User login
Cervical length/fetal fibronectin combo doesn’t predict preterm birth
ATLANTA – The combination of cervical length and self-collected fetal fibronectin did not accurately predict preterm birth in a cohort of nulliparous women.
Although each measurement in itself had some predictive value, the best measure – cervical length measured by transvaginal ultrasound at 22-30 weeks’ gestation – was only marginally clinically useful, identifying about 24% of those who had a preterm birth. The addition of fetal fibronectin added nothing to the predictive value of the cervical measurement, Dr. Michael Esplin reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“Based on this study, we must conclude that the routine use of self-collected quantitative fetal fibronectin and transvaginal cervical length is not a viable way to screen for preterm birth in a nulliparous population,” said Dr. Esplin of the University of Utah, Salt Lake City.
He reported the results of Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b). The prospective studycomprised more than 9,300 women and was conducted at eight sites in the United States. There were two parts to the investigational screening protocol: collection of a fetal fibronectin swab at three gestational time points (8-14 weeks, 16-22 weeks, and 22-30 weeks) and transvaginal ultrasound to measure cervical length at time of the second and third fibronectin measurement.
The main outcome measure was a live birth at less than 37 weeks, after spontaneous preterm labor; the secondary outcome was a live birth after spontaneous preterm labor at less than 32 weeks’ gestation.
Mean age of the women was 27 years. All the women were carrying a singleton pregnancy. There were 471 spontaneous preterm live births. These were more likely to occur in the youngest and oldest women in the cohort. Preterm births were more common in women who smoked during pregnancy (24% vs. 17%), those who had less than a high school education (11.5% vs. 7.8%), and those with a prepregnancy history of diabetes (3.6% vs. 1.5%).
At the second visit, cervical length of 25 mm or less identified 8% of those who went on to have a preterm birth, for a positive predictive value of 16% and an area under the curve (AUC) of 0.61. At the third visit, cervical length of 25 mm or less identified 24% of women with preterm birth, for a positive predictive value of 15% and an area under the curve of 0.67.
Fetal fibronectin alone performed similarly. No matter what visit, and whether the cutoff was 10, 50, or 200 ng/mL, the AUC stayed between 0.51-0.54. The positive predictive values of these measurements ranged from 6%-12%.
“All of these measures had a relatively low positive predictive value,” Dr. Esplin said. “And while that may be acceptable if the tests are very sensitive, these, in fact were not. Cervical length, for example, had only 7.9% sensitivity at visit 2 and 23% sensitivity at visit 3.”
Combining cervical length and fetal fibronectin did nothing to improve the test’s validity or clinical usefulness. For a test to be clinically useful, Dr. Esplin said, the AUC should be at least 0.73. None of the measures came close to meeting this standard.
The National Institute of Child Health and Human Development sponsored the study. Dr. Esplin reported having no financial disclosures.
ATLANTA – The combination of cervical length and self-collected fetal fibronectin did not accurately predict preterm birth in a cohort of nulliparous women.
Although each measurement in itself had some predictive value, the best measure – cervical length measured by transvaginal ultrasound at 22-30 weeks’ gestation – was only marginally clinically useful, identifying about 24% of those who had a preterm birth. The addition of fetal fibronectin added nothing to the predictive value of the cervical measurement, Dr. Michael Esplin reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“Based on this study, we must conclude that the routine use of self-collected quantitative fetal fibronectin and transvaginal cervical length is not a viable way to screen for preterm birth in a nulliparous population,” said Dr. Esplin of the University of Utah, Salt Lake City.
He reported the results of Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b). The prospective studycomprised more than 9,300 women and was conducted at eight sites in the United States. There were two parts to the investigational screening protocol: collection of a fetal fibronectin swab at three gestational time points (8-14 weeks, 16-22 weeks, and 22-30 weeks) and transvaginal ultrasound to measure cervical length at time of the second and third fibronectin measurement.
The main outcome measure was a live birth at less than 37 weeks, after spontaneous preterm labor; the secondary outcome was a live birth after spontaneous preterm labor at less than 32 weeks’ gestation.
Mean age of the women was 27 years. All the women were carrying a singleton pregnancy. There were 471 spontaneous preterm live births. These were more likely to occur in the youngest and oldest women in the cohort. Preterm births were more common in women who smoked during pregnancy (24% vs. 17%), those who had less than a high school education (11.5% vs. 7.8%), and those with a prepregnancy history of diabetes (3.6% vs. 1.5%).
At the second visit, cervical length of 25 mm or less identified 8% of those who went on to have a preterm birth, for a positive predictive value of 16% and an area under the curve (AUC) of 0.61. At the third visit, cervical length of 25 mm or less identified 24% of women with preterm birth, for a positive predictive value of 15% and an area under the curve of 0.67.
Fetal fibronectin alone performed similarly. No matter what visit, and whether the cutoff was 10, 50, or 200 ng/mL, the AUC stayed between 0.51-0.54. The positive predictive values of these measurements ranged from 6%-12%.
“All of these measures had a relatively low positive predictive value,” Dr. Esplin said. “And while that may be acceptable if the tests are very sensitive, these, in fact were not. Cervical length, for example, had only 7.9% sensitivity at visit 2 and 23% sensitivity at visit 3.”
Combining cervical length and fetal fibronectin did nothing to improve the test’s validity or clinical usefulness. For a test to be clinically useful, Dr. Esplin said, the AUC should be at least 0.73. None of the measures came close to meeting this standard.
The National Institute of Child Health and Human Development sponsored the study. Dr. Esplin reported having no financial disclosures.
ATLANTA – The combination of cervical length and self-collected fetal fibronectin did not accurately predict preterm birth in a cohort of nulliparous women.
Although each measurement in itself had some predictive value, the best measure – cervical length measured by transvaginal ultrasound at 22-30 weeks’ gestation – was only marginally clinically useful, identifying about 24% of those who had a preterm birth. The addition of fetal fibronectin added nothing to the predictive value of the cervical measurement, Dr. Michael Esplin reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“Based on this study, we must conclude that the routine use of self-collected quantitative fetal fibronectin and transvaginal cervical length is not a viable way to screen for preterm birth in a nulliparous population,” said Dr. Esplin of the University of Utah, Salt Lake City.
He reported the results of Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b). The prospective studycomprised more than 9,300 women and was conducted at eight sites in the United States. There were two parts to the investigational screening protocol: collection of a fetal fibronectin swab at three gestational time points (8-14 weeks, 16-22 weeks, and 22-30 weeks) and transvaginal ultrasound to measure cervical length at time of the second and third fibronectin measurement.
The main outcome measure was a live birth at less than 37 weeks, after spontaneous preterm labor; the secondary outcome was a live birth after spontaneous preterm labor at less than 32 weeks’ gestation.
Mean age of the women was 27 years. All the women were carrying a singleton pregnancy. There were 471 spontaneous preterm live births. These were more likely to occur in the youngest and oldest women in the cohort. Preterm births were more common in women who smoked during pregnancy (24% vs. 17%), those who had less than a high school education (11.5% vs. 7.8%), and those with a prepregnancy history of diabetes (3.6% vs. 1.5%).
At the second visit, cervical length of 25 mm or less identified 8% of those who went on to have a preterm birth, for a positive predictive value of 16% and an area under the curve (AUC) of 0.61. At the third visit, cervical length of 25 mm or less identified 24% of women with preterm birth, for a positive predictive value of 15% and an area under the curve of 0.67.
Fetal fibronectin alone performed similarly. No matter what visit, and whether the cutoff was 10, 50, or 200 ng/mL, the AUC stayed between 0.51-0.54. The positive predictive values of these measurements ranged from 6%-12%.
“All of these measures had a relatively low positive predictive value,” Dr. Esplin said. “And while that may be acceptable if the tests are very sensitive, these, in fact were not. Cervical length, for example, had only 7.9% sensitivity at visit 2 and 23% sensitivity at visit 3.”
Combining cervical length and fetal fibronectin did nothing to improve the test’s validity or clinical usefulness. For a test to be clinically useful, Dr. Esplin said, the AUC should be at least 0.73. None of the measures came close to meeting this standard.
The National Institute of Child Health and Human Development sponsored the study. Dr. Esplin reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Transvaginal cervical length plus fetal fibronectin did not predict preterm birth.
Major finding: Cervical length in the late second and early third trimesters was the best predictor of preterm birth, with an AUC of 0.67, but this was not considered clinically useful.
Data source: A prospective study comprising more than 9,300 women.
Disclosures: The National Institute of Child Health and Human Development sponsored the study. Dr. Esplin reported having no financial disclosures.
Risk Score Reliably Predicts Cesarean Delivery
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
AT THE PREGNANCY MEETING
Risk score reliably predicts cesarean delivery
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
ATLANTA – A risk score derived from five maternal and fetal parameters can help determine the overall risk of cesarean delivery in nulliparous women at term, according to findings from the prospective multicenter Genesis Study.
The score can be used to better inform patients of their individualized cesarean delivery risk in early pregnancy and late pregnancy, facilitating patient decision making about place and mode of delivery, Dr. Naomi Burke of the Royal College of Surgeons in Dublin, Ireland, reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Of 2,336 nulliparous women with a vertex presentation after 39 weeks’ gestation who were recruited for the Genesis Study, 491 had an unplanned C-section. On multivariate analysis, several factors were found to be associated with risk for cesarean delivery, and the combination of maternal age, maternal height, body mass index, fetal abdominal circumference, and fetal head circumference were found to be the best combined predictors of cesarean delivery, Dr. Burke said.
At the initial visit, the odds ratios for the maternal parameters were 1.22 for maternal age, -1.59 for maternal height, and 1.32 for body mass index. After 39 weeks’ gestation the odds ratios were 1.21, -1.72, and 1.29 for those parameters, respectively. The odds ratios were 1.23 for fetal abdominal circumference and 1.27 for fetal head circumference.
Individual z scores were calculated for demographic and biometric data to determine the odds ratios and a risk score for cesarean delivery. The individual scores were added to give a total risk score, which was then converted into a probability of cesarean delivery, Dr. Burke explained. The prediction model performed well in a bootstrapped cross-validation study, she said.
Actual outcomes “were almost exactly as predicted” in different risk categories. “For example, in a cohort of 614 women who had a 30%-40% risk of cesarean delivery, the actual cesarean delivery rate was 26%,” she said.
Further, of 52 women with a risk score over 50% for cesarean delivery, the actual rate was 56%. Among 23 women who had a vaginal delivery, 15 required an operative vaginal delivery, 5 had an obstetric anal sphincter injury, and 1 had shoulder dystocia with a fractured clavicle.
“So you can see that although these women avoided intrapartum cesarean, there was still significant maternal and neonatal morbidity associated,” she said.
The findings are important because cesarean delivery rates continue to generate concern and prior efforts to predict risk for unplanned cesarean delivery have failed. Despite extensive research and costly interventions, it has been unclear which women would suffer the greatest difficulty in childbirth, she said.
The current findings could change that.
“We can now tell, using our prediction model, which women are at high risk of unplanned cesarean delivery,” she said, noting that a randomized, controlled trial is already underway to assess how the implementation of this model can be used to assess maternal and neonatal morbidity.
The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no disclosures.
AT THE PREGNANCY MEETING
Key clinical point: A risk score derived from five parameters can help determine the overall risk of cesarean delivery in nulliparous women.
Major finding: Among 52 women with a risk score greater than 50% for cesarean delivery, the actual rate was 56%.
Data source: The prospective, multicenter Genesis study of 2,336 women.
Disclosures: The Genesis study is sponsored by Perinatal Ireland. Dr. Burke reported having no financial disclosures.
Adding azithromycin cuts postcesarean maternal infections
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Prophylactic azithromycin added to standard antibiotics decreased maternal infections after cesarean.
Major finding: The number needed to treat to prevent one postsurgical infection was 17.
Data source: The randomized, placebo-controlled trial comprised 2,013 women.
Disclosures: The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
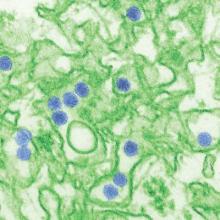
Zika virus in pregnancy linked to hydrops fetalis
Zika virus infection in pregnant women may be linked to hydrops fetalis and fetal demise, according to a case report published online Feb. 25 in PLOS Neglected Tropical Diseases.
A 20-year-old pregnant woman without history or signs of Zika virus infection was referred to the Hospital Geral Roberto Santos in Salvador, Brazil, in the 18th week of gestation because of low fetal weight, but by week 26 and 30, ultrasound examinations showed microcephaly, hydranencephaly, intracranial calcifications, destructive lesions of posterior fossa, and evidence of hydrothorax, ascites, and subcutaneous edema.
Ultrasound examination at week 32 showed fetal demise, and after delivery, researchers found evidence of Zika virus in the brain and in the cerebrospinal and amniotic fluid, but not in the heart, lung, liver, eye, or placenta (PLoS Negl Trop Dis. 2016 Feb 25. doi: 10.1371/journal.pntd.0004517).
“This case report of a fetus provides additional evidence for the link between ZIKV [Zika virus] infection and microcephaly,” wrote Dr. Manoel Sarno of Hospital Geral Roberto Santos, and his coauthors. “Furthermore, it serves as an alert to clinicians that in addition to central nervous system and ophthalmological manifestations, congenital ZIKV infection may cause hydrops fetalis and fetal demise.”
The researchers reported having no financial disclosures.
Zika virus infection in pregnant women may be linked to hydrops fetalis and fetal demise, according to a case report published online Feb. 25 in PLOS Neglected Tropical Diseases.
A 20-year-old pregnant woman without history or signs of Zika virus infection was referred to the Hospital Geral Roberto Santos in Salvador, Brazil, in the 18th week of gestation because of low fetal weight, but by week 26 and 30, ultrasound examinations showed microcephaly, hydranencephaly, intracranial calcifications, destructive lesions of posterior fossa, and evidence of hydrothorax, ascites, and subcutaneous edema.
Ultrasound examination at week 32 showed fetal demise, and after delivery, researchers found evidence of Zika virus in the brain and in the cerebrospinal and amniotic fluid, but not in the heart, lung, liver, eye, or placenta (PLoS Negl Trop Dis. 2016 Feb 25. doi: 10.1371/journal.pntd.0004517).
“This case report of a fetus provides additional evidence for the link between ZIKV [Zika virus] infection and microcephaly,” wrote Dr. Manoel Sarno of Hospital Geral Roberto Santos, and his coauthors. “Furthermore, it serves as an alert to clinicians that in addition to central nervous system and ophthalmological manifestations, congenital ZIKV infection may cause hydrops fetalis and fetal demise.”
The researchers reported having no financial disclosures.
Zika virus infection in pregnant women may be linked to hydrops fetalis and fetal demise, according to a case report published online Feb. 25 in PLOS Neglected Tropical Diseases.
A 20-year-old pregnant woman without history or signs of Zika virus infection was referred to the Hospital Geral Roberto Santos in Salvador, Brazil, in the 18th week of gestation because of low fetal weight, but by week 26 and 30, ultrasound examinations showed microcephaly, hydranencephaly, intracranial calcifications, destructive lesions of posterior fossa, and evidence of hydrothorax, ascites, and subcutaneous edema.
Ultrasound examination at week 32 showed fetal demise, and after delivery, researchers found evidence of Zika virus in the brain and in the cerebrospinal and amniotic fluid, but not in the heart, lung, liver, eye, or placenta (PLoS Negl Trop Dis. 2016 Feb 25. doi: 10.1371/journal.pntd.0004517).
“This case report of a fetus provides additional evidence for the link between ZIKV [Zika virus] infection and microcephaly,” wrote Dr. Manoel Sarno of Hospital Geral Roberto Santos, and his coauthors. “Furthermore, it serves as an alert to clinicians that in addition to central nervous system and ophthalmological manifestations, congenital ZIKV infection may cause hydrops fetalis and fetal demise.”
The researchers reported having no financial disclosures.
FROM PLOS NEGLECTED TROPICAL DISEASES
Key clinical point: Zika virus infection in pregnant women may be associated with hydrops fetalis and fetal demise.
Major finding: Congenital Zika virus infection was associated with microcephaly, hydranencephaly, and fetal demise in a single case.
Data source: Case report of a fetus with congenital Zika virus infection.
Disclosures: The researchers reported having no financial disclosures.
Donor human milk availability to VLBW infants associated with decreased NEC
For very low birth weight infants, the availability of donor human milk to newborns was associated with a decreased incidence of necrotizing enterocolitis and an increased rate of breastfeeding at discharge from a neonatal intensive care unit.
The researchers based their findings on data obtained from the California Perinatal Quality Care Collaborative, which gathers information on the care of greater than 90% of California’s neonatal intensive care unit (NICU) admissions of very low birth weight (VLBW) infants (defined as weighing less than or equal to 1.5 kg at birth), and the Mother’s Milk Bank of San Jose, a human milk bank serving 94 hospitals across several states, including California. All of the data was collected between 2007 and 2013 in over 42,000 VLBW babies. Babies were classified as breastfeeding at discharge, if they were feeding with human milk or human milk with fortifier or formula, but not if they were only feeding with formula.
Agata Kantorowska, a medical student at the University of Rochester (N.Y.) School of Medicine and Dentistry, and her colleagues noted that they did not know if donor human milk (DHM) was used primarily as a back-up feeding if mother’s milk was unavailable, in another way, or in conjunction with human milk-derived fortifiers; the proportion of VLBW infants within each NICU that received DHM; or the length of time that an individual received DHM.
Among the 22 hospitals studied that went from not having DHM available to making it available, on average, the rate of breastfeeding at discharge increased by 10% after DHM became available (P less than .0001). Among these same hospitals, the mean change in necrotizing enterocolitis (NEC) prevalence, following the introduction of DHM, was a 2.6% decrease (P = .0006). Before DHM became available in the 22 hospitals, 52.8% of VLBW infants were breastfeeding at discharge, compared with 61.7% after DHM became available. The rate of NEC was 6.6% among VLBW infants prior to DHM having becoming available at a hospital, versus 4.3% following the introduction of DHM to a hospital.
Following risk adjustment, not having DHM available in a hospital was a negative predictor for breastfeeding at discharge (odds ratio, 0.70) and a positive predictor of NEC (odds ratio, 1.15).
Ms. Kantorowska and her associates said while they found “a significant association between a hospital’s DHM status and increased breastfeeding and decreased NEC rates among VLBW infants,” factors other than the availability of DHM contributed to changes in breastfeeding and NEC rates that occurred. They also noted that they saw an increased rate of breastfeeding and a similar decreasing rate of NEC in hospitals that did not transition to using DHM.
“Societal attitudes toward breastfeeding are likely influencing mothers’ attempts to provide breast milk to their VLBW infants. ... The NICU battle against NEC is ongoing, and other advances in care that occurred from 2007 to 2013 could be contributing to the observed decrease in NEC rate in hospitals that acquired DHM,” the researchers said.
Read the full study in Pediatrics (doi: 10.1542/peds.2015-3123).
For very low birth weight infants, the availability of donor human milk to newborns was associated with a decreased incidence of necrotizing enterocolitis and an increased rate of breastfeeding at discharge from a neonatal intensive care unit.
The researchers based their findings on data obtained from the California Perinatal Quality Care Collaborative, which gathers information on the care of greater than 90% of California’s neonatal intensive care unit (NICU) admissions of very low birth weight (VLBW) infants (defined as weighing less than or equal to 1.5 kg at birth), and the Mother’s Milk Bank of San Jose, a human milk bank serving 94 hospitals across several states, including California. All of the data was collected between 2007 and 2013 in over 42,000 VLBW babies. Babies were classified as breastfeeding at discharge, if they were feeding with human milk or human milk with fortifier or formula, but not if they were only feeding with formula.
Agata Kantorowska, a medical student at the University of Rochester (N.Y.) School of Medicine and Dentistry, and her colleagues noted that they did not know if donor human milk (DHM) was used primarily as a back-up feeding if mother’s milk was unavailable, in another way, or in conjunction with human milk-derived fortifiers; the proportion of VLBW infants within each NICU that received DHM; or the length of time that an individual received DHM.
Among the 22 hospitals studied that went from not having DHM available to making it available, on average, the rate of breastfeeding at discharge increased by 10% after DHM became available (P less than .0001). Among these same hospitals, the mean change in necrotizing enterocolitis (NEC) prevalence, following the introduction of DHM, was a 2.6% decrease (P = .0006). Before DHM became available in the 22 hospitals, 52.8% of VLBW infants were breastfeeding at discharge, compared with 61.7% after DHM became available. The rate of NEC was 6.6% among VLBW infants prior to DHM having becoming available at a hospital, versus 4.3% following the introduction of DHM to a hospital.
Following risk adjustment, not having DHM available in a hospital was a negative predictor for breastfeeding at discharge (odds ratio, 0.70) and a positive predictor of NEC (odds ratio, 1.15).
Ms. Kantorowska and her associates said while they found “a significant association between a hospital’s DHM status and increased breastfeeding and decreased NEC rates among VLBW infants,” factors other than the availability of DHM contributed to changes in breastfeeding and NEC rates that occurred. They also noted that they saw an increased rate of breastfeeding and a similar decreasing rate of NEC in hospitals that did not transition to using DHM.
“Societal attitudes toward breastfeeding are likely influencing mothers’ attempts to provide breast milk to their VLBW infants. ... The NICU battle against NEC is ongoing, and other advances in care that occurred from 2007 to 2013 could be contributing to the observed decrease in NEC rate in hospitals that acquired DHM,” the researchers said.
Read the full study in Pediatrics (doi: 10.1542/peds.2015-3123).
For very low birth weight infants, the availability of donor human milk to newborns was associated with a decreased incidence of necrotizing enterocolitis and an increased rate of breastfeeding at discharge from a neonatal intensive care unit.
The researchers based their findings on data obtained from the California Perinatal Quality Care Collaborative, which gathers information on the care of greater than 90% of California’s neonatal intensive care unit (NICU) admissions of very low birth weight (VLBW) infants (defined as weighing less than or equal to 1.5 kg at birth), and the Mother’s Milk Bank of San Jose, a human milk bank serving 94 hospitals across several states, including California. All of the data was collected between 2007 and 2013 in over 42,000 VLBW babies. Babies were classified as breastfeeding at discharge, if they were feeding with human milk or human milk with fortifier or formula, but not if they were only feeding with formula.
Agata Kantorowska, a medical student at the University of Rochester (N.Y.) School of Medicine and Dentistry, and her colleagues noted that they did not know if donor human milk (DHM) was used primarily as a back-up feeding if mother’s milk was unavailable, in another way, or in conjunction with human milk-derived fortifiers; the proportion of VLBW infants within each NICU that received DHM; or the length of time that an individual received DHM.
Among the 22 hospitals studied that went from not having DHM available to making it available, on average, the rate of breastfeeding at discharge increased by 10% after DHM became available (P less than .0001). Among these same hospitals, the mean change in necrotizing enterocolitis (NEC) prevalence, following the introduction of DHM, was a 2.6% decrease (P = .0006). Before DHM became available in the 22 hospitals, 52.8% of VLBW infants were breastfeeding at discharge, compared with 61.7% after DHM became available. The rate of NEC was 6.6% among VLBW infants prior to DHM having becoming available at a hospital, versus 4.3% following the introduction of DHM to a hospital.
Following risk adjustment, not having DHM available in a hospital was a negative predictor for breastfeeding at discharge (odds ratio, 0.70) and a positive predictor of NEC (odds ratio, 1.15).
Ms. Kantorowska and her associates said while they found “a significant association between a hospital’s DHM status and increased breastfeeding and decreased NEC rates among VLBW infants,” factors other than the availability of DHM contributed to changes in breastfeeding and NEC rates that occurred. They also noted that they saw an increased rate of breastfeeding and a similar decreasing rate of NEC in hospitals that did not transition to using DHM.
“Societal attitudes toward breastfeeding are likely influencing mothers’ attempts to provide breast milk to their VLBW infants. ... The NICU battle against NEC is ongoing, and other advances in care that occurred from 2007 to 2013 could be contributing to the observed decrease in NEC rate in hospitals that acquired DHM,” the researchers said.
Read the full study in Pediatrics (doi: 10.1542/peds.2015-3123).
FROM PEDIATRICS
CDC investigating 14 suspected Zika virus cases
Fourteen new reports of possible sexual transmission of Zika virus are being investigated by health officials in the United States, including several that involve pregnant women.
According to a media statement released by the Centers for Disease Control and Prevention on Feb. 23, in 2 of the 14 suspected cases, Zika virus infection “has been confirmed in women whose only known risk factor was sexual contact with an ill male partner who had recently traveled to an area with local Zika virus transmission; testing for the male partners is still pending.”
Confirmatory tests are pending for four additional suspected sexual transmission events, and the investigation is ongoing for an additional eight suspected cases.
“Like previously reported cases of sexual transmission, these cases involve possible transmission of the virus from men to their sex partners,” the statement reads. “At this time, there is no evidence that women can transmit Zika virus to their sex partners; however, more research is needed to understand this issue.”
In a separate announcement on Feb. 23, the CDC added Trinidad and Tobago and the Marshall Islands to the Zika virus travel notices. A full list of affected countries regions can be found at http://wwwnc.cdc.gov/travel/page/zika-information.
Fourteen new reports of possible sexual transmission of Zika virus are being investigated by health officials in the United States, including several that involve pregnant women.
According to a media statement released by the Centers for Disease Control and Prevention on Feb. 23, in 2 of the 14 suspected cases, Zika virus infection “has been confirmed in women whose only known risk factor was sexual contact with an ill male partner who had recently traveled to an area with local Zika virus transmission; testing for the male partners is still pending.”
Confirmatory tests are pending for four additional suspected sexual transmission events, and the investigation is ongoing for an additional eight suspected cases.
“Like previously reported cases of sexual transmission, these cases involve possible transmission of the virus from men to their sex partners,” the statement reads. “At this time, there is no evidence that women can transmit Zika virus to their sex partners; however, more research is needed to understand this issue.”
In a separate announcement on Feb. 23, the CDC added Trinidad and Tobago and the Marshall Islands to the Zika virus travel notices. A full list of affected countries regions can be found at http://wwwnc.cdc.gov/travel/page/zika-information.
Fourteen new reports of possible sexual transmission of Zika virus are being investigated by health officials in the United States, including several that involve pregnant women.
According to a media statement released by the Centers for Disease Control and Prevention on Feb. 23, in 2 of the 14 suspected cases, Zika virus infection “has been confirmed in women whose only known risk factor was sexual contact with an ill male partner who had recently traveled to an area with local Zika virus transmission; testing for the male partners is still pending.”
Confirmatory tests are pending for four additional suspected sexual transmission events, and the investigation is ongoing for an additional eight suspected cases.
“Like previously reported cases of sexual transmission, these cases involve possible transmission of the virus from men to their sex partners,” the statement reads. “At this time, there is no evidence that women can transmit Zika virus to their sex partners; however, more research is needed to understand this issue.”
In a separate announcement on Feb. 23, the CDC added Trinidad and Tobago and the Marshall Islands to the Zika virus travel notices. A full list of affected countries regions can be found at http://wwwnc.cdc.gov/travel/page/zika-information.
Treating influenza: A guide to antiviral safety in pregnancy
Oseltamivir and zanamivir are competitive inhibitors for the neuraminidase enzyme for the influenza virus. They block the surface receptor enzyme and prevent release of virus from the host cell, thus limiting propagation of the infection. These medications can be given as prophylaxis after exposure to influenza or can be given therapeutically for a suspected or confirmed infection. Oseltamivir is recommended for treatment of suspected or confirmed influenza infection in the special population of pregnant women, as the risk for complications of influenza is increased in this group.
Safety evidence
However, there are limited data on the safety and efficacy of the neuraminidase inhibitors in pregnancy. With respect to safety, there have been seven publications in the literature addressing the risk for major birth defects following treatment or prophylaxis with one or both of these products, with the majority of the published data relating to oseltamivir exposure.
In a review by Tanaka et al. in 2009, 90 pregnancies treated therapeutically with oseltamivir in the first trimester were reported to two teratogen information services in Japan; one major birth defect (1.1%) was reported (CMAJ. 2009 Jul 7;181[1-2]:55-8). A year later, Greer et al. published a retrospective chart review at a Texas hospital between 2003 and 2008. During that period, 137 pregnancies that involved a pharmacy record of dispensing of oseltamivir were identified. Of these, 18 were dispensed in the first trimester, and none were linked to a major birth defect outcome (Obstet Gynecol. 2010 Apr;115[4]:711-6).
A 2011 record linkage study in Sweden identified 86 pregnant women for whom oseltamivir (n=81) or zanamivir had been prescribed. Of these, four were linked to a major birth defect in the infant; however, only one of the four prescriptions had been filled in the first trimester (Pharmacoepidemiol Drug Saf. 2011 Oct;20[10]:1030-4). In 2013, Saito et al. reported on a case series gathered from 157 obstetric facilities in Japan. Among 156 infants born to women exposed to oseltamivir in the first trimester, 2 (1.3%) were reported to have a major congenital anomaly; there were no congenital malformations reported in the 15 first-trimester exposures to zanamivir (Am J Obstet Gynecol. 2013 Aug;209[2[:130.e1-9).
In 2014, a teratogen information service in the United Kingdom reported on eight first-trimester exposures to oseltamivir and 37 to zanamivir, with no major birth defects noted in either group (BJOG. 2014 Jun;121[7]:901-6). Additionally, a French prescription database study identified 49 pregnancies thought to be exposed to oseltamivir in the first trimester with one reported congenital anomaly (BJOG. 2014 Jun;121[7]:895-900).
Finally, the manufacturer of oseltamivir published a summary of pregnancies from global pharmacovigilance data accumulated through spontaneous reports and other studies between 2000 and 2012 (Pharmacoepidemiol Drug Saf. 2014 Oct;23[10]:1035-42). Outcomes were available for 1,875 infants. Among these, 81 (4.3%) had major birth defects. However, following case review, the authors indicated that only 11 of the defects (occurring in 9 infants) were biologically plausible based on the timing of the exposure to oseltamivir.
Efficacy examined
With respect to efficacy, two small studies have addressed the pharmacokinetics of oseltamivir in pregnancy to determine if the recommended dosages for nonpregnant individuals are appropriate for pregnancy.
In the earlier of the two studies, Greer et al. looked at the pharmacokinetics of oseltamivir in 30 pregnant women, 10 in each of the three trimesters, who were taking 75 mg of the drug either once or twice daily. Maternal samples were drawn before and after the first dose of oseltamivir. They found little evidence of differences across the three trimesters and concluded that the parent drug values were in the pharmacologic range for clinical efficacy (Am J Obstet Gynecol. 2011 Jun;204[6 Suppl 1]:S89-93).
In contrast, Pillai et al. enrolled a small sample of women being treated with oseltamivir; they evaluated pharmacokinetics for the active metabolite of oseltamivir following 48 or more hours of treatment in 29 pregnant and 35 nonpregnant women (Br J Clin Pharmacol. 2015 Nov;80[5]:1042-50). Significantly lower levels of the active metabolite were noted in the pregnant women, compared with nonpregnant women. The authors suggested that the physiologic changes of pregnancy, correlated with increased renal clearance, produced an approximate 30% lower exposure to the drug in the pregnant state. While they were not able to relate this to maternal or infant outcomes, this finding suggested that further work is needed to determine if dosing recommendations should be adjusted in pregnancy.
The current recommendation is that pregnant women or women within 2 weeks post partum be given oseltamivir for treatment of suspected or confirmed influenza regardless of trimester of pregnancy. The limited safety data that are currently available have not suggested an increased risk for major birth defects following treatment with this product. However, the data are sparse for oseltamivir and even more so for zanamivir. Larger studies focused on these treatments are needed.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She reported having no financial disclosures relevant to this column, but has received research funding Roche-Genentech and GlaxoSmithKline unrelated to antiviral medications. Email her at [email protected].
Oseltamivir and zanamivir are competitive inhibitors for the neuraminidase enzyme for the influenza virus. They block the surface receptor enzyme and prevent release of virus from the host cell, thus limiting propagation of the infection. These medications can be given as prophylaxis after exposure to influenza or can be given therapeutically for a suspected or confirmed infection. Oseltamivir is recommended for treatment of suspected or confirmed influenza infection in the special population of pregnant women, as the risk for complications of influenza is increased in this group.
Safety evidence
However, there are limited data on the safety and efficacy of the neuraminidase inhibitors in pregnancy. With respect to safety, there have been seven publications in the literature addressing the risk for major birth defects following treatment or prophylaxis with one or both of these products, with the majority of the published data relating to oseltamivir exposure.
In a review by Tanaka et al. in 2009, 90 pregnancies treated therapeutically with oseltamivir in the first trimester were reported to two teratogen information services in Japan; one major birth defect (1.1%) was reported (CMAJ. 2009 Jul 7;181[1-2]:55-8). A year later, Greer et al. published a retrospective chart review at a Texas hospital between 2003 and 2008. During that period, 137 pregnancies that involved a pharmacy record of dispensing of oseltamivir were identified. Of these, 18 were dispensed in the first trimester, and none were linked to a major birth defect outcome (Obstet Gynecol. 2010 Apr;115[4]:711-6).
A 2011 record linkage study in Sweden identified 86 pregnant women for whom oseltamivir (n=81) or zanamivir had been prescribed. Of these, four were linked to a major birth defect in the infant; however, only one of the four prescriptions had been filled in the first trimester (Pharmacoepidemiol Drug Saf. 2011 Oct;20[10]:1030-4). In 2013, Saito et al. reported on a case series gathered from 157 obstetric facilities in Japan. Among 156 infants born to women exposed to oseltamivir in the first trimester, 2 (1.3%) were reported to have a major congenital anomaly; there were no congenital malformations reported in the 15 first-trimester exposures to zanamivir (Am J Obstet Gynecol. 2013 Aug;209[2[:130.e1-9).
In 2014, a teratogen information service in the United Kingdom reported on eight first-trimester exposures to oseltamivir and 37 to zanamivir, with no major birth defects noted in either group (BJOG. 2014 Jun;121[7]:901-6). Additionally, a French prescription database study identified 49 pregnancies thought to be exposed to oseltamivir in the first trimester with one reported congenital anomaly (BJOG. 2014 Jun;121[7]:895-900).
Finally, the manufacturer of oseltamivir published a summary of pregnancies from global pharmacovigilance data accumulated through spontaneous reports and other studies between 2000 and 2012 (Pharmacoepidemiol Drug Saf. 2014 Oct;23[10]:1035-42). Outcomes were available for 1,875 infants. Among these, 81 (4.3%) had major birth defects. However, following case review, the authors indicated that only 11 of the defects (occurring in 9 infants) were biologically plausible based on the timing of the exposure to oseltamivir.
Efficacy examined
With respect to efficacy, two small studies have addressed the pharmacokinetics of oseltamivir in pregnancy to determine if the recommended dosages for nonpregnant individuals are appropriate for pregnancy.
In the earlier of the two studies, Greer et al. looked at the pharmacokinetics of oseltamivir in 30 pregnant women, 10 in each of the three trimesters, who were taking 75 mg of the drug either once or twice daily. Maternal samples were drawn before and after the first dose of oseltamivir. They found little evidence of differences across the three trimesters and concluded that the parent drug values were in the pharmacologic range for clinical efficacy (Am J Obstet Gynecol. 2011 Jun;204[6 Suppl 1]:S89-93).
In contrast, Pillai et al. enrolled a small sample of women being treated with oseltamivir; they evaluated pharmacokinetics for the active metabolite of oseltamivir following 48 or more hours of treatment in 29 pregnant and 35 nonpregnant women (Br J Clin Pharmacol. 2015 Nov;80[5]:1042-50). Significantly lower levels of the active metabolite were noted in the pregnant women, compared with nonpregnant women. The authors suggested that the physiologic changes of pregnancy, correlated with increased renal clearance, produced an approximate 30% lower exposure to the drug in the pregnant state. While they were not able to relate this to maternal or infant outcomes, this finding suggested that further work is needed to determine if dosing recommendations should be adjusted in pregnancy.
The current recommendation is that pregnant women or women within 2 weeks post partum be given oseltamivir for treatment of suspected or confirmed influenza regardless of trimester of pregnancy. The limited safety data that are currently available have not suggested an increased risk for major birth defects following treatment with this product. However, the data are sparse for oseltamivir and even more so for zanamivir. Larger studies focused on these treatments are needed.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She reported having no financial disclosures relevant to this column, but has received research funding Roche-Genentech and GlaxoSmithKline unrelated to antiviral medications. Email her at [email protected].
Oseltamivir and zanamivir are competitive inhibitors for the neuraminidase enzyme for the influenza virus. They block the surface receptor enzyme and prevent release of virus from the host cell, thus limiting propagation of the infection. These medications can be given as prophylaxis after exposure to influenza or can be given therapeutically for a suspected or confirmed infection. Oseltamivir is recommended for treatment of suspected or confirmed influenza infection in the special population of pregnant women, as the risk for complications of influenza is increased in this group.
Safety evidence
However, there are limited data on the safety and efficacy of the neuraminidase inhibitors in pregnancy. With respect to safety, there have been seven publications in the literature addressing the risk for major birth defects following treatment or prophylaxis with one or both of these products, with the majority of the published data relating to oseltamivir exposure.
In a review by Tanaka et al. in 2009, 90 pregnancies treated therapeutically with oseltamivir in the first trimester were reported to two teratogen information services in Japan; one major birth defect (1.1%) was reported (CMAJ. 2009 Jul 7;181[1-2]:55-8). A year later, Greer et al. published a retrospective chart review at a Texas hospital between 2003 and 2008. During that period, 137 pregnancies that involved a pharmacy record of dispensing of oseltamivir were identified. Of these, 18 were dispensed in the first trimester, and none were linked to a major birth defect outcome (Obstet Gynecol. 2010 Apr;115[4]:711-6).
A 2011 record linkage study in Sweden identified 86 pregnant women for whom oseltamivir (n=81) or zanamivir had been prescribed. Of these, four were linked to a major birth defect in the infant; however, only one of the four prescriptions had been filled in the first trimester (Pharmacoepidemiol Drug Saf. 2011 Oct;20[10]:1030-4). In 2013, Saito et al. reported on a case series gathered from 157 obstetric facilities in Japan. Among 156 infants born to women exposed to oseltamivir in the first trimester, 2 (1.3%) were reported to have a major congenital anomaly; there were no congenital malformations reported in the 15 first-trimester exposures to zanamivir (Am J Obstet Gynecol. 2013 Aug;209[2[:130.e1-9).
In 2014, a teratogen information service in the United Kingdom reported on eight first-trimester exposures to oseltamivir and 37 to zanamivir, with no major birth defects noted in either group (BJOG. 2014 Jun;121[7]:901-6). Additionally, a French prescription database study identified 49 pregnancies thought to be exposed to oseltamivir in the first trimester with one reported congenital anomaly (BJOG. 2014 Jun;121[7]:895-900).
Finally, the manufacturer of oseltamivir published a summary of pregnancies from global pharmacovigilance data accumulated through spontaneous reports and other studies between 2000 and 2012 (Pharmacoepidemiol Drug Saf. 2014 Oct;23[10]:1035-42). Outcomes were available for 1,875 infants. Among these, 81 (4.3%) had major birth defects. However, following case review, the authors indicated that only 11 of the defects (occurring in 9 infants) were biologically plausible based on the timing of the exposure to oseltamivir.
Efficacy examined
With respect to efficacy, two small studies have addressed the pharmacokinetics of oseltamivir in pregnancy to determine if the recommended dosages for nonpregnant individuals are appropriate for pregnancy.
In the earlier of the two studies, Greer et al. looked at the pharmacokinetics of oseltamivir in 30 pregnant women, 10 in each of the three trimesters, who were taking 75 mg of the drug either once or twice daily. Maternal samples were drawn before and after the first dose of oseltamivir. They found little evidence of differences across the three trimesters and concluded that the parent drug values were in the pharmacologic range for clinical efficacy (Am J Obstet Gynecol. 2011 Jun;204[6 Suppl 1]:S89-93).
In contrast, Pillai et al. enrolled a small sample of women being treated with oseltamivir; they evaluated pharmacokinetics for the active metabolite of oseltamivir following 48 or more hours of treatment in 29 pregnant and 35 nonpregnant women (Br J Clin Pharmacol. 2015 Nov;80[5]:1042-50). Significantly lower levels of the active metabolite were noted in the pregnant women, compared with nonpregnant women. The authors suggested that the physiologic changes of pregnancy, correlated with increased renal clearance, produced an approximate 30% lower exposure to the drug in the pregnant state. While they were not able to relate this to maternal or infant outcomes, this finding suggested that further work is needed to determine if dosing recommendations should be adjusted in pregnancy.
The current recommendation is that pregnant women or women within 2 weeks post partum be given oseltamivir for treatment of suspected or confirmed influenza regardless of trimester of pregnancy. The limited safety data that are currently available have not suggested an increased risk for major birth defects following treatment with this product. However, the data are sparse for oseltamivir and even more so for zanamivir. Larger studies focused on these treatments are needed.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She reported having no financial disclosures relevant to this column, but has received research funding Roche-Genentech and GlaxoSmithKline unrelated to antiviral medications. Email her at [email protected].
Cardiovascular Abnormalities Persist After Preeclamptic Pregnancy
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
FROM HYPERTENSION
Cardiovascular abnormalities persist after preeclamptic pregnancy
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
For 12-18 months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy, according to a case-control study published online Feb. 22 in Hypertension.
If these findings are confirmed in further studies, it might become possible to identify women at high risk for recurrent preeclampsia by performing a cardiovascular assessment before they attempt a second pregnancy, said Dr. Herbert Valensise of the department of obstetrics and gynecology, Tor Vergata University, Rome, and his associates.
An estimated 3%-8% of pregnancies are complicated by preeclampsia, and women who have preeclampsia once are seven times more likely to have a recurrence in subsequent pregnancies than are women who never had the disorder. At present, it is difficult to predict which women will have a recurrence. The investigators assessed cardiac function in women who had completed a first pregnancy and had not yet attempted a second pregnancy; 75 of these women had early preeclampsia during their initial pregnancies and were compared with 147 control subjects who did not. All these study participants were then followed through their second pregnancies to determine whether preeclampsia recurred.
The 22 women who had recurrent preeclampsia in their second pregnancies showed several cardiovascular abnormalities during the nonpregnant state, compared with the control subjects and the 53 women who did not develop preeclampsia in their second pregnancies. The affected women had lower stroke volume (63 mL vs. 73 mL and 70 mL, respectively), elevated total vascular resistance (1,638 vs. 1,341 and 1,383 dyne·s−1·cm−5), lower cardiac output (4.6 vs. 5.3 and 5.2 L), higher diastolic blood pressure (77 vs. 68 and 69 mm Hg), greater thickness of the left-ventricular wall (35 vs. 28 and 33), and “a tendency to a concentric geometry of the left ventricle,” Dr. Valensise and his associates said. All differences were statistically significant at P less than .05 (Hypertension. 2016 Feb 22. doi: 10.1161/HYPERTENSIONAHA.115.06674).
These findings “suggest that cardiac dysfunction and cardiovascular maladaptation precede the appearance of a recurrent preeclampsia months before a second pregnancy,” they said.
The preeclampsia during the first pregnancy was no more severe among women who had a recurrence than it was among the women who did not, so the severity of the first episode was not a useful guide for predicting recurrence, the investigators added.
No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.
FROM HYPERTENSION
Key clinical point: For months following a preeclamptic pregnancy, cardiovascular abnormalities persist in some women and appear to raise their risk for recurrent preeclampsia in a subsequent pregnancy.
Major finding: In the nonpregnant state, women who went on to develop recurrent preeclampsia showed elevated total vascular resistance, lower cardiac output, higher diastolic blood pressure, greater thickness of the left-ventricular wall, and concentric geometry of the left ventricle.
Data source: A case-control study comparing CV abnormalities between 75 nonpregnant women who had preeclampsia during a previous pregnancy and 147 control subjects who did not.
Disclosures: No funding source was identified for this study. Dr. Valensise and his associates reported having no relevant financial disclosures.