User login
Time-Restricted Eating Is Not a Metabolic Magic Bullet
This transcript has been edited for clarity.
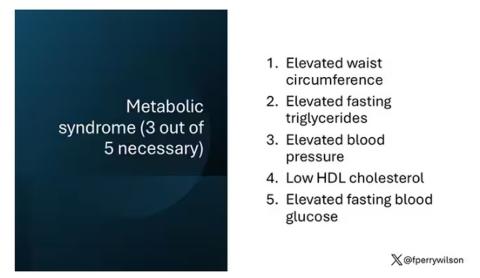
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
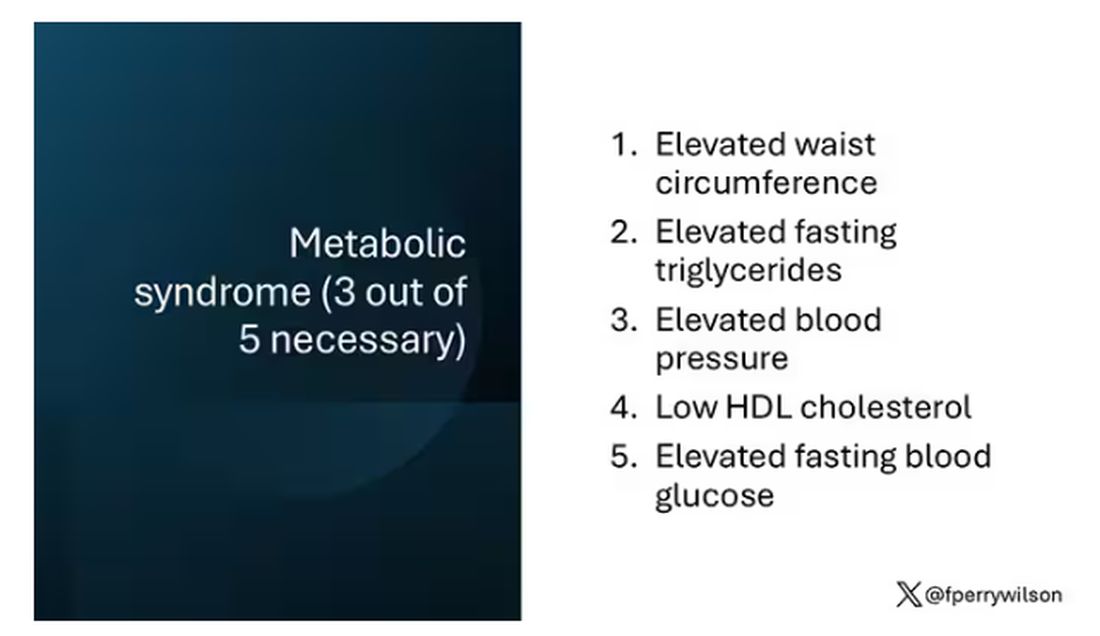
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.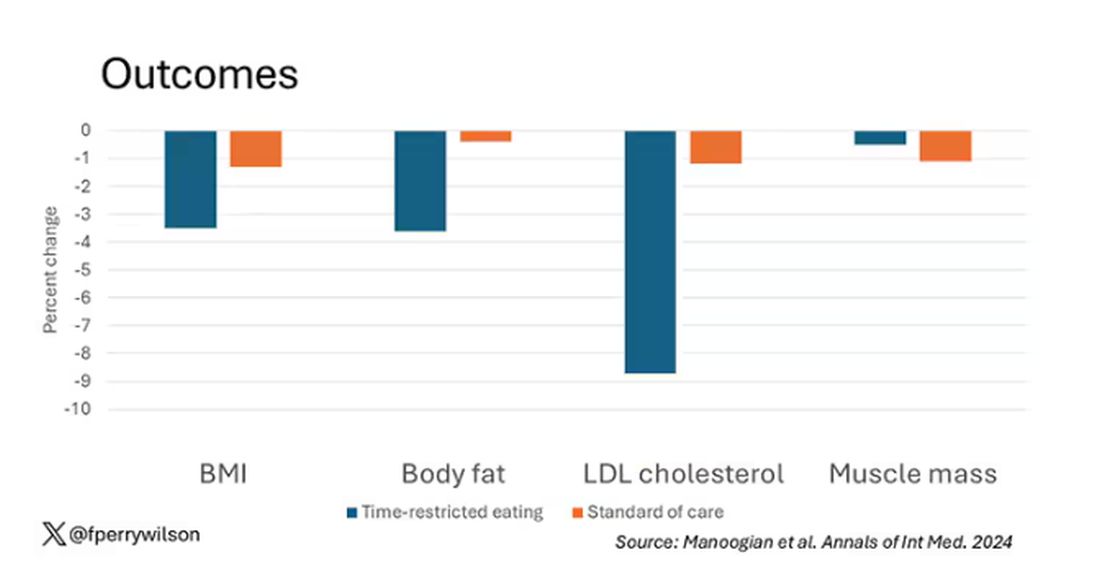
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 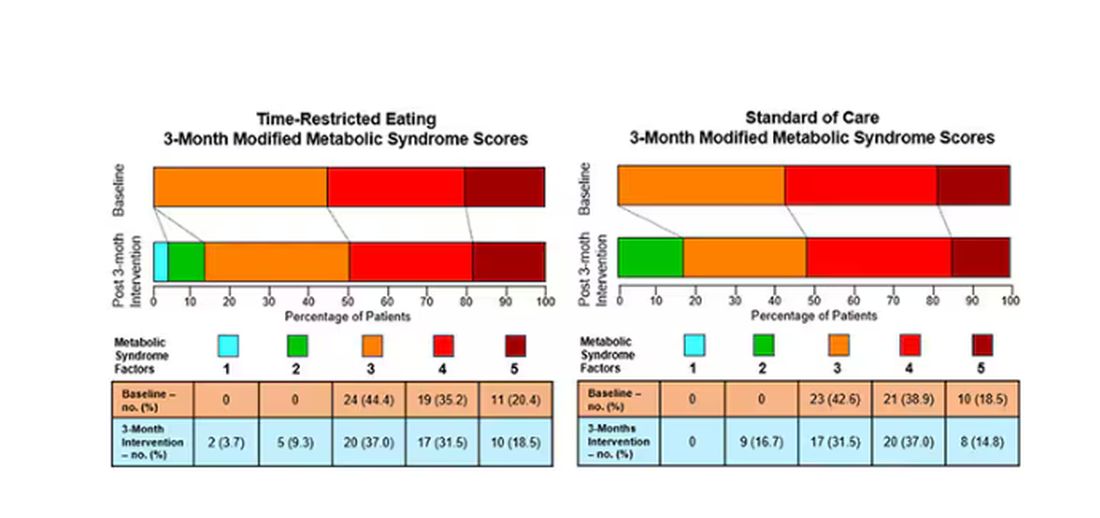
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.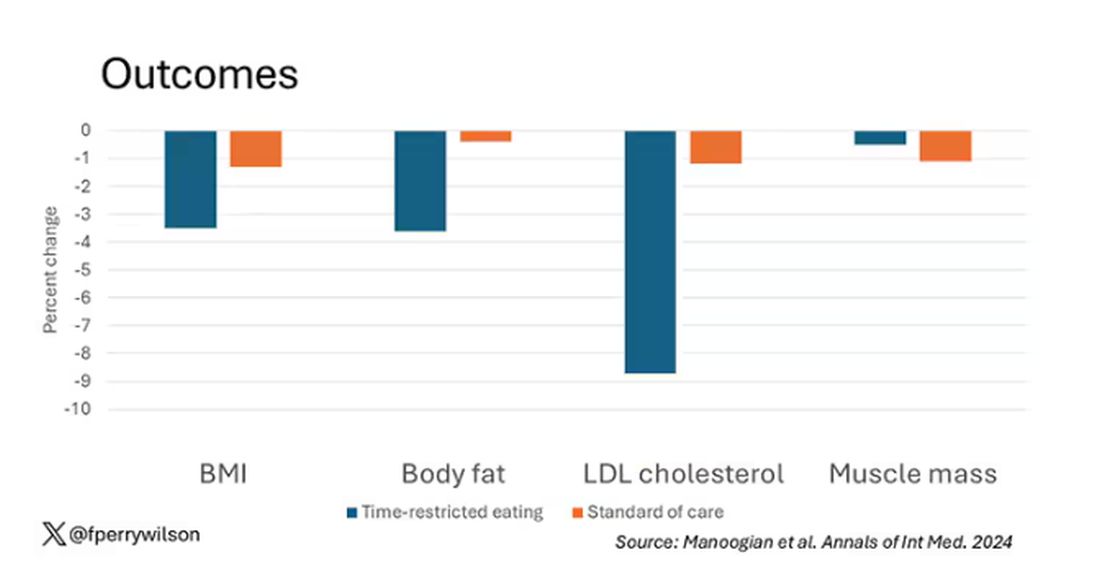
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.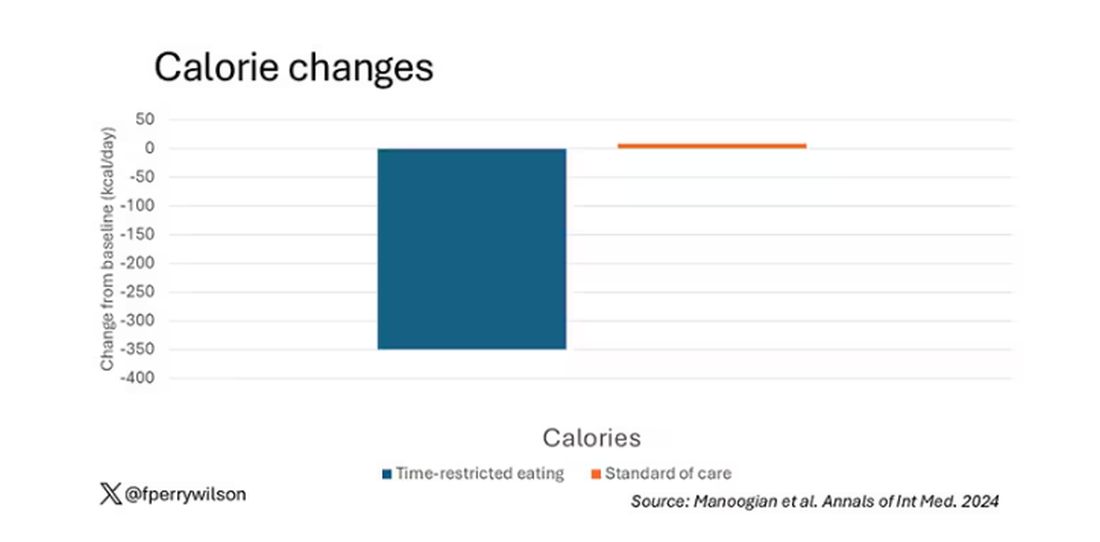
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 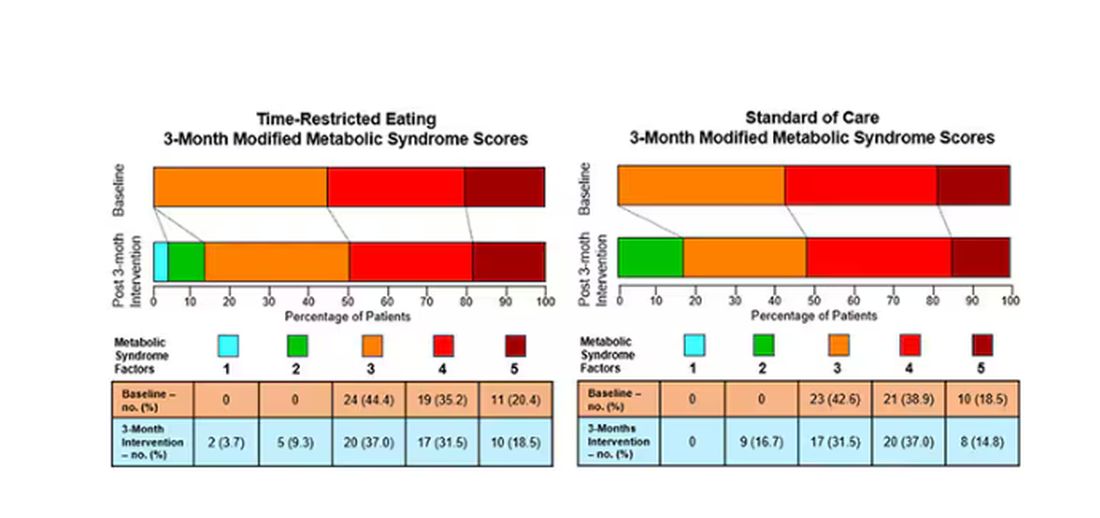
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.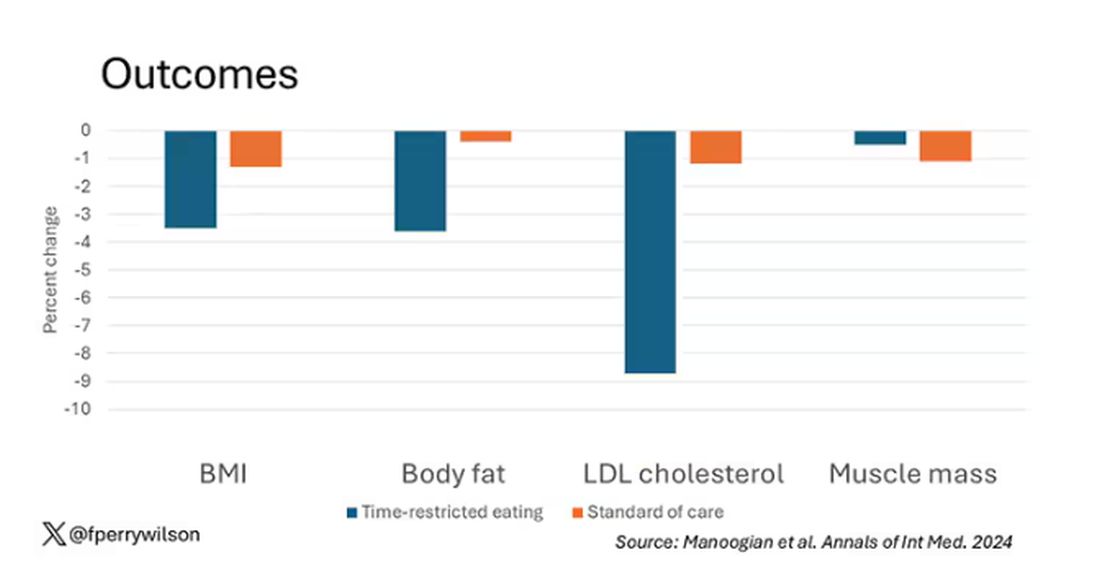
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.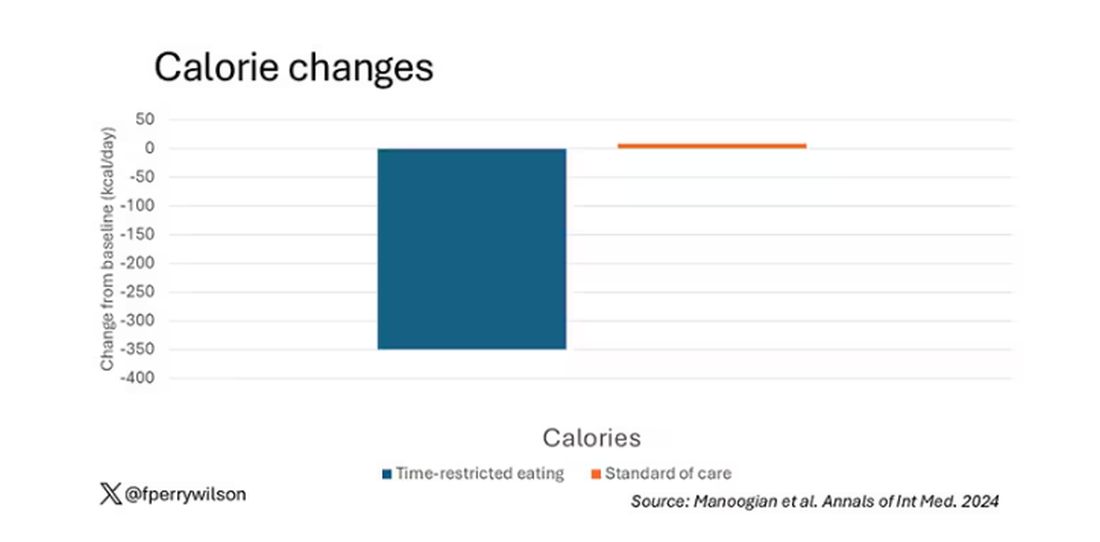
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 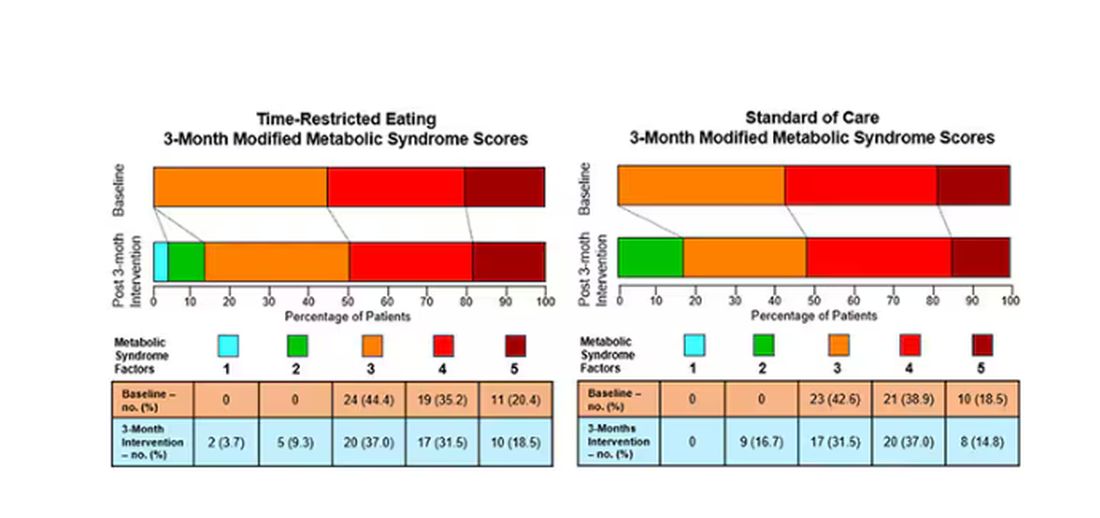
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Detecting Type 2 Diabetes Through Voice: How Does It Work?
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
FROM EASD 2024
Cannabis Use Rising in Diabetes: What Do Endos Need to Know?
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
Hypothyroidism Treatment Does Not Affect Cognitive Decline in Menopausal Women
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
First Patient-Derived Stem Cell Transplant a Success in T1D
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
FROM CELL
Hyperandrogenic PCOS Linked to Lower Pregnancy and Live Birth Rates
TOPLINE:
Women with hyperandrogenic polycystic ovary syndrome (PCOS) have lower pregnancy (29.9%) and live birth rates (20.1%) than those with nonhyperandrogenic PCOS (40.2% and 33.1%, respectively).
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 1376 participants from the PPCOS I and II trials, all meeting National Institutes of Health diagnostic criteria for PCOS.
- Participants were categorized into hyperandrogenic (A and B) and nonhyperandrogenic (D) PCOS phenotypes on the basis of medical interviews, demographics, physical examinations, and laboratory data.
- Outcomes of interest included clinical pregnancy, pregnancy loss, live birth, obstetric complications, and neonatal outcomes.
- Fasting blood samples were analyzed for hormonal assays, and Homeostatic Model Assessment for Insulin Resistance scores were calculated using fasting glucose and insulin values.
TAKEAWAY:
- Participants with hyperandrogenic PCOS had higher body mass index (35.5 ± 8.9 vs 31.9 ± 9.3; P < .001) and fasting insulin levels (21.6 ± 27.7 vs 14.7 ± 15.0 μIU/mL; P < .001) than those with nonhyperandrogenic PCOS.
- Participants with hyperandrogenic PCOS had lower odds of achieving pregnancy (odds ratio [OR], 0.63; 95% CI, 0.44-0.92) and live birth (OR, 0.51; 95% CI, 0.34-0.76) than those with nonhyperandrogenic PCOS.
- No significant differences were found in pregnancy loss rates (23.9% vs 32.3%, P = .06) or neonatal outcomes between the two groups.
- The study lacked the power to detect differences in neonatal outcomes because of the low prevalence of these outcomes.
IN PRACTICE:
“Patients with nonhyperandrogenic PCOS may represent a different disease process with unique morbidities and outcomes and could be counseled differently than hyperandrogenic PCOS,” wrote the authors of the study.
SOURCE:
The study was led by Jessica L. Chan, MD, MSCE, Cedars-Sinai Medical Center in Los Angeles, California. It was published online in Obstetrics & Gynecology.
LIMITATIONS:
The primary limitation of this study was that it is a secondary analysis of previously collected randomized controlled trial data, which may affect the availability of certain information. Additionally, the lower number of participants in the nonhyperandrogenic PCOS group could affect the power of the results. The study was underpowered to detect statistically significant differences in neonatal outcomes because of their low prevalence.
DISCLOSURES:
The study was supported by a grant from the ASRM/NICHD/Duke Clinical Research/Reproductive Scientist Training Program. One coauthor disclosed receiving payments from Celmatix, Ferring Pharmaceuticals, Exeltis, Organon, and Monsanto; another disclosed receiving payments from Ferring Pharmaceuticals. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hyperandrogenic polycystic ovary syndrome (PCOS) have lower pregnancy (29.9%) and live birth rates (20.1%) than those with nonhyperandrogenic PCOS (40.2% and 33.1%, respectively).
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 1376 participants from the PPCOS I and II trials, all meeting National Institutes of Health diagnostic criteria for PCOS.
- Participants were categorized into hyperandrogenic (A and B) and nonhyperandrogenic (D) PCOS phenotypes on the basis of medical interviews, demographics, physical examinations, and laboratory data.
- Outcomes of interest included clinical pregnancy, pregnancy loss, live birth, obstetric complications, and neonatal outcomes.
- Fasting blood samples were analyzed for hormonal assays, and Homeostatic Model Assessment for Insulin Resistance scores were calculated using fasting glucose and insulin values.
TAKEAWAY:
- Participants with hyperandrogenic PCOS had higher body mass index (35.5 ± 8.9 vs 31.9 ± 9.3; P < .001) and fasting insulin levels (21.6 ± 27.7 vs 14.7 ± 15.0 μIU/mL; P < .001) than those with nonhyperandrogenic PCOS.
- Participants with hyperandrogenic PCOS had lower odds of achieving pregnancy (odds ratio [OR], 0.63; 95% CI, 0.44-0.92) and live birth (OR, 0.51; 95% CI, 0.34-0.76) than those with nonhyperandrogenic PCOS.
- No significant differences were found in pregnancy loss rates (23.9% vs 32.3%, P = .06) or neonatal outcomes between the two groups.
- The study lacked the power to detect differences in neonatal outcomes because of the low prevalence of these outcomes.
IN PRACTICE:
“Patients with nonhyperandrogenic PCOS may represent a different disease process with unique morbidities and outcomes and could be counseled differently than hyperandrogenic PCOS,” wrote the authors of the study.
SOURCE:
The study was led by Jessica L. Chan, MD, MSCE, Cedars-Sinai Medical Center in Los Angeles, California. It was published online in Obstetrics & Gynecology.
LIMITATIONS:
The primary limitation of this study was that it is a secondary analysis of previously collected randomized controlled trial data, which may affect the availability of certain information. Additionally, the lower number of participants in the nonhyperandrogenic PCOS group could affect the power of the results. The study was underpowered to detect statistically significant differences in neonatal outcomes because of their low prevalence.
DISCLOSURES:
The study was supported by a grant from the ASRM/NICHD/Duke Clinical Research/Reproductive Scientist Training Program. One coauthor disclosed receiving payments from Celmatix, Ferring Pharmaceuticals, Exeltis, Organon, and Monsanto; another disclosed receiving payments from Ferring Pharmaceuticals. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hyperandrogenic polycystic ovary syndrome (PCOS) have lower pregnancy (29.9%) and live birth rates (20.1%) than those with nonhyperandrogenic PCOS (40.2% and 33.1%, respectively).
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 1376 participants from the PPCOS I and II trials, all meeting National Institutes of Health diagnostic criteria for PCOS.
- Participants were categorized into hyperandrogenic (A and B) and nonhyperandrogenic (D) PCOS phenotypes on the basis of medical interviews, demographics, physical examinations, and laboratory data.
- Outcomes of interest included clinical pregnancy, pregnancy loss, live birth, obstetric complications, and neonatal outcomes.
- Fasting blood samples were analyzed for hormonal assays, and Homeostatic Model Assessment for Insulin Resistance scores were calculated using fasting glucose and insulin values.
TAKEAWAY:
- Participants with hyperandrogenic PCOS had higher body mass index (35.5 ± 8.9 vs 31.9 ± 9.3; P < .001) and fasting insulin levels (21.6 ± 27.7 vs 14.7 ± 15.0 μIU/mL; P < .001) than those with nonhyperandrogenic PCOS.
- Participants with hyperandrogenic PCOS had lower odds of achieving pregnancy (odds ratio [OR], 0.63; 95% CI, 0.44-0.92) and live birth (OR, 0.51; 95% CI, 0.34-0.76) than those with nonhyperandrogenic PCOS.
- No significant differences were found in pregnancy loss rates (23.9% vs 32.3%, P = .06) or neonatal outcomes between the two groups.
- The study lacked the power to detect differences in neonatal outcomes because of the low prevalence of these outcomes.
IN PRACTICE:
“Patients with nonhyperandrogenic PCOS may represent a different disease process with unique morbidities and outcomes and could be counseled differently than hyperandrogenic PCOS,” wrote the authors of the study.
SOURCE:
The study was led by Jessica L. Chan, MD, MSCE, Cedars-Sinai Medical Center in Los Angeles, California. It was published online in Obstetrics & Gynecology.
LIMITATIONS:
The primary limitation of this study was that it is a secondary analysis of previously collected randomized controlled trial data, which may affect the availability of certain information. Additionally, the lower number of participants in the nonhyperandrogenic PCOS group could affect the power of the results. The study was underpowered to detect statistically significant differences in neonatal outcomes because of their low prevalence.
DISCLOSURES:
The study was supported by a grant from the ASRM/NICHD/Duke Clinical Research/Reproductive Scientist Training Program. One coauthor disclosed receiving payments from Celmatix, Ferring Pharmaceuticals, Exeltis, Organon, and Monsanto; another disclosed receiving payments from Ferring Pharmaceuticals. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Doctors Seek Additional Obesity Training in Wake of Obesity Patient Boom
Gitanjali Srivastava, MD, professor of medicine, pediatrics, and surgery, and medical director of obesity medicine at Vanderbilt University School of Medicine in Nashville, Tennessee, was nearly 10 years into practicing pediatric medicine when she graduated from the obesity medicine fellowship at Massachusetts General Hospital in Boston in 2013. “We were the very first sort of fellows to speak of then; there were no standards or curriculum,” she said.
Obesity was already epidemic, but stigma and bias were still pervasive in the medical community and within the public. After graduating, Dr. Srivastava spent months vying for a position with hospital CEOs. She traveled across the country explaining the specialty and its value, going into detail about the budget, business model, space requirement, and revenue potential of obesity medicine.
Today marks a very different era.
Obesity medicine is exploding. Patients are spilling into doctors’ offices looking for obesity treatment. Healthcare systems are seeking out obesity specialists and building metabolic health centers. Next month, another 2115 doctors from primary care, surgery, orthopedics, pediatrics, fertility, endocrinology, and beyond will sit for the 2024 exam. The once niche specialty is quickly becoming intertwined with most of modern medicine.
The Need to Treat
It’s no mystery that the rapid expansion of obesity medicine coincides with the US Food and Drug Administration’s approval of GLP-1 injections. The drugs’ radical weight loss properties have captured headlines and driven up patient demand. Meanwhile, doctors are finally able to offer effective treatment for a disease that affects 40% of US adults.
“We are finally treating it as a chronic disease, not as a lifestyle,” said Marcio Griebeler, MD, director of the obesity medicine fellowship at the Cleveland Clinic. And “I think it’s fulfilling for physicians,” he said.
For so long, the advice for obesity was about lifestyle. Move more, eat less, and harness willpower, “which really is a fallacy,” said Kimberly Gudzune, MD, MPH, an obesity medicine specialist and chief medical officer for the American Board of Obesity Medicine (ABOM) Foundation. For people with obesity, “your brain is operating differently,” she said. “Your body really is set up to work against you.”
Brianna Johnson-Rabbett, MD, medical director of the ABOM, told this news organization that with the advent of GLP-1s, “there’s a clearer recognition that obesity is a disease that needs to be treated like other diseases.” Some of that is thanks to clinical trial data showing that just as with other diseases such as high blood pressure or diabetes, obesity can be treated with medication and it resurges when the medication is stopped, she said.
Doctors don’t have to go looking for patients with obesity, dr. Griebeler added. Now that treatment options exist, they’re showing up in droves at the doctor’s office — all the doctors’ offices. In primary care, endocrinology, surgery, pediatrics — a wide variety of doctors are being asked about obesity drugs, Dr. Griebeler noted.
And while doctors are often just as excited as patients about the potential for treatment, many find themselves under-equipped when it comes to obesity. “More physicians are ... recognizing the value in treating this, and some are realizing, “Oh gosh, I never learned how to do this,” said Dr. Gudzune.
Information Patients Have Been Waiting For
Medical training has traditionally devoted minimal, if any, curriculum to obesity and metabolism. “To be honest, we didn’t really cover this at all in my training,” said Nina Paddu, MD, obesity medicine specialist at Maimonides Medical Center in New York City who finished her training only 2 years ago. “The guidance even in residency was ‘let’s send them to nutrition’ and ‘recommend exercising.’ ”
In addition to the medical education gap, until recently there was a “paucity of robust evidence,” Dr. Srivastava said. Leaders in the field wanted to establish standards and guidelines, but there wasn’t enough strong evidence on obesity and its treatments to build them, she said.
Only in the last 5 years or so has the evidence-based understanding of obesity’s pathophysiology truly accelerated: The brain’s driving roles, its interplay with hormones, and its interactions with other diseases. “We are just at the cusp of understanding all the different factors,” Dr. Gudzune said.
But already endocrinologists, surgeons, fertility specialists, gynecologists, and oncologists, to name a few, see the critical overlap with their own field. “Conditions were once suspected of being intertwined [with obesity], and now we have data to connect them,” Dr. Srivastava said. For example, there’s now data connecting semaglutide to a 20% reduction in cardiovascular events for people with obesity. That’s a game changer for multiple specialties, she told this news organization.
Getting Trained in Obesity Management
The recent uptick in obesity insights and increased patient need has doctors from every career stage seeking additional training.
The ABOM offers two board certification pathways: 60 hours of CME credits or a 12-month fellowship. Both paths require doctors to pass the board’s exam.
Many doctors incorporate the training into their existing practice. The CME credit pathway, especially, is designed to help get doctors up to speed without requiring them to upend their lives for a fellowship.
Dr. Srivastava said that the fellowship is more consuming and immersive. While it’s often younger doctors just out of training who apply to fellowship, every year, “I’m astonished at the number of talented physicians with clinical and research experience who want to immerse themselves in a fellowship experience.”
Some doctors return to their previous specialties after fellowship. But many will go on to take obesity medicine–specific roles or set aside clinic hours for obesity medicine. Their credentials are “really attractive to institutions, especially those looking to open up obesity medicine or weight management programs,” said Dr. Srivastava.
Dr. Paddu, who finished her obesity medicine fellowship this year, said there are a variety of obesity medicine jobs to choose from — far different from Dr. Srivastava’s job search 15 years ago. Dr. Paddu’s new role combines 2 days of primary care with 2 days devoted to obesity medicine and 1 day each week set aside for administrative work so she can build up the hospital’s new metabolic health clinic.
Still Not Enough Obesity Specialists
As with all things, rapid growth requires careful oversight. “Part of the responsibility of the board is to think critically of how the field is growing” and conduct ongoing monitoring, Dr. Gudzune said.
This is also why the board’s credentials are time-limited and must be recertified, Dr. Johnson-Rabbett added.
But even with the rise in certified doctors and obesity medicine positions, the 8263 doctors certified by ABOM are only a tiny fraction of US physicians. As a result, there’s genuine likelihood that many patients seeking GLP-1s or other obesity treatment don’t yet have access to the holistic care they need. Plus, doctors may still not have obesity expertise within their networks.
“The field has grown rapidly, but it’s still such a small field relative to the patient need,” said Dr. Gudzune.
A version of this article appeared on Medscape.com.
Gitanjali Srivastava, MD, professor of medicine, pediatrics, and surgery, and medical director of obesity medicine at Vanderbilt University School of Medicine in Nashville, Tennessee, was nearly 10 years into practicing pediatric medicine when she graduated from the obesity medicine fellowship at Massachusetts General Hospital in Boston in 2013. “We were the very first sort of fellows to speak of then; there were no standards or curriculum,” she said.
Obesity was already epidemic, but stigma and bias were still pervasive in the medical community and within the public. After graduating, Dr. Srivastava spent months vying for a position with hospital CEOs. She traveled across the country explaining the specialty and its value, going into detail about the budget, business model, space requirement, and revenue potential of obesity medicine.
Today marks a very different era.
Obesity medicine is exploding. Patients are spilling into doctors’ offices looking for obesity treatment. Healthcare systems are seeking out obesity specialists and building metabolic health centers. Next month, another 2115 doctors from primary care, surgery, orthopedics, pediatrics, fertility, endocrinology, and beyond will sit for the 2024 exam. The once niche specialty is quickly becoming intertwined with most of modern medicine.
The Need to Treat
It’s no mystery that the rapid expansion of obesity medicine coincides with the US Food and Drug Administration’s approval of GLP-1 injections. The drugs’ radical weight loss properties have captured headlines and driven up patient demand. Meanwhile, doctors are finally able to offer effective treatment for a disease that affects 40% of US adults.
“We are finally treating it as a chronic disease, not as a lifestyle,” said Marcio Griebeler, MD, director of the obesity medicine fellowship at the Cleveland Clinic. And “I think it’s fulfilling for physicians,” he said.
For so long, the advice for obesity was about lifestyle. Move more, eat less, and harness willpower, “which really is a fallacy,” said Kimberly Gudzune, MD, MPH, an obesity medicine specialist and chief medical officer for the American Board of Obesity Medicine (ABOM) Foundation. For people with obesity, “your brain is operating differently,” she said. “Your body really is set up to work against you.”
Brianna Johnson-Rabbett, MD, medical director of the ABOM, told this news organization that with the advent of GLP-1s, “there’s a clearer recognition that obesity is a disease that needs to be treated like other diseases.” Some of that is thanks to clinical trial data showing that just as with other diseases such as high blood pressure or diabetes, obesity can be treated with medication and it resurges when the medication is stopped, she said.
Doctors don’t have to go looking for patients with obesity, dr. Griebeler added. Now that treatment options exist, they’re showing up in droves at the doctor’s office — all the doctors’ offices. In primary care, endocrinology, surgery, pediatrics — a wide variety of doctors are being asked about obesity drugs, Dr. Griebeler noted.
And while doctors are often just as excited as patients about the potential for treatment, many find themselves under-equipped when it comes to obesity. “More physicians are ... recognizing the value in treating this, and some are realizing, “Oh gosh, I never learned how to do this,” said Dr. Gudzune.
Information Patients Have Been Waiting For
Medical training has traditionally devoted minimal, if any, curriculum to obesity and metabolism. “To be honest, we didn’t really cover this at all in my training,” said Nina Paddu, MD, obesity medicine specialist at Maimonides Medical Center in New York City who finished her training only 2 years ago. “The guidance even in residency was ‘let’s send them to nutrition’ and ‘recommend exercising.’ ”
In addition to the medical education gap, until recently there was a “paucity of robust evidence,” Dr. Srivastava said. Leaders in the field wanted to establish standards and guidelines, but there wasn’t enough strong evidence on obesity and its treatments to build them, she said.
Only in the last 5 years or so has the evidence-based understanding of obesity’s pathophysiology truly accelerated: The brain’s driving roles, its interplay with hormones, and its interactions with other diseases. “We are just at the cusp of understanding all the different factors,” Dr. Gudzune said.
But already endocrinologists, surgeons, fertility specialists, gynecologists, and oncologists, to name a few, see the critical overlap with their own field. “Conditions were once suspected of being intertwined [with obesity], and now we have data to connect them,” Dr. Srivastava said. For example, there’s now data connecting semaglutide to a 20% reduction in cardiovascular events for people with obesity. That’s a game changer for multiple specialties, she told this news organization.
Getting Trained in Obesity Management
The recent uptick in obesity insights and increased patient need has doctors from every career stage seeking additional training.
The ABOM offers two board certification pathways: 60 hours of CME credits or a 12-month fellowship. Both paths require doctors to pass the board’s exam.
Many doctors incorporate the training into their existing practice. The CME credit pathway, especially, is designed to help get doctors up to speed without requiring them to upend their lives for a fellowship.
Dr. Srivastava said that the fellowship is more consuming and immersive. While it’s often younger doctors just out of training who apply to fellowship, every year, “I’m astonished at the number of talented physicians with clinical and research experience who want to immerse themselves in a fellowship experience.”
Some doctors return to their previous specialties after fellowship. But many will go on to take obesity medicine–specific roles or set aside clinic hours for obesity medicine. Their credentials are “really attractive to institutions, especially those looking to open up obesity medicine or weight management programs,” said Dr. Srivastava.
Dr. Paddu, who finished her obesity medicine fellowship this year, said there are a variety of obesity medicine jobs to choose from — far different from Dr. Srivastava’s job search 15 years ago. Dr. Paddu’s new role combines 2 days of primary care with 2 days devoted to obesity medicine and 1 day each week set aside for administrative work so she can build up the hospital’s new metabolic health clinic.
Still Not Enough Obesity Specialists
As with all things, rapid growth requires careful oversight. “Part of the responsibility of the board is to think critically of how the field is growing” and conduct ongoing monitoring, Dr. Gudzune said.
This is also why the board’s credentials are time-limited and must be recertified, Dr. Johnson-Rabbett added.
But even with the rise in certified doctors and obesity medicine positions, the 8263 doctors certified by ABOM are only a tiny fraction of US physicians. As a result, there’s genuine likelihood that many patients seeking GLP-1s or other obesity treatment don’t yet have access to the holistic care they need. Plus, doctors may still not have obesity expertise within their networks.
“The field has grown rapidly, but it’s still such a small field relative to the patient need,” said Dr. Gudzune.
A version of this article appeared on Medscape.com.
Gitanjali Srivastava, MD, professor of medicine, pediatrics, and surgery, and medical director of obesity medicine at Vanderbilt University School of Medicine in Nashville, Tennessee, was nearly 10 years into practicing pediatric medicine when she graduated from the obesity medicine fellowship at Massachusetts General Hospital in Boston in 2013. “We were the very first sort of fellows to speak of then; there were no standards or curriculum,” she said.
Obesity was already epidemic, but stigma and bias were still pervasive in the medical community and within the public. After graduating, Dr. Srivastava spent months vying for a position with hospital CEOs. She traveled across the country explaining the specialty and its value, going into detail about the budget, business model, space requirement, and revenue potential of obesity medicine.
Today marks a very different era.
Obesity medicine is exploding. Patients are spilling into doctors’ offices looking for obesity treatment. Healthcare systems are seeking out obesity specialists and building metabolic health centers. Next month, another 2115 doctors from primary care, surgery, orthopedics, pediatrics, fertility, endocrinology, and beyond will sit for the 2024 exam. The once niche specialty is quickly becoming intertwined with most of modern medicine.
The Need to Treat
It’s no mystery that the rapid expansion of obesity medicine coincides with the US Food and Drug Administration’s approval of GLP-1 injections. The drugs’ radical weight loss properties have captured headlines and driven up patient demand. Meanwhile, doctors are finally able to offer effective treatment for a disease that affects 40% of US adults.
“We are finally treating it as a chronic disease, not as a lifestyle,” said Marcio Griebeler, MD, director of the obesity medicine fellowship at the Cleveland Clinic. And “I think it’s fulfilling for physicians,” he said.
For so long, the advice for obesity was about lifestyle. Move more, eat less, and harness willpower, “which really is a fallacy,” said Kimberly Gudzune, MD, MPH, an obesity medicine specialist and chief medical officer for the American Board of Obesity Medicine (ABOM) Foundation. For people with obesity, “your brain is operating differently,” she said. “Your body really is set up to work against you.”
Brianna Johnson-Rabbett, MD, medical director of the ABOM, told this news organization that with the advent of GLP-1s, “there’s a clearer recognition that obesity is a disease that needs to be treated like other diseases.” Some of that is thanks to clinical trial data showing that just as with other diseases such as high blood pressure or diabetes, obesity can be treated with medication and it resurges when the medication is stopped, she said.
Doctors don’t have to go looking for patients with obesity, dr. Griebeler added. Now that treatment options exist, they’re showing up in droves at the doctor’s office — all the doctors’ offices. In primary care, endocrinology, surgery, pediatrics — a wide variety of doctors are being asked about obesity drugs, Dr. Griebeler noted.
And while doctors are often just as excited as patients about the potential for treatment, many find themselves under-equipped when it comes to obesity. “More physicians are ... recognizing the value in treating this, and some are realizing, “Oh gosh, I never learned how to do this,” said Dr. Gudzune.
Information Patients Have Been Waiting For
Medical training has traditionally devoted minimal, if any, curriculum to obesity and metabolism. “To be honest, we didn’t really cover this at all in my training,” said Nina Paddu, MD, obesity medicine specialist at Maimonides Medical Center in New York City who finished her training only 2 years ago. “The guidance even in residency was ‘let’s send them to nutrition’ and ‘recommend exercising.’ ”
In addition to the medical education gap, until recently there was a “paucity of robust evidence,” Dr. Srivastava said. Leaders in the field wanted to establish standards and guidelines, but there wasn’t enough strong evidence on obesity and its treatments to build them, she said.
Only in the last 5 years or so has the evidence-based understanding of obesity’s pathophysiology truly accelerated: The brain’s driving roles, its interplay with hormones, and its interactions with other diseases. “We are just at the cusp of understanding all the different factors,” Dr. Gudzune said.
But already endocrinologists, surgeons, fertility specialists, gynecologists, and oncologists, to name a few, see the critical overlap with their own field. “Conditions were once suspected of being intertwined [with obesity], and now we have data to connect them,” Dr. Srivastava said. For example, there’s now data connecting semaglutide to a 20% reduction in cardiovascular events for people with obesity. That’s a game changer for multiple specialties, she told this news organization.
Getting Trained in Obesity Management
The recent uptick in obesity insights and increased patient need has doctors from every career stage seeking additional training.
The ABOM offers two board certification pathways: 60 hours of CME credits or a 12-month fellowship. Both paths require doctors to pass the board’s exam.
Many doctors incorporate the training into their existing practice. The CME credit pathway, especially, is designed to help get doctors up to speed without requiring them to upend their lives for a fellowship.
Dr. Srivastava said that the fellowship is more consuming and immersive. While it’s often younger doctors just out of training who apply to fellowship, every year, “I’m astonished at the number of talented physicians with clinical and research experience who want to immerse themselves in a fellowship experience.”
Some doctors return to their previous specialties after fellowship. But many will go on to take obesity medicine–specific roles or set aside clinic hours for obesity medicine. Their credentials are “really attractive to institutions, especially those looking to open up obesity medicine or weight management programs,” said Dr. Srivastava.
Dr. Paddu, who finished her obesity medicine fellowship this year, said there are a variety of obesity medicine jobs to choose from — far different from Dr. Srivastava’s job search 15 years ago. Dr. Paddu’s new role combines 2 days of primary care with 2 days devoted to obesity medicine and 1 day each week set aside for administrative work so she can build up the hospital’s new metabolic health clinic.
Still Not Enough Obesity Specialists
As with all things, rapid growth requires careful oversight. “Part of the responsibility of the board is to think critically of how the field is growing” and conduct ongoing monitoring, Dr. Gudzune said.
This is also why the board’s credentials are time-limited and must be recertified, Dr. Johnson-Rabbett added.
But even with the rise in certified doctors and obesity medicine positions, the 8263 doctors certified by ABOM are only a tiny fraction of US physicians. As a result, there’s genuine likelihood that many patients seeking GLP-1s or other obesity treatment don’t yet have access to the holistic care they need. Plus, doctors may still not have obesity expertise within their networks.
“The field has grown rapidly, but it’s still such a small field relative to the patient need,” said Dr. Gudzune.
A version of this article appeared on Medscape.com.
Cannabis Linked to Bulging Eyes in Graves’ Disease
TOPLINE:
Among patients with autoimmune hyperthyroidism, those who use cannabis are 1.9 times more likely to develop exophthalmos — eyes that appear to bulge from the face — within 1 year of diagnosis, than those who do not use the drug. However, the added risk may wane over time.
METHODOLOGY:
- Researchers analyzed data from TriNetX, an electronic health record platform, for more than 36,000 patients with autoimmune hyperthyroidism between 2003 and 2023.
- The dataset included cannabis users (n = 783), nicotine users (n = 17,310), and control individuals (n = 18,093) who did not use either substance.
- Primary outcomes included presentations of thyroid eye disease (TED) and the use of treatments for the condition, such as teprotumumab, steroids, eyelid retraction repair, tarsorrhaphy, strabismus surgery, or orbital decompression.
- The investigators used propensity matching to control for characteristics such as age, sex, race, and prior thyroidectomy or radio ablation.
TAKEAWAY:
- The incidence of exophthalmos at 1 year was 4.1% among nicotine users, 4.1% among cannabis users, and 2.2% among controls.
- Cannabis users were 1.9 times more likely than controls to develop exophthalmos within 1 year (P = .03).
- At 2 years, the researchers identified a trend toward more TED in cannabis users than in controls, but the difference was no longer statistically significant.
- Cannabis users were about 2.5 times more likely than controls to be prescribed steroids throughout the 2-year follow-up period.
IN PRACTICE:
“These findings altogether suggest that cannabis usage may be associated with earlier progression or increased short-term severity of TED symptoms,” the authors of the study wrote. The mechanisms may be like those for cigarette smoking and could include inflammation and vascular congestion, they added.
SOURCE:
The study was conducted by Amanda M. Zong and Anne Barmettler, MD, with Albert Einstein College of Medicine in New York City. It was published online in Ophthalmic Plastic and Reconstructive Surgery.
LIMITATIONS:
The number of cannabis users was relatively small and included only patients who had received a diagnosis of a cannabis-usage disorder prior to the diagnosis of autoimmune hyperthyroidism, the researchers noted. TED lacks a specific International Classification of Diseases–10 code, which necessitated the use of indirect measures. “Furthermore, the mode of administration, duration, and frequency of cannabis and nicotine usage were not available in the dataset used, limiting analysis of degree of association and modifiable risk,” they wrote.
DISCLOSURES:
The researchers disclosed no relevant financial relationships.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Among patients with autoimmune hyperthyroidism, those who use cannabis are 1.9 times more likely to develop exophthalmos — eyes that appear to bulge from the face — within 1 year of diagnosis, than those who do not use the drug. However, the added risk may wane over time.
METHODOLOGY:
- Researchers analyzed data from TriNetX, an electronic health record platform, for more than 36,000 patients with autoimmune hyperthyroidism between 2003 and 2023.
- The dataset included cannabis users (n = 783), nicotine users (n = 17,310), and control individuals (n = 18,093) who did not use either substance.
- Primary outcomes included presentations of thyroid eye disease (TED) and the use of treatments for the condition, such as teprotumumab, steroids, eyelid retraction repair, tarsorrhaphy, strabismus surgery, or orbital decompression.
- The investigators used propensity matching to control for characteristics such as age, sex, race, and prior thyroidectomy or radio ablation.
TAKEAWAY:
- The incidence of exophthalmos at 1 year was 4.1% among nicotine users, 4.1% among cannabis users, and 2.2% among controls.
- Cannabis users were 1.9 times more likely than controls to develop exophthalmos within 1 year (P = .03).
- At 2 years, the researchers identified a trend toward more TED in cannabis users than in controls, but the difference was no longer statistically significant.
- Cannabis users were about 2.5 times more likely than controls to be prescribed steroids throughout the 2-year follow-up period.
IN PRACTICE:
“These findings altogether suggest that cannabis usage may be associated with earlier progression or increased short-term severity of TED symptoms,” the authors of the study wrote. The mechanisms may be like those for cigarette smoking and could include inflammation and vascular congestion, they added.
SOURCE:
The study was conducted by Amanda M. Zong and Anne Barmettler, MD, with Albert Einstein College of Medicine in New York City. It was published online in Ophthalmic Plastic and Reconstructive Surgery.
LIMITATIONS:
The number of cannabis users was relatively small and included only patients who had received a diagnosis of a cannabis-usage disorder prior to the diagnosis of autoimmune hyperthyroidism, the researchers noted. TED lacks a specific International Classification of Diseases–10 code, which necessitated the use of indirect measures. “Furthermore, the mode of administration, duration, and frequency of cannabis and nicotine usage were not available in the dataset used, limiting analysis of degree of association and modifiable risk,” they wrote.
DISCLOSURES:
The researchers disclosed no relevant financial relationships.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Among patients with autoimmune hyperthyroidism, those who use cannabis are 1.9 times more likely to develop exophthalmos — eyes that appear to bulge from the face — within 1 year of diagnosis, than those who do not use the drug. However, the added risk may wane over time.
METHODOLOGY:
- Researchers analyzed data from TriNetX, an electronic health record platform, for more than 36,000 patients with autoimmune hyperthyroidism between 2003 and 2023.
- The dataset included cannabis users (n = 783), nicotine users (n = 17,310), and control individuals (n = 18,093) who did not use either substance.
- Primary outcomes included presentations of thyroid eye disease (TED) and the use of treatments for the condition, such as teprotumumab, steroids, eyelid retraction repair, tarsorrhaphy, strabismus surgery, or orbital decompression.
- The investigators used propensity matching to control for characteristics such as age, sex, race, and prior thyroidectomy or radio ablation.
TAKEAWAY:
- The incidence of exophthalmos at 1 year was 4.1% among nicotine users, 4.1% among cannabis users, and 2.2% among controls.
- Cannabis users were 1.9 times more likely than controls to develop exophthalmos within 1 year (P = .03).
- At 2 years, the researchers identified a trend toward more TED in cannabis users than in controls, but the difference was no longer statistically significant.
- Cannabis users were about 2.5 times more likely than controls to be prescribed steroids throughout the 2-year follow-up period.
IN PRACTICE:
“These findings altogether suggest that cannabis usage may be associated with earlier progression or increased short-term severity of TED symptoms,” the authors of the study wrote. The mechanisms may be like those for cigarette smoking and could include inflammation and vascular congestion, they added.
SOURCE:
The study was conducted by Amanda M. Zong and Anne Barmettler, MD, with Albert Einstein College of Medicine in New York City. It was published online in Ophthalmic Plastic and Reconstructive Surgery.
LIMITATIONS:
The number of cannabis users was relatively small and included only patients who had received a diagnosis of a cannabis-usage disorder prior to the diagnosis of autoimmune hyperthyroidism, the researchers noted. TED lacks a specific International Classification of Diseases–10 code, which necessitated the use of indirect measures. “Furthermore, the mode of administration, duration, and frequency of cannabis and nicotine usage were not available in the dataset used, limiting analysis of degree of association and modifiable risk,” they wrote.
DISCLOSURES:
The researchers disclosed no relevant financial relationships.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Air Travel Alters Insulin Pump Delivery on Takeoff, Landing
MADRID —
This phenomenon is due to air bubble formation and reabsorption in the insulin caused by ambient pressure changes in the airplane’s cabin. It has nothing to do with the pump itself and happens with all insulin pumps, including those in hybrid closed-loop systems, Bruce King, MD, said at the European Association for the Study of Diabetes (EASD) 2024 Annual Meeting.
The extent to which this affects people with diabetes who use insulin pumps depends on their dose and insulin sensitivity among other factors, but all who fly should be aware of the possibility and take precautions, particularly with children, Dr. King, a pediatric endocrinologist at John Hunter Children’s Hospital, Newcastle, Australia, told this news organization.
“Basically, the pumps are very safe in flight, but they deliver a little bit of extra insulin when you go up and stop delivery when you come back down again. There are a couple of simple steps that people can take to make sure that they don’t have problems during the flight,” he said.
Specifically, he advised that for pumps with tubing, wearers can disconnect just prior to takeoff and reconnect when the plane reaches cruising altitude, about 20 minutes into the flight. The insulin will still come out, but it won’t be delivered to the person, Dr. King said.
On descent, they can disconnect after landing and prime the line to remove the insulin deficit.
With the Omnipod, which can’t be disconnected, the only solution is to eat a small snack on takeoff. And on landing, eat another small snack such as a banana, and give a bolus for it to overcome the blockage of insulin delivery.
In any case, Dr. King said, “One of the most important things is informing people with diabetes about this effect so they’re aware of it and can act appropriately when they fly.”
Asked to comment, Nicholas B. Argento, MD, a practicing endocrinologist in Columbia, Maryland, and author of the American Diabetes Association’s book, “Putting Your Patients on the Pump,” called the issue a “minor effect,” adding, “While I think it would be reasonable to make those changes ... it seems like a lot of effort for a difference of 0.6 units extra on ascent and 0.5 units less on descent.”
He noted there is a risk that the individual might forget to reattach the pump after 20 minutes, leading to hyperglycemia and even diabetic ketoacidosis. Instead, “one could put the pump on suspend for 1 hour on ascent. That would not stop the extra insulin but would net less insulin during that time period.”
And after descent, “you have to walk a lot in most cases, so I don’t think they need to take this into consideration. So many other factors change in air travel that I don’t think this is a significant enough effect to make the effort.”
A Known Phenomenon, the Manufacturers Are Aware
This phenomenon has been described previously, including by Dr. King in a 2011 Diabetes Care paper. The new research is among a series of experiments funded by the European Union Aviation Safety Agency in collaboration with the pump manufacturers Medtronic (MiniMed), Tandem (t:slim), and Insulet (Omnipod), primarily aimed at establishing safety parameters for airline pilots with insulin-treated diabetes.
Both the Omnipod DASH and Omnipod 5 User Guides include warnings about unintended insulin delivery during flight, and both advise users to check their blood glucose levels frequently while flying.
In a statement, Jordan Pinsker, MD, Chief Medical Officer at Tandem Diabetes Care, told this news organization, “While it has long been known that routine air travel pressure changes can cause minor fluctuations in insulin pump delivery, the impact of these variations have been found to be generally minor as it relates to glycemic control.”
Dr. Pinsker added that the Tandem Mobi user manual includes a warning related to significant pressure changes in specific air travel situations and offers guidance to disconnect. However, “the t:slim X2 pump’s microdelivery technology limits how much extra insulin can get delivered from air pressure changes due to a mechanism between the tubing and the contents of the bag inside the cartridge.”
Medtronic’s user guide says that the 780G system has not been tested at altitudes higher than 10,150 feet.
Hypobaric Chamber Used to Simulate Flight
The study was conducted in vitro, in a hypobaric chamber designed to mimic atmospheric changes during commercial flight. A total of 10 Medtronic MiniMed 780G, 10 Tandem t:slim X2, and six Insulet Omnipod DASH pumps were tested.
The hypobaric chamber was depressurized to 550 mm Hg over a 20-minute ascent, maintained at a 30-minute cruise, followed by a 20-minute descent to ground (750 mm Hg). During the simulated flights, insulin infusion was set at 0.6 units per hour, a rate typical for both adults and children, to allow accurate measurements with multiple flights.
Insulin delivery rates and bubble formation were recorded by attaching infusion sets to open-ended 100 µL capillary tubes against 1-mm grid paper.
Full cartridges — Medtronic: 3 mL, t:slim: 3 mL, and Omnipod: 2 mL — all over-delivered 0.60 units of insulin over a 20-minute ascent compared with delivery at ground level. And during descent, the cartridges under-delivered 0.51 units of insulin.
But if There’s Rapid Decompression…
In a separate protocol, insulin infusion sets without pumps were tested in a simulation of rapid decompression. Insulin delivery during both ascent and descent showed statistically significant differences compared with delivery at ground level (both P < .001). In this scenario, fluid delivery was equivalent to 5.6 units of excess insulin.
Dr. King pointed out that while these are rare events, about 40-50 occur annually. One was the widely publicized Alaska Airlines flight in January 2024 when the door fell off in midair.
Dr. Argento said, “The catastrophic decompression is of note, and I would want patients to be aware of this, but it is asking a lot for someone thinking they are going to die to remember to disconnect as it starts.”
The researchers are investigating this phenomenon further in people, including airline pilots.
Dr. King’s research group has been involved in research with Medtronic, Tandem, and Insulet. Dr. Argento has consulted or been on advisory boards for Eli Lilly Diabetes, Dexcom, Diabeloop, Convatec, and Senseonics and served on the speakers’ bureaus for Boehringer Ingelheim, Dexcom, Eli Lilly Diabetes, MannKind, Novo Nordisk, Xeris, and Zealand Pharma.
A version of this article appeared on Medscape.com.
MADRID —
This phenomenon is due to air bubble formation and reabsorption in the insulin caused by ambient pressure changes in the airplane’s cabin. It has nothing to do with the pump itself and happens with all insulin pumps, including those in hybrid closed-loop systems, Bruce King, MD, said at the European Association for the Study of Diabetes (EASD) 2024 Annual Meeting.
The extent to which this affects people with diabetes who use insulin pumps depends on their dose and insulin sensitivity among other factors, but all who fly should be aware of the possibility and take precautions, particularly with children, Dr. King, a pediatric endocrinologist at John Hunter Children’s Hospital, Newcastle, Australia, told this news organization.
“Basically, the pumps are very safe in flight, but they deliver a little bit of extra insulin when you go up and stop delivery when you come back down again. There are a couple of simple steps that people can take to make sure that they don’t have problems during the flight,” he said.
Specifically, he advised that for pumps with tubing, wearers can disconnect just prior to takeoff and reconnect when the plane reaches cruising altitude, about 20 minutes into the flight. The insulin will still come out, but it won’t be delivered to the person, Dr. King said.
On descent, they can disconnect after landing and prime the line to remove the insulin deficit.
With the Omnipod, which can’t be disconnected, the only solution is to eat a small snack on takeoff. And on landing, eat another small snack such as a banana, and give a bolus for it to overcome the blockage of insulin delivery.
In any case, Dr. King said, “One of the most important things is informing people with diabetes about this effect so they’re aware of it and can act appropriately when they fly.”
Asked to comment, Nicholas B. Argento, MD, a practicing endocrinologist in Columbia, Maryland, and author of the American Diabetes Association’s book, “Putting Your Patients on the Pump,” called the issue a “minor effect,” adding, “While I think it would be reasonable to make those changes ... it seems like a lot of effort for a difference of 0.6 units extra on ascent and 0.5 units less on descent.”
He noted there is a risk that the individual might forget to reattach the pump after 20 minutes, leading to hyperglycemia and even diabetic ketoacidosis. Instead, “one could put the pump on suspend for 1 hour on ascent. That would not stop the extra insulin but would net less insulin during that time period.”
And after descent, “you have to walk a lot in most cases, so I don’t think they need to take this into consideration. So many other factors change in air travel that I don’t think this is a significant enough effect to make the effort.”
A Known Phenomenon, the Manufacturers Are Aware
This phenomenon has been described previously, including by Dr. King in a 2011 Diabetes Care paper. The new research is among a series of experiments funded by the European Union Aviation Safety Agency in collaboration with the pump manufacturers Medtronic (MiniMed), Tandem (t:slim), and Insulet (Omnipod), primarily aimed at establishing safety parameters for airline pilots with insulin-treated diabetes.
Both the Omnipod DASH and Omnipod 5 User Guides include warnings about unintended insulin delivery during flight, and both advise users to check their blood glucose levels frequently while flying.
In a statement, Jordan Pinsker, MD, Chief Medical Officer at Tandem Diabetes Care, told this news organization, “While it has long been known that routine air travel pressure changes can cause minor fluctuations in insulin pump delivery, the impact of these variations have been found to be generally minor as it relates to glycemic control.”
Dr. Pinsker added that the Tandem Mobi user manual includes a warning related to significant pressure changes in specific air travel situations and offers guidance to disconnect. However, “the t:slim X2 pump’s microdelivery technology limits how much extra insulin can get delivered from air pressure changes due to a mechanism between the tubing and the contents of the bag inside the cartridge.”
Medtronic’s user guide says that the 780G system has not been tested at altitudes higher than 10,150 feet.
Hypobaric Chamber Used to Simulate Flight
The study was conducted in vitro, in a hypobaric chamber designed to mimic atmospheric changes during commercial flight. A total of 10 Medtronic MiniMed 780G, 10 Tandem t:slim X2, and six Insulet Omnipod DASH pumps were tested.
The hypobaric chamber was depressurized to 550 mm Hg over a 20-minute ascent, maintained at a 30-minute cruise, followed by a 20-minute descent to ground (750 mm Hg). During the simulated flights, insulin infusion was set at 0.6 units per hour, a rate typical for both adults and children, to allow accurate measurements with multiple flights.
Insulin delivery rates and bubble formation were recorded by attaching infusion sets to open-ended 100 µL capillary tubes against 1-mm grid paper.
Full cartridges — Medtronic: 3 mL, t:slim: 3 mL, and Omnipod: 2 mL — all over-delivered 0.60 units of insulin over a 20-minute ascent compared with delivery at ground level. And during descent, the cartridges under-delivered 0.51 units of insulin.
But if There’s Rapid Decompression…
In a separate protocol, insulin infusion sets without pumps were tested in a simulation of rapid decompression. Insulin delivery during both ascent and descent showed statistically significant differences compared with delivery at ground level (both P < .001). In this scenario, fluid delivery was equivalent to 5.6 units of excess insulin.
Dr. King pointed out that while these are rare events, about 40-50 occur annually. One was the widely publicized Alaska Airlines flight in January 2024 when the door fell off in midair.
Dr. Argento said, “The catastrophic decompression is of note, and I would want patients to be aware of this, but it is asking a lot for someone thinking they are going to die to remember to disconnect as it starts.”
The researchers are investigating this phenomenon further in people, including airline pilots.
Dr. King’s research group has been involved in research with Medtronic, Tandem, and Insulet. Dr. Argento has consulted or been on advisory boards for Eli Lilly Diabetes, Dexcom, Diabeloop, Convatec, and Senseonics and served on the speakers’ bureaus for Boehringer Ingelheim, Dexcom, Eli Lilly Diabetes, MannKind, Novo Nordisk, Xeris, and Zealand Pharma.
A version of this article appeared on Medscape.com.
MADRID —
This phenomenon is due to air bubble formation and reabsorption in the insulin caused by ambient pressure changes in the airplane’s cabin. It has nothing to do with the pump itself and happens with all insulin pumps, including those in hybrid closed-loop systems, Bruce King, MD, said at the European Association for the Study of Diabetes (EASD) 2024 Annual Meeting.
The extent to which this affects people with diabetes who use insulin pumps depends on their dose and insulin sensitivity among other factors, but all who fly should be aware of the possibility and take precautions, particularly with children, Dr. King, a pediatric endocrinologist at John Hunter Children’s Hospital, Newcastle, Australia, told this news organization.
“Basically, the pumps are very safe in flight, but they deliver a little bit of extra insulin when you go up and stop delivery when you come back down again. There are a couple of simple steps that people can take to make sure that they don’t have problems during the flight,” he said.
Specifically, he advised that for pumps with tubing, wearers can disconnect just prior to takeoff and reconnect when the plane reaches cruising altitude, about 20 minutes into the flight. The insulin will still come out, but it won’t be delivered to the person, Dr. King said.
On descent, they can disconnect after landing and prime the line to remove the insulin deficit.
With the Omnipod, which can’t be disconnected, the only solution is to eat a small snack on takeoff. And on landing, eat another small snack such as a banana, and give a bolus for it to overcome the blockage of insulin delivery.
In any case, Dr. King said, “One of the most important things is informing people with diabetes about this effect so they’re aware of it and can act appropriately when they fly.”
Asked to comment, Nicholas B. Argento, MD, a practicing endocrinologist in Columbia, Maryland, and author of the American Diabetes Association’s book, “Putting Your Patients on the Pump,” called the issue a “minor effect,” adding, “While I think it would be reasonable to make those changes ... it seems like a lot of effort for a difference of 0.6 units extra on ascent and 0.5 units less on descent.”
He noted there is a risk that the individual might forget to reattach the pump after 20 minutes, leading to hyperglycemia and even diabetic ketoacidosis. Instead, “one could put the pump on suspend for 1 hour on ascent. That would not stop the extra insulin but would net less insulin during that time period.”
And after descent, “you have to walk a lot in most cases, so I don’t think they need to take this into consideration. So many other factors change in air travel that I don’t think this is a significant enough effect to make the effort.”
A Known Phenomenon, the Manufacturers Are Aware
This phenomenon has been described previously, including by Dr. King in a 2011 Diabetes Care paper. The new research is among a series of experiments funded by the European Union Aviation Safety Agency in collaboration with the pump manufacturers Medtronic (MiniMed), Tandem (t:slim), and Insulet (Omnipod), primarily aimed at establishing safety parameters for airline pilots with insulin-treated diabetes.
Both the Omnipod DASH and Omnipod 5 User Guides include warnings about unintended insulin delivery during flight, and both advise users to check their blood glucose levels frequently while flying.
In a statement, Jordan Pinsker, MD, Chief Medical Officer at Tandem Diabetes Care, told this news organization, “While it has long been known that routine air travel pressure changes can cause minor fluctuations in insulin pump delivery, the impact of these variations have been found to be generally minor as it relates to glycemic control.”
Dr. Pinsker added that the Tandem Mobi user manual includes a warning related to significant pressure changes in specific air travel situations and offers guidance to disconnect. However, “the t:slim X2 pump’s microdelivery technology limits how much extra insulin can get delivered from air pressure changes due to a mechanism between the tubing and the contents of the bag inside the cartridge.”
Medtronic’s user guide says that the 780G system has not been tested at altitudes higher than 10,150 feet.
Hypobaric Chamber Used to Simulate Flight
The study was conducted in vitro, in a hypobaric chamber designed to mimic atmospheric changes during commercial flight. A total of 10 Medtronic MiniMed 780G, 10 Tandem t:slim X2, and six Insulet Omnipod DASH pumps were tested.
The hypobaric chamber was depressurized to 550 mm Hg over a 20-minute ascent, maintained at a 30-minute cruise, followed by a 20-minute descent to ground (750 mm Hg). During the simulated flights, insulin infusion was set at 0.6 units per hour, a rate typical for both adults and children, to allow accurate measurements with multiple flights.
Insulin delivery rates and bubble formation were recorded by attaching infusion sets to open-ended 100 µL capillary tubes against 1-mm grid paper.
Full cartridges — Medtronic: 3 mL, t:slim: 3 mL, and Omnipod: 2 mL — all over-delivered 0.60 units of insulin over a 20-minute ascent compared with delivery at ground level. And during descent, the cartridges under-delivered 0.51 units of insulin.
But if There’s Rapid Decompression…
In a separate protocol, insulin infusion sets without pumps were tested in a simulation of rapid decompression. Insulin delivery during both ascent and descent showed statistically significant differences compared with delivery at ground level (both P < .001). In this scenario, fluid delivery was equivalent to 5.6 units of excess insulin.
Dr. King pointed out that while these are rare events, about 40-50 occur annually. One was the widely publicized Alaska Airlines flight in January 2024 when the door fell off in midair.
Dr. Argento said, “The catastrophic decompression is of note, and I would want patients to be aware of this, but it is asking a lot for someone thinking they are going to die to remember to disconnect as it starts.”
The researchers are investigating this phenomenon further in people, including airline pilots.
Dr. King’s research group has been involved in research with Medtronic, Tandem, and Insulet. Dr. Argento has consulted or been on advisory boards for Eli Lilly Diabetes, Dexcom, Diabeloop, Convatec, and Senseonics and served on the speakers’ bureaus for Boehringer Ingelheim, Dexcom, Eli Lilly Diabetes, MannKind, Novo Nordisk, Xeris, and Zealand Pharma.
A version of this article appeared on Medscape.com.
FROM EASD 2024
Five Essential Nutrients for Patients on GLP-1s
Fatigue, nausea, acid reflux, muscle loss, and the dreaded “Ozempic face” are side effects from using glucagon-like peptide 1 (GLP-1) receptor agonists (RAs) such as semaglutide or the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA tirzepatide to control blood sugar and promote weight loss.
But what I’ve learned from working with hundreds of patients on these medications, and others, is that most (if not all) of these side effects can be minimized by ensuring proper nutrition.
Setting patients up for success requires dietary education and counseling, along with regular monitoring to determine any nutritional deficiencies. Although adequate intake of all the macro and micronutrients is obviously important,
Protein
My patients are probably sick of hearing me talk about protein, but without the constant reinforcement, many of them wouldn’t consume enough of this macronutrient to maintain their baseline lean body mass. The recommended dietary allowance (RDA) for protein (0.8 g/kg bodyweight) doesn’t cut it, especially for older, obese patients, who need closer to 1.0-1.2 g/kg bodyweight to maintain their muscle mass. For example, for a 250-lb patient, I would recommend 114-136 g protein per day. This is equivalent to roughly 15 oz of cooked animal protein. It’s important to note, though, that individuals with kidney disease must limit their protein intake to 0.6-0.8 g/kg bodyweight per day, to avoid overtaxing their kidneys. In this situation, the benefit of increased protein intake does not outweigh the risk of harming the kidneys.
It’s often challenging for patients with suppressed appetites to even think about eating a large hunk of meat or fish, let alone consume it. Plus, eating more than 3-4 oz of protein in one meal can make some patients extremely uncomfortable, owing to the medication’s effect on gastric emptying. This means that daily protein intake must be spread out over multiple mini-meals.
For patients who need more than 100 g of protein per day, protein powders and premade protein shakes can provide 20-30 g protein to fill in the gaps. Although I always try to promote food first, protein supplements have been game changers for my patients, especially those who find solid food less appealing on the medication, or those who avoid animal protein.
Clinicians should have their patients monitor changes in their lean body mass using a dual-energy x-ray absorptiometry scan or a bioelectrical impedance scale; this can be a helpful tool in assessing whether protein intake is sufficient.
Fiber
Even my most knowledgeable and compliant patients will experience some constipation. Generally speaking, when you eat less, you will have fewer bowel movements. Combine that with delayed gastric emptying and reduced fiber intake, and you have a perfect storm. Many patients are simply not able to get in the recommended 25-35 g fiber per day through food, because fibrous foods are filling. If they are prioritizing the protein in their meal, they will not have enough room for all the vegetables on their plate.
To ensure that patients are getting sufficient fiber, clinicians should push consumption of certain vegetables and fruits, such as carrots, broccoli, Brussels sprouts, raspberries, blackberries, and apples, as well as beans and legumes. (Salads are great, but greens like spinach are not as fibrous as one might think.) If the fruit and veggie intake isn’t up to par, a fiber supplement such as psyllium husk can provide an effective boost.
Vitamin B12
Use of these medications is associated with a reduction in vitamin B12 levels, in part because delayed gastric emptying may affect B12 absorption. Low dietary intake of B12 while on the medications can also be to blame, though. The best food sources are animal proteins, so if possible, patients should prioritize having fish, lean meat, eggs, and dairy daily.
Vegetarians and vegans, who are at an increased risk for deficiency, can incorporate nutritional yeast, an excellent source of vitamin B12, into their daily routine. It is beneficial for patients to get blood work periodically to check on B12 status, because insufficient B12 can contribute to the fatigue patients experience while on the medication.
Calcium
Individuals should have calcium on their radar, because weight loss is associated with a decrease in bone mineral density. Adequate intake of the mineral is crucial for optimal bone health, particularly among postmenopausal women and those who are at risk of developing osteoporosis. The RDA for calcium is 1000-1200 mg/d, which an estimated 50% of obese individuals do not take in.
Although dairy products are well-known for being rich in calcium, there are other great sources. Dark green leafy vegetables, such as cooked collard greens and spinach, provide nearly 300 mg per cup. Tofu and sardines are also calcium powerhouses. Despite the plethora of calcium-rich foods, however, some patients may need a calcium supplement.
Vitamin D
Vitamin D deficiency or insufficiency is common among individuals with obesity, so even before these patients start the medications, supplementation may be warranted. The vitamin’s role in promoting calcium absorption, as well as in bone remodeling, make adequate intake essential for patients experiencing significant weight loss.
Clinicians should emphasize regular consumption of fatty fish, such as salmon, as well as eggs, mushrooms, and vitamin D–fortified milks. But unfortunately, that’s where the list of vitamin D–rich foods ends, so taking a vitamin D supplement will be necessary for many patients.
Regularly monitoring patients on GLP-1 RAs through blood work to check vitamin levels and body composition analysis can be helpful in assessing nutritional status while losing weight. Clinicians can also encourage their patients to work with a registered dietitian who is familiar with these medications, so they can develop optimal eating habits throughout their health journey.
Ms. Hanks, a registered dietitian in New York City, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Fatigue, nausea, acid reflux, muscle loss, and the dreaded “Ozempic face” are side effects from using glucagon-like peptide 1 (GLP-1) receptor agonists (RAs) such as semaglutide or the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA tirzepatide to control blood sugar and promote weight loss.
But what I’ve learned from working with hundreds of patients on these medications, and others, is that most (if not all) of these side effects can be minimized by ensuring proper nutrition.
Setting patients up for success requires dietary education and counseling, along with regular monitoring to determine any nutritional deficiencies. Although adequate intake of all the macro and micronutrients is obviously important,
Protein
My patients are probably sick of hearing me talk about protein, but without the constant reinforcement, many of them wouldn’t consume enough of this macronutrient to maintain their baseline lean body mass. The recommended dietary allowance (RDA) for protein (0.8 g/kg bodyweight) doesn’t cut it, especially for older, obese patients, who need closer to 1.0-1.2 g/kg bodyweight to maintain their muscle mass. For example, for a 250-lb patient, I would recommend 114-136 g protein per day. This is equivalent to roughly 15 oz of cooked animal protein. It’s important to note, though, that individuals with kidney disease must limit their protein intake to 0.6-0.8 g/kg bodyweight per day, to avoid overtaxing their kidneys. In this situation, the benefit of increased protein intake does not outweigh the risk of harming the kidneys.
It’s often challenging for patients with suppressed appetites to even think about eating a large hunk of meat or fish, let alone consume it. Plus, eating more than 3-4 oz of protein in one meal can make some patients extremely uncomfortable, owing to the medication’s effect on gastric emptying. This means that daily protein intake must be spread out over multiple mini-meals.
For patients who need more than 100 g of protein per day, protein powders and premade protein shakes can provide 20-30 g protein to fill in the gaps. Although I always try to promote food first, protein supplements have been game changers for my patients, especially those who find solid food less appealing on the medication, or those who avoid animal protein.
Clinicians should have their patients monitor changes in their lean body mass using a dual-energy x-ray absorptiometry scan or a bioelectrical impedance scale; this can be a helpful tool in assessing whether protein intake is sufficient.
Fiber
Even my most knowledgeable and compliant patients will experience some constipation. Generally speaking, when you eat less, you will have fewer bowel movements. Combine that with delayed gastric emptying and reduced fiber intake, and you have a perfect storm. Many patients are simply not able to get in the recommended 25-35 g fiber per day through food, because fibrous foods are filling. If they are prioritizing the protein in their meal, they will not have enough room for all the vegetables on their plate.
To ensure that patients are getting sufficient fiber, clinicians should push consumption of certain vegetables and fruits, such as carrots, broccoli, Brussels sprouts, raspberries, blackberries, and apples, as well as beans and legumes. (Salads are great, but greens like spinach are not as fibrous as one might think.) If the fruit and veggie intake isn’t up to par, a fiber supplement such as psyllium husk can provide an effective boost.
Vitamin B12
Use of these medications is associated with a reduction in vitamin B12 levels, in part because delayed gastric emptying may affect B12 absorption. Low dietary intake of B12 while on the medications can also be to blame, though. The best food sources are animal proteins, so if possible, patients should prioritize having fish, lean meat, eggs, and dairy daily.
Vegetarians and vegans, who are at an increased risk for deficiency, can incorporate nutritional yeast, an excellent source of vitamin B12, into their daily routine. It is beneficial for patients to get blood work periodically to check on B12 status, because insufficient B12 can contribute to the fatigue patients experience while on the medication.
Calcium
Individuals should have calcium on their radar, because weight loss is associated with a decrease in bone mineral density. Adequate intake of the mineral is crucial for optimal bone health, particularly among postmenopausal women and those who are at risk of developing osteoporosis. The RDA for calcium is 1000-1200 mg/d, which an estimated 50% of obese individuals do not take in.
Although dairy products are well-known for being rich in calcium, there are other great sources. Dark green leafy vegetables, such as cooked collard greens and spinach, provide nearly 300 mg per cup. Tofu and sardines are also calcium powerhouses. Despite the plethora of calcium-rich foods, however, some patients may need a calcium supplement.
Vitamin D
Vitamin D deficiency or insufficiency is common among individuals with obesity, so even before these patients start the medications, supplementation may be warranted. The vitamin’s role in promoting calcium absorption, as well as in bone remodeling, make adequate intake essential for patients experiencing significant weight loss.
Clinicians should emphasize regular consumption of fatty fish, such as salmon, as well as eggs, mushrooms, and vitamin D–fortified milks. But unfortunately, that’s where the list of vitamin D–rich foods ends, so taking a vitamin D supplement will be necessary for many patients.
Regularly monitoring patients on GLP-1 RAs through blood work to check vitamin levels and body composition analysis can be helpful in assessing nutritional status while losing weight. Clinicians can also encourage their patients to work with a registered dietitian who is familiar with these medications, so they can develop optimal eating habits throughout their health journey.
Ms. Hanks, a registered dietitian in New York City, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Fatigue, nausea, acid reflux, muscle loss, and the dreaded “Ozempic face” are side effects from using glucagon-like peptide 1 (GLP-1) receptor agonists (RAs) such as semaglutide or the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA tirzepatide to control blood sugar and promote weight loss.
But what I’ve learned from working with hundreds of patients on these medications, and others, is that most (if not all) of these side effects can be minimized by ensuring proper nutrition.
Setting patients up for success requires dietary education and counseling, along with regular monitoring to determine any nutritional deficiencies. Although adequate intake of all the macro and micronutrients is obviously important,
Protein
My patients are probably sick of hearing me talk about protein, but without the constant reinforcement, many of them wouldn’t consume enough of this macronutrient to maintain their baseline lean body mass. The recommended dietary allowance (RDA) for protein (0.8 g/kg bodyweight) doesn’t cut it, especially for older, obese patients, who need closer to 1.0-1.2 g/kg bodyweight to maintain their muscle mass. For example, for a 250-lb patient, I would recommend 114-136 g protein per day. This is equivalent to roughly 15 oz of cooked animal protein. It’s important to note, though, that individuals with kidney disease must limit their protein intake to 0.6-0.8 g/kg bodyweight per day, to avoid overtaxing their kidneys. In this situation, the benefit of increased protein intake does not outweigh the risk of harming the kidneys.
It’s often challenging for patients with suppressed appetites to even think about eating a large hunk of meat or fish, let alone consume it. Plus, eating more than 3-4 oz of protein in one meal can make some patients extremely uncomfortable, owing to the medication’s effect on gastric emptying. This means that daily protein intake must be spread out over multiple mini-meals.
For patients who need more than 100 g of protein per day, protein powders and premade protein shakes can provide 20-30 g protein to fill in the gaps. Although I always try to promote food first, protein supplements have been game changers for my patients, especially those who find solid food less appealing on the medication, or those who avoid animal protein.
Clinicians should have their patients monitor changes in their lean body mass using a dual-energy x-ray absorptiometry scan or a bioelectrical impedance scale; this can be a helpful tool in assessing whether protein intake is sufficient.
Fiber
Even my most knowledgeable and compliant patients will experience some constipation. Generally speaking, when you eat less, you will have fewer bowel movements. Combine that with delayed gastric emptying and reduced fiber intake, and you have a perfect storm. Many patients are simply not able to get in the recommended 25-35 g fiber per day through food, because fibrous foods are filling. If they are prioritizing the protein in their meal, they will not have enough room for all the vegetables on their plate.
To ensure that patients are getting sufficient fiber, clinicians should push consumption of certain vegetables and fruits, such as carrots, broccoli, Brussels sprouts, raspberries, blackberries, and apples, as well as beans and legumes. (Salads are great, but greens like spinach are not as fibrous as one might think.) If the fruit and veggie intake isn’t up to par, a fiber supplement such as psyllium husk can provide an effective boost.
Vitamin B12
Use of these medications is associated with a reduction in vitamin B12 levels, in part because delayed gastric emptying may affect B12 absorption. Low dietary intake of B12 while on the medications can also be to blame, though. The best food sources are animal proteins, so if possible, patients should prioritize having fish, lean meat, eggs, and dairy daily.
Vegetarians and vegans, who are at an increased risk for deficiency, can incorporate nutritional yeast, an excellent source of vitamin B12, into their daily routine. It is beneficial for patients to get blood work periodically to check on B12 status, because insufficient B12 can contribute to the fatigue patients experience while on the medication.
Calcium
Individuals should have calcium on their radar, because weight loss is associated with a decrease in bone mineral density. Adequate intake of the mineral is crucial for optimal bone health, particularly among postmenopausal women and those who are at risk of developing osteoporosis. The RDA for calcium is 1000-1200 mg/d, which an estimated 50% of obese individuals do not take in.
Although dairy products are well-known for being rich in calcium, there are other great sources. Dark green leafy vegetables, such as cooked collard greens and spinach, provide nearly 300 mg per cup. Tofu and sardines are also calcium powerhouses. Despite the plethora of calcium-rich foods, however, some patients may need a calcium supplement.
Vitamin D
Vitamin D deficiency or insufficiency is common among individuals with obesity, so even before these patients start the medications, supplementation may be warranted. The vitamin’s role in promoting calcium absorption, as well as in bone remodeling, make adequate intake essential for patients experiencing significant weight loss.
Clinicians should emphasize regular consumption of fatty fish, such as salmon, as well as eggs, mushrooms, and vitamin D–fortified milks. But unfortunately, that’s where the list of vitamin D–rich foods ends, so taking a vitamin D supplement will be necessary for many patients.
Regularly monitoring patients on GLP-1 RAs through blood work to check vitamin levels and body composition analysis can be helpful in assessing nutritional status while losing weight. Clinicians can also encourage their patients to work with a registered dietitian who is familiar with these medications, so they can develop optimal eating habits throughout their health journey.
Ms. Hanks, a registered dietitian in New York City, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.