User login
Gastric Bypass Benefits Persist at 6 Years' Follow-Up
Both weight loss and its associated improvements in cardiovascular and metabolic risk factors persisted for 6 years in most of the 418 severely obese adults who underwent Roux-en-Y gastric bypass surgery in a prospective study published in the Sept. 19 JAMA.
Despite some weight regain over time, surgery patients showed a mean weight loss of 28% at 6-year follow-up, as well as higher remission rates for diabetes, dyslipidemia, and hypertension, compared with the two control groups, said Ted D. Adams, Ph.D., of the department of internal medicine, University of Utah, Salt Lake City, and his associates.
"Considering the 5%-9% weight loss at 1 year with only 2%-6% weight loss after 4 years of intensive lifestyle-based and medication-based therapy, the weight-loss maintenance of 28% ... in our Utah study is quite significant," they noted.
The study involved severely obese adults with a body mass index of 35 kg/m2 or higher (mean BMI 45.9 kg/m2), of whom 82% were women and 96% were white. In addition to the patients who underwent either open or laparoscopic gastric bypass, there were 417 obese subjects in the first control group who were assessed for the surgery at the same time as the intervention group but did not have the surgery, and 321 obese subjects in the second control group who were randomly selected from a population-based sample of Utah residents.
Subjects in the control groups did not receive any weight-loss intervention as part of the study but were free to pursue it on their own. Over time, 101 of the subjects from both control groups chose to have bariatric surgery.
In the surgical group, mean weight loss was 35% at 2 years and 28% at 6 years, representing a 7% regain over time. By comparison, neither control group showed any significant weight loss or regain.
Diabetes remitted in 75% of the bypass group at 2 years, decreasing to 62% at 6 years. Despite the recurrence of diabetes in some patients, this long-term remission rate was dramatically better than the remission rates in the control groups (8% and 6%, respectively).
Similarly, the proportion of bypass patients who developed index diabetes during follow-up was markedly lower in the bypass group (2%) than in either control group (17% and 15%, respectively).
Remission of hypertension also was greater 6 years after bypass surgery (42%) than in the control groups (18% and 9%, respectively). Rates of high LDL cholesterol and triglycerides followed the same pattern, Dr. Adams and his colleagues wrote (JAMA 2012;308:1122-31).
Importantly, the weight loss and the concurrent improvement in cardiovascular and metabolic risk factors did not improve mortality. There were 29 deaths: 12 in the bypass group (3%); 14 in the first control group (3%); and 3 in the second control group (1%).
Notably, suicide was significantly more common in the bypass patients than in the control subjects. There were four suicides and three poisonings "of undetermined intention" overall, and six of these seven events occurred in bypass patients. The reason for this excess in the surgery group is unknown, but it is consistent with the finding that the mental component of the SF-36 fails to improve during follow-up, even though the physical component improves markedly among gastric bypass patients.
Other investigators have postulated that bariatric surgery precipitates profound changes "that may generate tension and pose special social, psychological, and lifestyle challenges. Preoperative and postoperative psychological assessment of social and emotional status related to post–bariatric surgical expectations and the potential risk of self-destructive behavior might be warranted," Dr. Adams and his associates said.
The rate of perioperative complications was 3% in the surgery group, and there were 38 hospitalizations for bypass-related indications.
This study was supported by the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Center for Research Resources. Dr. Adams’s associates reported ties to Vivus, Orexigen, GlaxoSmithKline, Health Outcome Solutions, and Ethicon Endo-Surgery.
Dr. Adams and his associates show that, despite some weight regain and some recurrence of diabetes, "the control of comorbid conditions remained very good" several years after severely obese patients underwent gastric bypass surgery, said Dr. Anita P. Courcoulas.
Most weight-loss studies are limited by very high dropout rates, so it was remarkable that follow-up was 96% in the intervention group in this study. "These findings are important because they show in a Roux-en-Y cohort and control group with nearly complete follow-up at 6 years that weight loss and associated health benefits ... are durable," she noted.
Anita P. Courcoulas, M.D., is in the department of minimally invasive bariatric and general surgery at the University of Pittsburgh Medical Center. She reported ties to Ethicon, Endogastric Solutions, Pfizer, Allergan, Stryker Endoscopy, Covidien, and Nutrisystem. These remarks were taken from her editorial comment accompanying the report (JAMA 2012;308:1160-1).
Dr. Adams and his associates show that, despite some weight regain and some recurrence of diabetes, "the control of comorbid conditions remained very good" several years after severely obese patients underwent gastric bypass surgery, said Dr. Anita P. Courcoulas.
Most weight-loss studies are limited by very high dropout rates, so it was remarkable that follow-up was 96% in the intervention group in this study. "These findings are important because they show in a Roux-en-Y cohort and control group with nearly complete follow-up at 6 years that weight loss and associated health benefits ... are durable," she noted.
Anita P. Courcoulas, M.D., is in the department of minimally invasive bariatric and general surgery at the University of Pittsburgh Medical Center. She reported ties to Ethicon, Endogastric Solutions, Pfizer, Allergan, Stryker Endoscopy, Covidien, and Nutrisystem. These remarks were taken from her editorial comment accompanying the report (JAMA 2012;308:1160-1).
Dr. Adams and his associates show that, despite some weight regain and some recurrence of diabetes, "the control of comorbid conditions remained very good" several years after severely obese patients underwent gastric bypass surgery, said Dr. Anita P. Courcoulas.
Most weight-loss studies are limited by very high dropout rates, so it was remarkable that follow-up was 96% in the intervention group in this study. "These findings are important because they show in a Roux-en-Y cohort and control group with nearly complete follow-up at 6 years that weight loss and associated health benefits ... are durable," she noted.
Anita P. Courcoulas, M.D., is in the department of minimally invasive bariatric and general surgery at the University of Pittsburgh Medical Center. She reported ties to Ethicon, Endogastric Solutions, Pfizer, Allergan, Stryker Endoscopy, Covidien, and Nutrisystem. These remarks were taken from her editorial comment accompanying the report (JAMA 2012;308:1160-1).
Both weight loss and its associated improvements in cardiovascular and metabolic risk factors persisted for 6 years in most of the 418 severely obese adults who underwent Roux-en-Y gastric bypass surgery in a prospective study published in the Sept. 19 JAMA.
Despite some weight regain over time, surgery patients showed a mean weight loss of 28% at 6-year follow-up, as well as higher remission rates for diabetes, dyslipidemia, and hypertension, compared with the two control groups, said Ted D. Adams, Ph.D., of the department of internal medicine, University of Utah, Salt Lake City, and his associates.
"Considering the 5%-9% weight loss at 1 year with only 2%-6% weight loss after 4 years of intensive lifestyle-based and medication-based therapy, the weight-loss maintenance of 28% ... in our Utah study is quite significant," they noted.
The study involved severely obese adults with a body mass index of 35 kg/m2 or higher (mean BMI 45.9 kg/m2), of whom 82% were women and 96% were white. In addition to the patients who underwent either open or laparoscopic gastric bypass, there were 417 obese subjects in the first control group who were assessed for the surgery at the same time as the intervention group but did not have the surgery, and 321 obese subjects in the second control group who were randomly selected from a population-based sample of Utah residents.
Subjects in the control groups did not receive any weight-loss intervention as part of the study but were free to pursue it on their own. Over time, 101 of the subjects from both control groups chose to have bariatric surgery.
In the surgical group, mean weight loss was 35% at 2 years and 28% at 6 years, representing a 7% regain over time. By comparison, neither control group showed any significant weight loss or regain.
Diabetes remitted in 75% of the bypass group at 2 years, decreasing to 62% at 6 years. Despite the recurrence of diabetes in some patients, this long-term remission rate was dramatically better than the remission rates in the control groups (8% and 6%, respectively).
Similarly, the proportion of bypass patients who developed index diabetes during follow-up was markedly lower in the bypass group (2%) than in either control group (17% and 15%, respectively).
Remission of hypertension also was greater 6 years after bypass surgery (42%) than in the control groups (18% and 9%, respectively). Rates of high LDL cholesterol and triglycerides followed the same pattern, Dr. Adams and his colleagues wrote (JAMA 2012;308:1122-31).
Importantly, the weight loss and the concurrent improvement in cardiovascular and metabolic risk factors did not improve mortality. There were 29 deaths: 12 in the bypass group (3%); 14 in the first control group (3%); and 3 in the second control group (1%).
Notably, suicide was significantly more common in the bypass patients than in the control subjects. There were four suicides and three poisonings "of undetermined intention" overall, and six of these seven events occurred in bypass patients. The reason for this excess in the surgery group is unknown, but it is consistent with the finding that the mental component of the SF-36 fails to improve during follow-up, even though the physical component improves markedly among gastric bypass patients.
Other investigators have postulated that bariatric surgery precipitates profound changes "that may generate tension and pose special social, psychological, and lifestyle challenges. Preoperative and postoperative psychological assessment of social and emotional status related to post–bariatric surgical expectations and the potential risk of self-destructive behavior might be warranted," Dr. Adams and his associates said.
The rate of perioperative complications was 3% in the surgery group, and there were 38 hospitalizations for bypass-related indications.
This study was supported by the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Center for Research Resources. Dr. Adams’s associates reported ties to Vivus, Orexigen, GlaxoSmithKline, Health Outcome Solutions, and Ethicon Endo-Surgery.
Both weight loss and its associated improvements in cardiovascular and metabolic risk factors persisted for 6 years in most of the 418 severely obese adults who underwent Roux-en-Y gastric bypass surgery in a prospective study published in the Sept. 19 JAMA.
Despite some weight regain over time, surgery patients showed a mean weight loss of 28% at 6-year follow-up, as well as higher remission rates for diabetes, dyslipidemia, and hypertension, compared with the two control groups, said Ted D. Adams, Ph.D., of the department of internal medicine, University of Utah, Salt Lake City, and his associates.
"Considering the 5%-9% weight loss at 1 year with only 2%-6% weight loss after 4 years of intensive lifestyle-based and medication-based therapy, the weight-loss maintenance of 28% ... in our Utah study is quite significant," they noted.
The study involved severely obese adults with a body mass index of 35 kg/m2 or higher (mean BMI 45.9 kg/m2), of whom 82% were women and 96% were white. In addition to the patients who underwent either open or laparoscopic gastric bypass, there were 417 obese subjects in the first control group who were assessed for the surgery at the same time as the intervention group but did not have the surgery, and 321 obese subjects in the second control group who were randomly selected from a population-based sample of Utah residents.
Subjects in the control groups did not receive any weight-loss intervention as part of the study but were free to pursue it on their own. Over time, 101 of the subjects from both control groups chose to have bariatric surgery.
In the surgical group, mean weight loss was 35% at 2 years and 28% at 6 years, representing a 7% regain over time. By comparison, neither control group showed any significant weight loss or regain.
Diabetes remitted in 75% of the bypass group at 2 years, decreasing to 62% at 6 years. Despite the recurrence of diabetes in some patients, this long-term remission rate was dramatically better than the remission rates in the control groups (8% and 6%, respectively).
Similarly, the proportion of bypass patients who developed index diabetes during follow-up was markedly lower in the bypass group (2%) than in either control group (17% and 15%, respectively).
Remission of hypertension also was greater 6 years after bypass surgery (42%) than in the control groups (18% and 9%, respectively). Rates of high LDL cholesterol and triglycerides followed the same pattern, Dr. Adams and his colleagues wrote (JAMA 2012;308:1122-31).
Importantly, the weight loss and the concurrent improvement in cardiovascular and metabolic risk factors did not improve mortality. There were 29 deaths: 12 in the bypass group (3%); 14 in the first control group (3%); and 3 in the second control group (1%).
Notably, suicide was significantly more common in the bypass patients than in the control subjects. There were four suicides and three poisonings "of undetermined intention" overall, and six of these seven events occurred in bypass patients. The reason for this excess in the surgery group is unknown, but it is consistent with the finding that the mental component of the SF-36 fails to improve during follow-up, even though the physical component improves markedly among gastric bypass patients.
Other investigators have postulated that bariatric surgery precipitates profound changes "that may generate tension and pose special social, psychological, and lifestyle challenges. Preoperative and postoperative psychological assessment of social and emotional status related to post–bariatric surgical expectations and the potential risk of self-destructive behavior might be warranted," Dr. Adams and his associates said.
The rate of perioperative complications was 3% in the surgery group, and there were 38 hospitalizations for bypass-related indications.
This study was supported by the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Center for Research Resources. Dr. Adams’s associates reported ties to Vivus, Orexigen, GlaxoSmithKline, Health Outcome Solutions, and Ethicon Endo-Surgery.
FROM JAMA
Major Finding: Six years after undergoing gastric bypass, patients showed a mean weight loss of 28%, a diabetes remission rate of 62%, a hypertension remission rate of 42%, and improved lipid profiles.
Data Source: A prospective case-control study involving 1,156 severely obese adults, comparing outcomes at long-term follow-up between 418 who had undergone Roux-en-Y gastric bypass and 738 who had not.
Disclosures: This study was supported by the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Center for Research Resources. Dr. Adams’s associates reported ties to Vivus, Orexigen, GlaxoSmithKline, Health Outcome Solutions, and Ethicon Endo-Surgery.
Withholding Warfarin After GI Bleed Raises Risk of Thrombosis, Death
Deciding not to resume warfarin therapy after an episode of gastrointestinal bleeding raises the risk of thrombosis by a factor of 10 and the risk of death threefold, according to a retrospective cohort study published online September 17 in Archives of Internal Medicine.
"For many patients who have experienced gastrointestinal bleeding, the benefits of resuming warfarin therapy will outweigh the risks," said Daniel M. Witt, Pharm.D., of the clinical pharmacy anticoagulation service at Kaiser Permanente of Colorado, Aurora, and his associates.
"Surprisingly little is known about warfarin therapy and resumption" following a GI bleed, and there is no consensus as to the optimal timing or the risks of restarting anticoagulation. Dr. Witt and his colleagues used Kaiser’s administrative and clinical databases to study the incidence of thrombosis, recurrent bleeding episodes, and death from any cause in 442 adults who presented to a hospital or emergency department with warfarin-associated GI bleeding in 2005-2009 and who were followed for 90 days.
The mean patient age was 74 years, and the study population was equally comprised of men and women. Half of the study subjects were taking warfarin to prevent atrial fibrillation–related stroke or systemic embolization. One-quarter of patients used it to treat or prevent a second venous thrombosis, 10% were on it to prevent thromboembolic complications from prosthetic heart valves, and the remainder took it for other indications.
After an index GI bleed, 260 patients (59%) resumed warfarin therapy, usually within a week. The median time to resumption of warfarin was 4 days. In 41 of these patients, warfarin therapy was never suspended. It was suspended and never resumed in the remaining 182 patients.
During the 90-day follow-up, 11 patients (2.5%) had a thrombotic event. There were six arterial events, including five strokes and one systemic embolus, and five venous events, including three pulmonary embolisms and two deep vein thromboses (DVTs).
The rate of thrombotic events was 0.4% among the patients who resumed warfarin therapy (one DVT), compared with 5.5% among those who did not resume warfarin (five strokes, one systemic embolus, three pulmonary embolisms, and one DVT), a significant difference, the investigators said (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.5261]).
"Patients who either never interrupted warfarin therapy or resumed therapy within 14 days of the index GI bleed experienced no thromboses," they added.
GI bleeding recurred in 36 patients (8.4%) overall. A numerically higher proportion of patients who resumed warfarin therapy had recurrent GI bleeding (10%) than those who did not resume warfarin (5.5%), but this difference was not statistically significant.
In addition, a multivariable analysis that accounted for numerous possible confounders – including patient age, sex, propensity for complications; the INR at admission; acute treatment for the GI bleed; and location of GI bleed – also showed that the risk for rebleeding was not significantly greater in patients who resumed warfarin therapy than in those who did not.
Moreover, recurrent GI bleeding was never fatal. Fatal strokes did occur, however, in three patients with atrial fibrillation whose warfarin therapy was withdrawn and never resumed, Dr. Witt and his associates said.
A total of 52 patients (12%) died during follow-up. The most common cause of death was related to malignancy (29% of deaths), infection (19% of deaths), or cardiac disease (17%).
Resumption of warfarin therapy was strongly associated with a threefold decrease in the risk of death from any cause.
The investigators also performed a post hoc analysis excluding all patients who died within 1 week of the index GI bleed to rule out those who may not have had an opportunity to resume warfarin therapy. In this analysis, the strong association between resumption of warfarin and decreased mortality persisted.
Mortality was lowest among patients who resumed warfarin therapy within 15-90 days of the index GI bleed, the researchers said.
"Our results provide some guidance regarding the optimal timing of warfarin therapy resumption following GI bleeding, but clinical judgment remains a critical factor in this difficult decision," they noted.
This study was funded by CSL Behring. Dr. Witt’s associates, but not Dr. Witt, reported ties to numerous industry sources.
This study provides high-quality, real-world data showing that the risk of recurrent bleeding was acceptably low (10%), none of the episodes of recurrence were fatal, and most physicians and patients were willing to resume anticoagulation soon after GI bleeding, said Dr. Daniel J. Brotman and Dr. Amir K. Jaffer.
Dr. Amir K. Jaffer |
"We would hesitate to continue concurrent antiplatelet therapy in these patients without a compelling indication to do so (such as a recent coronary stent), and also would caution against extrapolating these findings to newer anticoagulants, such as dabigatran and rivaroxaban, that may be associated with more GI bleeding than warfarin when used long term and whose effects are not easily reversed," they said.
Dr. Brotman is with the hospitalist program at Johns Hopkins Hospital, Baltimore. Dr. Jaffer is with the division of hospital medicine at the University of Miami. Dr. Brotman reported ties to Gerson Lehrman Group, the Dunn Group, Quantia Communications, Siemens Healthcare Diagnostics, and Amerigroup Corporation. Dr. Jaffer reported ties to Sanofi-Aventis, Boehringer Ingelheim, Bristol Myers Squibb, Janssen Pharmaceuticals, Canyon Pharmaceuticals, and CSL. These remarks were taken from their invited commentary accompanying Dr. Witt’s report (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.4309]).
This study provides high-quality, real-world data showing that the risk of recurrent bleeding was acceptably low (10%), none of the episodes of recurrence were fatal, and most physicians and patients were willing to resume anticoagulation soon after GI bleeding, said Dr. Daniel J. Brotman and Dr. Amir K. Jaffer.
Dr. Amir K. Jaffer |
"We would hesitate to continue concurrent antiplatelet therapy in these patients without a compelling indication to do so (such as a recent coronary stent), and also would caution against extrapolating these findings to newer anticoagulants, such as dabigatran and rivaroxaban, that may be associated with more GI bleeding than warfarin when used long term and whose effects are not easily reversed," they said.
Dr. Brotman is with the hospitalist program at Johns Hopkins Hospital, Baltimore. Dr. Jaffer is with the division of hospital medicine at the University of Miami. Dr. Brotman reported ties to Gerson Lehrman Group, the Dunn Group, Quantia Communications, Siemens Healthcare Diagnostics, and Amerigroup Corporation. Dr. Jaffer reported ties to Sanofi-Aventis, Boehringer Ingelheim, Bristol Myers Squibb, Janssen Pharmaceuticals, Canyon Pharmaceuticals, and CSL. These remarks were taken from their invited commentary accompanying Dr. Witt’s report (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.4309]).
This study provides high-quality, real-world data showing that the risk of recurrent bleeding was acceptably low (10%), none of the episodes of recurrence were fatal, and most physicians and patients were willing to resume anticoagulation soon after GI bleeding, said Dr. Daniel J. Brotman and Dr. Amir K. Jaffer.
Dr. Amir K. Jaffer |
"We would hesitate to continue concurrent antiplatelet therapy in these patients without a compelling indication to do so (such as a recent coronary stent), and also would caution against extrapolating these findings to newer anticoagulants, such as dabigatran and rivaroxaban, that may be associated with more GI bleeding than warfarin when used long term and whose effects are not easily reversed," they said.
Dr. Brotman is with the hospitalist program at Johns Hopkins Hospital, Baltimore. Dr. Jaffer is with the division of hospital medicine at the University of Miami. Dr. Brotman reported ties to Gerson Lehrman Group, the Dunn Group, Quantia Communications, Siemens Healthcare Diagnostics, and Amerigroup Corporation. Dr. Jaffer reported ties to Sanofi-Aventis, Boehringer Ingelheim, Bristol Myers Squibb, Janssen Pharmaceuticals, Canyon Pharmaceuticals, and CSL. These remarks were taken from their invited commentary accompanying Dr. Witt’s report (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.4309]).
Deciding not to resume warfarin therapy after an episode of gastrointestinal bleeding raises the risk of thrombosis by a factor of 10 and the risk of death threefold, according to a retrospective cohort study published online September 17 in Archives of Internal Medicine.
"For many patients who have experienced gastrointestinal bleeding, the benefits of resuming warfarin therapy will outweigh the risks," said Daniel M. Witt, Pharm.D., of the clinical pharmacy anticoagulation service at Kaiser Permanente of Colorado, Aurora, and his associates.
"Surprisingly little is known about warfarin therapy and resumption" following a GI bleed, and there is no consensus as to the optimal timing or the risks of restarting anticoagulation. Dr. Witt and his colleagues used Kaiser’s administrative and clinical databases to study the incidence of thrombosis, recurrent bleeding episodes, and death from any cause in 442 adults who presented to a hospital or emergency department with warfarin-associated GI bleeding in 2005-2009 and who were followed for 90 days.
The mean patient age was 74 years, and the study population was equally comprised of men and women. Half of the study subjects were taking warfarin to prevent atrial fibrillation–related stroke or systemic embolization. One-quarter of patients used it to treat or prevent a second venous thrombosis, 10% were on it to prevent thromboembolic complications from prosthetic heart valves, and the remainder took it for other indications.
After an index GI bleed, 260 patients (59%) resumed warfarin therapy, usually within a week. The median time to resumption of warfarin was 4 days. In 41 of these patients, warfarin therapy was never suspended. It was suspended and never resumed in the remaining 182 patients.
During the 90-day follow-up, 11 patients (2.5%) had a thrombotic event. There were six arterial events, including five strokes and one systemic embolus, and five venous events, including three pulmonary embolisms and two deep vein thromboses (DVTs).
The rate of thrombotic events was 0.4% among the patients who resumed warfarin therapy (one DVT), compared with 5.5% among those who did not resume warfarin (five strokes, one systemic embolus, three pulmonary embolisms, and one DVT), a significant difference, the investigators said (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.5261]).
"Patients who either never interrupted warfarin therapy or resumed therapy within 14 days of the index GI bleed experienced no thromboses," they added.
GI bleeding recurred in 36 patients (8.4%) overall. A numerically higher proportion of patients who resumed warfarin therapy had recurrent GI bleeding (10%) than those who did not resume warfarin (5.5%), but this difference was not statistically significant.
In addition, a multivariable analysis that accounted for numerous possible confounders – including patient age, sex, propensity for complications; the INR at admission; acute treatment for the GI bleed; and location of GI bleed – also showed that the risk for rebleeding was not significantly greater in patients who resumed warfarin therapy than in those who did not.
Moreover, recurrent GI bleeding was never fatal. Fatal strokes did occur, however, in three patients with atrial fibrillation whose warfarin therapy was withdrawn and never resumed, Dr. Witt and his associates said.
A total of 52 patients (12%) died during follow-up. The most common cause of death was related to malignancy (29% of deaths), infection (19% of deaths), or cardiac disease (17%).
Resumption of warfarin therapy was strongly associated with a threefold decrease in the risk of death from any cause.
The investigators also performed a post hoc analysis excluding all patients who died within 1 week of the index GI bleed to rule out those who may not have had an opportunity to resume warfarin therapy. In this analysis, the strong association between resumption of warfarin and decreased mortality persisted.
Mortality was lowest among patients who resumed warfarin therapy within 15-90 days of the index GI bleed, the researchers said.
"Our results provide some guidance regarding the optimal timing of warfarin therapy resumption following GI bleeding, but clinical judgment remains a critical factor in this difficult decision," they noted.
This study was funded by CSL Behring. Dr. Witt’s associates, but not Dr. Witt, reported ties to numerous industry sources.
Deciding not to resume warfarin therapy after an episode of gastrointestinal bleeding raises the risk of thrombosis by a factor of 10 and the risk of death threefold, according to a retrospective cohort study published online September 17 in Archives of Internal Medicine.
"For many patients who have experienced gastrointestinal bleeding, the benefits of resuming warfarin therapy will outweigh the risks," said Daniel M. Witt, Pharm.D., of the clinical pharmacy anticoagulation service at Kaiser Permanente of Colorado, Aurora, and his associates.
"Surprisingly little is known about warfarin therapy and resumption" following a GI bleed, and there is no consensus as to the optimal timing or the risks of restarting anticoagulation. Dr. Witt and his colleagues used Kaiser’s administrative and clinical databases to study the incidence of thrombosis, recurrent bleeding episodes, and death from any cause in 442 adults who presented to a hospital or emergency department with warfarin-associated GI bleeding in 2005-2009 and who were followed for 90 days.
The mean patient age was 74 years, and the study population was equally comprised of men and women. Half of the study subjects were taking warfarin to prevent atrial fibrillation–related stroke or systemic embolization. One-quarter of patients used it to treat or prevent a second venous thrombosis, 10% were on it to prevent thromboembolic complications from prosthetic heart valves, and the remainder took it for other indications.
After an index GI bleed, 260 patients (59%) resumed warfarin therapy, usually within a week. The median time to resumption of warfarin was 4 days. In 41 of these patients, warfarin therapy was never suspended. It was suspended and never resumed in the remaining 182 patients.
During the 90-day follow-up, 11 patients (2.5%) had a thrombotic event. There were six arterial events, including five strokes and one systemic embolus, and five venous events, including three pulmonary embolisms and two deep vein thromboses (DVTs).
The rate of thrombotic events was 0.4% among the patients who resumed warfarin therapy (one DVT), compared with 5.5% among those who did not resume warfarin (five strokes, one systemic embolus, three pulmonary embolisms, and one DVT), a significant difference, the investigators said (Arch. Intern. Med. 2012 [doi:10.1001/archinternmed.2012.5261]).
"Patients who either never interrupted warfarin therapy or resumed therapy within 14 days of the index GI bleed experienced no thromboses," they added.
GI bleeding recurred in 36 patients (8.4%) overall. A numerically higher proportion of patients who resumed warfarin therapy had recurrent GI bleeding (10%) than those who did not resume warfarin (5.5%), but this difference was not statistically significant.
In addition, a multivariable analysis that accounted for numerous possible confounders – including patient age, sex, propensity for complications; the INR at admission; acute treatment for the GI bleed; and location of GI bleed – also showed that the risk for rebleeding was not significantly greater in patients who resumed warfarin therapy than in those who did not.
Moreover, recurrent GI bleeding was never fatal. Fatal strokes did occur, however, in three patients with atrial fibrillation whose warfarin therapy was withdrawn and never resumed, Dr. Witt and his associates said.
A total of 52 patients (12%) died during follow-up. The most common cause of death was related to malignancy (29% of deaths), infection (19% of deaths), or cardiac disease (17%).
Resumption of warfarin therapy was strongly associated with a threefold decrease in the risk of death from any cause.
The investigators also performed a post hoc analysis excluding all patients who died within 1 week of the index GI bleed to rule out those who may not have had an opportunity to resume warfarin therapy. In this analysis, the strong association between resumption of warfarin and decreased mortality persisted.
Mortality was lowest among patients who resumed warfarin therapy within 15-90 days of the index GI bleed, the researchers said.
"Our results provide some guidance regarding the optimal timing of warfarin therapy resumption following GI bleeding, but clinical judgment remains a critical factor in this difficult decision," they noted.
This study was funded by CSL Behring. Dr. Witt’s associates, but not Dr. Witt, reported ties to numerous industry sources.
FROM ARCHIVES OF INTERNAL MEDICINE
Major Finding: The rate of thrombotic events was 0.4% in patients who resumed warfarin therapy after an episode of GI bleeding, compared with 5.5% in those who did not resume warfarin.
Data Source: A retrospective cohort study compared outcomes between 260 patients who resumed warfarin therapy and 182 who did not, who were followed for 90 days.
Disclosures: This study was funded by CSL Behring. Dr. Witt’s associates, but not Dr. Witt, reported ties to numerous industry sources.
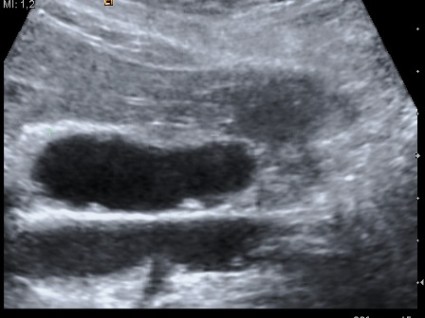
Snag Larger Gallbladder Polyps, Follow Smaller
A policy of regular ultrasound exams for small gallbladder polyps and resection on only larger ones could catch five more gallbladder cancers per year and save more than $200,000.
A retrospective study also found that 50% of gallbladder polyps were not followed at all, setting the stage for the rare – but potentially dangerous – cancers to develop, Dr. Giuseppe Garcea and his colleagues wrote in the Aug. 20 online issue of Archives of Surgery.
"All gallbladder polyps represent potentially premalignant disease and require discussion at a hepatobiliary multidisciplinary team meeting because this would enhance and standardize the management of this condition," wrote Dr. Garcea of the University Hospitals of Leicester (England).
The investigators reviewed the records of 986 patients with confirmed gallbladder polyps who were followed up for a median period of 39 months. The patients’ median age was 57 years.
About half of the polyps were detected by ultrasound after a complaint of upper abdominal pain, thought to have been caused by gallstones. The rest were found incidentally. Most of the findings were of single polyps (62%), but 24% of the lesions occurred in groups of three or more.
Specialist consultation was uncommon, with only 5% of cases discussed at a hepatobiliary multidisciplinary meeting. Half of the patients were not followed at all for changes in polyp morphology. Follow-up was more common in patients seen by a specialist than in those who were not (60% vs.10%).
Although 23% of the patients had an increased number of polyps over the follow-up period, only 7% of these lesions increased in size. Those polyps that did get larger were also significantly larger at presentation than those with a stable size (7 mm vs. 5 mm).
Surgery was performed on 134 patients. Histologic examination showed that in almost half of the gallbladders, the only abnormality was cholesterolosis or cholesterol polyps; 94% of the gallbladders had benign conditions. A malignant or potentially malignant pathology occurred in just five patients, with one polyp showing signs of malignant differentiation.
Polyps that were found to be malignant or potentially malignant during follow-up had also been significantly larger than nonmalignant polyps at presentation (median, 10 mm vs. 5 mm). All of the malignant polyps had also become larger during the follow-up period. A baseline size of more than 10 mm and increases in size during follow-up were the best predictors of malignant polyps (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1948]).
Based on an incidence of 504 cases per 100,000 people in the United Kingdom, the authors pegged the annual socioeconomic cost of gallbladder surgery at about U.S. $78 million each year. They constructed a mathematical model assuming biannual ultrasound follow-up, and a 20-year expected life span after age at diagnosis. The model predicted that ultrasound surveillance would catch five patients with gallbladder cancer every year and save U.S. $507,986 per year in associated costs.
In the very young patients, however, "an argument may be made for prophylactic cholecystectomy even with polyps less than 10 mm, because the long protracted follow-up involved would be impractical and probably unsustainable," the investigators said.
To maximize effectiveness and financial gains, they determined that polyps sized 5-10 mm should be followed, and those larger than 10 mm should be removed. No study has determined the likelihood of a 5- to 10-mm polyp becoming malignant, they said, but because the risks associated with ultrasound surveillance and any subsequent gallbladder surgery are so small, they concluded that regular follow-up would still be cost effective.
Neither Dr. Garcea nor any of his coauthors reported any financial conflicts.
Despite this study’s finding that the vast majority of gallbladder polyps were benign, surgeons will continue to worry about these lesions – whether large or small, Dr. Jonathan Koea wrote in an accompanying editorial (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1959]).
"Set against this very benign picture is the specter of carcinoma of the gallbladder, which, when treatable, requires major hepatic surgery and for which there are no particularly effective adjuvant therapies. This provides an impetus to monitor or treat all gallbladder polyps," he said.
Large surveillance programs are only truly effective when there is a high prevalence of potentially malignant lesions in a group. This is problematic for gallbladder polyps because they are difficult to visualize in detail with ultrasound, Dr. Koea noted.
"In addition, serial ultrasonography also has a significant financial and emotional cost to patients and relies on compliance and patient recall procedures. With this level of uncertainty in diagnosis and persisting concerns over the natural history of polyps, many patients and their surgeons will opt for a safely performed laparoscopic cholecystectomy to define the diagnosis and conclusively treat the problem rather than a prolonged period of surveillance," he wrote.
Dr. Koea is a surgeon at the North Shore Hospital, Takapuna, New Zealand. He did not report any financial conflicts.
Despite this study’s finding that the vast majority of gallbladder polyps were benign, surgeons will continue to worry about these lesions – whether large or small, Dr. Jonathan Koea wrote in an accompanying editorial (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1959]).
"Set against this very benign picture is the specter of carcinoma of the gallbladder, which, when treatable, requires major hepatic surgery and for which there are no particularly effective adjuvant therapies. This provides an impetus to monitor or treat all gallbladder polyps," he said.
Large surveillance programs are only truly effective when there is a high prevalence of potentially malignant lesions in a group. This is problematic for gallbladder polyps because they are difficult to visualize in detail with ultrasound, Dr. Koea noted.
"In addition, serial ultrasonography also has a significant financial and emotional cost to patients and relies on compliance and patient recall procedures. With this level of uncertainty in diagnosis and persisting concerns over the natural history of polyps, many patients and their surgeons will opt for a safely performed laparoscopic cholecystectomy to define the diagnosis and conclusively treat the problem rather than a prolonged period of surveillance," he wrote.
Dr. Koea is a surgeon at the North Shore Hospital, Takapuna, New Zealand. He did not report any financial conflicts.
Despite this study’s finding that the vast majority of gallbladder polyps were benign, surgeons will continue to worry about these lesions – whether large or small, Dr. Jonathan Koea wrote in an accompanying editorial (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1959]).
"Set against this very benign picture is the specter of carcinoma of the gallbladder, which, when treatable, requires major hepatic surgery and for which there are no particularly effective adjuvant therapies. This provides an impetus to monitor or treat all gallbladder polyps," he said.
Large surveillance programs are only truly effective when there is a high prevalence of potentially malignant lesions in a group. This is problematic for gallbladder polyps because they are difficult to visualize in detail with ultrasound, Dr. Koea noted.
"In addition, serial ultrasonography also has a significant financial and emotional cost to patients and relies on compliance and patient recall procedures. With this level of uncertainty in diagnosis and persisting concerns over the natural history of polyps, many patients and their surgeons will opt for a safely performed laparoscopic cholecystectomy to define the diagnosis and conclusively treat the problem rather than a prolonged period of surveillance," he wrote.
Dr. Koea is a surgeon at the North Shore Hospital, Takapuna, New Zealand. He did not report any financial conflicts.
A policy of regular ultrasound exams for small gallbladder polyps and resection on only larger ones could catch five more gallbladder cancers per year and save more than $200,000.
A retrospective study also found that 50% of gallbladder polyps were not followed at all, setting the stage for the rare – but potentially dangerous – cancers to develop, Dr. Giuseppe Garcea and his colleagues wrote in the Aug. 20 online issue of Archives of Surgery.
"All gallbladder polyps represent potentially premalignant disease and require discussion at a hepatobiliary multidisciplinary team meeting because this would enhance and standardize the management of this condition," wrote Dr. Garcea of the University Hospitals of Leicester (England).
The investigators reviewed the records of 986 patients with confirmed gallbladder polyps who were followed up for a median period of 39 months. The patients’ median age was 57 years.
About half of the polyps were detected by ultrasound after a complaint of upper abdominal pain, thought to have been caused by gallstones. The rest were found incidentally. Most of the findings were of single polyps (62%), but 24% of the lesions occurred in groups of three or more.
Specialist consultation was uncommon, with only 5% of cases discussed at a hepatobiliary multidisciplinary meeting. Half of the patients were not followed at all for changes in polyp morphology. Follow-up was more common in patients seen by a specialist than in those who were not (60% vs.10%).
Although 23% of the patients had an increased number of polyps over the follow-up period, only 7% of these lesions increased in size. Those polyps that did get larger were also significantly larger at presentation than those with a stable size (7 mm vs. 5 mm).
Surgery was performed on 134 patients. Histologic examination showed that in almost half of the gallbladders, the only abnormality was cholesterolosis or cholesterol polyps; 94% of the gallbladders had benign conditions. A malignant or potentially malignant pathology occurred in just five patients, with one polyp showing signs of malignant differentiation.
Polyps that were found to be malignant or potentially malignant during follow-up had also been significantly larger than nonmalignant polyps at presentation (median, 10 mm vs. 5 mm). All of the malignant polyps had also become larger during the follow-up period. A baseline size of more than 10 mm and increases in size during follow-up were the best predictors of malignant polyps (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1948]).
Based on an incidence of 504 cases per 100,000 people in the United Kingdom, the authors pegged the annual socioeconomic cost of gallbladder surgery at about U.S. $78 million each year. They constructed a mathematical model assuming biannual ultrasound follow-up, and a 20-year expected life span after age at diagnosis. The model predicted that ultrasound surveillance would catch five patients with gallbladder cancer every year and save U.S. $507,986 per year in associated costs.
In the very young patients, however, "an argument may be made for prophylactic cholecystectomy even with polyps less than 10 mm, because the long protracted follow-up involved would be impractical and probably unsustainable," the investigators said.
To maximize effectiveness and financial gains, they determined that polyps sized 5-10 mm should be followed, and those larger than 10 mm should be removed. No study has determined the likelihood of a 5- to 10-mm polyp becoming malignant, they said, but because the risks associated with ultrasound surveillance and any subsequent gallbladder surgery are so small, they concluded that regular follow-up would still be cost effective.
Neither Dr. Garcea nor any of his coauthors reported any financial conflicts.
A policy of regular ultrasound exams for small gallbladder polyps and resection on only larger ones could catch five more gallbladder cancers per year and save more than $200,000.
A retrospective study also found that 50% of gallbladder polyps were not followed at all, setting the stage for the rare – but potentially dangerous – cancers to develop, Dr. Giuseppe Garcea and his colleagues wrote in the Aug. 20 online issue of Archives of Surgery.
"All gallbladder polyps represent potentially premalignant disease and require discussion at a hepatobiliary multidisciplinary team meeting because this would enhance and standardize the management of this condition," wrote Dr. Garcea of the University Hospitals of Leicester (England).
The investigators reviewed the records of 986 patients with confirmed gallbladder polyps who were followed up for a median period of 39 months. The patients’ median age was 57 years.
About half of the polyps were detected by ultrasound after a complaint of upper abdominal pain, thought to have been caused by gallstones. The rest were found incidentally. Most of the findings were of single polyps (62%), but 24% of the lesions occurred in groups of three or more.
Specialist consultation was uncommon, with only 5% of cases discussed at a hepatobiliary multidisciplinary meeting. Half of the patients were not followed at all for changes in polyp morphology. Follow-up was more common in patients seen by a specialist than in those who were not (60% vs.10%).
Although 23% of the patients had an increased number of polyps over the follow-up period, only 7% of these lesions increased in size. Those polyps that did get larger were also significantly larger at presentation than those with a stable size (7 mm vs. 5 mm).
Surgery was performed on 134 patients. Histologic examination showed that in almost half of the gallbladders, the only abnormality was cholesterolosis or cholesterol polyps; 94% of the gallbladders had benign conditions. A malignant or potentially malignant pathology occurred in just five patients, with one polyp showing signs of malignant differentiation.
Polyps that were found to be malignant or potentially malignant during follow-up had also been significantly larger than nonmalignant polyps at presentation (median, 10 mm vs. 5 mm). All of the malignant polyps had also become larger during the follow-up period. A baseline size of more than 10 mm and increases in size during follow-up were the best predictors of malignant polyps (Arch. Surg. 2012 Aug. 20 [doi:10.1001/archsurg.2012.1948]).
Based on an incidence of 504 cases per 100,000 people in the United Kingdom, the authors pegged the annual socioeconomic cost of gallbladder surgery at about U.S. $78 million each year. They constructed a mathematical model assuming biannual ultrasound follow-up, and a 20-year expected life span after age at diagnosis. The model predicted that ultrasound surveillance would catch five patients with gallbladder cancer every year and save U.S. $507,986 per year in associated costs.
In the very young patients, however, "an argument may be made for prophylactic cholecystectomy even with polyps less than 10 mm, because the long protracted follow-up involved would be impractical and probably unsustainable," the investigators said.
To maximize effectiveness and financial gains, they determined that polyps sized 5-10 mm should be followed, and those larger than 10 mm should be removed. No study has determined the likelihood of a 5- to 10-mm polyp becoming malignant, they said, but because the risks associated with ultrasound surveillance and any subsequent gallbladder surgery are so small, they concluded that regular follow-up would still be cost effective.
Neither Dr. Garcea nor any of his coauthors reported any financial conflicts.
FROM ARCHIVES OF SURGERY
Major Finding: Biannual ultrasound surveillance of gallbladder polyps measuring less than 10 cm could catch 5 potential malignancies per 1,000 individuals per year, and save hundreds of thousands of dollars in health care and related social costs.
Data Source: A chart review of 986 patients was conducted.
Disclosures: Neither Dr. Garcea nor any of his coauthors reported any relevant financial conflicts.
Post-Polypectomy Surveillance Guidelines Updated
Adults with no polyps at baseline colonoscopy and average risk for colorectal cancer can still wait 10 years until their next colonoscopy, according to updated surveillance guidelines from the U.S. Multi-Society Task Force on Colorectal Cancer. The guidelines were published in the September issue of Gastroenterology.
New concerns, including the risk of interval colorectal cancer (CRC), the risk of proximal colorectal cancer, and the role of serrated polyps in carcinogenesis prompted an update to the guidelines, which were last revised in 2006, according to lead author Dr. David A. Lieberman of Oregon Health and Science University, Portland, and his colleagues.
The task force is composed of GI specialists representing the three major GI professional organizations: the American Gastroenterological Association (AGA) Institute, American College of Gastroenterology (ACG), and American Society for Gastrointestinal Endoscopy (ASGE).
Overall, the recommendations have not changed, but the task force reviewed the most recent literature and found additional evidence to support several categories of surveillance and screening intervals for adults with average risk of CRC at the time of a baseline screening.
Recommendations supported by new evidence include a 10-year interval for individuals with no polyps, and a 5- to 10-year interval for those with one or two tubular adenomas less than 10 mm in size. New evidence also supports a 3-year interval for patients with 3-10 tubular adenomas of any size, and also 3 years for patients with one or more tubular adenomas 10 mm or larger. In addition, data reported since 2006 support a 3-year surveillance interval for patients with one or more villous adenomas.
Recommendations that remain unchanged without additional evidence are a 10-year surveillance interval for individuals with hyperplastic polyps in the rectum or sigmoid, an interval of less than 3 years for those with more than 10 adenomas, and an interval of 3 years in cases of an adenoma with high-grade dysplasia.
In addition, serrated lesions are now included as part of the surveillance schedule after a baseline colonoscopy. Individuals with one or more sessile serrated polyps less than 10 mm in size and no dysplasia should be rescreened after 5 years. Those with one or more sessile serrated polyps 10 mm or larger, or any sessile serrated polyp with dysplasia, or a traditional serrated adenoma should be rescreened after 3 years.
Individuals with serrated polyposis syndrome (SPS) should be rescreened after 1 year. Serrated polyposis syndrome is defined as meeting one of three criteria (in agreement with the World Health Organization definition): at least five serrated polyps proximal to the sigmoid, with at least two measuring 10 mm or larger; any serrated polyps proximal to the sigmoid in patients with a family history of SPS; and more than 20 serrated polyps of any size throughout the colon.
The authors noted that the quality of the evidence supporting the current guidelines is low, and will require updates. "There are no longitudinal studies available on which to base surveillance intervals after resection," they said.
In addition, given new evidence about the increased risk of colonoscopy with advancing age, surveillance and screening should be discontinued when the risks outweigh the benefits, according to the guidelines. "The United States Preventive Services Task Forces determined that screening should not be continued after age 85 years because risk could exceed potential benefit," the task force noted. "It is the opinion of the MSTF that the decision to continue surveillance should be individualized, based on an assessment of benefit, risk, and co-morbidities."
However, "the guidelines are dynamic, and will be revised in the future, based on new evidence. This new evidence should include information about the quality of the baseline examinations," the authors said. "The task force recommends that all endoscopists monitor key quality indicators as part of a colonoscopy screening and surveillance program," they noted.
Lead author Dr. David Lieberman has served on the advisory boards of Given Imaging and Exact Sciences.
Adults with no polyps at baseline colonoscopy and average risk for colorectal cancer can still wait 10 years until their next colonoscopy, according to updated surveillance guidelines from the U.S. Multi-Society Task Force on Colorectal Cancer. The guidelines were published in the September issue of Gastroenterology.
New concerns, including the risk of interval colorectal cancer (CRC), the risk of proximal colorectal cancer, and the role of serrated polyps in carcinogenesis prompted an update to the guidelines, which were last revised in 2006, according to lead author Dr. David A. Lieberman of Oregon Health and Science University, Portland, and his colleagues.
The task force is composed of GI specialists representing the three major GI professional organizations: the American Gastroenterological Association (AGA) Institute, American College of Gastroenterology (ACG), and American Society for Gastrointestinal Endoscopy (ASGE).
Overall, the recommendations have not changed, but the task force reviewed the most recent literature and found additional evidence to support several categories of surveillance and screening intervals for adults with average risk of CRC at the time of a baseline screening.
Recommendations supported by new evidence include a 10-year interval for individuals with no polyps, and a 5- to 10-year interval for those with one or two tubular adenomas less than 10 mm in size. New evidence also supports a 3-year interval for patients with 3-10 tubular adenomas of any size, and also 3 years for patients with one or more tubular adenomas 10 mm or larger. In addition, data reported since 2006 support a 3-year surveillance interval for patients with one or more villous adenomas.
Recommendations that remain unchanged without additional evidence are a 10-year surveillance interval for individuals with hyperplastic polyps in the rectum or sigmoid, an interval of less than 3 years for those with more than 10 adenomas, and an interval of 3 years in cases of an adenoma with high-grade dysplasia.
In addition, serrated lesions are now included as part of the surveillance schedule after a baseline colonoscopy. Individuals with one or more sessile serrated polyps less than 10 mm in size and no dysplasia should be rescreened after 5 years. Those with one or more sessile serrated polyps 10 mm or larger, or any sessile serrated polyp with dysplasia, or a traditional serrated adenoma should be rescreened after 3 years.
Individuals with serrated polyposis syndrome (SPS) should be rescreened after 1 year. Serrated polyposis syndrome is defined as meeting one of three criteria (in agreement with the World Health Organization definition): at least five serrated polyps proximal to the sigmoid, with at least two measuring 10 mm or larger; any serrated polyps proximal to the sigmoid in patients with a family history of SPS; and more than 20 serrated polyps of any size throughout the colon.
The authors noted that the quality of the evidence supporting the current guidelines is low, and will require updates. "There are no longitudinal studies available on which to base surveillance intervals after resection," they said.
In addition, given new evidence about the increased risk of colonoscopy with advancing age, surveillance and screening should be discontinued when the risks outweigh the benefits, according to the guidelines. "The United States Preventive Services Task Forces determined that screening should not be continued after age 85 years because risk could exceed potential benefit," the task force noted. "It is the opinion of the MSTF that the decision to continue surveillance should be individualized, based on an assessment of benefit, risk, and co-morbidities."
However, "the guidelines are dynamic, and will be revised in the future, based on new evidence. This new evidence should include information about the quality of the baseline examinations," the authors said. "The task force recommends that all endoscopists monitor key quality indicators as part of a colonoscopy screening and surveillance program," they noted.
Lead author Dr. David Lieberman has served on the advisory boards of Given Imaging and Exact Sciences.
Adults with no polyps at baseline colonoscopy and average risk for colorectal cancer can still wait 10 years until their next colonoscopy, according to updated surveillance guidelines from the U.S. Multi-Society Task Force on Colorectal Cancer. The guidelines were published in the September issue of Gastroenterology.
New concerns, including the risk of interval colorectal cancer (CRC), the risk of proximal colorectal cancer, and the role of serrated polyps in carcinogenesis prompted an update to the guidelines, which were last revised in 2006, according to lead author Dr. David A. Lieberman of Oregon Health and Science University, Portland, and his colleagues.
The task force is composed of GI specialists representing the three major GI professional organizations: the American Gastroenterological Association (AGA) Institute, American College of Gastroenterology (ACG), and American Society for Gastrointestinal Endoscopy (ASGE).
Overall, the recommendations have not changed, but the task force reviewed the most recent literature and found additional evidence to support several categories of surveillance and screening intervals for adults with average risk of CRC at the time of a baseline screening.
Recommendations supported by new evidence include a 10-year interval for individuals with no polyps, and a 5- to 10-year interval for those with one or two tubular adenomas less than 10 mm in size. New evidence also supports a 3-year interval for patients with 3-10 tubular adenomas of any size, and also 3 years for patients with one or more tubular adenomas 10 mm or larger. In addition, data reported since 2006 support a 3-year surveillance interval for patients with one or more villous adenomas.
Recommendations that remain unchanged without additional evidence are a 10-year surveillance interval for individuals with hyperplastic polyps in the rectum or sigmoid, an interval of less than 3 years for those with more than 10 adenomas, and an interval of 3 years in cases of an adenoma with high-grade dysplasia.
In addition, serrated lesions are now included as part of the surveillance schedule after a baseline colonoscopy. Individuals with one or more sessile serrated polyps less than 10 mm in size and no dysplasia should be rescreened after 5 years. Those with one or more sessile serrated polyps 10 mm or larger, or any sessile serrated polyp with dysplasia, or a traditional serrated adenoma should be rescreened after 3 years.
Individuals with serrated polyposis syndrome (SPS) should be rescreened after 1 year. Serrated polyposis syndrome is defined as meeting one of three criteria (in agreement with the World Health Organization definition): at least five serrated polyps proximal to the sigmoid, with at least two measuring 10 mm or larger; any serrated polyps proximal to the sigmoid in patients with a family history of SPS; and more than 20 serrated polyps of any size throughout the colon.
The authors noted that the quality of the evidence supporting the current guidelines is low, and will require updates. "There are no longitudinal studies available on which to base surveillance intervals after resection," they said.
In addition, given new evidence about the increased risk of colonoscopy with advancing age, surveillance and screening should be discontinued when the risks outweigh the benefits, according to the guidelines. "The United States Preventive Services Task Forces determined that screening should not be continued after age 85 years because risk could exceed potential benefit," the task force noted. "It is the opinion of the MSTF that the decision to continue surveillance should be individualized, based on an assessment of benefit, risk, and co-morbidities."
However, "the guidelines are dynamic, and will be revised in the future, based on new evidence. This new evidence should include information about the quality of the baseline examinations," the authors said. "The task force recommends that all endoscopists monitor key quality indicators as part of a colonoscopy screening and surveillance program," they noted.
Lead author Dr. David Lieberman has served on the advisory boards of Given Imaging and Exact Sciences.
FROM GASTROENTEROLOGY
Major Finding: Recommendations supported by new evidence include a 5- to 10-year interval for individuals with one or two tubular adenomas less than 10 mm in size.
Data Source: The data come from a review of English-language articles published between 2005 and 2011.
Disclosures: Lead author Dr. David Lieberman has served on the advisory boards of Given Imaging and Exact Sciences.
Endoscopy Falls Short for Eosinophilic Esophagitis
Endoscopic findings alone are not sufficient to diagnose eosinophilic esophagitis and instead, biopsies are needed, reported Ms. Hannah P. Kim and her colleagues in the September issue of Clinical Gastroenterology and Hepatology.
Indeed, while findings like rings, strictures, and linear furrows ought to raise suspicion, a meta-analysis of more than 4,600 patients confirms that "low sensitivity and variable predictive values make them inadequate both for the diagnosis of EoE [eosinophilic esophagitis] and for the decision of whether or not to obtain biopsies."
Ms. Kim of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and her colleagues analyzed data from 80 articles and 20 abstracts that included a total of 4,678 patients with EoE and 2,742 patients without, who served as controls.
The studies were culled from PubMed, EMBASE, and gastroenterology meetings. All studies included in the analysis had more than 10 patients with EoE and provided information on the associated endoscopic findings. The mean age of participants ranged from 6 years to 55 years in the different studies.
In an analysis, the authors found that the overall pooled prevalence of esophageal rings in the sample was 44%. For strictures, the prevalence was 21%, and for linear furrows, 48% (Clin. Gastroenterol. Hepatol. 2012 [doi:10.1016/j.cgh.2012.04.019]).
Narrow-caliber esophagus findings had a pooled prevalence of only 9% of the total sample, while the presence of white plaques or exudates was 27%. Visible pallor or decreased vasculature on endoscopy was seen in 41% of patients, and erosive esophagitis in 17%.
"The endoscopic examination was normal in 17% of cases," added the authors.
They also found a difference in prevalence according to age of patients. For example, rings and strictures were more prevalent in adults (57% and 25%, respectively) than in children (11% and 8%; P less than .05 for each).
"On the other hand, white plaques and pallor or decreased vasculature were more prevalent in children (36% and 58%) than in adults (19% and 18%; P less than .05 for each)."
Finally, Ms. Kim and her associates assessed the overall sensitivity, specificity, pooled positive predictive value (PPV), and pooled negative predictive value (NPV) for each of the assessed endoscopic characteristics.
For rings, the overall sensitivity was 48%, the specificity was 91%, the PPV was 64%, and NPV was 84%. Strictures had an overall sensitivity of 15%, specificity of 95%, PPV of 51%, and NPV of 76%.
"The operating characteristics were slightly higher for linear furrows, with a sensitivity of 40%, specificity 95%, PPV 73%, and NPV 83%," wrote the authors.
And for the endoscopic finding of pallor and/or decreased vasculature, sensitivity was 43%, specificity 90%, PPV 65%, and NPV 79%.
"In contrast to the low sensitivity of individual endoscopic findings, when examining the presence of at least one endoscopic finding, an abnormal endoscopy had a sensitivity of 87%, specificity of 47%, PPV of 42%, and NPV of 89%," the authors added.
"Although endoscopic features of EoE such as esophageal rings, linear furrows, and white plaques or exudates are often considered to be typical features of EoE, these are not always identified by endoscopists," wrote the researchers.
And while most patients with EoE have abnormal findings on upper endoscopy examinations, "the sensitivity values of individual endoscopic findings were modest, and although the specificity values were higher, the predictive values were inadequate for diagnostic purposes."
"Esophageal biopsies should be obtained from all patients who present with symptoms of EoE, regardless of the endoscopic appearance of the esophagus."
The authors stated that the study was supported by grants from the National Institutes of Health and the Doris Duke Charitable Foundation. They stated that they had no individual disclosures.
Endoscopic findings alone are not sufficient to diagnose eosinophilic esophagitis and instead, biopsies are needed, reported Ms. Hannah P. Kim and her colleagues in the September issue of Clinical Gastroenterology and Hepatology.
Indeed, while findings like rings, strictures, and linear furrows ought to raise suspicion, a meta-analysis of more than 4,600 patients confirms that "low sensitivity and variable predictive values make them inadequate both for the diagnosis of EoE [eosinophilic esophagitis] and for the decision of whether or not to obtain biopsies."
Ms. Kim of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and her colleagues analyzed data from 80 articles and 20 abstracts that included a total of 4,678 patients with EoE and 2,742 patients without, who served as controls.
The studies were culled from PubMed, EMBASE, and gastroenterology meetings. All studies included in the analysis had more than 10 patients with EoE and provided information on the associated endoscopic findings. The mean age of participants ranged from 6 years to 55 years in the different studies.
In an analysis, the authors found that the overall pooled prevalence of esophageal rings in the sample was 44%. For strictures, the prevalence was 21%, and for linear furrows, 48% (Clin. Gastroenterol. Hepatol. 2012 [doi:10.1016/j.cgh.2012.04.019]).
Narrow-caliber esophagus findings had a pooled prevalence of only 9% of the total sample, while the presence of white plaques or exudates was 27%. Visible pallor or decreased vasculature on endoscopy was seen in 41% of patients, and erosive esophagitis in 17%.
"The endoscopic examination was normal in 17% of cases," added the authors.
They also found a difference in prevalence according to age of patients. For example, rings and strictures were more prevalent in adults (57% and 25%, respectively) than in children (11% and 8%; P less than .05 for each).
"On the other hand, white plaques and pallor or decreased vasculature were more prevalent in children (36% and 58%) than in adults (19% and 18%; P less than .05 for each)."
Finally, Ms. Kim and her associates assessed the overall sensitivity, specificity, pooled positive predictive value (PPV), and pooled negative predictive value (NPV) for each of the assessed endoscopic characteristics.
For rings, the overall sensitivity was 48%, the specificity was 91%, the PPV was 64%, and NPV was 84%. Strictures had an overall sensitivity of 15%, specificity of 95%, PPV of 51%, and NPV of 76%.
"The operating characteristics were slightly higher for linear furrows, with a sensitivity of 40%, specificity 95%, PPV 73%, and NPV 83%," wrote the authors.
And for the endoscopic finding of pallor and/or decreased vasculature, sensitivity was 43%, specificity 90%, PPV 65%, and NPV 79%.
"In contrast to the low sensitivity of individual endoscopic findings, when examining the presence of at least one endoscopic finding, an abnormal endoscopy had a sensitivity of 87%, specificity of 47%, PPV of 42%, and NPV of 89%," the authors added.
"Although endoscopic features of EoE such as esophageal rings, linear furrows, and white plaques or exudates are often considered to be typical features of EoE, these are not always identified by endoscopists," wrote the researchers.
And while most patients with EoE have abnormal findings on upper endoscopy examinations, "the sensitivity values of individual endoscopic findings were modest, and although the specificity values were higher, the predictive values were inadequate for diagnostic purposes."
"Esophageal biopsies should be obtained from all patients who present with symptoms of EoE, regardless of the endoscopic appearance of the esophagus."
The authors stated that the study was supported by grants from the National Institutes of Health and the Doris Duke Charitable Foundation. They stated that they had no individual disclosures.
Endoscopic findings alone are not sufficient to diagnose eosinophilic esophagitis and instead, biopsies are needed, reported Ms. Hannah P. Kim and her colleagues in the September issue of Clinical Gastroenterology and Hepatology.
Indeed, while findings like rings, strictures, and linear furrows ought to raise suspicion, a meta-analysis of more than 4,600 patients confirms that "low sensitivity and variable predictive values make them inadequate both for the diagnosis of EoE [eosinophilic esophagitis] and for the decision of whether or not to obtain biopsies."
Ms. Kim of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and her colleagues analyzed data from 80 articles and 20 abstracts that included a total of 4,678 patients with EoE and 2,742 patients without, who served as controls.
The studies were culled from PubMed, EMBASE, and gastroenterology meetings. All studies included in the analysis had more than 10 patients with EoE and provided information on the associated endoscopic findings. The mean age of participants ranged from 6 years to 55 years in the different studies.
In an analysis, the authors found that the overall pooled prevalence of esophageal rings in the sample was 44%. For strictures, the prevalence was 21%, and for linear furrows, 48% (Clin. Gastroenterol. Hepatol. 2012 [doi:10.1016/j.cgh.2012.04.019]).
Narrow-caliber esophagus findings had a pooled prevalence of only 9% of the total sample, while the presence of white plaques or exudates was 27%. Visible pallor or decreased vasculature on endoscopy was seen in 41% of patients, and erosive esophagitis in 17%.
"The endoscopic examination was normal in 17% of cases," added the authors.
They also found a difference in prevalence according to age of patients. For example, rings and strictures were more prevalent in adults (57% and 25%, respectively) than in children (11% and 8%; P less than .05 for each).
"On the other hand, white plaques and pallor or decreased vasculature were more prevalent in children (36% and 58%) than in adults (19% and 18%; P less than .05 for each)."
Finally, Ms. Kim and her associates assessed the overall sensitivity, specificity, pooled positive predictive value (PPV), and pooled negative predictive value (NPV) for each of the assessed endoscopic characteristics.
For rings, the overall sensitivity was 48%, the specificity was 91%, the PPV was 64%, and NPV was 84%. Strictures had an overall sensitivity of 15%, specificity of 95%, PPV of 51%, and NPV of 76%.
"The operating characteristics were slightly higher for linear furrows, with a sensitivity of 40%, specificity 95%, PPV 73%, and NPV 83%," wrote the authors.
And for the endoscopic finding of pallor and/or decreased vasculature, sensitivity was 43%, specificity 90%, PPV 65%, and NPV 79%.
"In contrast to the low sensitivity of individual endoscopic findings, when examining the presence of at least one endoscopic finding, an abnormal endoscopy had a sensitivity of 87%, specificity of 47%, PPV of 42%, and NPV of 89%," the authors added.
"Although endoscopic features of EoE such as esophageal rings, linear furrows, and white plaques or exudates are often considered to be typical features of EoE, these are not always identified by endoscopists," wrote the researchers.
And while most patients with EoE have abnormal findings on upper endoscopy examinations, "the sensitivity values of individual endoscopic findings were modest, and although the specificity values were higher, the predictive values were inadequate for diagnostic purposes."
"Esophageal biopsies should be obtained from all patients who present with symptoms of EoE, regardless of the endoscopic appearance of the esophagus."
The authors stated that the study was supported by grants from the National Institutes of Health and the Doris Duke Charitable Foundation. They stated that they had no individual disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Major Finding: On endoscopy, rings and strictures were more prevalent in adults (57% and 25%, respectively) than in children (11% and 8%; P less than .05 for each).
Data Source: A systematic review and meta-analysis of studies including more than 4,600 EoE patients and 2,700 controls.
Disclosures: The authors stated that the study was supported by grants from the National Institutes of Health and the Doris Duke Charitable Foundation. They stated that they had no individual disclosures.
Robotic Device for Gastric Neoplasia Found Safe in Five Patients
A novel robotic system designed to perform endoscopic submucosal dissection of early gastric neoplasia was safe and effective in a five-patient trial, reported Soo Jay Phee, Ph.D., and colleagues in Clinical Gastroenterology and Hepatology.
Indeed, the first human study of the robotic device showed that it achieved clear margins, no cases of major bleeding or perforation, and discharge within hours for several of the patients.
Dr. Phee of the School of Mechanical and Aerospace Engineering at Nanyang Technological University in Singapore and first author Dr. D. Nageshwar Reddy of the Asian Institute of Gastroenterology in Somajiguda, India, enrolled five patients from two centers in India and one in Hong Kong.
Only patients with gastric neoplasia limited to the mucosa, confirmed by biopsy and histopathology, were included.
All patients underwent endoscopic submucosal dissection with the assistance of a novel device called the Master and Slave Transluminal Endoscopic Robot (MASTER). The MASTER device has been described previously (Gastrointest. Endoscopy 2010;72:593-9).
According to the authors, the device is controlled by two operators, "one responsible for the steering of the endoscope while the other would be performing the submucosal dissection with the two robotic arms."
The investigators added, "The open edge of the mucosa with the tumor was grasped by one of the robotic arms to retract the mucosa and enhance exposure of the submucosa, while submucosal dissection was completed with the other L hook arm" (Clin. Gastroenterol. Hepatol. 2012 October [doi:10.1016/j.cgh.2012.05.019]).
All procedures were performed under general anesthesia and with ventilation by naso- or orotracheal intubation. All operators trained on porcine models prior to the study.
In the case of the first patient, a 41-year-old man with a 2-cm adenocarcinoma in the body of the stomach, "the submucosal dissection with the robotic system was successfully done in 19 minutes," reported the authors.
There was no bleeding for perforation, and histopathology of the specimen after retrieval showed intramucosal well-differentiated adenocarcinoma with clear resection margins. The patient was discharged after 12 hours.
The second case, a 60-year-old man, was found to have a 1.5-cm mucosal adenocarcinoma in the gastric antrum. "The submucosal dissection was completed in only 5 minutes," wrote the authors, with no complications, and clear margins on histopathology. The patient was discharged in 6 hours.
Similarly, the third patient (a 39-year-old man) had a 2-cm sessile lesion in the gastric antrum. Submucosal dissection with the MASTER was completed in 3 minutes, with no complications, clear margins, and discharge from the hospital 4 hours later.
The longest procedure was done in a 51-year-old woman with a 3-cm early gastric cancer; this procedure took 50 minutes. She had no major bleeding or perforation, had clear margins on histopathology, and had a 3-day hospital stay.
Finally, a 50-year-old man with a 2.5-cm sessile polypoid in the inferior wall of the prepyloric canal underwent a 16-minute dissection. "Severe bleeding was encountered during the procedure and required exchange of the MASTER-mounted endoscope for a waterjet endoscope to stop the bleeding with coagulation grapser," wrote the authors.
"The pathology showed hyperplastic polyp with clear margins. He was discharged from hospital on day 3 after the procedure."
At 30 days’ follow-up, no complications were reported by any of the patients, and the follow-up endoscopy showed "complete healing" of the resection site. At 6 months, the three patients with data available were "doing well," according to the authors.
The study was supported by a MedTech Seeding Fund from the National University of Singapore. The authors reported having no other relevant financial disclosures.
A novel robotic system designed to perform endoscopic submucosal dissection of early gastric neoplasia was safe and effective in a five-patient trial, reported Soo Jay Phee, Ph.D., and colleagues in Clinical Gastroenterology and Hepatology.
Indeed, the first human study of the robotic device showed that it achieved clear margins, no cases of major bleeding or perforation, and discharge within hours for several of the patients.
Dr. Phee of the School of Mechanical and Aerospace Engineering at Nanyang Technological University in Singapore and first author Dr. D. Nageshwar Reddy of the Asian Institute of Gastroenterology in Somajiguda, India, enrolled five patients from two centers in India and one in Hong Kong.
Only patients with gastric neoplasia limited to the mucosa, confirmed by biopsy and histopathology, were included.
All patients underwent endoscopic submucosal dissection with the assistance of a novel device called the Master and Slave Transluminal Endoscopic Robot (MASTER). The MASTER device has been described previously (Gastrointest. Endoscopy 2010;72:593-9).
According to the authors, the device is controlled by two operators, "one responsible for the steering of the endoscope while the other would be performing the submucosal dissection with the two robotic arms."
The investigators added, "The open edge of the mucosa with the tumor was grasped by one of the robotic arms to retract the mucosa and enhance exposure of the submucosa, while submucosal dissection was completed with the other L hook arm" (Clin. Gastroenterol. Hepatol. 2012 October [doi:10.1016/j.cgh.2012.05.019]).
All procedures were performed under general anesthesia and with ventilation by naso- or orotracheal intubation. All operators trained on porcine models prior to the study.
In the case of the first patient, a 41-year-old man with a 2-cm adenocarcinoma in the body of the stomach, "the submucosal dissection with the robotic system was successfully done in 19 minutes," reported the authors.
There was no bleeding for perforation, and histopathology of the specimen after retrieval showed intramucosal well-differentiated adenocarcinoma with clear resection margins. The patient was discharged after 12 hours.
The second case, a 60-year-old man, was found to have a 1.5-cm mucosal adenocarcinoma in the gastric antrum. "The submucosal dissection was completed in only 5 minutes," wrote the authors, with no complications, and clear margins on histopathology. The patient was discharged in 6 hours.
Similarly, the third patient (a 39-year-old man) had a 2-cm sessile lesion in the gastric antrum. Submucosal dissection with the MASTER was completed in 3 minutes, with no complications, clear margins, and discharge from the hospital 4 hours later.
The longest procedure was done in a 51-year-old woman with a 3-cm early gastric cancer; this procedure took 50 minutes. She had no major bleeding or perforation, had clear margins on histopathology, and had a 3-day hospital stay.
Finally, a 50-year-old man with a 2.5-cm sessile polypoid in the inferior wall of the prepyloric canal underwent a 16-minute dissection. "Severe bleeding was encountered during the procedure and required exchange of the MASTER-mounted endoscope for a waterjet endoscope to stop the bleeding with coagulation grapser," wrote the authors.
"The pathology showed hyperplastic polyp with clear margins. He was discharged from hospital on day 3 after the procedure."
At 30 days’ follow-up, no complications were reported by any of the patients, and the follow-up endoscopy showed "complete healing" of the resection site. At 6 months, the three patients with data available were "doing well," according to the authors.
The study was supported by a MedTech Seeding Fund from the National University of Singapore. The authors reported having no other relevant financial disclosures.
A novel robotic system designed to perform endoscopic submucosal dissection of early gastric neoplasia was safe and effective in a five-patient trial, reported Soo Jay Phee, Ph.D., and colleagues in Clinical Gastroenterology and Hepatology.
Indeed, the first human study of the robotic device showed that it achieved clear margins, no cases of major bleeding or perforation, and discharge within hours for several of the patients.
Dr. Phee of the School of Mechanical and Aerospace Engineering at Nanyang Technological University in Singapore and first author Dr. D. Nageshwar Reddy of the Asian Institute of Gastroenterology in Somajiguda, India, enrolled five patients from two centers in India and one in Hong Kong.
Only patients with gastric neoplasia limited to the mucosa, confirmed by biopsy and histopathology, were included.
All patients underwent endoscopic submucosal dissection with the assistance of a novel device called the Master and Slave Transluminal Endoscopic Robot (MASTER). The MASTER device has been described previously (Gastrointest. Endoscopy 2010;72:593-9).
According to the authors, the device is controlled by two operators, "one responsible for the steering of the endoscope while the other would be performing the submucosal dissection with the two robotic arms."
The investigators added, "The open edge of the mucosa with the tumor was grasped by one of the robotic arms to retract the mucosa and enhance exposure of the submucosa, while submucosal dissection was completed with the other L hook arm" (Clin. Gastroenterol. Hepatol. 2012 October [doi:10.1016/j.cgh.2012.05.019]).
All procedures were performed under general anesthesia and with ventilation by naso- or orotracheal intubation. All operators trained on porcine models prior to the study.
In the case of the first patient, a 41-year-old man with a 2-cm adenocarcinoma in the body of the stomach, "the submucosal dissection with the robotic system was successfully done in 19 minutes," reported the authors.
There was no bleeding for perforation, and histopathology of the specimen after retrieval showed intramucosal well-differentiated adenocarcinoma with clear resection margins. The patient was discharged after 12 hours.
The second case, a 60-year-old man, was found to have a 1.5-cm mucosal adenocarcinoma in the gastric antrum. "The submucosal dissection was completed in only 5 minutes," wrote the authors, with no complications, and clear margins on histopathology. The patient was discharged in 6 hours.
Similarly, the third patient (a 39-year-old man) had a 2-cm sessile lesion in the gastric antrum. Submucosal dissection with the MASTER was completed in 3 minutes, with no complications, clear margins, and discharge from the hospital 4 hours later.
The longest procedure was done in a 51-year-old woman with a 3-cm early gastric cancer; this procedure took 50 minutes. She had no major bleeding or perforation, had clear margins on histopathology, and had a 3-day hospital stay.
Finally, a 50-year-old man with a 2.5-cm sessile polypoid in the inferior wall of the prepyloric canal underwent a 16-minute dissection. "Severe bleeding was encountered during the procedure and required exchange of the MASTER-mounted endoscope for a waterjet endoscope to stop the bleeding with coagulation grapser," wrote the authors.
"The pathology showed hyperplastic polyp with clear margins. He was discharged from hospital on day 3 after the procedure."
At 30 days’ follow-up, no complications were reported by any of the patients, and the follow-up endoscopy showed "complete healing" of the resection site. At 6 months, the three patients with data available were "doing well," according to the authors.
The study was supported by a MedTech Seeding Fund from the National University of Singapore. The authors reported having no other relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Major Finding: Five patients who underwent endoscopic submucosal dissection of early-stage gastric neoplasia with the use of a novel robotic system had good 30-day outcomes and clear resection margins.
Data Source: The findings came from five case studies in India and Hong Kong.
Disclosures: The study was supported by a MedTech Seeding Fund from the National University of Singapore. The authors reported having no other relevant financial disclosures.
Bile Duct Stones: Adequate Dilation Time Cuts Pancreatitis Risk
When treating choledocholithiasis, a shorter duration of endoscopic papillary balloon dilation increases, rather than decreases, the risk of postprocedure pancreatitis, reported Dr. Wei-Chih Liao and his colleagues in Clinical Gastroenterology and Hepatology.
"This meta-analysis contradicts the common belief that pancreatitis results from direct pancreatic duct compression during balloon dilation, and thus dilation duration should be short," he and his colleagues wrote. On the contrary, "[endoscopic papillary balloon dilation] with an adequate duration (around 5 minutes) has lower complication rates than the current standard of endoscopic sphincterotomy, and may be used as the first-line treatment for bile duct stones."
Dr. Liao, of the National Taiwan University College of Medicine, Taipei, conducted a systematic review of Medline, the Cochrane databases, and clinicaltrials.gov to identify randomized controlled trials of endoscopic papillary balloon dilation (EPBD), endoscopic sphincteroplasty, endoscopic balloon sphincter dilation, and endoscopic balloon dilation. Studies were excluded if dilation duration was not clearly reported.
Overall, 12 studies were included in the analysis: 11 compared EPBD with endoscopic sphincterotomy (EST); 4 compared short-duration EPBD (1 minute or less) with EST; and 7 looked at long-duration EPBD (more than 1 minute) versus EST.
Only one study compared long-duration EPBD with short-duration EPBD, they wrote (Clin. Gastroenterol. Hepatol. 2012 [doi: 10.1016/j.cgh.2012.05.017]).
First, the authors looked at the risk of pancreatitis when comparing EST to short-duration EPBD. They found that the latter had a significantly higher pancreatitis risk, with a pooled odds ratio of 3.87 for developing pancreatitis post procedure, compared with EST (95% confidence interval, 1.08-13.84).
However, long-duration EPBD did not pose a significantly higher risk compared with EST (OR, 1.14; 95% CI, 0.56-2.35).
Similarly, looking at overall complications, the researchers noted a trend toward a higher overall complication rate in short-duration EPBD compared with EST (OR, 1.71; 95% CI, 0.67-4.35). "By contrast, long EPBD seemed to have a lower overall complication rate (pooled OR, 0.61; 95% CI, 0.36-1.04)," wrote the authors.
The researchers also calculated the regression coefficient of dilation duration, and found it to be –0.69, "meaning that every 1-minute increase in dilation duration up to 3 minutes was associated with a 49.8% (95% CI, –9.4% –77.0%) reduction in OR," they wrote.
The finding was similar for overall complications, with every 1-minute increase in dilation duration up to 5 minutes associated with a 45.1% reduction in OR.
In an attempt to explain the findings, Dr. Liao noted that recent evidence suggests that EPBD with dilation duration of 1 minute or less "carries a higher risk of inadequate sphincter loosening, which increases the risks of pancreatitis and failed stone extraction."
"An inadequately loosened sphincter from short-duration EPBD may limit volume expansion of its encircled contents as in a compartment syndrome, thus [worsening] compression of the pancreatic duct from post-EPBD edema and [increasing] pancreatitis risk."
The researchers added that the longest reported EPBD duration is 5 minutes.
"It is unknown whether dilation duration longer than 5 minutes may further reduce pancreatitis risk, but the degree of sphincter loosening can only increase to a certain point. ... Further studies on EPBD with different durations will be helpful to corroborate our findings and determine the optimal duration."
The study was funded by grants from the Royal Society, London; the National Science Council, Taiwan; and the National Taiwan University Hospital, Taipei. The authors stated that they had no individual conflicts to disclose.
Endoscopic papillary balloon dilation (EPBD) using small diameter balloons (less than 10 mm) as an alterative to endoscopic sphincterotomy (ES) for removal of small bile duct stones is not new. Potential advantages of EPBD over ES are avoidance of bleeding and perforation while preserving biliary sphincter function. Potential disadvantages are potential for post-ERCP pancreatitis (PEP) and recurrence of choledocholithiasis, particularly in patients with an intact gallbladder.
Data on EPBD has been accrued from Asian populations, where the short-term and long-term outcomes are favorable, though with a significantly higher but acceptable risk of PEP. Unfortunately, the one randomized study from the U.S. was stopped prematurely due to two deaths from PEP. This has led to divergence in acceptance of EPBD between endoscopists in the East and West leading to the need for ways to reduce PEP after EPBD, including varying the duration of balloon inflation. In the present meta-analysis by Dr. Liao and his colleagues, longer duration of balloon dilation was found to be associated with less PEP than shorter duration. This finding may seem counterintuitive as longer duration would be expected to lead increased edema and obstruction of the pancreatic duct.
One factor not considered was the rapidity of dilation from zero pressure to the maximum. I believe this factor may be more important than duration since it influences shearing stress and force, tearing of tissue and subsequent peripapillary edema. Could it be that rapid inflation was more common when shorter-duration of inflation was performed? In short, the findings of Dr. Liao and his associates might influence the technique of EPBD in the East, but a more important question might be will these findings increase acceptance of EPBD in the West? Perhaps, but other ways to prevent PEP after EPBD, including the use of pancreatic duct stents and rectally administered non-steroidal anti-inflammatory agents, are more likely.
Todd Baron, M.D., is a professor of medicine and director of pancreaticobiliary endoscopy at the Mayo Clinic, Rochester, Minn. He has no relevant disclosures.
Endoscopic papillary balloon dilation (EPBD) using small diameter balloons (less than 10 mm) as an alterative to endoscopic sphincterotomy (ES) for removal of small bile duct stones is not new. Potential advantages of EPBD over ES are avoidance of bleeding and perforation while preserving biliary sphincter function. Potential disadvantages are potential for post-ERCP pancreatitis (PEP) and recurrence of choledocholithiasis, particularly in patients with an intact gallbladder.
Data on EPBD has been accrued from Asian populations, where the short-term and long-term outcomes are favorable, though with a significantly higher but acceptable risk of PEP. Unfortunately, the one randomized study from the U.S. was stopped prematurely due to two deaths from PEP. This has led to divergence in acceptance of EPBD between endoscopists in the East and West leading to the need for ways to reduce PEP after EPBD, including varying the duration of balloon inflation. In the present meta-analysis by Dr. Liao and his colleagues, longer duration of balloon dilation was found to be associated with less PEP than shorter duration. This finding may seem counterintuitive as longer duration would be expected to lead increased edema and obstruction of the pancreatic duct.
One factor not considered was the rapidity of dilation from zero pressure to the maximum. I believe this factor may be more important than duration since it influences shearing stress and force, tearing of tissue and subsequent peripapillary edema. Could it be that rapid inflation was more common when shorter-duration of inflation was performed? In short, the findings of Dr. Liao and his associates might influence the technique of EPBD in the East, but a more important question might be will these findings increase acceptance of EPBD in the West? Perhaps, but other ways to prevent PEP after EPBD, including the use of pancreatic duct stents and rectally administered non-steroidal anti-inflammatory agents, are more likely.
Todd Baron, M.D., is a professor of medicine and director of pancreaticobiliary endoscopy at the Mayo Clinic, Rochester, Minn. He has no relevant disclosures.
Endoscopic papillary balloon dilation (EPBD) using small diameter balloons (less than 10 mm) as an alterative to endoscopic sphincterotomy (ES) for removal of small bile duct stones is not new. Potential advantages of EPBD over ES are avoidance of bleeding and perforation while preserving biliary sphincter function. Potential disadvantages are potential for post-ERCP pancreatitis (PEP) and recurrence of choledocholithiasis, particularly in patients with an intact gallbladder.
Data on EPBD has been accrued from Asian populations, where the short-term and long-term outcomes are favorable, though with a significantly higher but acceptable risk of PEP. Unfortunately, the one randomized study from the U.S. was stopped prematurely due to two deaths from PEP. This has led to divergence in acceptance of EPBD between endoscopists in the East and West leading to the need for ways to reduce PEP after EPBD, including varying the duration of balloon inflation. In the present meta-analysis by Dr. Liao and his colleagues, longer duration of balloon dilation was found to be associated with less PEP than shorter duration. This finding may seem counterintuitive as longer duration would be expected to lead increased edema and obstruction of the pancreatic duct.
One factor not considered was the rapidity of dilation from zero pressure to the maximum. I believe this factor may be more important than duration since it influences shearing stress and force, tearing of tissue and subsequent peripapillary edema. Could it be that rapid inflation was more common when shorter-duration of inflation was performed? In short, the findings of Dr. Liao and his associates might influence the technique of EPBD in the East, but a more important question might be will these findings increase acceptance of EPBD in the West? Perhaps, but other ways to prevent PEP after EPBD, including the use of pancreatic duct stents and rectally administered non-steroidal anti-inflammatory agents, are more likely.
Todd Baron, M.D., is a professor of medicine and director of pancreaticobiliary endoscopy at the Mayo Clinic, Rochester, Minn. He has no relevant disclosures.
When treating choledocholithiasis, a shorter duration of endoscopic papillary balloon dilation increases, rather than decreases, the risk of postprocedure pancreatitis, reported Dr. Wei-Chih Liao and his colleagues in Clinical Gastroenterology and Hepatology.
"This meta-analysis contradicts the common belief that pancreatitis results from direct pancreatic duct compression during balloon dilation, and thus dilation duration should be short," he and his colleagues wrote. On the contrary, "[endoscopic papillary balloon dilation] with an adequate duration (around 5 minutes) has lower complication rates than the current standard of endoscopic sphincterotomy, and may be used as the first-line treatment for bile duct stones."
Dr. Liao, of the National Taiwan University College of Medicine, Taipei, conducted a systematic review of Medline, the Cochrane databases, and clinicaltrials.gov to identify randomized controlled trials of endoscopic papillary balloon dilation (EPBD), endoscopic sphincteroplasty, endoscopic balloon sphincter dilation, and endoscopic balloon dilation. Studies were excluded if dilation duration was not clearly reported.
Overall, 12 studies were included in the analysis: 11 compared EPBD with endoscopic sphincterotomy (EST); 4 compared short-duration EPBD (1 minute or less) with EST; and 7 looked at long-duration EPBD (more than 1 minute) versus EST.
Only one study compared long-duration EPBD with short-duration EPBD, they wrote (Clin. Gastroenterol. Hepatol. 2012 [doi: 10.1016/j.cgh.2012.05.017]).
First, the authors looked at the risk of pancreatitis when comparing EST to short-duration EPBD. They found that the latter had a significantly higher pancreatitis risk, with a pooled odds ratio of 3.87 for developing pancreatitis post procedure, compared with EST (95% confidence interval, 1.08-13.84).
However, long-duration EPBD did not pose a significantly higher risk compared with EST (OR, 1.14; 95% CI, 0.56-2.35).
Similarly, looking at overall complications, the researchers noted a trend toward a higher overall complication rate in short-duration EPBD compared with EST (OR, 1.71; 95% CI, 0.67-4.35). "By contrast, long EPBD seemed to have a lower overall complication rate (pooled OR, 0.61; 95% CI, 0.36-1.04)," wrote the authors.
The researchers also calculated the regression coefficient of dilation duration, and found it to be –0.69, "meaning that every 1-minute increase in dilation duration up to 3 minutes was associated with a 49.8% (95% CI, –9.4% –77.0%) reduction in OR," they wrote.
The finding was similar for overall complications, with every 1-minute increase in dilation duration up to 5 minutes associated with a 45.1% reduction in OR.
In an attempt to explain the findings, Dr. Liao noted that recent evidence suggests that EPBD with dilation duration of 1 minute or less "carries a higher risk of inadequate sphincter loosening, which increases the risks of pancreatitis and failed stone extraction."
"An inadequately loosened sphincter from short-duration EPBD may limit volume expansion of its encircled contents as in a compartment syndrome, thus [worsening] compression of the pancreatic duct from post-EPBD edema and [increasing] pancreatitis risk."
The researchers added that the longest reported EPBD duration is 5 minutes.
"It is unknown whether dilation duration longer than 5 minutes may further reduce pancreatitis risk, but the degree of sphincter loosening can only increase to a certain point. ... Further studies on EPBD with different durations will be helpful to corroborate our findings and determine the optimal duration."
The study was funded by grants from the Royal Society, London; the National Science Council, Taiwan; and the National Taiwan University Hospital, Taipei. The authors stated that they had no individual conflicts to disclose.
When treating choledocholithiasis, a shorter duration of endoscopic papillary balloon dilation increases, rather than decreases, the risk of postprocedure pancreatitis, reported Dr. Wei-Chih Liao and his colleagues in Clinical Gastroenterology and Hepatology.
"This meta-analysis contradicts the common belief that pancreatitis results from direct pancreatic duct compression during balloon dilation, and thus dilation duration should be short," he and his colleagues wrote. On the contrary, "[endoscopic papillary balloon dilation] with an adequate duration (around 5 minutes) has lower complication rates than the current standard of endoscopic sphincterotomy, and may be used as the first-line treatment for bile duct stones."
Dr. Liao, of the National Taiwan University College of Medicine, Taipei, conducted a systematic review of Medline, the Cochrane databases, and clinicaltrials.gov to identify randomized controlled trials of endoscopic papillary balloon dilation (EPBD), endoscopic sphincteroplasty, endoscopic balloon sphincter dilation, and endoscopic balloon dilation. Studies were excluded if dilation duration was not clearly reported.
Overall, 12 studies were included in the analysis: 11 compared EPBD with endoscopic sphincterotomy (EST); 4 compared short-duration EPBD (1 minute or less) with EST; and 7 looked at long-duration EPBD (more than 1 minute) versus EST.
Only one study compared long-duration EPBD with short-duration EPBD, they wrote (Clin. Gastroenterol. Hepatol. 2012 [doi: 10.1016/j.cgh.2012.05.017]).
First, the authors looked at the risk of pancreatitis when comparing EST to short-duration EPBD. They found that the latter had a significantly higher pancreatitis risk, with a pooled odds ratio of 3.87 for developing pancreatitis post procedure, compared with EST (95% confidence interval, 1.08-13.84).
However, long-duration EPBD did not pose a significantly higher risk compared with EST (OR, 1.14; 95% CI, 0.56-2.35).
Similarly, looking at overall complications, the researchers noted a trend toward a higher overall complication rate in short-duration EPBD compared with EST (OR, 1.71; 95% CI, 0.67-4.35). "By contrast, long EPBD seemed to have a lower overall complication rate (pooled OR, 0.61; 95% CI, 0.36-1.04)," wrote the authors.
The researchers also calculated the regression coefficient of dilation duration, and found it to be –0.69, "meaning that every 1-minute increase in dilation duration up to 3 minutes was associated with a 49.8% (95% CI, –9.4% –77.0%) reduction in OR," they wrote.
The finding was similar for overall complications, with every 1-minute increase in dilation duration up to 5 minutes associated with a 45.1% reduction in OR.
In an attempt to explain the findings, Dr. Liao noted that recent evidence suggests that EPBD with dilation duration of 1 minute or less "carries a higher risk of inadequate sphincter loosening, which increases the risks of pancreatitis and failed stone extraction."
"An inadequately loosened sphincter from short-duration EPBD may limit volume expansion of its encircled contents as in a compartment syndrome, thus [worsening] compression of the pancreatic duct from post-EPBD edema and [increasing] pancreatitis risk."
The researchers added that the longest reported EPBD duration is 5 minutes.
"It is unknown whether dilation duration longer than 5 minutes may further reduce pancreatitis risk, but the degree of sphincter loosening can only increase to a certain point. ... Further studies on EPBD with different durations will be helpful to corroborate our findings and determine the optimal duration."
The study was funded by grants from the Royal Society, London; the National Science Council, Taiwan; and the National Taiwan University Hospital, Taipei. The authors stated that they had no individual conflicts to disclose.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Major Finding: Endoscopic papillary balloon dilation for a short duration was associated with a greater risk for pancreatitis post procedure, compared with endoscopic sphincterotomy (odds ratio, 3.87), but longer-duration EPBD was less likely to cause pancreatitis.
Data Source: This study was a meta-analysis of 12 randomized controlled trials.
Disclosures: The study was funded by grants from the Royal Society, London; the National Science Council, Taiwan; and the National Taiwan University Hospital, Taipei. The authors stated that they had no individual conflicts to disclose.
Bariatric Surgery Prevents Type 2 Diabetes
Bariatric surgery reduced the incidence of type 2 diabetes by 78% compared with usual care at 15 years in a prospective, case-matched study of more than 3,000 obese adults.
This significant risk reduction was seen with all types of bariatric surgery and regardless of baseline body mass index. And, it occurred despite the fact that the matching process unexpectedly resulted in the bariatric surgery group having a higher mean body weight and more severe risk factors at baseline than the controls.
The impact of bariatric surgery was even greater, with an 87% risk reduction, for those with impaired fasting glucose at baseline, said Dr. Lena M.S. Carlsson of the Sahlgrenska Academy at the University of Gothenburg, Sweden, and her associates (N. Engl. J. Med. 2012;367:695-704).
"Our data indicate that bariatric surgery has a preventive effect on incident type 2 diabetes, particularly in participants with impaired fasting glucose. In contrast, baseline BMI did not influence the preventive effect of bariatric surgery on type 2 diabetes, implying that anthropometric data are not useful in the selection of candidates for bariatric surgery, whereas data on impaired fasting glucose may be helpful," the authors wrote.
The finding comes from the Swedish Obese Subjects (SOS) trial, which included 1,658 patients who chose to undergo bariatric surgery and 1,771 matched controls. All patients in both groups entered the study with the intention of losing weight. None had diabetes at baseline.
In the bariatric surgery group, the types of procedures were banding in 311, vertical banded gastroplasty in 1,140, and gastric bypass in 207. Patients in the control group received the customary treatment for obesity at their primary health care centers, which in Sweden ranges from advanced lifestyle modification – including recommendations regarding eating behavior, food selection, energy intake, and physical activity – to no treatment. About half (54%) of the controls reported receiving professional guidance in attempts to lose weight.
There were several significant differences between groups at baseline. The bariatric surgery group weighed an average of 6 kg more than did the controls, and had a greater mean BMI (42.4 vs. 40.2 kg/m2). They also had higher mean blood pressures and total cholesterol and triglyceride levels, and were more likely to smoke and to be less active.
After adjustment for follow-up of less than 15 years and for death, the 15-year participation rate was 54%. At 15 years, the bariatric surgery group had lost 31 kg after 1 year, but then regained weight, so the average loss at 10 and 15 years was about 20 kg. The control group never lost or gained more than 3 kg over the entire study period, regardless of whether they had professional help.
During the follow-up, type 2 diabetes developed in 110 of the bariatric surgery patients and in 392 controls, corresponding to incidence rates of 6.8 and 28.4 cases per 1,000 person-years, respectively (P less than .001). The unadjusted hazard ratio was 0.22, which dropped to 0.17 following multivariate adjustments. Aside from treatment group, other strong univariate predictors of diabetes outcome were baseline blood glucose and the presence or absence of impaired fasting glucose, Dr. Carlsson and her associates reported.
In a sensitivity analysis performed to account for the low participation rate, the impact of treatment on the incidence of type 2 diabetes was at least as strong after 2 years and 10 years of follow-up as after 15 years. All types of bariatric surgery were associated with a reduced incidence of diabetes, with no significant differences among them. There were also no differences by receipt of professional weight-loss assistance, or by BMI at baseline, the investigators noted.
A total of 3 patients (0.2%) died within 90 days of surgery, and 245 patients in the surgery group (15%) reported at least one complication. Of those, 46 (2.8%) were serious enough to require a reoperation.
The risk reduction seen among those with impaired fasting glucose was at least twice as large as the risk reduction achieved with lifestyle interventions in large, long-term trials of moderately obese people with prediabetes (Lancet 2006;368:1673-9, Lancet 2009;374:1677-86, and Lancet 2008;371:1783-9), the investigators noted.
The ongoing SOS study is supported by grants from the Swedish Research Council, the Swedish Foundation for Strategic Research to the Sahlgrenska Center for Cardiovascular and Metabolic Research, the Swedish federal government, the VINNOVA-VINNMER program, and the Wenner-Gren Foundations. The SOS study has previously been supported by grants to one of the authors from Hoffmann-La Roche, AstraZeneca, and other companies. Dr. Carlsson reported receiving consulting fees from AstraZeneca and owning stock in Sahltech. Other coinvestigators also had financial disclosures.
The long-term findings of the SOS study are both provocative and exciting, especially the findings suggesting that bariatric surgery may prevent the conversion of abnormalities in glucose metabolism to frank diabetes.
The findings of previous studies, showing that bariatric surgery can have a prolonged, positive effect on blood sugar beyond that attainable with medication, have led to speculation about whether surgery might be considered earlier in the course of disease in patients with adult-onset diabetes.
However, it remains impractical and unjustified to contemplate the performance of bariatric surgery in the millions of eligible obese adults. And to be certain, the authors do not suggest such an approach. Rather, the current study should provide an impetus to develop a more complete understanding of the mechanisms by which the various bariatric procedures exert their beneficial effects. Such understanding will be important because it will enable the identification of individuals who are the most appropriate candidates for surgery.
The cause of type 2 diabetes is multifactorial, and this long-term study shows that surgery did not prevent the development of diabetes in all patients. Furthermore, it is possible that interventions that are even less invasive may accomplish the very desirable goal of decreasing the incidence of type 2 diabetes and its attendant complications.
Danny O. Jacobs, M.D., is chair of surgery at the Duke University School of Medicine, Durham, N.C. These remarks were taken from his editorial accompanying Dr. Carlson’s report (N. Engl. J. Med. 2012;367:764-5). Dr. Jacobs has consulting, research, and/or educational services working relationships with Ethicon, Surgisphere, and other companies.
The long-term findings of the SOS study are both provocative and exciting, especially the findings suggesting that bariatric surgery may prevent the conversion of abnormalities in glucose metabolism to frank diabetes.
The findings of previous studies, showing that bariatric surgery can have a prolonged, positive effect on blood sugar beyond that attainable with medication, have led to speculation about whether surgery might be considered earlier in the course of disease in patients with adult-onset diabetes.
However, it remains impractical and unjustified to contemplate the performance of bariatric surgery in the millions of eligible obese adults. And to be certain, the authors do not suggest such an approach. Rather, the current study should provide an impetus to develop a more complete understanding of the mechanisms by which the various bariatric procedures exert their beneficial effects. Such understanding will be important because it will enable the identification of individuals who are the most appropriate candidates for surgery.
The cause of type 2 diabetes is multifactorial, and this long-term study shows that surgery did not prevent the development of diabetes in all patients. Furthermore, it is possible that interventions that are even less invasive may accomplish the very desirable goal of decreasing the incidence of type 2 diabetes and its attendant complications.
Danny O. Jacobs, M.D., is chair of surgery at the Duke University School of Medicine, Durham, N.C. These remarks were taken from his editorial accompanying Dr. Carlson’s report (N. Engl. J. Med. 2012;367:764-5). Dr. Jacobs has consulting, research, and/or educational services working relationships with Ethicon, Surgisphere, and other companies.
The long-term findings of the SOS study are both provocative and exciting, especially the findings suggesting that bariatric surgery may prevent the conversion of abnormalities in glucose metabolism to frank diabetes.
The findings of previous studies, showing that bariatric surgery can have a prolonged, positive effect on blood sugar beyond that attainable with medication, have led to speculation about whether surgery might be considered earlier in the course of disease in patients with adult-onset diabetes.
However, it remains impractical and unjustified to contemplate the performance of bariatric surgery in the millions of eligible obese adults. And to be certain, the authors do not suggest such an approach. Rather, the current study should provide an impetus to develop a more complete understanding of the mechanisms by which the various bariatric procedures exert their beneficial effects. Such understanding will be important because it will enable the identification of individuals who are the most appropriate candidates for surgery.
The cause of type 2 diabetes is multifactorial, and this long-term study shows that surgery did not prevent the development of diabetes in all patients. Furthermore, it is possible that interventions that are even less invasive may accomplish the very desirable goal of decreasing the incidence of type 2 diabetes and its attendant complications.
Danny O. Jacobs, M.D., is chair of surgery at the Duke University School of Medicine, Durham, N.C. These remarks were taken from his editorial accompanying Dr. Carlson’s report (N. Engl. J. Med. 2012;367:764-5). Dr. Jacobs has consulting, research, and/or educational services working relationships with Ethicon, Surgisphere, and other companies.
Bariatric surgery reduced the incidence of type 2 diabetes by 78% compared with usual care at 15 years in a prospective, case-matched study of more than 3,000 obese adults.
This significant risk reduction was seen with all types of bariatric surgery and regardless of baseline body mass index. And, it occurred despite the fact that the matching process unexpectedly resulted in the bariatric surgery group having a higher mean body weight and more severe risk factors at baseline than the controls.
The impact of bariatric surgery was even greater, with an 87% risk reduction, for those with impaired fasting glucose at baseline, said Dr. Lena M.S. Carlsson of the Sahlgrenska Academy at the University of Gothenburg, Sweden, and her associates (N. Engl. J. Med. 2012;367:695-704).
"Our data indicate that bariatric surgery has a preventive effect on incident type 2 diabetes, particularly in participants with impaired fasting glucose. In contrast, baseline BMI did not influence the preventive effect of bariatric surgery on type 2 diabetes, implying that anthropometric data are not useful in the selection of candidates for bariatric surgery, whereas data on impaired fasting glucose may be helpful," the authors wrote.
The finding comes from the Swedish Obese Subjects (SOS) trial, which included 1,658 patients who chose to undergo bariatric surgery and 1,771 matched controls. All patients in both groups entered the study with the intention of losing weight. None had diabetes at baseline.
In the bariatric surgery group, the types of procedures were banding in 311, vertical banded gastroplasty in 1,140, and gastric bypass in 207. Patients in the control group received the customary treatment for obesity at their primary health care centers, which in Sweden ranges from advanced lifestyle modification – including recommendations regarding eating behavior, food selection, energy intake, and physical activity – to no treatment. About half (54%) of the controls reported receiving professional guidance in attempts to lose weight.
There were several significant differences between groups at baseline. The bariatric surgery group weighed an average of 6 kg more than did the controls, and had a greater mean BMI (42.4 vs. 40.2 kg/m2). They also had higher mean blood pressures and total cholesterol and triglyceride levels, and were more likely to smoke and to be less active.
After adjustment for follow-up of less than 15 years and for death, the 15-year participation rate was 54%. At 15 years, the bariatric surgery group had lost 31 kg after 1 year, but then regained weight, so the average loss at 10 and 15 years was about 20 kg. The control group never lost or gained more than 3 kg over the entire study period, regardless of whether they had professional help.
During the follow-up, type 2 diabetes developed in 110 of the bariatric surgery patients and in 392 controls, corresponding to incidence rates of 6.8 and 28.4 cases per 1,000 person-years, respectively (P less than .001). The unadjusted hazard ratio was 0.22, which dropped to 0.17 following multivariate adjustments. Aside from treatment group, other strong univariate predictors of diabetes outcome were baseline blood glucose and the presence or absence of impaired fasting glucose, Dr. Carlsson and her associates reported.
In a sensitivity analysis performed to account for the low participation rate, the impact of treatment on the incidence of type 2 diabetes was at least as strong after 2 years and 10 years of follow-up as after 15 years. All types of bariatric surgery were associated with a reduced incidence of diabetes, with no significant differences among them. There were also no differences by receipt of professional weight-loss assistance, or by BMI at baseline, the investigators noted.
A total of 3 patients (0.2%) died within 90 days of surgery, and 245 patients in the surgery group (15%) reported at least one complication. Of those, 46 (2.8%) were serious enough to require a reoperation.
The risk reduction seen among those with impaired fasting glucose was at least twice as large as the risk reduction achieved with lifestyle interventions in large, long-term trials of moderately obese people with prediabetes (Lancet 2006;368:1673-9, Lancet 2009;374:1677-86, and Lancet 2008;371:1783-9), the investigators noted.
The ongoing SOS study is supported by grants from the Swedish Research Council, the Swedish Foundation for Strategic Research to the Sahlgrenska Center for Cardiovascular and Metabolic Research, the Swedish federal government, the VINNOVA-VINNMER program, and the Wenner-Gren Foundations. The SOS study has previously been supported by grants to one of the authors from Hoffmann-La Roche, AstraZeneca, and other companies. Dr. Carlsson reported receiving consulting fees from AstraZeneca and owning stock in Sahltech. Other coinvestigators also had financial disclosures.
Bariatric surgery reduced the incidence of type 2 diabetes by 78% compared with usual care at 15 years in a prospective, case-matched study of more than 3,000 obese adults.
This significant risk reduction was seen with all types of bariatric surgery and regardless of baseline body mass index. And, it occurred despite the fact that the matching process unexpectedly resulted in the bariatric surgery group having a higher mean body weight and more severe risk factors at baseline than the controls.
The impact of bariatric surgery was even greater, with an 87% risk reduction, for those with impaired fasting glucose at baseline, said Dr. Lena M.S. Carlsson of the Sahlgrenska Academy at the University of Gothenburg, Sweden, and her associates (N. Engl. J. Med. 2012;367:695-704).
"Our data indicate that bariatric surgery has a preventive effect on incident type 2 diabetes, particularly in participants with impaired fasting glucose. In contrast, baseline BMI did not influence the preventive effect of bariatric surgery on type 2 diabetes, implying that anthropometric data are not useful in the selection of candidates for bariatric surgery, whereas data on impaired fasting glucose may be helpful," the authors wrote.
The finding comes from the Swedish Obese Subjects (SOS) trial, which included 1,658 patients who chose to undergo bariatric surgery and 1,771 matched controls. All patients in both groups entered the study with the intention of losing weight. None had diabetes at baseline.
In the bariatric surgery group, the types of procedures were banding in 311, vertical banded gastroplasty in 1,140, and gastric bypass in 207. Patients in the control group received the customary treatment for obesity at their primary health care centers, which in Sweden ranges from advanced lifestyle modification – including recommendations regarding eating behavior, food selection, energy intake, and physical activity – to no treatment. About half (54%) of the controls reported receiving professional guidance in attempts to lose weight.
There were several significant differences between groups at baseline. The bariatric surgery group weighed an average of 6 kg more than did the controls, and had a greater mean BMI (42.4 vs. 40.2 kg/m2). They also had higher mean blood pressures and total cholesterol and triglyceride levels, and were more likely to smoke and to be less active.
After adjustment for follow-up of less than 15 years and for death, the 15-year participation rate was 54%. At 15 years, the bariatric surgery group had lost 31 kg after 1 year, but then regained weight, so the average loss at 10 and 15 years was about 20 kg. The control group never lost or gained more than 3 kg over the entire study period, regardless of whether they had professional help.
During the follow-up, type 2 diabetes developed in 110 of the bariatric surgery patients and in 392 controls, corresponding to incidence rates of 6.8 and 28.4 cases per 1,000 person-years, respectively (P less than .001). The unadjusted hazard ratio was 0.22, which dropped to 0.17 following multivariate adjustments. Aside from treatment group, other strong univariate predictors of diabetes outcome were baseline blood glucose and the presence or absence of impaired fasting glucose, Dr. Carlsson and her associates reported.
In a sensitivity analysis performed to account for the low participation rate, the impact of treatment on the incidence of type 2 diabetes was at least as strong after 2 years and 10 years of follow-up as after 15 years. All types of bariatric surgery were associated with a reduced incidence of diabetes, with no significant differences among them. There were also no differences by receipt of professional weight-loss assistance, or by BMI at baseline, the investigators noted.
A total of 3 patients (0.2%) died within 90 days of surgery, and 245 patients in the surgery group (15%) reported at least one complication. Of those, 46 (2.8%) were serious enough to require a reoperation.
The risk reduction seen among those with impaired fasting glucose was at least twice as large as the risk reduction achieved with lifestyle interventions in large, long-term trials of moderately obese people with prediabetes (Lancet 2006;368:1673-9, Lancet 2009;374:1677-86, and Lancet 2008;371:1783-9), the investigators noted.
The ongoing SOS study is supported by grants from the Swedish Research Council, the Swedish Foundation for Strategic Research to the Sahlgrenska Center for Cardiovascular and Metabolic Research, the Swedish federal government, the VINNOVA-VINNMER program, and the Wenner-Gren Foundations. The SOS study has previously been supported by grants to one of the authors from Hoffmann-La Roche, AstraZeneca, and other companies. Dr. Carlsson reported receiving consulting fees from AstraZeneca and owning stock in Sahltech. Other coinvestigators also had financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: During follow-up, type 2 diabetes developed in 110 of the bariatric surgery patients and in 392 controls, corresponding to incidence rates of 6.8 versus 28.4 cases per 1,000 person-years, respectively (P less than .001).
Data Source: The Swedish Obese Subjects (SOS) study is a prospective, case-matched 15-year comparison of diabetes incidence between 1,658 obese nondiabetic individuals who chose to undergo bariatric surgery and 1,771 who received usual weight loss management.
Disclosures: The ongoing SOS study is supported by grants from the Swedish Research Council, the Swedish Foundation for Strategic Research to the Sahlgrenska Center for Cardiovascular and Metabolic Research, the Swedish federal government, the VINNOVA-VINNMER program, and the Wenner-Gren Foundations. The SOS study has previously been supported by grants to one of the authors from Hoffmann-La Roche, AstraZeneca, and other companies. Dr. Carlsson reported receiving consulting fees from AstraZeneca and owning stock in Sahltech. Other coinvestigators also had financial disclosures.
Transfusion Rates Vary Widely at Academic Hospitals
Wide variations in perioperative blood transfusion rates among patients undergoing major noncardiac procedures across U.S. hospitals highlight the need to further investigate evidence-based "transfusion triggers" in this population of surgical patients, according to a study published ahead of print in Annals of Surgery.
"In light of the increased risk of mortality and major complications associated with blood transfusion, the extensive variability in hospital transfusion practice in noncardiac surgery may represent an important opportunity to improve surgical outcomes," wrote Feng Qian, Ph.D., of the University of Rochester (N.Y.), and associates.
The researchers used the University HealthSystem Consortium hospital database to compare transfusion rates of allogeneic red blood cells, fresh frozen plasma, and platelets in patients undergoing elective primary total hip replacement (54,405 patients), colectomy (21,334), or pancreaticoduodenectomy (7,929) at 77 hospitals between June 2006 and September 2010. Most of the hospitals were teaching hospitals with at least 500 beds.
Transfusion rates varied widely before and after adjustment for comorbidities and other patient risk factors. Patients who were treated in hospitals with high rates of transfusions were about twice as likely to receive a blood transfusion as were patients at hospitals with average transfusion rates (Ann. Surg. 2012 July 13[doi:10.1097/SLA.0b013e31825ffc37]).
In hospitals where the transfusion rate for one procedure was high, transfusion rates also tended to be high for the other two procedures. There was some evidence indicating that a higher volume of surgical cases was associated with lower transfusion rates.
After adjusting for patient risk factors, the authors determined that transfusion rates for the different blood components among those undergoing a total hip replacement ranged from 1.3% to almost 75% (red blood cells), from 0.1% to 7.7% (fresh frozen plasma), and from 0.1% to 2% (platelets). Among colectomy patients, transfusion rates ranged from 1.9% to 47.8% (RBCs), from 1.4% to 17.7% (fresh frozen plasma), and from 1.3% to 6.2% (platelets). Among those undergoing a pancreaticoduodenectomy, the rates ranged from 3% to 78.6% (RBCs), from 1% to 47% (fresh frozen plasma), and from 1.4% to 12.6% (platelets).
The variability, the authors said, "reflects, in part, the complexity of the medical decision-making process underlying transfusion therapy." Because the data included patients from 90% of academic medical centers in the United States, the results provide "a broad and contemporary picture of transfusion practices in academic surgical centers" and "reflect transfusion practices that are being taught to the next generation of academic and private-practice clinicians during residency training," they noted.
To the best of their knowledge, the authors said, there are no large randomized studies that have compared liberal and restrictive transfusion strategies in noncardiac surgery patients, and they believe that such trials are "urgently needed to better define evidence-based transfusion triggers for patients undergoing noncardiac surgery."
The study was supported by a grant from the Agency for Healthcare and Quality Research and funding from the department of anesthesiology at the University of Rochester. No disclosures were reported by the authors.
Wide variations in perioperative blood transfusion rates among patients undergoing major noncardiac procedures across U.S. hospitals highlight the need to further investigate evidence-based "transfusion triggers" in this population of surgical patients, according to a study published ahead of print in Annals of Surgery.
"In light of the increased risk of mortality and major complications associated with blood transfusion, the extensive variability in hospital transfusion practice in noncardiac surgery may represent an important opportunity to improve surgical outcomes," wrote Feng Qian, Ph.D., of the University of Rochester (N.Y.), and associates.
The researchers used the University HealthSystem Consortium hospital database to compare transfusion rates of allogeneic red blood cells, fresh frozen plasma, and platelets in patients undergoing elective primary total hip replacement (54,405 patients), colectomy (21,334), or pancreaticoduodenectomy (7,929) at 77 hospitals between June 2006 and September 2010. Most of the hospitals were teaching hospitals with at least 500 beds.
Transfusion rates varied widely before and after adjustment for comorbidities and other patient risk factors. Patients who were treated in hospitals with high rates of transfusions were about twice as likely to receive a blood transfusion as were patients at hospitals with average transfusion rates (Ann. Surg. 2012 July 13[doi:10.1097/SLA.0b013e31825ffc37]).
In hospitals where the transfusion rate for one procedure was high, transfusion rates also tended to be high for the other two procedures. There was some evidence indicating that a higher volume of surgical cases was associated with lower transfusion rates.
After adjusting for patient risk factors, the authors determined that transfusion rates for the different blood components among those undergoing a total hip replacement ranged from 1.3% to almost 75% (red blood cells), from 0.1% to 7.7% (fresh frozen plasma), and from 0.1% to 2% (platelets). Among colectomy patients, transfusion rates ranged from 1.9% to 47.8% (RBCs), from 1.4% to 17.7% (fresh frozen plasma), and from 1.3% to 6.2% (platelets). Among those undergoing a pancreaticoduodenectomy, the rates ranged from 3% to 78.6% (RBCs), from 1% to 47% (fresh frozen plasma), and from 1.4% to 12.6% (platelets).
The variability, the authors said, "reflects, in part, the complexity of the medical decision-making process underlying transfusion therapy." Because the data included patients from 90% of academic medical centers in the United States, the results provide "a broad and contemporary picture of transfusion practices in academic surgical centers" and "reflect transfusion practices that are being taught to the next generation of academic and private-practice clinicians during residency training," they noted.
To the best of their knowledge, the authors said, there are no large randomized studies that have compared liberal and restrictive transfusion strategies in noncardiac surgery patients, and they believe that such trials are "urgently needed to better define evidence-based transfusion triggers for patients undergoing noncardiac surgery."
The study was supported by a grant from the Agency for Healthcare and Quality Research and funding from the department of anesthesiology at the University of Rochester. No disclosures were reported by the authors.
Wide variations in perioperative blood transfusion rates among patients undergoing major noncardiac procedures across U.S. hospitals highlight the need to further investigate evidence-based "transfusion triggers" in this population of surgical patients, according to a study published ahead of print in Annals of Surgery.
"In light of the increased risk of mortality and major complications associated with blood transfusion, the extensive variability in hospital transfusion practice in noncardiac surgery may represent an important opportunity to improve surgical outcomes," wrote Feng Qian, Ph.D., of the University of Rochester (N.Y.), and associates.
The researchers used the University HealthSystem Consortium hospital database to compare transfusion rates of allogeneic red blood cells, fresh frozen plasma, and platelets in patients undergoing elective primary total hip replacement (54,405 patients), colectomy (21,334), or pancreaticoduodenectomy (7,929) at 77 hospitals between June 2006 and September 2010. Most of the hospitals were teaching hospitals with at least 500 beds.
Transfusion rates varied widely before and after adjustment for comorbidities and other patient risk factors. Patients who were treated in hospitals with high rates of transfusions were about twice as likely to receive a blood transfusion as were patients at hospitals with average transfusion rates (Ann. Surg. 2012 July 13[doi:10.1097/SLA.0b013e31825ffc37]).
In hospitals where the transfusion rate for one procedure was high, transfusion rates also tended to be high for the other two procedures. There was some evidence indicating that a higher volume of surgical cases was associated with lower transfusion rates.
After adjusting for patient risk factors, the authors determined that transfusion rates for the different blood components among those undergoing a total hip replacement ranged from 1.3% to almost 75% (red blood cells), from 0.1% to 7.7% (fresh frozen plasma), and from 0.1% to 2% (platelets). Among colectomy patients, transfusion rates ranged from 1.9% to 47.8% (RBCs), from 1.4% to 17.7% (fresh frozen plasma), and from 1.3% to 6.2% (platelets). Among those undergoing a pancreaticoduodenectomy, the rates ranged from 3% to 78.6% (RBCs), from 1% to 47% (fresh frozen plasma), and from 1.4% to 12.6% (platelets).
The variability, the authors said, "reflects, in part, the complexity of the medical decision-making process underlying transfusion therapy." Because the data included patients from 90% of academic medical centers in the United States, the results provide "a broad and contemporary picture of transfusion practices in academic surgical centers" and "reflect transfusion practices that are being taught to the next generation of academic and private-practice clinicians during residency training," they noted.
To the best of their knowledge, the authors said, there are no large randomized studies that have compared liberal and restrictive transfusion strategies in noncardiac surgery patients, and they believe that such trials are "urgently needed to better define evidence-based transfusion triggers for patients undergoing noncardiac surgery."
The study was supported by a grant from the Agency for Healthcare and Quality Research and funding from the department of anesthesiology at the University of Rochester. No disclosures were reported by the authors.
FROM THE ANNALS OF SURGERY
Major Finding: Transfusion rates of red blood cells, fresh frozen plasma, and platelets among patients undergoing noncardiac procedures varied widely across different U.S. academic-affiliated hospitals.
Data Source: Data from a national database of academic medical centers were used to compare transfusions in patients undergoing one of three elective noncardiac surgical procedures at 77 academic hospitals between June 2006 and September 2010.
Disclosures: The study was supported by a grant from the Agency for Healthcare and Quality Research and funding from the department of anesthesiology at the University of Rochester (N.Y.). The authors reported no disclosures.
Reversal of Lap-Band to Sleeve Gastrectomy Feasible
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: Weight loss was more pronounced among patients who underwent reversal of Lap-Band to sleeve gastrectomy because of band slippage, erosion, or infection than because of dissatisfaction with weight loss (mean total BMI loss, –15.8 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
Data Source: The study consisted of 34 patients who underwent reversal of Lap-Band to sleeve gastrectomy at two centers from January 2004 to October 2011.
Disclosures: Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.