User login
Low phosphate linked to postop infection risk
BOSTON – Phosphate levels following colorectal surgery are predictive of risk for intra-abdominal infections, and can be helpful in identifying low-risk patients who may be suitable for early discharge after surgery, investigators say.
“The association between hypophosphatemia and intra-abdominal infections after colorectal resection is a novel finding,” said Dr. Eran Sadot, a visiting surgical oncology fellow at Memorial Sloan Kettering Cancer Center in New York City.
He described an intra-abdominal infection (IAI) risk-prediction tool at the annual Society of Surgical Oncology Cancer Symposium.
An estimated 5%-15% of patients who undergo colorectal surgery develop an IAI, largely from anastomotic leak, fistula, or intra-abdominal abscess. IAIs are associated with prolonged length of stay and higher costs, as well as an estimated 20% increase in short-term mortality, and reduced long-term survival, he said.
“These complications typically become clinically evident beyond postop day 5, and early identification of intra-abdominal infections can potentially lead to early intervention and limit sepsis, “ he said.
Several studies have shown that hypophosphatemia is associated with poor outcomes in various clinical settings – among hospitalized patients in general, in surgical and cardiac intensive care units, following open heart surgery, and after hepatic resections, he noted.
The investigators hypothesized that patients who develop IAIs have an intense acute-phase response accompanied by hypophosphatemia, and that early measurement of postoperative phosphate levels could serve as a marker for systemic response and early IAI. They conducted a retrospective study of data on patients who underwent first colorectal resection at their center from 2005 through 2015. They looked at postoperative hypophosphatemia, defined as serum levels less than 2.5 mg/dL, and they used logistic regression to create a risk model.
The sample included 7,423 patients with a median age of 61 years, including 42% who underwent resection for colon cancer, 26% for rectal cancer, and the remainder for various diagnoses.
In all, 399 patients (5%) developed IAIs, and two of these patients (0.5%) died.
The authors looked at the course of perioperative serum phosphate levels and saw that all patients had a slight rise in phosphate levels on the day of surgery, which then dropped rapidly to a nadir on postoperative day, and began to recover on day 3. They found that patients who did not have IAIs had more rapid recovery of phosphate levels than did patients who developed infections. In addition, they found that hypophosphatemia on postoperative day 3 was associated with a 50% increased risk of IAI (P = .001).
In a multivariable model of the cohort characteristics stratified by IAI, the researchers saw that risk factors independently associated with IAI included body mass index greater than 30 kg.m2 (odds ratio [OR] 1.4, P = .04), combined liver resection (OR 1.9, P less than .001), estimated blood loss greater than 400 mL (OR 1.7, P = .01), hypophosphatemia on postoperative day 3 (OR 1.4, P = .03), and abnormal white blood cell count on postoperative day 3 (OR 1.9, P less than .001).
They then created an IAI risk score assigning 1 point each to the risk factors just mentioned and tested it as a risk prediction tool. A score of 0 or 1 was associated with a low, 5% predicted risk of IAI, giving the score a negative predictive value of 95%. Scores of 2-3 were associated with moderate risk of IAI (9%-15%), and scores of 4 or 5 were associated with high risk (17%-21%) of infection.
The area under the receiver operating characteristic curve was 0.66 (95% confidence interval 0.61-0.7), indicating a test with a good mix of sensitivity and specificity.
“This model may be used in conjunction with the recently developed enhanced recovery or ERAS pathways to safely reduce the hospital stay,” Dr. Sadot concluded.
The study was internally supported. Dr. Sadot and colleagues reported no conflicts of interest.
BOSTON – Phosphate levels following colorectal surgery are predictive of risk for intra-abdominal infections, and can be helpful in identifying low-risk patients who may be suitable for early discharge after surgery, investigators say.
“The association between hypophosphatemia and intra-abdominal infections after colorectal resection is a novel finding,” said Dr. Eran Sadot, a visiting surgical oncology fellow at Memorial Sloan Kettering Cancer Center in New York City.
He described an intra-abdominal infection (IAI) risk-prediction tool at the annual Society of Surgical Oncology Cancer Symposium.
An estimated 5%-15% of patients who undergo colorectal surgery develop an IAI, largely from anastomotic leak, fistula, or intra-abdominal abscess. IAIs are associated with prolonged length of stay and higher costs, as well as an estimated 20% increase in short-term mortality, and reduced long-term survival, he said.
“These complications typically become clinically evident beyond postop day 5, and early identification of intra-abdominal infections can potentially lead to early intervention and limit sepsis, “ he said.
Several studies have shown that hypophosphatemia is associated with poor outcomes in various clinical settings – among hospitalized patients in general, in surgical and cardiac intensive care units, following open heart surgery, and after hepatic resections, he noted.
The investigators hypothesized that patients who develop IAIs have an intense acute-phase response accompanied by hypophosphatemia, and that early measurement of postoperative phosphate levels could serve as a marker for systemic response and early IAI. They conducted a retrospective study of data on patients who underwent first colorectal resection at their center from 2005 through 2015. They looked at postoperative hypophosphatemia, defined as serum levels less than 2.5 mg/dL, and they used logistic regression to create a risk model.
The sample included 7,423 patients with a median age of 61 years, including 42% who underwent resection for colon cancer, 26% for rectal cancer, and the remainder for various diagnoses.
In all, 399 patients (5%) developed IAIs, and two of these patients (0.5%) died.
The authors looked at the course of perioperative serum phosphate levels and saw that all patients had a slight rise in phosphate levels on the day of surgery, which then dropped rapidly to a nadir on postoperative day, and began to recover on day 3. They found that patients who did not have IAIs had more rapid recovery of phosphate levels than did patients who developed infections. In addition, they found that hypophosphatemia on postoperative day 3 was associated with a 50% increased risk of IAI (P = .001).
In a multivariable model of the cohort characteristics stratified by IAI, the researchers saw that risk factors independently associated with IAI included body mass index greater than 30 kg.m2 (odds ratio [OR] 1.4, P = .04), combined liver resection (OR 1.9, P less than .001), estimated blood loss greater than 400 mL (OR 1.7, P = .01), hypophosphatemia on postoperative day 3 (OR 1.4, P = .03), and abnormal white blood cell count on postoperative day 3 (OR 1.9, P less than .001).
They then created an IAI risk score assigning 1 point each to the risk factors just mentioned and tested it as a risk prediction tool. A score of 0 or 1 was associated with a low, 5% predicted risk of IAI, giving the score a negative predictive value of 95%. Scores of 2-3 were associated with moderate risk of IAI (9%-15%), and scores of 4 or 5 were associated with high risk (17%-21%) of infection.
The area under the receiver operating characteristic curve was 0.66 (95% confidence interval 0.61-0.7), indicating a test with a good mix of sensitivity and specificity.
“This model may be used in conjunction with the recently developed enhanced recovery or ERAS pathways to safely reduce the hospital stay,” Dr. Sadot concluded.
The study was internally supported. Dr. Sadot and colleagues reported no conflicts of interest.
BOSTON – Phosphate levels following colorectal surgery are predictive of risk for intra-abdominal infections, and can be helpful in identifying low-risk patients who may be suitable for early discharge after surgery, investigators say.
“The association between hypophosphatemia and intra-abdominal infections after colorectal resection is a novel finding,” said Dr. Eran Sadot, a visiting surgical oncology fellow at Memorial Sloan Kettering Cancer Center in New York City.
He described an intra-abdominal infection (IAI) risk-prediction tool at the annual Society of Surgical Oncology Cancer Symposium.
An estimated 5%-15% of patients who undergo colorectal surgery develop an IAI, largely from anastomotic leak, fistula, or intra-abdominal abscess. IAIs are associated with prolonged length of stay and higher costs, as well as an estimated 20% increase in short-term mortality, and reduced long-term survival, he said.
“These complications typically become clinically evident beyond postop day 5, and early identification of intra-abdominal infections can potentially lead to early intervention and limit sepsis, “ he said.
Several studies have shown that hypophosphatemia is associated with poor outcomes in various clinical settings – among hospitalized patients in general, in surgical and cardiac intensive care units, following open heart surgery, and after hepatic resections, he noted.
The investigators hypothesized that patients who develop IAIs have an intense acute-phase response accompanied by hypophosphatemia, and that early measurement of postoperative phosphate levels could serve as a marker for systemic response and early IAI. They conducted a retrospective study of data on patients who underwent first colorectal resection at their center from 2005 through 2015. They looked at postoperative hypophosphatemia, defined as serum levels less than 2.5 mg/dL, and they used logistic regression to create a risk model.
The sample included 7,423 patients with a median age of 61 years, including 42% who underwent resection for colon cancer, 26% for rectal cancer, and the remainder for various diagnoses.
In all, 399 patients (5%) developed IAIs, and two of these patients (0.5%) died.
The authors looked at the course of perioperative serum phosphate levels and saw that all patients had a slight rise in phosphate levels on the day of surgery, which then dropped rapidly to a nadir on postoperative day, and began to recover on day 3. They found that patients who did not have IAIs had more rapid recovery of phosphate levels than did patients who developed infections. In addition, they found that hypophosphatemia on postoperative day 3 was associated with a 50% increased risk of IAI (P = .001).
In a multivariable model of the cohort characteristics stratified by IAI, the researchers saw that risk factors independently associated with IAI included body mass index greater than 30 kg.m2 (odds ratio [OR] 1.4, P = .04), combined liver resection (OR 1.9, P less than .001), estimated blood loss greater than 400 mL (OR 1.7, P = .01), hypophosphatemia on postoperative day 3 (OR 1.4, P = .03), and abnormal white blood cell count on postoperative day 3 (OR 1.9, P less than .001).
They then created an IAI risk score assigning 1 point each to the risk factors just mentioned and tested it as a risk prediction tool. A score of 0 or 1 was associated with a low, 5% predicted risk of IAI, giving the score a negative predictive value of 95%. Scores of 2-3 were associated with moderate risk of IAI (9%-15%), and scores of 4 or 5 were associated with high risk (17%-21%) of infection.
The area under the receiver operating characteristic curve was 0.66 (95% confidence interval 0.61-0.7), indicating a test with a good mix of sensitivity and specificity.
“This model may be used in conjunction with the recently developed enhanced recovery or ERAS pathways to safely reduce the hospital stay,” Dr. Sadot concluded.
The study was internally supported. Dr. Sadot and colleagues reported no conflicts of interest.
Key clinical point: Hypophosphatemia may be a risk marker for intra-abdominal infections (IAI) following colorectal surgery.
Major finding: Hypophosphatemia on postoperative day 3 was associated with a 50% increased risk of IAI.
Data source: Retrospective review of data on 7,423 consecutive colorectal surgery patients.
Disclosures: The study was internally supported. Dr. Sadot and colleagues reported no conflicts of interest.
P. aeruginosa, Serratia have high potential to spread in the NICU
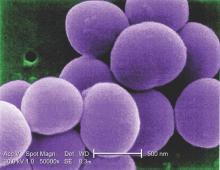
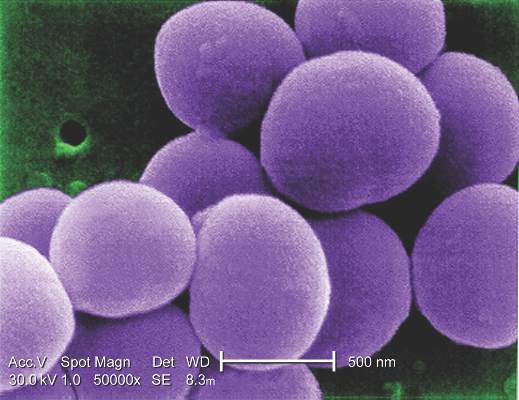
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
FROM PEDIATRICS
Key clinical point: Blood stream infection with P. aeruginosa or Serratia spp. in a very-low-birth-weight infant confers a markedly high risk of same-pathogen infection to other NICU infants.
Major finding: Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants.
Data source: An analysis of data from 44,818 very-low-birth-weight infants who were born in Germany between Jan. 1, 2000, and Dec. 31, 2011.
Disclosures: The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
Antibiotic-resistant infections remain a persistent threat
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
FROM MMWR
Study: 2.6% of patients discharged from U.S. hospital used probiotics
Probiotics were used by 2.6% of patients who had been discharged from 145 U.S. hospitals in 2012, according to an analysis of data by Sarah H. Yi of the Centers for Disease Control and Prevention and her colleagues.
“Whether probiotics are effective in preserving or restoring a healthy microbiome remains unknown, but the high prevalence of probiotic use among hospitalized patients may indicate a growing belief among clinicians that these agents may be an effective strategy for doing so,” Ms. Yi and her colleagues wrote.
The researchers used information contained in the Truven Health MarketScan Hospital Drug Database to estimate probiotic use in the inpatient setting.
Among 1,976,167 pediatric and adult patients discharged from 145 hospitals in 2012, 51,723 (2.6%) of the patients used probiotics. The individuals who used probiotics had been patients at 139 of the 145 hospitals. Compared with patients who had not used probiotics, the patients who had used probiotics were 21 times more likely to have a discharge diagnosis of Clostridium difficile infection (P less than .0001), almost 9 times more likely to have used antimicrobials (P less than .0001), more likely to have been admitted from another inpatient health care facility (P less than .0001), and more likely to have been transferred to another health care facility at discharge (P less than .001). Each of the probiotic formulations used contained between one and four organisms identified at the species level. Saccharomyces boulardii, Lactobacillus acidophilus, L. bulgaricus, and L. rhamnosus were the most commonly used probiotic formulations.
The top five diagnoses for the patients who received probiotics were septicemia (except in labor); pneumonia (except that caused by tuberculosis or sexually transmitted disease); intestinal infection; skin and subcutaneous tissue infections; and urinary tract infections. For those patients not taking probiotics, live-born infants, osteoarthritis, septicemia (except during labor), pneumonia (except that caused by tuberculosis or sexually transmitted disease), and heart failure (nonhypertensive) were the most commonly received diagnoses.
The researchers also analyzed a study of the use of probiotics at 60 hospitals during 2006-2012, which showed annual increases of probiotic use among discharged patients and an overall 2.9-fold increase in probiotic use during those years. Specifically, 10,722 discharged patients used probiotics in 2006, compared with 28,871 patients in 2012.
“Because the patients most likely to benefit [from probiotic use] are also most at risk for an adverse event, preclinical research focused on the selection of likely probiotics and carefully designed clinical trials with systematic assessment of safety is particularly important,” the researchers said.
Among the questions needed to addressed in future research on probiotic use is “which strain-specific organisms, which patient populations, at what doses, and in what time frames (related to antibiotic use in particular) are both safe and effective in the prevention or treatment of which diseases?” according to the researchers.
Read the study in American Journal of Infection Control (doi: 10.1016/j.ajic.2015.12.001).
Probiotics were used by 2.6% of patients who had been discharged from 145 U.S. hospitals in 2012, according to an analysis of data by Sarah H. Yi of the Centers for Disease Control and Prevention and her colleagues.
“Whether probiotics are effective in preserving or restoring a healthy microbiome remains unknown, but the high prevalence of probiotic use among hospitalized patients may indicate a growing belief among clinicians that these agents may be an effective strategy for doing so,” Ms. Yi and her colleagues wrote.
The researchers used information contained in the Truven Health MarketScan Hospital Drug Database to estimate probiotic use in the inpatient setting.
Among 1,976,167 pediatric and adult patients discharged from 145 hospitals in 2012, 51,723 (2.6%) of the patients used probiotics. The individuals who used probiotics had been patients at 139 of the 145 hospitals. Compared with patients who had not used probiotics, the patients who had used probiotics were 21 times more likely to have a discharge diagnosis of Clostridium difficile infection (P less than .0001), almost 9 times more likely to have used antimicrobials (P less than .0001), more likely to have been admitted from another inpatient health care facility (P less than .0001), and more likely to have been transferred to another health care facility at discharge (P less than .001). Each of the probiotic formulations used contained between one and four organisms identified at the species level. Saccharomyces boulardii, Lactobacillus acidophilus, L. bulgaricus, and L. rhamnosus were the most commonly used probiotic formulations.
The top five diagnoses for the patients who received probiotics were septicemia (except in labor); pneumonia (except that caused by tuberculosis or sexually transmitted disease); intestinal infection; skin and subcutaneous tissue infections; and urinary tract infections. For those patients not taking probiotics, live-born infants, osteoarthritis, septicemia (except during labor), pneumonia (except that caused by tuberculosis or sexually transmitted disease), and heart failure (nonhypertensive) were the most commonly received diagnoses.
The researchers also analyzed a study of the use of probiotics at 60 hospitals during 2006-2012, which showed annual increases of probiotic use among discharged patients and an overall 2.9-fold increase in probiotic use during those years. Specifically, 10,722 discharged patients used probiotics in 2006, compared with 28,871 patients in 2012.
“Because the patients most likely to benefit [from probiotic use] are also most at risk for an adverse event, preclinical research focused on the selection of likely probiotics and carefully designed clinical trials with systematic assessment of safety is particularly important,” the researchers said.
Among the questions needed to addressed in future research on probiotic use is “which strain-specific organisms, which patient populations, at what doses, and in what time frames (related to antibiotic use in particular) are both safe and effective in the prevention or treatment of which diseases?” according to the researchers.
Read the study in American Journal of Infection Control (doi: 10.1016/j.ajic.2015.12.001).
Probiotics were used by 2.6% of patients who had been discharged from 145 U.S. hospitals in 2012, according to an analysis of data by Sarah H. Yi of the Centers for Disease Control and Prevention and her colleagues.
“Whether probiotics are effective in preserving or restoring a healthy microbiome remains unknown, but the high prevalence of probiotic use among hospitalized patients may indicate a growing belief among clinicians that these agents may be an effective strategy for doing so,” Ms. Yi and her colleagues wrote.
The researchers used information contained in the Truven Health MarketScan Hospital Drug Database to estimate probiotic use in the inpatient setting.
Among 1,976,167 pediatric and adult patients discharged from 145 hospitals in 2012, 51,723 (2.6%) of the patients used probiotics. The individuals who used probiotics had been patients at 139 of the 145 hospitals. Compared with patients who had not used probiotics, the patients who had used probiotics were 21 times more likely to have a discharge diagnosis of Clostridium difficile infection (P less than .0001), almost 9 times more likely to have used antimicrobials (P less than .0001), more likely to have been admitted from another inpatient health care facility (P less than .0001), and more likely to have been transferred to another health care facility at discharge (P less than .001). Each of the probiotic formulations used contained between one and four organisms identified at the species level. Saccharomyces boulardii, Lactobacillus acidophilus, L. bulgaricus, and L. rhamnosus were the most commonly used probiotic formulations.
The top five diagnoses for the patients who received probiotics were septicemia (except in labor); pneumonia (except that caused by tuberculosis or sexually transmitted disease); intestinal infection; skin and subcutaneous tissue infections; and urinary tract infections. For those patients not taking probiotics, live-born infants, osteoarthritis, septicemia (except during labor), pneumonia (except that caused by tuberculosis or sexually transmitted disease), and heart failure (nonhypertensive) were the most commonly received diagnoses.
The researchers also analyzed a study of the use of probiotics at 60 hospitals during 2006-2012, which showed annual increases of probiotic use among discharged patients and an overall 2.9-fold increase in probiotic use during those years. Specifically, 10,722 discharged patients used probiotics in 2006, compared with 28,871 patients in 2012.
“Because the patients most likely to benefit [from probiotic use] are also most at risk for an adverse event, preclinical research focused on the selection of likely probiotics and carefully designed clinical trials with systematic assessment of safety is particularly important,” the researchers said.
Among the questions needed to addressed in future research on probiotic use is “which strain-specific organisms, which patient populations, at what doses, and in what time frames (related to antibiotic use in particular) are both safe and effective in the prevention or treatment of which diseases?” according to the researchers.
Read the study in American Journal of Infection Control (doi: 10.1016/j.ajic.2015.12.001).
FROM AMERICAN JOURNAL OF INFECTION CONTROL
Infection control is everyone’s responsibility
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Adding azithromycin cuts postcesarean maternal infections
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Prophylactic azithromycin added to standard antibiotics decreased maternal infections after cesarean.
Major finding: The number needed to treat to prevent one postsurgical infection was 17.
Data source: The randomized, placebo-controlled trial comprised 2,013 women.
Disclosures: The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
Manufacturer issues new reprocessing instructions for ED-3490TK video duodenoscope
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.
Sepsis redefined by joint U.S.-European critical care task force
ORLANDO – New consensus definitions for sepsis and septic shock focus on host dysregulation in the face of infection, propose a three-item quick-scoring option for bedside assessment, and introduce serum lactate as an important marker of cellular metabolic stress in identifying septic shock.
Sepsis is now defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection,” according to a 19-member task force convened jointly by the U.S. Society for Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) (JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287).
Since sepsis itself is inherently a life-threatening diagnosis, the term “severe sepsis” is redundant and should be eliminated, according to Dr. Mervyn Singer and his fellow task force members and coauthors. Together with his coauthors, Dr. Singer, professor of intensive care medicine at University College London, also recommended moving away from an “excessive focus on inflammation” and “the misleading model that sepsis follows a continuum through severe sepsis to shock.”
Systemic inflammatory response syndrome (SIRS) is a serious manifestation of an appropriate host response to infection, rather than the dysregulated host response that characterizes sepsis. So although it’s no longer included in sepsis criteria. “We are not discounting SIRS,” Dr. Singer said in a presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine. The consensus statement was released and the presentation was made simultaneously.
Organ dysfunction, for the purposes of the revised definition, is defined as a 2 or more point increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score. This increase is associated with a 10% or more rise in mortality while in hospital. Task force members, after review, recommended standardizing sepsis assessment with the SOFA score.
The criteria require an increase of 2 or more points on the SOFA score because many patients suspected of sepsis will have comorbidities that will “earn” them SOFA points at baseline, said Dr. Singer.
Operationalizing the sepsis definition through SOFA made sense, said Dr. Singer, because the set of five laboratory measures and one clinician-administered scale – the Glasgow Coma Scale (GCS) – are already likely to be part of daily assessments for a seriously ill hospitalized adult.
Septic shock, as defined by the task force, is associated with in-hospital mortality of over 40%. Septic shock is now defined as “a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone.” Clinically, patients have septic shock if they require a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater, and have a serum lactate level greater than 18 mg/dL (2 mmol/L) without hypovolemia.
The definitions introduce an abbreviated bedside sepsis identification tool termed quickSOFA (qSOFA). For adults suspected of infection, qSOFA requires two of the three clinical criteria of respiratory rate of 22 breaths/min or greater, altered mentation, or systolic blood pressure of 100 mm Hg or less. “This model was robust to multiple sensitivity analyses,” wrote Dr. Singer and his coauthors, and worked well in out-of-hospital, emergency department, and ward settings both within and outside of the United States. “We are encouraging prospective validation in different health care settings,” for example, in resource-poor environments, said Dr. Singer.
The extensive review process included a large meta-analysis and systematic review of observational studies of adults with sepsis to evaluate diagnostic systems and criteria currently in use. The results of the review were used to inform the task force’s Delphi study, which then led to cohort studies to test the proposed variables, through the Surviving Sepsis Campaign. A comprehensive description of the work of the task force was published concurrently with the new sepsis and septic shock definitions (JAMA. 2016;315[8]:775-87. doi: 10.1001/jama.2016.0289).
“We had what I call a soft launch” of the new definitions, said Dr. Singer. The definitions and criteria have been available for review and discussion for about a year, and discussions in the public forum are already shaping thoughts about the way forward. “We expect lots and lots of discussion,” said Dr. Singer.
Limitations of the new definitions were enumerated by Dr. Singer and his coauthors, and also brought forward in an accompanying editorial by Dr. Edward Abraham, dean of the Wake Forest School of Medicine, Winston-Salem, N.C. These include that sepsis is not defined for children, that the reliance on serum lactate levels may not be feasible in resource-poor environments, and that there are limitations to the datasets used to generate the new guidelines.
The guidelines also offer suggested International Classification of Diseases-9 (ICD-9) and ICD-10 codes for sepsis and septic shock, in the hope that “greater clarity and consistency will also facilitate research and more accurate coding,” wrote Dr. Singer and his coauthors.
Multiple task force members reported relationships with pharmaceutical companies. The work of the task force was supported in part by grants from SCCM and ESICM.
The guidelines and accompanying information are available at www.sccm.org/sepsisredefined.
On Twitter @karioakes
ORLANDO – New consensus definitions for sepsis and septic shock focus on host dysregulation in the face of infection, propose a three-item quick-scoring option for bedside assessment, and introduce serum lactate as an important marker of cellular metabolic stress in identifying septic shock.
Sepsis is now defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection,” according to a 19-member task force convened jointly by the U.S. Society for Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) (JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287).
Since sepsis itself is inherently a life-threatening diagnosis, the term “severe sepsis” is redundant and should be eliminated, according to Dr. Mervyn Singer and his fellow task force members and coauthors. Together with his coauthors, Dr. Singer, professor of intensive care medicine at University College London, also recommended moving away from an “excessive focus on inflammation” and “the misleading model that sepsis follows a continuum through severe sepsis to shock.”
Systemic inflammatory response syndrome (SIRS) is a serious manifestation of an appropriate host response to infection, rather than the dysregulated host response that characterizes sepsis. So although it’s no longer included in sepsis criteria. “We are not discounting SIRS,” Dr. Singer said in a presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine. The consensus statement was released and the presentation was made simultaneously.
Organ dysfunction, for the purposes of the revised definition, is defined as a 2 or more point increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score. This increase is associated with a 10% or more rise in mortality while in hospital. Task force members, after review, recommended standardizing sepsis assessment with the SOFA score.
The criteria require an increase of 2 or more points on the SOFA score because many patients suspected of sepsis will have comorbidities that will “earn” them SOFA points at baseline, said Dr. Singer.
Operationalizing the sepsis definition through SOFA made sense, said Dr. Singer, because the set of five laboratory measures and one clinician-administered scale – the Glasgow Coma Scale (GCS) – are already likely to be part of daily assessments for a seriously ill hospitalized adult.
Septic shock, as defined by the task force, is associated with in-hospital mortality of over 40%. Septic shock is now defined as “a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone.” Clinically, patients have septic shock if they require a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater, and have a serum lactate level greater than 18 mg/dL (2 mmol/L) without hypovolemia.
The definitions introduce an abbreviated bedside sepsis identification tool termed quickSOFA (qSOFA). For adults suspected of infection, qSOFA requires two of the three clinical criteria of respiratory rate of 22 breaths/min or greater, altered mentation, or systolic blood pressure of 100 mm Hg or less. “This model was robust to multiple sensitivity analyses,” wrote Dr. Singer and his coauthors, and worked well in out-of-hospital, emergency department, and ward settings both within and outside of the United States. “We are encouraging prospective validation in different health care settings,” for example, in resource-poor environments, said Dr. Singer.
The extensive review process included a large meta-analysis and systematic review of observational studies of adults with sepsis to evaluate diagnostic systems and criteria currently in use. The results of the review were used to inform the task force’s Delphi study, which then led to cohort studies to test the proposed variables, through the Surviving Sepsis Campaign. A comprehensive description of the work of the task force was published concurrently with the new sepsis and septic shock definitions (JAMA. 2016;315[8]:775-87. doi: 10.1001/jama.2016.0289).
“We had what I call a soft launch” of the new definitions, said Dr. Singer. The definitions and criteria have been available for review and discussion for about a year, and discussions in the public forum are already shaping thoughts about the way forward. “We expect lots and lots of discussion,” said Dr. Singer.
Limitations of the new definitions were enumerated by Dr. Singer and his coauthors, and also brought forward in an accompanying editorial by Dr. Edward Abraham, dean of the Wake Forest School of Medicine, Winston-Salem, N.C. These include that sepsis is not defined for children, that the reliance on serum lactate levels may not be feasible in resource-poor environments, and that there are limitations to the datasets used to generate the new guidelines.
The guidelines also offer suggested International Classification of Diseases-9 (ICD-9) and ICD-10 codes for sepsis and septic shock, in the hope that “greater clarity and consistency will also facilitate research and more accurate coding,” wrote Dr. Singer and his coauthors.
Multiple task force members reported relationships with pharmaceutical companies. The work of the task force was supported in part by grants from SCCM and ESICM.
The guidelines and accompanying information are available at www.sccm.org/sepsisredefined.
On Twitter @karioakes
ORLANDO – New consensus definitions for sepsis and septic shock focus on host dysregulation in the face of infection, propose a three-item quick-scoring option for bedside assessment, and introduce serum lactate as an important marker of cellular metabolic stress in identifying septic shock.
Sepsis is now defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection,” according to a 19-member task force convened jointly by the U.S. Society for Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) (JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287).
Since sepsis itself is inherently a life-threatening diagnosis, the term “severe sepsis” is redundant and should be eliminated, according to Dr. Mervyn Singer and his fellow task force members and coauthors. Together with his coauthors, Dr. Singer, professor of intensive care medicine at University College London, also recommended moving away from an “excessive focus on inflammation” and “the misleading model that sepsis follows a continuum through severe sepsis to shock.”
Systemic inflammatory response syndrome (SIRS) is a serious manifestation of an appropriate host response to infection, rather than the dysregulated host response that characterizes sepsis. So although it’s no longer included in sepsis criteria. “We are not discounting SIRS,” Dr. Singer said in a presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine. The consensus statement was released and the presentation was made simultaneously.
Organ dysfunction, for the purposes of the revised definition, is defined as a 2 or more point increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score. This increase is associated with a 10% or more rise in mortality while in hospital. Task force members, after review, recommended standardizing sepsis assessment with the SOFA score.
The criteria require an increase of 2 or more points on the SOFA score because many patients suspected of sepsis will have comorbidities that will “earn” them SOFA points at baseline, said Dr. Singer.
Operationalizing the sepsis definition through SOFA made sense, said Dr. Singer, because the set of five laboratory measures and one clinician-administered scale – the Glasgow Coma Scale (GCS) – are already likely to be part of daily assessments for a seriously ill hospitalized adult.
Septic shock, as defined by the task force, is associated with in-hospital mortality of over 40%. Septic shock is now defined as “a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone.” Clinically, patients have septic shock if they require a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater, and have a serum lactate level greater than 18 mg/dL (2 mmol/L) without hypovolemia.
The definitions introduce an abbreviated bedside sepsis identification tool termed quickSOFA (qSOFA). For adults suspected of infection, qSOFA requires two of the three clinical criteria of respiratory rate of 22 breaths/min or greater, altered mentation, or systolic blood pressure of 100 mm Hg or less. “This model was robust to multiple sensitivity analyses,” wrote Dr. Singer and his coauthors, and worked well in out-of-hospital, emergency department, and ward settings both within and outside of the United States. “We are encouraging prospective validation in different health care settings,” for example, in resource-poor environments, said Dr. Singer.
The extensive review process included a large meta-analysis and systematic review of observational studies of adults with sepsis to evaluate diagnostic systems and criteria currently in use. The results of the review were used to inform the task force’s Delphi study, which then led to cohort studies to test the proposed variables, through the Surviving Sepsis Campaign. A comprehensive description of the work of the task force was published concurrently with the new sepsis and septic shock definitions (JAMA. 2016;315[8]:775-87. doi: 10.1001/jama.2016.0289).
“We had what I call a soft launch” of the new definitions, said Dr. Singer. The definitions and criteria have been available for review and discussion for about a year, and discussions in the public forum are already shaping thoughts about the way forward. “We expect lots and lots of discussion,” said Dr. Singer.
Limitations of the new definitions were enumerated by Dr. Singer and his coauthors, and also brought forward in an accompanying editorial by Dr. Edward Abraham, dean of the Wake Forest School of Medicine, Winston-Salem, N.C. These include that sepsis is not defined for children, that the reliance on serum lactate levels may not be feasible in resource-poor environments, and that there are limitations to the datasets used to generate the new guidelines.
The guidelines also offer suggested International Classification of Diseases-9 (ICD-9) and ICD-10 codes for sepsis and septic shock, in the hope that “greater clarity and consistency will also facilitate research and more accurate coding,” wrote Dr. Singer and his coauthors.
Multiple task force members reported relationships with pharmaceutical companies. The work of the task force was supported in part by grants from SCCM and ESICM.
The guidelines and accompanying information are available at www.sccm.org/sepsisredefined.
On Twitter @karioakes
AT THE CRITICAL CARE CONGRESS
Chlorhexidine baths help hospitals control extensively drug-resistant pathogen
With an outbreak of the extensively drug-resistant pathogen Acinetobacter baumannii (XDR-Ab), patient screening and daily chlorhexidine baths were part of a comprehensive outbreak control strategy, a new study suggested.
XDR-Ab transmission within hospitals has been documented via direct and indirect patient contact, inadequate sterilization of medical devices, contamination of rooms, and colonized health care workers, said Dr. Yves Longtin, chair of the infection prevention and control unit at Jewish General Hospital in Montreal. Dr. Longtin and his coauthors described the epidemiology and control of an XDR-Ab outbreak that involved multiple units of a large Canadian hospital in a recent article published in the Journal of Hospital Infection.
The outbreak was the result of a single clonal strain of XDR-Ab that colonized or infected 29 patients, 5 of whom died of XDR-Ab bacteremia. Transmission occurred primarily on two wards, either directly between patients or indirectly through staff, shared equipment, or the environment, investigators found. There is currently no consensus on optimal screening procedures, nor on the best combination of interventions to prevent transmission among patients, Dr. Longtin and his colleagues said.
The outbreak described in the study ended following the application of intensive screening, environmental disinfection, source control, reinforcement of routine hygiene, and isolation procedures including cohorting and unit closure. Intensive screening – screening of rectum, groin, throat, urine (in catheterized patients), wounds, and other catheter sites – revealed that 57% of infected patients were rectal carriers of the bacterium. Thus, a single rectal screening, considered standard for detection of carbapenem-resistant Enterobacteriaceae, would not have been sufficient to detect all infected patients.
Colonized patients received daily chlorhexidine baths, a strategy that is a useful tool in the control of other antibiotic-resistant nosocomial pathogens, such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci, but is not mentioned in the recent acinetobacter-specific guidelines or reviews, Dr. Longtin and coauthors said. They hypothesized that the prompt resolution of the outbreak may have been due in part to the use of the chlorhexidine baths.
Read the full study in the Journal of Hospital Infection (doi: 10.1016/j.jhin.2015.12.013).
On Twitter @richpizzi
With an outbreak of the extensively drug-resistant pathogen Acinetobacter baumannii (XDR-Ab), patient screening and daily chlorhexidine baths were part of a comprehensive outbreak control strategy, a new study suggested.
XDR-Ab transmission within hospitals has been documented via direct and indirect patient contact, inadequate sterilization of medical devices, contamination of rooms, and colonized health care workers, said Dr. Yves Longtin, chair of the infection prevention and control unit at Jewish General Hospital in Montreal. Dr. Longtin and his coauthors described the epidemiology and control of an XDR-Ab outbreak that involved multiple units of a large Canadian hospital in a recent article published in the Journal of Hospital Infection.
The outbreak was the result of a single clonal strain of XDR-Ab that colonized or infected 29 patients, 5 of whom died of XDR-Ab bacteremia. Transmission occurred primarily on two wards, either directly between patients or indirectly through staff, shared equipment, or the environment, investigators found. There is currently no consensus on optimal screening procedures, nor on the best combination of interventions to prevent transmission among patients, Dr. Longtin and his colleagues said.
The outbreak described in the study ended following the application of intensive screening, environmental disinfection, source control, reinforcement of routine hygiene, and isolation procedures including cohorting and unit closure. Intensive screening – screening of rectum, groin, throat, urine (in catheterized patients), wounds, and other catheter sites – revealed that 57% of infected patients were rectal carriers of the bacterium. Thus, a single rectal screening, considered standard for detection of carbapenem-resistant Enterobacteriaceae, would not have been sufficient to detect all infected patients.
Colonized patients received daily chlorhexidine baths, a strategy that is a useful tool in the control of other antibiotic-resistant nosocomial pathogens, such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci, but is not mentioned in the recent acinetobacter-specific guidelines or reviews, Dr. Longtin and coauthors said. They hypothesized that the prompt resolution of the outbreak may have been due in part to the use of the chlorhexidine baths.
Read the full study in the Journal of Hospital Infection (doi: 10.1016/j.jhin.2015.12.013).
On Twitter @richpizzi
With an outbreak of the extensively drug-resistant pathogen Acinetobacter baumannii (XDR-Ab), patient screening and daily chlorhexidine baths were part of a comprehensive outbreak control strategy, a new study suggested.
XDR-Ab transmission within hospitals has been documented via direct and indirect patient contact, inadequate sterilization of medical devices, contamination of rooms, and colonized health care workers, said Dr. Yves Longtin, chair of the infection prevention and control unit at Jewish General Hospital in Montreal. Dr. Longtin and his coauthors described the epidemiology and control of an XDR-Ab outbreak that involved multiple units of a large Canadian hospital in a recent article published in the Journal of Hospital Infection.
The outbreak was the result of a single clonal strain of XDR-Ab that colonized or infected 29 patients, 5 of whom died of XDR-Ab bacteremia. Transmission occurred primarily on two wards, either directly between patients or indirectly through staff, shared equipment, or the environment, investigators found. There is currently no consensus on optimal screening procedures, nor on the best combination of interventions to prevent transmission among patients, Dr. Longtin and his colleagues said.
The outbreak described in the study ended following the application of intensive screening, environmental disinfection, source control, reinforcement of routine hygiene, and isolation procedures including cohorting and unit closure. Intensive screening – screening of rectum, groin, throat, urine (in catheterized patients), wounds, and other catheter sites – revealed that 57% of infected patients were rectal carriers of the bacterium. Thus, a single rectal screening, considered standard for detection of carbapenem-resistant Enterobacteriaceae, would not have been sufficient to detect all infected patients.
Colonized patients received daily chlorhexidine baths, a strategy that is a useful tool in the control of other antibiotic-resistant nosocomial pathogens, such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci, but is not mentioned in the recent acinetobacter-specific guidelines or reviews, Dr. Longtin and coauthors said. They hypothesized that the prompt resolution of the outbreak may have been due in part to the use of the chlorhexidine baths.
Read the full study in the Journal of Hospital Infection (doi: 10.1016/j.jhin.2015.12.013).
On Twitter @richpizzi
FROM THE JOURNAL OF HOSPITAL INFECTION
Chlorhexidine beats iodine for preventing C-section wound infections
ATLANTA – A chlorhexidine/alcohol skin antiseptic cut cesarean section surgical site infections by half, compared with a solution of iodine and alcohol.
The chlorhexidine solution significantly reduced the risk of both superficial and deep incisional infections, Dr. Methodius G. Tuuli reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The study was simultaneously published in the New England Journal of Medicine (2016 Feb 4. doi: 10.1056/NEJMoa1511048).
The randomized trial is the first to examine the two antiseptics in obstetric surgery, noted Dr. Tuuli of Washington University, St. Louis. The results echo those repeatedly found in the general surgical literature, and, he said, clearly show that chlorhexidine-based skin prep is more effective than the more often–employed iodine-based prep.
“We become comfortable doing the things we have always done, because that’s the way we were taught, and we see no reason to change,” he said in an interview. “I think now is the time to make a change for our patients.”
Dr. Tuuli’s study comprised 1,147 patients who delivered via cesarean section from 2011-2015. They were randomized to either a chlorhexidine/alcohol antiseptic (2% chlorhexidine gluconate with 70% isopropyl alcohol) or the iodine/alcohol combination (8.3% povidone-iodine with 72.5% isopropyl alcohol). Both groups received standard-of-care systemic antibiotic prophylaxis.
They were followed daily until discharge from the hospital, and then with a telephone call 30 days after delivery to assess whether a surgical site infection had occurred, as well as any visits to a physician’s office or emergency department that were related to a wound complication.
The co-primary endpoints were superficial and deep incisional infections. Secondary endpoints included length of hospital stay; physician office visits; hospital readmissions for infection-related complications; endometritis; positive wound culture; skin irritation; and allergic reaction.
Surgical site infections occurred in 23 patients in the chlorhexidine group and 42 in the iodine group (4.0% vs. 7.3%) – a significant 45% risk reduction (relative risk, 0.55). Superficial infections were significantly less common in the chlorhexidine group (3.0% vs. 4.9%), as were deep infections (1.0% vs. 2.4%).
A subgroup analysis examined unscheduled vs. scheduled cesarean; obese vs. nonobese patients; suture vs. staple closure; diabetes vs. no diabetes; and chronic comorbidities vs. none. Chlorhexidine was significantly more effective than iodine in each of these groups.
Antiseptic type did not affect rates of skin separation, seroma, hematoma, or cellulitis. Nor did it affect the rates of endometritis, hospitalization for infectious complications, or length of hospital stay. However, those in the chlorhexidine group were significantly less likely to visit a physician for wound care (7.9% vs. 12.5%)
Cultures were obtained on 32 patients with a confirmed infection; 27 of these specimens were positive. About half of the positive cultures were polymicrobial. The most common isolate was Staphylococcus aureus (37%). Methicillin-resistant S. aureus (MRSA) was present in 12% of cultures in the chlorhexidine group and 17% in the iodine group.
In an interview, Dr. Tuuli said that chlorhexidine has several properties that make it more effective than iodine. It is effective against both gram-negative and gram-positive organisms, including MRSA, and is not inactivated by organic matter. Although chlorhexidine is more likely than iodine to provoke an allergic reaction, none were observed in this study.
The study was supported by a grant from the National Institutes of Health. Dr. Tuuli reported having no financial disclosures; the antiseptics were procured and paid for by the medical center.
Watch Dr. Tuuli discuss the study results here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – A chlorhexidine/alcohol skin antiseptic cut cesarean section surgical site infections by half, compared with a solution of iodine and alcohol.
The chlorhexidine solution significantly reduced the risk of both superficial and deep incisional infections, Dr. Methodius G. Tuuli reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The study was simultaneously published in the New England Journal of Medicine (2016 Feb 4. doi: 10.1056/NEJMoa1511048).
The randomized trial is the first to examine the two antiseptics in obstetric surgery, noted Dr. Tuuli of Washington University, St. Louis. The results echo those repeatedly found in the general surgical literature, and, he said, clearly show that chlorhexidine-based skin prep is more effective than the more often–employed iodine-based prep.
“We become comfortable doing the things we have always done, because that’s the way we were taught, and we see no reason to change,” he said in an interview. “I think now is the time to make a change for our patients.”
Dr. Tuuli’s study comprised 1,147 patients who delivered via cesarean section from 2011-2015. They were randomized to either a chlorhexidine/alcohol antiseptic (2% chlorhexidine gluconate with 70% isopropyl alcohol) or the iodine/alcohol combination (8.3% povidone-iodine with 72.5% isopropyl alcohol). Both groups received standard-of-care systemic antibiotic prophylaxis.
They were followed daily until discharge from the hospital, and then with a telephone call 30 days after delivery to assess whether a surgical site infection had occurred, as well as any visits to a physician’s office or emergency department that were related to a wound complication.
The co-primary endpoints were superficial and deep incisional infections. Secondary endpoints included length of hospital stay; physician office visits; hospital readmissions for infection-related complications; endometritis; positive wound culture; skin irritation; and allergic reaction.
Surgical site infections occurred in 23 patients in the chlorhexidine group and 42 in the iodine group (4.0% vs. 7.3%) – a significant 45% risk reduction (relative risk, 0.55). Superficial infections were significantly less common in the chlorhexidine group (3.0% vs. 4.9%), as were deep infections (1.0% vs. 2.4%).
A subgroup analysis examined unscheduled vs. scheduled cesarean; obese vs. nonobese patients; suture vs. staple closure; diabetes vs. no diabetes; and chronic comorbidities vs. none. Chlorhexidine was significantly more effective than iodine in each of these groups.
Antiseptic type did not affect rates of skin separation, seroma, hematoma, or cellulitis. Nor did it affect the rates of endometritis, hospitalization for infectious complications, or length of hospital stay. However, those in the chlorhexidine group were significantly less likely to visit a physician for wound care (7.9% vs. 12.5%)
Cultures were obtained on 32 patients with a confirmed infection; 27 of these specimens were positive. About half of the positive cultures were polymicrobial. The most common isolate was Staphylococcus aureus (37%). Methicillin-resistant S. aureus (MRSA) was present in 12% of cultures in the chlorhexidine group and 17% in the iodine group.
In an interview, Dr. Tuuli said that chlorhexidine has several properties that make it more effective than iodine. It is effective against both gram-negative and gram-positive organisms, including MRSA, and is not inactivated by organic matter. Although chlorhexidine is more likely than iodine to provoke an allergic reaction, none were observed in this study.
The study was supported by a grant from the National Institutes of Health. Dr. Tuuli reported having no financial disclosures; the antiseptics were procured and paid for by the medical center.
Watch Dr. Tuuli discuss the study results here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – A chlorhexidine/alcohol skin antiseptic cut cesarean section surgical site infections by half, compared with a solution of iodine and alcohol.
The chlorhexidine solution significantly reduced the risk of both superficial and deep incisional infections, Dr. Methodius G. Tuuli reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The study was simultaneously published in the New England Journal of Medicine (2016 Feb 4. doi: 10.1056/NEJMoa1511048).
The randomized trial is the first to examine the two antiseptics in obstetric surgery, noted Dr. Tuuli of Washington University, St. Louis. The results echo those repeatedly found in the general surgical literature, and, he said, clearly show that chlorhexidine-based skin prep is more effective than the more often–employed iodine-based prep.
“We become comfortable doing the things we have always done, because that’s the way we were taught, and we see no reason to change,” he said in an interview. “I think now is the time to make a change for our patients.”
Dr. Tuuli’s study comprised 1,147 patients who delivered via cesarean section from 2011-2015. They were randomized to either a chlorhexidine/alcohol antiseptic (2% chlorhexidine gluconate with 70% isopropyl alcohol) or the iodine/alcohol combination (8.3% povidone-iodine with 72.5% isopropyl alcohol). Both groups received standard-of-care systemic antibiotic prophylaxis.
They were followed daily until discharge from the hospital, and then with a telephone call 30 days after delivery to assess whether a surgical site infection had occurred, as well as any visits to a physician’s office or emergency department that were related to a wound complication.
The co-primary endpoints were superficial and deep incisional infections. Secondary endpoints included length of hospital stay; physician office visits; hospital readmissions for infection-related complications; endometritis; positive wound culture; skin irritation; and allergic reaction.
Surgical site infections occurred in 23 patients in the chlorhexidine group and 42 in the iodine group (4.0% vs. 7.3%) – a significant 45% risk reduction (relative risk, 0.55). Superficial infections were significantly less common in the chlorhexidine group (3.0% vs. 4.9%), as were deep infections (1.0% vs. 2.4%).
A subgroup analysis examined unscheduled vs. scheduled cesarean; obese vs. nonobese patients; suture vs. staple closure; diabetes vs. no diabetes; and chronic comorbidities vs. none. Chlorhexidine was significantly more effective than iodine in each of these groups.
Antiseptic type did not affect rates of skin separation, seroma, hematoma, or cellulitis. Nor did it affect the rates of endometritis, hospitalization for infectious complications, or length of hospital stay. However, those in the chlorhexidine group were significantly less likely to visit a physician for wound care (7.9% vs. 12.5%)
Cultures were obtained on 32 patients with a confirmed infection; 27 of these specimens were positive. About half of the positive cultures were polymicrobial. The most common isolate was Staphylococcus aureus (37%). Methicillin-resistant S. aureus (MRSA) was present in 12% of cultures in the chlorhexidine group and 17% in the iodine group.
In an interview, Dr. Tuuli said that chlorhexidine has several properties that make it more effective than iodine. It is effective against both gram-negative and gram-positive organisms, including MRSA, and is not inactivated by organic matter. Although chlorhexidine is more likely than iodine to provoke an allergic reaction, none were observed in this study.
The study was supported by a grant from the National Institutes of Health. Dr. Tuuli reported having no financial disclosures; the antiseptics were procured and paid for by the medical center.
Watch Dr. Tuuli discuss the study results here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE PREGNANCY MEETING
Key clinical point: A chlorhexidine/alcohol antiseptic was significantly more effective at preventing cesarean section incision infections than an iodine/alcohol antiseptic.
Major finding: The chlorhexidine solution decreased surgical site infections by half, compared with the iodine-based solution.
Data source: A randomized study of 1,147 women who delivered via cesarean from 2011-2015.
Disclosures: The study was supported by a grant from the National Institutes of Health. Dr. Tuuli reported having no financial disclosures; the antiseptics were procured and paid for by the medical center.