User login
Barcelona beckons for first hybrid ESC Congress
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
One hour of walking per week may boost longevity for octogenarians
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
FROM ESC CONGRESS 2022
Cholesterol levels lowering in U.S., but disparities emerge
Cholesterol levels in American adults have improved over the previous decade, but a large cross-sectional analysis of more than 30,000 U.S. adults has found notable disparities in cholesterol control, particularly among Asian adults, lower lipid control rates among Black and other Hispanic adults compared to Whites, and no appreciable improvements for people taking statins.
“We found that total cholesterol improved significantly among U.S. adults from 2008 to 2018,” senior study author Rishi Wadhera, MD, of Beth Israel Deaconess Medical Center in Boston, said in an interview. “When we looked at rates of lipid control among adults treated with statins, we found no significant improvements from 2008 through 2018.”
He noted the patterns for lipid control were consistent for women and men, adding, “In contrast to all other racial and ethnic groups, Mexican American and Black adults did experience significant improvements in cholesterol control. Despite this progress, rates of cholesterol control still remained significantly lower in Black adults compared to White adults.”
The study analyzed lipid concentrations from 33,040 adults ages 20 and older from the National Health and Nutrition Examination Surveys (NHANES), using 2007-2008 as the baseline and 2017-2018 as the endpoint. With lipid control defined as total cholesterol of 200 mg/dL or less, the analysis showed that total cholesterol improved in the overall population from 197 to 189 mg/dL in that time (95% confidence interval, –12.2 to –4.9 mg/dL; P < .001).
The study analyzed lipid trends in several demographic categories. Age-adjusted total cholesterol for women improved significantly, from 199 to 192 mg/dL (95% confidence interval [CI], –11.6 to –3.6 mg/dL; P < .001), but improved slightly more for men, from 195 to 185 mg/dL (95% CI, –14 to –5.1 mg/dL; P < .001).
Overall, age-adjusted total cholesterol improved significantly for Blacks (–7.8 mg/dL), Mexican Americans (–11.3 mg/dL), other Hispanic adults (–8 mg/dL) and Whites (–8.8 mg/dL; P < .001 for all), but not for Asian adults, measured from 2011-2012 to 2017-2018: –.2 mg/dL (95% CI, –6.5 to 6.2 mg/dL; P = .9).
The study found that LDL cholesterol, on an age-adjusted basis, improved significantly overall, from 116 mg/dL in 2007-2008 to 111 mg/dL in 2017-2018 (95% CI, –8.3 to –1.4 mg/dL; P = .001). However, unlike total cholesterol, this improvement didn’t carry over to most ethnic groups. Mexican American adults (–8 mg/dL; P = .01) and Whites (–5.9 mg/dL; P = .001) showed significant improvements, but Asian, Black or other Hispanic adults didn’t.
The study also evaluated lipid control in people taking statins and found that, overall, it didn’t change significantly: from 78.5% in 2007-2008 to 79.5% in 2017-2018 (P = .27). Mexican American adults were the only ethnic group that showed significant improvement in lipid control, going from 73% in 2007-2008 to 86.5% in 2017-2018 (P = .008).
Disparities in lipid control
Women had notably lower lipid control rates than men, with an odds ratio of .52 in 2007-2010 (P < .001), with similar patterns found in 2011-2014 (OR, 0.48) and 2015-2018 (OR, 0.54, P < .001 for both).
Lipid control worsened over time for Black and other Hispanic adults compared to Whites. In 2007-2010, lipid control rates among the studied ethnic groups were similar, a trend that carried over to the 2011-2014 study interval and included Asian adults. However, in 2015-2018, Blacks had lower rates of lipid control compared to Whites (OR, 0.66; 95% CI, .47-.94; P = .03), as did other Hispanic adults (OR, 0.59; 95% CI, .37-.95; P = .04).
These disparities between sexes and ethnic groups warrant further investigation, Dr. Wadhera said. “We were surprised that women had significantly lower rates of cholesterol control than men,” he said. “We need to better understand whether gaps in care, such barriers in access, less frequent lab monitoring of cholesterol, or less intensive prescribing of important treatments, contribute to these differences.”
He called the lower lipid control rates in Black and Hispanic adults “concerning, especially because rates of heart attacks and strokes remain high in these groups. ... Efforts to identify gaps in care and increase and intensify medical therapy are needed, as treatment rates in these populations are low.”
While the study collected data before the COVID-19 pandemic, Dr. Wadhera acknowledged that the management of cardiovascular risk factors may have worsened because of it. “Monitoring cholesterol levels and control rates in the U.S. population as we emerge from the pandemic will be critically important,” he said.
In an accompanying editorial, Hermes Florez, MD, PhD, of the Medical University of South Carolina in Charleston, and colleagues called for adequately powered studies to further investigate the disparities in the Asian and Hispanic populations. “Worse rates of cholesterol control observed in women and in minority populations deserve special attention,” they wrote.
They noted that future studies should consider the impact of guidelines and recommendations that emerged since the study started, namely from the American College of Cardiology/American Heart Association 2013 guidelines, Healthy People 2030, and the U.S. Preventive Services Task Force (JAMA. 2022 Aug 23. doi: 10.1001/jama.2022.13044).
“More important, future work must focus on how to effectively eliminate those disparities and better control modifiable risk factors to enhance outcomes for all individuals regardless of race and ethnicity,” Dr. Florez and colleagues wrote.
The study received funding from the National Heart, Lung, and Blood Institute. Dr. Wadhera disclosed relationships with CVS Health and Abbott. Dr. Florez and colleagues have no disclosures.
Cholesterol levels in American adults have improved over the previous decade, but a large cross-sectional analysis of more than 30,000 U.S. adults has found notable disparities in cholesterol control, particularly among Asian adults, lower lipid control rates among Black and other Hispanic adults compared to Whites, and no appreciable improvements for people taking statins.
“We found that total cholesterol improved significantly among U.S. adults from 2008 to 2018,” senior study author Rishi Wadhera, MD, of Beth Israel Deaconess Medical Center in Boston, said in an interview. “When we looked at rates of lipid control among adults treated with statins, we found no significant improvements from 2008 through 2018.”
He noted the patterns for lipid control were consistent for women and men, adding, “In contrast to all other racial and ethnic groups, Mexican American and Black adults did experience significant improvements in cholesterol control. Despite this progress, rates of cholesterol control still remained significantly lower in Black adults compared to White adults.”
The study analyzed lipid concentrations from 33,040 adults ages 20 and older from the National Health and Nutrition Examination Surveys (NHANES), using 2007-2008 as the baseline and 2017-2018 as the endpoint. With lipid control defined as total cholesterol of 200 mg/dL or less, the analysis showed that total cholesterol improved in the overall population from 197 to 189 mg/dL in that time (95% confidence interval, –12.2 to –4.9 mg/dL; P < .001).
The study analyzed lipid trends in several demographic categories. Age-adjusted total cholesterol for women improved significantly, from 199 to 192 mg/dL (95% confidence interval [CI], –11.6 to –3.6 mg/dL; P < .001), but improved slightly more for men, from 195 to 185 mg/dL (95% CI, –14 to –5.1 mg/dL; P < .001).
Overall, age-adjusted total cholesterol improved significantly for Blacks (–7.8 mg/dL), Mexican Americans (–11.3 mg/dL), other Hispanic adults (–8 mg/dL) and Whites (–8.8 mg/dL; P < .001 for all), but not for Asian adults, measured from 2011-2012 to 2017-2018: –.2 mg/dL (95% CI, –6.5 to 6.2 mg/dL; P = .9).
The study found that LDL cholesterol, on an age-adjusted basis, improved significantly overall, from 116 mg/dL in 2007-2008 to 111 mg/dL in 2017-2018 (95% CI, –8.3 to –1.4 mg/dL; P = .001). However, unlike total cholesterol, this improvement didn’t carry over to most ethnic groups. Mexican American adults (–8 mg/dL; P = .01) and Whites (–5.9 mg/dL; P = .001) showed significant improvements, but Asian, Black or other Hispanic adults didn’t.
The study also evaluated lipid control in people taking statins and found that, overall, it didn’t change significantly: from 78.5% in 2007-2008 to 79.5% in 2017-2018 (P = .27). Mexican American adults were the only ethnic group that showed significant improvement in lipid control, going from 73% in 2007-2008 to 86.5% in 2017-2018 (P = .008).
Disparities in lipid control
Women had notably lower lipid control rates than men, with an odds ratio of .52 in 2007-2010 (P < .001), with similar patterns found in 2011-2014 (OR, 0.48) and 2015-2018 (OR, 0.54, P < .001 for both).
Lipid control worsened over time for Black and other Hispanic adults compared to Whites. In 2007-2010, lipid control rates among the studied ethnic groups were similar, a trend that carried over to the 2011-2014 study interval and included Asian adults. However, in 2015-2018, Blacks had lower rates of lipid control compared to Whites (OR, 0.66; 95% CI, .47-.94; P = .03), as did other Hispanic adults (OR, 0.59; 95% CI, .37-.95; P = .04).
These disparities between sexes and ethnic groups warrant further investigation, Dr. Wadhera said. “We were surprised that women had significantly lower rates of cholesterol control than men,” he said. “We need to better understand whether gaps in care, such barriers in access, less frequent lab monitoring of cholesterol, or less intensive prescribing of important treatments, contribute to these differences.”
He called the lower lipid control rates in Black and Hispanic adults “concerning, especially because rates of heart attacks and strokes remain high in these groups. ... Efforts to identify gaps in care and increase and intensify medical therapy are needed, as treatment rates in these populations are low.”
While the study collected data before the COVID-19 pandemic, Dr. Wadhera acknowledged that the management of cardiovascular risk factors may have worsened because of it. “Monitoring cholesterol levels and control rates in the U.S. population as we emerge from the pandemic will be critically important,” he said.
In an accompanying editorial, Hermes Florez, MD, PhD, of the Medical University of South Carolina in Charleston, and colleagues called for adequately powered studies to further investigate the disparities in the Asian and Hispanic populations. “Worse rates of cholesterol control observed in women and in minority populations deserve special attention,” they wrote.
They noted that future studies should consider the impact of guidelines and recommendations that emerged since the study started, namely from the American College of Cardiology/American Heart Association 2013 guidelines, Healthy People 2030, and the U.S. Preventive Services Task Force (JAMA. 2022 Aug 23. doi: 10.1001/jama.2022.13044).
“More important, future work must focus on how to effectively eliminate those disparities and better control modifiable risk factors to enhance outcomes for all individuals regardless of race and ethnicity,” Dr. Florez and colleagues wrote.
The study received funding from the National Heart, Lung, and Blood Institute. Dr. Wadhera disclosed relationships with CVS Health and Abbott. Dr. Florez and colleagues have no disclosures.
Cholesterol levels in American adults have improved over the previous decade, but a large cross-sectional analysis of more than 30,000 U.S. adults has found notable disparities in cholesterol control, particularly among Asian adults, lower lipid control rates among Black and other Hispanic adults compared to Whites, and no appreciable improvements for people taking statins.
“We found that total cholesterol improved significantly among U.S. adults from 2008 to 2018,” senior study author Rishi Wadhera, MD, of Beth Israel Deaconess Medical Center in Boston, said in an interview. “When we looked at rates of lipid control among adults treated with statins, we found no significant improvements from 2008 through 2018.”
He noted the patterns for lipid control were consistent for women and men, adding, “In contrast to all other racial and ethnic groups, Mexican American and Black adults did experience significant improvements in cholesterol control. Despite this progress, rates of cholesterol control still remained significantly lower in Black adults compared to White adults.”
The study analyzed lipid concentrations from 33,040 adults ages 20 and older from the National Health and Nutrition Examination Surveys (NHANES), using 2007-2008 as the baseline and 2017-2018 as the endpoint. With lipid control defined as total cholesterol of 200 mg/dL or less, the analysis showed that total cholesterol improved in the overall population from 197 to 189 mg/dL in that time (95% confidence interval, –12.2 to –4.9 mg/dL; P < .001).
The study analyzed lipid trends in several demographic categories. Age-adjusted total cholesterol for women improved significantly, from 199 to 192 mg/dL (95% confidence interval [CI], –11.6 to –3.6 mg/dL; P < .001), but improved slightly more for men, from 195 to 185 mg/dL (95% CI, –14 to –5.1 mg/dL; P < .001).
Overall, age-adjusted total cholesterol improved significantly for Blacks (–7.8 mg/dL), Mexican Americans (–11.3 mg/dL), other Hispanic adults (–8 mg/dL) and Whites (–8.8 mg/dL; P < .001 for all), but not for Asian adults, measured from 2011-2012 to 2017-2018: –.2 mg/dL (95% CI, –6.5 to 6.2 mg/dL; P = .9).
The study found that LDL cholesterol, on an age-adjusted basis, improved significantly overall, from 116 mg/dL in 2007-2008 to 111 mg/dL in 2017-2018 (95% CI, –8.3 to –1.4 mg/dL; P = .001). However, unlike total cholesterol, this improvement didn’t carry over to most ethnic groups. Mexican American adults (–8 mg/dL; P = .01) and Whites (–5.9 mg/dL; P = .001) showed significant improvements, but Asian, Black or other Hispanic adults didn’t.
The study also evaluated lipid control in people taking statins and found that, overall, it didn’t change significantly: from 78.5% in 2007-2008 to 79.5% in 2017-2018 (P = .27). Mexican American adults were the only ethnic group that showed significant improvement in lipid control, going from 73% in 2007-2008 to 86.5% in 2017-2018 (P = .008).
Disparities in lipid control
Women had notably lower lipid control rates than men, with an odds ratio of .52 in 2007-2010 (P < .001), with similar patterns found in 2011-2014 (OR, 0.48) and 2015-2018 (OR, 0.54, P < .001 for both).
Lipid control worsened over time for Black and other Hispanic adults compared to Whites. In 2007-2010, lipid control rates among the studied ethnic groups were similar, a trend that carried over to the 2011-2014 study interval and included Asian adults. However, in 2015-2018, Blacks had lower rates of lipid control compared to Whites (OR, 0.66; 95% CI, .47-.94; P = .03), as did other Hispanic adults (OR, 0.59; 95% CI, .37-.95; P = .04).
These disparities between sexes and ethnic groups warrant further investigation, Dr. Wadhera said. “We were surprised that women had significantly lower rates of cholesterol control than men,” he said. “We need to better understand whether gaps in care, such barriers in access, less frequent lab monitoring of cholesterol, or less intensive prescribing of important treatments, contribute to these differences.”
He called the lower lipid control rates in Black and Hispanic adults “concerning, especially because rates of heart attacks and strokes remain high in these groups. ... Efforts to identify gaps in care and increase and intensify medical therapy are needed, as treatment rates in these populations are low.”
While the study collected data before the COVID-19 pandemic, Dr. Wadhera acknowledged that the management of cardiovascular risk factors may have worsened because of it. “Monitoring cholesterol levels and control rates in the U.S. population as we emerge from the pandemic will be critically important,” he said.
In an accompanying editorial, Hermes Florez, MD, PhD, of the Medical University of South Carolina in Charleston, and colleagues called for adequately powered studies to further investigate the disparities in the Asian and Hispanic populations. “Worse rates of cholesterol control observed in women and in minority populations deserve special attention,” they wrote.
They noted that future studies should consider the impact of guidelines and recommendations that emerged since the study started, namely from the American College of Cardiology/American Heart Association 2013 guidelines, Healthy People 2030, and the U.S. Preventive Services Task Force (JAMA. 2022 Aug 23. doi: 10.1001/jama.2022.13044).
“More important, future work must focus on how to effectively eliminate those disparities and better control modifiable risk factors to enhance outcomes for all individuals regardless of race and ethnicity,” Dr. Florez and colleagues wrote.
The study received funding from the National Heart, Lung, and Blood Institute. Dr. Wadhera disclosed relationships with CVS Health and Abbott. Dr. Florez and colleagues have no disclosures.
FROM JAMA
Does DTC heart drug advertising discourage lifestyle changes?
A 5-minute bout of direct-to-consumer advertising (DTCA) for prescription heart drugs was associated with favorable perceptions of both medication use and pharmaceutical companies, but did not seem to negate intentions to use lifestyle interventions, a survey study shows.
Participants who watched ads for various prescription heart drugs, with or without price disclosure, were more likely to report positive perceptions of drug companies and intentions to take actions such as switching medications.
The ads did not seem to affect intentions to eat healthfully and exercise.
The study was published online in JAMA Health Forum.
DTCA ‘unlikely to have an adverse effect’
“Increasing prevalence of DTCA may promote an overreliance on medication over healthy lifestyle choices to manage chronic conditions,” coauthor Yashaswini Singh, MPA, a PhD candidate at the Johns Hopkins University, Baltimore, told this news organization. “Thus, we hypothesized that DTCA exposure would reduce the likelihood of individuals engaging in preventive health behaviors.”
“However,” she said, “our results did not support this hypothesis, suggesting that exposure to DTCA for heart disease medication is unlikely to have an adverse effect on individuals’ intentions to engage in diet and exercise.”
That said, she added, “DTCA of prescription drugs can contribute to rising drug costs due to overprescribing of both inappropriate and brand-name drugs over cheaper generic alternatives. While we do not examine this mechanism in our paper, this remains an important question for future research.”
For the study, the team recruited 2,874 individuals (mean age, 53.8 years; 54% men; 83% White) from a U.S. nationally representative sample of people at high risk of cardiovascular disease, the Ipsos Public Affairs KnowledgePanel.
Participants were randomly assigned to one of three interventions: DTCA for heart disease medications, DTCA for heart disease medications with price disclosure, or nonpharmaceutical advertising (control). Each group watched five 1-minute videos for a total of 5 minutes of advertising exposure.
One group viewed ads for four heart disease medications – two ads for sacubitril/valsartan (Entresto, Novartis) and one each for rivaroxaban (Xarelto, Bayer), evolocumab (Repatha, Amgen), and ticagrelor (Brilinta, AstraZeneca); the second group saw the same ads, but with prices spliced in; and controls watched videos for nondrug products, such as consumer electronics.
Participants then completed a questionnaire to measure medication- and lifestyle-related intentions, as well as health-related beliefs and perceptions. Using a scale of 1 (highly unlikely) to 5 (highly likely), they rated the likelihood of their switching medication, asking a physician or insurer about a medication, searching for the drug online, or taking it as directed. The same scale was used to rate the likelihood of their being more physically active or eating more healthfully.
On a scale of 1 (always disagree) to 5 (always agree), they also related their perceptions of pharmaceutical manufacturers as being competent, innovative, and trustworthy.
To measure the magnitude of DTCA associations, the researchers calculated marginal effects (MEs) of treatment – that is, the difference in probability of an outcome between the treatment and control arms.
They found a positive association between DTCA and medication-related behavioral intentions, including intention to switch medication (ME, 0.004; P = .002) and engage in information-seeking behaviors (ME, 0.02; P = .01).
There was no evidence suggesting that pharmaceutical DTCA discouraged use of nonpharmacologic lifestyle interventions to help manage heart disease. DTCA also was positively associated with consumers’ favorable perceptions of pharmaceutical manufacturers (competence: ME, 0.03; P = .01; innovative: ME, 0.03; P = .008).
No differential associations were seen for price disclosures in DTCA.
Questions remain
The authors acknowledged that the study focused on short-term behavioral intentions and that “future research should focus on the long-term effects of advertising in a real-world randomized setting.”
Ms. Singh said additional questions, some of which her team is investigating, include “understanding the interaction between government policies [such as] drug pricing reforms and firms’ advertising decisions; understanding whether observed changes in individuals’ health beliefs translate into actual changes to information-seeking behavior and health care utilization; and whether the demographic, political, and social characteristics of individuals shape their behavioral responses to advertising.”
Johanna Contreras, MD, an advanced heart failure and transplantation cardiologist at Mount Sinai Hospital, New York, said in an interview that the findings don’t surprise her. “The caveat is that this study was an online survey, so it only captured the beliefs and intentions, but not patient demand for the product and use of the product.”
“I do believe DTCA can create positive intentions towards the product ... and could make people more receptive to interventions,” she said. However, the information must be presented in a balanced way.
In addition, she noted, “price is still important. I think people take pricing into account when deciding to proceed with an intervention. If the price is ‘right’ or a little lower than expected, then they will likely consider the product. But if the price is significantly lower, then they may not trust that it is a good product. Generic drugs are an example. Even though they are approved and far cheaper than brand names, patients are often skeptical to take them.”
The study was funded with a grant from the Blue Cross Blue Shield of Illinois Affordability Cures Consortium. Ms. Singh and coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A 5-minute bout of direct-to-consumer advertising (DTCA) for prescription heart drugs was associated with favorable perceptions of both medication use and pharmaceutical companies, but did not seem to negate intentions to use lifestyle interventions, a survey study shows.
Participants who watched ads for various prescription heart drugs, with or without price disclosure, were more likely to report positive perceptions of drug companies and intentions to take actions such as switching medications.
The ads did not seem to affect intentions to eat healthfully and exercise.
The study was published online in JAMA Health Forum.
DTCA ‘unlikely to have an adverse effect’
“Increasing prevalence of DTCA may promote an overreliance on medication over healthy lifestyle choices to manage chronic conditions,” coauthor Yashaswini Singh, MPA, a PhD candidate at the Johns Hopkins University, Baltimore, told this news organization. “Thus, we hypothesized that DTCA exposure would reduce the likelihood of individuals engaging in preventive health behaviors.”
“However,” she said, “our results did not support this hypothesis, suggesting that exposure to DTCA for heart disease medication is unlikely to have an adverse effect on individuals’ intentions to engage in diet and exercise.”
That said, she added, “DTCA of prescription drugs can contribute to rising drug costs due to overprescribing of both inappropriate and brand-name drugs over cheaper generic alternatives. While we do not examine this mechanism in our paper, this remains an important question for future research.”
For the study, the team recruited 2,874 individuals (mean age, 53.8 years; 54% men; 83% White) from a U.S. nationally representative sample of people at high risk of cardiovascular disease, the Ipsos Public Affairs KnowledgePanel.
Participants were randomly assigned to one of three interventions: DTCA for heart disease medications, DTCA for heart disease medications with price disclosure, or nonpharmaceutical advertising (control). Each group watched five 1-minute videos for a total of 5 minutes of advertising exposure.
One group viewed ads for four heart disease medications – two ads for sacubitril/valsartan (Entresto, Novartis) and one each for rivaroxaban (Xarelto, Bayer), evolocumab (Repatha, Amgen), and ticagrelor (Brilinta, AstraZeneca); the second group saw the same ads, but with prices spliced in; and controls watched videos for nondrug products, such as consumer electronics.
Participants then completed a questionnaire to measure medication- and lifestyle-related intentions, as well as health-related beliefs and perceptions. Using a scale of 1 (highly unlikely) to 5 (highly likely), they rated the likelihood of their switching medication, asking a physician or insurer about a medication, searching for the drug online, or taking it as directed. The same scale was used to rate the likelihood of their being more physically active or eating more healthfully.
On a scale of 1 (always disagree) to 5 (always agree), they also related their perceptions of pharmaceutical manufacturers as being competent, innovative, and trustworthy.
To measure the magnitude of DTCA associations, the researchers calculated marginal effects (MEs) of treatment – that is, the difference in probability of an outcome between the treatment and control arms.
They found a positive association between DTCA and medication-related behavioral intentions, including intention to switch medication (ME, 0.004; P = .002) and engage in information-seeking behaviors (ME, 0.02; P = .01).
There was no evidence suggesting that pharmaceutical DTCA discouraged use of nonpharmacologic lifestyle interventions to help manage heart disease. DTCA also was positively associated with consumers’ favorable perceptions of pharmaceutical manufacturers (competence: ME, 0.03; P = .01; innovative: ME, 0.03; P = .008).
No differential associations were seen for price disclosures in DTCA.
Questions remain
The authors acknowledged that the study focused on short-term behavioral intentions and that “future research should focus on the long-term effects of advertising in a real-world randomized setting.”
Ms. Singh said additional questions, some of which her team is investigating, include “understanding the interaction between government policies [such as] drug pricing reforms and firms’ advertising decisions; understanding whether observed changes in individuals’ health beliefs translate into actual changes to information-seeking behavior and health care utilization; and whether the demographic, political, and social characteristics of individuals shape their behavioral responses to advertising.”
Johanna Contreras, MD, an advanced heart failure and transplantation cardiologist at Mount Sinai Hospital, New York, said in an interview that the findings don’t surprise her. “The caveat is that this study was an online survey, so it only captured the beliefs and intentions, but not patient demand for the product and use of the product.”
“I do believe DTCA can create positive intentions towards the product ... and could make people more receptive to interventions,” she said. However, the information must be presented in a balanced way.
In addition, she noted, “price is still important. I think people take pricing into account when deciding to proceed with an intervention. If the price is ‘right’ or a little lower than expected, then they will likely consider the product. But if the price is significantly lower, then they may not trust that it is a good product. Generic drugs are an example. Even though they are approved and far cheaper than brand names, patients are often skeptical to take them.”
The study was funded with a grant from the Blue Cross Blue Shield of Illinois Affordability Cures Consortium. Ms. Singh and coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A 5-minute bout of direct-to-consumer advertising (DTCA) for prescription heart drugs was associated with favorable perceptions of both medication use and pharmaceutical companies, but did not seem to negate intentions to use lifestyle interventions, a survey study shows.
Participants who watched ads for various prescription heart drugs, with or without price disclosure, were more likely to report positive perceptions of drug companies and intentions to take actions such as switching medications.
The ads did not seem to affect intentions to eat healthfully and exercise.
The study was published online in JAMA Health Forum.
DTCA ‘unlikely to have an adverse effect’
“Increasing prevalence of DTCA may promote an overreliance on medication over healthy lifestyle choices to manage chronic conditions,” coauthor Yashaswini Singh, MPA, a PhD candidate at the Johns Hopkins University, Baltimore, told this news organization. “Thus, we hypothesized that DTCA exposure would reduce the likelihood of individuals engaging in preventive health behaviors.”
“However,” she said, “our results did not support this hypothesis, suggesting that exposure to DTCA for heart disease medication is unlikely to have an adverse effect on individuals’ intentions to engage in diet and exercise.”
That said, she added, “DTCA of prescription drugs can contribute to rising drug costs due to overprescribing of both inappropriate and brand-name drugs over cheaper generic alternatives. While we do not examine this mechanism in our paper, this remains an important question for future research.”
For the study, the team recruited 2,874 individuals (mean age, 53.8 years; 54% men; 83% White) from a U.S. nationally representative sample of people at high risk of cardiovascular disease, the Ipsos Public Affairs KnowledgePanel.
Participants were randomly assigned to one of three interventions: DTCA for heart disease medications, DTCA for heart disease medications with price disclosure, or nonpharmaceutical advertising (control). Each group watched five 1-minute videos for a total of 5 minutes of advertising exposure.
One group viewed ads for four heart disease medications – two ads for sacubitril/valsartan (Entresto, Novartis) and one each for rivaroxaban (Xarelto, Bayer), evolocumab (Repatha, Amgen), and ticagrelor (Brilinta, AstraZeneca); the second group saw the same ads, but with prices spliced in; and controls watched videos for nondrug products, such as consumer electronics.
Participants then completed a questionnaire to measure medication- and lifestyle-related intentions, as well as health-related beliefs and perceptions. Using a scale of 1 (highly unlikely) to 5 (highly likely), they rated the likelihood of their switching medication, asking a physician or insurer about a medication, searching for the drug online, or taking it as directed. The same scale was used to rate the likelihood of their being more physically active or eating more healthfully.
On a scale of 1 (always disagree) to 5 (always agree), they also related their perceptions of pharmaceutical manufacturers as being competent, innovative, and trustworthy.
To measure the magnitude of DTCA associations, the researchers calculated marginal effects (MEs) of treatment – that is, the difference in probability of an outcome between the treatment and control arms.
They found a positive association between DTCA and medication-related behavioral intentions, including intention to switch medication (ME, 0.004; P = .002) and engage in information-seeking behaviors (ME, 0.02; P = .01).
There was no evidence suggesting that pharmaceutical DTCA discouraged use of nonpharmacologic lifestyle interventions to help manage heart disease. DTCA also was positively associated with consumers’ favorable perceptions of pharmaceutical manufacturers (competence: ME, 0.03; P = .01; innovative: ME, 0.03; P = .008).
No differential associations were seen for price disclosures in DTCA.
Questions remain
The authors acknowledged that the study focused on short-term behavioral intentions and that “future research should focus on the long-term effects of advertising in a real-world randomized setting.”
Ms. Singh said additional questions, some of which her team is investigating, include “understanding the interaction between government policies [such as] drug pricing reforms and firms’ advertising decisions; understanding whether observed changes in individuals’ health beliefs translate into actual changes to information-seeking behavior and health care utilization; and whether the demographic, political, and social characteristics of individuals shape their behavioral responses to advertising.”
Johanna Contreras, MD, an advanced heart failure and transplantation cardiologist at Mount Sinai Hospital, New York, said in an interview that the findings don’t surprise her. “The caveat is that this study was an online survey, so it only captured the beliefs and intentions, but not patient demand for the product and use of the product.”
“I do believe DTCA can create positive intentions towards the product ... and could make people more receptive to interventions,” she said. However, the information must be presented in a balanced way.
In addition, she noted, “price is still important. I think people take pricing into account when deciding to proceed with an intervention. If the price is ‘right’ or a little lower than expected, then they will likely consider the product. But if the price is significantly lower, then they may not trust that it is a good product. Generic drugs are an example. Even though they are approved and far cheaper than brand names, patients are often skeptical to take them.”
The study was funded with a grant from the Blue Cross Blue Shield of Illinois Affordability Cures Consortium. Ms. Singh and coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Antibiotic before oral surgery spares endocarditis; study validates guidelines
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Atrial cardiopathy linked to 35% higher dementia risk
“We cautiously suggest that an understanding of this relationship might provide a basis for new interventional strategies to help thwart the development of dementia,” the authors write.
The research, led by Michelle C. Johansen, MD, department of neurology, Johns Hopkins University, Baltimore, was published online in the Journal of the American Heart Association.
Atrial cardiopathy, characterized by abnormal size and function of the left atrium, has been associated with an increased risk of stroke and atrial fibrillation (AFib), and because both stroke and AFib are associated with an increased dementia risk, the authors write, it was important to investigate whether atrial cardiopathy is linked to dementia.
If that’s the case, they reasoned, the next question was whether that link is independent of AFib and stroke, and their new research suggests that it is.
For this analysis, the researchers conducted a prospective cohort analysis of participants in the Atherosclerosis Risk in Communities (ARIC) study who were attending visit 5 (2011-2013). During their fifth, sixth, and seventh clinical visits, the ARIC participants were evaluated for cognitive decline indicating dementia.
They studied a diverse population of 5,078 older adults living in four U.S. communities: Washington County, Md.; Forsyth County, N.C.; the northwestern suburbs of Minneapolis; and Jackson, Miss.
Just more than a third (34%) had atrial cardiopathy (average age, 75 years; 59% female; 21% Black) and 763 participants developed dementia.
Investigators found that atrial cardiopathy was significantly associated with dementia (adjusted hazard ratio, 1.35 [95% confidence interval, 1.16-1.58]).
They considered ARIC participants to have atrial cardiopathy if they had at least one of the following: P-wave terminal force greater than 5,000 mV·ms in ECG lead V1; NTproBNP greater than 250 pg/mL; or left atrial volume index greater than or equal to 34 mL/m2 by transthoracic echocardiography.
The risk of dementia was even stronger when the researchers defined cardiopathy by at least two biomarkers instead of one (aHR, 1.54 [95% CI, 1.25-1.89]).
The authors point out, however, that this study is observational and cannot make a causal link.
Clifford Kavinsky, MD, PhD, head of the Comprehensive Stroke and Cardiology Clinic at Rush University Medical Center, Chicago, told this news organization that much more research would need to be done to show convincingly that atrial cardiopathy causes dementia.
He called the findings “provocative in trying to understand in a general sense how cardiac dysfunction leads to dementia.”
“We all know heart failure leads to dementia, but now we see there may be a relationship with just dysfunction of the upper chambers,” he said.
Unresolved questions
But it still not clear is what is mediating the connection, who is at risk, and how the increased risk can be prevented, he said.
He said he also wonders whether the results eliminated all patients with atrial fibrillation, a point the authors acknowledge as well.
Researchers list in the limitations that “asymptomatic AFib or silent cerebral infarction may have been missed by the ARIC adjudication process.”
There is broad understanding that preventing heart disease is important for a wide array of reasons, Dr. Kavinsky noted, and one of the reasons is cognitive deterioration.
He said this study helps identify that “even dysfunction of the upper chambers of the heart contributes to the evolution of dementia.”
The study amplifies the need to shift to prevention with heart disease in general, and more specifically in atrial dysfunction, Dr. Kavinsky said, noting a lot of atrial dysfunction is mediated by underlying hypertension and coronary disease.
Researchers evaluated cognitive decline in all participants with a comprehensive array of neuropsychological tests and interviewed some of the patients.
“A diagnosis of dementia was generated based on testing results by a computer diagnostic algorithm and then decided upon by an expert based on the Diagnostic and Statistical Manual of Mental Disorders and the criteria outlined by the National Institutes of Health and the National Institutes of Health,” they write.
Dr. Johansen reported funding from National Institute of Neurological Disorders and Stroke. Study coauthor disclosures are listed in the paper. Dr. Kavinsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“We cautiously suggest that an understanding of this relationship might provide a basis for new interventional strategies to help thwart the development of dementia,” the authors write.
The research, led by Michelle C. Johansen, MD, department of neurology, Johns Hopkins University, Baltimore, was published online in the Journal of the American Heart Association.
Atrial cardiopathy, characterized by abnormal size and function of the left atrium, has been associated with an increased risk of stroke and atrial fibrillation (AFib), and because both stroke and AFib are associated with an increased dementia risk, the authors write, it was important to investigate whether atrial cardiopathy is linked to dementia.
If that’s the case, they reasoned, the next question was whether that link is independent of AFib and stroke, and their new research suggests that it is.
For this analysis, the researchers conducted a prospective cohort analysis of participants in the Atherosclerosis Risk in Communities (ARIC) study who were attending visit 5 (2011-2013). During their fifth, sixth, and seventh clinical visits, the ARIC participants were evaluated for cognitive decline indicating dementia.
They studied a diverse population of 5,078 older adults living in four U.S. communities: Washington County, Md.; Forsyth County, N.C.; the northwestern suburbs of Minneapolis; and Jackson, Miss.
Just more than a third (34%) had atrial cardiopathy (average age, 75 years; 59% female; 21% Black) and 763 participants developed dementia.
Investigators found that atrial cardiopathy was significantly associated with dementia (adjusted hazard ratio, 1.35 [95% confidence interval, 1.16-1.58]).
They considered ARIC participants to have atrial cardiopathy if they had at least one of the following: P-wave terminal force greater than 5,000 mV·ms in ECG lead V1; NTproBNP greater than 250 pg/mL; or left atrial volume index greater than or equal to 34 mL/m2 by transthoracic echocardiography.
The risk of dementia was even stronger when the researchers defined cardiopathy by at least two biomarkers instead of one (aHR, 1.54 [95% CI, 1.25-1.89]).
The authors point out, however, that this study is observational and cannot make a causal link.
Clifford Kavinsky, MD, PhD, head of the Comprehensive Stroke and Cardiology Clinic at Rush University Medical Center, Chicago, told this news organization that much more research would need to be done to show convincingly that atrial cardiopathy causes dementia.
He called the findings “provocative in trying to understand in a general sense how cardiac dysfunction leads to dementia.”
“We all know heart failure leads to dementia, but now we see there may be a relationship with just dysfunction of the upper chambers,” he said.
Unresolved questions
But it still not clear is what is mediating the connection, who is at risk, and how the increased risk can be prevented, he said.
He said he also wonders whether the results eliminated all patients with atrial fibrillation, a point the authors acknowledge as well.
Researchers list in the limitations that “asymptomatic AFib or silent cerebral infarction may have been missed by the ARIC adjudication process.”
There is broad understanding that preventing heart disease is important for a wide array of reasons, Dr. Kavinsky noted, and one of the reasons is cognitive deterioration.
He said this study helps identify that “even dysfunction of the upper chambers of the heart contributes to the evolution of dementia.”
The study amplifies the need to shift to prevention with heart disease in general, and more specifically in atrial dysfunction, Dr. Kavinsky said, noting a lot of atrial dysfunction is mediated by underlying hypertension and coronary disease.
Researchers evaluated cognitive decline in all participants with a comprehensive array of neuropsychological tests and interviewed some of the patients.
“A diagnosis of dementia was generated based on testing results by a computer diagnostic algorithm and then decided upon by an expert based on the Diagnostic and Statistical Manual of Mental Disorders and the criteria outlined by the National Institutes of Health and the National Institutes of Health,” they write.
Dr. Johansen reported funding from National Institute of Neurological Disorders and Stroke. Study coauthor disclosures are listed in the paper. Dr. Kavinsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“We cautiously suggest that an understanding of this relationship might provide a basis for new interventional strategies to help thwart the development of dementia,” the authors write.
The research, led by Michelle C. Johansen, MD, department of neurology, Johns Hopkins University, Baltimore, was published online in the Journal of the American Heart Association.
Atrial cardiopathy, characterized by abnormal size and function of the left atrium, has been associated with an increased risk of stroke and atrial fibrillation (AFib), and because both stroke and AFib are associated with an increased dementia risk, the authors write, it was important to investigate whether atrial cardiopathy is linked to dementia.
If that’s the case, they reasoned, the next question was whether that link is independent of AFib and stroke, and their new research suggests that it is.
For this analysis, the researchers conducted a prospective cohort analysis of participants in the Atherosclerosis Risk in Communities (ARIC) study who were attending visit 5 (2011-2013). During their fifth, sixth, and seventh clinical visits, the ARIC participants were evaluated for cognitive decline indicating dementia.
They studied a diverse population of 5,078 older adults living in four U.S. communities: Washington County, Md.; Forsyth County, N.C.; the northwestern suburbs of Minneapolis; and Jackson, Miss.
Just more than a third (34%) had atrial cardiopathy (average age, 75 years; 59% female; 21% Black) and 763 participants developed dementia.
Investigators found that atrial cardiopathy was significantly associated with dementia (adjusted hazard ratio, 1.35 [95% confidence interval, 1.16-1.58]).
They considered ARIC participants to have atrial cardiopathy if they had at least one of the following: P-wave terminal force greater than 5,000 mV·ms in ECG lead V1; NTproBNP greater than 250 pg/mL; or left atrial volume index greater than or equal to 34 mL/m2 by transthoracic echocardiography.
The risk of dementia was even stronger when the researchers defined cardiopathy by at least two biomarkers instead of one (aHR, 1.54 [95% CI, 1.25-1.89]).
The authors point out, however, that this study is observational and cannot make a causal link.
Clifford Kavinsky, MD, PhD, head of the Comprehensive Stroke and Cardiology Clinic at Rush University Medical Center, Chicago, told this news organization that much more research would need to be done to show convincingly that atrial cardiopathy causes dementia.
He called the findings “provocative in trying to understand in a general sense how cardiac dysfunction leads to dementia.”
“We all know heart failure leads to dementia, but now we see there may be a relationship with just dysfunction of the upper chambers,” he said.
Unresolved questions
But it still not clear is what is mediating the connection, who is at risk, and how the increased risk can be prevented, he said.
He said he also wonders whether the results eliminated all patients with atrial fibrillation, a point the authors acknowledge as well.
Researchers list in the limitations that “asymptomatic AFib or silent cerebral infarction may have been missed by the ARIC adjudication process.”
There is broad understanding that preventing heart disease is important for a wide array of reasons, Dr. Kavinsky noted, and one of the reasons is cognitive deterioration.
He said this study helps identify that “even dysfunction of the upper chambers of the heart contributes to the evolution of dementia.”
The study amplifies the need to shift to prevention with heart disease in general, and more specifically in atrial dysfunction, Dr. Kavinsky said, noting a lot of atrial dysfunction is mediated by underlying hypertension and coronary disease.
Researchers evaluated cognitive decline in all participants with a comprehensive array of neuropsychological tests and interviewed some of the patients.
“A diagnosis of dementia was generated based on testing results by a computer diagnostic algorithm and then decided upon by an expert based on the Diagnostic and Statistical Manual of Mental Disorders and the criteria outlined by the National Institutes of Health and the National Institutes of Health,” they write.
Dr. Johansen reported funding from National Institute of Neurological Disorders and Stroke. Study coauthor disclosures are listed in the paper. Dr. Kavinsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AHA statement outlines symptoms of common heart diseases
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Rich or poor, educated or not, all face risk for hypertension
Hypertension is a global problem that affects poorer countries as much as it affects more affluent ones, a new study suggests.
A cross-sectional study of some 1.2 million adults in low- and middle-income countries (LMICs) found that overall, rates of hypertension were similar across all levels of education and wealth.
The one outlier was Southeast Asia. There, higher levels of education and household wealth were associated with a greater prevalence of hypertension, but the absolute difference was small.
However, the authors of the study caution that hypertension may increasingly affect adults in the lowest socioeconomic groups as LMICs develop economically.
The study is published online in the Journal of the American College of Cardiology.
Assumptions about hypertension are wrong
“We found that the differences in hypertension prevalence between education and household wealth groups were small in most low- and middle-income countries, so the frequent assumption that hypertension mostly affects the wealthiest and most educated groups in low-and middle-income countries appears to be largely untenable,” senior author Pascal Geldsetzer, MD, MPH, PhD, assistant professor of medicine at Stanford (Calif.) University, told this news organization.
High blood pressure is sometimes assumed to be a result of “Westernized” lifestyles characterized by a high intake of calorie-dense foods and salt and low physical activity. As a result, the condition is frequently thought of as mainly afflicting wealthier segments of society in LMICs, which may in part be responsible for the low degree of funding and attention that hypertension in LMICs has received thus far, Dr. Geldsetzer said.
Traditionally, other global health issues, particularly HIV, tuberculosis, and malaria, have received the lion’s share of government funding. Hypertension, thought to be a condition affecting more affluent countries because it is associated with obesity and a sedentary lifestyle, was ignored, he said.
Knowing the socioeconomic gradients associated with hypertension in LMICs and how these may change in the future is important for policy makers, Dr. Geldsetzer added.
Led by Tabea K. Kirschbaum, MD, Heidelberg Institute of Global Health, University of Heidelberg, Germany, the researchers examined hypertension prevalence by education and household wealth from 76 LMICs in 1,211,386 participants and assessed whether the effect was modified by the country’s gross domestic product (GDP).
Their analysis included 76 surveys, of which 58 were World Health Organization Stepwise Approach to Surveillance surveys. The median age of the participants was 40 years, and 58.5% were women.
Overall, hypertension prevalence tended to be similar across all educational and household wealth levels and across countries with lower and higher GDPs, although there were some “negligible” country and regional variations.
Treatment rates with blood pressure–lowering drugs for participants who had hypertension were higher in countries with higher GDPs.
Women were more likely to be taking medication than were men.
In some countries, the proportion of individuals taking blood pressure–lowering medication was higher in wealthier households.
In Southeast Asia, however, there was a strong association found between the prevalence of hypertension and higher household wealth levels. Compared with the least wealthy, the risk ratio for the wealthiest was 1.28 (95% confidence interval, 1.22-1.34). A similar association was found for education levels as well.
Education was negatively associated with hypertension in the Eastern Mediterranean. Rates were higher among men than among women.
In an accompanying editorial, Yashashwi Pokharel, MBBS, MSCR, from Wake Forest School of Medicine, Winston-Salem, N.C., and colleagues write:
“Now that we know that hypertension prevalence is not different in the poorest, the least educated, or the least economically developed countries, compared with their wealthier and educated counterparts, we should develop, test, and implement effective strategies to enhance global equity in hypertension care.”
Dr. Pokharel told this news organization that, despite the study’s limitations including heterogeneous data, measurement techniques, and blood pressure monitor use across countries, the signal is loud and clear.
“We urgently need to focus on turning off the faucet by addressing the major determinants of increasing hypertension burden, including the sociocultural and political determinants,” he said. “In this regard, setting funding priorities by donors for hypertension, capacity building, and testing and scaling effective population level hypertension prevention and treatment strategies, developed together with local stakeholders, can have a long-lasting effect. If we perpetuate the neglect, we will ineffectively spend more time mopping up the floor.”
Dr. Geldsetzer is a Chan Zuckerberg Biohub investigator. Dr. Pokharel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hypertension is a global problem that affects poorer countries as much as it affects more affluent ones, a new study suggests.
A cross-sectional study of some 1.2 million adults in low- and middle-income countries (LMICs) found that overall, rates of hypertension were similar across all levels of education and wealth.
The one outlier was Southeast Asia. There, higher levels of education and household wealth were associated with a greater prevalence of hypertension, but the absolute difference was small.
However, the authors of the study caution that hypertension may increasingly affect adults in the lowest socioeconomic groups as LMICs develop economically.
The study is published online in the Journal of the American College of Cardiology.
Assumptions about hypertension are wrong
“We found that the differences in hypertension prevalence between education and household wealth groups were small in most low- and middle-income countries, so the frequent assumption that hypertension mostly affects the wealthiest and most educated groups in low-and middle-income countries appears to be largely untenable,” senior author Pascal Geldsetzer, MD, MPH, PhD, assistant professor of medicine at Stanford (Calif.) University, told this news organization.
High blood pressure is sometimes assumed to be a result of “Westernized” lifestyles characterized by a high intake of calorie-dense foods and salt and low physical activity. As a result, the condition is frequently thought of as mainly afflicting wealthier segments of society in LMICs, which may in part be responsible for the low degree of funding and attention that hypertension in LMICs has received thus far, Dr. Geldsetzer said.
Traditionally, other global health issues, particularly HIV, tuberculosis, and malaria, have received the lion’s share of government funding. Hypertension, thought to be a condition affecting more affluent countries because it is associated with obesity and a sedentary lifestyle, was ignored, he said.
Knowing the socioeconomic gradients associated with hypertension in LMICs and how these may change in the future is important for policy makers, Dr. Geldsetzer added.
Led by Tabea K. Kirschbaum, MD, Heidelberg Institute of Global Health, University of Heidelberg, Germany, the researchers examined hypertension prevalence by education and household wealth from 76 LMICs in 1,211,386 participants and assessed whether the effect was modified by the country’s gross domestic product (GDP).
Their analysis included 76 surveys, of which 58 were World Health Organization Stepwise Approach to Surveillance surveys. The median age of the participants was 40 years, and 58.5% were women.
Overall, hypertension prevalence tended to be similar across all educational and household wealth levels and across countries with lower and higher GDPs, although there were some “negligible” country and regional variations.
Treatment rates with blood pressure–lowering drugs for participants who had hypertension were higher in countries with higher GDPs.
Women were more likely to be taking medication than were men.
In some countries, the proportion of individuals taking blood pressure–lowering medication was higher in wealthier households.
In Southeast Asia, however, there was a strong association found between the prevalence of hypertension and higher household wealth levels. Compared with the least wealthy, the risk ratio for the wealthiest was 1.28 (95% confidence interval, 1.22-1.34). A similar association was found for education levels as well.
Education was negatively associated with hypertension in the Eastern Mediterranean. Rates were higher among men than among women.
In an accompanying editorial, Yashashwi Pokharel, MBBS, MSCR, from Wake Forest School of Medicine, Winston-Salem, N.C., and colleagues write:
“Now that we know that hypertension prevalence is not different in the poorest, the least educated, or the least economically developed countries, compared with their wealthier and educated counterparts, we should develop, test, and implement effective strategies to enhance global equity in hypertension care.”
Dr. Pokharel told this news organization that, despite the study’s limitations including heterogeneous data, measurement techniques, and blood pressure monitor use across countries, the signal is loud and clear.
“We urgently need to focus on turning off the faucet by addressing the major determinants of increasing hypertension burden, including the sociocultural and political determinants,” he said. “In this regard, setting funding priorities by donors for hypertension, capacity building, and testing and scaling effective population level hypertension prevention and treatment strategies, developed together with local stakeholders, can have a long-lasting effect. If we perpetuate the neglect, we will ineffectively spend more time mopping up the floor.”
Dr. Geldsetzer is a Chan Zuckerberg Biohub investigator. Dr. Pokharel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hypertension is a global problem that affects poorer countries as much as it affects more affluent ones, a new study suggests.
A cross-sectional study of some 1.2 million adults in low- and middle-income countries (LMICs) found that overall, rates of hypertension were similar across all levels of education and wealth.
The one outlier was Southeast Asia. There, higher levels of education and household wealth were associated with a greater prevalence of hypertension, but the absolute difference was small.
However, the authors of the study caution that hypertension may increasingly affect adults in the lowest socioeconomic groups as LMICs develop economically.
The study is published online in the Journal of the American College of Cardiology.
Assumptions about hypertension are wrong
“We found that the differences in hypertension prevalence between education and household wealth groups were small in most low- and middle-income countries, so the frequent assumption that hypertension mostly affects the wealthiest and most educated groups in low-and middle-income countries appears to be largely untenable,” senior author Pascal Geldsetzer, MD, MPH, PhD, assistant professor of medicine at Stanford (Calif.) University, told this news organization.
High blood pressure is sometimes assumed to be a result of “Westernized” lifestyles characterized by a high intake of calorie-dense foods and salt and low physical activity. As a result, the condition is frequently thought of as mainly afflicting wealthier segments of society in LMICs, which may in part be responsible for the low degree of funding and attention that hypertension in LMICs has received thus far, Dr. Geldsetzer said.
Traditionally, other global health issues, particularly HIV, tuberculosis, and malaria, have received the lion’s share of government funding. Hypertension, thought to be a condition affecting more affluent countries because it is associated with obesity and a sedentary lifestyle, was ignored, he said.
Knowing the socioeconomic gradients associated with hypertension in LMICs and how these may change in the future is important for policy makers, Dr. Geldsetzer added.
Led by Tabea K. Kirschbaum, MD, Heidelberg Institute of Global Health, University of Heidelberg, Germany, the researchers examined hypertension prevalence by education and household wealth from 76 LMICs in 1,211,386 participants and assessed whether the effect was modified by the country’s gross domestic product (GDP).
Their analysis included 76 surveys, of which 58 were World Health Organization Stepwise Approach to Surveillance surveys. The median age of the participants was 40 years, and 58.5% were women.
Overall, hypertension prevalence tended to be similar across all educational and household wealth levels and across countries with lower and higher GDPs, although there were some “negligible” country and regional variations.
Treatment rates with blood pressure–lowering drugs for participants who had hypertension were higher in countries with higher GDPs.
Women were more likely to be taking medication than were men.
In some countries, the proportion of individuals taking blood pressure–lowering medication was higher in wealthier households.
In Southeast Asia, however, there was a strong association found between the prevalence of hypertension and higher household wealth levels. Compared with the least wealthy, the risk ratio for the wealthiest was 1.28 (95% confidence interval, 1.22-1.34). A similar association was found for education levels as well.
Education was negatively associated with hypertension in the Eastern Mediterranean. Rates were higher among men than among women.
In an accompanying editorial, Yashashwi Pokharel, MBBS, MSCR, from Wake Forest School of Medicine, Winston-Salem, N.C., and colleagues write:
“Now that we know that hypertension prevalence is not different in the poorest, the least educated, or the least economically developed countries, compared with their wealthier and educated counterparts, we should develop, test, and implement effective strategies to enhance global equity in hypertension care.”
Dr. Pokharel told this news organization that, despite the study’s limitations including heterogeneous data, measurement techniques, and blood pressure monitor use across countries, the signal is loud and clear.
“We urgently need to focus on turning off the faucet by addressing the major determinants of increasing hypertension burden, including the sociocultural and political determinants,” he said. “In this regard, setting funding priorities by donors for hypertension, capacity building, and testing and scaling effective population level hypertension prevention and treatment strategies, developed together with local stakeholders, can have a long-lasting effect. If we perpetuate the neglect, we will ineffectively spend more time mopping up the floor.”
Dr. Geldsetzer is a Chan Zuckerberg Biohub investigator. Dr. Pokharel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
‘Obesity paradox’ in AFib challenged as mortality climbs with BMI
The relationship between body mass index (BMI) and all-cause mortality in patients with atrial fibrillation (AFib) is U-shaped, with the risk highest in those who are underweight or severely obese and lowest in patients defined simply as obese, a registry analysis suggests. It also showed a similar relationship between BMI and risk for new or worsening heart failure (HF).
Mortality bottomed out at a BMI of about 30-35 kg/m2, which suggests that mild obesity was protective, compared even with “normal-weight” or “overweight” BMI. Still, mortality went up sharply from there with rising BMI.
But higher BMI, a surrogate for obesity, apparently didn’t worsen outcomes by itself. The risk for death from any cause at higher obesity levels was found to depend a lot on related risk factors and comorbidities when the analysis controlled for conditions such as diabetes and hypertension.
The findings suggest an inverse relationship between BMI and all-cause mortality in AFib only for patients with BMI less than about 30. They therefore argue against any “obesity paradox” in AFib that posits consistently better survival with increasing levels of obesity, say researchers, based on their analysis of patients with new-onset AFib in the GARFIELD-AF registry.
“It’s common practice now for clinicians to discuss weight within a clinic setting when they’re talking to their AFib patients,” observed Christian Fielder Camm, BM, BCh, University of Oxford (England), and Royal Berkshire NHS Foundation Trust, Reading, England. So studies suggesting an inverse association between BMI and AFib-related risk can be a concern.
Such studies “seem to suggest that once you’ve got AFib, maintaining a high or very high BMI may in some way be protective – which is contrary to what would seem to make sense and certainly contrary to what our results have shown,” Dr. Camm told this news organization.
“I think that having further evidence now to suggest, actually, that greater BMI is associated with a greater risk of all-cause mortality and heart failure helps reframe that discussion at the physician-patient interaction level more clearly, and ensures that we’re able to talk to our patients appropriately about risks associated with BMI and atrial fibrillation,” said Dr. Camm, who is lead author on the analysis published in Open Heart.
“Obesity is a cause of most cardiovascular diseases, but [these] data would support that being overweight or having mild obesity does not increase the risk,” observed Carl J. Lavie, MD, of the John Ochsner Heart and Vascular Institute, New Orleans, La., and the Ochsner Clinical School at the University of Queensland, Brisbane, Australia.
“At a BMI of 40, it’s very important for them to lose weight for their long-term prognosis,” Dr. Lavie noted, but “at a BMI of 30, the important thing would be to prevent further weight gain. And if they could keep their BMI of 30, they should have a good prognosis. Their prognosis would be particularly good if they didn’t gain weight and put themselves in a more extreme obesity class that is associated with worse risk.”
The current analysis, Dr. Lavie said, “is way better than the AFFIRM study,” which yielded an obesity-paradox report on its patients with AFib about a dozen years ago. “It’s got more data, more numbers, more statistical power,” and breaks BMI into more categories.
That previous analysis based on the influential AFFIRM randomized trial separated its 4,060 patients with AFib into normal (BMI, 18.5-25), overweight (BMI, 25-30), and obese (BMI, > 30) categories, per the convention at the time. It concluded that “obese patients with atrial fibrillation appear to have better long-term outcomes than nonobese patients.”
Bleeding risk on oral anticoagulants
Also noteworthy in the current analysis, variation in BMI didn’t seem to affect mortality or risk for major bleeding or nonhemorrhagic stroke according to choice of oral anticoagulant – whether a new oral anticoagulant (NOAC) or a vitamin K antagonist (VKA).
“We saw that even in the obese and extremely obese group, all-cause mortality was lower in the group taking NOACs, compared with taking warfarin,” Dr. Camm observed, “which goes against the idea that we would need any kind of dose adjustments for increased BMI.”
Indeed, the report notes, use of NOACs, compared with VKA, was associated with a 23% drop in risk for death among patients who were either normal weight or overweight and also in those who were obese or extremely obese.
Those findings “are basically saying that the NOACs look better than warfarin regardless of weight,” agreed Dr. Lavie. “The problem is that the study is not very powered.”
Whereas the benefits of NOACs, compared to VKA, seem similar for patients with a BMI of 30 or 34, compared with a BMI of 23, for example, “none of the studies has many people with 50 BMI.” Many clinicians “feel uncomfortable giving the same dose of NOAC to somebody who has a 60 BMI,” he said. At least with warfarin, “you can check the INR [international normalized ratio].”
The current analysis included 40,482 patients with recently diagnosed AFib and at least one other stroke risk factor from among the registry’s more than 50,000 patients from 35 countries, enrolled from 2010 to 2016. They were followed for 2 years.
The 703 patients with BMI under 18.5 at AFib diagnosis were classified per World Health Organization definitions as underweight; the 13,095 with BMI 18.5-25 as normal weight; the 15,043 with BMI 25-30 as overweight; the 7,560 with BMI 30-35 as obese; and the 4,081 with BMI above 35 as extremely obese. Their ages averaged 71 years, and 55.6% were men.
BMI effects on different outcomes
Relationships between BMI and all-cause mortality and between BMI and new or worsening HF emerged as U-shaped, the risk climbing with both increasing and decreasing BMI. The nadir BMI for risk was about 30 in the case of mortality and about 25 for new or worsening HF.
The all-cause mortality risk rose by 32% for every 5 BMI points lower than a BMI of 30, and by 16% for every 5 BMI points higher than 30, in a partially adjusted analysis. The risk for new or worsening HF rose significantly with increasing but not decreasing BMI, and the reverse was observed for the endpoint of major bleeding.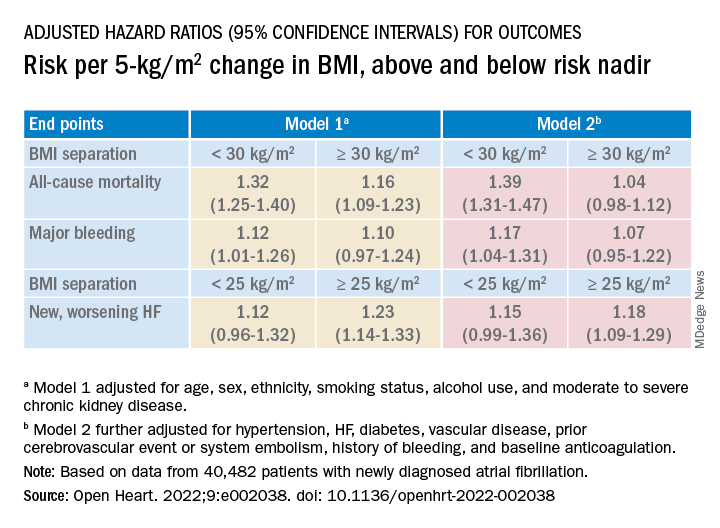
The effect of BMI on all-cause mortality was “substantially attenuated” when the analysis was further adjusted with “likely mediators of any association between BMI and outcomes,” including hypertension, diabetes, HF, cerebrovascular events, and history of bleeding, Dr. Camm said.
That blunted BMI-mortality relationship, he said, “suggests that a lot of the effect is mediated through relatively traditional risk factors like hypertension and diabetes.”
The 2010 AFFIRM analysis by BMI, Dr. Lavie noted, “didn’t even look at the underweight; they actually threw them out.” Yet, such patients with AFib, who tend to be extremely frail or have chronic diseases or conditions other than the arrhythmia, are common. A take-home of the current study is that “the underweight with atrial fibrillation have a really bad prognosis.”
That message isn’t heard as much, he observed, “but is as important as saying that BMI 30 has the best prognosis. The worst prognosis is with the underweight or the really extreme obese.”
Dr. Camm discloses research funding from the British Heart Foundation. Disclosures for the other authors are in the report. Dr. Lavie has previously disclosed serving as a speaker and consultant for PAI Health and DSM Nutritional Products and is the author of “The Obesity Paradox: When Thinner Means Sicker and Heavier Means Healthier” (Avery, 2014).
A version of this article first appeared on Medscape.com.
The relationship between body mass index (BMI) and all-cause mortality in patients with atrial fibrillation (AFib) is U-shaped, with the risk highest in those who are underweight or severely obese and lowest in patients defined simply as obese, a registry analysis suggests. It also showed a similar relationship between BMI and risk for new or worsening heart failure (HF).
Mortality bottomed out at a BMI of about 30-35 kg/m2, which suggests that mild obesity was protective, compared even with “normal-weight” or “overweight” BMI. Still, mortality went up sharply from there with rising BMI.
But higher BMI, a surrogate for obesity, apparently didn’t worsen outcomes by itself. The risk for death from any cause at higher obesity levels was found to depend a lot on related risk factors and comorbidities when the analysis controlled for conditions such as diabetes and hypertension.
The findings suggest an inverse relationship between BMI and all-cause mortality in AFib only for patients with BMI less than about 30. They therefore argue against any “obesity paradox” in AFib that posits consistently better survival with increasing levels of obesity, say researchers, based on their analysis of patients with new-onset AFib in the GARFIELD-AF registry.
“It’s common practice now for clinicians to discuss weight within a clinic setting when they’re talking to their AFib patients,” observed Christian Fielder Camm, BM, BCh, University of Oxford (England), and Royal Berkshire NHS Foundation Trust, Reading, England. So studies suggesting an inverse association between BMI and AFib-related risk can be a concern.
Such studies “seem to suggest that once you’ve got AFib, maintaining a high or very high BMI may in some way be protective – which is contrary to what would seem to make sense and certainly contrary to what our results have shown,” Dr. Camm told this news organization.
“I think that having further evidence now to suggest, actually, that greater BMI is associated with a greater risk of all-cause mortality and heart failure helps reframe that discussion at the physician-patient interaction level more clearly, and ensures that we’re able to talk to our patients appropriately about risks associated with BMI and atrial fibrillation,” said Dr. Camm, who is lead author on the analysis published in Open Heart.
“Obesity is a cause of most cardiovascular diseases, but [these] data would support that being overweight or having mild obesity does not increase the risk,” observed Carl J. Lavie, MD, of the John Ochsner Heart and Vascular Institute, New Orleans, La., and the Ochsner Clinical School at the University of Queensland, Brisbane, Australia.
“At a BMI of 40, it’s very important for them to lose weight for their long-term prognosis,” Dr. Lavie noted, but “at a BMI of 30, the important thing would be to prevent further weight gain. And if they could keep their BMI of 30, they should have a good prognosis. Their prognosis would be particularly good if they didn’t gain weight and put themselves in a more extreme obesity class that is associated with worse risk.”
The current analysis, Dr. Lavie said, “is way better than the AFFIRM study,” which yielded an obesity-paradox report on its patients with AFib about a dozen years ago. “It’s got more data, more numbers, more statistical power,” and breaks BMI into more categories.
That previous analysis based on the influential AFFIRM randomized trial separated its 4,060 patients with AFib into normal (BMI, 18.5-25), overweight (BMI, 25-30), and obese (BMI, > 30) categories, per the convention at the time. It concluded that “obese patients with atrial fibrillation appear to have better long-term outcomes than nonobese patients.”
Bleeding risk on oral anticoagulants
Also noteworthy in the current analysis, variation in BMI didn’t seem to affect mortality or risk for major bleeding or nonhemorrhagic stroke according to choice of oral anticoagulant – whether a new oral anticoagulant (NOAC) or a vitamin K antagonist (VKA).
“We saw that even in the obese and extremely obese group, all-cause mortality was lower in the group taking NOACs, compared with taking warfarin,” Dr. Camm observed, “which goes against the idea that we would need any kind of dose adjustments for increased BMI.”
Indeed, the report notes, use of NOACs, compared with VKA, was associated with a 23% drop in risk for death among patients who were either normal weight or overweight and also in those who were obese or extremely obese.
Those findings “are basically saying that the NOACs look better than warfarin regardless of weight,” agreed Dr. Lavie. “The problem is that the study is not very powered.”
Whereas the benefits of NOACs, compared to VKA, seem similar for patients with a BMI of 30 or 34, compared with a BMI of 23, for example, “none of the studies has many people with 50 BMI.” Many clinicians “feel uncomfortable giving the same dose of NOAC to somebody who has a 60 BMI,” he said. At least with warfarin, “you can check the INR [international normalized ratio].”
The current analysis included 40,482 patients with recently diagnosed AFib and at least one other stroke risk factor from among the registry’s more than 50,000 patients from 35 countries, enrolled from 2010 to 2016. They were followed for 2 years.
The 703 patients with BMI under 18.5 at AFib diagnosis were classified per World Health Organization definitions as underweight; the 13,095 with BMI 18.5-25 as normal weight; the 15,043 with BMI 25-30 as overweight; the 7,560 with BMI 30-35 as obese; and the 4,081 with BMI above 35 as extremely obese. Their ages averaged 71 years, and 55.6% were men.
BMI effects on different outcomes
Relationships between BMI and all-cause mortality and between BMI and new or worsening HF emerged as U-shaped, the risk climbing with both increasing and decreasing BMI. The nadir BMI for risk was about 30 in the case of mortality and about 25 for new or worsening HF.
The all-cause mortality risk rose by 32% for every 5 BMI points lower than a BMI of 30, and by 16% for every 5 BMI points higher than 30, in a partially adjusted analysis. The risk for new or worsening HF rose significantly with increasing but not decreasing BMI, and the reverse was observed for the endpoint of major bleeding.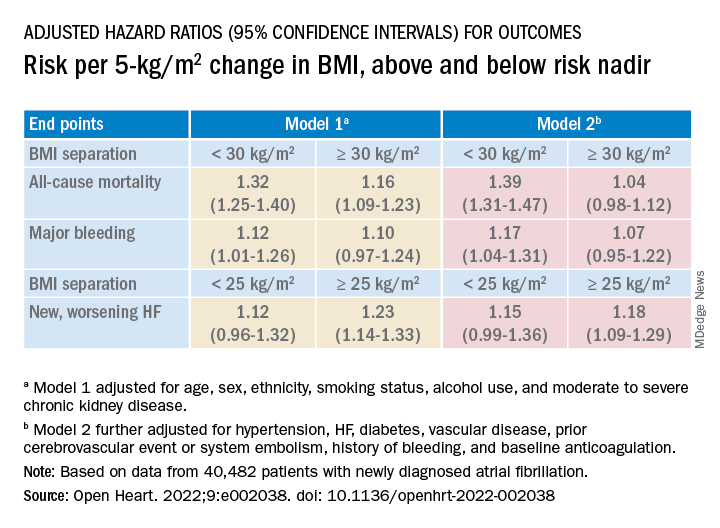
The effect of BMI on all-cause mortality was “substantially attenuated” when the analysis was further adjusted with “likely mediators of any association between BMI and outcomes,” including hypertension, diabetes, HF, cerebrovascular events, and history of bleeding, Dr. Camm said.
That blunted BMI-mortality relationship, he said, “suggests that a lot of the effect is mediated through relatively traditional risk factors like hypertension and diabetes.”
The 2010 AFFIRM analysis by BMI, Dr. Lavie noted, “didn’t even look at the underweight; they actually threw them out.” Yet, such patients with AFib, who tend to be extremely frail or have chronic diseases or conditions other than the arrhythmia, are common. A take-home of the current study is that “the underweight with atrial fibrillation have a really bad prognosis.”
That message isn’t heard as much, he observed, “but is as important as saying that BMI 30 has the best prognosis. The worst prognosis is with the underweight or the really extreme obese.”
Dr. Camm discloses research funding from the British Heart Foundation. Disclosures for the other authors are in the report. Dr. Lavie has previously disclosed serving as a speaker and consultant for PAI Health and DSM Nutritional Products and is the author of “The Obesity Paradox: When Thinner Means Sicker and Heavier Means Healthier” (Avery, 2014).
A version of this article first appeared on Medscape.com.
The relationship between body mass index (BMI) and all-cause mortality in patients with atrial fibrillation (AFib) is U-shaped, with the risk highest in those who are underweight or severely obese and lowest in patients defined simply as obese, a registry analysis suggests. It also showed a similar relationship between BMI and risk for new or worsening heart failure (HF).
Mortality bottomed out at a BMI of about 30-35 kg/m2, which suggests that mild obesity was protective, compared even with “normal-weight” or “overweight” BMI. Still, mortality went up sharply from there with rising BMI.
But higher BMI, a surrogate for obesity, apparently didn’t worsen outcomes by itself. The risk for death from any cause at higher obesity levels was found to depend a lot on related risk factors and comorbidities when the analysis controlled for conditions such as diabetes and hypertension.
The findings suggest an inverse relationship between BMI and all-cause mortality in AFib only for patients with BMI less than about 30. They therefore argue against any “obesity paradox” in AFib that posits consistently better survival with increasing levels of obesity, say researchers, based on their analysis of patients with new-onset AFib in the GARFIELD-AF registry.
“It’s common practice now for clinicians to discuss weight within a clinic setting when they’re talking to their AFib patients,” observed Christian Fielder Camm, BM, BCh, University of Oxford (England), and Royal Berkshire NHS Foundation Trust, Reading, England. So studies suggesting an inverse association between BMI and AFib-related risk can be a concern.
Such studies “seem to suggest that once you’ve got AFib, maintaining a high or very high BMI may in some way be protective – which is contrary to what would seem to make sense and certainly contrary to what our results have shown,” Dr. Camm told this news organization.
“I think that having further evidence now to suggest, actually, that greater BMI is associated with a greater risk of all-cause mortality and heart failure helps reframe that discussion at the physician-patient interaction level more clearly, and ensures that we’re able to talk to our patients appropriately about risks associated with BMI and atrial fibrillation,” said Dr. Camm, who is lead author on the analysis published in Open Heart.
“Obesity is a cause of most cardiovascular diseases, but [these] data would support that being overweight or having mild obesity does not increase the risk,” observed Carl J. Lavie, MD, of the John Ochsner Heart and Vascular Institute, New Orleans, La., and the Ochsner Clinical School at the University of Queensland, Brisbane, Australia.
“At a BMI of 40, it’s very important for them to lose weight for their long-term prognosis,” Dr. Lavie noted, but “at a BMI of 30, the important thing would be to prevent further weight gain. And if they could keep their BMI of 30, they should have a good prognosis. Their prognosis would be particularly good if they didn’t gain weight and put themselves in a more extreme obesity class that is associated with worse risk.”
The current analysis, Dr. Lavie said, “is way better than the AFFIRM study,” which yielded an obesity-paradox report on its patients with AFib about a dozen years ago. “It’s got more data, more numbers, more statistical power,” and breaks BMI into more categories.
That previous analysis based on the influential AFFIRM randomized trial separated its 4,060 patients with AFib into normal (BMI, 18.5-25), overweight (BMI, 25-30), and obese (BMI, > 30) categories, per the convention at the time. It concluded that “obese patients with atrial fibrillation appear to have better long-term outcomes than nonobese patients.”
Bleeding risk on oral anticoagulants
Also noteworthy in the current analysis, variation in BMI didn’t seem to affect mortality or risk for major bleeding or nonhemorrhagic stroke according to choice of oral anticoagulant – whether a new oral anticoagulant (NOAC) or a vitamin K antagonist (VKA).
“We saw that even in the obese and extremely obese group, all-cause mortality was lower in the group taking NOACs, compared with taking warfarin,” Dr. Camm observed, “which goes against the idea that we would need any kind of dose adjustments for increased BMI.”
Indeed, the report notes, use of NOACs, compared with VKA, was associated with a 23% drop in risk for death among patients who were either normal weight or overweight and also in those who were obese or extremely obese.
Those findings “are basically saying that the NOACs look better than warfarin regardless of weight,” agreed Dr. Lavie. “The problem is that the study is not very powered.”
Whereas the benefits of NOACs, compared to VKA, seem similar for patients with a BMI of 30 or 34, compared with a BMI of 23, for example, “none of the studies has many people with 50 BMI.” Many clinicians “feel uncomfortable giving the same dose of NOAC to somebody who has a 60 BMI,” he said. At least with warfarin, “you can check the INR [international normalized ratio].”
The current analysis included 40,482 patients with recently diagnosed AFib and at least one other stroke risk factor from among the registry’s more than 50,000 patients from 35 countries, enrolled from 2010 to 2016. They were followed for 2 years.
The 703 patients with BMI under 18.5 at AFib diagnosis were classified per World Health Organization definitions as underweight; the 13,095 with BMI 18.5-25 as normal weight; the 15,043 with BMI 25-30 as overweight; the 7,560 with BMI 30-35 as obese; and the 4,081 with BMI above 35 as extremely obese. Their ages averaged 71 years, and 55.6% were men.
BMI effects on different outcomes
Relationships between BMI and all-cause mortality and between BMI and new or worsening HF emerged as U-shaped, the risk climbing with both increasing and decreasing BMI. The nadir BMI for risk was about 30 in the case of mortality and about 25 for new or worsening HF.
The all-cause mortality risk rose by 32% for every 5 BMI points lower than a BMI of 30, and by 16% for every 5 BMI points higher than 30, in a partially adjusted analysis. The risk for new or worsening HF rose significantly with increasing but not decreasing BMI, and the reverse was observed for the endpoint of major bleeding.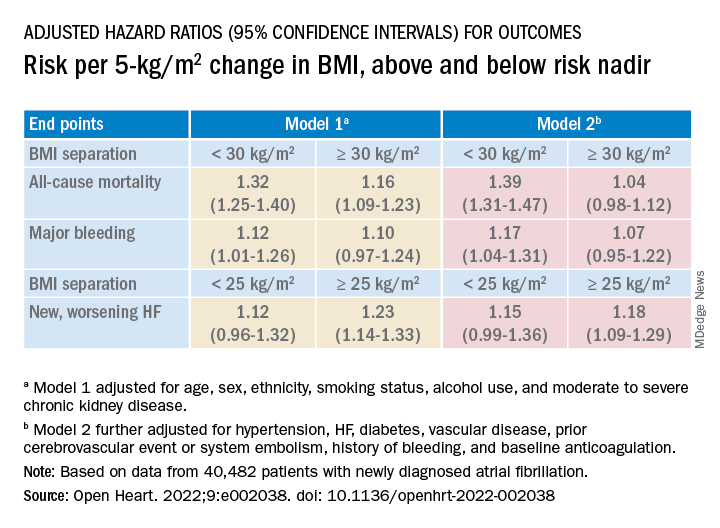
The effect of BMI on all-cause mortality was “substantially attenuated” when the analysis was further adjusted with “likely mediators of any association between BMI and outcomes,” including hypertension, diabetes, HF, cerebrovascular events, and history of bleeding, Dr. Camm said.
That blunted BMI-mortality relationship, he said, “suggests that a lot of the effect is mediated through relatively traditional risk factors like hypertension and diabetes.”
The 2010 AFFIRM analysis by BMI, Dr. Lavie noted, “didn’t even look at the underweight; they actually threw them out.” Yet, such patients with AFib, who tend to be extremely frail or have chronic diseases or conditions other than the arrhythmia, are common. A take-home of the current study is that “the underweight with atrial fibrillation have a really bad prognosis.”
That message isn’t heard as much, he observed, “but is as important as saying that BMI 30 has the best prognosis. The worst prognosis is with the underweight or the really extreme obese.”
Dr. Camm discloses research funding from the British Heart Foundation. Disclosures for the other authors are in the report. Dr. Lavie has previously disclosed serving as a speaker and consultant for PAI Health and DSM Nutritional Products and is the author of “The Obesity Paradox: When Thinner Means Sicker and Heavier Means Healthier” (Avery, 2014).
A version of this article first appeared on Medscape.com.
FROM OPEN HEART
Blood pressure smartphone app fails to beat standard self-monitoring
Here’s another vote for less screen time.
“By itself, standard self-measured blood pressure (SMBP) has minimal effect on BP control,” wrote lead author Mark J. Pletcher, MD, of the University of California, San Francisco, and colleagues in JAMA Internal Medicine. “To improve BP control, SMBP must be accompanied by patient feedback, counseling, or other cointerventions, and the BP-lowering effects of SMBP appear to be proportional to the intensity of the cointervention.”
While this is known, higher-intensity cointerventions demand both money and time, prompting development of new devices that link with smartphone apps, they continued.
In the prospective randomized trial, patients with hypertension were randomly assigned to self-measure their blood pressure using a standard device that paired with a connected smartphone application or to self-measure their blood pressure with a standard device alone. Both groups achieved about an 11 mm Hg reduction in systolic BP over 6 months, reported similar levels of satisfaction with the monitoring process, and shared their readings with their physicians with similar frequency.
Methods
Dr. Pletcher and colleagues enrolled 2,101 adults who self-reported a systolic BP greater than 145 mm Hg and expressed a commitment to reduce their BP by at least 10 points in their trial. The participants, who were generally middle-aged or older, were randomized in a 1:1 ratio to monitor their BP using standard SMBP or “enhanced” SMBP. The standard group used the OMRON BP monitor alone, while the enhanced group used the same BP monitor coupled with the OMRON Connect smartphone app.
After 6 months of follow-up for each patient, mean BP reduction from baseline in the standard group was 10.6 mm Hg, compared with 10.7 mm Hg in the enhanced group, a nonsignificant difference (P = .81). While slightly more patients in the enhanced group achieved a BP lower than 140/90 mm Hg (32% vs. 29%; odds ratio, 1.17; 95% confidence interval, 1.01-1.34), this trend did not extend below the 130/80 mm Hg threshold.
Other secondary outcomes were also similar between groups. For example, 70% of participants in the enhanced group said they would recommend their SMBP process to a friend, compared with 69% of participants who followed the standard monitoring approach. The smartphone app had little impact on sharing readings with physicians, either, based on a 44% share rate in the enhanced group versus 48% in the standard group (P = .22).
“Enhanced SMBP does not provide any additional reduction in BP,” the investigators concluded.
New devices that link with smartphone apps, like the one used in this trial, “transmit BP measurements via wireless connection to the patient’s smartphone, where they are processed in a smartphone application to support tracking, visualization, interpretation, reminders to measure BP and/or take medications; recommendations for lifestyle interventions, medication adherence, or to discuss their BP with their clinician; and communications (for example, emailing a summary to a family member or clinician),” the researchers explained. While these devices are “only slightly more expensive than standard SMBP devices,” their relative efficacy over standard SMBP is “unclear.”
Findings can likely be extrapolated to other apps
Although the trial evaluated just one smartphone app, Dr. Pletcher suggested that the findings can likely be extrapolated to other apps.
“Most basic BP-tracking apps have some version or subset of the same essential functionality,” he said, in an interview. “My guess is that apps that meet this description without some substantially different technology or feature would likely show the same basic results as we did.”
Making a similar remark, Matthew Jung, MD, of Keck Medicine of USC, Los Angeles, stated that the findings can be “reasonably extrapolated” to other BP-tracking apps with similar functionality “if we put aside the study’s issues with power.”
When it comes to smartphone apps, active engagement is needed to achieve greater impacts on blood pressure, Dr. Pletcher said, but “there is so much competition for people’s attention on their phone that it is hard to maintain active engagement with any health-related app for long.”
Still, Dr. Pletcher hasn’t given up on biometric apps, noting that “with the right technology and connectivity and user experience (for both patient and clinician), they still could be game-changing for managing chronic conditions like hypertension.”
To this end, he and his colleagues are exploring technologies to passively monitor health-related measurements like BP, potentially sidestepping the pitfall of active engagement.
Dr. Jung said the study is noteworthy for several reasons, including its large size, similar level of comfort with technology reported by both groups, and representation of Black and Hispanic participants, who accounted for almost one-third of the population.
Study limitations
Dr. Jung pointed out several study limitations, including the lack of standardized measurement of BP, which left more than one-third of patients unevaluated via chart review, as well as gaps in usage data, such as that one-third of the participants never confirmed receipt of a device, and less than half of the enhanced group reported using the smartphone application.
These limitations “may have detracted from its ability to identify the true efficacy of an enhanced app-based BP tracking device,” he said. “In contrast, each of these issues also helped us get a better picture for how well these devices may work in the real world.”
Dr. Jung also commented on the duration of the study, noting that only 10 weeks passed, on average, from baseline to follow-up BP measurement, which “may not have been sufficient for a possible difference between enhanced and standard BP monitoring to become noticeable.”
“This may be especially important when taking into consideration the time required to mail the devices out to patients, for patients to become familiar with usage of the devices, and for them to start using the devices in a meaningful way,” he added.
The study was supported the Patient-Centered Outcomes Research Institute, the American Medical Association, and the American Heart Association. The investigators disclosed additional relationships with Pfizer, Bristol Myers Squibb, and Novartis. Dr. Jung, who was not involved in the study, disclosed no relevant conflicts of interest.
Here’s another vote for less screen time.
“By itself, standard self-measured blood pressure (SMBP) has minimal effect on BP control,” wrote lead author Mark J. Pletcher, MD, of the University of California, San Francisco, and colleagues in JAMA Internal Medicine. “To improve BP control, SMBP must be accompanied by patient feedback, counseling, or other cointerventions, and the BP-lowering effects of SMBP appear to be proportional to the intensity of the cointervention.”
While this is known, higher-intensity cointerventions demand both money and time, prompting development of new devices that link with smartphone apps, they continued.
In the prospective randomized trial, patients with hypertension were randomly assigned to self-measure their blood pressure using a standard device that paired with a connected smartphone application or to self-measure their blood pressure with a standard device alone. Both groups achieved about an 11 mm Hg reduction in systolic BP over 6 months, reported similar levels of satisfaction with the monitoring process, and shared their readings with their physicians with similar frequency.
Methods
Dr. Pletcher and colleagues enrolled 2,101 adults who self-reported a systolic BP greater than 145 mm Hg and expressed a commitment to reduce their BP by at least 10 points in their trial. The participants, who were generally middle-aged or older, were randomized in a 1:1 ratio to monitor their BP using standard SMBP or “enhanced” SMBP. The standard group used the OMRON BP monitor alone, while the enhanced group used the same BP monitor coupled with the OMRON Connect smartphone app.
After 6 months of follow-up for each patient, mean BP reduction from baseline in the standard group was 10.6 mm Hg, compared with 10.7 mm Hg in the enhanced group, a nonsignificant difference (P = .81). While slightly more patients in the enhanced group achieved a BP lower than 140/90 mm Hg (32% vs. 29%; odds ratio, 1.17; 95% confidence interval, 1.01-1.34), this trend did not extend below the 130/80 mm Hg threshold.
Other secondary outcomes were also similar between groups. For example, 70% of participants in the enhanced group said they would recommend their SMBP process to a friend, compared with 69% of participants who followed the standard monitoring approach. The smartphone app had little impact on sharing readings with physicians, either, based on a 44% share rate in the enhanced group versus 48% in the standard group (P = .22).
“Enhanced SMBP does not provide any additional reduction in BP,” the investigators concluded.
New devices that link with smartphone apps, like the one used in this trial, “transmit BP measurements via wireless connection to the patient’s smartphone, where they are processed in a smartphone application to support tracking, visualization, interpretation, reminders to measure BP and/or take medications; recommendations for lifestyle interventions, medication adherence, or to discuss their BP with their clinician; and communications (for example, emailing a summary to a family member or clinician),” the researchers explained. While these devices are “only slightly more expensive than standard SMBP devices,” their relative efficacy over standard SMBP is “unclear.”
Findings can likely be extrapolated to other apps
Although the trial evaluated just one smartphone app, Dr. Pletcher suggested that the findings can likely be extrapolated to other apps.
“Most basic BP-tracking apps have some version or subset of the same essential functionality,” he said, in an interview. “My guess is that apps that meet this description without some substantially different technology or feature would likely show the same basic results as we did.”
Making a similar remark, Matthew Jung, MD, of Keck Medicine of USC, Los Angeles, stated that the findings can be “reasonably extrapolated” to other BP-tracking apps with similar functionality “if we put aside the study’s issues with power.”
When it comes to smartphone apps, active engagement is needed to achieve greater impacts on blood pressure, Dr. Pletcher said, but “there is so much competition for people’s attention on their phone that it is hard to maintain active engagement with any health-related app for long.”
Still, Dr. Pletcher hasn’t given up on biometric apps, noting that “with the right technology and connectivity and user experience (for both patient and clinician), they still could be game-changing for managing chronic conditions like hypertension.”
To this end, he and his colleagues are exploring technologies to passively monitor health-related measurements like BP, potentially sidestepping the pitfall of active engagement.
Dr. Jung said the study is noteworthy for several reasons, including its large size, similar level of comfort with technology reported by both groups, and representation of Black and Hispanic participants, who accounted for almost one-third of the population.
Study limitations
Dr. Jung pointed out several study limitations, including the lack of standardized measurement of BP, which left more than one-third of patients unevaluated via chart review, as well as gaps in usage data, such as that one-third of the participants never confirmed receipt of a device, and less than half of the enhanced group reported using the smartphone application.
These limitations “may have detracted from its ability to identify the true efficacy of an enhanced app-based BP tracking device,” he said. “In contrast, each of these issues also helped us get a better picture for how well these devices may work in the real world.”
Dr. Jung also commented on the duration of the study, noting that only 10 weeks passed, on average, from baseline to follow-up BP measurement, which “may not have been sufficient for a possible difference between enhanced and standard BP monitoring to become noticeable.”
“This may be especially important when taking into consideration the time required to mail the devices out to patients, for patients to become familiar with usage of the devices, and for them to start using the devices in a meaningful way,” he added.
The study was supported the Patient-Centered Outcomes Research Institute, the American Medical Association, and the American Heart Association. The investigators disclosed additional relationships with Pfizer, Bristol Myers Squibb, and Novartis. Dr. Jung, who was not involved in the study, disclosed no relevant conflicts of interest.
Here’s another vote for less screen time.
“By itself, standard self-measured blood pressure (SMBP) has minimal effect on BP control,” wrote lead author Mark J. Pletcher, MD, of the University of California, San Francisco, and colleagues in JAMA Internal Medicine. “To improve BP control, SMBP must be accompanied by patient feedback, counseling, or other cointerventions, and the BP-lowering effects of SMBP appear to be proportional to the intensity of the cointervention.”
While this is known, higher-intensity cointerventions demand both money and time, prompting development of new devices that link with smartphone apps, they continued.
In the prospective randomized trial, patients with hypertension were randomly assigned to self-measure their blood pressure using a standard device that paired with a connected smartphone application or to self-measure their blood pressure with a standard device alone. Both groups achieved about an 11 mm Hg reduction in systolic BP over 6 months, reported similar levels of satisfaction with the monitoring process, and shared their readings with their physicians with similar frequency.
Methods
Dr. Pletcher and colleagues enrolled 2,101 adults who self-reported a systolic BP greater than 145 mm Hg and expressed a commitment to reduce their BP by at least 10 points in their trial. The participants, who were generally middle-aged or older, were randomized in a 1:1 ratio to monitor their BP using standard SMBP or “enhanced” SMBP. The standard group used the OMRON BP monitor alone, while the enhanced group used the same BP monitor coupled with the OMRON Connect smartphone app.
After 6 months of follow-up for each patient, mean BP reduction from baseline in the standard group was 10.6 mm Hg, compared with 10.7 mm Hg in the enhanced group, a nonsignificant difference (P = .81). While slightly more patients in the enhanced group achieved a BP lower than 140/90 mm Hg (32% vs. 29%; odds ratio, 1.17; 95% confidence interval, 1.01-1.34), this trend did not extend below the 130/80 mm Hg threshold.
Other secondary outcomes were also similar between groups. For example, 70% of participants in the enhanced group said they would recommend their SMBP process to a friend, compared with 69% of participants who followed the standard monitoring approach. The smartphone app had little impact on sharing readings with physicians, either, based on a 44% share rate in the enhanced group versus 48% in the standard group (P = .22).
“Enhanced SMBP does not provide any additional reduction in BP,” the investigators concluded.
New devices that link with smartphone apps, like the one used in this trial, “transmit BP measurements via wireless connection to the patient’s smartphone, where they are processed in a smartphone application to support tracking, visualization, interpretation, reminders to measure BP and/or take medications; recommendations for lifestyle interventions, medication adherence, or to discuss their BP with their clinician; and communications (for example, emailing a summary to a family member or clinician),” the researchers explained. While these devices are “only slightly more expensive than standard SMBP devices,” their relative efficacy over standard SMBP is “unclear.”
Findings can likely be extrapolated to other apps
Although the trial evaluated just one smartphone app, Dr. Pletcher suggested that the findings can likely be extrapolated to other apps.
“Most basic BP-tracking apps have some version or subset of the same essential functionality,” he said, in an interview. “My guess is that apps that meet this description without some substantially different technology or feature would likely show the same basic results as we did.”
Making a similar remark, Matthew Jung, MD, of Keck Medicine of USC, Los Angeles, stated that the findings can be “reasonably extrapolated” to other BP-tracking apps with similar functionality “if we put aside the study’s issues with power.”
When it comes to smartphone apps, active engagement is needed to achieve greater impacts on blood pressure, Dr. Pletcher said, but “there is so much competition for people’s attention on their phone that it is hard to maintain active engagement with any health-related app for long.”
Still, Dr. Pletcher hasn’t given up on biometric apps, noting that “with the right technology and connectivity and user experience (for both patient and clinician), they still could be game-changing for managing chronic conditions like hypertension.”
To this end, he and his colleagues are exploring technologies to passively monitor health-related measurements like BP, potentially sidestepping the pitfall of active engagement.
Dr. Jung said the study is noteworthy for several reasons, including its large size, similar level of comfort with technology reported by both groups, and representation of Black and Hispanic participants, who accounted for almost one-third of the population.
Study limitations
Dr. Jung pointed out several study limitations, including the lack of standardized measurement of BP, which left more than one-third of patients unevaluated via chart review, as well as gaps in usage data, such as that one-third of the participants never confirmed receipt of a device, and less than half of the enhanced group reported using the smartphone application.
These limitations “may have detracted from its ability to identify the true efficacy of an enhanced app-based BP tracking device,” he said. “In contrast, each of these issues also helped us get a better picture for how well these devices may work in the real world.”
Dr. Jung also commented on the duration of the study, noting that only 10 weeks passed, on average, from baseline to follow-up BP measurement, which “may not have been sufficient for a possible difference between enhanced and standard BP monitoring to become noticeable.”
“This may be especially important when taking into consideration the time required to mail the devices out to patients, for patients to become familiar with usage of the devices, and for them to start using the devices in a meaningful way,” he added.
The study was supported the Patient-Centered Outcomes Research Institute, the American Medical Association, and the American Heart Association. The investigators disclosed additional relationships with Pfizer, Bristol Myers Squibb, and Novartis. Dr. Jung, who was not involved in the study, disclosed no relevant conflicts of interest.
FROM JAMA INTERNAL MEDICINE













