User login
Duloxetine reduces chemo-induced neuropathy
A 5-week course of daily oral duloxetine reduced pain and improved function and quality of life for patients with chemotherapy-induced peripheral neuropathy, according to a report in the April 3 issue of JAMA.
Duloxetine’s effects on chemotherapy-induced peripheral neuropathic pain were measured in a randomized, double-blind, placebo-controlled, crossover clinical trial involving 231 cancer patients aged 25 years and older who had been treated with platinum or taxane agents. Study subjects were approximately twice as likely to experience a 30% reduction in pain while taking duloxetine than while taking placebo and were 2.4 times more likely to experience a 50% reduction in pain, said Ellen M. Lavoie Smith, Ph.D., of the University of Michigan School of Nursing, Ann Arbor, and her associates. The data were presented at the 2012 annual meeting of the American Society of Clinical Oncology.
Patients also reported better daily functioning with duloxetine, compared with placebo, including improved scores on measures assessing numbness, tingling, or discomfort of the hands or feet; tinnitus or difficulty hearing; joint pain; muscle cramps and weakness; and difficulty walking, dressing, or feeling small objects in the hands. Pain-related quality of life also improved to a greater degree with duloxetine (mean change of 2.44 points out of 44 possible points on the Functional Assessment of Cancer Treatment, Gynecologic Oncology Group Neurotoxicity subscale) than with placebo (mean change of 0.87 points).
There were no hematologic or grade 4 adverse events. Mild adverse events were reported by 16% during duloxetine treatment and 27% during placebo treatment, and moderate adverse effects were reported by 7% and 3%, respectively. These included fatigue, insomnia, and nausea in both patient groups, the investigators said (JAMA 2013;309:1359-67).
This study was supported by the National Cancer Institute and the Alliance Statistics and Data Center. Study drugs and placebo were supplied by Eli Lilly. Dr. Smith reported no conflicts of interest, and one of her associates reported ties to Genentech.
A 5-week course of daily oral duloxetine reduced pain and improved function and quality of life for patients with chemotherapy-induced peripheral neuropathy, according to a report in the April 3 issue of JAMA.
Duloxetine’s effects on chemotherapy-induced peripheral neuropathic pain were measured in a randomized, double-blind, placebo-controlled, crossover clinical trial involving 231 cancer patients aged 25 years and older who had been treated with platinum or taxane agents. Study subjects were approximately twice as likely to experience a 30% reduction in pain while taking duloxetine than while taking placebo and were 2.4 times more likely to experience a 50% reduction in pain, said Ellen M. Lavoie Smith, Ph.D., of the University of Michigan School of Nursing, Ann Arbor, and her associates. The data were presented at the 2012 annual meeting of the American Society of Clinical Oncology.
Patients also reported better daily functioning with duloxetine, compared with placebo, including improved scores on measures assessing numbness, tingling, or discomfort of the hands or feet; tinnitus or difficulty hearing; joint pain; muscle cramps and weakness; and difficulty walking, dressing, or feeling small objects in the hands. Pain-related quality of life also improved to a greater degree with duloxetine (mean change of 2.44 points out of 44 possible points on the Functional Assessment of Cancer Treatment, Gynecologic Oncology Group Neurotoxicity subscale) than with placebo (mean change of 0.87 points).
There were no hematologic or grade 4 adverse events. Mild adverse events were reported by 16% during duloxetine treatment and 27% during placebo treatment, and moderate adverse effects were reported by 7% and 3%, respectively. These included fatigue, insomnia, and nausea in both patient groups, the investigators said (JAMA 2013;309:1359-67).
This study was supported by the National Cancer Institute and the Alliance Statistics and Data Center. Study drugs and placebo were supplied by Eli Lilly. Dr. Smith reported no conflicts of interest, and one of her associates reported ties to Genentech.
A 5-week course of daily oral duloxetine reduced pain and improved function and quality of life for patients with chemotherapy-induced peripheral neuropathy, according to a report in the April 3 issue of JAMA.
Duloxetine’s effects on chemotherapy-induced peripheral neuropathic pain were measured in a randomized, double-blind, placebo-controlled, crossover clinical trial involving 231 cancer patients aged 25 years and older who had been treated with platinum or taxane agents. Study subjects were approximately twice as likely to experience a 30% reduction in pain while taking duloxetine than while taking placebo and were 2.4 times more likely to experience a 50% reduction in pain, said Ellen M. Lavoie Smith, Ph.D., of the University of Michigan School of Nursing, Ann Arbor, and her associates. The data were presented at the 2012 annual meeting of the American Society of Clinical Oncology.
Patients also reported better daily functioning with duloxetine, compared with placebo, including improved scores on measures assessing numbness, tingling, or discomfort of the hands or feet; tinnitus or difficulty hearing; joint pain; muscle cramps and weakness; and difficulty walking, dressing, or feeling small objects in the hands. Pain-related quality of life also improved to a greater degree with duloxetine (mean change of 2.44 points out of 44 possible points on the Functional Assessment of Cancer Treatment, Gynecologic Oncology Group Neurotoxicity subscale) than with placebo (mean change of 0.87 points).
There were no hematologic or grade 4 adverse events. Mild adverse events were reported by 16% during duloxetine treatment and 27% during placebo treatment, and moderate adverse effects were reported by 7% and 3%, respectively. These included fatigue, insomnia, and nausea in both patient groups, the investigators said (JAMA 2013;309:1359-67).
This study was supported by the National Cancer Institute and the Alliance Statistics and Data Center. Study drugs and placebo were supplied by Eli Lilly. Dr. Smith reported no conflicts of interest, and one of her associates reported ties to Genentech.
FROM JAMA
Major finding: Study subjects were 2.4 times more likely to experience a 50% pain reduction while taking duloxetine than while taking placebo.
Data source: A randomized, double-blind, placebo-controlled crossover trial involving 231 cancer patients.
Disclosures: This study was supported by the National Cancer Institute and the Alliance Statistics and Data Center. Study drugs and placebo were supplied by Eli Lilly. Dr. Smith reported no conflicts of interest, and one of her associates reported ties to Genentech.
'Chemobrain' starts before chemotherapy in breast cancer study
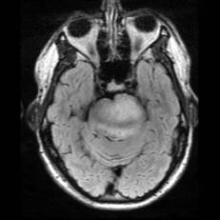
SAN ANTONIO – The muddled thinking that sometimes affects breast cancer patients is manifested by decreased activity in a brain region that plays a key role in working memory, according to results of a functional imaging study.
"Chemobrain," as it’s sometimes known, appears even before chemotherapy starts, suggesting that more may be at play than a cognitive reaction to the medications, Bernadine Cimprich, Ph.D., reported at the annual San Antonio Breast Cancer Symposium.
The findings of her functional imaging study show a strong correlation between fatigue and decreased activation in the left inferior frontal gyrus.
There’s no question that chemotherapy agents can have cognitive effects, said Dr. Cimprich, an associate professor emeritus of nursing at the University of Michigan, Ann Arbor. "But even before treatment, we saw reduced function in the regions needed to perform this task."
Her prospective comparative study comprised 69 women with localized (stage 0-III) breast cancer, and 32 age-matched healthy controls. The patients were 24-34 days post surgery, but had not yet received either chemotherapy (29) or radiotherapy (37). All of the women reported their levels of fatigue.
Before and after treatment, the patients performed a verbal test of working memory while undergoing functional magnetic resonance brain imaging both before and after treatments. Each test had several difficulty levels. Patients also self-reported fatigue at both time points.
The patients were an average of 51 years old. Half of the chemotherapy group and 95% of the radiotherapy group had undergone a breast-conserving surgical procedure. The other half of the chemotherapy group had mastectomies.
The subjects performed the Verbal Working Memory Task during scanning. Following the scan, they completed the Attentional Function Index and the Functional Assessment of Cancer Therapy-Fatigue. The memory test involved three levels of difficulty, from low to high demand.
Compared with the radiotherapy and control groups, the chemotherapy group reported more fatigue at both time points, and performed significantly more poorly on the cognitive test at both time points (P less than .05). Greater fatigue in the chemotherapy group was positively associated with and correlated with poorer cognitive performance; the difference was significant in the post-treatment period (P = .03).
The radiotherapy group performed significantly better than the chemotherapy group, and significantly worse than the control group. Fatigue scores also fell between those of the chemotherapy group and the control group.
Imaging showed a positive correlation between poor cognitive performance and decreased activity in the left anterior frontal inferior gyrus. The score differences in the chemotherapy group "were mainly due to lower pretreatment activation in an area of the prefrontal cortex supporting working memory, the anatomical left inferior frontal gyrus, at the higher task demand," Dr. Cimprich said at a press briefing.
The level of inactivation in the region also significantly predicted the severity of fatigue in both treatment groups (P less than .01). The post-treatment imaging, conducted about 5 months after the baseline assessment, showed no differences in brain activation. However, those who had the lowest activation also had the highest post-treatment fatigue, she added.
"Women who were not able to activate this region suffered significantly greater fatigue after treatment, regardless of whether they received chemotherapy or radiotherapy," Dr. Cimprich said.
Dr. Cimprich had no financial disclosures. The study was supported by the National Institutes of Health and the National Institute of Nursing Research.
SAN ANTONIO – The muddled thinking that sometimes affects breast cancer patients is manifested by decreased activity in a brain region that plays a key role in working memory, according to results of a functional imaging study.
"Chemobrain," as it’s sometimes known, appears even before chemotherapy starts, suggesting that more may be at play than a cognitive reaction to the medications, Bernadine Cimprich, Ph.D., reported at the annual San Antonio Breast Cancer Symposium.
The findings of her functional imaging study show a strong correlation between fatigue and decreased activation in the left inferior frontal gyrus.
There’s no question that chemotherapy agents can have cognitive effects, said Dr. Cimprich, an associate professor emeritus of nursing at the University of Michigan, Ann Arbor. "But even before treatment, we saw reduced function in the regions needed to perform this task."
Her prospective comparative study comprised 69 women with localized (stage 0-III) breast cancer, and 32 age-matched healthy controls. The patients were 24-34 days post surgery, but had not yet received either chemotherapy (29) or radiotherapy (37). All of the women reported their levels of fatigue.
Before and after treatment, the patients performed a verbal test of working memory while undergoing functional magnetic resonance brain imaging both before and after treatments. Each test had several difficulty levels. Patients also self-reported fatigue at both time points.
The patients were an average of 51 years old. Half of the chemotherapy group and 95% of the radiotherapy group had undergone a breast-conserving surgical procedure. The other half of the chemotherapy group had mastectomies.
The subjects performed the Verbal Working Memory Task during scanning. Following the scan, they completed the Attentional Function Index and the Functional Assessment of Cancer Therapy-Fatigue. The memory test involved three levels of difficulty, from low to high demand.
Compared with the radiotherapy and control groups, the chemotherapy group reported more fatigue at both time points, and performed significantly more poorly on the cognitive test at both time points (P less than .05). Greater fatigue in the chemotherapy group was positively associated with and correlated with poorer cognitive performance; the difference was significant in the post-treatment period (P = .03).
The radiotherapy group performed significantly better than the chemotherapy group, and significantly worse than the control group. Fatigue scores also fell between those of the chemotherapy group and the control group.
Imaging showed a positive correlation between poor cognitive performance and decreased activity in the left anterior frontal inferior gyrus. The score differences in the chemotherapy group "were mainly due to lower pretreatment activation in an area of the prefrontal cortex supporting working memory, the anatomical left inferior frontal gyrus, at the higher task demand," Dr. Cimprich said at a press briefing.
The level of inactivation in the region also significantly predicted the severity of fatigue in both treatment groups (P less than .01). The post-treatment imaging, conducted about 5 months after the baseline assessment, showed no differences in brain activation. However, those who had the lowest activation also had the highest post-treatment fatigue, she added.
"Women who were not able to activate this region suffered significantly greater fatigue after treatment, regardless of whether they received chemotherapy or radiotherapy," Dr. Cimprich said.
Dr. Cimprich had no financial disclosures. The study was supported by the National Institutes of Health and the National Institute of Nursing Research.
SAN ANTONIO – The muddled thinking that sometimes affects breast cancer patients is manifested by decreased activity in a brain region that plays a key role in working memory, according to results of a functional imaging study.
"Chemobrain," as it’s sometimes known, appears even before chemotherapy starts, suggesting that more may be at play than a cognitive reaction to the medications, Bernadine Cimprich, Ph.D., reported at the annual San Antonio Breast Cancer Symposium.
The findings of her functional imaging study show a strong correlation between fatigue and decreased activation in the left inferior frontal gyrus.
There’s no question that chemotherapy agents can have cognitive effects, said Dr. Cimprich, an associate professor emeritus of nursing at the University of Michigan, Ann Arbor. "But even before treatment, we saw reduced function in the regions needed to perform this task."
Her prospective comparative study comprised 69 women with localized (stage 0-III) breast cancer, and 32 age-matched healthy controls. The patients were 24-34 days post surgery, but had not yet received either chemotherapy (29) or radiotherapy (37). All of the women reported their levels of fatigue.
Before and after treatment, the patients performed a verbal test of working memory while undergoing functional magnetic resonance brain imaging both before and after treatments. Each test had several difficulty levels. Patients also self-reported fatigue at both time points.
The patients were an average of 51 years old. Half of the chemotherapy group and 95% of the radiotherapy group had undergone a breast-conserving surgical procedure. The other half of the chemotherapy group had mastectomies.
The subjects performed the Verbal Working Memory Task during scanning. Following the scan, they completed the Attentional Function Index and the Functional Assessment of Cancer Therapy-Fatigue. The memory test involved three levels of difficulty, from low to high demand.
Compared with the radiotherapy and control groups, the chemotherapy group reported more fatigue at both time points, and performed significantly more poorly on the cognitive test at both time points (P less than .05). Greater fatigue in the chemotherapy group was positively associated with and correlated with poorer cognitive performance; the difference was significant in the post-treatment period (P = .03).
The radiotherapy group performed significantly better than the chemotherapy group, and significantly worse than the control group. Fatigue scores also fell between those of the chemotherapy group and the control group.
Imaging showed a positive correlation between poor cognitive performance and decreased activity in the left anterior frontal inferior gyrus. The score differences in the chemotherapy group "were mainly due to lower pretreatment activation in an area of the prefrontal cortex supporting working memory, the anatomical left inferior frontal gyrus, at the higher task demand," Dr. Cimprich said at a press briefing.
The level of inactivation in the region also significantly predicted the severity of fatigue in both treatment groups (P less than .01). The post-treatment imaging, conducted about 5 months after the baseline assessment, showed no differences in brain activation. However, those who had the lowest activation also had the highest post-treatment fatigue, she added.
"Women who were not able to activate this region suffered significantly greater fatigue after treatment, regardless of whether they received chemotherapy or radiotherapy," Dr. Cimprich said.
Dr. Cimprich had no financial disclosures. The study was supported by the National Institutes of Health and the National Institute of Nursing Research.
AT THE ANNUAL SAN ANTONIO BREAST CANCER SYMPOSIUM
Major Finding: Women scheduled to undergo chemotherapy after surgery for breast cancer were significantly more likely to show low brain activation in a task of working memory than other groups studied (P less than .05).
Data Source: A prospective, comparative study of 69 patients and 32 matched controls.
Disclosures: Dr. Cimprich had no financial disclosures. The study was supported by the National Institutes of Health and the National Institute of Nursing Research.
PET/CT Pinpoints Physiological Evidence of Chemo Brain
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036).
Data Source: This was a retrospective analysis of PET/CT scans from 115 patients with advanced breast cancer.
Disclosures: Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
Early Surgery Yields Survival Benefit for Low-Grade Gliomas
Adults in Norway with diffuse low-grade gliomas who were treated at a hospital advocating early surgical resection had better overall survival than those treated at a hospital advocating "watchful waiting," according to a report published online Oct. 30 in JAMA.
This finding significantly strengthens the sparse evidence in support of early resection for newly diagnosed diffuse low-grade gliomas, said Dr. Asgeir S. Jakola of the department of neurosurgery, St. Olav’s University Hospital, Trondheim (Norway) and his associates.
Management of these tumors is one of the major controversies in both neurology and oncology today, largely because the effect of surgery on survival is still unclear. The only evidence available until now was based solely on uncontrolled surgical series; some of these have reported that it is safe to withhold surgery until the lesions progress, while others have reported that immediate resection improves survival and delays the time to malignant transformation.
Both patients and physicians are reluctant to undertake immediate surgery when the evidence supporting that strategy has been so tenuous. They also are concerned that the risk of early and aggressive surgery outweighs the benefit, particularly when most patients are capable of normal activity and have a reasonably long life expectancy at diagnosis, the investigators said.
It is unlikely that a randomized, controlled study comparing the two approaches will ever be performed. Dr. Jakola and his colleagues therefore conducted a retrospective, population-based parallel-cohort study at two neurosurgical centers, each of which preferred one of these strategies over the other. Their "natural experiment" was possible because in Norway, there were two such facilities that were relatively close geographically and served a homogenous population. The nationalized health care system distributes training, resources, and personnel equally throughout the country, so the two hospitals were quite similar in other respects. And patient follow-up is 100%.
The 12-year study involved 153 adults with diffuse, histologically verified supratentorial grade I and II tumors diagnosed in 1998-2009, who were followed until death or until April 2011. The median follow-up was 7 years. Gliomas included astrocytomas, oligodendrogliomas, and oligoastrocytomas.
For patients with newly diagnosed low-grade gliomas, hospital A favored biopsy and watchful waiting. The 66 patients treated there typically were followed with MRI at 3 and 6 months, then yearly thereafter. They usually were offered surgical resection, if the lesions grew or showed signs of malignant transformation.
Hospital B favored immediate maximal safe tumor resection for the 87 patients treated there, with MRI follow-up at 6 and 12 months, then annually thereafter. This strategy was not pursued in some patients, however: notably, those who were elderly or had comorbidities and were likely to die from another cause before malignant transformation would take place, and those who had very widespread tumor infiltration that made resection impractical.
The two study groups were well balanced with regard to patient age and comorbidities, and rates of surgical rescue therapy were the same. There also were no differences between the two groups in complications or acquired neurologic deficits.
At the end of the study period, 34 patients (52%) from hospital A had died, compared with only 28 patients (32%) from hospital B. Median survival was 5.9 years at hospital A, but median survival had not yet been reached at hospital B, the researchers said (JAMA 2012;308: [doi:10.1001/jama.2012.12807]).
This survival advantage increased over time. Expected 3-year survival was 70% at hospital A vs. 80% at hospital B; expected 5-year survival was 60% at hospital A vs. 74% at hospital B; and expected 7-year survival was 44% at hospital A vs. 68% at hospital B.
In a post hoc analysis that attempted to account for differences between the two study groups in prognostic factors, the survival benefit for immediate resection remained robust. It also remained robust in another post hoc analysis that examined the subgroup of patients who had the most common glioma, a grade II astrocytoma. Median survival was 5.6 years at the hospital favoring watchful waiting, compared with 9.7 years at the hospital favoring early resection, in this large subgroup of patients.
Based on these findings, hospital A has changed its preferred strategy from watchful waiting to early resection, Dr. Jakola and his associates said.
"Despite the clear survival advantage seen, clinical judgment is still necessary in individual patients with suspected low-grade glioma since results will depend on patient and disease characteristics together with surgical results in terms of resection grades and complication rates," they added.
One of Dr. Jakola’s associates reported holding stock in Sonowand, manufacturer of the 3-D ultrasound-based imaging system used in one of the study hospitals.
This "natural experiment" may be the best source of evidence supporting early surgical resection that we’re likely to get, but the study by Dr. Jakola and his colleagues did have some limitations, said Dr. James M. Markert.
The confidence intervals around the point estimates for survival in both groups overlapped, which means the patients must be followed for a longer period to ensure that the confidence intervals eventually separate definitively. Also, one potentially important difference between the two study groups was not accounted for: the proportion of oligodendrogliomas, which are highly survivable, was higher at hospital B (19%) than at hospital A (9%).
In addition, radiation therapy was administered more often at the hospital favoring resection (43% of patients) than at the hospital favoring watchful waiting (29%), which may have affected survival rates. And although the authors reported no differences between the two groups in complications or neurologic deficits, "assessment methods were not delineated and the data were insufficient to reach a definitive conclusion," he noted.
Dr. Markert is in the division of neurosurgery at the University of Alabama at Birmingham. He reported ties to Catherex and Tocgen. These remarks were taken from his editorial accompanying Dr. Jakola’s report (JAMA 2012 Oct. 25 [doi:10.1001/jama.2012.14523]).
This "natural experiment" may be the best source of evidence supporting early surgical resection that we’re likely to get, but the study by Dr. Jakola and his colleagues did have some limitations, said Dr. James M. Markert.
The confidence intervals around the point estimates for survival in both groups overlapped, which means the patients must be followed for a longer period to ensure that the confidence intervals eventually separate definitively. Also, one potentially important difference between the two study groups was not accounted for: the proportion of oligodendrogliomas, which are highly survivable, was higher at hospital B (19%) than at hospital A (9%).
In addition, radiation therapy was administered more often at the hospital favoring resection (43% of patients) than at the hospital favoring watchful waiting (29%), which may have affected survival rates. And although the authors reported no differences between the two groups in complications or neurologic deficits, "assessment methods were not delineated and the data were insufficient to reach a definitive conclusion," he noted.
Dr. Markert is in the division of neurosurgery at the University of Alabama at Birmingham. He reported ties to Catherex and Tocgen. These remarks were taken from his editorial accompanying Dr. Jakola’s report (JAMA 2012 Oct. 25 [doi:10.1001/jama.2012.14523]).
This "natural experiment" may be the best source of evidence supporting early surgical resection that we’re likely to get, but the study by Dr. Jakola and his colleagues did have some limitations, said Dr. James M. Markert.
The confidence intervals around the point estimates for survival in both groups overlapped, which means the patients must be followed for a longer period to ensure that the confidence intervals eventually separate definitively. Also, one potentially important difference between the two study groups was not accounted for: the proportion of oligodendrogliomas, which are highly survivable, was higher at hospital B (19%) than at hospital A (9%).
In addition, radiation therapy was administered more often at the hospital favoring resection (43% of patients) than at the hospital favoring watchful waiting (29%), which may have affected survival rates. And although the authors reported no differences between the two groups in complications or neurologic deficits, "assessment methods were not delineated and the data were insufficient to reach a definitive conclusion," he noted.
Dr. Markert is in the division of neurosurgery at the University of Alabama at Birmingham. He reported ties to Catherex and Tocgen. These remarks were taken from his editorial accompanying Dr. Jakola’s report (JAMA 2012 Oct. 25 [doi:10.1001/jama.2012.14523]).
Adults in Norway with diffuse low-grade gliomas who were treated at a hospital advocating early surgical resection had better overall survival than those treated at a hospital advocating "watchful waiting," according to a report published online Oct. 30 in JAMA.
This finding significantly strengthens the sparse evidence in support of early resection for newly diagnosed diffuse low-grade gliomas, said Dr. Asgeir S. Jakola of the department of neurosurgery, St. Olav’s University Hospital, Trondheim (Norway) and his associates.
Management of these tumors is one of the major controversies in both neurology and oncology today, largely because the effect of surgery on survival is still unclear. The only evidence available until now was based solely on uncontrolled surgical series; some of these have reported that it is safe to withhold surgery until the lesions progress, while others have reported that immediate resection improves survival and delays the time to malignant transformation.
Both patients and physicians are reluctant to undertake immediate surgery when the evidence supporting that strategy has been so tenuous. They also are concerned that the risk of early and aggressive surgery outweighs the benefit, particularly when most patients are capable of normal activity and have a reasonably long life expectancy at diagnosis, the investigators said.
It is unlikely that a randomized, controlled study comparing the two approaches will ever be performed. Dr. Jakola and his colleagues therefore conducted a retrospective, population-based parallel-cohort study at two neurosurgical centers, each of which preferred one of these strategies over the other. Their "natural experiment" was possible because in Norway, there were two such facilities that were relatively close geographically and served a homogenous population. The nationalized health care system distributes training, resources, and personnel equally throughout the country, so the two hospitals were quite similar in other respects. And patient follow-up is 100%.
The 12-year study involved 153 adults with diffuse, histologically verified supratentorial grade I and II tumors diagnosed in 1998-2009, who were followed until death or until April 2011. The median follow-up was 7 years. Gliomas included astrocytomas, oligodendrogliomas, and oligoastrocytomas.
For patients with newly diagnosed low-grade gliomas, hospital A favored biopsy and watchful waiting. The 66 patients treated there typically were followed with MRI at 3 and 6 months, then yearly thereafter. They usually were offered surgical resection, if the lesions grew or showed signs of malignant transformation.
Hospital B favored immediate maximal safe tumor resection for the 87 patients treated there, with MRI follow-up at 6 and 12 months, then annually thereafter. This strategy was not pursued in some patients, however: notably, those who were elderly or had comorbidities and were likely to die from another cause before malignant transformation would take place, and those who had very widespread tumor infiltration that made resection impractical.
The two study groups were well balanced with regard to patient age and comorbidities, and rates of surgical rescue therapy were the same. There also were no differences between the two groups in complications or acquired neurologic deficits.
At the end of the study period, 34 patients (52%) from hospital A had died, compared with only 28 patients (32%) from hospital B. Median survival was 5.9 years at hospital A, but median survival had not yet been reached at hospital B, the researchers said (JAMA 2012;308: [doi:10.1001/jama.2012.12807]).
This survival advantage increased over time. Expected 3-year survival was 70% at hospital A vs. 80% at hospital B; expected 5-year survival was 60% at hospital A vs. 74% at hospital B; and expected 7-year survival was 44% at hospital A vs. 68% at hospital B.
In a post hoc analysis that attempted to account for differences between the two study groups in prognostic factors, the survival benefit for immediate resection remained robust. It also remained robust in another post hoc analysis that examined the subgroup of patients who had the most common glioma, a grade II astrocytoma. Median survival was 5.6 years at the hospital favoring watchful waiting, compared with 9.7 years at the hospital favoring early resection, in this large subgroup of patients.
Based on these findings, hospital A has changed its preferred strategy from watchful waiting to early resection, Dr. Jakola and his associates said.
"Despite the clear survival advantage seen, clinical judgment is still necessary in individual patients with suspected low-grade glioma since results will depend on patient and disease characteristics together with surgical results in terms of resection grades and complication rates," they added.
One of Dr. Jakola’s associates reported holding stock in Sonowand, manufacturer of the 3-D ultrasound-based imaging system used in one of the study hospitals.
Adults in Norway with diffuse low-grade gliomas who were treated at a hospital advocating early surgical resection had better overall survival than those treated at a hospital advocating "watchful waiting," according to a report published online Oct. 30 in JAMA.
This finding significantly strengthens the sparse evidence in support of early resection for newly diagnosed diffuse low-grade gliomas, said Dr. Asgeir S. Jakola of the department of neurosurgery, St. Olav’s University Hospital, Trondheim (Norway) and his associates.
Management of these tumors is one of the major controversies in both neurology and oncology today, largely because the effect of surgery on survival is still unclear. The only evidence available until now was based solely on uncontrolled surgical series; some of these have reported that it is safe to withhold surgery until the lesions progress, while others have reported that immediate resection improves survival and delays the time to malignant transformation.
Both patients and physicians are reluctant to undertake immediate surgery when the evidence supporting that strategy has been so tenuous. They also are concerned that the risk of early and aggressive surgery outweighs the benefit, particularly when most patients are capable of normal activity and have a reasonably long life expectancy at diagnosis, the investigators said.
It is unlikely that a randomized, controlled study comparing the two approaches will ever be performed. Dr. Jakola and his colleagues therefore conducted a retrospective, population-based parallel-cohort study at two neurosurgical centers, each of which preferred one of these strategies over the other. Their "natural experiment" was possible because in Norway, there were two such facilities that were relatively close geographically and served a homogenous population. The nationalized health care system distributes training, resources, and personnel equally throughout the country, so the two hospitals were quite similar in other respects. And patient follow-up is 100%.
The 12-year study involved 153 adults with diffuse, histologically verified supratentorial grade I and II tumors diagnosed in 1998-2009, who were followed until death or until April 2011. The median follow-up was 7 years. Gliomas included astrocytomas, oligodendrogliomas, and oligoastrocytomas.
For patients with newly diagnosed low-grade gliomas, hospital A favored biopsy and watchful waiting. The 66 patients treated there typically were followed with MRI at 3 and 6 months, then yearly thereafter. They usually were offered surgical resection, if the lesions grew or showed signs of malignant transformation.
Hospital B favored immediate maximal safe tumor resection for the 87 patients treated there, with MRI follow-up at 6 and 12 months, then annually thereafter. This strategy was not pursued in some patients, however: notably, those who were elderly or had comorbidities and were likely to die from another cause before malignant transformation would take place, and those who had very widespread tumor infiltration that made resection impractical.
The two study groups were well balanced with regard to patient age and comorbidities, and rates of surgical rescue therapy were the same. There also were no differences between the two groups in complications or acquired neurologic deficits.
At the end of the study period, 34 patients (52%) from hospital A had died, compared with only 28 patients (32%) from hospital B. Median survival was 5.9 years at hospital A, but median survival had not yet been reached at hospital B, the researchers said (JAMA 2012;308: [doi:10.1001/jama.2012.12807]).
This survival advantage increased over time. Expected 3-year survival was 70% at hospital A vs. 80% at hospital B; expected 5-year survival was 60% at hospital A vs. 74% at hospital B; and expected 7-year survival was 44% at hospital A vs. 68% at hospital B.
In a post hoc analysis that attempted to account for differences between the two study groups in prognostic factors, the survival benefit for immediate resection remained robust. It also remained robust in another post hoc analysis that examined the subgroup of patients who had the most common glioma, a grade II astrocytoma. Median survival was 5.6 years at the hospital favoring watchful waiting, compared with 9.7 years at the hospital favoring early resection, in this large subgroup of patients.
Based on these findings, hospital A has changed its preferred strategy from watchful waiting to early resection, Dr. Jakola and his associates said.
"Despite the clear survival advantage seen, clinical judgment is still necessary in individual patients with suspected low-grade glioma since results will depend on patient and disease characteristics together with surgical results in terms of resection grades and complication rates," they added.
One of Dr. Jakola’s associates reported holding stock in Sonowand, manufacturer of the 3-D ultrasound-based imaging system used in one of the study hospitals.
FROM JAMA
Major Finding: Overall mortality was 52% with watchful waiting and 32% with early resection; median survival was 5.9 years in the first group but has not yet been reached in the second group.
Data Source: Investigators compared survival rates in one hospital that advocated watchful waiting (66 patients) and another that advocated early resection (87 patients) for low-grade gliomas.
Disclosures: One of Dr. Jakola’s associates reported holding stock in Sonowand, manufacturer of the 3-D ultrasound-based imaging system used in one of the study hospitals.
Memantine Protects Cognitive Function After Whole Brain Irradiation
BOSTON – Memantine, a drug normally prescribed for slowing cognitive decline in Alzheimer’s disease, can help to preserve cognitive function in cancer patients who have undergone whole brain irradiation, a study showed.
In a phase III trial, patients with brain metastases were randomly assigned to take 20 mg memantine (Namenda) or placebo daily for 24 weeks after whole brain radiation therapy (WBRT). The memantine cohort had a 17% relative reduction in cognitive decline compared with patients who got a placebo, Dr. Nadia N. Laack reported at the annual meeting of the American Society for Radiation Oncology.
The finding teetered on the edge of statistical significance (P = .059), however, because only one-third of patients (32%) completed the 24 weeks of drug therapy, due to death (survival was poorer than expected), disease progression, or noncompliance, said Dr. Laack. a radiation oncologist at the Mayo Clinic in Rochester, Minn.
"Overall, we feel that the weight of evidence supports our conclusion that memantine helps to preserve cognitive function after whole brain radiotherapy in patients with brain metastases," Dr. Laack said at a briefing prior to presenting the data at a plenary session.
WBRT is associated with cognitive impairment in a majority of patients who receive it, Dr. Laack said, noting that at 4 months post radiation, 60% of patients will have declines in one or more cognitive domains.
Because the mechanism of decline is similar to that seen with Alzheimer\'s and vascular dementias, and because memantine has been shown to modestly improve mild to moderate cognition in both dementia types, Dr. Laack and his colleagues hypothesized that it might protect brains exposed to therapeutic doses of radiation.
A total of 508 patients were tested at baseline and at 8, 16, 24, and 52 weeks after radiation with 37.5 Gy in 15 fractions. They were evaluated with MRI and cognitive assessment; domains of memory, processing speed, executive function, global function, self-reported cognitive function, and quality of life were evaluated. Median overall follow-up was 12.4 months.
There were no differences between the treatment groups in overall survival at a median of 6 months or in progression-free survival at 5 months.
Among 149 patients available for analysis at 24 weeks, patients who took memantine had a significantly longer time to memory decline than did those on placebo (P = .02), and had a trend toward less decline in the primary end point, the Hopkins Verbal Learning Test–Revised delayed recall instrument (median decline of 0 standard deviation, vs. –2 standard deviations for patients on placebo).
For the secondary objective of cognitive function decline/failure, defined as a change greater than reversible cognitive impairment or 2 standard deviations decline from baseline on any domain of brain function, the hazard ratio for memantine at 24 weeks was 0.784 (P = .01), indicating a significant reduction in the incidence of cognitive dysfunction.
"Although memantine was discontinued at 6 months, the effect on cognitive function was maintained for the duration of the trial, suggesting that memantine may be preventing radiation injury rather than simply treating cognitive dysfunction," Dr. Laack said.
The trial was sponsored by grants from the National Cancer Institute and Forest Pharmaceuticals. Dr. Laack reported no relevant financial disclosures.
BOSTON – Memantine, a drug normally prescribed for slowing cognitive decline in Alzheimer’s disease, can help to preserve cognitive function in cancer patients who have undergone whole brain irradiation, a study showed.
In a phase III trial, patients with brain metastases were randomly assigned to take 20 mg memantine (Namenda) or placebo daily for 24 weeks after whole brain radiation therapy (WBRT). The memantine cohort had a 17% relative reduction in cognitive decline compared with patients who got a placebo, Dr. Nadia N. Laack reported at the annual meeting of the American Society for Radiation Oncology.
The finding teetered on the edge of statistical significance (P = .059), however, because only one-third of patients (32%) completed the 24 weeks of drug therapy, due to death (survival was poorer than expected), disease progression, or noncompliance, said Dr. Laack. a radiation oncologist at the Mayo Clinic in Rochester, Minn.
"Overall, we feel that the weight of evidence supports our conclusion that memantine helps to preserve cognitive function after whole brain radiotherapy in patients with brain metastases," Dr. Laack said at a briefing prior to presenting the data at a plenary session.
WBRT is associated with cognitive impairment in a majority of patients who receive it, Dr. Laack said, noting that at 4 months post radiation, 60% of patients will have declines in one or more cognitive domains.
Because the mechanism of decline is similar to that seen with Alzheimer\'s and vascular dementias, and because memantine has been shown to modestly improve mild to moderate cognition in both dementia types, Dr. Laack and his colleagues hypothesized that it might protect brains exposed to therapeutic doses of radiation.
A total of 508 patients were tested at baseline and at 8, 16, 24, and 52 weeks after radiation with 37.5 Gy in 15 fractions. They were evaluated with MRI and cognitive assessment; domains of memory, processing speed, executive function, global function, self-reported cognitive function, and quality of life were evaluated. Median overall follow-up was 12.4 months.
There were no differences between the treatment groups in overall survival at a median of 6 months or in progression-free survival at 5 months.
Among 149 patients available for analysis at 24 weeks, patients who took memantine had a significantly longer time to memory decline than did those on placebo (P = .02), and had a trend toward less decline in the primary end point, the Hopkins Verbal Learning Test–Revised delayed recall instrument (median decline of 0 standard deviation, vs. –2 standard deviations for patients on placebo).
For the secondary objective of cognitive function decline/failure, defined as a change greater than reversible cognitive impairment or 2 standard deviations decline from baseline on any domain of brain function, the hazard ratio for memantine at 24 weeks was 0.784 (P = .01), indicating a significant reduction in the incidence of cognitive dysfunction.
"Although memantine was discontinued at 6 months, the effect on cognitive function was maintained for the duration of the trial, suggesting that memantine may be preventing radiation injury rather than simply treating cognitive dysfunction," Dr. Laack said.
The trial was sponsored by grants from the National Cancer Institute and Forest Pharmaceuticals. Dr. Laack reported no relevant financial disclosures.
BOSTON – Memantine, a drug normally prescribed for slowing cognitive decline in Alzheimer’s disease, can help to preserve cognitive function in cancer patients who have undergone whole brain irradiation, a study showed.
In a phase III trial, patients with brain metastases were randomly assigned to take 20 mg memantine (Namenda) or placebo daily for 24 weeks after whole brain radiation therapy (WBRT). The memantine cohort had a 17% relative reduction in cognitive decline compared with patients who got a placebo, Dr. Nadia N. Laack reported at the annual meeting of the American Society for Radiation Oncology.
The finding teetered on the edge of statistical significance (P = .059), however, because only one-third of patients (32%) completed the 24 weeks of drug therapy, due to death (survival was poorer than expected), disease progression, or noncompliance, said Dr. Laack. a radiation oncologist at the Mayo Clinic in Rochester, Minn.
"Overall, we feel that the weight of evidence supports our conclusion that memantine helps to preserve cognitive function after whole brain radiotherapy in patients with brain metastases," Dr. Laack said at a briefing prior to presenting the data at a plenary session.
WBRT is associated with cognitive impairment in a majority of patients who receive it, Dr. Laack said, noting that at 4 months post radiation, 60% of patients will have declines in one or more cognitive domains.
Because the mechanism of decline is similar to that seen with Alzheimer\'s and vascular dementias, and because memantine has been shown to modestly improve mild to moderate cognition in both dementia types, Dr. Laack and his colleagues hypothesized that it might protect brains exposed to therapeutic doses of radiation.
A total of 508 patients were tested at baseline and at 8, 16, 24, and 52 weeks after radiation with 37.5 Gy in 15 fractions. They were evaluated with MRI and cognitive assessment; domains of memory, processing speed, executive function, global function, self-reported cognitive function, and quality of life were evaluated. Median overall follow-up was 12.4 months.
There were no differences between the treatment groups in overall survival at a median of 6 months or in progression-free survival at 5 months.
Among 149 patients available for analysis at 24 weeks, patients who took memantine had a significantly longer time to memory decline than did those on placebo (P = .02), and had a trend toward less decline in the primary end point, the Hopkins Verbal Learning Test–Revised delayed recall instrument (median decline of 0 standard deviation, vs. –2 standard deviations for patients on placebo).
For the secondary objective of cognitive function decline/failure, defined as a change greater than reversible cognitive impairment or 2 standard deviations decline from baseline on any domain of brain function, the hazard ratio for memantine at 24 weeks was 0.784 (P = .01), indicating a significant reduction in the incidence of cognitive dysfunction.
"Although memantine was discontinued at 6 months, the effect on cognitive function was maintained for the duration of the trial, suggesting that memantine may be preventing radiation injury rather than simply treating cognitive dysfunction," Dr. Laack said.
The trial was sponsored by grants from the National Cancer Institute and Forest Pharmaceuticals. Dr. Laack reported no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Cancer patients with brain metastases had a 17% relative reduction in cognitive decline after whole brain radiation if they took memantine vs. placebo for 24 weeks.
Data Source: Investigators randomized 508 patients in a placebo-controlled clinical trial.
Disclosures: The trial was sponsored by grants from the National Cancer Institute and Forest Pharmaceuticals. Dr. Laack reported no relevant financial disclosures.
Can Lapatinib Prevent Brain Metastases from Breast Cancer? Data 'Inconclusive'
VIENNA – Mixed results in phase II and III clinical trials leave open the question of whether lapatinib can prevent brain metastases in women with HER2-positive breast cancer.
Lapatinib (Tykerb) did not decrease the development of brain metastases when compared with trastuzumab (Herceptin) – each added to capecitabine (Xeloda) – in the open-label phase III CEREBREL trial. The results were inconclusive, however, for the primary end point of the incidence of central nervous system events as a first sign of relapse.
Favorable findings were reported from the 45-patient phase II LANDSCAPE study. Two-thirds of patients had an objective CNS response to up-front lapatinib plus capecitabine in the single-arm study.
Investigators from both trials reported outcomes at the European Society for Medical Oncology Congress.
‘No Conclusion Can Be Made...’
In the CEREBREL trial, 251 women were treated with lapatinib in combination with capecitabine. Eight (3%) exhibited CNS progression as the first site of relapse. In comparison, 12 (5%) of 250 women given trastuzumab plus capecitabine exhibited CNS progression (P = .360).
The incidence of CNS progression at any time (7% vs. 6%, respectively) and the median time to first CNS progression (5.7 vs. 4.4 months) also did not differ significantly.
"No conclusion should be made from these results," said Dr. Xavier Pivot of the Université de Franche-Comté in Besançon, France.
Dr. Pivot noted that a very low rate of CNS events had occurred in the trial because of the stringent accrual process, undermining the conclusions that can be drawn.
Trial Excluded Asymptomatic Brain Metastases
"The CEREBREL study was a front-line study, but the problem was that asymptomatic brain metastases were being screened out of the population," Dr. Stephen Johnston, who was not involved the study, commented in an interview.
"The overall incidence of brain metastases that they found in the study was a lot lower than they were anticipating, so they were never going to meet their end point," added Dr. Johnston, a consultant medical oncologist and director of clinical research and development at the Royal Marsden and the Institute of Cancer Research in London.
CEREBREL enrolled 540 of a planned 650 women with HER2-positive metastatic breast cancer who had received prior treatment with an anthracycline or taxane but who had no CNS metastases. To ensure that no metastases were present, patients had a baseline MRI scan, with 20% of women excluded because they had asymptomatic lesions.
In total, 271 women received lapatinib (1,250 mg/day) plus capecitabine (2,000 mg/m2/day on days 1-14 every 21 days) and 269 trastuzumab (6 mg/kg every 21 days) plus capecitabine (2,500 mg/m2/day on days 1-14 every 21 days).
PFS Longer with Trastuzumab and Capecitabine
The trial results also showed that median progression-free survival (PFS) was longer in patients who received trastuzumab in combination with the chemotherapy than in those who received lapatinib (8 months vs. 6.6 months, hazard ratio 1.3, P = .021).
This effect dissipated, however, when prior treatment with trastuzumab was considered; it had been received by 62% of patients in the lapatinib-containing arm and 59% of patients in the trastuzumab-containing arm.
While there was no difference in PFS among patients who had previously been treated with trastuzumab, those who had never received the drug before the trial appeared to obtain a greater benefit.
Commenting on these data, Dr. Johnston noted that they do seem to suggest that the combination of lapatinib and capecitabine was not equivalent and was actually inferior to trastuzumab plus capecitabine.
Nevertheless, "I think the question about the effects of lapatinib on brain metastases is still relevant," he said.
"We’re doing a trial [LANTERN] of lapatinib-capecitabine versus continuing the trastuzumab and adding in capecitabine, to see if switching the HER2-targeting keeps the brain disease under control for longer," Dr. Johnston explained. "This is where lapatinib may still have a role."
LANDSCAPE Results Favorable
The primary hypothesis of the phase II LANDSCAPE study was that up-front treatment with lapatinib might help prevent brain metastasis in HER2-positive metastatic breast cancer and delay the need for whole-brain radiation and its associated neurotoxicity, said study investigator Dr. Thomas Bachelot, on behalf of the Unicancer Federation Française group.
Dr. Bachelot of INSERM in Lyon said the response and overall survival results compared favorably with published data for whole-brain radiotherapy (WBRT).
Two thirds (66%) of patients treated with lapatinib and capecitabine exhibited a CNS objective response: 46% achieved a reduction in brain metastases of 50%-80%, and 20% exhibited a reduction in brain metastases of 80% or more. The median time to progression was 5.5 months, and the median time to WBRT was 7.8 months. Median overall survival was 17 months.
"This strategy could help delay whole-brain radiotherapy and its associated [neurological] toxicity," Dr. Bachelot concluded, noting that the up-front use of lapatinib and capecitabine warrants further evaluation.
The first analysis of the LANDSCAPE trial was presented at the American Society of Clinical Oncology (ASCO) in 2011.
Both the CEREBREL and LANDSCAPE studies were supported by funding from GlaxoSmithKline. All authors have received research support or consultancy fees from GlaxoSmithKline and Roche. Dr. Bachelot and Dr. Johnston have also received consultancy fees from Novartis.
VIENNA – Mixed results in phase II and III clinical trials leave open the question of whether lapatinib can prevent brain metastases in women with HER2-positive breast cancer.
Lapatinib (Tykerb) did not decrease the development of brain metastases when compared with trastuzumab (Herceptin) – each added to capecitabine (Xeloda) – in the open-label phase III CEREBREL trial. The results were inconclusive, however, for the primary end point of the incidence of central nervous system events as a first sign of relapse.
Favorable findings were reported from the 45-patient phase II LANDSCAPE study. Two-thirds of patients had an objective CNS response to up-front lapatinib plus capecitabine in the single-arm study.
Investigators from both trials reported outcomes at the European Society for Medical Oncology Congress.
‘No Conclusion Can Be Made...’
In the CEREBREL trial, 251 women were treated with lapatinib in combination with capecitabine. Eight (3%) exhibited CNS progression as the first site of relapse. In comparison, 12 (5%) of 250 women given trastuzumab plus capecitabine exhibited CNS progression (P = .360).
The incidence of CNS progression at any time (7% vs. 6%, respectively) and the median time to first CNS progression (5.7 vs. 4.4 months) also did not differ significantly.
"No conclusion should be made from these results," said Dr. Xavier Pivot of the Université de Franche-Comté in Besançon, France.
Dr. Pivot noted that a very low rate of CNS events had occurred in the trial because of the stringent accrual process, undermining the conclusions that can be drawn.
Trial Excluded Asymptomatic Brain Metastases
"The CEREBREL study was a front-line study, but the problem was that asymptomatic brain metastases were being screened out of the population," Dr. Stephen Johnston, who was not involved the study, commented in an interview.
"The overall incidence of brain metastases that they found in the study was a lot lower than they were anticipating, so they were never going to meet their end point," added Dr. Johnston, a consultant medical oncologist and director of clinical research and development at the Royal Marsden and the Institute of Cancer Research in London.
CEREBREL enrolled 540 of a planned 650 women with HER2-positive metastatic breast cancer who had received prior treatment with an anthracycline or taxane but who had no CNS metastases. To ensure that no metastases were present, patients had a baseline MRI scan, with 20% of women excluded because they had asymptomatic lesions.
In total, 271 women received lapatinib (1,250 mg/day) plus capecitabine (2,000 mg/m2/day on days 1-14 every 21 days) and 269 trastuzumab (6 mg/kg every 21 days) plus capecitabine (2,500 mg/m2/day on days 1-14 every 21 days).
PFS Longer with Trastuzumab and Capecitabine
The trial results also showed that median progression-free survival (PFS) was longer in patients who received trastuzumab in combination with the chemotherapy than in those who received lapatinib (8 months vs. 6.6 months, hazard ratio 1.3, P = .021).
This effect dissipated, however, when prior treatment with trastuzumab was considered; it had been received by 62% of patients in the lapatinib-containing arm and 59% of patients in the trastuzumab-containing arm.
While there was no difference in PFS among patients who had previously been treated with trastuzumab, those who had never received the drug before the trial appeared to obtain a greater benefit.
Commenting on these data, Dr. Johnston noted that they do seem to suggest that the combination of lapatinib and capecitabine was not equivalent and was actually inferior to trastuzumab plus capecitabine.
Nevertheless, "I think the question about the effects of lapatinib on brain metastases is still relevant," he said.
"We’re doing a trial [LANTERN] of lapatinib-capecitabine versus continuing the trastuzumab and adding in capecitabine, to see if switching the HER2-targeting keeps the brain disease under control for longer," Dr. Johnston explained. "This is where lapatinib may still have a role."
LANDSCAPE Results Favorable
The primary hypothesis of the phase II LANDSCAPE study was that up-front treatment with lapatinib might help prevent brain metastasis in HER2-positive metastatic breast cancer and delay the need for whole-brain radiation and its associated neurotoxicity, said study investigator Dr. Thomas Bachelot, on behalf of the Unicancer Federation Française group.
Dr. Bachelot of INSERM in Lyon said the response and overall survival results compared favorably with published data for whole-brain radiotherapy (WBRT).
Two thirds (66%) of patients treated with lapatinib and capecitabine exhibited a CNS objective response: 46% achieved a reduction in brain metastases of 50%-80%, and 20% exhibited a reduction in brain metastases of 80% or more. The median time to progression was 5.5 months, and the median time to WBRT was 7.8 months. Median overall survival was 17 months.
"This strategy could help delay whole-brain radiotherapy and its associated [neurological] toxicity," Dr. Bachelot concluded, noting that the up-front use of lapatinib and capecitabine warrants further evaluation.
The first analysis of the LANDSCAPE trial was presented at the American Society of Clinical Oncology (ASCO) in 2011.
Both the CEREBREL and LANDSCAPE studies were supported by funding from GlaxoSmithKline. All authors have received research support or consultancy fees from GlaxoSmithKline and Roche. Dr. Bachelot and Dr. Johnston have also received consultancy fees from Novartis.
VIENNA – Mixed results in phase II and III clinical trials leave open the question of whether lapatinib can prevent brain metastases in women with HER2-positive breast cancer.
Lapatinib (Tykerb) did not decrease the development of brain metastases when compared with trastuzumab (Herceptin) – each added to capecitabine (Xeloda) – in the open-label phase III CEREBREL trial. The results were inconclusive, however, for the primary end point of the incidence of central nervous system events as a first sign of relapse.
Favorable findings were reported from the 45-patient phase II LANDSCAPE study. Two-thirds of patients had an objective CNS response to up-front lapatinib plus capecitabine in the single-arm study.
Investigators from both trials reported outcomes at the European Society for Medical Oncology Congress.
‘No Conclusion Can Be Made...’
In the CEREBREL trial, 251 women were treated with lapatinib in combination with capecitabine. Eight (3%) exhibited CNS progression as the first site of relapse. In comparison, 12 (5%) of 250 women given trastuzumab plus capecitabine exhibited CNS progression (P = .360).
The incidence of CNS progression at any time (7% vs. 6%, respectively) and the median time to first CNS progression (5.7 vs. 4.4 months) also did not differ significantly.
"No conclusion should be made from these results," said Dr. Xavier Pivot of the Université de Franche-Comté in Besançon, France.
Dr. Pivot noted that a very low rate of CNS events had occurred in the trial because of the stringent accrual process, undermining the conclusions that can be drawn.
Trial Excluded Asymptomatic Brain Metastases
"The CEREBREL study was a front-line study, but the problem was that asymptomatic brain metastases were being screened out of the population," Dr. Stephen Johnston, who was not involved the study, commented in an interview.
"The overall incidence of brain metastases that they found in the study was a lot lower than they were anticipating, so they were never going to meet their end point," added Dr. Johnston, a consultant medical oncologist and director of clinical research and development at the Royal Marsden and the Institute of Cancer Research in London.
CEREBREL enrolled 540 of a planned 650 women with HER2-positive metastatic breast cancer who had received prior treatment with an anthracycline or taxane but who had no CNS metastases. To ensure that no metastases were present, patients had a baseline MRI scan, with 20% of women excluded because they had asymptomatic lesions.
In total, 271 women received lapatinib (1,250 mg/day) plus capecitabine (2,000 mg/m2/day on days 1-14 every 21 days) and 269 trastuzumab (6 mg/kg every 21 days) plus capecitabine (2,500 mg/m2/day on days 1-14 every 21 days).
PFS Longer with Trastuzumab and Capecitabine
The trial results also showed that median progression-free survival (PFS) was longer in patients who received trastuzumab in combination with the chemotherapy than in those who received lapatinib (8 months vs. 6.6 months, hazard ratio 1.3, P = .021).
This effect dissipated, however, when prior treatment with trastuzumab was considered; it had been received by 62% of patients in the lapatinib-containing arm and 59% of patients in the trastuzumab-containing arm.
While there was no difference in PFS among patients who had previously been treated with trastuzumab, those who had never received the drug before the trial appeared to obtain a greater benefit.
Commenting on these data, Dr. Johnston noted that they do seem to suggest that the combination of lapatinib and capecitabine was not equivalent and was actually inferior to trastuzumab plus capecitabine.
Nevertheless, "I think the question about the effects of lapatinib on brain metastases is still relevant," he said.
"We’re doing a trial [LANTERN] of lapatinib-capecitabine versus continuing the trastuzumab and adding in capecitabine, to see if switching the HER2-targeting keeps the brain disease under control for longer," Dr. Johnston explained. "This is where lapatinib may still have a role."
LANDSCAPE Results Favorable
The primary hypothesis of the phase II LANDSCAPE study was that up-front treatment with lapatinib might help prevent brain metastasis in HER2-positive metastatic breast cancer and delay the need for whole-brain radiation and its associated neurotoxicity, said study investigator Dr. Thomas Bachelot, on behalf of the Unicancer Federation Française group.
Dr. Bachelot of INSERM in Lyon said the response and overall survival results compared favorably with published data for whole-brain radiotherapy (WBRT).
Two thirds (66%) of patients treated with lapatinib and capecitabine exhibited a CNS objective response: 46% achieved a reduction in brain metastases of 50%-80%, and 20% exhibited a reduction in brain metastases of 80% or more. The median time to progression was 5.5 months, and the median time to WBRT was 7.8 months. Median overall survival was 17 months.
"This strategy could help delay whole-brain radiotherapy and its associated [neurological] toxicity," Dr. Bachelot concluded, noting that the up-front use of lapatinib and capecitabine warrants further evaluation.
The first analysis of the LANDSCAPE trial was presented at the American Society of Clinical Oncology (ASCO) in 2011.
Both the CEREBREL and LANDSCAPE studies were supported by funding from GlaxoSmithKline. All authors have received research support or consultancy fees from GlaxoSmithKline and Roche. Dr. Bachelot and Dr. Johnston have also received consultancy fees from Novartis.
AT THE EUROPEAN SOCIETY FOR MEDICAL ONCOLOGY CONGRESS
Major Findings: The primary end point of CNS as first site of relapse was no different comparing lapatinib-capecitabine (3%) vs. trastuzumab-capecitabine (5%) in the CEREBREL trial. The LANDSCAPE study showed a CNS objective response in 66% of patients treated with up-front lapatinib plus capecitabine.
Data Source: CEREBREL was an open-label phase III study, and LANDSCAPE was a phase II study. Both enrolled women with metastatic breast cancer.
Disclosures: Both studies were supported by funding from GlaxoSmithKline. All authors have received research support or consultancy fees from GlaxoSmithKline and Roche. Dr. Bachelot and Dr. Johnston have also received consultancy fees from Novartis.
Acetyl-l-Carnitine Yields Mixed Results for Chemo-Induced Neuropathy
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF CLINICAL ONCOLOGY
Major Finding: Patients taking ALC for prevention were more likely to have a greater than 5-point worsening of FACT-NTX score (38% vs. 28%), whereas patients taking ALC for treatment were more likely to have an improvement of at least one grade in neuropathy (51% vs. 24%).
Data Source: Investigators presented separate, randomized, placebo-controlled phase III trials among 410 women receiving adjuvant taxane chemotherapy for breast cancer and 239 patients with cancer and chemotherapy-induced peripheral neuropathy.
Disclosures: Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
Labs Find Evidence of Cancer Stem Cells
In an era of targeted cancer therapies, laboratory scientists working with mice may have found the ultimate target – a reservoir of stem cells that drive cancers to grow and metastasize.
Separate reports in the journals Science and Nature document the presence of cancer stem cells in intestinal adenomas (Science 2012 Aug. 1 [doi:10.1126/science.1224676]), squamous skin cancer, (Nature 2012 Aug. 1 [doi:10.1038/nature11344]), and glioblastoma multiforme (Nature 2012 Aug. 1 [doi:10.1038/nature11287]).
In the last study, mice with these highly lethal brain tumors were given temozolomide (Temodar), an approved treatment in humans, along with ganciclovir, an antiviral. Despite a transient therapeutic response to chemotherapy, the cancers continued to grow, driven by "a relatively quiescent subset of endogenous glioma cells, with properties similar to those proposed for cancer stem cells," the authors wrote.
Whether these reports will resolve controversy over the existence of stem cells or lead to clinically meaningful treatments remains to be seen. There is no doubt, however, that they will lead to further investigation.
In an era of targeted cancer therapies, laboratory scientists working with mice may have found the ultimate target – a reservoir of stem cells that drive cancers to grow and metastasize.
Separate reports in the journals Science and Nature document the presence of cancer stem cells in intestinal adenomas (Science 2012 Aug. 1 [doi:10.1126/science.1224676]), squamous skin cancer, (Nature 2012 Aug. 1 [doi:10.1038/nature11344]), and glioblastoma multiforme (Nature 2012 Aug. 1 [doi:10.1038/nature11287]).
In the last study, mice with these highly lethal brain tumors were given temozolomide (Temodar), an approved treatment in humans, along with ganciclovir, an antiviral. Despite a transient therapeutic response to chemotherapy, the cancers continued to grow, driven by "a relatively quiescent subset of endogenous glioma cells, with properties similar to those proposed for cancer stem cells," the authors wrote.
Whether these reports will resolve controversy over the existence of stem cells or lead to clinically meaningful treatments remains to be seen. There is no doubt, however, that they will lead to further investigation.
In an era of targeted cancer therapies, laboratory scientists working with mice may have found the ultimate target – a reservoir of stem cells that drive cancers to grow and metastasize.
Separate reports in the journals Science and Nature document the presence of cancer stem cells in intestinal adenomas (Science 2012 Aug. 1 [doi:10.1126/science.1224676]), squamous skin cancer, (Nature 2012 Aug. 1 [doi:10.1038/nature11344]), and glioblastoma multiforme (Nature 2012 Aug. 1 [doi:10.1038/nature11287]).
In the last study, mice with these highly lethal brain tumors were given temozolomide (Temodar), an approved treatment in humans, along with ganciclovir, an antiviral. Despite a transient therapeutic response to chemotherapy, the cancers continued to grow, driven by "a relatively quiescent subset of endogenous glioma cells, with properties similar to those proposed for cancer stem cells," the authors wrote.
Whether these reports will resolve controversy over the existence of stem cells or lead to clinically meaningful treatments remains to be seen. There is no doubt, however, that they will lead to further investigation.
Treating Brain Tumors With Bacteria Gets Neurosurgeons Banned
Are a few animal studies and a handful of human case reports enough to let physicians skirt institutional review boards?
Two neurosurgeons in California did just that when they used Enterobacter aerogenes to infect the surgical wounds of three terminally ill glioblastoma patients. Two of the patients died from the infections.
Dr. J. Paul Muizelaar and Dr. Rudolph J. Schrot of the University of California, Davis, said their attempt to stimulate their patients’ immune response was not research but "a one-time procedure" – exempt from review, according to a report in the Sacramento Bee.
Now both are banned from human research projects and the institutional review board is the subject of its own investigation.
For an account of the scientific thinking behind the deployment of bacteria in these patients and of ongoing efforts to develop immunotherapies against cancer, see the journal Nature (2012 July 27 [doi:10.1038/nature.2012.11080]).
Are a few animal studies and a handful of human case reports enough to let physicians skirt institutional review boards?
Two neurosurgeons in California did just that when they used Enterobacter aerogenes to infect the surgical wounds of three terminally ill glioblastoma patients. Two of the patients died from the infections.
Dr. J. Paul Muizelaar and Dr. Rudolph J. Schrot of the University of California, Davis, said their attempt to stimulate their patients’ immune response was not research but "a one-time procedure" – exempt from review, according to a report in the Sacramento Bee.
Now both are banned from human research projects and the institutional review board is the subject of its own investigation.
For an account of the scientific thinking behind the deployment of bacteria in these patients and of ongoing efforts to develop immunotherapies against cancer, see the journal Nature (2012 July 27 [doi:10.1038/nature.2012.11080]).
Are a few animal studies and a handful of human case reports enough to let physicians skirt institutional review boards?
Two neurosurgeons in California did just that when they used Enterobacter aerogenes to infect the surgical wounds of three terminally ill glioblastoma patients. Two of the patients died from the infections.
Dr. J. Paul Muizelaar and Dr. Rudolph J. Schrot of the University of California, Davis, said their attempt to stimulate their patients’ immune response was not research but "a one-time procedure" – exempt from review, according to a report in the Sacramento Bee.
Now both are banned from human research projects and the institutional review board is the subject of its own investigation.
For an account of the scientific thinking behind the deployment of bacteria in these patients and of ongoing efforts to develop immunotherapies against cancer, see the journal Nature (2012 July 27 [doi:10.1038/nature.2012.11080]).
Rare Brainstem Glioma Doesn't Stop Former Marine
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.