User login
AACE: Try medical management before surgery for hyperinsulinemic hypoglycemia after gastric bypass
NASHVILLE, TENN. – Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgery can be managed or even corrected by medical management with calcium channel blockers or acarbose.
First described in 2005, it is a rare complication distinct from dumping syndrome, which is common after bypass. For unknown reasons, the pancreas starts to oversecrete insulin in response to even small meals a few months to a few decades after gastric bypass surgery. Until now, treatment has often meant partial or even total pancreatectomy (N. Engl. J. Med. 2005;353:249-54).
“The message from me is very simple: There’s a medical alternative to surgery. Before you take these people to surgery, try medical management,” said Dr. John Mordes, an endocrinologist and professor of medicine at the University of Massachusetts Medical School in Worcester.
The study involved five patients, who were seen there after suddenly developing severe, sometimes daily, postprandial hypoglycemic attacks from 1 to 26 years after Roux-en-Y bypass; several had passed out after meals. On 75-g fasting-glucose challenges, their insulin levels were at or above 17 microU/mL, despite glucose concentrations at or below 54 mg/dL. None of the patients had evidence of insulinomas, and none was on exogenous insulin or diabetes drugs. Their hemoglobin A1c levels were below 6% (Endocr. Pract. 2015;21:237-46).
The first patient refused surgery, “so we researched the literature” and found that nifedipine helped infants with congenital nesidioblastosis in a study from India. The drug worked at a dose of 30 mg extended release once daily; 30 mg t.i.d. worked in the second patient. Calcium channel blockers blunt insulin secretion, which probably explains why nifedipine helped, Dr. Mordes said at the annual meeting of the American Association of Clinical Endocrinologists.
Both patients stopped taking the pills on their own after about 3 years; their symptoms hadn’t returned after a year or more of follow-up.
The third and fourth patients couldn’t tolerate nifedipine, so Dr. Mordes tried acarbose to slow absorption of glucose from the gut; it also worked. One patient has had only two mild attacks on 50 mg t.i.d for 15 months; the fourth was symptom free while on 25 mg t.i.d for 2 months. That patient stopped the drug at that point, and remained symptom free for 9 more months, but since then has had about one attack a month. The fifth patient has been symptom free for about 6 months on a combination of nifedipine 20 mg t.i.d. and acarbose 50 mg t.i.d, and has no intention of stopping either.
The subjects gained from a few to almost 50 pounds while on the drugs, which might also have contributed to their recovery. Overall, they “are fine now. None of them have needed surgery,” and they’re happy to have avoided it, Dr. Mordes said.
All that’s needed to diagnose the problem is a history of exclusively postprandial symptoms of hypoglycemia with no vasomotor or bowel symptoms suggestive of dumping, plus confirmatory blood work. Invasive tests aren’t necessary, he said.
A sixth patient didn’t respond to nifedipine, acarbose, or the insulinoma drug diazoxide, but she was atypical in that she had a decades-long history of nocturnal hypoglycemic events following a gastric bypass in Mexico at age 13 years for pyloric stenosis. “Something is very different about her,” Dr. Mordes said.
He said he had no relevant financial disclosures, and no outside funding for his work.
NASHVILLE, TENN. – Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgery can be managed or even corrected by medical management with calcium channel blockers or acarbose.
First described in 2005, it is a rare complication distinct from dumping syndrome, which is common after bypass. For unknown reasons, the pancreas starts to oversecrete insulin in response to even small meals a few months to a few decades after gastric bypass surgery. Until now, treatment has often meant partial or even total pancreatectomy (N. Engl. J. Med. 2005;353:249-54).
“The message from me is very simple: There’s a medical alternative to surgery. Before you take these people to surgery, try medical management,” said Dr. John Mordes, an endocrinologist and professor of medicine at the University of Massachusetts Medical School in Worcester.
The study involved five patients, who were seen there after suddenly developing severe, sometimes daily, postprandial hypoglycemic attacks from 1 to 26 years after Roux-en-Y bypass; several had passed out after meals. On 75-g fasting-glucose challenges, their insulin levels were at or above 17 microU/mL, despite glucose concentrations at or below 54 mg/dL. None of the patients had evidence of insulinomas, and none was on exogenous insulin or diabetes drugs. Their hemoglobin A1c levels were below 6% (Endocr. Pract. 2015;21:237-46).
The first patient refused surgery, “so we researched the literature” and found that nifedipine helped infants with congenital nesidioblastosis in a study from India. The drug worked at a dose of 30 mg extended release once daily; 30 mg t.i.d. worked in the second patient. Calcium channel blockers blunt insulin secretion, which probably explains why nifedipine helped, Dr. Mordes said at the annual meeting of the American Association of Clinical Endocrinologists.
Both patients stopped taking the pills on their own after about 3 years; their symptoms hadn’t returned after a year or more of follow-up.
The third and fourth patients couldn’t tolerate nifedipine, so Dr. Mordes tried acarbose to slow absorption of glucose from the gut; it also worked. One patient has had only two mild attacks on 50 mg t.i.d for 15 months; the fourth was symptom free while on 25 mg t.i.d for 2 months. That patient stopped the drug at that point, and remained symptom free for 9 more months, but since then has had about one attack a month. The fifth patient has been symptom free for about 6 months on a combination of nifedipine 20 mg t.i.d. and acarbose 50 mg t.i.d, and has no intention of stopping either.
The subjects gained from a few to almost 50 pounds while on the drugs, which might also have contributed to their recovery. Overall, they “are fine now. None of them have needed surgery,” and they’re happy to have avoided it, Dr. Mordes said.
All that’s needed to diagnose the problem is a history of exclusively postprandial symptoms of hypoglycemia with no vasomotor or bowel symptoms suggestive of dumping, plus confirmatory blood work. Invasive tests aren’t necessary, he said.
A sixth patient didn’t respond to nifedipine, acarbose, or the insulinoma drug diazoxide, but she was atypical in that she had a decades-long history of nocturnal hypoglycemic events following a gastric bypass in Mexico at age 13 years for pyloric stenosis. “Something is very different about her,” Dr. Mordes said.
He said he had no relevant financial disclosures, and no outside funding for his work.
NASHVILLE, TENN. – Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgery can be managed or even corrected by medical management with calcium channel blockers or acarbose.
First described in 2005, it is a rare complication distinct from dumping syndrome, which is common after bypass. For unknown reasons, the pancreas starts to oversecrete insulin in response to even small meals a few months to a few decades after gastric bypass surgery. Until now, treatment has often meant partial or even total pancreatectomy (N. Engl. J. Med. 2005;353:249-54).
“The message from me is very simple: There’s a medical alternative to surgery. Before you take these people to surgery, try medical management,” said Dr. John Mordes, an endocrinologist and professor of medicine at the University of Massachusetts Medical School in Worcester.
The study involved five patients, who were seen there after suddenly developing severe, sometimes daily, postprandial hypoglycemic attacks from 1 to 26 years after Roux-en-Y bypass; several had passed out after meals. On 75-g fasting-glucose challenges, their insulin levels were at or above 17 microU/mL, despite glucose concentrations at or below 54 mg/dL. None of the patients had evidence of insulinomas, and none was on exogenous insulin or diabetes drugs. Their hemoglobin A1c levels were below 6% (Endocr. Pract. 2015;21:237-46).
The first patient refused surgery, “so we researched the literature” and found that nifedipine helped infants with congenital nesidioblastosis in a study from India. The drug worked at a dose of 30 mg extended release once daily; 30 mg t.i.d. worked in the second patient. Calcium channel blockers blunt insulin secretion, which probably explains why nifedipine helped, Dr. Mordes said at the annual meeting of the American Association of Clinical Endocrinologists.
Both patients stopped taking the pills on their own after about 3 years; their symptoms hadn’t returned after a year or more of follow-up.
The third and fourth patients couldn’t tolerate nifedipine, so Dr. Mordes tried acarbose to slow absorption of glucose from the gut; it also worked. One patient has had only two mild attacks on 50 mg t.i.d for 15 months; the fourth was symptom free while on 25 mg t.i.d for 2 months. That patient stopped the drug at that point, and remained symptom free for 9 more months, but since then has had about one attack a month. The fifth patient has been symptom free for about 6 months on a combination of nifedipine 20 mg t.i.d. and acarbose 50 mg t.i.d, and has no intention of stopping either.
The subjects gained from a few to almost 50 pounds while on the drugs, which might also have contributed to their recovery. Overall, they “are fine now. None of them have needed surgery,” and they’re happy to have avoided it, Dr. Mordes said.
All that’s needed to diagnose the problem is a history of exclusively postprandial symptoms of hypoglycemia with no vasomotor or bowel symptoms suggestive of dumping, plus confirmatory blood work. Invasive tests aren’t necessary, he said.
A sixth patient didn’t respond to nifedipine, acarbose, or the insulinoma drug diazoxide, but she was atypical in that she had a decades-long history of nocturnal hypoglycemic events following a gastric bypass in Mexico at age 13 years for pyloric stenosis. “Something is very different about her,” Dr. Mordes said.
He said he had no relevant financial disclosures, and no outside funding for his work.
AT AACE 2015
Key clinical point: Hyperinsulinemic hypoglycemia after gastric bypass doesn’t require surgery.
Major finding: Hypoglycemic attacks were reduced or eliminated by nifedipine, acarbose, or both in five patients with hyperinsulinemic hypoglycemia after gastric bypass.
Data source: A case series at the University of Massachusetts Medical School.
Disclosures: The investigator said he had no relevant financial disclosures, and no outside funding for his work.
Thyroid surgery on the rise
There was a steady rise in the number of endocrine procedures being performed in the United States over the past decade, according to a new publication from the Endocrine Society.
Thyroid disease treatment costs in U.S. women alone totaled $4.3 billion in 2008, representing a cost of $343 per patient, according to the report, authored by the Endocrine Society under the guidance of an advisory committee chaired by Dr. Robert A. Vigersky, head of the Diabetes Institute at Walter Reed National Military Medical Center in Bethesda, Md.
The number of endocrine procedures also has increased steadily, mainly because of new and improved surgical techniques, but the annual case number is predicted to go as high as 173,000 by 2020.
Thyroid conditions affect five times as many women as men, particularly in the case of Hashimoto’s disease – the incidence in women is more than eight times that in men – and Graves’ disease, where women have a nearly sixfold higher incidence than men, according to the report, which is available online.
The most common thyroid disease is thyroid nodules, which international studies estimate affect up to 60% of the population. In the United States, findings from a study using chest radiography found nearly one in four adult outpatients had thyroid nodules.
The diagnosis of thyroid nodules has increased as imaging technologies such as CT scanning, ultrasound, and MRI improve on the traditional diagnostic method of physical examination. The increase in thyroid surgery for this condition has raised questions about whether this has led to improved outcomes.
Hyperthyroidism and hypothyroidism have a lower prevalence, although estimates suggest as much as 13% of the U.S. population has subclinical hypothyroidism.
This has implications particularly in pregnancy, as subclinical hypothyroidism may increase the risk of pregnancy complications, including preeclampsia, placental abruption, preterm birth, and neonatal mortality.
One study found that 12.4% of healthy pregnant women with no known thyroid disease had subclinical hypothyroidism. Overt hypothyroidism affects around 0.8% of adults, while overt hyperthyroidism affects just 0.5% of adults, the report stated.
Graves’ disease is one form of hyperthyroidism, and it has a prevalence in the U.S. population of 0.63%-1.49%, mostly affecting women, African Americans, and Asian/Pacific Islanders.
This condition is most commonly treated with antithyroid drugs or radioactive iodine therapy, although around 0.7% of patients undergo thyroidectomies.
Another group of thyroid diseases, grouped under the umbrella term of thyroiditis, includes a common element of inflammation of the thyroid gland. Among them is the autoimmune condition Hashimoto’s thyroiditis, which is thought to affect around 4.6% of the population.
Postpartum thyroiditis – an inflammatory autoimmune condition that develops in the first year after delivery – is estimated to have a prevalence around 4.5%, according to one review.
“Evidence is emerging that as women age subclinical hypothyroidism – as a sequel of postpartum thyroiditis – predisposes them to cardiovascular disease,” wrote Dr. Vigersky, also of the Uniformed Services University of the Health Sciences, and the other panel members.
“Hence, postpartum thyroiditis is no longer considered a mild and transient disorder.”
The report was produced by the Endocrine Society. There were no conflicts of interest declared.
There was a steady rise in the number of endocrine procedures being performed in the United States over the past decade, according to a new publication from the Endocrine Society.
Thyroid disease treatment costs in U.S. women alone totaled $4.3 billion in 2008, representing a cost of $343 per patient, according to the report, authored by the Endocrine Society under the guidance of an advisory committee chaired by Dr. Robert A. Vigersky, head of the Diabetes Institute at Walter Reed National Military Medical Center in Bethesda, Md.
The number of endocrine procedures also has increased steadily, mainly because of new and improved surgical techniques, but the annual case number is predicted to go as high as 173,000 by 2020.
Thyroid conditions affect five times as many women as men, particularly in the case of Hashimoto’s disease – the incidence in women is more than eight times that in men – and Graves’ disease, where women have a nearly sixfold higher incidence than men, according to the report, which is available online.
The most common thyroid disease is thyroid nodules, which international studies estimate affect up to 60% of the population. In the United States, findings from a study using chest radiography found nearly one in four adult outpatients had thyroid nodules.
The diagnosis of thyroid nodules has increased as imaging technologies such as CT scanning, ultrasound, and MRI improve on the traditional diagnostic method of physical examination. The increase in thyroid surgery for this condition has raised questions about whether this has led to improved outcomes.
Hyperthyroidism and hypothyroidism have a lower prevalence, although estimates suggest as much as 13% of the U.S. population has subclinical hypothyroidism.
This has implications particularly in pregnancy, as subclinical hypothyroidism may increase the risk of pregnancy complications, including preeclampsia, placental abruption, preterm birth, and neonatal mortality.
One study found that 12.4% of healthy pregnant women with no known thyroid disease had subclinical hypothyroidism. Overt hypothyroidism affects around 0.8% of adults, while overt hyperthyroidism affects just 0.5% of adults, the report stated.
Graves’ disease is one form of hyperthyroidism, and it has a prevalence in the U.S. population of 0.63%-1.49%, mostly affecting women, African Americans, and Asian/Pacific Islanders.
This condition is most commonly treated with antithyroid drugs or radioactive iodine therapy, although around 0.7% of patients undergo thyroidectomies.
Another group of thyroid diseases, grouped under the umbrella term of thyroiditis, includes a common element of inflammation of the thyroid gland. Among them is the autoimmune condition Hashimoto’s thyroiditis, which is thought to affect around 4.6% of the population.
Postpartum thyroiditis – an inflammatory autoimmune condition that develops in the first year after delivery – is estimated to have a prevalence around 4.5%, according to one review.
“Evidence is emerging that as women age subclinical hypothyroidism – as a sequel of postpartum thyroiditis – predisposes them to cardiovascular disease,” wrote Dr. Vigersky, also of the Uniformed Services University of the Health Sciences, and the other panel members.
“Hence, postpartum thyroiditis is no longer considered a mild and transient disorder.”
The report was produced by the Endocrine Society. There were no conflicts of interest declared.
There was a steady rise in the number of endocrine procedures being performed in the United States over the past decade, according to a new publication from the Endocrine Society.
Thyroid disease treatment costs in U.S. women alone totaled $4.3 billion in 2008, representing a cost of $343 per patient, according to the report, authored by the Endocrine Society under the guidance of an advisory committee chaired by Dr. Robert A. Vigersky, head of the Diabetes Institute at Walter Reed National Military Medical Center in Bethesda, Md.
The number of endocrine procedures also has increased steadily, mainly because of new and improved surgical techniques, but the annual case number is predicted to go as high as 173,000 by 2020.
Thyroid conditions affect five times as many women as men, particularly in the case of Hashimoto’s disease – the incidence in women is more than eight times that in men – and Graves’ disease, where women have a nearly sixfold higher incidence than men, according to the report, which is available online.
The most common thyroid disease is thyroid nodules, which international studies estimate affect up to 60% of the population. In the United States, findings from a study using chest radiography found nearly one in four adult outpatients had thyroid nodules.
The diagnosis of thyroid nodules has increased as imaging technologies such as CT scanning, ultrasound, and MRI improve on the traditional diagnostic method of physical examination. The increase in thyroid surgery for this condition has raised questions about whether this has led to improved outcomes.
Hyperthyroidism and hypothyroidism have a lower prevalence, although estimates suggest as much as 13% of the U.S. population has subclinical hypothyroidism.
This has implications particularly in pregnancy, as subclinical hypothyroidism may increase the risk of pregnancy complications, including preeclampsia, placental abruption, preterm birth, and neonatal mortality.
One study found that 12.4% of healthy pregnant women with no known thyroid disease had subclinical hypothyroidism. Overt hypothyroidism affects around 0.8% of adults, while overt hyperthyroidism affects just 0.5% of adults, the report stated.
Graves’ disease is one form of hyperthyroidism, and it has a prevalence in the U.S. population of 0.63%-1.49%, mostly affecting women, African Americans, and Asian/Pacific Islanders.
This condition is most commonly treated with antithyroid drugs or radioactive iodine therapy, although around 0.7% of patients undergo thyroidectomies.
Another group of thyroid diseases, grouped under the umbrella term of thyroiditis, includes a common element of inflammation of the thyroid gland. Among them is the autoimmune condition Hashimoto’s thyroiditis, which is thought to affect around 4.6% of the population.
Postpartum thyroiditis – an inflammatory autoimmune condition that develops in the first year after delivery – is estimated to have a prevalence around 4.5%, according to one review.
“Evidence is emerging that as women age subclinical hypothyroidism – as a sequel of postpartum thyroiditis – predisposes them to cardiovascular disease,” wrote Dr. Vigersky, also of the Uniformed Services University of the Health Sciences, and the other panel members.
“Hence, postpartum thyroiditis is no longer considered a mild and transient disorder.”
The report was produced by the Endocrine Society. There were no conflicts of interest declared.
Key clinical point: There was a steady rise in the number of endocrine procedures performed in the United States over the past decade.
Major finding: In 2008, thyroid disease treatment costs in women alone totaled $4.3 billion.
Data source: A publication of the Endocrine Society.
Disclosures: The report was produced by the Endocrine Society. There were no conflicts of interest declared.
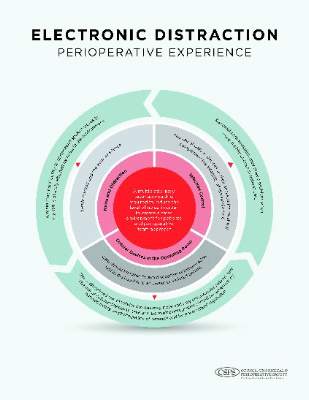
Distractions in the OR increase surgeons’ stress
Distractions in the operating room are associated with increased mental strain, stress, and poor teamwork, according to findings of a cross-sectional, prospective observational study of 90 general surgery cases.
Ana Wheelock of the department of surgery and cancer, Imperial College, London, and her associates stated that previous studies have described a variety of distractions in the OR, but have failed to explore the impact of this factor on surgeons, anesthesiologists, and nurses (Ann. Surg. 2015;261:1079-84).
There is evidence to suggest that distractions such as noise and non–case-related conversation in the OR are linked to a higher rate of errors and adverse events, but the chain of events leading to these errors has been understudied (World J. Surg. 2008;32:1643-50; Qual. Saf. Health Care 2007;16:135-9).
For this study, to capture the variety of events and resulting impacts on the work process in the OR, two trained researchers – one surgeon and one behavioral scientist – observed each case. To prevent a Hawthorne effect, the researchers were present in the OR before the study began to acclimatize staff to their presence.
The case sample yielded 69 hours and 40 minutes of real-time observation. Both open and laparoscopic procedures were represented, and cases included appendectomy, inguinal hernia repair, thyroidectomy, varicose vein surgery, and mastectomy. Mean operative time for the cases was 46 minutes, and American Society of Anesthesiologists (ASA) classification of the cases ranged from I to IV. Data were collected from 85 staff (23 surgeons, 28 anesthesiologists, and 34 nurses).
The study focused on three factors with implications for performance: workload, stress, and teamwork. Workload was measured with the validated NASA-Task Load Index tool, widely used in aviation and other high-risk occupations. Six aspects of workload (mental, physical, and temporal demands; frustration; effort; and performance) were measured via interview in each team member after each procedure. Stress level was scored with the State Trait Anxiety Inventory (STAI) in the same way. Teamwork factors were reported with a validated Observational Teamwork Assessment for Surgery (OTAS) tool.
The findings show that distractions were ubiquitous: Fewer than 2% of cases occurred with zero distractions. The most prevalent distraction involved staff entering the OR (81% of which were deemed unnecessary), followed by case-irrelevant conversation, and equipment failures or absences.
The observers noted a wide variety of disruptions: cell phones ringing, missing equipment, malfunctioning lights, requests by an administrator for a few minutes of the surgeon’s time during the operation, overlapping and nonrelevant conversations among nurses about misplaced files and lunch, and external staff entering and leaving the OR. Distractions occurred in 98% of the operations observed and coincided with normal noise of OR machines, dropped instruments, and distant paging. The mean number of intraoperative distractions was 11 per case.
How did these distractions affect surgeons? Teamwork scores (communication, coordination, leadership, and monitoring) were correlated negatively (r = –0.46) with distractions, case-irrelevant conversation initiated by fellow surgeons in particular. Equipment failures also had a negative impact on these teamwork elements for surgeons (r = –0.41). Workload and stress scores for surgeons showed a negative correlation between these factors and the amount of conversation initiated by other surgeons (r = –0.31 and –0.26, respectively). Acoustic distractions from cell phones, monitors, equipment, and dropped instruments were positively associated with higher stress levels among surgeons (r = 0.30).
Fewer distractions were observed, however, in longer cases and also in cases with a higher degree of patient morbidity.
The study is limited by the case mix of relatively short procedures and low patient ASAs. Only global scores were obtained, which did not allow a more detailed analysis of different stages of procedures. In addition, surgical outcomes were not assessed. The researchers noted, however, that “although there were no associations between external distractions and our outcome measures [ASA classification], the sheer number of unnecessary external visitors to the ORs that we observed should be a cause for concern, as high personnel flow through ORs has been significantly associated with hospital acquired infections” (Clin. Infect. Dis. 1991;13:S800-4).
The takeaway from this study, according to the researchers, is that many of these distractions that have a negative impact on workload, stress, and teamwork function are preventable. “Although some distractions may be inevitable, others, particularly during tasks that require undivided attention, should be proactively limited as they can induce human error and have negative consequences on patient safety ... a clearer understanding of the interaction between the team and the OR environment is imperative if we are to truly recognize and mitigate all factors that impact upon team performance and error.”
The (U.K.) National Institute for Health Research funded the study. The authors have no disclosures.
Distractions in the operating room are associated with increased mental strain, stress, and poor teamwork, according to findings of a cross-sectional, prospective observational study of 90 general surgery cases.
Ana Wheelock of the department of surgery and cancer, Imperial College, London, and her associates stated that previous studies have described a variety of distractions in the OR, but have failed to explore the impact of this factor on surgeons, anesthesiologists, and nurses (Ann. Surg. 2015;261:1079-84).
There is evidence to suggest that distractions such as noise and non–case-related conversation in the OR are linked to a higher rate of errors and adverse events, but the chain of events leading to these errors has been understudied (World J. Surg. 2008;32:1643-50; Qual. Saf. Health Care 2007;16:135-9).
For this study, to capture the variety of events and resulting impacts on the work process in the OR, two trained researchers – one surgeon and one behavioral scientist – observed each case. To prevent a Hawthorne effect, the researchers were present in the OR before the study began to acclimatize staff to their presence.
The case sample yielded 69 hours and 40 minutes of real-time observation. Both open and laparoscopic procedures were represented, and cases included appendectomy, inguinal hernia repair, thyroidectomy, varicose vein surgery, and mastectomy. Mean operative time for the cases was 46 minutes, and American Society of Anesthesiologists (ASA) classification of the cases ranged from I to IV. Data were collected from 85 staff (23 surgeons, 28 anesthesiologists, and 34 nurses).
The study focused on three factors with implications for performance: workload, stress, and teamwork. Workload was measured with the validated NASA-Task Load Index tool, widely used in aviation and other high-risk occupations. Six aspects of workload (mental, physical, and temporal demands; frustration; effort; and performance) were measured via interview in each team member after each procedure. Stress level was scored with the State Trait Anxiety Inventory (STAI) in the same way. Teamwork factors were reported with a validated Observational Teamwork Assessment for Surgery (OTAS) tool.
The findings show that distractions were ubiquitous: Fewer than 2% of cases occurred with zero distractions. The most prevalent distraction involved staff entering the OR (81% of which were deemed unnecessary), followed by case-irrelevant conversation, and equipment failures or absences.
The observers noted a wide variety of disruptions: cell phones ringing, missing equipment, malfunctioning lights, requests by an administrator for a few minutes of the surgeon’s time during the operation, overlapping and nonrelevant conversations among nurses about misplaced files and lunch, and external staff entering and leaving the OR. Distractions occurred in 98% of the operations observed and coincided with normal noise of OR machines, dropped instruments, and distant paging. The mean number of intraoperative distractions was 11 per case.
How did these distractions affect surgeons? Teamwork scores (communication, coordination, leadership, and monitoring) were correlated negatively (r = –0.46) with distractions, case-irrelevant conversation initiated by fellow surgeons in particular. Equipment failures also had a negative impact on these teamwork elements for surgeons (r = –0.41). Workload and stress scores for surgeons showed a negative correlation between these factors and the amount of conversation initiated by other surgeons (r = –0.31 and –0.26, respectively). Acoustic distractions from cell phones, monitors, equipment, and dropped instruments were positively associated with higher stress levels among surgeons (r = 0.30).
Fewer distractions were observed, however, in longer cases and also in cases with a higher degree of patient morbidity.
The study is limited by the case mix of relatively short procedures and low patient ASAs. Only global scores were obtained, which did not allow a more detailed analysis of different stages of procedures. In addition, surgical outcomes were not assessed. The researchers noted, however, that “although there were no associations between external distractions and our outcome measures [ASA classification], the sheer number of unnecessary external visitors to the ORs that we observed should be a cause for concern, as high personnel flow through ORs has been significantly associated with hospital acquired infections” (Clin. Infect. Dis. 1991;13:S800-4).
The takeaway from this study, according to the researchers, is that many of these distractions that have a negative impact on workload, stress, and teamwork function are preventable. “Although some distractions may be inevitable, others, particularly during tasks that require undivided attention, should be proactively limited as they can induce human error and have negative consequences on patient safety ... a clearer understanding of the interaction between the team and the OR environment is imperative if we are to truly recognize and mitigate all factors that impact upon team performance and error.”
The (U.K.) National Institute for Health Research funded the study. The authors have no disclosures.
Distractions in the operating room are associated with increased mental strain, stress, and poor teamwork, according to findings of a cross-sectional, prospective observational study of 90 general surgery cases.
Ana Wheelock of the department of surgery and cancer, Imperial College, London, and her associates stated that previous studies have described a variety of distractions in the OR, but have failed to explore the impact of this factor on surgeons, anesthesiologists, and nurses (Ann. Surg. 2015;261:1079-84).
There is evidence to suggest that distractions such as noise and non–case-related conversation in the OR are linked to a higher rate of errors and adverse events, but the chain of events leading to these errors has been understudied (World J. Surg. 2008;32:1643-50; Qual. Saf. Health Care 2007;16:135-9).
For this study, to capture the variety of events and resulting impacts on the work process in the OR, two trained researchers – one surgeon and one behavioral scientist – observed each case. To prevent a Hawthorne effect, the researchers were present in the OR before the study began to acclimatize staff to their presence.
The case sample yielded 69 hours and 40 minutes of real-time observation. Both open and laparoscopic procedures were represented, and cases included appendectomy, inguinal hernia repair, thyroidectomy, varicose vein surgery, and mastectomy. Mean operative time for the cases was 46 minutes, and American Society of Anesthesiologists (ASA) classification of the cases ranged from I to IV. Data were collected from 85 staff (23 surgeons, 28 anesthesiologists, and 34 nurses).
The study focused on three factors with implications for performance: workload, stress, and teamwork. Workload was measured with the validated NASA-Task Load Index tool, widely used in aviation and other high-risk occupations. Six aspects of workload (mental, physical, and temporal demands; frustration; effort; and performance) were measured via interview in each team member after each procedure. Stress level was scored with the State Trait Anxiety Inventory (STAI) in the same way. Teamwork factors were reported with a validated Observational Teamwork Assessment for Surgery (OTAS) tool.
The findings show that distractions were ubiquitous: Fewer than 2% of cases occurred with zero distractions. The most prevalent distraction involved staff entering the OR (81% of which were deemed unnecessary), followed by case-irrelevant conversation, and equipment failures or absences.
The observers noted a wide variety of disruptions: cell phones ringing, missing equipment, malfunctioning lights, requests by an administrator for a few minutes of the surgeon’s time during the operation, overlapping and nonrelevant conversations among nurses about misplaced files and lunch, and external staff entering and leaving the OR. Distractions occurred in 98% of the operations observed and coincided with normal noise of OR machines, dropped instruments, and distant paging. The mean number of intraoperative distractions was 11 per case.
How did these distractions affect surgeons? Teamwork scores (communication, coordination, leadership, and monitoring) were correlated negatively (r = –0.46) with distractions, case-irrelevant conversation initiated by fellow surgeons in particular. Equipment failures also had a negative impact on these teamwork elements for surgeons (r = –0.41). Workload and stress scores for surgeons showed a negative correlation between these factors and the amount of conversation initiated by other surgeons (r = –0.31 and –0.26, respectively). Acoustic distractions from cell phones, monitors, equipment, and dropped instruments were positively associated with higher stress levels among surgeons (r = 0.30).
Fewer distractions were observed, however, in longer cases and also in cases with a higher degree of patient morbidity.
The study is limited by the case mix of relatively short procedures and low patient ASAs. Only global scores were obtained, which did not allow a more detailed analysis of different stages of procedures. In addition, surgical outcomes were not assessed. The researchers noted, however, that “although there were no associations between external distractions and our outcome measures [ASA classification], the sheer number of unnecessary external visitors to the ORs that we observed should be a cause for concern, as high personnel flow through ORs has been significantly associated with hospital acquired infections” (Clin. Infect. Dis. 1991;13:S800-4).
The takeaway from this study, according to the researchers, is that many of these distractions that have a negative impact on workload, stress, and teamwork function are preventable. “Although some distractions may be inevitable, others, particularly during tasks that require undivided attention, should be proactively limited as they can induce human error and have negative consequences on patient safety ... a clearer understanding of the interaction between the team and the OR environment is imperative if we are to truly recognize and mitigate all factors that impact upon team performance and error.”
The (U.K.) National Institute for Health Research funded the study. The authors have no disclosures.
Key clinical point: Distractions during surgical operations were negatively correlated to stress, workload, and teamwork function scores among surgeons, anesthesiologists, and nurses.
Major finding: Surgeons’ teamwork, workload, and stress scores were negatively associated with case-irrelevant, surgeon-initiated conversation in the OR.
Data source: A cross-sectional, prospective observational study of 90 general surgery cases and 85 staff members.
Disclosures: The National Institute for Health Research funded the study. The authors have no disclosures.
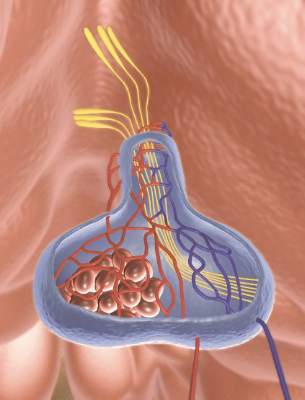
DDW: Intragastric balloon eyed for primary obesity intervention
WASHINGTON – Obese patients implanted with an intragastric balloon lost significantly more weight than those following a behavioral modification program in a randomized, nonblinded trial.
Moreover, weight loss was preserved even after device removal, study author Dr. Barham Abu Dayyeh said at the annual Digestive Disease Week.
The Orbera intragastric balloon (Apollo Endosurgery) could fill a gap in the United States between obesity lifestyle interventions that are minimally effective and a range of bariatric surgical interventions that are effective, but come at a cost of increased complications and health care costs, he said. Moreover, only 1% of qualified patients actually end up having bariatric surgery.
The silicone, saline-filled intragastric balloon (IGB) has been widely used outside the U.S. for more than 17 years in more than 200,000 patients, added Dr. Abu Dayyeh* of Mayo Clinic in Rochester, Minn.
The multicenter trial was designed for premarketing approval in the U.S. of the Orbera IGB and randomly assigned 273 adults with a body mass index (BMI) of 30-40 kg/m2 for more than 2 years to a 12-month behavioral modification program with or without endoscopic placement of the IGB filled to 500-600 cc. The balloon was removed at month 6, with regular office visits through 1 year.
Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months. The mean baseline BMI was 35 kg/m2 and 90% of patients were female.
At 6 months, the mean percent total body weight loss was greater in the IGB group than the control group (about 10% vs. 4%; P < .001), Dr. Abu Dayyeh said, noting that total body weight loss was significantly higher in the balloon group at each time point: 3, 6, 9, and 12 months.
Similarly, the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P < .001). The majority of excess weight loss achieved at 6 months was also maintained at 12 months, he said.
At 9 months (3 months after device removal), 45.6% of patients in the IGB group had an excess weight loss at least 15% higher than patients in the control group, which exceeded the 30% threshold set as a primary study outcome, he said.
The mean percent excess weight loss was 26.5% at 9 months in the balloon group, which also exceeded the 25% threshold set as a second primary outcome.
This IGB system “appears to meet the thresholds set forth by the ASGE/ASMBS PIVI for endoscopic bariatric therapies intended as a primary obesity intervention,” Dr. Abu Dayyeh said.
The American Society for Gastrointestinal Endoscopy/American Society for Metabolic and Bariatric Surgery PIVI (Preservation and Incorporation of Valuable endoscopic Innovations) recommends that endoscopic bariatric therapies intended as a primary obesity intervention achieve a mean minimum threshold of 25% excess weight loss at 12 months.
At 52 weeks, both groups had an improvement from baseline in diabetes, hypertension, and lipids, but the improvement was greater with the IGB, he said.
Beck Depression Scores and quality of life also improved in both groups, with the improvement again greater with the IGB.
Serious adverse events were reported by 7% of controls and 9.6% of the balloon group including 8 early removals for intolerance, 1 gastric outlet obstruction, 1 laryngospasm during placement, 1 case of severe abdominal cramping, and 1 case of severe dehydration.
Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. No deaths occurred in the trial.
*Changed on July 8, 2015.
On Twitter @pwendl
WASHINGTON – Obese patients implanted with an intragastric balloon lost significantly more weight than those following a behavioral modification program in a randomized, nonblinded trial.
Moreover, weight loss was preserved even after device removal, study author Dr. Barham Abu Dayyeh said at the annual Digestive Disease Week.
The Orbera intragastric balloon (Apollo Endosurgery) could fill a gap in the United States between obesity lifestyle interventions that are minimally effective and a range of bariatric surgical interventions that are effective, but come at a cost of increased complications and health care costs, he said. Moreover, only 1% of qualified patients actually end up having bariatric surgery.
The silicone, saline-filled intragastric balloon (IGB) has been widely used outside the U.S. for more than 17 years in more than 200,000 patients, added Dr. Abu Dayyeh* of Mayo Clinic in Rochester, Minn.
The multicenter trial was designed for premarketing approval in the U.S. of the Orbera IGB and randomly assigned 273 adults with a body mass index (BMI) of 30-40 kg/m2 for more than 2 years to a 12-month behavioral modification program with or without endoscopic placement of the IGB filled to 500-600 cc. The balloon was removed at month 6, with regular office visits through 1 year.
Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months. The mean baseline BMI was 35 kg/m2 and 90% of patients were female.
At 6 months, the mean percent total body weight loss was greater in the IGB group than the control group (about 10% vs. 4%; P < .001), Dr. Abu Dayyeh said, noting that total body weight loss was significantly higher in the balloon group at each time point: 3, 6, 9, and 12 months.
Similarly, the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P < .001). The majority of excess weight loss achieved at 6 months was also maintained at 12 months, he said.
At 9 months (3 months after device removal), 45.6% of patients in the IGB group had an excess weight loss at least 15% higher than patients in the control group, which exceeded the 30% threshold set as a primary study outcome, he said.
The mean percent excess weight loss was 26.5% at 9 months in the balloon group, which also exceeded the 25% threshold set as a second primary outcome.
This IGB system “appears to meet the thresholds set forth by the ASGE/ASMBS PIVI for endoscopic bariatric therapies intended as a primary obesity intervention,” Dr. Abu Dayyeh said.
The American Society for Gastrointestinal Endoscopy/American Society for Metabolic and Bariatric Surgery PIVI (Preservation and Incorporation of Valuable endoscopic Innovations) recommends that endoscopic bariatric therapies intended as a primary obesity intervention achieve a mean minimum threshold of 25% excess weight loss at 12 months.
At 52 weeks, both groups had an improvement from baseline in diabetes, hypertension, and lipids, but the improvement was greater with the IGB, he said.
Beck Depression Scores and quality of life also improved in both groups, with the improvement again greater with the IGB.
Serious adverse events were reported by 7% of controls and 9.6% of the balloon group including 8 early removals for intolerance, 1 gastric outlet obstruction, 1 laryngospasm during placement, 1 case of severe abdominal cramping, and 1 case of severe dehydration.
Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. No deaths occurred in the trial.
*Changed on July 8, 2015.
On Twitter @pwendl
WASHINGTON – Obese patients implanted with an intragastric balloon lost significantly more weight than those following a behavioral modification program in a randomized, nonblinded trial.
Moreover, weight loss was preserved even after device removal, study author Dr. Barham Abu Dayyeh said at the annual Digestive Disease Week.
The Orbera intragastric balloon (Apollo Endosurgery) could fill a gap in the United States between obesity lifestyle interventions that are minimally effective and a range of bariatric surgical interventions that are effective, but come at a cost of increased complications and health care costs, he said. Moreover, only 1% of qualified patients actually end up having bariatric surgery.
The silicone, saline-filled intragastric balloon (IGB) has been widely used outside the U.S. for more than 17 years in more than 200,000 patients, added Dr. Abu Dayyeh* of Mayo Clinic in Rochester, Minn.
The multicenter trial was designed for premarketing approval in the U.S. of the Orbera IGB and randomly assigned 273 adults with a body mass index (BMI) of 30-40 kg/m2 for more than 2 years to a 12-month behavioral modification program with or without endoscopic placement of the IGB filled to 500-600 cc. The balloon was removed at month 6, with regular office visits through 1 year.
Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months. The mean baseline BMI was 35 kg/m2 and 90% of patients were female.
At 6 months, the mean percent total body weight loss was greater in the IGB group than the control group (about 10% vs. 4%; P < .001), Dr. Abu Dayyeh said, noting that total body weight loss was significantly higher in the balloon group at each time point: 3, 6, 9, and 12 months.
Similarly, the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P < .001). The majority of excess weight loss achieved at 6 months was also maintained at 12 months, he said.
At 9 months (3 months after device removal), 45.6% of patients in the IGB group had an excess weight loss at least 15% higher than patients in the control group, which exceeded the 30% threshold set as a primary study outcome, he said.
The mean percent excess weight loss was 26.5% at 9 months in the balloon group, which also exceeded the 25% threshold set as a second primary outcome.
This IGB system “appears to meet the thresholds set forth by the ASGE/ASMBS PIVI for endoscopic bariatric therapies intended as a primary obesity intervention,” Dr. Abu Dayyeh said.
The American Society for Gastrointestinal Endoscopy/American Society for Metabolic and Bariatric Surgery PIVI (Preservation and Incorporation of Valuable endoscopic Innovations) recommends that endoscopic bariatric therapies intended as a primary obesity intervention achieve a mean minimum threshold of 25% excess weight loss at 12 months.
At 52 weeks, both groups had an improvement from baseline in diabetes, hypertension, and lipids, but the improvement was greater with the IGB, he said.
Beck Depression Scores and quality of life also improved in both groups, with the improvement again greater with the IGB.
Serious adverse events were reported by 7% of controls and 9.6% of the balloon group including 8 early removals for intolerance, 1 gastric outlet obstruction, 1 laryngospasm during placement, 1 case of severe abdominal cramping, and 1 case of severe dehydration.
Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. No deaths occurred in the trial.
*Changed on July 8, 2015.
On Twitter @pwendl
AT DDW® 2015
Key clinical point: An intragastric balloon system is an effective adjunct to lifestyle intervention for weight loss in obese patients with a BMI of 30-40 kg/m2.
Major finding: Mean percent excess weight loss at 6 months was about 40% for the intragastric balloon group vs. 13% for controls (P < .001).
Data source: Prospective, randomized, nonblinded study in 273 obese patients with a BMI of 30-40 kg/m2.
Disclosures: Apollo Endosurgery sponsored the study. Dr. Dayyeh reported financial relationships with Apollo Endosurgery, Aspire Bariatrics, and GI Dynamics.
Early combination laser treatment boosts scar healing
KISSIMMEE, FLA. – Early treatment with fractional carbon dioxide ablative laser and light-emitting diode phototherapy sped healing and improved texture, discoloration, and range of motion in hypertrophic burn scars in a controlled, blinded study of 20 patients.
“I think as long as we have intact epithelium, we’re going to have improvements if we can laser these patients as early as possible,” Dr. Jill Waibel said at the annual conference of the American Society for Laser Medicine and Surgery.
Approximately 100 million new scars occur annually in developed countries, almost a third of which result from trauma or burns, noted Dr. Waibel, a dermatologist specializing in treating burn scars at the Miami Dermatology and Laser Institute. Scarred areas begin to hypertrophy about 3-7 months after injury, when they undergo increased collagen production and slowed collagen breakdown, said Dr. Waibel. “Traditionally, reconstructive efforts have been delayed until a year after injury,” she emphasized. “But by this time, many patients have formed hypertrophic scars and have significant decreases in range of motion.”
To determine how early treatment with a combination of laser/LED therapy might interrupt hypertrophy and improve outcomes, Dr. Waibel and coinvestigator Ashley Rudnick treated 20 patients aged 21-55 years with moderate to severe burns on at least 5% of the body surface area that had occurred in the past 1-3 months. For each patient, they divided similarly scarred areas into four 5- by 5-cm squares, one of which served as an untreated control. They treated the other three areas with 120-micron spot fractional ablative carbon dioxide laser only, continuous wave LED phototherapy only, or fractional ablative laser followed by LED. They spaced the three laser sessions 2 months apart, and used eight 20-minute LED treatments per laser session. The fractional laser wavelength was 10,600 nm, energy was 80-120 mJ per pixel, and the frequency was up to 200 Hz, Dr. Waibel said. The LED wavelength was 830 nm, and energy intensity was 40-100 mW per cm2.
All treated areas improved more than the untreated control areas of scarring, but combining the modalities was associated with the fastest healing, according to blinded photographic reviews by physicians based on the visual analog Manchester scar scale, Dr. Waibel reported.
Phototherapy with LED can penetrate up to an inch of tissue and promotes selective ATP production and DNA and RNA activity, she added. “The positive effects occur only in injured cells,” she said. “LED has wound healing and anti-inflammatory effects that might benefit acutely wounded skin.”
Based on her experience, patients usually need from three to five sessions of fractional laser/LED sessions to see clear results, Dr. Waibel said in response to a question from an audience member. “We know that every time we treat a hypertrophic scar, it will get better,” she added. “When patients stop coming for treatment, you know they’re happy. If you can combine modalities softly and safely, you’ll need fewer treatments.”
Dr. Waibel disclosed financial and advisory relationships with ALMA, Cutera, DUSA, Harvest Technologies, L’Oreal/SkinCeuticals, Lumenis, Lutronics, Sebacia, Syneron-Candela, Valeant, and Zeltiq.
KISSIMMEE, FLA. – Early treatment with fractional carbon dioxide ablative laser and light-emitting diode phototherapy sped healing and improved texture, discoloration, and range of motion in hypertrophic burn scars in a controlled, blinded study of 20 patients.
“I think as long as we have intact epithelium, we’re going to have improvements if we can laser these patients as early as possible,” Dr. Jill Waibel said at the annual conference of the American Society for Laser Medicine and Surgery.
Approximately 100 million new scars occur annually in developed countries, almost a third of which result from trauma or burns, noted Dr. Waibel, a dermatologist specializing in treating burn scars at the Miami Dermatology and Laser Institute. Scarred areas begin to hypertrophy about 3-7 months after injury, when they undergo increased collagen production and slowed collagen breakdown, said Dr. Waibel. “Traditionally, reconstructive efforts have been delayed until a year after injury,” she emphasized. “But by this time, many patients have formed hypertrophic scars and have significant decreases in range of motion.”
To determine how early treatment with a combination of laser/LED therapy might interrupt hypertrophy and improve outcomes, Dr. Waibel and coinvestigator Ashley Rudnick treated 20 patients aged 21-55 years with moderate to severe burns on at least 5% of the body surface area that had occurred in the past 1-3 months. For each patient, they divided similarly scarred areas into four 5- by 5-cm squares, one of which served as an untreated control. They treated the other three areas with 120-micron spot fractional ablative carbon dioxide laser only, continuous wave LED phototherapy only, or fractional ablative laser followed by LED. They spaced the three laser sessions 2 months apart, and used eight 20-minute LED treatments per laser session. The fractional laser wavelength was 10,600 nm, energy was 80-120 mJ per pixel, and the frequency was up to 200 Hz, Dr. Waibel said. The LED wavelength was 830 nm, and energy intensity was 40-100 mW per cm2.
All treated areas improved more than the untreated control areas of scarring, but combining the modalities was associated with the fastest healing, according to blinded photographic reviews by physicians based on the visual analog Manchester scar scale, Dr. Waibel reported.
Phototherapy with LED can penetrate up to an inch of tissue and promotes selective ATP production and DNA and RNA activity, she added. “The positive effects occur only in injured cells,” she said. “LED has wound healing and anti-inflammatory effects that might benefit acutely wounded skin.”
Based on her experience, patients usually need from three to five sessions of fractional laser/LED sessions to see clear results, Dr. Waibel said in response to a question from an audience member. “We know that every time we treat a hypertrophic scar, it will get better,” she added. “When patients stop coming for treatment, you know they’re happy. If you can combine modalities softly and safely, you’ll need fewer treatments.”
Dr. Waibel disclosed financial and advisory relationships with ALMA, Cutera, DUSA, Harvest Technologies, L’Oreal/SkinCeuticals, Lumenis, Lutronics, Sebacia, Syneron-Candela, Valeant, and Zeltiq.
KISSIMMEE, FLA. – Early treatment with fractional carbon dioxide ablative laser and light-emitting diode phototherapy sped healing and improved texture, discoloration, and range of motion in hypertrophic burn scars in a controlled, blinded study of 20 patients.
“I think as long as we have intact epithelium, we’re going to have improvements if we can laser these patients as early as possible,” Dr. Jill Waibel said at the annual conference of the American Society for Laser Medicine and Surgery.
Approximately 100 million new scars occur annually in developed countries, almost a third of which result from trauma or burns, noted Dr. Waibel, a dermatologist specializing in treating burn scars at the Miami Dermatology and Laser Institute. Scarred areas begin to hypertrophy about 3-7 months after injury, when they undergo increased collagen production and slowed collagen breakdown, said Dr. Waibel. “Traditionally, reconstructive efforts have been delayed until a year after injury,” she emphasized. “But by this time, many patients have formed hypertrophic scars and have significant decreases in range of motion.”
To determine how early treatment with a combination of laser/LED therapy might interrupt hypertrophy and improve outcomes, Dr. Waibel and coinvestigator Ashley Rudnick treated 20 patients aged 21-55 years with moderate to severe burns on at least 5% of the body surface area that had occurred in the past 1-3 months. For each patient, they divided similarly scarred areas into four 5- by 5-cm squares, one of which served as an untreated control. They treated the other three areas with 120-micron spot fractional ablative carbon dioxide laser only, continuous wave LED phototherapy only, or fractional ablative laser followed by LED. They spaced the three laser sessions 2 months apart, and used eight 20-minute LED treatments per laser session. The fractional laser wavelength was 10,600 nm, energy was 80-120 mJ per pixel, and the frequency was up to 200 Hz, Dr. Waibel said. The LED wavelength was 830 nm, and energy intensity was 40-100 mW per cm2.
All treated areas improved more than the untreated control areas of scarring, but combining the modalities was associated with the fastest healing, according to blinded photographic reviews by physicians based on the visual analog Manchester scar scale, Dr. Waibel reported.
Phototherapy with LED can penetrate up to an inch of tissue and promotes selective ATP production and DNA and RNA activity, she added. “The positive effects occur only in injured cells,” she said. “LED has wound healing and anti-inflammatory effects that might benefit acutely wounded skin.”
Based on her experience, patients usually need from three to five sessions of fractional laser/LED sessions to see clear results, Dr. Waibel said in response to a question from an audience member. “We know that every time we treat a hypertrophic scar, it will get better,” she added. “When patients stop coming for treatment, you know they’re happy. If you can combine modalities softly and safely, you’ll need fewer treatments.”
Dr. Waibel disclosed financial and advisory relationships with ALMA, Cutera, DUSA, Harvest Technologies, L’Oreal/SkinCeuticals, Lumenis, Lutronics, Sebacia, Syneron-Candela, Valeant, and Zeltiq.
AT LASER 2015
Key clinical point: Fractional carbon dioxide ablative laser with light-emitting diode (LED) phototherapy sped healing and improved the appearance and function of burn scars.
Major finding: Both laser and LED alone improved scar healing, compared with untreated control scars, but combining the modalities led to the best outcomes. The fractional laser wavelength was 10,600 nm, and the LED wavelength was 830 nm.
Data source: Prospective, blinded, controlled study of 20 adults with acute moderate to severe burns.
Disclosures: Dr. Waibel disclosed financial and advisory relationships with ALMA, Cutera, DUSA, Harvest Technologies, L’Oreal/Skinceuticals, Lumenis, Lutronic, Sebacia, Syneron-Candela, Valeant, and Zeltiq.
Warfarin bridge therapy ups bleeding risk, with no reduction in VTE
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
Key clinical point: Bridge therapy for warfarin patients undergoing invasive therapy is associated with an increased risk of bleeding without a reduction in thromboembolism risk.
Major finding: Patients given bridge therapy during invasive therapy had a 17-fold increase in the risk of clinically significant bleeding.
Data source: A retrospective cohort study of 1,812 procedures in 1,178 patients.
Disclosures: The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with AstraZeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
APA: Honest talk about opioid dependence encouraged
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
AT THE APA ANNUAL MEETING
Key clinical point: Physicians are overprescribing opioids, starting many patients on the road to opioid dependence.
Major finding: In a random sample of patients receiving treatment for opioid dependence, 58% received their first opioids from a doctor’s prescription. At the time they considered themselves addicted, 45% were still being prescribed opioids.
Data source: An observational study of 50 people.
Disclosures: Dr. Chiodo reported no relevant financial disclosures.
Reconstruction, transplantation successful for gut failure after bariatric surgery
SAN DIEGO – Treating gut failure after bariatric surgery involves meeting patients’ nutritional needs while avoiding a recurrence of morbid obesity, according to Dr. Kareem Abu-Elmagd of the Cleveland Clinic.
Surgeons must be flexible, and should be familiar with a variety of reconstructive techniques to restore patients to nutritional autonomy while minimizing the need for visceral transplantation, he said.
Gut failure is a rare but serious and potentially life-threatening complication of bariatric surgery. When it occurs, the patient can no longer meet nutritional needs autonomously, but rather requires total parenteral nutrition (TPN). Although comprehensive medical management including TPN is necessary when gut failure occurs, reconstructive surgery or visceral transplantation is the only means to allow patients to regain nutritional autonomy.
Dr. Abu-Elmagd reported the results of 2 decades of experience with post–bariatric surgery gut failure at the Cleveland Clinic and the University of Pittsburgh Medical Center at the annual meeting of the American Surgical Association. He and his coinvestigators at the two facilities assessed a total of 131 patients who were referred for gut failure from 1995 to 2015. The number of referrals, said Dr. Abu-Elmagd, has been increasing sharply, with nearly two-thirds of patients referred over the past 5 years.
The study sought to identify the types and causes of gut failures seen, to describe surgical techniques used for repair or transplant, and to track outcomes for patients after surgical repair for gut failure. Of the 131 patients in the study, 100 had a Roux-en-Y or similar combined malabsorptive and restrictive surgery as their primary bariatric procedure. Overall, 85% of patients were female.
Dr. Abu-Elmagd classified gut failure into three major groups: 55 patients (42%) had type I or catastrophic gut loss, which included strangulation and vascular occlusion; 43 patients (33%) had type II gut failure, caused by technical complications such as loss of gut continuity, strictures, and fistulae; and 33 patients (25%) had type III gut failure, caused by dysfunctional syndromes such as dysmotility, restriction, or absorption.
Of the 131 patients referred, 116 went on to have a total of 317 restorative procedures. Most (n = 84, 72%) needed reversal of their primary bariatric procedure. Patients received a total of 198 autologous reconstruction procedures, while 10 intestinal-lengthening procedures and 25 visceral transplantations were performed.
Dr. Abu-Elmagd and his colleagues characterized the reconstruction procedures according to the embryonic origins of the structures repaired. Seventy-eight patients had major reconstruction of the foregut, “the most tedious and technically challenging procedure … to restore normal gut anatomy and physiology,” said Dr. Abu-Elmagd. Three other patients had gastroplasty to restore the foregut, and seven needed to have an alimentary conduit interposed in order to restore normal alimentary flow. Mid- and hindgut reconstructions (n = 110) were essential to maximize absorption and restore nutritional autonomy, he said.
If patients had less than 100 cm of small bowel remaining, they received serial transverse enteroplasty, an intestinal-lengthening procedure. The few patients who needed intestinal, liver-intestine, or multivisceral transplantations had ultrashort gut syndrome and could not be maintained on TPN.
Five-year cumulative survival for those receiving reconstruction or transplantation was 84%, and plateaued at 72% at 10 and 15 years post restoration. For the subset who received transplantation, the 5-year survival was 69%. Among the first 100 surviving surgical patients, 83% retained full nutritional autonomy.
Bariatric surgery, noted discussant Dr. Debra Sudan of Duke University, “is clearly the most effective treatment for obesity and has tremendous impact on comorbidities,” but, since it is an elective procedure, “it’s devastating when complications develop.” She asked what considerations were specific to the bariatric population when dealing with gut failure.
Bariatric patients, said Dr. Abu-Elmegd, have the advantage that they do not have an underlying disease process, and overall they have the ability to adapt and return to more normal gut function very quickly. From a surgical perspective, the solutions must be flexible and tailored to the patient. He said, “Whatever the patient has, you fix it.”
The authors reported no relevant financial disclosures.
SAN DIEGO – Treating gut failure after bariatric surgery involves meeting patients’ nutritional needs while avoiding a recurrence of morbid obesity, according to Dr. Kareem Abu-Elmagd of the Cleveland Clinic.
Surgeons must be flexible, and should be familiar with a variety of reconstructive techniques to restore patients to nutritional autonomy while minimizing the need for visceral transplantation, he said.
Gut failure is a rare but serious and potentially life-threatening complication of bariatric surgery. When it occurs, the patient can no longer meet nutritional needs autonomously, but rather requires total parenteral nutrition (TPN). Although comprehensive medical management including TPN is necessary when gut failure occurs, reconstructive surgery or visceral transplantation is the only means to allow patients to regain nutritional autonomy.
Dr. Abu-Elmagd reported the results of 2 decades of experience with post–bariatric surgery gut failure at the Cleveland Clinic and the University of Pittsburgh Medical Center at the annual meeting of the American Surgical Association. He and his coinvestigators at the two facilities assessed a total of 131 patients who were referred for gut failure from 1995 to 2015. The number of referrals, said Dr. Abu-Elmagd, has been increasing sharply, with nearly two-thirds of patients referred over the past 5 years.
The study sought to identify the types and causes of gut failures seen, to describe surgical techniques used for repair or transplant, and to track outcomes for patients after surgical repair for gut failure. Of the 131 patients in the study, 100 had a Roux-en-Y or similar combined malabsorptive and restrictive surgery as their primary bariatric procedure. Overall, 85% of patients were female.
Dr. Abu-Elmagd classified gut failure into three major groups: 55 patients (42%) had type I or catastrophic gut loss, which included strangulation and vascular occlusion; 43 patients (33%) had type II gut failure, caused by technical complications such as loss of gut continuity, strictures, and fistulae; and 33 patients (25%) had type III gut failure, caused by dysfunctional syndromes such as dysmotility, restriction, or absorption.
Of the 131 patients referred, 116 went on to have a total of 317 restorative procedures. Most (n = 84, 72%) needed reversal of their primary bariatric procedure. Patients received a total of 198 autologous reconstruction procedures, while 10 intestinal-lengthening procedures and 25 visceral transplantations were performed.
Dr. Abu-Elmagd and his colleagues characterized the reconstruction procedures according to the embryonic origins of the structures repaired. Seventy-eight patients had major reconstruction of the foregut, “the most tedious and technically challenging procedure … to restore normal gut anatomy and physiology,” said Dr. Abu-Elmagd. Three other patients had gastroplasty to restore the foregut, and seven needed to have an alimentary conduit interposed in order to restore normal alimentary flow. Mid- and hindgut reconstructions (n = 110) were essential to maximize absorption and restore nutritional autonomy, he said.
If patients had less than 100 cm of small bowel remaining, they received serial transverse enteroplasty, an intestinal-lengthening procedure. The few patients who needed intestinal, liver-intestine, or multivisceral transplantations had ultrashort gut syndrome and could not be maintained on TPN.
Five-year cumulative survival for those receiving reconstruction or transplantation was 84%, and plateaued at 72% at 10 and 15 years post restoration. For the subset who received transplantation, the 5-year survival was 69%. Among the first 100 surviving surgical patients, 83% retained full nutritional autonomy.
Bariatric surgery, noted discussant Dr. Debra Sudan of Duke University, “is clearly the most effective treatment for obesity and has tremendous impact on comorbidities,” but, since it is an elective procedure, “it’s devastating when complications develop.” She asked what considerations were specific to the bariatric population when dealing with gut failure.
Bariatric patients, said Dr. Abu-Elmegd, have the advantage that they do not have an underlying disease process, and overall they have the ability to adapt and return to more normal gut function very quickly. From a surgical perspective, the solutions must be flexible and tailored to the patient. He said, “Whatever the patient has, you fix it.”
The authors reported no relevant financial disclosures.
SAN DIEGO – Treating gut failure after bariatric surgery involves meeting patients’ nutritional needs while avoiding a recurrence of morbid obesity, according to Dr. Kareem Abu-Elmagd of the Cleveland Clinic.
Surgeons must be flexible, and should be familiar with a variety of reconstructive techniques to restore patients to nutritional autonomy while minimizing the need for visceral transplantation, he said.
Gut failure is a rare but serious and potentially life-threatening complication of bariatric surgery. When it occurs, the patient can no longer meet nutritional needs autonomously, but rather requires total parenteral nutrition (TPN). Although comprehensive medical management including TPN is necessary when gut failure occurs, reconstructive surgery or visceral transplantation is the only means to allow patients to regain nutritional autonomy.
Dr. Abu-Elmagd reported the results of 2 decades of experience with post–bariatric surgery gut failure at the Cleveland Clinic and the University of Pittsburgh Medical Center at the annual meeting of the American Surgical Association. He and his coinvestigators at the two facilities assessed a total of 131 patients who were referred for gut failure from 1995 to 2015. The number of referrals, said Dr. Abu-Elmagd, has been increasing sharply, with nearly two-thirds of patients referred over the past 5 years.
The study sought to identify the types and causes of gut failures seen, to describe surgical techniques used for repair or transplant, and to track outcomes for patients after surgical repair for gut failure. Of the 131 patients in the study, 100 had a Roux-en-Y or similar combined malabsorptive and restrictive surgery as their primary bariatric procedure. Overall, 85% of patients were female.
Dr. Abu-Elmagd classified gut failure into three major groups: 55 patients (42%) had type I or catastrophic gut loss, which included strangulation and vascular occlusion; 43 patients (33%) had type II gut failure, caused by technical complications such as loss of gut continuity, strictures, and fistulae; and 33 patients (25%) had type III gut failure, caused by dysfunctional syndromes such as dysmotility, restriction, or absorption.
Of the 131 patients referred, 116 went on to have a total of 317 restorative procedures. Most (n = 84, 72%) needed reversal of their primary bariatric procedure. Patients received a total of 198 autologous reconstruction procedures, while 10 intestinal-lengthening procedures and 25 visceral transplantations were performed.
Dr. Abu-Elmagd and his colleagues characterized the reconstruction procedures according to the embryonic origins of the structures repaired. Seventy-eight patients had major reconstruction of the foregut, “the most tedious and technically challenging procedure … to restore normal gut anatomy and physiology,” said Dr. Abu-Elmagd. Three other patients had gastroplasty to restore the foregut, and seven needed to have an alimentary conduit interposed in order to restore normal alimentary flow. Mid- and hindgut reconstructions (n = 110) were essential to maximize absorption and restore nutritional autonomy, he said.
If patients had less than 100 cm of small bowel remaining, they received serial transverse enteroplasty, an intestinal-lengthening procedure. The few patients who needed intestinal, liver-intestine, or multivisceral transplantations had ultrashort gut syndrome and could not be maintained on TPN.
Five-year cumulative survival for those receiving reconstruction or transplantation was 84%, and plateaued at 72% at 10 and 15 years post restoration. For the subset who received transplantation, the 5-year survival was 69%. Among the first 100 surviving surgical patients, 83% retained full nutritional autonomy.
Bariatric surgery, noted discussant Dr. Debra Sudan of Duke University, “is clearly the most effective treatment for obesity and has tremendous impact on comorbidities,” but, since it is an elective procedure, “it’s devastating when complications develop.” She asked what considerations were specific to the bariatric population when dealing with gut failure.
Bariatric patients, said Dr. Abu-Elmegd, have the advantage that they do not have an underlying disease process, and overall they have the ability to adapt and return to more normal gut function very quickly. From a surgical perspective, the solutions must be flexible and tailored to the patient. He said, “Whatever the patient has, you fix it.”
The authors reported no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Gut failure after bariatric surgery was successfully repaired by a variety of surgical techniques in most patients.
Major findings: Autologous reconstruction or transplantation successfully repaired gut failure in nearly 90% of a series of 116 patients.
Data source: A retrospective study of 131 patients treated for post–bariatric surgery gut failure at tertiary referral centers.
Disclosures: The authors reported no relevant financial disclosures.
Consider laser ablation therapy for treatment of benign thyroid nodules
NASHVILLE – Ultrasound-guided laser ablation therapy was found to be a clinically safe, effective, and well-tolerated option for the treatment of benign thyroid nodules, both solid and mixed, in a retrospective, multicenter study presented at the annual meeting of the American Association of Clinical Endocrinologists.
“We know that image-guided laser ablation of solid thyroid nodules has demonstrated favorable results in several prospective randomized trials,” said Dr. Enrico Papini of Regina Apostolorum Hospital in Rome. “However, these results were obtained in selected patients, with single treatments and fixed modalities of treatment; so the question is, what happens in a real. clinical practice?”
Dr. Papini explained that the aim of the study was to assess clinical efficacy and side effects of laser ablation therapy (LAT) in a large series of unselected benign thyroid nodules of variable structure and size, using data from centers who use LAT as a standard operating technique. Patients with solid or mixed nodules with up to 40% fluid composition, benign cytological findings, and normal thyroid function were included.
Clinical records of 1,534 thyroid nodules in 1,531 patients, all of whom were treated in the last 10 years, was collected from eight Italian thyroid referral centers. A total of 1,837 LAT procedures were performed on these nodules, of which 1,280 (83% of 1,534) were treated in a single session. All nodules were treated in no more than three consecutive sessions, with a fixed output power of 3 watts. According to Dr. Papini, the laser is only fired for up to 10 minutes.
Mean nodule volume significantly decreased following LAT from 27 ± 24 mL at baseline to 8 ± 8 mL at 12 months after treatment (P < .001), and mean nodule volume reduction was 72% ± 11%, with an overall range of 48%-100%. Mixed nodules experienced significantly larger decreases than solid ones. On average, mixed nodule volume decreased 79% ± 7%, versus 72% ± 11% for solid nodules (P < .001) because of fluid components being drained prior to LAT.
Symptoms decreased from 49% at baseline to 10% at 12 months post-treatment. Similarly robust reductions were also seen in cosmetic signs, which decreased 86% to 8% over 12 months. Only 17 patients experienced a complication, including 8 with a “major” complication of dysphonia, which resolved within 2-84 days, and 9 with “minor” complications, such as skin burn and hematoma.
“Laser ablation was performed in outpatient setting, with no hospital admission after treatment,” said Dr. Papini. “It was well-tolerated, and severe pain – requiring more than 3 days of analgesics – occurred in less than 2% of patients.”
Dr. Papini did not report any relevant financial disclosures.
NASHVILLE – Ultrasound-guided laser ablation therapy was found to be a clinically safe, effective, and well-tolerated option for the treatment of benign thyroid nodules, both solid and mixed, in a retrospective, multicenter study presented at the annual meeting of the American Association of Clinical Endocrinologists.
“We know that image-guided laser ablation of solid thyroid nodules has demonstrated favorable results in several prospective randomized trials,” said Dr. Enrico Papini of Regina Apostolorum Hospital in Rome. “However, these results were obtained in selected patients, with single treatments and fixed modalities of treatment; so the question is, what happens in a real. clinical practice?”
Dr. Papini explained that the aim of the study was to assess clinical efficacy and side effects of laser ablation therapy (LAT) in a large series of unselected benign thyroid nodules of variable structure and size, using data from centers who use LAT as a standard operating technique. Patients with solid or mixed nodules with up to 40% fluid composition, benign cytological findings, and normal thyroid function were included.
Clinical records of 1,534 thyroid nodules in 1,531 patients, all of whom were treated in the last 10 years, was collected from eight Italian thyroid referral centers. A total of 1,837 LAT procedures were performed on these nodules, of which 1,280 (83% of 1,534) were treated in a single session. All nodules were treated in no more than three consecutive sessions, with a fixed output power of 3 watts. According to Dr. Papini, the laser is only fired for up to 10 minutes.
Mean nodule volume significantly decreased following LAT from 27 ± 24 mL at baseline to 8 ± 8 mL at 12 months after treatment (P < .001), and mean nodule volume reduction was 72% ± 11%, with an overall range of 48%-100%. Mixed nodules experienced significantly larger decreases than solid ones. On average, mixed nodule volume decreased 79% ± 7%, versus 72% ± 11% for solid nodules (P < .001) because of fluid components being drained prior to LAT.
Symptoms decreased from 49% at baseline to 10% at 12 months post-treatment. Similarly robust reductions were also seen in cosmetic signs, which decreased 86% to 8% over 12 months. Only 17 patients experienced a complication, including 8 with a “major” complication of dysphonia, which resolved within 2-84 days, and 9 with “minor” complications, such as skin burn and hematoma.
“Laser ablation was performed in outpatient setting, with no hospital admission after treatment,” said Dr. Papini. “It was well-tolerated, and severe pain – requiring more than 3 days of analgesics – occurred in less than 2% of patients.”
Dr. Papini did not report any relevant financial disclosures.
NASHVILLE – Ultrasound-guided laser ablation therapy was found to be a clinically safe, effective, and well-tolerated option for the treatment of benign thyroid nodules, both solid and mixed, in a retrospective, multicenter study presented at the annual meeting of the American Association of Clinical Endocrinologists.
“We know that image-guided laser ablation of solid thyroid nodules has demonstrated favorable results in several prospective randomized trials,” said Dr. Enrico Papini of Regina Apostolorum Hospital in Rome. “However, these results were obtained in selected patients, with single treatments and fixed modalities of treatment; so the question is, what happens in a real. clinical practice?”
Dr. Papini explained that the aim of the study was to assess clinical efficacy and side effects of laser ablation therapy (LAT) in a large series of unselected benign thyroid nodules of variable structure and size, using data from centers who use LAT as a standard operating technique. Patients with solid or mixed nodules with up to 40% fluid composition, benign cytological findings, and normal thyroid function were included.
Clinical records of 1,534 thyroid nodules in 1,531 patients, all of whom were treated in the last 10 years, was collected from eight Italian thyroid referral centers. A total of 1,837 LAT procedures were performed on these nodules, of which 1,280 (83% of 1,534) were treated in a single session. All nodules were treated in no more than three consecutive sessions, with a fixed output power of 3 watts. According to Dr. Papini, the laser is only fired for up to 10 minutes.
Mean nodule volume significantly decreased following LAT from 27 ± 24 mL at baseline to 8 ± 8 mL at 12 months after treatment (P < .001), and mean nodule volume reduction was 72% ± 11%, with an overall range of 48%-100%. Mixed nodules experienced significantly larger decreases than solid ones. On average, mixed nodule volume decreased 79% ± 7%, versus 72% ± 11% for solid nodules (P < .001) because of fluid components being drained prior to LAT.
Symptoms decreased from 49% at baseline to 10% at 12 months post-treatment. Similarly robust reductions were also seen in cosmetic signs, which decreased 86% to 8% over 12 months. Only 17 patients experienced a complication, including 8 with a “major” complication of dysphonia, which resolved within 2-84 days, and 9 with “minor” complications, such as skin burn and hematoma.
“Laser ablation was performed in outpatient setting, with no hospital admission after treatment,” said Dr. Papini. “It was well-tolerated, and severe pain – requiring more than 3 days of analgesics – occurred in less than 2% of patients.”
Dr. Papini did not report any relevant financial disclosures.
AT AACE 2015
Key clinical point: Ultrasound-guided laser ablation therapy is a clinically effective and well-tolerated tool for treating benign solid and mixed thyroid nodules.
Major finding: In 1,837 treatments for 1,534 nodules, mean nodule volume decreased from 27 ± 24 mL at baseline to 8 ± 8 mL at 12 months after treatment (P < .001), and mean nodule volume reduction was 72% ± 11% (range 48%-100%).
Data source: Retrospective, multicenter study of 1,534 benign solid and mixed thyroid nodules.
Disclosures: Dr. Papini did not report any relevant financial disclosures.
Copeptin levels predicted diabetes insipidus after pituitary surgery
Copeptin levels of less than 2.5 pmol/L reliably identified diabetes insipidus after pituitary surgery, while levels of more than 30 pmol/L ruled out the condition, investigators reported online in the Journal of Clinical Endocrinology and Metabolism.
“Copeptin represents a new, early, and reliable single marker for postoperative diabetes insipidus in the post–pituitary surgery setting, where no such marker currently is known,” said Dr. Bettina Winzeler at University Hospital of Basel (Switzerland) and her associates. Postoperative measures of copeptin levels might help clinicians to differentiate patients who need closer postsurgical inpatient observation from those who can safely be discharged.
About 16%-34% of patients who undergo surgery in the sellar region develop central diabetes insipidus, which, without prompt rehydration, can cause severe hypernatremia, Dr. Winzeler and her associates noted. Risk factors for postoperative diabetes insipidus are not useful markers; however, copeptin, a surrogate of arginine vasopressin, is stable and can be measured quickly and reliably.
The researchers hypothesized that patients with postoperative diabetes insipidus would not have the markedly elevated copeptin levels that surgical stress normally triggers when posterior pituitary function is adequate. To test that theory, they measured daily postoperative copeptin levels for 205 consecutive patients who underwent surgeries for sellar lesions or tumors near the hypothalamus or pituitary gland (J. Clin. Endocrinol. Metab. 2015 Apr. 29 [doi:10.1210/jc.2014-4527]).
One day after surgery, 22 (81.5%) of the 27 patients whose copeptin levels were less than 2.5 pmol/L had diabetes insipidus (positive predictive value, 81%; specificity, 97%), said the researchers. In contrast, one of 40 (2.5%) patients with copeptin levels greater than 30 pmol/L had diabetes insipidus (negative predictive value 95%; sensitivity, 94%). Patients with diabetes insipidus also had significantly lower median and interquartile (25th-75th percentile) copeptin levels, compared with other patients (median for patients with diabetes insipidus, 2.9 pmol/L; interquartile range, 1.9-7.9 pmol/L; median for other patients, 10.8 pmol/L; IQR, 5.2-30.4 pmol/L; P less than .001). In the multivariate analysis, low postoperative copeptin levels remained associated with diabetes insipidus after adjusting for age, gender, body-mass index, tumor size and type of surgery, history of surgery or radiotherapy, cerebrospinal fluid leakage, and serum sodium concentration, the investigators reported (odds ratio, 1.62; 95% confidence interval, 1.25-2.10; P less than .001).
The study did not use standardized diagnostic criteria for diabetes insipidus, and postoperative blood samples were obtained as part of daily care and not at fixed time points, Dr. Winzeler and her associates noted. “Absence of standardized sampling for copeptin measurement at a defined early time point presumably decreased copeptin accuracy in this study, rendering our findings conservative,” they cautioned.
The Swiss National Foundation partially funded the research. Three coauthors reported having received speaker honoraria from Thermo Scientific Biomarkers, which develops and makes the copeptin assay.
Copeptin levels of less than 2.5 pmol/L reliably identified diabetes insipidus after pituitary surgery, while levels of more than 30 pmol/L ruled out the condition, investigators reported online in the Journal of Clinical Endocrinology and Metabolism.
“Copeptin represents a new, early, and reliable single marker for postoperative diabetes insipidus in the post–pituitary surgery setting, where no such marker currently is known,” said Dr. Bettina Winzeler at University Hospital of Basel (Switzerland) and her associates. Postoperative measures of copeptin levels might help clinicians to differentiate patients who need closer postsurgical inpatient observation from those who can safely be discharged.
About 16%-34% of patients who undergo surgery in the sellar region develop central diabetes insipidus, which, without prompt rehydration, can cause severe hypernatremia, Dr. Winzeler and her associates noted. Risk factors for postoperative diabetes insipidus are not useful markers; however, copeptin, a surrogate of arginine vasopressin, is stable and can be measured quickly and reliably.
The researchers hypothesized that patients with postoperative diabetes insipidus would not have the markedly elevated copeptin levels that surgical stress normally triggers when posterior pituitary function is adequate. To test that theory, they measured daily postoperative copeptin levels for 205 consecutive patients who underwent surgeries for sellar lesions or tumors near the hypothalamus or pituitary gland (J. Clin. Endocrinol. Metab. 2015 Apr. 29 [doi:10.1210/jc.2014-4527]).
One day after surgery, 22 (81.5%) of the 27 patients whose copeptin levels were less than 2.5 pmol/L had diabetes insipidus (positive predictive value, 81%; specificity, 97%), said the researchers. In contrast, one of 40 (2.5%) patients with copeptin levels greater than 30 pmol/L had diabetes insipidus (negative predictive value 95%; sensitivity, 94%). Patients with diabetes insipidus also had significantly lower median and interquartile (25th-75th percentile) copeptin levels, compared with other patients (median for patients with diabetes insipidus, 2.9 pmol/L; interquartile range, 1.9-7.9 pmol/L; median for other patients, 10.8 pmol/L; IQR, 5.2-30.4 pmol/L; P less than .001). In the multivariate analysis, low postoperative copeptin levels remained associated with diabetes insipidus after adjusting for age, gender, body-mass index, tumor size and type of surgery, history of surgery or radiotherapy, cerebrospinal fluid leakage, and serum sodium concentration, the investigators reported (odds ratio, 1.62; 95% confidence interval, 1.25-2.10; P less than .001).
The study did not use standardized diagnostic criteria for diabetes insipidus, and postoperative blood samples were obtained as part of daily care and not at fixed time points, Dr. Winzeler and her associates noted. “Absence of standardized sampling for copeptin measurement at a defined early time point presumably decreased copeptin accuracy in this study, rendering our findings conservative,” they cautioned.
The Swiss National Foundation partially funded the research. Three coauthors reported having received speaker honoraria from Thermo Scientific Biomarkers, which develops and makes the copeptin assay.
Copeptin levels of less than 2.5 pmol/L reliably identified diabetes insipidus after pituitary surgery, while levels of more than 30 pmol/L ruled out the condition, investigators reported online in the Journal of Clinical Endocrinology and Metabolism.
“Copeptin represents a new, early, and reliable single marker for postoperative diabetes insipidus in the post–pituitary surgery setting, where no such marker currently is known,” said Dr. Bettina Winzeler at University Hospital of Basel (Switzerland) and her associates. Postoperative measures of copeptin levels might help clinicians to differentiate patients who need closer postsurgical inpatient observation from those who can safely be discharged.
About 16%-34% of patients who undergo surgery in the sellar region develop central diabetes insipidus, which, without prompt rehydration, can cause severe hypernatremia, Dr. Winzeler and her associates noted. Risk factors for postoperative diabetes insipidus are not useful markers; however, copeptin, a surrogate of arginine vasopressin, is stable and can be measured quickly and reliably.
The researchers hypothesized that patients with postoperative diabetes insipidus would not have the markedly elevated copeptin levels that surgical stress normally triggers when posterior pituitary function is adequate. To test that theory, they measured daily postoperative copeptin levels for 205 consecutive patients who underwent surgeries for sellar lesions or tumors near the hypothalamus or pituitary gland (J. Clin. Endocrinol. Metab. 2015 Apr. 29 [doi:10.1210/jc.2014-4527]).
One day after surgery, 22 (81.5%) of the 27 patients whose copeptin levels were less than 2.5 pmol/L had diabetes insipidus (positive predictive value, 81%; specificity, 97%), said the researchers. In contrast, one of 40 (2.5%) patients with copeptin levels greater than 30 pmol/L had diabetes insipidus (negative predictive value 95%; sensitivity, 94%). Patients with diabetes insipidus also had significantly lower median and interquartile (25th-75th percentile) copeptin levels, compared with other patients (median for patients with diabetes insipidus, 2.9 pmol/L; interquartile range, 1.9-7.9 pmol/L; median for other patients, 10.8 pmol/L; IQR, 5.2-30.4 pmol/L; P less than .001). In the multivariate analysis, low postoperative copeptin levels remained associated with diabetes insipidus after adjusting for age, gender, body-mass index, tumor size and type of surgery, history of surgery or radiotherapy, cerebrospinal fluid leakage, and serum sodium concentration, the investigators reported (odds ratio, 1.62; 95% confidence interval, 1.25-2.10; P less than .001).
The study did not use standardized diagnostic criteria for diabetes insipidus, and postoperative blood samples were obtained as part of daily care and not at fixed time points, Dr. Winzeler and her associates noted. “Absence of standardized sampling for copeptin measurement at a defined early time point presumably decreased copeptin accuracy in this study, rendering our findings conservative,” they cautioned.
The Swiss National Foundation partially funded the research. Three coauthors reported having received speaker honoraria from Thermo Scientific Biomarkers, which develops and makes the copeptin assay.
Key clinical point: Low copeptin levels reliably predicted diabetes insipidus after pituitary surgery.
Major finding: A day after surgery, 81.5% of patients with copeptin levels less than 2.5 pmol/L had diabetes insipidus, compared with 2.5% of patients with levels greater than 30 pmol/L.
Data source: Multicenter, prospective, observational cohort study of 205 consecutive pituitary surgery patients.
Disclosures: The Swiss National Foundation partially funded the research. Three coauthors reported having received speaker honoraria from Thermo Scientific Biomarkers, which develops and makes the copeptin assay.