User login
Loop Diuretics
Q: When (at what GFR) do you change over from hydrochlorothiazide (HCTZ) to loop diuretics? And what should be the starting dose?
The Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines for hypertension and antihypertensive agents in chronic kidney disease1 (CKD) recommend replacing thiazide diuretics with loop diuretics once a patient’s glomerular filtration rate (GFR) falls below 30 mL/min/1.73 m2.
The mechanism of action for thiazide and loop diuretics differs by site of action in the kidney. Thiazide diuretics work in the distal convoluted tubules by inhibiting sodium (Na+)/chloride (Cl-) channels while the action of loop diuretics is exerted by inhibiting Na+/potassium (K+)/2Cl- channels in the thick ascending limb of the loop of Henle.2 Thiazide diuretics, with exception of metolazone, are ineffective in CKD stages 4 and 5 due to thiazide’s inability to reach the site of action.1,3
The initial furosemide dose should be 40 to 80 mg/d by mouth, preferably divided into two doses to minimize rebound sodium reabsorption.1,4 Weekly dose titrations by 25% to 50% may be made based on fluid status, blood pressure, and potassium level.1 Bumetanide and torsemide are loop diuretics that may also be used to therapeutically replace HCTZ when the GFR falls below 30 mL/min/1.73 m2. The relative potency of bumetanide: furosemide: torsemide is 1:40:20, respectively.5 The relative initiating dose equivalency of furosemide 40 mg would be bumetanide 1 mg or torsemide 20 mg.5,6
Finally, metolazone is a thiazide-related diuretic that retains its effectiveness even at GFR below 30 mL/min/1.73 m2.1,6 Metolazone can be initiated at oral doses of 2.5 to 5.0 mg/d and titrated up to 10 to 20 mg/d. Patients with residual renal function, defined as daily urine output exceeding 100 mL, may continue to use metolazone and loop diuretics even after dialysis is initated.5,7 Upon the loss of residual renal function, all diuretics should be discontinued.
Min Sik Shin
PharmD candidate, 2012, College of Pharmacy, University of Illinois at Chicago
Cheryl L. Gilmartin, PharmD
Clinical Assistant Professor, Department of Pharmacy Practice, College of Pharmacy, University of Illinois at Chicago;
Clinical Pharmacist, Ambulatory Pharmacy Services, University of Illinois Hospital and Health Sciences System, Chicago
REFERENCES
1. K/DOQI [Kidney Disease Outcome Quality Initiative] clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
2. Reilly RF, Jackson EK. Ch 25. Regulation of renal function and vascular volume. In: Chabner BA, Brunton LL, Knollman BC, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Professional; 2010.
3. Sica DA, Gehr TW. Diuretic use in stage 5 chronic kidney disease and end-stage renal disease. Curr Opin Nephrol Hypertens. 2003;12(5): 483-490.
4. Cohen DL, Townsend RR. Treatment of hypertension in patients with chronic kidney disease. US Cardiology. 2009;6(2):54-58.
5. Wickersham RM, ed. Drug Facts and Comparisons. St. Louis, MO: Wolters Kluwer Health; 2009.
6. Comparison of commonly used diuretics (Detail Document). Pharmacist’s Letter/Prescriber’s Letter. February 2012.
7. DRUGDEX® System [Internet database]. Greenwood Village, Colo: Thomson Reuters (Healthcare) Inc. Updated periodically.
8. National Kidney Foundation. MIPPA Kidney Disease Education Benefit. Your Treatment, Your Choice (2010). www.kidney.org/professionals/KLS/YTYC.cfm. Accessed September 19, 2012.
9. Turner JM, Bauer C, Abramowitz MK, et al. Treatment of chronic kidney disease. Kidney Int. 2012;81(4):351-362.
Q: When (at what GFR) do you change over from hydrochlorothiazide (HCTZ) to loop diuretics? And what should be the starting dose?
The Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines for hypertension and antihypertensive agents in chronic kidney disease1 (CKD) recommend replacing thiazide diuretics with loop diuretics once a patient’s glomerular filtration rate (GFR) falls below 30 mL/min/1.73 m2.
The mechanism of action for thiazide and loop diuretics differs by site of action in the kidney. Thiazide diuretics work in the distal convoluted tubules by inhibiting sodium (Na+)/chloride (Cl-) channels while the action of loop diuretics is exerted by inhibiting Na+/potassium (K+)/2Cl- channels in the thick ascending limb of the loop of Henle.2 Thiazide diuretics, with exception of metolazone, are ineffective in CKD stages 4 and 5 due to thiazide’s inability to reach the site of action.1,3
The initial furosemide dose should be 40 to 80 mg/d by mouth, preferably divided into two doses to minimize rebound sodium reabsorption.1,4 Weekly dose titrations by 25% to 50% may be made based on fluid status, blood pressure, and potassium level.1 Bumetanide and torsemide are loop diuretics that may also be used to therapeutically replace HCTZ when the GFR falls below 30 mL/min/1.73 m2. The relative potency of bumetanide: furosemide: torsemide is 1:40:20, respectively.5 The relative initiating dose equivalency of furosemide 40 mg would be bumetanide 1 mg or torsemide 20 mg.5,6
Finally, metolazone is a thiazide-related diuretic that retains its effectiveness even at GFR below 30 mL/min/1.73 m2.1,6 Metolazone can be initiated at oral doses of 2.5 to 5.0 mg/d and titrated up to 10 to 20 mg/d. Patients with residual renal function, defined as daily urine output exceeding 100 mL, may continue to use metolazone and loop diuretics even after dialysis is initated.5,7 Upon the loss of residual renal function, all diuretics should be discontinued.
Min Sik Shin
PharmD candidate, 2012, College of Pharmacy, University of Illinois at Chicago
Cheryl L. Gilmartin, PharmD
Clinical Assistant Professor, Department of Pharmacy Practice, College of Pharmacy, University of Illinois at Chicago;
Clinical Pharmacist, Ambulatory Pharmacy Services, University of Illinois Hospital and Health Sciences System, Chicago
REFERENCES
1. K/DOQI [Kidney Disease Outcome Quality Initiative] clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
2. Reilly RF, Jackson EK. Ch 25. Regulation of renal function and vascular volume. In: Chabner BA, Brunton LL, Knollman BC, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Professional; 2010.
3. Sica DA, Gehr TW. Diuretic use in stage 5 chronic kidney disease and end-stage renal disease. Curr Opin Nephrol Hypertens. 2003;12(5): 483-490.
4. Cohen DL, Townsend RR. Treatment of hypertension in patients with chronic kidney disease. US Cardiology. 2009;6(2):54-58.
5. Wickersham RM, ed. Drug Facts and Comparisons. St. Louis, MO: Wolters Kluwer Health; 2009.
6. Comparison of commonly used diuretics (Detail Document). Pharmacist’s Letter/Prescriber’s Letter. February 2012.
7. DRUGDEX® System [Internet database]. Greenwood Village, Colo: Thomson Reuters (Healthcare) Inc. Updated periodically.
8. National Kidney Foundation. MIPPA Kidney Disease Education Benefit. Your Treatment, Your Choice (2010). www.kidney.org/professionals/KLS/YTYC.cfm. Accessed September 19, 2012.
9. Turner JM, Bauer C, Abramowitz MK, et al. Treatment of chronic kidney disease. Kidney Int. 2012;81(4):351-362.
Q: When (at what GFR) do you change over from hydrochlorothiazide (HCTZ) to loop diuretics? And what should be the starting dose?
The Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines for hypertension and antihypertensive agents in chronic kidney disease1 (CKD) recommend replacing thiazide diuretics with loop diuretics once a patient’s glomerular filtration rate (GFR) falls below 30 mL/min/1.73 m2.
The mechanism of action for thiazide and loop diuretics differs by site of action in the kidney. Thiazide diuretics work in the distal convoluted tubules by inhibiting sodium (Na+)/chloride (Cl-) channels while the action of loop diuretics is exerted by inhibiting Na+/potassium (K+)/2Cl- channels in the thick ascending limb of the loop of Henle.2 Thiazide diuretics, with exception of metolazone, are ineffective in CKD stages 4 and 5 due to thiazide’s inability to reach the site of action.1,3
The initial furosemide dose should be 40 to 80 mg/d by mouth, preferably divided into two doses to minimize rebound sodium reabsorption.1,4 Weekly dose titrations by 25% to 50% may be made based on fluid status, blood pressure, and potassium level.1 Bumetanide and torsemide are loop diuretics that may also be used to therapeutically replace HCTZ when the GFR falls below 30 mL/min/1.73 m2. The relative potency of bumetanide: furosemide: torsemide is 1:40:20, respectively.5 The relative initiating dose equivalency of furosemide 40 mg would be bumetanide 1 mg or torsemide 20 mg.5,6
Finally, metolazone is a thiazide-related diuretic that retains its effectiveness even at GFR below 30 mL/min/1.73 m2.1,6 Metolazone can be initiated at oral doses of 2.5 to 5.0 mg/d and titrated up to 10 to 20 mg/d. Patients with residual renal function, defined as daily urine output exceeding 100 mL, may continue to use metolazone and loop diuretics even after dialysis is initated.5,7 Upon the loss of residual renal function, all diuretics should be discontinued.
Min Sik Shin
PharmD candidate, 2012, College of Pharmacy, University of Illinois at Chicago
Cheryl L. Gilmartin, PharmD
Clinical Assistant Professor, Department of Pharmacy Practice, College of Pharmacy, University of Illinois at Chicago;
Clinical Pharmacist, Ambulatory Pharmacy Services, University of Illinois Hospital and Health Sciences System, Chicago
REFERENCES
1. K/DOQI [Kidney Disease Outcome Quality Initiative] clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
2. Reilly RF, Jackson EK. Ch 25. Regulation of renal function and vascular volume. In: Chabner BA, Brunton LL, Knollman BC, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Professional; 2010.
3. Sica DA, Gehr TW. Diuretic use in stage 5 chronic kidney disease and end-stage renal disease. Curr Opin Nephrol Hypertens. 2003;12(5): 483-490.
4. Cohen DL, Townsend RR. Treatment of hypertension in patients with chronic kidney disease. US Cardiology. 2009;6(2):54-58.
5. Wickersham RM, ed. Drug Facts and Comparisons. St. Louis, MO: Wolters Kluwer Health; 2009.
6. Comparison of commonly used diuretics (Detail Document). Pharmacist’s Letter/Prescriber’s Letter. February 2012.
7. DRUGDEX® System [Internet database]. Greenwood Village, Colo: Thomson Reuters (Healthcare) Inc. Updated periodically.
8. National Kidney Foundation. MIPPA Kidney Disease Education Benefit. Your Treatment, Your Choice (2010). www.kidney.org/professionals/KLS/YTYC.cfm. Accessed September 19, 2012.
9. Turner JM, Bauer C, Abramowitz MK, et al. Treatment of chronic kidney disease. Kidney Int. 2012;81(4):351-362.
Can calcium supplements cause serious adverse effects in healthy people?
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
Evidence-based answers from the Family Physicians Inquiries Network
Rhabdomyolysis after spin class?
Primary care physicians frequently encourage patients to lead a more active, healthy lifestyle. The rise in popularity of endurance events, yoga, and organized gym-based fitness classes has, no doubt, improved the health of those who participate. But what happens when an individual moves too quickly from a sedentary existence to a more physically active one?
In this article we describe 2 clinical cases of rhabdomyolysis that occurred after healthy individuals participated for the first time in a class involving high-intensity stationary cycling, known as “spinning.” This exercise activity originated in California around 1989 when a competitive cyclist introduced variable resistance and speed training to stationary cycle workouts.1 Over the last 10 years, spinning has gained a worldwide following as a means of building cardiovascular endurance while achieving a significant calorie burn.
CASE 1: Lack of conditioning, improper hydration spell trouble
A previously healthy 38-year-old white man presented with left lower extremity pain and dark urine. Three days earlier, he had participated in a spin class for the first time. Despite a sedentary lifestyle, he had no difficulty completing the session and felt fine during the class. He did feel mildly fatigued afterward. The next day, he played 18 holes of golf in hot, humid weather. He admitted to poor fluid intake, stating he “drank a few beers” during the round. The next day, he began noticing discomfort and swelling in his left knee, which progressed to his anterior thigh. That evening, he became concerned because of a dark red tint to his urine. He was not taking any medications.
The physical exam was unremarkable except for a moderately swollen, tender knee with reduced range of motion. An x-ray of the knee showed a moderate suprapatellar effusion, but no fracture or dislocation. Urinalysis was remarkable for blood and myoglobin. The CPK value was 149,985 U/L (normal, 24-170 U/L), AST was 2234 U/L (normal, 9-25 U/L), ALT was 570 U/L (normal, 7-30 U/L), and BMI was 26.6 kg/m2. Renal function was normal, as evidenced by a BUN of 17 mg/dL and a creatinine level of 1.0 mg/dL. He was afebrile and his WBC count was 9.6 x 103/mm3.
We hospitalized the patient with a diagnosis of rhabdomyolysis and started him on aggressive intravenous (IV) hydration. The patient’s CPK and transaminase levels started trending down the next day, urine output (UOP) remained at goal, and renal function remained stable. Pain and swelling diminished over the next 3 days. He was discharged home on Day 4. At discharge, his CPK level was 26,180 U/L, BUN 10 mg/dL, and creatinine 0.8 mg/dL. At 1 month follow-up, his CPK was within normal limits.
CASE 2: Even those who exercise regularly can overdo it
A previously healthy 26-year-old white woman sought care at our clinic complaining of bilateral leg pain and dark urine. Despite being overweight, she regularly engaged in moderate exercise, and 2 days prior had participated in her first spin class. She felt some discomfort 30 minutes into the class, and the next day noted discomfort in her anterior thighs, which progressively worsened. Two days after the workout, her pain was worse and her urine became reddish-brown. She was not taking any medications.
The physical exam was unremarkable except for antalgic gait and tenderness of the anterior thighs, which were also moderately firm and warm to the touch. Urinalysis showed a large blood concentration and was positive for myoglobin. ALT was 366 U/L, AST was 1383 U/L, CPK was 86,592 U/L, and BMI was 33.36 kg/m2. A BUN level of 11 mg/dL and creatinine level of 0.8 mg/dL suggested normal renal function. Her WBC count was 12.2 x 103/mm3.
We hospitalized the patient for a presumptive diagnosis of rhabdomyolysis, and initiated aggressive IV hydration to achieve a UOP of at least 200 mL/h. CPK levels and renal and liver function were closely monitored. On hospital Day 2, the patient’s thighs were tender and tight, so we consulted orthopedics about possible compartment syndrome. The consultant believed that intervention was unwarranted.
By Day 3, the swelling and pain began to resolve. UOP remained at target, and CPK and transaminase levels continued to trend down. Renal function remained stable. The patient was discharged home on Day 4 with a CPK of 11,388 U/L, BUN of 8 mg/dL, and creatinine of 0.7 mg/dL. At her 2-week follow-up, CPK was down to 772 U/L, and transaminases were within normal limits.
Discussion
Rhabdomyolysis occurs as a result of damage to the striated muscle cell membranes. Such injury releases into the systemic circulation calcium, potassium, phosphate, urate myoglobin, CPK, aldolase, lactate dehydrogenase, AST, and ALT. In the presence of excess calcium, further muscle fiber necrosis occurs and can lead to acute renal failure.2,3 Serum haptoglobin binding capacity becomes overly saturated. This results in free myoglobin, causing renal tubular obstruction. Myoglobin then dissociates into ferrihemate and globulin. Ferrihemate further exacerbates failure of the renal tubular transport system, eventually resulting in cell death and renal failure.2
Military trainees and casual athletes comprise many of the cases of exercise- induced rhabdomyolysis.4-6 People who exercise regularly are less likely to develop the condition than their more sedentary counterparts. As with our cases, a sudden increase in the intensity and duration of vigorous exercise, without proper training, may increase the likelihood of rhabdomyolysis.6
Other potential underlying causes. In addition to exercise and dehydration as depicted in our cases, rhabdomyolysis can result from burns, shock, acidosis, infections, crush trauma, immobility, malignancy, medications, toxins, abuse of drugs, or pre-existing illness such as sickle cell trait or other metabolic conditions.7,8
Clinical presentation varies. Regardless of the cause, patients typically present with muscle pain, weakness and cramping, and discolored urine.4,8 However, many patients will have dark urine associated with other symptoms, such as general malaise, visceral pain, swelling, muscle stiffness and tightness, fever, tachycardia, nausea, and vomiting.2,3 A careful history may help elucidate the cause.
Laboratory clues. Diagnostic guidelines commonly specify a serum CPK level 5 times the upper limit of normal as an indication of rhabdomyolysis, specifically in the exertional variety.9 Typically the level of this is around 1000 U/L.3 However, there is no agreement on what CPK level is diagnostic of rhabdomyolysis. Suggestions range from 1000 to 20,000 U/L.3,8 A CPK level in excess of 5000 U/L increases the risk for acute renal failure and renal cell death.3,10 In athletes, an elevated CPK after working out is not uncommon and may be much higher than in other individuals.6,8 Endurance exercises such as marathon running or cycling have been noted to elevate CPK for up to 2 hours postexercise.8
Myoglobin becomes detectable in urine when it exceeds 1.5 mg/dL.10 Urine becomes tea-colored or reddish-brown when myoglobin is >100 mg/dL.10
Complications from rhabdomyolysis include compartment syndrome, hyperkalemia, disseminated intravascular coagulation, coagulopathies, and acute renal failure.
Treatment for rhabdomyolysis consists of aggressive IV hydration with normal saline (with variable rate) or crystalloids to maintain a UOP of 200 to 300 mL/h.2,3,11 Avoid fluid overload in the elderly and those with renal or cardiac disease.2 As CPK and myoglobin continue to trend down, it’s important to adjust IV fluids and electrolyte replacement.2,11 Using bicarbonate to alkalinize the urine is controversial, with no studies showing any benefit.3,10 In severe situations, consider a nephrology consult for hemodialysis to bring down CPK, which may be secondary to renal failure and hyperkalemia.2,10 However, renal failure is less likely to occur in physically active, healthy athletes.
Advice after recovery. After an episode of acute rhabdomyolysis, conditioned athletes can return to physical training with resolution of their symptoms or a CPK level from 1000 to 5000 U/L, usually within a week.6 A more judicious approach may be needed for less fit individuals. Regardless of their fitness level, advise patients to avoid diuretics and alcohol before exercise, remain hydrated during and after exercise, and avoid overheating to decrease the likelihood of developing rhabdomyolysis.4 However, in patients with sickle cell trait, exertional sickling can occur with intensity of exercise without overheating.7
In the case of our male patient, poor physical conditioning and intensive, prolonged exercise followed by poor hydration and the diuretic effect of alcohol created the perfect storm for the development of rhabdomyolysis. On the other hand, our female patient routinely exercised, but still pushed herself beyond her limit and went too far too fast. Although BMI may play a role in the development of rhabdomyolysis, it does not appear to be as significant a factor as hydration status and overall physical conditioning.
Our patients’ prompt attention to the need for medical help and the recognition of the problem by their clinicians contributed to good outcomes in both cases.
CORRESPONDENCE Jacqueline DuBose, MD, Department of Family Medicine, Georgia Health Sciences University, 1120 15th Street, Augusta, GA 30912; [email protected]
1. Metzker G. The man who put a new spin on stationary bikes. Los Angeles Times. April 17, 2000. Available at: http://articles.latimes.com/2000/apr/17/health/he-20459. Accessed February 7, 2012.
2. Sauret JM, Marinides G, Wang GK. Rhabdomyolysis. Am Fam Physician. 2002;65:907-912.
3. Cervellin G, Comelli I, Lippi G. Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Clin Chem Lab Med. 2010;48:749-756.
4. Sayers SP, Clarkson PM. Excercise-induced rhabdomyolysis. Curr Sports Med Rep. 2002;1:59-60.
5. Alpers JP, Jones LK. Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010;42:487-491.
6. Eichner ER. Exertional rhabdomyolysis. Curr Sports Med Rep. 2008;7:3-4.
7. Eichner ER. Pearls and pitfalls: exertional sickling. Curr Sports Med Rep. 2010;9:3-4.
8. Clarkson PM, Eichner ER. Exertional rhabdomyolysis: does elevated blood creatine kinase foretell renal failure? Curr Sports Med Rep. 2006;5:57-60.
9. Capaccchione JF, Muldoon SM. The relationship between exertional heat illness, exertional rhabdomyolysis, and malignant hyperthermia. Anesth Analg. 2009;109:1065-1069.
10. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis—an overview for clinicians. Crit Care. 2005;9:158-169.
11. Young IM, Thomson K. Spinning-induced rhabdomyolysis: a case report. Eur J Emerg Med. 2004;11:358-359.
Primary care physicians frequently encourage patients to lead a more active, healthy lifestyle. The rise in popularity of endurance events, yoga, and organized gym-based fitness classes has, no doubt, improved the health of those who participate. But what happens when an individual moves too quickly from a sedentary existence to a more physically active one?
In this article we describe 2 clinical cases of rhabdomyolysis that occurred after healthy individuals participated for the first time in a class involving high-intensity stationary cycling, known as “spinning.” This exercise activity originated in California around 1989 when a competitive cyclist introduced variable resistance and speed training to stationary cycle workouts.1 Over the last 10 years, spinning has gained a worldwide following as a means of building cardiovascular endurance while achieving a significant calorie burn.
CASE 1: Lack of conditioning, improper hydration spell trouble
A previously healthy 38-year-old white man presented with left lower extremity pain and dark urine. Three days earlier, he had participated in a spin class for the first time. Despite a sedentary lifestyle, he had no difficulty completing the session and felt fine during the class. He did feel mildly fatigued afterward. The next day, he played 18 holes of golf in hot, humid weather. He admitted to poor fluid intake, stating he “drank a few beers” during the round. The next day, he began noticing discomfort and swelling in his left knee, which progressed to his anterior thigh. That evening, he became concerned because of a dark red tint to his urine. He was not taking any medications.
The physical exam was unremarkable except for a moderately swollen, tender knee with reduced range of motion. An x-ray of the knee showed a moderate suprapatellar effusion, but no fracture or dislocation. Urinalysis was remarkable for blood and myoglobin. The CPK value was 149,985 U/L (normal, 24-170 U/L), AST was 2234 U/L (normal, 9-25 U/L), ALT was 570 U/L (normal, 7-30 U/L), and BMI was 26.6 kg/m2. Renal function was normal, as evidenced by a BUN of 17 mg/dL and a creatinine level of 1.0 mg/dL. He was afebrile and his WBC count was 9.6 x 103/mm3.
We hospitalized the patient with a diagnosis of rhabdomyolysis and started him on aggressive intravenous (IV) hydration. The patient’s CPK and transaminase levels started trending down the next day, urine output (UOP) remained at goal, and renal function remained stable. Pain and swelling diminished over the next 3 days. He was discharged home on Day 4. At discharge, his CPK level was 26,180 U/L, BUN 10 mg/dL, and creatinine 0.8 mg/dL. At 1 month follow-up, his CPK was within normal limits.
CASE 2: Even those who exercise regularly can overdo it
A previously healthy 26-year-old white woman sought care at our clinic complaining of bilateral leg pain and dark urine. Despite being overweight, she regularly engaged in moderate exercise, and 2 days prior had participated in her first spin class. She felt some discomfort 30 minutes into the class, and the next day noted discomfort in her anterior thighs, which progressively worsened. Two days after the workout, her pain was worse and her urine became reddish-brown. She was not taking any medications.
The physical exam was unremarkable except for antalgic gait and tenderness of the anterior thighs, which were also moderately firm and warm to the touch. Urinalysis showed a large blood concentration and was positive for myoglobin. ALT was 366 U/L, AST was 1383 U/L, CPK was 86,592 U/L, and BMI was 33.36 kg/m2. A BUN level of 11 mg/dL and creatinine level of 0.8 mg/dL suggested normal renal function. Her WBC count was 12.2 x 103/mm3.
We hospitalized the patient for a presumptive diagnosis of rhabdomyolysis, and initiated aggressive IV hydration to achieve a UOP of at least 200 mL/h. CPK levels and renal and liver function were closely monitored. On hospital Day 2, the patient’s thighs were tender and tight, so we consulted orthopedics about possible compartment syndrome. The consultant believed that intervention was unwarranted.
By Day 3, the swelling and pain began to resolve. UOP remained at target, and CPK and transaminase levels continued to trend down. Renal function remained stable. The patient was discharged home on Day 4 with a CPK of 11,388 U/L, BUN of 8 mg/dL, and creatinine of 0.7 mg/dL. At her 2-week follow-up, CPK was down to 772 U/L, and transaminases were within normal limits.
Discussion
Rhabdomyolysis occurs as a result of damage to the striated muscle cell membranes. Such injury releases into the systemic circulation calcium, potassium, phosphate, urate myoglobin, CPK, aldolase, lactate dehydrogenase, AST, and ALT. In the presence of excess calcium, further muscle fiber necrosis occurs and can lead to acute renal failure.2,3 Serum haptoglobin binding capacity becomes overly saturated. This results in free myoglobin, causing renal tubular obstruction. Myoglobin then dissociates into ferrihemate and globulin. Ferrihemate further exacerbates failure of the renal tubular transport system, eventually resulting in cell death and renal failure.2
Military trainees and casual athletes comprise many of the cases of exercise- induced rhabdomyolysis.4-6 People who exercise regularly are less likely to develop the condition than their more sedentary counterparts. As with our cases, a sudden increase in the intensity and duration of vigorous exercise, without proper training, may increase the likelihood of rhabdomyolysis.6
Other potential underlying causes. In addition to exercise and dehydration as depicted in our cases, rhabdomyolysis can result from burns, shock, acidosis, infections, crush trauma, immobility, malignancy, medications, toxins, abuse of drugs, or pre-existing illness such as sickle cell trait or other metabolic conditions.7,8
Clinical presentation varies. Regardless of the cause, patients typically present with muscle pain, weakness and cramping, and discolored urine.4,8 However, many patients will have dark urine associated with other symptoms, such as general malaise, visceral pain, swelling, muscle stiffness and tightness, fever, tachycardia, nausea, and vomiting.2,3 A careful history may help elucidate the cause.
Laboratory clues. Diagnostic guidelines commonly specify a serum CPK level 5 times the upper limit of normal as an indication of rhabdomyolysis, specifically in the exertional variety.9 Typically the level of this is around 1000 U/L.3 However, there is no agreement on what CPK level is diagnostic of rhabdomyolysis. Suggestions range from 1000 to 20,000 U/L.3,8 A CPK level in excess of 5000 U/L increases the risk for acute renal failure and renal cell death.3,10 In athletes, an elevated CPK after working out is not uncommon and may be much higher than in other individuals.6,8 Endurance exercises such as marathon running or cycling have been noted to elevate CPK for up to 2 hours postexercise.8
Myoglobin becomes detectable in urine when it exceeds 1.5 mg/dL.10 Urine becomes tea-colored or reddish-brown when myoglobin is >100 mg/dL.10
Complications from rhabdomyolysis include compartment syndrome, hyperkalemia, disseminated intravascular coagulation, coagulopathies, and acute renal failure.
Treatment for rhabdomyolysis consists of aggressive IV hydration with normal saline (with variable rate) or crystalloids to maintain a UOP of 200 to 300 mL/h.2,3,11 Avoid fluid overload in the elderly and those with renal or cardiac disease.2 As CPK and myoglobin continue to trend down, it’s important to adjust IV fluids and electrolyte replacement.2,11 Using bicarbonate to alkalinize the urine is controversial, with no studies showing any benefit.3,10 In severe situations, consider a nephrology consult for hemodialysis to bring down CPK, which may be secondary to renal failure and hyperkalemia.2,10 However, renal failure is less likely to occur in physically active, healthy athletes.
Advice after recovery. After an episode of acute rhabdomyolysis, conditioned athletes can return to physical training with resolution of their symptoms or a CPK level from 1000 to 5000 U/L, usually within a week.6 A more judicious approach may be needed for less fit individuals. Regardless of their fitness level, advise patients to avoid diuretics and alcohol before exercise, remain hydrated during and after exercise, and avoid overheating to decrease the likelihood of developing rhabdomyolysis.4 However, in patients with sickle cell trait, exertional sickling can occur with intensity of exercise without overheating.7
In the case of our male patient, poor physical conditioning and intensive, prolonged exercise followed by poor hydration and the diuretic effect of alcohol created the perfect storm for the development of rhabdomyolysis. On the other hand, our female patient routinely exercised, but still pushed herself beyond her limit and went too far too fast. Although BMI may play a role in the development of rhabdomyolysis, it does not appear to be as significant a factor as hydration status and overall physical conditioning.
Our patients’ prompt attention to the need for medical help and the recognition of the problem by their clinicians contributed to good outcomes in both cases.
CORRESPONDENCE Jacqueline DuBose, MD, Department of Family Medicine, Georgia Health Sciences University, 1120 15th Street, Augusta, GA 30912; [email protected]
Primary care physicians frequently encourage patients to lead a more active, healthy lifestyle. The rise in popularity of endurance events, yoga, and organized gym-based fitness classes has, no doubt, improved the health of those who participate. But what happens when an individual moves too quickly from a sedentary existence to a more physically active one?
In this article we describe 2 clinical cases of rhabdomyolysis that occurred after healthy individuals participated for the first time in a class involving high-intensity stationary cycling, known as “spinning.” This exercise activity originated in California around 1989 when a competitive cyclist introduced variable resistance and speed training to stationary cycle workouts.1 Over the last 10 years, spinning has gained a worldwide following as a means of building cardiovascular endurance while achieving a significant calorie burn.
CASE 1: Lack of conditioning, improper hydration spell trouble
A previously healthy 38-year-old white man presented with left lower extremity pain and dark urine. Three days earlier, he had participated in a spin class for the first time. Despite a sedentary lifestyle, he had no difficulty completing the session and felt fine during the class. He did feel mildly fatigued afterward. The next day, he played 18 holes of golf in hot, humid weather. He admitted to poor fluid intake, stating he “drank a few beers” during the round. The next day, he began noticing discomfort and swelling in his left knee, which progressed to his anterior thigh. That evening, he became concerned because of a dark red tint to his urine. He was not taking any medications.
The physical exam was unremarkable except for a moderately swollen, tender knee with reduced range of motion. An x-ray of the knee showed a moderate suprapatellar effusion, but no fracture or dislocation. Urinalysis was remarkable for blood and myoglobin. The CPK value was 149,985 U/L (normal, 24-170 U/L), AST was 2234 U/L (normal, 9-25 U/L), ALT was 570 U/L (normal, 7-30 U/L), and BMI was 26.6 kg/m2. Renal function was normal, as evidenced by a BUN of 17 mg/dL and a creatinine level of 1.0 mg/dL. He was afebrile and his WBC count was 9.6 x 103/mm3.
We hospitalized the patient with a diagnosis of rhabdomyolysis and started him on aggressive intravenous (IV) hydration. The patient’s CPK and transaminase levels started trending down the next day, urine output (UOP) remained at goal, and renal function remained stable. Pain and swelling diminished over the next 3 days. He was discharged home on Day 4. At discharge, his CPK level was 26,180 U/L, BUN 10 mg/dL, and creatinine 0.8 mg/dL. At 1 month follow-up, his CPK was within normal limits.
CASE 2: Even those who exercise regularly can overdo it
A previously healthy 26-year-old white woman sought care at our clinic complaining of bilateral leg pain and dark urine. Despite being overweight, she regularly engaged in moderate exercise, and 2 days prior had participated in her first spin class. She felt some discomfort 30 minutes into the class, and the next day noted discomfort in her anterior thighs, which progressively worsened. Two days after the workout, her pain was worse and her urine became reddish-brown. She was not taking any medications.
The physical exam was unremarkable except for antalgic gait and tenderness of the anterior thighs, which were also moderately firm and warm to the touch. Urinalysis showed a large blood concentration and was positive for myoglobin. ALT was 366 U/L, AST was 1383 U/L, CPK was 86,592 U/L, and BMI was 33.36 kg/m2. A BUN level of 11 mg/dL and creatinine level of 0.8 mg/dL suggested normal renal function. Her WBC count was 12.2 x 103/mm3.
We hospitalized the patient for a presumptive diagnosis of rhabdomyolysis, and initiated aggressive IV hydration to achieve a UOP of at least 200 mL/h. CPK levels and renal and liver function were closely monitored. On hospital Day 2, the patient’s thighs were tender and tight, so we consulted orthopedics about possible compartment syndrome. The consultant believed that intervention was unwarranted.
By Day 3, the swelling and pain began to resolve. UOP remained at target, and CPK and transaminase levels continued to trend down. Renal function remained stable. The patient was discharged home on Day 4 with a CPK of 11,388 U/L, BUN of 8 mg/dL, and creatinine of 0.7 mg/dL. At her 2-week follow-up, CPK was down to 772 U/L, and transaminases were within normal limits.
Discussion
Rhabdomyolysis occurs as a result of damage to the striated muscle cell membranes. Such injury releases into the systemic circulation calcium, potassium, phosphate, urate myoglobin, CPK, aldolase, lactate dehydrogenase, AST, and ALT. In the presence of excess calcium, further muscle fiber necrosis occurs and can lead to acute renal failure.2,3 Serum haptoglobin binding capacity becomes overly saturated. This results in free myoglobin, causing renal tubular obstruction. Myoglobin then dissociates into ferrihemate and globulin. Ferrihemate further exacerbates failure of the renal tubular transport system, eventually resulting in cell death and renal failure.2
Military trainees and casual athletes comprise many of the cases of exercise- induced rhabdomyolysis.4-6 People who exercise regularly are less likely to develop the condition than their more sedentary counterparts. As with our cases, a sudden increase in the intensity and duration of vigorous exercise, without proper training, may increase the likelihood of rhabdomyolysis.6
Other potential underlying causes. In addition to exercise and dehydration as depicted in our cases, rhabdomyolysis can result from burns, shock, acidosis, infections, crush trauma, immobility, malignancy, medications, toxins, abuse of drugs, or pre-existing illness such as sickle cell trait or other metabolic conditions.7,8
Clinical presentation varies. Regardless of the cause, patients typically present with muscle pain, weakness and cramping, and discolored urine.4,8 However, many patients will have dark urine associated with other symptoms, such as general malaise, visceral pain, swelling, muscle stiffness and tightness, fever, tachycardia, nausea, and vomiting.2,3 A careful history may help elucidate the cause.
Laboratory clues. Diagnostic guidelines commonly specify a serum CPK level 5 times the upper limit of normal as an indication of rhabdomyolysis, specifically in the exertional variety.9 Typically the level of this is around 1000 U/L.3 However, there is no agreement on what CPK level is diagnostic of rhabdomyolysis. Suggestions range from 1000 to 20,000 U/L.3,8 A CPK level in excess of 5000 U/L increases the risk for acute renal failure and renal cell death.3,10 In athletes, an elevated CPK after working out is not uncommon and may be much higher than in other individuals.6,8 Endurance exercises such as marathon running or cycling have been noted to elevate CPK for up to 2 hours postexercise.8
Myoglobin becomes detectable in urine when it exceeds 1.5 mg/dL.10 Urine becomes tea-colored or reddish-brown when myoglobin is >100 mg/dL.10
Complications from rhabdomyolysis include compartment syndrome, hyperkalemia, disseminated intravascular coagulation, coagulopathies, and acute renal failure.
Treatment for rhabdomyolysis consists of aggressive IV hydration with normal saline (with variable rate) or crystalloids to maintain a UOP of 200 to 300 mL/h.2,3,11 Avoid fluid overload in the elderly and those with renal or cardiac disease.2 As CPK and myoglobin continue to trend down, it’s important to adjust IV fluids and electrolyte replacement.2,11 Using bicarbonate to alkalinize the urine is controversial, with no studies showing any benefit.3,10 In severe situations, consider a nephrology consult for hemodialysis to bring down CPK, which may be secondary to renal failure and hyperkalemia.2,10 However, renal failure is less likely to occur in physically active, healthy athletes.
Advice after recovery. After an episode of acute rhabdomyolysis, conditioned athletes can return to physical training with resolution of their symptoms or a CPK level from 1000 to 5000 U/L, usually within a week.6 A more judicious approach may be needed for less fit individuals. Regardless of their fitness level, advise patients to avoid diuretics and alcohol before exercise, remain hydrated during and after exercise, and avoid overheating to decrease the likelihood of developing rhabdomyolysis.4 However, in patients with sickle cell trait, exertional sickling can occur with intensity of exercise without overheating.7
In the case of our male patient, poor physical conditioning and intensive, prolonged exercise followed by poor hydration and the diuretic effect of alcohol created the perfect storm for the development of rhabdomyolysis. On the other hand, our female patient routinely exercised, but still pushed herself beyond her limit and went too far too fast. Although BMI may play a role in the development of rhabdomyolysis, it does not appear to be as significant a factor as hydration status and overall physical conditioning.
Our patients’ prompt attention to the need for medical help and the recognition of the problem by their clinicians contributed to good outcomes in both cases.
CORRESPONDENCE Jacqueline DuBose, MD, Department of Family Medicine, Georgia Health Sciences University, 1120 15th Street, Augusta, GA 30912; [email protected]
1. Metzker G. The man who put a new spin on stationary bikes. Los Angeles Times. April 17, 2000. Available at: http://articles.latimes.com/2000/apr/17/health/he-20459. Accessed February 7, 2012.
2. Sauret JM, Marinides G, Wang GK. Rhabdomyolysis. Am Fam Physician. 2002;65:907-912.
3. Cervellin G, Comelli I, Lippi G. Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Clin Chem Lab Med. 2010;48:749-756.
4. Sayers SP, Clarkson PM. Excercise-induced rhabdomyolysis. Curr Sports Med Rep. 2002;1:59-60.
5. Alpers JP, Jones LK. Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010;42:487-491.
6. Eichner ER. Exertional rhabdomyolysis. Curr Sports Med Rep. 2008;7:3-4.
7. Eichner ER. Pearls and pitfalls: exertional sickling. Curr Sports Med Rep. 2010;9:3-4.
8. Clarkson PM, Eichner ER. Exertional rhabdomyolysis: does elevated blood creatine kinase foretell renal failure? Curr Sports Med Rep. 2006;5:57-60.
9. Capaccchione JF, Muldoon SM. The relationship between exertional heat illness, exertional rhabdomyolysis, and malignant hyperthermia. Anesth Analg. 2009;109:1065-1069.
10. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis—an overview for clinicians. Crit Care. 2005;9:158-169.
11. Young IM, Thomson K. Spinning-induced rhabdomyolysis: a case report. Eur J Emerg Med. 2004;11:358-359.
1. Metzker G. The man who put a new spin on stationary bikes. Los Angeles Times. April 17, 2000. Available at: http://articles.latimes.com/2000/apr/17/health/he-20459. Accessed February 7, 2012.
2. Sauret JM, Marinides G, Wang GK. Rhabdomyolysis. Am Fam Physician. 2002;65:907-912.
3. Cervellin G, Comelli I, Lippi G. Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Clin Chem Lab Med. 2010;48:749-756.
4. Sayers SP, Clarkson PM. Excercise-induced rhabdomyolysis. Curr Sports Med Rep. 2002;1:59-60.
5. Alpers JP, Jones LK. Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010;42:487-491.
6. Eichner ER. Exertional rhabdomyolysis. Curr Sports Med Rep. 2008;7:3-4.
7. Eichner ER. Pearls and pitfalls: exertional sickling. Curr Sports Med Rep. 2010;9:3-4.
8. Clarkson PM, Eichner ER. Exertional rhabdomyolysis: does elevated blood creatine kinase foretell renal failure? Curr Sports Med Rep. 2006;5:57-60.
9. Capaccchione JF, Muldoon SM. The relationship between exertional heat illness, exertional rhabdomyolysis, and malignant hyperthermia. Anesth Analg. 2009;109:1065-1069.
10. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis—an overview for clinicians. Crit Care. 2005;9:158-169.
11. Young IM, Thomson K. Spinning-induced rhabdomyolysis: a case report. Eur J Emerg Med. 2004;11:358-359.
Guideline Reflects New Thinking on Renal Scarring
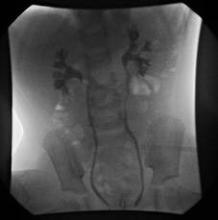
VAIL, COLO. – The most recent American Academy of Pediatrics guidelines on management of urinary tract infections do an abrupt about-face by recommending that a voiding cystourethrogram no longer be routinely performed after a first febrile UTI in children aged 2 months to 2 years.
"This is confusing. On a dime, we have changed our recommendations regarding radiographic imaging," noted Dr. John W. Ogle, vice chair and director of pediatrics at Denver Health.
The previous 1999 AAP guidelines on UTIs stated unequivocally that "infants and children 2 months through 2 years of age who have the expected response to antimicrobials should have a sonogram and either voiding cystourethrogram or radionuclide scan at the earliest convenient time" (Pediatrics 1999;10[4 Pt 1]:843-52).
This sharp shift away from this stance in the current guidelines reflects new thinking regarding the pathogenesis of renal scarring, Dr. Ogle said at a conference on pediatric infectious diseases sponsored by Children’s Hospital Colorado.
"The assumption that has been made in the past is that UTI in the presence of reflux is the primary thing that leads to renal scarring. That’s not so clear anymore. Some of what we call scarring may be congenital cortical defects in the kidney that we discover because we’ve studied the child. There are good studies demonstrating that you can have scarring from pyelonephritis with complete absence of reflux," said Dr. Ogle, who is also a professor of pediatrics at the University of Colorado, Denver.
The operative hypothesis up until the current guidelines were released in 2011 (Pediatrics 2011;128:595-610) was that identifying reflux via a voiding cystourethrogram (VCUG) allowed physicians to intervene surgically or with prophylactic antimicrobials to prevent further reflux nephropathy with further scarring.
"The evidence seems to be quite clear now that the interventions don’t change those important outcomes of renal scarring. So why look for the reflux? Why do the study, with its cost and discomfort, if you don’t have data that an intervention is going to positively affect the child?" Dr. Ogle said.
A key piece of evidence that triggered the change in AAP recommendations was a Cochrane review of 11 studies totaling 1,148 children. The analysis concluded that correction of vesicoureteral reflux by surgery or medical interventions did not reduce the risk of renal scarring (Cochrane Database Syst. Rev. 2007 July 18;(3):CD001532).
The shift in the AAP guidelines has generated controversy among urologists, some of whom are in agreement with the change while others are opposed.
"I think for pediatricians, adopting these guidelines is an easy step," according to Dr. Ogle. "Many pediatricians in office practice had already adopted this years ago. They have not routinely done a VCUG on every child that presented with a febrile UTI. So for them, the impact of the 2011 Academy guidelines has been to say, ‘What you’ve been doing for the last 10 years is probably appropriate.’ "
He predicted that the current guidelines won’t be the final word on the topic of imaging in patients with febrile UTIs.
"What the guidelines don’t tell us is who exactly you should worry about. They don’t tell you which first-time UTIs you should consider VCUG in, and what’s the strategy for second-time UTIs. So stay tuned, there’s going to be further debate with regard to this, and hopefully further evidence," Dr. Ogle said.
"Remember," he continued, "the great history of American medicine is that first we adopt strategies for interventions in medical conditions, then we study them to see if our interventions are right."
Dr. Ogle reported having no relevant financial conflicts.
VAIL, COLO. – The most recent American Academy of Pediatrics guidelines on management of urinary tract infections do an abrupt about-face by recommending that a voiding cystourethrogram no longer be routinely performed after a first febrile UTI in children aged 2 months to 2 years.
"This is confusing. On a dime, we have changed our recommendations regarding radiographic imaging," noted Dr. John W. Ogle, vice chair and director of pediatrics at Denver Health.
The previous 1999 AAP guidelines on UTIs stated unequivocally that "infants and children 2 months through 2 years of age who have the expected response to antimicrobials should have a sonogram and either voiding cystourethrogram or radionuclide scan at the earliest convenient time" (Pediatrics 1999;10[4 Pt 1]:843-52).
This sharp shift away from this stance in the current guidelines reflects new thinking regarding the pathogenesis of renal scarring, Dr. Ogle said at a conference on pediatric infectious diseases sponsored by Children’s Hospital Colorado.
"The assumption that has been made in the past is that UTI in the presence of reflux is the primary thing that leads to renal scarring. That’s not so clear anymore. Some of what we call scarring may be congenital cortical defects in the kidney that we discover because we’ve studied the child. There are good studies demonstrating that you can have scarring from pyelonephritis with complete absence of reflux," said Dr. Ogle, who is also a professor of pediatrics at the University of Colorado, Denver.
The operative hypothesis up until the current guidelines were released in 2011 (Pediatrics 2011;128:595-610) was that identifying reflux via a voiding cystourethrogram (VCUG) allowed physicians to intervene surgically or with prophylactic antimicrobials to prevent further reflux nephropathy with further scarring.
"The evidence seems to be quite clear now that the interventions don’t change those important outcomes of renal scarring. So why look for the reflux? Why do the study, with its cost and discomfort, if you don’t have data that an intervention is going to positively affect the child?" Dr. Ogle said.
A key piece of evidence that triggered the change in AAP recommendations was a Cochrane review of 11 studies totaling 1,148 children. The analysis concluded that correction of vesicoureteral reflux by surgery or medical interventions did not reduce the risk of renal scarring (Cochrane Database Syst. Rev. 2007 July 18;(3):CD001532).
The shift in the AAP guidelines has generated controversy among urologists, some of whom are in agreement with the change while others are opposed.
"I think for pediatricians, adopting these guidelines is an easy step," according to Dr. Ogle. "Many pediatricians in office practice had already adopted this years ago. They have not routinely done a VCUG on every child that presented with a febrile UTI. So for them, the impact of the 2011 Academy guidelines has been to say, ‘What you’ve been doing for the last 10 years is probably appropriate.’ "
He predicted that the current guidelines won’t be the final word on the topic of imaging in patients with febrile UTIs.
"What the guidelines don’t tell us is who exactly you should worry about. They don’t tell you which first-time UTIs you should consider VCUG in, and what’s the strategy for second-time UTIs. So stay tuned, there’s going to be further debate with regard to this, and hopefully further evidence," Dr. Ogle said.
"Remember," he continued, "the great history of American medicine is that first we adopt strategies for interventions in medical conditions, then we study them to see if our interventions are right."
Dr. Ogle reported having no relevant financial conflicts.
VAIL, COLO. – The most recent American Academy of Pediatrics guidelines on management of urinary tract infections do an abrupt about-face by recommending that a voiding cystourethrogram no longer be routinely performed after a first febrile UTI in children aged 2 months to 2 years.
"This is confusing. On a dime, we have changed our recommendations regarding radiographic imaging," noted Dr. John W. Ogle, vice chair and director of pediatrics at Denver Health.
The previous 1999 AAP guidelines on UTIs stated unequivocally that "infants and children 2 months through 2 years of age who have the expected response to antimicrobials should have a sonogram and either voiding cystourethrogram or radionuclide scan at the earliest convenient time" (Pediatrics 1999;10[4 Pt 1]:843-52).
This sharp shift away from this stance in the current guidelines reflects new thinking regarding the pathogenesis of renal scarring, Dr. Ogle said at a conference on pediatric infectious diseases sponsored by Children’s Hospital Colorado.
"The assumption that has been made in the past is that UTI in the presence of reflux is the primary thing that leads to renal scarring. That’s not so clear anymore. Some of what we call scarring may be congenital cortical defects in the kidney that we discover because we’ve studied the child. There are good studies demonstrating that you can have scarring from pyelonephritis with complete absence of reflux," said Dr. Ogle, who is also a professor of pediatrics at the University of Colorado, Denver.
The operative hypothesis up until the current guidelines were released in 2011 (Pediatrics 2011;128:595-610) was that identifying reflux via a voiding cystourethrogram (VCUG) allowed physicians to intervene surgically or with prophylactic antimicrobials to prevent further reflux nephropathy with further scarring.
"The evidence seems to be quite clear now that the interventions don’t change those important outcomes of renal scarring. So why look for the reflux? Why do the study, with its cost and discomfort, if you don’t have data that an intervention is going to positively affect the child?" Dr. Ogle said.
A key piece of evidence that triggered the change in AAP recommendations was a Cochrane review of 11 studies totaling 1,148 children. The analysis concluded that correction of vesicoureteral reflux by surgery or medical interventions did not reduce the risk of renal scarring (Cochrane Database Syst. Rev. 2007 July 18;(3):CD001532).
The shift in the AAP guidelines has generated controversy among urologists, some of whom are in agreement with the change while others are opposed.
"I think for pediatricians, adopting these guidelines is an easy step," according to Dr. Ogle. "Many pediatricians in office practice had already adopted this years ago. They have not routinely done a VCUG on every child that presented with a febrile UTI. So for them, the impact of the 2011 Academy guidelines has been to say, ‘What you’ve been doing for the last 10 years is probably appropriate.’ "
He predicted that the current guidelines won’t be the final word on the topic of imaging in patients with febrile UTIs.
"What the guidelines don’t tell us is who exactly you should worry about. They don’t tell you which first-time UTIs you should consider VCUG in, and what’s the strategy for second-time UTIs. So stay tuned, there’s going to be further debate with regard to this, and hopefully further evidence," Dr. Ogle said.
"Remember," he continued, "the great history of American medicine is that first we adopt strategies for interventions in medical conditions, then we study them to see if our interventions are right."
Dr. Ogle reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM A CONFERENCE ON PEDIATRIC INFECTIOUS DISEASES SPONSORED BY CHILDREN'S HOSPITAL COLORADO
Apixaban Cuts Bleeding Risk in Renal Dysfunction Patients
MUNICH - Patients with renal dysfunction as well as atrial fibrillation who received apixaban to prevent strokes and systemic embolism had the biggest drop in major bleeding events compared with control patients on warfarin in a prespecified substudy of the ARISTOTLE trial.
"Our findings suggest that apixaban may be particularly suited to address the unmet need for more effective and safe stroke prevention in patients with atrial fibrillation and renal dysfunction," Dr. Stefan H. Hohnloser said at the annual congress of the European Society of Cardiology.
The finding is especially relevant to practice because of the high coprevalence of atrial fibrillation and chronic kidney disease. A recent U.S. study of patients with chronic kidney disease found an 18% prevalence of atrial fibrillation – two- to threefold higher than in the general population – and a greater than 25% prevalence of atrial fibrillation among patients with renal dysfunction who were at least 70 year old (Am. Heart J. 2010;159:1102-7).
But while apixiban triggered significantly fewer major bleeds compared with warfarin among patients with renal dysfunction enrolled in the pivotal Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial, apixaban’s efficacy for stroke and embolism protection in atrial fibrillation patients with renal dysfunction was just as good as it was in patients with normal renal activity.
"When compared with warfarin, apixaban treatment reduced the rate of stroke, death, and major bleeding, regardless of renal function," Dr. Hohnloser and his associates wrote in a published report on their findings that appeared online concurrent with his report at the meeting (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs274]).
"We know that patients with atrial fibrillation and impaired renal function not only have a high stroke rate, but also have a significantly higher bleeding rate with respect to patients with normal renal function. The message from the new analysis is that, in patients with impaired renal function, apixaban is superior to warfarin with respect to the risk of major bleeding," said Dr. Gerhard Hindricks, professor and director of the department of electrophysiology at the Leipzig (Germany) University Heart Center.
The new findings also drew a sharp contrast between apixaban and another new oral anticoagulant, dabigatran, noted Dr. Hindricks and Dr. Jan Steffel of University Hospital Zurich in an editorial they wrote that appeared online concurrent with the main report (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs267]).
"Dabigatran, which is 80% renally cleared, has a significant potential for severe bleeding in patients with reduced renal function," they wrote.
In addition, they added, "major bleeding events are the single most prevalent reason why proper anticoagulation is withheld in patients with atrial fibrillation, especially those with impaired renal function. ... Chronic kidney disease certainly appears to be the ‘Achilles heel’ of dabigatran, as accumulation is likely to occur due to mainly renal elimination. Hence, in our view of the available data, apixaban would probably be the preferred agent over dabigatran in these patients."
Dr. Hindricks and Dr. Steffel concluded that the new findings from ARISTOTLE provide "solid evidence for the superiority of apixaban in patients with atrial fibrillation and chronic kidney disease. In the light of these data, apixaban appears to be a very appealing option for these individuals, potentially leading to a substantial increase in the numbers of appropriately anticoagulated patients."
The substudy analysis calculated estimated glomerular filtration rates (eGFR) for patients enrolled in ARISTOTLE by three difference methods: the Cockcroft-Gault formula, the Chronic Kidney Disease-Epidemiology Collaboration formula, and based on cystatin C measurement. It focused on 18,122 of the patients enrolled in ARISTOTLE who had data available that allowed calculation of their eGFR. All three methods found that about 15% of the enrolled patients had an eGFR of 50 mL/min per 1.73 m2 or less.
The new analysis showed that patients with an eGFR of 50 mL/min or less had the greatest reduction in major bleeding episodes during apixaban treatment, compared with warfarin treatment. Among patients with impaired renal function, the bleeding risk on apixaban dropped by 35%-52%, depending on which formula the researchers used to identify patients with an eGFR that low, reported Dr. Hohnloser, professor and director of the department of clinical electrophysiology at J.W. Goethe University in Frankfurt, Germany.
In contrast, the primary efficacy end point of stroke or systemic embolism occurred consistently less often among patients treated with apixaban than in those on warfarin regardless of their eGFR.
The ARISTOTLE trial was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Hohnloser said that he has received consulting and lecture fees from Bristol-Myers Squibb, Pfizer, and other drug companies and research grants from Sanofi-Aventis and St. Jude. Dr. Hindricks said that he has received honoraria from and has been a consultant to Biosense, Stereotaxis, St. Jude, and Biotronik.
Renal dysfunction is highly prevalent in patients with atrial fibrillation and is associated with both stroke and bleeding risk. In ARISTOTLE, the overall findings of the trial are consistent with the outcomes seen in patients with moderate renal dysfunction, with an estimated glomerular filtration rate (eGFR) of less than 50 mL/min per 1.73 m2.
The ARISTOTLE results showed that the rate of ischemic stroke was twofold higher, the rate of major bleeds was threefold higher, and the mortality rate was threefold higher among patients with an eGFR of 50 mL/min per 1.73 m2 or less compared with patients with an eGFR of greater than 80 mL/min per 1.73 m2.
The benefit over warfarin of reduced bleeding appears to be more marked in patients with moderate renal dysfunction. These patients received a reduced apixaban dosage, 2.5 mg b.i.d. instead of the full dosage of 5 mg b.i.d., but results of a sensitivity analysis by the researchers suggested that this reduced dosage was not the key factor producing the reduced rate of major bleeds.
In my view, apixaban provides a treatment option and advantages over warfarin in atrial fibrillation patients with moderate renal dysfunction, a group of patients who currently receive suboptimal management.
Keith A.A. Fox, M.D., is professor of cardiology at the University of Edinburgh. He said that he has received grant funding and honoraria from Sanofi, Lilly, Bayer/Johnson & Johnson, Astra Zeneca, and Boehringer Ingelheim. He made these comments as designated discussant for the report by Dr. Hohnloser.
Renal dysfunction is highly prevalent in patients with atrial fibrillation and is associated with both stroke and bleeding risk. In ARISTOTLE, the overall findings of the trial are consistent with the outcomes seen in patients with moderate renal dysfunction, with an estimated glomerular filtration rate (eGFR) of less than 50 mL/min per 1.73 m2.
The ARISTOTLE results showed that the rate of ischemic stroke was twofold higher, the rate of major bleeds was threefold higher, and the mortality rate was threefold higher among patients with an eGFR of 50 mL/min per 1.73 m2 or less compared with patients with an eGFR of greater than 80 mL/min per 1.73 m2.
The benefit over warfarin of reduced bleeding appears to be more marked in patients with moderate renal dysfunction. These patients received a reduced apixaban dosage, 2.5 mg b.i.d. instead of the full dosage of 5 mg b.i.d., but results of a sensitivity analysis by the researchers suggested that this reduced dosage was not the key factor producing the reduced rate of major bleeds.
In my view, apixaban provides a treatment option and advantages over warfarin in atrial fibrillation patients with moderate renal dysfunction, a group of patients who currently receive suboptimal management.
Keith A.A. Fox, M.D., is professor of cardiology at the University of Edinburgh. He said that he has received grant funding and honoraria from Sanofi, Lilly, Bayer/Johnson & Johnson, Astra Zeneca, and Boehringer Ingelheim. He made these comments as designated discussant for the report by Dr. Hohnloser.
Renal dysfunction is highly prevalent in patients with atrial fibrillation and is associated with both stroke and bleeding risk. In ARISTOTLE, the overall findings of the trial are consistent with the outcomes seen in patients with moderate renal dysfunction, with an estimated glomerular filtration rate (eGFR) of less than 50 mL/min per 1.73 m2.
The ARISTOTLE results showed that the rate of ischemic stroke was twofold higher, the rate of major bleeds was threefold higher, and the mortality rate was threefold higher among patients with an eGFR of 50 mL/min per 1.73 m2 or less compared with patients with an eGFR of greater than 80 mL/min per 1.73 m2.
The benefit over warfarin of reduced bleeding appears to be more marked in patients with moderate renal dysfunction. These patients received a reduced apixaban dosage, 2.5 mg b.i.d. instead of the full dosage of 5 mg b.i.d., but results of a sensitivity analysis by the researchers suggested that this reduced dosage was not the key factor producing the reduced rate of major bleeds.
In my view, apixaban provides a treatment option and advantages over warfarin in atrial fibrillation patients with moderate renal dysfunction, a group of patients who currently receive suboptimal management.
Keith A.A. Fox, M.D., is professor of cardiology at the University of Edinburgh. He said that he has received grant funding and honoraria from Sanofi, Lilly, Bayer/Johnson & Johnson, Astra Zeneca, and Boehringer Ingelheim. He made these comments as designated discussant for the report by Dr. Hohnloser.
MUNICH - Patients with renal dysfunction as well as atrial fibrillation who received apixaban to prevent strokes and systemic embolism had the biggest drop in major bleeding events compared with control patients on warfarin in a prespecified substudy of the ARISTOTLE trial.
"Our findings suggest that apixaban may be particularly suited to address the unmet need for more effective and safe stroke prevention in patients with atrial fibrillation and renal dysfunction," Dr. Stefan H. Hohnloser said at the annual congress of the European Society of Cardiology.
The finding is especially relevant to practice because of the high coprevalence of atrial fibrillation and chronic kidney disease. A recent U.S. study of patients with chronic kidney disease found an 18% prevalence of atrial fibrillation – two- to threefold higher than in the general population – and a greater than 25% prevalence of atrial fibrillation among patients with renal dysfunction who were at least 70 year old (Am. Heart J. 2010;159:1102-7).
But while apixiban triggered significantly fewer major bleeds compared with warfarin among patients with renal dysfunction enrolled in the pivotal Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial, apixaban’s efficacy for stroke and embolism protection in atrial fibrillation patients with renal dysfunction was just as good as it was in patients with normal renal activity.
"When compared with warfarin, apixaban treatment reduced the rate of stroke, death, and major bleeding, regardless of renal function," Dr. Hohnloser and his associates wrote in a published report on their findings that appeared online concurrent with his report at the meeting (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs274]).
"We know that patients with atrial fibrillation and impaired renal function not only have a high stroke rate, but also have a significantly higher bleeding rate with respect to patients with normal renal function. The message from the new analysis is that, in patients with impaired renal function, apixaban is superior to warfarin with respect to the risk of major bleeding," said Dr. Gerhard Hindricks, professor and director of the department of electrophysiology at the Leipzig (Germany) University Heart Center.
The new findings also drew a sharp contrast between apixaban and another new oral anticoagulant, dabigatran, noted Dr. Hindricks and Dr. Jan Steffel of University Hospital Zurich in an editorial they wrote that appeared online concurrent with the main report (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs267]).
"Dabigatran, which is 80% renally cleared, has a significant potential for severe bleeding in patients with reduced renal function," they wrote.
In addition, they added, "major bleeding events are the single most prevalent reason why proper anticoagulation is withheld in patients with atrial fibrillation, especially those with impaired renal function. ... Chronic kidney disease certainly appears to be the ‘Achilles heel’ of dabigatran, as accumulation is likely to occur due to mainly renal elimination. Hence, in our view of the available data, apixaban would probably be the preferred agent over dabigatran in these patients."
Dr. Hindricks and Dr. Steffel concluded that the new findings from ARISTOTLE provide "solid evidence for the superiority of apixaban in patients with atrial fibrillation and chronic kidney disease. In the light of these data, apixaban appears to be a very appealing option for these individuals, potentially leading to a substantial increase in the numbers of appropriately anticoagulated patients."
The substudy analysis calculated estimated glomerular filtration rates (eGFR) for patients enrolled in ARISTOTLE by three difference methods: the Cockcroft-Gault formula, the Chronic Kidney Disease-Epidemiology Collaboration formula, and based on cystatin C measurement. It focused on 18,122 of the patients enrolled in ARISTOTLE who had data available that allowed calculation of their eGFR. All three methods found that about 15% of the enrolled patients had an eGFR of 50 mL/min per 1.73 m2 or less.
The new analysis showed that patients with an eGFR of 50 mL/min or less had the greatest reduction in major bleeding episodes during apixaban treatment, compared with warfarin treatment. Among patients with impaired renal function, the bleeding risk on apixaban dropped by 35%-52%, depending on which formula the researchers used to identify patients with an eGFR that low, reported Dr. Hohnloser, professor and director of the department of clinical electrophysiology at J.W. Goethe University in Frankfurt, Germany.
In contrast, the primary efficacy end point of stroke or systemic embolism occurred consistently less often among patients treated with apixaban than in those on warfarin regardless of their eGFR.
The ARISTOTLE trial was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Hohnloser said that he has received consulting and lecture fees from Bristol-Myers Squibb, Pfizer, and other drug companies and research grants from Sanofi-Aventis and St. Jude. Dr. Hindricks said that he has received honoraria from and has been a consultant to Biosense, Stereotaxis, St. Jude, and Biotronik.
MUNICH - Patients with renal dysfunction as well as atrial fibrillation who received apixaban to prevent strokes and systemic embolism had the biggest drop in major bleeding events compared with control patients on warfarin in a prespecified substudy of the ARISTOTLE trial.
"Our findings suggest that apixaban may be particularly suited to address the unmet need for more effective and safe stroke prevention in patients with atrial fibrillation and renal dysfunction," Dr. Stefan H. Hohnloser said at the annual congress of the European Society of Cardiology.
The finding is especially relevant to practice because of the high coprevalence of atrial fibrillation and chronic kidney disease. A recent U.S. study of patients with chronic kidney disease found an 18% prevalence of atrial fibrillation – two- to threefold higher than in the general population – and a greater than 25% prevalence of atrial fibrillation among patients with renal dysfunction who were at least 70 year old (Am. Heart J. 2010;159:1102-7).
But while apixiban triggered significantly fewer major bleeds compared with warfarin among patients with renal dysfunction enrolled in the pivotal Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial, apixaban’s efficacy for stroke and embolism protection in atrial fibrillation patients with renal dysfunction was just as good as it was in patients with normal renal activity.
"When compared with warfarin, apixaban treatment reduced the rate of stroke, death, and major bleeding, regardless of renal function," Dr. Hohnloser and his associates wrote in a published report on their findings that appeared online concurrent with his report at the meeting (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs274]).
"We know that patients with atrial fibrillation and impaired renal function not only have a high stroke rate, but also have a significantly higher bleeding rate with respect to patients with normal renal function. The message from the new analysis is that, in patients with impaired renal function, apixaban is superior to warfarin with respect to the risk of major bleeding," said Dr. Gerhard Hindricks, professor and director of the department of electrophysiology at the Leipzig (Germany) University Heart Center.
The new findings also drew a sharp contrast between apixaban and another new oral anticoagulant, dabigatran, noted Dr. Hindricks and Dr. Jan Steffel of University Hospital Zurich in an editorial they wrote that appeared online concurrent with the main report (Eur. Heart J. 2012 [doi:10.1093/eurheartj/ehs267]).
"Dabigatran, which is 80% renally cleared, has a significant potential for severe bleeding in patients with reduced renal function," they wrote.
In addition, they added, "major bleeding events are the single most prevalent reason why proper anticoagulation is withheld in patients with atrial fibrillation, especially those with impaired renal function. ... Chronic kidney disease certainly appears to be the ‘Achilles heel’ of dabigatran, as accumulation is likely to occur due to mainly renal elimination. Hence, in our view of the available data, apixaban would probably be the preferred agent over dabigatran in these patients."
Dr. Hindricks and Dr. Steffel concluded that the new findings from ARISTOTLE provide "solid evidence for the superiority of apixaban in patients with atrial fibrillation and chronic kidney disease. In the light of these data, apixaban appears to be a very appealing option for these individuals, potentially leading to a substantial increase in the numbers of appropriately anticoagulated patients."
The substudy analysis calculated estimated glomerular filtration rates (eGFR) for patients enrolled in ARISTOTLE by three difference methods: the Cockcroft-Gault formula, the Chronic Kidney Disease-Epidemiology Collaboration formula, and based on cystatin C measurement. It focused on 18,122 of the patients enrolled in ARISTOTLE who had data available that allowed calculation of their eGFR. All three methods found that about 15% of the enrolled patients had an eGFR of 50 mL/min per 1.73 m2 or less.
The new analysis showed that patients with an eGFR of 50 mL/min or less had the greatest reduction in major bleeding episodes during apixaban treatment, compared with warfarin treatment. Among patients with impaired renal function, the bleeding risk on apixaban dropped by 35%-52%, depending on which formula the researchers used to identify patients with an eGFR that low, reported Dr. Hohnloser, professor and director of the department of clinical electrophysiology at J.W. Goethe University in Frankfurt, Germany.
In contrast, the primary efficacy end point of stroke or systemic embolism occurred consistently less often among patients treated with apixaban than in those on warfarin regardless of their eGFR.
The ARISTOTLE trial was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Hohnloser said that he has received consulting and lecture fees from Bristol-Myers Squibb, Pfizer, and other drug companies and research grants from Sanofi-Aventis and St. Jude. Dr. Hindricks said that he has received honoraria from and has been a consultant to Biosense, Stereotaxis, St. Jude, and Biotronik.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: Among atrial fibrillation patients with renal dysfunction, apixiban produced 35%-52% fewer major bleeding episodes compared with warfarin.
Data Source: A prespecified substudy of ARISTOTLE, a multicenter, randomized trial of 18,201 patients with atrial fibrillation.
Disclosures: The ARISTOTLE trial was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Hohnloser said that he has received consulting and lecture fees from Bristol-Myers Squibb, Pfizer, and other drug companies and research grants from sanofi-aventis and St. Jude. Dr. Hindricks said that he has received honoraria from and has been a consultant to Biosense, Stereotaxis, St. Jude, and Biotronik.
Agent Shunts Fluid Overload Via GI Tract
SEATTLE – An investigational agent that eliminates excess fluid through the gastrointestinal tract appears promising for treatment in patients with heart failure–related fluid overload who also have chronic kidney disease, new data suggest.
In a phase II trial among 111 such patients who were starting spironolactone, the new agent – known as cross-linked polyelectrolyte (CLP) – did not improve serum potassium levels when compared with placebo, the trial’s primary end point, investigators reported at the annual meeting of the Heart Failure Society of America. However, it did improve body weight and New York Heart Association (NYHA) functional class.
The CLP group had a higher rate of gastrointestinal adverse effects. Additionally, the mortality rate was about 7% with the medication, compared with 0% with placebo. None of the deaths appeared to be related to treatment, according to the study’s lead investigator, Dr. Barry M. Massie, chief of the cardiology division at the San Francisco Veterans Affairs Medical Center.
"Use of CLP in the gastrointestinal tract may be an effective means for removal of sodium and water in heart failure patients already treated with guideline therapy including diuretics," said Dr. Massie. "Such extrarenal removal of fluid appears to result in meaningful improvements in function and symptoms in these patients, and warrants further investigation."
"An adequately powered trial is needed both to confirm the efficacy and further evaluate safety of the compound," he added.
Dr. Stephen S. Gottlieb of the University of Maryland, Baltimore, who was invited to discuss the trial, said that it addressed two critical issues in this population: hyperkalemia (a major barrier to using and adequately titrating cardiovascular medications) and fluid status (an ongoing problem as existing diuretics have known limitations).
"Unfortunately, CLP did not prevent hyperkalemia, and we clearly need ways to safely control potassium," he said. "We know that CLP caused sustained fluid loss. What we don’t know is how that compares with other ways of removing fluid: Would patients have done as well if they were given loop diuretics? Clearly, if we are going to address this issue, we have to decide whether, as compared to loop diuretics, is it really more efficacious, is it really safer, and does it lead to better outcomes."
The trial was conducted at 24 sites in Armenia, Georgia, and Moldova. Patients were eligible if they had heart failure with New York Heart Association class III or IV plus chronic kidney disease, and had recently been hospitalized for decompensation associated with fluid overload.
They were randomized to double-blind treatment with CLP (manufactured by Sorbent Therapeutics) or placebo for 8 weeks. Patients in both groups were also started on spironolactone.
CLP is an orally administered superabsorbent polymer that is neither metabolized nor absorbed, explained Dr. Massie, who also is professor of medicine at the University of California, San Francisco. It binds cations and water, and is excreted in stool.
Trial results showed that changes in serum potassium levels from baseline did not differ significantly between treatment groups. Also, the rate of trial discontinuation due to hyperkalemia was about 10% in each group.
However, patients in the CLP group had a significant reduction in body weight relative to their counterparts in the placebo group at weeks 1 and 2, and there was a trend toward a greater reduction over the entire 8 weeks (P = .065).
The CLP group was more likely to rate their dyspnea as moderately or markedly better (37% vs. 22%). According to physician ratings, the proportion having marked or disabling dyspnea on exertion fell in both groups over time, but to a greater extent among those in the CLP group.
Patients in the CLP group were also more likely to have an improvement of at least one NYHA class from baseline (49% vs. 17%, P = .0018).
Both groups had better 6-minute walk test results at 8 weeks, but the magnitude of improvement was 24% with CLP vs. 14% with placebo, corresponding to an absolute difference of 20 meters (P = .07). CLP also was associated with better scores on the Kansas City Cardiomyopathy Questionnaire.
In terms of safety, there were no clinically important changes in various ions or in serum aldosterone levels, according to Dr. Massie.
The overall rate of adverse events was 36% in the CLP group and 31% in the placebo group, a difference largely caused by a higher rate of gastrointestinal events (mainly abdominal discomfort) in the former (24% vs. 14%).
There were four deaths, all in the CLP group. However, there did not appear to be any common pattern, and investigators did not judge any deaths to be related to the study medication, according to Dr. Massie.
Yet, the higher death rate with CLP "is certainly something to think about down the road," he acknowledged. "Obviously, as we proceed with clinical trials, we will try to decipher that and hope that it is a fluke and not an effect of the drug," he said.
Dr. Massie disclosed that he is a consultant to Sorbent Therapeutics, which sponsored the trial. Dr. Gottlieb disclosed no relevant conflicts of interest.
SEATTLE – An investigational agent that eliminates excess fluid through the gastrointestinal tract appears promising for treatment in patients with heart failure–related fluid overload who also have chronic kidney disease, new data suggest.
In a phase II trial among 111 such patients who were starting spironolactone, the new agent – known as cross-linked polyelectrolyte (CLP) – did not improve serum potassium levels when compared with placebo, the trial’s primary end point, investigators reported at the annual meeting of the Heart Failure Society of America. However, it did improve body weight and New York Heart Association (NYHA) functional class.
The CLP group had a higher rate of gastrointestinal adverse effects. Additionally, the mortality rate was about 7% with the medication, compared with 0% with placebo. None of the deaths appeared to be related to treatment, according to the study’s lead investigator, Dr. Barry M. Massie, chief of the cardiology division at the San Francisco Veterans Affairs Medical Center.
"Use of CLP in the gastrointestinal tract may be an effective means for removal of sodium and water in heart failure patients already treated with guideline therapy including diuretics," said Dr. Massie. "Such extrarenal removal of fluid appears to result in meaningful improvements in function and symptoms in these patients, and warrants further investigation."
"An adequately powered trial is needed both to confirm the efficacy and further evaluate safety of the compound," he added.
Dr. Stephen S. Gottlieb of the University of Maryland, Baltimore, who was invited to discuss the trial, said that it addressed two critical issues in this population: hyperkalemia (a major barrier to using and adequately titrating cardiovascular medications) and fluid status (an ongoing problem as existing diuretics have known limitations).
"Unfortunately, CLP did not prevent hyperkalemia, and we clearly need ways to safely control potassium," he said. "We know that CLP caused sustained fluid loss. What we don’t know is how that compares with other ways of removing fluid: Would patients have done as well if they were given loop diuretics? Clearly, if we are going to address this issue, we have to decide whether, as compared to loop diuretics, is it really more efficacious, is it really safer, and does it lead to better outcomes."
The trial was conducted at 24 sites in Armenia, Georgia, and Moldova. Patients were eligible if they had heart failure with New York Heart Association class III or IV plus chronic kidney disease, and had recently been hospitalized for decompensation associated with fluid overload.
They were randomized to double-blind treatment with CLP (manufactured by Sorbent Therapeutics) or placebo for 8 weeks. Patients in both groups were also started on spironolactone.
CLP is an orally administered superabsorbent polymer that is neither metabolized nor absorbed, explained Dr. Massie, who also is professor of medicine at the University of California, San Francisco. It binds cations and water, and is excreted in stool.
Trial results showed that changes in serum potassium levels from baseline did not differ significantly between treatment groups. Also, the rate of trial discontinuation due to hyperkalemia was about 10% in each group.
However, patients in the CLP group had a significant reduction in body weight relative to their counterparts in the placebo group at weeks 1 and 2, and there was a trend toward a greater reduction over the entire 8 weeks (P = .065).
The CLP group was more likely to rate their dyspnea as moderately or markedly better (37% vs. 22%). According to physician ratings, the proportion having marked or disabling dyspnea on exertion fell in both groups over time, but to a greater extent among those in the CLP group.
Patients in the CLP group were also more likely to have an improvement of at least one NYHA class from baseline (49% vs. 17%, P = .0018).
Both groups had better 6-minute walk test results at 8 weeks, but the magnitude of improvement was 24% with CLP vs. 14% with placebo, corresponding to an absolute difference of 20 meters (P = .07). CLP also was associated with better scores on the Kansas City Cardiomyopathy Questionnaire.
In terms of safety, there were no clinically important changes in various ions or in serum aldosterone levels, according to Dr. Massie.
The overall rate of adverse events was 36% in the CLP group and 31% in the placebo group, a difference largely caused by a higher rate of gastrointestinal events (mainly abdominal discomfort) in the former (24% vs. 14%).
There were four deaths, all in the CLP group. However, there did not appear to be any common pattern, and investigators did not judge any deaths to be related to the study medication, according to Dr. Massie.
Yet, the higher death rate with CLP "is certainly something to think about down the road," he acknowledged. "Obviously, as we proceed with clinical trials, we will try to decipher that and hope that it is a fluke and not an effect of the drug," he said.
Dr. Massie disclosed that he is a consultant to Sorbent Therapeutics, which sponsored the trial. Dr. Gottlieb disclosed no relevant conflicts of interest.
SEATTLE – An investigational agent that eliminates excess fluid through the gastrointestinal tract appears promising for treatment in patients with heart failure–related fluid overload who also have chronic kidney disease, new data suggest.
In a phase II trial among 111 such patients who were starting spironolactone, the new agent – known as cross-linked polyelectrolyte (CLP) – did not improve serum potassium levels when compared with placebo, the trial’s primary end point, investigators reported at the annual meeting of the Heart Failure Society of America. However, it did improve body weight and New York Heart Association (NYHA) functional class.
The CLP group had a higher rate of gastrointestinal adverse effects. Additionally, the mortality rate was about 7% with the medication, compared with 0% with placebo. None of the deaths appeared to be related to treatment, according to the study’s lead investigator, Dr. Barry M. Massie, chief of the cardiology division at the San Francisco Veterans Affairs Medical Center.
"Use of CLP in the gastrointestinal tract may be an effective means for removal of sodium and water in heart failure patients already treated with guideline therapy including diuretics," said Dr. Massie. "Such extrarenal removal of fluid appears to result in meaningful improvements in function and symptoms in these patients, and warrants further investigation."
"An adequately powered trial is needed both to confirm the efficacy and further evaluate safety of the compound," he added.
Dr. Stephen S. Gottlieb of the University of Maryland, Baltimore, who was invited to discuss the trial, said that it addressed two critical issues in this population: hyperkalemia (a major barrier to using and adequately titrating cardiovascular medications) and fluid status (an ongoing problem as existing diuretics have known limitations).
"Unfortunately, CLP did not prevent hyperkalemia, and we clearly need ways to safely control potassium," he said. "We know that CLP caused sustained fluid loss. What we don’t know is how that compares with other ways of removing fluid: Would patients have done as well if they were given loop diuretics? Clearly, if we are going to address this issue, we have to decide whether, as compared to loop diuretics, is it really more efficacious, is it really safer, and does it lead to better outcomes."
The trial was conducted at 24 sites in Armenia, Georgia, and Moldova. Patients were eligible if they had heart failure with New York Heart Association class III or IV plus chronic kidney disease, and had recently been hospitalized for decompensation associated with fluid overload.
They were randomized to double-blind treatment with CLP (manufactured by Sorbent Therapeutics) or placebo for 8 weeks. Patients in both groups were also started on spironolactone.
CLP is an orally administered superabsorbent polymer that is neither metabolized nor absorbed, explained Dr. Massie, who also is professor of medicine at the University of California, San Francisco. It binds cations and water, and is excreted in stool.
Trial results showed that changes in serum potassium levels from baseline did not differ significantly between treatment groups. Also, the rate of trial discontinuation due to hyperkalemia was about 10% in each group.
However, patients in the CLP group had a significant reduction in body weight relative to their counterparts in the placebo group at weeks 1 and 2, and there was a trend toward a greater reduction over the entire 8 weeks (P = .065).
The CLP group was more likely to rate their dyspnea as moderately or markedly better (37% vs. 22%). According to physician ratings, the proportion having marked or disabling dyspnea on exertion fell in both groups over time, but to a greater extent among those in the CLP group.
Patients in the CLP group were also more likely to have an improvement of at least one NYHA class from baseline (49% vs. 17%, P = .0018).
Both groups had better 6-minute walk test results at 8 weeks, but the magnitude of improvement was 24% with CLP vs. 14% with placebo, corresponding to an absolute difference of 20 meters (P = .07). CLP also was associated with better scores on the Kansas City Cardiomyopathy Questionnaire.
In terms of safety, there were no clinically important changes in various ions or in serum aldosterone levels, according to Dr. Massie.
The overall rate of adverse events was 36% in the CLP group and 31% in the placebo group, a difference largely caused by a higher rate of gastrointestinal events (mainly abdominal discomfort) in the former (24% vs. 14%).
There were four deaths, all in the CLP group. However, there did not appear to be any common pattern, and investigators did not judge any deaths to be related to the study medication, according to Dr. Massie.
Yet, the higher death rate with CLP "is certainly something to think about down the road," he acknowledged. "Obviously, as we proceed with clinical trials, we will try to decipher that and hope that it is a fluke and not an effect of the drug," he said.
Dr. Massie disclosed that he is a consultant to Sorbent Therapeutics, which sponsored the trial. Dr. Gottlieb disclosed no relevant conflicts of interest.
AT THE ANNUAL MEETING OF THE HEART FAILURE SOCIETY OF AMERICA
Major Finding: Compared with placebo, CLP was associated with improvements in body weight and New York Heart Association functional class, but not serum potassium levels.
Data Source: A randomized phase II trial among 111 patients experiencing heart failure with fluid overload and chronic kidney disease.
Disclosures: Dr. Massie disclosed that he is a consultant to Sorbent Therapeutics. Dr. Gottlieb disclosed no relevant conflicts of interest. The trial was sponsored by Sorbent Therapeutics.
Analysis Supports First-Line Daptomycin Against Catheter-Related Bacteremia
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Daptomycin was successful in 83% of patients who received it as a first-line treatment for catheter-related bacteremia (57% cured, 26% improved).
Data Source: Results were taken from a multicenter analysis of 148 patients enrolled in the ongoing EUCORE (European Cubicin Outcomes Registry and Experience) study.
Disclosures: The investigator is employed by Novartis Pharmaceuticals UK, which markets daptomycin and funded the study.
Active Surveillance Favored for Low-Risk Prostate Cancer
Compared with immediate radical prostatectomy, active surveillance for men with low-risk prostate cancer produces only a "very modest" 1.8-month decrease in cancer-specific survival, according to a report published online Sept. 24 in Clinical Cancer Research.
However, men on active surveillance enjoyed 6 more years of life free from treatment and its adverse effects than men who had immediate surgery, said Dr. Ruth Etzioni of the division of public health services, Fred Hutchinson Cancer Research Center, Seattle, and her associates.
These are the findings of a new simulation model they developed to predict prostate cancer mortality in a virtual population of 1 million contemporary U.S. cases, using the best available data from contemporary studies of the issue.
The investigators first incorporated into their simulation model the findings from an active surveillance program in which men with low-risk prostate cancer are biopsied every year and referred for further treatment if any adverse changes are found. This program also allows patients to self-refer for further treatment for several other reasons, including if their prostate-specific antigen level rises or if they become too anxious over "watchful waiting."
The researchers then incorporated into the model information from a large longitudinal database on the interval between radical prostatectomy and recurrence. The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) database enrolled nearly 14,000 men treated at 40 urology practices, and included 1,000 clinical and patient variables.
Lastly, Dr. Etzioni and her colleagues used data from another cohort study of 3,470 men to model the time from prostate cancer recurrence until death. They then computed the cumulative cancer-specific mortality in their virtual cohort for men under active surveillance compared with men who underwent immediate radical prostatectomy.
The model projected that the 20-year cumulative rate of prostate cancer–specific mortality would be 2.78% with active surveillance and 1.64% with immediate radical prostatectomy. This corresponded with an average of 1.8 months of life saved per case, which was considered a "very modest" advantage, the investigators said (Clin. Cancer Res. 2012 Sept. 24 [doi:10.1158/1078-0432.CCR-12-1502]).
However, the model also showed that men on active surveillance "had on average 6.4 more years of life free from treatment and its side effects," which could be a substantial advantage.
Three separate sensitivity analyses demonstrated that the model’s projections were robust even when multiple variables were altered. "All sensitivity analyses produced only modest differences in cumulative prostate cancer mortality under active surveillance, and supported our projection that active surveillance would have a minimal impact on life expectancy for low-risk cancer cases," Dr. Etzioni and her associates said.
"Ultimately, the model predicts that approximately 64% of men on active surveillance would be treated [for prostate cancer] within their lifetimes. ... Thus, under active surveillance, 36% of men could avoid being treated," they said.
These findings are consistent with those of at least one other modeling study and with those of the longitudinal PIVOT (Prostate Cancer Intervention versus Observation Trial) study that tracked disease-free survival for 12 years.
"Although this is not a new result, it is confirmation of what we expected, and it substantiates data from previous studies looking at watchful waiting. Very few men with low-risk disease die from prostate cancer regardless, and the difference between treatments appears to be very modest," Dr. Etzioni said in a press statement accompanying this report.
This study was supported by the National Cancer Institute and the Centers for Disease Control and Prevention. No financial conflicts of interest were reported.
Compared with immediate radical prostatectomy, active surveillance for men with low-risk prostate cancer produces only a "very modest" 1.8-month decrease in cancer-specific survival, according to a report published online Sept. 24 in Clinical Cancer Research.
However, men on active surveillance enjoyed 6 more years of life free from treatment and its adverse effects than men who had immediate surgery, said Dr. Ruth Etzioni of the division of public health services, Fred Hutchinson Cancer Research Center, Seattle, and her associates.
These are the findings of a new simulation model they developed to predict prostate cancer mortality in a virtual population of 1 million contemporary U.S. cases, using the best available data from contemporary studies of the issue.
The investigators first incorporated into their simulation model the findings from an active surveillance program in which men with low-risk prostate cancer are biopsied every year and referred for further treatment if any adverse changes are found. This program also allows patients to self-refer for further treatment for several other reasons, including if their prostate-specific antigen level rises or if they become too anxious over "watchful waiting."
The researchers then incorporated into the model information from a large longitudinal database on the interval between radical prostatectomy and recurrence. The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) database enrolled nearly 14,000 men treated at 40 urology practices, and included 1,000 clinical and patient variables.
Lastly, Dr. Etzioni and her colleagues used data from another cohort study of 3,470 men to model the time from prostate cancer recurrence until death. They then computed the cumulative cancer-specific mortality in their virtual cohort for men under active surveillance compared with men who underwent immediate radical prostatectomy.
The model projected that the 20-year cumulative rate of prostate cancer–specific mortality would be 2.78% with active surveillance and 1.64% with immediate radical prostatectomy. This corresponded with an average of 1.8 months of life saved per case, which was considered a "very modest" advantage, the investigators said (Clin. Cancer Res. 2012 Sept. 24 [doi:10.1158/1078-0432.CCR-12-1502]).
However, the model also showed that men on active surveillance "had on average 6.4 more years of life free from treatment and its side effects," which could be a substantial advantage.
Three separate sensitivity analyses demonstrated that the model’s projections were robust even when multiple variables were altered. "All sensitivity analyses produced only modest differences in cumulative prostate cancer mortality under active surveillance, and supported our projection that active surveillance would have a minimal impact on life expectancy for low-risk cancer cases," Dr. Etzioni and her associates said.
"Ultimately, the model predicts that approximately 64% of men on active surveillance would be treated [for prostate cancer] within their lifetimes. ... Thus, under active surveillance, 36% of men could avoid being treated," they said.
These findings are consistent with those of at least one other modeling study and with those of the longitudinal PIVOT (Prostate Cancer Intervention versus Observation Trial) study that tracked disease-free survival for 12 years.
"Although this is not a new result, it is confirmation of what we expected, and it substantiates data from previous studies looking at watchful waiting. Very few men with low-risk disease die from prostate cancer regardless, and the difference between treatments appears to be very modest," Dr. Etzioni said in a press statement accompanying this report.
This study was supported by the National Cancer Institute and the Centers for Disease Control and Prevention. No financial conflicts of interest were reported.
Compared with immediate radical prostatectomy, active surveillance for men with low-risk prostate cancer produces only a "very modest" 1.8-month decrease in cancer-specific survival, according to a report published online Sept. 24 in Clinical Cancer Research.
However, men on active surveillance enjoyed 6 more years of life free from treatment and its adverse effects than men who had immediate surgery, said Dr. Ruth Etzioni of the division of public health services, Fred Hutchinson Cancer Research Center, Seattle, and her associates.
These are the findings of a new simulation model they developed to predict prostate cancer mortality in a virtual population of 1 million contemporary U.S. cases, using the best available data from contemporary studies of the issue.
The investigators first incorporated into their simulation model the findings from an active surveillance program in which men with low-risk prostate cancer are biopsied every year and referred for further treatment if any adverse changes are found. This program also allows patients to self-refer for further treatment for several other reasons, including if their prostate-specific antigen level rises or if they become too anxious over "watchful waiting."
The researchers then incorporated into the model information from a large longitudinal database on the interval between radical prostatectomy and recurrence. The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) database enrolled nearly 14,000 men treated at 40 urology practices, and included 1,000 clinical and patient variables.
Lastly, Dr. Etzioni and her colleagues used data from another cohort study of 3,470 men to model the time from prostate cancer recurrence until death. They then computed the cumulative cancer-specific mortality in their virtual cohort for men under active surveillance compared with men who underwent immediate radical prostatectomy.
The model projected that the 20-year cumulative rate of prostate cancer–specific mortality would be 2.78% with active surveillance and 1.64% with immediate radical prostatectomy. This corresponded with an average of 1.8 months of life saved per case, which was considered a "very modest" advantage, the investigators said (Clin. Cancer Res. 2012 Sept. 24 [doi:10.1158/1078-0432.CCR-12-1502]).
However, the model also showed that men on active surveillance "had on average 6.4 more years of life free from treatment and its side effects," which could be a substantial advantage.
Three separate sensitivity analyses demonstrated that the model’s projections were robust even when multiple variables were altered. "All sensitivity analyses produced only modest differences in cumulative prostate cancer mortality under active surveillance, and supported our projection that active surveillance would have a minimal impact on life expectancy for low-risk cancer cases," Dr. Etzioni and her associates said.
"Ultimately, the model predicts that approximately 64% of men on active surveillance would be treated [for prostate cancer] within their lifetimes. ... Thus, under active surveillance, 36% of men could avoid being treated," they said.
These findings are consistent with those of at least one other modeling study and with those of the longitudinal PIVOT (Prostate Cancer Intervention versus Observation Trial) study that tracked disease-free survival for 12 years.
"Although this is not a new result, it is confirmation of what we expected, and it substantiates data from previous studies looking at watchful waiting. Very few men with low-risk disease die from prostate cancer regardless, and the difference between treatments appears to be very modest," Dr. Etzioni said in a press statement accompanying this report.
This study was supported by the National Cancer Institute and the Centers for Disease Control and Prevention. No financial conflicts of interest were reported.
FROM CLINICAL CANCER RESEARCH
Major Finding: The predicted 20-year cumulative rate of prostate cancer–specific mortality showed 1.8 months of life saved per patient who chose surgery over watchful waiting, but the watchful waiting group benefited from 6.4 more years of freedom from treatment and treatment-related side effects.
Data Source: Investigators ran a simulation model that predicted prostate cancer–specific mortality in a virtual population of 1,000 U.S. men with low-risk disease.
Disclosures: This study was supported by the National Cancer Institute and the Centers for Disease Control and Prevention. No financial conflicts of interest were reported.
Antibiotic Resistance May Drive Cystitis Rx Changes
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Between 1998 and 2009, prescriptions for the first-line urinary anti-infectives trimethoprim/ sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin for uncomplicated cystitis in women remained constant (P = .10); yet prescriptions for quinolones grew by 10% and prescriptions for cephalosporins grew by 3% (P less than .01 and P = .02, respectively).
Data Source: This was an analysis of data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey related to an estimated 124,978,631 visits for cystitis over the 10-year period.
Disclosures: Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
FDA Panel Votes Against Approval of Hyponatremia Drug
SILVER SPRING, MD. – A Food and Drug Administration advisory panel has recommended against the approval of lixivaptan, an orally administered vasopressin-2 receptor antagonist, for treating hyponatremia in two groups of adult patients at a meeting on Sept. 13.
The manufacturer, Cardiokine Biopharma, has proposed that lixivaptan be approved for the treatment of hypervolemic hyponatremia associated with heart failure, and for the treatment of euvolemic hyponatremia associated with syndrome of inappropriate antidiuretic hormone (SIADH). The company submitted the results of three phase III placebo-controlled trials that evaluated the changes from baseline in serum sodium at day 7 of treatment, the primary efficacy end point. The company proposed that for the SIADH indication, treatment could be initiated in an outpatient setting, which would be a potential benefit over existing treatments, including the only approved orally administered vasopressin-2 receptor antagonist that is approved for hyponatremia, tolvaptan (Samsca). Tolvaptan is approved for inpatients with diagnoses that include SIADH, heart failure, and cirrhosis, and is initiated in the hospital. The other approved "vaptan" – zomivaptan (Vaprisol), approved in 2005 – is administered intravenously.
Lixivaptan acts specifically on the vasopressin-2 receptor in the kidneys, "causing water to be excreted while sparing sodium without affecting other electrolytes," according to Cardiokine. While the changes in serum sodium from baseline to day 7 among treated patients over placebo were statistically significant, the improvements were modest and were not associated with improved cognitive function, the FDA reviewers pointed out.
In the study of patients with hypervolemic hyponatremia hospitalized with New York Heart Association (NYHA) class III or IV heart failure (652 patients), the increase in serum sodium at day 7 was 1.2 mEq/L greater among treated patients, compared with those on placebo. The mortality rate was 17.7% among those who had at least one dose of lixivaptan, compared with 14.3% on placebo; most deaths were related to heart failure, according to Cardiokine, which was recently acquired by Cornerstone Therapeutics.
In the two other studies, comprising a total of 312 patients with SIADH, the increases in serum sodium at day 7 over placebo were 2.2 mEq/L and 2.4 mEq/L.
But at the meeting of the FDA’s Cardiovascular and Renal Drugs Advisory Committee, the panel unanimously voted against approval of lixivaptan for the heart failure indication, because its members were not convinced that the modest effect of treatment on hyponatremia observed in the study of heart failure patients provided evidence that it benefited patients. The panel also agreed that more data on how improvements in serum sodium translated to clinical benefits, such as quality of life improvements, were needed. Another concern was that mortality was higher among the patients treated with lixivaptan than in those on placebo, particularly early in treatment.
The panel voted 5 to 3 against approval for treatment of hyponatremia in patients with SIADH, with clinicians voting on both sides of this question.
Dr. Linda Fried, professor of medicine at the VA Health Care System in Pittsburgh, voted in favor of approval because she said she believed that the vaptans directly affect pathophysiology in SIADH, and because she did not see a safety signal.
But Dr. Mori Krantz, associate professor of cardiology at the University of Colorado, Denver, voted against approval, because there were not enough data to show whether the improvements with treatment were clinically meaningful. He said that a larger study evaluating the effects of improvements in serum sodium with treatment on quality of life and other measures was needed, "to at least give clinicians some sense of security that they are helping patients."
Most panelists questioned the feasibility of initiating treatment as an outpatient, in most clinical settings.
The FDA is expected to make a decision on approval by Oct. 29.
Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at this meeting.
SILVER SPRING, MD. – A Food and Drug Administration advisory panel has recommended against the approval of lixivaptan, an orally administered vasopressin-2 receptor antagonist, for treating hyponatremia in two groups of adult patients at a meeting on Sept. 13.
The manufacturer, Cardiokine Biopharma, has proposed that lixivaptan be approved for the treatment of hypervolemic hyponatremia associated with heart failure, and for the treatment of euvolemic hyponatremia associated with syndrome of inappropriate antidiuretic hormone (SIADH). The company submitted the results of three phase III placebo-controlled trials that evaluated the changes from baseline in serum sodium at day 7 of treatment, the primary efficacy end point. The company proposed that for the SIADH indication, treatment could be initiated in an outpatient setting, which would be a potential benefit over existing treatments, including the only approved orally administered vasopressin-2 receptor antagonist that is approved for hyponatremia, tolvaptan (Samsca). Tolvaptan is approved for inpatients with diagnoses that include SIADH, heart failure, and cirrhosis, and is initiated in the hospital. The other approved "vaptan" – zomivaptan (Vaprisol), approved in 2005 – is administered intravenously.
Lixivaptan acts specifically on the vasopressin-2 receptor in the kidneys, "causing water to be excreted while sparing sodium without affecting other electrolytes," according to Cardiokine. While the changes in serum sodium from baseline to day 7 among treated patients over placebo were statistically significant, the improvements were modest and were not associated with improved cognitive function, the FDA reviewers pointed out.
In the study of patients with hypervolemic hyponatremia hospitalized with New York Heart Association (NYHA) class III or IV heart failure (652 patients), the increase in serum sodium at day 7 was 1.2 mEq/L greater among treated patients, compared with those on placebo. The mortality rate was 17.7% among those who had at least one dose of lixivaptan, compared with 14.3% on placebo; most deaths were related to heart failure, according to Cardiokine, which was recently acquired by Cornerstone Therapeutics.
In the two other studies, comprising a total of 312 patients with SIADH, the increases in serum sodium at day 7 over placebo were 2.2 mEq/L and 2.4 mEq/L.
But at the meeting of the FDA’s Cardiovascular and Renal Drugs Advisory Committee, the panel unanimously voted against approval of lixivaptan for the heart failure indication, because its members were not convinced that the modest effect of treatment on hyponatremia observed in the study of heart failure patients provided evidence that it benefited patients. The panel also agreed that more data on how improvements in serum sodium translated to clinical benefits, such as quality of life improvements, were needed. Another concern was that mortality was higher among the patients treated with lixivaptan than in those on placebo, particularly early in treatment.
The panel voted 5 to 3 against approval for treatment of hyponatremia in patients with SIADH, with clinicians voting on both sides of this question.
Dr. Linda Fried, professor of medicine at the VA Health Care System in Pittsburgh, voted in favor of approval because she said she believed that the vaptans directly affect pathophysiology in SIADH, and because she did not see a safety signal.
But Dr. Mori Krantz, associate professor of cardiology at the University of Colorado, Denver, voted against approval, because there were not enough data to show whether the improvements with treatment were clinically meaningful. He said that a larger study evaluating the effects of improvements in serum sodium with treatment on quality of life and other measures was needed, "to at least give clinicians some sense of security that they are helping patients."
Most panelists questioned the feasibility of initiating treatment as an outpatient, in most clinical settings.
The FDA is expected to make a decision on approval by Oct. 29.
Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at this meeting.
SILVER SPRING, MD. – A Food and Drug Administration advisory panel has recommended against the approval of lixivaptan, an orally administered vasopressin-2 receptor antagonist, for treating hyponatremia in two groups of adult patients at a meeting on Sept. 13.
The manufacturer, Cardiokine Biopharma, has proposed that lixivaptan be approved for the treatment of hypervolemic hyponatremia associated with heart failure, and for the treatment of euvolemic hyponatremia associated with syndrome of inappropriate antidiuretic hormone (SIADH). The company submitted the results of three phase III placebo-controlled trials that evaluated the changes from baseline in serum sodium at day 7 of treatment, the primary efficacy end point. The company proposed that for the SIADH indication, treatment could be initiated in an outpatient setting, which would be a potential benefit over existing treatments, including the only approved orally administered vasopressin-2 receptor antagonist that is approved for hyponatremia, tolvaptan (Samsca). Tolvaptan is approved for inpatients with diagnoses that include SIADH, heart failure, and cirrhosis, and is initiated in the hospital. The other approved "vaptan" – zomivaptan (Vaprisol), approved in 2005 – is administered intravenously.
Lixivaptan acts specifically on the vasopressin-2 receptor in the kidneys, "causing water to be excreted while sparing sodium without affecting other electrolytes," according to Cardiokine. While the changes in serum sodium from baseline to day 7 among treated patients over placebo were statistically significant, the improvements were modest and were not associated with improved cognitive function, the FDA reviewers pointed out.
In the study of patients with hypervolemic hyponatremia hospitalized with New York Heart Association (NYHA) class III or IV heart failure (652 patients), the increase in serum sodium at day 7 was 1.2 mEq/L greater among treated patients, compared with those on placebo. The mortality rate was 17.7% among those who had at least one dose of lixivaptan, compared with 14.3% on placebo; most deaths were related to heart failure, according to Cardiokine, which was recently acquired by Cornerstone Therapeutics.
In the two other studies, comprising a total of 312 patients with SIADH, the increases in serum sodium at day 7 over placebo were 2.2 mEq/L and 2.4 mEq/L.
But at the meeting of the FDA’s Cardiovascular and Renal Drugs Advisory Committee, the panel unanimously voted against approval of lixivaptan for the heart failure indication, because its members were not convinced that the modest effect of treatment on hyponatremia observed in the study of heart failure patients provided evidence that it benefited patients. The panel also agreed that more data on how improvements in serum sodium translated to clinical benefits, such as quality of life improvements, were needed. Another concern was that mortality was higher among the patients treated with lixivaptan than in those on placebo, particularly early in treatment.
The panel voted 5 to 3 against approval for treatment of hyponatremia in patients with SIADH, with clinicians voting on both sides of this question.
Dr. Linda Fried, professor of medicine at the VA Health Care System in Pittsburgh, voted in favor of approval because she said she believed that the vaptans directly affect pathophysiology in SIADH, and because she did not see a safety signal.
But Dr. Mori Krantz, associate professor of cardiology at the University of Colorado, Denver, voted against approval, because there were not enough data to show whether the improvements with treatment were clinically meaningful. He said that a larger study evaluating the effects of improvements in serum sodium with treatment on quality of life and other measures was needed, "to at least give clinicians some sense of security that they are helping patients."
Most panelists questioned the feasibility of initiating treatment as an outpatient, in most clinical settings.
The FDA is expected to make a decision on approval by Oct. 29.
Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at this meeting.