User login
Gout: new data support treat-to-target approach
CHICAGO – Failure to reach the therapeutic target of a serum urate level below 6 mg/dL in gout patients is an independent risk factor for all-cause mortality conferring a 139% increased risk, Fernando Perez-Ruiz, MD, PhD, said at the annual meeting of the American College of Rheumatology.
This new finding from a prospective cohort study of 1,193 gout patients constitutes a ringing endorsement that a treat-to-target approach should become the standard in the management of this disease, declared Dr. Perez-Ruiz, a rheumatologist at Hospital Universitario Cruces, Barakaldo, Spain.
“This is encouraging news. We can say to patients and clinicians that we should make every effort to reach the therapeutic target. This is a concept that’s not new in medicine. We do it for diabetes, for hypertension, for hyperlipidemia, and I think now for the first time we will do it for gout,” the rheumatologist said at a press conference highlighting the study findings.
“A lot of physicians including, unfortunately, rheumatologists don’t treat gout to target. They feel like if a patient is doing nicely, that’s good enough. But it’s like lowering cholesterol: If you’re at 400 mg/dL and you go to 300, does that mean it’s fine and you won’t get a myocardial infarction?” he asked rhetorically.
The study included 1,193 gout patients with a mean age at baseline of 60 years, 6.8 years disease duration, and an average of 3-4 flares during the previous year. Mean follow-up was 48 months, translating to 4,830 patient-years of prospective observation. Overall mortality was 13%, mostly from cardiovascular causes.
The mean baseline serum urate level was 9.1 mg/dL. Although both ACR and EULAR guidelines recommend a serum urate level below 6 mg/dL as a therapeutic target, 16.3% of subjects had a level of 6 mg/dL or more despite treatment. The crude mortality rate during follow-up was 80.9 deaths per 1,000 person-years in those with serum urate levels of 6 mg/dL or more, compared with 25.7 per 1,000 person-years in patients with serum urate levels below 6 mg/dL. In a multivariate analysis adjusted for age, prior cardiovascular events, other comorbid conditions, sex, baseline serum urate level, alcohol intake, and other potential confounders, a serum urate of 6 mg/dL or more was independently associated with a 139% increased risk of mortality during follow-up.
“I think the message we would like to give to clinicians is, ‘If you can do that [i.e., maintain the serum urate level below 6 mg/dL], do it. You have the knowledge, you have the means, make the effort. Your patient will benefit from that. Don’t take risks,’” Dr. Perez-Ruiz said.
Session moderator Shraddha Jatwani, MD, a rheumatologist at St. Vincent Hospital in Evansville, Ind., pronounced this a message she will take home to her clinical practice.
“What we usually see in clinical practice is that gout patients are among the most noncompliant. Once they stop hurting they just don’t see the need to take their medication daily. And now that we have this data, we can tell them that their gout medications are like statins, which help reduce the risk of heart attacks. Taking their gout medication will help them reduce their mortality risk. This information will help us to change patient perception,” she said.
Dr. Perez-Ruiz reported relationships with Amgen, Grünenthal, and Menarini.
SOURCE: Perez-Ruiz F et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 869.
CHICAGO – Failure to reach the therapeutic target of a serum urate level below 6 mg/dL in gout patients is an independent risk factor for all-cause mortality conferring a 139% increased risk, Fernando Perez-Ruiz, MD, PhD, said at the annual meeting of the American College of Rheumatology.
This new finding from a prospective cohort study of 1,193 gout patients constitutes a ringing endorsement that a treat-to-target approach should become the standard in the management of this disease, declared Dr. Perez-Ruiz, a rheumatologist at Hospital Universitario Cruces, Barakaldo, Spain.
“This is encouraging news. We can say to patients and clinicians that we should make every effort to reach the therapeutic target. This is a concept that’s not new in medicine. We do it for diabetes, for hypertension, for hyperlipidemia, and I think now for the first time we will do it for gout,” the rheumatologist said at a press conference highlighting the study findings.
“A lot of physicians including, unfortunately, rheumatologists don’t treat gout to target. They feel like if a patient is doing nicely, that’s good enough. But it’s like lowering cholesterol: If you’re at 400 mg/dL and you go to 300, does that mean it’s fine and you won’t get a myocardial infarction?” he asked rhetorically.
The study included 1,193 gout patients with a mean age at baseline of 60 years, 6.8 years disease duration, and an average of 3-4 flares during the previous year. Mean follow-up was 48 months, translating to 4,830 patient-years of prospective observation. Overall mortality was 13%, mostly from cardiovascular causes.
The mean baseline serum urate level was 9.1 mg/dL. Although both ACR and EULAR guidelines recommend a serum urate level below 6 mg/dL as a therapeutic target, 16.3% of subjects had a level of 6 mg/dL or more despite treatment. The crude mortality rate during follow-up was 80.9 deaths per 1,000 person-years in those with serum urate levels of 6 mg/dL or more, compared with 25.7 per 1,000 person-years in patients with serum urate levels below 6 mg/dL. In a multivariate analysis adjusted for age, prior cardiovascular events, other comorbid conditions, sex, baseline serum urate level, alcohol intake, and other potential confounders, a serum urate of 6 mg/dL or more was independently associated with a 139% increased risk of mortality during follow-up.
“I think the message we would like to give to clinicians is, ‘If you can do that [i.e., maintain the serum urate level below 6 mg/dL], do it. You have the knowledge, you have the means, make the effort. Your patient will benefit from that. Don’t take risks,’” Dr. Perez-Ruiz said.
Session moderator Shraddha Jatwani, MD, a rheumatologist at St. Vincent Hospital in Evansville, Ind., pronounced this a message she will take home to her clinical practice.
“What we usually see in clinical practice is that gout patients are among the most noncompliant. Once they stop hurting they just don’t see the need to take their medication daily. And now that we have this data, we can tell them that their gout medications are like statins, which help reduce the risk of heart attacks. Taking their gout medication will help them reduce their mortality risk. This information will help us to change patient perception,” she said.
Dr. Perez-Ruiz reported relationships with Amgen, Grünenthal, and Menarini.
SOURCE: Perez-Ruiz F et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 869.
CHICAGO – Failure to reach the therapeutic target of a serum urate level below 6 mg/dL in gout patients is an independent risk factor for all-cause mortality conferring a 139% increased risk, Fernando Perez-Ruiz, MD, PhD, said at the annual meeting of the American College of Rheumatology.
This new finding from a prospective cohort study of 1,193 gout patients constitutes a ringing endorsement that a treat-to-target approach should become the standard in the management of this disease, declared Dr. Perez-Ruiz, a rheumatologist at Hospital Universitario Cruces, Barakaldo, Spain.
“This is encouraging news. We can say to patients and clinicians that we should make every effort to reach the therapeutic target. This is a concept that’s not new in medicine. We do it for diabetes, for hypertension, for hyperlipidemia, and I think now for the first time we will do it for gout,” the rheumatologist said at a press conference highlighting the study findings.
“A lot of physicians including, unfortunately, rheumatologists don’t treat gout to target. They feel like if a patient is doing nicely, that’s good enough. But it’s like lowering cholesterol: If you’re at 400 mg/dL and you go to 300, does that mean it’s fine and you won’t get a myocardial infarction?” he asked rhetorically.
The study included 1,193 gout patients with a mean age at baseline of 60 years, 6.8 years disease duration, and an average of 3-4 flares during the previous year. Mean follow-up was 48 months, translating to 4,830 patient-years of prospective observation. Overall mortality was 13%, mostly from cardiovascular causes.
The mean baseline serum urate level was 9.1 mg/dL. Although both ACR and EULAR guidelines recommend a serum urate level below 6 mg/dL as a therapeutic target, 16.3% of subjects had a level of 6 mg/dL or more despite treatment. The crude mortality rate during follow-up was 80.9 deaths per 1,000 person-years in those with serum urate levels of 6 mg/dL or more, compared with 25.7 per 1,000 person-years in patients with serum urate levels below 6 mg/dL. In a multivariate analysis adjusted for age, prior cardiovascular events, other comorbid conditions, sex, baseline serum urate level, alcohol intake, and other potential confounders, a serum urate of 6 mg/dL or more was independently associated with a 139% increased risk of mortality during follow-up.
“I think the message we would like to give to clinicians is, ‘If you can do that [i.e., maintain the serum urate level below 6 mg/dL], do it. You have the knowledge, you have the means, make the effort. Your patient will benefit from that. Don’t take risks,’” Dr. Perez-Ruiz said.
Session moderator Shraddha Jatwani, MD, a rheumatologist at St. Vincent Hospital in Evansville, Ind., pronounced this a message she will take home to her clinical practice.
“What we usually see in clinical practice is that gout patients are among the most noncompliant. Once they stop hurting they just don’t see the need to take their medication daily. And now that we have this data, we can tell them that their gout medications are like statins, which help reduce the risk of heart attacks. Taking their gout medication will help them reduce their mortality risk. This information will help us to change patient perception,” she said.
Dr. Perez-Ruiz reported relationships with Amgen, Grünenthal, and Menarini.
SOURCE: Perez-Ruiz F et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 869.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Lowering serum urate in gout patients confers a survival advantage.
Major finding: A serum urate of 6 mg/dL or more in gout patients was independently associated with a 139% increased risk of all-cause mortality.
Study details: This was a prospective study of 1,193 gout patients followed for an average of 4 years.
Disclosures: Dr. Perez-Ruiz reported relationships with Amgen, Grünenthal, and Menarini.
Source: Perez-Ruiz F et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 869.
Symptomatic hyperuricemia may respond to urate-lowering therapy
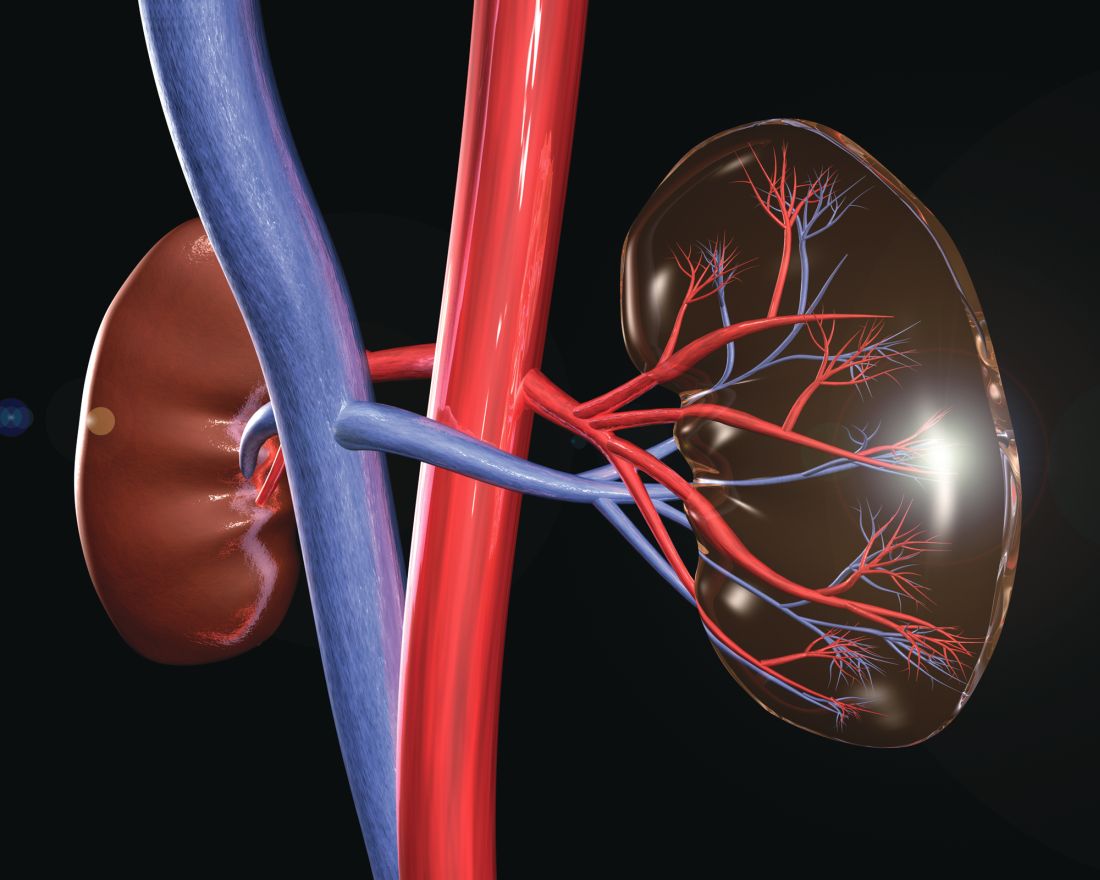
Persistent and nonepisodic foot pain in hyperuricemia is associated with ultrasound features of monosodium urate deposition within joints that is responsive to urate-lowering therapy, a case-control study shows.
, reported Yousef Mohammed Alammari, of the department of rheumatology, Tallaght University Hospital, Dublin, and associates.
Furthermore, the researchers wrote in Annals of the Rheumatic Diseases, their findings serve as “potential rationale” for reclassification of the ACR/EULAR 2015 gout classification criteria.
The research team noted that the gout classification criteria from the two rheumatology organizations require a history of a “prior episode of swelling, pain, or tenderness of a peripheral joint/bursa before confirmation either through MSU crystal identification in synovial fluid or through achieving a score of greater than 8 using a predefined scoring system of radiological, laboratory, and clinical features.”
Yet, emerging evidence suggests that foot pain could be a preclinical and clinical phase of gout that might occur prior to a first episodic gout attack, the investigators noted.
The current study involved 16 hyperuricemia individuals with persistent, nonepisodic foot pain who did not fulfill ACR/EULAR 2015 gout classification criteria but received febuxostat 80 mg once daily for 3 months. Controls were 15 individuals with asymptomatic hyperuricemia.
Results showed that double contour sign erosion and tophus occurred in 44%, 37%, and 37% of the cases, respectively, whereas no ultrasound features of gout were seen in the controls.
No significant difference in baseline serum urate was observed between the cases (450 plus or minus 18 mg/dL) and controls (426 plus or minus 7; P = nonsignificant), but at 1- and 3-month time points, serum urate fell in the cases (200 plus or minus 18; P less than 0.001 and 223 plus or minus 28; P less than less than 0.001).
In the cases, baseline 24-hour pain visual analogue score (65 plus or minus 4.9) reduced at 1 month (41 plus or minus 6.6; P = 0.001) and 3 months (33 plus or minus 7.2; P less than 0.001) of urate lowering therapy, as did the 7-day pain visual analogue score (70 plus or minus 4.7) scores (44 plus or minus 7.1; P less than 0.001 at 1 month; 38 plus or minus 8; P less than 0.001 at 3 months).
The Manchester Foot Pain and Disability Index also decreased at 1 month (21 plus or minus 2.9; P = 0.019) and 3 months (17 plus or minus 2.8; P = 0.012).
When the investigators grouped the cases according to the presence (n = 7) or absence (n = 9) of double contour sign on baseline ultrasound, no differences were observed for baseline pain scores.
However, after treatment with ultrasound, 24-hour pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months.
In addition, the researchers found, the 7-day pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months. No significant differences were seen between double contour positive and double contour negative patients in the Manchester Foot Pain and Disability Index or serum urate at 1 or 3 months of ultrasound.
The investigators noted that their findings indicated that persistent, nonepisodic foot pain in hyperuricemia was both associated with ultrasound features of monosodium urate deposition and was responsive to urate lowering therapy.
“Symptomatic hyperuricemia occurring prior to episodic gout therefore represents an earlier or alternative disease presentation,” they wrote. “Changes to the ACR/ EULAR classification criteria to include nonepisodic foot pain in the presence of [ultrasound] features of gout may increase the sensitivity of disease classification at an early stage, leading to improved future treatment strategies and long-term outcomes.”
No disclosures were declared.
SOURCE: Alammari YM et al. Ann Rheum Dis. 2018. doi: 10.1136/annrheumdis-2018-214305.
Persistent and nonepisodic foot pain in hyperuricemia is associated with ultrasound features of monosodium urate deposition within joints that is responsive to urate-lowering therapy, a case-control study shows.
, reported Yousef Mohammed Alammari, of the department of rheumatology, Tallaght University Hospital, Dublin, and associates.
Furthermore, the researchers wrote in Annals of the Rheumatic Diseases, their findings serve as “potential rationale” for reclassification of the ACR/EULAR 2015 gout classification criteria.
The research team noted that the gout classification criteria from the two rheumatology organizations require a history of a “prior episode of swelling, pain, or tenderness of a peripheral joint/bursa before confirmation either through MSU crystal identification in synovial fluid or through achieving a score of greater than 8 using a predefined scoring system of radiological, laboratory, and clinical features.”
Yet, emerging evidence suggests that foot pain could be a preclinical and clinical phase of gout that might occur prior to a first episodic gout attack, the investigators noted.
The current study involved 16 hyperuricemia individuals with persistent, nonepisodic foot pain who did not fulfill ACR/EULAR 2015 gout classification criteria but received febuxostat 80 mg once daily for 3 months. Controls were 15 individuals with asymptomatic hyperuricemia.
Results showed that double contour sign erosion and tophus occurred in 44%, 37%, and 37% of the cases, respectively, whereas no ultrasound features of gout were seen in the controls.
No significant difference in baseline serum urate was observed between the cases (450 plus or minus 18 mg/dL) and controls (426 plus or minus 7; P = nonsignificant), but at 1- and 3-month time points, serum urate fell in the cases (200 plus or minus 18; P less than 0.001 and 223 plus or minus 28; P less than less than 0.001).
In the cases, baseline 24-hour pain visual analogue score (65 plus or minus 4.9) reduced at 1 month (41 plus or minus 6.6; P = 0.001) and 3 months (33 plus or minus 7.2; P less than 0.001) of urate lowering therapy, as did the 7-day pain visual analogue score (70 plus or minus 4.7) scores (44 plus or minus 7.1; P less than 0.001 at 1 month; 38 plus or minus 8; P less than 0.001 at 3 months).
The Manchester Foot Pain and Disability Index also decreased at 1 month (21 plus or minus 2.9; P = 0.019) and 3 months (17 plus or minus 2.8; P = 0.012).
When the investigators grouped the cases according to the presence (n = 7) or absence (n = 9) of double contour sign on baseline ultrasound, no differences were observed for baseline pain scores.
However, after treatment with ultrasound, 24-hour pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months.
In addition, the researchers found, the 7-day pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months. No significant differences were seen between double contour positive and double contour negative patients in the Manchester Foot Pain and Disability Index or serum urate at 1 or 3 months of ultrasound.
The investigators noted that their findings indicated that persistent, nonepisodic foot pain in hyperuricemia was both associated with ultrasound features of monosodium urate deposition and was responsive to urate lowering therapy.
“Symptomatic hyperuricemia occurring prior to episodic gout therefore represents an earlier or alternative disease presentation,” they wrote. “Changes to the ACR/ EULAR classification criteria to include nonepisodic foot pain in the presence of [ultrasound] features of gout may increase the sensitivity of disease classification at an early stage, leading to improved future treatment strategies and long-term outcomes.”
No disclosures were declared.
SOURCE: Alammari YM et al. Ann Rheum Dis. 2018. doi: 10.1136/annrheumdis-2018-214305.
Persistent and nonepisodic foot pain in hyperuricemia is associated with ultrasound features of monosodium urate deposition within joints that is responsive to urate-lowering therapy, a case-control study shows.
, reported Yousef Mohammed Alammari, of the department of rheumatology, Tallaght University Hospital, Dublin, and associates.
Furthermore, the researchers wrote in Annals of the Rheumatic Diseases, their findings serve as “potential rationale” for reclassification of the ACR/EULAR 2015 gout classification criteria.
The research team noted that the gout classification criteria from the two rheumatology organizations require a history of a “prior episode of swelling, pain, or tenderness of a peripheral joint/bursa before confirmation either through MSU crystal identification in synovial fluid or through achieving a score of greater than 8 using a predefined scoring system of radiological, laboratory, and clinical features.”
Yet, emerging evidence suggests that foot pain could be a preclinical and clinical phase of gout that might occur prior to a first episodic gout attack, the investigators noted.
The current study involved 16 hyperuricemia individuals with persistent, nonepisodic foot pain who did not fulfill ACR/EULAR 2015 gout classification criteria but received febuxostat 80 mg once daily for 3 months. Controls were 15 individuals with asymptomatic hyperuricemia.
Results showed that double contour sign erosion and tophus occurred in 44%, 37%, and 37% of the cases, respectively, whereas no ultrasound features of gout were seen in the controls.
No significant difference in baseline serum urate was observed between the cases (450 plus or minus 18 mg/dL) and controls (426 plus or minus 7; P = nonsignificant), but at 1- and 3-month time points, serum urate fell in the cases (200 plus or minus 18; P less than 0.001 and 223 plus or minus 28; P less than less than 0.001).
In the cases, baseline 24-hour pain visual analogue score (65 plus or minus 4.9) reduced at 1 month (41 plus or minus 6.6; P = 0.001) and 3 months (33 plus or minus 7.2; P less than 0.001) of urate lowering therapy, as did the 7-day pain visual analogue score (70 plus or minus 4.7) scores (44 plus or minus 7.1; P less than 0.001 at 1 month; 38 plus or minus 8; P less than 0.001 at 3 months).
The Manchester Foot Pain and Disability Index also decreased at 1 month (21 plus or minus 2.9; P = 0.019) and 3 months (17 plus or minus 2.8; P = 0.012).
When the investigators grouped the cases according to the presence (n = 7) or absence (n = 9) of double contour sign on baseline ultrasound, no differences were observed for baseline pain scores.
However, after treatment with ultrasound, 24-hour pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months.
In addition, the researchers found, the 7-day pain visual analogue scores were significantly lower in double contour positive patients at 1 month and 3 months. No significant differences were seen between double contour positive and double contour negative patients in the Manchester Foot Pain and Disability Index or serum urate at 1 or 3 months of ultrasound.
The investigators noted that their findings indicated that persistent, nonepisodic foot pain in hyperuricemia was both associated with ultrasound features of monosodium urate deposition and was responsive to urate lowering therapy.
“Symptomatic hyperuricemia occurring prior to episodic gout therefore represents an earlier or alternative disease presentation,” they wrote. “Changes to the ACR/ EULAR classification criteria to include nonepisodic foot pain in the presence of [ultrasound] features of gout may increase the sensitivity of disease classification at an early stage, leading to improved future treatment strategies and long-term outcomes.”
No disclosures were declared.
SOURCE: Alammari YM et al. Ann Rheum Dis. 2018. doi: 10.1136/annrheumdis-2018-214305.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Persistent and nonepisodic foot pain in hyperuricemia is associated with ultrasound features of monosodium urate (MSU) deposition within joints that is responsive to urate-lowering therapy.
Major finding: Persistent, nonepisodic foot pain in hyperuricemia was both associated with ultrasound features of monosodium urate deposition and was responsive to ultrasound.
Study details: Case-control study involving 16 hyperuricemic individuals with persistent, nonepisodic foot pain who did not fulfill ACR/EULAR 2015 gout classification criteria.
Disclosures: No disclosures were declared.
Source: Alammari YM et al. Ann Rheum Dis. 2018. doi: 10.1136/annrheumdis-2018-214305.
Genes found more important than diet in hyperuricemia
CHICAGO – Diet plays a significantly less important role than genes in the development of high serum urate levels that typically precede gout, research from New Zealand has revealed.
These findings stem from a first-ever systematic analysis of a large data set to “determine the relative contributions of inherited genetic variants and overall diet to variance in serum urate concentrations,” Tanya J. Major, PhD, of the University of Otago in Dunedin, New Zealand, and her colleagues first reported in The BMJ and then less than 2 weeks later at the annual meeting of the American College of Rheumatology.
Prior studies have estimated that genetic factors explain 25%-60% of the variability in serum urate levels, but diet also has long been considered a risk factor for gout, with certain diets such as the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean diet shown in studies to reduce serum urate levels and the risk of gout, the researchers noted.
The new study found that common genetic factors accounted for nearly 24% of the variation in serum urate levels, whereas diet accounted for less than 1%.
Before these findings, the impact of diet on hyperuricemia was known to be limited, but that doesn’t mean that diet is meaningless, Michael H. Pillinger, MD, who was not involved in the study, said in an interview at the ACR annual meeting.
“What this work does from a scientific point of view is underline the genetic basis [of hyperuricemia]. What it does from a practical and clinical point of view is tell us that diet is a meaningful thing to adjust. It will provide other health benefits, but it isn’t the solution, and we know that it rarely is,” said Dr. Pillinger, professor of medicine and biochemistry and molecular pharmacology at New York University. “We shouldn’t expect a really large impact from diet, and we shouldn’t make people feel guilty about their diets, and optimally you want to manage a diet that a patient can tolerate and not one that will be impossible to sustain.”
Dr. Major had a similar message in an interview at the meeting: “By focusing on diet and treating urate levels through diet, you start to kind of get this blame element going on that the reason you’ve got gout is you’re eating the wrong foods, and so then it makes people less likely to want to go to see their doctor to start with. And then when they do try to follow their doctor’s advice about their diet, and nothing changes, then it starts to get frustrating for them as well.”
The research team analyzed dietary survey data from five U.S. cohort studies (Atherosclerosis Risk in Communities, Coronary Artery Risk Development in [Young] Adults, Cardiovascular Heart Study, Framingham Heart Study, and Third National Health and Nutrition Examination Survey [NHANES III]) that altogether included 16,760 individuals (8,414 men and 8,346 women) of European ancestry.
Participants were aged 18 years or older, did not have gout or kidney disease, and were not taking urate-lowering or diuretic drugs. Serum urate measurements, dietary survey data, and confounders such as gender, age, body mass index, smoking status, and average daily calorie intake were all recorded.
The results showed that 15 foods were significantly associated with serum urate levels. Six were established urate-modifying foods: beer, liquor, wine, soft drinks, skim milk, and meat (beef, pork, or lamb). The remaining nine foods included two less established urate-modifying foods (cheese and noncitrus fruit) and seven food items without established associations: poultry, potatoes, brown bread, peanuts, margarine, cold cereal, and eggs.
Beer and liquor had the strongest urate-raising effect, associated with a 1.38 micromol/L increase in serum urate per serving per week, equating to a 9.66 micromol/L (0.16 mg/dL) increase per daily serving.
The authors noted that the associations seen with known and confirmed serum urate–influencing foods were consistent with previously reported associations in terms of effect and magnitude. Nevertheless, they noted that “each of these established foods explained less than 1% of variation in serum urate levels within the full cohort.”
When the researchers analyzed the data according to three diet scores based on healthy diet guidelines, they found that diet explained “very little variance in serum urate levels (0.28% for the DASH diet, 0.15% for the Healthy Eating diet, 0.06% for the Mediterranean diet, and 0.16% for the data-driven diet pattern).”
However, they noted that even though their findings, along with previous research, suggest that a clinically relevant decrease in serum urate levels could be achieved with the DASH diet, the implementation of such a diet might not be “straightforward” because “the barriers to implementing this diet both at a population level and in a primary care setting are yet to be overcome.”
In contrast, when the research team looked at genes in the cohort they found that common genetic factors explained 23.9% of variation in serum urate levels in the full cohort (excluding the NHANES III study because of a lack of genotype data).
Baseline visit diet information for these cohort studies ranged from the mid-1980s to the early to mid-2000s, making it hard to account for changes in food composition over time. Dr. Major said that food compositions overall were likely to be more processed over time and contain more urate-raising foods. However, any effects of food composition changes on urate levels over time would be more likely be felt at the level of individual food products, not on diets overall, she said.
The variability in the diet scores that the investigators noted across individuals and regions in these U.S. cohort studies did not appear to affect the results, Dr. Major noted. Furthermore, adjustment within models for these diet scores did not affect the degree of variation in urate levels that genetics accounted for, whereas adjustment for genetics lowered the amount of variation that diet contributed to urate levels.
The findings also don’t have any say on the relative contribution of diet versus genetics on gout flares, which is a separate issue. Many patients would agree that they suspect certain foods trigger gout flares even if they don’t affect baseline urate levels very much, Dr. Pillinger said.
The next steps for Dr. Major and her coinvestigators may be to see if diet is influencing urate levels to the same degree in people with gout as this study shows for the general population, she said.The investigators noted that the use of different food questionnaires between the five studies is one limitation of the analysis, and there should be some caution in generalizing the results to people with gout or those of non-European ancestry.
The study was supported by the Health Research Council of New Zealand and the University of Otago. One author reported receiving consulting and speaker fees or grants from several pharmaceutical companies that manufacture urate-lowering drugs.
This article was updated 10/25/18.
SOURCE: Major TJ et al. BMJ. 2018. doi: 10.1136/bmj.k3951.
People with gout are often stigmatized by society because of the common misconception that the condition is caused by an unhealthy diet and lifestyle. This well-established and harmful view, which also exists among health professionals and the media, can stop people from seeking help for their condition, which means opportunities to initiate treatment can be missed.
The study by Major et al. provides valuable evidence that a considerable part of a person’s predisposition to high serum urate levels, and therefore gout, is not modifiable. It should be noted, however, that the findings do not provide evidence to support a change in current guidelines, which recommend that people with gout adopt a diet that avoids excessive consumption of high-risk foods.
Nevertheless, the findings have broad implications for both people with gout and the health professionals who care for them. They provide a welcome opportunity to address these serious barriers to treatment and reduce the burden associated with what is a common and easily treatable condition.
While the authors caution against extending their findings to people with clinically diagnosed gout, it is unlikely that the causes of hyperuricemia in this patient population are different from those studied in patients with gout.
Lorraine Watson and Edward Roddy, DM, are affiliated with Arthritis Research UK Primary Care Centre at Keele University, Staffordshire, England. These comments are adapted from their accompanying editorial (BMJ. 2018. doi: 10.1136/bmj.k4140). They declared no relevant conflicts of interest.
People with gout are often stigmatized by society because of the common misconception that the condition is caused by an unhealthy diet and lifestyle. This well-established and harmful view, which also exists among health professionals and the media, can stop people from seeking help for their condition, which means opportunities to initiate treatment can be missed.
The study by Major et al. provides valuable evidence that a considerable part of a person’s predisposition to high serum urate levels, and therefore gout, is not modifiable. It should be noted, however, that the findings do not provide evidence to support a change in current guidelines, which recommend that people with gout adopt a diet that avoids excessive consumption of high-risk foods.
Nevertheless, the findings have broad implications for both people with gout and the health professionals who care for them. They provide a welcome opportunity to address these serious barriers to treatment and reduce the burden associated with what is a common and easily treatable condition.
While the authors caution against extending their findings to people with clinically diagnosed gout, it is unlikely that the causes of hyperuricemia in this patient population are different from those studied in patients with gout.
Lorraine Watson and Edward Roddy, DM, are affiliated with Arthritis Research UK Primary Care Centre at Keele University, Staffordshire, England. These comments are adapted from their accompanying editorial (BMJ. 2018. doi: 10.1136/bmj.k4140). They declared no relevant conflicts of interest.
People with gout are often stigmatized by society because of the common misconception that the condition is caused by an unhealthy diet and lifestyle. This well-established and harmful view, which also exists among health professionals and the media, can stop people from seeking help for their condition, which means opportunities to initiate treatment can be missed.
The study by Major et al. provides valuable evidence that a considerable part of a person’s predisposition to high serum urate levels, and therefore gout, is not modifiable. It should be noted, however, that the findings do not provide evidence to support a change in current guidelines, which recommend that people with gout adopt a diet that avoids excessive consumption of high-risk foods.
Nevertheless, the findings have broad implications for both people with gout and the health professionals who care for them. They provide a welcome opportunity to address these serious barriers to treatment and reduce the burden associated with what is a common and easily treatable condition.
While the authors caution against extending their findings to people with clinically diagnosed gout, it is unlikely that the causes of hyperuricemia in this patient population are different from those studied in patients with gout.
Lorraine Watson and Edward Roddy, DM, are affiliated with Arthritis Research UK Primary Care Centre at Keele University, Staffordshire, England. These comments are adapted from their accompanying editorial (BMJ. 2018. doi: 10.1136/bmj.k4140). They declared no relevant conflicts of interest.
CHICAGO – Diet plays a significantly less important role than genes in the development of high serum urate levels that typically precede gout, research from New Zealand has revealed.
These findings stem from a first-ever systematic analysis of a large data set to “determine the relative contributions of inherited genetic variants and overall diet to variance in serum urate concentrations,” Tanya J. Major, PhD, of the University of Otago in Dunedin, New Zealand, and her colleagues first reported in The BMJ and then less than 2 weeks later at the annual meeting of the American College of Rheumatology.
Prior studies have estimated that genetic factors explain 25%-60% of the variability in serum urate levels, but diet also has long been considered a risk factor for gout, with certain diets such as the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean diet shown in studies to reduce serum urate levels and the risk of gout, the researchers noted.
The new study found that common genetic factors accounted for nearly 24% of the variation in serum urate levels, whereas diet accounted for less than 1%.
Before these findings, the impact of diet on hyperuricemia was known to be limited, but that doesn’t mean that diet is meaningless, Michael H. Pillinger, MD, who was not involved in the study, said in an interview at the ACR annual meeting.
“What this work does from a scientific point of view is underline the genetic basis [of hyperuricemia]. What it does from a practical and clinical point of view is tell us that diet is a meaningful thing to adjust. It will provide other health benefits, but it isn’t the solution, and we know that it rarely is,” said Dr. Pillinger, professor of medicine and biochemistry and molecular pharmacology at New York University. “We shouldn’t expect a really large impact from diet, and we shouldn’t make people feel guilty about their diets, and optimally you want to manage a diet that a patient can tolerate and not one that will be impossible to sustain.”
Dr. Major had a similar message in an interview at the meeting: “By focusing on diet and treating urate levels through diet, you start to kind of get this blame element going on that the reason you’ve got gout is you’re eating the wrong foods, and so then it makes people less likely to want to go to see their doctor to start with. And then when they do try to follow their doctor’s advice about their diet, and nothing changes, then it starts to get frustrating for them as well.”
The research team analyzed dietary survey data from five U.S. cohort studies (Atherosclerosis Risk in Communities, Coronary Artery Risk Development in [Young] Adults, Cardiovascular Heart Study, Framingham Heart Study, and Third National Health and Nutrition Examination Survey [NHANES III]) that altogether included 16,760 individuals (8,414 men and 8,346 women) of European ancestry.
Participants were aged 18 years or older, did not have gout or kidney disease, and were not taking urate-lowering or diuretic drugs. Serum urate measurements, dietary survey data, and confounders such as gender, age, body mass index, smoking status, and average daily calorie intake were all recorded.
The results showed that 15 foods were significantly associated with serum urate levels. Six were established urate-modifying foods: beer, liquor, wine, soft drinks, skim milk, and meat (beef, pork, or lamb). The remaining nine foods included two less established urate-modifying foods (cheese and noncitrus fruit) and seven food items without established associations: poultry, potatoes, brown bread, peanuts, margarine, cold cereal, and eggs.
Beer and liquor had the strongest urate-raising effect, associated with a 1.38 micromol/L increase in serum urate per serving per week, equating to a 9.66 micromol/L (0.16 mg/dL) increase per daily serving.
The authors noted that the associations seen with known and confirmed serum urate–influencing foods were consistent with previously reported associations in terms of effect and magnitude. Nevertheless, they noted that “each of these established foods explained less than 1% of variation in serum urate levels within the full cohort.”
When the researchers analyzed the data according to three diet scores based on healthy diet guidelines, they found that diet explained “very little variance in serum urate levels (0.28% for the DASH diet, 0.15% for the Healthy Eating diet, 0.06% for the Mediterranean diet, and 0.16% for the data-driven diet pattern).”
However, they noted that even though their findings, along with previous research, suggest that a clinically relevant decrease in serum urate levels could be achieved with the DASH diet, the implementation of such a diet might not be “straightforward” because “the barriers to implementing this diet both at a population level and in a primary care setting are yet to be overcome.”
In contrast, when the research team looked at genes in the cohort they found that common genetic factors explained 23.9% of variation in serum urate levels in the full cohort (excluding the NHANES III study because of a lack of genotype data).
Baseline visit diet information for these cohort studies ranged from the mid-1980s to the early to mid-2000s, making it hard to account for changes in food composition over time. Dr. Major said that food compositions overall were likely to be more processed over time and contain more urate-raising foods. However, any effects of food composition changes on urate levels over time would be more likely be felt at the level of individual food products, not on diets overall, she said.
The variability in the diet scores that the investigators noted across individuals and regions in these U.S. cohort studies did not appear to affect the results, Dr. Major noted. Furthermore, adjustment within models for these diet scores did not affect the degree of variation in urate levels that genetics accounted for, whereas adjustment for genetics lowered the amount of variation that diet contributed to urate levels.
The findings also don’t have any say on the relative contribution of diet versus genetics on gout flares, which is a separate issue. Many patients would agree that they suspect certain foods trigger gout flares even if they don’t affect baseline urate levels very much, Dr. Pillinger said.
The next steps for Dr. Major and her coinvestigators may be to see if diet is influencing urate levels to the same degree in people with gout as this study shows for the general population, she said.The investigators noted that the use of different food questionnaires between the five studies is one limitation of the analysis, and there should be some caution in generalizing the results to people with gout or those of non-European ancestry.
The study was supported by the Health Research Council of New Zealand and the University of Otago. One author reported receiving consulting and speaker fees or grants from several pharmaceutical companies that manufacture urate-lowering drugs.
This article was updated 10/25/18.
SOURCE: Major TJ et al. BMJ. 2018. doi: 10.1136/bmj.k3951.
CHICAGO – Diet plays a significantly less important role than genes in the development of high serum urate levels that typically precede gout, research from New Zealand has revealed.
These findings stem from a first-ever systematic analysis of a large data set to “determine the relative contributions of inherited genetic variants and overall diet to variance in serum urate concentrations,” Tanya J. Major, PhD, of the University of Otago in Dunedin, New Zealand, and her colleagues first reported in The BMJ and then less than 2 weeks later at the annual meeting of the American College of Rheumatology.
Prior studies have estimated that genetic factors explain 25%-60% of the variability in serum urate levels, but diet also has long been considered a risk factor for gout, with certain diets such as the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean diet shown in studies to reduce serum urate levels and the risk of gout, the researchers noted.
The new study found that common genetic factors accounted for nearly 24% of the variation in serum urate levels, whereas diet accounted for less than 1%.
Before these findings, the impact of diet on hyperuricemia was known to be limited, but that doesn’t mean that diet is meaningless, Michael H. Pillinger, MD, who was not involved in the study, said in an interview at the ACR annual meeting.
“What this work does from a scientific point of view is underline the genetic basis [of hyperuricemia]. What it does from a practical and clinical point of view is tell us that diet is a meaningful thing to adjust. It will provide other health benefits, but it isn’t the solution, and we know that it rarely is,” said Dr. Pillinger, professor of medicine and biochemistry and molecular pharmacology at New York University. “We shouldn’t expect a really large impact from diet, and we shouldn’t make people feel guilty about their diets, and optimally you want to manage a diet that a patient can tolerate and not one that will be impossible to sustain.”
Dr. Major had a similar message in an interview at the meeting: “By focusing on diet and treating urate levels through diet, you start to kind of get this blame element going on that the reason you’ve got gout is you’re eating the wrong foods, and so then it makes people less likely to want to go to see their doctor to start with. And then when they do try to follow their doctor’s advice about their diet, and nothing changes, then it starts to get frustrating for them as well.”
The research team analyzed dietary survey data from five U.S. cohort studies (Atherosclerosis Risk in Communities, Coronary Artery Risk Development in [Young] Adults, Cardiovascular Heart Study, Framingham Heart Study, and Third National Health and Nutrition Examination Survey [NHANES III]) that altogether included 16,760 individuals (8,414 men and 8,346 women) of European ancestry.
Participants were aged 18 years or older, did not have gout or kidney disease, and were not taking urate-lowering or diuretic drugs. Serum urate measurements, dietary survey data, and confounders such as gender, age, body mass index, smoking status, and average daily calorie intake were all recorded.
The results showed that 15 foods were significantly associated with serum urate levels. Six were established urate-modifying foods: beer, liquor, wine, soft drinks, skim milk, and meat (beef, pork, or lamb). The remaining nine foods included two less established urate-modifying foods (cheese and noncitrus fruit) and seven food items without established associations: poultry, potatoes, brown bread, peanuts, margarine, cold cereal, and eggs.
Beer and liquor had the strongest urate-raising effect, associated with a 1.38 micromol/L increase in serum urate per serving per week, equating to a 9.66 micromol/L (0.16 mg/dL) increase per daily serving.
The authors noted that the associations seen with known and confirmed serum urate–influencing foods were consistent with previously reported associations in terms of effect and magnitude. Nevertheless, they noted that “each of these established foods explained less than 1% of variation in serum urate levels within the full cohort.”
When the researchers analyzed the data according to three diet scores based on healthy diet guidelines, they found that diet explained “very little variance in serum urate levels (0.28% for the DASH diet, 0.15% for the Healthy Eating diet, 0.06% for the Mediterranean diet, and 0.16% for the data-driven diet pattern).”
However, they noted that even though their findings, along with previous research, suggest that a clinically relevant decrease in serum urate levels could be achieved with the DASH diet, the implementation of such a diet might not be “straightforward” because “the barriers to implementing this diet both at a population level and in a primary care setting are yet to be overcome.”
In contrast, when the research team looked at genes in the cohort they found that common genetic factors explained 23.9% of variation in serum urate levels in the full cohort (excluding the NHANES III study because of a lack of genotype data).
Baseline visit diet information for these cohort studies ranged from the mid-1980s to the early to mid-2000s, making it hard to account for changes in food composition over time. Dr. Major said that food compositions overall were likely to be more processed over time and contain more urate-raising foods. However, any effects of food composition changes on urate levels over time would be more likely be felt at the level of individual food products, not on diets overall, she said.
The variability in the diet scores that the investigators noted across individuals and regions in these U.S. cohort studies did not appear to affect the results, Dr. Major noted. Furthermore, adjustment within models for these diet scores did not affect the degree of variation in urate levels that genetics accounted for, whereas adjustment for genetics lowered the amount of variation that diet contributed to urate levels.
The findings also don’t have any say on the relative contribution of diet versus genetics on gout flares, which is a separate issue. Many patients would agree that they suspect certain foods trigger gout flares even if they don’t affect baseline urate levels very much, Dr. Pillinger said.
The next steps for Dr. Major and her coinvestigators may be to see if diet is influencing urate levels to the same degree in people with gout as this study shows for the general population, she said.The investigators noted that the use of different food questionnaires between the five studies is one limitation of the analysis, and there should be some caution in generalizing the results to people with gout or those of non-European ancestry.
The study was supported by the Health Research Council of New Zealand and the University of Otago. One author reported receiving consulting and speaker fees or grants from several pharmaceutical companies that manufacture urate-lowering drugs.
This article was updated 10/25/18.
SOURCE: Major TJ et al. BMJ. 2018. doi: 10.1136/bmj.k3951.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point:
Major finding: Diet explained less than 1% of variation in urate levels, whereas common genetic factors explained 23.9% of the variation in urate levels.
Study details: A meta-analysis of five U.S. cohort studies that included dietary survey data from 16,760 people of European ancestry.
Disclosures: The study was supported by the Health Research Council of New Zealand and the University of Otago. One author reported receiving consulting and speaker fees or grants from several pharmaceutical companies that manufacture urate-lowering drugs.
Source: Major T et al. BMJ. 2018. doi: 10.1136/bmj.k3951.
Allopurinol reduces risk of renal decline in gout patients
In patients with gout, at least 300 mg of allopurinol daily may reduce the risk of renal function decline, according to a new study.
Since no evidence supports allopurinol nephrotoxicity and usage does not appear to worsen chronic kidney disease (CKD), clinicians should consider other causes of declining renal function, according to lead author Ana Beatriz Vargas-Santos, MD, of the rheumatology unit at the State University of Rio de Janeiro and her colleagues.
These findings reinforce the American College of Rheumatology’s 2012 treatment recommendation that the dose of allopurinol, a urate-lowering therapy (ULT), “can be raised above 300 mg daily, even with renal impairment, as long as it is accompanied by adequate patient education and monitoring for drug toxicity may worsen renal function.”*
“Renal-dosing of allopurinol compounds the poor management of gout and adds to the perception that allopurinol may be detrimental for renal function,” the investigators wrote in JAMA Internal Medicine. “In contrast, recent studies provide support for starting allopurinol at a low dose with gradual dose escalation to serum urate target with close monitoring, even among patients with renal insufficiency, without increased risk of allopurinol hypersensitivity syndrome (AHS). Further, there is emerging evidence that ULT may be beneficial for kidney dysfunction.”
Building upon these developments, the investigators “aimed to assess the relation of allopurinol initiation to the risk of developing CKD stage 3 or higher among people with newly diagnosed gout.”
Patients for the cohort study were drawn from the Health Improvement Network (THIN), a database of records from general practitioners in the United Kingdom. Included patients were recently diagnosed with gout but did not have stage 3 or higher chronic kidney disease or ULT usage within a year prior to diagnosis. After screening, 4,760 allopurinol users were matched with 4,760 allopurinol nonusers. Overall, 71% of patients had CKD stage 2, while the remaining 29% had CKD stage 1 or normal kidney function.
The primary outcome of CKD stage 3 or higher was defined as glomerular filtration rate below 60 mL/min (recorded at least twice in 1 year with a 3-month interval between readings and GFR never exceeding 75 mL/min during the intervening period), kidney transplant, or dialysis. The mean follow-up time was 5 years for allopurinol users and 4 years for nonusers.
The investigators found that 579 allopurinol users developed CKD stage 3 or higher, compared with 623 nonusers, suggesting that allopurinol reduced risk of CKD stage 3 or higher by 13%. Allopurinol doses of at least 300 mg/day were associated with a hazard ratio of 0.87, but lower doses did not share this association (HR = 1.02).
In defense of their findings, Dr. Vargas-Santos and her associates evaluated the relevance of their study, compared with previous allopurinol studies.
“This study is one of few that have evaluated the relation of allopurinol to renal function among patients with gout and normal or near-normal kidney function at baseline,” the authors wrote, noting that most gout patients do not have severe kidney disease.
Previous studies have suggested that allopurinol worsens kidney function, but these studies were often conducted in nongout populations, with patients exhibiting CKD stage 3 or higher, they noted. Instead of allopurinol-induced kidney damage, renal decline in gout patients is likely multifactorial.
“Because people with gout have intrinsic differences compared with those with asymptomatic hyperuricemia, including higher mortality, more comorbidities, and more NSAID use, these studies’ results are not directly applicable to gout patients,” the investigators wrote.
“At minimum, allopurinol does not seem to have a detrimental effect on renal function in individuals with gout,” Dr. Vargas-Santos and her associates concluded. “Clinicians should consider evaluating other factors when faced with renal function decline in their patients with gout rather than lowering the dose of or discontinuing allopurinol, a strategy that has contributed to the ongoing suboptimal treatment of gout.”
The authors reported funding from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq); Ministry of Science, Technology and Innovation of Brazil; and National Institutes of Health. Dr Vargas-Santos has received speaking fees and support for international medical events from Grünenthal. No other disclosures were reported.
SOURCE: Vargas-Santos AB et al. JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.4463
*Correction, 11/5/2018: An earlier version of this story incorrectly stated the American College of Rheumatology’s 2012 gout treatment recommendation for using allopurinol in patients with renal impairment.
Physicians should consider the inherent limitations of observational studies before altering clinical decisions, according to Jonathan Zipursky, MD, and David N. Juurlink, MD, PhD. This is particularly important since the findings in this paper challenge the American College of Rheumatology, which recommends lower allopurinol doses in patients with chronic kidney disease (CKD).
On one hand, they noted, observational studies have some advantages over randomized trials.
“Observational studies frequently include patients who are ineligible for RCTs, and extended follow-up enables examination of outcomes that might not have arisen earlier in treatment,” Dr. Zipursky and Dr. Juurlink wrote in an editorial. “Moreover, sample sizes often greatly exceed those of RCTs, facilitating detection of less common adverse events. Consequently, population-based observational studies are critical to postmarketing surveillance and, increasingly, evidence-based prescribing recommendations.”
On the other hand, observational studies are less tightly controlled than randomized trials.
As “treatment allocation is nonrandom, it raises the possibilities of selection bias and confounding by indication,” Dr. Zipursky and Dr. Juurlink wrote. “Perhaps the drugs were preferentially prescribed to patients destined to tolerate them, or fare better in some other way apparent to prescribers but beyond the resolution of large databases. For example, of the nearly 43,000 patients in the study by Vargos-Santos et al, only 10% were started on 300 mg or more per day of allopurinol. This leaves readers to wonder what motivated practitioners to start such doses, or, conversely, what it was about the remaining 90% of patients that led them to receive lower doses of allopurinol or none at all.”
Along with these unanswered questions, the study compared treated patients to untreated ones, but “it is generally desirable to compare 1 drug with another used for the same indication, which can help mitigate the effect of unmeasured factors that might have influenced the decision to treat in the first place.”
Familiarity with observational studies is essential for clinicians, as Dr. Zipursky and Dr. Juurlink expect such trials will become more common in the future, and they provide useful insight if clinicians maintain an appropriate viewpoint.
“The findings will need to be contextualized and viewed with more skepticism than RCTs,” they wrote, “but in some instances, they can be thoughtfully integrated into our treatment decisions.”
Dr. Zipursky and Dr. Juurlink are with the department of medicine at Sunnybrook Health Sciences Centre, Toronto. These comments are adapted from their accompanying editorial (JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.5766).
Physicians should consider the inherent limitations of observational studies before altering clinical decisions, according to Jonathan Zipursky, MD, and David N. Juurlink, MD, PhD. This is particularly important since the findings in this paper challenge the American College of Rheumatology, which recommends lower allopurinol doses in patients with chronic kidney disease (CKD).
On one hand, they noted, observational studies have some advantages over randomized trials.
“Observational studies frequently include patients who are ineligible for RCTs, and extended follow-up enables examination of outcomes that might not have arisen earlier in treatment,” Dr. Zipursky and Dr. Juurlink wrote in an editorial. “Moreover, sample sizes often greatly exceed those of RCTs, facilitating detection of less common adverse events. Consequently, population-based observational studies are critical to postmarketing surveillance and, increasingly, evidence-based prescribing recommendations.”
On the other hand, observational studies are less tightly controlled than randomized trials.
As “treatment allocation is nonrandom, it raises the possibilities of selection bias and confounding by indication,” Dr. Zipursky and Dr. Juurlink wrote. “Perhaps the drugs were preferentially prescribed to patients destined to tolerate them, or fare better in some other way apparent to prescribers but beyond the resolution of large databases. For example, of the nearly 43,000 patients in the study by Vargos-Santos et al, only 10% were started on 300 mg or more per day of allopurinol. This leaves readers to wonder what motivated practitioners to start such doses, or, conversely, what it was about the remaining 90% of patients that led them to receive lower doses of allopurinol or none at all.”
Along with these unanswered questions, the study compared treated patients to untreated ones, but “it is generally desirable to compare 1 drug with another used for the same indication, which can help mitigate the effect of unmeasured factors that might have influenced the decision to treat in the first place.”
Familiarity with observational studies is essential for clinicians, as Dr. Zipursky and Dr. Juurlink expect such trials will become more common in the future, and they provide useful insight if clinicians maintain an appropriate viewpoint.
“The findings will need to be contextualized and viewed with more skepticism than RCTs,” they wrote, “but in some instances, they can be thoughtfully integrated into our treatment decisions.”
Dr. Zipursky and Dr. Juurlink are with the department of medicine at Sunnybrook Health Sciences Centre, Toronto. These comments are adapted from their accompanying editorial (JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.5766).
Physicians should consider the inherent limitations of observational studies before altering clinical decisions, according to Jonathan Zipursky, MD, and David N. Juurlink, MD, PhD. This is particularly important since the findings in this paper challenge the American College of Rheumatology, which recommends lower allopurinol doses in patients with chronic kidney disease (CKD).
On one hand, they noted, observational studies have some advantages over randomized trials.
“Observational studies frequently include patients who are ineligible for RCTs, and extended follow-up enables examination of outcomes that might not have arisen earlier in treatment,” Dr. Zipursky and Dr. Juurlink wrote in an editorial. “Moreover, sample sizes often greatly exceed those of RCTs, facilitating detection of less common adverse events. Consequently, population-based observational studies are critical to postmarketing surveillance and, increasingly, evidence-based prescribing recommendations.”
On the other hand, observational studies are less tightly controlled than randomized trials.
As “treatment allocation is nonrandom, it raises the possibilities of selection bias and confounding by indication,” Dr. Zipursky and Dr. Juurlink wrote. “Perhaps the drugs were preferentially prescribed to patients destined to tolerate them, or fare better in some other way apparent to prescribers but beyond the resolution of large databases. For example, of the nearly 43,000 patients in the study by Vargos-Santos et al, only 10% were started on 300 mg or more per day of allopurinol. This leaves readers to wonder what motivated practitioners to start such doses, or, conversely, what it was about the remaining 90% of patients that led them to receive lower doses of allopurinol or none at all.”
Along with these unanswered questions, the study compared treated patients to untreated ones, but “it is generally desirable to compare 1 drug with another used for the same indication, which can help mitigate the effect of unmeasured factors that might have influenced the decision to treat in the first place.”
Familiarity with observational studies is essential for clinicians, as Dr. Zipursky and Dr. Juurlink expect such trials will become more common in the future, and they provide useful insight if clinicians maintain an appropriate viewpoint.
“The findings will need to be contextualized and viewed with more skepticism than RCTs,” they wrote, “but in some instances, they can be thoughtfully integrated into our treatment decisions.”
Dr. Zipursky and Dr. Juurlink are with the department of medicine at Sunnybrook Health Sciences Centre, Toronto. These comments are adapted from their accompanying editorial (JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.5766).
In patients with gout, at least 300 mg of allopurinol daily may reduce the risk of renal function decline, according to a new study.
Since no evidence supports allopurinol nephrotoxicity and usage does not appear to worsen chronic kidney disease (CKD), clinicians should consider other causes of declining renal function, according to lead author Ana Beatriz Vargas-Santos, MD, of the rheumatology unit at the State University of Rio de Janeiro and her colleagues.
These findings reinforce the American College of Rheumatology’s 2012 treatment recommendation that the dose of allopurinol, a urate-lowering therapy (ULT), “can be raised above 300 mg daily, even with renal impairment, as long as it is accompanied by adequate patient education and monitoring for drug toxicity may worsen renal function.”*
“Renal-dosing of allopurinol compounds the poor management of gout and adds to the perception that allopurinol may be detrimental for renal function,” the investigators wrote in JAMA Internal Medicine. “In contrast, recent studies provide support for starting allopurinol at a low dose with gradual dose escalation to serum urate target with close monitoring, even among patients with renal insufficiency, without increased risk of allopurinol hypersensitivity syndrome (AHS). Further, there is emerging evidence that ULT may be beneficial for kidney dysfunction.”
Building upon these developments, the investigators “aimed to assess the relation of allopurinol initiation to the risk of developing CKD stage 3 or higher among people with newly diagnosed gout.”
Patients for the cohort study were drawn from the Health Improvement Network (THIN), a database of records from general practitioners in the United Kingdom. Included patients were recently diagnosed with gout but did not have stage 3 or higher chronic kidney disease or ULT usage within a year prior to diagnosis. After screening, 4,760 allopurinol users were matched with 4,760 allopurinol nonusers. Overall, 71% of patients had CKD stage 2, while the remaining 29% had CKD stage 1 or normal kidney function.
The primary outcome of CKD stage 3 or higher was defined as glomerular filtration rate below 60 mL/min (recorded at least twice in 1 year with a 3-month interval between readings and GFR never exceeding 75 mL/min during the intervening period), kidney transplant, or dialysis. The mean follow-up time was 5 years for allopurinol users and 4 years for nonusers.
The investigators found that 579 allopurinol users developed CKD stage 3 or higher, compared with 623 nonusers, suggesting that allopurinol reduced risk of CKD stage 3 or higher by 13%. Allopurinol doses of at least 300 mg/day were associated with a hazard ratio of 0.87, but lower doses did not share this association (HR = 1.02).
In defense of their findings, Dr. Vargas-Santos and her associates evaluated the relevance of their study, compared with previous allopurinol studies.
“This study is one of few that have evaluated the relation of allopurinol to renal function among patients with gout and normal or near-normal kidney function at baseline,” the authors wrote, noting that most gout patients do not have severe kidney disease.
Previous studies have suggested that allopurinol worsens kidney function, but these studies were often conducted in nongout populations, with patients exhibiting CKD stage 3 or higher, they noted. Instead of allopurinol-induced kidney damage, renal decline in gout patients is likely multifactorial.
“Because people with gout have intrinsic differences compared with those with asymptomatic hyperuricemia, including higher mortality, more comorbidities, and more NSAID use, these studies’ results are not directly applicable to gout patients,” the investigators wrote.
“At minimum, allopurinol does not seem to have a detrimental effect on renal function in individuals with gout,” Dr. Vargas-Santos and her associates concluded. “Clinicians should consider evaluating other factors when faced with renal function decline in their patients with gout rather than lowering the dose of or discontinuing allopurinol, a strategy that has contributed to the ongoing suboptimal treatment of gout.”
The authors reported funding from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq); Ministry of Science, Technology and Innovation of Brazil; and National Institutes of Health. Dr Vargas-Santos has received speaking fees and support for international medical events from Grünenthal. No other disclosures were reported.
SOURCE: Vargas-Santos AB et al. JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.4463
*Correction, 11/5/2018: An earlier version of this story incorrectly stated the American College of Rheumatology’s 2012 gout treatment recommendation for using allopurinol in patients with renal impairment.
In patients with gout, at least 300 mg of allopurinol daily may reduce the risk of renal function decline, according to a new study.
Since no evidence supports allopurinol nephrotoxicity and usage does not appear to worsen chronic kidney disease (CKD), clinicians should consider other causes of declining renal function, according to lead author Ana Beatriz Vargas-Santos, MD, of the rheumatology unit at the State University of Rio de Janeiro and her colleagues.
These findings reinforce the American College of Rheumatology’s 2012 treatment recommendation that the dose of allopurinol, a urate-lowering therapy (ULT), “can be raised above 300 mg daily, even with renal impairment, as long as it is accompanied by adequate patient education and monitoring for drug toxicity may worsen renal function.”*
“Renal-dosing of allopurinol compounds the poor management of gout and adds to the perception that allopurinol may be detrimental for renal function,” the investigators wrote in JAMA Internal Medicine. “In contrast, recent studies provide support for starting allopurinol at a low dose with gradual dose escalation to serum urate target with close monitoring, even among patients with renal insufficiency, without increased risk of allopurinol hypersensitivity syndrome (AHS). Further, there is emerging evidence that ULT may be beneficial for kidney dysfunction.”
Building upon these developments, the investigators “aimed to assess the relation of allopurinol initiation to the risk of developing CKD stage 3 or higher among people with newly diagnosed gout.”
Patients for the cohort study were drawn from the Health Improvement Network (THIN), a database of records from general practitioners in the United Kingdom. Included patients were recently diagnosed with gout but did not have stage 3 or higher chronic kidney disease or ULT usage within a year prior to diagnosis. After screening, 4,760 allopurinol users were matched with 4,760 allopurinol nonusers. Overall, 71% of patients had CKD stage 2, while the remaining 29% had CKD stage 1 or normal kidney function.
The primary outcome of CKD stage 3 or higher was defined as glomerular filtration rate below 60 mL/min (recorded at least twice in 1 year with a 3-month interval between readings and GFR never exceeding 75 mL/min during the intervening period), kidney transplant, or dialysis. The mean follow-up time was 5 years for allopurinol users and 4 years for nonusers.
The investigators found that 579 allopurinol users developed CKD stage 3 or higher, compared with 623 nonusers, suggesting that allopurinol reduced risk of CKD stage 3 or higher by 13%. Allopurinol doses of at least 300 mg/day were associated with a hazard ratio of 0.87, but lower doses did not share this association (HR = 1.02).
In defense of their findings, Dr. Vargas-Santos and her associates evaluated the relevance of their study, compared with previous allopurinol studies.
“This study is one of few that have evaluated the relation of allopurinol to renal function among patients with gout and normal or near-normal kidney function at baseline,” the authors wrote, noting that most gout patients do not have severe kidney disease.
Previous studies have suggested that allopurinol worsens kidney function, but these studies were often conducted in nongout populations, with patients exhibiting CKD stage 3 or higher, they noted. Instead of allopurinol-induced kidney damage, renal decline in gout patients is likely multifactorial.
“Because people with gout have intrinsic differences compared with those with asymptomatic hyperuricemia, including higher mortality, more comorbidities, and more NSAID use, these studies’ results are not directly applicable to gout patients,” the investigators wrote.
“At minimum, allopurinol does not seem to have a detrimental effect on renal function in individuals with gout,” Dr. Vargas-Santos and her associates concluded. “Clinicians should consider evaluating other factors when faced with renal function decline in their patients with gout rather than lowering the dose of or discontinuing allopurinol, a strategy that has contributed to the ongoing suboptimal treatment of gout.”
The authors reported funding from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq); Ministry of Science, Technology and Innovation of Brazil; and National Institutes of Health. Dr Vargas-Santos has received speaking fees and support for international medical events from Grünenthal. No other disclosures were reported.
SOURCE: Vargas-Santos AB et al. JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.4463
*Correction, 11/5/2018: An earlier version of this story incorrectly stated the American College of Rheumatology’s 2012 gout treatment recommendation for using allopurinol in patients with renal impairment.
FROM JAMA INTERNAL MEDICINE
Key clinical point: In patients with gout, allopurinol was associated with a reduced risk of renal function decline.
Major finding: Allopurinol doses of at least 300 mg/day reduced risk of stage-3 or higher chronic kidney disease by 13%.
Study details: A retrospective, observational study involving newly diagnosed gout patients who either started allopurinol or did not (n = 4,760 in each group).
Disclosures: The authors reported funding from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq); Ministry of Science, Technology and Innovation of Brazil; and National Institutes of Health. Dr Vargas-Santos has received speaking fees and support for international medical events from Grünenthal. No other disclosures were reported.
Source: Vargas-Santos AB et al. JAMA Intern Med. 2018 Oct 8. doi: 10.1001/jamainternmed.2018.4463
Stop treating gout and start curing it, physician urges
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM THE ANNUAL PERSPECTIVES IN RHEUMATIC DISEASES
ICYMI: Canakinumab reduced risk of gout attacks
Canakinumab, an interleukin-1–beta blocker, reduced the risk of a gout attack by 52% when administered every 3 months, according to a secondary exploratory analysis of data from the multicenter, randomized, double-blind, placebo-controlled CANTOS trial (NCT01327846). The results of this analysis were published Sept. 17 in the Annals of Internal Medicine (doi: 10.7326/M18-1167).
We covered this story before it was published in the journal. Find our conference coverage at the links below.
Canakinumab, an interleukin-1–beta blocker, reduced the risk of a gout attack by 52% when administered every 3 months, according to a secondary exploratory analysis of data from the multicenter, randomized, double-blind, placebo-controlled CANTOS trial (NCT01327846). The results of this analysis were published Sept. 17 in the Annals of Internal Medicine (doi: 10.7326/M18-1167).
We covered this story before it was published in the journal. Find our conference coverage at the links below.
Canakinumab, an interleukin-1–beta blocker, reduced the risk of a gout attack by 52% when administered every 3 months, according to a secondary exploratory analysis of data from the multicenter, randomized, double-blind, placebo-controlled CANTOS trial (NCT01327846). The results of this analysis were published Sept. 17 in the Annals of Internal Medicine (doi: 10.7326/M18-1167).
We covered this story before it was published in the journal. Find our conference coverage at the links below.
FROM THE ANNALS OF INTERNAL MEDICINE
Obstructive sleep apnea may promote gout
Adults with obstructive sleep apnea are approximately twice as likely as are those without it to develop gout, according to data from a large, retrospective study with a median 5-year follow-up.
Data from previous studies have shown an increased risk in developing gout within the first year of an obstructive sleep apnea (OSA) diagnosis, wrote Milica Blagojevic-Bucknall, PhD, of Keele (England) University, and her colleagues.
In a study published in Arthritis & Rheumatology, the researchers compared 15,879 patients with OSA and 63,296 without.
Overall, 4.9% of OSA patients and 2.6% non‐OSA controls developed gout over a median follow‐up period of 5.8 years. The incidence rate for gout per 1,000 person‐years was 7.83 among patients with OSA and 4.03 for controls (adjusted hazard ratio, 1.42). The greatest risk for gout in the OSA patients occurred approximately 1-2 years after their diagnosis.
The researchers also found significant associations between body mass index and gout risk in sleep apnea across all BMI categories, but the strongest association occurred in the normal BMI group (HR 2.02) at 2-5 years after the index date of OSA.
“The novelty of this study lies in assessing both the short- and long-term association of OSA with incident gout in a large primary care-based population,” the researchers said. They proposed that the most likely explanation for the events was that “intermittent hypoxia increases nucleotide turnover which enhances endogenous uric acid production.”
The study findings were limited by several factors including potential misclassification of OSA and the impact of confounding variables such as genetics and diet, they noted.
However, the results support the association between sleep apnea and gout, but also serve to highlight that clinicians should “consider the possibility of gout in patients with sleep apnea regardless of obesity,” the researchers wrote.
The National Institute for Health Research funded the study. The authors have no conflicts of interest to declare.
SOURCE: Blagojevic-Bucknall M et al. Arthritis Rheumatol. 2018 Aug 30. doi: 10.1002/art.40662.
Adults with obstructive sleep apnea are approximately twice as likely as are those without it to develop gout, according to data from a large, retrospective study with a median 5-year follow-up.
Data from previous studies have shown an increased risk in developing gout within the first year of an obstructive sleep apnea (OSA) diagnosis, wrote Milica Blagojevic-Bucknall, PhD, of Keele (England) University, and her colleagues.
In a study published in Arthritis & Rheumatology, the researchers compared 15,879 patients with OSA and 63,296 without.
Overall, 4.9% of OSA patients and 2.6% non‐OSA controls developed gout over a median follow‐up period of 5.8 years. The incidence rate for gout per 1,000 person‐years was 7.83 among patients with OSA and 4.03 for controls (adjusted hazard ratio, 1.42). The greatest risk for gout in the OSA patients occurred approximately 1-2 years after their diagnosis.
The researchers also found significant associations between body mass index and gout risk in sleep apnea across all BMI categories, but the strongest association occurred in the normal BMI group (HR 2.02) at 2-5 years after the index date of OSA.
“The novelty of this study lies in assessing both the short- and long-term association of OSA with incident gout in a large primary care-based population,” the researchers said. They proposed that the most likely explanation for the events was that “intermittent hypoxia increases nucleotide turnover which enhances endogenous uric acid production.”
The study findings were limited by several factors including potential misclassification of OSA and the impact of confounding variables such as genetics and diet, they noted.
However, the results support the association between sleep apnea and gout, but also serve to highlight that clinicians should “consider the possibility of gout in patients with sleep apnea regardless of obesity,” the researchers wrote.
The National Institute for Health Research funded the study. The authors have no conflicts of interest to declare.
SOURCE: Blagojevic-Bucknall M et al. Arthritis Rheumatol. 2018 Aug 30. doi: 10.1002/art.40662.
Adults with obstructive sleep apnea are approximately twice as likely as are those without it to develop gout, according to data from a large, retrospective study with a median 5-year follow-up.
Data from previous studies have shown an increased risk in developing gout within the first year of an obstructive sleep apnea (OSA) diagnosis, wrote Milica Blagojevic-Bucknall, PhD, of Keele (England) University, and her colleagues.
In a study published in Arthritis & Rheumatology, the researchers compared 15,879 patients with OSA and 63,296 without.
Overall, 4.9% of OSA patients and 2.6% non‐OSA controls developed gout over a median follow‐up period of 5.8 years. The incidence rate for gout per 1,000 person‐years was 7.83 among patients with OSA and 4.03 for controls (adjusted hazard ratio, 1.42). The greatest risk for gout in the OSA patients occurred approximately 1-2 years after their diagnosis.
The researchers also found significant associations between body mass index and gout risk in sleep apnea across all BMI categories, but the strongest association occurred in the normal BMI group (HR 2.02) at 2-5 years after the index date of OSA.
“The novelty of this study lies in assessing both the short- and long-term association of OSA with incident gout in a large primary care-based population,” the researchers said. They proposed that the most likely explanation for the events was that “intermittent hypoxia increases nucleotide turnover which enhances endogenous uric acid production.”
The study findings were limited by several factors including potential misclassification of OSA and the impact of confounding variables such as genetics and diet, they noted.
However, the results support the association between sleep apnea and gout, but also serve to highlight that clinicians should “consider the possibility of gout in patients with sleep apnea regardless of obesity,” the researchers wrote.
The National Institute for Health Research funded the study. The authors have no conflicts of interest to declare.
SOURCE: Blagojevic-Bucknall M et al. Arthritis Rheumatol. 2018 Aug 30. doi: 10.1002/art.40662.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Adults with obstructive sleep apnea were more likely to develop gout than were those without the condition.
Major finding: Over a median follow‐up of 5.8 years, 4.9% of OSA patients and 2.6% of controls without OSA developed gout.
Study details: A matched retrospective cohort study of 15,879 OSA patients and 63,296 controls.
Disclosures: The National Institute for Health Research funded the study. The researchers had no financial conflicts to disclose.
Source: Blagojevich-Bucknall M et al. Arthritis Rheumatol. 2018 Aug 30. doi: 10.1002/art.40662.
Ultrasound aids treat-to-target approach for gout
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Deceasing uric acid load during a treat-to-target approach can be seen on ultrasound.
Major finding: Ultrasound scores decreased with decreasing urate levels at 3, 6 and 12 month, with the highest numeric difference from baseline seen at 12 months for double contour sign (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2).
Study details: A prospective, observational study of 161 patients with urate crystal–proven gout treated with urate-lowering therapy.
Disclosures: Dr. Hammer had no conflicts of interest to disclose.
Sources: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
Canakinumab cut gout attacks in CANTOS
AMSTERDAM – in an exploratory, post hoc analysis of data collected from more than 10,000 patients in the CANTOS multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While this result is only a hypothesis-generating suggestion that blocking interleukin (IL)-1 beta can have a significant impact on the frequency of gout flares, it serves as a proof-of-concept that IL-1 beta blockade is a potentially clinically meaningful strategy for future efforts to block gout attacks, Daniel H. Solomon, MD, said at the European Congress of Rheumatology.
“IL-1 beta is incredibly important in the inflammation associated with gout. Gout is considered by many to be the canonical IL-1 beta disease,” and hence it was important to examine the impact that treatment with the IL-1 beta blocker canakinumab had on gout in the CANTOS trial, Dr. Solomon explained in a video interview.
The answer was that treatment with canakinumab was linked with a roughly 50% reduction in gout flares in the total study group. The same reduction was seen in both the subgroups of patients with and without a history of gout. The effect was seen across all three subgroups of patients, based on their baseline serum urate levels including those with normal, elevated, or very elevated levels and across all the other prespecified subgroups including divisions based on sex, age, baseline body mass index, and baseline level of high-sensitivity C-reactive protein (hsCRP).
It’s also unclear that canakinumab (Ilaris) is the best type of IL-1 beta blocking drug to use for prevention of gout flares. In CANTOS, this expensive drug was administered subcutaneously every 3 months. A more appropriate agent might be an oral, small-molecule drug that blocks IL-1 beta. Several examples of this type of agent are currently in clinical development, said Dr. Solomon, a professor of medicine at Harvard Medical School and a rheumatologist at Brigham and Women’s Hospital, both in Boston.
CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) randomized 10,061 patients with a history of MI and a hsCRP level of at least 2 mg/L at centers in 39 countries. The study’s primary endpoint was the combined rate of cardiovascular death, MI, or stroke, and canakinumab treatment at the 150-mg dosage level linked with a 15% relative reduction in this endpoint, compared with placebo in this secondary-prevention study (N Engl J Med. 2017 Sept 21;377[12]:1119-31). The study also randomized patients to either of two other canakinumab dosages, 50 mg or 300 mg, administered every 3 months, and, while each of these produced reductions in the primary endpoint relative to placebo, the 150-mg dosage had the largest effect. In the gout analysis reported by Dr. Solomon, the three different canakinumab dosages produced somewhat different levels of gout-flare reductions, but, generally, the effect was similar across the three treatment groups.
In the total study population, regardless of gout history, treatment with 50 mg, 150 mg, and 300 mg canakinumab every 3 months was linked with a reduction in gout attacks of 46%, 57%, and 53%, respectively, compared with placebo-treated patients, Dr. Solomon reported. The three dosages also uniformly produced significantly drops in serum levels of hsCRP, compared with placebo, but canakinumab treatment had no impact on serum urate levels, indicating that the gout-reducing effects of the drug did not occur via a mechanism that involved serum urate.
Because CANTOS exclusively enrolled patients with established coronary disease, the new analysis could not address whether IL-1 beta blockade would also be an effective strategy for reducing gout flares in people without cardiovascular disease, Dr. Solomon cautioned. Although it probably would, he said. He also stressed that treatment with an IL-1 blocking drug should not be seen as a substitute for appropriate urate-lowering treatment in patients with elevated levels of serum urate.
SOURCE: Solomon DH et al. Ann Rheum Dis. 2018;77(Suppl 2):56. Abstract OP0014.
AMSTERDAM – in an exploratory, post hoc analysis of data collected from more than 10,000 patients in the CANTOS multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While this result is only a hypothesis-generating suggestion that blocking interleukin (IL)-1 beta can have a significant impact on the frequency of gout flares, it serves as a proof-of-concept that IL-1 beta blockade is a potentially clinically meaningful strategy for future efforts to block gout attacks, Daniel H. Solomon, MD, said at the European Congress of Rheumatology.
“IL-1 beta is incredibly important in the inflammation associated with gout. Gout is considered by many to be the canonical IL-1 beta disease,” and hence it was important to examine the impact that treatment with the IL-1 beta blocker canakinumab had on gout in the CANTOS trial, Dr. Solomon explained in a video interview.
The answer was that treatment with canakinumab was linked with a roughly 50% reduction in gout flares in the total study group. The same reduction was seen in both the subgroups of patients with and without a history of gout. The effect was seen across all three subgroups of patients, based on their baseline serum urate levels including those with normal, elevated, or very elevated levels and across all the other prespecified subgroups including divisions based on sex, age, baseline body mass index, and baseline level of high-sensitivity C-reactive protein (hsCRP).
It’s also unclear that canakinumab (Ilaris) is the best type of IL-1 beta blocking drug to use for prevention of gout flares. In CANTOS, this expensive drug was administered subcutaneously every 3 months. A more appropriate agent might be an oral, small-molecule drug that blocks IL-1 beta. Several examples of this type of agent are currently in clinical development, said Dr. Solomon, a professor of medicine at Harvard Medical School and a rheumatologist at Brigham and Women’s Hospital, both in Boston.
CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) randomized 10,061 patients with a history of MI and a hsCRP level of at least 2 mg/L at centers in 39 countries. The study’s primary endpoint was the combined rate of cardiovascular death, MI, or stroke, and canakinumab treatment at the 150-mg dosage level linked with a 15% relative reduction in this endpoint, compared with placebo in this secondary-prevention study (N Engl J Med. 2017 Sept 21;377[12]:1119-31). The study also randomized patients to either of two other canakinumab dosages, 50 mg or 300 mg, administered every 3 months, and, while each of these produced reductions in the primary endpoint relative to placebo, the 150-mg dosage had the largest effect. In the gout analysis reported by Dr. Solomon, the three different canakinumab dosages produced somewhat different levels of gout-flare reductions, but, generally, the effect was similar across the three treatment groups.
In the total study population, regardless of gout history, treatment with 50 mg, 150 mg, and 300 mg canakinumab every 3 months was linked with a reduction in gout attacks of 46%, 57%, and 53%, respectively, compared with placebo-treated patients, Dr. Solomon reported. The three dosages also uniformly produced significantly drops in serum levels of hsCRP, compared with placebo, but canakinumab treatment had no impact on serum urate levels, indicating that the gout-reducing effects of the drug did not occur via a mechanism that involved serum urate.
Because CANTOS exclusively enrolled patients with established coronary disease, the new analysis could not address whether IL-1 beta blockade would also be an effective strategy for reducing gout flares in people without cardiovascular disease, Dr. Solomon cautioned. Although it probably would, he said. He also stressed that treatment with an IL-1 blocking drug should not be seen as a substitute for appropriate urate-lowering treatment in patients with elevated levels of serum urate.
SOURCE: Solomon DH et al. Ann Rheum Dis. 2018;77(Suppl 2):56. Abstract OP0014.
AMSTERDAM – in an exploratory, post hoc analysis of data collected from more than 10,000 patients in the CANTOS multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While this result is only a hypothesis-generating suggestion that blocking interleukin (IL)-1 beta can have a significant impact on the frequency of gout flares, it serves as a proof-of-concept that IL-1 beta blockade is a potentially clinically meaningful strategy for future efforts to block gout attacks, Daniel H. Solomon, MD, said at the European Congress of Rheumatology.
“IL-1 beta is incredibly important in the inflammation associated with gout. Gout is considered by many to be the canonical IL-1 beta disease,” and hence it was important to examine the impact that treatment with the IL-1 beta blocker canakinumab had on gout in the CANTOS trial, Dr. Solomon explained in a video interview.
The answer was that treatment with canakinumab was linked with a roughly 50% reduction in gout flares in the total study group. The same reduction was seen in both the subgroups of patients with and without a history of gout. The effect was seen across all three subgroups of patients, based on their baseline serum urate levels including those with normal, elevated, or very elevated levels and across all the other prespecified subgroups including divisions based on sex, age, baseline body mass index, and baseline level of high-sensitivity C-reactive protein (hsCRP).
It’s also unclear that canakinumab (Ilaris) is the best type of IL-1 beta blocking drug to use for prevention of gout flares. In CANTOS, this expensive drug was administered subcutaneously every 3 months. A more appropriate agent might be an oral, small-molecule drug that blocks IL-1 beta. Several examples of this type of agent are currently in clinical development, said Dr. Solomon, a professor of medicine at Harvard Medical School and a rheumatologist at Brigham and Women’s Hospital, both in Boston.
CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) randomized 10,061 patients with a history of MI and a hsCRP level of at least 2 mg/L at centers in 39 countries. The study’s primary endpoint was the combined rate of cardiovascular death, MI, or stroke, and canakinumab treatment at the 150-mg dosage level linked with a 15% relative reduction in this endpoint, compared with placebo in this secondary-prevention study (N Engl J Med. 2017 Sept 21;377[12]:1119-31). The study also randomized patients to either of two other canakinumab dosages, 50 mg or 300 mg, administered every 3 months, and, while each of these produced reductions in the primary endpoint relative to placebo, the 150-mg dosage had the largest effect. In the gout analysis reported by Dr. Solomon, the three different canakinumab dosages produced somewhat different levels of gout-flare reductions, but, generally, the effect was similar across the three treatment groups.
In the total study population, regardless of gout history, treatment with 50 mg, 150 mg, and 300 mg canakinumab every 3 months was linked with a reduction in gout attacks of 46%, 57%, and 53%, respectively, compared with placebo-treated patients, Dr. Solomon reported. The three dosages also uniformly produced significantly drops in serum levels of hsCRP, compared with placebo, but canakinumab treatment had no impact on serum urate levels, indicating that the gout-reducing effects of the drug did not occur via a mechanism that involved serum urate.
Because CANTOS exclusively enrolled patients with established coronary disease, the new analysis could not address whether IL-1 beta blockade would also be an effective strategy for reducing gout flares in people without cardiovascular disease, Dr. Solomon cautioned. Although it probably would, he said. He also stressed that treatment with an IL-1 blocking drug should not be seen as a substitute for appropriate urate-lowering treatment in patients with elevated levels of serum urate.
SOURCE: Solomon DH et al. Ann Rheum Dis. 2018;77(Suppl 2):56. Abstract OP0014.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: IL-1 blockade seems to be an effective way to cut the incidence of gout attacks.
Major finding: IL-1 blockade with canakinumab was linked with about a 50% cut in gout flares, compared with placebo.
Study details: CANTOS, a multicenter, randomized trial with 10,061 patients.
Disclosures: CANTOS was funded by Novartis, the company that markets canakinumab. Dr. Solomon has no relationships with Novartis. Brigham and Women’s Hospital, the center at which he works, has received research funding from Amgen, Bristol-Myers Squibb, Genentech, and Pfizer for studies that Dr. Solomon has helped direct.
Source: Solomon DH et al. Ann Rheum Dis. 2018;77(Suppl 2):56. Abstract OP0014.
EULAR scientific program highlights spectrum of translational research
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”