User login
Early age at first period raises type 2 diabetes risk
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Reducing albumin improves kidney and heart function in people with type 2 diabetes
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.
Evaluating Pharmacists’ Time Collecting Self-Monitoring Blood Glucose Data
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
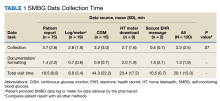
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
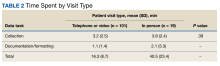
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
What is the dark side of GLP-1 receptor agonists?
The approval of the GLP-1 receptor agonist semaglutide for weight regulation in January 2023 ushered in a new era of obesity therapy. In recent months, however,
“When millions of people are treated with medications like semaglutide, even relatively rare side effects occur in a large number of individuals,” Susan Yanovski, MD, codirector of the Office of Obesity Research at the National Institute of Diabetes and Digestive and Kidney Diseases in Bethesda, Maryland, said in a JAMA news report.
Despite the low incidence of these adverse events and the likelihood that the benefits outweigh these risks in individuals with severe obesity, doctors and patients should be aware of these serious side effects, she added.
GLP-1 receptor agonists like semaglutide or liraglutide mimic certain intestinal hormones. Almost all their characteristic side effects involve the gastrointestinal tract: nausea, vomiting, constipation, and diarrhea. However, these are not the rare, severe side effects that are gaining increasing attention.
Severe Gastric Problems
A recent analysis published in JAMA shows that GLP-1 receptor agonists are associated with a ninefold higher risk of pancreatitis, compared with bupropion, an older weight-loss medication. Patients receiving GLP-1 receptor agonists also had four times more frequent intestinal obstruction and more than three times more frequent gastroparesis. The absolute risks for these complications, however, were less than 1% per year of use.
There were no indications of an increased risk for gallbladder diseases. Acute pancreatitis and acute gallbladder diseases are known complications of GLP-1 receptor agonists.
These results “reinforce that these are effective medications, and all medications have side effects,” said Dr. Yanovski. She emphasized that despite a significant increase in relative risk, however, the absolute risk remains very low.
Anesthetic Complications
In the spring of 2023, reports of patients taking GLP-1 receptor agonists and vomiting or aspirating food during anesthesia surfaced in some scientific journals. It was particularly noticeable that some of these patients vomited unusually large amounts of stomach contents, even though they had not eaten anything, as directed by the doctor before the operation.
Experts believe that the slowed gastric emptying intentionally caused by GLP-1 receptor agonists could be responsible for these problems.
The American Society of Anesthesiologists now recommends that patients do not take GLP-1 receptor agonists on the day of surgery and discontinue weekly administered agents like Wegovy 7 days before the procedure.
Increased Suicidality Risk?
In July, case reports of depression and suicidal ideation led the European Medicines Agency to investigate about 150 cases of potential self-harm and suicidal thoughts in patients who had received liraglutide or semaglutide. The review now also includes other GLP-1 receptor agonists. Results of the review process are expected in December.
Dr. Yanovski noted that it is unclear whether these incidents are caused by the drugs, but suicidal thoughts and suicidal behavior have also been observed with other medications for obesity treatment (eg, rimonabant). “It is certainly a good idea to use these medications cautiously in patients with a history of suicidality and monitor the patients accordingly,” she said.
Long-Term Safety
GLP-1 receptor agonists likely need to be used long term, potentially for life, for the effects on body weight to persist. Whether there are side effects and complications that only become apparent over time is currently unknown — especially when these medications are used for weight reduction.
Studies in rodents have suggested an increased risk of medullary thyroid carcinomas. Whether a similar signal exists in humans may only become apparent in many years. In patients who have had medullary thyroid carcinoma themselves or in the family, dulaglutide, liraglutide, semaglutide, and tirzepatide, a dual GLP-1/GIP receptor agonist, are contraindicated.
With dual agonists like tirzepatide or even triple agonists like retatrutide (GLP-1/GIP/glucagon), patients can lose significantly more weight than with the monoagonist semaglutide. Gastrointestinal events were also frequent in studies of dual agonists.
Awaiting Guideline Updates
Guidelines for using these new medications are still scarce. “There are clinical guidelines for obesity therapy, but they were all written before the GLP-1 receptor agonists came on the market,” said Dr. Yanovski. “Medical societies are currently working intensively to develop new guidelines to help doctors use these medications safely and effectively in clinical practice.”
This article was translated from the Medscape German edition. A version of this article appeared on Medscape.com.
The approval of the GLP-1 receptor agonist semaglutide for weight regulation in January 2023 ushered in a new era of obesity therapy. In recent months, however,
“When millions of people are treated with medications like semaglutide, even relatively rare side effects occur in a large number of individuals,” Susan Yanovski, MD, codirector of the Office of Obesity Research at the National Institute of Diabetes and Digestive and Kidney Diseases in Bethesda, Maryland, said in a JAMA news report.
Despite the low incidence of these adverse events and the likelihood that the benefits outweigh these risks in individuals with severe obesity, doctors and patients should be aware of these serious side effects, she added.
GLP-1 receptor agonists like semaglutide or liraglutide mimic certain intestinal hormones. Almost all their characteristic side effects involve the gastrointestinal tract: nausea, vomiting, constipation, and diarrhea. However, these are not the rare, severe side effects that are gaining increasing attention.
Severe Gastric Problems
A recent analysis published in JAMA shows that GLP-1 receptor agonists are associated with a ninefold higher risk of pancreatitis, compared with bupropion, an older weight-loss medication. Patients receiving GLP-1 receptor agonists also had four times more frequent intestinal obstruction and more than three times more frequent gastroparesis. The absolute risks for these complications, however, were less than 1% per year of use.
There were no indications of an increased risk for gallbladder diseases. Acute pancreatitis and acute gallbladder diseases are known complications of GLP-1 receptor agonists.
These results “reinforce that these are effective medications, and all medications have side effects,” said Dr. Yanovski. She emphasized that despite a significant increase in relative risk, however, the absolute risk remains very low.
Anesthetic Complications
In the spring of 2023, reports of patients taking GLP-1 receptor agonists and vomiting or aspirating food during anesthesia surfaced in some scientific journals. It was particularly noticeable that some of these patients vomited unusually large amounts of stomach contents, even though they had not eaten anything, as directed by the doctor before the operation.
Experts believe that the slowed gastric emptying intentionally caused by GLP-1 receptor agonists could be responsible for these problems.
The American Society of Anesthesiologists now recommends that patients do not take GLP-1 receptor agonists on the day of surgery and discontinue weekly administered agents like Wegovy 7 days before the procedure.
Increased Suicidality Risk?
In July, case reports of depression and suicidal ideation led the European Medicines Agency to investigate about 150 cases of potential self-harm and suicidal thoughts in patients who had received liraglutide or semaglutide. The review now also includes other GLP-1 receptor agonists. Results of the review process are expected in December.
Dr. Yanovski noted that it is unclear whether these incidents are caused by the drugs, but suicidal thoughts and suicidal behavior have also been observed with other medications for obesity treatment (eg, rimonabant). “It is certainly a good idea to use these medications cautiously in patients with a history of suicidality and monitor the patients accordingly,” she said.
Long-Term Safety
GLP-1 receptor agonists likely need to be used long term, potentially for life, for the effects on body weight to persist. Whether there are side effects and complications that only become apparent over time is currently unknown — especially when these medications are used for weight reduction.
Studies in rodents have suggested an increased risk of medullary thyroid carcinomas. Whether a similar signal exists in humans may only become apparent in many years. In patients who have had medullary thyroid carcinoma themselves or in the family, dulaglutide, liraglutide, semaglutide, and tirzepatide, a dual GLP-1/GIP receptor agonist, are contraindicated.
With dual agonists like tirzepatide or even triple agonists like retatrutide (GLP-1/GIP/glucagon), patients can lose significantly more weight than with the monoagonist semaglutide. Gastrointestinal events were also frequent in studies of dual agonists.
Awaiting Guideline Updates
Guidelines for using these new medications are still scarce. “There are clinical guidelines for obesity therapy, but they were all written before the GLP-1 receptor agonists came on the market,” said Dr. Yanovski. “Medical societies are currently working intensively to develop new guidelines to help doctors use these medications safely and effectively in clinical practice.”
This article was translated from the Medscape German edition. A version of this article appeared on Medscape.com.
The approval of the GLP-1 receptor agonist semaglutide for weight regulation in January 2023 ushered in a new era of obesity therapy. In recent months, however,
“When millions of people are treated with medications like semaglutide, even relatively rare side effects occur in a large number of individuals,” Susan Yanovski, MD, codirector of the Office of Obesity Research at the National Institute of Diabetes and Digestive and Kidney Diseases in Bethesda, Maryland, said in a JAMA news report.
Despite the low incidence of these adverse events and the likelihood that the benefits outweigh these risks in individuals with severe obesity, doctors and patients should be aware of these serious side effects, she added.
GLP-1 receptor agonists like semaglutide or liraglutide mimic certain intestinal hormones. Almost all their characteristic side effects involve the gastrointestinal tract: nausea, vomiting, constipation, and diarrhea. However, these are not the rare, severe side effects that are gaining increasing attention.
Severe Gastric Problems
A recent analysis published in JAMA shows that GLP-1 receptor agonists are associated with a ninefold higher risk of pancreatitis, compared with bupropion, an older weight-loss medication. Patients receiving GLP-1 receptor agonists also had four times more frequent intestinal obstruction and more than three times more frequent gastroparesis. The absolute risks for these complications, however, were less than 1% per year of use.
There were no indications of an increased risk for gallbladder diseases. Acute pancreatitis and acute gallbladder diseases are known complications of GLP-1 receptor agonists.
These results “reinforce that these are effective medications, and all medications have side effects,” said Dr. Yanovski. She emphasized that despite a significant increase in relative risk, however, the absolute risk remains very low.
Anesthetic Complications
In the spring of 2023, reports of patients taking GLP-1 receptor agonists and vomiting or aspirating food during anesthesia surfaced in some scientific journals. It was particularly noticeable that some of these patients vomited unusually large amounts of stomach contents, even though they had not eaten anything, as directed by the doctor before the operation.
Experts believe that the slowed gastric emptying intentionally caused by GLP-1 receptor agonists could be responsible for these problems.
The American Society of Anesthesiologists now recommends that patients do not take GLP-1 receptor agonists on the day of surgery and discontinue weekly administered agents like Wegovy 7 days before the procedure.
Increased Suicidality Risk?
In July, case reports of depression and suicidal ideation led the European Medicines Agency to investigate about 150 cases of potential self-harm and suicidal thoughts in patients who had received liraglutide or semaglutide. The review now also includes other GLP-1 receptor agonists. Results of the review process are expected in December.
Dr. Yanovski noted that it is unclear whether these incidents are caused by the drugs, but suicidal thoughts and suicidal behavior have also been observed with other medications for obesity treatment (eg, rimonabant). “It is certainly a good idea to use these medications cautiously in patients with a history of suicidality and monitor the patients accordingly,” she said.
Long-Term Safety
GLP-1 receptor agonists likely need to be used long term, potentially for life, for the effects on body weight to persist. Whether there are side effects and complications that only become apparent over time is currently unknown — especially when these medications are used for weight reduction.
Studies in rodents have suggested an increased risk of medullary thyroid carcinomas. Whether a similar signal exists in humans may only become apparent in many years. In patients who have had medullary thyroid carcinoma themselves or in the family, dulaglutide, liraglutide, semaglutide, and tirzepatide, a dual GLP-1/GIP receptor agonist, are contraindicated.
With dual agonists like tirzepatide or even triple agonists like retatrutide (GLP-1/GIP/glucagon), patients can lose significantly more weight than with the monoagonist semaglutide. Gastrointestinal events were also frequent in studies of dual agonists.
Awaiting Guideline Updates
Guidelines for using these new medications are still scarce. “There are clinical guidelines for obesity therapy, but they were all written before the GLP-1 receptor agonists came on the market,” said Dr. Yanovski. “Medical societies are currently working intensively to develop new guidelines to help doctors use these medications safely and effectively in clinical practice.”
This article was translated from the Medscape German edition. A version of this article appeared on Medscape.com.
FROM JAMA
Insufficient sleep impairs women’s insulin sensitivity
Women, particularly those who are postmenopausal, who sleep less than the recommended 7 hours per night may have impaired insulin sensitivity regardless of their degree of adiposity, a randomized crossover trial reveals.
The research was published recently in Diabetes Care.
Nearly 40 women were randomly assigned to either restricted sleep or adequate sleep for 6 weeks, then crossed over to the other sleep condition. During sleep restriction, women slept an average of 6.2 hours per night versus 7-9 hours per night.
Both fasting insulin levels and insulin resistance were significantly increased during sleep restriction, with the effect on insulin resistance particularly notable in postmenopausal women. This was independent of adiposity and changes in adiposity.
“What we’re seeing is that more insulin is needed to normalize glucose levels in the women under conditions of sleep restriction,” said senior author Marie-Pierre St-Onge, PhD, director of the Center of Excellence for Sleep and Circadian Research at Columbia University Vagelos College of Physicians and Surgeons, New York, in a release.
“Even then, the insulin may not have been doing enough to counteract rising blood glucose levels of postmenopausal women,” she stated.
Prolonged lack of sleep may accelerate diabetes progression
Dr. St-Onge added,
Dr. St-Onge said in an interview that it was crucial to show the impact of sleep restriction in a randomized study, because “observational studies don’t provide information on causality.”
The study did not rely on people “living in our clinical research facility,” but instead enrolled individuals who were “living their lives,” and the reduction in sleep achieved was “similar to what is seen in the general population with sleep,” she said.
Dr. St-Onge therefore believes the findings indicate that sleep has been overlooked as a contributory factor in insulin sensitivity.
Robert Gabbay, MD, PhD, chief scientific and medical officer at the American Diabetes Association, said in an interview that this is an “important study [that] builds on what we have seen on the importance of sleep for metabolic outcomes and diabetes.”
He continued, “There have been several studies showing the association of sleep and diabetes, but that does not necessarily mean cause and effect.”
On the other hand, Dr. Gabbay said, “randomizing people can help see sleep influences on key metabolic measures of diabetes, [which] helps to build a stronger case that sleep disturbances can cause worsening metabolic health.”
He emphasized that both the quantity and quality of sleep are “critical for optimal diabetes health” and highlighted that the ADA’s Standards of Care “recommends screening for sleep issues and counseling to improve sleep.”
“This study provides new insight into the health effects of even small sleep deficits in women across all stages of adulthood and racial and ethnic backgrounds,” commented Corinne Silva, PhD, program director in the Division of Diabetes, Endocrinology, and Metabolic Diseases at the National Institute of Diabetes and Digestive and Kidney Diseases, which co-funded the study.
The authors note that more than one-third of adults sleep less than the recommended 7 hours per night, which is “concerning given robust associations of short sleep with cardiometabolic diseases.”
Moreover, “women report poorer sleep than men,” explained Marishka Brown, PhD, director of the National Center on Sleep Disorders Research at the National Heart, Lung, and Blood Institute, which also co-funded the study.
“So understanding how sleep disturbances impact their health across the lifespan is critical, especially for postmenopausal women,” she said, particularly because previous studies have not reflected real-world sleep patterns or have focused on men.
The researchers conducted a trial to evaluate the causal impact of prolonged, mild sleep restriction on cardiometabolic risk factors in women as part of the American Heart Association Go Red for Women Strategically Focused Research Network.
They recruited metabolically healthy women aged 20-75 years who were at increased risk for cardiometabolic disease due to having either overweight or class I obesity or at least one parent with type 2 diabetes, hyperlipidemia, or cardiovascular disease.
They were also required to have a habitual total sleep time on actigraphy of 7-9 hours per night and low risk for sleep apnea. Exclusion criteria included excessive caffeine intake, a significantly advanced or delayed sleep phase, shift work, and travel across time zones.
The participants were randomly assigned to either adequate sleep, defined as 7-9 hours per night, or sleep restriction, defined as a reduction in sleep duration of 1.5 hours per night, for 6 weeks. They were then crossed over to the other sleep condition.
Assessments, including MRI and oral glucose tolerance tests, were performed at baseline and at the end of each study phase.
The researchers report on 38 women who took part in the trial, of whom 11 were postmenopausal. The mean age was 37.6 years; 31.6% self-identified as Black and 26.3% as Hispanic. The mean body mass index (BMI) was 25.5.
Postmenopausal women had a higher mean age than other women, at 56.1 years versus 30.1 years, and a higher baseline fasting blood glucose, at 5.26 mmol/L (94.68 mg/dL) versus 4.70 mmol/L (84.6 mg/dL).
The team reported that compliance with the sleep protocol was “excellent,” with women during sleep restriction having a reduction in total sleep time of 1.34 hours per night versus women in the adequate sleep arm (P < .0001).
Sleep restriction was also associated with significant increases in fasting plasma insulin versus adequate sleep, at a beta value of 0.68 pmol/L (P = .016), and significantly increased Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) values (beta = 0.30; P = .016).
The impact on HOMA-IR values was significantly more pronounced in postmenopausal than menopausal women, at beta values of 0.45 versus 0.27 (P for interaction = .042).
Sleep restriction had no significant effect on fasting plasma glucose levels, and the association between sleep duration and cardiometabolic parameters was not modified by the proportion of either total or visceral adipose tissue, or by changes in adiposity.
This clinical trial was supported by the American Heart Association, a National Institutes of Health Clinical and Translational Science Award to Columbia University, and N.Y. Nutrition Obesity Research Center. Individual authors received support from the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. No relevant financial relationships were declared.
A version of this article appeared on Medscape.com.
Women, particularly those who are postmenopausal, who sleep less than the recommended 7 hours per night may have impaired insulin sensitivity regardless of their degree of adiposity, a randomized crossover trial reveals.
The research was published recently in Diabetes Care.
Nearly 40 women were randomly assigned to either restricted sleep or adequate sleep for 6 weeks, then crossed over to the other sleep condition. During sleep restriction, women slept an average of 6.2 hours per night versus 7-9 hours per night.
Both fasting insulin levels and insulin resistance were significantly increased during sleep restriction, with the effect on insulin resistance particularly notable in postmenopausal women. This was independent of adiposity and changes in adiposity.
“What we’re seeing is that more insulin is needed to normalize glucose levels in the women under conditions of sleep restriction,” said senior author Marie-Pierre St-Onge, PhD, director of the Center of Excellence for Sleep and Circadian Research at Columbia University Vagelos College of Physicians and Surgeons, New York, in a release.
“Even then, the insulin may not have been doing enough to counteract rising blood glucose levels of postmenopausal women,” she stated.
Prolonged lack of sleep may accelerate diabetes progression
Dr. St-Onge added,
Dr. St-Onge said in an interview that it was crucial to show the impact of sleep restriction in a randomized study, because “observational studies don’t provide information on causality.”
The study did not rely on people “living in our clinical research facility,” but instead enrolled individuals who were “living their lives,” and the reduction in sleep achieved was “similar to what is seen in the general population with sleep,” she said.
Dr. St-Onge therefore believes the findings indicate that sleep has been overlooked as a contributory factor in insulin sensitivity.
Robert Gabbay, MD, PhD, chief scientific and medical officer at the American Diabetes Association, said in an interview that this is an “important study [that] builds on what we have seen on the importance of sleep for metabolic outcomes and diabetes.”
He continued, “There have been several studies showing the association of sleep and diabetes, but that does not necessarily mean cause and effect.”
On the other hand, Dr. Gabbay said, “randomizing people can help see sleep influences on key metabolic measures of diabetes, [which] helps to build a stronger case that sleep disturbances can cause worsening metabolic health.”
He emphasized that both the quantity and quality of sleep are “critical for optimal diabetes health” and highlighted that the ADA’s Standards of Care “recommends screening for sleep issues and counseling to improve sleep.”
“This study provides new insight into the health effects of even small sleep deficits in women across all stages of adulthood and racial and ethnic backgrounds,” commented Corinne Silva, PhD, program director in the Division of Diabetes, Endocrinology, and Metabolic Diseases at the National Institute of Diabetes and Digestive and Kidney Diseases, which co-funded the study.
The authors note that more than one-third of adults sleep less than the recommended 7 hours per night, which is “concerning given robust associations of short sleep with cardiometabolic diseases.”
Moreover, “women report poorer sleep than men,” explained Marishka Brown, PhD, director of the National Center on Sleep Disorders Research at the National Heart, Lung, and Blood Institute, which also co-funded the study.
“So understanding how sleep disturbances impact their health across the lifespan is critical, especially for postmenopausal women,” she said, particularly because previous studies have not reflected real-world sleep patterns or have focused on men.
The researchers conducted a trial to evaluate the causal impact of prolonged, mild sleep restriction on cardiometabolic risk factors in women as part of the American Heart Association Go Red for Women Strategically Focused Research Network.
They recruited metabolically healthy women aged 20-75 years who were at increased risk for cardiometabolic disease due to having either overweight or class I obesity or at least one parent with type 2 diabetes, hyperlipidemia, or cardiovascular disease.
They were also required to have a habitual total sleep time on actigraphy of 7-9 hours per night and low risk for sleep apnea. Exclusion criteria included excessive caffeine intake, a significantly advanced or delayed sleep phase, shift work, and travel across time zones.
The participants were randomly assigned to either adequate sleep, defined as 7-9 hours per night, or sleep restriction, defined as a reduction in sleep duration of 1.5 hours per night, for 6 weeks. They were then crossed over to the other sleep condition.
Assessments, including MRI and oral glucose tolerance tests, were performed at baseline and at the end of each study phase.
The researchers report on 38 women who took part in the trial, of whom 11 were postmenopausal. The mean age was 37.6 years; 31.6% self-identified as Black and 26.3% as Hispanic. The mean body mass index (BMI) was 25.5.
Postmenopausal women had a higher mean age than other women, at 56.1 years versus 30.1 years, and a higher baseline fasting blood glucose, at 5.26 mmol/L (94.68 mg/dL) versus 4.70 mmol/L (84.6 mg/dL).
The team reported that compliance with the sleep protocol was “excellent,” with women during sleep restriction having a reduction in total sleep time of 1.34 hours per night versus women in the adequate sleep arm (P < .0001).
Sleep restriction was also associated with significant increases in fasting plasma insulin versus adequate sleep, at a beta value of 0.68 pmol/L (P = .016), and significantly increased Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) values (beta = 0.30; P = .016).
The impact on HOMA-IR values was significantly more pronounced in postmenopausal than menopausal women, at beta values of 0.45 versus 0.27 (P for interaction = .042).
Sleep restriction had no significant effect on fasting plasma glucose levels, and the association between sleep duration and cardiometabolic parameters was not modified by the proportion of either total or visceral adipose tissue, or by changes in adiposity.
This clinical trial was supported by the American Heart Association, a National Institutes of Health Clinical and Translational Science Award to Columbia University, and N.Y. Nutrition Obesity Research Center. Individual authors received support from the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. No relevant financial relationships were declared.
A version of this article appeared on Medscape.com.
Women, particularly those who are postmenopausal, who sleep less than the recommended 7 hours per night may have impaired insulin sensitivity regardless of their degree of adiposity, a randomized crossover trial reveals.
The research was published recently in Diabetes Care.
Nearly 40 women were randomly assigned to either restricted sleep or adequate sleep for 6 weeks, then crossed over to the other sleep condition. During sleep restriction, women slept an average of 6.2 hours per night versus 7-9 hours per night.
Both fasting insulin levels and insulin resistance were significantly increased during sleep restriction, with the effect on insulin resistance particularly notable in postmenopausal women. This was independent of adiposity and changes in adiposity.
“What we’re seeing is that more insulin is needed to normalize glucose levels in the women under conditions of sleep restriction,” said senior author Marie-Pierre St-Onge, PhD, director of the Center of Excellence for Sleep and Circadian Research at Columbia University Vagelos College of Physicians and Surgeons, New York, in a release.
“Even then, the insulin may not have been doing enough to counteract rising blood glucose levels of postmenopausal women,” she stated.
Prolonged lack of sleep may accelerate diabetes progression
Dr. St-Onge added,
Dr. St-Onge said in an interview that it was crucial to show the impact of sleep restriction in a randomized study, because “observational studies don’t provide information on causality.”
The study did not rely on people “living in our clinical research facility,” but instead enrolled individuals who were “living their lives,” and the reduction in sleep achieved was “similar to what is seen in the general population with sleep,” she said.
Dr. St-Onge therefore believes the findings indicate that sleep has been overlooked as a contributory factor in insulin sensitivity.
Robert Gabbay, MD, PhD, chief scientific and medical officer at the American Diabetes Association, said in an interview that this is an “important study [that] builds on what we have seen on the importance of sleep for metabolic outcomes and diabetes.”
He continued, “There have been several studies showing the association of sleep and diabetes, but that does not necessarily mean cause and effect.”
On the other hand, Dr. Gabbay said, “randomizing people can help see sleep influences on key metabolic measures of diabetes, [which] helps to build a stronger case that sleep disturbances can cause worsening metabolic health.”
He emphasized that both the quantity and quality of sleep are “critical for optimal diabetes health” and highlighted that the ADA’s Standards of Care “recommends screening for sleep issues and counseling to improve sleep.”
“This study provides new insight into the health effects of even small sleep deficits in women across all stages of adulthood and racial and ethnic backgrounds,” commented Corinne Silva, PhD, program director in the Division of Diabetes, Endocrinology, and Metabolic Diseases at the National Institute of Diabetes and Digestive and Kidney Diseases, which co-funded the study.
The authors note that more than one-third of adults sleep less than the recommended 7 hours per night, which is “concerning given robust associations of short sleep with cardiometabolic diseases.”
Moreover, “women report poorer sleep than men,” explained Marishka Brown, PhD, director of the National Center on Sleep Disorders Research at the National Heart, Lung, and Blood Institute, which also co-funded the study.
“So understanding how sleep disturbances impact their health across the lifespan is critical, especially for postmenopausal women,” she said, particularly because previous studies have not reflected real-world sleep patterns or have focused on men.
The researchers conducted a trial to evaluate the causal impact of prolonged, mild sleep restriction on cardiometabolic risk factors in women as part of the American Heart Association Go Red for Women Strategically Focused Research Network.
They recruited metabolically healthy women aged 20-75 years who were at increased risk for cardiometabolic disease due to having either overweight or class I obesity or at least one parent with type 2 diabetes, hyperlipidemia, or cardiovascular disease.
They were also required to have a habitual total sleep time on actigraphy of 7-9 hours per night and low risk for sleep apnea. Exclusion criteria included excessive caffeine intake, a significantly advanced or delayed sleep phase, shift work, and travel across time zones.
The participants were randomly assigned to either adequate sleep, defined as 7-9 hours per night, or sleep restriction, defined as a reduction in sleep duration of 1.5 hours per night, for 6 weeks. They were then crossed over to the other sleep condition.
Assessments, including MRI and oral glucose tolerance tests, were performed at baseline and at the end of each study phase.
The researchers report on 38 women who took part in the trial, of whom 11 were postmenopausal. The mean age was 37.6 years; 31.6% self-identified as Black and 26.3% as Hispanic. The mean body mass index (BMI) was 25.5.
Postmenopausal women had a higher mean age than other women, at 56.1 years versus 30.1 years, and a higher baseline fasting blood glucose, at 5.26 mmol/L (94.68 mg/dL) versus 4.70 mmol/L (84.6 mg/dL).
The team reported that compliance with the sleep protocol was “excellent,” with women during sleep restriction having a reduction in total sleep time of 1.34 hours per night versus women in the adequate sleep arm (P < .0001).
Sleep restriction was also associated with significant increases in fasting plasma insulin versus adequate sleep, at a beta value of 0.68 pmol/L (P = .016), and significantly increased Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) values (beta = 0.30; P = .016).
The impact on HOMA-IR values was significantly more pronounced in postmenopausal than menopausal women, at beta values of 0.45 versus 0.27 (P for interaction = .042).
Sleep restriction had no significant effect on fasting plasma glucose levels, and the association between sleep duration and cardiometabolic parameters was not modified by the proportion of either total or visceral adipose tissue, or by changes in adiposity.
This clinical trial was supported by the American Heart Association, a National Institutes of Health Clinical and Translational Science Award to Columbia University, and N.Y. Nutrition Obesity Research Center. Individual authors received support from the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. No relevant financial relationships were declared.
A version of this article appeared on Medscape.com.
FROM DIABETES CARE
Bariatric surgery still best option for some with obesity
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Study confirms link between red meat and diabetes risk
This association was confirmed by a new study published in the American Journal of Clinical Nutrition, a data analysis of nearly 217,000 people who were monitored for three decades as part of several cohort studies. “Our study supports the current dietary recommendations of limiting consumption of red meat and highlights the importance of different alternative sources of protein in preventing type 2 diabetes,” the researchers wrote.
Consumption and risk
The study included men and women who took part in the Nurses’ Health Study, the Nurses’ Health Study II, or the Health Professionals Follow-up Study. Questionnaires were used to collect data every 2-4 years on the frequency of specific food consumption. Information on the onset of diseases and on different health-related aspects was collected every 2 years.
Those who consumed more red meat had a higher body mass index, higher total energy intake, and greater likelihood of being a smoker. They were physically less active and less likely to take multivitamins. In a follow-up of 5.48 million person-years, 22,761 cases of type 2 diabetes were recorded.
The link between consumption of processed and unprocessed red meat (and both combined) and a higher risk of diabetes was observed in all cohorts when analyzed separately and jointly. The people in the highest quintile for combined red meat consumption had a 2% greater risk of developing the disease, compared with those in the lowest quintile. The risk increases associated with processed and unprocessed meat were 51% and 40%, respectively. One additional serving per day of processed red meat was associated with a 1.46-fold greater risk of diabetes. This risk was 1.24 times greater for unprocessed meat and 1.28 times greater for both types combined.
The associations had a linear dose-response relationship and remained firm even after accounting for BMI, which the researchers stressed could be a mediating factor. Finally, the associations were stronger when considering the average cumulative consumption over the 30-year follow-up period and still stronger following the calibration of meat consumption with data extrapolated from food registers. The latter step was taken to account for measurement errors.
Alternatives are better
By analyzing alternative protein sources, the researchers discovered that nuts and legumes are associated with the most substantial reductions in diabetes risk. “This discovery is consistent with the evidence that shows that sources of unsaturated fatty acids and antioxidants have beneficial effects on glycemic control, insulin response, and inflammation,” they wrote. By replacing a serving of processed red meat, unprocessed red meat, or a combination of the two with a serving of dry fruit or legumes, the risk of developing diabetes is lowered by 30%, 41%, and 29%, respectively. Replacing red meat with a serving of dairy products is also associated with a reduced risk.
Confirmation
Several biological mechanisms could contribute to the increased risk for type 2 diabetes in people who consume red meat. The high level of saturated fats or the relatively low level of polyunsaturated fats, heme iron, or the high nitrate content in processed red meats could play a role. A strong positive association between consumption of this meat, particularly when processed, and the onset of diabetes has already emerged from other studies, including a trial carried out several years ago in the same cohorts. “In the current study, we wanted to look at this association in the same three cohorts in more detail, with over 9,000 additional cases of type 2 diabetes documented with extensive follow-up,” the researchers explained.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
This association was confirmed by a new study published in the American Journal of Clinical Nutrition, a data analysis of nearly 217,000 people who were monitored for three decades as part of several cohort studies. “Our study supports the current dietary recommendations of limiting consumption of red meat and highlights the importance of different alternative sources of protein in preventing type 2 diabetes,” the researchers wrote.
Consumption and risk
The study included men and women who took part in the Nurses’ Health Study, the Nurses’ Health Study II, or the Health Professionals Follow-up Study. Questionnaires were used to collect data every 2-4 years on the frequency of specific food consumption. Information on the onset of diseases and on different health-related aspects was collected every 2 years.
Those who consumed more red meat had a higher body mass index, higher total energy intake, and greater likelihood of being a smoker. They were physically less active and less likely to take multivitamins. In a follow-up of 5.48 million person-years, 22,761 cases of type 2 diabetes were recorded.
The link between consumption of processed and unprocessed red meat (and both combined) and a higher risk of diabetes was observed in all cohorts when analyzed separately and jointly. The people in the highest quintile for combined red meat consumption had a 2% greater risk of developing the disease, compared with those in the lowest quintile. The risk increases associated with processed and unprocessed meat were 51% and 40%, respectively. One additional serving per day of processed red meat was associated with a 1.46-fold greater risk of diabetes. This risk was 1.24 times greater for unprocessed meat and 1.28 times greater for both types combined.
The associations had a linear dose-response relationship and remained firm even after accounting for BMI, which the researchers stressed could be a mediating factor. Finally, the associations were stronger when considering the average cumulative consumption over the 30-year follow-up period and still stronger following the calibration of meat consumption with data extrapolated from food registers. The latter step was taken to account for measurement errors.
Alternatives are better
By analyzing alternative protein sources, the researchers discovered that nuts and legumes are associated with the most substantial reductions in diabetes risk. “This discovery is consistent with the evidence that shows that sources of unsaturated fatty acids and antioxidants have beneficial effects on glycemic control, insulin response, and inflammation,” they wrote. By replacing a serving of processed red meat, unprocessed red meat, or a combination of the two with a serving of dry fruit or legumes, the risk of developing diabetes is lowered by 30%, 41%, and 29%, respectively. Replacing red meat with a serving of dairy products is also associated with a reduced risk.
Confirmation
Several biological mechanisms could contribute to the increased risk for type 2 diabetes in people who consume red meat. The high level of saturated fats or the relatively low level of polyunsaturated fats, heme iron, or the high nitrate content in processed red meats could play a role. A strong positive association between consumption of this meat, particularly when processed, and the onset of diabetes has already emerged from other studies, including a trial carried out several years ago in the same cohorts. “In the current study, we wanted to look at this association in the same three cohorts in more detail, with over 9,000 additional cases of type 2 diabetes documented with extensive follow-up,” the researchers explained.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
This association was confirmed by a new study published in the American Journal of Clinical Nutrition, a data analysis of nearly 217,000 people who were monitored for three decades as part of several cohort studies. “Our study supports the current dietary recommendations of limiting consumption of red meat and highlights the importance of different alternative sources of protein in preventing type 2 diabetes,” the researchers wrote.
Consumption and risk
The study included men and women who took part in the Nurses’ Health Study, the Nurses’ Health Study II, or the Health Professionals Follow-up Study. Questionnaires were used to collect data every 2-4 years on the frequency of specific food consumption. Information on the onset of diseases and on different health-related aspects was collected every 2 years.
Those who consumed more red meat had a higher body mass index, higher total energy intake, and greater likelihood of being a smoker. They were physically less active and less likely to take multivitamins. In a follow-up of 5.48 million person-years, 22,761 cases of type 2 diabetes were recorded.
The link between consumption of processed and unprocessed red meat (and both combined) and a higher risk of diabetes was observed in all cohorts when analyzed separately and jointly. The people in the highest quintile for combined red meat consumption had a 2% greater risk of developing the disease, compared with those in the lowest quintile. The risk increases associated with processed and unprocessed meat were 51% and 40%, respectively. One additional serving per day of processed red meat was associated with a 1.46-fold greater risk of diabetes. This risk was 1.24 times greater for unprocessed meat and 1.28 times greater for both types combined.
The associations had a linear dose-response relationship and remained firm even after accounting for BMI, which the researchers stressed could be a mediating factor. Finally, the associations were stronger when considering the average cumulative consumption over the 30-year follow-up period and still stronger following the calibration of meat consumption with data extrapolated from food registers. The latter step was taken to account for measurement errors.
Alternatives are better
By analyzing alternative protein sources, the researchers discovered that nuts and legumes are associated with the most substantial reductions in diabetes risk. “This discovery is consistent with the evidence that shows that sources of unsaturated fatty acids and antioxidants have beneficial effects on glycemic control, insulin response, and inflammation,” they wrote. By replacing a serving of processed red meat, unprocessed red meat, or a combination of the two with a serving of dry fruit or legumes, the risk of developing diabetes is lowered by 30%, 41%, and 29%, respectively. Replacing red meat with a serving of dairy products is also associated with a reduced risk.
Confirmation
Several biological mechanisms could contribute to the increased risk for type 2 diabetes in people who consume red meat. The high level of saturated fats or the relatively low level of polyunsaturated fats, heme iron, or the high nitrate content in processed red meats could play a role. A strong positive association between consumption of this meat, particularly when processed, and the onset of diabetes has already emerged from other studies, including a trial carried out several years ago in the same cohorts. “In the current study, we wanted to look at this association in the same three cohorts in more detail, with over 9,000 additional cases of type 2 diabetes documented with extensive follow-up,” the researchers explained.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF CLINICAL NUTRITION
PREVENT: AHA’s new risk calculator incorporates CKM health
.
The new Predicting Risk of CVD Events (PREVENT) calculator is the first risk calculator that combines measures of cardiovascular, kidney, and metabolic health to estimate risk for CVD.
It follows an AHA presidential advisory and scientific statement published in October, formally defining cardiovascular-kidney-metabolic (CKM) syndrome.
The PREVENT calculator also “starts earlier and goes longer” than the pooled cohort equations (PCE), Sadiya Khan, MD, MSc, chair of the statement writing committee, told this news organization.
PREVENT is for use in adults aged 30-79 years and estimates the 10- and 30-year risk of total CVD including, for the first time, heart failure. The PCE were designed to assess 10-year risk of only myocardial infarction and stroke and only in adults aged 40-79 years.
“The new PREVENT equations are important for doctors because they allow us to start conversations earlier and more comprehensively and accurately calculate risk for our patients,” said Dr. Khan, preventive cardiologist at Northwestern Medicine and associate professor at Northwestern University in Chicago.
“We want to support clinicians in starting these conversations around optimizing CKM health earlier and begin to engage in discussions on ways to optimize health,” Dr. Khan added.
The AHA scientific statement on the PREVENT calculator, with Dr. Khan as lead author, was published online in Circulation, with an accompanying article that describes development and validation of the tool.
Going beyond the PCE
The new calculator was developed using health information from more than 6 million adults from diverse racial and ethnic, socioeconomic, and geographic backgrounds.
In addition to blood pressure and cholesterol levels, the PREVENT equations allow for inclusion of hemoglobin A1c, if necessary, to monitor metabolic health.
It also includes estimated glomerular filtration rate (eGFR), a measure of kidney function, and allows for use of albumin excretion to monitor kidney disease to further individualize risk assessment and help inform personalized treatment options.
The new calculator also asks about tobacco use and use of medications for CVD risk factors and factors in age and sex, and it removes race from the risk calculations.
“The inclusion of race in risk prediction may imply that differences by race are not modifiable and may reify race as a biological construct, which may worsen health disparities. Therefore, it was decided a priori not to include race as a predictor in the development of PREVENT,” the writing group said.
They emphasized that the PREVENT calculator has similar accuracy among varied racial and ethnic groups.
The equations include an option to use the Social Deprivation Index, which incorporates measures of adverse social determinants of health such as education, poverty, unemployment, and factors based on a person’s environment.
The PREVENT equations are a “critical first step” toward including CKM health and social factors in risk prediction for CVD, Dr. Khan said in a news release.
“We are working on finalizing the online tool and it should be available soon – hopefully in a few weeks,” Dr. Khan told this news organization.
Knowledge gaps
The scientific statement lists several knowledge gaps and areas for more research. These include:
- Incorporating “net benefit” to identify the expected benefit of treatment recommendations based on an individual’s level of risk.
- Collecting more data from people of diverse race and ethnic backgrounds to better represent the increasing diversity in the United States. The number of Hispanic and Asian people included in the PREVENT datasets is lower than national estimates in the general U.S. population, so risk estimations in these populations may be less precise.
- Expanding the collection, reporting, and standardization of social determinants of health data, such as individual information rather than neighborhood information.
- Expanding risk assessment and prevention to earlier in life (childhood and/or adolescence) and in key life periods, such as during the peripartum period, since adverse pregnancy outcomes are associated with increased CVD risk.
- Investigating whether predicting adverse kidney outcomes, particularly among people with and without type 2 diabetes, may further optimize cardiovascular risk prediction.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA. Dr. Khan reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
.
The new Predicting Risk of CVD Events (PREVENT) calculator is the first risk calculator that combines measures of cardiovascular, kidney, and metabolic health to estimate risk for CVD.
It follows an AHA presidential advisory and scientific statement published in October, formally defining cardiovascular-kidney-metabolic (CKM) syndrome.
The PREVENT calculator also “starts earlier and goes longer” than the pooled cohort equations (PCE), Sadiya Khan, MD, MSc, chair of the statement writing committee, told this news organization.
PREVENT is for use in adults aged 30-79 years and estimates the 10- and 30-year risk of total CVD including, for the first time, heart failure. The PCE were designed to assess 10-year risk of only myocardial infarction and stroke and only in adults aged 40-79 years.
“The new PREVENT equations are important for doctors because they allow us to start conversations earlier and more comprehensively and accurately calculate risk for our patients,” said Dr. Khan, preventive cardiologist at Northwestern Medicine and associate professor at Northwestern University in Chicago.
“We want to support clinicians in starting these conversations around optimizing CKM health earlier and begin to engage in discussions on ways to optimize health,” Dr. Khan added.
The AHA scientific statement on the PREVENT calculator, with Dr. Khan as lead author, was published online in Circulation, with an accompanying article that describes development and validation of the tool.
Going beyond the PCE
The new calculator was developed using health information from more than 6 million adults from diverse racial and ethnic, socioeconomic, and geographic backgrounds.
In addition to blood pressure and cholesterol levels, the PREVENT equations allow for inclusion of hemoglobin A1c, if necessary, to monitor metabolic health.
It also includes estimated glomerular filtration rate (eGFR), a measure of kidney function, and allows for use of albumin excretion to monitor kidney disease to further individualize risk assessment and help inform personalized treatment options.
The new calculator also asks about tobacco use and use of medications for CVD risk factors and factors in age and sex, and it removes race from the risk calculations.
“The inclusion of race in risk prediction may imply that differences by race are not modifiable and may reify race as a biological construct, which may worsen health disparities. Therefore, it was decided a priori not to include race as a predictor in the development of PREVENT,” the writing group said.
They emphasized that the PREVENT calculator has similar accuracy among varied racial and ethnic groups.
The equations include an option to use the Social Deprivation Index, which incorporates measures of adverse social determinants of health such as education, poverty, unemployment, and factors based on a person’s environment.
The PREVENT equations are a “critical first step” toward including CKM health and social factors in risk prediction for CVD, Dr. Khan said in a news release.
“We are working on finalizing the online tool and it should be available soon – hopefully in a few weeks,” Dr. Khan told this news organization.
Knowledge gaps
The scientific statement lists several knowledge gaps and areas for more research. These include:
- Incorporating “net benefit” to identify the expected benefit of treatment recommendations based on an individual’s level of risk.
- Collecting more data from people of diverse race and ethnic backgrounds to better represent the increasing diversity in the United States. The number of Hispanic and Asian people included in the PREVENT datasets is lower than national estimates in the general U.S. population, so risk estimations in these populations may be less precise.
- Expanding the collection, reporting, and standardization of social determinants of health data, such as individual information rather than neighborhood information.
- Expanding risk assessment and prevention to earlier in life (childhood and/or adolescence) and in key life periods, such as during the peripartum period, since adverse pregnancy outcomes are associated with increased CVD risk.
- Investigating whether predicting adverse kidney outcomes, particularly among people with and without type 2 diabetes, may further optimize cardiovascular risk prediction.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA. Dr. Khan reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
.
The new Predicting Risk of CVD Events (PREVENT) calculator is the first risk calculator that combines measures of cardiovascular, kidney, and metabolic health to estimate risk for CVD.
It follows an AHA presidential advisory and scientific statement published in October, formally defining cardiovascular-kidney-metabolic (CKM) syndrome.
The PREVENT calculator also “starts earlier and goes longer” than the pooled cohort equations (PCE), Sadiya Khan, MD, MSc, chair of the statement writing committee, told this news organization.
PREVENT is for use in adults aged 30-79 years and estimates the 10- and 30-year risk of total CVD including, for the first time, heart failure. The PCE were designed to assess 10-year risk of only myocardial infarction and stroke and only in adults aged 40-79 years.
“The new PREVENT equations are important for doctors because they allow us to start conversations earlier and more comprehensively and accurately calculate risk for our patients,” said Dr. Khan, preventive cardiologist at Northwestern Medicine and associate professor at Northwestern University in Chicago.
“We want to support clinicians in starting these conversations around optimizing CKM health earlier and begin to engage in discussions on ways to optimize health,” Dr. Khan added.
The AHA scientific statement on the PREVENT calculator, with Dr. Khan as lead author, was published online in Circulation, with an accompanying article that describes development and validation of the tool.
Going beyond the PCE
The new calculator was developed using health information from more than 6 million adults from diverse racial and ethnic, socioeconomic, and geographic backgrounds.
In addition to blood pressure and cholesterol levels, the PREVENT equations allow for inclusion of hemoglobin A1c, if necessary, to monitor metabolic health.
It also includes estimated glomerular filtration rate (eGFR), a measure of kidney function, and allows for use of albumin excretion to monitor kidney disease to further individualize risk assessment and help inform personalized treatment options.
The new calculator also asks about tobacco use and use of medications for CVD risk factors and factors in age and sex, and it removes race from the risk calculations.
“The inclusion of race in risk prediction may imply that differences by race are not modifiable and may reify race as a biological construct, which may worsen health disparities. Therefore, it was decided a priori not to include race as a predictor in the development of PREVENT,” the writing group said.
They emphasized that the PREVENT calculator has similar accuracy among varied racial and ethnic groups.
The equations include an option to use the Social Deprivation Index, which incorporates measures of adverse social determinants of health such as education, poverty, unemployment, and factors based on a person’s environment.
The PREVENT equations are a “critical first step” toward including CKM health and social factors in risk prediction for CVD, Dr. Khan said in a news release.
“We are working on finalizing the online tool and it should be available soon – hopefully in a few weeks,” Dr. Khan told this news organization.
Knowledge gaps
The scientific statement lists several knowledge gaps and areas for more research. These include:
- Incorporating “net benefit” to identify the expected benefit of treatment recommendations based on an individual’s level of risk.
- Collecting more data from people of diverse race and ethnic backgrounds to better represent the increasing diversity in the United States. The number of Hispanic and Asian people included in the PREVENT datasets is lower than national estimates in the general U.S. population, so risk estimations in these populations may be less precise.
- Expanding the collection, reporting, and standardization of social determinants of health data, such as individual information rather than neighborhood information.
- Expanding risk assessment and prevention to earlier in life (childhood and/or adolescence) and in key life periods, such as during the peripartum period, since adverse pregnancy outcomes are associated with increased CVD risk.
- Investigating whether predicting adverse kidney outcomes, particularly among people with and without type 2 diabetes, may further optimize cardiovascular risk prediction.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA. Dr. Khan reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Already-available drug could help treat type 1 diabetes
“I think we have lots of potential to improve people’s quality of life who are living with type 1 diabetes if we can increase their endogenous insulin secretion. ... I think long-term combination therapy is going to be the answer,” study author Emily K. Sims, MD, a pediatric endocrinologist at Indiana University, Indianapolis, said in an interview.
DFMO inhibits the polyamine biosynthesis pathway, which plays a role in the inflammatory responses in autoimmune diseases, including type 1 diabetes. It’s sold under the name eflornithine as an intravenous treatment for African sleeping sickness (trypanosomiasis) and as a cream for unwanted hair growth in women. It also has orphan designations for treating various cancers, including neuroblastoma.
In type 1 diabetes, the immune system destroys insulin-producing pancreatic beta cells. Insulin treatment is required. Recently, the monoclonal antibody teplizumab (Tzield, Sanofi) was approved as a treatment for delaying the onset of type 1 diabetes in people with autoantibodies that signify a preclinical stage of the condition. As yet, no agent has been approved for preserving beta-cell function after the onset of type 1 diabetes, but many are under investigation.
The new safety study by Dr. Sims and colleagues, which was published in Cell Medicine Reports, enrolled 41 people with type 1 diabetes who had been diagnosed within the previous 8 months, including 31 children. Participants were randomly assigned to undergo oral treatment with DFMO at one of five doses or placebo for 3 months, with 3 additional months of follow-up.
Following a mixed-meal tolerance test at 6 months, the C-peptide area under the curve – a measure of beta-cell function – was significantly higher with the three highest DFMO doses compared to placebo (P = .02, .03, and .02 for 125 mg/m2, 750 mg/m2, and 1,000 mg/m2, respectively).
Two individuals dropped out, one because of anaphylaxis. There were no dose-limiting toxicities or serious adverse events, while mild gastrointestinal events, anemia, and headache were common. “Although there’s no [Food and Drug Administration] approval for the oral form right now, there’s a lot of safety data, including in kids from the neuroblastoma studies,” Dr. Sims explained.
There were no differences in C-peptide at 3 months or in hemoglobin A1c at any time point. Glucose areas under the curve were significantly lower for DFMO, compared with placebo in the 125-mg/m2 and 750-mg/m2 treatment groups at the 6-month time point (P = .03 and .04, respectively).
In their article, Dr. Sims and colleagues also reported confirmatory analyses in mice, as well as testing in the humans showing that there didn’t appear to be significant immune system modulation. “So, we can envision giving DFMO in addition to something that targets the immune system, as a combination therapy,” said Dr. Sims, who also worked on the pivotal study of teplizumab.
“I’m excited. The sample size is small, so I was kind of expecting no efficacy signals. ... It’s definitely worth following up,” she said.
However, she noted, “it wasn’t a slam-dunk huge effect. It was subtle. It seemed that things were kind of more stable compared to placebo over time versus ... a big increase in C-peptide over time.”
But, she added, “I believe that even teplizumab will need to be used in combination. It delays the onset of type 1 diabetes and improves C-peptide, but it didn’t get everyone off insulin. I don’t think we’ve seen any drug that won’t need to be used in combination.”
Dr. Sims pointed to other investigational agents, such as verapamil and various Janus kinase inhibitors, that may also serve in combination to forestall or reduce insulin dependency for people with either new-onset type 1 diabetes or those who have been identified via screening as having type 1 diabetes–related autoantibodies. “I think there are a lot of potential different interventions.”
Dr. Sims and colleagues are now conducting a larger six-center JDRF-funded study of DFMO in early-onset type 1 diabetes that will be fully powered and that will use the highest tolerated doses from the preliminary study.
She believes there will likely be benefit even if the agent doesn’t completely reverse the disease. “The people who are making more insulin are just easier to manage, with more time in range and less hypoglycemia.” Even if the drugs only delay but don’t prevent type 1 diabetes entirely in those at risk, “the improvement in quality of life of being able to delay insulin for a few years is really palpable. ... I’m really optimistic.”
Dr. Sims disclosed no relevant financial relationships. Three other authors are coauthors on a patent application for the use of DFMO for the treatment of beta-cell dysfunction in type 1 diabetes; one of those three authors is an employee of Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
“I think we have lots of potential to improve people’s quality of life who are living with type 1 diabetes if we can increase their endogenous insulin secretion. ... I think long-term combination therapy is going to be the answer,” study author Emily K. Sims, MD, a pediatric endocrinologist at Indiana University, Indianapolis, said in an interview.
DFMO inhibits the polyamine biosynthesis pathway, which plays a role in the inflammatory responses in autoimmune diseases, including type 1 diabetes. It’s sold under the name eflornithine as an intravenous treatment for African sleeping sickness (trypanosomiasis) and as a cream for unwanted hair growth in women. It also has orphan designations for treating various cancers, including neuroblastoma.
In type 1 diabetes, the immune system destroys insulin-producing pancreatic beta cells. Insulin treatment is required. Recently, the monoclonal antibody teplizumab (Tzield, Sanofi) was approved as a treatment for delaying the onset of type 1 diabetes in people with autoantibodies that signify a preclinical stage of the condition. As yet, no agent has been approved for preserving beta-cell function after the onset of type 1 diabetes, but many are under investigation.
The new safety study by Dr. Sims and colleagues, which was published in Cell Medicine Reports, enrolled 41 people with type 1 diabetes who had been diagnosed within the previous 8 months, including 31 children. Participants were randomly assigned to undergo oral treatment with DFMO at one of five doses or placebo for 3 months, with 3 additional months of follow-up.
Following a mixed-meal tolerance test at 6 months, the C-peptide area under the curve – a measure of beta-cell function – was significantly higher with the three highest DFMO doses compared to placebo (P = .02, .03, and .02 for 125 mg/m2, 750 mg/m2, and 1,000 mg/m2, respectively).
Two individuals dropped out, one because of anaphylaxis. There were no dose-limiting toxicities or serious adverse events, while mild gastrointestinal events, anemia, and headache were common. “Although there’s no [Food and Drug Administration] approval for the oral form right now, there’s a lot of safety data, including in kids from the neuroblastoma studies,” Dr. Sims explained.
There were no differences in C-peptide at 3 months or in hemoglobin A1c at any time point. Glucose areas under the curve were significantly lower for DFMO, compared with placebo in the 125-mg/m2 and 750-mg/m2 treatment groups at the 6-month time point (P = .03 and .04, respectively).
In their article, Dr. Sims and colleagues also reported confirmatory analyses in mice, as well as testing in the humans showing that there didn’t appear to be significant immune system modulation. “So, we can envision giving DFMO in addition to something that targets the immune system, as a combination therapy,” said Dr. Sims, who also worked on the pivotal study of teplizumab.
“I’m excited. The sample size is small, so I was kind of expecting no efficacy signals. ... It’s definitely worth following up,” she said.
However, she noted, “it wasn’t a slam-dunk huge effect. It was subtle. It seemed that things were kind of more stable compared to placebo over time versus ... a big increase in C-peptide over time.”
But, she added, “I believe that even teplizumab will need to be used in combination. It delays the onset of type 1 diabetes and improves C-peptide, but it didn’t get everyone off insulin. I don’t think we’ve seen any drug that won’t need to be used in combination.”
Dr. Sims pointed to other investigational agents, such as verapamil and various Janus kinase inhibitors, that may also serve in combination to forestall or reduce insulin dependency for people with either new-onset type 1 diabetes or those who have been identified via screening as having type 1 diabetes–related autoantibodies. “I think there are a lot of potential different interventions.”
Dr. Sims and colleagues are now conducting a larger six-center JDRF-funded study of DFMO in early-onset type 1 diabetes that will be fully powered and that will use the highest tolerated doses from the preliminary study.
She believes there will likely be benefit even if the agent doesn’t completely reverse the disease. “The people who are making more insulin are just easier to manage, with more time in range and less hypoglycemia.” Even if the drugs only delay but don’t prevent type 1 diabetes entirely in those at risk, “the improvement in quality of life of being able to delay insulin for a few years is really palpable. ... I’m really optimistic.”
Dr. Sims disclosed no relevant financial relationships. Three other authors are coauthors on a patent application for the use of DFMO for the treatment of beta-cell dysfunction in type 1 diabetes; one of those three authors is an employee of Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
“I think we have lots of potential to improve people’s quality of life who are living with type 1 diabetes if we can increase their endogenous insulin secretion. ... I think long-term combination therapy is going to be the answer,” study author Emily K. Sims, MD, a pediatric endocrinologist at Indiana University, Indianapolis, said in an interview.
DFMO inhibits the polyamine biosynthesis pathway, which plays a role in the inflammatory responses in autoimmune diseases, including type 1 diabetes. It’s sold under the name eflornithine as an intravenous treatment for African sleeping sickness (trypanosomiasis) and as a cream for unwanted hair growth in women. It also has orphan designations for treating various cancers, including neuroblastoma.
In type 1 diabetes, the immune system destroys insulin-producing pancreatic beta cells. Insulin treatment is required. Recently, the monoclonal antibody teplizumab (Tzield, Sanofi) was approved as a treatment for delaying the onset of type 1 diabetes in people with autoantibodies that signify a preclinical stage of the condition. As yet, no agent has been approved for preserving beta-cell function after the onset of type 1 diabetes, but many are under investigation.
The new safety study by Dr. Sims and colleagues, which was published in Cell Medicine Reports, enrolled 41 people with type 1 diabetes who had been diagnosed within the previous 8 months, including 31 children. Participants were randomly assigned to undergo oral treatment with DFMO at one of five doses or placebo for 3 months, with 3 additional months of follow-up.
Following a mixed-meal tolerance test at 6 months, the C-peptide area under the curve – a measure of beta-cell function – was significantly higher with the three highest DFMO doses compared to placebo (P = .02, .03, and .02 for 125 mg/m2, 750 mg/m2, and 1,000 mg/m2, respectively).
Two individuals dropped out, one because of anaphylaxis. There were no dose-limiting toxicities or serious adverse events, while mild gastrointestinal events, anemia, and headache were common. “Although there’s no [Food and Drug Administration] approval for the oral form right now, there’s a lot of safety data, including in kids from the neuroblastoma studies,” Dr. Sims explained.
There were no differences in C-peptide at 3 months or in hemoglobin A1c at any time point. Glucose areas under the curve were significantly lower for DFMO, compared with placebo in the 125-mg/m2 and 750-mg/m2 treatment groups at the 6-month time point (P = .03 and .04, respectively).
In their article, Dr. Sims and colleagues also reported confirmatory analyses in mice, as well as testing in the humans showing that there didn’t appear to be significant immune system modulation. “So, we can envision giving DFMO in addition to something that targets the immune system, as a combination therapy,” said Dr. Sims, who also worked on the pivotal study of teplizumab.
“I’m excited. The sample size is small, so I was kind of expecting no efficacy signals. ... It’s definitely worth following up,” she said.
However, she noted, “it wasn’t a slam-dunk huge effect. It was subtle. It seemed that things were kind of more stable compared to placebo over time versus ... a big increase in C-peptide over time.”
But, she added, “I believe that even teplizumab will need to be used in combination. It delays the onset of type 1 diabetes and improves C-peptide, but it didn’t get everyone off insulin. I don’t think we’ve seen any drug that won’t need to be used in combination.”
Dr. Sims pointed to other investigational agents, such as verapamil and various Janus kinase inhibitors, that may also serve in combination to forestall or reduce insulin dependency for people with either new-onset type 1 diabetes or those who have been identified via screening as having type 1 diabetes–related autoantibodies. “I think there are a lot of potential different interventions.”
Dr. Sims and colleagues are now conducting a larger six-center JDRF-funded study of DFMO in early-onset type 1 diabetes that will be fully powered and that will use the highest tolerated doses from the preliminary study.
She believes there will likely be benefit even if the agent doesn’t completely reverse the disease. “The people who are making more insulin are just easier to manage, with more time in range and less hypoglycemia.” Even if the drugs only delay but don’t prevent type 1 diabetes entirely in those at risk, “the improvement in quality of life of being able to delay insulin for a few years is really palpable. ... I’m really optimistic.”
Dr. Sims disclosed no relevant financial relationships. Three other authors are coauthors on a patent application for the use of DFMO for the treatment of beta-cell dysfunction in type 1 diabetes; one of those three authors is an employee of Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM CELL MEDICINE REPORTS
WHO: Smoking cessation reduces risk of type 2 diabetes up to 40%
TOPLINE:
, and quitting even after one has developed type 2 diabetes is important in preventing a worsening of the disease’s many serious comorbidities, according to a new policy brief jointly issued by the World Health Organization, the International Diabetes Federation (IDF), and the University of Newcastle, Callaghan, Australia.
With type 2 diabetes representing one of the most prevalent chronic diseases worldwide and the ninth cause of death globally, the potential to reduce the risk and worsening of the disease by quitting smoking adds to the urgency of smoking cessation as a public health interest.
METHODOLOGY:
- The policy brief summarizes the evidence on the health impacts of type 2 diabetes, tobacco smoking, and the pathophysiology of tobacco use and its role in the development of type 2 diabetes.
- The brief also describes the latest data on newer products that target smokers or potential smokers, including smokeless tobacco, new nicotine and tobacco products, and their relationship with type 2 diabetes. For instance, evidence suggests that even with smokeless tobacco, heavy use or high consumption increases the risk of developing type 2 diabetes, as the products often contain nicotine, known to contribute to the development of type 2 diabetes and related health conditions.
- Evidence on the effectiveness of tobacco control interventions among those with type 2 diabetes is also summarized, including discussion of a systematic review of six studies suggesting that interventions focusing on education and the involvement of health care professionals and pharmacists can be beneficial for people with type 2 diabetes.
TAKEAWAY:
- Smoking exacerbates the known serious complications of diabetic neuropathy and foot ulcers with type 2 diabetes, while further impeding wound healing.
- Smoking also causes damage to retinal blood vessels already at risk with type 2 diabetes, increasing the risk of diabetic retinopathy and vision loss.
- Quitting tobacco use can help prevent those and other major health complications already linked to diabetes, including kidney failure and cardiovascular events.
- Studies show that key misconceptions among smokers with type 2 diabetes that can prevent cessation include concerns about post-cessation weight gain, the influence of peers who smoke, and the psychological aspect of addiction.
- Clinicians are urged to provide advice on how to stop smoking to all tobacco users during the course of a routine consultation or interaction, which can be accomplished in only a few minutes.
IN PRACTICE:
“Health professionals play a vital role in motivating and guiding individuals with type 2 diabetes in their journey to quit tobacco,” Ruediger Krech, MD, director of the Department of Health Promotion at the World Health Organization in Geneva, Switzerland, said in a press statement on the policy brief.
“Simultaneously, governments must take the crucial step of ensuring all indoor public places, workplaces, and public transport are completely smoke-free. These interventions are essential safeguards against the onset and progression of this and many other chronic diseases,” he emphasized.
SOURCE:
The policy brief was jointly developed by the World Health Organization, the International Diabetes Federation, and the University of Newcastle.
The detailed policy brief can be downloaded on the IDF website.
LIMITATIONS:
Research remains limited on some issues, including the effectiveness of tobacco control interventions and smoking cessation methods for people with type 2 diabetes.
Likewise, specific guidelines for smoking cessation in the type 2 diabetes population are lacking. However, the general approaches of building patient motivation, behavioral interventions, and pharmacological treatments are advised.
“These interventions should be at least as intensive as those for the general population, while considering the unique characteristics of the disease and the individual,” the authors asserted.
DISCLOSURES:
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, and quitting even after one has developed type 2 diabetes is important in preventing a worsening of the disease’s many serious comorbidities, according to a new policy brief jointly issued by the World Health Organization, the International Diabetes Federation (IDF), and the University of Newcastle, Callaghan, Australia.
With type 2 diabetes representing one of the most prevalent chronic diseases worldwide and the ninth cause of death globally, the potential to reduce the risk and worsening of the disease by quitting smoking adds to the urgency of smoking cessation as a public health interest.
METHODOLOGY:
- The policy brief summarizes the evidence on the health impacts of type 2 diabetes, tobacco smoking, and the pathophysiology of tobacco use and its role in the development of type 2 diabetes.
- The brief also describes the latest data on newer products that target smokers or potential smokers, including smokeless tobacco, new nicotine and tobacco products, and their relationship with type 2 diabetes. For instance, evidence suggests that even with smokeless tobacco, heavy use or high consumption increases the risk of developing type 2 diabetes, as the products often contain nicotine, known to contribute to the development of type 2 diabetes and related health conditions.
- Evidence on the effectiveness of tobacco control interventions among those with type 2 diabetes is also summarized, including discussion of a systematic review of six studies suggesting that interventions focusing on education and the involvement of health care professionals and pharmacists can be beneficial for people with type 2 diabetes.
TAKEAWAY:
- Smoking exacerbates the known serious complications of diabetic neuropathy and foot ulcers with type 2 diabetes, while further impeding wound healing.
- Smoking also causes damage to retinal blood vessels already at risk with type 2 diabetes, increasing the risk of diabetic retinopathy and vision loss.
- Quitting tobacco use can help prevent those and other major health complications already linked to diabetes, including kidney failure and cardiovascular events.
- Studies show that key misconceptions among smokers with type 2 diabetes that can prevent cessation include concerns about post-cessation weight gain, the influence of peers who smoke, and the psychological aspect of addiction.
- Clinicians are urged to provide advice on how to stop smoking to all tobacco users during the course of a routine consultation or interaction, which can be accomplished in only a few minutes.
IN PRACTICE:
“Health professionals play a vital role in motivating and guiding individuals with type 2 diabetes in their journey to quit tobacco,” Ruediger Krech, MD, director of the Department of Health Promotion at the World Health Organization in Geneva, Switzerland, said in a press statement on the policy brief.
“Simultaneously, governments must take the crucial step of ensuring all indoor public places, workplaces, and public transport are completely smoke-free. These interventions are essential safeguards against the onset and progression of this and many other chronic diseases,” he emphasized.
SOURCE:
The policy brief was jointly developed by the World Health Organization, the International Diabetes Federation, and the University of Newcastle.
The detailed policy brief can be downloaded on the IDF website.
LIMITATIONS:
Research remains limited on some issues, including the effectiveness of tobacco control interventions and smoking cessation methods for people with type 2 diabetes.
Likewise, specific guidelines for smoking cessation in the type 2 diabetes population are lacking. However, the general approaches of building patient motivation, behavioral interventions, and pharmacological treatments are advised.
“These interventions should be at least as intensive as those for the general population, while considering the unique characteristics of the disease and the individual,” the authors asserted.
DISCLOSURES:
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, and quitting even after one has developed type 2 diabetes is important in preventing a worsening of the disease’s many serious comorbidities, according to a new policy brief jointly issued by the World Health Organization, the International Diabetes Federation (IDF), and the University of Newcastle, Callaghan, Australia.
With type 2 diabetes representing one of the most prevalent chronic diseases worldwide and the ninth cause of death globally, the potential to reduce the risk and worsening of the disease by quitting smoking adds to the urgency of smoking cessation as a public health interest.
METHODOLOGY:
- The policy brief summarizes the evidence on the health impacts of type 2 diabetes, tobacco smoking, and the pathophysiology of tobacco use and its role in the development of type 2 diabetes.
- The brief also describes the latest data on newer products that target smokers or potential smokers, including smokeless tobacco, new nicotine and tobacco products, and their relationship with type 2 diabetes. For instance, evidence suggests that even with smokeless tobacco, heavy use or high consumption increases the risk of developing type 2 diabetes, as the products often contain nicotine, known to contribute to the development of type 2 diabetes and related health conditions.
- Evidence on the effectiveness of tobacco control interventions among those with type 2 diabetes is also summarized, including discussion of a systematic review of six studies suggesting that interventions focusing on education and the involvement of health care professionals and pharmacists can be beneficial for people with type 2 diabetes.
TAKEAWAY:
- Smoking exacerbates the known serious complications of diabetic neuropathy and foot ulcers with type 2 diabetes, while further impeding wound healing.
- Smoking also causes damage to retinal blood vessels already at risk with type 2 diabetes, increasing the risk of diabetic retinopathy and vision loss.
- Quitting tobacco use can help prevent those and other major health complications already linked to diabetes, including kidney failure and cardiovascular events.
- Studies show that key misconceptions among smokers with type 2 diabetes that can prevent cessation include concerns about post-cessation weight gain, the influence of peers who smoke, and the psychological aspect of addiction.
- Clinicians are urged to provide advice on how to stop smoking to all tobacco users during the course of a routine consultation or interaction, which can be accomplished in only a few minutes.
IN PRACTICE:
“Health professionals play a vital role in motivating and guiding individuals with type 2 diabetes in their journey to quit tobacco,” Ruediger Krech, MD, director of the Department of Health Promotion at the World Health Organization in Geneva, Switzerland, said in a press statement on the policy brief.
“Simultaneously, governments must take the crucial step of ensuring all indoor public places, workplaces, and public transport are completely smoke-free. These interventions are essential safeguards against the onset and progression of this and many other chronic diseases,” he emphasized.
SOURCE:
The policy brief was jointly developed by the World Health Organization, the International Diabetes Federation, and the University of Newcastle.
The detailed policy brief can be downloaded on the IDF website.
LIMITATIONS:
Research remains limited on some issues, including the effectiveness of tobacco control interventions and smoking cessation methods for people with type 2 diabetes.
Likewise, specific guidelines for smoking cessation in the type 2 diabetes population are lacking. However, the general approaches of building patient motivation, behavioral interventions, and pharmacological treatments are advised.
“These interventions should be at least as intensive as those for the general population, while considering the unique characteristics of the disease and the individual,” the authors asserted.
DISCLOSURES:
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.