User login
Some improvements seen in neurocognition post-bariatric surgery
ATLANTA – Some patients experienced improvement in at least one neurocognitive domain up to 3 years after having bariatric surgery, a small, systematic review has shown.
The most significant improvements were reported in memory, with nine studies showing some statistically significant improvement in a post-bariatric surgery cohort. Four studies showed statistically significant improvement in attention and executive function, and two did so in language.
Dr. Gurneet S. Thiara, a psychiatry resident at the University of Toronto, presented the findings during a scientific session at this year’s annual meeting of the American Psychiatric Association.
Because the studies that form the basis of the analysis did not follow a standard pre-surgery neurocognitive assessment, the actual scope of bariatric surgery’s impact on neurocognition is hard to determine. This shortcoming provides evidence that instituting a standardized method of psychiatric assessment pre-bariatric surgery could help clinicians better anticipate overall neurocognitive outcomes, he said.
“It’s hard to pinpoint the one domain that affects [this cohort] most,” said Dr. Thiara.
One study included in the analysis showed no neurocognitive improvement, although Dr. Thiara noted this was possibly due to the under- or non-reporting of negative outcomes by researchers who conducted studies that might have met his inclusion criteria.
Dr. Thiara and his colleagues were not able to draw conclusions as to which patients would be affected in which domains and by what mechanism of action. Their analysis did suggest possible relationships between gastric bypass and changes in metabolism, levels of leptin and ghrelin, vascular function, hypoperfusion in the brain, and even shifts in the gut microbiome.
Dr. Thiara sought studies with bariatric surgery patients whose neurocognitive and psychological outcomes were followed anywhere from one to three years post-surgery. After analyzing 422 studies published between January 1990 and August 2015, only ten studies, with patient sample sizes ranging from 10 to 156, met the criteria.
The study was not intended to determine a relationship between neurocognitive outcomes and type of bypass surgery performed, but Dr. Thiara said the majority of the procedures analyzed tended to be Roux-en-Y rather than the gastric bypass sleeve.
On Twitter @whitneymcknight
ATLANTA – Some patients experienced improvement in at least one neurocognitive domain up to 3 years after having bariatric surgery, a small, systematic review has shown.
The most significant improvements were reported in memory, with nine studies showing some statistically significant improvement in a post-bariatric surgery cohort. Four studies showed statistically significant improvement in attention and executive function, and two did so in language.
Dr. Gurneet S. Thiara, a psychiatry resident at the University of Toronto, presented the findings during a scientific session at this year’s annual meeting of the American Psychiatric Association.
Because the studies that form the basis of the analysis did not follow a standard pre-surgery neurocognitive assessment, the actual scope of bariatric surgery’s impact on neurocognition is hard to determine. This shortcoming provides evidence that instituting a standardized method of psychiatric assessment pre-bariatric surgery could help clinicians better anticipate overall neurocognitive outcomes, he said.
“It’s hard to pinpoint the one domain that affects [this cohort] most,” said Dr. Thiara.
One study included in the analysis showed no neurocognitive improvement, although Dr. Thiara noted this was possibly due to the under- or non-reporting of negative outcomes by researchers who conducted studies that might have met his inclusion criteria.
Dr. Thiara and his colleagues were not able to draw conclusions as to which patients would be affected in which domains and by what mechanism of action. Their analysis did suggest possible relationships between gastric bypass and changes in metabolism, levels of leptin and ghrelin, vascular function, hypoperfusion in the brain, and even shifts in the gut microbiome.
Dr. Thiara sought studies with bariatric surgery patients whose neurocognitive and psychological outcomes were followed anywhere from one to three years post-surgery. After analyzing 422 studies published between January 1990 and August 2015, only ten studies, with patient sample sizes ranging from 10 to 156, met the criteria.
The study was not intended to determine a relationship between neurocognitive outcomes and type of bypass surgery performed, but Dr. Thiara said the majority of the procedures analyzed tended to be Roux-en-Y rather than the gastric bypass sleeve.
On Twitter @whitneymcknight
ATLANTA – Some patients experienced improvement in at least one neurocognitive domain up to 3 years after having bariatric surgery, a small, systematic review has shown.
The most significant improvements were reported in memory, with nine studies showing some statistically significant improvement in a post-bariatric surgery cohort. Four studies showed statistically significant improvement in attention and executive function, and two did so in language.
Dr. Gurneet S. Thiara, a psychiatry resident at the University of Toronto, presented the findings during a scientific session at this year’s annual meeting of the American Psychiatric Association.
Because the studies that form the basis of the analysis did not follow a standard pre-surgery neurocognitive assessment, the actual scope of bariatric surgery’s impact on neurocognition is hard to determine. This shortcoming provides evidence that instituting a standardized method of psychiatric assessment pre-bariatric surgery could help clinicians better anticipate overall neurocognitive outcomes, he said.
“It’s hard to pinpoint the one domain that affects [this cohort] most,” said Dr. Thiara.
One study included in the analysis showed no neurocognitive improvement, although Dr. Thiara noted this was possibly due to the under- or non-reporting of negative outcomes by researchers who conducted studies that might have met his inclusion criteria.
Dr. Thiara and his colleagues were not able to draw conclusions as to which patients would be affected in which domains and by what mechanism of action. Their analysis did suggest possible relationships between gastric bypass and changes in metabolism, levels of leptin and ghrelin, vascular function, hypoperfusion in the brain, and even shifts in the gut microbiome.
Dr. Thiara sought studies with bariatric surgery patients whose neurocognitive and psychological outcomes were followed anywhere from one to three years post-surgery. After analyzing 422 studies published between January 1990 and August 2015, only ten studies, with patient sample sizes ranging from 10 to 156, met the criteria.
The study was not intended to determine a relationship between neurocognitive outcomes and type of bypass surgery performed, but Dr. Thiara said the majority of the procedures analyzed tended to be Roux-en-Y rather than the gastric bypass sleeve.
On Twitter @whitneymcknight
AT APA 2016
Key clinical point: Neurocognitive testing in patients before bariatric surgery could be a useful tool for tracking overall psychosocial outcomes.
Major finding: Improvements in neurocognitive function were found across several domains in some patients in the years after bariatric surgery.
Data source: Systematic review of neurocognitive outcomes in post-bariatric surgery patients followed for at least 1 year in 10 studies of between 10 and 156 patients.
Disclosures: Dr. Thiara had no relevant disclosures. This study was sponsored in part by the Toronto Western Hospital Bariatric Psychosocial Surgery Program, part of the University Health Network, Toronto, Ont.
Fresh Press: ACS Surgery News May issue is live on the website!
The digital May issue of ACS Surgery News is available online. Use the mobile app to download or view as a pdf.
The growing problem with reproducibility and sloppy use of statistical tools in biomedical research is the topic of this month’s feature. Even lab mice can be the sources of misleading research results. Dr. Peter Angelos reflects on what all this can mean for surgical research.
Don’t miss Dr. Tyler Hughes’s lighthearted look at a fictional surgeon of the future, Dr. ‘Bones’ McCoy, and how some of Dr. McCoy’s challenges are all too familiar to today’s surgeons.
This issue has news from on-site coverage of the annual meetings of the American Association of Endocrine Surgeons, the American Surgical Association, and the Central Surgical Association.
The digital May issue of ACS Surgery News is available online. Use the mobile app to download or view as a pdf.
The growing problem with reproducibility and sloppy use of statistical tools in biomedical research is the topic of this month’s feature. Even lab mice can be the sources of misleading research results. Dr. Peter Angelos reflects on what all this can mean for surgical research.
Don’t miss Dr. Tyler Hughes’s lighthearted look at a fictional surgeon of the future, Dr. ‘Bones’ McCoy, and how some of Dr. McCoy’s challenges are all too familiar to today’s surgeons.
This issue has news from on-site coverage of the annual meetings of the American Association of Endocrine Surgeons, the American Surgical Association, and the Central Surgical Association.
The digital May issue of ACS Surgery News is available online. Use the mobile app to download or view as a pdf.
The growing problem with reproducibility and sloppy use of statistical tools in biomedical research is the topic of this month’s feature. Even lab mice can be the sources of misleading research results. Dr. Peter Angelos reflects on what all this can mean for surgical research.
Don’t miss Dr. Tyler Hughes’s lighthearted look at a fictional surgeon of the future, Dr. ‘Bones’ McCoy, and how some of Dr. McCoy’s challenges are all too familiar to today’s surgeons.
This issue has news from on-site coverage of the annual meetings of the American Association of Endocrine Surgeons, the American Surgical Association, and the Central Surgical Association.
Focus on patient-level factors, postop complications to reduce readmissions
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications.
Major finding: Including both preoperative and operative data in the model predicted only 10% of the variability in readmission rates.
Data source: A retrospective study of data for nearly 244,000 VA patients.
Disclosures: Dr. Morris reported having no disclosures.
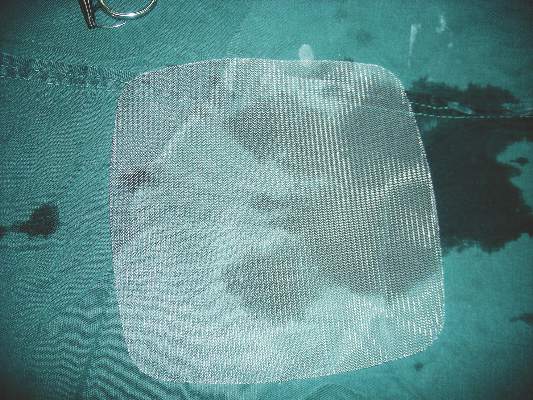
Light mesh doesn’t outweigh heavy mesh for hernia repair
Lightweight mesh has no significant benefit over heavyweight mesh for inguinal hernia repair and was associated with greater pain and higher risk of recurrence, based on data from a randomized trial of 950 patients published in the May issue of the Annals of Surgery.
Although the use of mesh for hernia surgery has been associated with lower recurrence rates and less chronic pain in open hernia repair procedures, the benefits of lightweight vs. heavyweight mesh for laparoscopic procedures has not been well studied, “and there is no consensus which type of mesh is optimal in these procedures,” wrote Dr. Josephina P.J. Burgmans of Diakonessenhuis Utrecht/Zeist (the Netherlands) and colleagues (Ann. Surg. 2016;263[5]:862-6).
To compare the clinical outcomes for patients who received lightweight vs. heavyweight mesh in hernia repairs, the researchers randomized 478 patients to a lightweight-mesh group and 471 to a heavyweight-mesh group. One patient was excluded because the type of mesh was unknown. The study population included men older than 18 years with a primary, reducible, unilateral inguinal hernia who underwent surgery at a single center with one of four surgeons between March 2010 and October 2012. Demographic characteristics were similar between the two groups, as were preoperation pain, operation time, and complications during and after surgery.
At 1 year post surgery, the prevalence of reported relevant pain was significantly higher in the lightweight group, compared with the heavyweight group (2.9% vs. 0.7%). The difference remained statistically significant at 2 years’ follow-up, with relevant pain reported in 3.0% of the lightweight group and 0.9% of the heavyweight group; the difference also remained significant after controlling for factors including age, body mass index, hernia type, severe preoperative pain, recurrence, and surgeon).
Recurrence rates were similar between the two groups at 3 months (two cases in each group), but recurrences became more common in the lightweight group, compared with the heavyweight group, at 1 year (1.7% vs. 0.6%) and significantly more common at 2 years (2.7% vs. 0.8%). The difference remained significant after controlling for multiple variables including hernia type, operating time, surgeon, and body mass index.
No significant differences in foreign body feeling, testicular pain, or sexual-related pain or discomfort were reported between the two groups at the 1-year and 2-year follow-ups.
The study’s strengths include the large patient population and prospective data collection, the researchers noted. The findings were limited by the small number of patients with relevant pain at 1 and 2 years; the homogenous, male-only study population; and the use of questionnaires, which might affect the accuracy of recurrence-rate reports. The results, however, suggest that “there is no benefit for lightweight [meshes] and a conventional heavyweight standard polypropylene 10 cm × 15 cm mesh is recommended for laparoscopic inguinal hernia repair,” Dr. Burgmans and associates wrote
The study was sponsored in part by a grant to the Hernia Centre Zeist from Johnson & Johnston. The researchers had no other relevant financial conflicts to disclose.
Lightweight mesh has no significant benefit over heavyweight mesh for inguinal hernia repair and was associated with greater pain and higher risk of recurrence, based on data from a randomized trial of 950 patients published in the May issue of the Annals of Surgery.
Although the use of mesh for hernia surgery has been associated with lower recurrence rates and less chronic pain in open hernia repair procedures, the benefits of lightweight vs. heavyweight mesh for laparoscopic procedures has not been well studied, “and there is no consensus which type of mesh is optimal in these procedures,” wrote Dr. Josephina P.J. Burgmans of Diakonessenhuis Utrecht/Zeist (the Netherlands) and colleagues (Ann. Surg. 2016;263[5]:862-6).
To compare the clinical outcomes for patients who received lightweight vs. heavyweight mesh in hernia repairs, the researchers randomized 478 patients to a lightweight-mesh group and 471 to a heavyweight-mesh group. One patient was excluded because the type of mesh was unknown. The study population included men older than 18 years with a primary, reducible, unilateral inguinal hernia who underwent surgery at a single center with one of four surgeons between March 2010 and October 2012. Demographic characteristics were similar between the two groups, as were preoperation pain, operation time, and complications during and after surgery.
At 1 year post surgery, the prevalence of reported relevant pain was significantly higher in the lightweight group, compared with the heavyweight group (2.9% vs. 0.7%). The difference remained statistically significant at 2 years’ follow-up, with relevant pain reported in 3.0% of the lightweight group and 0.9% of the heavyweight group; the difference also remained significant after controlling for factors including age, body mass index, hernia type, severe preoperative pain, recurrence, and surgeon).
Recurrence rates were similar between the two groups at 3 months (two cases in each group), but recurrences became more common in the lightweight group, compared with the heavyweight group, at 1 year (1.7% vs. 0.6%) and significantly more common at 2 years (2.7% vs. 0.8%). The difference remained significant after controlling for multiple variables including hernia type, operating time, surgeon, and body mass index.
No significant differences in foreign body feeling, testicular pain, or sexual-related pain or discomfort were reported between the two groups at the 1-year and 2-year follow-ups.
The study’s strengths include the large patient population and prospective data collection, the researchers noted. The findings were limited by the small number of patients with relevant pain at 1 and 2 years; the homogenous, male-only study population; and the use of questionnaires, which might affect the accuracy of recurrence-rate reports. The results, however, suggest that “there is no benefit for lightweight [meshes] and a conventional heavyweight standard polypropylene 10 cm × 15 cm mesh is recommended for laparoscopic inguinal hernia repair,” Dr. Burgmans and associates wrote
The study was sponsored in part by a grant to the Hernia Centre Zeist from Johnson & Johnston. The researchers had no other relevant financial conflicts to disclose.
Lightweight mesh has no significant benefit over heavyweight mesh for inguinal hernia repair and was associated with greater pain and higher risk of recurrence, based on data from a randomized trial of 950 patients published in the May issue of the Annals of Surgery.
Although the use of mesh for hernia surgery has been associated with lower recurrence rates and less chronic pain in open hernia repair procedures, the benefits of lightweight vs. heavyweight mesh for laparoscopic procedures has not been well studied, “and there is no consensus which type of mesh is optimal in these procedures,” wrote Dr. Josephina P.J. Burgmans of Diakonessenhuis Utrecht/Zeist (the Netherlands) and colleagues (Ann. Surg. 2016;263[5]:862-6).
To compare the clinical outcomes for patients who received lightweight vs. heavyweight mesh in hernia repairs, the researchers randomized 478 patients to a lightweight-mesh group and 471 to a heavyweight-mesh group. One patient was excluded because the type of mesh was unknown. The study population included men older than 18 years with a primary, reducible, unilateral inguinal hernia who underwent surgery at a single center with one of four surgeons between March 2010 and October 2012. Demographic characteristics were similar between the two groups, as were preoperation pain, operation time, and complications during and after surgery.
At 1 year post surgery, the prevalence of reported relevant pain was significantly higher in the lightweight group, compared with the heavyweight group (2.9% vs. 0.7%). The difference remained statistically significant at 2 years’ follow-up, with relevant pain reported in 3.0% of the lightweight group and 0.9% of the heavyweight group; the difference also remained significant after controlling for factors including age, body mass index, hernia type, severe preoperative pain, recurrence, and surgeon).
Recurrence rates were similar between the two groups at 3 months (two cases in each group), but recurrences became more common in the lightweight group, compared with the heavyweight group, at 1 year (1.7% vs. 0.6%) and significantly more common at 2 years (2.7% vs. 0.8%). The difference remained significant after controlling for multiple variables including hernia type, operating time, surgeon, and body mass index.
No significant differences in foreign body feeling, testicular pain, or sexual-related pain or discomfort were reported between the two groups at the 1-year and 2-year follow-ups.
The study’s strengths include the large patient population and prospective data collection, the researchers noted. The findings were limited by the small number of patients with relevant pain at 1 and 2 years; the homogenous, male-only study population; and the use of questionnaires, which might affect the accuracy of recurrence-rate reports. The results, however, suggest that “there is no benefit for lightweight [meshes] and a conventional heavyweight standard polypropylene 10 cm × 15 cm mesh is recommended for laparoscopic inguinal hernia repair,” Dr. Burgmans and associates wrote
The study was sponsored in part by a grant to the Hernia Centre Zeist from Johnson & Johnston. The researchers had no other relevant financial conflicts to disclose.
FROM ANNALS OF SURGERY
Key clinical point: Lightweight mesh was associated with more pain and higher recurrence risk 1 and 2 years after surgery.
Major finding: Two years after surgery, relevant pain was reported in 3.0% of the lightweight-mesh patients vs. 0.9% of heavyweight-mesh patients.
Data source: A randomized trial including 950 adult men with inguinal hernias.
Disclosures: The study was sponsored in part by a grant to the Hernia Centre Zeist from Johnson & Johnston. The researchers had no other relevant financial conflicts to disclose.
New interventions improve symptoms of GERD
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Admission to surgical service appears optimal for adhesive small-bowel obstruction
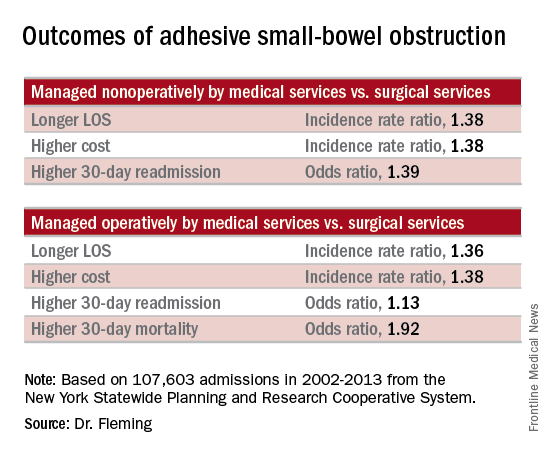
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
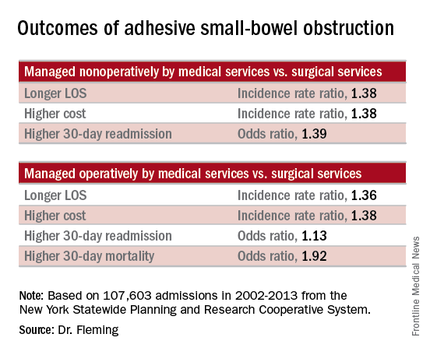
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
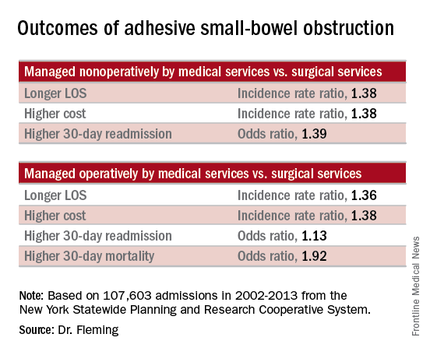
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
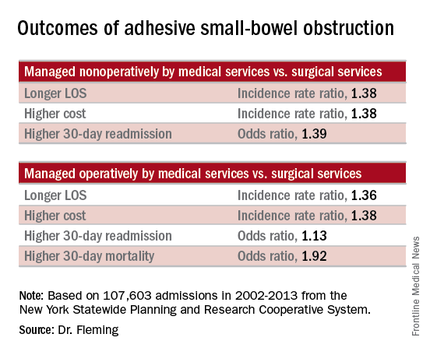
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggest.
Major finding: Management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion.
Data source: A population-based study of more than 107,600 hospital admissions
Disclosures: Dr. Fleming reported having no relevant financial disclosures.
Seven procedures account for most emergency general surgery costs and deaths
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
FROM JAMA SURGERY
Key clinical point: National quality benchmarks and cost reduction efforts should focus on the seven most common, complicated, and costly emergency general surgery procedures.
Major finding: The majority (80%) of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide can be accounted for by seven representative procedures.
Data sources: The 2008-2011 Healthcare Cost and Utilization Project’s National Inpatient Sample claims database.
Disclosures: No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
The perils of hospital air
Hospital air is a potential route of transmission of beta-lactam–resistant bacteria (BLRB), which are important causative agents of nosocomial infections, according to research published in the American Journal of Infection Control.
Dr. Mahnaz Nikaeen of the department of environmental health engineering at Isfahan (Iran) University of Medical Sciences, and his coauthors collected and tested 64 air samples from four hospital wards to determine the prevalence of airborne BLRB in different teaching hospitals, to evaluate the frequency of five common beta-lactamase–encoding genes in isolated resistant bacteria, and to identify the most predominant BLRB by 16s rRNA gene sequencing. The sampling locations in each hospital included operating rooms, ICUs, surgery wards, and internal medicine wards.
The investigators detected airborne bacteria by using culture plates with and without beta-lactams.
The prevalence of BLRB in the air samples ranged between 3% and 34%, Dr. Nikaeen said. Oxacillin-resistant bacteria had the highest prevalence, followed by ceftazidime- and cefazolin-resistant bacteria. Acinetobacter spp, Acinetobacter baumannii, and Staphylococcus spp were the most predominant BLRB.
Gene sequencing revealed that the frequency of beta-lactamase–encoding genes in isolated BLRB ranged between 0% and 47%, with the highest and lowest detection for OXA-23, commonly found in Acinetobacter spp, and CTX-m-32, a gene prevalent in extended-spectrum beta-lactamase–producing Enterobacteriaceae, respectively. MecA, a genetic element found in methicillin-resistant Staphylococcus spp, had a relatively high frequency in surgery wards and operating rooms, whereas the frequency of blaTEM, another common extended-spectrum beta-lactamase produced by Enterobacteriaceae, was higher in intensive care units and internal medicine wards. OXA-51, a chromosomally located intrinsic gene in A. baumannii, was detected in four wards.
“Isolation of beta-lactam–resistant Staphylococcus spp and A. baumannii as the most predominant BLRB indicated the potential role of airborne bacteria in dissemination of nosocomial infections,” Dr. Nikaeen and his coauthors said. “The results confirm the necessity for application of effective control measures that significantly decrease the exposure of high-risk patients to potentially airborne nosocomial infections.”
The authors reported having no conflicts.
Read the complete study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.041).
On Twitter @richpizzi
Hospital air is a potential route of transmission of beta-lactam–resistant bacteria (BLRB), which are important causative agents of nosocomial infections, according to research published in the American Journal of Infection Control.
Dr. Mahnaz Nikaeen of the department of environmental health engineering at Isfahan (Iran) University of Medical Sciences, and his coauthors collected and tested 64 air samples from four hospital wards to determine the prevalence of airborne BLRB in different teaching hospitals, to evaluate the frequency of five common beta-lactamase–encoding genes in isolated resistant bacteria, and to identify the most predominant BLRB by 16s rRNA gene sequencing. The sampling locations in each hospital included operating rooms, ICUs, surgery wards, and internal medicine wards.
The investigators detected airborne bacteria by using culture plates with and without beta-lactams.
The prevalence of BLRB in the air samples ranged between 3% and 34%, Dr. Nikaeen said. Oxacillin-resistant bacteria had the highest prevalence, followed by ceftazidime- and cefazolin-resistant bacteria. Acinetobacter spp, Acinetobacter baumannii, and Staphylococcus spp were the most predominant BLRB.
Gene sequencing revealed that the frequency of beta-lactamase–encoding genes in isolated BLRB ranged between 0% and 47%, with the highest and lowest detection for OXA-23, commonly found in Acinetobacter spp, and CTX-m-32, a gene prevalent in extended-spectrum beta-lactamase–producing Enterobacteriaceae, respectively. MecA, a genetic element found in methicillin-resistant Staphylococcus spp, had a relatively high frequency in surgery wards and operating rooms, whereas the frequency of blaTEM, another common extended-spectrum beta-lactamase produced by Enterobacteriaceae, was higher in intensive care units and internal medicine wards. OXA-51, a chromosomally located intrinsic gene in A. baumannii, was detected in four wards.
“Isolation of beta-lactam–resistant Staphylococcus spp and A. baumannii as the most predominant BLRB indicated the potential role of airborne bacteria in dissemination of nosocomial infections,” Dr. Nikaeen and his coauthors said. “The results confirm the necessity for application of effective control measures that significantly decrease the exposure of high-risk patients to potentially airborne nosocomial infections.”
The authors reported having no conflicts.
Read the complete study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.041).
On Twitter @richpizzi
Hospital air is a potential route of transmission of beta-lactam–resistant bacteria (BLRB), which are important causative agents of nosocomial infections, according to research published in the American Journal of Infection Control.
Dr. Mahnaz Nikaeen of the department of environmental health engineering at Isfahan (Iran) University of Medical Sciences, and his coauthors collected and tested 64 air samples from four hospital wards to determine the prevalence of airborne BLRB in different teaching hospitals, to evaluate the frequency of five common beta-lactamase–encoding genes in isolated resistant bacteria, and to identify the most predominant BLRB by 16s rRNA gene sequencing. The sampling locations in each hospital included operating rooms, ICUs, surgery wards, and internal medicine wards.
The investigators detected airborne bacteria by using culture plates with and without beta-lactams.
The prevalence of BLRB in the air samples ranged between 3% and 34%, Dr. Nikaeen said. Oxacillin-resistant bacteria had the highest prevalence, followed by ceftazidime- and cefazolin-resistant bacteria. Acinetobacter spp, Acinetobacter baumannii, and Staphylococcus spp were the most predominant BLRB.
Gene sequencing revealed that the frequency of beta-lactamase–encoding genes in isolated BLRB ranged between 0% and 47%, with the highest and lowest detection for OXA-23, commonly found in Acinetobacter spp, and CTX-m-32, a gene prevalent in extended-spectrum beta-lactamase–producing Enterobacteriaceae, respectively. MecA, a genetic element found in methicillin-resistant Staphylococcus spp, had a relatively high frequency in surgery wards and operating rooms, whereas the frequency of blaTEM, another common extended-spectrum beta-lactamase produced by Enterobacteriaceae, was higher in intensive care units and internal medicine wards. OXA-51, a chromosomally located intrinsic gene in A. baumannii, was detected in four wards.
“Isolation of beta-lactam–resistant Staphylococcus spp and A. baumannii as the most predominant BLRB indicated the potential role of airborne bacteria in dissemination of nosocomial infections,” Dr. Nikaeen and his coauthors said. “The results confirm the necessity for application of effective control measures that significantly decrease the exposure of high-risk patients to potentially airborne nosocomial infections.”
The authors reported having no conflicts.
Read the complete study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.041).
On Twitter @richpizzi
FROM AMERICAN JOURNAL OF INFECTION CONTROL
Surgery for PHPT improves sleep quality
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
AT AAES 2016
Key clinical point: A large proportion of “asymptomatic” patients with primary hyperparathyroidism (PHPT) actually have sleep disturbances.
Major finding: Sleep scores a month after parathyroidectomy were found to improve in 50% of patients with PHPT.
Data source: Single institution, prospective study of 155 patients comparing sleep patterns in patients with PHPT and thyroid controls.
Disclosures: Mr. La and his coauthors reported having no financial disclosures.
Post-parathyroidectomy follow-up may need to be open-ended
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
FROM AAES 2016
Key clinical point: Long-term recurrence rates for hyperparathyroidism (HPT) after “curative” parathyroidectomy are likely higher than previously reported.
Major finding: Approximately one-third of patients were found to have recurrences 10 or more years after the initial operation.
Data source: Single-institution cohort of 196 patients who had initial parathyroidectomy for HPT between November 2000 and June 2005.
Disclosures: Dr. Lou and her study coauthors reported having no financial disclosures.