User login
Draft guidelines advise HIV screening for most teens and adults
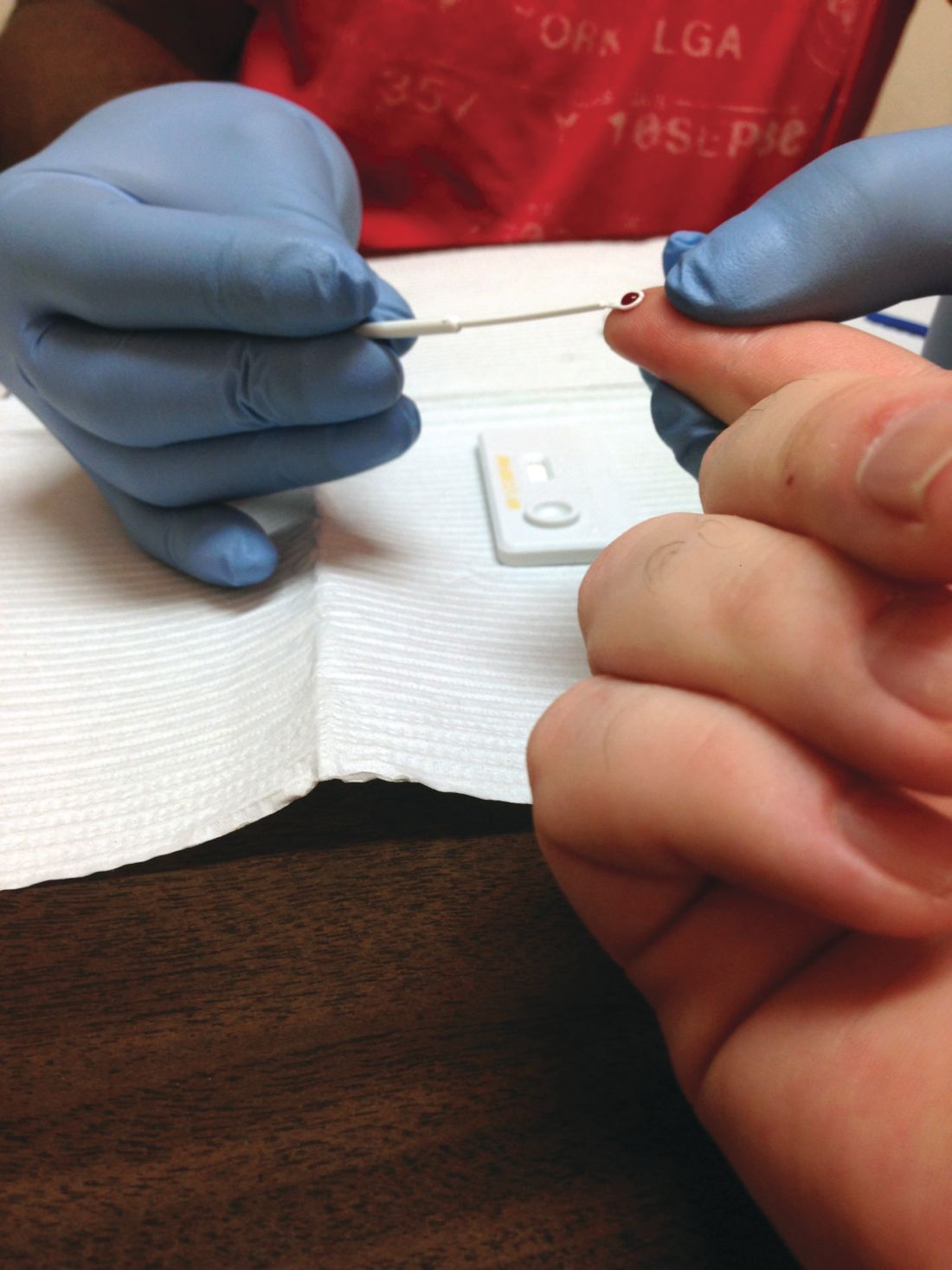
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Are Doctors Willing to PrEP Young Patients?
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
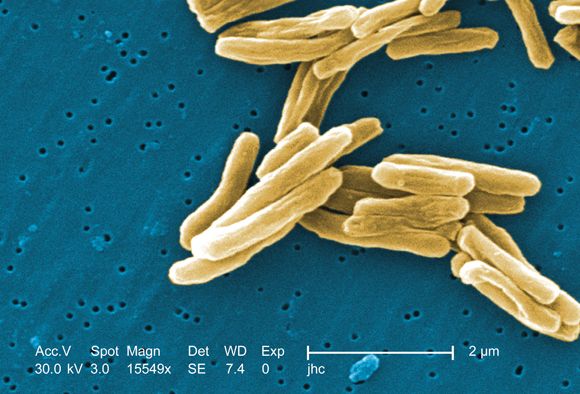
ICYMI: Prednisone lowers IRIS risk in patients with HIV
In patients with HIV, treatment with prednisone for 4 weeks after antiretroviral therapy initiation significantly reduced the risk of tuberculosis-associated immune reconstitution inflammatory syndrome (IRIS). The results from the randomized, double-blind, placebo-controlled trial were published in the New England Journal of Medicine (2018 Nov 14. doi: 10.1056/NEJMoa1800762).
A total of 240 patients were enrolled in the study, with a median age of 36 years; 60% were men, and 73% had microbiologically confirmed tuberculosis. The median CD4 count of the patients was 49 cells/mcL and the median HIV type 1 RNA viral load was 5.5 log10 copies/mL. A total of 120 patients were assigned to each group, with 18 patients lost to follow-up or withdrawn. Tuberculosis-associated IRIS was diagnosed in 39 patients (32.5%) in the prednisone group and in 56 (46.7%) in the placebo group, yielding a relative IRIS risk of 0.70 (95% confidence interval, 0.51-0.96; P = .03), according to the researchers for the PredART (Preventing TB-IRIS in High-Risk Patients: a Randomized Placebo-Controlled Trial of Prednisone) study team.
We covered this story before it was published in the journal. Find our coverage from the Conference on Retroviruses & Opportunistic Infections at the link below.
In patients with HIV, treatment with prednisone for 4 weeks after antiretroviral therapy initiation significantly reduced the risk of tuberculosis-associated immune reconstitution inflammatory syndrome (IRIS). The results from the randomized, double-blind, placebo-controlled trial were published in the New England Journal of Medicine (2018 Nov 14. doi: 10.1056/NEJMoa1800762).
A total of 240 patients were enrolled in the study, with a median age of 36 years; 60% were men, and 73% had microbiologically confirmed tuberculosis. The median CD4 count of the patients was 49 cells/mcL and the median HIV type 1 RNA viral load was 5.5 log10 copies/mL. A total of 120 patients were assigned to each group, with 18 patients lost to follow-up or withdrawn. Tuberculosis-associated IRIS was diagnosed in 39 patients (32.5%) in the prednisone group and in 56 (46.7%) in the placebo group, yielding a relative IRIS risk of 0.70 (95% confidence interval, 0.51-0.96; P = .03), according to the researchers for the PredART (Preventing TB-IRIS in High-Risk Patients: a Randomized Placebo-Controlled Trial of Prednisone) study team.
We covered this story before it was published in the journal. Find our coverage from the Conference on Retroviruses & Opportunistic Infections at the link below.
In patients with HIV, treatment with prednisone for 4 weeks after antiretroviral therapy initiation significantly reduced the risk of tuberculosis-associated immune reconstitution inflammatory syndrome (IRIS). The results from the randomized, double-blind, placebo-controlled trial were published in the New England Journal of Medicine (2018 Nov 14. doi: 10.1056/NEJMoa1800762).
A total of 240 patients were enrolled in the study, with a median age of 36 years; 60% were men, and 73% had microbiologically confirmed tuberculosis. The median CD4 count of the patients was 49 cells/mcL and the median HIV type 1 RNA viral load was 5.5 log10 copies/mL. A total of 120 patients were assigned to each group, with 18 patients lost to follow-up or withdrawn. Tuberculosis-associated IRIS was diagnosed in 39 patients (32.5%) in the prednisone group and in 56 (46.7%) in the placebo group, yielding a relative IRIS risk of 0.70 (95% confidence interval, 0.51-0.96; P = .03), according to the researchers for the PredART (Preventing TB-IRIS in High-Risk Patients: a Randomized Placebo-Controlled Trial of Prednisone) study team.
We covered this story before it was published in the journal. Find our coverage from the Conference on Retroviruses & Opportunistic Infections at the link below.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Rate of STIs is rising, and many U.S. teens are sexually active
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
EXPERT ANALYSIS FROM AAP 18
‘Flexible’ Intervention Helps Patients Overcome Barriers to HIV Treatment
People living with HIV who inject drugs often encounter multiple obstacles, both personal and system related, to beginning and adhering to treatment. But NIH researchers found that an “integrated and flexible intervention” not only helped patients overcome those barriers, but also cut deaths by 50%.
The study, HPTN 074, took place in Indonesia, Ukraine, and Vietnam—3 countries with HIV epidemics driven by injection drug use. Researchers enrolled 502 adults with HIV who inject drugs, and 806 adults without HIV, who inject drugs with them (their injection partners). At ≥ 1 injection partner of every person in the study enrolled. The HIV participants were assigned either the national standard of care for HIV infection and drug use, or the standard of care plus the intervention designed to facilitate treatment. The participants were followed for 1 to 2 years.
In the intervention group, participants were referred to local health care providers for anti-HIV therapy. They were also each assigned a systems navigator, who helped the patient identify and overcome structural barriers to starting and staying in care, such as unfamiliarity with how to enroll in medical care, or difficulty keeping appointments. Psychosocial counselors helped each participant overcome their unique psychological obstacles, such as lack of interest in therapy or fear of stigma.
At the end of the study, 15% of participants with HIV who received standard care had died, compared with 7% of the intervention patients. About 26% of deaths among HIV participants were “clearly” HIV related; 3% were due to drug overdose. Among the 42% of patients who died of unknown cause, 24% had weak immune systems.
The intervention had a “remarkably positive impact” on the participants, said Protocol Chair William Miller, MD, PhD. After 1 year, 41% of the intervention group had undetectable levels of HIV, compared with 24% of the standard-care group. Moreover, 72% of the intervention group were still in treatment, compared with 43% of the standard-care group. Similarly, 41% of intervention patients were in treatment for substance use, compared with 25% of standard-care patients.
The study is designed to be scalable to other settings. Investigators have offered the intervention to all the study participants living with HIV. They will be followed for a second year to find out whether the positive impact is sustained.
Source:
National Institutes of Health. Novel intervention halves rate of death among people living with HIV who inject drugs. https://www.nih.gov/news-events/news-releases/novel-intervention-halves-rate-death-among-people-living-hiv-who-inject-drugs. Published August 31,2018. Accessed October 25, 2018.
People living with HIV who inject drugs often encounter multiple obstacles, both personal and system related, to beginning and adhering to treatment. But NIH researchers found that an “integrated and flexible intervention” not only helped patients overcome those barriers, but also cut deaths by 50%.
The study, HPTN 074, took place in Indonesia, Ukraine, and Vietnam—3 countries with HIV epidemics driven by injection drug use. Researchers enrolled 502 adults with HIV who inject drugs, and 806 adults without HIV, who inject drugs with them (their injection partners). At ≥ 1 injection partner of every person in the study enrolled. The HIV participants were assigned either the national standard of care for HIV infection and drug use, or the standard of care plus the intervention designed to facilitate treatment. The participants were followed for 1 to 2 years.
In the intervention group, participants were referred to local health care providers for anti-HIV therapy. They were also each assigned a systems navigator, who helped the patient identify and overcome structural barriers to starting and staying in care, such as unfamiliarity with how to enroll in medical care, or difficulty keeping appointments. Psychosocial counselors helped each participant overcome their unique psychological obstacles, such as lack of interest in therapy or fear of stigma.
At the end of the study, 15% of participants with HIV who received standard care had died, compared with 7% of the intervention patients. About 26% of deaths among HIV participants were “clearly” HIV related; 3% were due to drug overdose. Among the 42% of patients who died of unknown cause, 24% had weak immune systems.
The intervention had a “remarkably positive impact” on the participants, said Protocol Chair William Miller, MD, PhD. After 1 year, 41% of the intervention group had undetectable levels of HIV, compared with 24% of the standard-care group. Moreover, 72% of the intervention group were still in treatment, compared with 43% of the standard-care group. Similarly, 41% of intervention patients were in treatment for substance use, compared with 25% of standard-care patients.
The study is designed to be scalable to other settings. Investigators have offered the intervention to all the study participants living with HIV. They will be followed for a second year to find out whether the positive impact is sustained.
Source:
National Institutes of Health. Novel intervention halves rate of death among people living with HIV who inject drugs. https://www.nih.gov/news-events/news-releases/novel-intervention-halves-rate-death-among-people-living-hiv-who-inject-drugs. Published August 31,2018. Accessed October 25, 2018.
People living with HIV who inject drugs often encounter multiple obstacles, both personal and system related, to beginning and adhering to treatment. But NIH researchers found that an “integrated and flexible intervention” not only helped patients overcome those barriers, but also cut deaths by 50%.
The study, HPTN 074, took place in Indonesia, Ukraine, and Vietnam—3 countries with HIV epidemics driven by injection drug use. Researchers enrolled 502 adults with HIV who inject drugs, and 806 adults without HIV, who inject drugs with them (their injection partners). At ≥ 1 injection partner of every person in the study enrolled. The HIV participants were assigned either the national standard of care for HIV infection and drug use, or the standard of care plus the intervention designed to facilitate treatment. The participants were followed for 1 to 2 years.
In the intervention group, participants were referred to local health care providers for anti-HIV therapy. They were also each assigned a systems navigator, who helped the patient identify and overcome structural barriers to starting and staying in care, such as unfamiliarity with how to enroll in medical care, or difficulty keeping appointments. Psychosocial counselors helped each participant overcome their unique psychological obstacles, such as lack of interest in therapy or fear of stigma.
At the end of the study, 15% of participants with HIV who received standard care had died, compared with 7% of the intervention patients. About 26% of deaths among HIV participants were “clearly” HIV related; 3% were due to drug overdose. Among the 42% of patients who died of unknown cause, 24% had weak immune systems.
The intervention had a “remarkably positive impact” on the participants, said Protocol Chair William Miller, MD, PhD. After 1 year, 41% of the intervention group had undetectable levels of HIV, compared with 24% of the standard-care group. Moreover, 72% of the intervention group were still in treatment, compared with 43% of the standard-care group. Similarly, 41% of intervention patients were in treatment for substance use, compared with 25% of standard-care patients.
The study is designed to be scalable to other settings. Investigators have offered the intervention to all the study participants living with HIV. They will be followed for a second year to find out whether the positive impact is sustained.
Source:
National Institutes of Health. Novel intervention halves rate of death among people living with HIV who inject drugs. https://www.nih.gov/news-events/news-releases/novel-intervention-halves-rate-death-among-people-living-hiv-who-inject-drugs. Published August 31,2018. Accessed October 25, 2018.
HIV superinfection: No boost to broadly neutralizing antibodies
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
FROM CELL HOST & MICROBE
Key clinical point: Sequential immunizations with heterologous HIV Env immunogens are unlikely to promote broadly neutralizing antibodies.
Major finding: HIV superinfection does not efficiently recruit cross-reactive memory B cells.
Study details: Neutralizing antibody responses were compared between 4 superinfected individuals and 22 singly infected individuals in the CAPRISA 002 cohort.
Disclosures: The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
Source: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
Checkpoint inhibitor seems safe and effective for patients with HIV
MUNICH – Patients with HIV who are treated with nivolumab, a programmed death-1 (PD-1) inhibitor, appear to have similar safety and efficacy outcomes compared with HIV-negative patients treated with the same agent, investigators found.
The retrospective study also showed that viral load and CD4 status were largely unchanged by immunotherapy, lead author Aurélien Gobert, MD, of Groupe Hospitalier Pitié Salpêtrière, Paris, reported at the European Society for Medical Oncology Congress.
HIV increases risks of certain cancer types, Dr. Gobert said in a press release. “These patients are at higher risk for a number of cancers: AIDS-defining forms, the diagnosis of which results in the categorization of a person as suffering from AIDS, but also various other types that they are two to three times more likely to develop than in the general population, such as anal, skin, head and neck, and lung cancer,” he said.
Despite the increased risks, few studies have evaluated cancer treatments for patients with HIV due to exclusions from most clinical trials. As HIV is an immune-based disease, concerns have arisen surrounding the safety and efficacy of using anti-neoplastic immunotherapies for HIV-positive patients. Considering that millions of people worldwide are HIV positive, research in this area can have real-world consequences.
Dr. Gobert and his colleagues analyzed data from CANCERVIH, a French national database of patients with cancer and HIV. Since May 2014, nivolumab has been administered to 20 patients. Nineteen had metastatic non–small-cell lung cancer and 1 had metastatic melanoma. At diagnosis, the median CD4 count was 338.5 per cubic millimeter. Seventeen patients had undetectable viral load, two had fewer than 40 copies per millimeter, and one patient’s viral load was unknown. Dr. Gobert described the population as “demographically homogenous,” with “most patients being males around 60 years old.”
Analysis showed that nivolumab had little impact on CD4 count or viral load. One patient had a decreased CD4 count and an increased viral load, but this occurred during an interruption to antiretroviral therapy, which clouds potential associations with nivolumab. No immune-related adverse events or deaths due to drug toxicity occurred. Efficacy was assessed in 17 patients: Four (24%) showed a partial response, 2 (12%) had stable disease, and 11 (64%) had disease progression.
“Based on these preliminary data, treatment with anti-PD-1 ... seems to be feasible in people with HIV,” Dr. Gobert reported. He added that “antiretroviral therapy should not be interrupted.”
In a comment for ESMO, John Haanen, PhD, of the Netherlands Cancer Institute, Amsterdam, said that the results “confirm those of other, smaller cohorts in showing that while on antiretroviral therapy, cancer patients living with HIV can safely receive anti-PD-1 treatment. The efficacy data also suggests that the overall response rate of HIV-positive patients seems to be similar to that of other cancer patients. These promising results need to be confirmed in larger studies – ideally, in a prospective clinical trial.”
Principal investigator Jean-Philippe Spano, MD, PhD, disclosed relationships with Gilead, Roche, BMS, and others.
SOURCE: Gobert et al. ESMO 2018, Abstract 1213P_PR.
MUNICH – Patients with HIV who are treated with nivolumab, a programmed death-1 (PD-1) inhibitor, appear to have similar safety and efficacy outcomes compared with HIV-negative patients treated with the same agent, investigators found.
The retrospective study also showed that viral load and CD4 status were largely unchanged by immunotherapy, lead author Aurélien Gobert, MD, of Groupe Hospitalier Pitié Salpêtrière, Paris, reported at the European Society for Medical Oncology Congress.
HIV increases risks of certain cancer types, Dr. Gobert said in a press release. “These patients are at higher risk for a number of cancers: AIDS-defining forms, the diagnosis of which results in the categorization of a person as suffering from AIDS, but also various other types that they are two to three times more likely to develop than in the general population, such as anal, skin, head and neck, and lung cancer,” he said.
Despite the increased risks, few studies have evaluated cancer treatments for patients with HIV due to exclusions from most clinical trials. As HIV is an immune-based disease, concerns have arisen surrounding the safety and efficacy of using anti-neoplastic immunotherapies for HIV-positive patients. Considering that millions of people worldwide are HIV positive, research in this area can have real-world consequences.
Dr. Gobert and his colleagues analyzed data from CANCERVIH, a French national database of patients with cancer and HIV. Since May 2014, nivolumab has been administered to 20 patients. Nineteen had metastatic non–small-cell lung cancer and 1 had metastatic melanoma. At diagnosis, the median CD4 count was 338.5 per cubic millimeter. Seventeen patients had undetectable viral load, two had fewer than 40 copies per millimeter, and one patient’s viral load was unknown. Dr. Gobert described the population as “demographically homogenous,” with “most patients being males around 60 years old.”
Analysis showed that nivolumab had little impact on CD4 count or viral load. One patient had a decreased CD4 count and an increased viral load, but this occurred during an interruption to antiretroviral therapy, which clouds potential associations with nivolumab. No immune-related adverse events or deaths due to drug toxicity occurred. Efficacy was assessed in 17 patients: Four (24%) showed a partial response, 2 (12%) had stable disease, and 11 (64%) had disease progression.
“Based on these preliminary data, treatment with anti-PD-1 ... seems to be feasible in people with HIV,” Dr. Gobert reported. He added that “antiretroviral therapy should not be interrupted.”
In a comment for ESMO, John Haanen, PhD, of the Netherlands Cancer Institute, Amsterdam, said that the results “confirm those of other, smaller cohorts in showing that while on antiretroviral therapy, cancer patients living with HIV can safely receive anti-PD-1 treatment. The efficacy data also suggests that the overall response rate of HIV-positive patients seems to be similar to that of other cancer patients. These promising results need to be confirmed in larger studies – ideally, in a prospective clinical trial.”
Principal investigator Jean-Philippe Spano, MD, PhD, disclosed relationships with Gilead, Roche, BMS, and others.
SOURCE: Gobert et al. ESMO 2018, Abstract 1213P_PR.
MUNICH – Patients with HIV who are treated with nivolumab, a programmed death-1 (PD-1) inhibitor, appear to have similar safety and efficacy outcomes compared with HIV-negative patients treated with the same agent, investigators found.
The retrospective study also showed that viral load and CD4 status were largely unchanged by immunotherapy, lead author Aurélien Gobert, MD, of Groupe Hospitalier Pitié Salpêtrière, Paris, reported at the European Society for Medical Oncology Congress.
HIV increases risks of certain cancer types, Dr. Gobert said in a press release. “These patients are at higher risk for a number of cancers: AIDS-defining forms, the diagnosis of which results in the categorization of a person as suffering from AIDS, but also various other types that they are two to three times more likely to develop than in the general population, such as anal, skin, head and neck, and lung cancer,” he said.
Despite the increased risks, few studies have evaluated cancer treatments for patients with HIV due to exclusions from most clinical trials. As HIV is an immune-based disease, concerns have arisen surrounding the safety and efficacy of using anti-neoplastic immunotherapies for HIV-positive patients. Considering that millions of people worldwide are HIV positive, research in this area can have real-world consequences.
Dr. Gobert and his colleagues analyzed data from CANCERVIH, a French national database of patients with cancer and HIV. Since May 2014, nivolumab has been administered to 20 patients. Nineteen had metastatic non–small-cell lung cancer and 1 had metastatic melanoma. At diagnosis, the median CD4 count was 338.5 per cubic millimeter. Seventeen patients had undetectable viral load, two had fewer than 40 copies per millimeter, and one patient’s viral load was unknown. Dr. Gobert described the population as “demographically homogenous,” with “most patients being males around 60 years old.”
Analysis showed that nivolumab had little impact on CD4 count or viral load. One patient had a decreased CD4 count and an increased viral load, but this occurred during an interruption to antiretroviral therapy, which clouds potential associations with nivolumab. No immune-related adverse events or deaths due to drug toxicity occurred. Efficacy was assessed in 17 patients: Four (24%) showed a partial response, 2 (12%) had stable disease, and 11 (64%) had disease progression.
“Based on these preliminary data, treatment with anti-PD-1 ... seems to be feasible in people with HIV,” Dr. Gobert reported. He added that “antiretroviral therapy should not be interrupted.”
In a comment for ESMO, John Haanen, PhD, of the Netherlands Cancer Institute, Amsterdam, said that the results “confirm those of other, smaller cohorts in showing that while on antiretroviral therapy, cancer patients living with HIV can safely receive anti-PD-1 treatment. The efficacy data also suggests that the overall response rate of HIV-positive patients seems to be similar to that of other cancer patients. These promising results need to be confirmed in larger studies – ideally, in a prospective clinical trial.”
Principal investigator Jean-Philippe Spano, MD, PhD, disclosed relationships with Gilead, Roche, BMS, and others.
SOURCE: Gobert et al. ESMO 2018, Abstract 1213P_PR.
REPORTING FROM ESMO 2018
Key clinical point: Patients with HIV who are treated with nivolumab, a programmed death-1 (PD-1) inhibitor, appear to have similar safety and efficacy outcomes compared with HIV-negative patients treated with the same agent.
Major finding: No immune-related adverse events or deaths due to drug toxicity occurred.
Study details: A retrospective analysis of 20 patients with HIV who received nivolumab immunotherapy.
Disclosures: Jean-Philippe Spano, principal investigator, disclosed relationships with Gilead, Roche, BMS, and others.
Source: Gobert et al. ESMO 2018, Abstract 1213P_PR.
Pay attention to kidney disease risk in people living with HIV
The prevalence of chronic kidney disease (CKD) in people living with HIV varied widely, depending on population and criteria, according to a systematic literature review of the PubMed and PsycInfo databases for articles published from January 2000 through August 2016.
The review included all studies that involved adults older than 21 years of age, investigated people living with HIV with CKD, reported prevalence of CKD, and were published in a peer-reviewed journal, according to Jungmin Park, PhD, RN, of CHA University, Pocheon-Si, South Korea, and her colleague.
Out of an initial search yielding 1,960 citations in PubMed and 5,356 citations in PsycInfo, the results were pared down to 21 articles, which met all of the inclusion/exclusion criteria and were used for the final analysis.
The risk factors for CKD in people living with HIV cited most often in the studies consisted of medications, hypertension, older age, diabetes mellitus, hepatitis coinfection (with hepatitis C virus more prominent than hepatitis B virus), low CD4+ T-cell count, and race, Dr. Park and her colleague reported.
Of the various risk factors, the only ones unique to HIV were viral load and CD4+ T-cell count. One study reporting on 5,538 treatment-naive patients in mainland China suggested that HIV viral replication in renal cells may be the cause of renal damage in patients with high viral loads, meaning that viral suppression would improve renal function. However, all of these risk factors are intrinsically linked, according to Dr. Park and her colleague. They added that managing viral load alone would be ineffective in preventing CKD: “Therefore [people living with HIV] will need to effectively manage every aspect of their health, including metabolic and cardiovascular systems.”
Of the 43,114 people living with HIV across the 21 studies, 3,218 (7.3%) had CKD. The reported prevalence of CKD ranged from 2.3% to 53.3%, with the African population having the highest prevalence. Some of the wide variation was possibly attributable to differences in the definitions of CKD used across the various studies.
“The risk of under-diagnosis of CKD can lead to long-term health complications. Health care providers must monitor kidney function and treatment for renal damage carefully, especially for people living with HIV with additional diagnoses of diabetes and/or hypertension, and for those who are aging,” Dr. Park and her colleague concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Park, J et al. J Assoc Nurses AIDS Care. 2018;29:655-66.
The prevalence of chronic kidney disease (CKD) in people living with HIV varied widely, depending on population and criteria, according to a systematic literature review of the PubMed and PsycInfo databases for articles published from January 2000 through August 2016.
The review included all studies that involved adults older than 21 years of age, investigated people living with HIV with CKD, reported prevalence of CKD, and were published in a peer-reviewed journal, according to Jungmin Park, PhD, RN, of CHA University, Pocheon-Si, South Korea, and her colleague.
Out of an initial search yielding 1,960 citations in PubMed and 5,356 citations in PsycInfo, the results were pared down to 21 articles, which met all of the inclusion/exclusion criteria and were used for the final analysis.
The risk factors for CKD in people living with HIV cited most often in the studies consisted of medications, hypertension, older age, diabetes mellitus, hepatitis coinfection (with hepatitis C virus more prominent than hepatitis B virus), low CD4+ T-cell count, and race, Dr. Park and her colleague reported.
Of the various risk factors, the only ones unique to HIV were viral load and CD4+ T-cell count. One study reporting on 5,538 treatment-naive patients in mainland China suggested that HIV viral replication in renal cells may be the cause of renal damage in patients with high viral loads, meaning that viral suppression would improve renal function. However, all of these risk factors are intrinsically linked, according to Dr. Park and her colleague. They added that managing viral load alone would be ineffective in preventing CKD: “Therefore [people living with HIV] will need to effectively manage every aspect of their health, including metabolic and cardiovascular systems.”
Of the 43,114 people living with HIV across the 21 studies, 3,218 (7.3%) had CKD. The reported prevalence of CKD ranged from 2.3% to 53.3%, with the African population having the highest prevalence. Some of the wide variation was possibly attributable to differences in the definitions of CKD used across the various studies.
“The risk of under-diagnosis of CKD can lead to long-term health complications. Health care providers must monitor kidney function and treatment for renal damage carefully, especially for people living with HIV with additional diagnoses of diabetes and/or hypertension, and for those who are aging,” Dr. Park and her colleague concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Park, J et al. J Assoc Nurses AIDS Care. 2018;29:655-66.
The prevalence of chronic kidney disease (CKD) in people living with HIV varied widely, depending on population and criteria, according to a systematic literature review of the PubMed and PsycInfo databases for articles published from January 2000 through August 2016.
The review included all studies that involved adults older than 21 years of age, investigated people living with HIV with CKD, reported prevalence of CKD, and were published in a peer-reviewed journal, according to Jungmin Park, PhD, RN, of CHA University, Pocheon-Si, South Korea, and her colleague.
Out of an initial search yielding 1,960 citations in PubMed and 5,356 citations in PsycInfo, the results were pared down to 21 articles, which met all of the inclusion/exclusion criteria and were used for the final analysis.
The risk factors for CKD in people living with HIV cited most often in the studies consisted of medications, hypertension, older age, diabetes mellitus, hepatitis coinfection (with hepatitis C virus more prominent than hepatitis B virus), low CD4+ T-cell count, and race, Dr. Park and her colleague reported.
Of the various risk factors, the only ones unique to HIV were viral load and CD4+ T-cell count. One study reporting on 5,538 treatment-naive patients in mainland China suggested that HIV viral replication in renal cells may be the cause of renal damage in patients with high viral loads, meaning that viral suppression would improve renal function. However, all of these risk factors are intrinsically linked, according to Dr. Park and her colleague. They added that managing viral load alone would be ineffective in preventing CKD: “Therefore [people living with HIV] will need to effectively manage every aspect of their health, including metabolic and cardiovascular systems.”
Of the 43,114 people living with HIV across the 21 studies, 3,218 (7.3%) had CKD. The reported prevalence of CKD ranged from 2.3% to 53.3%, with the African population having the highest prevalence. Some of the wide variation was possibly attributable to differences in the definitions of CKD used across the various studies.
“The risk of under-diagnosis of CKD can lead to long-term health complications. Health care providers must monitor kidney function and treatment for renal damage carefully, especially for people living with HIV with additional diagnoses of diabetes and/or hypertension, and for those who are aging,” Dr. Park and her colleague concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Park, J et al. J Assoc Nurses AIDS Care. 2018;29:655-66.
FROM THE JOURNAL OF THE ASSOCIATION OF NURSES IN AIDS CARE
Key clinical point: Chronic kidney disease in people living with HIV varies widely across geographic regions.
Major finding: The reported prevalence of CKD in PLWH ranged from 2.3% to 53.3%, with the African population having the highest prevalence.
Study details: Systematic literature review of the PubMed and PsycInfo databases for articles published from January 2000 through August 2016.
Disclosures: The authors reported that they had no conflicts of interest.
Source: J Assoc Nurses AIDS Care. 2018;29:655-66).
HIV testing low in U.S. women engaged in risky behavior
HIV testing rates were low among women whose sexual behaviors increased their risk of HIV infection, and they were especially low among women who reported having anal sex, according to a report published in the American Journal of Obstetrics & Gynecology.
Data from the 2011-2015 National Survey of Family Growth were analyzed to estimate the proportion of sexually active, nonpregnant U.S. women aged 15-44 years who had had an HIV test within the past year. The data was stratified by those who reported anal sex and other risk factors, including having more than two sexual partners, condomless sex with a new partner or multiple partners, gonorrhea in the past year, or any history of syphilis, according to Mary Evans, MD, of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at the Centers for Disease Control and Prevention and her colleagues.
Among the 42.4 million sexually active women assessed, 9.0 million (20%) reported they had had anal sex in the past year. Of these, 19% reported that their providers asked about their types of intercourse, and 20% reported an HIV test within the past year. Overall, HIV testing was higher among women who reported anal sex and whose providers asked about types of sex engaged in than it was among those women whose provider did not ask (38% vs. 16%, respectively; P less than .001). However, HIV testing in the past year was higher for women with other forms of risky behaviors as compared with anal sex, ranging from 35.8% to 47.2%.
“Women who report sexual behaviors such as anal sex would benefit from an HIV test and an assessment for [prevention with preexposure prophylaxis] eligibility. Women’s health care providers are uniquely poised to provide HIV prevention for women who tend to have frequent encounters with the health care system,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Evans ME et al. Am J Obstet Gynecol. 2018 Oct;219(4):383.e1-7.
HIV testing rates were low among women whose sexual behaviors increased their risk of HIV infection, and they were especially low among women who reported having anal sex, according to a report published in the American Journal of Obstetrics & Gynecology.
Data from the 2011-2015 National Survey of Family Growth were analyzed to estimate the proportion of sexually active, nonpregnant U.S. women aged 15-44 years who had had an HIV test within the past year. The data was stratified by those who reported anal sex and other risk factors, including having more than two sexual partners, condomless sex with a new partner or multiple partners, gonorrhea in the past year, or any history of syphilis, according to Mary Evans, MD, of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at the Centers for Disease Control and Prevention and her colleagues.
Among the 42.4 million sexually active women assessed, 9.0 million (20%) reported they had had anal sex in the past year. Of these, 19% reported that their providers asked about their types of intercourse, and 20% reported an HIV test within the past year. Overall, HIV testing was higher among women who reported anal sex and whose providers asked about types of sex engaged in than it was among those women whose provider did not ask (38% vs. 16%, respectively; P less than .001). However, HIV testing in the past year was higher for women with other forms of risky behaviors as compared with anal sex, ranging from 35.8% to 47.2%.
“Women who report sexual behaviors such as anal sex would benefit from an HIV test and an assessment for [prevention with preexposure prophylaxis] eligibility. Women’s health care providers are uniquely poised to provide HIV prevention for women who tend to have frequent encounters with the health care system,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Evans ME et al. Am J Obstet Gynecol. 2018 Oct;219(4):383.e1-7.
HIV testing rates were low among women whose sexual behaviors increased their risk of HIV infection, and they were especially low among women who reported having anal sex, according to a report published in the American Journal of Obstetrics & Gynecology.
Data from the 2011-2015 National Survey of Family Growth were analyzed to estimate the proportion of sexually active, nonpregnant U.S. women aged 15-44 years who had had an HIV test within the past year. The data was stratified by those who reported anal sex and other risk factors, including having more than two sexual partners, condomless sex with a new partner or multiple partners, gonorrhea in the past year, or any history of syphilis, according to Mary Evans, MD, of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at the Centers for Disease Control and Prevention and her colleagues.
Among the 42.4 million sexually active women assessed, 9.0 million (20%) reported they had had anal sex in the past year. Of these, 19% reported that their providers asked about their types of intercourse, and 20% reported an HIV test within the past year. Overall, HIV testing was higher among women who reported anal sex and whose providers asked about types of sex engaged in than it was among those women whose provider did not ask (38% vs. 16%, respectively; P less than .001). However, HIV testing in the past year was higher for women with other forms of risky behaviors as compared with anal sex, ranging from 35.8% to 47.2%.
“Women who report sexual behaviors such as anal sex would benefit from an HIV test and an assessment for [prevention with preexposure prophylaxis] eligibility. Women’s health care providers are uniquely poised to provide HIV prevention for women who tend to have frequent encounters with the health care system,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Evans ME et al. Am J Obstet Gynecol. 2018 Oct;219(4):383.e1-7.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Key clinical point: Health care providers don’t ask sexually active women about risky behavior that would raise their risk of HIV infection.
Major finding: Of women who reported having anal sex, 19% reported that their providers asked about their types of intercourse.
Study details: Data from the 2011-2015 National Survey of Family Growth.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Evans ME et al. Am J Obstet Gynecol. 2018 Oct;219(4):383.e1-7.
Treating cryptococcal meningitis in patients with HIV
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
FROM COCHRANE DATABASE OF SYSTEMIC REVIEWS
Key clinical point: Shorter drug treatment beat the gold standard for HIV-associated cryptococcal meningitis according to a literature review.
Major finding:
Study details: Updated review of articles, registries, and clinical trials during Jan. 1, 1980–July 9, 2018.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Source: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.