User login
HIV not a risk factor for postappendectomy complications
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients.
Major finding: Risk of death and complications were similar across both groups, although hospital stays were about 26% longer and cost about 10% more for patients with HIV.
Data source: Query of Nationwide Inpatient Sample (NIS) database during 2005-2012 of 812 HIV and 338,425 non-HIV patients who had appendectomy for acute appendicitis.
Disclosures: The study authors reported having no financial disclosures.
Damage to nearby structure common cause of hernia malpractice claim
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Failure to diagnose a complication caused by damage to a nearby structure during hernia repair surgery is the most common cause for a malpractice claim for hernia repair.
Major finding: In malpractice cases involving hernia surgery that go to trial, 59% of the rulings are for the plaintiff physicians and about 14% go to settlement before a judge or jury decision.
Data source: Sample of 250 hernia surgical malpractice cases from 1985 to 2015 in the Westlaw Next legal database.
Disclosures: The study authors reported having no financial disclosures.
Can ‘big data’ predict postop complications?
JACKSONVILLE, FLA. The potential of “big data” to predict surgical complications has long been expected and that potential may now in the process of becoming a reality.
As health care moves to a value-based system that penalizes surgeons and hospitals for readmissions, the inability to predict postop complications remains a problem, but investigators at University of Wisconsin have found a way to use “big data” to create a model that may help surgeons identify at-risk individuals before complications occur.
Shara Feld, Ph.D., a medical student at Wisconsin, reported on the development of a Markov chain model that sequences random variables to calculate varying states over time. “A Markov model represents the patient progression through a series of health states,” Dr. Feld said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress
“A Markov chain model combining information about prior complications and the time to occurrence after surgery can inform our likelihood of specific future complications,” she said. “Understanding these relationships among complications can improve our ability to select targeted interventions, to avoid cascades of multiple complications, counsel patients and family on prognosis, assist with care decisions, and develop quality improvement measures.”
The model draws on 3 million operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database from 2005 to 2013. Of those, 400,000 cases involved one complication and 132,000 two or more complications, Dr. Feld said. From that, the investigators identified 21 different complications, including superficial, deep and organ surgical site infections, cardiac arrest, and pneumonia. The study accounted for complications within 30 days of the operation.
Dr. Feld pointed to one of the challenges using the existing literature on surgical risk assessment: “We know that patients can have one complication that can snowball into multiple complications, and as this snowball of complications develops, the postoperative risk in patient prognosis can change from what it was based on preoperative risk factors,” she said.
The model was best at predicting death, coma longer than a day, cardiac arrest, septic shock, renal failure, pneumonia, unplanned reintubation, ventilator use of more than 2 days, and bleeding transfusion, Dr. Feld said.
The study also found that complications most likely to cascade to a higher level were cardiac arrest, renal insufficiency or failure, stroke, intubation, septic shock, and coma, Dr. Feld said. For example, a patient who has a coma has an odds ratio greater than 1.5 of dying within 30 days of the operation while the odds ratio for death following a diagnosis of superficial surgical site infection is less than 0.5, the study found.
Evaluating population-based complication risks after surgery was difficult before the large ACS NSQIP database became available to researchers, Dr. Feld said. The model reveals the impact of specific complications, complication timing, and how combinations of multiple postoperative complications change the risk for the development of future complications..
This model has not to date looked at what type of procedure led to the complications but this line of research may be developed in the future, Dr. Feld said.
The authors had no financial relationships to disclose.
JACKSONVILLE, FLA. The potential of “big data” to predict surgical complications has long been expected and that potential may now in the process of becoming a reality.
As health care moves to a value-based system that penalizes surgeons and hospitals for readmissions, the inability to predict postop complications remains a problem, but investigators at University of Wisconsin have found a way to use “big data” to create a model that may help surgeons identify at-risk individuals before complications occur.
Shara Feld, Ph.D., a medical student at Wisconsin, reported on the development of a Markov chain model that sequences random variables to calculate varying states over time. “A Markov model represents the patient progression through a series of health states,” Dr. Feld said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress
“A Markov chain model combining information about prior complications and the time to occurrence after surgery can inform our likelihood of specific future complications,” she said. “Understanding these relationships among complications can improve our ability to select targeted interventions, to avoid cascades of multiple complications, counsel patients and family on prognosis, assist with care decisions, and develop quality improvement measures.”
The model draws on 3 million operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database from 2005 to 2013. Of those, 400,000 cases involved one complication and 132,000 two or more complications, Dr. Feld said. From that, the investigators identified 21 different complications, including superficial, deep and organ surgical site infections, cardiac arrest, and pneumonia. The study accounted for complications within 30 days of the operation.
Dr. Feld pointed to one of the challenges using the existing literature on surgical risk assessment: “We know that patients can have one complication that can snowball into multiple complications, and as this snowball of complications develops, the postoperative risk in patient prognosis can change from what it was based on preoperative risk factors,” she said.
The model was best at predicting death, coma longer than a day, cardiac arrest, septic shock, renal failure, pneumonia, unplanned reintubation, ventilator use of more than 2 days, and bleeding transfusion, Dr. Feld said.
The study also found that complications most likely to cascade to a higher level were cardiac arrest, renal insufficiency or failure, stroke, intubation, septic shock, and coma, Dr. Feld said. For example, a patient who has a coma has an odds ratio greater than 1.5 of dying within 30 days of the operation while the odds ratio for death following a diagnosis of superficial surgical site infection is less than 0.5, the study found.
Evaluating population-based complication risks after surgery was difficult before the large ACS NSQIP database became available to researchers, Dr. Feld said. The model reveals the impact of specific complications, complication timing, and how combinations of multiple postoperative complications change the risk for the development of future complications..
This model has not to date looked at what type of procedure led to the complications but this line of research may be developed in the future, Dr. Feld said.
The authors had no financial relationships to disclose.
JACKSONVILLE, FLA. The potential of “big data” to predict surgical complications has long been expected and that potential may now in the process of becoming a reality.
As health care moves to a value-based system that penalizes surgeons and hospitals for readmissions, the inability to predict postop complications remains a problem, but investigators at University of Wisconsin have found a way to use “big data” to create a model that may help surgeons identify at-risk individuals before complications occur.
Shara Feld, Ph.D., a medical student at Wisconsin, reported on the development of a Markov chain model that sequences random variables to calculate varying states over time. “A Markov model represents the patient progression through a series of health states,” Dr. Feld said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress
“A Markov chain model combining information about prior complications and the time to occurrence after surgery can inform our likelihood of specific future complications,” she said. “Understanding these relationships among complications can improve our ability to select targeted interventions, to avoid cascades of multiple complications, counsel patients and family on prognosis, assist with care decisions, and develop quality improvement measures.”
The model draws on 3 million operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database from 2005 to 2013. Of those, 400,000 cases involved one complication and 132,000 two or more complications, Dr. Feld said. From that, the investigators identified 21 different complications, including superficial, deep and organ surgical site infections, cardiac arrest, and pneumonia. The study accounted for complications within 30 days of the operation.
Dr. Feld pointed to one of the challenges using the existing literature on surgical risk assessment: “We know that patients can have one complication that can snowball into multiple complications, and as this snowball of complications develops, the postoperative risk in patient prognosis can change from what it was based on preoperative risk factors,” she said.
The model was best at predicting death, coma longer than a day, cardiac arrest, septic shock, renal failure, pneumonia, unplanned reintubation, ventilator use of more than 2 days, and bleeding transfusion, Dr. Feld said.
The study also found that complications most likely to cascade to a higher level were cardiac arrest, renal insufficiency or failure, stroke, intubation, septic shock, and coma, Dr. Feld said. For example, a patient who has a coma has an odds ratio greater than 1.5 of dying within 30 days of the operation while the odds ratio for death following a diagnosis of superficial surgical site infection is less than 0.5, the study found.
Evaluating population-based complication risks after surgery was difficult before the large ACS NSQIP database became available to researchers, Dr. Feld said. The model reveals the impact of specific complications, complication timing, and how combinations of multiple postoperative complications change the risk for the development of future complications..
This model has not to date looked at what type of procedure led to the complications but this line of research may be developed in the future, Dr. Feld said.
The authors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: A Markov chain model using data from the American College of Surgeons National Surgical Quality Improvement Program may provide a tool for predicting complications after surgery.
Major finding: The model was best at predicting death, coma longer than a day, cardiac arrest, septic shock, renal failure, pneumonia, unplanned reintubation, ventilator use of more than 2 days, and bleeding.
Data source: The model draws on 3 million operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database from 2005 to 2013.
Disclosures: The study authors reported having no financial disclosures.
The no-operation quality assessment ‘blind spot’
JACKSONVILLE, FLA. – About one-third of patients admitted to the hospital for abdominal problems like diverticulitis and small bowel obstruction get discharged without having surgery, but their outcomes are not typically included in quality assessment, leaving this group of patients in a “blind spot” of surgical quality, according to Dr. Michael Wandling.
However, researchers from Northwestern University in Chicago have analyzed data from the Nationwide (National) Inpatient Sample and determined how many cases of diverticulitis, small bowel obstruction (SBO), cholecystitis, and acute appendicitis are managed without surgery and the clinical factors that may influence that, he reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Surgeons frequently will admit patients for nonoperative management of diagnoses such as diverticulitis, small bowel obstruction, cholecystitis, and perforated appendicitis,” said Dr. Wandling, a general surgery resident at Northwestern. “Yet nonoperative management does not really factor into current surgical quality assessment. In fact, nonoperative management is not frequently evaluated, and utilization rates have not even really been quantified.”
The researchers’ goal was to evaluate hospital-level variability in nonoperative management practices and identify hospital characteristics associated with high rates of nonoperative management, Dr. Wandling said.
“What we found was that smaller bed size, fewer annual discharges, being a public government-run hospital, being a nonteaching hospital, and being rural or located in the Midwest were all associated with greater use of nonoperative management,” he said.
They extracted a sample from the Nationwide (National) Inpatient Sample that analyzed admission and discharge data on 1.6 million patients admitted for one of the four studied diagnoses from 1998 to 2011. Overall, the four diagnoses accounted for more than 500,000 annual admissions, “and this rate has been increasing over time,” Dr. Wandling said. To calculate rates of nonoperative management for each diagnosis, the researchers concentrated on data from 2010 and 2011. They found the following rates of nonoperative management: 87.1% for diverticulitis, 38.1% for SBO, 11.3% for cholecystitis, and 3.7% for appendicitis. The overall rate of nonoperative management for all four diagnoses was 32.8%, Dr. Wandling said.
They also evaluated the overall rates of nonoperative management for each year from 1998 to 2011 and found they steadily increased from 25.6% to 32.8%, Dr. Wandling said. “Nonoperative management is not uncommon, with approximately 190,000 patients being admitted for nonoperative management each year, and this number has also been increasing,” he said.
Dr. Wandling acknowledged some limitations with the study because it used an administrative dataset with data collected retrospectively and because the data do not track patients after discharge, making it impossible to know if any patients managed nonoperatively were subsequently readmitted for surgery. “Current surgical quality assessment only focuses on patients who have surgery, which can be seen through public reporting programs like Hospital Compare, pay-for-performance initiatives like [Centers for Medicare & Medicaid Services] valued-based purchasing, and clinical data registries,” he said. “As a result, patients who are managed nonoperatively are really left in a blind spot of surgical quality.”
Dr. Wandling said he and his coauthors are working with the American College of Surgeons National Surgical Quality Improvement Program to develop an Emergency General Surgery (EGS) Pilot to evaluate performance in operative and nonoperative care for SBO, cholecystitis, and appendicitis. Fourteen centers have so far collected more than 6 months of data as part of the EGS Pilot, he said, and additional hospitals are currently being recruited to participate.
“Ultimately the goal is to identify optimal nonoperative management strategies in general surgery so that all patients can receive high-quality surgical care, not just those who we operate on,” Dr. Wandling said.
He and his coauthors had no relevant financial disclosures.
JACKSONVILLE, FLA. – About one-third of patients admitted to the hospital for abdominal problems like diverticulitis and small bowel obstruction get discharged without having surgery, but their outcomes are not typically included in quality assessment, leaving this group of patients in a “blind spot” of surgical quality, according to Dr. Michael Wandling.
However, researchers from Northwestern University in Chicago have analyzed data from the Nationwide (National) Inpatient Sample and determined how many cases of diverticulitis, small bowel obstruction (SBO), cholecystitis, and acute appendicitis are managed without surgery and the clinical factors that may influence that, he reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Surgeons frequently will admit patients for nonoperative management of diagnoses such as diverticulitis, small bowel obstruction, cholecystitis, and perforated appendicitis,” said Dr. Wandling, a general surgery resident at Northwestern. “Yet nonoperative management does not really factor into current surgical quality assessment. In fact, nonoperative management is not frequently evaluated, and utilization rates have not even really been quantified.”
The researchers’ goal was to evaluate hospital-level variability in nonoperative management practices and identify hospital characteristics associated with high rates of nonoperative management, Dr. Wandling said.
“What we found was that smaller bed size, fewer annual discharges, being a public government-run hospital, being a nonteaching hospital, and being rural or located in the Midwest were all associated with greater use of nonoperative management,” he said.
They extracted a sample from the Nationwide (National) Inpatient Sample that analyzed admission and discharge data on 1.6 million patients admitted for one of the four studied diagnoses from 1998 to 2011. Overall, the four diagnoses accounted for more than 500,000 annual admissions, “and this rate has been increasing over time,” Dr. Wandling said. To calculate rates of nonoperative management for each diagnosis, the researchers concentrated on data from 2010 and 2011. They found the following rates of nonoperative management: 87.1% for diverticulitis, 38.1% for SBO, 11.3% for cholecystitis, and 3.7% for appendicitis. The overall rate of nonoperative management for all four diagnoses was 32.8%, Dr. Wandling said.
They also evaluated the overall rates of nonoperative management for each year from 1998 to 2011 and found they steadily increased from 25.6% to 32.8%, Dr. Wandling said. “Nonoperative management is not uncommon, with approximately 190,000 patients being admitted for nonoperative management each year, and this number has also been increasing,” he said.
Dr. Wandling acknowledged some limitations with the study because it used an administrative dataset with data collected retrospectively and because the data do not track patients after discharge, making it impossible to know if any patients managed nonoperatively were subsequently readmitted for surgery. “Current surgical quality assessment only focuses on patients who have surgery, which can be seen through public reporting programs like Hospital Compare, pay-for-performance initiatives like [Centers for Medicare & Medicaid Services] valued-based purchasing, and clinical data registries,” he said. “As a result, patients who are managed nonoperatively are really left in a blind spot of surgical quality.”
Dr. Wandling said he and his coauthors are working with the American College of Surgeons National Surgical Quality Improvement Program to develop an Emergency General Surgery (EGS) Pilot to evaluate performance in operative and nonoperative care for SBO, cholecystitis, and appendicitis. Fourteen centers have so far collected more than 6 months of data as part of the EGS Pilot, he said, and additional hospitals are currently being recruited to participate.
“Ultimately the goal is to identify optimal nonoperative management strategies in general surgery so that all patients can receive high-quality surgical care, not just those who we operate on,” Dr. Wandling said.
He and his coauthors had no relevant financial disclosures.
JACKSONVILLE, FLA. – About one-third of patients admitted to the hospital for abdominal problems like diverticulitis and small bowel obstruction get discharged without having surgery, but their outcomes are not typically included in quality assessment, leaving this group of patients in a “blind spot” of surgical quality, according to Dr. Michael Wandling.
However, researchers from Northwestern University in Chicago have analyzed data from the Nationwide (National) Inpatient Sample and determined how many cases of diverticulitis, small bowel obstruction (SBO), cholecystitis, and acute appendicitis are managed without surgery and the clinical factors that may influence that, he reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Surgeons frequently will admit patients for nonoperative management of diagnoses such as diverticulitis, small bowel obstruction, cholecystitis, and perforated appendicitis,” said Dr. Wandling, a general surgery resident at Northwestern. “Yet nonoperative management does not really factor into current surgical quality assessment. In fact, nonoperative management is not frequently evaluated, and utilization rates have not even really been quantified.”
The researchers’ goal was to evaluate hospital-level variability in nonoperative management practices and identify hospital characteristics associated with high rates of nonoperative management, Dr. Wandling said.
“What we found was that smaller bed size, fewer annual discharges, being a public government-run hospital, being a nonteaching hospital, and being rural or located in the Midwest were all associated with greater use of nonoperative management,” he said.
They extracted a sample from the Nationwide (National) Inpatient Sample that analyzed admission and discharge data on 1.6 million patients admitted for one of the four studied diagnoses from 1998 to 2011. Overall, the four diagnoses accounted for more than 500,000 annual admissions, “and this rate has been increasing over time,” Dr. Wandling said. To calculate rates of nonoperative management for each diagnosis, the researchers concentrated on data from 2010 and 2011. They found the following rates of nonoperative management: 87.1% for diverticulitis, 38.1% for SBO, 11.3% for cholecystitis, and 3.7% for appendicitis. The overall rate of nonoperative management for all four diagnoses was 32.8%, Dr. Wandling said.
They also evaluated the overall rates of nonoperative management for each year from 1998 to 2011 and found they steadily increased from 25.6% to 32.8%, Dr. Wandling said. “Nonoperative management is not uncommon, with approximately 190,000 patients being admitted for nonoperative management each year, and this number has also been increasing,” he said.
Dr. Wandling acknowledged some limitations with the study because it used an administrative dataset with data collected retrospectively and because the data do not track patients after discharge, making it impossible to know if any patients managed nonoperatively were subsequently readmitted for surgery. “Current surgical quality assessment only focuses on patients who have surgery, which can be seen through public reporting programs like Hospital Compare, pay-for-performance initiatives like [Centers for Medicare & Medicaid Services] valued-based purchasing, and clinical data registries,” he said. “As a result, patients who are managed nonoperatively are really left in a blind spot of surgical quality.”
Dr. Wandling said he and his coauthors are working with the American College of Surgeons National Surgical Quality Improvement Program to develop an Emergency General Surgery (EGS) Pilot to evaluate performance in operative and nonoperative care for SBO, cholecystitis, and appendicitis. Fourteen centers have so far collected more than 6 months of data as part of the EGS Pilot, he said, and additional hospitals are currently being recruited to participate.
“Ultimately the goal is to identify optimal nonoperative management strategies in general surgery so that all patients can receive high-quality surgical care, not just those who we operate on,” Dr. Wandling said.
He and his coauthors had no relevant financial disclosures.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Quality assessment of surgical outcomes does not account for cases that are managed medically without an operation; this study evaluated nonoperative management for four common diagnoses of abdominal pain.
Major finding: The overall rate of nonoperative management for diverticulitis, small bowel obstruction, cholecystitis, and appendicitis was 32.8% with rates increasing steadily over the 13-year study period.
Data source: An analysis of a sampling of 1.6 million admissions from the Nationwide (National) Inpatient Sample from 1998 to 2011, with concentration on data from 2010 and 2011.
Disclosures: The study authors reported having no relevant financial disclosures.
Study measures post-thyroidectomy voice changes
JACKSONVILLE, FLA. – Voice quality changes after thyroid surgery are detectable by using both subjective and objective measures, according to investigators at Monash University in Melbourne, Australia.
After thyroid surgery, up to 80% of patients with functional recurrent laryngeal nerves (RLNs) have reported voice changes, so the investigators set out to evaluate the extent of those voice changes and how the extent of the operation and RLN edema may affect them.
“It has been confirmed that thyroid procedures do alter the voice without necessarily causing a measurable recurrent laryngeal nerve palsy,” said lead investigator Dr. James Lee, “and the change of voice is correlated to the extent of surgery and the amount of nerve swelling.” The findings were presented at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study evaluated 62 patients who had total and partial thyroidectomy surgery between 2010 and 2011 at the Monash University Endocrine Surgery Unit. To subjectively measure voice quality after surgery, the researchers used the Voice Disorder Index (VDI), which measures voice quality on a 0-40 scale from best to worst. After surgery, the mean VDI score in this group showed a 5.2 plus or minus 1.2–point deterioration from 4.2 to 9.4 (P less than .001). For objective evaluation, the researchers used the Dysphonia Severity Index (DSI), which scores voice quality on a scale of –5 to 5 from worst to best. After surgery, the mean DSI score showed a 1.1 plus or minus 0.2–point deterioration from 3.9 to 2.8 (P less than .001). Two speech pathologists conducted the voice assessments.
“Subjective scoring of both hemithyroidectomy and total thyroidectomy reported worse voice postoperatively,” Dr. Lee said. “However, when you take a close look at the numbers, those undergoing total thyroidectomy reported a higher measure of deterioration in their voice.”
Patients who had either partial and total thyroidectomy reported significant subjective deterioration of their voice with mean VDI change from 5.4 to 7.9 (P = 0.02) and 3.5 to 10.6 (P less than .001), respectively. However, on objective evaluation, only the total thyroidectomy patients showed significant voice deterioration, with a mean DSI change from 4 to 2.5 (P less than .001).
Dr. Lee noted that study outcomes between partial and total thyroidectomy patients diverged in another respect: the impact RLN swelling had on voice deterioration. To evaluate RLN swelling, the researchers measured the diameter of the nerve with Vernier calipers before and after the lobectomy during each operation. RLN diameter increased 0.58 plus or minus 0.05 mm on average (P less than .001). In patients who had partial thyroidectomy, the greater the RLN swelling, the worse the subjective score (P = .03). This was not the case in the total thyroidectomy patients where involvement of two nerves complicates the interaction, he said.
During follow-up, the investigators came upon a revelatory finding. “With median 8-month follow-up, the self-reported, VDI scores had returned to baseline levels,” Dr. Lee said. “Interestingly, not only did the objective DSI scores show a return to baseline levels, but it exceeded the baseline levels, meaning the voice had scored better after surgery than before.” However, he noted only 13 patients completed the follow-up.
“Voice change post-thyroidectomy without recurrent laryngeal nerve injury is a complex phenomenon and is likely multifactorial, and we only looked at two of those factors: the extent of surgery and the gradient of recurrent laryngeal nerve injury with nerve edema as a surrogate,” Dr. Lee said. Future studies should evaluate other factors, including the role of the external branch of the superior laryngeal nerve and patient factors such as diabetes or smoking, he said.
Dr. Lee and his coauthors had no disclosures.
JACKSONVILLE, FLA. – Voice quality changes after thyroid surgery are detectable by using both subjective and objective measures, according to investigators at Monash University in Melbourne, Australia.
After thyroid surgery, up to 80% of patients with functional recurrent laryngeal nerves (RLNs) have reported voice changes, so the investigators set out to evaluate the extent of those voice changes and how the extent of the operation and RLN edema may affect them.
“It has been confirmed that thyroid procedures do alter the voice without necessarily causing a measurable recurrent laryngeal nerve palsy,” said lead investigator Dr. James Lee, “and the change of voice is correlated to the extent of surgery and the amount of nerve swelling.” The findings were presented at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study evaluated 62 patients who had total and partial thyroidectomy surgery between 2010 and 2011 at the Monash University Endocrine Surgery Unit. To subjectively measure voice quality after surgery, the researchers used the Voice Disorder Index (VDI), which measures voice quality on a 0-40 scale from best to worst. After surgery, the mean VDI score in this group showed a 5.2 plus or minus 1.2–point deterioration from 4.2 to 9.4 (P less than .001). For objective evaluation, the researchers used the Dysphonia Severity Index (DSI), which scores voice quality on a scale of –5 to 5 from worst to best. After surgery, the mean DSI score showed a 1.1 plus or minus 0.2–point deterioration from 3.9 to 2.8 (P less than .001). Two speech pathologists conducted the voice assessments.
“Subjective scoring of both hemithyroidectomy and total thyroidectomy reported worse voice postoperatively,” Dr. Lee said. “However, when you take a close look at the numbers, those undergoing total thyroidectomy reported a higher measure of deterioration in their voice.”
Patients who had either partial and total thyroidectomy reported significant subjective deterioration of their voice with mean VDI change from 5.4 to 7.9 (P = 0.02) and 3.5 to 10.6 (P less than .001), respectively. However, on objective evaluation, only the total thyroidectomy patients showed significant voice deterioration, with a mean DSI change from 4 to 2.5 (P less than .001).
Dr. Lee noted that study outcomes between partial and total thyroidectomy patients diverged in another respect: the impact RLN swelling had on voice deterioration. To evaluate RLN swelling, the researchers measured the diameter of the nerve with Vernier calipers before and after the lobectomy during each operation. RLN diameter increased 0.58 plus or minus 0.05 mm on average (P less than .001). In patients who had partial thyroidectomy, the greater the RLN swelling, the worse the subjective score (P = .03). This was not the case in the total thyroidectomy patients where involvement of two nerves complicates the interaction, he said.
During follow-up, the investigators came upon a revelatory finding. “With median 8-month follow-up, the self-reported, VDI scores had returned to baseline levels,” Dr. Lee said. “Interestingly, not only did the objective DSI scores show a return to baseline levels, but it exceeded the baseline levels, meaning the voice had scored better after surgery than before.” However, he noted only 13 patients completed the follow-up.
“Voice change post-thyroidectomy without recurrent laryngeal nerve injury is a complex phenomenon and is likely multifactorial, and we only looked at two of those factors: the extent of surgery and the gradient of recurrent laryngeal nerve injury with nerve edema as a surrogate,” Dr. Lee said. Future studies should evaluate other factors, including the role of the external branch of the superior laryngeal nerve and patient factors such as diabetes or smoking, he said.
Dr. Lee and his coauthors had no disclosures.
JACKSONVILLE, FLA. – Voice quality changes after thyroid surgery are detectable by using both subjective and objective measures, according to investigators at Monash University in Melbourne, Australia.
After thyroid surgery, up to 80% of patients with functional recurrent laryngeal nerves (RLNs) have reported voice changes, so the investigators set out to evaluate the extent of those voice changes and how the extent of the operation and RLN edema may affect them.
“It has been confirmed that thyroid procedures do alter the voice without necessarily causing a measurable recurrent laryngeal nerve palsy,” said lead investigator Dr. James Lee, “and the change of voice is correlated to the extent of surgery and the amount of nerve swelling.” The findings were presented at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study evaluated 62 patients who had total and partial thyroidectomy surgery between 2010 and 2011 at the Monash University Endocrine Surgery Unit. To subjectively measure voice quality after surgery, the researchers used the Voice Disorder Index (VDI), which measures voice quality on a 0-40 scale from best to worst. After surgery, the mean VDI score in this group showed a 5.2 plus or minus 1.2–point deterioration from 4.2 to 9.4 (P less than .001). For objective evaluation, the researchers used the Dysphonia Severity Index (DSI), which scores voice quality on a scale of –5 to 5 from worst to best. After surgery, the mean DSI score showed a 1.1 plus or minus 0.2–point deterioration from 3.9 to 2.8 (P less than .001). Two speech pathologists conducted the voice assessments.
“Subjective scoring of both hemithyroidectomy and total thyroidectomy reported worse voice postoperatively,” Dr. Lee said. “However, when you take a close look at the numbers, those undergoing total thyroidectomy reported a higher measure of deterioration in their voice.”
Patients who had either partial and total thyroidectomy reported significant subjective deterioration of their voice with mean VDI change from 5.4 to 7.9 (P = 0.02) and 3.5 to 10.6 (P less than .001), respectively. However, on objective evaluation, only the total thyroidectomy patients showed significant voice deterioration, with a mean DSI change from 4 to 2.5 (P less than .001).
Dr. Lee noted that study outcomes between partial and total thyroidectomy patients diverged in another respect: the impact RLN swelling had on voice deterioration. To evaluate RLN swelling, the researchers measured the diameter of the nerve with Vernier calipers before and after the lobectomy during each operation. RLN diameter increased 0.58 plus or minus 0.05 mm on average (P less than .001). In patients who had partial thyroidectomy, the greater the RLN swelling, the worse the subjective score (P = .03). This was not the case in the total thyroidectomy patients where involvement of two nerves complicates the interaction, he said.
During follow-up, the investigators came upon a revelatory finding. “With median 8-month follow-up, the self-reported, VDI scores had returned to baseline levels,” Dr. Lee said. “Interestingly, not only did the objective DSI scores show a return to baseline levels, but it exceeded the baseline levels, meaning the voice had scored better after surgery than before.” However, he noted only 13 patients completed the follow-up.
“Voice change post-thyroidectomy without recurrent laryngeal nerve injury is a complex phenomenon and is likely multifactorial, and we only looked at two of those factors: the extent of surgery and the gradient of recurrent laryngeal nerve injury with nerve edema as a surrogate,” Dr. Lee said. Future studies should evaluate other factors, including the role of the external branch of the superior laryngeal nerve and patient factors such as diabetes or smoking, he said.
Dr. Lee and his coauthors had no disclosures.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Voice changes after thyroid surgery directly correlate to the amount of swelling of the recurrent laryngeal nerves as well as the duration and intensity of the operation.
Major finding: Mean subjective voice scores declined from 4.2 to 9.4 on the Voice Disorder Index and mean objective voice scores declined from 3.9 to 2.8 on the Dysphonia Severity Index after thyroidectomy.
Data source: Sixty-two patients undergoing total and hemithyroidectomy were prospectively recruited from the Monash University Endocrine Surgery Unit between 2010 and 2011.
Disclosures: The study authors reported having no financial disclosures.
Study validates cholecystectomy safe in obese
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
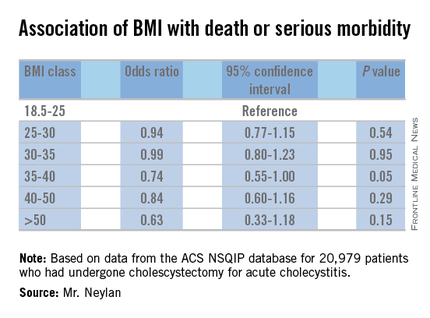
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
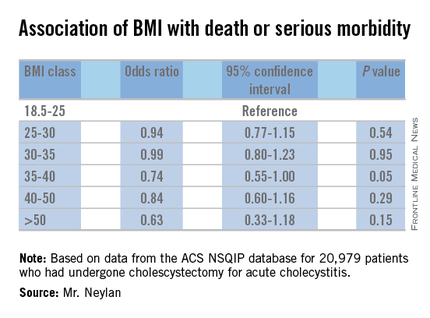
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
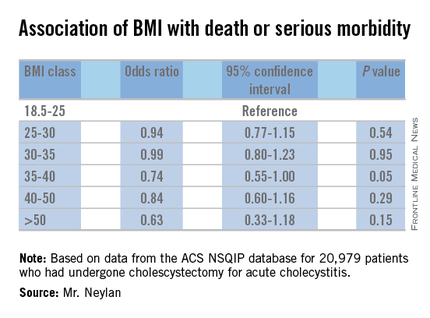
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Cholecystectomy for acute cholecystitis has been found to have a similar safety profile in obese and normal-weight patients.
Major finding: Rates of death/serious morbidity ranged from 6% to 9% across six different weight classes ranging from normal weight to morbidly obese.
Data source: Retrospective analysis of 20,979 patients who had cholecystectomy for cholecystitis from 2008 to 2015 drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database.
Disclosures: The study authors reported having no financial disclosures.
Fresh press: ACS Surgery News February issue online
The February ACS Surgery News digital issue is available online.
This month’s issue features a report on recent trends in prescribing by surgeons in the wake of the DEA reclassification of hydrocodone-containing drugs, a review of the perils of “noncompete” clauses in employment contracts, and a message from the President of the American College of Surgeons, Dr. J. David Richardson.
Don’t miss the commentary on General Surgery’s Place in the World by Dr. Tyler Hughes, now the Associate Editor of ACS Surgery News.
Use the mobile app to download the issue or view as a pdf.
The February ACS Surgery News digital issue is available online.
This month’s issue features a report on recent trends in prescribing by surgeons in the wake of the DEA reclassification of hydrocodone-containing drugs, a review of the perils of “noncompete” clauses in employment contracts, and a message from the President of the American College of Surgeons, Dr. J. David Richardson.
Don’t miss the commentary on General Surgery’s Place in the World by Dr. Tyler Hughes, now the Associate Editor of ACS Surgery News.
Use the mobile app to download the issue or view as a pdf.
The February ACS Surgery News digital issue is available online.
This month’s issue features a report on recent trends in prescribing by surgeons in the wake of the DEA reclassification of hydrocodone-containing drugs, a review of the perils of “noncompete” clauses in employment contracts, and a message from the President of the American College of Surgeons, Dr. J. David Richardson.
Don’t miss the commentary on General Surgery’s Place in the World by Dr. Tyler Hughes, now the Associate Editor of ACS Surgery News.
Use the mobile app to download the issue or view as a pdf.
Best closure for contaminated ventral hernia depends on primary surgical objective
Outcomes after contaminated open ventral hernia repair did not differ significantly, whether the incision was closed using sutures, low- or mid-density polypropylene mesh, or non–cross-linked biologic matrix material, in a multicenter study reported online in the Journal of Surgical Research.
In the absence of high-level evidence favoring any of these approaches, surgeons should carefully balance the risks and costs against the benefits when choosing how to close such incisions, said Ioana L. Bondre of the department of surgery, University of Texas Health Science Center, Houston, and her associates.
At present, there is no widely accepted consensus and certainly no clinical guidelines regarding closure of contaminated ventral hernias. It is assumed that synthetic mesh and biologic mesh reduce the rate of hernia recurrence but at the cost of increased wound complications and surgical site infections. To examine this issue, the investigators performed a retrospective analysis of information in a database of all consecutive open ventral hernia repairs performed at seven medical centers during a 2-year period.
They focused on 761 patients in whom the repair was closed using sutures (38%), synthetic mesh (40%), or biologic matrix (22%). Thirty-day rates of surgical site infection (15.1%, 17.8%, and 21.0%, respectively), hernia recurrence (17.8%, 13.5%, and 21.5%, respectively), and reoperation (31.7%, 10.9%, and 15.6%, respectively) did not differ significantly among these three groups, Ms. Bondre and her associates said (J Surg Res. 2016 Feb;200[2]:488-94).
“Based on the available evidence, we currently recommend decisions to be based on the primary purpose of the procedure. If the primary purpose is not to perform a hernia repair (e.g., laparoscopic appendectomy for appendicitis), then a suture repair should be performed (e.g., umbilical hernia repair with sutures). However, if the primary purpose of the procedure includes hernia repair (e.g., colostomy reversal and parastomal hernia repair), mesh reinforcement should be used. Given the current evidence and practice patterns, we use mid-density synthetic mesh in wound class I procedures and biologic mesh in wound class II-IV repairs,” they noted.
This study was limited in that many patients were followed for only 1 month, which may not be sufficient time to capture long-term outcomes. Moreover, the database didn’t include information regarding outcomes that are most important to patients, such as chronic pain, chronic infections, and nonhealing surgical wounds, Ms. Bondre and her associates added.
This study was supported by the Center for Clinical and Translational Sciences. The authors’ financial disclosures were not reported.
Outcomes after contaminated open ventral hernia repair did not differ significantly, whether the incision was closed using sutures, low- or mid-density polypropylene mesh, or non–cross-linked biologic matrix material, in a multicenter study reported online in the Journal of Surgical Research.
In the absence of high-level evidence favoring any of these approaches, surgeons should carefully balance the risks and costs against the benefits when choosing how to close such incisions, said Ioana L. Bondre of the department of surgery, University of Texas Health Science Center, Houston, and her associates.
At present, there is no widely accepted consensus and certainly no clinical guidelines regarding closure of contaminated ventral hernias. It is assumed that synthetic mesh and biologic mesh reduce the rate of hernia recurrence but at the cost of increased wound complications and surgical site infections. To examine this issue, the investigators performed a retrospective analysis of information in a database of all consecutive open ventral hernia repairs performed at seven medical centers during a 2-year period.
They focused on 761 patients in whom the repair was closed using sutures (38%), synthetic mesh (40%), or biologic matrix (22%). Thirty-day rates of surgical site infection (15.1%, 17.8%, and 21.0%, respectively), hernia recurrence (17.8%, 13.5%, and 21.5%, respectively), and reoperation (31.7%, 10.9%, and 15.6%, respectively) did not differ significantly among these three groups, Ms. Bondre and her associates said (J Surg Res. 2016 Feb;200[2]:488-94).
“Based on the available evidence, we currently recommend decisions to be based on the primary purpose of the procedure. If the primary purpose is not to perform a hernia repair (e.g., laparoscopic appendectomy for appendicitis), then a suture repair should be performed (e.g., umbilical hernia repair with sutures). However, if the primary purpose of the procedure includes hernia repair (e.g., colostomy reversal and parastomal hernia repair), mesh reinforcement should be used. Given the current evidence and practice patterns, we use mid-density synthetic mesh in wound class I procedures and biologic mesh in wound class II-IV repairs,” they noted.
This study was limited in that many patients were followed for only 1 month, which may not be sufficient time to capture long-term outcomes. Moreover, the database didn’t include information regarding outcomes that are most important to patients, such as chronic pain, chronic infections, and nonhealing surgical wounds, Ms. Bondre and her associates added.
This study was supported by the Center for Clinical and Translational Sciences. The authors’ financial disclosures were not reported.
Outcomes after contaminated open ventral hernia repair did not differ significantly, whether the incision was closed using sutures, low- or mid-density polypropylene mesh, or non–cross-linked biologic matrix material, in a multicenter study reported online in the Journal of Surgical Research.
In the absence of high-level evidence favoring any of these approaches, surgeons should carefully balance the risks and costs against the benefits when choosing how to close such incisions, said Ioana L. Bondre of the department of surgery, University of Texas Health Science Center, Houston, and her associates.
At present, there is no widely accepted consensus and certainly no clinical guidelines regarding closure of contaminated ventral hernias. It is assumed that synthetic mesh and biologic mesh reduce the rate of hernia recurrence but at the cost of increased wound complications and surgical site infections. To examine this issue, the investigators performed a retrospective analysis of information in a database of all consecutive open ventral hernia repairs performed at seven medical centers during a 2-year period.
They focused on 761 patients in whom the repair was closed using sutures (38%), synthetic mesh (40%), or biologic matrix (22%). Thirty-day rates of surgical site infection (15.1%, 17.8%, and 21.0%, respectively), hernia recurrence (17.8%, 13.5%, and 21.5%, respectively), and reoperation (31.7%, 10.9%, and 15.6%, respectively) did not differ significantly among these three groups, Ms. Bondre and her associates said (J Surg Res. 2016 Feb;200[2]:488-94).
“Based on the available evidence, we currently recommend decisions to be based on the primary purpose of the procedure. If the primary purpose is not to perform a hernia repair (e.g., laparoscopic appendectomy for appendicitis), then a suture repair should be performed (e.g., umbilical hernia repair with sutures). However, if the primary purpose of the procedure includes hernia repair (e.g., colostomy reversal and parastomal hernia repair), mesh reinforcement should be used. Given the current evidence and practice patterns, we use mid-density synthetic mesh in wound class I procedures and biologic mesh in wound class II-IV repairs,” they noted.
This study was limited in that many patients were followed for only 1 month, which may not be sufficient time to capture long-term outcomes. Moreover, the database didn’t include information regarding outcomes that are most important to patients, such as chronic pain, chronic infections, and nonhealing surgical wounds, Ms. Bondre and her associates added.
This study was supported by the Center for Clinical and Translational Sciences. The authors’ financial disclosures were not reported.
FROM JOURNAL OF SURGICAL RESEARCH
Key clinical point: Outcomes after surgery did not differ significantly, whether the incision was closed using sutures, low- or mid-density polypropylene mesh, or non–cross-linked biologic matrix material.
Major finding: Thirty-day rates of surgical site infection, hernia recurrence, and reoperation did not differ significantly among patients in whom the repair was closed using sutures (38%), synthetic mesh (40%), or biologic matrix (22%).
Data source: A retrospective analysis of consecutive open contaminated ventral hernia repairs performed at seven medical centers during a 2-year period.
Disclosures: This study was supported by the Center for Clinical and Translational Sciences. The authors’ financial disclosures were not reported.
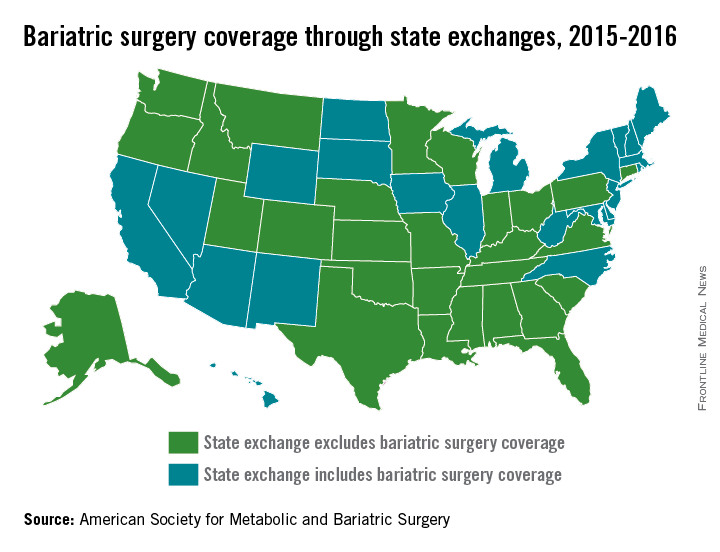
Majority of state exchanges exclude bariatric coverage
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
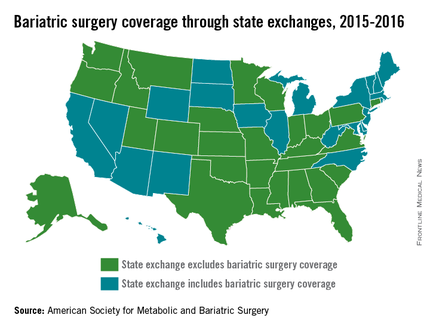
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
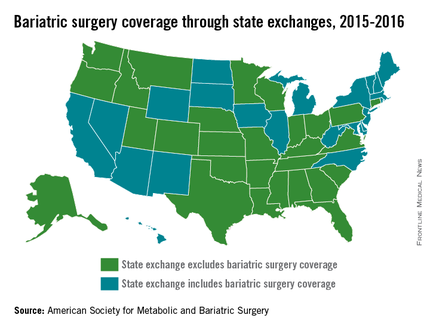
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
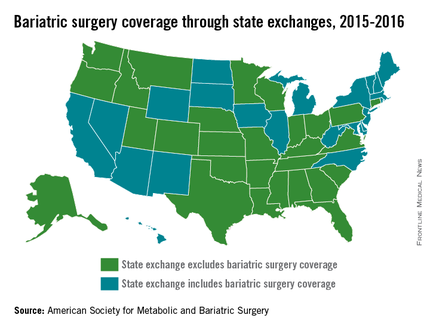
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”
Hernia repair: Studies don’t support use of higher-cost biological mesh
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point: The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, and the expense associated with their use cannot be justified at this time, a systematic review of the literature suggested.
Major finding: Available evidence remains insufficient to determine whether cost and clinical benefits exist with the use of biological mesh for abdominal wall hernia repair.
Data source: A systematic review of the literature, yielding 20 eligible studies.
Disclosures: This study was supported by the Hudson-Penn Endowment fund at University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.