User login
Bleed Disorders Are Possible in VA Population
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
One Year In, Mission Act Transforms Community Care for Veterans
One year into the implementation of the Mission Act, the US Department of Veterans Affairs (VA) continues to expand a wide-ranging third-party-administered program to boost the access of veterans to the civilian medical system, a VA official told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO). “VA has given to the third-party administrators what they do well, which is payment of claims, and VA has taken back what we think we can do better—scheduling, care coordination, and customer service,” said Elizabeth Brill, MD, MBA, chief medical officer and senior adviser to the acting assistant undersecretary for Health for Community Care.
The 2 third-party contractors that run the Community Care Network (CCN) are Optum and TriWest. Both companies now proces patients at all VA medical facilities in the continental US. Optum serves all the states that are entirely (or mainly) in the Central and Eastern Time Zones—except for Texas—plus Puerto Rico, Washington D.C., and the US Virgin Islands. TriWest serves Texas, Hawaii, and the states that are entirely (or mainly) in the Mountain and Pacific Time Zones. The VA has not yet assigned any contractor for Alaska, Guam, American Samoa, and the Northern Mariana Islands.
“We have tried to consolidate as much as possible into the Community Care Network, pulling in a lot of services that were not previously covered, but it’s still not covering 100% of all services that veterans need outside VA medical centers,” said Brill.
Although the VA continues to rely on Veterans Care Agreements, in which health care providers contract directly with the VA, “the main focus of community care is the Community Care Network.” Said Brill. In a pair of regions—encompassing the Midwest, Northeast, and a few other states—90% of private health services are now provided through the network, she said.
One benefit of the new system is a better experience for the health care providers who work with Optum and TriWest. These administrators are responsible for finding providers and providing them with credentials based on appropriate criteria, Brill said. “In prior days, VA paid community providers directly, and some of you may be familiar with the delays that occurred in the system,” she said. “In the new system, we have third-party administrators who pay the providers quickly, and then VA pays them.”
Urgent care services are now available through CCN in most of the continental US and will be expanded to Texas, the Mountain region and the West by the end of September, she said. “We’ve been very pleased to see the response.” Meanwhile, flu shots for enrolled veterans are now available through the system via 60,000 locations.
There are requirements for private health care providers: They must meet new training requirements and submit claims within 180 days. Patients also must meet standards to get community care. For example, patients are eligible for access if the VA can’t serve them within a 30-minute drive time for primary care and mental health care and a 60-minute drive time for specialty care. Similarly, veterans are eligible if they cannot get an appointment within 20 days for primary and mental health care and 28 days for specialty care.
However, Brill insisted, the Mission Act is “not a move toward privatization. Internal VA care is just as important as external VA care,” she said. “This just gives them more choice.”
Brill also noted that there’s more to the Mission Act than expanded access. For example, an expansion of the Program of Comprehensive Assistance for Family Caregivers Program “will start kicking in this fall and the winter,” she said. It will include families of veterans from all eras of service.
The act also is designed to improve infrastructure, although the coronavirus pandemic may disrupt timing, she said. And, she added, it will strengthen the VA’s ability to recruit and keep health care providers through projects like a new scholarship program and more access to medical education debt reduction.
One year into the implementation of the Mission Act, the US Department of Veterans Affairs (VA) continues to expand a wide-ranging third-party-administered program to boost the access of veterans to the civilian medical system, a VA official told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO). “VA has given to the third-party administrators what they do well, which is payment of claims, and VA has taken back what we think we can do better—scheduling, care coordination, and customer service,” said Elizabeth Brill, MD, MBA, chief medical officer and senior adviser to the acting assistant undersecretary for Health for Community Care.
The 2 third-party contractors that run the Community Care Network (CCN) are Optum and TriWest. Both companies now proces patients at all VA medical facilities in the continental US. Optum serves all the states that are entirely (or mainly) in the Central and Eastern Time Zones—except for Texas—plus Puerto Rico, Washington D.C., and the US Virgin Islands. TriWest serves Texas, Hawaii, and the states that are entirely (or mainly) in the Mountain and Pacific Time Zones. The VA has not yet assigned any contractor for Alaska, Guam, American Samoa, and the Northern Mariana Islands.
“We have tried to consolidate as much as possible into the Community Care Network, pulling in a lot of services that were not previously covered, but it’s still not covering 100% of all services that veterans need outside VA medical centers,” said Brill.
Although the VA continues to rely on Veterans Care Agreements, in which health care providers contract directly with the VA, “the main focus of community care is the Community Care Network.” Said Brill. In a pair of regions—encompassing the Midwest, Northeast, and a few other states—90% of private health services are now provided through the network, she said.
One benefit of the new system is a better experience for the health care providers who work with Optum and TriWest. These administrators are responsible for finding providers and providing them with credentials based on appropriate criteria, Brill said. “In prior days, VA paid community providers directly, and some of you may be familiar with the delays that occurred in the system,” she said. “In the new system, we have third-party administrators who pay the providers quickly, and then VA pays them.”
Urgent care services are now available through CCN in most of the continental US and will be expanded to Texas, the Mountain region and the West by the end of September, she said. “We’ve been very pleased to see the response.” Meanwhile, flu shots for enrolled veterans are now available through the system via 60,000 locations.
There are requirements for private health care providers: They must meet new training requirements and submit claims within 180 days. Patients also must meet standards to get community care. For example, patients are eligible for access if the VA can’t serve them within a 30-minute drive time for primary care and mental health care and a 60-minute drive time for specialty care. Similarly, veterans are eligible if they cannot get an appointment within 20 days for primary and mental health care and 28 days for specialty care.
However, Brill insisted, the Mission Act is “not a move toward privatization. Internal VA care is just as important as external VA care,” she said. “This just gives them more choice.”
Brill also noted that there’s more to the Mission Act than expanded access. For example, an expansion of the Program of Comprehensive Assistance for Family Caregivers Program “will start kicking in this fall and the winter,” she said. It will include families of veterans from all eras of service.
The act also is designed to improve infrastructure, although the coronavirus pandemic may disrupt timing, she said. And, she added, it will strengthen the VA’s ability to recruit and keep health care providers through projects like a new scholarship program and more access to medical education debt reduction.
One year into the implementation of the Mission Act, the US Department of Veterans Affairs (VA) continues to expand a wide-ranging third-party-administered program to boost the access of veterans to the civilian medical system, a VA official told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO). “VA has given to the third-party administrators what they do well, which is payment of claims, and VA has taken back what we think we can do better—scheduling, care coordination, and customer service,” said Elizabeth Brill, MD, MBA, chief medical officer and senior adviser to the acting assistant undersecretary for Health for Community Care.
The 2 third-party contractors that run the Community Care Network (CCN) are Optum and TriWest. Both companies now proces patients at all VA medical facilities in the continental US. Optum serves all the states that are entirely (or mainly) in the Central and Eastern Time Zones—except for Texas—plus Puerto Rico, Washington D.C., and the US Virgin Islands. TriWest serves Texas, Hawaii, and the states that are entirely (or mainly) in the Mountain and Pacific Time Zones. The VA has not yet assigned any contractor for Alaska, Guam, American Samoa, and the Northern Mariana Islands.
“We have tried to consolidate as much as possible into the Community Care Network, pulling in a lot of services that were not previously covered, but it’s still not covering 100% of all services that veterans need outside VA medical centers,” said Brill.
Although the VA continues to rely on Veterans Care Agreements, in which health care providers contract directly with the VA, “the main focus of community care is the Community Care Network.” Said Brill. In a pair of regions—encompassing the Midwest, Northeast, and a few other states—90% of private health services are now provided through the network, she said.
One benefit of the new system is a better experience for the health care providers who work with Optum and TriWest. These administrators are responsible for finding providers and providing them with credentials based on appropriate criteria, Brill said. “In prior days, VA paid community providers directly, and some of you may be familiar with the delays that occurred in the system,” she said. “In the new system, we have third-party administrators who pay the providers quickly, and then VA pays them.”
Urgent care services are now available through CCN in most of the continental US and will be expanded to Texas, the Mountain region and the West by the end of September, she said. “We’ve been very pleased to see the response.” Meanwhile, flu shots for enrolled veterans are now available through the system via 60,000 locations.
There are requirements for private health care providers: They must meet new training requirements and submit claims within 180 days. Patients also must meet standards to get community care. For example, patients are eligible for access if the VA can’t serve them within a 30-minute drive time for primary care and mental health care and a 60-minute drive time for specialty care. Similarly, veterans are eligible if they cannot get an appointment within 20 days for primary and mental health care and 28 days for specialty care.
However, Brill insisted, the Mission Act is “not a move toward privatization. Internal VA care is just as important as external VA care,” she said. “This just gives them more choice.”
Brill also noted that there’s more to the Mission Act than expanded access. For example, an expansion of the Program of Comprehensive Assistance for Family Caregivers Program “will start kicking in this fall and the winter,” she said. It will include families of veterans from all eras of service.
The act also is designed to improve infrastructure, although the coronavirus pandemic may disrupt timing, she said. And, she added, it will strengthen the VA’s ability to recruit and keep health care providers through projects like a new scholarship program and more access to medical education debt reduction.
VA Looks to Increase Real-World Impact of Clinical Research
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
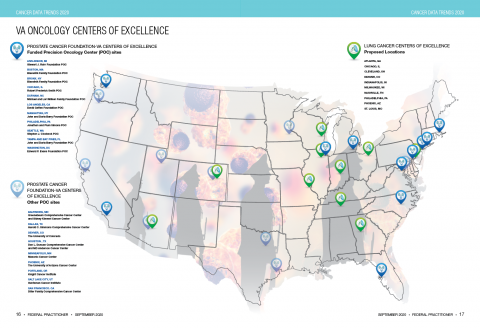
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
Lusutrombopag found safe, effective for severe thrombocytopenia in patients with hepatocellular carcinoma
For patients with severe thrombocytopenia and chronic liver diseases, including hepatocellular carcinoma, treatment with lusutrombopag prior to invasive procedures significantly decreased the need for platelet transfusions without increasing the need for rescue treatment for bleeding or the rate of thromboembolic events.
In a post hoc analysis of data from 270 patients in two manufacturer-sponsored, multicenter, randomized, double-blind, placebo-controlled, phase 3 trials, significantly more lusutrombopag recipients met the primary efficacy endpoint, including patients with hepatocellular carcinoma (68.0% vs. 8.9% in the placebo group; P < .0001) and those without it (77.0% vs. 21.6%; P < .0001). Rates of treatment-emergent adverse events were similar between the lusutrombopag and placebo groups, and patients with hepatocellular carcinoma were not at increased risk for thrombosis, Naim Alkhouri, MD, of Texas Liver Institute in San Antonio, and associates wrote in Clinical Gastroenterology and Hepatology.
Platelet transfusion is the treatment mainstay for patients with thrombocytopenia related to cirrhosis who are undergoing invasive procedures, but its effects are short-lived, and at least one in five transfusions fails. Thrombopoietin agonists such as lusutrombopag are efficacious and approved in this setting, but they can be prothrombotic, particularly in patients with hepatocellular carcinoma, who already are at heightened risk for portal vein thrombosis.
Dr. Alkhouri and associates performed an integrated analysis of the PLUS 1 trial (Japan, October 2013–May 2014) and the L-PLUS 2 (global, June 2015–April 2017). Participants were adults with Child-Pugh Class A or B chronic liver disease and baseline platelet counts under 50 x 109 per L who were scheduled for invasive procedures. Of the 270 patients, 95 had hepatocellular carcinoma. Patients were randomly assigned on a one-to-one basis to receive either lusutrombopag (3 mg) or placebo daily for up to 7 days before procedures. The primary endpoint was the percentage of patients in the per-protocol population who did not need a platelet transfusion before the invasive procedure or rescue therapy within 7 days afterward.
The treatment and placebo arms were similar except that patients with hepatocellular carcinoma were about 10 years older on average. In patients with hepatocellular carcinoma, 60.5% more lusutrombopag recipients than placebo recipients met the primary endpoint, and rates of bleeding-related adverse events were 9.1% and 15.7%, respectively. In patients with other chronic liver diseases, 52.6% more lusutrombopag recipients met the primary endpoint. Rates of bleeding-related adverse events were 5% and 10.6%.
“Approximately 88% of patients with hepatocellular carcinoma underwent a liver-related procedure, compared with approximately 10% of patients without hepatocellular carcinoma,” the investigators wrote. “This is significant because ablations or transcatheter arterial chemoembolizations can be associated with serious bleeding complications. It is clinically important that, given the greater number of liver-related procedures, the incidence of bleeding-related adverse events was lower in patients treated with lusutrombopag than placebo.”
Imaging after the procedures confirmed low rates of thromboses in both groups and subgroups. Four patients developed portal vein thromboses, including two lusutrombopag recipients (one of whom had hepatocellular carcinoma) and two placebo recipients without hepatocellular carcinoma.
These trials excluded patients undergoing major surgical procedures and those with decompensated cirrhosis; portal vein thrombosis; hematopoietic tumors; aplastic anemia; myelodysplastic syndrome; myelofibrosis; liver transplantation; splenectomy; and thrombocytopenia that was congenital, autoimmune, or drug induced. “A limitation of this study was the high rate of protocol violations related to platelet transfusions,” the researchers noted. “A number of patients [42 in all] were excluded from the per-protocol population owing to receipt of unnecessary platelet transfusions, or because they did not receive a needed platelet transfusion.”Shionogi makes lusutrombopag and sponsored the study. Dr. Alkhouri reported an advisory relationship with Shionogi and Dova Pharma. Two coinvestigators reported being employed by Shionogi. Three coinvestigators also disclosed ties to Shionogi and to several other pharmaceutical companies.
SOURCE: Alkhouri N et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.032.
Thrombocytopenia is of clinical concern in patients with cirrhosis, as it complicates routine patient care and results in delayed or canceled procedures due to concern for risk of bleeding. In the last few years, availability of thrombopoietin (TPO) receptor agonists have facilitated the performance of elective invasive procedures in cirrhotic patients with severe thrombocytopenia.
In this integrated analysis of data from two phase 3 studies, Alkhouri et al. demonstrated the efficacy of a novel TPO receptor agonist, lusutrombopag, in reducing bleeding events and need for platelet transfusion in cirrhotic patients undergoing invasive procedures. The risk for thrombosis-related adverse events was not increased in lusutrombopag recipients with or without HCC. Previous studies with another TPO, eltrombopag, resulted in high rate of symptomatic portal vein thrombosis. Avatrombopag, a recently approved TPO receptor agonist reported few thrombotic symptomatic events but no prospective imaging for evaluation of thrombotic events was included in the protocol. A unique strength of this study was inclusion of prospective imaging for evaluation of portal vein thrombosis. Strategic scheduling is required with use of TPO agonists. Lusutrombopag can be given orally in convenient daily doses and provides a 7-10-day procedural window for scheduling and performing elective invasive procedures. However, because of several days of lag period for platelet production, these agents cannot be used for emergent cases.
Gagan K. Sood, MD, AGAF, FAASLD, is an associate professor of medicine and surgery, division of gastroenterology and hepatology and division of abdominal transplantation, Baylor College of Medicine, Houston. He has no conflicts of interest.
Thrombocytopenia is of clinical concern in patients with cirrhosis, as it complicates routine patient care and results in delayed or canceled procedures due to concern for risk of bleeding. In the last few years, availability of thrombopoietin (TPO) receptor agonists have facilitated the performance of elective invasive procedures in cirrhotic patients with severe thrombocytopenia.
In this integrated analysis of data from two phase 3 studies, Alkhouri et al. demonstrated the efficacy of a novel TPO receptor agonist, lusutrombopag, in reducing bleeding events and need for platelet transfusion in cirrhotic patients undergoing invasive procedures. The risk for thrombosis-related adverse events was not increased in lusutrombopag recipients with or without HCC. Previous studies with another TPO, eltrombopag, resulted in high rate of symptomatic portal vein thrombosis. Avatrombopag, a recently approved TPO receptor agonist reported few thrombotic symptomatic events but no prospective imaging for evaluation of thrombotic events was included in the protocol. A unique strength of this study was inclusion of prospective imaging for evaluation of portal vein thrombosis. Strategic scheduling is required with use of TPO agonists. Lusutrombopag can be given orally in convenient daily doses and provides a 7-10-day procedural window for scheduling and performing elective invasive procedures. However, because of several days of lag period for platelet production, these agents cannot be used for emergent cases.
Gagan K. Sood, MD, AGAF, FAASLD, is an associate professor of medicine and surgery, division of gastroenterology and hepatology and division of abdominal transplantation, Baylor College of Medicine, Houston. He has no conflicts of interest.
Thrombocytopenia is of clinical concern in patients with cirrhosis, as it complicates routine patient care and results in delayed or canceled procedures due to concern for risk of bleeding. In the last few years, availability of thrombopoietin (TPO) receptor agonists have facilitated the performance of elective invasive procedures in cirrhotic patients with severe thrombocytopenia.
In this integrated analysis of data from two phase 3 studies, Alkhouri et al. demonstrated the efficacy of a novel TPO receptor agonist, lusutrombopag, in reducing bleeding events and need for platelet transfusion in cirrhotic patients undergoing invasive procedures. The risk for thrombosis-related adverse events was not increased in lusutrombopag recipients with or without HCC. Previous studies with another TPO, eltrombopag, resulted in high rate of symptomatic portal vein thrombosis. Avatrombopag, a recently approved TPO receptor agonist reported few thrombotic symptomatic events but no prospective imaging for evaluation of thrombotic events was included in the protocol. A unique strength of this study was inclusion of prospective imaging for evaluation of portal vein thrombosis. Strategic scheduling is required with use of TPO agonists. Lusutrombopag can be given orally in convenient daily doses and provides a 7-10-day procedural window for scheduling and performing elective invasive procedures. However, because of several days of lag period for platelet production, these agents cannot be used for emergent cases.
Gagan K. Sood, MD, AGAF, FAASLD, is an associate professor of medicine and surgery, division of gastroenterology and hepatology and division of abdominal transplantation, Baylor College of Medicine, Houston. He has no conflicts of interest.
For patients with severe thrombocytopenia and chronic liver diseases, including hepatocellular carcinoma, treatment with lusutrombopag prior to invasive procedures significantly decreased the need for platelet transfusions without increasing the need for rescue treatment for bleeding or the rate of thromboembolic events.
In a post hoc analysis of data from 270 patients in two manufacturer-sponsored, multicenter, randomized, double-blind, placebo-controlled, phase 3 trials, significantly more lusutrombopag recipients met the primary efficacy endpoint, including patients with hepatocellular carcinoma (68.0% vs. 8.9% in the placebo group; P < .0001) and those without it (77.0% vs. 21.6%; P < .0001). Rates of treatment-emergent adverse events were similar between the lusutrombopag and placebo groups, and patients with hepatocellular carcinoma were not at increased risk for thrombosis, Naim Alkhouri, MD, of Texas Liver Institute in San Antonio, and associates wrote in Clinical Gastroenterology and Hepatology.
Platelet transfusion is the treatment mainstay for patients with thrombocytopenia related to cirrhosis who are undergoing invasive procedures, but its effects are short-lived, and at least one in five transfusions fails. Thrombopoietin agonists such as lusutrombopag are efficacious and approved in this setting, but they can be prothrombotic, particularly in patients with hepatocellular carcinoma, who already are at heightened risk for portal vein thrombosis.
Dr. Alkhouri and associates performed an integrated analysis of the PLUS 1 trial (Japan, October 2013–May 2014) and the L-PLUS 2 (global, June 2015–April 2017). Participants were adults with Child-Pugh Class A or B chronic liver disease and baseline platelet counts under 50 x 109 per L who were scheduled for invasive procedures. Of the 270 patients, 95 had hepatocellular carcinoma. Patients were randomly assigned on a one-to-one basis to receive either lusutrombopag (3 mg) or placebo daily for up to 7 days before procedures. The primary endpoint was the percentage of patients in the per-protocol population who did not need a platelet transfusion before the invasive procedure or rescue therapy within 7 days afterward.
The treatment and placebo arms were similar except that patients with hepatocellular carcinoma were about 10 years older on average. In patients with hepatocellular carcinoma, 60.5% more lusutrombopag recipients than placebo recipients met the primary endpoint, and rates of bleeding-related adverse events were 9.1% and 15.7%, respectively. In patients with other chronic liver diseases, 52.6% more lusutrombopag recipients met the primary endpoint. Rates of bleeding-related adverse events were 5% and 10.6%.
“Approximately 88% of patients with hepatocellular carcinoma underwent a liver-related procedure, compared with approximately 10% of patients without hepatocellular carcinoma,” the investigators wrote. “This is significant because ablations or transcatheter arterial chemoembolizations can be associated with serious bleeding complications. It is clinically important that, given the greater number of liver-related procedures, the incidence of bleeding-related adverse events was lower in patients treated with lusutrombopag than placebo.”
Imaging after the procedures confirmed low rates of thromboses in both groups and subgroups. Four patients developed portal vein thromboses, including two lusutrombopag recipients (one of whom had hepatocellular carcinoma) and two placebo recipients without hepatocellular carcinoma.
These trials excluded patients undergoing major surgical procedures and those with decompensated cirrhosis; portal vein thrombosis; hematopoietic tumors; aplastic anemia; myelodysplastic syndrome; myelofibrosis; liver transplantation; splenectomy; and thrombocytopenia that was congenital, autoimmune, or drug induced. “A limitation of this study was the high rate of protocol violations related to platelet transfusions,” the researchers noted. “A number of patients [42 in all] were excluded from the per-protocol population owing to receipt of unnecessary platelet transfusions, or because they did not receive a needed platelet transfusion.”Shionogi makes lusutrombopag and sponsored the study. Dr. Alkhouri reported an advisory relationship with Shionogi and Dova Pharma. Two coinvestigators reported being employed by Shionogi. Three coinvestigators also disclosed ties to Shionogi and to several other pharmaceutical companies.
SOURCE: Alkhouri N et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.032.
For patients with severe thrombocytopenia and chronic liver diseases, including hepatocellular carcinoma, treatment with lusutrombopag prior to invasive procedures significantly decreased the need for platelet transfusions without increasing the need for rescue treatment for bleeding or the rate of thromboembolic events.
In a post hoc analysis of data from 270 patients in two manufacturer-sponsored, multicenter, randomized, double-blind, placebo-controlled, phase 3 trials, significantly more lusutrombopag recipients met the primary efficacy endpoint, including patients with hepatocellular carcinoma (68.0% vs. 8.9% in the placebo group; P < .0001) and those without it (77.0% vs. 21.6%; P < .0001). Rates of treatment-emergent adverse events were similar between the lusutrombopag and placebo groups, and patients with hepatocellular carcinoma were not at increased risk for thrombosis, Naim Alkhouri, MD, of Texas Liver Institute in San Antonio, and associates wrote in Clinical Gastroenterology and Hepatology.
Platelet transfusion is the treatment mainstay for patients with thrombocytopenia related to cirrhosis who are undergoing invasive procedures, but its effects are short-lived, and at least one in five transfusions fails. Thrombopoietin agonists such as lusutrombopag are efficacious and approved in this setting, but they can be prothrombotic, particularly in patients with hepatocellular carcinoma, who already are at heightened risk for portal vein thrombosis.
Dr. Alkhouri and associates performed an integrated analysis of the PLUS 1 trial (Japan, October 2013–May 2014) and the L-PLUS 2 (global, June 2015–April 2017). Participants were adults with Child-Pugh Class A or B chronic liver disease and baseline platelet counts under 50 x 109 per L who were scheduled for invasive procedures. Of the 270 patients, 95 had hepatocellular carcinoma. Patients were randomly assigned on a one-to-one basis to receive either lusutrombopag (3 mg) or placebo daily for up to 7 days before procedures. The primary endpoint was the percentage of patients in the per-protocol population who did not need a platelet transfusion before the invasive procedure or rescue therapy within 7 days afterward.
The treatment and placebo arms were similar except that patients with hepatocellular carcinoma were about 10 years older on average. In patients with hepatocellular carcinoma, 60.5% more lusutrombopag recipients than placebo recipients met the primary endpoint, and rates of bleeding-related adverse events were 9.1% and 15.7%, respectively. In patients with other chronic liver diseases, 52.6% more lusutrombopag recipients met the primary endpoint. Rates of bleeding-related adverse events were 5% and 10.6%.
“Approximately 88% of patients with hepatocellular carcinoma underwent a liver-related procedure, compared with approximately 10% of patients without hepatocellular carcinoma,” the investigators wrote. “This is significant because ablations or transcatheter arterial chemoembolizations can be associated with serious bleeding complications. It is clinically important that, given the greater number of liver-related procedures, the incidence of bleeding-related adverse events was lower in patients treated with lusutrombopag than placebo.”
Imaging after the procedures confirmed low rates of thromboses in both groups and subgroups. Four patients developed portal vein thromboses, including two lusutrombopag recipients (one of whom had hepatocellular carcinoma) and two placebo recipients without hepatocellular carcinoma.
These trials excluded patients undergoing major surgical procedures and those with decompensated cirrhosis; portal vein thrombosis; hematopoietic tumors; aplastic anemia; myelodysplastic syndrome; myelofibrosis; liver transplantation; splenectomy; and thrombocytopenia that was congenital, autoimmune, or drug induced. “A limitation of this study was the high rate of protocol violations related to platelet transfusions,” the researchers noted. “A number of patients [42 in all] were excluded from the per-protocol population owing to receipt of unnecessary platelet transfusions, or because they did not receive a needed platelet transfusion.”Shionogi makes lusutrombopag and sponsored the study. Dr. Alkhouri reported an advisory relationship with Shionogi and Dova Pharma. Two coinvestigators reported being employed by Shionogi. Three coinvestigators also disclosed ties to Shionogi and to several other pharmaceutical companies.
SOURCE: Alkhouri N et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.032.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
2020 Cancer Data Trends
Low VWF levels or blood group O not linked to intracerebral hemorrhage risk
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
FROM THROMBOSIS RESEARCH
August 2020 Advances in Precision Oncology
Click here to access August 2020 Advances in Precision Oncology
Table of Contents
- Foreword
- Introduction: Precision Oncology Changes the Game for VA Health Care
- VA National Precision Oncology Program
- Prostate Cancer Foundation-Department of Veterans Affairs Partnership: A Model to Advance Treatment and Care of Invasive Cancers
- The Precision Oncology Program for Cancer of the Prostate Network: A VA-Prostate Cancer Foundation Alliance
- Leveraging Veterans Health Administration Clinical and Research Resources to Accelerate Discovery and Testing in Precision Oncology
- Strategic Initiatives for Veterans With Lung Cancer
- Integrating Germline Genetics Into Precision Oncology Practice in the Veterans Health Administration: Challenges and Opportunities

Click here to access August 2020 Advances in Precision Oncology
Table of Contents
- Foreword
- Introduction: Precision Oncology Changes the Game for VA Health Care
- VA National Precision Oncology Program
- Prostate Cancer Foundation-Department of Veterans Affairs Partnership: A Model to Advance Treatment and Care of Invasive Cancers
- The Precision Oncology Program for Cancer of the Prostate Network: A VA-Prostate Cancer Foundation Alliance
- Leveraging Veterans Health Administration Clinical and Research Resources to Accelerate Discovery and Testing in Precision Oncology
- Strategic Initiatives for Veterans With Lung Cancer
- Integrating Germline Genetics Into Precision Oncology Practice in the Veterans Health Administration: Challenges and Opportunities

Click here to access August 2020 Advances in Precision Oncology
Table of Contents
- Foreword
- Introduction: Precision Oncology Changes the Game for VA Health Care
- VA National Precision Oncology Program
- Prostate Cancer Foundation-Department of Veterans Affairs Partnership: A Model to Advance Treatment and Care of Invasive Cancers
- The Precision Oncology Program for Cancer of the Prostate Network: A VA-Prostate Cancer Foundation Alliance
- Leveraging Veterans Health Administration Clinical and Research Resources to Accelerate Discovery and Testing in Precision Oncology
- Strategic Initiatives for Veterans With Lung Cancer
- Integrating Germline Genetics Into Precision Oncology Practice in the Veterans Health Administration: Challenges and Opportunities

Abstracts Presented at the 2020 AVAHO Annual Meeting (Digital Edition)
FDA approves first maintenance therapy for AML
The Food and Drug Administration has approved an oral form of azacitidine (Onureg) for use as maintenance therapy for patients with acute myeloid leukemia (AML) who have achieved a first complete remission.
The approval extends to patients who have achieved complete remission with incomplete blood count recovery following intensive induction chemotherapy and who are unable to complete intensive curative therapy.
The approval was based on data from the QUAZAR AML-001 trial, which showed that oral azacitidine significantly improved overall survival when compared with placebo.
“It’s not too hard to get these patients into remission,” Harry P. Erba, MD, PhD, director of the Leukemia Program at the Duke Cancer Institute, Durham, N.C., said in an interview last year when these results were first presented at the 2019 annual meeting of the American Society of Hematology. “The problem comes in keeping them in remission.”
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, Australia, said.
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” he said.
Azacitidine is a hypomethylating agent that incorporates into DNA and RNA. It has long been used as an injectable therapy for the treatment of myelodysplastic syndromes.
The approval of the new oral formulation for the new indication of AML “is the culmination of over a decade of research and 13 preclinical and clinical trials,” said Giovanni Caforio, M.D., chairman and chief executive officer of Bristol-Myers Squibb, in a statement.
QUAZAR results
The QUAZAR AML-001 trial was a phase 3, international study involving 472 patients with AML who were within achieving a first complete remission or remission with incomplete blood recovery. All patients had received intensive induction chemotherapy with or without consolidation treatment per investigator preference prior to study entry and were not candidates for hematopoietic stem cell transplant at the time of screening.
Patients were randomly assigned to receive either oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or underwent transplant.
At a median follow-up of more than 41.2 months, the median overall survival was significantly longer for patients who received oral azacitidine at 24.7 months versus 14.8 months for those who received placebo (hazard ratio, 0.69; P < .0009).
Relapse-free survival was also significantly prolonged to 10.2 months for patients who received oral azacitidine vs. 4.8 months for those who received placebo (HR, 0.65; P < .0001).
Serious adverse reactions occurred in 15% of patients who received azacitidine. Events that occurred in 2% of patients or more include pneumonia (8%) and febrile neutropenia (7%). There was one fatal event.
The most common adverse reactions were nausea (65% vs. 24%), vomiting (60% vs. 10%), diarrhea (50% vs. 21%), fatigue/asthenia (44% vs. 25%), constipation (39% vs. 24%), pneumonia (27% vs. 17%), abdominal pain (22% vs. 13%) arthralgia (14% vs. 10%), decreased appetite (13% vs. 6%), febrile neutropenia (12% vs. 8%), dizziness (11% vs. 9%), and pain in extremity (11% vs. 5%). Permanent discontinuation because of an adverse reaction occurred in 8% of patients.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved an oral form of azacitidine (Onureg) for use as maintenance therapy for patients with acute myeloid leukemia (AML) who have achieved a first complete remission.
The approval extends to patients who have achieved complete remission with incomplete blood count recovery following intensive induction chemotherapy and who are unable to complete intensive curative therapy.
The approval was based on data from the QUAZAR AML-001 trial, which showed that oral azacitidine significantly improved overall survival when compared with placebo.
“It’s not too hard to get these patients into remission,” Harry P. Erba, MD, PhD, director of the Leukemia Program at the Duke Cancer Institute, Durham, N.C., said in an interview last year when these results were first presented at the 2019 annual meeting of the American Society of Hematology. “The problem comes in keeping them in remission.”
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, Australia, said.
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” he said.
Azacitidine is a hypomethylating agent that incorporates into DNA and RNA. It has long been used as an injectable therapy for the treatment of myelodysplastic syndromes.
The approval of the new oral formulation for the new indication of AML “is the culmination of over a decade of research and 13 preclinical and clinical trials,” said Giovanni Caforio, M.D., chairman and chief executive officer of Bristol-Myers Squibb, in a statement.
QUAZAR results
The QUAZAR AML-001 trial was a phase 3, international study involving 472 patients with AML who were within achieving a first complete remission or remission with incomplete blood recovery. All patients had received intensive induction chemotherapy with or without consolidation treatment per investigator preference prior to study entry and were not candidates for hematopoietic stem cell transplant at the time of screening.
Patients were randomly assigned to receive either oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or underwent transplant.
At a median follow-up of more than 41.2 months, the median overall survival was significantly longer for patients who received oral azacitidine at 24.7 months versus 14.8 months for those who received placebo (hazard ratio, 0.69; P < .0009).
Relapse-free survival was also significantly prolonged to 10.2 months for patients who received oral azacitidine vs. 4.8 months for those who received placebo (HR, 0.65; P < .0001).
Serious adverse reactions occurred in 15% of patients who received azacitidine. Events that occurred in 2% of patients or more include pneumonia (8%) and febrile neutropenia (7%). There was one fatal event.
The most common adverse reactions were nausea (65% vs. 24%), vomiting (60% vs. 10%), diarrhea (50% vs. 21%), fatigue/asthenia (44% vs. 25%), constipation (39% vs. 24%), pneumonia (27% vs. 17%), abdominal pain (22% vs. 13%) arthralgia (14% vs. 10%), decreased appetite (13% vs. 6%), febrile neutropenia (12% vs. 8%), dizziness (11% vs. 9%), and pain in extremity (11% vs. 5%). Permanent discontinuation because of an adverse reaction occurred in 8% of patients.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved an oral form of azacitidine (Onureg) for use as maintenance therapy for patients with acute myeloid leukemia (AML) who have achieved a first complete remission.
The approval extends to patients who have achieved complete remission with incomplete blood count recovery following intensive induction chemotherapy and who are unable to complete intensive curative therapy.
The approval was based on data from the QUAZAR AML-001 trial, which showed that oral azacitidine significantly improved overall survival when compared with placebo.
“It’s not too hard to get these patients into remission,” Harry P. Erba, MD, PhD, director of the Leukemia Program at the Duke Cancer Institute, Durham, N.C., said in an interview last year when these results were first presented at the 2019 annual meeting of the American Society of Hematology. “The problem comes in keeping them in remission.”
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, Australia, said.
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” he said.
Azacitidine is a hypomethylating agent that incorporates into DNA and RNA. It has long been used as an injectable therapy for the treatment of myelodysplastic syndromes.
The approval of the new oral formulation for the new indication of AML “is the culmination of over a decade of research and 13 preclinical and clinical trials,” said Giovanni Caforio, M.D., chairman and chief executive officer of Bristol-Myers Squibb, in a statement.
QUAZAR results
The QUAZAR AML-001 trial was a phase 3, international study involving 472 patients with AML who were within achieving a first complete remission or remission with incomplete blood recovery. All patients had received intensive induction chemotherapy with or without consolidation treatment per investigator preference prior to study entry and were not candidates for hematopoietic stem cell transplant at the time of screening.
Patients were randomly assigned to receive either oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or underwent transplant.
At a median follow-up of more than 41.2 months, the median overall survival was significantly longer for patients who received oral azacitidine at 24.7 months versus 14.8 months for those who received placebo (hazard ratio, 0.69; P < .0009).
Relapse-free survival was also significantly prolonged to 10.2 months for patients who received oral azacitidine vs. 4.8 months for those who received placebo (HR, 0.65; P < .0001).
Serious adverse reactions occurred in 15% of patients who received azacitidine. Events that occurred in 2% of patients or more include pneumonia (8%) and febrile neutropenia (7%). There was one fatal event.
The most common adverse reactions were nausea (65% vs. 24%), vomiting (60% vs. 10%), diarrhea (50% vs. 21%), fatigue/asthenia (44% vs. 25%), constipation (39% vs. 24%), pneumonia (27% vs. 17%), abdominal pain (22% vs. 13%) arthralgia (14% vs. 10%), decreased appetite (13% vs. 6%), febrile neutropenia (12% vs. 8%), dizziness (11% vs. 9%), and pain in extremity (11% vs. 5%). Permanent discontinuation because of an adverse reaction occurred in 8% of patients.
A version of this article originally appeared on Medscape.com.
The Vaping Epidemic: Implications for Cancer Care
BACKGROUND: There has been an unprecedented increase in vaping by young people. In 2019, an outbreak of acute lung injuries linked to vaping was later recognized as a disease entity known as e-cigarette or vaping product-use associated lung injury (EVALI). A number of cancer therapeutics have been associated with pulmonary toxicity, and the incidence and severity of immune- and chemotherapy-related pneumonitis may be additionally compounded by EVALI. Here we present the case of a 42-year-old male with good-risk advanced seminoma treated with three cycles of bleomycin, etoposide, and cisplatin for curative intent.
CASE REPORT: The patient developed febrile neutropenia after the third cycle of treatment, and upon count recovery, he rapidly deteriorated into acute hypoxic respiratory failure that was ultimately fatal and most consistent with bleomycin-induced lung toxicity. It was later revealed that the patient had been an avid user of tetrahydrocannabinol-containing vaping products, and whether this contributed to a more progressive injurious picture is unknown.
DISCUSION: We have also encountered several cases of non-infectious hypoxic respiratory failure in patients who reported a history of vaping while receiving checkpoint inhibitor immunotherapy for advanced lung cancer. While the incidence of EVALI has declined following its highly publicized notoriety, vaping remains quite popular despite known hazards and represents a significant public health challenge. The risks posed by the use of vaping products may be higher for individuals with cancer who are often older and more frequently suffer from comorbidities that may increase susceptibility to drug-induced lung injury. Consequently, additional efforts should be made to increase awareness of the harmful effects of vaping, especially in the era of COVID-19. To minimize oncology-related pulmonary complications for which vaping may be a risk factor, we updated our infusion nursing evaluation to include questions on vaping activities and implemented provider notification before administering cancer-directed therapy. We have also educated our oncology team about the importance of obtaining a vaping history.
CONCLUSION: As oncology providers for the Veteran population, we should be mindful to counsel our cancer patients about the health risks of vaping and encourage alternative nicotine replacement therapy for those who use nicotine-based vaping products for smoking cessation.
BACKGROUND: There has been an unprecedented increase in vaping by young people. In 2019, an outbreak of acute lung injuries linked to vaping was later recognized as a disease entity known as e-cigarette or vaping product-use associated lung injury (EVALI). A number of cancer therapeutics have been associated with pulmonary toxicity, and the incidence and severity of immune- and chemotherapy-related pneumonitis may be additionally compounded by EVALI. Here we present the case of a 42-year-old male with good-risk advanced seminoma treated with three cycles of bleomycin, etoposide, and cisplatin for curative intent.
CASE REPORT: The patient developed febrile neutropenia after the third cycle of treatment, and upon count recovery, he rapidly deteriorated into acute hypoxic respiratory failure that was ultimately fatal and most consistent with bleomycin-induced lung toxicity. It was later revealed that the patient had been an avid user of tetrahydrocannabinol-containing vaping products, and whether this contributed to a more progressive injurious picture is unknown.
DISCUSION: We have also encountered several cases of non-infectious hypoxic respiratory failure in patients who reported a history of vaping while receiving checkpoint inhibitor immunotherapy for advanced lung cancer. While the incidence of EVALI has declined following its highly publicized notoriety, vaping remains quite popular despite known hazards and represents a significant public health challenge. The risks posed by the use of vaping products may be higher for individuals with cancer who are often older and more frequently suffer from comorbidities that may increase susceptibility to drug-induced lung injury. Consequently, additional efforts should be made to increase awareness of the harmful effects of vaping, especially in the era of COVID-19. To minimize oncology-related pulmonary complications for which vaping may be a risk factor, we updated our infusion nursing evaluation to include questions on vaping activities and implemented provider notification before administering cancer-directed therapy. We have also educated our oncology team about the importance of obtaining a vaping history.
CONCLUSION: As oncology providers for the Veteran population, we should be mindful to counsel our cancer patients about the health risks of vaping and encourage alternative nicotine replacement therapy for those who use nicotine-based vaping products for smoking cessation.
BACKGROUND: There has been an unprecedented increase in vaping by young people. In 2019, an outbreak of acute lung injuries linked to vaping was later recognized as a disease entity known as e-cigarette or vaping product-use associated lung injury (EVALI). A number of cancer therapeutics have been associated with pulmonary toxicity, and the incidence and severity of immune- and chemotherapy-related pneumonitis may be additionally compounded by EVALI. Here we present the case of a 42-year-old male with good-risk advanced seminoma treated with three cycles of bleomycin, etoposide, and cisplatin for curative intent.
CASE REPORT: The patient developed febrile neutropenia after the third cycle of treatment, and upon count recovery, he rapidly deteriorated into acute hypoxic respiratory failure that was ultimately fatal and most consistent with bleomycin-induced lung toxicity. It was later revealed that the patient had been an avid user of tetrahydrocannabinol-containing vaping products, and whether this contributed to a more progressive injurious picture is unknown.
DISCUSION: We have also encountered several cases of non-infectious hypoxic respiratory failure in patients who reported a history of vaping while receiving checkpoint inhibitor immunotherapy for advanced lung cancer. While the incidence of EVALI has declined following its highly publicized notoriety, vaping remains quite popular despite known hazards and represents a significant public health challenge. The risks posed by the use of vaping products may be higher for individuals with cancer who are often older and more frequently suffer from comorbidities that may increase susceptibility to drug-induced lung injury. Consequently, additional efforts should be made to increase awareness of the harmful effects of vaping, especially in the era of COVID-19. To minimize oncology-related pulmonary complications for which vaping may be a risk factor, we updated our infusion nursing evaluation to include questions on vaping activities and implemented provider notification before administering cancer-directed therapy. We have also educated our oncology team about the importance of obtaining a vaping history.
CONCLUSION: As oncology providers for the Veteran population, we should be mindful to counsel our cancer patients about the health risks of vaping and encourage alternative nicotine replacement therapy for those who use nicotine-based vaping products for smoking cessation.