User login
Supreme Court reprieve lets 10 Texas abortion clinics stay open for now
June 30 would have been the last day of operation for 10 Texas clinics that provide abortion. But on June 29 the U.S. Supreme Court, in one of its final actions this session, said the clinics can remain open while clinic lawyers ask the court for a full review of a strict abortion law.
Two dozen states have passed regulations similar to the ones being fought over in Texas.
Two years ago, when Texas passed one of the toughest laws in the country regarding abortion, the number of clinics offering the procedure dropped from 41 to 19. Amy Hagstrom Miller, chief executive of Whole Woman’s Health, has already closed two clinics in Texas because of the law and was about to close two more.
“Honestly I just can’t stop smiling,” Ms. Hagstrom Miller said. “It’s been so much up and down … so much uncertainty for my team and the women that we serve.”
The Texas law says doctors who perform abortions must have admitting privileges at a nearby hospital. But some hospitals are reluctant to grant those privileges because of religious reasons or because abortion is so controversial.
The law also requires that clinics meet the same standards as outpatient surgery centers. Those upgrades can cost $1 million or more.
“It’s an example of the rash of laws … that have taken a sneaky approach by enacting regulations that pretend to be about health and safety but are actually designed to close down clinics,” said Nancy Northrup, chief executive of the Center for Reproductive Rights, which is representing clinics in their fight to overturn the Texas law.
Supporters of the law said every woman deserves good medical care whatever the procedure.
“While we hope that she would not be compelled to choose abortion, we hope that her life would of course not be at risk should she choose to do that,” said Emily Horne of Texas Right to Life. “Pro-life does not just mean care for the life of the unborn child; it’s care for the life of the woman undergoing the abortion as well.”
The law has had a drastic effect in Texas, the country’s second most populous state, leaving most of the remaining clinics in major cities.
There’s just one clinic left along the Mexican border and one in far west El Paso – they were among the nine about to shut down.
If they had closed, the women there faced round-trips of 300 miles or more to get an abortion.
Ms. Hagstrom Miller said all these clinic rules and the doctor restrictions are a deliberate strategy waged by antiabortion groups. “They’re going state by state by state,” she said. “They can’t make it illegal, so they’re basically making it completely inaccessible.”
Other states that have passed similar laws are also facing legal challenges.
Ms. Horne of Texas Right to Life said her group would welcome a legal review by the U.S. Supreme Court.
“With this case, issuing some more guidance on that could be very helpful for the pro-life movement in determining what courses to pursue, which laws they might pass in other states in the future,” she said.
The clinics in Texas can stay open at least until the fall. If the court decides to take the case, it would hear arguments in its next term that starts in October.
This story is part of a reporting partnership that includes Houston Public Media, NPR, and Kaiser Health News.
Kaiser Health News (KHN) is a nonprofit national health policy news service.
June 30 would have been the last day of operation for 10 Texas clinics that provide abortion. But on June 29 the U.S. Supreme Court, in one of its final actions this session, said the clinics can remain open while clinic lawyers ask the court for a full review of a strict abortion law.
Two dozen states have passed regulations similar to the ones being fought over in Texas.
Two years ago, when Texas passed one of the toughest laws in the country regarding abortion, the number of clinics offering the procedure dropped from 41 to 19. Amy Hagstrom Miller, chief executive of Whole Woman’s Health, has already closed two clinics in Texas because of the law and was about to close two more.
“Honestly I just can’t stop smiling,” Ms. Hagstrom Miller said. “It’s been so much up and down … so much uncertainty for my team and the women that we serve.”
The Texas law says doctors who perform abortions must have admitting privileges at a nearby hospital. But some hospitals are reluctant to grant those privileges because of religious reasons or because abortion is so controversial.
The law also requires that clinics meet the same standards as outpatient surgery centers. Those upgrades can cost $1 million or more.
“It’s an example of the rash of laws … that have taken a sneaky approach by enacting regulations that pretend to be about health and safety but are actually designed to close down clinics,” said Nancy Northrup, chief executive of the Center for Reproductive Rights, which is representing clinics in their fight to overturn the Texas law.
Supporters of the law said every woman deserves good medical care whatever the procedure.
“While we hope that she would not be compelled to choose abortion, we hope that her life would of course not be at risk should she choose to do that,” said Emily Horne of Texas Right to Life. “Pro-life does not just mean care for the life of the unborn child; it’s care for the life of the woman undergoing the abortion as well.”
The law has had a drastic effect in Texas, the country’s second most populous state, leaving most of the remaining clinics in major cities.
There’s just one clinic left along the Mexican border and one in far west El Paso – they were among the nine about to shut down.
If they had closed, the women there faced round-trips of 300 miles or more to get an abortion.
Ms. Hagstrom Miller said all these clinic rules and the doctor restrictions are a deliberate strategy waged by antiabortion groups. “They’re going state by state by state,” she said. “They can’t make it illegal, so they’re basically making it completely inaccessible.”
Other states that have passed similar laws are also facing legal challenges.
Ms. Horne of Texas Right to Life said her group would welcome a legal review by the U.S. Supreme Court.
“With this case, issuing some more guidance on that could be very helpful for the pro-life movement in determining what courses to pursue, which laws they might pass in other states in the future,” she said.
The clinics in Texas can stay open at least until the fall. If the court decides to take the case, it would hear arguments in its next term that starts in October.
This story is part of a reporting partnership that includes Houston Public Media, NPR, and Kaiser Health News.
Kaiser Health News (KHN) is a nonprofit national health policy news service.
June 30 would have been the last day of operation for 10 Texas clinics that provide abortion. But on June 29 the U.S. Supreme Court, in one of its final actions this session, said the clinics can remain open while clinic lawyers ask the court for a full review of a strict abortion law.
Two dozen states have passed regulations similar to the ones being fought over in Texas.
Two years ago, when Texas passed one of the toughest laws in the country regarding abortion, the number of clinics offering the procedure dropped from 41 to 19. Amy Hagstrom Miller, chief executive of Whole Woman’s Health, has already closed two clinics in Texas because of the law and was about to close two more.
“Honestly I just can’t stop smiling,” Ms. Hagstrom Miller said. “It’s been so much up and down … so much uncertainty for my team and the women that we serve.”
The Texas law says doctors who perform abortions must have admitting privileges at a nearby hospital. But some hospitals are reluctant to grant those privileges because of religious reasons or because abortion is so controversial.
The law also requires that clinics meet the same standards as outpatient surgery centers. Those upgrades can cost $1 million or more.
“It’s an example of the rash of laws … that have taken a sneaky approach by enacting regulations that pretend to be about health and safety but are actually designed to close down clinics,” said Nancy Northrup, chief executive of the Center for Reproductive Rights, which is representing clinics in their fight to overturn the Texas law.
Supporters of the law said every woman deserves good medical care whatever the procedure.
“While we hope that she would not be compelled to choose abortion, we hope that her life would of course not be at risk should she choose to do that,” said Emily Horne of Texas Right to Life. “Pro-life does not just mean care for the life of the unborn child; it’s care for the life of the woman undergoing the abortion as well.”
The law has had a drastic effect in Texas, the country’s second most populous state, leaving most of the remaining clinics in major cities.
There’s just one clinic left along the Mexican border and one in far west El Paso – they were among the nine about to shut down.
If they had closed, the women there faced round-trips of 300 miles or more to get an abortion.
Ms. Hagstrom Miller said all these clinic rules and the doctor restrictions are a deliberate strategy waged by antiabortion groups. “They’re going state by state by state,” she said. “They can’t make it illegal, so they’re basically making it completely inaccessible.”
Other states that have passed similar laws are also facing legal challenges.
Ms. Horne of Texas Right to Life said her group would welcome a legal review by the U.S. Supreme Court.
“With this case, issuing some more guidance on that could be very helpful for the pro-life movement in determining what courses to pursue, which laws they might pass in other states in the future,” she said.
The clinics in Texas can stay open at least until the fall. If the court decides to take the case, it would hear arguments in its next term that starts in October.
This story is part of a reporting partnership that includes Houston Public Media, NPR, and Kaiser Health News.
Kaiser Health News (KHN) is a nonprofit national health policy news service.
Cuba eliminates mother-to-child transmission of HIV, syphilis
Cuba has become the first country to receive official validation from the World Health Organization that it has eliminated mother-to-child transmission of HIV and syphilis – an achievement that officials credit to a long-standing tradition of universal health care coverage and access in the island nation.
“This historic achievement was made possible by a health system that provides equitable, integrated health services based on primary health care that include difficult and complex interventions like those required for prevention of mother-to-child transmission of HIV and syphilis,” Dr. Carissa F. Etienne, director of the Pan American Health Organization (PAHO), WHO’s Regional Office of the Americas, said during a press briefing.
Cuba’s success demonstrates that universal access and universal health coverage are feasible and are, indeed, the key to success, even against challenges as daunting as HIV, she added.
Several other countries are also poised to request validation of the elimination of vertical HIV and syphilis transmission – defined as fewer than two cases of HIV in every 100 babies born to women with HIV and fewer than one case of syphilis for every 2,000 live births, according to Dr. Etienne.
Even some larger countries – including the United States and Canada – may have also achieved elimination of vertical transmission of HIV and syphilis, but they have not requested validation yet, she said.
The validation process is rigorous and requires a visit by an international panel of experts convened by PAHO/WHO; in Cuba, the panel spent several days visiting health centers, laboratories, and government offices, and also interviewed health officials and other key players, paying particular attention to human rights issues.
Validation requires that impact indicators (such as achieving fewer than 50 cases of new pediatric infections caused by mother-to-child transmissions per 100,000 live births and an HIV transmission rate of less than 5% in breastfeeding populations and less than 2% in non–breastfeeding populations) be met for at least a year. Additionally, process indicators, (95% of pregnant women receiving an antenatal visit, knowing their HIV status and/or being tested for syphilis, and receiving appropriate treatment) must be met for at least 2 years.
Cuba, which has been part of a regional initiative led by PAHO and WHO to eliminate vertical transmission of HIV and syphilis, achieved its goal by ensuring early access to prenatal care, HIV and syphilis testing for pregnant women and their partners, treatment for those who test positive and their babies, substitution of breastfeeding among those affected, and prevention of HIV and syphilis before and during pregnancy through promotion of condoms use and other measures.
Cuba, and any country that receives validation of elimination must maintain ongoing programs to ensure continued success.
Every year, an estimated 1.4 million women living with HIV become pregnant. If untreated, they have a 15%-45% chance of transmitting the virus to their children during pregnancy, labor, delivery, or breast-feeding. That risk drops to just over 1% if antiretroviral medicines are given to both mothers and children throughout the stages when infection can occur, according to PAHO/WHO, which noted in a press release that the number of children born annually with HIV has almost halved since 2009 – down from 400,000 to 240,000 in 2013.
However, stepped-up efforts will be needed to reach the global target of less than 40,000 new child infections per year.
“To achieve that, we need a final push to ensure that all pregnant women have access to sexual and reproductive health services that include HIV and syphilis testing and antiretroviral and penicillin treatment,” Dr. Etienne said. “Treatment is essential to save women’s lives, to clear maternal syphilis, and to reduce the chances that mothers will transmit these infections to their babies.”
Cuba has become the first country to receive official validation from the World Health Organization that it has eliminated mother-to-child transmission of HIV and syphilis – an achievement that officials credit to a long-standing tradition of universal health care coverage and access in the island nation.
“This historic achievement was made possible by a health system that provides equitable, integrated health services based on primary health care that include difficult and complex interventions like those required for prevention of mother-to-child transmission of HIV and syphilis,” Dr. Carissa F. Etienne, director of the Pan American Health Organization (PAHO), WHO’s Regional Office of the Americas, said during a press briefing.
Cuba’s success demonstrates that universal access and universal health coverage are feasible and are, indeed, the key to success, even against challenges as daunting as HIV, she added.
Several other countries are also poised to request validation of the elimination of vertical HIV and syphilis transmission – defined as fewer than two cases of HIV in every 100 babies born to women with HIV and fewer than one case of syphilis for every 2,000 live births, according to Dr. Etienne.
Even some larger countries – including the United States and Canada – may have also achieved elimination of vertical transmission of HIV and syphilis, but they have not requested validation yet, she said.
The validation process is rigorous and requires a visit by an international panel of experts convened by PAHO/WHO; in Cuba, the panel spent several days visiting health centers, laboratories, and government offices, and also interviewed health officials and other key players, paying particular attention to human rights issues.
Validation requires that impact indicators (such as achieving fewer than 50 cases of new pediatric infections caused by mother-to-child transmissions per 100,000 live births and an HIV transmission rate of less than 5% in breastfeeding populations and less than 2% in non–breastfeeding populations) be met for at least a year. Additionally, process indicators, (95% of pregnant women receiving an antenatal visit, knowing their HIV status and/or being tested for syphilis, and receiving appropriate treatment) must be met for at least 2 years.
Cuba, which has been part of a regional initiative led by PAHO and WHO to eliminate vertical transmission of HIV and syphilis, achieved its goal by ensuring early access to prenatal care, HIV and syphilis testing for pregnant women and their partners, treatment for those who test positive and their babies, substitution of breastfeeding among those affected, and prevention of HIV and syphilis before and during pregnancy through promotion of condoms use and other measures.
Cuba, and any country that receives validation of elimination must maintain ongoing programs to ensure continued success.
Every year, an estimated 1.4 million women living with HIV become pregnant. If untreated, they have a 15%-45% chance of transmitting the virus to their children during pregnancy, labor, delivery, or breast-feeding. That risk drops to just over 1% if antiretroviral medicines are given to both mothers and children throughout the stages when infection can occur, according to PAHO/WHO, which noted in a press release that the number of children born annually with HIV has almost halved since 2009 – down from 400,000 to 240,000 in 2013.
However, stepped-up efforts will be needed to reach the global target of less than 40,000 new child infections per year.
“To achieve that, we need a final push to ensure that all pregnant women have access to sexual and reproductive health services that include HIV and syphilis testing and antiretroviral and penicillin treatment,” Dr. Etienne said. “Treatment is essential to save women’s lives, to clear maternal syphilis, and to reduce the chances that mothers will transmit these infections to their babies.”
Cuba has become the first country to receive official validation from the World Health Organization that it has eliminated mother-to-child transmission of HIV and syphilis – an achievement that officials credit to a long-standing tradition of universal health care coverage and access in the island nation.
“This historic achievement was made possible by a health system that provides equitable, integrated health services based on primary health care that include difficult and complex interventions like those required for prevention of mother-to-child transmission of HIV and syphilis,” Dr. Carissa F. Etienne, director of the Pan American Health Organization (PAHO), WHO’s Regional Office of the Americas, said during a press briefing.
Cuba’s success demonstrates that universal access and universal health coverage are feasible and are, indeed, the key to success, even against challenges as daunting as HIV, she added.
Several other countries are also poised to request validation of the elimination of vertical HIV and syphilis transmission – defined as fewer than two cases of HIV in every 100 babies born to women with HIV and fewer than one case of syphilis for every 2,000 live births, according to Dr. Etienne.
Even some larger countries – including the United States and Canada – may have also achieved elimination of vertical transmission of HIV and syphilis, but they have not requested validation yet, she said.
The validation process is rigorous and requires a visit by an international panel of experts convened by PAHO/WHO; in Cuba, the panel spent several days visiting health centers, laboratories, and government offices, and also interviewed health officials and other key players, paying particular attention to human rights issues.
Validation requires that impact indicators (such as achieving fewer than 50 cases of new pediatric infections caused by mother-to-child transmissions per 100,000 live births and an HIV transmission rate of less than 5% in breastfeeding populations and less than 2% in non–breastfeeding populations) be met for at least a year. Additionally, process indicators, (95% of pregnant women receiving an antenatal visit, knowing their HIV status and/or being tested for syphilis, and receiving appropriate treatment) must be met for at least 2 years.
Cuba, which has been part of a regional initiative led by PAHO and WHO to eliminate vertical transmission of HIV and syphilis, achieved its goal by ensuring early access to prenatal care, HIV and syphilis testing for pregnant women and their partners, treatment for those who test positive and their babies, substitution of breastfeeding among those affected, and prevention of HIV and syphilis before and during pregnancy through promotion of condoms use and other measures.
Cuba, and any country that receives validation of elimination must maintain ongoing programs to ensure continued success.
Every year, an estimated 1.4 million women living with HIV become pregnant. If untreated, they have a 15%-45% chance of transmitting the virus to their children during pregnancy, labor, delivery, or breast-feeding. That risk drops to just over 1% if antiretroviral medicines are given to both mothers and children throughout the stages when infection can occur, according to PAHO/WHO, which noted in a press release that the number of children born annually with HIV has almost halved since 2009 – down from 400,000 to 240,000 in 2013.
However, stepped-up efforts will be needed to reach the global target of less than 40,000 new child infections per year.
“To achieve that, we need a final push to ensure that all pregnant women have access to sexual and reproductive health services that include HIV and syphilis testing and antiretroviral and penicillin treatment,” Dr. Etienne said. “Treatment is essential to save women’s lives, to clear maternal syphilis, and to reduce the chances that mothers will transmit these infections to their babies.”
ACOG, SMFM cautious on wider use of cell-free DNA screening
Conventional prenatal screening methods are still the gold standard for most pregnant women despite the availability of cell-free DNA screening for aneuploidy, according to a consensus statement from the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine.
The two organizations cited the limits of cell-free DNA screening performance and the limited data on cost effectiveness in the low-risk obstetric population for encouraging ob.gyns. to stick with conventional screening methods in the general obstetric population.
After cell-free DNA analysis became clinically available in 2011, ACOG and SMFM recommended it for women at increased risk of fetal aneuploidy, including women 35 years or older, fetuses with ultrasonographic findings indicative of an increased risk of aneuploidy, women with a history of trisomy-affected offspring, a parent carrying a balanced robertsonian translocation with an increased risk of trisomy 13 or trisomy 21, and women with positive first-trimester or second-trimester screening test results.
And in a 2012 joint committee opinion, ACOG and SMFM said that cell-free DNA testing should not be offered to low-risk women or women with multiple gestations because it hadn’t been sufficiently studied.
The updated committee opinion, outlines the pros and cons of using cell-free DNA screening in the general obstetric population.
“Patients should be counseled that cell-free DNA screening does not replace the precision obtained with diagnostic tests, such as chorionic villus sampling or amniocentesis, and therefore, is limited in its ability to identify all chromosome abnormalities,” the groups wrote in the updated opinion. “Not only can there be false-positive test results, but a positive cell-free DNA test result for aneuploidy does not determine if the trisomy is due to a translocation, which affects the risk of recurrence. If a fetal structural anomaly is identified on ultrasound examination, diagnostic testing should be offered rather than cell-free DNA screening.”
The sensitivity and specificity of the cell-free DNA screen in the general obstetric population are similar to those in high-risk patients. But the positive predictive value is lower in the general population because of the lower prevalence of aneuploidy. “That is, fewer women with a positive test result will actually have an affected fetus, and there will be more false-positive test results,” ACOG and SMFM wrote.
As a result, the revised opinion includes a recommendation specifying that management decisions, including the decision to terminate a pregnancy, should not be based on the results of cell-free DNA screening alone. Further diagnostic testing is now recommended for any patient who receives a positive result on cell-free DNA screening.
Similarly, women whose results are indeterminate, uninterpretable (“no call” result), or not reported at all should receive further genetic counseling and be offered comprehensive ultrasound evaluation and diagnostic testing. And women whose results are negative should be counseled that a negative cell-free DNA test does not ensure a normal pregnancy.
Additionally, most cell-free DNA testing identifies only trisomies 13, 18, and 21, which comprise a smaller proportion of the chromosomal anomalies found in the general obstetric population than among high-risk women. In one study cited in the opinion, up to 17% of clinically significant chromosomal abnormalities would not be detectable by most current cell-free DNA techniques.
The joint opinion now includes a recommendation against routinely using cell-free DNA screening for microdeletion syndromes. And it reminds physicians that cell-free DNA testing also doesn’t assess fetal anomalies such as neural tube defects or ventral wall defects, so patients who undergo cell-free DNA screening should still be offered maternal serum alpha-fetoprotein screening or ultrasound assessment. The latest opinion continues to recommend against the use of cell-free DNA testing for women with multiple gestations.
Conventional prenatal screening methods are still the gold standard for most pregnant women despite the availability of cell-free DNA screening for aneuploidy, according to a consensus statement from the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine.
The two organizations cited the limits of cell-free DNA screening performance and the limited data on cost effectiveness in the low-risk obstetric population for encouraging ob.gyns. to stick with conventional screening methods in the general obstetric population.
After cell-free DNA analysis became clinically available in 2011, ACOG and SMFM recommended it for women at increased risk of fetal aneuploidy, including women 35 years or older, fetuses with ultrasonographic findings indicative of an increased risk of aneuploidy, women with a history of trisomy-affected offspring, a parent carrying a balanced robertsonian translocation with an increased risk of trisomy 13 or trisomy 21, and women with positive first-trimester or second-trimester screening test results.
And in a 2012 joint committee opinion, ACOG and SMFM said that cell-free DNA testing should not be offered to low-risk women or women with multiple gestations because it hadn’t been sufficiently studied.
The updated committee opinion, outlines the pros and cons of using cell-free DNA screening in the general obstetric population.
“Patients should be counseled that cell-free DNA screening does not replace the precision obtained with diagnostic tests, such as chorionic villus sampling or amniocentesis, and therefore, is limited in its ability to identify all chromosome abnormalities,” the groups wrote in the updated opinion. “Not only can there be false-positive test results, but a positive cell-free DNA test result for aneuploidy does not determine if the trisomy is due to a translocation, which affects the risk of recurrence. If a fetal structural anomaly is identified on ultrasound examination, diagnostic testing should be offered rather than cell-free DNA screening.”
The sensitivity and specificity of the cell-free DNA screen in the general obstetric population are similar to those in high-risk patients. But the positive predictive value is lower in the general population because of the lower prevalence of aneuploidy. “That is, fewer women with a positive test result will actually have an affected fetus, and there will be more false-positive test results,” ACOG and SMFM wrote.
As a result, the revised opinion includes a recommendation specifying that management decisions, including the decision to terminate a pregnancy, should not be based on the results of cell-free DNA screening alone. Further diagnostic testing is now recommended for any patient who receives a positive result on cell-free DNA screening.
Similarly, women whose results are indeterminate, uninterpretable (“no call” result), or not reported at all should receive further genetic counseling and be offered comprehensive ultrasound evaluation and diagnostic testing. And women whose results are negative should be counseled that a negative cell-free DNA test does not ensure a normal pregnancy.
Additionally, most cell-free DNA testing identifies only trisomies 13, 18, and 21, which comprise a smaller proportion of the chromosomal anomalies found in the general obstetric population than among high-risk women. In one study cited in the opinion, up to 17% of clinically significant chromosomal abnormalities would not be detectable by most current cell-free DNA techniques.
The joint opinion now includes a recommendation against routinely using cell-free DNA screening for microdeletion syndromes. And it reminds physicians that cell-free DNA testing also doesn’t assess fetal anomalies such as neural tube defects or ventral wall defects, so patients who undergo cell-free DNA screening should still be offered maternal serum alpha-fetoprotein screening or ultrasound assessment. The latest opinion continues to recommend against the use of cell-free DNA testing for women with multiple gestations.
Conventional prenatal screening methods are still the gold standard for most pregnant women despite the availability of cell-free DNA screening for aneuploidy, according to a consensus statement from the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine.
The two organizations cited the limits of cell-free DNA screening performance and the limited data on cost effectiveness in the low-risk obstetric population for encouraging ob.gyns. to stick with conventional screening methods in the general obstetric population.
After cell-free DNA analysis became clinically available in 2011, ACOG and SMFM recommended it for women at increased risk of fetal aneuploidy, including women 35 years or older, fetuses with ultrasonographic findings indicative of an increased risk of aneuploidy, women with a history of trisomy-affected offspring, a parent carrying a balanced robertsonian translocation with an increased risk of trisomy 13 or trisomy 21, and women with positive first-trimester or second-trimester screening test results.
And in a 2012 joint committee opinion, ACOG and SMFM said that cell-free DNA testing should not be offered to low-risk women or women with multiple gestations because it hadn’t been sufficiently studied.
The updated committee opinion, outlines the pros and cons of using cell-free DNA screening in the general obstetric population.
“Patients should be counseled that cell-free DNA screening does not replace the precision obtained with diagnostic tests, such as chorionic villus sampling or amniocentesis, and therefore, is limited in its ability to identify all chromosome abnormalities,” the groups wrote in the updated opinion. “Not only can there be false-positive test results, but a positive cell-free DNA test result for aneuploidy does not determine if the trisomy is due to a translocation, which affects the risk of recurrence. If a fetal structural anomaly is identified on ultrasound examination, diagnostic testing should be offered rather than cell-free DNA screening.”
The sensitivity and specificity of the cell-free DNA screen in the general obstetric population are similar to those in high-risk patients. But the positive predictive value is lower in the general population because of the lower prevalence of aneuploidy. “That is, fewer women with a positive test result will actually have an affected fetus, and there will be more false-positive test results,” ACOG and SMFM wrote.
As a result, the revised opinion includes a recommendation specifying that management decisions, including the decision to terminate a pregnancy, should not be based on the results of cell-free DNA screening alone. Further diagnostic testing is now recommended for any patient who receives a positive result on cell-free DNA screening.
Similarly, women whose results are indeterminate, uninterpretable (“no call” result), or not reported at all should receive further genetic counseling and be offered comprehensive ultrasound evaluation and diagnostic testing. And women whose results are negative should be counseled that a negative cell-free DNA test does not ensure a normal pregnancy.
Additionally, most cell-free DNA testing identifies only trisomies 13, 18, and 21, which comprise a smaller proportion of the chromosomal anomalies found in the general obstetric population than among high-risk women. In one study cited in the opinion, up to 17% of clinically significant chromosomal abnormalities would not be detectable by most current cell-free DNA techniques.
The joint opinion now includes a recommendation against routinely using cell-free DNA screening for microdeletion syndromes. And it reminds physicians that cell-free DNA testing also doesn’t assess fetal anomalies such as neural tube defects or ventral wall defects, so patients who undergo cell-free DNA screening should still be offered maternal serum alpha-fetoprotein screening or ultrasound assessment. The latest opinion continues to recommend against the use of cell-free DNA testing for women with multiple gestations.
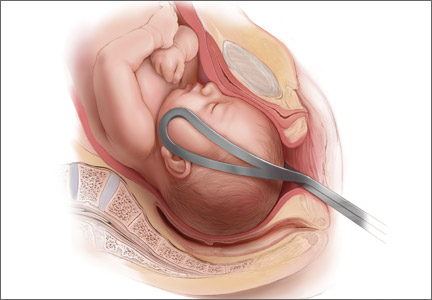
2015 Update on operative vaginal delivery
There’s a cyclical lament in obstetrics, and it goes something like this: Forceps are waning and are going to fade away completely if something isn’t done about it. This lament resounds every few decades, as a look at the literature confirms:
- 1963: “Midforceps delivery—a vanishing art?”1
- 1992: “Kielland’s forceps delivery: Is it a dying art?”2
- 2000: “Operative obstetrics: a lost art?”3
- 2015: “Forceps: towards obsolescence or revival?”4
In this, our latest cycle of lament, 4 or 5 papers have suggested that forceps in general and Kielland forceps in particular ought not be abandoned because outcomes are better than those suggested by the older literature. With the cesarean delivery rate hovering at about 31% in the United States, perhaps it is time to revisit the issue.
This Update is not intended to be a comprehensive review of the literature. Rather, it offers a snapshot of articles published within the past year—articles that highlight some new features of a very old debate:
- a nested observational study of 478 nulliparous women at term undergoing instrumental delivery, which found that instrument placement was “suboptimal” in a significant percentage of deliveries
- a retrospective study of major teaching hospitals, minor teaching facilities, and nonteaching institutions in 9 states, which found forceps delivery volumes so low they may make it difficult for clinicians to maintain their skills and prevent many trainees from acquiring proficiency
- a commentary calling for the discontinuation of forceps deliveries in light of an ultrasonographically identified injury to the pelvic floor—levator ani muscle avulsion—and a cadaveric study refuting this argument
- a systematic review and meta-analysis of maternal and neonatal morbidity following cesarean delivery in the first stage versus the second stage of labor.
Forceps and vacuum device placement is “suboptimal” in almost 30% of operative vaginal deliveries
Ramphul M, Kennelly MM, Burke G, Murphy DJ. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial ISRCTN 72230496. BJOG. 2015;122(4):558–563.
Rouse DJ. Instrument placement is sub-optimal in three of ten attempted operative vaginal deliveries. BJOG. 2015;122(4):564.
Over the years, many clinicians have argued that we don’t do enough forceps deliveries to maintain our own competence with the procedure, let alone teach residents how to perform it. This observational study nested in a randomized clinical trial is intriguing because Ramphul and colleagues looked for objective evidence of clinicians’ skill at the vacuum and forceps. Specifically, they looked for evidence that the forceps or vacuum was malpositioned during attempts at operative vaginal delivery. In the process, they nicely documented the absolute rate of malpositioning of the forceps and vacuum, finding that it is much higher than expected, even in an institution that performs a lot of operative vaginal deliveries.
Details of the trial
A cohort of 478 nulliparous women at term (≥37 weeks) underwent instrumental delivery at 2 university-affiliated maternity hospitals in Ireland. Ramphul and colleagues documented fetal head position prior to application of the instrument and at delivery. The midwife or neonatologist attending each delivery examined the neonate after birth and recorded the markings of the instrument on the infant’s head to determine whether instrument placement had been optimal.
Instrument placement was considered optimal when the vacuum cup included the flexion point (3 cm anterior to the posterior fontanelle) and the posterior fontanelle, with central placement. For forceps, instrument placement was considered optimal when the blades were positioned bilaterally and symmetrically over the malar bones. Two main types of forceps were used in this study—direct-traction Neville Barnes forceps (n = 138) and rotational Kielland forceps (n = 13)—and the rates of optimal and suboptimal placement were similar between them.
Each case was labeled as “optimal” or “suboptimal” by 2 investigators, with a third observer arbitrating when the 2 investigators differed in opinion.
Instrument placement was clearly documented in 478 deliveries, 138 of which (28.8%) involved suboptimal placement. There was a lower rate of induction of labor among deliveries with suboptimal placement (42.8% vs 53.2%; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.44–0.98; P = .038). There were no differences between the optimal and suboptimal groups in terms of duration of labor, use of oxytocin, and analgesia. In addition, the seniority of obstetricians performing operative vaginal delivery was similar between groups.
Fetal malposition was more common in the suboptimal group (58.7% vs 37.4%; OR, 2.44; 95% CI, 1.62–3.66; P<.0001). Midcavity station also was more common in the suboptimal group (82.6% vs 73.8%; OR, 1.68; 95% CI, 1.02–2.78; P = .042).
Maternal and neonatal outcomes
Postpartum hemorrhage was more common in the suboptimal placement group (24.6% vs 14.4%; OR, 1.94; 95% CI, 1.19–3.17; P = .008), as was prolonged hospitalization (26.8% vs 14.7%; OR, 2.13; 95% CI, 1.31–3.44; P = .02).
In addition, the incidence of neonatal trauma was higher in the group with suboptimal placement (15.9% vs 3.9%; OR, 4.64; 95% CI, 2.25–9.58; P<.0001) and included such effects as Erb’s palsy, fracture, retinal hemorrhage, cephalhematoma, and cerebral hemorrhage.
After adjustment for potential confounding factors, including induction of labor, seniority of the obstetrician, fetal malposition, caput above +1, midcavity station, regional analgesia, and the instrument used, the association remained significant between suboptimal placement and prolonged hospitalization (adjusted OR, 2.28; 95% CI, 1.30–4.02) and neonatal trauma (adjusted OR, 4.25; 95% CI, 1.85–9.72).
Dwindling statistics for operative vaginal delivery
In an editorial accompanying the study by Ramphul and colleagues, Dwight J. Rouse, MD,points to the waning of instrumental vaginal delivery in many parts of the world, most notably the United States, where, in 2012, only 2.8% of live births involved use of a vacuum device and only 0.6% involved the forceps.5
“When the rate of cesarean delivery is 10 times the combined rate of vaginal vacuum and forceps delivery (as it is in the USA), it is fair to argue that operative vaginal delivery is underutilized,” Dr. Rouse writes. “So kudos to Ramphul et al for providing insight into how we might continue to perform operative vaginal delivery safely.”
What this EVIDENCE means for practice
The study by Ramphul and colleagues very clearly confirms that correct placement of the vacuum device or forceps is key to safety.
Should we continue forceps education using the apprenticeship model of training?
Kyser KL, Lu X, Santillan D, et al. Forceps delivery volumes in teaching and nonteaching hospitals: Are volumes sufficient for physicians to acquire and maintain competence? Acad Med. 2014;89(1):71–76.
Ericsson KA. Necessity is the mother of invention: video recording firsthand perspectives of critical medical procedures to make simulated training more effective. Acad Med. 2014;89(1):17–20.
Kyser and colleagues have provided the best current snapshot of the opportunity for teaching instrumental vaginal delivery in the United States. They conducted a retrospective cohort study using new state inpatient data from 9 states in diverse geographic locations to capture experience at large and small teaching hospitals, as well as nonteaching institutions. They demonstrated that the opportunity for hands-on experience with these difficult and technically demanding deliveries is extremely limited and probably insufficient for all practicing physicians to maintain their skills if we continue to rely on traditional ways of teaching.
Details of the study
Using State Inpatient Data from 9 states, Kyser and colleagues identified all women hospitalized for childbirth in 2008. Of 1,344,305 deliveries in 835 hospitals, the final cohort included 624,000 operative deliveries—424,224 cesarean deliveries, 174,036 vacuum extractions, 6,158 forceps deliveries, and 19,582 deliveries that required more than 1 method. Of the 835 hospitals in this study, 68 were major teaching hospitals, 130 were minor teaching facilities, and 637 were nonteaching institutions.
The mean annual volumes for cesarean delivery for major teaching, minor teaching, and nonteaching hospitals were 969.8, 757.8, and 406.9, respectively (P<.0001).
The mean annual volumes for vacuum delivery were 301.0, 304.2, and 190.4, respectively (P<.0001).
The mean annual volumes for forceps delivery were 25.2, 15.3, and 8.9, respectively (P<.0001).
Three hundred twenty hospitals (38.3% of all hospitals) failed to perform a single forceps delivery in 2008, including 11 major teaching hospitals (16.2% of major teaching hospitals), 30 minor teaching hospitals (23.1% of minor teaching hospitals), and 279 nonteaching hospitals (43.8% of nonteaching hospitals) (P<.0001).
We need to rethink the apprenticeship model
In a commentary accompanying the study by Kyser and colleagues, K. Anders Ericsson, PhD, revisits the “see one, do one, teach one” model that has long characterized medical education. “Both the limitations on learning opportunities available in the clinics and the restrictions on resident work hours have created a real problem for the traditional apprenticeship model for training doctors,” he writes.
Ericsson notes that other specialists, such as concert musicians, chess players, and professional athletes do not learn using an apprenticeship model. For example, chess players do not play game after game of chess to become expert. And when a game is concluded, usually after several hours have passed, they are unlikely to be aware of the specific moves that lost or won them the game (unless an observer points them out). That is why, when training, chess players focus on particular aspects of the game (often identified by a mentor) as being crucial to improve their overall performance.
In today’s chess-learning environment, Ericsson notes, the computer plays a key role and can provide accurate feedback on each move the player executes. Computer chess programs have evolved to the point that they “are far superior in skill to any human chess player. Most important, computers can provide more accurate feedback on each chess move and are available at any time for practice,” writes Ericsson.
The same is true in sports. A tennis player does not practice by playing an endless series of games—though an ability to win a game is the ultimate goal. Rather, the athlete focuses on aspects of the game—the serve, for example—that can make the difference between winning or losing. Ericsson also notes that most musicians, dancers, and athletes “spend most of their time training by themselves to get ready to exhibit their skills for the first time in front of a large audience.”
These approaches are a better model for improving performance than the apprenticeship model, Ericsson argues. In medicine, one alternative might be the video recording of medical procedures in the clinic from multiple points of view—so that later viewers get both the “big picture” and a close-up view from the point of technical performance. After the recording is digitized and stored on a server, it can serve as valuable teaching for an unlimited number of residents.
Simulator training offers another venue for education, as it makes possible the isolation of difficult aspects of a procedure, which can then be repeated by the trainee as many times as necessary. In the future, it should be possible to link video recordings directly to simulators “so trainees could focus on particular aspects of the procedures and be required to respond to prompts with recordable actions,” Ericsson writes.
What this EVIDENCE means for practice
Given the extremely limited opportunities for observing forceps deliveries in the United States, it is time for us to explore new avenues for teaching other than the traditional apprenticeship model.
Is ultrasound evidence of levator muscle “avulsion” a real anatomic entity?
Dietz HP. Forceps: toward obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
Da Silva AS, Digesu GA, Dell’Utri C, Fritsch H, Piffarotti P, Khullar V. Do ultrasound findings of levator ani “avulsion” correlate with anatomical findings? A multicenter cadaveric study [published online ahead of print May 15, 2015]. Neurourol Urodyn. doi:10.1002 /nau.22781.
Dietz takes a new tack in the debate over cesarean versus forceps by pointing to a recently highlighted abnormality in women who deliver by forceps: levator ani muscle avulsion, or LMA—traumatic disconnection of the levator ani from the pelvic sidewall. It has long been known that forceps deliveries can increase the risk of obstetric anal sphincter injuries (OASIS). Dietz contends that OASIS occurs at a rate as high as 40% to 60% after forceps delivery. He also notes, with some consternation, that the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine have advocated forceps as a way of reducing the high cesarean delivery rate.
When a parturient has been pushing for an extended period of time and there is a positional abnormality of the fetus, such as persistent occiput posterior position, cesarean delivery is often favored as a way of protecting the rectal sphincter. Dietz argues that cesarean delivery also protects against LMA, which “has only recently been recognized as a major etiological factor in pelvic floor dysfunction.” Dietz then presents a list of studies that have produced ultrasound findings of LMA in a high percentage of women undergoing forceps delivery—percentages on the order of 10% to 40%.
Enter Da Silva and colleagues, who argue that “the only true place to visualize the 3D structure of the human body, [and] thus validate imaging findings, [is] on cadaveric or live tissue dissections.” They undertook a cadaveric study to validate—or not—some of the findings of LMA summarized by Dietz.
Details of the study
The pubovisceral muscle (PVM) anatomy of 30 female cadavers was analyzed via 3D translabial ultrasonography to confirm LMA. The cadavers were then dissected to assess the finding anatomically. Da Silva and colleagues found LMA on imaging in 11 (36.7%) cadavers. LMA was unilateral in 10 (33.3%) cadavers and bilateral in 1 (3.3%). However, no LMA was found at dissection.
When an additional 39 cadavers were dissected, no LMA was identified.
On ultrasound, LMA is strongly associated with a narrower PVM insertion depth (mean of 4.79 mm vs 6.32 mm; P = .001). Da Silva and colleagues concluded that “there is a clear difference between anatomical and ultrasonographic findings. The imaged appearance of an ‘avulsion’ does not represent a true anatomical ‘avulsion’ as confirmed on dissection.”
What this EVIDENCE means for practice
Before we prematurely adopt ultrasound evidence of LMA as a significant morbidity, we need to learn more about its true etiology, pathophysiology, and epidemiology. We don’t yet know enough to say that it’s such a bad injury, when imaged via ultrasound, that it warrants cesarean delivery to avoid it.
When deciding between cesarean and forceps, keep the risks of second-stage cesarean in mind
Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
This expert systematic review and meta-analysis summarizes the morbidity of second-stage cesarean delivery. When an obstetrician has a patient who is arrested at persistent occiput posterior position, say, and is trying to decide on cesarean delivery versus Kielland’s rotation or other forceps delivery, it is necessary to balance the risks and benefits of the 2 options. And as all clinicians are aware, when cesarean delivery is performed late in labor and the patient has been pushing for a prolonged period of time in the second stage—cesarean can be a challenging procedure. Moreover, these late cesareans are associated with much greater risks than cesarean deliveries performed earlier in labor.
Details of the review
Pergialiotis and colleagues selected 10 studies comparing maternal and neonatal morbidity and mortality between cesarean delivery at full dilatation and cesarean delivery prior to full dilatation. These studies involved 23,104 women with a singleton fetus who underwent cesarean delivery in the first (n = 18,160) or second (n = 4,944) stage of labor.
They found that second-stage cesarean was associated with a higher rate of maternal death (OR, 7.96; 95% CI, 1.61–39.39), a higher rate of maternal admission to the intensive care unit (OR, 7.41; 95% CI, 2.47–22.5), and a higher maternal transfusion rate (OR, 2.60; 95% CI, 1.49–2.54).
The rate of neonatal death also was higher among second-stage cesareans (OR, 5.20; 95% CI, 2.49–10.85), as was admission to the neonatal intensive care unit (OR, 1.63; 95% CI, 0.91–2.91), and the 5-minute Apgar score was more likely to be less than 7 (OR, 2.77; 95% CI, 1.02–7.50).
According to the authors, this study is the “first systematic review and meta-analysis that investigates the impact of the stage of labor on maternal and neonatal outcomes among women delivering by cesarean section.” The findings demonstrate with authority that second-stage cesareans can be a risky undertaking.
What this EVIDENCE means for practice
Cesareans performed late in the second stage of labor are distinct from those performed in the first stage, carrying much higher risks, especially for the mother. When deciding whether to proceed with cesarean, vacuum, or forceps, the added risk of second-stage cesarean is an important aspect of both the consent conversation and clinical decision making.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Danforth DN, Ellis AH. Midforceps delivery—a vanishing art? Am J Obstet Gynecol. 1963;86:29–37.
2. Tan KH, Sim R, Yam KL. Kielland’s forceps delivery: Is it a dying art? Singapore Med J. 1992;33(4):380–382.
3. Bofill JA. Operative obstetrics: a lost art? Obstet Gynecol Surv. 2000;55(7):405–406.
4. Dietz HP. Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
5. Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Surtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):9.
There’s a cyclical lament in obstetrics, and it goes something like this: Forceps are waning and are going to fade away completely if something isn’t done about it. This lament resounds every few decades, as a look at the literature confirms:
- 1963: “Midforceps delivery—a vanishing art?”1
- 1992: “Kielland’s forceps delivery: Is it a dying art?”2
- 2000: “Operative obstetrics: a lost art?”3
- 2015: “Forceps: towards obsolescence or revival?”4
In this, our latest cycle of lament, 4 or 5 papers have suggested that forceps in general and Kielland forceps in particular ought not be abandoned because outcomes are better than those suggested by the older literature. With the cesarean delivery rate hovering at about 31% in the United States, perhaps it is time to revisit the issue.
This Update is not intended to be a comprehensive review of the literature. Rather, it offers a snapshot of articles published within the past year—articles that highlight some new features of a very old debate:
- a nested observational study of 478 nulliparous women at term undergoing instrumental delivery, which found that instrument placement was “suboptimal” in a significant percentage of deliveries
- a retrospective study of major teaching hospitals, minor teaching facilities, and nonteaching institutions in 9 states, which found forceps delivery volumes so low they may make it difficult for clinicians to maintain their skills and prevent many trainees from acquiring proficiency
- a commentary calling for the discontinuation of forceps deliveries in light of an ultrasonographically identified injury to the pelvic floor—levator ani muscle avulsion—and a cadaveric study refuting this argument
- a systematic review and meta-analysis of maternal and neonatal morbidity following cesarean delivery in the first stage versus the second stage of labor.
Forceps and vacuum device placement is “suboptimal” in almost 30% of operative vaginal deliveries
Ramphul M, Kennelly MM, Burke G, Murphy DJ. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial ISRCTN 72230496. BJOG. 2015;122(4):558–563.
Rouse DJ. Instrument placement is sub-optimal in three of ten attempted operative vaginal deliveries. BJOG. 2015;122(4):564.
Over the years, many clinicians have argued that we don’t do enough forceps deliveries to maintain our own competence with the procedure, let alone teach residents how to perform it. This observational study nested in a randomized clinical trial is intriguing because Ramphul and colleagues looked for objective evidence of clinicians’ skill at the vacuum and forceps. Specifically, they looked for evidence that the forceps or vacuum was malpositioned during attempts at operative vaginal delivery. In the process, they nicely documented the absolute rate of malpositioning of the forceps and vacuum, finding that it is much higher than expected, even in an institution that performs a lot of operative vaginal deliveries.
Details of the trial
A cohort of 478 nulliparous women at term (≥37 weeks) underwent instrumental delivery at 2 university-affiliated maternity hospitals in Ireland. Ramphul and colleagues documented fetal head position prior to application of the instrument and at delivery. The midwife or neonatologist attending each delivery examined the neonate after birth and recorded the markings of the instrument on the infant’s head to determine whether instrument placement had been optimal.
Instrument placement was considered optimal when the vacuum cup included the flexion point (3 cm anterior to the posterior fontanelle) and the posterior fontanelle, with central placement. For forceps, instrument placement was considered optimal when the blades were positioned bilaterally and symmetrically over the malar bones. Two main types of forceps were used in this study—direct-traction Neville Barnes forceps (n = 138) and rotational Kielland forceps (n = 13)—and the rates of optimal and suboptimal placement were similar between them.
Each case was labeled as “optimal” or “suboptimal” by 2 investigators, with a third observer arbitrating when the 2 investigators differed in opinion.
Instrument placement was clearly documented in 478 deliveries, 138 of which (28.8%) involved suboptimal placement. There was a lower rate of induction of labor among deliveries with suboptimal placement (42.8% vs 53.2%; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.44–0.98; P = .038). There were no differences between the optimal and suboptimal groups in terms of duration of labor, use of oxytocin, and analgesia. In addition, the seniority of obstetricians performing operative vaginal delivery was similar between groups.
Fetal malposition was more common in the suboptimal group (58.7% vs 37.4%; OR, 2.44; 95% CI, 1.62–3.66; P<.0001). Midcavity station also was more common in the suboptimal group (82.6% vs 73.8%; OR, 1.68; 95% CI, 1.02–2.78; P = .042).
Maternal and neonatal outcomes
Postpartum hemorrhage was more common in the suboptimal placement group (24.6% vs 14.4%; OR, 1.94; 95% CI, 1.19–3.17; P = .008), as was prolonged hospitalization (26.8% vs 14.7%; OR, 2.13; 95% CI, 1.31–3.44; P = .02).
In addition, the incidence of neonatal trauma was higher in the group with suboptimal placement (15.9% vs 3.9%; OR, 4.64; 95% CI, 2.25–9.58; P<.0001) and included such effects as Erb’s palsy, fracture, retinal hemorrhage, cephalhematoma, and cerebral hemorrhage.
After adjustment for potential confounding factors, including induction of labor, seniority of the obstetrician, fetal malposition, caput above +1, midcavity station, regional analgesia, and the instrument used, the association remained significant between suboptimal placement and prolonged hospitalization (adjusted OR, 2.28; 95% CI, 1.30–4.02) and neonatal trauma (adjusted OR, 4.25; 95% CI, 1.85–9.72).
Dwindling statistics for operative vaginal delivery
In an editorial accompanying the study by Ramphul and colleagues, Dwight J. Rouse, MD,points to the waning of instrumental vaginal delivery in many parts of the world, most notably the United States, where, in 2012, only 2.8% of live births involved use of a vacuum device and only 0.6% involved the forceps.5
“When the rate of cesarean delivery is 10 times the combined rate of vaginal vacuum and forceps delivery (as it is in the USA), it is fair to argue that operative vaginal delivery is underutilized,” Dr. Rouse writes. “So kudos to Ramphul et al for providing insight into how we might continue to perform operative vaginal delivery safely.”
What this EVIDENCE means for practice
The study by Ramphul and colleagues very clearly confirms that correct placement of the vacuum device or forceps is key to safety.
Should we continue forceps education using the apprenticeship model of training?
Kyser KL, Lu X, Santillan D, et al. Forceps delivery volumes in teaching and nonteaching hospitals: Are volumes sufficient for physicians to acquire and maintain competence? Acad Med. 2014;89(1):71–76.
Ericsson KA. Necessity is the mother of invention: video recording firsthand perspectives of critical medical procedures to make simulated training more effective. Acad Med. 2014;89(1):17–20.
Kyser and colleagues have provided the best current snapshot of the opportunity for teaching instrumental vaginal delivery in the United States. They conducted a retrospective cohort study using new state inpatient data from 9 states in diverse geographic locations to capture experience at large and small teaching hospitals, as well as nonteaching institutions. They demonstrated that the opportunity for hands-on experience with these difficult and technically demanding deliveries is extremely limited and probably insufficient for all practicing physicians to maintain their skills if we continue to rely on traditional ways of teaching.
Details of the study
Using State Inpatient Data from 9 states, Kyser and colleagues identified all women hospitalized for childbirth in 2008. Of 1,344,305 deliveries in 835 hospitals, the final cohort included 624,000 operative deliveries—424,224 cesarean deliveries, 174,036 vacuum extractions, 6,158 forceps deliveries, and 19,582 deliveries that required more than 1 method. Of the 835 hospitals in this study, 68 were major teaching hospitals, 130 were minor teaching facilities, and 637 were nonteaching institutions.
The mean annual volumes for cesarean delivery for major teaching, minor teaching, and nonteaching hospitals were 969.8, 757.8, and 406.9, respectively (P<.0001).
The mean annual volumes for vacuum delivery were 301.0, 304.2, and 190.4, respectively (P<.0001).
The mean annual volumes for forceps delivery were 25.2, 15.3, and 8.9, respectively (P<.0001).
Three hundred twenty hospitals (38.3% of all hospitals) failed to perform a single forceps delivery in 2008, including 11 major teaching hospitals (16.2% of major teaching hospitals), 30 minor teaching hospitals (23.1% of minor teaching hospitals), and 279 nonteaching hospitals (43.8% of nonteaching hospitals) (P<.0001).
We need to rethink the apprenticeship model
In a commentary accompanying the study by Kyser and colleagues, K. Anders Ericsson, PhD, revisits the “see one, do one, teach one” model that has long characterized medical education. “Both the limitations on learning opportunities available in the clinics and the restrictions on resident work hours have created a real problem for the traditional apprenticeship model for training doctors,” he writes.
Ericsson notes that other specialists, such as concert musicians, chess players, and professional athletes do not learn using an apprenticeship model. For example, chess players do not play game after game of chess to become expert. And when a game is concluded, usually after several hours have passed, they are unlikely to be aware of the specific moves that lost or won them the game (unless an observer points them out). That is why, when training, chess players focus on particular aspects of the game (often identified by a mentor) as being crucial to improve their overall performance.
In today’s chess-learning environment, Ericsson notes, the computer plays a key role and can provide accurate feedback on each move the player executes. Computer chess programs have evolved to the point that they “are far superior in skill to any human chess player. Most important, computers can provide more accurate feedback on each chess move and are available at any time for practice,” writes Ericsson.
The same is true in sports. A tennis player does not practice by playing an endless series of games—though an ability to win a game is the ultimate goal. Rather, the athlete focuses on aspects of the game—the serve, for example—that can make the difference between winning or losing. Ericsson also notes that most musicians, dancers, and athletes “spend most of their time training by themselves to get ready to exhibit their skills for the first time in front of a large audience.”
These approaches are a better model for improving performance than the apprenticeship model, Ericsson argues. In medicine, one alternative might be the video recording of medical procedures in the clinic from multiple points of view—so that later viewers get both the “big picture” and a close-up view from the point of technical performance. After the recording is digitized and stored on a server, it can serve as valuable teaching for an unlimited number of residents.
Simulator training offers another venue for education, as it makes possible the isolation of difficult aspects of a procedure, which can then be repeated by the trainee as many times as necessary. In the future, it should be possible to link video recordings directly to simulators “so trainees could focus on particular aspects of the procedures and be required to respond to prompts with recordable actions,” Ericsson writes.
What this EVIDENCE means for practice
Given the extremely limited opportunities for observing forceps deliveries in the United States, it is time for us to explore new avenues for teaching other than the traditional apprenticeship model.
Is ultrasound evidence of levator muscle “avulsion” a real anatomic entity?
Dietz HP. Forceps: toward obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
Da Silva AS, Digesu GA, Dell’Utri C, Fritsch H, Piffarotti P, Khullar V. Do ultrasound findings of levator ani “avulsion” correlate with anatomical findings? A multicenter cadaveric study [published online ahead of print May 15, 2015]. Neurourol Urodyn. doi:10.1002 /nau.22781.
Dietz takes a new tack in the debate over cesarean versus forceps by pointing to a recently highlighted abnormality in women who deliver by forceps: levator ani muscle avulsion, or LMA—traumatic disconnection of the levator ani from the pelvic sidewall. It has long been known that forceps deliveries can increase the risk of obstetric anal sphincter injuries (OASIS). Dietz contends that OASIS occurs at a rate as high as 40% to 60% after forceps delivery. He also notes, with some consternation, that the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine have advocated forceps as a way of reducing the high cesarean delivery rate.
When a parturient has been pushing for an extended period of time and there is a positional abnormality of the fetus, such as persistent occiput posterior position, cesarean delivery is often favored as a way of protecting the rectal sphincter. Dietz argues that cesarean delivery also protects against LMA, which “has only recently been recognized as a major etiological factor in pelvic floor dysfunction.” Dietz then presents a list of studies that have produced ultrasound findings of LMA in a high percentage of women undergoing forceps delivery—percentages on the order of 10% to 40%.
Enter Da Silva and colleagues, who argue that “the only true place to visualize the 3D structure of the human body, [and] thus validate imaging findings, [is] on cadaveric or live tissue dissections.” They undertook a cadaveric study to validate—or not—some of the findings of LMA summarized by Dietz.
Details of the study
The pubovisceral muscle (PVM) anatomy of 30 female cadavers was analyzed via 3D translabial ultrasonography to confirm LMA. The cadavers were then dissected to assess the finding anatomically. Da Silva and colleagues found LMA on imaging in 11 (36.7%) cadavers. LMA was unilateral in 10 (33.3%) cadavers and bilateral in 1 (3.3%). However, no LMA was found at dissection.
When an additional 39 cadavers were dissected, no LMA was identified.
On ultrasound, LMA is strongly associated with a narrower PVM insertion depth (mean of 4.79 mm vs 6.32 mm; P = .001). Da Silva and colleagues concluded that “there is a clear difference between anatomical and ultrasonographic findings. The imaged appearance of an ‘avulsion’ does not represent a true anatomical ‘avulsion’ as confirmed on dissection.”
What this EVIDENCE means for practice
Before we prematurely adopt ultrasound evidence of LMA as a significant morbidity, we need to learn more about its true etiology, pathophysiology, and epidemiology. We don’t yet know enough to say that it’s such a bad injury, when imaged via ultrasound, that it warrants cesarean delivery to avoid it.
When deciding between cesarean and forceps, keep the risks of second-stage cesarean in mind
Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
This expert systematic review and meta-analysis summarizes the morbidity of second-stage cesarean delivery. When an obstetrician has a patient who is arrested at persistent occiput posterior position, say, and is trying to decide on cesarean delivery versus Kielland’s rotation or other forceps delivery, it is necessary to balance the risks and benefits of the 2 options. And as all clinicians are aware, when cesarean delivery is performed late in labor and the patient has been pushing for a prolonged period of time in the second stage—cesarean can be a challenging procedure. Moreover, these late cesareans are associated with much greater risks than cesarean deliveries performed earlier in labor.
Details of the review
Pergialiotis and colleagues selected 10 studies comparing maternal and neonatal morbidity and mortality between cesarean delivery at full dilatation and cesarean delivery prior to full dilatation. These studies involved 23,104 women with a singleton fetus who underwent cesarean delivery in the first (n = 18,160) or second (n = 4,944) stage of labor.
They found that second-stage cesarean was associated with a higher rate of maternal death (OR, 7.96; 95% CI, 1.61–39.39), a higher rate of maternal admission to the intensive care unit (OR, 7.41; 95% CI, 2.47–22.5), and a higher maternal transfusion rate (OR, 2.60; 95% CI, 1.49–2.54).
The rate of neonatal death also was higher among second-stage cesareans (OR, 5.20; 95% CI, 2.49–10.85), as was admission to the neonatal intensive care unit (OR, 1.63; 95% CI, 0.91–2.91), and the 5-minute Apgar score was more likely to be less than 7 (OR, 2.77; 95% CI, 1.02–7.50).
According to the authors, this study is the “first systematic review and meta-analysis that investigates the impact of the stage of labor on maternal and neonatal outcomes among women delivering by cesarean section.” The findings demonstrate with authority that second-stage cesareans can be a risky undertaking.
What this EVIDENCE means for practice
Cesareans performed late in the second stage of labor are distinct from those performed in the first stage, carrying much higher risks, especially for the mother. When deciding whether to proceed with cesarean, vacuum, or forceps, the added risk of second-stage cesarean is an important aspect of both the consent conversation and clinical decision making.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
There’s a cyclical lament in obstetrics, and it goes something like this: Forceps are waning and are going to fade away completely if something isn’t done about it. This lament resounds every few decades, as a look at the literature confirms:
- 1963: “Midforceps delivery—a vanishing art?”1
- 1992: “Kielland’s forceps delivery: Is it a dying art?”2
- 2000: “Operative obstetrics: a lost art?”3
- 2015: “Forceps: towards obsolescence or revival?”4
In this, our latest cycle of lament, 4 or 5 papers have suggested that forceps in general and Kielland forceps in particular ought not be abandoned because outcomes are better than those suggested by the older literature. With the cesarean delivery rate hovering at about 31% in the United States, perhaps it is time to revisit the issue.
This Update is not intended to be a comprehensive review of the literature. Rather, it offers a snapshot of articles published within the past year—articles that highlight some new features of a very old debate:
- a nested observational study of 478 nulliparous women at term undergoing instrumental delivery, which found that instrument placement was “suboptimal” in a significant percentage of deliveries
- a retrospective study of major teaching hospitals, minor teaching facilities, and nonteaching institutions in 9 states, which found forceps delivery volumes so low they may make it difficult for clinicians to maintain their skills and prevent many trainees from acquiring proficiency
- a commentary calling for the discontinuation of forceps deliveries in light of an ultrasonographically identified injury to the pelvic floor—levator ani muscle avulsion—and a cadaveric study refuting this argument
- a systematic review and meta-analysis of maternal and neonatal morbidity following cesarean delivery in the first stage versus the second stage of labor.
Forceps and vacuum device placement is “suboptimal” in almost 30% of operative vaginal deliveries
Ramphul M, Kennelly MM, Burke G, Murphy DJ. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial ISRCTN 72230496. BJOG. 2015;122(4):558–563.
Rouse DJ. Instrument placement is sub-optimal in three of ten attempted operative vaginal deliveries. BJOG. 2015;122(4):564.
Over the years, many clinicians have argued that we don’t do enough forceps deliveries to maintain our own competence with the procedure, let alone teach residents how to perform it. This observational study nested in a randomized clinical trial is intriguing because Ramphul and colleagues looked for objective evidence of clinicians’ skill at the vacuum and forceps. Specifically, they looked for evidence that the forceps or vacuum was malpositioned during attempts at operative vaginal delivery. In the process, they nicely documented the absolute rate of malpositioning of the forceps and vacuum, finding that it is much higher than expected, even in an institution that performs a lot of operative vaginal deliveries.
Details of the trial
A cohort of 478 nulliparous women at term (≥37 weeks) underwent instrumental delivery at 2 university-affiliated maternity hospitals in Ireland. Ramphul and colleagues documented fetal head position prior to application of the instrument and at delivery. The midwife or neonatologist attending each delivery examined the neonate after birth and recorded the markings of the instrument on the infant’s head to determine whether instrument placement had been optimal.
Instrument placement was considered optimal when the vacuum cup included the flexion point (3 cm anterior to the posterior fontanelle) and the posterior fontanelle, with central placement. For forceps, instrument placement was considered optimal when the blades were positioned bilaterally and symmetrically over the malar bones. Two main types of forceps were used in this study—direct-traction Neville Barnes forceps (n = 138) and rotational Kielland forceps (n = 13)—and the rates of optimal and suboptimal placement were similar between them.
Each case was labeled as “optimal” or “suboptimal” by 2 investigators, with a third observer arbitrating when the 2 investigators differed in opinion.
Instrument placement was clearly documented in 478 deliveries, 138 of which (28.8%) involved suboptimal placement. There was a lower rate of induction of labor among deliveries with suboptimal placement (42.8% vs 53.2%; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.44–0.98; P = .038). There were no differences between the optimal and suboptimal groups in terms of duration of labor, use of oxytocin, and analgesia. In addition, the seniority of obstetricians performing operative vaginal delivery was similar between groups.
Fetal malposition was more common in the suboptimal group (58.7% vs 37.4%; OR, 2.44; 95% CI, 1.62–3.66; P<.0001). Midcavity station also was more common in the suboptimal group (82.6% vs 73.8%; OR, 1.68; 95% CI, 1.02–2.78; P = .042).
Maternal and neonatal outcomes
Postpartum hemorrhage was more common in the suboptimal placement group (24.6% vs 14.4%; OR, 1.94; 95% CI, 1.19–3.17; P = .008), as was prolonged hospitalization (26.8% vs 14.7%; OR, 2.13; 95% CI, 1.31–3.44; P = .02).
In addition, the incidence of neonatal trauma was higher in the group with suboptimal placement (15.9% vs 3.9%; OR, 4.64; 95% CI, 2.25–9.58; P<.0001) and included such effects as Erb’s palsy, fracture, retinal hemorrhage, cephalhematoma, and cerebral hemorrhage.
After adjustment for potential confounding factors, including induction of labor, seniority of the obstetrician, fetal malposition, caput above +1, midcavity station, regional analgesia, and the instrument used, the association remained significant between suboptimal placement and prolonged hospitalization (adjusted OR, 2.28; 95% CI, 1.30–4.02) and neonatal trauma (adjusted OR, 4.25; 95% CI, 1.85–9.72).
Dwindling statistics for operative vaginal delivery
In an editorial accompanying the study by Ramphul and colleagues, Dwight J. Rouse, MD,points to the waning of instrumental vaginal delivery in many parts of the world, most notably the United States, where, in 2012, only 2.8% of live births involved use of a vacuum device and only 0.6% involved the forceps.5
“When the rate of cesarean delivery is 10 times the combined rate of vaginal vacuum and forceps delivery (as it is in the USA), it is fair to argue that operative vaginal delivery is underutilized,” Dr. Rouse writes. “So kudos to Ramphul et al for providing insight into how we might continue to perform operative vaginal delivery safely.”
What this EVIDENCE means for practice
The study by Ramphul and colleagues very clearly confirms that correct placement of the vacuum device or forceps is key to safety.
Should we continue forceps education using the apprenticeship model of training?
Kyser KL, Lu X, Santillan D, et al. Forceps delivery volumes in teaching and nonteaching hospitals: Are volumes sufficient for physicians to acquire and maintain competence? Acad Med. 2014;89(1):71–76.
Ericsson KA. Necessity is the mother of invention: video recording firsthand perspectives of critical medical procedures to make simulated training more effective. Acad Med. 2014;89(1):17–20.
Kyser and colleagues have provided the best current snapshot of the opportunity for teaching instrumental vaginal delivery in the United States. They conducted a retrospective cohort study using new state inpatient data from 9 states in diverse geographic locations to capture experience at large and small teaching hospitals, as well as nonteaching institutions. They demonstrated that the opportunity for hands-on experience with these difficult and technically demanding deliveries is extremely limited and probably insufficient for all practicing physicians to maintain their skills if we continue to rely on traditional ways of teaching.
Details of the study
Using State Inpatient Data from 9 states, Kyser and colleagues identified all women hospitalized for childbirth in 2008. Of 1,344,305 deliveries in 835 hospitals, the final cohort included 624,000 operative deliveries—424,224 cesarean deliveries, 174,036 vacuum extractions, 6,158 forceps deliveries, and 19,582 deliveries that required more than 1 method. Of the 835 hospitals in this study, 68 were major teaching hospitals, 130 were minor teaching facilities, and 637 were nonteaching institutions.
The mean annual volumes for cesarean delivery for major teaching, minor teaching, and nonteaching hospitals were 969.8, 757.8, and 406.9, respectively (P<.0001).
The mean annual volumes for vacuum delivery were 301.0, 304.2, and 190.4, respectively (P<.0001).
The mean annual volumes for forceps delivery were 25.2, 15.3, and 8.9, respectively (P<.0001).
Three hundred twenty hospitals (38.3% of all hospitals) failed to perform a single forceps delivery in 2008, including 11 major teaching hospitals (16.2% of major teaching hospitals), 30 minor teaching hospitals (23.1% of minor teaching hospitals), and 279 nonteaching hospitals (43.8% of nonteaching hospitals) (P<.0001).
We need to rethink the apprenticeship model
In a commentary accompanying the study by Kyser and colleagues, K. Anders Ericsson, PhD, revisits the “see one, do one, teach one” model that has long characterized medical education. “Both the limitations on learning opportunities available in the clinics and the restrictions on resident work hours have created a real problem for the traditional apprenticeship model for training doctors,” he writes.
Ericsson notes that other specialists, such as concert musicians, chess players, and professional athletes do not learn using an apprenticeship model. For example, chess players do not play game after game of chess to become expert. And when a game is concluded, usually after several hours have passed, they are unlikely to be aware of the specific moves that lost or won them the game (unless an observer points them out). That is why, when training, chess players focus on particular aspects of the game (often identified by a mentor) as being crucial to improve their overall performance.
In today’s chess-learning environment, Ericsson notes, the computer plays a key role and can provide accurate feedback on each move the player executes. Computer chess programs have evolved to the point that they “are far superior in skill to any human chess player. Most important, computers can provide more accurate feedback on each chess move and are available at any time for practice,” writes Ericsson.
The same is true in sports. A tennis player does not practice by playing an endless series of games—though an ability to win a game is the ultimate goal. Rather, the athlete focuses on aspects of the game—the serve, for example—that can make the difference between winning or losing. Ericsson also notes that most musicians, dancers, and athletes “spend most of their time training by themselves to get ready to exhibit their skills for the first time in front of a large audience.”
These approaches are a better model for improving performance than the apprenticeship model, Ericsson argues. In medicine, one alternative might be the video recording of medical procedures in the clinic from multiple points of view—so that later viewers get both the “big picture” and a close-up view from the point of technical performance. After the recording is digitized and stored on a server, it can serve as valuable teaching for an unlimited number of residents.
Simulator training offers another venue for education, as it makes possible the isolation of difficult aspects of a procedure, which can then be repeated by the trainee as many times as necessary. In the future, it should be possible to link video recordings directly to simulators “so trainees could focus on particular aspects of the procedures and be required to respond to prompts with recordable actions,” Ericsson writes.
What this EVIDENCE means for practice
Given the extremely limited opportunities for observing forceps deliveries in the United States, it is time for us to explore new avenues for teaching other than the traditional apprenticeship model.
Is ultrasound evidence of levator muscle “avulsion” a real anatomic entity?
Dietz HP. Forceps: toward obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
Da Silva AS, Digesu GA, Dell’Utri C, Fritsch H, Piffarotti P, Khullar V. Do ultrasound findings of levator ani “avulsion” correlate with anatomical findings? A multicenter cadaveric study [published online ahead of print May 15, 2015]. Neurourol Urodyn. doi:10.1002 /nau.22781.
Dietz takes a new tack in the debate over cesarean versus forceps by pointing to a recently highlighted abnormality in women who deliver by forceps: levator ani muscle avulsion, or LMA—traumatic disconnection of the levator ani from the pelvic sidewall. It has long been known that forceps deliveries can increase the risk of obstetric anal sphincter injuries (OASIS). Dietz contends that OASIS occurs at a rate as high as 40% to 60% after forceps delivery. He also notes, with some consternation, that the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine have advocated forceps as a way of reducing the high cesarean delivery rate.
When a parturient has been pushing for an extended period of time and there is a positional abnormality of the fetus, such as persistent occiput posterior position, cesarean delivery is often favored as a way of protecting the rectal sphincter. Dietz argues that cesarean delivery also protects against LMA, which “has only recently been recognized as a major etiological factor in pelvic floor dysfunction.” Dietz then presents a list of studies that have produced ultrasound findings of LMA in a high percentage of women undergoing forceps delivery—percentages on the order of 10% to 40%.
Enter Da Silva and colleagues, who argue that “the only true place to visualize the 3D structure of the human body, [and] thus validate imaging findings, [is] on cadaveric or live tissue dissections.” They undertook a cadaveric study to validate—or not—some of the findings of LMA summarized by Dietz.
Details of the study
The pubovisceral muscle (PVM) anatomy of 30 female cadavers was analyzed via 3D translabial ultrasonography to confirm LMA. The cadavers were then dissected to assess the finding anatomically. Da Silva and colleagues found LMA on imaging in 11 (36.7%) cadavers. LMA was unilateral in 10 (33.3%) cadavers and bilateral in 1 (3.3%). However, no LMA was found at dissection.
When an additional 39 cadavers were dissected, no LMA was identified.
On ultrasound, LMA is strongly associated with a narrower PVM insertion depth (mean of 4.79 mm vs 6.32 mm; P = .001). Da Silva and colleagues concluded that “there is a clear difference between anatomical and ultrasonographic findings. The imaged appearance of an ‘avulsion’ does not represent a true anatomical ‘avulsion’ as confirmed on dissection.”
What this EVIDENCE means for practice
Before we prematurely adopt ultrasound evidence of LMA as a significant morbidity, we need to learn more about its true etiology, pathophysiology, and epidemiology. We don’t yet know enough to say that it’s such a bad injury, when imaged via ultrasound, that it warrants cesarean delivery to avoid it.
When deciding between cesarean and forceps, keep the risks of second-stage cesarean in mind
Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
This expert systematic review and meta-analysis summarizes the morbidity of second-stage cesarean delivery. When an obstetrician has a patient who is arrested at persistent occiput posterior position, say, and is trying to decide on cesarean delivery versus Kielland’s rotation or other forceps delivery, it is necessary to balance the risks and benefits of the 2 options. And as all clinicians are aware, when cesarean delivery is performed late in labor and the patient has been pushing for a prolonged period of time in the second stage—cesarean can be a challenging procedure. Moreover, these late cesareans are associated with much greater risks than cesarean deliveries performed earlier in labor.
Details of the review
Pergialiotis and colleagues selected 10 studies comparing maternal and neonatal morbidity and mortality between cesarean delivery at full dilatation and cesarean delivery prior to full dilatation. These studies involved 23,104 women with a singleton fetus who underwent cesarean delivery in the first (n = 18,160) or second (n = 4,944) stage of labor.
They found that second-stage cesarean was associated with a higher rate of maternal death (OR, 7.96; 95% CI, 1.61–39.39), a higher rate of maternal admission to the intensive care unit (OR, 7.41; 95% CI, 2.47–22.5), and a higher maternal transfusion rate (OR, 2.60; 95% CI, 1.49–2.54).
The rate of neonatal death also was higher among second-stage cesareans (OR, 5.20; 95% CI, 2.49–10.85), as was admission to the neonatal intensive care unit (OR, 1.63; 95% CI, 0.91–2.91), and the 5-minute Apgar score was more likely to be less than 7 (OR, 2.77; 95% CI, 1.02–7.50).
According to the authors, this study is the “first systematic review and meta-analysis that investigates the impact of the stage of labor on maternal and neonatal outcomes among women delivering by cesarean section.” The findings demonstrate with authority that second-stage cesareans can be a risky undertaking.
What this EVIDENCE means for practice
Cesareans performed late in the second stage of labor are distinct from those performed in the first stage, carrying much higher risks, especially for the mother. When deciding whether to proceed with cesarean, vacuum, or forceps, the added risk of second-stage cesarean is an important aspect of both the consent conversation and clinical decision making.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Danforth DN, Ellis AH. Midforceps delivery—a vanishing art? Am J Obstet Gynecol. 1963;86:29–37.
2. Tan KH, Sim R, Yam KL. Kielland’s forceps delivery: Is it a dying art? Singapore Med J. 1992;33(4):380–382.
3. Bofill JA. Operative obstetrics: a lost art? Obstet Gynecol Surv. 2000;55(7):405–406.
4. Dietz HP. Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
5. Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Surtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):9.
1. Danforth DN, Ellis AH. Midforceps delivery—a vanishing art? Am J Obstet Gynecol. 1963;86:29–37.
2. Tan KH, Sim R, Yam KL. Kielland’s forceps delivery: Is it a dying art? Singapore Med J. 1992;33(4):380–382.
3. Bofill JA. Operative obstetrics: a lost art? Obstet Gynecol Surv. 2000;55(7):405–406.
4. Dietz HP. Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand. 2015;94(4):347–351.
5. Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Surtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):9.
In this Article
- Rate of suboptimal instrument placement
- Are we educating ourselves in the most productive manner?
- Keep the risks of second-stage cesarean in mind
Laparoscopic management of interstitial ectopic pregnancy
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Diet coaching curbs weight gain in women at GDM risk
BOSTON – Women at risk for gestational diabetes held off excess weight gain better when coached on healthy eating alone compared with those coached about physical activity, or on diet and exercise together.
The findings, presented at the annual scientific sessions of the American Diabetes Association, come from a pilot study in 150 obese pregnant women recruited from nine European countries randomized to one of the three lifestyle interventions.
The pilot study is the precursor to a larger ongoing randomized trial called DALI (Vitamin D & Lifestyle Intervention for Gestational Diabetes Mellitus Prevention). Dr. David Simmons of the University of Western Sydney, Australia, who presented the pilot study’s findings at the meeting, said he and his coinvestigators found it puzzling that a combined diet-and-exercise intervention would be less effective than a diet-alone intervention.
The women, all recruited at or before week 19 of their pregnancies (most entered around week 14), were well matched across the study arms for body mass index (mean 34.1-34.8) and fasting glucose and insulin sensitivity measurements at baseline. A glucose tolerance test was used to exclude women with GDM at baseline, though some of the women in the cohort had previous GDM. Also excluded were women unable to comply with the recommendations because of physical or psychiatric disability.
The researchers created five sets of recommendations for physical activity (for example: sitting less, building strength, taking more steps) and another seven for eating (including increasing intake of protein, vegetables, and fiber, and reducing intake of carbohydrates and fat) that were emphasized and detailed by lifestyle coaches during the intervention. The intervention was delivered over five in-person, one-on-one coaching sessions 30-45 minutes long, with follow-up phone calls in between. The sessions lasted through week 30.
Women in the combined group received all 12 of the diet and exercise messages. The problem may have been an overload of guidance in that arm of the study, Dr. Simmons said.
“We thought it was a no-brainer that the more you put in, the more you’d get out,” he said. But possibly, “having 12 messages kind of swamped people, and it was just too much for them to focus on.”
Women randomized to physical activity counseling alone (n = 50) saw 2.6 kilograms more weight gain at 24-28 weeks of pregnancy than did women randomized to nutrition counseling alone (n = 50), Dr. Simmons reported. The difference narrowed to 1.6 kilos by 35-37 weeks but remained significant.
Fasting glucose measurements were significantly higher in the exercise group at 35-37 weeks compared with the nutrition group. The combined intervention was not significantly better than was exercise alone for either the fasting glucose or weight measures. Though the study was not powered to detect significant differences in GDM risk, women in the physical activity group saw a higher incidence of GDM, 42%, compared to 31% for the combined intervention and 28% for the diet-only group.
The findings suggest “that healthy eating was the more efficacious strategy in dealing with excess weight gain,” which is a risk factor for GDM, said Dr. Simmons. “What we see now certainly justifies the use of early healthy eating interventions in obese pregnant women.”
He added that the larger trial, which will randomize 440 women with the same characteristics to one of the three lifestyle interventions or no intervention, will seek to confirm the findings and will be powered to pick up significant differences in GDM risk.
A separate trial under DALI, recruiting another 440 obese pregnant women, will look at vitamin D supplementation alone and alongside lifestyle inventions, and placebo.
The DALI studies are funded by the European Commission. Dr. Simmons declared no conflict of interest.
BOSTON – Women at risk for gestational diabetes held off excess weight gain better when coached on healthy eating alone compared with those coached about physical activity, or on diet and exercise together.
The findings, presented at the annual scientific sessions of the American Diabetes Association, come from a pilot study in 150 obese pregnant women recruited from nine European countries randomized to one of the three lifestyle interventions.
The pilot study is the precursor to a larger ongoing randomized trial called DALI (Vitamin D & Lifestyle Intervention for Gestational Diabetes Mellitus Prevention). Dr. David Simmons of the University of Western Sydney, Australia, who presented the pilot study’s findings at the meeting, said he and his coinvestigators found it puzzling that a combined diet-and-exercise intervention would be less effective than a diet-alone intervention.
The women, all recruited at or before week 19 of their pregnancies (most entered around week 14), were well matched across the study arms for body mass index (mean 34.1-34.8) and fasting glucose and insulin sensitivity measurements at baseline. A glucose tolerance test was used to exclude women with GDM at baseline, though some of the women in the cohort had previous GDM. Also excluded were women unable to comply with the recommendations because of physical or psychiatric disability.
The researchers created five sets of recommendations for physical activity (for example: sitting less, building strength, taking more steps) and another seven for eating (including increasing intake of protein, vegetables, and fiber, and reducing intake of carbohydrates and fat) that were emphasized and detailed by lifestyle coaches during the intervention. The intervention was delivered over five in-person, one-on-one coaching sessions 30-45 minutes long, with follow-up phone calls in between. The sessions lasted through week 30.
Women in the combined group received all 12 of the diet and exercise messages. The problem may have been an overload of guidance in that arm of the study, Dr. Simmons said.
“We thought it was a no-brainer that the more you put in, the more you’d get out,” he said. But possibly, “having 12 messages kind of swamped people, and it was just too much for them to focus on.”
Women randomized to physical activity counseling alone (n = 50) saw 2.6 kilograms more weight gain at 24-28 weeks of pregnancy than did women randomized to nutrition counseling alone (n = 50), Dr. Simmons reported. The difference narrowed to 1.6 kilos by 35-37 weeks but remained significant.
Fasting glucose measurements were significantly higher in the exercise group at 35-37 weeks compared with the nutrition group. The combined intervention was not significantly better than was exercise alone for either the fasting glucose or weight measures. Though the study was not powered to detect significant differences in GDM risk, women in the physical activity group saw a higher incidence of GDM, 42%, compared to 31% for the combined intervention and 28% for the diet-only group.
The findings suggest “that healthy eating was the more efficacious strategy in dealing with excess weight gain,” which is a risk factor for GDM, said Dr. Simmons. “What we see now certainly justifies the use of early healthy eating interventions in obese pregnant women.”
He added that the larger trial, which will randomize 440 women with the same characteristics to one of the three lifestyle interventions or no intervention, will seek to confirm the findings and will be powered to pick up significant differences in GDM risk.
A separate trial under DALI, recruiting another 440 obese pregnant women, will look at vitamin D supplementation alone and alongside lifestyle inventions, and placebo.
The DALI studies are funded by the European Commission. Dr. Simmons declared no conflict of interest.
BOSTON – Women at risk for gestational diabetes held off excess weight gain better when coached on healthy eating alone compared with those coached about physical activity, or on diet and exercise together.
The findings, presented at the annual scientific sessions of the American Diabetes Association, come from a pilot study in 150 obese pregnant women recruited from nine European countries randomized to one of the three lifestyle interventions.
The pilot study is the precursor to a larger ongoing randomized trial called DALI (Vitamin D & Lifestyle Intervention for Gestational Diabetes Mellitus Prevention). Dr. David Simmons of the University of Western Sydney, Australia, who presented the pilot study’s findings at the meeting, said he and his coinvestigators found it puzzling that a combined diet-and-exercise intervention would be less effective than a diet-alone intervention.
The women, all recruited at or before week 19 of their pregnancies (most entered around week 14), were well matched across the study arms for body mass index (mean 34.1-34.8) and fasting glucose and insulin sensitivity measurements at baseline. A glucose tolerance test was used to exclude women with GDM at baseline, though some of the women in the cohort had previous GDM. Also excluded were women unable to comply with the recommendations because of physical or psychiatric disability.
The researchers created five sets of recommendations for physical activity (for example: sitting less, building strength, taking more steps) and another seven for eating (including increasing intake of protein, vegetables, and fiber, and reducing intake of carbohydrates and fat) that were emphasized and detailed by lifestyle coaches during the intervention. The intervention was delivered over five in-person, one-on-one coaching sessions 30-45 minutes long, with follow-up phone calls in between. The sessions lasted through week 30.
Women in the combined group received all 12 of the diet and exercise messages. The problem may have been an overload of guidance in that arm of the study, Dr. Simmons said.
“We thought it was a no-brainer that the more you put in, the more you’d get out,” he said. But possibly, “having 12 messages kind of swamped people, and it was just too much for them to focus on.”
Women randomized to physical activity counseling alone (n = 50) saw 2.6 kilograms more weight gain at 24-28 weeks of pregnancy than did women randomized to nutrition counseling alone (n = 50), Dr. Simmons reported. The difference narrowed to 1.6 kilos by 35-37 weeks but remained significant.
Fasting glucose measurements were significantly higher in the exercise group at 35-37 weeks compared with the nutrition group. The combined intervention was not significantly better than was exercise alone for either the fasting glucose or weight measures. Though the study was not powered to detect significant differences in GDM risk, women in the physical activity group saw a higher incidence of GDM, 42%, compared to 31% for the combined intervention and 28% for the diet-only group.
The findings suggest “that healthy eating was the more efficacious strategy in dealing with excess weight gain,” which is a risk factor for GDM, said Dr. Simmons. “What we see now certainly justifies the use of early healthy eating interventions in obese pregnant women.”
He added that the larger trial, which will randomize 440 women with the same characteristics to one of the three lifestyle interventions or no intervention, will seek to confirm the findings and will be powered to pick up significant differences in GDM risk.
A separate trial under DALI, recruiting another 440 obese pregnant women, will look at vitamin D supplementation alone and alongside lifestyle inventions, and placebo.
The DALI studies are funded by the European Commission. Dr. Simmons declared no conflict of interest.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: A lifestyle intervention aimed exclusively at dietary choices was associated with significantly less excess weight gain in obese pregnant women compared with interventions promoting exercise alone or a combination of diet and exercise.
Major finding: Women randomized to physical activity counseling alone gained 2.6 kilograms more at 24-28 weeks of pregnancy than did women randomized to nutrition counseling alone (P= .03). The difference narrowed to 1.6 kilos by 35-37 weeks (P = .01).
Data source: A randomized controlled trial of 150 obese pregnant women (minimum BMI 29) before gestational week 19 randomized to five sessions of dietary counseling (n = 50), physical activity counseling (n = 50), or combined diet and exercise counseling (n = 50) from clinics in nine European countries. Subjects were counseled through week 30 and followed for weight, insulin resistance, and fasting glucose through week 37.
Disclosures: The European Commission funded the study. No conflicts of interest were reported.
GnRH-antagonist protocol trims ovarian hyperstimulation
LISBON – Women undergoing assisted reproduction had similar pregnancy rates with gonadotropin-releasing hormone agonist and antagonist protocols, but less ovarian hyperstimulation syndrome with the GnRH-antagonist protocol in a large randomized trial.
Severe ovarian hyperstimulation syndrome (OHSS) was roughly halved with the GnRH-antagonist vs. the GnRH-agonist protocol (3.2% vs. 6.1%; P = .03), as were ascites punctures (0 vs. 2%: P = .001) and treatment changes due to risk of OHSS (5.7% vs. 10.3%; P = .006).
Hospital admissions for OHSS also favored the GnRH antagonist protocol (1.7% vs. 3.6%; P = .06), Dr. Mette Toftager reported at the annual meeting of the European Society of Human Reproduction and Embryology.
The exact impact of these protocols has been controversial following early reports that GnRH antagonists were associated with lower pregnancy rates.
Two 2006 meta-analyses yielded conflicting results, but were based on small heterogeneous trials that were not powered for OHSS nor pregnancy rates and were conducted in selected populations, said Dr. Toftager of Fertility Clinic, Hvidovre Hospital, Denmark.
The current noninferiority trial used few inclusion criteria – just age 18-40 years and first in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) cycle – to prospectively enroll 1,099 women and evenly randomize them to a classic short GnRH-antagonist protocol or a classic long GnRH-agonist protocol.
Women received a fixed dose of either recombinant follicle stimulating hormone 150 IU or 225 IU based on age (≤ 36 years vs. > 36 years) and were given the option to adjust the rFSH dose based on ovarian response at stimulation day 6.
The trial was designed to detect a 2.5% difference in moderate/severe OHSS per Golan OHSS criteria between the two groups, stratified by age, IVF center, and IVF/ICSI.
At baseline, the two groups were comparable in age (mean 32 years), cycle length (mean 28.9 days), and nulliparity (92.3%). The study included women with irregular cycles and polycystic ovary syndrome, who represented about 13% of each group.
Regarding stimulation, significant differences were found between the GnRH-antagonist and GnRH-agonist groups in total rFSH dose (mean 1,522 IU vs. 1,999 IU), days of stimulation (mean 9 vs. 11), and the number of aspirated oocytes (mean 8.5 vs. 10; P < .0001 for all), Dr. Toftager reported.
The GnRH-antagonist and GnRH-agonist groups had the same number of embryos transferred (mean 1.1 vs. 1.2), use of embryo freezing (50% vs. 53%), and number of frozen embryos (mean 3.2 vs. 3.4).
By all measures used, pregnancy outcomes were similar between protocols, she said.
The GnRH-antagonist and GnRH-agonist groups had similar clinical pregnancy rates (35% vs. 35.7%) and clinical pregnancies per embryo transfer (42.6% vs. 41%). There were similar results for ongoing pregnancy rates analyzed per randomization (25.5% vs. 26.4%), if patient started stimulation (24.8% vs. 24.0%), and per embryo transfer (30.7% vs. 29%).
During a discussion of the results, an audience member questioned the high FSH starting doses and suggested they may be the cause of OHSS. Dr. Toftager said the trial was designed in 2007 and that they now use lower FSH doses, but that starting doses were the same in both groups.
Another attendee asked whether OHSS rates remained statistically significant after controlling for the number of oocytes collected and the gonadotropin dose, which were significantly lower in the GnRH-antagonist group and hence, so was OHSS. That analysis will likely be conducted, but the data were just received days before the presentation, Dr. Toftager said.
Merck Sharp & Dohme sponsored the study. Dr. Toftager reported having no financial conflicts.
On Twitter @pwendl
LISBON – Women undergoing assisted reproduction had similar pregnancy rates with gonadotropin-releasing hormone agonist and antagonist protocols, but less ovarian hyperstimulation syndrome with the GnRH-antagonist protocol in a large randomized trial.
Severe ovarian hyperstimulation syndrome (OHSS) was roughly halved with the GnRH-antagonist vs. the GnRH-agonist protocol (3.2% vs. 6.1%; P = .03), as were ascites punctures (0 vs. 2%: P = .001) and treatment changes due to risk of OHSS (5.7% vs. 10.3%; P = .006).
Hospital admissions for OHSS also favored the GnRH antagonist protocol (1.7% vs. 3.6%; P = .06), Dr. Mette Toftager reported at the annual meeting of the European Society of Human Reproduction and Embryology.
The exact impact of these protocols has been controversial following early reports that GnRH antagonists were associated with lower pregnancy rates.
Two 2006 meta-analyses yielded conflicting results, but were based on small heterogeneous trials that were not powered for OHSS nor pregnancy rates and were conducted in selected populations, said Dr. Toftager of Fertility Clinic, Hvidovre Hospital, Denmark.
The current noninferiority trial used few inclusion criteria – just age 18-40 years and first in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) cycle – to prospectively enroll 1,099 women and evenly randomize them to a classic short GnRH-antagonist protocol or a classic long GnRH-agonist protocol.
Women received a fixed dose of either recombinant follicle stimulating hormone 150 IU or 225 IU based on age (≤ 36 years vs. > 36 years) and were given the option to adjust the rFSH dose based on ovarian response at stimulation day 6.
The trial was designed to detect a 2.5% difference in moderate/severe OHSS per Golan OHSS criteria between the two groups, stratified by age, IVF center, and IVF/ICSI.
At baseline, the two groups were comparable in age (mean 32 years), cycle length (mean 28.9 days), and nulliparity (92.3%). The study included women with irregular cycles and polycystic ovary syndrome, who represented about 13% of each group.
Regarding stimulation, significant differences were found between the GnRH-antagonist and GnRH-agonist groups in total rFSH dose (mean 1,522 IU vs. 1,999 IU), days of stimulation (mean 9 vs. 11), and the number of aspirated oocytes (mean 8.5 vs. 10; P < .0001 for all), Dr. Toftager reported.
The GnRH-antagonist and GnRH-agonist groups had the same number of embryos transferred (mean 1.1 vs. 1.2), use of embryo freezing (50% vs. 53%), and number of frozen embryos (mean 3.2 vs. 3.4).
By all measures used, pregnancy outcomes were similar between protocols, she said.
The GnRH-antagonist and GnRH-agonist groups had similar clinical pregnancy rates (35% vs. 35.7%) and clinical pregnancies per embryo transfer (42.6% vs. 41%). There were similar results for ongoing pregnancy rates analyzed per randomization (25.5% vs. 26.4%), if patient started stimulation (24.8% vs. 24.0%), and per embryo transfer (30.7% vs. 29%).
During a discussion of the results, an audience member questioned the high FSH starting doses and suggested they may be the cause of OHSS. Dr. Toftager said the trial was designed in 2007 and that they now use lower FSH doses, but that starting doses were the same in both groups.
Another attendee asked whether OHSS rates remained statistically significant after controlling for the number of oocytes collected and the gonadotropin dose, which were significantly lower in the GnRH-antagonist group and hence, so was OHSS. That analysis will likely be conducted, but the data were just received days before the presentation, Dr. Toftager said.
Merck Sharp & Dohme sponsored the study. Dr. Toftager reported having no financial conflicts.
On Twitter @pwendl
LISBON – Women undergoing assisted reproduction had similar pregnancy rates with gonadotropin-releasing hormone agonist and antagonist protocols, but less ovarian hyperstimulation syndrome with the GnRH-antagonist protocol in a large randomized trial.
Severe ovarian hyperstimulation syndrome (OHSS) was roughly halved with the GnRH-antagonist vs. the GnRH-agonist protocol (3.2% vs. 6.1%; P = .03), as were ascites punctures (0 vs. 2%: P = .001) and treatment changes due to risk of OHSS (5.7% vs. 10.3%; P = .006).
Hospital admissions for OHSS also favored the GnRH antagonist protocol (1.7% vs. 3.6%; P = .06), Dr. Mette Toftager reported at the annual meeting of the European Society of Human Reproduction and Embryology.
The exact impact of these protocols has been controversial following early reports that GnRH antagonists were associated with lower pregnancy rates.
Two 2006 meta-analyses yielded conflicting results, but were based on small heterogeneous trials that were not powered for OHSS nor pregnancy rates and were conducted in selected populations, said Dr. Toftager of Fertility Clinic, Hvidovre Hospital, Denmark.
The current noninferiority trial used few inclusion criteria – just age 18-40 years and first in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) cycle – to prospectively enroll 1,099 women and evenly randomize them to a classic short GnRH-antagonist protocol or a classic long GnRH-agonist protocol.
Women received a fixed dose of either recombinant follicle stimulating hormone 150 IU or 225 IU based on age (≤ 36 years vs. > 36 years) and were given the option to adjust the rFSH dose based on ovarian response at stimulation day 6.
The trial was designed to detect a 2.5% difference in moderate/severe OHSS per Golan OHSS criteria between the two groups, stratified by age, IVF center, and IVF/ICSI.
At baseline, the two groups were comparable in age (mean 32 years), cycle length (mean 28.9 days), and nulliparity (92.3%). The study included women with irregular cycles and polycystic ovary syndrome, who represented about 13% of each group.
Regarding stimulation, significant differences were found between the GnRH-antagonist and GnRH-agonist groups in total rFSH dose (mean 1,522 IU vs. 1,999 IU), days of stimulation (mean 9 vs. 11), and the number of aspirated oocytes (mean 8.5 vs. 10; P < .0001 for all), Dr. Toftager reported.
The GnRH-antagonist and GnRH-agonist groups had the same number of embryos transferred (mean 1.1 vs. 1.2), use of embryo freezing (50% vs. 53%), and number of frozen embryos (mean 3.2 vs. 3.4).
By all measures used, pregnancy outcomes were similar between protocols, she said.
The GnRH-antagonist and GnRH-agonist groups had similar clinical pregnancy rates (35% vs. 35.7%) and clinical pregnancies per embryo transfer (42.6% vs. 41%). There were similar results for ongoing pregnancy rates analyzed per randomization (25.5% vs. 26.4%), if patient started stimulation (24.8% vs. 24.0%), and per embryo transfer (30.7% vs. 29%).
During a discussion of the results, an audience member questioned the high FSH starting doses and suggested they may be the cause of OHSS. Dr. Toftager said the trial was designed in 2007 and that they now use lower FSH doses, but that starting doses were the same in both groups.
Another attendee asked whether OHSS rates remained statistically significant after controlling for the number of oocytes collected and the gonadotropin dose, which were significantly lower in the GnRH-antagonist group and hence, so was OHSS. That analysis will likely be conducted, but the data were just received days before the presentation, Dr. Toftager said.
Merck Sharp & Dohme sponsored the study. Dr. Toftager reported having no financial conflicts.
On Twitter @pwendl
AT ESHRE 2015
Key clinical point: Pregnancy rates are similar with short GnRH-antagonist and long GnRH-agonist protocols, but severe ovarian hyperstimulation is reduced with the short protocol in first IVF/ICSI-cycle patients.
Major finding: Severe OHSS occurred in 3.2% with the GnRH-antagonist protocol vs. 6.1% with the GnRH-agonist protocol (P = .03).
Data source: A randomized, controlled trial of 1,099 first IVF/ICSI-cycle women.
Disclosures: Merck Sharp & Dohme sponsored the study. Dr. Toftager reported having no financial conflicts.
5 ways to reduce infection risk during pregnancy
Pregnant women may be more severelyaffected by certain microorganisms than nonpregnant individuals.1 In a recent review, Kourtis and colleagues cited evidence for increased mortality risk for pregnant patients related to 5 specific infections.1 What are those infections and why does pregnancy put a woman at greater risk for adverse outcomes? I review these topics in this article and, based on this evidence, I suggest 5 specific ways to avoid infection during pregnancy.
Five infections that can lead to detrimental outcomes during pregnancy
Influenza
During the pandemic of 1918, maternal mortality was 27%. During the 1957 pandemic, 50% of influenza-related deaths among women of reproductive age occurred among pregnant women. In the 2009 H1N1 influenza A pandemic, pregnant women were clearly at increased risk for severe disease, reflected by an increased frequency of hospitalization and increased likelihood of admission to an intensive care unit.
Hepatitis E
Compared with nonpregnant women and men, pregnant women also are at markedly increased risk for mortality due to hepa-titis E infection, especially in Southeast Asia, the Middle East, and Africa. The pathophysiologic basis for this increase is not well understood. Interestingly, in a report from India, 33% to 43% of pregnant women infected with hepatitis E had such severe disease that they developed hepatic failure.
Herpes simplex virus
Pregnant women with primary herpes simplex virus (HSV) infection are at increased risk for hepatitis and for disseminated infection, compared with other nonpregnant adults. Only patients with obvious immunodeficiency disorders are at greater risk for disseminated HSV infection.
Malaria
Pregnant women are at significantly increased risk for acquiring Plasmodium falciparum malaria and developing severe, life-threatening disease. In multiple studies from the Asia-Pacific region, pregnant women have been threefold more likely to acquire malaria compared with nonpregnant individuals. In India, during the period 2004 to 2006, malaria was the most common cause of maternal death.
The most likely explanation for the deleterious effect of this particular form of malaria is the fact that the P falciparum parasites accumulate selectively in the placenta because they bind avidly to syncytiotrophoblastic chondroitin sulfate A. Intense inflammation in the placenta, in turn, can lead to early pregnancy loss, preterm delivery, and fetal infection.
Listeria
Another important infection to which pregnant women are particularly susceptible is listeriosis. Listeria monocytogenes may contaminate several types of food such as uncooked meats and vegetables, unpasteurized milk, and soft cheeses. The organism has a predilection to attack the placenta and fetus and can cause spontaneous abortion, stillbirth, preterm delivery, and neonatal infection. Hispanic women may be at unusually high risk for listeria.
Immune system changes during pregnancy
Certain subtle changes occur in the immune system during pregnancy, which may help explain the increased risk of acquired infection and subsequent adverse effects. These changes include1:
- Progesterone presence, which may suppress the maternal immune response and alter the balance between type-1 helper T-cell response and type-2 helper T-cell response. Type-2 cells stimulate B lymphocytes, increase antibody production, and suppress the cytotoxic T-lymphocyte response. The net effect of these changes is to decrease the robustness of cell-mediated immunity, which may impair the response of the pregnant patient to selected viral respiratory pathogens such as influenza virus.
- Increasing serum concentrations of estrogen and progesterone, which may lead to a reversible thymic involution.
- Serum concentrations of interferon-gamma, monocyte chemoattractant protein 1, and eotaxin are decreased in most pregnant women.
- Overall, serum concentrations of inflammatory cytokines are reduced and concentrations of cytokines that induce phagocytic-cell recruitment are increased.
5 ways to reduce infection risk during pregnancy
Pregnant patients clearly are not as immunosuppressed as patients receiving chemotherapy or high doses of systemic glucocorticoids. Nevertheless, the subtle alterations in their immune system just described make pregnant women increasingly susceptible to certain infections. Therefore, I suggest these take-home messages for reducing infection risk in your pregnant patients.
1. Vaccinate against the flu
All pregnant women should be vaccinated each year for influenza. If your patient becomes infected despite vaccination, treat her promptly with an antiviral medication such as oseltamivir and observe her carefully for evidence of superimposed bacterial pneumonia. If the latter complication develops, hospitalize the patient immediately and treat her with appropriate broad spectrum antibiotics. (See, “Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!”)
Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!
More than 17,000 deaths occurred worldwide in the 2009 H1N1 influenza A global pandemic.1 The dominant circulating virus in the US 2013–2014 influenza season was again H1N1. In California, H1N1 accounted for about 94% of subtyped specimens.2
In a recent case series,1 Louie and colleagues reviewed California Department of Public Health data on pregnant and postpartum women (6 weeks or less from delivery) with laboratory-confirmed influenza who died or required hospitalization in intensive care units in the 2013−2014 influenza season.
They found that, from September 29, 2013, through May 17, 2014, 17 pregnant women (median age, 29 years [range, 17−44 years]) with severe influenza were reported. Fifteen patients were hospitalized, 9 required mechanical ventilation, 5 required emergent cesarean delivery, and 4 died. Sixteen of the 17 patients were in the second or third trimester; one was in the first trimester. An additional patient was 36 days postpartum and required intensive care unit admission and mechanical ventilation for influenza-associated acute respiratory distress syndrome.
Only 2 patients, of the 14 with available information, received influenza vaccination during their pregnancy.
The 7 patients who tested positive for influenza by polymerase chain reaction also had rapid influenza diagnostic testing performed; only 1 patient had a positive rapid influenza diagnostic test result.
The authors point out that, although rapid influenza diagnostic tests produce very quick results, they can have poor sensitivity, depending on specimen type, patient age, and even virus type.3 Therefore, it is imperative to begin empiric antiviral therapy promptly in a pregnant or postpartum patient who has clinical manifestations of viral influenza regardless of rapid influenza diagnostic test results or vaccination status. Such manifestations include malaise, myalgias, arthalgias, fever, chills, cough, and pleuritic chest pain.
Treat patients with oseltamivir 75 mg orally twice daily for 5 days. If a patient is unable to take oral medications, she can be treated with zanamivir, 2 puffs inhaled twice daily for 5 days. To be most effective, treatment should be started within 48 hours of the onset of symptoms.
References
2. Ayscue P, Murray E, Uyeki T, et al. Influenza-associated intensive-care unit admissions and deaths—California, September 29, 2013-January 18, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(7):143−147.
3. Centers for Disease Control and Prevention. Evaluation of 11 commercially available rapid influenza diagnostic tests—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2012;61(43):873−876.
2. Avoid hepatitis E−endemic areas
Ideally, our patients should avoid travel to areas of the world where hepatitis E is endemic. If travel cannot be avoided, the patient should receive the new hepatitis E vaccine. This vaccine is administered in a 3-dose series; in clinical trials, it has had an efficacy of 85% to 90%.2
If a patient acquires hepatitis E infection, she should receive aggressive supportive care, with hospitalization strongly considered because of the increased risk for hepatic failure.
The clinical manifestations of hepatitis Eare very similar to those of hepatitis A: fever, malaise, anorexia, nausea, pain and tenderness in the right upper quadrant, jaundice, darkened urine, and clay-colored stools. Laboratory abnormalities in affected patients include elevated transaminase enzymes, elevated bilirubin, positive immunoglobulin M antibody against hepatitis E virus, a fourfold increase in a prior immunoglobulin G antibody titer against hepatitis E virus, and a positive test for hepatitis E RNA.2
3. Treat patients with HSV infection to avoid an outbreak during delivery
Pregnant women who develop primary or recurrent HSV infection should be treated promptly with therapeutic doses of acyclovir or valacyclovir. Patients with frequent recurrences should receive daily anti-HSV prophylaxis throughout pregnancy. Other patients should be treated prophylactically from week 36 until delivery.
4. Recommend malaria prophylaxis when appropriate
If your pregnant patient is traveling to an area of the world where malaria is endemic, she should receive appropriate prophylaxis, especially against P falciparum.
5. Vaccinate during pregnancy and promptly treat developed infections
All infections in pregnant women should be treated in a timely manner with appropriate antibiotics. Moreover, we should make a firm effort to provide all pregnant women with the following vaccinations: influenza, Tdap, and hepatitis B (if susceptible). Select patients also should receive pneumococcal vaccine (those who are immunosuppressed; have chronic medical illnessess, particulary cardiopulmonary disease; or have had a splenectomy).
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211−2218.
2. Zhang J, Zhang XF, Huang SJ, et al. Long-term efficacy of a hepatitis E vaccine. N Engl J Med. 2015;372(10):914−922.
Pregnant women may be more severelyaffected by certain microorganisms than nonpregnant individuals.1 In a recent review, Kourtis and colleagues cited evidence for increased mortality risk for pregnant patients related to 5 specific infections.1 What are those infections and why does pregnancy put a woman at greater risk for adverse outcomes? I review these topics in this article and, based on this evidence, I suggest 5 specific ways to avoid infection during pregnancy.
Five infections that can lead to detrimental outcomes during pregnancy
Influenza
During the pandemic of 1918, maternal mortality was 27%. During the 1957 pandemic, 50% of influenza-related deaths among women of reproductive age occurred among pregnant women. In the 2009 H1N1 influenza A pandemic, pregnant women were clearly at increased risk for severe disease, reflected by an increased frequency of hospitalization and increased likelihood of admission to an intensive care unit.
Hepatitis E
Compared with nonpregnant women and men, pregnant women also are at markedly increased risk for mortality due to hepa-titis E infection, especially in Southeast Asia, the Middle East, and Africa. The pathophysiologic basis for this increase is not well understood. Interestingly, in a report from India, 33% to 43% of pregnant women infected with hepatitis E had such severe disease that they developed hepatic failure.
Herpes simplex virus
Pregnant women with primary herpes simplex virus (HSV) infection are at increased risk for hepatitis and for disseminated infection, compared with other nonpregnant adults. Only patients with obvious immunodeficiency disorders are at greater risk for disseminated HSV infection.
Malaria
Pregnant women are at significantly increased risk for acquiring Plasmodium falciparum malaria and developing severe, life-threatening disease. In multiple studies from the Asia-Pacific region, pregnant women have been threefold more likely to acquire malaria compared with nonpregnant individuals. In India, during the period 2004 to 2006, malaria was the most common cause of maternal death.
The most likely explanation for the deleterious effect of this particular form of malaria is the fact that the P falciparum parasites accumulate selectively in the placenta because they bind avidly to syncytiotrophoblastic chondroitin sulfate A. Intense inflammation in the placenta, in turn, can lead to early pregnancy loss, preterm delivery, and fetal infection.
Listeria
Another important infection to which pregnant women are particularly susceptible is listeriosis. Listeria monocytogenes may contaminate several types of food such as uncooked meats and vegetables, unpasteurized milk, and soft cheeses. The organism has a predilection to attack the placenta and fetus and can cause spontaneous abortion, stillbirth, preterm delivery, and neonatal infection. Hispanic women may be at unusually high risk for listeria.
Immune system changes during pregnancy
Certain subtle changes occur in the immune system during pregnancy, which may help explain the increased risk of acquired infection and subsequent adverse effects. These changes include1:
- Progesterone presence, which may suppress the maternal immune response and alter the balance between type-1 helper T-cell response and type-2 helper T-cell response. Type-2 cells stimulate B lymphocytes, increase antibody production, and suppress the cytotoxic T-lymphocyte response. The net effect of these changes is to decrease the robustness of cell-mediated immunity, which may impair the response of the pregnant patient to selected viral respiratory pathogens such as influenza virus.
- Increasing serum concentrations of estrogen and progesterone, which may lead to a reversible thymic involution.
- Serum concentrations of interferon-gamma, monocyte chemoattractant protein 1, and eotaxin are decreased in most pregnant women.
- Overall, serum concentrations of inflammatory cytokines are reduced and concentrations of cytokines that induce phagocytic-cell recruitment are increased.
5 ways to reduce infection risk during pregnancy
Pregnant patients clearly are not as immunosuppressed as patients receiving chemotherapy or high doses of systemic glucocorticoids. Nevertheless, the subtle alterations in their immune system just described make pregnant women increasingly susceptible to certain infections. Therefore, I suggest these take-home messages for reducing infection risk in your pregnant patients.
1. Vaccinate against the flu
All pregnant women should be vaccinated each year for influenza. If your patient becomes infected despite vaccination, treat her promptly with an antiviral medication such as oseltamivir and observe her carefully for evidence of superimposed bacterial pneumonia. If the latter complication develops, hospitalize the patient immediately and treat her with appropriate broad spectrum antibiotics. (See, “Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!”)
Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!
More than 17,000 deaths occurred worldwide in the 2009 H1N1 influenza A global pandemic.1 The dominant circulating virus in the US 2013–2014 influenza season was again H1N1. In California, H1N1 accounted for about 94% of subtyped specimens.2
In a recent case series,1 Louie and colleagues reviewed California Department of Public Health data on pregnant and postpartum women (6 weeks or less from delivery) with laboratory-confirmed influenza who died or required hospitalization in intensive care units in the 2013−2014 influenza season.
They found that, from September 29, 2013, through May 17, 2014, 17 pregnant women (median age, 29 years [range, 17−44 years]) with severe influenza were reported. Fifteen patients were hospitalized, 9 required mechanical ventilation, 5 required emergent cesarean delivery, and 4 died. Sixteen of the 17 patients were in the second or third trimester; one was in the first trimester. An additional patient was 36 days postpartum and required intensive care unit admission and mechanical ventilation for influenza-associated acute respiratory distress syndrome.
Only 2 patients, of the 14 with available information, received influenza vaccination during their pregnancy.
The 7 patients who tested positive for influenza by polymerase chain reaction also had rapid influenza diagnostic testing performed; only 1 patient had a positive rapid influenza diagnostic test result.
The authors point out that, although rapid influenza diagnostic tests produce very quick results, they can have poor sensitivity, depending on specimen type, patient age, and even virus type.3 Therefore, it is imperative to begin empiric antiviral therapy promptly in a pregnant or postpartum patient who has clinical manifestations of viral influenza regardless of rapid influenza diagnostic test results or vaccination status. Such manifestations include malaise, myalgias, arthalgias, fever, chills, cough, and pleuritic chest pain.
Treat patients with oseltamivir 75 mg orally twice daily for 5 days. If a patient is unable to take oral medications, she can be treated with zanamivir, 2 puffs inhaled twice daily for 5 days. To be most effective, treatment should be started within 48 hours of the onset of symptoms.
References
2. Ayscue P, Murray E, Uyeki T, et al. Influenza-associated intensive-care unit admissions and deaths—California, September 29, 2013-January 18, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(7):143−147.
3. Centers for Disease Control and Prevention. Evaluation of 11 commercially available rapid influenza diagnostic tests—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2012;61(43):873−876.
2. Avoid hepatitis E−endemic areas
Ideally, our patients should avoid travel to areas of the world where hepatitis E is endemic. If travel cannot be avoided, the patient should receive the new hepatitis E vaccine. This vaccine is administered in a 3-dose series; in clinical trials, it has had an efficacy of 85% to 90%.2
If a patient acquires hepatitis E infection, she should receive aggressive supportive care, with hospitalization strongly considered because of the increased risk for hepatic failure.
The clinical manifestations of hepatitis Eare very similar to those of hepatitis A: fever, malaise, anorexia, nausea, pain and tenderness in the right upper quadrant, jaundice, darkened urine, and clay-colored stools. Laboratory abnormalities in affected patients include elevated transaminase enzymes, elevated bilirubin, positive immunoglobulin M antibody against hepatitis E virus, a fourfold increase in a prior immunoglobulin G antibody titer against hepatitis E virus, and a positive test for hepatitis E RNA.2
3. Treat patients with HSV infection to avoid an outbreak during delivery
Pregnant women who develop primary or recurrent HSV infection should be treated promptly with therapeutic doses of acyclovir or valacyclovir. Patients with frequent recurrences should receive daily anti-HSV prophylaxis throughout pregnancy. Other patients should be treated prophylactically from week 36 until delivery.
4. Recommend malaria prophylaxis when appropriate
If your pregnant patient is traveling to an area of the world where malaria is endemic, she should receive appropriate prophylaxis, especially against P falciparum.
5. Vaccinate during pregnancy and promptly treat developed infections
All infections in pregnant women should be treated in a timely manner with appropriate antibiotics. Moreover, we should make a firm effort to provide all pregnant women with the following vaccinations: influenza, Tdap, and hepatitis B (if susceptible). Select patients also should receive pneumococcal vaccine (those who are immunosuppressed; have chronic medical illnessess, particulary cardiopulmonary disease; or have had a splenectomy).
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Pregnant women may be more severelyaffected by certain microorganisms than nonpregnant individuals.1 In a recent review, Kourtis and colleagues cited evidence for increased mortality risk for pregnant patients related to 5 specific infections.1 What are those infections and why does pregnancy put a woman at greater risk for adverse outcomes? I review these topics in this article and, based on this evidence, I suggest 5 specific ways to avoid infection during pregnancy.
Five infections that can lead to detrimental outcomes during pregnancy
Influenza
During the pandemic of 1918, maternal mortality was 27%. During the 1957 pandemic, 50% of influenza-related deaths among women of reproductive age occurred among pregnant women. In the 2009 H1N1 influenza A pandemic, pregnant women were clearly at increased risk for severe disease, reflected by an increased frequency of hospitalization and increased likelihood of admission to an intensive care unit.
Hepatitis E
Compared with nonpregnant women and men, pregnant women also are at markedly increased risk for mortality due to hepa-titis E infection, especially in Southeast Asia, the Middle East, and Africa. The pathophysiologic basis for this increase is not well understood. Interestingly, in a report from India, 33% to 43% of pregnant women infected with hepatitis E had such severe disease that they developed hepatic failure.
Herpes simplex virus
Pregnant women with primary herpes simplex virus (HSV) infection are at increased risk for hepatitis and for disseminated infection, compared with other nonpregnant adults. Only patients with obvious immunodeficiency disorders are at greater risk for disseminated HSV infection.
Malaria
Pregnant women are at significantly increased risk for acquiring Plasmodium falciparum malaria and developing severe, life-threatening disease. In multiple studies from the Asia-Pacific region, pregnant women have been threefold more likely to acquire malaria compared with nonpregnant individuals. In India, during the period 2004 to 2006, malaria was the most common cause of maternal death.
The most likely explanation for the deleterious effect of this particular form of malaria is the fact that the P falciparum parasites accumulate selectively in the placenta because they bind avidly to syncytiotrophoblastic chondroitin sulfate A. Intense inflammation in the placenta, in turn, can lead to early pregnancy loss, preterm delivery, and fetal infection.
Listeria
Another important infection to which pregnant women are particularly susceptible is listeriosis. Listeria monocytogenes may contaminate several types of food such as uncooked meats and vegetables, unpasteurized milk, and soft cheeses. The organism has a predilection to attack the placenta and fetus and can cause spontaneous abortion, stillbirth, preterm delivery, and neonatal infection. Hispanic women may be at unusually high risk for listeria.
Immune system changes during pregnancy
Certain subtle changes occur in the immune system during pregnancy, which may help explain the increased risk of acquired infection and subsequent adverse effects. These changes include1:
- Progesterone presence, which may suppress the maternal immune response and alter the balance between type-1 helper T-cell response and type-2 helper T-cell response. Type-2 cells stimulate B lymphocytes, increase antibody production, and suppress the cytotoxic T-lymphocyte response. The net effect of these changes is to decrease the robustness of cell-mediated immunity, which may impair the response of the pregnant patient to selected viral respiratory pathogens such as influenza virus.
- Increasing serum concentrations of estrogen and progesterone, which may lead to a reversible thymic involution.
- Serum concentrations of interferon-gamma, monocyte chemoattractant protein 1, and eotaxin are decreased in most pregnant women.
- Overall, serum concentrations of inflammatory cytokines are reduced and concentrations of cytokines that induce phagocytic-cell recruitment are increased.
5 ways to reduce infection risk during pregnancy
Pregnant patients clearly are not as immunosuppressed as patients receiving chemotherapy or high doses of systemic glucocorticoids. Nevertheless, the subtle alterations in their immune system just described make pregnant women increasingly susceptible to certain infections. Therefore, I suggest these take-home messages for reducing infection risk in your pregnant patients.
1. Vaccinate against the flu
All pregnant women should be vaccinated each year for influenza. If your patient becomes infected despite vaccination, treat her promptly with an antiviral medication such as oseltamivir and observe her carefully for evidence of superimposed bacterial pneumonia. If the latter complication develops, hospitalize the patient immediately and treat her with appropriate broad spectrum antibiotics. (See, “Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!”)
Don’t wait for rapid flu test results. Treat your pregnant patient with antiviral therapy!
More than 17,000 deaths occurred worldwide in the 2009 H1N1 influenza A global pandemic.1 The dominant circulating virus in the US 2013–2014 influenza season was again H1N1. In California, H1N1 accounted for about 94% of subtyped specimens.2
In a recent case series,1 Louie and colleagues reviewed California Department of Public Health data on pregnant and postpartum women (6 weeks or less from delivery) with laboratory-confirmed influenza who died or required hospitalization in intensive care units in the 2013−2014 influenza season.
They found that, from September 29, 2013, through May 17, 2014, 17 pregnant women (median age, 29 years [range, 17−44 years]) with severe influenza were reported. Fifteen patients were hospitalized, 9 required mechanical ventilation, 5 required emergent cesarean delivery, and 4 died. Sixteen of the 17 patients were in the second or third trimester; one was in the first trimester. An additional patient was 36 days postpartum and required intensive care unit admission and mechanical ventilation for influenza-associated acute respiratory distress syndrome.
Only 2 patients, of the 14 with available information, received influenza vaccination during their pregnancy.
The 7 patients who tested positive for influenza by polymerase chain reaction also had rapid influenza diagnostic testing performed; only 1 patient had a positive rapid influenza diagnostic test result.
The authors point out that, although rapid influenza diagnostic tests produce very quick results, they can have poor sensitivity, depending on specimen type, patient age, and even virus type.3 Therefore, it is imperative to begin empiric antiviral therapy promptly in a pregnant or postpartum patient who has clinical manifestations of viral influenza regardless of rapid influenza diagnostic test results or vaccination status. Such manifestations include malaise, myalgias, arthalgias, fever, chills, cough, and pleuritic chest pain.
Treat patients with oseltamivir 75 mg orally twice daily for 5 days. If a patient is unable to take oral medications, she can be treated with zanamivir, 2 puffs inhaled twice daily for 5 days. To be most effective, treatment should be started within 48 hours of the onset of symptoms.
References
2. Ayscue P, Murray E, Uyeki T, et al. Influenza-associated intensive-care unit admissions and deaths—California, September 29, 2013-January 18, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(7):143−147.
3. Centers for Disease Control and Prevention. Evaluation of 11 commercially available rapid influenza diagnostic tests—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2012;61(43):873−876.
2. Avoid hepatitis E−endemic areas
Ideally, our patients should avoid travel to areas of the world where hepatitis E is endemic. If travel cannot be avoided, the patient should receive the new hepatitis E vaccine. This vaccine is administered in a 3-dose series; in clinical trials, it has had an efficacy of 85% to 90%.2
If a patient acquires hepatitis E infection, she should receive aggressive supportive care, with hospitalization strongly considered because of the increased risk for hepatic failure.
The clinical manifestations of hepatitis Eare very similar to those of hepatitis A: fever, malaise, anorexia, nausea, pain and tenderness in the right upper quadrant, jaundice, darkened urine, and clay-colored stools. Laboratory abnormalities in affected patients include elevated transaminase enzymes, elevated bilirubin, positive immunoglobulin M antibody against hepatitis E virus, a fourfold increase in a prior immunoglobulin G antibody titer against hepatitis E virus, and a positive test for hepatitis E RNA.2
3. Treat patients with HSV infection to avoid an outbreak during delivery
Pregnant women who develop primary or recurrent HSV infection should be treated promptly with therapeutic doses of acyclovir or valacyclovir. Patients with frequent recurrences should receive daily anti-HSV prophylaxis throughout pregnancy. Other patients should be treated prophylactically from week 36 until delivery.
4. Recommend malaria prophylaxis when appropriate
If your pregnant patient is traveling to an area of the world where malaria is endemic, she should receive appropriate prophylaxis, especially against P falciparum.
5. Vaccinate during pregnancy and promptly treat developed infections
All infections in pregnant women should be treated in a timely manner with appropriate antibiotics. Moreover, we should make a firm effort to provide all pregnant women with the following vaccinations: influenza, Tdap, and hepatitis B (if susceptible). Select patients also should receive pneumococcal vaccine (those who are immunosuppressed; have chronic medical illnessess, particulary cardiopulmonary disease; or have had a splenectomy).
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211−2218.
2. Zhang J, Zhang XF, Huang SJ, et al. Long-term efficacy of a hepatitis E vaccine. N Engl J Med. 2015;372(10):914−922.
1. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211−2218.
2. Zhang J, Zhang XF, Huang SJ, et al. Long-term efficacy of a hepatitis E vaccine. N Engl J Med. 2015;372(10):914−922.
In this article
- Infections to avoid in pregnancy
- Don’t wait for rapid flu test results!
- 5 ways to reduce infection risk
Who was responsible for excessive oxytocin doses? $18.2M verdict
Who was responsible for excessive oxytocin doses? $18.2M verdict
Early in the morning, a woman at 40 weeks’ gestation presented to the hospital for induction of labor managed by her ObGyn. Labor was lengthy, and the mother was given increasing doses of 22, 24, and 26 mIU/min of oxytocin to stimulate labor. The baby was delivered in the evening. The child suffered a hypoxic birth injury and has cerebral palsy.
Parents’ claim Excessive oxytocin was administered, causing uterine hyperstimulation and excessive contractions. Nurses failed to inform the ObGyn of an abnormal fetal heart rate during the afternoon.
Defendants’ defense The parties disputed the oxytocin orders. The ObGyn claimed she has a standing order against oxytocin doses over 20 mIU/min. The nurses claimed that the dosage was based on the ObGyn’s verbal orders, which the ObGyn denied. The ObGyn denied negligence and maintained that if she’d known of the oxytocin administration greater than 20 mIU/min and the abnormal fetal heart rate, she immediately would have called for cesarean delivery. The hospital denied negligence and maintained that the oxytocin was administered 10 hours before delivery and played no role in fetal distress.
Verdict At trial, the ObGyn did not call expert witnesses and, in closing arguments, the physician’s attorney asked for exoneration of the ObGyn and a finding of fault solely against the hospital. An $18.2 million Washington verdict was returned against the hospital.
What caused the child’s Erb’s palsy?
A mother presented to the hospital for induction of labor. Oxytocin was administered and the first stage of labor progressed normally. When the mother began pushing, the ObGyn noted a turtle sign at crowning and called for assistance. The ObGyn attempted to deliver the fetus with downward guidance of the fetal head but encountered shoulder dystocia and a nuchal cord. He unwrapped the cord and instructed the nursing staff to place the mother in the McRobert’s position to help dislodge the right shoulder. When that did not work, the ObGyn performed a first-degree episiotomy and completed delivery. The child was found to have Erb’s palsy of the right arm. She underwent decompression and neurolysis of the brachial plexus using sural nerve grafts but still has reduced use of her right arm.
Parents’ claim Shoulder dystocia was improperly managed, causing the brachial plexus injury.
Defendants’ defense The ObGyn and hospital system denied negligence. The child’s injury occurred in utero due to natural forces of the mother’s uterine contractions.
Verdict An Ohio defense verdict was returned.
Woman claims lack of proper consent
A 47-year-old woman underwent endometrial ablation performed by her ObGyn. During the procedure, the uterus was perforated and the ObGyn performed a hysterectomy. Six days later, the patient was found to have peritonitis and underwent bowel repair surgery. The patient developed untreatable bowel adhesions that cause chronic pain.
Patient’s claim There were less expensive and invasive alternatives to the ablation that the ObGyn did not offer. The patient claimed lack of informed consent for the ablation and hysterectomy and negligence in perforating the bowel. The ObGyn was also negligent in failing to recognize the perforation and to diagnose peritonitis in a timely manner.
Texas state law requires consent for hysterectomies without documented evidence of immediate danger to life. Her husband did not have the authority to consent on her behalf.
Physician’s defense The husband gave informed consent. Failure to recognize the perforation was not negligent; it is a known risk of the surgery. The patient’s care was transferred to another physician after the second postoperative day.
Verdict A $200,000 Texas settlement was reached.
Bowel obstruction in pregnant woman
A 29-year-old woman at 27 weeks’ gestation had abdominal pain. She went to a community hospital where a hospitalist was assigned to her care. After a day, the patient was found to have a small bowel obstruction and necrosis of the bowel. The baby was delivered preterm. The mother underwent 12 operations; half of her intestines were resected. The mother is being treated for posttraumatic stress syndrome. The child is autistic.
Parents’ claim The hospitalist did not diagnose the mother’s intestinal blockage in a timely manner and did not obtain an obstetric consult or notify the patient’s ObGyn. The hospital staff did not follow protocol to notify the mother’s ObGyn. The child’s autism is a result of preterm delivery.
Defendants’ defense The hospital denied any duty to notify the ObGyn if the patient was admitted to the hospital for nonobstetric reasons. The case was settled during trial.
Verdict A $4.2 million Washington settlement was reached including $3 million from the hospital.
Fourth-degree perineal tear and continuing pain after delivery
A woman in her 30s went to the hospital for induction of labor. After many hours, the ObGyn used vacuum extraction due to maternal fatigue. The baby emerged in compound presentation, with her hand at the side of her head. She weighed 9 lb 12 oz at birth. A fourth-degree perineal tear occurred at birth. Postpartum, a rectovaginal fistula developed that required several repair operations. The mother is unable to have intercourse due to continuing vaginal pain and discomfort.
Patient’s Claim Knowing that the father’s head was overly large, the ObGyn should have better estimated the fetus’ size, and should have performed cesarean delivery.
Physician’s defense The ObGyn admitted that he knew the baby was large but maintained that a large fetus does not mandate a cesarean delivery. There were no indications that the baby’s head or body was too large to fit through the mother’s pelvis, so a vaginal delivery was appropriate. A perineal tear is a known complication of childbirth and could not be prevented. The patient’s current pain is unrelated to the perineal tear.
Verdict A Pennsylvania defense verdict was returned.
Breast cancer missed in woman with dense breasts
In 2003, a 44-year-old woman was told she had dense fibrocystic breasts. From 2003 through 2009 she regularly saw a breast surgeon due to concern that breast cancer might be difficult to detect.
In August 2009, her ObGyn identified a questionable mass in her left breast after ultrasonography and mammography. The patient saw the surgeon in late September 2009; no further imaging was ordered and she was told to return in a year.
The patient, concerned about the mass, returned to the surgeon in May 2010. Testing revealed cancer, and she underwent radical mastectomy and other treatment.
Patient’s claim Because the mass had not been treated in a timely manner, her 5-year survival rate in May 2010 was less than 50%. The surgeon was negligent in failing to order additional testing in September 2009. Magnetic resonance imaging (MRI) would have detected the cancer at a time when her survival rate could have been 80%.
Physician’s defense The cancer was diagnosed in a timely manner. An earlier diagnosis would not have changed the outcome.
Verdict A Tennessee defense verdict was returned.
Child stillborn, mother injured after vacuum extraction
When the mother’s labor slowed at a birthing center, she received several medications including castor oil, blue cohosh, and black cohosh to induce labor. The mother was later transferred by ambulance to a hospital. Ninety minutes after admission, the ObGyn used vacuum extraction to deliver a stillborn child. The mother sustained damage to her rectum, uterus, and vagina, had repair surgery, and has been unable to get pregnant again.
Parents’ claim While in labor at the birthing center, the castor oil, blue cohosh, and black cohosh caused the patient’s uterus to contract excessively and contributed to fetal death. The patient should have been transferred to the hospital earlier. Cesarean delivery should have been performed immediately upon her arrival at the hospital but the ObGyn did not arrive at the hospital for an hour after the patient’s admission.
Defendants’ defense The head midwife at the birthing center conceded negligence. The hospital claimed that the fetus was already dead before the mother arrived. The ObGyn denied negligence, arguing that he had no supervisory role or ownership in the birthing center and was not present during the mother’s labor. He also claimed that the fetus was dead in utero 12 or more hours before delivery and that an infectious process had developed in the mother during the 17 hours that she was at the birthing center.
Verdict A $4,095,000 Florida verdict was returned against the ObGyn. A directed verdict was granted for the hospital.
Patient still in pain after labia reduction
A 44-year-old woman underwent surgical reduction of her labia minora performed by a gynecologist. The procedure was intended to relieve discomfort during sexual activity. The patient continues to have pain.
Patient’s claim An excessive amount of the right labia minora was removed because proper presurgical demarcation of the operative area was not performed. Her pain during intercourse has worsened and she cannot properly urinate.
Physician’s defense Presurgical demarcation was correctly completed using clamps. Surgery was properly performed. The asymmetry is due to poor healing of the surgical wound. The patient’s clitoris was not scarred. The patient never reported complications related to urination to her gynecologist. Her ongoing pain is due to an estrogen deficiency.
Verdict A New York defense verdict was returned.
Uterine rupture after version for breech presentation: $7M
A woman went to the hospital for delivery of her baby. The fetus was in breech position, but the mother requested vaginal delivery. When the ObGyn attempted an external cephalic version to turn the baby, the uterus ruptured and the placenta was damaged. The baby sustained hypoxic-ischemic encephalopathy resulting in cerebral palsy (CP). He requires constant nursing care.
Parents’ claim The ObGyn failed to recognize fetal distress during the breech version. The ObGyn improperly performed the version, causing the uterine rupture. There was lack of informed consent for the version.
Defendants’ defense The case was settled during trial.
Verdict A $7 million New Jersey settlement was reached.
Sepsis following hysterectomy
An ObGyn performed total abdominal hysterectomy to treat uterine fibroids in a 26-year-old woman. Despite reporting abdominal pain, the patient was discharged on postsurgical day 4.
Three days later, she went to a different hospital with moderate diffuse abdominal pain, constipation, nausea, emesis, tachycardia, and low-grade fever. An abdominal radiograph was taken, the patient was given morphine and ketorolac, and she was sent home.
She returned to the first hospital 3 days later reporting fever, nausea, emesis, diarrhea, and severe abdominal pain. After an abdominal computed tomography (CT) scan revealed numerous fluid- and gas-filled collections, indicative of abscess, intravenous antibiotics were ordered and administered.
Six days later, an infectious disease physician was consulted. He made a diagnosis of sepsis secondary to abdominal infection.
The next day, an abdominal CT scan revealed enlargement of multiple abdominal and pelvic fluid collections.
At exploratory laparotomy, purulent fluid was found in the anterior fascial compartment, with gross pus in the abdomen. The entire bowel was dilated, inflamed, and matted. Necrotic rind and infection were noted on multiple surfaces of the colon and small intestine and the transverse colon was gangrenous and sealed to the right lower quadrant. The patient’s intestines were resected and an ileostomy was placed, which was reversed several months later.
Patient’s claim The ObGyn did not offer an alternative to hysterectomy. The ObGyn was negligent in injuring the small intestine during surgery and failing to recognize and treat it intraoperatively. The patient should not have been discharged based on her reported symptoms. Failure to recognize and treat the injury led to sepsis with severe complications and months of recuperation.
Physician’s defense There was no negligence; small bowel injury is a known risk of hysterectomy. Other caregivers at both hospitals were at fault for not properly diagnosing and treating the infection.
Verdict A $901,420 Nevada verdict was returned; the ObGyn was found 85% at fault and other parties 15% at fault. The court granted the physician’s motion to reduce the verdict to $436,954, which included $371,411 from the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements, & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Who was responsible for excessive oxytocin doses? $18.2M verdict
Early in the morning, a woman at 40 weeks’ gestation presented to the hospital for induction of labor managed by her ObGyn. Labor was lengthy, and the mother was given increasing doses of 22, 24, and 26 mIU/min of oxytocin to stimulate labor. The baby was delivered in the evening. The child suffered a hypoxic birth injury and has cerebral palsy.
Parents’ claim Excessive oxytocin was administered, causing uterine hyperstimulation and excessive contractions. Nurses failed to inform the ObGyn of an abnormal fetal heart rate during the afternoon.
Defendants’ defense The parties disputed the oxytocin orders. The ObGyn claimed she has a standing order against oxytocin doses over 20 mIU/min. The nurses claimed that the dosage was based on the ObGyn’s verbal orders, which the ObGyn denied. The ObGyn denied negligence and maintained that if she’d known of the oxytocin administration greater than 20 mIU/min and the abnormal fetal heart rate, she immediately would have called for cesarean delivery. The hospital denied negligence and maintained that the oxytocin was administered 10 hours before delivery and played no role in fetal distress.
Verdict At trial, the ObGyn did not call expert witnesses and, in closing arguments, the physician’s attorney asked for exoneration of the ObGyn and a finding of fault solely against the hospital. An $18.2 million Washington verdict was returned against the hospital.
What caused the child’s Erb’s palsy?
A mother presented to the hospital for induction of labor. Oxytocin was administered and the first stage of labor progressed normally. When the mother began pushing, the ObGyn noted a turtle sign at crowning and called for assistance. The ObGyn attempted to deliver the fetus with downward guidance of the fetal head but encountered shoulder dystocia and a nuchal cord. He unwrapped the cord and instructed the nursing staff to place the mother in the McRobert’s position to help dislodge the right shoulder. When that did not work, the ObGyn performed a first-degree episiotomy and completed delivery. The child was found to have Erb’s palsy of the right arm. She underwent decompression and neurolysis of the brachial plexus using sural nerve grafts but still has reduced use of her right arm.
Parents’ claim Shoulder dystocia was improperly managed, causing the brachial plexus injury.
Defendants’ defense The ObGyn and hospital system denied negligence. The child’s injury occurred in utero due to natural forces of the mother’s uterine contractions.
Verdict An Ohio defense verdict was returned.
Woman claims lack of proper consent
A 47-year-old woman underwent endometrial ablation performed by her ObGyn. During the procedure, the uterus was perforated and the ObGyn performed a hysterectomy. Six days later, the patient was found to have peritonitis and underwent bowel repair surgery. The patient developed untreatable bowel adhesions that cause chronic pain.
Patient’s claim There were less expensive and invasive alternatives to the ablation that the ObGyn did not offer. The patient claimed lack of informed consent for the ablation and hysterectomy and negligence in perforating the bowel. The ObGyn was also negligent in failing to recognize the perforation and to diagnose peritonitis in a timely manner.
Texas state law requires consent for hysterectomies without documented evidence of immediate danger to life. Her husband did not have the authority to consent on her behalf.
Physician’s defense The husband gave informed consent. Failure to recognize the perforation was not negligent; it is a known risk of the surgery. The patient’s care was transferred to another physician after the second postoperative day.
Verdict A $200,000 Texas settlement was reached.
Bowel obstruction in pregnant woman
A 29-year-old woman at 27 weeks’ gestation had abdominal pain. She went to a community hospital where a hospitalist was assigned to her care. After a day, the patient was found to have a small bowel obstruction and necrosis of the bowel. The baby was delivered preterm. The mother underwent 12 operations; half of her intestines were resected. The mother is being treated for posttraumatic stress syndrome. The child is autistic.
Parents’ claim The hospitalist did not diagnose the mother’s intestinal blockage in a timely manner and did not obtain an obstetric consult or notify the patient’s ObGyn. The hospital staff did not follow protocol to notify the mother’s ObGyn. The child’s autism is a result of preterm delivery.
Defendants’ defense The hospital denied any duty to notify the ObGyn if the patient was admitted to the hospital for nonobstetric reasons. The case was settled during trial.
Verdict A $4.2 million Washington settlement was reached including $3 million from the hospital.
Fourth-degree perineal tear and continuing pain after delivery
A woman in her 30s went to the hospital for induction of labor. After many hours, the ObGyn used vacuum extraction due to maternal fatigue. The baby emerged in compound presentation, with her hand at the side of her head. She weighed 9 lb 12 oz at birth. A fourth-degree perineal tear occurred at birth. Postpartum, a rectovaginal fistula developed that required several repair operations. The mother is unable to have intercourse due to continuing vaginal pain and discomfort.
Patient’s Claim Knowing that the father’s head was overly large, the ObGyn should have better estimated the fetus’ size, and should have performed cesarean delivery.
Physician’s defense The ObGyn admitted that he knew the baby was large but maintained that a large fetus does not mandate a cesarean delivery. There were no indications that the baby’s head or body was too large to fit through the mother’s pelvis, so a vaginal delivery was appropriate. A perineal tear is a known complication of childbirth and could not be prevented. The patient’s current pain is unrelated to the perineal tear.
Verdict A Pennsylvania defense verdict was returned.
Breast cancer missed in woman with dense breasts
In 2003, a 44-year-old woman was told she had dense fibrocystic breasts. From 2003 through 2009 she regularly saw a breast surgeon due to concern that breast cancer might be difficult to detect.
In August 2009, her ObGyn identified a questionable mass in her left breast after ultrasonography and mammography. The patient saw the surgeon in late September 2009; no further imaging was ordered and she was told to return in a year.
The patient, concerned about the mass, returned to the surgeon in May 2010. Testing revealed cancer, and she underwent radical mastectomy and other treatment.
Patient’s claim Because the mass had not been treated in a timely manner, her 5-year survival rate in May 2010 was less than 50%. The surgeon was negligent in failing to order additional testing in September 2009. Magnetic resonance imaging (MRI) would have detected the cancer at a time when her survival rate could have been 80%.
Physician’s defense The cancer was diagnosed in a timely manner. An earlier diagnosis would not have changed the outcome.
Verdict A Tennessee defense verdict was returned.
Child stillborn, mother injured after vacuum extraction
When the mother’s labor slowed at a birthing center, she received several medications including castor oil, blue cohosh, and black cohosh to induce labor. The mother was later transferred by ambulance to a hospital. Ninety minutes after admission, the ObGyn used vacuum extraction to deliver a stillborn child. The mother sustained damage to her rectum, uterus, and vagina, had repair surgery, and has been unable to get pregnant again.
Parents’ claim While in labor at the birthing center, the castor oil, blue cohosh, and black cohosh caused the patient’s uterus to contract excessively and contributed to fetal death. The patient should have been transferred to the hospital earlier. Cesarean delivery should have been performed immediately upon her arrival at the hospital but the ObGyn did not arrive at the hospital for an hour after the patient’s admission.
Defendants’ defense The head midwife at the birthing center conceded negligence. The hospital claimed that the fetus was already dead before the mother arrived. The ObGyn denied negligence, arguing that he had no supervisory role or ownership in the birthing center and was not present during the mother’s labor. He also claimed that the fetus was dead in utero 12 or more hours before delivery and that an infectious process had developed in the mother during the 17 hours that she was at the birthing center.
Verdict A $4,095,000 Florida verdict was returned against the ObGyn. A directed verdict was granted for the hospital.
Patient still in pain after labia reduction
A 44-year-old woman underwent surgical reduction of her labia minora performed by a gynecologist. The procedure was intended to relieve discomfort during sexual activity. The patient continues to have pain.
Patient’s claim An excessive amount of the right labia minora was removed because proper presurgical demarcation of the operative area was not performed. Her pain during intercourse has worsened and she cannot properly urinate.
Physician’s defense Presurgical demarcation was correctly completed using clamps. Surgery was properly performed. The asymmetry is due to poor healing of the surgical wound. The patient’s clitoris was not scarred. The patient never reported complications related to urination to her gynecologist. Her ongoing pain is due to an estrogen deficiency.
Verdict A New York defense verdict was returned.
Uterine rupture after version for breech presentation: $7M
A woman went to the hospital for delivery of her baby. The fetus was in breech position, but the mother requested vaginal delivery. When the ObGyn attempted an external cephalic version to turn the baby, the uterus ruptured and the placenta was damaged. The baby sustained hypoxic-ischemic encephalopathy resulting in cerebral palsy (CP). He requires constant nursing care.
Parents’ claim The ObGyn failed to recognize fetal distress during the breech version. The ObGyn improperly performed the version, causing the uterine rupture. There was lack of informed consent for the version.
Defendants’ defense The case was settled during trial.
Verdict A $7 million New Jersey settlement was reached.
Sepsis following hysterectomy
An ObGyn performed total abdominal hysterectomy to treat uterine fibroids in a 26-year-old woman. Despite reporting abdominal pain, the patient was discharged on postsurgical day 4.
Three days later, she went to a different hospital with moderate diffuse abdominal pain, constipation, nausea, emesis, tachycardia, and low-grade fever. An abdominal radiograph was taken, the patient was given morphine and ketorolac, and she was sent home.
She returned to the first hospital 3 days later reporting fever, nausea, emesis, diarrhea, and severe abdominal pain. After an abdominal computed tomography (CT) scan revealed numerous fluid- and gas-filled collections, indicative of abscess, intravenous antibiotics were ordered and administered.
Six days later, an infectious disease physician was consulted. He made a diagnosis of sepsis secondary to abdominal infection.
The next day, an abdominal CT scan revealed enlargement of multiple abdominal and pelvic fluid collections.
At exploratory laparotomy, purulent fluid was found in the anterior fascial compartment, with gross pus in the abdomen. The entire bowel was dilated, inflamed, and matted. Necrotic rind and infection were noted on multiple surfaces of the colon and small intestine and the transverse colon was gangrenous and sealed to the right lower quadrant. The patient’s intestines were resected and an ileostomy was placed, which was reversed several months later.
Patient’s claim The ObGyn did not offer an alternative to hysterectomy. The ObGyn was negligent in injuring the small intestine during surgery and failing to recognize and treat it intraoperatively. The patient should not have been discharged based on her reported symptoms. Failure to recognize and treat the injury led to sepsis with severe complications and months of recuperation.
Physician’s defense There was no negligence; small bowel injury is a known risk of hysterectomy. Other caregivers at both hospitals were at fault for not properly diagnosing and treating the infection.
Verdict A $901,420 Nevada verdict was returned; the ObGyn was found 85% at fault and other parties 15% at fault. The court granted the physician’s motion to reduce the verdict to $436,954, which included $371,411 from the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements, & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Who was responsible for excessive oxytocin doses? $18.2M verdict
Early in the morning, a woman at 40 weeks’ gestation presented to the hospital for induction of labor managed by her ObGyn. Labor was lengthy, and the mother was given increasing doses of 22, 24, and 26 mIU/min of oxytocin to stimulate labor. The baby was delivered in the evening. The child suffered a hypoxic birth injury and has cerebral palsy.
Parents’ claim Excessive oxytocin was administered, causing uterine hyperstimulation and excessive contractions. Nurses failed to inform the ObGyn of an abnormal fetal heart rate during the afternoon.
Defendants’ defense The parties disputed the oxytocin orders. The ObGyn claimed she has a standing order against oxytocin doses over 20 mIU/min. The nurses claimed that the dosage was based on the ObGyn’s verbal orders, which the ObGyn denied. The ObGyn denied negligence and maintained that if she’d known of the oxytocin administration greater than 20 mIU/min and the abnormal fetal heart rate, she immediately would have called for cesarean delivery. The hospital denied negligence and maintained that the oxytocin was administered 10 hours before delivery and played no role in fetal distress.
Verdict At trial, the ObGyn did not call expert witnesses and, in closing arguments, the physician’s attorney asked for exoneration of the ObGyn and a finding of fault solely against the hospital. An $18.2 million Washington verdict was returned against the hospital.
What caused the child’s Erb’s palsy?
A mother presented to the hospital for induction of labor. Oxytocin was administered and the first stage of labor progressed normally. When the mother began pushing, the ObGyn noted a turtle sign at crowning and called for assistance. The ObGyn attempted to deliver the fetus with downward guidance of the fetal head but encountered shoulder dystocia and a nuchal cord. He unwrapped the cord and instructed the nursing staff to place the mother in the McRobert’s position to help dislodge the right shoulder. When that did not work, the ObGyn performed a first-degree episiotomy and completed delivery. The child was found to have Erb’s palsy of the right arm. She underwent decompression and neurolysis of the brachial plexus using sural nerve grafts but still has reduced use of her right arm.
Parents’ claim Shoulder dystocia was improperly managed, causing the brachial plexus injury.
Defendants’ defense The ObGyn and hospital system denied negligence. The child’s injury occurred in utero due to natural forces of the mother’s uterine contractions.
Verdict An Ohio defense verdict was returned.
Woman claims lack of proper consent
A 47-year-old woman underwent endometrial ablation performed by her ObGyn. During the procedure, the uterus was perforated and the ObGyn performed a hysterectomy. Six days later, the patient was found to have peritonitis and underwent bowel repair surgery. The patient developed untreatable bowel adhesions that cause chronic pain.
Patient’s claim There were less expensive and invasive alternatives to the ablation that the ObGyn did not offer. The patient claimed lack of informed consent for the ablation and hysterectomy and negligence in perforating the bowel. The ObGyn was also negligent in failing to recognize the perforation and to diagnose peritonitis in a timely manner.
Texas state law requires consent for hysterectomies without documented evidence of immediate danger to life. Her husband did not have the authority to consent on her behalf.
Physician’s defense The husband gave informed consent. Failure to recognize the perforation was not negligent; it is a known risk of the surgery. The patient’s care was transferred to another physician after the second postoperative day.
Verdict A $200,000 Texas settlement was reached.
Bowel obstruction in pregnant woman
A 29-year-old woman at 27 weeks’ gestation had abdominal pain. She went to a community hospital where a hospitalist was assigned to her care. After a day, the patient was found to have a small bowel obstruction and necrosis of the bowel. The baby was delivered preterm. The mother underwent 12 operations; half of her intestines were resected. The mother is being treated for posttraumatic stress syndrome. The child is autistic.
Parents’ claim The hospitalist did not diagnose the mother’s intestinal blockage in a timely manner and did not obtain an obstetric consult or notify the patient’s ObGyn. The hospital staff did not follow protocol to notify the mother’s ObGyn. The child’s autism is a result of preterm delivery.
Defendants’ defense The hospital denied any duty to notify the ObGyn if the patient was admitted to the hospital for nonobstetric reasons. The case was settled during trial.
Verdict A $4.2 million Washington settlement was reached including $3 million from the hospital.
Fourth-degree perineal tear and continuing pain after delivery
A woman in her 30s went to the hospital for induction of labor. After many hours, the ObGyn used vacuum extraction due to maternal fatigue. The baby emerged in compound presentation, with her hand at the side of her head. She weighed 9 lb 12 oz at birth. A fourth-degree perineal tear occurred at birth. Postpartum, a rectovaginal fistula developed that required several repair operations. The mother is unable to have intercourse due to continuing vaginal pain and discomfort.
Patient’s Claim Knowing that the father’s head was overly large, the ObGyn should have better estimated the fetus’ size, and should have performed cesarean delivery.
Physician’s defense The ObGyn admitted that he knew the baby was large but maintained that a large fetus does not mandate a cesarean delivery. There were no indications that the baby’s head or body was too large to fit through the mother’s pelvis, so a vaginal delivery was appropriate. A perineal tear is a known complication of childbirth and could not be prevented. The patient’s current pain is unrelated to the perineal tear.
Verdict A Pennsylvania defense verdict was returned.
Breast cancer missed in woman with dense breasts
In 2003, a 44-year-old woman was told she had dense fibrocystic breasts. From 2003 through 2009 she regularly saw a breast surgeon due to concern that breast cancer might be difficult to detect.
In August 2009, her ObGyn identified a questionable mass in her left breast after ultrasonography and mammography. The patient saw the surgeon in late September 2009; no further imaging was ordered and she was told to return in a year.
The patient, concerned about the mass, returned to the surgeon in May 2010. Testing revealed cancer, and she underwent radical mastectomy and other treatment.
Patient’s claim Because the mass had not been treated in a timely manner, her 5-year survival rate in May 2010 was less than 50%. The surgeon was negligent in failing to order additional testing in September 2009. Magnetic resonance imaging (MRI) would have detected the cancer at a time when her survival rate could have been 80%.
Physician’s defense The cancer was diagnosed in a timely manner. An earlier diagnosis would not have changed the outcome.
Verdict A Tennessee defense verdict was returned.
Child stillborn, mother injured after vacuum extraction
When the mother’s labor slowed at a birthing center, she received several medications including castor oil, blue cohosh, and black cohosh to induce labor. The mother was later transferred by ambulance to a hospital. Ninety minutes after admission, the ObGyn used vacuum extraction to deliver a stillborn child. The mother sustained damage to her rectum, uterus, and vagina, had repair surgery, and has been unable to get pregnant again.
Parents’ claim While in labor at the birthing center, the castor oil, blue cohosh, and black cohosh caused the patient’s uterus to contract excessively and contributed to fetal death. The patient should have been transferred to the hospital earlier. Cesarean delivery should have been performed immediately upon her arrival at the hospital but the ObGyn did not arrive at the hospital for an hour after the patient’s admission.
Defendants’ defense The head midwife at the birthing center conceded negligence. The hospital claimed that the fetus was already dead before the mother arrived. The ObGyn denied negligence, arguing that he had no supervisory role or ownership in the birthing center and was not present during the mother’s labor. He also claimed that the fetus was dead in utero 12 or more hours before delivery and that an infectious process had developed in the mother during the 17 hours that she was at the birthing center.
Verdict A $4,095,000 Florida verdict was returned against the ObGyn. A directed verdict was granted for the hospital.
Patient still in pain after labia reduction
A 44-year-old woman underwent surgical reduction of her labia minora performed by a gynecologist. The procedure was intended to relieve discomfort during sexual activity. The patient continues to have pain.
Patient’s claim An excessive amount of the right labia minora was removed because proper presurgical demarcation of the operative area was not performed. Her pain during intercourse has worsened and she cannot properly urinate.
Physician’s defense Presurgical demarcation was correctly completed using clamps. Surgery was properly performed. The asymmetry is due to poor healing of the surgical wound. The patient’s clitoris was not scarred. The patient never reported complications related to urination to her gynecologist. Her ongoing pain is due to an estrogen deficiency.
Verdict A New York defense verdict was returned.
Uterine rupture after version for breech presentation: $7M
A woman went to the hospital for delivery of her baby. The fetus was in breech position, but the mother requested vaginal delivery. When the ObGyn attempted an external cephalic version to turn the baby, the uterus ruptured and the placenta was damaged. The baby sustained hypoxic-ischemic encephalopathy resulting in cerebral palsy (CP). He requires constant nursing care.
Parents’ claim The ObGyn failed to recognize fetal distress during the breech version. The ObGyn improperly performed the version, causing the uterine rupture. There was lack of informed consent for the version.
Defendants’ defense The case was settled during trial.
Verdict A $7 million New Jersey settlement was reached.
Sepsis following hysterectomy
An ObGyn performed total abdominal hysterectomy to treat uterine fibroids in a 26-year-old woman. Despite reporting abdominal pain, the patient was discharged on postsurgical day 4.
Three days later, she went to a different hospital with moderate diffuse abdominal pain, constipation, nausea, emesis, tachycardia, and low-grade fever. An abdominal radiograph was taken, the patient was given morphine and ketorolac, and she was sent home.
She returned to the first hospital 3 days later reporting fever, nausea, emesis, diarrhea, and severe abdominal pain. After an abdominal computed tomography (CT) scan revealed numerous fluid- and gas-filled collections, indicative of abscess, intravenous antibiotics were ordered and administered.
Six days later, an infectious disease physician was consulted. He made a diagnosis of sepsis secondary to abdominal infection.
The next day, an abdominal CT scan revealed enlargement of multiple abdominal and pelvic fluid collections.
At exploratory laparotomy, purulent fluid was found in the anterior fascial compartment, with gross pus in the abdomen. The entire bowel was dilated, inflamed, and matted. Necrotic rind and infection were noted on multiple surfaces of the colon and small intestine and the transverse colon was gangrenous and sealed to the right lower quadrant. The patient’s intestines were resected and an ileostomy was placed, which was reversed several months later.
Patient’s claim The ObGyn did not offer an alternative to hysterectomy. The ObGyn was negligent in injuring the small intestine during surgery and failing to recognize and treat it intraoperatively. The patient should not have been discharged based on her reported symptoms. Failure to recognize and treat the injury led to sepsis with severe complications and months of recuperation.
Physician’s defense There was no negligence; small bowel injury is a known risk of hysterectomy. Other caregivers at both hospitals were at fault for not properly diagnosing and treating the infection.
Verdict A $901,420 Nevada verdict was returned; the ObGyn was found 85% at fault and other parties 15% at fault. The court granted the physician’s motion to reduce the verdict to $436,954, which included $371,411 from the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements, & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this article
- What caused the child’s Erb’s palsy?
- Woman claims lack of proper consent
- Bowel obstruction in pregnant woman
- Fourth-degree perineal tear and continuing pain after delivery
- Breast cancer missed in woman with dense breasts
- Child stillborn, mother injured after vacuum extraction
- Patient still in pain after labia reduction
- Uterine rupture after version for breech presentation: $7M
- Sepsis following hysterectomy
Earlier start to plasma transfusions for persistent postpartum hemorrhage does not improve maternal outcomes
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
AT 2015 ISTH
Key clinical point: Plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes.
Major finding: No significant differences were seen in maternal outcomes (ncluding arterial embolism, hysterectomy and maternal mortality) between the patients treated with plasma transfusions early (within 60 minutes) and late (after 60 minutes) (odds ratios, 1.1 and 0.8, respectively).
Data source: 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions I.
Disclosures: Dr. Henriquez declared no disclosures.