User login
Early drain removal safe in 60% of pancreaticoduodenectomy patients
The majority of patients undergoing pancreaticoduodenectomy will not develop pancreatic fistula and may safely have drains removed on the first postoperative day, a prospective cohort study has found.
Less than 1% of patients with drain amylase levels below 600 U/L on postoperative day 1 will develop pancreatic fistula (PF). This means that in this group – which represents about 60% of PD patients – early drain removal may be a safe management option.
For their research, published online in Annals of Surgery (2015 Jan. 12 [doi:10.1097/SLA.0000000000001038), Dr. Zhi Ven Fong and colleagues at Massachusetts General Hospital and Harvard Medical School, Boston, sought to find the threshold value for drain amylase that predicts fistula, with the goal of helping guide surgeons’ decisions on drain management.
Most surgeons place intraperitoneal drains during PD to control leakage in the event that anastomoses fail. However, some surgeons have abandoned drain placement after PD out of concerns that drains can introduce infection and cause other complications, with risks increasing the longer drains are in place. Drain placement followed by amylase measurement and early removal in low-risk patients “represents a middle ground between the two practices,” Dr. Fong and colleagues wrote.
The investigators evaluated results from two cohorts of consecutive patients undergoing pancreaticoduodenectomy at their surgical center, an initial training cohort (n = 126) and a validation cohort (n = 369). Closed-suction drains were used in all patients, and drain output and amylase levels were prospectively measured daily until drain removal or patient discharge.
Results from the first cohort showed that a drain amylase level of 612 U/L or higher showed the best accuracy (86%), sensitivity (93%), and specificity (79%) in predicting fistula, compared with other established variables.
In the larger validation cohort, the 140 patients with drain amylase values of 600 or higher on postoperative day 1 saw a PF rate of 31.4% (odds ratio = 52, P < .0001). Of the 229 patients with values lower than 600, a group comprising 62.1% of the cohort, fistula developed in only two cases (0.9%). An amylase value below 600 proved a stronger predictor of the absence of PF (OR = 0.0192, P < .0001) than pancreatic gland texture (OR = 0.193, P = .002) and duct diameter (OR = 0.861, P = .835).
“We believe that the debate [over] current intraperitoneal drain management after PD should not be ‘to drain or not to drain’ but rather ‘who and when can we stop draining,’ ” Dr. Fong and colleagues wrote.
“Risk of PF is less than 1% if POD [postoperative day] 1 drain amylase level is lower than 600 U/L. We propose that in this group, which comprises more than 60% of patients, intraperitoneal drains should be removed on PODs 1 and 2, and are currently validating this strategy in our practice,” they wrote.
The investigators cautioned, however, that theirs was a one-site study at an institution whose fistula rates after PD are low, compared with historic rates. “Utilizing POD 1 drain amylase of less than 600 U/L as an early stratification of patients to guide drain removal should not be assumed to be a universally safe practice,” they wrote, until data from larger multisite studies become available.
Dr. Fong and colleagues disclosed no external funding or conflicts of interest.
The majority of patients undergoing pancreaticoduodenectomy will not develop pancreatic fistula and may safely have drains removed on the first postoperative day, a prospective cohort study has found.
Less than 1% of patients with drain amylase levels below 600 U/L on postoperative day 1 will develop pancreatic fistula (PF). This means that in this group – which represents about 60% of PD patients – early drain removal may be a safe management option.
For their research, published online in Annals of Surgery (2015 Jan. 12 [doi:10.1097/SLA.0000000000001038), Dr. Zhi Ven Fong and colleagues at Massachusetts General Hospital and Harvard Medical School, Boston, sought to find the threshold value for drain amylase that predicts fistula, with the goal of helping guide surgeons’ decisions on drain management.
Most surgeons place intraperitoneal drains during PD to control leakage in the event that anastomoses fail. However, some surgeons have abandoned drain placement after PD out of concerns that drains can introduce infection and cause other complications, with risks increasing the longer drains are in place. Drain placement followed by amylase measurement and early removal in low-risk patients “represents a middle ground between the two practices,” Dr. Fong and colleagues wrote.
The investigators evaluated results from two cohorts of consecutive patients undergoing pancreaticoduodenectomy at their surgical center, an initial training cohort (n = 126) and a validation cohort (n = 369). Closed-suction drains were used in all patients, and drain output and amylase levels were prospectively measured daily until drain removal or patient discharge.
Results from the first cohort showed that a drain amylase level of 612 U/L or higher showed the best accuracy (86%), sensitivity (93%), and specificity (79%) in predicting fistula, compared with other established variables.
In the larger validation cohort, the 140 patients with drain amylase values of 600 or higher on postoperative day 1 saw a PF rate of 31.4% (odds ratio = 52, P < .0001). Of the 229 patients with values lower than 600, a group comprising 62.1% of the cohort, fistula developed in only two cases (0.9%). An amylase value below 600 proved a stronger predictor of the absence of PF (OR = 0.0192, P < .0001) than pancreatic gland texture (OR = 0.193, P = .002) and duct diameter (OR = 0.861, P = .835).
“We believe that the debate [over] current intraperitoneal drain management after PD should not be ‘to drain or not to drain’ but rather ‘who and when can we stop draining,’ ” Dr. Fong and colleagues wrote.
“Risk of PF is less than 1% if POD [postoperative day] 1 drain amylase level is lower than 600 U/L. We propose that in this group, which comprises more than 60% of patients, intraperitoneal drains should be removed on PODs 1 and 2, and are currently validating this strategy in our practice,” they wrote.
The investigators cautioned, however, that theirs was a one-site study at an institution whose fistula rates after PD are low, compared with historic rates. “Utilizing POD 1 drain amylase of less than 600 U/L as an early stratification of patients to guide drain removal should not be assumed to be a universally safe practice,” they wrote, until data from larger multisite studies become available.
Dr. Fong and colleagues disclosed no external funding or conflicts of interest.
The majority of patients undergoing pancreaticoduodenectomy will not develop pancreatic fistula and may safely have drains removed on the first postoperative day, a prospective cohort study has found.
Less than 1% of patients with drain amylase levels below 600 U/L on postoperative day 1 will develop pancreatic fistula (PF). This means that in this group – which represents about 60% of PD patients – early drain removal may be a safe management option.
For their research, published online in Annals of Surgery (2015 Jan. 12 [doi:10.1097/SLA.0000000000001038), Dr. Zhi Ven Fong and colleagues at Massachusetts General Hospital and Harvard Medical School, Boston, sought to find the threshold value for drain amylase that predicts fistula, with the goal of helping guide surgeons’ decisions on drain management.
Most surgeons place intraperitoneal drains during PD to control leakage in the event that anastomoses fail. However, some surgeons have abandoned drain placement after PD out of concerns that drains can introduce infection and cause other complications, with risks increasing the longer drains are in place. Drain placement followed by amylase measurement and early removal in low-risk patients “represents a middle ground between the two practices,” Dr. Fong and colleagues wrote.
The investigators evaluated results from two cohorts of consecutive patients undergoing pancreaticoduodenectomy at their surgical center, an initial training cohort (n = 126) and a validation cohort (n = 369). Closed-suction drains were used in all patients, and drain output and amylase levels were prospectively measured daily until drain removal or patient discharge.
Results from the first cohort showed that a drain amylase level of 612 U/L or higher showed the best accuracy (86%), sensitivity (93%), and specificity (79%) in predicting fistula, compared with other established variables.
In the larger validation cohort, the 140 patients with drain amylase values of 600 or higher on postoperative day 1 saw a PF rate of 31.4% (odds ratio = 52, P < .0001). Of the 229 patients with values lower than 600, a group comprising 62.1% of the cohort, fistula developed in only two cases (0.9%). An amylase value below 600 proved a stronger predictor of the absence of PF (OR = 0.0192, P < .0001) than pancreatic gland texture (OR = 0.193, P = .002) and duct diameter (OR = 0.861, P = .835).
“We believe that the debate [over] current intraperitoneal drain management after PD should not be ‘to drain or not to drain’ but rather ‘who and when can we stop draining,’ ” Dr. Fong and colleagues wrote.
“Risk of PF is less than 1% if POD [postoperative day] 1 drain amylase level is lower than 600 U/L. We propose that in this group, which comprises more than 60% of patients, intraperitoneal drains should be removed on PODs 1 and 2, and are currently validating this strategy in our practice,” they wrote.
The investigators cautioned, however, that theirs was a one-site study at an institution whose fistula rates after PD are low, compared with historic rates. “Utilizing POD 1 drain amylase of less than 600 U/L as an early stratification of patients to guide drain removal should not be assumed to be a universally safe practice,” they wrote, until data from larger multisite studies become available.
Dr. Fong and colleagues disclosed no external funding or conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Most patients undergoing pancreaticoduodenectomy can safely have drains removed 1 or 2 days following the procedure, reducing complication risks associated with longer-term drain use.
Major finding: Drain amylase values below 600 U/L on postoperative day 1, seen in more than 60% of the cohort, correspond with a low risk of fistula development.
Data source: A prospective cohort study evaluating about 500 patients, all undergoing PD at a major surgical center.
Disclosures: Dr. Fong and colleagues disclosed no external funding or conflicts of interest.
Trio of risk factors predict gangrenous cholecystitis
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: Older age, diabetes and elevated bilirubin were risk factors for acute gangrenous cholecystitis.
Major finding: Patients with acute gangrenous cholecystitis vs. cholecystitis without necrosis were older (55.8 vs. 40.8 years; P value ≤ .001), more likely to have diabetes (32% vs. 6.7%; P≤ .05) and an elevated bilirubin (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
Data source: Retrospective analysis of 489 patients undergoing cholecystectomy.
Disclosures: The authors reported having no relevant financial disclosures.
FDA approves first internal tissue adhesive for use in abdominoplasty
The Food and Drug Administration has approved a urethane-based surgical adhesive for use during abdominoplasty, the first synthetic tissue adhesive approved for internal use, the FDA announced on Feb. 4.
The approved indication for the adhesive, called TissuGlu, is for “the approximation of tissue layers where subcutaneous dead space exists between the tissue planes in abdominoplasty.” The use of this product “will help some abdominoplasty patients get back to their daily routine after surgery more quickly than if surgical drains had been inserted,” Dr. William Maisel, deputy director for science at the FDA’s Center for Devices and Radiological Health, said in the statement announcing the approval.
To apply TissuGlu, the surgeon uses a hand-held applicator to apply drops of the adhesive to the tissue surface, then positions the abdominoplasty flap in place. “Water in the patient’s tissue starts a chemical reaction that bonds the flaps together. The surgeon then proceeds with standard closure of the skin using sutures,” according to the statement, which adds that use of an internal adhesive to connect the tissue flaps “may reduce or eliminate the need for postoperative surgical draining of fluid between the abdominoplasty tissue flaps.”
The data reviewed by the FDA included a study of 130 patients who were undergoing an elective abdominoplasty; surgical drains were used in half of the patients and half received TissuGlu only. Among those who received TissuGlu only, 73% required no postoperative interventions to drain fluid that had accumulated between the abdominoplasty tissue flaps, but those who needed interventions “were more likely to require another operation to insert surgical drains,” the statement said.
Patients treated with TissuGlu who did not require a surgical drain were “generally able to return to most daily activities such as showering, climbing stairs, and resuming their usual routines sooner than those who had surgical drains,” but the levels of surgery-related pain or discomfort reported by the patients were not different between the two groups.
Cohera Medical is the manufacturer of TissuGlu, which has been on the market in the European Union since 2011, according to the company.
TissuGlu was reviewed at a meeting of the FDA’s general and plastic surgery devices advisory panel in August 2014.
Information on the approval, as well as patient and physician labeling, is available on the FDA website.
The Food and Drug Administration has approved a urethane-based surgical adhesive for use during abdominoplasty, the first synthetic tissue adhesive approved for internal use, the FDA announced on Feb. 4.
The approved indication for the adhesive, called TissuGlu, is for “the approximation of tissue layers where subcutaneous dead space exists between the tissue planes in abdominoplasty.” The use of this product “will help some abdominoplasty patients get back to their daily routine after surgery more quickly than if surgical drains had been inserted,” Dr. William Maisel, deputy director for science at the FDA’s Center for Devices and Radiological Health, said in the statement announcing the approval.
To apply TissuGlu, the surgeon uses a hand-held applicator to apply drops of the adhesive to the tissue surface, then positions the abdominoplasty flap in place. “Water in the patient’s tissue starts a chemical reaction that bonds the flaps together. The surgeon then proceeds with standard closure of the skin using sutures,” according to the statement, which adds that use of an internal adhesive to connect the tissue flaps “may reduce or eliminate the need for postoperative surgical draining of fluid between the abdominoplasty tissue flaps.”
The data reviewed by the FDA included a study of 130 patients who were undergoing an elective abdominoplasty; surgical drains were used in half of the patients and half received TissuGlu only. Among those who received TissuGlu only, 73% required no postoperative interventions to drain fluid that had accumulated between the abdominoplasty tissue flaps, but those who needed interventions “were more likely to require another operation to insert surgical drains,” the statement said.
Patients treated with TissuGlu who did not require a surgical drain were “generally able to return to most daily activities such as showering, climbing stairs, and resuming their usual routines sooner than those who had surgical drains,” but the levels of surgery-related pain or discomfort reported by the patients were not different between the two groups.
Cohera Medical is the manufacturer of TissuGlu, which has been on the market in the European Union since 2011, according to the company.
TissuGlu was reviewed at a meeting of the FDA’s general and plastic surgery devices advisory panel in August 2014.
Information on the approval, as well as patient and physician labeling, is available on the FDA website.
The Food and Drug Administration has approved a urethane-based surgical adhesive for use during abdominoplasty, the first synthetic tissue adhesive approved for internal use, the FDA announced on Feb. 4.
The approved indication for the adhesive, called TissuGlu, is for “the approximation of tissue layers where subcutaneous dead space exists between the tissue planes in abdominoplasty.” The use of this product “will help some abdominoplasty patients get back to their daily routine after surgery more quickly than if surgical drains had been inserted,” Dr. William Maisel, deputy director for science at the FDA’s Center for Devices and Radiological Health, said in the statement announcing the approval.
To apply TissuGlu, the surgeon uses a hand-held applicator to apply drops of the adhesive to the tissue surface, then positions the abdominoplasty flap in place. “Water in the patient’s tissue starts a chemical reaction that bonds the flaps together. The surgeon then proceeds with standard closure of the skin using sutures,” according to the statement, which adds that use of an internal adhesive to connect the tissue flaps “may reduce or eliminate the need for postoperative surgical draining of fluid between the abdominoplasty tissue flaps.”
The data reviewed by the FDA included a study of 130 patients who were undergoing an elective abdominoplasty; surgical drains were used in half of the patients and half received TissuGlu only. Among those who received TissuGlu only, 73% required no postoperative interventions to drain fluid that had accumulated between the abdominoplasty tissue flaps, but those who needed interventions “were more likely to require another operation to insert surgical drains,” the statement said.
Patients treated with TissuGlu who did not require a surgical drain were “generally able to return to most daily activities such as showering, climbing stairs, and resuming their usual routines sooner than those who had surgical drains,” but the levels of surgery-related pain or discomfort reported by the patients were not different between the two groups.
Cohera Medical is the manufacturer of TissuGlu, which has been on the market in the European Union since 2011, according to the company.
TissuGlu was reviewed at a meeting of the FDA’s general and plastic surgery devices advisory panel in August 2014.
Information on the approval, as well as patient and physician labeling, is available on the FDA website.
Study: Surgical readmissions tied to new discharge complications, not prior conditions
Surgical site infection and ileus were the most frequent reason for hospital readmission within 30 days, according to an analysis of data from the National Surgical Quality Improvement Program.
The findings, published online in the Feb. 3 JAMA, suggest that policies that penalize hospitals for readmissions may be ineffective and potentially counterproductive.
Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and his colleagues examined patient data from 346 hospitals participating in the American College of Surgeon’s National Surgical Quality Improvement Program (ACS NSQIP) between January 2012 and December 2012. Readmission rates and reasons were assessed for all surgical procedures and for six representative operations: bariatric surgery, colectomy or proctectomy, hysterectomy, total hip or knee arthroplasty, ventral hernia repair, and lower extremity vascular bypass (JAMA 2015;313;483-95 [doi:10.1001/jama.2014.18614]).
Of the 498, 875 patient sample, the overall readmission rate was 5.7%. For individual procedures, the readmission rate ranged from 3.8% for hysterectomy to 14.9% for lower extremity vascular bypass.
The most common reason for readmission was surgical site infection (SSI; 19.5%), ranging from 11.4% after bariatric surgery to 36.4% after lower extremity vascular bypass. Ileus was the most common reason for readmission after bariatric surgery (24.5%) and the second most common reason overall (10.3%). Other common causes for readmission included dehydration or nutritional deficiency, bleeding or anemia, venous thromboembolism, and prosthesis or graft issues (after arthroplasty and lower extremity vascular bypass procedures). Only 2% of patients were readmitted for the same complication they had experienced during their index hospitalization. Just 3% of patients readmitted for SSIs had experienced an SSI during their index hospitalization.
The results show readmissions after surgery may not be an appropriate measure for pay-for-performance and cost-containment programs, such as the Centers for Medicare & Medicaid Service’s Hospital Readmissions Reduction Program, Dr. Bilimoria said. Performance targets without accepted courses of intervention might be more prone to unintended or ineffective behaviors and consequences, he noted.
“Surgical readmissions mostly reflect postdischarge complications, and readmission rates may be difficult to reduce until effective strategies are put forth to reduce common complications such as SSI,” he said. “Efforts should focus on reducing complication rates overall than simply those that occur after discharge, and this will subsequently reduce readmission rates as well.”
On Twitter @legal_med
These findings provide an unprecedented opportunity to apply these lessons and make substantial reductions in surgical complications, Dr. Lucian L. Leape said in an editorial accompanying the study.
Changing systems is hard work and requires serious commitment. Changing hospital systems is especially difficult because of long-standing traditions and entrenched practices. Successful change requires leadership by those with the will, the determination, and the perseverance to overcome obstacles and motivate colleagues. It requires commitment, which comes from a sense of urgency and a sense of possibility.
One way to develop a sense of urgency is to translate rates into numbers – i.e., actual patients. For example, in this study, surgical site infections accounted for 19.5% of the unplanned readmissions. Even though this only represents 1% of the 498,875 ACS NSQIP patients undergoing surgery in 2012, that 1% equals 5,565 patients. Reducing that number by half would reduce pain and suffering for more than 2,700 patients. If similar success were achieved nationwide, the total would be many times that.
Dr. Lucian L. Leape is with the department of health policy and management at Harvard School of Public Health, Boston, and made these comments in an accompanying editorial (doi:10.1001/jama.2014.18666). He reported having no relevant financial disclosures.
These findings provide an unprecedented opportunity to apply these lessons and make substantial reductions in surgical complications, Dr. Lucian L. Leape said in an editorial accompanying the study.
Changing systems is hard work and requires serious commitment. Changing hospital systems is especially difficult because of long-standing traditions and entrenched practices. Successful change requires leadership by those with the will, the determination, and the perseverance to overcome obstacles and motivate colleagues. It requires commitment, which comes from a sense of urgency and a sense of possibility.
One way to develop a sense of urgency is to translate rates into numbers – i.e., actual patients. For example, in this study, surgical site infections accounted for 19.5% of the unplanned readmissions. Even though this only represents 1% of the 498,875 ACS NSQIP patients undergoing surgery in 2012, that 1% equals 5,565 patients. Reducing that number by half would reduce pain and suffering for more than 2,700 patients. If similar success were achieved nationwide, the total would be many times that.
Dr. Lucian L. Leape is with the department of health policy and management at Harvard School of Public Health, Boston, and made these comments in an accompanying editorial (doi:10.1001/jama.2014.18666). He reported having no relevant financial disclosures.
These findings provide an unprecedented opportunity to apply these lessons and make substantial reductions in surgical complications, Dr. Lucian L. Leape said in an editorial accompanying the study.
Changing systems is hard work and requires serious commitment. Changing hospital systems is especially difficult because of long-standing traditions and entrenched practices. Successful change requires leadership by those with the will, the determination, and the perseverance to overcome obstacles and motivate colleagues. It requires commitment, which comes from a sense of urgency and a sense of possibility.
One way to develop a sense of urgency is to translate rates into numbers – i.e., actual patients. For example, in this study, surgical site infections accounted for 19.5% of the unplanned readmissions. Even though this only represents 1% of the 498,875 ACS NSQIP patients undergoing surgery in 2012, that 1% equals 5,565 patients. Reducing that number by half would reduce pain and suffering for more than 2,700 patients. If similar success were achieved nationwide, the total would be many times that.
Dr. Lucian L. Leape is with the department of health policy and management at Harvard School of Public Health, Boston, and made these comments in an accompanying editorial (doi:10.1001/jama.2014.18666). He reported having no relevant financial disclosures.
Surgical site infection and ileus were the most frequent reason for hospital readmission within 30 days, according to an analysis of data from the National Surgical Quality Improvement Program.
The findings, published online in the Feb. 3 JAMA, suggest that policies that penalize hospitals for readmissions may be ineffective and potentially counterproductive.
Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and his colleagues examined patient data from 346 hospitals participating in the American College of Surgeon’s National Surgical Quality Improvement Program (ACS NSQIP) between January 2012 and December 2012. Readmission rates and reasons were assessed for all surgical procedures and for six representative operations: bariatric surgery, colectomy or proctectomy, hysterectomy, total hip or knee arthroplasty, ventral hernia repair, and lower extremity vascular bypass (JAMA 2015;313;483-95 [doi:10.1001/jama.2014.18614]).
Of the 498, 875 patient sample, the overall readmission rate was 5.7%. For individual procedures, the readmission rate ranged from 3.8% for hysterectomy to 14.9% for lower extremity vascular bypass.
The most common reason for readmission was surgical site infection (SSI; 19.5%), ranging from 11.4% after bariatric surgery to 36.4% after lower extremity vascular bypass. Ileus was the most common reason for readmission after bariatric surgery (24.5%) and the second most common reason overall (10.3%). Other common causes for readmission included dehydration or nutritional deficiency, bleeding or anemia, venous thromboembolism, and prosthesis or graft issues (after arthroplasty and lower extremity vascular bypass procedures). Only 2% of patients were readmitted for the same complication they had experienced during their index hospitalization. Just 3% of patients readmitted for SSIs had experienced an SSI during their index hospitalization.
The results show readmissions after surgery may not be an appropriate measure for pay-for-performance and cost-containment programs, such as the Centers for Medicare & Medicaid Service’s Hospital Readmissions Reduction Program, Dr. Bilimoria said. Performance targets without accepted courses of intervention might be more prone to unintended or ineffective behaviors and consequences, he noted.
“Surgical readmissions mostly reflect postdischarge complications, and readmission rates may be difficult to reduce until effective strategies are put forth to reduce common complications such as SSI,” he said. “Efforts should focus on reducing complication rates overall than simply those that occur after discharge, and this will subsequently reduce readmission rates as well.”
On Twitter @legal_med
Surgical site infection and ileus were the most frequent reason for hospital readmission within 30 days, according to an analysis of data from the National Surgical Quality Improvement Program.
The findings, published online in the Feb. 3 JAMA, suggest that policies that penalize hospitals for readmissions may be ineffective and potentially counterproductive.
Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and his colleagues examined patient data from 346 hospitals participating in the American College of Surgeon’s National Surgical Quality Improvement Program (ACS NSQIP) between January 2012 and December 2012. Readmission rates and reasons were assessed for all surgical procedures and for six representative operations: bariatric surgery, colectomy or proctectomy, hysterectomy, total hip or knee arthroplasty, ventral hernia repair, and lower extremity vascular bypass (JAMA 2015;313;483-95 [doi:10.1001/jama.2014.18614]).
Of the 498, 875 patient sample, the overall readmission rate was 5.7%. For individual procedures, the readmission rate ranged from 3.8% for hysterectomy to 14.9% for lower extremity vascular bypass.
The most common reason for readmission was surgical site infection (SSI; 19.5%), ranging from 11.4% after bariatric surgery to 36.4% after lower extremity vascular bypass. Ileus was the most common reason for readmission after bariatric surgery (24.5%) and the second most common reason overall (10.3%). Other common causes for readmission included dehydration or nutritional deficiency, bleeding or anemia, venous thromboembolism, and prosthesis or graft issues (after arthroplasty and lower extremity vascular bypass procedures). Only 2% of patients were readmitted for the same complication they had experienced during their index hospitalization. Just 3% of patients readmitted for SSIs had experienced an SSI during their index hospitalization.
The results show readmissions after surgery may not be an appropriate measure for pay-for-performance and cost-containment programs, such as the Centers for Medicare & Medicaid Service’s Hospital Readmissions Reduction Program, Dr. Bilimoria said. Performance targets without accepted courses of intervention might be more prone to unintended or ineffective behaviors and consequences, he noted.
“Surgical readmissions mostly reflect postdischarge complications, and readmission rates may be difficult to reduce until effective strategies are put forth to reduce common complications such as SSI,” he said. “Efforts should focus on reducing complication rates overall than simply those that occur after discharge, and this will subsequently reduce readmission rates as well.”
On Twitter @legal_med
Key clinical point: The majority of 30-day readmissions after surgery are associated with new postdischarge complications and not the worsening of medical conditions patients had when initially hospitalized.
Major finding: Of 498,875 patients, the overall unplanned readmission rate was 5.7%. Only 2% of patients were readmitted for the same complication they had experienced during their index hospitalization. The most common reason for readmission was surgical site infections (19.5%).
Data source: A study of 346 hospitals participating in the American College of Surgeon’s National Surgical Quality Improvement Program (ACS NSQIP) between January and December 2012.
Disclosures: The investigators reported no relevant conflicts of interest.
Abuse-deterrent formulation of extended-release hydrocodone approved
A new formulation of extended-release hydrocodone with abuse-deterrent properties has been approved by the Food and Drug Administration, the manufacturer, Zogenix, has announced.
The new formulation, marketed as Zohydro ER, contains extended-release hydrocodone with “pharmaceutical excipients that immediately form a viscous gel when crushed and dissolved in liquids or solvents,” according to the Jan. 30 statement released by the company. The technology is called “BeadTek.”
The company expects to start transitioning from the currently available Zohydro ER product to the newly formulated product in the second quarter of 2015 for all the prescribed strengths of Zohydro ER, to avoid disrupting patients who are being treated with the product, the statement said.
Zohydro ER is an opioid agonist approved for the management of pain “severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate,” according to the prescribing information.
In the second half of this year, the company plans to submit the results of ongoing Human Abuse Liability studies, “which will further characterize the abuse-deterrent properties of the new formulation” and will support the addition of abuse-deterrent claims to the prescribing information, the company statement said. The statement refers to the FDA’s draft guidance for the evaluation and labeling of abuse-deterrent opioids, which describes the abuse-deterrent claims.
Zohydro ER was approved by the FDA in 2013.
A new formulation of extended-release hydrocodone with abuse-deterrent properties has been approved by the Food and Drug Administration, the manufacturer, Zogenix, has announced.
The new formulation, marketed as Zohydro ER, contains extended-release hydrocodone with “pharmaceutical excipients that immediately form a viscous gel when crushed and dissolved in liquids or solvents,” according to the Jan. 30 statement released by the company. The technology is called “BeadTek.”
The company expects to start transitioning from the currently available Zohydro ER product to the newly formulated product in the second quarter of 2015 for all the prescribed strengths of Zohydro ER, to avoid disrupting patients who are being treated with the product, the statement said.
Zohydro ER is an opioid agonist approved for the management of pain “severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate,” according to the prescribing information.
In the second half of this year, the company plans to submit the results of ongoing Human Abuse Liability studies, “which will further characterize the abuse-deterrent properties of the new formulation” and will support the addition of abuse-deterrent claims to the prescribing information, the company statement said. The statement refers to the FDA’s draft guidance for the evaluation and labeling of abuse-deterrent opioids, which describes the abuse-deterrent claims.
Zohydro ER was approved by the FDA in 2013.
A new formulation of extended-release hydrocodone with abuse-deterrent properties has been approved by the Food and Drug Administration, the manufacturer, Zogenix, has announced.
The new formulation, marketed as Zohydro ER, contains extended-release hydrocodone with “pharmaceutical excipients that immediately form a viscous gel when crushed and dissolved in liquids or solvents,” according to the Jan. 30 statement released by the company. The technology is called “BeadTek.”
The company expects to start transitioning from the currently available Zohydro ER product to the newly formulated product in the second quarter of 2015 for all the prescribed strengths of Zohydro ER, to avoid disrupting patients who are being treated with the product, the statement said.
Zohydro ER is an opioid agonist approved for the management of pain “severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate,” according to the prescribing information.
In the second half of this year, the company plans to submit the results of ongoing Human Abuse Liability studies, “which will further characterize the abuse-deterrent properties of the new formulation” and will support the addition of abuse-deterrent claims to the prescribing information, the company statement said. The statement refers to the FDA’s draft guidance for the evaluation and labeling of abuse-deterrent opioids, which describes the abuse-deterrent claims.
Zohydro ER was approved by the FDA in 2013.
Transoral fundoplication can be effective against GERD symptoms
Transoral esophagogastric fundoplication can be an effective treatment for patients seeking to alleviate symptoms associated with gastroesophageal reflux disease, particularly in individuals with persistent regurgitation despite prior treatment with proton pump inhibitor therapy, according to the results of a new study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.009).
“Gastroesophageal reflux disease (GERD) remains one of the most common conditions for which Americans take daily medication, and PPI use has more than doubled in the last decade,” wrote lead authors Dr. John G. Hunter of Oregon Health & Science University in Portland, and Dr. Peter J. Kahrilas of Northwestern University in Chicago, and their associates. “Despite this, up to 40% of proton pump inhibitor (PPI)–dependent GERD patients have troublesome symptoms of GERD, despite PPI therapy.”
In the Randomized EsophyX vs Sham, Placebo-Controlled Transoral Fundoplication (RESPECT) trial, investigators screened 696 patients who were experiencing “troublesome regurgitation” despite daily PPI treatment. These subjects were evaluated via three validated GERD-specific symptom scales, and were either on or off PPI use at the time of trial commencement. Post trial, patients were blinded to therapy and were reassessed at intervals of 2, 12, and 26 weeks. All patients underwent 48-hour esophageal pH monitoring and esophagogastroduodenoscopy at 66 months after the trial ended.
Regurgitation severity was based on the Montreal definition, which was used to measure efficacy of treatments given as part of the study. The Montreal definition of reflux is described by the authors as “either mucosal damage or troublesome symptoms attributable to reflux.” Those with “least troublesome” regurgitation while on PPIs “underwent barium swallow, esophagogastroduodenoscopy, 48-hour esophageal pH monitoring (off PPIs), and high-resolution esophageal manometry analyses.”
Eighty-seven subjects with GERD and hiatal hernias of at least 2 centimeters were randomly assigned to groups that underwent transoral fundoplication (TF) followed by placebo treatment after 6 months, while 42 subjects, who made up the control group, underwent a “sham surgery” and began regimens of once- or twice-daily omeprazole medication for 6 months.
Results showed that 67% of patients who received TF treatment experienced elimination of adverse regurgitation vs. 45% of those treated with PPI (P = .023). Control of esophageal pH also improved noticeably in patients who received TF treatment versus those who did not (9.3% vs. 6.3% on average, respectively, P < .001), but not in patients who received the “sham surgery” (8.6% preop vs. 8.9% postop on average). Fewer patients who received TF treatment recorded having “no response” after 3 months compared with those in the control group (11% vs. 36%, respectively, P = .004).
“Transoral fundoplication may fill the ‘therapeutic gap’ that exists between PPI and laparoscopic fundoplication,” wrote the authors. “Considering the virtual absence of dysphagia and bloating after TF, which may be problematic with LINX [LINX Reflux Management System], it would appear that TF is an option for patients with troublesome regurgitation, as well as for patients with troublesome GERD symptoms who wish not to take PPI over a protracted period of time.”
Several coauthors disclosed ties with the study sponsor EndoGastric Solutions of Redmond, Wash., as well as individual potential conflicts of interest.
Transoral esophagogastric fundoplication can be an effective treatment for patients seeking to alleviate symptoms associated with gastroesophageal reflux disease, particularly in individuals with persistent regurgitation despite prior treatment with proton pump inhibitor therapy, according to the results of a new study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.009).
“Gastroesophageal reflux disease (GERD) remains one of the most common conditions for which Americans take daily medication, and PPI use has more than doubled in the last decade,” wrote lead authors Dr. John G. Hunter of Oregon Health & Science University in Portland, and Dr. Peter J. Kahrilas of Northwestern University in Chicago, and their associates. “Despite this, up to 40% of proton pump inhibitor (PPI)–dependent GERD patients have troublesome symptoms of GERD, despite PPI therapy.”
In the Randomized EsophyX vs Sham, Placebo-Controlled Transoral Fundoplication (RESPECT) trial, investigators screened 696 patients who were experiencing “troublesome regurgitation” despite daily PPI treatment. These subjects were evaluated via three validated GERD-specific symptom scales, and were either on or off PPI use at the time of trial commencement. Post trial, patients were blinded to therapy and were reassessed at intervals of 2, 12, and 26 weeks. All patients underwent 48-hour esophageal pH monitoring and esophagogastroduodenoscopy at 66 months after the trial ended.
Regurgitation severity was based on the Montreal definition, which was used to measure efficacy of treatments given as part of the study. The Montreal definition of reflux is described by the authors as “either mucosal damage or troublesome symptoms attributable to reflux.” Those with “least troublesome” regurgitation while on PPIs “underwent barium swallow, esophagogastroduodenoscopy, 48-hour esophageal pH monitoring (off PPIs), and high-resolution esophageal manometry analyses.”
Eighty-seven subjects with GERD and hiatal hernias of at least 2 centimeters were randomly assigned to groups that underwent transoral fundoplication (TF) followed by placebo treatment after 6 months, while 42 subjects, who made up the control group, underwent a “sham surgery” and began regimens of once- or twice-daily omeprazole medication for 6 months.
Results showed that 67% of patients who received TF treatment experienced elimination of adverse regurgitation vs. 45% of those treated with PPI (P = .023). Control of esophageal pH also improved noticeably in patients who received TF treatment versus those who did not (9.3% vs. 6.3% on average, respectively, P < .001), but not in patients who received the “sham surgery” (8.6% preop vs. 8.9% postop on average). Fewer patients who received TF treatment recorded having “no response” after 3 months compared with those in the control group (11% vs. 36%, respectively, P = .004).
“Transoral fundoplication may fill the ‘therapeutic gap’ that exists between PPI and laparoscopic fundoplication,” wrote the authors. “Considering the virtual absence of dysphagia and bloating after TF, which may be problematic with LINX [LINX Reflux Management System], it would appear that TF is an option for patients with troublesome regurgitation, as well as for patients with troublesome GERD symptoms who wish not to take PPI over a protracted period of time.”
Several coauthors disclosed ties with the study sponsor EndoGastric Solutions of Redmond, Wash., as well as individual potential conflicts of interest.
Transoral esophagogastric fundoplication can be an effective treatment for patients seeking to alleviate symptoms associated with gastroesophageal reflux disease, particularly in individuals with persistent regurgitation despite prior treatment with proton pump inhibitor therapy, according to the results of a new study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.009).
“Gastroesophageal reflux disease (GERD) remains one of the most common conditions for which Americans take daily medication, and PPI use has more than doubled in the last decade,” wrote lead authors Dr. John G. Hunter of Oregon Health & Science University in Portland, and Dr. Peter J. Kahrilas of Northwestern University in Chicago, and their associates. “Despite this, up to 40% of proton pump inhibitor (PPI)–dependent GERD patients have troublesome symptoms of GERD, despite PPI therapy.”
In the Randomized EsophyX vs Sham, Placebo-Controlled Transoral Fundoplication (RESPECT) trial, investigators screened 696 patients who were experiencing “troublesome regurgitation” despite daily PPI treatment. These subjects were evaluated via three validated GERD-specific symptom scales, and were either on or off PPI use at the time of trial commencement. Post trial, patients were blinded to therapy and were reassessed at intervals of 2, 12, and 26 weeks. All patients underwent 48-hour esophageal pH monitoring and esophagogastroduodenoscopy at 66 months after the trial ended.
Regurgitation severity was based on the Montreal definition, which was used to measure efficacy of treatments given as part of the study. The Montreal definition of reflux is described by the authors as “either mucosal damage or troublesome symptoms attributable to reflux.” Those with “least troublesome” regurgitation while on PPIs “underwent barium swallow, esophagogastroduodenoscopy, 48-hour esophageal pH monitoring (off PPIs), and high-resolution esophageal manometry analyses.”
Eighty-seven subjects with GERD and hiatal hernias of at least 2 centimeters were randomly assigned to groups that underwent transoral fundoplication (TF) followed by placebo treatment after 6 months, while 42 subjects, who made up the control group, underwent a “sham surgery” and began regimens of once- or twice-daily omeprazole medication for 6 months.
Results showed that 67% of patients who received TF treatment experienced elimination of adverse regurgitation vs. 45% of those treated with PPI (P = .023). Control of esophageal pH also improved noticeably in patients who received TF treatment versus those who did not (9.3% vs. 6.3% on average, respectively, P < .001), but not in patients who received the “sham surgery” (8.6% preop vs. 8.9% postop on average). Fewer patients who received TF treatment recorded having “no response” after 3 months compared with those in the control group (11% vs. 36%, respectively, P = .004).
“Transoral fundoplication may fill the ‘therapeutic gap’ that exists between PPI and laparoscopic fundoplication,” wrote the authors. “Considering the virtual absence of dysphagia and bloating after TF, which may be problematic with LINX [LINX Reflux Management System], it would appear that TF is an option for patients with troublesome regurgitation, as well as for patients with troublesome GERD symptoms who wish not to take PPI over a protracted period of time.”
Several coauthors disclosed ties with the study sponsor EndoGastric Solutions of Redmond, Wash., as well as individual potential conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Transoral esophagogastric fundoplication (TF) is an effective treatment for gastroesophageal reflux disease symptoms, particularly in patients with persistent regurgitation despite proton pump inhibitor therapy (PPI).
Major finding: Of patients who received TF, 67% experienced elimination of adverse regurgitation, compared with 45% of those treated with PPI (P = .023).
Data source: Randomized EsophyX vs Sham, Placebo-Controlled Transoral Fundoplication (RESPECT) trial.
Disclosures: Several coauthors disclosed ties with the study sponsor EndoGastric Solutions of Redmond, Wash., as well as individual potential conflicts of interest.
Postop pancreatectomy complications most deadly in elderly
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
FROM THE ANNALS OF SURGERY
Key clinical point: Significantly higher rates of mortality are experienced in pancreatectomy patients aged 80 years or older, requiring urgent attention toward minimizing postoperative complications.
Major finding: In-hospital mortality rates were significant higher in the cohort aged 80 years and older (3.0%) than in the younger group (1.1%) (P = .01) even though rates of complications between the two groups were relatively similar.
Data source: Retrospective cohort study of 2,694 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project at 37 high-volume U.S. centers.
Disclosures: Study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
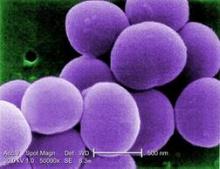
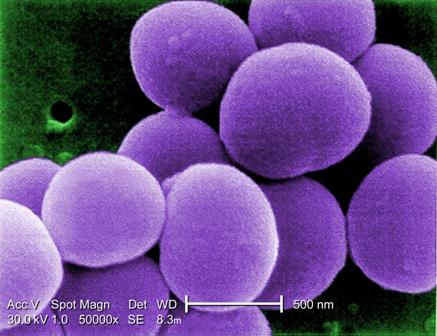
Bundled intervention tackles S. aureus SSIs
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
AT IDWEEK 2014
Key clinical point: Implementing a bundled intervention reduced S. aureus SSIs and could reduce patient morbidity and costs.
Major finding: The pooled S. aureus SSI rate decreased from 0.36% to 0.20% (rate ratio, 0.58).
Data source: A multicenter quasi-experimental effectiveness study of 42,534 procedures.
Disclosures: The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
FDA approves IV antibacterial for complicated UTIs, abdominal infections
A combination of a cephalosporin and a beta-lactamase inhibitor in an intravenous formulation has been approved for treating complicated intra-abdominal infections and complicated urinary tract infections in adults, the Food and Drug Administration announced on Dec. 19.
The cephalosporin is ceftolozane and the beta-lactamase inhibitor is tazobactam; it will be marketed as Zerbaxa by Cubist Pharmaceuticals.
This is the fourth antibacterial drug product approved by the FDA in 2014 and, like the other three, it was designated as a Qualified Infectious Disease Product (QIDP) and was given priority review, according to the FDA statement. Zerbaxa was granted a QIDP designation under the Generating Antibiotic Incentives Now (GAIN) Act of the FDA Safety and Innovation Act, “because it is an antibacterial or antifungal human drug intended to treat a serious or life-threatening infection,” the statement said.
As part of the QIDP program, the manufacturer has also been granted an extra 5 years of “exclusivity” – exclusive marketing rights – by the FDA.
Ceftolozane-tazobactam was approved for treating complicated intra-abdominal infections in combination with metronidazole; approval for this indication was based on a study of 979 adults, randomized to the combination or to meropenem.
Approval for complicated urinary tract infections, including pyelonephritis, was based on a study of 1,068 adults, randomized to treatment with ceftolozane-tazobactam or levofloxacin.
The prescribing information includes a warning about decreased efficacy in patients with renal impairment (a baseline creatinine clearance of 30-50 mL/min or less, and the recommendation to monitor creatinine clearance “at least daily in patients with changing renal function,” and to adjust dose accordingly. Nausea, diarrhea, headache, and fever were the most common adverse events in studies, according to the FDA statement.
The other antibacterials approved by the FDA in 2014 were approved for treating acute bacterial skin and skin structure infections caused by certain susceptible bacteria. They were dalbavancin (Dalvance), approved in May; tedizolid (Sivextro), approved in June; and oritavancin (Orbactiv), approved in August.
Serious adverse events associated with Zerbaxa should be reported to the FDA’s MedWatch program at 800-332-1088 or http://www.fda.gov/Safety/MedWatch/HowToReport/default.htm.
A combination of a cephalosporin and a beta-lactamase inhibitor in an intravenous formulation has been approved for treating complicated intra-abdominal infections and complicated urinary tract infections in adults, the Food and Drug Administration announced on Dec. 19.
The cephalosporin is ceftolozane and the beta-lactamase inhibitor is tazobactam; it will be marketed as Zerbaxa by Cubist Pharmaceuticals.
This is the fourth antibacterial drug product approved by the FDA in 2014 and, like the other three, it was designated as a Qualified Infectious Disease Product (QIDP) and was given priority review, according to the FDA statement. Zerbaxa was granted a QIDP designation under the Generating Antibiotic Incentives Now (GAIN) Act of the FDA Safety and Innovation Act, “because it is an antibacterial or antifungal human drug intended to treat a serious or life-threatening infection,” the statement said.
As part of the QIDP program, the manufacturer has also been granted an extra 5 years of “exclusivity” – exclusive marketing rights – by the FDA.
Ceftolozane-tazobactam was approved for treating complicated intra-abdominal infections in combination with metronidazole; approval for this indication was based on a study of 979 adults, randomized to the combination or to meropenem.
Approval for complicated urinary tract infections, including pyelonephritis, was based on a study of 1,068 adults, randomized to treatment with ceftolozane-tazobactam or levofloxacin.
The prescribing information includes a warning about decreased efficacy in patients with renal impairment (a baseline creatinine clearance of 30-50 mL/min or less, and the recommendation to monitor creatinine clearance “at least daily in patients with changing renal function,” and to adjust dose accordingly. Nausea, diarrhea, headache, and fever were the most common adverse events in studies, according to the FDA statement.
The other antibacterials approved by the FDA in 2014 were approved for treating acute bacterial skin and skin structure infections caused by certain susceptible bacteria. They were dalbavancin (Dalvance), approved in May; tedizolid (Sivextro), approved in June; and oritavancin (Orbactiv), approved in August.
Serious adverse events associated with Zerbaxa should be reported to the FDA’s MedWatch program at 800-332-1088 or http://www.fda.gov/Safety/MedWatch/HowToReport/default.htm.
A combination of a cephalosporin and a beta-lactamase inhibitor in an intravenous formulation has been approved for treating complicated intra-abdominal infections and complicated urinary tract infections in adults, the Food and Drug Administration announced on Dec. 19.
The cephalosporin is ceftolozane and the beta-lactamase inhibitor is tazobactam; it will be marketed as Zerbaxa by Cubist Pharmaceuticals.
This is the fourth antibacterial drug product approved by the FDA in 2014 and, like the other three, it was designated as a Qualified Infectious Disease Product (QIDP) and was given priority review, according to the FDA statement. Zerbaxa was granted a QIDP designation under the Generating Antibiotic Incentives Now (GAIN) Act of the FDA Safety and Innovation Act, “because it is an antibacterial or antifungal human drug intended to treat a serious or life-threatening infection,” the statement said.
As part of the QIDP program, the manufacturer has also been granted an extra 5 years of “exclusivity” – exclusive marketing rights – by the FDA.
Ceftolozane-tazobactam was approved for treating complicated intra-abdominal infections in combination with metronidazole; approval for this indication was based on a study of 979 adults, randomized to the combination or to meropenem.
Approval for complicated urinary tract infections, including pyelonephritis, was based on a study of 1,068 adults, randomized to treatment with ceftolozane-tazobactam or levofloxacin.
The prescribing information includes a warning about decreased efficacy in patients with renal impairment (a baseline creatinine clearance of 30-50 mL/min or less, and the recommendation to monitor creatinine clearance “at least daily in patients with changing renal function,” and to adjust dose accordingly. Nausea, diarrhea, headache, and fever were the most common adverse events in studies, according to the FDA statement.
The other antibacterials approved by the FDA in 2014 were approved for treating acute bacterial skin and skin structure infections caused by certain susceptible bacteria. They were dalbavancin (Dalvance), approved in May; tedizolid (Sivextro), approved in June; and oritavancin (Orbactiv), approved in August.
Serious adverse events associated with Zerbaxa should be reported to the FDA’s MedWatch program at 800-332-1088 or http://www.fda.gov/Safety/MedWatch/HowToReport/default.htm.
Care bundle cut emergency laparotomy death rate by 39%
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
Key clinical point: A set of quality improvement measures cut 30-day emergency laparotomy mortality by about 39%.
Major finding: Thirty-day mortality dropped from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002).
Data source: Prospective, 8-month study of emergency laparotomy outcomes at four hospitals in England.
Disclosures: The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.