User login
‘Trigger zone’ resection ups seizure-free odds in temporal lobe epilepsy
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
FROM JAMA NEUROLOGY
Minimally invasive ICH lysis safely helps when clot adequately shrinks
HONOLULU – A minimally invasive approach to lysing an intracerebral hemorrhage clot was safe but failed to produce a statistically significant improvement in long-term functional outcome when compared with usual medical management in a phase 3 randomized trial of 499 patients. However, the results also showed that when the procedure met its acute goal of cutting residual clot to a volume of 15 mL or less, it significantly boosted the percentage of patients with a modified Rankin Scale score of 0-3 when assessed a year after treatment, Daniel F. Hanley Jr., MD, said at the International Stroke Conference, sponsored by the American Heart Association.
“Improved function and increased survival was produced by surgical [clot] reduction to 15 mL or less,” said Dr. Hanley, professor of neurology at Johns Hopkins University, Baltimore, and one of the organizers of the MISTIE III trial.
When assessed by another measure, treated patients showed significant, long-term functional improvement compared with controls when their clot burden dropped by at least 70% following the lytic procedure.
“This is the first description of specific thresholds of hematoma evacuation that impact functional outcomes in intracerebral hemorrhage surgery trials,” said Issam A. Awad, MD, professor of surgery and director of neurovascular surgery at the University of Chicago and coprincipal investigator of the trial.
The problem in the trial was that the surgeons who performed the interventions did not treat many patients aggressively enough to reach these thresholds. They achieved the prespecified goal of residual clot of 15 mL or less in 59% of patients, Dr. Hanley reported, even though the study protocol called for serial infusions of 1 mg of tissue plasminogen activator (Alteplase) into the clot via a placed catheter as many as nine times, administered at 8 hour intervals, with treatment to continue until patients reached the goal residual volume or until they had received all nine doses. In actual practice during the study, operators administered a median of four lytic doses.
“We showed that this goal was important, but not all sites embraced the goal,” Dr. Hanley said. Even though the participating clinicians had a specific interest in intracerebral hemorrhage patients and in this procedure, several nonetheless “had a poor understanding of the goal,” he said in an interview. He attributed the less-than-aggressive approach many operators took to the safety concern that further doses of the lytic drug could trigger recurrent hemorrhage.
“We showed that the goal was important. I think they will embrace the [hematoma evacuation] goal when they see these data,” Dr. Hanley predicted.
An as-treated analysis of the data that focused on the 145 of 246 patients who were treated with minimally invasive lysis and reached the target residual volume and who were then functionally assessed a year later, showed that the rate of patients with a modified Rankin Scale score of 0-3 was 53%, compared with 42% among the controls, an 11% difference.
This shows “a large treatment effect. This is a big, transformative treatment,” Dr. Hanley said. “Our data clearly show that more than half the patients had a positive outcome when their surgeons were more aggressive about clot removal.” He cautioned that the trial was not just about the volume of clot removed but was also about doing it in a gentle way, with a minimum of tissue trauma. Other approaches to reducing hematoma volume may be faster or more complete but they cannot now match the record of safety and efficacy documented in MISTIE III for minimally invasive clot lysis, Dr. Hanley noted.
MISTIE III (Minimally Invasive Surgery Plus Rt-PA for ICH Evacuation Phase III) enrolled patients at 78 centers in the United States and several other countries during 2013-2017. Patients had to enroll 12-72 hours after onset and present with a hematoma volume of at least 30 mL. Participating neurosurgeons used image-guided neuronavigation to place a 4- to 6-mm cannula through the clot, ideally straight through the hematoma’s long axis and with the tip placed within the largest clot segment. Among the 110 surgeons who performed this procedure during the study, 88% had never done it before, and operator and site experience linked with better performance. No surgeon who had already performed four minimally invasive lytic cases, and no center that had already performed seven cases, had a subsequent patient with a residual volume that exceeded 30 mL, Dr. Awad said. The surgical experience during the trial showed that catheter repositioning and using a second catheter were both safe ways to maximize evacuation of the hematoma, he added.
The trial’s primary endpoint, the rate of patients with a modified Rankin Scale score of 0-3 at 1 year after treatment in a modified intention-to-treat analysis that included all patients regardless of the amount of hematoma evacuation they received, showed a 45% rate among the patients who underwent minimally invasive lysis and a 41% rate among those in the control arm, a difference that was not statistically significant. Safety assessments showed that patients treated with the investigational approach had significantly lower mortality 7 days after treatment: 0.8% compared with 4.0%. By 1 year after treatment, mortality was cut by one-third in the minimally invasive patients, compared with the control patients, also a statistically significant difference. The rates of symptomatic bleeds and brain infections were similar in the two treatment groups, Dr. Hanley reported. Concurrently with his talk at the conference, a paper with the primary study results appeared online (Lancet. 2019 Feb 7. doi: 10.1016/S0140-6736[19]30195-3).
MISTIE III was supported by the National Institute of Neurological Disorders and Stroke. The trial received no commercial support aside from free tissue plasminogen activator (Alteplase) supplied by Genentech. Dr. Hanley has been a consultant to BrainScope, Neurotrope, Portola, and Op2Lysis, and he has served as an expert witness on behalf of Medtronic. Dr. Awad had no disclosures.
SOURCE: Hanley DF et al. ISC 2019, Abstract LB4; Awad IS et al. ISC 2019, Abstract LB5.
The MISTIE III results showed that this approach to clot lysis is safe and feasible for surgeons to perform even if they have had limited experience with the procedure. I think that based on these findings, minimally-invasive clot lysis will become widely adopted. It’s pretty simple to perform in most patients. At my center in Houston, we already use it on a routine basis in patients like those enrolled in MISTIE III.
Some people may focus on the neutral primary endpoint result from the MISTIE III trial, but the study made two very important findings. First, the results showed that we have improved medical management of patients who have an intracerebral hemorrhage. The 1-year functional outcomes of patients in the control group of the study who had a 41% rate of scoring 0-3 on the modified Rankin Scale after 1 year was much better than we have seen in these patients in the past. Second, the results gave a clear signal that the more clot an operator can lyse to get the residual clot to 15 mL or less, the better patients do. Faster clot lysis might also be important.
It’s hard to call the minimally-invasive approach used in MISTIE III the new standard-of-care approach for these patients given the neutral primary endpoint of the study. On the other hand, if you have a treatment that poses little risk to patients and that you know could benefit them if it succeeds in minimizing residual clot volume, then it makes sense to try it. It’s a low-risk treatment with reasonable potential for benefit. Its demonstrated safety is very important.
Louise D. McCullough, MD, PhD , is a professor of neurology and chair of neurology at the University of Texas, Houston. She had no disclosures. She made these comments in an interview.
The MISTIE III results showed that this approach to clot lysis is safe and feasible for surgeons to perform even if they have had limited experience with the procedure. I think that based on these findings, minimally-invasive clot lysis will become widely adopted. It’s pretty simple to perform in most patients. At my center in Houston, we already use it on a routine basis in patients like those enrolled in MISTIE III.
Some people may focus on the neutral primary endpoint result from the MISTIE III trial, but the study made two very important findings. First, the results showed that we have improved medical management of patients who have an intracerebral hemorrhage. The 1-year functional outcomes of patients in the control group of the study who had a 41% rate of scoring 0-3 on the modified Rankin Scale after 1 year was much better than we have seen in these patients in the past. Second, the results gave a clear signal that the more clot an operator can lyse to get the residual clot to 15 mL or less, the better patients do. Faster clot lysis might also be important.
It’s hard to call the minimally-invasive approach used in MISTIE III the new standard-of-care approach for these patients given the neutral primary endpoint of the study. On the other hand, if you have a treatment that poses little risk to patients and that you know could benefit them if it succeeds in minimizing residual clot volume, then it makes sense to try it. It’s a low-risk treatment with reasonable potential for benefit. Its demonstrated safety is very important.
Louise D. McCullough, MD, PhD , is a professor of neurology and chair of neurology at the University of Texas, Houston. She had no disclosures. She made these comments in an interview.
The MISTIE III results showed that this approach to clot lysis is safe and feasible for surgeons to perform even if they have had limited experience with the procedure. I think that based on these findings, minimally-invasive clot lysis will become widely adopted. It’s pretty simple to perform in most patients. At my center in Houston, we already use it on a routine basis in patients like those enrolled in MISTIE III.
Some people may focus on the neutral primary endpoint result from the MISTIE III trial, but the study made two very important findings. First, the results showed that we have improved medical management of patients who have an intracerebral hemorrhage. The 1-year functional outcomes of patients in the control group of the study who had a 41% rate of scoring 0-3 on the modified Rankin Scale after 1 year was much better than we have seen in these patients in the past. Second, the results gave a clear signal that the more clot an operator can lyse to get the residual clot to 15 mL or less, the better patients do. Faster clot lysis might also be important.
It’s hard to call the minimally-invasive approach used in MISTIE III the new standard-of-care approach for these patients given the neutral primary endpoint of the study. On the other hand, if you have a treatment that poses little risk to patients and that you know could benefit them if it succeeds in minimizing residual clot volume, then it makes sense to try it. It’s a low-risk treatment with reasonable potential for benefit. Its demonstrated safety is very important.
Louise D. McCullough, MD, PhD , is a professor of neurology and chair of neurology at the University of Texas, Houston. She had no disclosures. She made these comments in an interview.
HONOLULU – A minimally invasive approach to lysing an intracerebral hemorrhage clot was safe but failed to produce a statistically significant improvement in long-term functional outcome when compared with usual medical management in a phase 3 randomized trial of 499 patients. However, the results also showed that when the procedure met its acute goal of cutting residual clot to a volume of 15 mL or less, it significantly boosted the percentage of patients with a modified Rankin Scale score of 0-3 when assessed a year after treatment, Daniel F. Hanley Jr., MD, said at the International Stroke Conference, sponsored by the American Heart Association.
“Improved function and increased survival was produced by surgical [clot] reduction to 15 mL or less,” said Dr. Hanley, professor of neurology at Johns Hopkins University, Baltimore, and one of the organizers of the MISTIE III trial.
When assessed by another measure, treated patients showed significant, long-term functional improvement compared with controls when their clot burden dropped by at least 70% following the lytic procedure.
“This is the first description of specific thresholds of hematoma evacuation that impact functional outcomes in intracerebral hemorrhage surgery trials,” said Issam A. Awad, MD, professor of surgery and director of neurovascular surgery at the University of Chicago and coprincipal investigator of the trial.
The problem in the trial was that the surgeons who performed the interventions did not treat many patients aggressively enough to reach these thresholds. They achieved the prespecified goal of residual clot of 15 mL or less in 59% of patients, Dr. Hanley reported, even though the study protocol called for serial infusions of 1 mg of tissue plasminogen activator (Alteplase) into the clot via a placed catheter as many as nine times, administered at 8 hour intervals, with treatment to continue until patients reached the goal residual volume or until they had received all nine doses. In actual practice during the study, operators administered a median of four lytic doses.
“We showed that this goal was important, but not all sites embraced the goal,” Dr. Hanley said. Even though the participating clinicians had a specific interest in intracerebral hemorrhage patients and in this procedure, several nonetheless “had a poor understanding of the goal,” he said in an interview. He attributed the less-than-aggressive approach many operators took to the safety concern that further doses of the lytic drug could trigger recurrent hemorrhage.
“We showed that the goal was important. I think they will embrace the [hematoma evacuation] goal when they see these data,” Dr. Hanley predicted.
An as-treated analysis of the data that focused on the 145 of 246 patients who were treated with minimally invasive lysis and reached the target residual volume and who were then functionally assessed a year later, showed that the rate of patients with a modified Rankin Scale score of 0-3 was 53%, compared with 42% among the controls, an 11% difference.
This shows “a large treatment effect. This is a big, transformative treatment,” Dr. Hanley said. “Our data clearly show that more than half the patients had a positive outcome when their surgeons were more aggressive about clot removal.” He cautioned that the trial was not just about the volume of clot removed but was also about doing it in a gentle way, with a minimum of tissue trauma. Other approaches to reducing hematoma volume may be faster or more complete but they cannot now match the record of safety and efficacy documented in MISTIE III for minimally invasive clot lysis, Dr. Hanley noted.
MISTIE III (Minimally Invasive Surgery Plus Rt-PA for ICH Evacuation Phase III) enrolled patients at 78 centers in the United States and several other countries during 2013-2017. Patients had to enroll 12-72 hours after onset and present with a hematoma volume of at least 30 mL. Participating neurosurgeons used image-guided neuronavigation to place a 4- to 6-mm cannula through the clot, ideally straight through the hematoma’s long axis and with the tip placed within the largest clot segment. Among the 110 surgeons who performed this procedure during the study, 88% had never done it before, and operator and site experience linked with better performance. No surgeon who had already performed four minimally invasive lytic cases, and no center that had already performed seven cases, had a subsequent patient with a residual volume that exceeded 30 mL, Dr. Awad said. The surgical experience during the trial showed that catheter repositioning and using a second catheter were both safe ways to maximize evacuation of the hematoma, he added.
The trial’s primary endpoint, the rate of patients with a modified Rankin Scale score of 0-3 at 1 year after treatment in a modified intention-to-treat analysis that included all patients regardless of the amount of hematoma evacuation they received, showed a 45% rate among the patients who underwent minimally invasive lysis and a 41% rate among those in the control arm, a difference that was not statistically significant. Safety assessments showed that patients treated with the investigational approach had significantly lower mortality 7 days after treatment: 0.8% compared with 4.0%. By 1 year after treatment, mortality was cut by one-third in the minimally invasive patients, compared with the control patients, also a statistically significant difference. The rates of symptomatic bleeds and brain infections were similar in the two treatment groups, Dr. Hanley reported. Concurrently with his talk at the conference, a paper with the primary study results appeared online (Lancet. 2019 Feb 7. doi: 10.1016/S0140-6736[19]30195-3).
MISTIE III was supported by the National Institute of Neurological Disorders and Stroke. The trial received no commercial support aside from free tissue plasminogen activator (Alteplase) supplied by Genentech. Dr. Hanley has been a consultant to BrainScope, Neurotrope, Portola, and Op2Lysis, and he has served as an expert witness on behalf of Medtronic. Dr. Awad had no disclosures.
SOURCE: Hanley DF et al. ISC 2019, Abstract LB4; Awad IS et al. ISC 2019, Abstract LB5.
HONOLULU – A minimally invasive approach to lysing an intracerebral hemorrhage clot was safe but failed to produce a statistically significant improvement in long-term functional outcome when compared with usual medical management in a phase 3 randomized trial of 499 patients. However, the results also showed that when the procedure met its acute goal of cutting residual clot to a volume of 15 mL or less, it significantly boosted the percentage of patients with a modified Rankin Scale score of 0-3 when assessed a year after treatment, Daniel F. Hanley Jr., MD, said at the International Stroke Conference, sponsored by the American Heart Association.
“Improved function and increased survival was produced by surgical [clot] reduction to 15 mL or less,” said Dr. Hanley, professor of neurology at Johns Hopkins University, Baltimore, and one of the organizers of the MISTIE III trial.
When assessed by another measure, treated patients showed significant, long-term functional improvement compared with controls when their clot burden dropped by at least 70% following the lytic procedure.
“This is the first description of specific thresholds of hematoma evacuation that impact functional outcomes in intracerebral hemorrhage surgery trials,” said Issam A. Awad, MD, professor of surgery and director of neurovascular surgery at the University of Chicago and coprincipal investigator of the trial.
The problem in the trial was that the surgeons who performed the interventions did not treat many patients aggressively enough to reach these thresholds. They achieved the prespecified goal of residual clot of 15 mL or less in 59% of patients, Dr. Hanley reported, even though the study protocol called for serial infusions of 1 mg of tissue plasminogen activator (Alteplase) into the clot via a placed catheter as many as nine times, administered at 8 hour intervals, with treatment to continue until patients reached the goal residual volume or until they had received all nine doses. In actual practice during the study, operators administered a median of four lytic doses.
“We showed that this goal was important, but not all sites embraced the goal,” Dr. Hanley said. Even though the participating clinicians had a specific interest in intracerebral hemorrhage patients and in this procedure, several nonetheless “had a poor understanding of the goal,” he said in an interview. He attributed the less-than-aggressive approach many operators took to the safety concern that further doses of the lytic drug could trigger recurrent hemorrhage.
“We showed that the goal was important. I think they will embrace the [hematoma evacuation] goal when they see these data,” Dr. Hanley predicted.
An as-treated analysis of the data that focused on the 145 of 246 patients who were treated with minimally invasive lysis and reached the target residual volume and who were then functionally assessed a year later, showed that the rate of patients with a modified Rankin Scale score of 0-3 was 53%, compared with 42% among the controls, an 11% difference.
This shows “a large treatment effect. This is a big, transformative treatment,” Dr. Hanley said. “Our data clearly show that more than half the patients had a positive outcome when their surgeons were more aggressive about clot removal.” He cautioned that the trial was not just about the volume of clot removed but was also about doing it in a gentle way, with a minimum of tissue trauma. Other approaches to reducing hematoma volume may be faster or more complete but they cannot now match the record of safety and efficacy documented in MISTIE III for minimally invasive clot lysis, Dr. Hanley noted.
MISTIE III (Minimally Invasive Surgery Plus Rt-PA for ICH Evacuation Phase III) enrolled patients at 78 centers in the United States and several other countries during 2013-2017. Patients had to enroll 12-72 hours after onset and present with a hematoma volume of at least 30 mL. Participating neurosurgeons used image-guided neuronavigation to place a 4- to 6-mm cannula through the clot, ideally straight through the hematoma’s long axis and with the tip placed within the largest clot segment. Among the 110 surgeons who performed this procedure during the study, 88% had never done it before, and operator and site experience linked with better performance. No surgeon who had already performed four minimally invasive lytic cases, and no center that had already performed seven cases, had a subsequent patient with a residual volume that exceeded 30 mL, Dr. Awad said. The surgical experience during the trial showed that catheter repositioning and using a second catheter were both safe ways to maximize evacuation of the hematoma, he added.
The trial’s primary endpoint, the rate of patients with a modified Rankin Scale score of 0-3 at 1 year after treatment in a modified intention-to-treat analysis that included all patients regardless of the amount of hematoma evacuation they received, showed a 45% rate among the patients who underwent minimally invasive lysis and a 41% rate among those in the control arm, a difference that was not statistically significant. Safety assessments showed that patients treated with the investigational approach had significantly lower mortality 7 days after treatment: 0.8% compared with 4.0%. By 1 year after treatment, mortality was cut by one-third in the minimally invasive patients, compared with the control patients, also a statistically significant difference. The rates of symptomatic bleeds and brain infections were similar in the two treatment groups, Dr. Hanley reported. Concurrently with his talk at the conference, a paper with the primary study results appeared online (Lancet. 2019 Feb 7. doi: 10.1016/S0140-6736[19]30195-3).
MISTIE III was supported by the National Institute of Neurological Disorders and Stroke. The trial received no commercial support aside from free tissue plasminogen activator (Alteplase) supplied by Genentech. Dr. Hanley has been a consultant to BrainScope, Neurotrope, Portola, and Op2Lysis, and he has served as an expert witness on behalf of Medtronic. Dr. Awad had no disclosures.
SOURCE: Hanley DF et al. ISC 2019, Abstract LB4; Awad IS et al. ISC 2019, Abstract LB5.
REPORTING FROM ISC 2019
Key clinical point: Minimally-invasive intracerebral clot lysis was safe and often effective when the residual clot shrank to 15 mL or less.
Major finding: One year after entry, 45% of MISTIE-treated patients and 41% of controls had a modified Rankin Scale score of 0-3.
Study details: MISTIE III, a multicenter, international, randomized trial of 499 patients.
Disclosures: MISTIE III was supported by the National Institute of Neurological Disorders and Stroke. The trial received no commercial support aside from free tissue plasminogen activator (Alteplase) supplied by Genentech. Dr. Hanley has been a consultant to BrainScope, Neurotrope, Portola, and Op2Lysis, and he has served as an expert witness on behalf of Medtronic. Dr. Awad had no disclosures.
Source: Hanley DF et al. ISC 2019, Abstract LB4; Awad IS et al. ISC 2019, Abstract LB5.
Functional MRI detects consciousness after brain damage
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
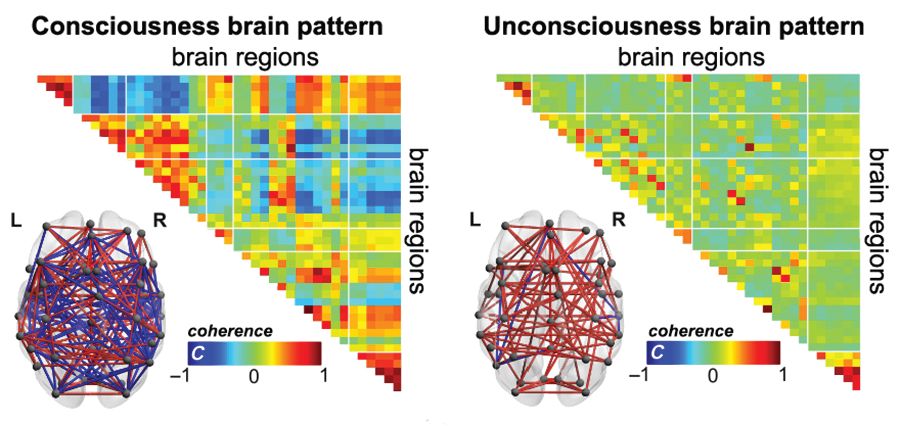
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
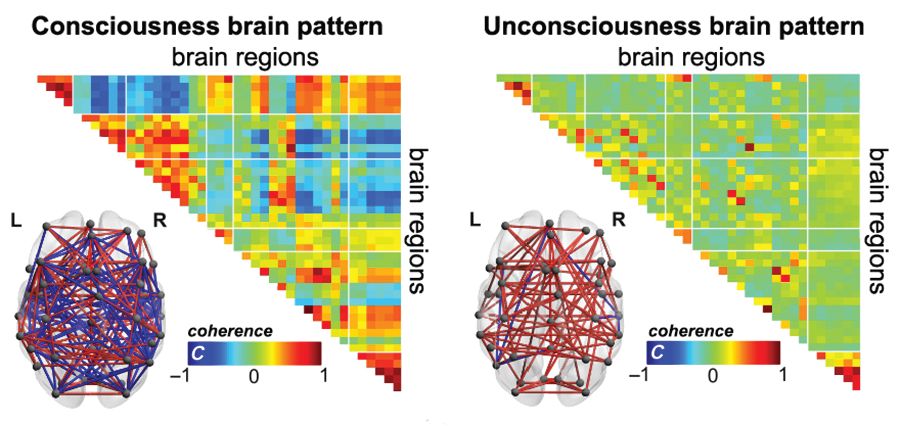
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
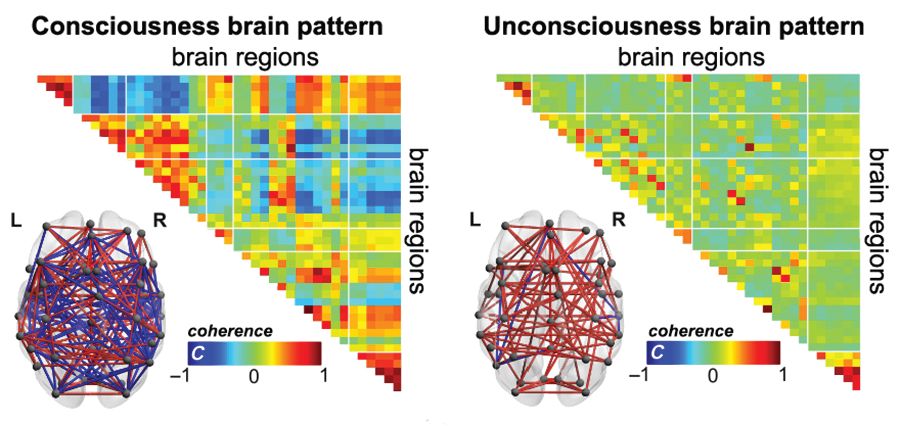
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
FROM SCIENCE ADVANCES
Key clinical point:
Major finding: A brain-wide coordination pattern of high complexity became increasingly common when moving from patients with unresponsive wakefulness syndrome (UWS) to patients in a minimally conscious state (MCS) to healthy control individuals.
Study details: A study involving blood oxygen level–dependent (BOLD) fMRI scans at rest or under anesthesia in 159 participants at four independent research facilities.
Disclosures: The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
Source: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Researchers compare focused ultrasound and DBS for essential tremor
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
REPORTING FROM NANS 2019
‘Error neuron’ EEG findings could open up future clinical applications
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
FROM NEURON
Resection, neurostimulation combo found successful in eloquent cortical regions
NEW ORLEANS – Concurrent surgical resection and implanted strip electrodes eliminated refractory focal seizures in two patients with focal cortical dysplasia and reduced them by 62% in a third patient, according a report presented at the annual meeting of the American Epilepsy Society.
None of the patients had been considered surgical candidates because their seizure foci were in eloquent cortical regions; if fully resected, patients would have experienced marked neurologic deficits. But the combination procedure of flanking the incomplete resected foci with implanted electrodes allowed neurosurgeons to remove less tissue, preserving function while effectively treating previously untreatable seizures, Emily Mirro said at the meeting.
The two-in-one technique makes good surgical sense for these patients, she said in an interview. “If we simply performed the resection and closed without implanting the electrodes, just waiting to see if seizures develop or not, then going back to implant the electrodes, the surgery is riskier and more difficult,” said Ms. Mirro, director of field clinical engineering for NeuroPace, which makes the stimulator system.
At the meeting, she presented three case studies on behalf of primary authors Lawrence Shuer, MD, and Babak Razavi, MD, PhD, both of Stanford (Calif.) University.
The first patient was a 26-year-old with a focal cortical dysplasia in the right parietal region, causing about six seizures each month. At the time of surgery, surgeons flanked the resected region with four cortical strip leads over sensory cortex. The RNS System detected the first postsurgical seizure 1 month afterward. Five months later, the system was enabled at 0.5 milliamps. For the next year, the patient received about 100 stimulations per day, amounting to a total daily stimulation time of about 20 seconds. Electrographic seizures did return, at which point the system increased neurostimulation to about 2,000 per day (a total stimulation time of about 7 minutes per day). At 1.3 years, the patient remains seizure free.
Patient two was a 20-year-old with a left frontal transmantle cortical dysplasia that involved the inferior frontal sulcus. The baseline seizure frequency was about two per day. Surgeons removed the dysplastic area with a 2.0 cm x 0.5 cm resection; the deficit was flanked with two left-front cortical strip leads. In the following 9 days, the patient experienced eight seizures. At 14 days out, the system was enabled at 1 milliamp. This patient became seizure free and remains so at 1.3 years, with about 100 stimulations per day to suppress electrographic abnormalities.
The third patient, also 20 years old, had a left-parietal resection to the margin of the motor cortex. The baseline seizure frequency was up to 150 nocturnal events per month and several seizures during each day as well. The resection was flanked by one strip lead over the motor cortex; one depth lead implanted into it. Immediately after surgery, the patient experienced both electrographic and clinical seizures. The stimulator was enabled a week after surgery at 0.5 milliamps; this was titrated to 3 milliamps over 1.4 years. At last follow-up, the patient had about a 62% reduction in seizure frequency; all are now nocturnal.
None of the patients experienced any peri- or postoperative surgical complications.
Ms. Mirro is an employee of NeuroPace.
SOURCE: Razavi B et al. AES 2018, Abstract 2.315
NEW ORLEANS – Concurrent surgical resection and implanted strip electrodes eliminated refractory focal seizures in two patients with focal cortical dysplasia and reduced them by 62% in a third patient, according a report presented at the annual meeting of the American Epilepsy Society.
None of the patients had been considered surgical candidates because their seizure foci were in eloquent cortical regions; if fully resected, patients would have experienced marked neurologic deficits. But the combination procedure of flanking the incomplete resected foci with implanted electrodes allowed neurosurgeons to remove less tissue, preserving function while effectively treating previously untreatable seizures, Emily Mirro said at the meeting.
The two-in-one technique makes good surgical sense for these patients, she said in an interview. “If we simply performed the resection and closed without implanting the electrodes, just waiting to see if seizures develop or not, then going back to implant the electrodes, the surgery is riskier and more difficult,” said Ms. Mirro, director of field clinical engineering for NeuroPace, which makes the stimulator system.
At the meeting, she presented three case studies on behalf of primary authors Lawrence Shuer, MD, and Babak Razavi, MD, PhD, both of Stanford (Calif.) University.
The first patient was a 26-year-old with a focal cortical dysplasia in the right parietal region, causing about six seizures each month. At the time of surgery, surgeons flanked the resected region with four cortical strip leads over sensory cortex. The RNS System detected the first postsurgical seizure 1 month afterward. Five months later, the system was enabled at 0.5 milliamps. For the next year, the patient received about 100 stimulations per day, amounting to a total daily stimulation time of about 20 seconds. Electrographic seizures did return, at which point the system increased neurostimulation to about 2,000 per day (a total stimulation time of about 7 minutes per day). At 1.3 years, the patient remains seizure free.
Patient two was a 20-year-old with a left frontal transmantle cortical dysplasia that involved the inferior frontal sulcus. The baseline seizure frequency was about two per day. Surgeons removed the dysplastic area with a 2.0 cm x 0.5 cm resection; the deficit was flanked with two left-front cortical strip leads. In the following 9 days, the patient experienced eight seizures. At 14 days out, the system was enabled at 1 milliamp. This patient became seizure free and remains so at 1.3 years, with about 100 stimulations per day to suppress electrographic abnormalities.
The third patient, also 20 years old, had a left-parietal resection to the margin of the motor cortex. The baseline seizure frequency was up to 150 nocturnal events per month and several seizures during each day as well. The resection was flanked by one strip lead over the motor cortex; one depth lead implanted into it. Immediately after surgery, the patient experienced both electrographic and clinical seizures. The stimulator was enabled a week after surgery at 0.5 milliamps; this was titrated to 3 milliamps over 1.4 years. At last follow-up, the patient had about a 62% reduction in seizure frequency; all are now nocturnal.
None of the patients experienced any peri- or postoperative surgical complications.
Ms. Mirro is an employee of NeuroPace.
SOURCE: Razavi B et al. AES 2018, Abstract 2.315
NEW ORLEANS – Concurrent surgical resection and implanted strip electrodes eliminated refractory focal seizures in two patients with focal cortical dysplasia and reduced them by 62% in a third patient, according a report presented at the annual meeting of the American Epilepsy Society.
None of the patients had been considered surgical candidates because their seizure foci were in eloquent cortical regions; if fully resected, patients would have experienced marked neurologic deficits. But the combination procedure of flanking the incomplete resected foci with implanted electrodes allowed neurosurgeons to remove less tissue, preserving function while effectively treating previously untreatable seizures, Emily Mirro said at the meeting.
The two-in-one technique makes good surgical sense for these patients, she said in an interview. “If we simply performed the resection and closed without implanting the electrodes, just waiting to see if seizures develop or not, then going back to implant the electrodes, the surgery is riskier and more difficult,” said Ms. Mirro, director of field clinical engineering for NeuroPace, which makes the stimulator system.
At the meeting, she presented three case studies on behalf of primary authors Lawrence Shuer, MD, and Babak Razavi, MD, PhD, both of Stanford (Calif.) University.
The first patient was a 26-year-old with a focal cortical dysplasia in the right parietal region, causing about six seizures each month. At the time of surgery, surgeons flanked the resected region with four cortical strip leads over sensory cortex. The RNS System detected the first postsurgical seizure 1 month afterward. Five months later, the system was enabled at 0.5 milliamps. For the next year, the patient received about 100 stimulations per day, amounting to a total daily stimulation time of about 20 seconds. Electrographic seizures did return, at which point the system increased neurostimulation to about 2,000 per day (a total stimulation time of about 7 minutes per day). At 1.3 years, the patient remains seizure free.
Patient two was a 20-year-old with a left frontal transmantle cortical dysplasia that involved the inferior frontal sulcus. The baseline seizure frequency was about two per day. Surgeons removed the dysplastic area with a 2.0 cm x 0.5 cm resection; the deficit was flanked with two left-front cortical strip leads. In the following 9 days, the patient experienced eight seizures. At 14 days out, the system was enabled at 1 milliamp. This patient became seizure free and remains so at 1.3 years, with about 100 stimulations per day to suppress electrographic abnormalities.
The third patient, also 20 years old, had a left-parietal resection to the margin of the motor cortex. The baseline seizure frequency was up to 150 nocturnal events per month and several seizures during each day as well. The resection was flanked by one strip lead over the motor cortex; one depth lead implanted into it. Immediately after surgery, the patient experienced both electrographic and clinical seizures. The stimulator was enabled a week after surgery at 0.5 milliamps; this was titrated to 3 milliamps over 1.4 years. At last follow-up, the patient had about a 62% reduction in seizure frequency; all are now nocturnal.
None of the patients experienced any peri- or postoperative surgical complications.
Ms. Mirro is an employee of NeuroPace.
SOURCE: Razavi B et al. AES 2018, Abstract 2.315
REPORTING FROM AES 2018
Key clinical point:
Major finding: Two patients became seizure free and one had a 62% reduction in seizures.
Study details: A three-patient case series.
Disclosures: NeuroPace makes the neurostimulator used in the study. The presenter is an employee of NeuroPace.
Source: Razavi B et al. AES 2018, Abstract 2.315.
AAP advises moderate physical, cognitive activity after sports concussion
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
FROM PEDIATRICS
Can biomarkers detect concussions? It’s complicated
A series of three studies in college students showed that some serum markers are associated with concussion but the background level of the markers can vary considerably. There was no association between the markers and history of concussion, and they markers varied significantly by sex and race.
The work, published in Neurology, suggests that there is hope for finding biomarkers for concussion, but much more work needs to be done.
Serum levels of amyloid beta 42 (Abeta42), total tau, and S100 calcium binding protein B (S100B) were associated with concussion, especially when tests were performed within 4 hours of the injury. However, the varying background levels indicate that these biomarkers are not yet ready for clinical application.
All three studies looked at serum levels of Abeta42, total tau, S100B, ubiquitin carboxyl-terminal hydrolase L1 (UCH-L1), glial fibrillary acidic protein (GFAP), microtubule-associated protein 2 (MAP2), and 2’,3’-cyclic-nucleotide 3’-phosphodiesterase (CNPase).
In the first study, researchers recruited 415 college athletes without a concussion (61% male, 40% white). The researchers took measurements outside of the athletes’ competitive sports season to maximize the odds that the levels would represent a true baseline. The median time between blood draw and the last risk of head impact was 80 days (mean, 98.4 days; interquartile range, 38-204 days).
Males had higher levels of UCH-L1 (Cohen d = 0.75; P less than .001) and S100B (Cohen d = 0.56; P less than .001), while females had higher levels of CNPase (Cohen d = 0.43; P less than .001). White subjects had higher levels of Abeta42 (Cohen d = .28; P = .005) and CNPase (Cohen d = 0.46; P less than .001). Black subjects had higher levels of UCH-L1 (Cohen d = 0.61; P less than .001) and S100 B (Cohen d = 1.1; P less than .001).
The measurements were not particularly reliable, with retests over 6- to 12-month periods yielding varying results such that none of the test/retest cutoff points reached the cutoff for acceptable reliability.
The second study was an observational cohort study of the same 415 subjects. The researchers assessed the self-reported concussion history and the cumulative exposure to collision sports with serum levels of the above biomarkers. The only relationship between a biomarker history and self-reported concussions was higher baseline Abeta42, but that had a small effect size (P = .005). Among football players, there was no association between approximate number of head impacts and any baseline biomarker.
The third study looked at 31 subjects who had experienced a sports-related concussion, 29 of whom had had both a baseline and a postconcussion blood draw, and compared them with nonconcussed, demographically matched athletes.
Of all the biomarkers studied, only levels of S100B rose following a concussion, with 67% of concussed subjects experiencing such a change (P = .003). When the researchers restricted the analysis to subjects who had a blood draw within 4 hours of the concussion, 88% of the tests showed an increase (P = .001). UCH-L1 also rose in 86% of subjects, but this change was not significant after adjustment for multiple comparisons (P greater than .007).
Compared with controls, concussed individuals had significantly higher levels of Abeta42, total tau, S100B, and GFAP. Of the concussed patients, 79.4% had Abeta42 levels higher than the median of controls, 67.6% had higher levels of total tau than the median of controls, and 83.3% had higher levels of S100B. Restriction of analysis to blood drawn within 4 hours of the injury yielded values of 81.3%, 75.0%, and 88.2%, respectively.
When limited to blood draws taken within 4 hours of injury, the researchers found fair diagnostic accuracy for measurements of Abeta42 (area under the curve, 0.75; 95% confidence interval, 0.59-0.91), total tau (AUC, 0.74; 95% CI, 0.58-0.90), and S100B (AUC, 0.75; 95% CI, 0.64-0.85). Abeta42 concentrations higher than 13.7 pg/mL were 75.0% sensitive and 82.4% specific to a sports-related concussion. Total tau concentrations higher than 1.7 pg/mL detected sports-related concussions at 75.0% sensitivity and 66.3% specificity, with acceptable diagnostic accuracy for white subjects (AUC, 0.82, 95% CI, 0.72-0.93). Also for white participants, S100B concentrations higher than 53 pg/mL predicted sports-related concussions with 83.3% sensitivity and 74.6% specificity.
The researchers found no associations between biomarkers and performance on clinical tests or time away from sports.
SOURCE: BM Asken et al. Neurology. 2018. doi: 10.1212/WNL.0000000000006613.
Concussion diagnosis has been constrained by reliance on subjective evidence, particularly in mild cases. Concussions also often result from a wide range of injuries, but focusing on sports-related concussions offers a chance to study biomarkers in a more controlled way.
These three studies represent the most comprehensive sports-related concussion biomarker work to date. The message may be that, for sports-related concussions, serum biomarkers may be able to detect the occurrence of a concussion, but they cannot predict motor, neurobehavioral, or neurocognitive outcome measures.
The study results also underline the need for larger, more complex prospective studies.
Erin Bigler, PhD, is a professor of psychology and neuroscience at Brigham Young University. Ellen Deibert, MD, is a neurologist in York, Pa. These comments were taken from an accompanying editorial (Neurology. 2018. doi: 10.1212/WNL.0000000000006609 ). Dr. Bigler and Dr. Deibert have no relevant conflicts of interest.
Concussion diagnosis has been constrained by reliance on subjective evidence, particularly in mild cases. Concussions also often result from a wide range of injuries, but focusing on sports-related concussions offers a chance to study biomarkers in a more controlled way.
These three studies represent the most comprehensive sports-related concussion biomarker work to date. The message may be that, for sports-related concussions, serum biomarkers may be able to detect the occurrence of a concussion, but they cannot predict motor, neurobehavioral, or neurocognitive outcome measures.
The study results also underline the need for larger, more complex prospective studies.
Erin Bigler, PhD, is a professor of psychology and neuroscience at Brigham Young University. Ellen Deibert, MD, is a neurologist in York, Pa. These comments were taken from an accompanying editorial (Neurology. 2018. doi: 10.1212/WNL.0000000000006609 ). Dr. Bigler and Dr. Deibert have no relevant conflicts of interest.
Concussion diagnosis has been constrained by reliance on subjective evidence, particularly in mild cases. Concussions also often result from a wide range of injuries, but focusing on sports-related concussions offers a chance to study biomarkers in a more controlled way.
These three studies represent the most comprehensive sports-related concussion biomarker work to date. The message may be that, for sports-related concussions, serum biomarkers may be able to detect the occurrence of a concussion, but they cannot predict motor, neurobehavioral, or neurocognitive outcome measures.
The study results also underline the need for larger, more complex prospective studies.
Erin Bigler, PhD, is a professor of psychology and neuroscience at Brigham Young University. Ellen Deibert, MD, is a neurologist in York, Pa. These comments were taken from an accompanying editorial (Neurology. 2018. doi: 10.1212/WNL.0000000000006609 ). Dr. Bigler and Dr. Deibert have no relevant conflicts of interest.
A series of three studies in college students showed that some serum markers are associated with concussion but the background level of the markers can vary considerably. There was no association between the markers and history of concussion, and they markers varied significantly by sex and race.
The work, published in Neurology, suggests that there is hope for finding biomarkers for concussion, but much more work needs to be done.
Serum levels of amyloid beta 42 (Abeta42), total tau, and S100 calcium binding protein B (S100B) were associated with concussion, especially when tests were performed within 4 hours of the injury. However, the varying background levels indicate that these biomarkers are not yet ready for clinical application.
All three studies looked at serum levels of Abeta42, total tau, S100B, ubiquitin carboxyl-terminal hydrolase L1 (UCH-L1), glial fibrillary acidic protein (GFAP), microtubule-associated protein 2 (MAP2), and 2’,3’-cyclic-nucleotide 3’-phosphodiesterase (CNPase).
In the first study, researchers recruited 415 college athletes without a concussion (61% male, 40% white). The researchers took measurements outside of the athletes’ competitive sports season to maximize the odds that the levels would represent a true baseline. The median time between blood draw and the last risk of head impact was 80 days (mean, 98.4 days; interquartile range, 38-204 days).
Males had higher levels of UCH-L1 (Cohen d = 0.75; P less than .001) and S100B (Cohen d = 0.56; P less than .001), while females had higher levels of CNPase (Cohen d = 0.43; P less than .001). White subjects had higher levels of Abeta42 (Cohen d = .28; P = .005) and CNPase (Cohen d = 0.46; P less than .001). Black subjects had higher levels of UCH-L1 (Cohen d = 0.61; P less than .001) and S100 B (Cohen d = 1.1; P less than .001).
The measurements were not particularly reliable, with retests over 6- to 12-month periods yielding varying results such that none of the test/retest cutoff points reached the cutoff for acceptable reliability.
The second study was an observational cohort study of the same 415 subjects. The researchers assessed the self-reported concussion history and the cumulative exposure to collision sports with serum levels of the above biomarkers. The only relationship between a biomarker history and self-reported concussions was higher baseline Abeta42, but that had a small effect size (P = .005). Among football players, there was no association between approximate number of head impacts and any baseline biomarker.
The third study looked at 31 subjects who had experienced a sports-related concussion, 29 of whom had had both a baseline and a postconcussion blood draw, and compared them with nonconcussed, demographically matched athletes.
Of all the biomarkers studied, only levels of S100B rose following a concussion, with 67% of concussed subjects experiencing such a change (P = .003). When the researchers restricted the analysis to subjects who had a blood draw within 4 hours of the concussion, 88% of the tests showed an increase (P = .001). UCH-L1 also rose in 86% of subjects, but this change was not significant after adjustment for multiple comparisons (P greater than .007).
Compared with controls, concussed individuals had significantly higher levels of Abeta42, total tau, S100B, and GFAP. Of the concussed patients, 79.4% had Abeta42 levels higher than the median of controls, 67.6% had higher levels of total tau than the median of controls, and 83.3% had higher levels of S100B. Restriction of analysis to blood drawn within 4 hours of the injury yielded values of 81.3%, 75.0%, and 88.2%, respectively.
When limited to blood draws taken within 4 hours of injury, the researchers found fair diagnostic accuracy for measurements of Abeta42 (area under the curve, 0.75; 95% confidence interval, 0.59-0.91), total tau (AUC, 0.74; 95% CI, 0.58-0.90), and S100B (AUC, 0.75; 95% CI, 0.64-0.85). Abeta42 concentrations higher than 13.7 pg/mL were 75.0% sensitive and 82.4% specific to a sports-related concussion. Total tau concentrations higher than 1.7 pg/mL detected sports-related concussions at 75.0% sensitivity and 66.3% specificity, with acceptable diagnostic accuracy for white subjects (AUC, 0.82, 95% CI, 0.72-0.93). Also for white participants, S100B concentrations higher than 53 pg/mL predicted sports-related concussions with 83.3% sensitivity and 74.6% specificity.
The researchers found no associations between biomarkers and performance on clinical tests or time away from sports.
SOURCE: BM Asken et al. Neurology. 2018. doi: 10.1212/WNL.0000000000006613.
A series of three studies in college students showed that some serum markers are associated with concussion but the background level of the markers can vary considerably. There was no association between the markers and history of concussion, and they markers varied significantly by sex and race.
The work, published in Neurology, suggests that there is hope for finding biomarkers for concussion, but much more work needs to be done.
Serum levels of amyloid beta 42 (Abeta42), total tau, and S100 calcium binding protein B (S100B) were associated with concussion, especially when tests were performed within 4 hours of the injury. However, the varying background levels indicate that these biomarkers are not yet ready for clinical application.
All three studies looked at serum levels of Abeta42, total tau, S100B, ubiquitin carboxyl-terminal hydrolase L1 (UCH-L1), glial fibrillary acidic protein (GFAP), microtubule-associated protein 2 (MAP2), and 2’,3’-cyclic-nucleotide 3’-phosphodiesterase (CNPase).
In the first study, researchers recruited 415 college athletes without a concussion (61% male, 40% white). The researchers took measurements outside of the athletes’ competitive sports season to maximize the odds that the levels would represent a true baseline. The median time between blood draw and the last risk of head impact was 80 days (mean, 98.4 days; interquartile range, 38-204 days).
Males had higher levels of UCH-L1 (Cohen d = 0.75; P less than .001) and S100B (Cohen d = 0.56; P less than .001), while females had higher levels of CNPase (Cohen d = 0.43; P less than .001). White subjects had higher levels of Abeta42 (Cohen d = .28; P = .005) and CNPase (Cohen d = 0.46; P less than .001). Black subjects had higher levels of UCH-L1 (Cohen d = 0.61; P less than .001) and S100 B (Cohen d = 1.1; P less than .001).
The measurements were not particularly reliable, with retests over 6- to 12-month periods yielding varying results such that none of the test/retest cutoff points reached the cutoff for acceptable reliability.
The second study was an observational cohort study of the same 415 subjects. The researchers assessed the self-reported concussion history and the cumulative exposure to collision sports with serum levels of the above biomarkers. The only relationship between a biomarker history and self-reported concussions was higher baseline Abeta42, but that had a small effect size (P = .005). Among football players, there was no association between approximate number of head impacts and any baseline biomarker.
The third study looked at 31 subjects who had experienced a sports-related concussion, 29 of whom had had both a baseline and a postconcussion blood draw, and compared them with nonconcussed, demographically matched athletes.
Of all the biomarkers studied, only levels of S100B rose following a concussion, with 67% of concussed subjects experiencing such a change (P = .003). When the researchers restricted the analysis to subjects who had a blood draw within 4 hours of the concussion, 88% of the tests showed an increase (P = .001). UCH-L1 also rose in 86% of subjects, but this change was not significant after adjustment for multiple comparisons (P greater than .007).
Compared with controls, concussed individuals had significantly higher levels of Abeta42, total tau, S100B, and GFAP. Of the concussed patients, 79.4% had Abeta42 levels higher than the median of controls, 67.6% had higher levels of total tau than the median of controls, and 83.3% had higher levels of S100B. Restriction of analysis to blood drawn within 4 hours of the injury yielded values of 81.3%, 75.0%, and 88.2%, respectively.
When limited to blood draws taken within 4 hours of injury, the researchers found fair diagnostic accuracy for measurements of Abeta42 (area under the curve, 0.75; 95% confidence interval, 0.59-0.91), total tau (AUC, 0.74; 95% CI, 0.58-0.90), and S100B (AUC, 0.75; 95% CI, 0.64-0.85). Abeta42 concentrations higher than 13.7 pg/mL were 75.0% sensitive and 82.4% specific to a sports-related concussion. Total tau concentrations higher than 1.7 pg/mL detected sports-related concussions at 75.0% sensitivity and 66.3% specificity, with acceptable diagnostic accuracy for white subjects (AUC, 0.82, 95% CI, 0.72-0.93). Also for white participants, S100B concentrations higher than 53 pg/mL predicted sports-related concussions with 83.3% sensitivity and 74.6% specificity.
The researchers found no associations between biomarkers and performance on clinical tests or time away from sports.
SOURCE: BM Asken et al. Neurology. 2018. doi: 10.1212/WNL.0000000000006613.
FROM NEUROLOGY
Key clinical point: Serum biomarkers show promise in concussion diagnosis, but much work remains.
Major finding: Serum levels of Abeta42, total tau, and S100B were elevated after concussions.
Study details: Prospective studies on 415 college athletes.
Disclosures: The study was funded by the Head Health Initiative, Banyan Biomarkers, and the United States Army Medical Research and Materiel Command.
Sources: BM Asken et al. Neurology. 2018. doi: 10.1212/WNL.0000000000006613.
New and Noteworthy Information—November 2018
Thrombolysis Benefits Patients With Stroke
In patients with acute stroke with an unknown time of onset, IV alteplase guided by a mismatch between diffusion-weighted imaging and fluid-attenuated inversion recovery (FLAIR) in the region of ischemia results in a significantly better functional outcome and more intracranial hemorrhages at 90 days, compared with placebo, according to a study published August 16 in the New England Journal of Medicine. Researchers randomly assigned 254 participants to receive IV alteplase and 249 participants to receive placebo. Participants had an ischemic lesion on MRI diffusion-weighted imaging, but no parenchymal hyperintensity on FLAIR. A favorable outcome (ie, a score of 0 or 1 on the modified Rankin Scale at 90 days) occurred in 53.3% of the alteplase group versus 41.8% of the placebo group.
Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018;379(7):611-622.
High Levels of Cortisol Linked to Impaired Memory
Middle-aged people with high levels of cortisol in their blood have impaired memory, compared with people with average levels of cortisol, according to a study published online ahead of print October 24 in Neurology. Researchers identified 2,231 people with an average age of 49 who did not have dementia. At the start of the study, each participant underwent a psychologic exam and assessments of memory and thinking skills. Participants’ memory and thinking skills were tested again at an average of eight years later. Participants also provided a blood sample. After adjusting for age, sex, smoking, and BMI, researchers found that people with high levels of cortisol had lower scores on tests of memory and thinking skills, compared with people with normal levels of cortisol.
Echouffo-Tcheugui JB, Conner SC, Himali JJ, et al. Circulating cortisol and cognitive and structural brain measures: The Framingham Heart Study. Neurology. 2018 Oct 24 [Epub ahead of print].
Is Nusinersen Effective If Initiated Later?
Patients with spinal muscular atrophy type 1 (SMA1) may benefit from nusinersen when the therapy is initiated after age 7 months, according to a study published online ahead of print August 29 in Neurology. In this study, 33 patients with SMA1 received intrathecal nusinersen injections. Researchers evaluated patients before treatment and at two months and six months after treatment. All patients were alive and continuing treatment at six months. Median progress on the modified Hammersmith Infant Neurologic Examination Part 2 score was 1.5 points after six months of treatment. The need for respiratory support significantly increased over time. The results are consistent with those of a phase III trial in which patients with SMA1 received nusinersen before age 7 months, the researchers said.
Aragon-Gawinska K, Seferian AM, Daron A, et al. Nusinersen in spinal muscular atrophy type 1 patients older than 7 months: a cohort study. Neurology. 2018 Aug 29 [Epub ahead of print].
Pre-Eclampsia Linked to Dementia in Late Life
Pre-eclampsia is associated with an increased risk of dementia, particularly vascular dementia, according to a study published October 17 in BMJ. The study cohort consisted of 1,178,005 Danish women with at least one live birth or stillbirth between 1978 and 2015. Women with a history of pre-eclampsia had more than three times the risk of vascular dementia later in life, compared with women with no history of pre-eclampsia. The association with vascular dementia seemed to be stronger for late-onset disease than for early-onset disease. Adjustment for diabetes, hypertension, and cardiovascular disease attenuated the hazard ratios moderately. Sensitivity analyses suggested that BMI was unlikely to explain the association with vascular dementia. In contrast, modest associations were observed for Alzheimer’s disease and other or unspecified dementia.
Basit S, Wohlfahrt J, Boyd HA. Pre-eclampsia and risk of dementia later in life: nationwide cohort study. BMJ. 2018;363:k4109.
Does Antiepileptic Drug Clearance Change During Pregnancy?
In pregnant women, antiepileptic drug (AED) clearance significantly changes by the first trimester for levetiracetam and by the second trimester for oxcarbazepine and topiramate, according to a study published September 25 in Neurology. This prospective, observational study included 40 women with epilepsy who were planning to conceive or were fewer than 16 weeks pregnant and who chose to continue their AEDs during pregnancy. Drug clearance values were obtained by blood draw at baseline and during pregnancy. Mean maximal clearances were 1.71 times the baseline clearance for levetiracetam, 1.63 times the baseline clearance for oxcarbazepine, and 1.39 the baseline clearance for topiramate. In 15 women on AED monotherapy, increased seizure frequency in the first, second, and all trimesters was associated with a lower ratio to target concentration.
Voinescu PE, Park S, Chen LQ, et al. Antiepileptic drug clearances during pregnancy and clinical implications for women with epilepsy. Neurology. 2018;91(13):e1228-e1236.
Do Dextroamphetamine and Physical Therapy Improve Function After Stroke?
Compared with placebo, dextroamphetamine combined with physical therapy does not improve recovery of motor function after stroke, according to a study published online ahead of print August 27 in JAMA Neurology. This pilot, double-blind, block-randomized clinical trial included patients with cortical or subcortical ischemic stroke and moderate or severe motor deficits. A total of 64 participants were randomized to receive 10 mg of dextroamphetamine or placebo one hour before a one-hour physical therapy session every four days for six sessions, in addition to standard rehabilitation. The primary outcome was the difference between groups in change in Fugl-Meyer motor scores from baseline to three months after stroke. Treatment was not associated with differences in the primary outcome, secondary measures, or subgroups based on stroke location or baseline severity.
Goldstein LB, Lennihan L, Rabadi MJ, et al. Effect of dextroamphetamine on poststroke motor recovery: a randomized clinical trial. JAMA Neurol. 2018 Aug 27 [Epub ahead of print].
FDA Approves Tegsedi for hATTR in Adults
The FDA has approved Tegsedi (inotersen) for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis (hATTR) in adults. The approval is based on data from the phase III randomized, double-blind, placebo-controlled, 15-month, international NEURO-TTR study in 172 patients with hATTR amyloidosis with symptoms of polyneuropathy. In NEURO-TTR, Tegsedi demonstrated significant benefit, compared with placebo, in neuropathy and quality of life, as measured by the modified Neuropathy Impairment Score +7 and the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy total score. Patients treated with Tegsedi experienced similar benefit regardless of subgroup, such as age, sex, race, region, Neuropathy Impairment Score, Val30Met mutation status, and disease stage. Akcea Therapeutics, an affiliate of Ionis Pharmaceuticals that is headquartered in Boston, markets Tegsedi.
Data Review Evaluates Nusinersen’s Efficacy in SMA
A panel has reviewed the evidence for nusinersen treatment of spinal muscular atrophy (SMA). The results were published online ahead of print October 12 in Neurology. The authors systematically reviewed clinical trials of nusinersen in patients with SMA and assigned level of evidence statements. Among four published clinical trials identified, three were rated above Class IV. There is Class I evidence that in term infants with SMA and two copies of SMN2, treatment with nusinersen started in children younger than 7 months results in a better motor milestone response and higher rates of event-free survival than sham control. There is Class I evidence that in children aged 2 to 12 with SMA symptom onset after age 6 months, nusinersen yields greater improvement in motor function at 15 months than sham control.
Michelson D, Ciafaloni E, Ashwal S, et al. Evidence in focus: nusinersen use in spinal muscular atrophy: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018 Oct 12 [Epub ahead of print].
Aortic Stiffness Predicts Incident Dementia
Arterial stiffness can predict a person’s likelihood of developing dementia, according to a study published October 16 in the Journal of Alzheimer’s Disease. Researchers analyzed the association between arterial stiffness and dementia among 356 older adults with an average age of 78 who were part of the Cardiovascular Health Study Cognition Study. Eligible participants were dementia-free when the study began in 1998. Investigators tested participants’ aortic stiffness with carotid-femoral pulse wave velocity. Participants also underwent MRI of their brains to measure signs of subclinical brain disease. The researchers found that participants with high carotid-femoral pulse wave velocity readings were 60% more likely to develop dementia during the following 15 years, compared with people with lower carotid-femoral pulse wave velocity values.
Cui C, Sekikawa A, Kuller LH, et al. Aortic stiffness is associated with increased risk of incident dementia in older adults. J Alzheimers Dis. 2018;66(1):297-306.
Early MoCA Score Predicts Long-Term Outcome After Stroke
Early cognitive testing with the Montreal Cognitive Assessment (MoCA) predicts long-term cognitive outcome, functional outcome, and mortality after stroke, according to a study published online ahead of print October 17 in Neurology. In this international study, 274 people with stroke were administered MoCA within a week of stroke onset. Participants were divided into two groups: people with no problems with thinking and memory skills and people with cognitive impairment. People who had cognitive impairment within one week of stroke were seven times more likely to die during the three years of the study than people without cognitive impairment. Furthermore, the survival rate for people with cognitive impairment after three years was 83%, and the rate was 97% for people who did not have early cognitive impairment.
Zietemann V, Georgakis MK, Dondaine T, et al. Early MoCA predicts long-term cognitive and functional outcome and mortality after stroke. Neurology. 2018 Oct 17 [Epub ahead of print].
Antiepileptic Drug Use Related to Increased Stroke Risk
In Alzheimer’s disease, antiepileptic drug (AED) use is related to an increased risk of stroke, according to a study published September 18 in the Journal of the American Heart Association. Investigators examined the Medication Use and Alzheimer’s Disease cohort, which included all Finnish people who received a clinically verified diagnosis of Alzheimer’s disease from 2005 to 2011. People with previous stroke were excluded. For each incident AED user, the investigators matched one nonuser according to sex, age, and time since Alzheimer’s disease diagnosis. Analyses were conducted with Cox proportional hazards models and inverse probability of treatment weighting. Compared with nonuse, AED use was associated with an increased risk of stroke, and the risk of stroke was strongest during the first 90 days of AED use (adjusted hazard ratio, 2.36).
Sarycheva T, Lavikainen P, Taipale H, et al. Antiepileptic drug use and the risk of stroke among community-dwelling people with Alzheimer disease: A matched cohort study. J Am Heart Assoc. 2018;7(18):e009742.
Thrombolysis Benefits Patients With Stroke
In patients with acute stroke with an unknown time of onset, IV alteplase guided by a mismatch between diffusion-weighted imaging and fluid-attenuated inversion recovery (FLAIR) in the region of ischemia results in a significantly better functional outcome and more intracranial hemorrhages at 90 days, compared with placebo, according to a study published August 16 in the New England Journal of Medicine. Researchers randomly assigned 254 participants to receive IV alteplase and 249 participants to receive placebo. Participants had an ischemic lesion on MRI diffusion-weighted imaging, but no parenchymal hyperintensity on FLAIR. A favorable outcome (ie, a score of 0 or 1 on the modified Rankin Scale at 90 days) occurred in 53.3% of the alteplase group versus 41.8% of the placebo group.
Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018;379(7):611-622.
High Levels of Cortisol Linked to Impaired Memory
Middle-aged people with high levels of cortisol in their blood have impaired memory, compared with people with average levels of cortisol, according to a study published online ahead of print October 24 in Neurology. Researchers identified 2,231 people with an average age of 49 who did not have dementia. At the start of the study, each participant underwent a psychologic exam and assessments of memory and thinking skills. Participants’ memory and thinking skills were tested again at an average of eight years later. Participants also provided a blood sample. After adjusting for age, sex, smoking, and BMI, researchers found that people with high levels of cortisol had lower scores on tests of memory and thinking skills, compared with people with normal levels of cortisol.
Echouffo-Tcheugui JB, Conner SC, Himali JJ, et al. Circulating cortisol and cognitive and structural brain measures: The Framingham Heart Study. Neurology. 2018 Oct 24 [Epub ahead of print].
Is Nusinersen Effective If Initiated Later?
Patients with spinal muscular atrophy type 1 (SMA1) may benefit from nusinersen when the therapy is initiated after age 7 months, according to a study published online ahead of print August 29 in Neurology. In this study, 33 patients with SMA1 received intrathecal nusinersen injections. Researchers evaluated patients before treatment and at two months and six months after treatment. All patients were alive and continuing treatment at six months. Median progress on the modified Hammersmith Infant Neurologic Examination Part 2 score was 1.5 points after six months of treatment. The need for respiratory support significantly increased over time. The results are consistent with those of a phase III trial in which patients with SMA1 received nusinersen before age 7 months, the researchers said.
Aragon-Gawinska K, Seferian AM, Daron A, et al. Nusinersen in spinal muscular atrophy type 1 patients older than 7 months: a cohort study. Neurology. 2018 Aug 29 [Epub ahead of print].
Pre-Eclampsia Linked to Dementia in Late Life
Pre-eclampsia is associated with an increased risk of dementia, particularly vascular dementia, according to a study published October 17 in BMJ. The study cohort consisted of 1,178,005 Danish women with at least one live birth or stillbirth between 1978 and 2015. Women with a history of pre-eclampsia had more than three times the risk of vascular dementia later in life, compared with women with no history of pre-eclampsia. The association with vascular dementia seemed to be stronger for late-onset disease than for early-onset disease. Adjustment for diabetes, hypertension, and cardiovascular disease attenuated the hazard ratios moderately. Sensitivity analyses suggested that BMI was unlikely to explain the association with vascular dementia. In contrast, modest associations were observed for Alzheimer’s disease and other or unspecified dementia.
Basit S, Wohlfahrt J, Boyd HA. Pre-eclampsia and risk of dementia later in life: nationwide cohort study. BMJ. 2018;363:k4109.
Does Antiepileptic Drug Clearance Change During Pregnancy?
In pregnant women, antiepileptic drug (AED) clearance significantly changes by the first trimester for levetiracetam and by the second trimester for oxcarbazepine and topiramate, according to a study published September 25 in Neurology. This prospective, observational study included 40 women with epilepsy who were planning to conceive or were fewer than 16 weeks pregnant and who chose to continue their AEDs during pregnancy. Drug clearance values were obtained by blood draw at baseline and during pregnancy. Mean maximal clearances were 1.71 times the baseline clearance for levetiracetam, 1.63 times the baseline clearance for oxcarbazepine, and 1.39 the baseline clearance for topiramate. In 15 women on AED monotherapy, increased seizure frequency in the first, second, and all trimesters was associated with a lower ratio to target concentration.
Voinescu PE, Park S, Chen LQ, et al. Antiepileptic drug clearances during pregnancy and clinical implications for women with epilepsy. Neurology. 2018;91(13):e1228-e1236.
Do Dextroamphetamine and Physical Therapy Improve Function After Stroke?
Compared with placebo, dextroamphetamine combined with physical therapy does not improve recovery of motor function after stroke, according to a study published online ahead of print August 27 in JAMA Neurology. This pilot, double-blind, block-randomized clinical trial included patients with cortical or subcortical ischemic stroke and moderate or severe motor deficits. A total of 64 participants were randomized to receive 10 mg of dextroamphetamine or placebo one hour before a one-hour physical therapy session every four days for six sessions, in addition to standard rehabilitation. The primary outcome was the difference between groups in change in Fugl-Meyer motor scores from baseline to three months after stroke. Treatment was not associated with differences in the primary outcome, secondary measures, or subgroups based on stroke location or baseline severity.
Goldstein LB, Lennihan L, Rabadi MJ, et al. Effect of dextroamphetamine on poststroke motor recovery: a randomized clinical trial. JAMA Neurol. 2018 Aug 27 [Epub ahead of print].
FDA Approves Tegsedi for hATTR in Adults
The FDA has approved Tegsedi (inotersen) for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis (hATTR) in adults. The approval is based on data from the phase III randomized, double-blind, placebo-controlled, 15-month, international NEURO-TTR study in 172 patients with hATTR amyloidosis with symptoms of polyneuropathy. In NEURO-TTR, Tegsedi demonstrated significant benefit, compared with placebo, in neuropathy and quality of life, as measured by the modified Neuropathy Impairment Score +7 and the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy total score. Patients treated with Tegsedi experienced similar benefit regardless of subgroup, such as age, sex, race, region, Neuropathy Impairment Score, Val30Met mutation status, and disease stage. Akcea Therapeutics, an affiliate of Ionis Pharmaceuticals that is headquartered in Boston, markets Tegsedi.
Data Review Evaluates Nusinersen’s Efficacy in SMA
A panel has reviewed the evidence for nusinersen treatment of spinal muscular atrophy (SMA). The results were published online ahead of print October 12 in Neurology. The authors systematically reviewed clinical trials of nusinersen in patients with SMA and assigned level of evidence statements. Among four published clinical trials identified, three were rated above Class IV. There is Class I evidence that in term infants with SMA and two copies of SMN2, treatment with nusinersen started in children younger than 7 months results in a better motor milestone response and higher rates of event-free survival than sham control. There is Class I evidence that in children aged 2 to 12 with SMA symptom onset after age 6 months, nusinersen yields greater improvement in motor function at 15 months than sham control.
Michelson D, Ciafaloni E, Ashwal S, et al. Evidence in focus: nusinersen use in spinal muscular atrophy: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018 Oct 12 [Epub ahead of print].
Aortic Stiffness Predicts Incident Dementia
Arterial stiffness can predict a person’s likelihood of developing dementia, according to a study published October 16 in the Journal of Alzheimer’s Disease. Researchers analyzed the association between arterial stiffness and dementia among 356 older adults with an average age of 78 who were part of the Cardiovascular Health Study Cognition Study. Eligible participants were dementia-free when the study began in 1998. Investigators tested participants’ aortic stiffness with carotid-femoral pulse wave velocity. Participants also underwent MRI of their brains to measure signs of subclinical brain disease. The researchers found that participants with high carotid-femoral pulse wave velocity readings were 60% more likely to develop dementia during the following 15 years, compared with people with lower carotid-femoral pulse wave velocity values.
Cui C, Sekikawa A, Kuller LH, et al. Aortic stiffness is associated with increased risk of incident dementia in older adults. J Alzheimers Dis. 2018;66(1):297-306.
Early MoCA Score Predicts Long-Term Outcome After Stroke
Early cognitive testing with the Montreal Cognitive Assessment (MoCA) predicts long-term cognitive outcome, functional outcome, and mortality after stroke, according to a study published online ahead of print October 17 in Neurology. In this international study, 274 people with stroke were administered MoCA within a week of stroke onset. Participants were divided into two groups: people with no problems with thinking and memory skills and people with cognitive impairment. People who had cognitive impairment within one week of stroke were seven times more likely to die during the three years of the study than people without cognitive impairment. Furthermore, the survival rate for people with cognitive impairment after three years was 83%, and the rate was 97% for people who did not have early cognitive impairment.
Zietemann V, Georgakis MK, Dondaine T, et al. Early MoCA predicts long-term cognitive and functional outcome and mortality after stroke. Neurology. 2018 Oct 17 [Epub ahead of print].
Antiepileptic Drug Use Related to Increased Stroke Risk
In Alzheimer’s disease, antiepileptic drug (AED) use is related to an increased risk of stroke, according to a study published September 18 in the Journal of the American Heart Association. Investigators examined the Medication Use and Alzheimer’s Disease cohort, which included all Finnish people who received a clinically verified diagnosis of Alzheimer’s disease from 2005 to 2011. People with previous stroke were excluded. For each incident AED user, the investigators matched one nonuser according to sex, age, and time since Alzheimer’s disease diagnosis. Analyses were conducted with Cox proportional hazards models and inverse probability of treatment weighting. Compared with nonuse, AED use was associated with an increased risk of stroke, and the risk of stroke was strongest during the first 90 days of AED use (adjusted hazard ratio, 2.36).
Sarycheva T, Lavikainen P, Taipale H, et al. Antiepileptic drug use and the risk of stroke among community-dwelling people with Alzheimer disease: A matched cohort study. J Am Heart Assoc. 2018;7(18):e009742.
Thrombolysis Benefits Patients With Stroke
In patients with acute stroke with an unknown time of onset, IV alteplase guided by a mismatch between diffusion-weighted imaging and fluid-attenuated inversion recovery (FLAIR) in the region of ischemia results in a significantly better functional outcome and more intracranial hemorrhages at 90 days, compared with placebo, according to a study published August 16 in the New England Journal of Medicine. Researchers randomly assigned 254 participants to receive IV alteplase and 249 participants to receive placebo. Participants had an ischemic lesion on MRI diffusion-weighted imaging, but no parenchymal hyperintensity on FLAIR. A favorable outcome (ie, a score of 0 or 1 on the modified Rankin Scale at 90 days) occurred in 53.3% of the alteplase group versus 41.8% of the placebo group.
Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018;379(7):611-622.
High Levels of Cortisol Linked to Impaired Memory
Middle-aged people with high levels of cortisol in their blood have impaired memory, compared with people with average levels of cortisol, according to a study published online ahead of print October 24 in Neurology. Researchers identified 2,231 people with an average age of 49 who did not have dementia. At the start of the study, each participant underwent a psychologic exam and assessments of memory and thinking skills. Participants’ memory and thinking skills were tested again at an average of eight years later. Participants also provided a blood sample. After adjusting for age, sex, smoking, and BMI, researchers found that people with high levels of cortisol had lower scores on tests of memory and thinking skills, compared with people with normal levels of cortisol.
Echouffo-Tcheugui JB, Conner SC, Himali JJ, et al. Circulating cortisol and cognitive and structural brain measures: The Framingham Heart Study. Neurology. 2018 Oct 24 [Epub ahead of print].
Is Nusinersen Effective If Initiated Later?
Patients with spinal muscular atrophy type 1 (SMA1) may benefit from nusinersen when the therapy is initiated after age 7 months, according to a study published online ahead of print August 29 in Neurology. In this study, 33 patients with SMA1 received intrathecal nusinersen injections. Researchers evaluated patients before treatment and at two months and six months after treatment. All patients were alive and continuing treatment at six months. Median progress on the modified Hammersmith Infant Neurologic Examination Part 2 score was 1.5 points after six months of treatment. The need for respiratory support significantly increased over time. The results are consistent with those of a phase III trial in which patients with SMA1 received nusinersen before age 7 months, the researchers said.
Aragon-Gawinska K, Seferian AM, Daron A, et al. Nusinersen in spinal muscular atrophy type 1 patients older than 7 months: a cohort study. Neurology. 2018 Aug 29 [Epub ahead of print].
Pre-Eclampsia Linked to Dementia in Late Life
Pre-eclampsia is associated with an increased risk of dementia, particularly vascular dementia, according to a study published October 17 in BMJ. The study cohort consisted of 1,178,005 Danish women with at least one live birth or stillbirth between 1978 and 2015. Women with a history of pre-eclampsia had more than three times the risk of vascular dementia later in life, compared with women with no history of pre-eclampsia. The association with vascular dementia seemed to be stronger for late-onset disease than for early-onset disease. Adjustment for diabetes, hypertension, and cardiovascular disease attenuated the hazard ratios moderately. Sensitivity analyses suggested that BMI was unlikely to explain the association with vascular dementia. In contrast, modest associations were observed for Alzheimer’s disease and other or unspecified dementia.
Basit S, Wohlfahrt J, Boyd HA. Pre-eclampsia and risk of dementia later in life: nationwide cohort study. BMJ. 2018;363:k4109.
Does Antiepileptic Drug Clearance Change During Pregnancy?
In pregnant women, antiepileptic drug (AED) clearance significantly changes by the first trimester for levetiracetam and by the second trimester for oxcarbazepine and topiramate, according to a study published September 25 in Neurology. This prospective, observational study included 40 women with epilepsy who were planning to conceive or were fewer than 16 weeks pregnant and who chose to continue their AEDs during pregnancy. Drug clearance values were obtained by blood draw at baseline and during pregnancy. Mean maximal clearances were 1.71 times the baseline clearance for levetiracetam, 1.63 times the baseline clearance for oxcarbazepine, and 1.39 the baseline clearance for topiramate. In 15 women on AED monotherapy, increased seizure frequency in the first, second, and all trimesters was associated with a lower ratio to target concentration.
Voinescu PE, Park S, Chen LQ, et al. Antiepileptic drug clearances during pregnancy and clinical implications for women with epilepsy. Neurology. 2018;91(13):e1228-e1236.
Do Dextroamphetamine and Physical Therapy Improve Function After Stroke?
Compared with placebo, dextroamphetamine combined with physical therapy does not improve recovery of motor function after stroke, according to a study published online ahead of print August 27 in JAMA Neurology. This pilot, double-blind, block-randomized clinical trial included patients with cortical or subcortical ischemic stroke and moderate or severe motor deficits. A total of 64 participants were randomized to receive 10 mg of dextroamphetamine or placebo one hour before a one-hour physical therapy session every four days for six sessions, in addition to standard rehabilitation. The primary outcome was the difference between groups in change in Fugl-Meyer motor scores from baseline to three months after stroke. Treatment was not associated with differences in the primary outcome, secondary measures, or subgroups based on stroke location or baseline severity.
Goldstein LB, Lennihan L, Rabadi MJ, et al. Effect of dextroamphetamine on poststroke motor recovery: a randomized clinical trial. JAMA Neurol. 2018 Aug 27 [Epub ahead of print].
FDA Approves Tegsedi for hATTR in Adults
The FDA has approved Tegsedi (inotersen) for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis (hATTR) in adults. The approval is based on data from the phase III randomized, double-blind, placebo-controlled, 15-month, international NEURO-TTR study in 172 patients with hATTR amyloidosis with symptoms of polyneuropathy. In NEURO-TTR, Tegsedi demonstrated significant benefit, compared with placebo, in neuropathy and quality of life, as measured by the modified Neuropathy Impairment Score +7 and the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy total score. Patients treated with Tegsedi experienced similar benefit regardless of subgroup, such as age, sex, race, region, Neuropathy Impairment Score, Val30Met mutation status, and disease stage. Akcea Therapeutics, an affiliate of Ionis Pharmaceuticals that is headquartered in Boston, markets Tegsedi.
Data Review Evaluates Nusinersen’s Efficacy in SMA
A panel has reviewed the evidence for nusinersen treatment of spinal muscular atrophy (SMA). The results were published online ahead of print October 12 in Neurology. The authors systematically reviewed clinical trials of nusinersen in patients with SMA and assigned level of evidence statements. Among four published clinical trials identified, three were rated above Class IV. There is Class I evidence that in term infants with SMA and two copies of SMN2, treatment with nusinersen started in children younger than 7 months results in a better motor milestone response and higher rates of event-free survival than sham control. There is Class I evidence that in children aged 2 to 12 with SMA symptom onset after age 6 months, nusinersen yields greater improvement in motor function at 15 months than sham control.
Michelson D, Ciafaloni E, Ashwal S, et al. Evidence in focus: nusinersen use in spinal muscular atrophy: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018 Oct 12 [Epub ahead of print].
Aortic Stiffness Predicts Incident Dementia
Arterial stiffness can predict a person’s likelihood of developing dementia, according to a study published October 16 in the Journal of Alzheimer’s Disease. Researchers analyzed the association between arterial stiffness and dementia among 356 older adults with an average age of 78 who were part of the Cardiovascular Health Study Cognition Study. Eligible participants were dementia-free when the study began in 1998. Investigators tested participants’ aortic stiffness with carotid-femoral pulse wave velocity. Participants also underwent MRI of their brains to measure signs of subclinical brain disease. The researchers found that participants with high carotid-femoral pulse wave velocity readings were 60% more likely to develop dementia during the following 15 years, compared with people with lower carotid-femoral pulse wave velocity values.
Cui C, Sekikawa A, Kuller LH, et al. Aortic stiffness is associated with increased risk of incident dementia in older adults. J Alzheimers Dis. 2018;66(1):297-306.
Early MoCA Score Predicts Long-Term Outcome After Stroke
Early cognitive testing with the Montreal Cognitive Assessment (MoCA) predicts long-term cognitive outcome, functional outcome, and mortality after stroke, according to a study published online ahead of print October 17 in Neurology. In this international study, 274 people with stroke were administered MoCA within a week of stroke onset. Participants were divided into two groups: people with no problems with thinking and memory skills and people with cognitive impairment. People who had cognitive impairment within one week of stroke were seven times more likely to die during the three years of the study than people without cognitive impairment. Furthermore, the survival rate for people with cognitive impairment after three years was 83%, and the rate was 97% for people who did not have early cognitive impairment.
Zietemann V, Georgakis MK, Dondaine T, et al. Early MoCA predicts long-term cognitive and functional outcome and mortality after stroke. Neurology. 2018 Oct 17 [Epub ahead of print].
Antiepileptic Drug Use Related to Increased Stroke Risk
In Alzheimer’s disease, antiepileptic drug (AED) use is related to an increased risk of stroke, according to a study published September 18 in the Journal of the American Heart Association. Investigators examined the Medication Use and Alzheimer’s Disease cohort, which included all Finnish people who received a clinically verified diagnosis of Alzheimer’s disease from 2005 to 2011. People with previous stroke were excluded. For each incident AED user, the investigators matched one nonuser according to sex, age, and time since Alzheimer’s disease diagnosis. Analyses were conducted with Cox proportional hazards models and inverse probability of treatment weighting. Compared with nonuse, AED use was associated with an increased risk of stroke, and the risk of stroke was strongest during the first 90 days of AED use (adjusted hazard ratio, 2.36).
Sarycheva T, Lavikainen P, Taipale H, et al. Antiepileptic drug use and the risk of stroke among community-dwelling people with Alzheimer disease: A matched cohort study. J Am Heart Assoc. 2018;7(18):e009742.
Investigational gene therapy for medically refractory Parkinson’s shows promise
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
REPORTING FROM ANA 2018
Key clinical point: AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated.
Major finding: At 12 months, the researchers observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively.
Study details: A study of 15 patients in three cohorts who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions.
Disclosures: The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.