drugs.
In a statement issued on May 31, 2023, the FDA cited reports of adverse events associated with the use of compounded weight-loss drugs as a lower-cost alternative to the approved product. The FDA emphasized that the agency does not review compounded versions of weight-loss drugs for safety, efficacy, or quality.
Dr. Kraftson cited the lack of quality control, transparency, and safety data as reasons to discourage his patients from pursuing compounded medications.
“If a patient insists on pursuing it, then I review the position statement from the Obesity Medicine Association,” he said. The OMA statement recommends that anti-obesity medications undergo clinical trials and noted the lack of FDA oversight on these products. The OMA statement also advises compounded peptides to be “legally produced by companies whose identities are readily disclosed, and who have documented manufacturing processes compliant with oversight by applicable regulatory agencies.”
Tracking outcomes might boost coverage
Robust data on the long-term cost-effectiveness of weight-loss medications are lacking, although this is changing, Dr. Kraftson said. A 2022 study published last year in the Journal of Managed Care and Specialty Pharmacy showed that a 2.4-mg dose of semaglutide was cost-effective, compared with no treatment, diet and exercise, and other anti-obesity medications based on gains in quality of life.
“Regardless, insurers are not as motivated by long-term cost effectiveness,” Dr. Kraftson said. Insurers are accustomed to employee turnover and are more likely to be motivated by short-term costs and benefits, he said. “Obesity treatment provides some short-term benefit, but the majority of the benefit can be experienced when we look at the long-term horizon,” he said.
Looking ahead, “We need better ways to account for the myriad benefits experienced by patients with successful weight control beyond what is currently measured as metrics of success, including better ways to qualify and quantify quality-of-life benefits,” Dr. Kraftson said.
Also, clinicians should address the stigma associated with obesity, Dr. Kraftson said.
“We would not see the spate of coverage restrictions if we were talking about heart disease or cancer; insurers can get away with this because obesity is held to a different standard and patients with obesity are used to being undertreated and mistreated by the medical community and society,” he said. “We need to better account for the true costs of excess weight/obesity beyond what is traditionally accepted. This would help make the case for the cost-effective nature of treatment.”
Dr. Kraftson and Dr. Oshman disclosed no relevant financial relationships. Dr. Kahan had no financial conflicts and serves on the Medscape Editorial Advisory Board.
You can’t argue with success, unless you are an insurance company faced with covering medications shown to improve obesity.
The ability of drugs originally designed for diabetes management to reduce body weight has spiked demand and taxed supplies, according to the U.S. Food and Drug Administration, which included semaglutide (both Wegovy and Ozempic) on its Drug Shortages List as of May 31, 2023.
Meanwhile, clinicians and patients report that insurance companies are pushing back against coverage of these medications that mimic glucagon-like peptide 1 (GLP-1) because of the costs. A recent study conducted by Prime Therapeutics, a pharmacy benefit management organization, showed that individuals who started GLP-1 drugs for weight loss and who were adherent to the treatment averaged a 59% increase in health care costs after 1 year; for those in a subgroup analysis who were treatment adherent, the increase in health care costs was 98%.
“Insurance coverage for obesity treatment is challenging, particularly regarding medications,” said Scott Kahan, MD, director of the National Center for Weight and Wellness at George Washington University, Washington, in an interview. Employers must opt in for patients to have coverage for these medications; therefore, relatively few patients have had access at reasonable out-of-pocket costs, he said.
For example, the University of Texas stated on its website that its prescription drug plans will no longer cover drugs with the active ingredients semaglutide (Wegovy) or liraglutide (Saxenda) for weight loss as of Sept. 1, 2023. Both products are FDA-approved for weight management, whereas the equally popular Ozempic is currently approved only as a treatment for diabetes. The school’s website noted that the current price of the drugs, which cost the plan more than $5 million per month as of May 2023, outstrips the most expensive cancer agents.
The University of Texas also found that among its patients, the compliance rate for those who began Wegovy or Saxenda for weight loss was only 46%, which was not enough to justify continued coverage. The plan advised patients to approach their insurers directly.
Eventually, more information may prompt more support from insurance across a range of medications, Dr. Kahan noted. “Most insurers are wanting cost-effectiveness data in order to support their investments in broader coverage,” he said.
However, costs do vary with and without insurance; some medications are less expensive than others without significant differences in outcomes, so encourage patients to explore all the options and not just one brand, Dr. Kahan said.
Educate patients on plan details
Clinicians can’t guarantee coverage, but they can offer guidance to their patients, according to said Andrew Kraftson, MD, an endocrinologist and internal medicine physician at the University of Michigan, Ann Arbor, who specializes in the care of people with obesity.
Unfortunately, some of the challenges to obtaining insurance coverage for weight-loss medications lie in the plan details because some insurers have a blanket prohibition against the use of weight-loss medications, he said.
If patients did not look for this particular aspect of coverage at the time of enrollment in their chosen plan, they may not have known about this exclusion, and they are disappointed to find that they are ineligible for weight-loss medications despite medical circumstances, Dr. Kraftson said in an interview.
If weight-loss medications are covered, prior authorization often is required, Dr. Kraftson added.
“Unfortunately, the requirements vary from insurer to insurer, and this can present challenges for the busy clinicians who may not have dedicated staff to assist with these authorizations. Sometimes, the requirements are exactingly particular, and denials can commonly occur,” he said.
Some insurers will cover weight-loss medications for an initial period then require a certain degree of weight loss before renewing the approval, Dr. Kraftson said.
“While this is reasonable, sometimes it is necessary to titrate a medication more slowly to help a patient get used to the medicine, so they may not reach the required weight loss in the time required by the insurer,” he said. “As such, the medical professional is ‘punished’ for trying to be safe and patient-sensitive, and the patient may lose coverage of the medicine.”
Clinicians can help patients increase their chances for insurance coverage by providing a patient instruction guide to walk them through the steps that allow the patient to make inquiries with their own insurer, Dr. Kraftson said.
This guide should instruct patients on how to read their prescription coverage card to correctly contact their insurer, along with a guide to medical coverage terminology.
Lauren Oshman, MD, also of the University of Michigan, heads a collaborative quality initiative in the state known as Michigan Collaborative for Type 2 Diabetes (MCT2D). Dr. Oshman and her colleagues created a user-friendly list of terms to help patients understand their plans and better advocate for coverage (see below). The list was designed to guide patients with diabetes but applies to any medication.
Learn the lingo (common insurance terms and definitions)
- Deductible: Predetermined amount that must be paid annually before insurance pays for anything.
- Copayment: Set amount paid for a prescription.
- Coinsurance: Amount you pay after your deductible is met. Your insurance pays their portion. Coinsurance only applies to prescriptions and services covered under your health plan.
- Medication tier: Levels of insurance medication coverage; you play a smaller amount for a lower tier and a higher amount for a higher tier.
- Out-of-pocket max: Annual limit on what you pay before insurance covers 100% of covered services. Deductibles, copayment, and coinsurance all apply toward your out-of-pocket maximum.
- Prior authorization: Request made by your doctor to insurance company for coverage of a medication.
- Quantity limit: Limitation on the number of pills covered for a period of time.
- Step therapy: Medication you must have tried prior to approval of a nonpreferred medication, typically prior to trying a more expensive medication.
(Source: Learn the Lingo: A Guide to Common Insurance Terms and Definitions, courtesy of Lauren Oshman, MD, and MCT2D)
Also, make sure patients understand that they need to find out whether they have a deductible and if so, how much it is, Dr. Kraftson said.
Pros and cons of compounding
Compounded drugs are not approved by the FDA; however, that does not mean they are not available, and patients may pursue them as an option for weight-loss drugs.
In a statement issued on May 31, 2023, the FDA cited reports of adverse events associated with the use of compounded weight-loss drugs as a lower-cost alternative to the approved product. The FDA emphasized that the agency does not review compounded versions of weight-loss drugs for safety, efficacy, or quality.
Dr. Kraftson cited the lack of quality control, transparency, and safety data as reasons to discourage his patients from pursuing compounded medications.
“If a patient insists on pursuing it, then I review the position statement from the Obesity Medicine Association,” he said. The OMA statement recommends that anti-obesity medications undergo clinical trials and noted the lack of FDA oversight on these products. The OMA statement also advises compounded peptides to be “legally produced by companies whose identities are readily disclosed, and who have documented manufacturing processes compliant with oversight by applicable regulatory agencies.”
Tracking outcomes might boost coverage
Robust data on the long-term cost-effectiveness of weight-loss medications are lacking, although this is changing, Dr. Kraftson said. A 2022 study published last year in the Journal of Managed Care and Specialty Pharmacy showed that a 2.4-mg dose of semaglutide was cost-effective, compared with no treatment, diet and exercise, and other anti-obesity medications based on gains in quality of life.
“Regardless, insurers are not as motivated by long-term cost effectiveness,” Dr. Kraftson said. Insurers are accustomed to employee turnover and are more likely to be motivated by short-term costs and benefits, he said. “Obesity treatment provides some short-term benefit, but the majority of the benefit can be experienced when we look at the long-term horizon,” he said.
Looking ahead, “We need better ways to account for the myriad benefits experienced by patients with successful weight control beyond what is currently measured as metrics of success, including better ways to qualify and quantify quality-of-life benefits,” Dr. Kraftson said.
Also, clinicians should address the stigma associated with obesity, Dr. Kraftson said.
“We would not see the spate of coverage restrictions if we were talking about heart disease or cancer; insurers can get away with this because obesity is held to a different standard and patients with obesity are used to being undertreated and mistreated by the medical community and society,” he said. “We need to better account for the true costs of excess weight/obesity beyond what is traditionally accepted. This would help make the case for the cost-effective nature of treatment.”
Dr. Kraftson and Dr. Oshman disclosed no relevant financial relationships. Dr. Kahan had no financial conflicts and serves on the Medscape Editorial Advisory Board.
You can’t argue with success, unless you are an insurance company faced with covering medications shown to improve obesity.
The ability of drugs originally designed for diabetes management to reduce body weight has spiked demand and taxed supplies, according to the U.S. Food and Drug Administration, which included semaglutide (both Wegovy and Ozempic) on its Drug Shortages List as of May 31, 2023.
Meanwhile, clinicians and patients report that insurance companies are pushing back against coverage of these medications that mimic glucagon-like peptide 1 (GLP-1) because of the costs. A recent study conducted by Prime Therapeutics, a pharmacy benefit management organization, showed that individuals who started GLP-1 drugs for weight loss and who were adherent to the treatment averaged a 59% increase in health care costs after 1 year; for those in a subgroup analysis who were treatment adherent, the increase in health care costs was 98%.
“Insurance coverage for obesity treatment is challenging, particularly regarding medications,” said Scott Kahan, MD, director of the National Center for Weight and Wellness at George Washington University, Washington, in an interview. Employers must opt in for patients to have coverage for these medications; therefore, relatively few patients have had access at reasonable out-of-pocket costs, he said.
For example, the University of Texas stated on its website that its prescription drug plans will no longer cover drugs with the active ingredients semaglutide (Wegovy) or liraglutide (Saxenda) for weight loss as of Sept. 1, 2023. Both products are FDA-approved for weight management, whereas the equally popular Ozempic is currently approved only as a treatment for diabetes. The school’s website noted that the current price of the drugs, which cost the plan more than $5 million per month as of May 2023, outstrips the most expensive cancer agents.
The University of Texas also found that among its patients, the compliance rate for those who began Wegovy or Saxenda for weight loss was only 46%, which was not enough to justify continued coverage. The plan advised patients to approach their insurers directly.
Eventually, more information may prompt more support from insurance across a range of medications, Dr. Kahan noted. “Most insurers are wanting cost-effectiveness data in order to support their investments in broader coverage,” he said.
However, costs do vary with and without insurance; some medications are less expensive than others without significant differences in outcomes, so encourage patients to explore all the options and not just one brand, Dr. Kahan said.
Educate patients on plan details
Clinicians can’t guarantee coverage, but they can offer guidance to their patients, according to said Andrew Kraftson, MD, an endocrinologist and internal medicine physician at the University of Michigan, Ann Arbor, who specializes in the care of people with obesity.
Unfortunately, some of the challenges to obtaining insurance coverage for weight-loss medications lie in the plan details because some insurers have a blanket prohibition against the use of weight-loss medications, he said.
If patients did not look for this particular aspect of coverage at the time of enrollment in their chosen plan, they may not have known about this exclusion, and they are disappointed to find that they are ineligible for weight-loss medications despite medical circumstances, Dr. Kraftson said in an interview.
If weight-loss medications are covered, prior authorization often is required, Dr. Kraftson added.
“Unfortunately, the requirements vary from insurer to insurer, and this can present challenges for the busy clinicians who may not have dedicated staff to assist with these authorizations. Sometimes, the requirements are exactingly particular, and denials can commonly occur,” he said.
Some insurers will cover weight-loss medications for an initial period then require a certain degree of weight loss before renewing the approval, Dr. Kraftson said.
“While this is reasonable, sometimes it is necessary to titrate a medication more slowly to help a patient get used to the medicine, so they may not reach the required weight loss in the time required by the insurer,” he said. “As such, the medical professional is ‘punished’ for trying to be safe and patient-sensitive, and the patient may lose coverage of the medicine.”
Clinicians can help patients increase their chances for insurance coverage by providing a patient instruction guide to walk them through the steps that allow the patient to make inquiries with their own insurer, Dr. Kraftson said.
This guide should instruct patients on how to read their prescription coverage card to correctly contact their insurer, along with a guide to medical coverage terminology.
Lauren Oshman, MD, also of the University of Michigan, heads a collaborative quality initiative in the state known as Michigan Collaborative for Type 2 Diabetes (MCT2D). Dr. Oshman and her colleagues created a user-friendly list of terms to help patients understand their plans and better advocate for coverage (see below). The list was designed to guide patients with diabetes but applies to any medication.
Learn the lingo (common insurance terms and definitions)
- Deductible: Predetermined amount that must be paid annually before insurance pays for anything.
- Copayment: Set amount paid for a prescription.
- Coinsurance: Amount you pay after your deductible is met. Your insurance pays their portion. Coinsurance only applies to prescriptions and services covered under your health plan.
- Medication tier: Levels of insurance medication coverage; you play a smaller amount for a lower tier and a higher amount for a higher tier.
- Out-of-pocket max: Annual limit on what you pay before insurance covers 100% of covered services. Deductibles, copayment, and coinsurance all apply toward your out-of-pocket maximum.
- Prior authorization: Request made by your doctor to insurance company for coverage of a medication.
- Quantity limit: Limitation on the number of pills covered for a period of time.
- Step therapy: Medication you must have tried prior to approval of a nonpreferred medication, typically prior to trying a more expensive medication.
(Source: Learn the Lingo: A Guide to Common Insurance Terms and Definitions, courtesy of Lauren Oshman, MD, and MCT2D)
Also, make sure patients understand that they need to find out whether they have a deductible and if so, how much it is, Dr. Kraftson said.
Pros and cons of compounding
Compounded drugs are not approved by the FDA; however, that does not mean they are not available, and patients may pursue them as an option for weight-loss drugs.
In a statement issued on May 31, 2023, the FDA cited reports of adverse events associated with the use of compounded weight-loss drugs as a lower-cost alternative to the approved product. The FDA emphasized that the agency does not review compounded versions of weight-loss drugs for safety, efficacy, or quality.
Dr. Kraftson cited the lack of quality control, transparency, and safety data as reasons to discourage his patients from pursuing compounded medications.
“If a patient insists on pursuing it, then I review the position statement from the Obesity Medicine Association,” he said. The OMA statement recommends that anti-obesity medications undergo clinical trials and noted the lack of FDA oversight on these products. The OMA statement also advises compounded peptides to be “legally produced by companies whose identities are readily disclosed, and who have documented manufacturing processes compliant with oversight by applicable regulatory agencies.”
Tracking outcomes might boost coverage
Robust data on the long-term cost-effectiveness of weight-loss medications are lacking, although this is changing, Dr. Kraftson said. A 2022 study published last year in the Journal of Managed Care and Specialty Pharmacy showed that a 2.4-mg dose of semaglutide was cost-effective, compared with no treatment, diet and exercise, and other anti-obesity medications based on gains in quality of life.
“Regardless, insurers are not as motivated by long-term cost effectiveness,” Dr. Kraftson said. Insurers are accustomed to employee turnover and are more likely to be motivated by short-term costs and benefits, he said. “Obesity treatment provides some short-term benefit, but the majority of the benefit can be experienced when we look at the long-term horizon,” he said.
Looking ahead, “We need better ways to account for the myriad benefits experienced by patients with successful weight control beyond what is currently measured as metrics of success, including better ways to qualify and quantify quality-of-life benefits,” Dr. Kraftson said.
Also, clinicians should address the stigma associated with obesity, Dr. Kraftson said.
“We would not see the spate of coverage restrictions if we were talking about heart disease or cancer; insurers can get away with this because obesity is held to a different standard and patients with obesity are used to being undertreated and mistreated by the medical community and society,” he said. “We need to better account for the true costs of excess weight/obesity beyond what is traditionally accepted. This would help make the case for the cost-effective nature of treatment.”
Dr. Kraftson and Dr. Oshman disclosed no relevant financial relationships. Dr. Kahan had no financial conflicts and serves on the Medscape Editorial Advisory Board.
Where do you stand on the Middle East conflict?
“What do you think about the whole Israel thing?”
That question came at the end of an otherwise routine appointment.
Maybe she was just chatting. Maybe she wanted something deeper. I have no idea. I just said, “I don’t discuss those things with patients.”
My answer surprised her, but she didn’t push it. She paid her copay, scheduled a follow-up for 3 months, and left.
As I’ve written before, I try to avoid all news except the local weather. The sad reality is that most of it is bad and there’s nothing I can really do about it. It only upsets me, which isn’t good for my mental health and blood pressure, and if I can’t change it, what’s the point of knowing? It falls under the serenity prayer.
Of course, some news stories are too big not to hear something. I pass TVs in the doctors lounge or coffee house, hear others talking as I stand in line for the elevator, or see blurbs go by when checking the weather. It’s not entirely unavoidable.
I’m not trivializing the Middle East. But, to me, it’s not part of the doctor-patient relationship any more than my political views are. You run the risk of driving a wedge between you and the person you’re caring for. If you don’t like their opinion, you may find yourself less interested in them and their care. If they don’t like your opinion on news, they may start to question your ability as a doctor.
That’s not what we strive for, but it can be human nature. For better or worse we often reduce things to “us against them,” and learning someone is on the opposite side may, even subconsciously, alter how you treat them.
That’s not good, so to me it’s best not to know.
Some may think I’m being petty, or aloof, to be unwilling to discuss nonmedical issues of significance, but I don’t see it that way. Time is limited at the appointment and is best spent on medical care. Something unrelated to the visit that may alter my objective opinion of a patient – or theirs of me as a doctor – is best left out of it.
I’m here to be your doctor, and to do the best I can for you. I’m not here to be a debate partner. Whenever a patient asks me a question on politics or news I always think of the Monty Python skit “Argument Clinic.” That’s not why you’re here. There are plenty places to discuss such things. My office isn’t one of them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“What do you think about the whole Israel thing?”
That question came at the end of an otherwise routine appointment.
Maybe she was just chatting. Maybe she wanted something deeper. I have no idea. I just said, “I don’t discuss those things with patients.”
My answer surprised her, but she didn’t push it. She paid her copay, scheduled a follow-up for 3 months, and left.
As I’ve written before, I try to avoid all news except the local weather. The sad reality is that most of it is bad and there’s nothing I can really do about it. It only upsets me, which isn’t good for my mental health and blood pressure, and if I can’t change it, what’s the point of knowing? It falls under the serenity prayer.
Of course, some news stories are too big not to hear something. I pass TVs in the doctors lounge or coffee house, hear others talking as I stand in line for the elevator, or see blurbs go by when checking the weather. It’s not entirely unavoidable.
I’m not trivializing the Middle East. But, to me, it’s not part of the doctor-patient relationship any more than my political views are. You run the risk of driving a wedge between you and the person you’re caring for. If you don’t like their opinion, you may find yourself less interested in them and their care. If they don’t like your opinion on news, they may start to question your ability as a doctor.
That’s not what we strive for, but it can be human nature. For better or worse we often reduce things to “us against them,” and learning someone is on the opposite side may, even subconsciously, alter how you treat them.
That’s not good, so to me it’s best not to know.
Some may think I’m being petty, or aloof, to be unwilling to discuss nonmedical issues of significance, but I don’t see it that way. Time is limited at the appointment and is best spent on medical care. Something unrelated to the visit that may alter my objective opinion of a patient – or theirs of me as a doctor – is best left out of it.
I’m here to be your doctor, and to do the best I can for you. I’m not here to be a debate partner. Whenever a patient asks me a question on politics or news I always think of the Monty Python skit “Argument Clinic.” That’s not why you’re here. There are plenty places to discuss such things. My office isn’t one of them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“What do you think about the whole Israel thing?”
That question came at the end of an otherwise routine appointment.
Maybe she was just chatting. Maybe she wanted something deeper. I have no idea. I just said, “I don’t discuss those things with patients.”
My answer surprised her, but she didn’t push it. She paid her copay, scheduled a follow-up for 3 months, and left.
As I’ve written before, I try to avoid all news except the local weather. The sad reality is that most of it is bad and there’s nothing I can really do about it. It only upsets me, which isn’t good for my mental health and blood pressure, and if I can’t change it, what’s the point of knowing? It falls under the serenity prayer.
Of course, some news stories are too big not to hear something. I pass TVs in the doctors lounge or coffee house, hear others talking as I stand in line for the elevator, or see blurbs go by when checking the weather. It’s not entirely unavoidable.
I’m not trivializing the Middle East. But, to me, it’s not part of the doctor-patient relationship any more than my political views are. You run the risk of driving a wedge between you and the person you’re caring for. If you don’t like their opinion, you may find yourself less interested in them and their care. If they don’t like your opinion on news, they may start to question your ability as a doctor.
That’s not what we strive for, but it can be human nature. For better or worse we often reduce things to “us against them,” and learning someone is on the opposite side may, even subconsciously, alter how you treat them.
That’s not good, so to me it’s best not to know.
Some may think I’m being petty, or aloof, to be unwilling to discuss nonmedical issues of significance, but I don’t see it that way. Time is limited at the appointment and is best spent on medical care. Something unrelated to the visit that may alter my objective opinion of a patient – or theirs of me as a doctor – is best left out of it.
I’m here to be your doctor, and to do the best I can for you. I’m not here to be a debate partner. Whenever a patient asks me a question on politics or news I always think of the Monty Python skit “Argument Clinic.” That’s not why you’re here. There are plenty places to discuss such things. My office isn’t one of them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Making time to care for patients with diabetes
Can busy primary care offices continue to care for patients with diabetes? No one would argue that it is involved and takes effort, and health care providers are bankrupt when it comes to sparing additional time for this chronic disease. With roughly 37 million people living with diabetes and 96 million with prediabetes or early type 2 diabetes, and just over 8,000 practicing endocrinologists in the United States, we all need to make time especially in primary care to provide insight and holistic care. With limited time and budget, how do we do this?
First, decide to be involved in caring for patients with diabetes. Diabetes is best managed by interprofessional care teams, so you’re not going it alone. These teams may include physicians; pharmacists; physician assistants; advanced practice nurses; registered nurses; certified diabetes care and education specialists (CDCES); dietitians; and other professionals such as social workers, behavioral health professionals, medical assistants, and community health workers. Know which professionals are available to serve on your team, either within your clinic or as a consultant, and reach out to them to share the care and ease the burden. Remember to refer to these professionals to reinforce the diabetes intervention message to the patient.
Second, incorporate “diabetes only” appointments into your schedule, allowing time to focus on current comprehensive diabetes treatment goals, barriers/inertia for care. Remember to have short-interval follow-up as needed to keep that patient engaged to achieve their targets. Instruct your office staff to create diabetes appointment templates and reminders to patients to bring diabetes-related technologies, medication lists, and diabetes questions to the appointment. When I implemented this change, my patients welcomed the focus on their diabetes health, and they knew we were prioritizing this disease that they have for a lifetime. These appointments did not take away from their other conditions; rather, they often reminded me to stay focused on their diabetes and associated coconditions.
Taking the time to establish efficient workflows before implementing diabetes care saves countless hours later and immediately maximizes health care provider–patient interactions. Assign specific staff duties and expectations related to diabetes appointments, such as downloading diabetes technology, medication reconciliation, laboratory data, point-of-care hemoglobin A1c, basic foot exam, and patient goals for diabetes care. This allows the prescriber to focus on the glycemic, cardiologic, renal, and metabolic goals and overcome the therapeutic inertia that plagues us all.
Incorporating diabetes-related technology into clinical practice can be a significant time-saver but requires initial onboarding. Set aside a few hours to create a technology clinic flow, and designate at least one team member to be responsible for obtaining patient data before, during, or after encounters. If possible, obtaining data ahead of the visit will enhance efficiency, allowing for meaningful discussion of blood glucose and lifestyle patterns. Diabetes technology reveals the gaps in care and enhances our ability to identify the areas where glycemic intervention is needed. In addition, it reveals the impact of food choices, activity level, stress, and medication adherence to the person living with diabetes.
Finally, be proactive about therapeutic inertia. This is defined as a prescribers’ failure to intensify or deintensify a patient’s treatment when appropriate to do so. Causes of therapeutic inertia can be placed at the primary care physician level, including time constraints or inexperience in treating diabetes; the patient level, such as concerns about side effects or new treatment regimens; or a systemic level, such as availability of medications or their costs. Be real with yourself: We all have inertia and can identify areas to overcome. Never let inertia be traced back to you.
Not all inertia lives with the health care provider. Patients bring apprehension and concerns, have questions, and just want to share the frustrations associated with living their best life with the disease. Don’t assume that you know what your patients’ treatment barriers are; ask them. If you don’t have an answer, then note it and come up with one by the next follow-up. Remember that this is a chronic disease – a marathon, not a sprint. You don’t have to solve everything at one appointment; rather, keep the momentum going.
Let’s put this into clinical practice. For the next patient with diabetes who comes into your office, discuss with them your intention to prioritize their diabetes by having an appointment set aside to specifically focus on their individual goals and targets for their disease. Have the patient list any barriers and treatment goals they would like to review; flag your schedule to indicate it is a diabetes-only visit; and orient your staff to reconcile diabetes medications and record the patient’s last eye exam, urine albumin-to-creatinine ratio, A1c result, and blood glucose data. During this encounter, identify the patient’s personal targets for control, examine their feet, and review or order necessary laboratory metrics. Explore the patient-reported barriers and make inroads to remove or alleviate these. Advance treatment intervention, and schedule follow-up: every 4-6 weeks if the A1c is > 9%, every 2 months if it’s 7% to < 9%, and every 3-6 months if it’s < 7%. Utilize team diabetes care, such as CDCES referrals, dietitians, online resources, and community members, to help reinforce care and enhance engagement.
We need to take steps in our clinical practice to make the necessary space to accommodate this pervasive disease affecting nearly one-third of our population. Take a moment to look up and determine what needs to be in place so that you can take care of the people in your practice with diabetes. Laying the groundwork for implementing diabetes-only appointments can be time-consuming, but establishing consistent procedures, developing efficient workflows, and clearly defining roles and responsibilities is well worth the effort. This solid foundation equips the office, health care providers, and staff to care for persons with diabetes and will be invaluable to ensure that time for this care is available in the day-to-day clinical practice.
A version of this article first appeared on Medscape.com.
Can busy primary care offices continue to care for patients with diabetes? No one would argue that it is involved and takes effort, and health care providers are bankrupt when it comes to sparing additional time for this chronic disease. With roughly 37 million people living with diabetes and 96 million with prediabetes or early type 2 diabetes, and just over 8,000 practicing endocrinologists in the United States, we all need to make time especially in primary care to provide insight and holistic care. With limited time and budget, how do we do this?
First, decide to be involved in caring for patients with diabetes. Diabetes is best managed by interprofessional care teams, so you’re not going it alone. These teams may include physicians; pharmacists; physician assistants; advanced practice nurses; registered nurses; certified diabetes care and education specialists (CDCES); dietitians; and other professionals such as social workers, behavioral health professionals, medical assistants, and community health workers. Know which professionals are available to serve on your team, either within your clinic or as a consultant, and reach out to them to share the care and ease the burden. Remember to refer to these professionals to reinforce the diabetes intervention message to the patient.
Second, incorporate “diabetes only” appointments into your schedule, allowing time to focus on current comprehensive diabetes treatment goals, barriers/inertia for care. Remember to have short-interval follow-up as needed to keep that patient engaged to achieve their targets. Instruct your office staff to create diabetes appointment templates and reminders to patients to bring diabetes-related technologies, medication lists, and diabetes questions to the appointment. When I implemented this change, my patients welcomed the focus on their diabetes health, and they knew we were prioritizing this disease that they have for a lifetime. These appointments did not take away from their other conditions; rather, they often reminded me to stay focused on their diabetes and associated coconditions.
Taking the time to establish efficient workflows before implementing diabetes care saves countless hours later and immediately maximizes health care provider–patient interactions. Assign specific staff duties and expectations related to diabetes appointments, such as downloading diabetes technology, medication reconciliation, laboratory data, point-of-care hemoglobin A1c, basic foot exam, and patient goals for diabetes care. This allows the prescriber to focus on the glycemic, cardiologic, renal, and metabolic goals and overcome the therapeutic inertia that plagues us all.
Incorporating diabetes-related technology into clinical practice can be a significant time-saver but requires initial onboarding. Set aside a few hours to create a technology clinic flow, and designate at least one team member to be responsible for obtaining patient data before, during, or after encounters. If possible, obtaining data ahead of the visit will enhance efficiency, allowing for meaningful discussion of blood glucose and lifestyle patterns. Diabetes technology reveals the gaps in care and enhances our ability to identify the areas where glycemic intervention is needed. In addition, it reveals the impact of food choices, activity level, stress, and medication adherence to the person living with diabetes.
Finally, be proactive about therapeutic inertia. This is defined as a prescribers’ failure to intensify or deintensify a patient’s treatment when appropriate to do so. Causes of therapeutic inertia can be placed at the primary care physician level, including time constraints or inexperience in treating diabetes; the patient level, such as concerns about side effects or new treatment regimens; or a systemic level, such as availability of medications or their costs. Be real with yourself: We all have inertia and can identify areas to overcome. Never let inertia be traced back to you.
Not all inertia lives with the health care provider. Patients bring apprehension and concerns, have questions, and just want to share the frustrations associated with living their best life with the disease. Don’t assume that you know what your patients’ treatment barriers are; ask them. If you don’t have an answer, then note it and come up with one by the next follow-up. Remember that this is a chronic disease – a marathon, not a sprint. You don’t have to solve everything at one appointment; rather, keep the momentum going.
Let’s put this into clinical practice. For the next patient with diabetes who comes into your office, discuss with them your intention to prioritize their diabetes by having an appointment set aside to specifically focus on their individual goals and targets for their disease. Have the patient list any barriers and treatment goals they would like to review; flag your schedule to indicate it is a diabetes-only visit; and orient your staff to reconcile diabetes medications and record the patient’s last eye exam, urine albumin-to-creatinine ratio, A1c result, and blood glucose data. During this encounter, identify the patient’s personal targets for control, examine their feet, and review or order necessary laboratory metrics. Explore the patient-reported barriers and make inroads to remove or alleviate these. Advance treatment intervention, and schedule follow-up: every 4-6 weeks if the A1c is > 9%, every 2 months if it’s 7% to < 9%, and every 3-6 months if it’s < 7%. Utilize team diabetes care, such as CDCES referrals, dietitians, online resources, and community members, to help reinforce care and enhance engagement.
We need to take steps in our clinical practice to make the necessary space to accommodate this pervasive disease affecting nearly one-third of our population. Take a moment to look up and determine what needs to be in place so that you can take care of the people in your practice with diabetes. Laying the groundwork for implementing diabetes-only appointments can be time-consuming, but establishing consistent procedures, developing efficient workflows, and clearly defining roles and responsibilities is well worth the effort. This solid foundation equips the office, health care providers, and staff to care for persons with diabetes and will be invaluable to ensure that time for this care is available in the day-to-day clinical practice.
A version of this article first appeared on Medscape.com.
Can busy primary care offices continue to care for patients with diabetes? No one would argue that it is involved and takes effort, and health care providers are bankrupt when it comes to sparing additional time for this chronic disease. With roughly 37 million people living with diabetes and 96 million with prediabetes or early type 2 diabetes, and just over 8,000 practicing endocrinologists in the United States, we all need to make time especially in primary care to provide insight and holistic care. With limited time and budget, how do we do this?
First, decide to be involved in caring for patients with diabetes. Diabetes is best managed by interprofessional care teams, so you’re not going it alone. These teams may include physicians; pharmacists; physician assistants; advanced practice nurses; registered nurses; certified diabetes care and education specialists (CDCES); dietitians; and other professionals such as social workers, behavioral health professionals, medical assistants, and community health workers. Know which professionals are available to serve on your team, either within your clinic or as a consultant, and reach out to them to share the care and ease the burden. Remember to refer to these professionals to reinforce the diabetes intervention message to the patient.
Second, incorporate “diabetes only” appointments into your schedule, allowing time to focus on current comprehensive diabetes treatment goals, barriers/inertia for care. Remember to have short-interval follow-up as needed to keep that patient engaged to achieve their targets. Instruct your office staff to create diabetes appointment templates and reminders to patients to bring diabetes-related technologies, medication lists, and diabetes questions to the appointment. When I implemented this change, my patients welcomed the focus on their diabetes health, and they knew we were prioritizing this disease that they have for a lifetime. These appointments did not take away from their other conditions; rather, they often reminded me to stay focused on their diabetes and associated coconditions.
Taking the time to establish efficient workflows before implementing diabetes care saves countless hours later and immediately maximizes health care provider–patient interactions. Assign specific staff duties and expectations related to diabetes appointments, such as downloading diabetes technology, medication reconciliation, laboratory data, point-of-care hemoglobin A1c, basic foot exam, and patient goals for diabetes care. This allows the prescriber to focus on the glycemic, cardiologic, renal, and metabolic goals and overcome the therapeutic inertia that plagues us all.
Incorporating diabetes-related technology into clinical practice can be a significant time-saver but requires initial onboarding. Set aside a few hours to create a technology clinic flow, and designate at least one team member to be responsible for obtaining patient data before, during, or after encounters. If possible, obtaining data ahead of the visit will enhance efficiency, allowing for meaningful discussion of blood glucose and lifestyle patterns. Diabetes technology reveals the gaps in care and enhances our ability to identify the areas where glycemic intervention is needed. In addition, it reveals the impact of food choices, activity level, stress, and medication adherence to the person living with diabetes.
Finally, be proactive about therapeutic inertia. This is defined as a prescribers’ failure to intensify or deintensify a patient’s treatment when appropriate to do so. Causes of therapeutic inertia can be placed at the primary care physician level, including time constraints or inexperience in treating diabetes; the patient level, such as concerns about side effects or new treatment regimens; or a systemic level, such as availability of medications or their costs. Be real with yourself: We all have inertia and can identify areas to overcome. Never let inertia be traced back to you.
Not all inertia lives with the health care provider. Patients bring apprehension and concerns, have questions, and just want to share the frustrations associated with living their best life with the disease. Don’t assume that you know what your patients’ treatment barriers are; ask them. If you don’t have an answer, then note it and come up with one by the next follow-up. Remember that this is a chronic disease – a marathon, not a sprint. You don’t have to solve everything at one appointment; rather, keep the momentum going.
Let’s put this into clinical practice. For the next patient with diabetes who comes into your office, discuss with them your intention to prioritize their diabetes by having an appointment set aside to specifically focus on their individual goals and targets for their disease. Have the patient list any barriers and treatment goals they would like to review; flag your schedule to indicate it is a diabetes-only visit; and orient your staff to reconcile diabetes medications and record the patient’s last eye exam, urine albumin-to-creatinine ratio, A1c result, and blood glucose data. During this encounter, identify the patient’s personal targets for control, examine their feet, and review or order necessary laboratory metrics. Explore the patient-reported barriers and make inroads to remove or alleviate these. Advance treatment intervention, and schedule follow-up: every 4-6 weeks if the A1c is > 9%, every 2 months if it’s 7% to < 9%, and every 3-6 months if it’s < 7%. Utilize team diabetes care, such as CDCES referrals, dietitians, online resources, and community members, to help reinforce care and enhance engagement.
We need to take steps in our clinical practice to make the necessary space to accommodate this pervasive disease affecting nearly one-third of our population. Take a moment to look up and determine what needs to be in place so that you can take care of the people in your practice with diabetes. Laying the groundwork for implementing diabetes-only appointments can be time-consuming, but establishing consistent procedures, developing efficient workflows, and clearly defining roles and responsibilities is well worth the effort. This solid foundation equips the office, health care providers, and staff to care for persons with diabetes and will be invaluable to ensure that time for this care is available in the day-to-day clinical practice.
A version of this article first appeared on Medscape.com.
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
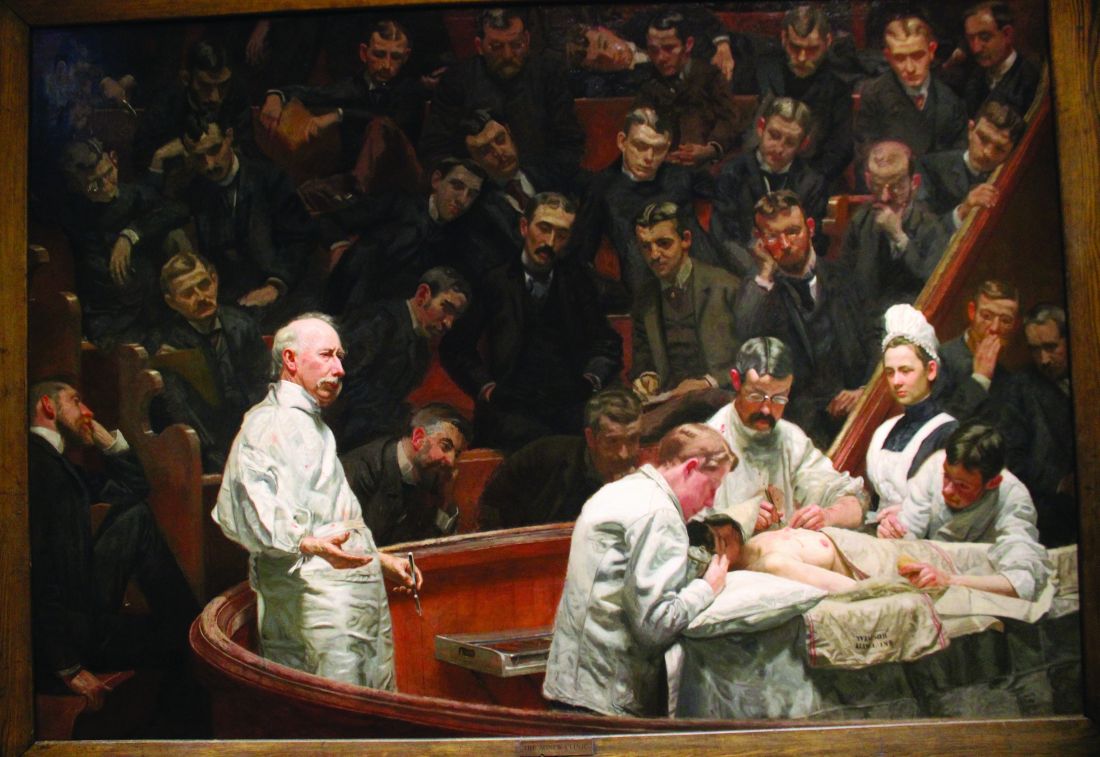
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
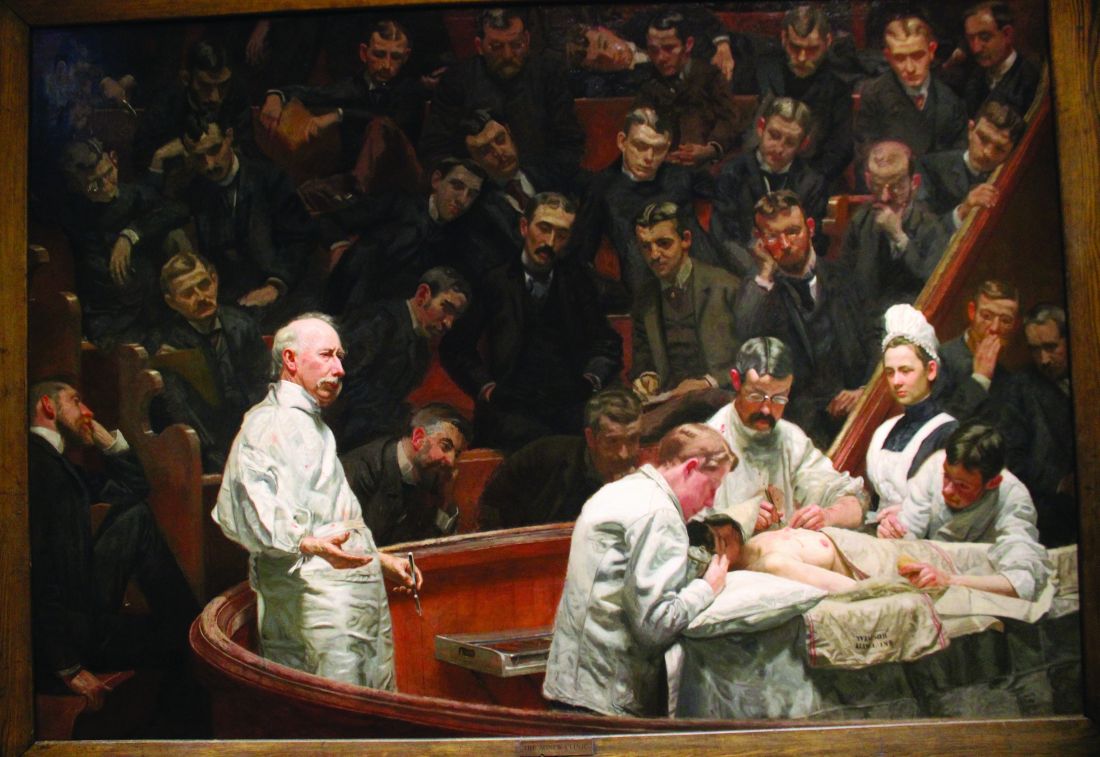
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
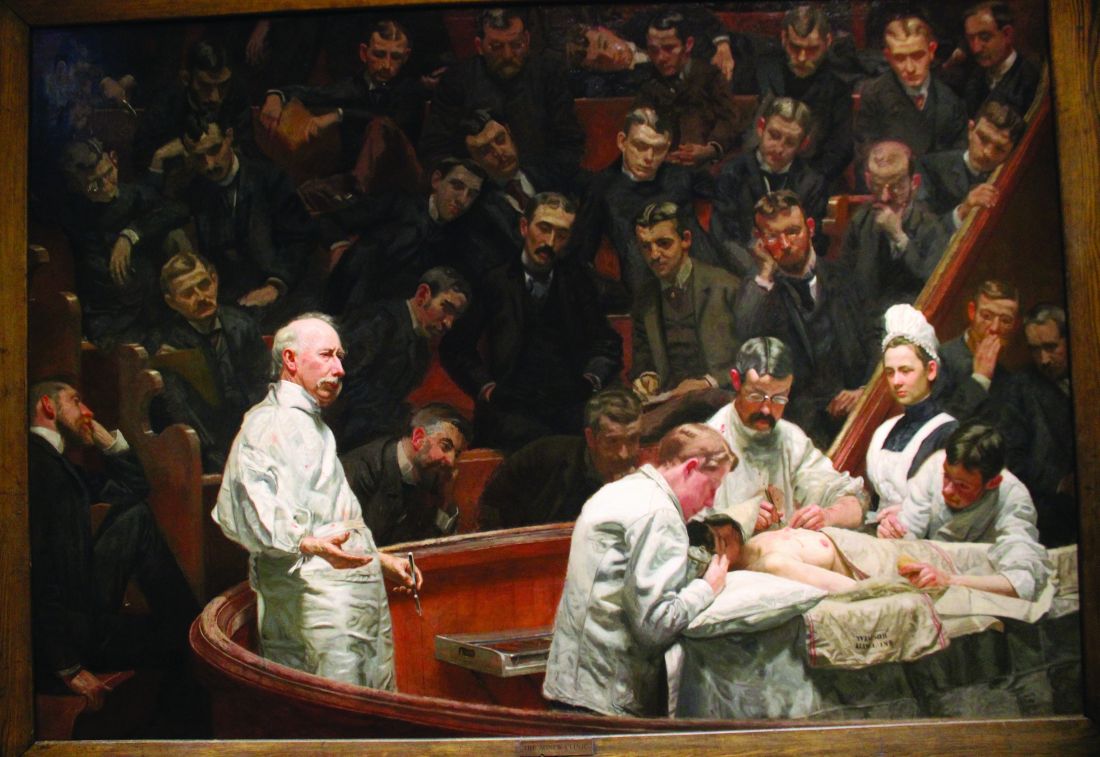
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]









