User login
New European restrictions on topiramate in pregnancy
While it’s well known that topiramate can cause major congenital malformations and fetal growth restriction when used during pregnancy, recent data also suggest a possibly increased risk for neurodevelopmental disorders when topiramate is used during pregnancy, the EMA said in a statement.
The data include two observational studies that showed children born to mothers with epilepsy and who were exposed to topiramate in the womb may have a two- to threefold higher risk for neurodevelopmental disorders, in particular autism spectrum disorders (ASD), intellectual disability, or attention deficit hyperactivity disorder (ADHD), compared with children born to mothers with epilepsy not taking antiepileptic medication.
For patients using topiramate for the treatment of epilepsy, the PRAC now recommends that the medicine not be used during pregnancy unless no other suitable treatment is available.
The PRAC had also recommended a pregnancy prevention program to avoid exposure of the developing fetus to topiramate. “These measures will inform any woman or girl who is able to have children of the risks of taking topiramate during pregnancy and the need to avoid becoming pregnant while taking topiramate,” the EMA said.
Regardless of indication, the agency said topiramate should be used in women of childbearing age only when the following conditions of the pregnancy prevention program are met:
- A pregnancy test before starting treatment.
- Counseling about the risks of topiramate treatment and the need for highly effective contraception throughout treatment.
- A review of ongoing treatment at least annually by completion of a risk awareness form.
The PRAC recommends that health care professionals ensure women of childbearing age are fully aware of the risks of taking topiramate during pregnancy. The committee noted that alternative treatment options should be considered and the need for topiramate treatment should be reassessed at least annually.
The product information for topiramate-containing medicines will be updated to further highlight the risks for neurodevelopmental disorders and the additional safety measures to be taken.
Patients and health care professionals will be provided with educational materials regarding the risks of using topiramate during pregnancy, and a patient card will be provided to the patient with each medicine package. A visible warning will also be added to the outer packaging of the medicine.
The new PRAC recommendations will be sent to the Coordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh), which will adopt a position.
A version of this article first appeared on Medscape.com.
While it’s well known that topiramate can cause major congenital malformations and fetal growth restriction when used during pregnancy, recent data also suggest a possibly increased risk for neurodevelopmental disorders when topiramate is used during pregnancy, the EMA said in a statement.
The data include two observational studies that showed children born to mothers with epilepsy and who were exposed to topiramate in the womb may have a two- to threefold higher risk for neurodevelopmental disorders, in particular autism spectrum disorders (ASD), intellectual disability, or attention deficit hyperactivity disorder (ADHD), compared with children born to mothers with epilepsy not taking antiepileptic medication.
For patients using topiramate for the treatment of epilepsy, the PRAC now recommends that the medicine not be used during pregnancy unless no other suitable treatment is available.
The PRAC had also recommended a pregnancy prevention program to avoid exposure of the developing fetus to topiramate. “These measures will inform any woman or girl who is able to have children of the risks of taking topiramate during pregnancy and the need to avoid becoming pregnant while taking topiramate,” the EMA said.
Regardless of indication, the agency said topiramate should be used in women of childbearing age only when the following conditions of the pregnancy prevention program are met:
- A pregnancy test before starting treatment.
- Counseling about the risks of topiramate treatment and the need for highly effective contraception throughout treatment.
- A review of ongoing treatment at least annually by completion of a risk awareness form.
The PRAC recommends that health care professionals ensure women of childbearing age are fully aware of the risks of taking topiramate during pregnancy. The committee noted that alternative treatment options should be considered and the need for topiramate treatment should be reassessed at least annually.
The product information for topiramate-containing medicines will be updated to further highlight the risks for neurodevelopmental disorders and the additional safety measures to be taken.
Patients and health care professionals will be provided with educational materials regarding the risks of using topiramate during pregnancy, and a patient card will be provided to the patient with each medicine package. A visible warning will also be added to the outer packaging of the medicine.
The new PRAC recommendations will be sent to the Coordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh), which will adopt a position.
A version of this article first appeared on Medscape.com.
While it’s well known that topiramate can cause major congenital malformations and fetal growth restriction when used during pregnancy, recent data also suggest a possibly increased risk for neurodevelopmental disorders when topiramate is used during pregnancy, the EMA said in a statement.
The data include two observational studies that showed children born to mothers with epilepsy and who were exposed to topiramate in the womb may have a two- to threefold higher risk for neurodevelopmental disorders, in particular autism spectrum disorders (ASD), intellectual disability, or attention deficit hyperactivity disorder (ADHD), compared with children born to mothers with epilepsy not taking antiepileptic medication.
For patients using topiramate for the treatment of epilepsy, the PRAC now recommends that the medicine not be used during pregnancy unless no other suitable treatment is available.
The PRAC had also recommended a pregnancy prevention program to avoid exposure of the developing fetus to topiramate. “These measures will inform any woman or girl who is able to have children of the risks of taking topiramate during pregnancy and the need to avoid becoming pregnant while taking topiramate,” the EMA said.
Regardless of indication, the agency said topiramate should be used in women of childbearing age only when the following conditions of the pregnancy prevention program are met:
- A pregnancy test before starting treatment.
- Counseling about the risks of topiramate treatment and the need for highly effective contraception throughout treatment.
- A review of ongoing treatment at least annually by completion of a risk awareness form.
The PRAC recommends that health care professionals ensure women of childbearing age are fully aware of the risks of taking topiramate during pregnancy. The committee noted that alternative treatment options should be considered and the need for topiramate treatment should be reassessed at least annually.
The product information for topiramate-containing medicines will be updated to further highlight the risks for neurodevelopmental disorders and the additional safety measures to be taken.
Patients and health care professionals will be provided with educational materials regarding the risks of using topiramate during pregnancy, and a patient card will be provided to the patient with each medicine package. A visible warning will also be added to the outer packaging of the medicine.
The new PRAC recommendations will be sent to the Coordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh), which will adopt a position.
A version of this article first appeared on Medscape.com.
Global burden of brain disorders surpasses cardiovascular disease and cancer
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AI model interprets EEGs with near-perfect accuracy
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
New DEA CME mandate affects 2 million prescribers
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
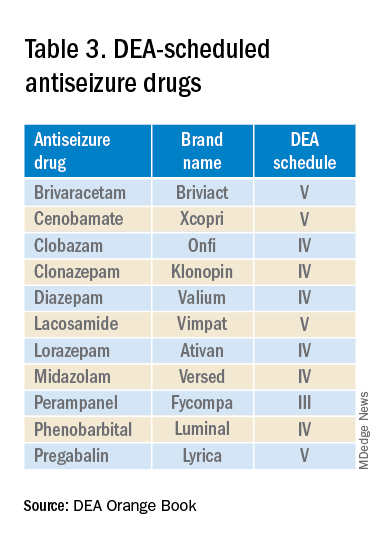
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.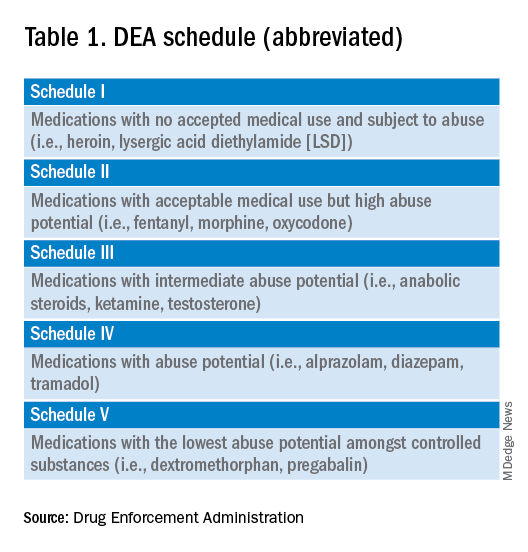
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 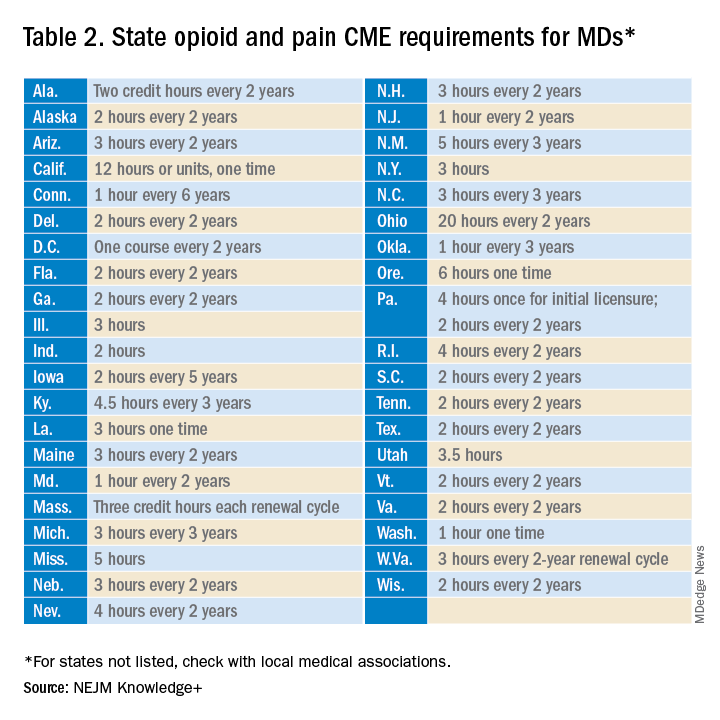
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
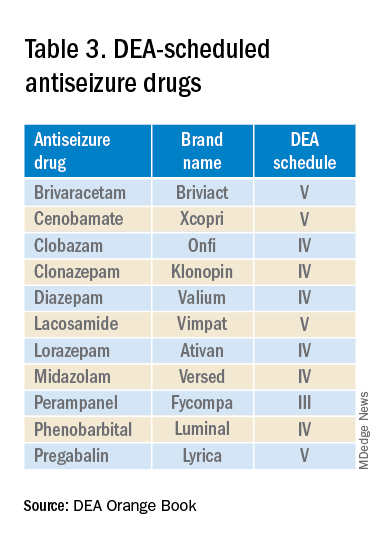
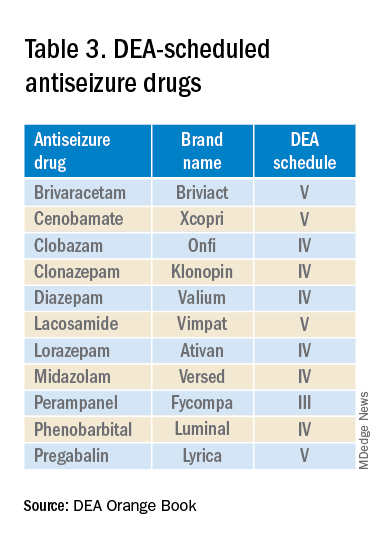
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.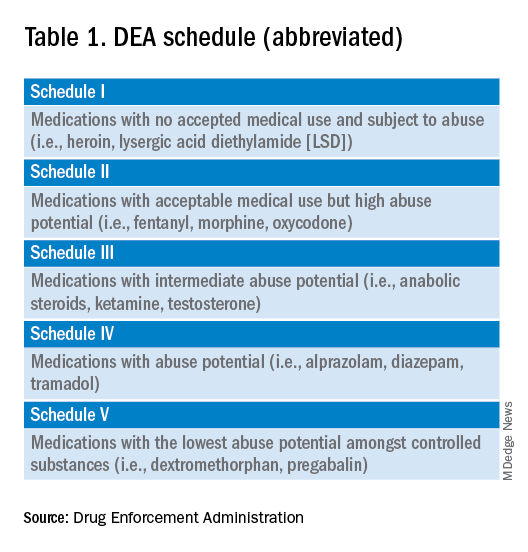
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 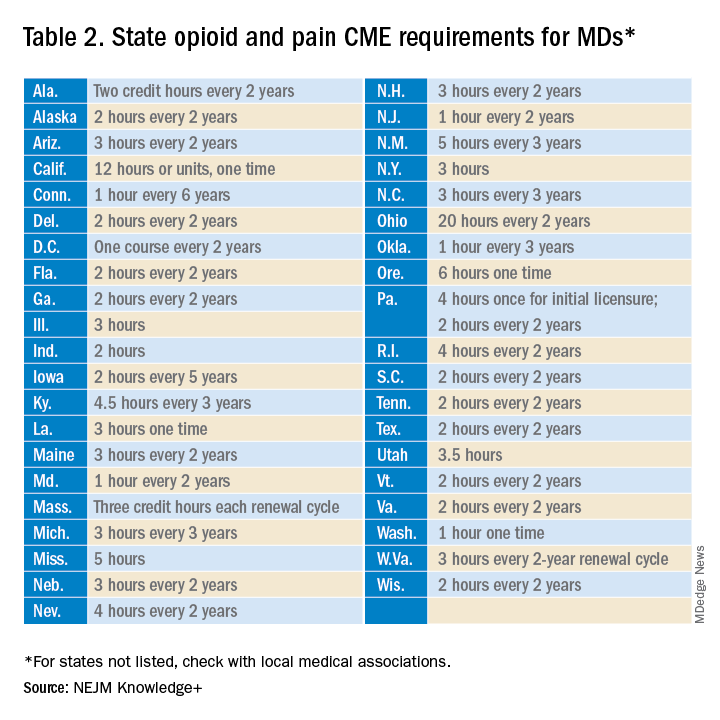
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.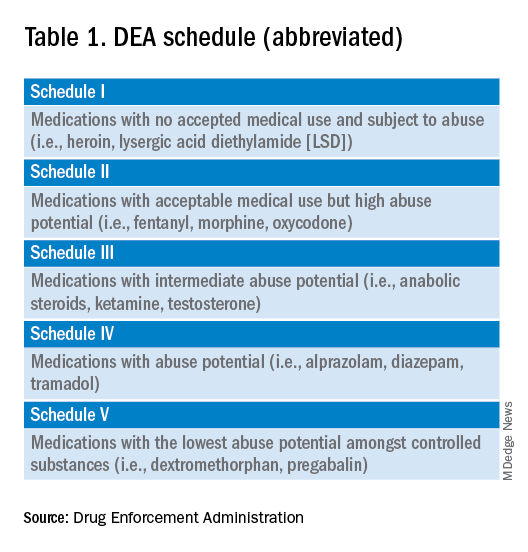
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 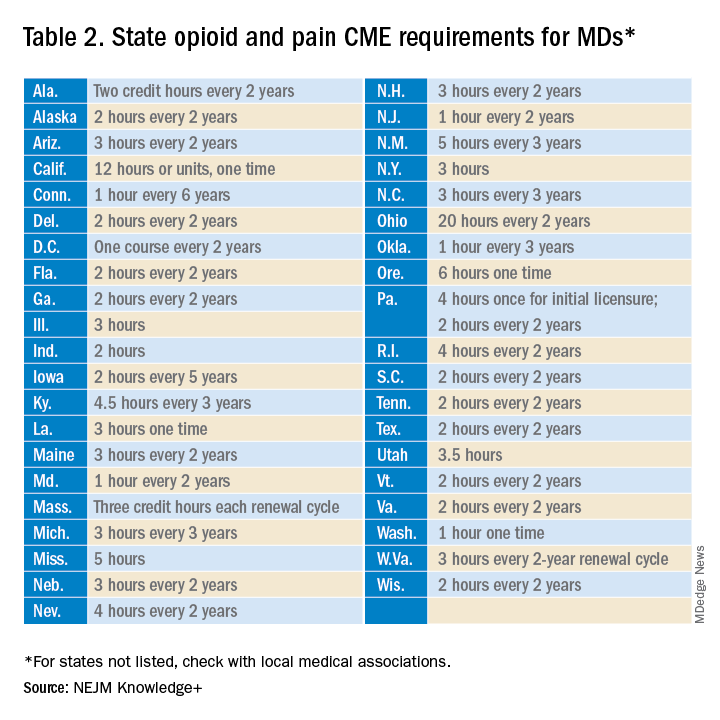
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
Noninvasive testing in midlife flags late-onset epilepsy risk
BOSTON – Noninvasive tests performed in midlife may help identify people who are at risk of late-onset epilepsy, a new study suggests. New data from the Framingham Heart Study show those who scored better on a neurocognitive test that measures executive function were 75% less likely to develop late-onset epilepsy.
An analysis of MRI revealed that those with higher cortical volumes also had a lower risk of epilepsy later in life, while those with higher white matter hyperintensities had an increased risk.
The study could help identify at-risk individuals years before symptoms of epilepsy appear.
,” said lead investigator Maria Stefanidou, MD, assistant professor of neurology at Boston University.
The findings were presented at the 2023 annual meeting of the American Academy of Neurology.
Protection against late-onset epilepsy?
Hypertension and stroke are known risk factors for late-onset epilepsy. Dementia is also a known risk factor. But in about 30% of cases, the cause of epilepsy in older individuals is unknown.
For this study, investigators analyzed data from the offspring cohort of the Framingham Heart Study. Participants were at least 45 years old; underwent neuropsychological evaluation and brain MRI; and had no prior history of stroke, dementia, or epilepsy. Cognitive measures included Visual Reproductions Delayed Recall, Logical Memory Delayed Recall, Similarities, Trail Making B-A (TrB-TrA), and the Hooper Visual Organization Test.
Participants also underwent an MRI to measure total cerebral brain volume, cortical gray matter volume, white matter hyperintensities, and hippocampal volume.
After a mean follow-up of 13.5 years, late-onset epilepsy was diagnosed in 31 of participants who underwent neuropsychological testing (n = 2,349) and in 27 of those who underwent MRI (n = 2,056).
Better performance on the TrB-TrA test (a measure of executive function, processing speed, and occult vascular injury) was associated with a reduced risk of late-onset epilepsy (adjusted hazard ratio, 0.25; P = .011).
The findings held even after adjusting for age, sex, educational level, and known risk factors for late-onset epilepsy, such as hypertension (aHR, 0.30; P = .0401).
Higher white matter hyperintensities, a measure of occult vascular injury, was associated with increased epilepsy risk (aHR, 1.5; P = .042) when adjusted only for age, sex, and education, but was no longer significant after adjusting for hypertension and other risk factors (aHR, 1.47; P = .065).
The analysis also revealed that participants with a higher cortical gray matter volume had a lower risk for late-onset epilepsy (aHR, 0.73; P = .001).
“There is increasing literature supporting that late-onset epilepsy may be secondary to accumulative occult cerebrovascular and neurodegenerative processes that occur during aging,” Dr. Stefanidou said. “Our findings likely reflect that a lesser degree of occult vascular brain injury in midlife may be protective against late-onset epilepsy.”
However, the epidemiological study points to association, not causation, Dr. Stefanidou cautions.
“Further studies will be needed to study our observations in the clinical setting,” she said.
‘Intriguing’ findings
Commenting on the findings, Joseph Sirven, MD, a neurologist at the Mayo Clinic in Jacksonville, Fla., said the findings are “intriguing,” but also raise some questions. “Late-onset epilepsy remains an issue for many and it’s common,” said Dr. Sirven, who has patients with late-onset epilepsy.
Dr. Sirven was particularly interested in the findings on white matter hyperintensities. “Hippocampal volumes have been used but not so much cortical volumes,” he said. “I would like to know more about how white matter changes suggest pathology that would explain epilepsy.”
Study funding was not disclosed. Dr. Stefanidou and Dr. Sirven report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Noninvasive tests performed in midlife may help identify people who are at risk of late-onset epilepsy, a new study suggests. New data from the Framingham Heart Study show those who scored better on a neurocognitive test that measures executive function were 75% less likely to develop late-onset epilepsy.
An analysis of MRI revealed that those with higher cortical volumes also had a lower risk of epilepsy later in life, while those with higher white matter hyperintensities had an increased risk.
The study could help identify at-risk individuals years before symptoms of epilepsy appear.
,” said lead investigator Maria Stefanidou, MD, assistant professor of neurology at Boston University.
The findings were presented at the 2023 annual meeting of the American Academy of Neurology.
Protection against late-onset epilepsy?
Hypertension and stroke are known risk factors for late-onset epilepsy. Dementia is also a known risk factor. But in about 30% of cases, the cause of epilepsy in older individuals is unknown.
For this study, investigators analyzed data from the offspring cohort of the Framingham Heart Study. Participants were at least 45 years old; underwent neuropsychological evaluation and brain MRI; and had no prior history of stroke, dementia, or epilepsy. Cognitive measures included Visual Reproductions Delayed Recall, Logical Memory Delayed Recall, Similarities, Trail Making B-A (TrB-TrA), and the Hooper Visual Organization Test.
Participants also underwent an MRI to measure total cerebral brain volume, cortical gray matter volume, white matter hyperintensities, and hippocampal volume.
After a mean follow-up of 13.5 years, late-onset epilepsy was diagnosed in 31 of participants who underwent neuropsychological testing (n = 2,349) and in 27 of those who underwent MRI (n = 2,056).
Better performance on the TrB-TrA test (a measure of executive function, processing speed, and occult vascular injury) was associated with a reduced risk of late-onset epilepsy (adjusted hazard ratio, 0.25; P = .011).
The findings held even after adjusting for age, sex, educational level, and known risk factors for late-onset epilepsy, such as hypertension (aHR, 0.30; P = .0401).
Higher white matter hyperintensities, a measure of occult vascular injury, was associated with increased epilepsy risk (aHR, 1.5; P = .042) when adjusted only for age, sex, and education, but was no longer significant after adjusting for hypertension and other risk factors (aHR, 1.47; P = .065).
The analysis also revealed that participants with a higher cortical gray matter volume had a lower risk for late-onset epilepsy (aHR, 0.73; P = .001).
“There is increasing literature supporting that late-onset epilepsy may be secondary to accumulative occult cerebrovascular and neurodegenerative processes that occur during aging,” Dr. Stefanidou said. “Our findings likely reflect that a lesser degree of occult vascular brain injury in midlife may be protective against late-onset epilepsy.”
However, the epidemiological study points to association, not causation, Dr. Stefanidou cautions.
“Further studies will be needed to study our observations in the clinical setting,” she said.
‘Intriguing’ findings
Commenting on the findings, Joseph Sirven, MD, a neurologist at the Mayo Clinic in Jacksonville, Fla., said the findings are “intriguing,” but also raise some questions. “Late-onset epilepsy remains an issue for many and it’s common,” said Dr. Sirven, who has patients with late-onset epilepsy.
Dr. Sirven was particularly interested in the findings on white matter hyperintensities. “Hippocampal volumes have been used but not so much cortical volumes,” he said. “I would like to know more about how white matter changes suggest pathology that would explain epilepsy.”
Study funding was not disclosed. Dr. Stefanidou and Dr. Sirven report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Noninvasive tests performed in midlife may help identify people who are at risk of late-onset epilepsy, a new study suggests. New data from the Framingham Heart Study show those who scored better on a neurocognitive test that measures executive function were 75% less likely to develop late-onset epilepsy.
An analysis of MRI revealed that those with higher cortical volumes also had a lower risk of epilepsy later in life, while those with higher white matter hyperintensities had an increased risk.
The study could help identify at-risk individuals years before symptoms of epilepsy appear.
,” said lead investigator Maria Stefanidou, MD, assistant professor of neurology at Boston University.
The findings were presented at the 2023 annual meeting of the American Academy of Neurology.
Protection against late-onset epilepsy?
Hypertension and stroke are known risk factors for late-onset epilepsy. Dementia is also a known risk factor. But in about 30% of cases, the cause of epilepsy in older individuals is unknown.
For this study, investigators analyzed data from the offspring cohort of the Framingham Heart Study. Participants were at least 45 years old; underwent neuropsychological evaluation and brain MRI; and had no prior history of stroke, dementia, or epilepsy. Cognitive measures included Visual Reproductions Delayed Recall, Logical Memory Delayed Recall, Similarities, Trail Making B-A (TrB-TrA), and the Hooper Visual Organization Test.
Participants also underwent an MRI to measure total cerebral brain volume, cortical gray matter volume, white matter hyperintensities, and hippocampal volume.
After a mean follow-up of 13.5 years, late-onset epilepsy was diagnosed in 31 of participants who underwent neuropsychological testing (n = 2,349) and in 27 of those who underwent MRI (n = 2,056).
Better performance on the TrB-TrA test (a measure of executive function, processing speed, and occult vascular injury) was associated with a reduced risk of late-onset epilepsy (adjusted hazard ratio, 0.25; P = .011).
The findings held even after adjusting for age, sex, educational level, and known risk factors for late-onset epilepsy, such as hypertension (aHR, 0.30; P = .0401).
Higher white matter hyperintensities, a measure of occult vascular injury, was associated with increased epilepsy risk (aHR, 1.5; P = .042) when adjusted only for age, sex, and education, but was no longer significant after adjusting for hypertension and other risk factors (aHR, 1.47; P = .065).
The analysis also revealed that participants with a higher cortical gray matter volume had a lower risk for late-onset epilepsy (aHR, 0.73; P = .001).
“There is increasing literature supporting that late-onset epilepsy may be secondary to accumulative occult cerebrovascular and neurodegenerative processes that occur during aging,” Dr. Stefanidou said. “Our findings likely reflect that a lesser degree of occult vascular brain injury in midlife may be protective against late-onset epilepsy.”
However, the epidemiological study points to association, not causation, Dr. Stefanidou cautions.
“Further studies will be needed to study our observations in the clinical setting,” she said.
‘Intriguing’ findings
Commenting on the findings, Joseph Sirven, MD, a neurologist at the Mayo Clinic in Jacksonville, Fla., said the findings are “intriguing,” but also raise some questions. “Late-onset epilepsy remains an issue for many and it’s common,” said Dr. Sirven, who has patients with late-onset epilepsy.
Dr. Sirven was particularly interested in the findings on white matter hyperintensities. “Hippocampal volumes have been used but not so much cortical volumes,” he said. “I would like to know more about how white matter changes suggest pathology that would explain epilepsy.”
Study funding was not disclosed. Dr. Stefanidou and Dr. Sirven report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2023
Novel neural cell therapy: A cure for focal epilepsy?
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2023
Thirty years of epilepsy therapy: ‘Plus ça change, plus c’est la même chose’?
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
Helping a patient buck the odds
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mortality risk in epilepsy: New data
new research shows.
“To our knowledge, this is the only study that has assessed the cause-specific mortality risk among people with epilepsy according to age and disease course,” investigators led by Seo-Young Lee, MD, PhD, of Kangwon National University, Chuncheon, South Korea, write. “Understanding cause-specific mortality risk, particularly the risk of external causes, is important because they are mostly preventable.”
The findings were published online in Neurology.
Higher mortality risk
For the study, researchers analyzed data from the National Health Insurance Service database in Korea from 2006 to 2017 and vital statistics from Statistics Korea from 2008 to 2017.
The study population included 138,998 patients with newly treated epilepsy, with an average at diagnosis of 48.6 years.
Over 665,928 person years of follow-up (mean follow-up, 4.79 years), 20.095 patients died.
People with epilepsy had more than twice the risk for death, compared with the overall population (standardized mortality ratio, 2.25; 95% confidence interval, 2.22-2.28). Mortality was highest in children aged 4 years or younger and was higher in the first year after diagnosis and in women at all age points.
People with epilepsy had a higher mortality risk, compared with the general public, regardless of how many anti-seizure medications they were taking. Those taking only one medication had a 156% higher risk for death (SMR, 1.56; 95% CI, 1.53-1.60), compared with 493% higher risk in those taking four or more medications (SMR, 4.93; 95% CI, 4.76-5.10).
Where patients lived also played a role in mortality risk. Living in a rural area was associated with a 247% higher risk for death, compared with people without epilepsy who lived in the same area (SMR, 2.47; 95% CI, 2.41-2.53), and the risk was 203% higher risk among those living in urban centers (SMR, 2.03; 95% CI, 1.98-2.09).
Although people with comorbidities had higher mortality rates, even those without any other health conditions had a 161% higher risk for death, compared with people without epilepsy (SMR, 1.61; 95% CI, 1.50-1.72).
Causes of death
The most frequent causes of death were malignant neoplasm and cerebrovascular disease, which researchers noted are thought to be underlying causes of epilepsy.
Among external causes of death, suicide was the most common cause (2.6%). The suicide rate was highest among younger patients and gradually decreased with age.
Deaths tied directly to epilepsy, transport accidents, or falls were lower in this study than had been previously reported, which may be due to adequate seizure control or because the number of older people with epilepsy and comorbidities is higher in Korea than that reported in other countries.
“To reduce mortality in people with epilepsy, comprehensive efforts [are needed], including a national policy against stigma of epilepsy and clinicians’ total management such as risk stratification, education about injury prevention, and monitoring for suicidal ideation with psychological intervention, as well as active control of seizures,” the authors write.
Generalizable findings
Joseph Sirven, MD, professor of neurology at Mayo Clinic Florida, Jacksonville, said that although the study included only Korean patients, the findings are applicable to other counties.
That researchers found patients with epilepsy were more than twice as likely to die prematurely, compared with the general population wasn’t particularly surprising, Dr. Sirven said.
“What struck me the most was the fact that even patients who were on a single drug and seemingly well controlled also had excess mortality reported,” Dr. Sirven said. “That these risks occur should be part of what we tell all patients with epilepsy so that they can better arm themselves with information and help to address some of the risks that this study showed.”
Another important finding is the risk for suicide in patients with epilepsy, especially those who are newly diagnosed, he said.
“When we treat a patient with epilepsy, it should not just be about seizures, but we need to inquire about the psychiatric comorbidities and more importantly manage them in a comprehensive manner,” Dr. Sirven said.
The study was funded by Soonchunhyang University Research Fund and the Korea Health Technology R&D Project. The study authors and Dr. Sirven report no relevant financial conflicts.
A version of this article first appeared on Medscape.com.
new research shows.
“To our knowledge, this is the only study that has assessed the cause-specific mortality risk among people with epilepsy according to age and disease course,” investigators led by Seo-Young Lee, MD, PhD, of Kangwon National University, Chuncheon, South Korea, write. “Understanding cause-specific mortality risk, particularly the risk of external causes, is important because they are mostly preventable.”
The findings were published online in Neurology.
Higher mortality risk
For the study, researchers analyzed data from the National Health Insurance Service database in Korea from 2006 to 2017 and vital statistics from Statistics Korea from 2008 to 2017.
The study population included 138,998 patients with newly treated epilepsy, with an average at diagnosis of 48.6 years.
Over 665,928 person years of follow-up (mean follow-up, 4.79 years), 20.095 patients died.
People with epilepsy had more than twice the risk for death, compared with the overall population (standardized mortality ratio, 2.25; 95% confidence interval, 2.22-2.28). Mortality was highest in children aged 4 years or younger and was higher in the first year after diagnosis and in women at all age points.
People with epilepsy had a higher mortality risk, compared with the general public, regardless of how many anti-seizure medications they were taking. Those taking only one medication had a 156% higher risk for death (SMR, 1.56; 95% CI, 1.53-1.60), compared with 493% higher risk in those taking four or more medications (SMR, 4.93; 95% CI, 4.76-5.10).
Where patients lived also played a role in mortality risk. Living in a rural area was associated with a 247% higher risk for death, compared with people without epilepsy who lived in the same area (SMR, 2.47; 95% CI, 2.41-2.53), and the risk was 203% higher risk among those living in urban centers (SMR, 2.03; 95% CI, 1.98-2.09).
Although people with comorbidities had higher mortality rates, even those without any other health conditions had a 161% higher risk for death, compared with people without epilepsy (SMR, 1.61; 95% CI, 1.50-1.72).
Causes of death
The most frequent causes of death were malignant neoplasm and cerebrovascular disease, which researchers noted are thought to be underlying causes of epilepsy.
Among external causes of death, suicide was the most common cause (2.6%). The suicide rate was highest among younger patients and gradually decreased with age.
Deaths tied directly to epilepsy, transport accidents, or falls were lower in this study than had been previously reported, which may be due to adequate seizure control or because the number of older people with epilepsy and comorbidities is higher in Korea than that reported in other countries.
“To reduce mortality in people with epilepsy, comprehensive efforts [are needed], including a national policy against stigma of epilepsy and clinicians’ total management such as risk stratification, education about injury prevention, and monitoring for suicidal ideation with psychological intervention, as well as active control of seizures,” the authors write.
Generalizable findings
Joseph Sirven, MD, professor of neurology at Mayo Clinic Florida, Jacksonville, said that although the study included only Korean patients, the findings are applicable to other counties.
That researchers found patients with epilepsy were more than twice as likely to die prematurely, compared with the general population wasn’t particularly surprising, Dr. Sirven said.
“What struck me the most was the fact that even patients who were on a single drug and seemingly well controlled also had excess mortality reported,” Dr. Sirven said. “That these risks occur should be part of what we tell all patients with epilepsy so that they can better arm themselves with information and help to address some of the risks that this study showed.”
Another important finding is the risk for suicide in patients with epilepsy, especially those who are newly diagnosed, he said.
“When we treat a patient with epilepsy, it should not just be about seizures, but we need to inquire about the psychiatric comorbidities and more importantly manage them in a comprehensive manner,” Dr. Sirven said.
The study was funded by Soonchunhyang University Research Fund and the Korea Health Technology R&D Project. The study authors and Dr. Sirven report no relevant financial conflicts.
A version of this article first appeared on Medscape.com.
new research shows.
“To our knowledge, this is the only study that has assessed the cause-specific mortality risk among people with epilepsy according to age and disease course,” investigators led by Seo-Young Lee, MD, PhD, of Kangwon National University, Chuncheon, South Korea, write. “Understanding cause-specific mortality risk, particularly the risk of external causes, is important because they are mostly preventable.”
The findings were published online in Neurology.
Higher mortality risk
For the study, researchers analyzed data from the National Health Insurance Service database in Korea from 2006 to 2017 and vital statistics from Statistics Korea from 2008 to 2017.
The study population included 138,998 patients with newly treated epilepsy, with an average at diagnosis of 48.6 years.
Over 665,928 person years of follow-up (mean follow-up, 4.79 years), 20.095 patients died.
People with epilepsy had more than twice the risk for death, compared with the overall population (standardized mortality ratio, 2.25; 95% confidence interval, 2.22-2.28). Mortality was highest in children aged 4 years or younger and was higher in the first year after diagnosis and in women at all age points.
People with epilepsy had a higher mortality risk, compared with the general public, regardless of how many anti-seizure medications they were taking. Those taking only one medication had a 156% higher risk for death (SMR, 1.56; 95% CI, 1.53-1.60), compared with 493% higher risk in those taking four or more medications (SMR, 4.93; 95% CI, 4.76-5.10).
Where patients lived also played a role in mortality risk. Living in a rural area was associated with a 247% higher risk for death, compared with people without epilepsy who lived in the same area (SMR, 2.47; 95% CI, 2.41-2.53), and the risk was 203% higher risk among those living in urban centers (SMR, 2.03; 95% CI, 1.98-2.09).
Although people with comorbidities had higher mortality rates, even those without any other health conditions had a 161% higher risk for death, compared with people without epilepsy (SMR, 1.61; 95% CI, 1.50-1.72).
Causes of death
The most frequent causes of death were malignant neoplasm and cerebrovascular disease, which researchers noted are thought to be underlying causes of epilepsy.
Among external causes of death, suicide was the most common cause (2.6%). The suicide rate was highest among younger patients and gradually decreased with age.
Deaths tied directly to epilepsy, transport accidents, or falls were lower in this study than had been previously reported, which may be due to adequate seizure control or because the number of older people with epilepsy and comorbidities is higher in Korea than that reported in other countries.
“To reduce mortality in people with epilepsy, comprehensive efforts [are needed], including a national policy against stigma of epilepsy and clinicians’ total management such as risk stratification, education about injury prevention, and monitoring for suicidal ideation with psychological intervention, as well as active control of seizures,” the authors write.
Generalizable findings
Joseph Sirven, MD, professor of neurology at Mayo Clinic Florida, Jacksonville, said that although the study included only Korean patients, the findings are applicable to other counties.
That researchers found patients with epilepsy were more than twice as likely to die prematurely, compared with the general population wasn’t particularly surprising, Dr. Sirven said.
“What struck me the most was the fact that even patients who were on a single drug and seemingly well controlled also had excess mortality reported,” Dr. Sirven said. “That these risks occur should be part of what we tell all patients with epilepsy so that they can better arm themselves with information and help to address some of the risks that this study showed.”
Another important finding is the risk for suicide in patients with epilepsy, especially those who are newly diagnosed, he said.
“When we treat a patient with epilepsy, it should not just be about seizures, but we need to inquire about the psychiatric comorbidities and more importantly manage them in a comprehensive manner,” Dr. Sirven said.
The study was funded by Soonchunhyang University Research Fund and the Korea Health Technology R&D Project. The study authors and Dr. Sirven report no relevant financial conflicts.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Minorities with epilepsy blocked from receiving ‘highest quality of care’
, new research shows.
Even after controlling for epilepsy severity, comorbid conditions, and other factors that might affect medication choice, researchers found that newer medication use was 29% less likely in Black patients, 23% less likely in Native Hawaiian and other Pacific Islander patients, and 7% less likely in Hispanic patients, compared with White individuals.
“I hope that clinicians will see from our findings that minoritized patients with epilepsy face a myriad of barriers in receiving the highest quality of care, including ASM use,” said lead investigator Wyatt P. Bensken, PhD, adjunct assistant professor of Population and Quantitative Health Sciences at Case Western Reserve University, Cleveland. “Considering your patients’ barriers, and how that influences their care – including ASM selection – will be critical to helping reduce these population-level inequities.”
The study was published online in Neurology Clinical Practice.
A prompt for practice change
For the study, researchers used Medicaid claims for more than 78,000 people who had filled at least two prescriptions for an ASM between 2010 and 2014.
Most patients were White (53.4%); 22.6% were Black; 11.9% were Hispanic; 1.6% were Asian; 1.5% were Native Hawaiian or other Pacific Islander; 0.6% American Indian or Alaskan Native; and 8.3% were classified as “other.”
One-quarter of participants were taking an older ASM, such as carbamazepine, phenytoin, and valproate. About 65% were taking second-generation ASMs, including gabapentin, levetiracetam, and zonisamide. A little less than 10% were taking lacosamide, perampenel, or another third-generation ASM.
Compared with White patients, newer medication prescriptions were significantly less likely in Black individuals (adjusted odds ratio, 0.71; 95% confidence interval, 0.68-0.75), Native Hawaiian or other Pacific Islanders (aOR, 0.77; 95% CI, 0.67-0.88), and Hispanic patients (aOR, 0.93; 95% CI, 0.88-0.99).
Third-generation ASMs were used by 10.7% of White patients versus 6% of Black individuals and 5.1% of American Indian or Alaskan Native patients.
Researchers also found that taking a second-generation ASM was associated with better treatment adherence (aOR, 1.17; 95% CI, 1.11-1.23) and that patients on newer ASMs were more than three times as likely to be under the care of a neurologist (aOR, 3.26; 95% CI, 3.13-3.41).
The findings draw attention to racial inequities surrounding access to medication and specialists and subspecialists, Dr. Bensken said. Identifying specific barriers and developing solutions is the long-range goal, he added.
“In the interim, increasing the attention to these inequities will, we hope, prompt changes across practices,” Dr. Bensken said.
A ‘wake-up call’
Commenting on the findings, Joseph Sirven, MD, professor of neurology at the Mayo Clinic Florida, Jacksonville, said the results were “striking” because newer ASMs are generally the go-to for most physicians who treat epilepsy.
“Use of first-generation ASMs is typically reserved [for] if one runs out of options,” Dr. Sirven said.
This study and others like it should serve as a “wake-up call” for clinicians, Dr. Sirven added.
“This study is important because it shows that whether we realize it or not, race and ethnicities are playing a role in ASM, and this is related to financial access to newer-generation drugs,” he said. “Similar findings are seen in impoverished countries where first-generation ASM drugs are routinely used because of drug pricing.”
More to explore
Also commenting on the study, Scott Mintzer, MD, a professor and director of the Epilepsy Monitoring Unit at Thomas Jefferson University, Philadelphia, said using first-generation ASMs as a proxy for quality of care is “a very innovative concept.”
“From that perspective, the finding that racial minority patients are more likely to be on a first-generation drug is not surprising. But after that it gets far more complicated to interpret,” he added.
Neither adherence nor care by a neurologist was different in a consistent direction within the various minority populations, Dr. Mintzer noted. In addition, Black patients were as likely to see a neurologist as White patients but still more likely to be on a first-generation drug.
There are also a few caveats to the findings that should be considered, Dr. Mintzer added. First, the sample included only Medicaid recipients, nearly 35% of whom had a comorbid psychosis. Those and other characteristics of the study pool suggest participants aren’t representative of the United States population as a whole. Second, significant shifts in ASM use have occurred since the study data cutoff in 2014, none of which are reflected in these findings.
“So, I don’t think we can really say how to address this yet,” Dr. Mintzer said. “There’s a lot to explore about whether this is still occurring, how generalizable these findings are, and what they might be due to, as there are a host of potential explanations, which the authors themselves acknowledge.”
The study was funded by the U.S. Centers for Disease Control and Prevention and the National Institute on Minority Health and Health Disparities. Dr. Bensken has received support for this work from NIMHD and serves on the Editorial Board of the journal Neurology. Dr. Sirven and Mintzer report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, new research shows.
Even after controlling for epilepsy severity, comorbid conditions, and other factors that might affect medication choice, researchers found that newer medication use was 29% less likely in Black patients, 23% less likely in Native Hawaiian and other Pacific Islander patients, and 7% less likely in Hispanic patients, compared with White individuals.
“I hope that clinicians will see from our findings that minoritized patients with epilepsy face a myriad of barriers in receiving the highest quality of care, including ASM use,” said lead investigator Wyatt P. Bensken, PhD, adjunct assistant professor of Population and Quantitative Health Sciences at Case Western Reserve University, Cleveland. “Considering your patients’ barriers, and how that influences their care – including ASM selection – will be critical to helping reduce these population-level inequities.”
The study was published online in Neurology Clinical Practice.
A prompt for practice change
For the study, researchers used Medicaid claims for more than 78,000 people who had filled at least two prescriptions for an ASM between 2010 and 2014.
Most patients were White (53.4%); 22.6% were Black; 11.9% were Hispanic; 1.6% were Asian; 1.5% were Native Hawaiian or other Pacific Islander; 0.6% American Indian or Alaskan Native; and 8.3% were classified as “other.”
One-quarter of participants were taking an older ASM, such as carbamazepine, phenytoin, and valproate. About 65% were taking second-generation ASMs, including gabapentin, levetiracetam, and zonisamide. A little less than 10% were taking lacosamide, perampenel, or another third-generation ASM.
Compared with White patients, newer medication prescriptions were significantly less likely in Black individuals (adjusted odds ratio, 0.71; 95% confidence interval, 0.68-0.75), Native Hawaiian or other Pacific Islanders (aOR, 0.77; 95% CI, 0.67-0.88), and Hispanic patients (aOR, 0.93; 95% CI, 0.88-0.99).
Third-generation ASMs were used by 10.7% of White patients versus 6% of Black individuals and 5.1% of American Indian or Alaskan Native patients.
Researchers also found that taking a second-generation ASM was associated with better treatment adherence (aOR, 1.17; 95% CI, 1.11-1.23) and that patients on newer ASMs were more than three times as likely to be under the care of a neurologist (aOR, 3.26; 95% CI, 3.13-3.41).
The findings draw attention to racial inequities surrounding access to medication and specialists and subspecialists, Dr. Bensken said. Identifying specific barriers and developing solutions is the long-range goal, he added.
“In the interim, increasing the attention to these inequities will, we hope, prompt changes across practices,” Dr. Bensken said.
A ‘wake-up call’
Commenting on the findings, Joseph Sirven, MD, professor of neurology at the Mayo Clinic Florida, Jacksonville, said the results were “striking” because newer ASMs are generally the go-to for most physicians who treat epilepsy.
“Use of first-generation ASMs is typically reserved [for] if one runs out of options,” Dr. Sirven said.
This study and others like it should serve as a “wake-up call” for clinicians, Dr. Sirven added.
“This study is important because it shows that whether we realize it or not, race and ethnicities are playing a role in ASM, and this is related to financial access to newer-generation drugs,” he said. “Similar findings are seen in impoverished countries where first-generation ASM drugs are routinely used because of drug pricing.”
More to explore
Also commenting on the study, Scott Mintzer, MD, a professor and director of the Epilepsy Monitoring Unit at Thomas Jefferson University, Philadelphia, said using first-generation ASMs as a proxy for quality of care is “a very innovative concept.”
“From that perspective, the finding that racial minority patients are more likely to be on a first-generation drug is not surprising. But after that it gets far more complicated to interpret,” he added.
Neither adherence nor care by a neurologist was different in a consistent direction within the various minority populations, Dr. Mintzer noted. In addition, Black patients were as likely to see a neurologist as White patients but still more likely to be on a first-generation drug.
There are also a few caveats to the findings that should be considered, Dr. Mintzer added. First, the sample included only Medicaid recipients, nearly 35% of whom had a comorbid psychosis. Those and other characteristics of the study pool suggest participants aren’t representative of the United States population as a whole. Second, significant shifts in ASM use have occurred since the study data cutoff in 2014, none of which are reflected in these findings.
“So, I don’t think we can really say how to address this yet,” Dr. Mintzer said. “There’s a lot to explore about whether this is still occurring, how generalizable these findings are, and what they might be due to, as there are a host of potential explanations, which the authors themselves acknowledge.”
The study was funded by the U.S. Centers for Disease Control and Prevention and the National Institute on Minority Health and Health Disparities. Dr. Bensken has received support for this work from NIMHD and serves on the Editorial Board of the journal Neurology. Dr. Sirven and Mintzer report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, new research shows.
Even after controlling for epilepsy severity, comorbid conditions, and other factors that might affect medication choice, researchers found that newer medication use was 29% less likely in Black patients, 23% less likely in Native Hawaiian and other Pacific Islander patients, and 7% less likely in Hispanic patients, compared with White individuals.
“I hope that clinicians will see from our findings that minoritized patients with epilepsy face a myriad of barriers in receiving the highest quality of care, including ASM use,” said lead investigator Wyatt P. Bensken, PhD, adjunct assistant professor of Population and Quantitative Health Sciences at Case Western Reserve University, Cleveland. “Considering your patients’ barriers, and how that influences their care – including ASM selection – will be critical to helping reduce these population-level inequities.”
The study was published online in Neurology Clinical Practice.
A prompt for practice change
For the study, researchers used Medicaid claims for more than 78,000 people who had filled at least two prescriptions for an ASM between 2010 and 2014.
Most patients were White (53.4%); 22.6% were Black; 11.9% were Hispanic; 1.6% were Asian; 1.5% were Native Hawaiian or other Pacific Islander; 0.6% American Indian or Alaskan Native; and 8.3% were classified as “other.”
One-quarter of participants were taking an older ASM, such as carbamazepine, phenytoin, and valproate. About 65% were taking second-generation ASMs, including gabapentin, levetiracetam, and zonisamide. A little less than 10% were taking lacosamide, perampenel, or another third-generation ASM.
Compared with White patients, newer medication prescriptions were significantly less likely in Black individuals (adjusted odds ratio, 0.71; 95% confidence interval, 0.68-0.75), Native Hawaiian or other Pacific Islanders (aOR, 0.77; 95% CI, 0.67-0.88), and Hispanic patients (aOR, 0.93; 95% CI, 0.88-0.99).
Third-generation ASMs were used by 10.7% of White patients versus 6% of Black individuals and 5.1% of American Indian or Alaskan Native patients.
Researchers also found that taking a second-generation ASM was associated with better treatment adherence (aOR, 1.17; 95% CI, 1.11-1.23) and that patients on newer ASMs were more than three times as likely to be under the care of a neurologist (aOR, 3.26; 95% CI, 3.13-3.41).
The findings draw attention to racial inequities surrounding access to medication and specialists and subspecialists, Dr. Bensken said. Identifying specific barriers and developing solutions is the long-range goal, he added.
“In the interim, increasing the attention to these inequities will, we hope, prompt changes across practices,” Dr. Bensken said.
A ‘wake-up call’
Commenting on the findings, Joseph Sirven, MD, professor of neurology at the Mayo Clinic Florida, Jacksonville, said the results were “striking” because newer ASMs are generally the go-to for most physicians who treat epilepsy.
“Use of first-generation ASMs is typically reserved [for] if one runs out of options,” Dr. Sirven said.
This study and others like it should serve as a “wake-up call” for clinicians, Dr. Sirven added.
“This study is important because it shows that whether we realize it or not, race and ethnicities are playing a role in ASM, and this is related to financial access to newer-generation drugs,” he said. “Similar findings are seen in impoverished countries where first-generation ASM drugs are routinely used because of drug pricing.”
More to explore
Also commenting on the study, Scott Mintzer, MD, a professor and director of the Epilepsy Monitoring Unit at Thomas Jefferson University, Philadelphia, said using first-generation ASMs as a proxy for quality of care is “a very innovative concept.”
“From that perspective, the finding that racial minority patients are more likely to be on a first-generation drug is not surprising. But after that it gets far more complicated to interpret,” he added.
Neither adherence nor care by a neurologist was different in a consistent direction within the various minority populations, Dr. Mintzer noted. In addition, Black patients were as likely to see a neurologist as White patients but still more likely to be on a first-generation drug.
There are also a few caveats to the findings that should be considered, Dr. Mintzer added. First, the sample included only Medicaid recipients, nearly 35% of whom had a comorbid psychosis. Those and other characteristics of the study pool suggest participants aren’t representative of the United States population as a whole. Second, significant shifts in ASM use have occurred since the study data cutoff in 2014, none of which are reflected in these findings.
“So, I don’t think we can really say how to address this yet,” Dr. Mintzer said. “There’s a lot to explore about whether this is still occurring, how generalizable these findings are, and what they might be due to, as there are a host of potential explanations, which the authors themselves acknowledge.”
The study was funded by the U.S. Centers for Disease Control and Prevention and the National Institute on Minority Health and Health Disparities. Dr. Bensken has received support for this work from NIMHD and serves on the Editorial Board of the journal Neurology. Dr. Sirven and Mintzer report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY CLINICAL PRACTICE





