User login
Lenvatinib/pembrolizumab has good activity in advanced RCC, other solid tumors
A combination of the tyrosine kinase inhibitor lenvatinib (Lenvima) and the immune checkpoint inhibitor pembrolizumab (Keytruda) was safe and showed promising activity against advanced renal cell carcinoma and other solid tumors in a phase 1b/2 study.
Overall response rates (ORR) at 24 weeks ranged from 63% for patients with advanced renal cell carcinomas (RCC) to 25% for patients with urothelial cancers, reported Matthew H. Taylor, MD, of Knight Cancer Institute at Oregon Health & Science University in Portland, and colleagues.
The findings from this study sparked additional clinical trials for patients with gastric cancer, gastroesophageal cancer, and differentiated thyroid cancer, and set the stage for larger phase 3 trials in patients with advanced RCC, endometrial cancer, malignant melanoma, and non–small cell lung cancer (NSCLC).
“In the future, we also plan to study lenvatinib plus pembrolizumab in patients with RCC who have had disease progression after treatment with immune checkpoint inhibitors,” they wrote. The report was published in Journal of Clinical Oncology.
Lenvatinib is a multitargeted tyrosine kinase inhibitor (TKI) with action against vascular endothelial growth factor (VEGF) receptors 1-3, fibroblast growth factor (FGF) receptors 1-4, platelet-derived growth factor receptors alpha and the RET and KIT kinases.
“Preclinical and clinical studies suggest that modulation of VEGF-mediated immune suppression via angiogenesis inhibition could potentially augment the immunotherapeutic activity of immune checkpoint inhibitors,” the investigators wrote.
They reported results from the dose finding (1b) phase including 13 patients and initial phase 2 expansion cohorts with a total of 124 patients.
The maximum tolerated dose of lenvatinib in combination with pembrolizumab was established as 20 mg/day.
At 24 weeks of follow-up, the ORR for 30 patients with RCC was 63%; two additional patients had responses after week 24, for a total ORR at study cutoff in this cohort of 70%. The median duration of response for these patients was 20 months, and the median progression-free survival (PFS) was 19.8 months. At the time of data cutoff for this analysis, 9 of the 30 patients with RCC were still on treatment.
For 23 patients with endometrial cancer, the 24-week and overall ORR were 52%, with a median duration of response not reached, and a median PFS of 9.7 months. Seven patients were still on treatment at data cutoff.
For 21 patients with melanoma, the 24-week and overall ORR were 48%, median duration of response was 12.5 months, and median PFS was 5.5 months. Two of the patients were still on treatment at data cutoff.
For the 22 patients with squamous cell cancer of the head and neck, the 24-week ORR was 36%, with two patients having a response after week 24 for a total ORR at data cutoff of 46%. The median duration of response was 8.2 months and the median PFS was 4.7 months. Three patients remained on treatment at data cutoff.
For 21 patients with NSCLC, the 24-week and overall ORR were 33%, the median duration of response was 10.9 months, and median PFS was 5.9 months. Six of the patients were still receiving treatment at data cutoff.
For 20 patients with urothelial cancer, the 24-week and overall ORR were 25%, with a median duration of response not reached, and a median PFS of 5.4 months. Three patients were still receiving the combination at the time of data cutoff.
Treatment related adverse events (TRAEs) occurred in 133 of all 137 patients enrolled in the two study phases. The adverse events were similar across all cohorts, with any grade of events including fatigue in 58%, diarrhea in 52%, hypertension in 47%, hypothyroidism in 42%, and decreased appetite in 39%.
The most frequent grade 3 or 4 TRAEs were hypertension in 20%, fatigue in 12%, diarrhea in 9%, proteinuria in 8%, and increased lipase levels in 7%.
In all, 85% of patients had a TRAE leading to lenvatinib dose reduction and/or interruption, and 13% required lenvatinib discontinuation.
Events leading to pembrolizumab dose interruption occurred in 45% of patients, and pembrolizumab discontinuation in 15%.
The study was sponsored by Eisai with collaboration from Merck Sharp & Dohme. Dr. Taylor disclosed a consulting or advisory role for Bristol-Myers Squibb, Eisai, Array BioPharma, Loxo, Bayer, ArQule, Blueprint Medicines, Novartis, and Sanofi/Genzyme, and speakers bureau activities for BMS and Eisai.
SOURCE: Taylor MH et al. J Clin Oncol. 2020 Jan. 21 doi: 10.1200/JCO.19.01598.
A combination of the tyrosine kinase inhibitor lenvatinib (Lenvima) and the immune checkpoint inhibitor pembrolizumab (Keytruda) was safe and showed promising activity against advanced renal cell carcinoma and other solid tumors in a phase 1b/2 study.
Overall response rates (ORR) at 24 weeks ranged from 63% for patients with advanced renal cell carcinomas (RCC) to 25% for patients with urothelial cancers, reported Matthew H. Taylor, MD, of Knight Cancer Institute at Oregon Health & Science University in Portland, and colleagues.
The findings from this study sparked additional clinical trials for patients with gastric cancer, gastroesophageal cancer, and differentiated thyroid cancer, and set the stage for larger phase 3 trials in patients with advanced RCC, endometrial cancer, malignant melanoma, and non–small cell lung cancer (NSCLC).
“In the future, we also plan to study lenvatinib plus pembrolizumab in patients with RCC who have had disease progression after treatment with immune checkpoint inhibitors,” they wrote. The report was published in Journal of Clinical Oncology.
Lenvatinib is a multitargeted tyrosine kinase inhibitor (TKI) with action against vascular endothelial growth factor (VEGF) receptors 1-3, fibroblast growth factor (FGF) receptors 1-4, platelet-derived growth factor receptors alpha and the RET and KIT kinases.
“Preclinical and clinical studies suggest that modulation of VEGF-mediated immune suppression via angiogenesis inhibition could potentially augment the immunotherapeutic activity of immune checkpoint inhibitors,” the investigators wrote.
They reported results from the dose finding (1b) phase including 13 patients and initial phase 2 expansion cohorts with a total of 124 patients.
The maximum tolerated dose of lenvatinib in combination with pembrolizumab was established as 20 mg/day.
At 24 weeks of follow-up, the ORR for 30 patients with RCC was 63%; two additional patients had responses after week 24, for a total ORR at study cutoff in this cohort of 70%. The median duration of response for these patients was 20 months, and the median progression-free survival (PFS) was 19.8 months. At the time of data cutoff for this analysis, 9 of the 30 patients with RCC were still on treatment.
For 23 patients with endometrial cancer, the 24-week and overall ORR were 52%, with a median duration of response not reached, and a median PFS of 9.7 months. Seven patients were still on treatment at data cutoff.
For 21 patients with melanoma, the 24-week and overall ORR were 48%, median duration of response was 12.5 months, and median PFS was 5.5 months. Two of the patients were still on treatment at data cutoff.
For the 22 patients with squamous cell cancer of the head and neck, the 24-week ORR was 36%, with two patients having a response after week 24 for a total ORR at data cutoff of 46%. The median duration of response was 8.2 months and the median PFS was 4.7 months. Three patients remained on treatment at data cutoff.
For 21 patients with NSCLC, the 24-week and overall ORR were 33%, the median duration of response was 10.9 months, and median PFS was 5.9 months. Six of the patients were still receiving treatment at data cutoff.
For 20 patients with urothelial cancer, the 24-week and overall ORR were 25%, with a median duration of response not reached, and a median PFS of 5.4 months. Three patients were still receiving the combination at the time of data cutoff.
Treatment related adverse events (TRAEs) occurred in 133 of all 137 patients enrolled in the two study phases. The adverse events were similar across all cohorts, with any grade of events including fatigue in 58%, diarrhea in 52%, hypertension in 47%, hypothyroidism in 42%, and decreased appetite in 39%.
The most frequent grade 3 or 4 TRAEs were hypertension in 20%, fatigue in 12%, diarrhea in 9%, proteinuria in 8%, and increased lipase levels in 7%.
In all, 85% of patients had a TRAE leading to lenvatinib dose reduction and/or interruption, and 13% required lenvatinib discontinuation.
Events leading to pembrolizumab dose interruption occurred in 45% of patients, and pembrolizumab discontinuation in 15%.
The study was sponsored by Eisai with collaboration from Merck Sharp & Dohme. Dr. Taylor disclosed a consulting or advisory role for Bristol-Myers Squibb, Eisai, Array BioPharma, Loxo, Bayer, ArQule, Blueprint Medicines, Novartis, and Sanofi/Genzyme, and speakers bureau activities for BMS and Eisai.
SOURCE: Taylor MH et al. J Clin Oncol. 2020 Jan. 21 doi: 10.1200/JCO.19.01598.
A combination of the tyrosine kinase inhibitor lenvatinib (Lenvima) and the immune checkpoint inhibitor pembrolizumab (Keytruda) was safe and showed promising activity against advanced renal cell carcinoma and other solid tumors in a phase 1b/2 study.
Overall response rates (ORR) at 24 weeks ranged from 63% for patients with advanced renal cell carcinomas (RCC) to 25% for patients with urothelial cancers, reported Matthew H. Taylor, MD, of Knight Cancer Institute at Oregon Health & Science University in Portland, and colleagues.
The findings from this study sparked additional clinical trials for patients with gastric cancer, gastroesophageal cancer, and differentiated thyroid cancer, and set the stage for larger phase 3 trials in patients with advanced RCC, endometrial cancer, malignant melanoma, and non–small cell lung cancer (NSCLC).
“In the future, we also plan to study lenvatinib plus pembrolizumab in patients with RCC who have had disease progression after treatment with immune checkpoint inhibitors,” they wrote. The report was published in Journal of Clinical Oncology.
Lenvatinib is a multitargeted tyrosine kinase inhibitor (TKI) with action against vascular endothelial growth factor (VEGF) receptors 1-3, fibroblast growth factor (FGF) receptors 1-4, platelet-derived growth factor receptors alpha and the RET and KIT kinases.
“Preclinical and clinical studies suggest that modulation of VEGF-mediated immune suppression via angiogenesis inhibition could potentially augment the immunotherapeutic activity of immune checkpoint inhibitors,” the investigators wrote.
They reported results from the dose finding (1b) phase including 13 patients and initial phase 2 expansion cohorts with a total of 124 patients.
The maximum tolerated dose of lenvatinib in combination with pembrolizumab was established as 20 mg/day.
At 24 weeks of follow-up, the ORR for 30 patients with RCC was 63%; two additional patients had responses after week 24, for a total ORR at study cutoff in this cohort of 70%. The median duration of response for these patients was 20 months, and the median progression-free survival (PFS) was 19.8 months. At the time of data cutoff for this analysis, 9 of the 30 patients with RCC were still on treatment.
For 23 patients with endometrial cancer, the 24-week and overall ORR were 52%, with a median duration of response not reached, and a median PFS of 9.7 months. Seven patients were still on treatment at data cutoff.
For 21 patients with melanoma, the 24-week and overall ORR were 48%, median duration of response was 12.5 months, and median PFS was 5.5 months. Two of the patients were still on treatment at data cutoff.
For the 22 patients with squamous cell cancer of the head and neck, the 24-week ORR was 36%, with two patients having a response after week 24 for a total ORR at data cutoff of 46%. The median duration of response was 8.2 months and the median PFS was 4.7 months. Three patients remained on treatment at data cutoff.
For 21 patients with NSCLC, the 24-week and overall ORR were 33%, the median duration of response was 10.9 months, and median PFS was 5.9 months. Six of the patients were still receiving treatment at data cutoff.
For 20 patients with urothelial cancer, the 24-week and overall ORR were 25%, with a median duration of response not reached, and a median PFS of 5.4 months. Three patients were still receiving the combination at the time of data cutoff.
Treatment related adverse events (TRAEs) occurred in 133 of all 137 patients enrolled in the two study phases. The adverse events were similar across all cohorts, with any grade of events including fatigue in 58%, diarrhea in 52%, hypertension in 47%, hypothyroidism in 42%, and decreased appetite in 39%.
The most frequent grade 3 or 4 TRAEs were hypertension in 20%, fatigue in 12%, diarrhea in 9%, proteinuria in 8%, and increased lipase levels in 7%.
In all, 85% of patients had a TRAE leading to lenvatinib dose reduction and/or interruption, and 13% required lenvatinib discontinuation.
Events leading to pembrolizumab dose interruption occurred in 45% of patients, and pembrolizumab discontinuation in 15%.
The study was sponsored by Eisai with collaboration from Merck Sharp & Dohme. Dr. Taylor disclosed a consulting or advisory role for Bristol-Myers Squibb, Eisai, Array BioPharma, Loxo, Bayer, ArQule, Blueprint Medicines, Novartis, and Sanofi/Genzyme, and speakers bureau activities for BMS and Eisai.
SOURCE: Taylor MH et al. J Clin Oncol. 2020 Jan. 21 doi: 10.1200/JCO.19.01598.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Multimodal therapies almost double survival in anaplastic thyroid cancer
CHICAGO –
Median survival for participants in a specialized program who have been able to benefit from targeted therapy and immunotherapy now stands at 16 months, with 43% of patients surviving 2 years or more, said Anastasios Maniakas, MD, at the annual meeting of the American Thyroid Association.
Median survival was 8 months during 2000-2013, before the program, dubbed FAST (Facilitating Anaplastic Thyroid Cancer Specialized Treatment), was initiated at the University of Texas MD Anderson Cancer Center, Houston.
These increased survival rates were driven primarily by better targeting of mutation-specific therapy and by immunotherapy, said Dr. Maniakas, a fellow in head and neck surgery at the center. This targeting, in turn, was facilitated by timely staging and genetic work-up, as well as appropriate clinical trial enrollment.
As word has spread about the program, referrals went up by 44%, said Dr. Maniakas. Members of the FAST team include representatives from oncologic endocrinology, head and neck surgery, radiation oncology, pathology, and basic science.
Historically, anaplastic thyroid cancer (ATC) has had a 12-month overall survival rate of less than 30% for patients who have advanced disease, said Dr. Maniakas, citing a recent analysis showing that, in 1,567 ATC cases, the median survival was just 4 months, and the 6-month survival rate was 35%.
The FAST team’s engagement starts with rapid intake whereby patients see a physician within 3-5 days of initial contact with the center, explained Dr. Maniakas. A prescheduled work-up is completed within another 3-7 days. It includes basic lab work, cell-free DNA testing, BRAF immunohistochemistry, and molecular testing. Additional consults and appropriate medical imaging for staging are also included in the initial work-up.
With these data in hand, physicians meet again with patients in a treatment-planning clinic to assess eligibility for participation in a clinical trial. Patients will otherwise receive standard-of-care therapy that may include surgery or BRAF-directed therapy. However, said Dr. Maniakas, the FAST approach has resulted in a boost of more than 30% in clinical trial participation by ATC patients. Adjunctive therapies are also tailored to patients under the care of the FAST team, which may include stereotactic body-radiation therapy, surgery, and immunotherapy.
The team is tracking a cohort of patients who received surgery with or without radiation therapy, preceded by neoadjuvant BRAF/MEK inhibitor therapy – an approach used since 2017. Of 20 patients who were positive for BRAF-V600E, 16 are still alive at a median 1.21 years of follow-up since diagnosis, said Dr. Maniakas. The median survival time for those who did not receive surgery is 0.8 years, whereas the median survival has not been reached for those who also had surgery.
Molecular testing and initial screening of ATC patients is an essential component of the cancer center’s precision medicine approach, said Dr. Maniakas. “Genetic profiling has become a key player in ATC management and survival.”
In looking at outcomes at the cancer center, Dr. Maniakas and his collaborators divided the patients into three groups. The first included 227 patients seen during 2000-2013, before the program was initiated. The 100 participants in the second group initiated treatment sometime during 2014-2016, after the program was launched but before the targeted therapy and immunotherapy trial was fully implemented. Since 2017, 152 participants in the third group have had the opportunity to participate in the clinical trial, as well as receiving surgery with or without radiation therapy after neoadjuvant immunotherapy.
Since 2017, 97% of ATC patients have had genetic profiling done. Most patients are receiving rapid determination of BRAF-V600E status with immunohistochemistry, with results available in a few days, followed by liquid biopsy (available in about 2 weeks), and then next-generation sequencing. Results for the latter, considered the gold standard, can take up to 3 weeks.
Patients participating in the program were aged a mean 65 years at diagnosis, and just over half were men. The number of patients receiving targeted therapy has continued to rise, said Dr. Maniakas. From 2000 to 2013, just 9% of patients received targeted therapy; from 2014 to 2016, that figure rose to 43%; and since 2017, 61% of patients have received targeted therapy (P less than .001).
“Landmark changes in the management of ATC patients as a whole have had a direct impact to the significant increase in overall survival,” said Dr. Maniakas.
He added that the cancer center’s experience could inform future ATC guidelines. Patients with this deadliest of thyroid cancers should all have rapid molecular testing, followed by timely, targeted therapy. Clinical trial eligibility should be considered for all patients. Finally, guideline authors should take note of the ongoing favorable survival rates seen for patients receiving surgery after neoadjuvant therapy.
Dr. Maniakas reported no outside sources of funding and that he had no relevant disclosures.
SOURCE: Maniakas A et al. ATA 2019, Short Call Oral Abstract 9.
CHICAGO –
Median survival for participants in a specialized program who have been able to benefit from targeted therapy and immunotherapy now stands at 16 months, with 43% of patients surviving 2 years or more, said Anastasios Maniakas, MD, at the annual meeting of the American Thyroid Association.
Median survival was 8 months during 2000-2013, before the program, dubbed FAST (Facilitating Anaplastic Thyroid Cancer Specialized Treatment), was initiated at the University of Texas MD Anderson Cancer Center, Houston.
These increased survival rates were driven primarily by better targeting of mutation-specific therapy and by immunotherapy, said Dr. Maniakas, a fellow in head and neck surgery at the center. This targeting, in turn, was facilitated by timely staging and genetic work-up, as well as appropriate clinical trial enrollment.
As word has spread about the program, referrals went up by 44%, said Dr. Maniakas. Members of the FAST team include representatives from oncologic endocrinology, head and neck surgery, radiation oncology, pathology, and basic science.
Historically, anaplastic thyroid cancer (ATC) has had a 12-month overall survival rate of less than 30% for patients who have advanced disease, said Dr. Maniakas, citing a recent analysis showing that, in 1,567 ATC cases, the median survival was just 4 months, and the 6-month survival rate was 35%.
The FAST team’s engagement starts with rapid intake whereby patients see a physician within 3-5 days of initial contact with the center, explained Dr. Maniakas. A prescheduled work-up is completed within another 3-7 days. It includes basic lab work, cell-free DNA testing, BRAF immunohistochemistry, and molecular testing. Additional consults and appropriate medical imaging for staging are also included in the initial work-up.
With these data in hand, physicians meet again with patients in a treatment-planning clinic to assess eligibility for participation in a clinical trial. Patients will otherwise receive standard-of-care therapy that may include surgery or BRAF-directed therapy. However, said Dr. Maniakas, the FAST approach has resulted in a boost of more than 30% in clinical trial participation by ATC patients. Adjunctive therapies are also tailored to patients under the care of the FAST team, which may include stereotactic body-radiation therapy, surgery, and immunotherapy.
The team is tracking a cohort of patients who received surgery with or without radiation therapy, preceded by neoadjuvant BRAF/MEK inhibitor therapy – an approach used since 2017. Of 20 patients who were positive for BRAF-V600E, 16 are still alive at a median 1.21 years of follow-up since diagnosis, said Dr. Maniakas. The median survival time for those who did not receive surgery is 0.8 years, whereas the median survival has not been reached for those who also had surgery.
Molecular testing and initial screening of ATC patients is an essential component of the cancer center’s precision medicine approach, said Dr. Maniakas. “Genetic profiling has become a key player in ATC management and survival.”
In looking at outcomes at the cancer center, Dr. Maniakas and his collaborators divided the patients into three groups. The first included 227 patients seen during 2000-2013, before the program was initiated. The 100 participants in the second group initiated treatment sometime during 2014-2016, after the program was launched but before the targeted therapy and immunotherapy trial was fully implemented. Since 2017, 152 participants in the third group have had the opportunity to participate in the clinical trial, as well as receiving surgery with or without radiation therapy after neoadjuvant immunotherapy.
Since 2017, 97% of ATC patients have had genetic profiling done. Most patients are receiving rapid determination of BRAF-V600E status with immunohistochemistry, with results available in a few days, followed by liquid biopsy (available in about 2 weeks), and then next-generation sequencing. Results for the latter, considered the gold standard, can take up to 3 weeks.
Patients participating in the program were aged a mean 65 years at diagnosis, and just over half were men. The number of patients receiving targeted therapy has continued to rise, said Dr. Maniakas. From 2000 to 2013, just 9% of patients received targeted therapy; from 2014 to 2016, that figure rose to 43%; and since 2017, 61% of patients have received targeted therapy (P less than .001).
“Landmark changes in the management of ATC patients as a whole have had a direct impact to the significant increase in overall survival,” said Dr. Maniakas.
He added that the cancer center’s experience could inform future ATC guidelines. Patients with this deadliest of thyroid cancers should all have rapid molecular testing, followed by timely, targeted therapy. Clinical trial eligibility should be considered for all patients. Finally, guideline authors should take note of the ongoing favorable survival rates seen for patients receiving surgery after neoadjuvant therapy.
Dr. Maniakas reported no outside sources of funding and that he had no relevant disclosures.
SOURCE: Maniakas A et al. ATA 2019, Short Call Oral Abstract 9.
CHICAGO –
Median survival for participants in a specialized program who have been able to benefit from targeted therapy and immunotherapy now stands at 16 months, with 43% of patients surviving 2 years or more, said Anastasios Maniakas, MD, at the annual meeting of the American Thyroid Association.
Median survival was 8 months during 2000-2013, before the program, dubbed FAST (Facilitating Anaplastic Thyroid Cancer Specialized Treatment), was initiated at the University of Texas MD Anderson Cancer Center, Houston.
These increased survival rates were driven primarily by better targeting of mutation-specific therapy and by immunotherapy, said Dr. Maniakas, a fellow in head and neck surgery at the center. This targeting, in turn, was facilitated by timely staging and genetic work-up, as well as appropriate clinical trial enrollment.
As word has spread about the program, referrals went up by 44%, said Dr. Maniakas. Members of the FAST team include representatives from oncologic endocrinology, head and neck surgery, radiation oncology, pathology, and basic science.
Historically, anaplastic thyroid cancer (ATC) has had a 12-month overall survival rate of less than 30% for patients who have advanced disease, said Dr. Maniakas, citing a recent analysis showing that, in 1,567 ATC cases, the median survival was just 4 months, and the 6-month survival rate was 35%.
The FAST team’s engagement starts with rapid intake whereby patients see a physician within 3-5 days of initial contact with the center, explained Dr. Maniakas. A prescheduled work-up is completed within another 3-7 days. It includes basic lab work, cell-free DNA testing, BRAF immunohistochemistry, and molecular testing. Additional consults and appropriate medical imaging for staging are also included in the initial work-up.
With these data in hand, physicians meet again with patients in a treatment-planning clinic to assess eligibility for participation in a clinical trial. Patients will otherwise receive standard-of-care therapy that may include surgery or BRAF-directed therapy. However, said Dr. Maniakas, the FAST approach has resulted in a boost of more than 30% in clinical trial participation by ATC patients. Adjunctive therapies are also tailored to patients under the care of the FAST team, which may include stereotactic body-radiation therapy, surgery, and immunotherapy.
The team is tracking a cohort of patients who received surgery with or without radiation therapy, preceded by neoadjuvant BRAF/MEK inhibitor therapy – an approach used since 2017. Of 20 patients who were positive for BRAF-V600E, 16 are still alive at a median 1.21 years of follow-up since diagnosis, said Dr. Maniakas. The median survival time for those who did not receive surgery is 0.8 years, whereas the median survival has not been reached for those who also had surgery.
Molecular testing and initial screening of ATC patients is an essential component of the cancer center’s precision medicine approach, said Dr. Maniakas. “Genetic profiling has become a key player in ATC management and survival.”
In looking at outcomes at the cancer center, Dr. Maniakas and his collaborators divided the patients into three groups. The first included 227 patients seen during 2000-2013, before the program was initiated. The 100 participants in the second group initiated treatment sometime during 2014-2016, after the program was launched but before the targeted therapy and immunotherapy trial was fully implemented. Since 2017, 152 participants in the third group have had the opportunity to participate in the clinical trial, as well as receiving surgery with or without radiation therapy after neoadjuvant immunotherapy.
Since 2017, 97% of ATC patients have had genetic profiling done. Most patients are receiving rapid determination of BRAF-V600E status with immunohistochemistry, with results available in a few days, followed by liquid biopsy (available in about 2 weeks), and then next-generation sequencing. Results for the latter, considered the gold standard, can take up to 3 weeks.
Patients participating in the program were aged a mean 65 years at diagnosis, and just over half were men. The number of patients receiving targeted therapy has continued to rise, said Dr. Maniakas. From 2000 to 2013, just 9% of patients received targeted therapy; from 2014 to 2016, that figure rose to 43%; and since 2017, 61% of patients have received targeted therapy (P less than .001).
“Landmark changes in the management of ATC patients as a whole have had a direct impact to the significant increase in overall survival,” said Dr. Maniakas.
He added that the cancer center’s experience could inform future ATC guidelines. Patients with this deadliest of thyroid cancers should all have rapid molecular testing, followed by timely, targeted therapy. Clinical trial eligibility should be considered for all patients. Finally, guideline authors should take note of the ongoing favorable survival rates seen for patients receiving surgery after neoadjuvant therapy.
Dr. Maniakas reported no outside sources of funding and that he had no relevant disclosures.
SOURCE: Maniakas A et al. ATA 2019, Short Call Oral Abstract 9.
REPORTING FROM ATA 2019
Opioid-free regimen after neck dissection keeps patients comfortable
CHICAGO – Many patients with thyroid cancer can be sent home after lateral neck dissections with few or no opioids, in the experience of an institution that made a sea change in opioid prescribing practices.
Between 2012 to mid-2019, Oregon Health & Science University (OHSU), Portland, saw 243 patients who received lateral neck dissections for thyroid cancer and were opioid naive. Before a shift in prescribing practices in early 2017, 5.3% of patients were discharged without opioids after lateral neck dissections for thyroid cancer, whereas after the shift, 41.7% of patients went home on an opioid-free regimen, James Y. Lim, MD, an endocrine surgeon and assistant professor at the university, said during a poster presentation at the annual meeting of the American Thyroid Association.
The initiative, led by Maisie L. Shindo, MD, was started at the OHSU Thyroid and Parathyroid Center in late 2016 in an effort to reduce the number of opioid prescriptions in postoperative patients, Dr. Lim explained in an interview after his presentation. Dr. Shindo, coauthor of the study, directs the thyroid and parathyroid surgery department at the university.
“Before the initiative, standard postoperative pain control consisted of opioids. However, it was common for patients to mention that they did not need them at all,” said Dr. Lim. “Our prescribing practices today reflect the ability to maintain patient comfort without having to resort to opioids. We are able to keep more than 90% of our patients comfortable with a multimodal approach to pain,” he said.
Dr. Lim and colleagues used a retrospective record review to tally how many opioids were initially prescribed at discharge after lateral neck dissections for thyroid cancer, along with the number and quantity of refills for opioids after discharge. Opioid doses were converted to morphine milligram equivalents (MME), and dosing patterns were compared for the periods before and after Feb. 1, 2017, when operating surgeons changed opioid prescribing patterns. These two subgroups were termed group 1 and group 2, respectively.
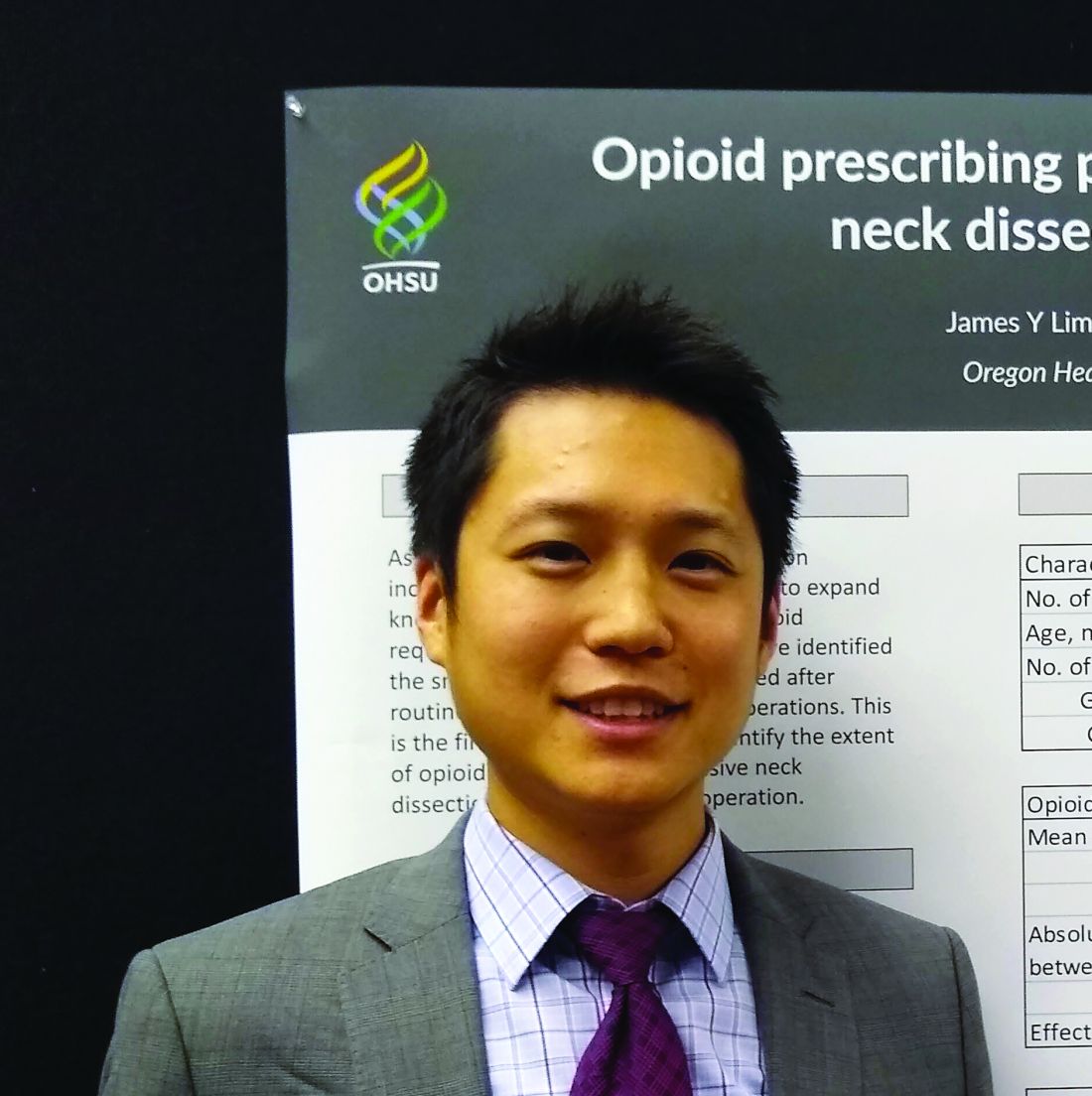
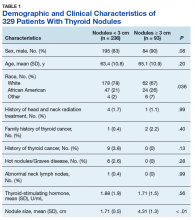
In all, 143 of the total 243 patients included in the study were women, and the mean age at the time of surgery was 47 years. Patients in group 1 had 170 surgeries, and those in group 2 had 103 surgeries.
Group 1 patients received a mean 295.4 MME after surgery, and group 2 patients received a mean 85.89 MME, though there was wide variation in discharge prescribing within each group. The absolute difference between the pre- and postinitiative groups was 209.51 MME (95% confidence interval, 157.8-261.2), for an effect size of 1.08. The MME figures for each group reflected both discharge medication and any refills or rescue prescriptions that were required.
“Decreasing the volume of opioids prescribed at discharge will decrease waste and reduce potential for addiction,” the authors noted.
As far as is known, “this is the first study that seeks to identify the extent of opioid needs after an extensive neck dissection for thyroid cancer operation,” said Dr. Lim, who added that he has been surprised at how well patients do after surgery. He said he and other surgeons had expected patients to have more pain from lateral neck dissections than they seem to experience.
“There have been studies, including from our own institution, that reported the relatively small need for opioids after a central neck procedure, such as a total thyroidectomy,” Dr. Lim said. “Our study showed that those requirements remain low even with more extensive lateral neck dissections. In the last 8 months of the study, more than 70% of patients with lateral neck dissections did not require opioids on discharge.”
Dr. Lim said that he and the rest of the care team advise patients to ramp up nonpharmacologic options, including ibuprofen, acetaminophen, ice packs, and throat lozenges – all of which can make a big difference in postoperative comfort.
Paying attention to how patients fare during an inpatient stay or even same-day procedures can help physicians estimate postdischarge needs, said Dr. Lim: “For our lateral neck dissections, patients usually stay overnight, and we can get a pretty good estimate of how their pain is being managed off opioids. For same-day procedures, it requires evaluating the patient before discharge and reassessing the pain needs at that time.”
Helping patients and their families understand the postoperative course and what level of discomfort they can expect has helped in the effort to minimize opioid use, Dr. Lim said. Overall, patients, family, and staff have received the changes “very well,” he added.
Practices that are considering a move toward opioid-free or opioid-sparing regimens after surgery should know that “it does require buy-in from all members of the medical team as well as the patients,” Dr. Lim emphasized.
“It starts at the initial surgical consultation, with surgeons educating patients on what to expect in terms of postoperative discomfort and pain. Patients are informed that they will have some discomfort and mild pain that is generally controlled with nonopioid, over-the-counter medications and cold therapy to the surgical site,” he explained.
“It requires education of the nurses and residents to encourage moving away from using opioids as a first-line therapy,” but it’s worth the hard work to get to a point where patients are going home with few, or no, opioids, said Dr. Lim. “Ultimately, patients are happier and are often relieved that their pain can be controlled without opioids,” he said.
Dr. Shindo is the senior author of a related study examining opioid reduction in neck dissection for a variety of head and neck cancers. In that study, she and her coauthors found that opioid requirements vary by cancer type. In an upcoming manuscript, the researchers are aiming to characterize typical opioid requirements for commonly performed procedures, to provide surgeons with evidence-based baselines for appropriate, but not excessive, opioid prescribing.
Dr. Lim reported no outside sources of funding. He, Dr. Shindo, and a third author reported that they had no conflicts of interest.
SOURCE: Lim J et al. ATA 2019, Poster 401.
CHICAGO – Many patients with thyroid cancer can be sent home after lateral neck dissections with few or no opioids, in the experience of an institution that made a sea change in opioid prescribing practices.
Between 2012 to mid-2019, Oregon Health & Science University (OHSU), Portland, saw 243 patients who received lateral neck dissections for thyroid cancer and were opioid naive. Before a shift in prescribing practices in early 2017, 5.3% of patients were discharged without opioids after lateral neck dissections for thyroid cancer, whereas after the shift, 41.7% of patients went home on an opioid-free regimen, James Y. Lim, MD, an endocrine surgeon and assistant professor at the university, said during a poster presentation at the annual meeting of the American Thyroid Association.
The initiative, led by Maisie L. Shindo, MD, was started at the OHSU Thyroid and Parathyroid Center in late 2016 in an effort to reduce the number of opioid prescriptions in postoperative patients, Dr. Lim explained in an interview after his presentation. Dr. Shindo, coauthor of the study, directs the thyroid and parathyroid surgery department at the university.
“Before the initiative, standard postoperative pain control consisted of opioids. However, it was common for patients to mention that they did not need them at all,” said Dr. Lim. “Our prescribing practices today reflect the ability to maintain patient comfort without having to resort to opioids. We are able to keep more than 90% of our patients comfortable with a multimodal approach to pain,” he said.
Dr. Lim and colleagues used a retrospective record review to tally how many opioids were initially prescribed at discharge after lateral neck dissections for thyroid cancer, along with the number and quantity of refills for opioids after discharge. Opioid doses were converted to morphine milligram equivalents (MME), and dosing patterns were compared for the periods before and after Feb. 1, 2017, when operating surgeons changed opioid prescribing patterns. These two subgroups were termed group 1 and group 2, respectively.
In all, 143 of the total 243 patients included in the study were women, and the mean age at the time of surgery was 47 years. Patients in group 1 had 170 surgeries, and those in group 2 had 103 surgeries.
Group 1 patients received a mean 295.4 MME after surgery, and group 2 patients received a mean 85.89 MME, though there was wide variation in discharge prescribing within each group. The absolute difference between the pre- and postinitiative groups was 209.51 MME (95% confidence interval, 157.8-261.2), for an effect size of 1.08. The MME figures for each group reflected both discharge medication and any refills or rescue prescriptions that were required.
“Decreasing the volume of opioids prescribed at discharge will decrease waste and reduce potential for addiction,” the authors noted.
As far as is known, “this is the first study that seeks to identify the extent of opioid needs after an extensive neck dissection for thyroid cancer operation,” said Dr. Lim, who added that he has been surprised at how well patients do after surgery. He said he and other surgeons had expected patients to have more pain from lateral neck dissections than they seem to experience.
“There have been studies, including from our own institution, that reported the relatively small need for opioids after a central neck procedure, such as a total thyroidectomy,” Dr. Lim said. “Our study showed that those requirements remain low even with more extensive lateral neck dissections. In the last 8 months of the study, more than 70% of patients with lateral neck dissections did not require opioids on discharge.”
Dr. Lim said that he and the rest of the care team advise patients to ramp up nonpharmacologic options, including ibuprofen, acetaminophen, ice packs, and throat lozenges – all of which can make a big difference in postoperative comfort.
Paying attention to how patients fare during an inpatient stay or even same-day procedures can help physicians estimate postdischarge needs, said Dr. Lim: “For our lateral neck dissections, patients usually stay overnight, and we can get a pretty good estimate of how their pain is being managed off opioids. For same-day procedures, it requires evaluating the patient before discharge and reassessing the pain needs at that time.”
Helping patients and their families understand the postoperative course and what level of discomfort they can expect has helped in the effort to minimize opioid use, Dr. Lim said. Overall, patients, family, and staff have received the changes “very well,” he added.
Practices that are considering a move toward opioid-free or opioid-sparing regimens after surgery should know that “it does require buy-in from all members of the medical team as well as the patients,” Dr. Lim emphasized.
“It starts at the initial surgical consultation, with surgeons educating patients on what to expect in terms of postoperative discomfort and pain. Patients are informed that they will have some discomfort and mild pain that is generally controlled with nonopioid, over-the-counter medications and cold therapy to the surgical site,” he explained.
“It requires education of the nurses and residents to encourage moving away from using opioids as a first-line therapy,” but it’s worth the hard work to get to a point where patients are going home with few, or no, opioids, said Dr. Lim. “Ultimately, patients are happier and are often relieved that their pain can be controlled without opioids,” he said.
Dr. Shindo is the senior author of a related study examining opioid reduction in neck dissection for a variety of head and neck cancers. In that study, she and her coauthors found that opioid requirements vary by cancer type. In an upcoming manuscript, the researchers are aiming to characterize typical opioid requirements for commonly performed procedures, to provide surgeons with evidence-based baselines for appropriate, but not excessive, opioid prescribing.
Dr. Lim reported no outside sources of funding. He, Dr. Shindo, and a third author reported that they had no conflicts of interest.
SOURCE: Lim J et al. ATA 2019, Poster 401.
CHICAGO – Many patients with thyroid cancer can be sent home after lateral neck dissections with few or no opioids, in the experience of an institution that made a sea change in opioid prescribing practices.
Between 2012 to mid-2019, Oregon Health & Science University (OHSU), Portland, saw 243 patients who received lateral neck dissections for thyroid cancer and were opioid naive. Before a shift in prescribing practices in early 2017, 5.3% of patients were discharged without opioids after lateral neck dissections for thyroid cancer, whereas after the shift, 41.7% of patients went home on an opioid-free regimen, James Y. Lim, MD, an endocrine surgeon and assistant professor at the university, said during a poster presentation at the annual meeting of the American Thyroid Association.
The initiative, led by Maisie L. Shindo, MD, was started at the OHSU Thyroid and Parathyroid Center in late 2016 in an effort to reduce the number of opioid prescriptions in postoperative patients, Dr. Lim explained in an interview after his presentation. Dr. Shindo, coauthor of the study, directs the thyroid and parathyroid surgery department at the university.
“Before the initiative, standard postoperative pain control consisted of opioids. However, it was common for patients to mention that they did not need them at all,” said Dr. Lim. “Our prescribing practices today reflect the ability to maintain patient comfort without having to resort to opioids. We are able to keep more than 90% of our patients comfortable with a multimodal approach to pain,” he said.
Dr. Lim and colleagues used a retrospective record review to tally how many opioids were initially prescribed at discharge after lateral neck dissections for thyroid cancer, along with the number and quantity of refills for opioids after discharge. Opioid doses were converted to morphine milligram equivalents (MME), and dosing patterns were compared for the periods before and after Feb. 1, 2017, when operating surgeons changed opioid prescribing patterns. These two subgroups were termed group 1 and group 2, respectively.
In all, 143 of the total 243 patients included in the study were women, and the mean age at the time of surgery was 47 years. Patients in group 1 had 170 surgeries, and those in group 2 had 103 surgeries.
Group 1 patients received a mean 295.4 MME after surgery, and group 2 patients received a mean 85.89 MME, though there was wide variation in discharge prescribing within each group. The absolute difference between the pre- and postinitiative groups was 209.51 MME (95% confidence interval, 157.8-261.2), for an effect size of 1.08. The MME figures for each group reflected both discharge medication and any refills or rescue prescriptions that were required.
“Decreasing the volume of opioids prescribed at discharge will decrease waste and reduce potential for addiction,” the authors noted.
As far as is known, “this is the first study that seeks to identify the extent of opioid needs after an extensive neck dissection for thyroid cancer operation,” said Dr. Lim, who added that he has been surprised at how well patients do after surgery. He said he and other surgeons had expected patients to have more pain from lateral neck dissections than they seem to experience.
“There have been studies, including from our own institution, that reported the relatively small need for opioids after a central neck procedure, such as a total thyroidectomy,” Dr. Lim said. “Our study showed that those requirements remain low even with more extensive lateral neck dissections. In the last 8 months of the study, more than 70% of patients with lateral neck dissections did not require opioids on discharge.”
Dr. Lim said that he and the rest of the care team advise patients to ramp up nonpharmacologic options, including ibuprofen, acetaminophen, ice packs, and throat lozenges – all of which can make a big difference in postoperative comfort.
Paying attention to how patients fare during an inpatient stay or even same-day procedures can help physicians estimate postdischarge needs, said Dr. Lim: “For our lateral neck dissections, patients usually stay overnight, and we can get a pretty good estimate of how their pain is being managed off opioids. For same-day procedures, it requires evaluating the patient before discharge and reassessing the pain needs at that time.”
Helping patients and their families understand the postoperative course and what level of discomfort they can expect has helped in the effort to minimize opioid use, Dr. Lim said. Overall, patients, family, and staff have received the changes “very well,” he added.
Practices that are considering a move toward opioid-free or opioid-sparing regimens after surgery should know that “it does require buy-in from all members of the medical team as well as the patients,” Dr. Lim emphasized.
“It starts at the initial surgical consultation, with surgeons educating patients on what to expect in terms of postoperative discomfort and pain. Patients are informed that they will have some discomfort and mild pain that is generally controlled with nonopioid, over-the-counter medications and cold therapy to the surgical site,” he explained.
“It requires education of the nurses and residents to encourage moving away from using opioids as a first-line therapy,” but it’s worth the hard work to get to a point where patients are going home with few, or no, opioids, said Dr. Lim. “Ultimately, patients are happier and are often relieved that their pain can be controlled without opioids,” he said.
Dr. Shindo is the senior author of a related study examining opioid reduction in neck dissection for a variety of head and neck cancers. In that study, she and her coauthors found that opioid requirements vary by cancer type. In an upcoming manuscript, the researchers are aiming to characterize typical opioid requirements for commonly performed procedures, to provide surgeons with evidence-based baselines for appropriate, but not excessive, opioid prescribing.
Dr. Lim reported no outside sources of funding. He, Dr. Shindo, and a third author reported that they had no conflicts of interest.
SOURCE: Lim J et al. ATA 2019, Poster 401.
REPORTING FROM ATA 2019
Toward Improving the Delivery of Oral Anticancer Drugs in the VA: Work IN PROGRESS
Purpose: An Innovation Network Spark award was received to develop “My Chemo Calendar,” a tool aimed at providing veterans with easy to understand critical information (eg drug name, schedule, side effects), to optimize the benefits of their oral anticancer drugs (OADs). Using a human-centered design approach, we are first obtaining insight from patients and providers on tools (including “my Chemo Calendar”) and strategies that may improve experiences with OADs.
Background: OADs often have complex dosing schedules, toxicity risk, and special handling precautions. Best tools and practices for ensuring safe and effective care for veterans who are prescribed OADs are not yet well established.
Methods: Surveys, focus groups, and semi-structured interviews are being conducted with patients and providers. Topics included: OAD education and knowledge, medication handling and adherence, and symptom management.
Data Analysis: Descriptive statistics will be used to summarize the survey data. Audio files from focus groups and semi-structured interviews will be transcribed and analyzed using NVivo.
Results: To date, data has been collected from two patients and eighteen oncology care providers. Both patients were ‘very satisfied’ with the information they received to successfully and safely take their OADs. They preferred to receive information from multiple sources (eg physician, internet, hand-outs). The majority of providers reported that they never/rarely/sometimes spoke about digesting an OAD with/without food, necessary diet modifications (e.g. no grapefruit), missed doses, medication storage temperatures, and refills. Most usually spoke about side effects, timing (eg morning), adverse effects, phone number to report side effects, and reporting concerning symptoms. Most were not/slightly/moderately confident that the patients were receiving all the necessary instructions to use the OAD properly. The oncology pharmacist was identified as the most appropriate oncology team member to provide patient education. Although, it was noted that it would be best for patients to receive information at various touch points from different team members. The concept of “My Chemo Calendar” was well received but how best to integrate it into care was unclear.
Implications: Data collection and analysis is still ongoing. This information will be used create and pilot new strategies and tools to improve experiences with OADs.
Purpose: An Innovation Network Spark award was received to develop “My Chemo Calendar,” a tool aimed at providing veterans with easy to understand critical information (eg drug name, schedule, side effects), to optimize the benefits of their oral anticancer drugs (OADs). Using a human-centered design approach, we are first obtaining insight from patients and providers on tools (including “my Chemo Calendar”) and strategies that may improve experiences with OADs.
Background: OADs often have complex dosing schedules, toxicity risk, and special handling precautions. Best tools and practices for ensuring safe and effective care for veterans who are prescribed OADs are not yet well established.
Methods: Surveys, focus groups, and semi-structured interviews are being conducted with patients and providers. Topics included: OAD education and knowledge, medication handling and adherence, and symptom management.
Data Analysis: Descriptive statistics will be used to summarize the survey data. Audio files from focus groups and semi-structured interviews will be transcribed and analyzed using NVivo.
Results: To date, data has been collected from two patients and eighteen oncology care providers. Both patients were ‘very satisfied’ with the information they received to successfully and safely take their OADs. They preferred to receive information from multiple sources (eg physician, internet, hand-outs). The majority of providers reported that they never/rarely/sometimes spoke about digesting an OAD with/without food, necessary diet modifications (e.g. no grapefruit), missed doses, medication storage temperatures, and refills. Most usually spoke about side effects, timing (eg morning), adverse effects, phone number to report side effects, and reporting concerning symptoms. Most were not/slightly/moderately confident that the patients were receiving all the necessary instructions to use the OAD properly. The oncology pharmacist was identified as the most appropriate oncology team member to provide patient education. Although, it was noted that it would be best for patients to receive information at various touch points from different team members. The concept of “My Chemo Calendar” was well received but how best to integrate it into care was unclear.
Implications: Data collection and analysis is still ongoing. This information will be used create and pilot new strategies and tools to improve experiences with OADs.
Purpose: An Innovation Network Spark award was received to develop “My Chemo Calendar,” a tool aimed at providing veterans with easy to understand critical information (eg drug name, schedule, side effects), to optimize the benefits of their oral anticancer drugs (OADs). Using a human-centered design approach, we are first obtaining insight from patients and providers on tools (including “my Chemo Calendar”) and strategies that may improve experiences with OADs.
Background: OADs often have complex dosing schedules, toxicity risk, and special handling precautions. Best tools and practices for ensuring safe and effective care for veterans who are prescribed OADs are not yet well established.
Methods: Surveys, focus groups, and semi-structured interviews are being conducted with patients and providers. Topics included: OAD education and knowledge, medication handling and adherence, and symptom management.
Data Analysis: Descriptive statistics will be used to summarize the survey data. Audio files from focus groups and semi-structured interviews will be transcribed and analyzed using NVivo.
Results: To date, data has been collected from two patients and eighteen oncology care providers. Both patients were ‘very satisfied’ with the information they received to successfully and safely take their OADs. They preferred to receive information from multiple sources (eg physician, internet, hand-outs). The majority of providers reported that they never/rarely/sometimes spoke about digesting an OAD with/without food, necessary diet modifications (e.g. no grapefruit), missed doses, medication storage temperatures, and refills. Most usually spoke about side effects, timing (eg morning), adverse effects, phone number to report side effects, and reporting concerning symptoms. Most were not/slightly/moderately confident that the patients were receiving all the necessary instructions to use the OAD properly. The oncology pharmacist was identified as the most appropriate oncology team member to provide patient education. Although, it was noted that it would be best for patients to receive information at various touch points from different team members. The concept of “My Chemo Calendar” was well received but how best to integrate it into care was unclear.
Implications: Data collection and analysis is still ongoing. This information will be used create and pilot new strategies and tools to improve experiences with OADs.
Evaluation of the Implementation of a 90-Minute Rituximab Infusion Protocol at the Richard L. Roudebush VA Medical Center
Background: The utilization of rituximab for a variety of different indications has historically been associated with logistical challenges related to time and labor. Institutions across the country have implemented protocols to shorten the infusion time of rituximab in order to help alleviate these challenges. The purpose of this study was to support the safe implementation of a 90-minute rapid infusion protocol for rituximab at the Richard L. Roudebush VA Medical Center and improve staff perception regarding similar initiatives in the future with other therapies.
Methods: Proactive measures were taken to educate physicians, pharmacists, and nurses about their role in the implementation of the protocol. A weekly report of patients receiving rituximab was generated from November 1st, 2018 to April 1st, 2019. Patients were then screened for future eligibility for rapid infusions of the drug based on prespecified criteria and providers were notified regarding potential candidates. After patients received their rapid infusions, a retrospective chart review was performed to evaluate patient tolerability and assess for any safety concerns.
Data Analysis: The primary endpoint for this study was the incidence of grade 3 and 4 infusion related reactions associated with the rapid infusions of rituximab based on criteria from CTCAE version 5.0. Secondary endpoints were savings in infusion clinic chair time and the proportion of patients experiencing a grade 3 or 4 infusion related reaction to the rapid infusion that received proper treatment according to the institution’s hypersensitivity protocol. All endpoints were analyzed using descriptive statistics.
Results: During the study period, 11 patients received a total of 24 rapid infusions of rituximab. One out of 24 infusions (4.17%) resulted in a grade 3 infusion related reaction. This patient was treated appropriately by nurses according to the institution’s hypersensitivity protocol. The average savings in infusion clinic chair time by rapid infusions was 39.3 minutes.
Conclusion: This study proved that a rapid infusion protocol for rituximab can be successfully implemented at the Richard L. Roudebush VA Medical Center. The proactive measures utilized to implement the protocol improved provider prescribing rates and nursing satisfaction. Future plans involve implementing a rapid infusion protocol for daratumumab.
Background: The utilization of rituximab for a variety of different indications has historically been associated with logistical challenges related to time and labor. Institutions across the country have implemented protocols to shorten the infusion time of rituximab in order to help alleviate these challenges. The purpose of this study was to support the safe implementation of a 90-minute rapid infusion protocol for rituximab at the Richard L. Roudebush VA Medical Center and improve staff perception regarding similar initiatives in the future with other therapies.
Methods: Proactive measures were taken to educate physicians, pharmacists, and nurses about their role in the implementation of the protocol. A weekly report of patients receiving rituximab was generated from November 1st, 2018 to April 1st, 2019. Patients were then screened for future eligibility for rapid infusions of the drug based on prespecified criteria and providers were notified regarding potential candidates. After patients received their rapid infusions, a retrospective chart review was performed to evaluate patient tolerability and assess for any safety concerns.
Data Analysis: The primary endpoint for this study was the incidence of grade 3 and 4 infusion related reactions associated with the rapid infusions of rituximab based on criteria from CTCAE version 5.0. Secondary endpoints were savings in infusion clinic chair time and the proportion of patients experiencing a grade 3 or 4 infusion related reaction to the rapid infusion that received proper treatment according to the institution’s hypersensitivity protocol. All endpoints were analyzed using descriptive statistics.
Results: During the study period, 11 patients received a total of 24 rapid infusions of rituximab. One out of 24 infusions (4.17%) resulted in a grade 3 infusion related reaction. This patient was treated appropriately by nurses according to the institution’s hypersensitivity protocol. The average savings in infusion clinic chair time by rapid infusions was 39.3 minutes.
Conclusion: This study proved that a rapid infusion protocol for rituximab can be successfully implemented at the Richard L. Roudebush VA Medical Center. The proactive measures utilized to implement the protocol improved provider prescribing rates and nursing satisfaction. Future plans involve implementing a rapid infusion protocol for daratumumab.
Background: The utilization of rituximab for a variety of different indications has historically been associated with logistical challenges related to time and labor. Institutions across the country have implemented protocols to shorten the infusion time of rituximab in order to help alleviate these challenges. The purpose of this study was to support the safe implementation of a 90-minute rapid infusion protocol for rituximab at the Richard L. Roudebush VA Medical Center and improve staff perception regarding similar initiatives in the future with other therapies.
Methods: Proactive measures were taken to educate physicians, pharmacists, and nurses about their role in the implementation of the protocol. A weekly report of patients receiving rituximab was generated from November 1st, 2018 to April 1st, 2019. Patients were then screened for future eligibility for rapid infusions of the drug based on prespecified criteria and providers were notified regarding potential candidates. After patients received their rapid infusions, a retrospective chart review was performed to evaluate patient tolerability and assess for any safety concerns.
Data Analysis: The primary endpoint for this study was the incidence of grade 3 and 4 infusion related reactions associated with the rapid infusions of rituximab based on criteria from CTCAE version 5.0. Secondary endpoints were savings in infusion clinic chair time and the proportion of patients experiencing a grade 3 or 4 infusion related reaction to the rapid infusion that received proper treatment according to the institution’s hypersensitivity protocol. All endpoints were analyzed using descriptive statistics.
Results: During the study period, 11 patients received a total of 24 rapid infusions of rituximab. One out of 24 infusions (4.17%) resulted in a grade 3 infusion related reaction. This patient was treated appropriately by nurses according to the institution’s hypersensitivity protocol. The average savings in infusion clinic chair time by rapid infusions was 39.3 minutes.
Conclusion: This study proved that a rapid infusion protocol for rituximab can be successfully implemented at the Richard L. Roudebush VA Medical Center. The proactive measures utilized to implement the protocol improved provider prescribing rates and nursing satisfaction. Future plans involve implementing a rapid infusion protocol for daratumumab.
Improving Oral Chemotherapy Documentation Using QOPI Audit, Plan-Do-Study-Act Cycles, and the Electronic Medical Record
Background: The use of oral chemotherapy in cancer patients continues to increase and proper documentation of patient adherence, duration of treatment and side effects while on these medications is important. The Quality Oncology Practice Initiative (QOPI) identified oral chemotherapy documentation as an area in need of improvement.
Methods: We used the QOPI audit to create a quality improvement project with the goal of improving our provider oral chemotherapy documentation including cycle number, adherence and side effects. An existing oral chemotherapy best practice alert template in our electronic medical record had already been created to help our providers document oral chemotherapy administration, and we sought to improve our documentation by increasing our provider compliance in completing this template. We utilized Plan-Do-Study- Act (PDSA) cycles to accomplish our goal. For the first PDSA cycle, we made bypassing the oral chemotherapy documentation template in our electronic medical record more difficult for our providers. Our providers were required to acknowledge the template by either following the link to complete the template or documenting a reason why the template was not completed. Requiring the provider to document a reason why the template was not completed made bypassing the template more difficult.
Results: By making this change to the template, we successfully improved our provider compliance with following the link to complete the template from 38% (83/220) to 71% (121/169). For the second PDSA cycle, we educated our medical oncology providers via email about the importance of utilizing the template to improve our oral chemotherapy documentation. By educating our providers, we improved our provider compliance with following the link to complete the template to 86.5% (155/179).
Conclusion: Our project showed how the QOPI audit can be used to create a quality improvement project. Our project also demonstrated how templates within the electronic medical record can be utilized to complete a successful quality improvement project.
Background: The use of oral chemotherapy in cancer patients continues to increase and proper documentation of patient adherence, duration of treatment and side effects while on these medications is important. The Quality Oncology Practice Initiative (QOPI) identified oral chemotherapy documentation as an area in need of improvement.
Methods: We used the QOPI audit to create a quality improvement project with the goal of improving our provider oral chemotherapy documentation including cycle number, adherence and side effects. An existing oral chemotherapy best practice alert template in our electronic medical record had already been created to help our providers document oral chemotherapy administration, and we sought to improve our documentation by increasing our provider compliance in completing this template. We utilized Plan-Do-Study- Act (PDSA) cycles to accomplish our goal. For the first PDSA cycle, we made bypassing the oral chemotherapy documentation template in our electronic medical record more difficult for our providers. Our providers were required to acknowledge the template by either following the link to complete the template or documenting a reason why the template was not completed. Requiring the provider to document a reason why the template was not completed made bypassing the template more difficult.
Results: By making this change to the template, we successfully improved our provider compliance with following the link to complete the template from 38% (83/220) to 71% (121/169). For the second PDSA cycle, we educated our medical oncology providers via email about the importance of utilizing the template to improve our oral chemotherapy documentation. By educating our providers, we improved our provider compliance with following the link to complete the template to 86.5% (155/179).
Conclusion: Our project showed how the QOPI audit can be used to create a quality improvement project. Our project also demonstrated how templates within the electronic medical record can be utilized to complete a successful quality improvement project.
Background: The use of oral chemotherapy in cancer patients continues to increase and proper documentation of patient adherence, duration of treatment and side effects while on these medications is important. The Quality Oncology Practice Initiative (QOPI) identified oral chemotherapy documentation as an area in need of improvement.
Methods: We used the QOPI audit to create a quality improvement project with the goal of improving our provider oral chemotherapy documentation including cycle number, adherence and side effects. An existing oral chemotherapy best practice alert template in our electronic medical record had already been created to help our providers document oral chemotherapy administration, and we sought to improve our documentation by increasing our provider compliance in completing this template. We utilized Plan-Do-Study- Act (PDSA) cycles to accomplish our goal. For the first PDSA cycle, we made bypassing the oral chemotherapy documentation template in our electronic medical record more difficult for our providers. Our providers were required to acknowledge the template by either following the link to complete the template or documenting a reason why the template was not completed. Requiring the provider to document a reason why the template was not completed made bypassing the template more difficult.
Results: By making this change to the template, we successfully improved our provider compliance with following the link to complete the template from 38% (83/220) to 71% (121/169). For the second PDSA cycle, we educated our medical oncology providers via email about the importance of utilizing the template to improve our oral chemotherapy documentation. By educating our providers, we improved our provider compliance with following the link to complete the template to 86.5% (155/179).
Conclusion: Our project showed how the QOPI audit can be used to create a quality improvement project. Our project also demonstrated how templates within the electronic medical record can be utilized to complete a successful quality improvement project.
Radiation Therapy Treatment Breaks and Weight Changes in Head and Neck Cancer Patients in a Veterans Affairs Radiation Oncology Clinic
Background: Unplanned radiation treatment breaks are shown to be related to increased risk of local recurrence, lower survival rates and reduced tumor control rates. Weight loss, along with other side effects, can be a major factor in radiation treatment breaks. This quality improvement project aimed to review weight changes and treatment breaks via retrospective chart review to better understand how to improve the combined nutritional and radiation oncology care of head and neck cancer (HNC) patients.
Methods: Utilizing the Lean Six Sigma Project Management approach to ensure critical components were assessed, this quality improvement project reviewed HNC cases via retrospective chart review that started and/or completed definitive radiation treatment from January 1, 2014 - December 31, 2018. Weights were assessed during the timeframe of treatment and limited to weights obtained within the same unit. Treatment breaks were confirmed via Electronic Medical Records (EMR) systems and defined as one or more missed or cancelled treatments, excluding those missed for nonclinical reasons. Charts were reviewed for documented dysphagia, mucositis, and skin reactions. Information on nutrition visits were assessed.
Results: The incidence of patients who experienced treatment breaks was 47.8%. Patients averaged 5.5 missed treatments. More than half of the patients who experienced treatment breaks had Stage IV disease and 62.5% experienced clinically significant weight loss within their treatment time frame. Approximately 15% of patients were seen within a designated oncology nutrition clinic. Side effects, such as mucositis, dysphagia, and skin reactions, were documented to have contributed to weight changes and treatment breaks.
Conclusion: This project highlighted the multifactorial nature associated with radiotherapy treatment of HNC patients. Based on prior experience with integration of nutrition and radiation oncology services and understanding expected treatment side effects, we recommend that nutrition services are integrated as part of the initial radiation consultation process to proactively approach the known weight loss and nutritionally relevant side effects. It is imperative to integrate medical informatics infrastructure to modernize the process of documenting treatment side effects and outcomes. Continued in-depth review of this data will facilitate us in creating a comprehensive multidisciplinary treatment approach for HNC patients undergoing radiation therapy.
Background: Unplanned radiation treatment breaks are shown to be related to increased risk of local recurrence, lower survival rates and reduced tumor control rates. Weight loss, along with other side effects, can be a major factor in radiation treatment breaks. This quality improvement project aimed to review weight changes and treatment breaks via retrospective chart review to better understand how to improve the combined nutritional and radiation oncology care of head and neck cancer (HNC) patients.
Methods: Utilizing the Lean Six Sigma Project Management approach to ensure critical components were assessed, this quality improvement project reviewed HNC cases via retrospective chart review that started and/or completed definitive radiation treatment from January 1, 2014 - December 31, 2018. Weights were assessed during the timeframe of treatment and limited to weights obtained within the same unit. Treatment breaks were confirmed via Electronic Medical Records (EMR) systems and defined as one or more missed or cancelled treatments, excluding those missed for nonclinical reasons. Charts were reviewed for documented dysphagia, mucositis, and skin reactions. Information on nutrition visits were assessed.
Results: The incidence of patients who experienced treatment breaks was 47.8%. Patients averaged 5.5 missed treatments. More than half of the patients who experienced treatment breaks had Stage IV disease and 62.5% experienced clinically significant weight loss within their treatment time frame. Approximately 15% of patients were seen within a designated oncology nutrition clinic. Side effects, such as mucositis, dysphagia, and skin reactions, were documented to have contributed to weight changes and treatment breaks.
Conclusion: This project highlighted the multifactorial nature associated with radiotherapy treatment of HNC patients. Based on prior experience with integration of nutrition and radiation oncology services and understanding expected treatment side effects, we recommend that nutrition services are integrated as part of the initial radiation consultation process to proactively approach the known weight loss and nutritionally relevant side effects. It is imperative to integrate medical informatics infrastructure to modernize the process of documenting treatment side effects and outcomes. Continued in-depth review of this data will facilitate us in creating a comprehensive multidisciplinary treatment approach for HNC patients undergoing radiation therapy.
Background: Unplanned radiation treatment breaks are shown to be related to increased risk of local recurrence, lower survival rates and reduced tumor control rates. Weight loss, along with other side effects, can be a major factor in radiation treatment breaks. This quality improvement project aimed to review weight changes and treatment breaks via retrospective chart review to better understand how to improve the combined nutritional and radiation oncology care of head and neck cancer (HNC) patients.
Methods: Utilizing the Lean Six Sigma Project Management approach to ensure critical components were assessed, this quality improvement project reviewed HNC cases via retrospective chart review that started and/or completed definitive radiation treatment from January 1, 2014 - December 31, 2018. Weights were assessed during the timeframe of treatment and limited to weights obtained within the same unit. Treatment breaks were confirmed via Electronic Medical Records (EMR) systems and defined as one or more missed or cancelled treatments, excluding those missed for nonclinical reasons. Charts were reviewed for documented dysphagia, mucositis, and skin reactions. Information on nutrition visits were assessed.
Results: The incidence of patients who experienced treatment breaks was 47.8%. Patients averaged 5.5 missed treatments. More than half of the patients who experienced treatment breaks had Stage IV disease and 62.5% experienced clinically significant weight loss within their treatment time frame. Approximately 15% of patients were seen within a designated oncology nutrition clinic. Side effects, such as mucositis, dysphagia, and skin reactions, were documented to have contributed to weight changes and treatment breaks.
Conclusion: This project highlighted the multifactorial nature associated with radiotherapy treatment of HNC patients. Based on prior experience with integration of nutrition and radiation oncology services and understanding expected treatment side effects, we recommend that nutrition services are integrated as part of the initial radiation consultation process to proactively approach the known weight loss and nutritionally relevant side effects. It is imperative to integrate medical informatics infrastructure to modernize the process of documenting treatment side effects and outcomes. Continued in-depth review of this data will facilitate us in creating a comprehensive multidisciplinary treatment approach for HNC patients undergoing radiation therapy.
Benefits of Psychosocial Participation in a Head and Neck Cancer Tumor Board at the VA Palo Alto Health Care System: Two Case Examples
Background: Multidisciplinary tumor boards (MTBs) have been shown to positively impact the assessment and treatment of cancer patients (Pillay et al, 2016) and increase referrals to specialty services present at the meetings (eg genetic testing in breast cancer, Cohen et al, 2016). However, no research to date has explored the impact of involvement of psychosocial providers on MTBs. The following two cases are presented as examples of multidisciplinary cancer care that was facilitated by psychology/social work involvement in the Head and Neck Cancer MTB at VAPAHCS.
Case Report 1: Mr. T is an 86-year-old veteran who was referred to the Oncology and ENT services in May 2017 for a recurrent squamous cell carcinoma in the neck, presumably from prior lip primary. The patient evaluated by Oncology, KC, and ENT who recommended surgical resection. The veteran consented but later cancelled his surgery due to beliefs that God would cure him. The MTB reviewed his case, and the veteran agreed to return for a visit to the Oncology clinic. SD met with the veteran first, and then accompanied him to a meeting with the Oncologist who arranged a same day appointment with an ENT surgeon and an anesthesiologist. SD integrated the veteran’s belief systems (eg, that God would cure his cancer) to help facilitate his decisions. The veteran’s surgery was expedited and completed 3 days later. At present, he has no evidence of recurrent disease.
Case Report 2: Mr. M is a 62-year-old veteran who was referred to the ENT and Oncology Services in October 2017 for squamous cell carcinoma of base of tongue. He was first seen by ENT, discussed in MTB, then seen by KC and BA. Significant psychosocial issues were identified that could complicate his care, including homelessness and PTSD symptoms that directly impacted his ability to stay in VA housing and interact with the medical system. A multidisciplinary treatment plan was created to meet the veteran’s housing/ hygiene needs and provide interventions to assist him in managing PTSD symptoms enough to proceed through treatment. The veteran was able to complete treatment, has no evidence of recurrent disease, and has returned to his goal of hiking the Pacific Crest.
Background: Multidisciplinary tumor boards (MTBs) have been shown to positively impact the assessment and treatment of cancer patients (Pillay et al, 2016) and increase referrals to specialty services present at the meetings (eg genetic testing in breast cancer, Cohen et al, 2016). However, no research to date has explored the impact of involvement of psychosocial providers on MTBs. The following two cases are presented as examples of multidisciplinary cancer care that was facilitated by psychology/social work involvement in the Head and Neck Cancer MTB at VAPAHCS.
Case Report 1: Mr. T is an 86-year-old veteran who was referred to the Oncology and ENT services in May 2017 for a recurrent squamous cell carcinoma in the neck, presumably from prior lip primary. The patient evaluated by Oncology, KC, and ENT who recommended surgical resection. The veteran consented but later cancelled his surgery due to beliefs that God would cure him. The MTB reviewed his case, and the veteran agreed to return for a visit to the Oncology clinic. SD met with the veteran first, and then accompanied him to a meeting with the Oncologist who arranged a same day appointment with an ENT surgeon and an anesthesiologist. SD integrated the veteran’s belief systems (eg, that God would cure his cancer) to help facilitate his decisions. The veteran’s surgery was expedited and completed 3 days later. At present, he has no evidence of recurrent disease.
Case Report 2: Mr. M is a 62-year-old veteran who was referred to the ENT and Oncology Services in October 2017 for squamous cell carcinoma of base of tongue. He was first seen by ENT, discussed in MTB, then seen by KC and BA. Significant psychosocial issues were identified that could complicate his care, including homelessness and PTSD symptoms that directly impacted his ability to stay in VA housing and interact with the medical system. A multidisciplinary treatment plan was created to meet the veteran’s housing/ hygiene needs and provide interventions to assist him in managing PTSD symptoms enough to proceed through treatment. The veteran was able to complete treatment, has no evidence of recurrent disease, and has returned to his goal of hiking the Pacific Crest.
Background: Multidisciplinary tumor boards (MTBs) have been shown to positively impact the assessment and treatment of cancer patients (Pillay et al, 2016) and increase referrals to specialty services present at the meetings (eg genetic testing in breast cancer, Cohen et al, 2016). However, no research to date has explored the impact of involvement of psychosocial providers on MTBs. The following two cases are presented as examples of multidisciplinary cancer care that was facilitated by psychology/social work involvement in the Head and Neck Cancer MTB at VAPAHCS.
Case Report 1: Mr. T is an 86-year-old veteran who was referred to the Oncology and ENT services in May 2017 for a recurrent squamous cell carcinoma in the neck, presumably from prior lip primary. The patient evaluated by Oncology, KC, and ENT who recommended surgical resection. The veteran consented but later cancelled his surgery due to beliefs that God would cure him. The MTB reviewed his case, and the veteran agreed to return for a visit to the Oncology clinic. SD met with the veteran first, and then accompanied him to a meeting with the Oncologist who arranged a same day appointment with an ENT surgeon and an anesthesiologist. SD integrated the veteran’s belief systems (eg, that God would cure his cancer) to help facilitate his decisions. The veteran’s surgery was expedited and completed 3 days later. At present, he has no evidence of recurrent disease.
Case Report 2: Mr. M is a 62-year-old veteran who was referred to the ENT and Oncology Services in October 2017 for squamous cell carcinoma of base of tongue. He was first seen by ENT, discussed in MTB, then seen by KC and BA. Significant psychosocial issues were identified that could complicate his care, including homelessness and PTSD symptoms that directly impacted his ability to stay in VA housing and interact with the medical system. A multidisciplinary treatment plan was created to meet the veteran’s housing/ hygiene needs and provide interventions to assist him in managing PTSD symptoms enough to proceed through treatment. The veteran was able to complete treatment, has no evidence of recurrent disease, and has returned to his goal of hiking the Pacific Crest.
Immune-related toxicities, hospitalization common with checkpoint inhibitor therapy
, according to a retrospective cohort study.
In addition, the majority of the immune-related toxicities were high-grade events of grade 3 or higher (65%), necessitated multidisciplinary care (91%), and eventually improved or resolved (65%). The results highlight potential risk factors for hospitalizations due to immune-related toxicities in oncology patients.
“[We aimed to] characterize the spectrum of toxicities, management, and outcomes of hospitalizations for immune-related adverse events,” wrote Aanika Balaji, BS, of Johns Hopkins University, Baltimore, and colleagues. The findings were reported in the Journal of Oncology Practice.
The researchers studied 443 patients admitted to solid tumor oncology service at an oncology center over a period of 6-months. Of these, 100 patients had at any point received checkpoint inhibitor therapy.
The proportion of hospital admissions for patients with confirmed immune-related toxicities and associations between hospitalizations due to immune-related toxicity and patient characteristics were assessed by the team. Nearly half of the patients admitted with immune-related toxicities had thoracic or head and neck cancers.
In the analysis, patients treated with combination checkpoint inhibitor therapy (odds ratio, 6.8; 95% confidence interval, 2.0-23.2), in addition to those aged 65 years and over (OR, 5.4; 95% CI, 1.6-17.8), were more likely to be hospitalized for immune-related toxicities.
Overall, 5% of all hospitalizations were the result of immune-related toxicities. Furthermore, 87% of patients discontinued checkpoint inhibitor therapy post discharge.
“We found that the most common immune-related adverse events warranting hospital admission were pneumonitis (26%) and colitis (17%),” they wrote.
The researchers acknowledged two key limitations of the study were the small sample size and lack of generalizability in community settings. Future studies that include patients from community oncology settings could improve the generalizability of the results.
“These data indicate potential risk factors for immune-related adverse event hospitalization and are likely to indicate future service needs” they concluded.
Financial support was provided by Jarushka Naidoo. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Compugen, Genentech, GlaxoSmithKline, Exelixis, MedImmune, and several others.
SOURCE: Balaji A et al. J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703.
, according to a retrospective cohort study.
In addition, the majority of the immune-related toxicities were high-grade events of grade 3 or higher (65%), necessitated multidisciplinary care (91%), and eventually improved or resolved (65%). The results highlight potential risk factors for hospitalizations due to immune-related toxicities in oncology patients.
“[We aimed to] characterize the spectrum of toxicities, management, and outcomes of hospitalizations for immune-related adverse events,” wrote Aanika Balaji, BS, of Johns Hopkins University, Baltimore, and colleagues. The findings were reported in the Journal of Oncology Practice.
The researchers studied 443 patients admitted to solid tumor oncology service at an oncology center over a period of 6-months. Of these, 100 patients had at any point received checkpoint inhibitor therapy.
The proportion of hospital admissions for patients with confirmed immune-related toxicities and associations between hospitalizations due to immune-related toxicity and patient characteristics were assessed by the team. Nearly half of the patients admitted with immune-related toxicities had thoracic or head and neck cancers.
In the analysis, patients treated with combination checkpoint inhibitor therapy (odds ratio, 6.8; 95% confidence interval, 2.0-23.2), in addition to those aged 65 years and over (OR, 5.4; 95% CI, 1.6-17.8), were more likely to be hospitalized for immune-related toxicities.
Overall, 5% of all hospitalizations were the result of immune-related toxicities. Furthermore, 87% of patients discontinued checkpoint inhibitor therapy post discharge.
“We found that the most common immune-related adverse events warranting hospital admission were pneumonitis (26%) and colitis (17%),” they wrote.
The researchers acknowledged two key limitations of the study were the small sample size and lack of generalizability in community settings. Future studies that include patients from community oncology settings could improve the generalizability of the results.
“These data indicate potential risk factors for immune-related adverse event hospitalization and are likely to indicate future service needs” they concluded.
Financial support was provided by Jarushka Naidoo. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Compugen, Genentech, GlaxoSmithKline, Exelixis, MedImmune, and several others.
SOURCE: Balaji A et al. J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703.
, according to a retrospective cohort study.
In addition, the majority of the immune-related toxicities were high-grade events of grade 3 or higher (65%), necessitated multidisciplinary care (91%), and eventually improved or resolved (65%). The results highlight potential risk factors for hospitalizations due to immune-related toxicities in oncology patients.
“[We aimed to] characterize the spectrum of toxicities, management, and outcomes of hospitalizations for immune-related adverse events,” wrote Aanika Balaji, BS, of Johns Hopkins University, Baltimore, and colleagues. The findings were reported in the Journal of Oncology Practice.
The researchers studied 443 patients admitted to solid tumor oncology service at an oncology center over a period of 6-months. Of these, 100 patients had at any point received checkpoint inhibitor therapy.
The proportion of hospital admissions for patients with confirmed immune-related toxicities and associations between hospitalizations due to immune-related toxicity and patient characteristics were assessed by the team. Nearly half of the patients admitted with immune-related toxicities had thoracic or head and neck cancers.
In the analysis, patients treated with combination checkpoint inhibitor therapy (odds ratio, 6.8; 95% confidence interval, 2.0-23.2), in addition to those aged 65 years and over (OR, 5.4; 95% CI, 1.6-17.8), were more likely to be hospitalized for immune-related toxicities.
Overall, 5% of all hospitalizations were the result of immune-related toxicities. Furthermore, 87% of patients discontinued checkpoint inhibitor therapy post discharge.
“We found that the most common immune-related adverse events warranting hospital admission were pneumonitis (26%) and colitis (17%),” they wrote.
The researchers acknowledged two key limitations of the study were the small sample size and lack of generalizability in community settings. Future studies that include patients from community oncology settings could improve the generalizability of the results.
“These data indicate potential risk factors for immune-related adverse event hospitalization and are likely to indicate future service needs” they concluded.
Financial support was provided by Jarushka Naidoo. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Compugen, Genentech, GlaxoSmithKline, Exelixis, MedImmune, and several others.
SOURCE: Balaji A et al. J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703.
FROM JOURNAL OF ONCOLOGY PRACTICE
Prevalence of Cancer in Thyroid Nodules In the Veteran Population (FULL)
Thyroid nodules are identified incidentally in 4% to 10% of the general population in the US.1,2 Clinicians and patients often are concerned about potential malignancy when thyroid nodules are identified because 5% to 15% of nodules will be cancerous.1 The most common form of cancer is papillary carcinoma followed by follicular carcinoma.2 Initially, serum thyroid-stimulating hormone (TSH) levels and thyroid ultrasound are used to evaluate a thyroid nodule because both tests can reveal vital information about malignancy potential.3 Ultrasound characteristics, such as macrocalcifications, hypoechogenicity, absence of halo, increased vascularity, and irregular nodular margins, increase suspicion for malignancy and warrant further investigation.3
Ultrasound-guided fine-needle aspiration (FNA) is the modality of choice for evaluation of thyroid nodules with sensitivity and specificity > 90%.2,4 Most patients receive a definitive diagnosis with this test; however, about 25% of cases are indeterminate based on the Bethesda System and require surgical investigation.3
Currently, it is well accepted clinical practice to refer all nodules > 4 cm for surgical intervention regardless of malignancy risk factors or the mass effect of the nodule.3-6 The preference for surgery—rather than FNA—is because of the notable false negative rate with FNA in larger nodules; studies have described false negative rates for FNA close to 10%.7,8 In contrast, Megwalu recently reported a FNA false negative rate of 0%.9
The risk of malignancy associated with nodule size has been researched for many years, but studies have produced conflicting results. In this retrospective cohort study, the authors compared malignancy rates between patients with nodules ≥ 3 cm and those with nodules < 3 cm.
Methods
The authors performed a retrospective chart review of the medical records of 329 patients presenting for thyroid nodule evaluation found on physical exam or incidentally identified with imaging at the Dayton Veteran Affairs Medical Center from January 2000 to May 2016. Data collection included sex, age, race, personal history of neck radiation treatment, family history of thyroid cancer, personal history of thyroid cancer, hot nodules/Graves disease, abnormal neck lymph nodes, and serum TSH levels. The authors looked for an association between TSH level and cancer. Hot thyroid nodules are known to have low risk of malignancy.
All patients aged 18 to 99 years with a thyroid nodule evaluated with FNA were included in the study. Patients were divided into 2 groups, those with nodules ≥ 3 cm and those with nodules < 3 cm. For nodules requiring subsequent biopsies, only the initial nodule biopsy was included in our study. The 3-cm cutoff was selected based on previous studies.1,5,10 Patients who did not undergo a FNA study were excluded. Indications for surgery were positive FNA results, suspicious imaging, size of nodule, or patient preference.
Means and standard deviations are reported for continuous variables and counts and percentages for categorical variables. We used the Mann-Whitney test for comparisons involving continuous variables with 2 groups and the Kruskal-Wallis test for 4 groups. The chi-square test—corrected for continuity if necessary—was used to compare 2 categorical variables. We used multiple logistic regression to adjust for demographic and clinical variables other than nodule size that were related to malignancy. Inferences were made at the 0.05 level of significance.
Results
A total of 329 patients with thyroid nodules were identified: 236 were < 3 cm and 93 were ≥ 3 cm. The 2 groups differed on race, with more white patients in the < 3-cm nodule group (78% vs 67%, P = .036) (Table 1).
Prevalence of cancer based on FNA in nodules < 3 cm was 6.4% (95% CI, 3.6%–10.3%) and nodules ≥ 3 cm was 8.6% (95% CI, 3.8%–16.2%; P = .23) (Table 2).
When divided into 4 subgroups, cancer using FNA was found in 35.1% of nodules < 2 cm, 21.1% of nodules 2 cm to < 3 cm, 42.1% of nodules 3 cm to 4 cm, and 18.2% of nodules > 4 cm (P = .32) (Table 3).
Surgical pathology results showed 17 cases of papillary carcinoma in nodules < 3 cm, whereas there were 9 cases of papillary carcinoma and 1 case of follicular carcinoma in nodules > 3 cm. When correlated with the cytology results, 10 cases were reported as benign, 11 were malignant, and 6 samples were non-diagnostic.
There were 30 nondiagnostic FNA samples: 7 patients had surgery, 19 were monitored with serial imaging, 2 were lost to follow-up, and 2 expired for other reasons. Of the 19 patients who were monitored with serial imaging, the nodules were stable and did not require repeat sampling.
Discussion
The authors found no relationship between thyroid nodule size and malignancy over a 16-year period in a veteran population, either with FNA or surgical pathology. The lack of relationship persists when adjusted for the only nonthyroid variable on which the 2 groups differed (race).
The finding of no relationship between larger thyroid nodule size and cancer is consistent with other studies. In a 10-year chart review of 695 patients at Walter Reed Army Medical Center, Burch and colleagues found a malignancy rate of 18.6% but no association between thyroid nodule size and malignancy.11 They concluded that nodules ≥ 4 cm did not increase malignancy risk. In a 3-year retrospective study of 326 patients, Mangister and colleagues reported that the malignancy rate was higher in nodules < 3 cm (48.4%) compared with nodules ≥ 3 cm (33.3%).10 This study concluded that the malignancy potential of thyroid nodules peaked at 2 cm and decreased at > 3 cm. Kamran and colleagues reported a nonlinear relationship between nodule size and malignancy with a threshold of 2 cm, beyond which there was no increased risk of malignancy.1
Conversely, in a prospective study Kuru and colleagues followed 571 patients who had undergone thyroidectomy and found that nodules ≥ 4 cm were associated with increased malignancy risk compared with nodules < 4 cm. However, with a cutoff of 3 cm there was no relationship.5 Discrepancies among studies might be because of variability in patient demographics and the prevalence of thyroid cancer in a specific institution. Although the majority of thyroid nodules are seen in females, the current study’s population was predominantly male and entirely veteran. Consequently, interpretation of these studies highlight the need to individualize clinical decision-making for each patient.
Limitations
This study has several limitations. It was conducted at a single institution with a group of veterans, which limits the ability to generalize its results to the general population. Second, data omissions are likely in retrospective chart reviews, and ensuring accuracy of data collection could be challenging. Third, all thyroid nodules found to be benign with cytology did not undergo surgical intervention to confirm the diagnosis; therefore, only 93 of 329 nodules were evaluated with the definitive diagnostic test. Therefore, selection bias was introduced into the nodule size comparisons when surgical intervention was used to measure the outcome. However, because false negative rates for FNA is low, likely few malignant nodules were missed. In addition, all patients with thyroid nodules are not referred for surgery because of potential complications.
Conclusion
This study strongly suggests there is no increased or decreased cancer risk for thyroid nodules ≥ 3 cm compared with those < 3 cm. Current clinical practice is to refer patients with larger nodules for surgical evaluation. In a large systemic review, Shin and colleagues reported higher pretest probability of malignancy in larger nodules and recommended consideration of surgical intervention for nodules > 3 cm because of false negatives and concerns for diagnostic inaccuracy with FNA.8 Although data were mixed, Shin and colleagues reported higher incidence of false negative FNA results in larger nodules.8 Given the authors’ findings and earlier conflicting results, the decision for surgical intervention cannot be made solely on nodule size and requires consideration of additional factors including FNA results, nodule characteristics, patient risk factors, and patient preference.
1. Kamran SC, Marqusee E, Kim MI, et al. Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab. 2013;98(2):564-570.
2. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-33.
3. Popoveniuc G, Jonklaas J. Thyroid nodules. Med Clin North Am. 2012;96(2):329-349.
4. Amrikachi M, Ramzy I, Rubenfeld S, Wheeler TM. Accuracy of fine needle aspiration of thyroid. Arch Pathol Lab Med. 2001;125(4):484-488.
5. Kuru B, Gulcelik NE, Gulcelik MA, Dincer H. Predictive index for carcinoma of thyroid nodules and its integration with fine-needle aspiration cytology. Head Neck. 2009;31(7):856-866.
6. Kim JH, Kim NK, Oh YL, et al. The validity of ultrasonography-guided fine needle aspiration biopsy in thyroid nodules 4 cm or larger depends on ultrasound characteristics. Endocrinol Metab (Seoul). 2014;29(4):545-552.
7. Wharry LI, McCoy KL, Stang MT, et al. Thyroid nodules (≥4 cm): can ultrasound and cytology reliably exclude cancer? World J Surg. 2014;38(3):614-621.
8. Pinchot SN, Al-Wagih H, Schaefer S, Sippel R, Chen H. Accuracy of fine needle aspiration biopsy for predicting neoplasm or carcinoma in thyroid nodules 4 cm or larger. Arch Surg. 2009;144(7):649-655.
9. Megwalu UC. Risk of malignancy in thyroid nodules 4 cm or larger. Endocrinol Metab (Seoul). 2017;32(1):77-82.
10. Magister MJ, Chaikhoutdinov I, Schaefer E, et al. Association of thyroid nodule size and Bethesda class with rate of malignant disease. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1089-1095.
11. Shrestha M, Crothers BA, Burch HB. The impact of thyroid nodule size on the risk of malignancy and accuracy of fine needle aspiration: a 10-year study from a single institution. Thyroid. 2012;22(12):1251-1256.
Thyroid nodules are identified incidentally in 4% to 10% of the general population in the US.1,2 Clinicians and patients often are concerned about potential malignancy when thyroid nodules are identified because 5% to 15% of nodules will be cancerous.1 The most common form of cancer is papillary carcinoma followed by follicular carcinoma.2 Initially, serum thyroid-stimulating hormone (TSH) levels and thyroid ultrasound are used to evaluate a thyroid nodule because both tests can reveal vital information about malignancy potential.3 Ultrasound characteristics, such as macrocalcifications, hypoechogenicity, absence of halo, increased vascularity, and irregular nodular margins, increase suspicion for malignancy and warrant further investigation.3
Ultrasound-guided fine-needle aspiration (FNA) is the modality of choice for evaluation of thyroid nodules with sensitivity and specificity > 90%.2,4 Most patients receive a definitive diagnosis with this test; however, about 25% of cases are indeterminate based on the Bethesda System and require surgical investigation.3
Currently, it is well accepted clinical practice to refer all nodules > 4 cm for surgical intervention regardless of malignancy risk factors or the mass effect of the nodule.3-6 The preference for surgery—rather than FNA—is because of the notable false negative rate with FNA in larger nodules; studies have described false negative rates for FNA close to 10%.7,8 In contrast, Megwalu recently reported a FNA false negative rate of 0%.9
The risk of malignancy associated with nodule size has been researched for many years, but studies have produced conflicting results. In this retrospective cohort study, the authors compared malignancy rates between patients with nodules ≥ 3 cm and those with nodules < 3 cm.
Methods
The authors performed a retrospective chart review of the medical records of 329 patients presenting for thyroid nodule evaluation found on physical exam or incidentally identified with imaging at the Dayton Veteran Affairs Medical Center from January 2000 to May 2016. Data collection included sex, age, race, personal history of neck radiation treatment, family history of thyroid cancer, personal history of thyroid cancer, hot nodules/Graves disease, abnormal neck lymph nodes, and serum TSH levels. The authors looked for an association between TSH level and cancer. Hot thyroid nodules are known to have low risk of malignancy.
All patients aged 18 to 99 years with a thyroid nodule evaluated with FNA were included in the study. Patients were divided into 2 groups, those with nodules ≥ 3 cm and those with nodules < 3 cm. For nodules requiring subsequent biopsies, only the initial nodule biopsy was included in our study. The 3-cm cutoff was selected based on previous studies.1,5,10 Patients who did not undergo a FNA study were excluded. Indications for surgery were positive FNA results, suspicious imaging, size of nodule, or patient preference.
Means and standard deviations are reported for continuous variables and counts and percentages for categorical variables. We used the Mann-Whitney test for comparisons involving continuous variables with 2 groups and the Kruskal-Wallis test for 4 groups. The chi-square test—corrected for continuity if necessary—was used to compare 2 categorical variables. We used multiple logistic regression to adjust for demographic and clinical variables other than nodule size that were related to malignancy. Inferences were made at the 0.05 level of significance.
Results
A total of 329 patients with thyroid nodules were identified: 236 were < 3 cm and 93 were ≥ 3 cm. The 2 groups differed on race, with more white patients in the < 3-cm nodule group (78% vs 67%, P = .036) (Table 1).
Prevalence of cancer based on FNA in nodules < 3 cm was 6.4% (95% CI, 3.6%–10.3%) and nodules ≥ 3 cm was 8.6% (95% CI, 3.8%–16.2%; P = .23) (Table 2).
When divided into 4 subgroups, cancer using FNA was found in 35.1% of nodules < 2 cm, 21.1% of nodules 2 cm to < 3 cm, 42.1% of nodules 3 cm to 4 cm, and 18.2% of nodules > 4 cm (P = .32) (Table 3).
Surgical pathology results showed 17 cases of papillary carcinoma in nodules < 3 cm, whereas there were 9 cases of papillary carcinoma and 1 case of follicular carcinoma in nodules > 3 cm. When correlated with the cytology results, 10 cases were reported as benign, 11 were malignant, and 6 samples were non-diagnostic.
There were 30 nondiagnostic FNA samples: 7 patients had surgery, 19 were monitored with serial imaging, 2 were lost to follow-up, and 2 expired for other reasons. Of the 19 patients who were monitored with serial imaging, the nodules were stable and did not require repeat sampling.
Discussion
The authors found no relationship between thyroid nodule size and malignancy over a 16-year period in a veteran population, either with FNA or surgical pathology. The lack of relationship persists when adjusted for the only nonthyroid variable on which the 2 groups differed (race).
The finding of no relationship between larger thyroid nodule size and cancer is consistent with other studies. In a 10-year chart review of 695 patients at Walter Reed Army Medical Center, Burch and colleagues found a malignancy rate of 18.6% but no association between thyroid nodule size and malignancy.11 They concluded that nodules ≥ 4 cm did not increase malignancy risk. In a 3-year retrospective study of 326 patients, Mangister and colleagues reported that the malignancy rate was higher in nodules < 3 cm (48.4%) compared with nodules ≥ 3 cm (33.3%).10 This study concluded that the malignancy potential of thyroid nodules peaked at 2 cm and decreased at > 3 cm. Kamran and colleagues reported a nonlinear relationship between nodule size and malignancy with a threshold of 2 cm, beyond which there was no increased risk of malignancy.1
Conversely, in a prospective study Kuru and colleagues followed 571 patients who had undergone thyroidectomy and found that nodules ≥ 4 cm were associated with increased malignancy risk compared with nodules < 4 cm. However, with a cutoff of 3 cm there was no relationship.5 Discrepancies among studies might be because of variability in patient demographics and the prevalence of thyroid cancer in a specific institution. Although the majority of thyroid nodules are seen in females, the current study’s population was predominantly male and entirely veteran. Consequently, interpretation of these studies highlight the need to individualize clinical decision-making for each patient.
Limitations
This study has several limitations. It was conducted at a single institution with a group of veterans, which limits the ability to generalize its results to the general population. Second, data omissions are likely in retrospective chart reviews, and ensuring accuracy of data collection could be challenging. Third, all thyroid nodules found to be benign with cytology did not undergo surgical intervention to confirm the diagnosis; therefore, only 93 of 329 nodules were evaluated with the definitive diagnostic test. Therefore, selection bias was introduced into the nodule size comparisons when surgical intervention was used to measure the outcome. However, because false negative rates for FNA is low, likely few malignant nodules were missed. In addition, all patients with thyroid nodules are not referred for surgery because of potential complications.
Conclusion
This study strongly suggests there is no increased or decreased cancer risk for thyroid nodules ≥ 3 cm compared with those < 3 cm. Current clinical practice is to refer patients with larger nodules for surgical evaluation. In a large systemic review, Shin and colleagues reported higher pretest probability of malignancy in larger nodules and recommended consideration of surgical intervention for nodules > 3 cm because of false negatives and concerns for diagnostic inaccuracy with FNA.8 Although data were mixed, Shin and colleagues reported higher incidence of false negative FNA results in larger nodules.8 Given the authors’ findings and earlier conflicting results, the decision for surgical intervention cannot be made solely on nodule size and requires consideration of additional factors including FNA results, nodule characteristics, patient risk factors, and patient preference.
Thyroid nodules are identified incidentally in 4% to 10% of the general population in the US.1,2 Clinicians and patients often are concerned about potential malignancy when thyroid nodules are identified because 5% to 15% of nodules will be cancerous.1 The most common form of cancer is papillary carcinoma followed by follicular carcinoma.2 Initially, serum thyroid-stimulating hormone (TSH) levels and thyroid ultrasound are used to evaluate a thyroid nodule because both tests can reveal vital information about malignancy potential.3 Ultrasound characteristics, such as macrocalcifications, hypoechogenicity, absence of halo, increased vascularity, and irregular nodular margins, increase suspicion for malignancy and warrant further investigation.3
Ultrasound-guided fine-needle aspiration (FNA) is the modality of choice for evaluation of thyroid nodules with sensitivity and specificity > 90%.2,4 Most patients receive a definitive diagnosis with this test; however, about 25% of cases are indeterminate based on the Bethesda System and require surgical investigation.3
Currently, it is well accepted clinical practice to refer all nodules > 4 cm for surgical intervention regardless of malignancy risk factors or the mass effect of the nodule.3-6 The preference for surgery—rather than FNA—is because of the notable false negative rate with FNA in larger nodules; studies have described false negative rates for FNA close to 10%.7,8 In contrast, Megwalu recently reported a FNA false negative rate of 0%.9
The risk of malignancy associated with nodule size has been researched for many years, but studies have produced conflicting results. In this retrospective cohort study, the authors compared malignancy rates between patients with nodules ≥ 3 cm and those with nodules < 3 cm.
Methods
The authors performed a retrospective chart review of the medical records of 329 patients presenting for thyroid nodule evaluation found on physical exam or incidentally identified with imaging at the Dayton Veteran Affairs Medical Center from January 2000 to May 2016. Data collection included sex, age, race, personal history of neck radiation treatment, family history of thyroid cancer, personal history of thyroid cancer, hot nodules/Graves disease, abnormal neck lymph nodes, and serum TSH levels. The authors looked for an association between TSH level and cancer. Hot thyroid nodules are known to have low risk of malignancy.
All patients aged 18 to 99 years with a thyroid nodule evaluated with FNA were included in the study. Patients were divided into 2 groups, those with nodules ≥ 3 cm and those with nodules < 3 cm. For nodules requiring subsequent biopsies, only the initial nodule biopsy was included in our study. The 3-cm cutoff was selected based on previous studies.1,5,10 Patients who did not undergo a FNA study were excluded. Indications for surgery were positive FNA results, suspicious imaging, size of nodule, or patient preference.
Means and standard deviations are reported for continuous variables and counts and percentages for categorical variables. We used the Mann-Whitney test for comparisons involving continuous variables with 2 groups and the Kruskal-Wallis test for 4 groups. The chi-square test—corrected for continuity if necessary—was used to compare 2 categorical variables. We used multiple logistic regression to adjust for demographic and clinical variables other than nodule size that were related to malignancy. Inferences were made at the 0.05 level of significance.
Results
A total of 329 patients with thyroid nodules were identified: 236 were < 3 cm and 93 were ≥ 3 cm. The 2 groups differed on race, with more white patients in the < 3-cm nodule group (78% vs 67%, P = .036) (Table 1).
Prevalence of cancer based on FNA in nodules < 3 cm was 6.4% (95% CI, 3.6%–10.3%) and nodules ≥ 3 cm was 8.6% (95% CI, 3.8%–16.2%; P = .23) (Table 2).
When divided into 4 subgroups, cancer using FNA was found in 35.1% of nodules < 2 cm, 21.1% of nodules 2 cm to < 3 cm, 42.1% of nodules 3 cm to 4 cm, and 18.2% of nodules > 4 cm (P = .32) (Table 3).
Surgical pathology results showed 17 cases of papillary carcinoma in nodules < 3 cm, whereas there were 9 cases of papillary carcinoma and 1 case of follicular carcinoma in nodules > 3 cm. When correlated with the cytology results, 10 cases were reported as benign, 11 were malignant, and 6 samples were non-diagnostic.
There were 30 nondiagnostic FNA samples: 7 patients had surgery, 19 were monitored with serial imaging, 2 were lost to follow-up, and 2 expired for other reasons. Of the 19 patients who were monitored with serial imaging, the nodules were stable and did not require repeat sampling.
Discussion
The authors found no relationship between thyroid nodule size and malignancy over a 16-year period in a veteran population, either with FNA or surgical pathology. The lack of relationship persists when adjusted for the only nonthyroid variable on which the 2 groups differed (race).
The finding of no relationship between larger thyroid nodule size and cancer is consistent with other studies. In a 10-year chart review of 695 patients at Walter Reed Army Medical Center, Burch and colleagues found a malignancy rate of 18.6% but no association between thyroid nodule size and malignancy.11 They concluded that nodules ≥ 4 cm did not increase malignancy risk. In a 3-year retrospective study of 326 patients, Mangister and colleagues reported that the malignancy rate was higher in nodules < 3 cm (48.4%) compared with nodules ≥ 3 cm (33.3%).10 This study concluded that the malignancy potential of thyroid nodules peaked at 2 cm and decreased at > 3 cm. Kamran and colleagues reported a nonlinear relationship between nodule size and malignancy with a threshold of 2 cm, beyond which there was no increased risk of malignancy.1
Conversely, in a prospective study Kuru and colleagues followed 571 patients who had undergone thyroidectomy and found that nodules ≥ 4 cm were associated with increased malignancy risk compared with nodules < 4 cm. However, with a cutoff of 3 cm there was no relationship.5 Discrepancies among studies might be because of variability in patient demographics and the prevalence of thyroid cancer in a specific institution. Although the majority of thyroid nodules are seen in females, the current study’s population was predominantly male and entirely veteran. Consequently, interpretation of these studies highlight the need to individualize clinical decision-making for each patient.
Limitations
This study has several limitations. It was conducted at a single institution with a group of veterans, which limits the ability to generalize its results to the general population. Second, data omissions are likely in retrospective chart reviews, and ensuring accuracy of data collection could be challenging. Third, all thyroid nodules found to be benign with cytology did not undergo surgical intervention to confirm the diagnosis; therefore, only 93 of 329 nodules were evaluated with the definitive diagnostic test. Therefore, selection bias was introduced into the nodule size comparisons when surgical intervention was used to measure the outcome. However, because false negative rates for FNA is low, likely few malignant nodules were missed. In addition, all patients with thyroid nodules are not referred for surgery because of potential complications.
Conclusion
This study strongly suggests there is no increased or decreased cancer risk for thyroid nodules ≥ 3 cm compared with those < 3 cm. Current clinical practice is to refer patients with larger nodules for surgical evaluation. In a large systemic review, Shin and colleagues reported higher pretest probability of malignancy in larger nodules and recommended consideration of surgical intervention for nodules > 3 cm because of false negatives and concerns for diagnostic inaccuracy with FNA.8 Although data were mixed, Shin and colleagues reported higher incidence of false negative FNA results in larger nodules.8 Given the authors’ findings and earlier conflicting results, the decision for surgical intervention cannot be made solely on nodule size and requires consideration of additional factors including FNA results, nodule characteristics, patient risk factors, and patient preference.
1. Kamran SC, Marqusee E, Kim MI, et al. Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab. 2013;98(2):564-570.
2. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-33.
3. Popoveniuc G, Jonklaas J. Thyroid nodules. Med Clin North Am. 2012;96(2):329-349.
4. Amrikachi M, Ramzy I, Rubenfeld S, Wheeler TM. Accuracy of fine needle aspiration of thyroid. Arch Pathol Lab Med. 2001;125(4):484-488.
5. Kuru B, Gulcelik NE, Gulcelik MA, Dincer H. Predictive index for carcinoma of thyroid nodules and its integration with fine-needle aspiration cytology. Head Neck. 2009;31(7):856-866.
6. Kim JH, Kim NK, Oh YL, et al. The validity of ultrasonography-guided fine needle aspiration biopsy in thyroid nodules 4 cm or larger depends on ultrasound characteristics. Endocrinol Metab (Seoul). 2014;29(4):545-552.
7. Wharry LI, McCoy KL, Stang MT, et al. Thyroid nodules (≥4 cm): can ultrasound and cytology reliably exclude cancer? World J Surg. 2014;38(3):614-621.
8. Pinchot SN, Al-Wagih H, Schaefer S, Sippel R, Chen H. Accuracy of fine needle aspiration biopsy for predicting neoplasm or carcinoma in thyroid nodules 4 cm or larger. Arch Surg. 2009;144(7):649-655.
9. Megwalu UC. Risk of malignancy in thyroid nodules 4 cm or larger. Endocrinol Metab (Seoul). 2017;32(1):77-82.
10. Magister MJ, Chaikhoutdinov I, Schaefer E, et al. Association of thyroid nodule size and Bethesda class with rate of malignant disease. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1089-1095.
11. Shrestha M, Crothers BA, Burch HB. The impact of thyroid nodule size on the risk of malignancy and accuracy of fine needle aspiration: a 10-year study from a single institution. Thyroid. 2012;22(12):1251-1256.
1. Kamran SC, Marqusee E, Kim MI, et al. Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab. 2013;98(2):564-570.
2. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-33.
3. Popoveniuc G, Jonklaas J. Thyroid nodules. Med Clin North Am. 2012;96(2):329-349.
4. Amrikachi M, Ramzy I, Rubenfeld S, Wheeler TM. Accuracy of fine needle aspiration of thyroid. Arch Pathol Lab Med. 2001;125(4):484-488.
5. Kuru B, Gulcelik NE, Gulcelik MA, Dincer H. Predictive index for carcinoma of thyroid nodules and its integration with fine-needle aspiration cytology. Head Neck. 2009;31(7):856-866.
6. Kim JH, Kim NK, Oh YL, et al. The validity of ultrasonography-guided fine needle aspiration biopsy in thyroid nodules 4 cm or larger depends on ultrasound characteristics. Endocrinol Metab (Seoul). 2014;29(4):545-552.
7. Wharry LI, McCoy KL, Stang MT, et al. Thyroid nodules (≥4 cm): can ultrasound and cytology reliably exclude cancer? World J Surg. 2014;38(3):614-621.
8. Pinchot SN, Al-Wagih H, Schaefer S, Sippel R, Chen H. Accuracy of fine needle aspiration biopsy for predicting neoplasm or carcinoma in thyroid nodules 4 cm or larger. Arch Surg. 2009;144(7):649-655.
9. Megwalu UC. Risk of malignancy in thyroid nodules 4 cm or larger. Endocrinol Metab (Seoul). 2017;32(1):77-82.
10. Magister MJ, Chaikhoutdinov I, Schaefer E, et al. Association of thyroid nodule size and Bethesda class with rate of malignant disease. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1089-1095.
11. Shrestha M, Crothers BA, Burch HB. The impact of thyroid nodule size on the risk of malignancy and accuracy of fine needle aspiration: a 10-year study from a single institution. Thyroid. 2012;22(12):1251-1256.