User login
Weekend surgery safer with more nurses, EMR use
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Surgeon-independent factors impacted patient outcomes for urgent surgical procedures.
Major finding: Facilities with an electronic medical record, higher nurse-to-bed ratios, and strong ancillary services were significantly less likely to exhibit the weekend effect for urgent surgical procedures, as measured by patient length of stay.
Data source: Healthcare Cost and Utilization Project State Inpatient Dataset and American Hospital Association Annual Survey database for the state of Florida for 2007-2011.
Disclosures: The authors reported no disclosures.
General surgeons have high confidence after training
SAN DIEGO – Graduates of U.S. surgical residency training are generally very satisfied with their postgraduate choices, whether they opt for fellowships or not.
However, the 20% who opt to practice as general surgeons rather than pursuing subspecialty and fellowship training are more confident of their skills as they emerge from residency. “Specialty training does not result in greater confidence,” said Dr. Mary Klingensmith, professor of surgery and vice chair for education at Washington University, St. Louis. She discussed these results and other insights drawn from a nationwide survey of surgical residency graduates at the annual meeting of the American Surgical Association.
Dr. Klingensmith noted that there is a growing deficit of general surgeons, with a 25% decline in practicing general surgeons over the last 2 decades and an additional 18% decline projected over the next 20 years. A need existed, she said, for a systematic survey of recent graduates to identify the factors that play into the decision to pursue postgraduate training rather than enter directly into practice as a general surgeon.
A survey developed by American Board of Surgery (ABS) directors and executive staff was sent to all allopathic general surgery (GS) graduates from 2009 to 2013. Of 5,512 graduates, 3,354 (61%) responded. About three-quarters of respondents were specialist surgeons (SS).
The analysis of survey results conducted by Dr. Klingensmith and her colleagues compared the general to the specialist surgeons’ responses, and linked the surveys to the ABS database, which provided demographic characteristics that included residency program type, performance on board exams, and the postgraduate fellowship pursued, if any.
Surgeons were surveyed about their level of confidence in the independent practice of 16 common general procedures, including such “bread and butter” procedures as laparoscopic appendectomy and cholecystectomy, herniorrhaphy, and screening colonoscopies. Respondents were also asked to indicate how confident they were performing less common procedures, including tracheostomies, arterioveneous (AV) fistulas for dialysis, laparoscopic Nissen fundoplications, thyroidectomies, and laparoscopic colon resections.
Responses on a five-point Likert scale were sorted by type of subspecialty training, if any. After the most confident group – pediatric surgeons – general surgeons were significantly more likely to feel confident in their surgical skills than were the other specialist surgeons (P < .0001). Essentially all general surgery respondents were “very” or “mostly” confident of their ability to perform such common procedures as laparoscopic appendectomies and cholecystectomies, as well as ventral herniorrhaphies. Confidence decreased for specialists and nonspecialists alike for the more complex and less common surgeries. Overall, 94% of general surgeons and 90% of specialist surgeons were very or mostly confident of their abilities.
For general surgeons, factors influencing their choices included the opportunity for a broad scope of practice (63%), the influence of a mentor (56%), readiness to be done with training (26%), and being confident with the amount of training received (26%). For the specialists, the most influential factors included high degree of interest in the chosen specialty (57%), interest in improving specific skills (35%), and the opportunity to increase confidence and experience (35%). Both groups felt they’d made the right decision overall: 94% of general surgery graduates and 90% of those pursuing fellowships were very or somewhat satisfied with their career choices.
Study limitations included the risk of nonresponder bias, and the fact that only the most common procedures were included in the survey. Also, no outcome data were available to validate self-perceptions of competence, said Dr. Klingensmith.
The survey and its analysis “have implications that are enormous for the workforce needs of the country, and it’s clear that lack of confidence is an issue for a small but likely significant number of trainees,” said discussant Dr. J. David Richardson of the University of Louisville (Ky.). Greater opportunities for general surgery rotations, as well as stronger general surgery mentorship during residency, may help increase the number of general surgeons entering practice in the future, said Dr. Klingensmith.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Graduates of U.S. surgical residency training are generally very satisfied with their postgraduate choices, whether they opt for fellowships or not.
However, the 20% who opt to practice as general surgeons rather than pursuing subspecialty and fellowship training are more confident of their skills as they emerge from residency. “Specialty training does not result in greater confidence,” said Dr. Mary Klingensmith, professor of surgery and vice chair for education at Washington University, St. Louis. She discussed these results and other insights drawn from a nationwide survey of surgical residency graduates at the annual meeting of the American Surgical Association.
Dr. Klingensmith noted that there is a growing deficit of general surgeons, with a 25% decline in practicing general surgeons over the last 2 decades and an additional 18% decline projected over the next 20 years. A need existed, she said, for a systematic survey of recent graduates to identify the factors that play into the decision to pursue postgraduate training rather than enter directly into practice as a general surgeon.
A survey developed by American Board of Surgery (ABS) directors and executive staff was sent to all allopathic general surgery (GS) graduates from 2009 to 2013. Of 5,512 graduates, 3,354 (61%) responded. About three-quarters of respondents were specialist surgeons (SS).
The analysis of survey results conducted by Dr. Klingensmith and her colleagues compared the general to the specialist surgeons’ responses, and linked the surveys to the ABS database, which provided demographic characteristics that included residency program type, performance on board exams, and the postgraduate fellowship pursued, if any.
Surgeons were surveyed about their level of confidence in the independent practice of 16 common general procedures, including such “bread and butter” procedures as laparoscopic appendectomy and cholecystectomy, herniorrhaphy, and screening colonoscopies. Respondents were also asked to indicate how confident they were performing less common procedures, including tracheostomies, arterioveneous (AV) fistulas for dialysis, laparoscopic Nissen fundoplications, thyroidectomies, and laparoscopic colon resections.
Responses on a five-point Likert scale were sorted by type of subspecialty training, if any. After the most confident group – pediatric surgeons – general surgeons were significantly more likely to feel confident in their surgical skills than were the other specialist surgeons (P < .0001). Essentially all general surgery respondents were “very” or “mostly” confident of their ability to perform such common procedures as laparoscopic appendectomies and cholecystectomies, as well as ventral herniorrhaphies. Confidence decreased for specialists and nonspecialists alike for the more complex and less common surgeries. Overall, 94% of general surgeons and 90% of specialist surgeons were very or mostly confident of their abilities.
For general surgeons, factors influencing their choices included the opportunity for a broad scope of practice (63%), the influence of a mentor (56%), readiness to be done with training (26%), and being confident with the amount of training received (26%). For the specialists, the most influential factors included high degree of interest in the chosen specialty (57%), interest in improving specific skills (35%), and the opportunity to increase confidence and experience (35%). Both groups felt they’d made the right decision overall: 94% of general surgery graduates and 90% of those pursuing fellowships were very or somewhat satisfied with their career choices.
Study limitations included the risk of nonresponder bias, and the fact that only the most common procedures were included in the survey. Also, no outcome data were available to validate self-perceptions of competence, said Dr. Klingensmith.
The survey and its analysis “have implications that are enormous for the workforce needs of the country, and it’s clear that lack of confidence is an issue for a small but likely significant number of trainees,” said discussant Dr. J. David Richardson of the University of Louisville (Ky.). Greater opportunities for general surgery rotations, as well as stronger general surgery mentorship during residency, may help increase the number of general surgeons entering practice in the future, said Dr. Klingensmith.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Graduates of U.S. surgical residency training are generally very satisfied with their postgraduate choices, whether they opt for fellowships or not.
However, the 20% who opt to practice as general surgeons rather than pursuing subspecialty and fellowship training are more confident of their skills as they emerge from residency. “Specialty training does not result in greater confidence,” said Dr. Mary Klingensmith, professor of surgery and vice chair for education at Washington University, St. Louis. She discussed these results and other insights drawn from a nationwide survey of surgical residency graduates at the annual meeting of the American Surgical Association.
Dr. Klingensmith noted that there is a growing deficit of general surgeons, with a 25% decline in practicing general surgeons over the last 2 decades and an additional 18% decline projected over the next 20 years. A need existed, she said, for a systematic survey of recent graduates to identify the factors that play into the decision to pursue postgraduate training rather than enter directly into practice as a general surgeon.
A survey developed by American Board of Surgery (ABS) directors and executive staff was sent to all allopathic general surgery (GS) graduates from 2009 to 2013. Of 5,512 graduates, 3,354 (61%) responded. About three-quarters of respondents were specialist surgeons (SS).
The analysis of survey results conducted by Dr. Klingensmith and her colleagues compared the general to the specialist surgeons’ responses, and linked the surveys to the ABS database, which provided demographic characteristics that included residency program type, performance on board exams, and the postgraduate fellowship pursued, if any.
Surgeons were surveyed about their level of confidence in the independent practice of 16 common general procedures, including such “bread and butter” procedures as laparoscopic appendectomy and cholecystectomy, herniorrhaphy, and screening colonoscopies. Respondents were also asked to indicate how confident they were performing less common procedures, including tracheostomies, arterioveneous (AV) fistulas for dialysis, laparoscopic Nissen fundoplications, thyroidectomies, and laparoscopic colon resections.
Responses on a five-point Likert scale were sorted by type of subspecialty training, if any. After the most confident group – pediatric surgeons – general surgeons were significantly more likely to feel confident in their surgical skills than were the other specialist surgeons (P < .0001). Essentially all general surgery respondents were “very” or “mostly” confident of their ability to perform such common procedures as laparoscopic appendectomies and cholecystectomies, as well as ventral herniorrhaphies. Confidence decreased for specialists and nonspecialists alike for the more complex and less common surgeries. Overall, 94% of general surgeons and 90% of specialist surgeons were very or mostly confident of their abilities.
For general surgeons, factors influencing their choices included the opportunity for a broad scope of practice (63%), the influence of a mentor (56%), readiness to be done with training (26%), and being confident with the amount of training received (26%). For the specialists, the most influential factors included high degree of interest in the chosen specialty (57%), interest in improving specific skills (35%), and the opportunity to increase confidence and experience (35%). Both groups felt they’d made the right decision overall: 94% of general surgery graduates and 90% of those pursuing fellowships were very or somewhat satisfied with their career choices.
Study limitations included the risk of nonresponder bias, and the fact that only the most common procedures were included in the survey. Also, no outcome data were available to validate self-perceptions of competence, said Dr. Klingensmith.
The survey and its analysis “have implications that are enormous for the workforce needs of the country, and it’s clear that lack of confidence is an issue for a small but likely significant number of trainees,” said discussant Dr. J. David Richardson of the University of Louisville (Ky.). Greater opportunities for general surgery rotations, as well as stronger general surgery mentorship during residency, may help increase the number of general surgeons entering practice in the future, said Dr. Klingensmith.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA Annual Meeting
Key clinical point: U.S. surgical residency graduates who opt for general surgery are generally more confident than are those choosing fellowships; both groups are satisfied with their choices.
Major findings: General surgery graduates were more confident than were those who chose fellowships, but 94% of general surgery graduates and 90% of those pursuing fellowships were satisfied with their career choices.
Data source: American Board of Surgery survey of all U.S. allopathic surgery residency graduates from 2009 to 2013 to ascertain levels of confidence, perceptions of autonomy, and reasons for opting in or out of postgraduate fellowship training.
Disclosures: The authors reported no conflicts of interest. The ABS provided data to study authors, but the presentation does not necessarily reflect the opinions or policies of the ABS.
Spray-dried fibrin sealant for surgical use approved by FDA
A product that contains a spray-dried, blended formulation of fibrinogen and thrombin, derived from human plasma, has been approved for use in helping control surgical bleeding, the Food and Drug Administration announced.
The approved indication for the fibrin sealant is for use with an absorbable gelatin sponge; it is the first spray-dried fibrin sealant approved by the FDA, according to its statement. The product, which will be marketed as Raplixa, can be applied from the product vial or sprayed onto the site of bleeding with a spray device.
“This approval provides surgeons an additional option to help control bleeding during surgery when needed,” Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA’s statement. “The spray-drying process used to manufacture Raplixa produces dried powders that can be combined into a single vial. This eliminates the need to combine the fibrinogen and thrombin before use and allows the product to be stored at room temperature,” she added.
Approval was based on a study of 719 people undergoing different types of surgical procedures, which showed that use of the fibrin sealant with an absorbable gelatin sponge reduced the time required to achieve hemostasis, compared with the use of a sponge alone. The manufacturing process includes viral inactivation and removal to reduce the risk of transmitting of blood-borne viruses, the FDA statement said.
The approved indication is “to provide adjunctive hemostasis for mild to moderate bleeding in adults undergoing surgery when control of bleeding by standard surgical techniques (such as suture, ligature and cautery) is ineffective or impractical,” according to an April 30 statement issued by the Medicines Company. The statement said that the product does not need to be thawed, reconstituted or mixed before use, and it describes the spray device as “a low-pressure spray applicator designed to deliver Raplixa to larger bleeding surfaces in difficult to reach areas.”
The product is manufactured by ProFibrix BV, a subsidiary of the Medicines Company.
A product that contains a spray-dried, blended formulation of fibrinogen and thrombin, derived from human plasma, has been approved for use in helping control surgical bleeding, the Food and Drug Administration announced.
The approved indication for the fibrin sealant is for use with an absorbable gelatin sponge; it is the first spray-dried fibrin sealant approved by the FDA, according to its statement. The product, which will be marketed as Raplixa, can be applied from the product vial or sprayed onto the site of bleeding with a spray device.
“This approval provides surgeons an additional option to help control bleeding during surgery when needed,” Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA’s statement. “The spray-drying process used to manufacture Raplixa produces dried powders that can be combined into a single vial. This eliminates the need to combine the fibrinogen and thrombin before use and allows the product to be stored at room temperature,” she added.
Approval was based on a study of 719 people undergoing different types of surgical procedures, which showed that use of the fibrin sealant with an absorbable gelatin sponge reduced the time required to achieve hemostasis, compared with the use of a sponge alone. The manufacturing process includes viral inactivation and removal to reduce the risk of transmitting of blood-borne viruses, the FDA statement said.
The approved indication is “to provide adjunctive hemostasis for mild to moderate bleeding in adults undergoing surgery when control of bleeding by standard surgical techniques (such as suture, ligature and cautery) is ineffective or impractical,” according to an April 30 statement issued by the Medicines Company. The statement said that the product does not need to be thawed, reconstituted or mixed before use, and it describes the spray device as “a low-pressure spray applicator designed to deliver Raplixa to larger bleeding surfaces in difficult to reach areas.”
The product is manufactured by ProFibrix BV, a subsidiary of the Medicines Company.
A product that contains a spray-dried, blended formulation of fibrinogen and thrombin, derived from human plasma, has been approved for use in helping control surgical bleeding, the Food and Drug Administration announced.
The approved indication for the fibrin sealant is for use with an absorbable gelatin sponge; it is the first spray-dried fibrin sealant approved by the FDA, according to its statement. The product, which will be marketed as Raplixa, can be applied from the product vial or sprayed onto the site of bleeding with a spray device.
“This approval provides surgeons an additional option to help control bleeding during surgery when needed,” Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA’s statement. “The spray-drying process used to manufacture Raplixa produces dried powders that can be combined into a single vial. This eliminates the need to combine the fibrinogen and thrombin before use and allows the product to be stored at room temperature,” she added.
Approval was based on a study of 719 people undergoing different types of surgical procedures, which showed that use of the fibrin sealant with an absorbable gelatin sponge reduced the time required to achieve hemostasis, compared with the use of a sponge alone. The manufacturing process includes viral inactivation and removal to reduce the risk of transmitting of blood-borne viruses, the FDA statement said.
The approved indication is “to provide adjunctive hemostasis for mild to moderate bleeding in adults undergoing surgery when control of bleeding by standard surgical techniques (such as suture, ligature and cautery) is ineffective or impractical,” according to an April 30 statement issued by the Medicines Company. The statement said that the product does not need to be thawed, reconstituted or mixed before use, and it describes the spray device as “a low-pressure spray applicator designed to deliver Raplixa to larger bleeding surfaces in difficult to reach areas.”
The product is manufactured by ProFibrix BV, a subsidiary of the Medicines Company.
FDA requests more data on antiseptics used in health care settings
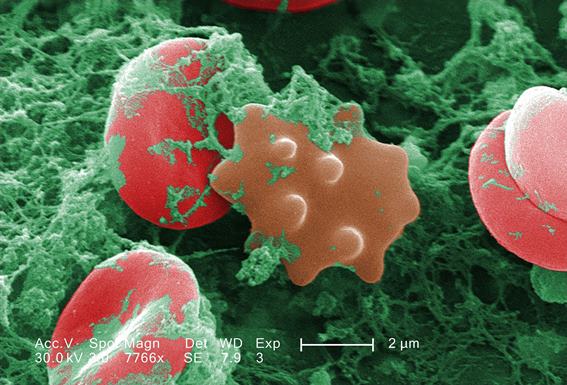
The Food and Drug Administration is requesting more scientific data on the safety and effectiveness of the active ingredients in antiseptic products used in hospitals, physician’s offices, and other health care settings in a proposed rule issued April 30.
“Today’s proposal seeks to ensure the FDA’s evaluations and determinations for all health care antiseptic active ingredients are consistent, up-to-date and appropriately reflect current scientific knowledge and patterns of use by health care professionals,” Dr. Theresa Michele, director of the division of nonprescription drug products in the FDA’s Center for Drug Evaluation and Research, said in a statement. The proposed rule “should not be taken to mean” that the agency believes these products are not effective or safe, according to the statement.
Alcohol and iodine are among the most common active ingredients in these products, which include hand washes and rubs, surgical hand scrubs and rubs, and preoperative skin preparations used on patients. These products are marketed under an over-the-counter drug monograph and are different than antibacterial soaps, hand sanitizers, and other consumer antiseptic products, which are not included in this proposed rule. To continue to market these products under the monograph, manufacturers must provide the FDA with more data on the safety and effectiveness of the active ingredients, including absorption, hormonal effects, and bacterial resistance, the statement said.
“Emerging science” suggests that, for at least some active ingredients used in these products, “systemic exposure … is higher than previously thought, and existing data raise potential concerns about the effects of repeated daily human exposure to some antiseptic active ingredients,” the statement said. The agency “is particularly interested in gathering additional data on the long-term safety of daily, repeated exposure to these ingredients in the health care setting and on the use of these products by certain populations, including pregnant and breastfeeding health care workers, for which topical absorption of the active ingredients may be important.”
The proposed rule is available at www.federalregister.gov. Public comments can be submitted until Oct. 27.
The Food and Drug Administration is requesting more scientific data on the safety and effectiveness of the active ingredients in antiseptic products used in hospitals, physician’s offices, and other health care settings in a proposed rule issued April 30.
“Today’s proposal seeks to ensure the FDA’s evaluations and determinations for all health care antiseptic active ingredients are consistent, up-to-date and appropriately reflect current scientific knowledge and patterns of use by health care professionals,” Dr. Theresa Michele, director of the division of nonprescription drug products in the FDA’s Center for Drug Evaluation and Research, said in a statement. The proposed rule “should not be taken to mean” that the agency believes these products are not effective or safe, according to the statement.
Alcohol and iodine are among the most common active ingredients in these products, which include hand washes and rubs, surgical hand scrubs and rubs, and preoperative skin preparations used on patients. These products are marketed under an over-the-counter drug monograph and are different than antibacterial soaps, hand sanitizers, and other consumer antiseptic products, which are not included in this proposed rule. To continue to market these products under the monograph, manufacturers must provide the FDA with more data on the safety and effectiveness of the active ingredients, including absorption, hormonal effects, and bacterial resistance, the statement said.
“Emerging science” suggests that, for at least some active ingredients used in these products, “systemic exposure … is higher than previously thought, and existing data raise potential concerns about the effects of repeated daily human exposure to some antiseptic active ingredients,” the statement said. The agency “is particularly interested in gathering additional data on the long-term safety of daily, repeated exposure to these ingredients in the health care setting and on the use of these products by certain populations, including pregnant and breastfeeding health care workers, for which topical absorption of the active ingredients may be important.”
The proposed rule is available at www.federalregister.gov. Public comments can be submitted until Oct. 27.
The Food and Drug Administration is requesting more scientific data on the safety and effectiveness of the active ingredients in antiseptic products used in hospitals, physician’s offices, and other health care settings in a proposed rule issued April 30.
“Today’s proposal seeks to ensure the FDA’s evaluations and determinations for all health care antiseptic active ingredients are consistent, up-to-date and appropriately reflect current scientific knowledge and patterns of use by health care professionals,” Dr. Theresa Michele, director of the division of nonprescription drug products in the FDA’s Center for Drug Evaluation and Research, said in a statement. The proposed rule “should not be taken to mean” that the agency believes these products are not effective or safe, according to the statement.
Alcohol and iodine are among the most common active ingredients in these products, which include hand washes and rubs, surgical hand scrubs and rubs, and preoperative skin preparations used on patients. These products are marketed under an over-the-counter drug monograph and are different than antibacterial soaps, hand sanitizers, and other consumer antiseptic products, which are not included in this proposed rule. To continue to market these products under the monograph, manufacturers must provide the FDA with more data on the safety and effectiveness of the active ingredients, including absorption, hormonal effects, and bacterial resistance, the statement said.
“Emerging science” suggests that, for at least some active ingredients used in these products, “systemic exposure … is higher than previously thought, and existing data raise potential concerns about the effects of repeated daily human exposure to some antiseptic active ingredients,” the statement said. The agency “is particularly interested in gathering additional data on the long-term safety of daily, repeated exposure to these ingredients in the health care setting and on the use of these products by certain populations, including pregnant and breastfeeding health care workers, for which topical absorption of the active ingredients may be important.”
The proposed rule is available at www.federalregister.gov. Public comments can be submitted until Oct. 27.
PAS: Fewer readmissions with narrow-spectrum antibiotics in children with appendicitis
SAN DIEGO – Narrow-spectrum antibiotics yield outcomes that are at least comparable, if not better, than broad-spectrum antibiotics when prescribed to children with appendicitis, according to a retrospective cohort study presented at the annual meeting of the Pediatric Academic Societies.
The study found that in cases of both complicated and uncomplicated appendicitis, rates of hospital readmission were consistently lower for children prescribed narrow-spectrum antibiotics versus broad-spectrum ones.
“Current guidelines recommend what we ended up defining as narrow-spectrum antibiotics, such as cefoxitin, for uncomplicated cases of appendicitis,” said Dr. Matthew P. Kronman of Seattle Children’s Hospital and the study’s lead author. “For the complicated appendicitis cases, the guidelines state that you can either use one of the narrow-spectrum antibiotics, or you can use other agents – such as piperacillin, ticarcillin, ceftazidime, cefepime, or a carbapenem, for example – that we defined as “broad spectrum” because they provide a wider range of protection and have so much activity that patients often don’t need.”
Dr. Kronman and his coinvestigators analyzed the records of 27,306 children aged 3-18 years, admitted to 1 of 23 hospitals for at least 1 day between 2011 and 2013 with appendicitis. The primary outcome was readmission within 30 days for any subsequent abdominal infection or procedure.
Uncomplicated cases accounted for 18.939 of subjects (69.9%), and complicated appendicitis was recorded in the remaining 8.367 (30.1%) of children. Subjects were given broad-spectrum antibiotics in 28.1% of uncomplicated cases and 64.7% of complicated cases.
Overall, 1.0% of patients with uncomplicated appendicitis (189) and 6.0% (498) of complicated cases were readmitted within 30 days. Of the uncomplicated cases, the readmission rate for patients who got broad-spectrum antibiotics was 1.4%, compared with 0.9% for patients who received narrow-spectrum ones; in cases of complicated appendicitis, 6.8% of subjects given broad-spectrum antibiotics were readmitted within 30 days, compared with 4.4% for patients on narrow-spectrum antibiotics.
Multivariate logistic regression was performed on the study population, with adjustments for demographic factors, as well as illness severity and length of stay. Investigators found that age, sex, and insurance type were not factors in the association between broad-spectrum antibiotic intake and readmission within 30 days. However, increased length of stay, illness severity, and placement of a peripherally inserted central catheter line, which was used exclusively for patients with complicated appendicitis, were associated with the primary outcome.
The association between broad-spectrum agents and higher readmission rates could be a result of confounding by indication, wherein patients are given broad-spectrum drugs by physicians because the patients present as very sick, Dr. Kronman said. However, that alone means that they’re at a higher risk for developing complications and being readmitted shortly after receiving treatment, he added.
“But I think it’s reasonable to conclude that those treated with narrow-spectrum antibiotics didn’t do worse, and if they didn’t do worse, there’s no reason that every kid with appendicitis shouldn’t be treated with narrow-spectrum antibiotics because we know that those treated with broader-spectrum antibiotics are more likely to develop colonization with resistant organisms, and can have other complications due to the spectrum of activity brought on by the antibiotics they were given,” Dr. Kronman said. “So if narrow-spectrum antibiotics are just as good, we should try to get every hospital to use them.”
Dr. Kronman did not report any financial disclosures. The study was supported by the Clinical Research Scholars Program at Seattle Children’s Hospital and by the National Center of Advancing Translational Sciences at the National Institutes of Health.
SAN DIEGO – Narrow-spectrum antibiotics yield outcomes that are at least comparable, if not better, than broad-spectrum antibiotics when prescribed to children with appendicitis, according to a retrospective cohort study presented at the annual meeting of the Pediatric Academic Societies.
The study found that in cases of both complicated and uncomplicated appendicitis, rates of hospital readmission were consistently lower for children prescribed narrow-spectrum antibiotics versus broad-spectrum ones.
“Current guidelines recommend what we ended up defining as narrow-spectrum antibiotics, such as cefoxitin, for uncomplicated cases of appendicitis,” said Dr. Matthew P. Kronman of Seattle Children’s Hospital and the study’s lead author. “For the complicated appendicitis cases, the guidelines state that you can either use one of the narrow-spectrum antibiotics, or you can use other agents – such as piperacillin, ticarcillin, ceftazidime, cefepime, or a carbapenem, for example – that we defined as “broad spectrum” because they provide a wider range of protection and have so much activity that patients often don’t need.”
Dr. Kronman and his coinvestigators analyzed the records of 27,306 children aged 3-18 years, admitted to 1 of 23 hospitals for at least 1 day between 2011 and 2013 with appendicitis. The primary outcome was readmission within 30 days for any subsequent abdominal infection or procedure.
Uncomplicated cases accounted for 18.939 of subjects (69.9%), and complicated appendicitis was recorded in the remaining 8.367 (30.1%) of children. Subjects were given broad-spectrum antibiotics in 28.1% of uncomplicated cases and 64.7% of complicated cases.
Overall, 1.0% of patients with uncomplicated appendicitis (189) and 6.0% (498) of complicated cases were readmitted within 30 days. Of the uncomplicated cases, the readmission rate for patients who got broad-spectrum antibiotics was 1.4%, compared with 0.9% for patients who received narrow-spectrum ones; in cases of complicated appendicitis, 6.8% of subjects given broad-spectrum antibiotics were readmitted within 30 days, compared with 4.4% for patients on narrow-spectrum antibiotics.
Multivariate logistic regression was performed on the study population, with adjustments for demographic factors, as well as illness severity and length of stay. Investigators found that age, sex, and insurance type were not factors in the association between broad-spectrum antibiotic intake and readmission within 30 days. However, increased length of stay, illness severity, and placement of a peripherally inserted central catheter line, which was used exclusively for patients with complicated appendicitis, were associated with the primary outcome.
The association between broad-spectrum agents and higher readmission rates could be a result of confounding by indication, wherein patients are given broad-spectrum drugs by physicians because the patients present as very sick, Dr. Kronman said. However, that alone means that they’re at a higher risk for developing complications and being readmitted shortly after receiving treatment, he added.
“But I think it’s reasonable to conclude that those treated with narrow-spectrum antibiotics didn’t do worse, and if they didn’t do worse, there’s no reason that every kid with appendicitis shouldn’t be treated with narrow-spectrum antibiotics because we know that those treated with broader-spectrum antibiotics are more likely to develop colonization with resistant organisms, and can have other complications due to the spectrum of activity brought on by the antibiotics they were given,” Dr. Kronman said. “So if narrow-spectrum antibiotics are just as good, we should try to get every hospital to use them.”
Dr. Kronman did not report any financial disclosures. The study was supported by the Clinical Research Scholars Program at Seattle Children’s Hospital and by the National Center of Advancing Translational Sciences at the National Institutes of Health.
SAN DIEGO – Narrow-spectrum antibiotics yield outcomes that are at least comparable, if not better, than broad-spectrum antibiotics when prescribed to children with appendicitis, according to a retrospective cohort study presented at the annual meeting of the Pediatric Academic Societies.
The study found that in cases of both complicated and uncomplicated appendicitis, rates of hospital readmission were consistently lower for children prescribed narrow-spectrum antibiotics versus broad-spectrum ones.
“Current guidelines recommend what we ended up defining as narrow-spectrum antibiotics, such as cefoxitin, for uncomplicated cases of appendicitis,” said Dr. Matthew P. Kronman of Seattle Children’s Hospital and the study’s lead author. “For the complicated appendicitis cases, the guidelines state that you can either use one of the narrow-spectrum antibiotics, or you can use other agents – such as piperacillin, ticarcillin, ceftazidime, cefepime, or a carbapenem, for example – that we defined as “broad spectrum” because they provide a wider range of protection and have so much activity that patients often don’t need.”
Dr. Kronman and his coinvestigators analyzed the records of 27,306 children aged 3-18 years, admitted to 1 of 23 hospitals for at least 1 day between 2011 and 2013 with appendicitis. The primary outcome was readmission within 30 days for any subsequent abdominal infection or procedure.
Uncomplicated cases accounted for 18.939 of subjects (69.9%), and complicated appendicitis was recorded in the remaining 8.367 (30.1%) of children. Subjects were given broad-spectrum antibiotics in 28.1% of uncomplicated cases and 64.7% of complicated cases.
Overall, 1.0% of patients with uncomplicated appendicitis (189) and 6.0% (498) of complicated cases were readmitted within 30 days. Of the uncomplicated cases, the readmission rate for patients who got broad-spectrum antibiotics was 1.4%, compared with 0.9% for patients who received narrow-spectrum ones; in cases of complicated appendicitis, 6.8% of subjects given broad-spectrum antibiotics were readmitted within 30 days, compared with 4.4% for patients on narrow-spectrum antibiotics.
Multivariate logistic regression was performed on the study population, with adjustments for demographic factors, as well as illness severity and length of stay. Investigators found that age, sex, and insurance type were not factors in the association between broad-spectrum antibiotic intake and readmission within 30 days. However, increased length of stay, illness severity, and placement of a peripherally inserted central catheter line, which was used exclusively for patients with complicated appendicitis, were associated with the primary outcome.
The association between broad-spectrum agents and higher readmission rates could be a result of confounding by indication, wherein patients are given broad-spectrum drugs by physicians because the patients present as very sick, Dr. Kronman said. However, that alone means that they’re at a higher risk for developing complications and being readmitted shortly after receiving treatment, he added.
“But I think it’s reasonable to conclude that those treated with narrow-spectrum antibiotics didn’t do worse, and if they didn’t do worse, there’s no reason that every kid with appendicitis shouldn’t be treated with narrow-spectrum antibiotics because we know that those treated with broader-spectrum antibiotics are more likely to develop colonization with resistant organisms, and can have other complications due to the spectrum of activity brought on by the antibiotics they were given,” Dr. Kronman said. “So if narrow-spectrum antibiotics are just as good, we should try to get every hospital to use them.”
Dr. Kronman did not report any financial disclosures. The study was supported by the Clinical Research Scholars Program at Seattle Children’s Hospital and by the National Center of Advancing Translational Sciences at the National Institutes of Health.
AT THE PAS ANNUAL MEETING
Key clinical point: Children with appendicitis who are treated with narrow-spectrum antibiotics experience comparable clinical outcomes to children who receive broad-spectrum antibiotics and, in some instances, achieve even better outcomes.
Major finding: The 30-day readmission rates were consistently higher in children who received broad-spectrum antibiotics, compared with narrow-spectrum antibiotics (1.4% vs. 0.9% in uncomplicated cases, 6.8% vs. 4.4% in complicated cases).
Data source: A retrospective cohort study of 27,306 patients aged 3-18 years, admitted to one of 23 hospitals from 2011 to 2013.
Disclosures: Dr. Kronman did not report any financial conflicts of interest. The study was supported in part by the Clinical Research Scholars Program at Seattle Children’s Hospital, and by the National Center of Advancing Translational Sciences of the National Institutes of Health.
Fatal opioid overdoses down dramatically since 2010
Two changes in the pharmaceutical market in late 2010 dramatically reversed the alarming rise in fatal opioid overdoses that occurred during the preceding decade, according to a report published online April 20 in JAMA Internal Medicine.
Overdose deaths attributed to prescription opioids quadrupled in the U.S. between 1999 and 2010, in parallel with rapidly expanding sales of the drugs. Two changes in the pharmaceutical market were undertaken to address these unrelenting increases: replacing the standard formulation of OxyContin with an abuse-deterrent formulation (resistant to crushing and dissolving the tablets for ingestion, snorting, or injection) and withdrawing propoxyphene from sale, wrote Dr. Marc R. Larochelle of Harvard Pilgrim Health Care Institute and the department of population medicine, Harvard, both in Boston, and his associates.
To assess the impact of these 2 interventions, the investigators examined hospitalizations for prescription opioids as well as dispensing patterns using an insurance database covering adults in all 50 states. The data comprised 31,316,598 patients aged 18-64 who were enrolled in a commercial health plan between 2003 and 2012. There were 12,164 overdoses attributed to prescription opioids during the study period.
The “sudden, substantial, and sustained decreases” in the dispensing of prescription opioids at the end of 2010 was associated with parallel declines in fatal overdoses, which dropped by 19% in 2011 and by a further 20% in 2012. “Extrapolating our estimates at 2 years to the 124 million commercially insured U.S. residents aged 18-64 years, there would be 5,456 fewer prescription opioid overdoses . . . annually,” Dr. Larochelle and his associates said (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamainternmed.2015.0914]).
“This is the first study to demonstrate that a decrease in opioid supply is associated with a decrease in overall prescription opioid overdose,” they noted. “Our results have significant implications for policymakers and health care professionals grappling with the epidemic of opioid abuse and overdose.”
The findings by Larochelle et al highlight the critical importance of one public health lever: controlling the market supply of opioids.
Another effective intervention is to promote judicious opioid prescribing: favoring nonopioid or nonpharmacologic approaches to pain management and, when opioids are necessary, prescribing the lowest possible dose for the shortest amount of time necessary to control pain. Oher promising public health strategies include prescription drug monitoring programs and the regulation of pain clinics.
Dr. Hillary V. Kunins is in the New York City Department of Health and Mental Hygiene, Queens. She reported having no relevant financial disclosures. Dr. Kunins made these remarks in an Invited Commentary (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamaintrnmed. 2015.0939]).
The findings by Larochelle et al highlight the critical importance of one public health lever: controlling the market supply of opioids.
Another effective intervention is to promote judicious opioid prescribing: favoring nonopioid or nonpharmacologic approaches to pain management and, when opioids are necessary, prescribing the lowest possible dose for the shortest amount of time necessary to control pain. Oher promising public health strategies include prescription drug monitoring programs and the regulation of pain clinics.
Dr. Hillary V. Kunins is in the New York City Department of Health and Mental Hygiene, Queens. She reported having no relevant financial disclosures. Dr. Kunins made these remarks in an Invited Commentary (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamaintrnmed. 2015.0939]).
The findings by Larochelle et al highlight the critical importance of one public health lever: controlling the market supply of opioids.
Another effective intervention is to promote judicious opioid prescribing: favoring nonopioid or nonpharmacologic approaches to pain management and, when opioids are necessary, prescribing the lowest possible dose for the shortest amount of time necessary to control pain. Oher promising public health strategies include prescription drug monitoring programs and the regulation of pain clinics.
Dr. Hillary V. Kunins is in the New York City Department of Health and Mental Hygiene, Queens. She reported having no relevant financial disclosures. Dr. Kunins made these remarks in an Invited Commentary (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamaintrnmed. 2015.0939]).
Two changes in the pharmaceutical market in late 2010 dramatically reversed the alarming rise in fatal opioid overdoses that occurred during the preceding decade, according to a report published online April 20 in JAMA Internal Medicine.
Overdose deaths attributed to prescription opioids quadrupled in the U.S. between 1999 and 2010, in parallel with rapidly expanding sales of the drugs. Two changes in the pharmaceutical market were undertaken to address these unrelenting increases: replacing the standard formulation of OxyContin with an abuse-deterrent formulation (resistant to crushing and dissolving the tablets for ingestion, snorting, or injection) and withdrawing propoxyphene from sale, wrote Dr. Marc R. Larochelle of Harvard Pilgrim Health Care Institute and the department of population medicine, Harvard, both in Boston, and his associates.
To assess the impact of these 2 interventions, the investigators examined hospitalizations for prescription opioids as well as dispensing patterns using an insurance database covering adults in all 50 states. The data comprised 31,316,598 patients aged 18-64 who were enrolled in a commercial health plan between 2003 and 2012. There were 12,164 overdoses attributed to prescription opioids during the study period.
The “sudden, substantial, and sustained decreases” in the dispensing of prescription opioids at the end of 2010 was associated with parallel declines in fatal overdoses, which dropped by 19% in 2011 and by a further 20% in 2012. “Extrapolating our estimates at 2 years to the 124 million commercially insured U.S. residents aged 18-64 years, there would be 5,456 fewer prescription opioid overdoses . . . annually,” Dr. Larochelle and his associates said (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamainternmed.2015.0914]).
“This is the first study to demonstrate that a decrease in opioid supply is associated with a decrease in overall prescription opioid overdose,” they noted. “Our results have significant implications for policymakers and health care professionals grappling with the epidemic of opioid abuse and overdose.”
Two changes in the pharmaceutical market in late 2010 dramatically reversed the alarming rise in fatal opioid overdoses that occurred during the preceding decade, according to a report published online April 20 in JAMA Internal Medicine.
Overdose deaths attributed to prescription opioids quadrupled in the U.S. between 1999 and 2010, in parallel with rapidly expanding sales of the drugs. Two changes in the pharmaceutical market were undertaken to address these unrelenting increases: replacing the standard formulation of OxyContin with an abuse-deterrent formulation (resistant to crushing and dissolving the tablets for ingestion, snorting, or injection) and withdrawing propoxyphene from sale, wrote Dr. Marc R. Larochelle of Harvard Pilgrim Health Care Institute and the department of population medicine, Harvard, both in Boston, and his associates.
To assess the impact of these 2 interventions, the investigators examined hospitalizations for prescription opioids as well as dispensing patterns using an insurance database covering adults in all 50 states. The data comprised 31,316,598 patients aged 18-64 who were enrolled in a commercial health plan between 2003 and 2012. There were 12,164 overdoses attributed to prescription opioids during the study period.
The “sudden, substantial, and sustained decreases” in the dispensing of prescription opioids at the end of 2010 was associated with parallel declines in fatal overdoses, which dropped by 19% in 2011 and by a further 20% in 2012. “Extrapolating our estimates at 2 years to the 124 million commercially insured U.S. residents aged 18-64 years, there would be 5,456 fewer prescription opioid overdoses . . . annually,” Dr. Larochelle and his associates said (JAMA Intern. Med. 2015 April 20 [doi:10.1001/jamainternmed.2015.0914]).
“This is the first study to demonstrate that a decrease in opioid supply is associated with a decrease in overall prescription opioid overdose,” they noted. “Our results have significant implications for policymakers and health care professionals grappling with the epidemic of opioid abuse and overdose.”
Key clinical point: Two changes in the pharmaceutical market dramatically reversed fatal opioid overdoses, along with opioid dispensing, in late 2010.
Major finding: “Sudden, substantial, and sustained decreases” in the dispensing of prescription opioids at the end of 2010 was associated with parallel declines in fatal overdoses of 19% in 2011 and 20% in 2012.
Data source: A retrospective cohort study analyzing opioid dispensing and overdose patterns among 31,316,598 privately insured adults during a 10-year period.
Disclosures: This study was supported by the Harvard Pilgrim Health Care Institute, the U.S. Health Resources and Services Administration, and the Ryoichi Sasakawa Fellowship Fund. Dr. Larochelle and his associates reported having no relevant financial disclosures.
U-tube drainage adds option for necrotizing pancreatitis
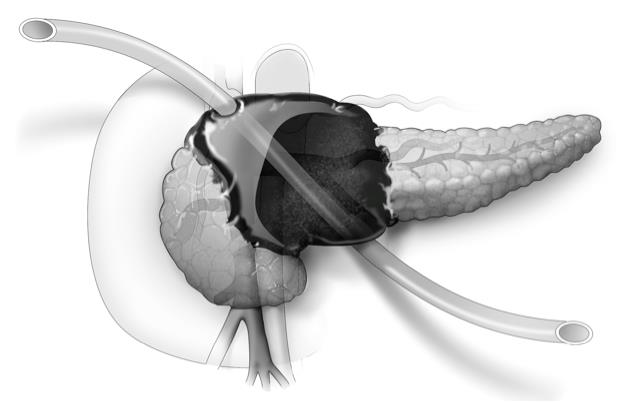
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: U-tube drainage may eliminate the need for surgery in severe necrotizing pancreatitis.
Major finding: Disease-specific mortality occurred in 2 of 22 patients.
Data source: Retrospective study of 22 patients with symptomatic and/or infected necrotizing pancreatitis.
Disclosures: The researchers reported having no financial conflicts.
VTE with transient risk factors is being overtreated
After a first episode of venous thromboembolism, more than 40% of patients with transient risk factors underwent anticoagulation therapy for 12 months or longer – a duration at least four times longer than the period recommended in guidelines, said authors of a large prospective cohort study.
Patients with VTE associated with surgery had about a 0.7% risk/patient-year of recurrence after 3 months of anticoagulation therapy. Patients with transient nonsurgical risk factors had about a 4% risk/patient-year of VTE recurrence.
Further, these patients were more likely to have major bleeding events than recurrent VTEs and were more likely to die of a fatal bleed than from a recurrent pulmonary embolism. Additionally, 38% of major bleeds among patients with transient risk factors occurred during the first 3 months of anticoagulation therapy.
“Our data suggest that in real life, physicians appear to be more concerned about the risk of recurrent VTE after discontinuing therapy than about the risk of bleeding,” said Dr. Walter Ageno at the University of Insubria in Varese, Italy, and his associates. “Clinicians base their treatment decisions on individual risk stratification, taking into account the location of VTE and the presence of additional risk factors for recurrence and bleeding. However, before adequately validated clinical prediction rules become available, this approach may expose a substantial proportion of patients, in particular those with VTE secondary to transient risk factors, to a possibly unnecessary risk of bleeding.”
The American College of Chest Physicians recommends 3 months of anticoagulation therapy for patients with VTE secondary to surgery or a transient, nonsurgical risk factor, and extended (possibly indefinite) anticoagulation for patients with unprovoked VTE or VTE caused by cancer. To look at real-world practice, the researchers carried out a prospective cohort study of 6,944 VTE patients in Italy, Spain, and Belgium. In all, 32% of patients had transient risk factors, 41% had unprovoked VTE, and 27% had cancer (Thrombosis Res. 2015;135:666-72). After excluding patients who died within a year after VTE, 42% of patients with transient risk factors such as recent surgery, pregnancy, or prolonged travel were treated with anticoagulants for more than 12 months, the researchers reported. Significant predictors of extended anticoagulation treatment including being older than 65 years old, having chronic heart failure, pulmonary embolism at presentation, and recurrent VTE during anticoagulation, the researchers also reported. Patients who weighed less than 75 kg, had anemia, or had transient risk factors for VTE were less likely to undergo prolonged treatment than were other patients.
“There is still uncertainty among experts on the optimal duration of secondary prevention of VTE,” concluded the investigators. “This decision should be taken by balancing the risk of recurrence after stopping treatment with the risk of bleeding if treatment is continued.”
Adequately validated clinical prediction rules are needed to make those decisions, the researchers said. Until such tools are validated, a substantial proportion of patients with transiet and secondary risk factors for VTE may be exposed to a possibly unnecessary risk of bleeding, they concluded.
Sanofi Spain and Bayer Pharma AG funded the study. The investigators reported having no relevant conflicts of interest.
After a first episode of venous thromboembolism, more than 40% of patients with transient risk factors underwent anticoagulation therapy for 12 months or longer – a duration at least four times longer than the period recommended in guidelines, said authors of a large prospective cohort study.
Patients with VTE associated with surgery had about a 0.7% risk/patient-year of recurrence after 3 months of anticoagulation therapy. Patients with transient nonsurgical risk factors had about a 4% risk/patient-year of VTE recurrence.
Further, these patients were more likely to have major bleeding events than recurrent VTEs and were more likely to die of a fatal bleed than from a recurrent pulmonary embolism. Additionally, 38% of major bleeds among patients with transient risk factors occurred during the first 3 months of anticoagulation therapy.
“Our data suggest that in real life, physicians appear to be more concerned about the risk of recurrent VTE after discontinuing therapy than about the risk of bleeding,” said Dr. Walter Ageno at the University of Insubria in Varese, Italy, and his associates. “Clinicians base their treatment decisions on individual risk stratification, taking into account the location of VTE and the presence of additional risk factors for recurrence and bleeding. However, before adequately validated clinical prediction rules become available, this approach may expose a substantial proportion of patients, in particular those with VTE secondary to transient risk factors, to a possibly unnecessary risk of bleeding.”
The American College of Chest Physicians recommends 3 months of anticoagulation therapy for patients with VTE secondary to surgery or a transient, nonsurgical risk factor, and extended (possibly indefinite) anticoagulation for patients with unprovoked VTE or VTE caused by cancer. To look at real-world practice, the researchers carried out a prospective cohort study of 6,944 VTE patients in Italy, Spain, and Belgium. In all, 32% of patients had transient risk factors, 41% had unprovoked VTE, and 27% had cancer (Thrombosis Res. 2015;135:666-72). After excluding patients who died within a year after VTE, 42% of patients with transient risk factors such as recent surgery, pregnancy, or prolonged travel were treated with anticoagulants for more than 12 months, the researchers reported. Significant predictors of extended anticoagulation treatment including being older than 65 years old, having chronic heart failure, pulmonary embolism at presentation, and recurrent VTE during anticoagulation, the researchers also reported. Patients who weighed less than 75 kg, had anemia, or had transient risk factors for VTE were less likely to undergo prolonged treatment than were other patients.
“There is still uncertainty among experts on the optimal duration of secondary prevention of VTE,” concluded the investigators. “This decision should be taken by balancing the risk of recurrence after stopping treatment with the risk of bleeding if treatment is continued.”
Adequately validated clinical prediction rules are needed to make those decisions, the researchers said. Until such tools are validated, a substantial proportion of patients with transiet and secondary risk factors for VTE may be exposed to a possibly unnecessary risk of bleeding, they concluded.
Sanofi Spain and Bayer Pharma AG funded the study. The investigators reported having no relevant conflicts of interest.
After a first episode of venous thromboembolism, more than 40% of patients with transient risk factors underwent anticoagulation therapy for 12 months or longer – a duration at least four times longer than the period recommended in guidelines, said authors of a large prospective cohort study.
Patients with VTE associated with surgery had about a 0.7% risk/patient-year of recurrence after 3 months of anticoagulation therapy. Patients with transient nonsurgical risk factors had about a 4% risk/patient-year of VTE recurrence.
Further, these patients were more likely to have major bleeding events than recurrent VTEs and were more likely to die of a fatal bleed than from a recurrent pulmonary embolism. Additionally, 38% of major bleeds among patients with transient risk factors occurred during the first 3 months of anticoagulation therapy.
“Our data suggest that in real life, physicians appear to be more concerned about the risk of recurrent VTE after discontinuing therapy than about the risk of bleeding,” said Dr. Walter Ageno at the University of Insubria in Varese, Italy, and his associates. “Clinicians base their treatment decisions on individual risk stratification, taking into account the location of VTE and the presence of additional risk factors for recurrence and bleeding. However, before adequately validated clinical prediction rules become available, this approach may expose a substantial proportion of patients, in particular those with VTE secondary to transient risk factors, to a possibly unnecessary risk of bleeding.”
The American College of Chest Physicians recommends 3 months of anticoagulation therapy for patients with VTE secondary to surgery or a transient, nonsurgical risk factor, and extended (possibly indefinite) anticoagulation for patients with unprovoked VTE or VTE caused by cancer. To look at real-world practice, the researchers carried out a prospective cohort study of 6,944 VTE patients in Italy, Spain, and Belgium. In all, 32% of patients had transient risk factors, 41% had unprovoked VTE, and 27% had cancer (Thrombosis Res. 2015;135:666-72). After excluding patients who died within a year after VTE, 42% of patients with transient risk factors such as recent surgery, pregnancy, or prolonged travel were treated with anticoagulants for more than 12 months, the researchers reported. Significant predictors of extended anticoagulation treatment including being older than 65 years old, having chronic heart failure, pulmonary embolism at presentation, and recurrent VTE during anticoagulation, the researchers also reported. Patients who weighed less than 75 kg, had anemia, or had transient risk factors for VTE were less likely to undergo prolonged treatment than were other patients.
“There is still uncertainty among experts on the optimal duration of secondary prevention of VTE,” concluded the investigators. “This decision should be taken by balancing the risk of recurrence after stopping treatment with the risk of bleeding if treatment is continued.”
Adequately validated clinical prediction rules are needed to make those decisions, the researchers said. Until such tools are validated, a substantial proportion of patients with transiet and secondary risk factors for VTE may be exposed to a possibly unnecessary risk of bleeding, they concluded.
Sanofi Spain and Bayer Pharma AG funded the study. The investigators reported having no relevant conflicts of interest.
FROM THROMBOSIS RESEARCH
Key clinical point: After venous thromboembolism, patients with transient or removable risk factors for VTE often underwent unneeded, prolonged anticoagulation therapy.
Major finding: Of patients with transient VTE risk factors, 42% underwent anticoagulation therapy for 12 months or longer.
Data source: Prospective cohort study of 6,944 patients with VTE.
Disclosures: Sanofi Spain and Bayer Pharma AG funded the study. The investigators reported having no relevant conflicts of interest.
‘Fresh’ no better than standard red cells
Compared with standard-issue red cells, transfusion of “fresh” red cells stored for fewer than 8 days failed to improve 90-day mortality in a large international study of adult ICU patients, which was reported online April 9 in the New England Journal of Medicine.
“Current regulations permit the storage of red cells for up to 42 days, but prolonged storage has been associated with changes that may render cells ineffective as oxygen carriers and that lead to the accumulation of substances that have untoward biologic effects,” said Dr. Jacques Lacroix of the University of Montreal and his associates.
A recent meta-analysis suggested that transfusion of older red cells was associated with a 16% increase in mortality among critically ill patients, but several randomized trials have failed to document any adverse effects on oxygenation, immunologic, or coagulation factors. Dr. Lacroix and his associates performed the Age of Blood Evaluation (ABLE) study, a prospective, blinded clinical trial involving ICU patients enrolled during a 5-year period at 64 medical centers in Canada, the United Kingdom, France, the Netherlands, and Belgium. A total of 1,211 participants were randomly assigned to receive “fresh” blood stored for an average of 6 days and 1,219 to receive standard blood stored for an average of 22 days – a difference that the investigators deemed statistically and clinically significant.
The primary outcome measure, 90-day all-cause mortality, was 37% in the fresh-blood group and 35% in the standard-blood group, a nonsignificant difference. There also were no significant differences in mortality between the two study groups in any of several subgroup analyses based on patient age; the number of units transfused; baseline APACHE II scores; major comorbidities; duration of respiratory, hemodynamic, or renal support; length of ICU stay; or length of hospital stay, Dr Lacroix and his associates said (N. Engl. J. Med. 2015 April 9 [doi:10.1056/NEJMoa1500704]).
“These findings have important implications for the critical care and blood transfusion communities. We surmise that the use of fresh red cells is not justified at this time. We might also infer that changes to red cells or the storage medium that have been documented in many laboratory studies may have limited clinical consequences,” they noted.
This trial was supported by the Canadian Institutes of Health Research, several other Canadian and French government agencies, and Sanquin Blood Supply. Dr. Lacroix reported having no financial disclosures; his associates reported ties to AKPA Pharma, Roche Diagnostics, GlaxoSmithKline, Novartis, and Amgen.
Compared with standard-issue red cells, transfusion of “fresh” red cells stored for fewer than 8 days failed to improve 90-day mortality in a large international study of adult ICU patients, which was reported online April 9 in the New England Journal of Medicine.
“Current regulations permit the storage of red cells for up to 42 days, but prolonged storage has been associated with changes that may render cells ineffective as oxygen carriers and that lead to the accumulation of substances that have untoward biologic effects,” said Dr. Jacques Lacroix of the University of Montreal and his associates.
A recent meta-analysis suggested that transfusion of older red cells was associated with a 16% increase in mortality among critically ill patients, but several randomized trials have failed to document any adverse effects on oxygenation, immunologic, or coagulation factors. Dr. Lacroix and his associates performed the Age of Blood Evaluation (ABLE) study, a prospective, blinded clinical trial involving ICU patients enrolled during a 5-year period at 64 medical centers in Canada, the United Kingdom, France, the Netherlands, and Belgium. A total of 1,211 participants were randomly assigned to receive “fresh” blood stored for an average of 6 days and 1,219 to receive standard blood stored for an average of 22 days – a difference that the investigators deemed statistically and clinically significant.
The primary outcome measure, 90-day all-cause mortality, was 37% in the fresh-blood group and 35% in the standard-blood group, a nonsignificant difference. There also were no significant differences in mortality between the two study groups in any of several subgroup analyses based on patient age; the number of units transfused; baseline APACHE II scores; major comorbidities; duration of respiratory, hemodynamic, or renal support; length of ICU stay; or length of hospital stay, Dr Lacroix and his associates said (N. Engl. J. Med. 2015 April 9 [doi:10.1056/NEJMoa1500704]).
“These findings have important implications for the critical care and blood transfusion communities. We surmise that the use of fresh red cells is not justified at this time. We might also infer that changes to red cells or the storage medium that have been documented in many laboratory studies may have limited clinical consequences,” they noted.
This trial was supported by the Canadian Institutes of Health Research, several other Canadian and French government agencies, and Sanquin Blood Supply. Dr. Lacroix reported having no financial disclosures; his associates reported ties to AKPA Pharma, Roche Diagnostics, GlaxoSmithKline, Novartis, and Amgen.
Compared with standard-issue red cells, transfusion of “fresh” red cells stored for fewer than 8 days failed to improve 90-day mortality in a large international study of adult ICU patients, which was reported online April 9 in the New England Journal of Medicine.
“Current regulations permit the storage of red cells for up to 42 days, but prolonged storage has been associated with changes that may render cells ineffective as oxygen carriers and that lead to the accumulation of substances that have untoward biologic effects,” said Dr. Jacques Lacroix of the University of Montreal and his associates.
A recent meta-analysis suggested that transfusion of older red cells was associated with a 16% increase in mortality among critically ill patients, but several randomized trials have failed to document any adverse effects on oxygenation, immunologic, or coagulation factors. Dr. Lacroix and his associates performed the Age of Blood Evaluation (ABLE) study, a prospective, blinded clinical trial involving ICU patients enrolled during a 5-year period at 64 medical centers in Canada, the United Kingdom, France, the Netherlands, and Belgium. A total of 1,211 participants were randomly assigned to receive “fresh” blood stored for an average of 6 days and 1,219 to receive standard blood stored for an average of 22 days – a difference that the investigators deemed statistically and clinically significant.
The primary outcome measure, 90-day all-cause mortality, was 37% in the fresh-blood group and 35% in the standard-blood group, a nonsignificant difference. There also were no significant differences in mortality between the two study groups in any of several subgroup analyses based on patient age; the number of units transfused; baseline APACHE II scores; major comorbidities; duration of respiratory, hemodynamic, or renal support; length of ICU stay; or length of hospital stay, Dr Lacroix and his associates said (N. Engl. J. Med. 2015 April 9 [doi:10.1056/NEJMoa1500704]).
“These findings have important implications for the critical care and blood transfusion communities. We surmise that the use of fresh red cells is not justified at this time. We might also infer that changes to red cells or the storage medium that have been documented in many laboratory studies may have limited clinical consequences,” they noted.
This trial was supported by the Canadian Institutes of Health Research, several other Canadian and French government agencies, and Sanquin Blood Supply. Dr. Lacroix reported having no financial disclosures; his associates reported ties to AKPA Pharma, Roche Diagnostics, GlaxoSmithKline, Novartis, and Amgen.
Key clinical point: Transfusing “fresher” red blood cells didn’t decrease 90-day mortality in ICU patients, compared with standard transfusions.
Major finding: The primary outcome measure, 90-day all-cause mortality, was 37% in the fresh-blood group and 35% in the standard-blood group.
Data source: A 5-year international, randomized, blinded clinical trial involving 2,430 adult ICU patients.
Disclosures: This trial was supported by the Canadian Institutes of Health Research, several other Canadian and French government agencies, and Sanquin Blood Supply. Dr. Lacroix reported having no financial disclosures; his associates reported ties to AKPA Pharma, Roche Diagnostics, GlaxoSmithKline, Novartis, and Amgen.
Smaller tubes take bite out of blood draws in critically ill
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Utilizing small-volume phlebotomy tubes minimizes diagnostic blood loss in the critically ill.
Major finding: Small tubes vs. conventional tubes reduced overall phlebotomy blood loss (174 mL vs. 299 mL; P < .001) and transfused packed RBCs (mean 4.4 units vs. 6.0 units; P = .16).
Data source: Retrospective case cohort in 248 critically ill patients.
Disclosures: Dr. Dolman reported having no financial disclosures.