User login
Drugs, Pregnancy, and Lactation: Herbs
Herbs are commonly consumed by pregnant and breast-feeding women, possibly because they believe that “natural products” are safer than drugs. However, even though some have been available for hundreds or thousands of years, little is known about their effects on the embryo, fetus, newborn, or nursing infant. Moreover, as unregulated products, the concentration, contents, and presence of contaminants cannot be easily determined. Detailed reviews of the 22 most commonly used herbs discussed here can be found in “Drugs in Pregnancy and Lactation,” Briggs GG, Freeman RK, 10th ed., Philadelphia: Wolters Kluwer Health, 2014).
In the following discussions, dose, one of the two key factors that determine the risk of developmental toxicity (abnormal growth, structural anomalies, functional and/or neurobehavioral deficits, or death), is rarely reported. In addition, all herbs contain multiple chemical compounds, few of which have been studied during pregnancy or lactation. Thus, with few exceptions, a woman who takes an herb in pregnancy should be informed that the risk to her developing baby is unknown.
Six herbs are considered contraindicated in pregnancy: arnica, black seed /kalanji, blue cohosh, feverfew, salvia divinorum, and valerian.
• Arnica. The dried flowers, and sometimes the roots and rhizomes, are the parts of this perennial plant that are used topically for their anti-inflammatory and analgesic effects. There is no clinical evidence to support this use. Occasional topical use probably represents a low risk, but absorption may occur when it is applied to broken skin. The Food and Drug Administration has classified arnica as an unsafe herb and, when used orally, it is considered a poison. It is a uterine stimulant and an abortifacient. Nevertheless, in homeopathic formulations, it has been promoted for use before and during labor for internal and external bruising of the mother and newborn. In Italy, it is one of the top 10 herbs taken by women (Pharmacoepidemiol. Drug Saf. 2006;15:354-9).
• Black seed/kalanji. This herb has been used for thousands of year as a medicine, food, or spice. Because of this, it is unlikely that it causes teratogenesis. Nevertheless, its use to stimulate menstruation and its potential contraceptive properties suggest that it is contraindicated in pregnancy.
• Blue cohosh. Some of the components of this herb have been shown to be teratogenic and toxic in various animal species, so it should be avoided in the first trimester. The herb has uterine stimulant properties that are used by nurse-midwives to stimulate labor. Blue cohosh was the most frequently used herbal preparation for this purpose. However, some sources believe that the potential fetal and newborn toxicity may outweigh any medical benefit (“PDR for Herbal Medicine,” 2nd ed., Montvale, N.J.: Medical Economics, 2000:109-10; “The Review of Natural Products,” St. Louis, MO: Facts and Comparisons, 2000).
• Feverfew. This herb has been used for labor, menstrual disorders, potential miscarriage, and morning sickness; as an abortifacient; and for several other indications. Because of its antipyretic properties, it has been known as “medieval aspirin.” The doses used for these indications have not been quantified. Because of its emmenagogic (capable of provoking menstruation) activity, the herb should not be used in pregnancy.
• Salvia divinorum. This herb has hallucinogenic effects and is used in certain regions of Mexico for healing and divinatory rituals. It is also thought to have antidiarrheal properties. The herb is either smoked or chewed, or its juices are ingested. When taken orally, systemic effects are dependent upon absorption across the oral mucosa as the active ingredient is destroyed in the GI tract. Persistent psychosis has been observed in people who smoked the herb, so it is contraindicated in pregnancy.
• Valerian. A large number of preparations containing valerian are available. It has been used as a sedative and hypnotic for anxiety, restlessness, and sleep disturbances, as well as several other pharmacologic claims. Because of the risk of cytotoxicity in the fetus and hepatotoxicity in the mother, the herb should be avoided during gestation.
For the remaining 16 herbs, small, infrequent doses probably cause no harm to the mother, embryo, fetus, or newborn. Nevertheless, as noted below, some of these herbs are best avoided during pregnancy.
• Chamomile. Excessive use of this herb should be avoided because it is thought to have uterine stimulant, emmenagogic, and abortifacient properties. Although controversial, some nurse-midwives prescribe chamomile teas for the treatment of morning sickness. Because the plant sources of the herb contain coumarin compounds, ingesting chamomile by pregnant women with coagulation disorders is a concern. However, the herb has been used for thousands of years, so the risk of harm, at least from occasional use, must be very rare.
• Echinacea. This herb is used topically to enhance wound healing and systemically as an immunostimulant. An IV formulation is used in Germany but is not available in the United States. It also has been recommended to assist in the prevention or treatment of viral upper respiratory tract infections. Its use in pregnancy is limited to one small study.
• Evening primrose oil. The oil contains two essential fatty acids: cis-linoleic and gamma-linolenic acid. In a national survey of nurse-midwives, it was the most frequently used herbal preparation for the induction of labor. No adverse effects have been reported in the fetus or newborn from this use. The doses used varied widely and included both oral and vaginal routes of administration. In addition, the oil has been used for rheumatoid arthritis and diabetic neuropathy, but there are no reports of these uses in pregnancy.
• Garlic. Garlic has been used for food flavoring since ancient times and appears to be safe during pregnancy. Some components cross the placenta, as shown by garlic odor in the amniotic fluid and on the newborn’s breath. Very high doses have the potential to induce menstruation or uterine contractions, but apparently these effects have not been reported.
• Ginger. No reports of ginger-induced developmental toxicity have been located. Ginger has been used as antiemetic for nausea and vomiting of pregnancy.
• Ginseng. The root is the most important part of this plant that is found throughout the world and has been used in medicine for more than 2,000 years. The herb has been promoted for multiple pharmacologic effects, including adaptogenic, CNS, cardiovascular, endocrine, ergogenic, antineoplastic, and immunomodulatory effects.
Hypertension and hypoglycemia have been reported in nonpregnant patients, but not in the limited human pregnancy data. A brief 1991 study compared 88 women who took the herb during pregnancy with 88 controls. No differences between the groups were found with regard to the mode of delivery, birth weight, low birth weight (< 2,500 ), preterm delivery (< 37 weeks), low Apgar score (< 7), stillbirths, neonatal deaths, or maternal complications (Asia Oceania J. Obstet. Gynaecol. 1991;17:379-80).
• Ginkgo biloba. The limited animal reproduction data suggest low risk, but there is no reported human pregnancy experience. Nevertheless, it is an ancient herbal preparation that is commonly used for organic brain syndrome, circulatory disorders, asthma, vertigo, and tinnitus. Because of its widespread use, it is doubtful that a major teratogenic effect would have escaped notice, but more subtle or low-incidence toxic effects may not have been detected.
• Kudzu. No human or animal data regarding pregnancy have been located. The herb has been used for more than 2,500 years for the treatment of alcohol hangover, drunkenness, alcoholism, muscle pain, and measles. Many of its chemical constituents can be found in foods. Nevertheless, high, frequent doses should be avoided.
• Nutmeg. This is a commonly used spice but, as with any herb, high doses can produce toxicity. The toxicity is caused by a chemical in the seeds, myristicin, which has anticholinergic properties. A woman at 30 weeks’ gestation misread a recipe and used a whole grated nutmeg rather than 1/8 teaspoon when making cookies. When she ate a cookie, she experienced sinus tachycardia, hypertension, and a sensation of impending doom. The fetus had tachycardia, and atropine-like poisoning was diagnosed. After about 12 hours, both mother and fetus made an uneventful recovery and a healthy infant was born at term.
• Passion flower. The name of this herb may refer to about 400 species of the genus Passiflora. It is available in both oral and topical forms and is used for nervousness, neuralgia, insomnia, pain, asthma, seizures, burns, hemorrhoids, and menopausal complaints. As with many herbs, it contains a large number of chemicals, none of which have undergone reproductive testing. No reports describing the use of this herb in human pregnancy have been located. However, because it has uterine stimulant properties, the oral formulation is best avoided in pregnancy.
• Peppermint. This popular flavoring appears to be harmless for the mother and developing baby when low, recommended doses are ingested. Peppermint oil is available in numerous topical and oral formulations. High oral doses, however, can cause significant toxicity, including death. During pregnancy, ingestion of more than the recommended doses is unsafe because of possible emmenagogic and abortifacient properties.
• Pumpkin seed. This herb, when used as a food, appears to be harmless for the mother and embryo-fetus, but no reports describing its use in pregnancy have been located. High doses, such as those used in traditional medicine or in eating disorders, should be avoided because of the potential for toxic effects from the many chemicals these seeds contain.
• Raspberry leaf. Raspberry leaf tea is commonly used by pregnant women. Nurse-midwives often prescribe the tea to treat nausea and vomiting and as a uterine tonic to shorten labor. A double-blind, randomized, placebo-controlled study evaluated the effect of raspberry leaf tablets (2 tablets/day) on pregnancy outcomes. Compared with controls, no differences were found for length of labor or stages of labor, mode of delivery, admission to the neonatal intensive care unit, Apgar score, and birth weight (J. Midwifery Womens Health 2001;46:51-9).
• Safflower. Safflower oil is commonly used in cooking and has been given for its laxative action. There are no reports describing the use of the herb in pregnancy. It is doubtful if such use would have any adverse effect on a pregnancy. Although abortifacient and emmenagogic effects have been suggested, there is no evidence supporting these effects when used as a food.
• St. John’s wort. No toxicity in pregnant humans has been reported. The use of the herb is widespread and dates back thousands of years. Thus, it is doubtful that the herb is a major teratogen or causes other elements of developmental toxicity. The herb has been used for the management of anxiety, depression, insomnia, inflammation, and gastritis. It is also used as a diuretic and, topically, for the treatment of hemorrhoids and enhanced wound healing.
• Yohimbine. The use of this herb in human pregnancies has not been reported. It has been used as an aphrodisiac and for weight loss, sexual dysfunction, and the treatment of orthostatic hypotension. Although it has no Food and Drug Administration–sanctioned indications, it is also available by prescription for male erectile dysfunction. Due to the lack of data regarding pregnancy, the herb is best avoided during pregnancy.
There are few data regarding the effects of the above herbs on a breast-feeding infant. Depending upon the herb, nursing infants will be exposed to many chemical compounds. For those herbs used as food, nursing is probably safe. The safety of the other herbs during lactation is unknown. However, toxicity has been reported in a 9-day-old term infant whose mother was taking arnica (Clin. Toxicol. 2009;47:726, abstract 120). The infant presented with lethargy, decreased milk intake, anemia, and jaundice but recovered with treatment. After the mother stopped the herb and resumed nursing, no further problems were noted in the infant.
Mr. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; clinical professor of pharmacy at the University of California, San Francisco; and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He had no relevant financial disclosures. Contact him at [email protected].
Herbs are commonly consumed by pregnant and breast-feeding women, possibly because they believe that “natural products” are safer than drugs. However, even though some have been available for hundreds or thousands of years, little is known about their effects on the embryo, fetus, newborn, or nursing infant. Moreover, as unregulated products, the concentration, contents, and presence of contaminants cannot be easily determined. Detailed reviews of the 22 most commonly used herbs discussed here can be found in “Drugs in Pregnancy and Lactation,” Briggs GG, Freeman RK, 10th ed., Philadelphia: Wolters Kluwer Health, 2014).
In the following discussions, dose, one of the two key factors that determine the risk of developmental toxicity (abnormal growth, structural anomalies, functional and/or neurobehavioral deficits, or death), is rarely reported. In addition, all herbs contain multiple chemical compounds, few of which have been studied during pregnancy or lactation. Thus, with few exceptions, a woman who takes an herb in pregnancy should be informed that the risk to her developing baby is unknown.
Six herbs are considered contraindicated in pregnancy: arnica, black seed /kalanji, blue cohosh, feverfew, salvia divinorum, and valerian.
• Arnica. The dried flowers, and sometimes the roots and rhizomes, are the parts of this perennial plant that are used topically for their anti-inflammatory and analgesic effects. There is no clinical evidence to support this use. Occasional topical use probably represents a low risk, but absorption may occur when it is applied to broken skin. The Food and Drug Administration has classified arnica as an unsafe herb and, when used orally, it is considered a poison. It is a uterine stimulant and an abortifacient. Nevertheless, in homeopathic formulations, it has been promoted for use before and during labor for internal and external bruising of the mother and newborn. In Italy, it is one of the top 10 herbs taken by women (Pharmacoepidemiol. Drug Saf. 2006;15:354-9).
• Black seed/kalanji. This herb has been used for thousands of year as a medicine, food, or spice. Because of this, it is unlikely that it causes teratogenesis. Nevertheless, its use to stimulate menstruation and its potential contraceptive properties suggest that it is contraindicated in pregnancy.
• Blue cohosh. Some of the components of this herb have been shown to be teratogenic and toxic in various animal species, so it should be avoided in the first trimester. The herb has uterine stimulant properties that are used by nurse-midwives to stimulate labor. Blue cohosh was the most frequently used herbal preparation for this purpose. However, some sources believe that the potential fetal and newborn toxicity may outweigh any medical benefit (“PDR for Herbal Medicine,” 2nd ed., Montvale, N.J.: Medical Economics, 2000:109-10; “The Review of Natural Products,” St. Louis, MO: Facts and Comparisons, 2000).
• Feverfew. This herb has been used for labor, menstrual disorders, potential miscarriage, and morning sickness; as an abortifacient; and for several other indications. Because of its antipyretic properties, it has been known as “medieval aspirin.” The doses used for these indications have not been quantified. Because of its emmenagogic (capable of provoking menstruation) activity, the herb should not be used in pregnancy.
• Salvia divinorum. This herb has hallucinogenic effects and is used in certain regions of Mexico for healing and divinatory rituals. It is also thought to have antidiarrheal properties. The herb is either smoked or chewed, or its juices are ingested. When taken orally, systemic effects are dependent upon absorption across the oral mucosa as the active ingredient is destroyed in the GI tract. Persistent psychosis has been observed in people who smoked the herb, so it is contraindicated in pregnancy.
• Valerian. A large number of preparations containing valerian are available. It has been used as a sedative and hypnotic for anxiety, restlessness, and sleep disturbances, as well as several other pharmacologic claims. Because of the risk of cytotoxicity in the fetus and hepatotoxicity in the mother, the herb should be avoided during gestation.
For the remaining 16 herbs, small, infrequent doses probably cause no harm to the mother, embryo, fetus, or newborn. Nevertheless, as noted below, some of these herbs are best avoided during pregnancy.
• Chamomile. Excessive use of this herb should be avoided because it is thought to have uterine stimulant, emmenagogic, and abortifacient properties. Although controversial, some nurse-midwives prescribe chamomile teas for the treatment of morning sickness. Because the plant sources of the herb contain coumarin compounds, ingesting chamomile by pregnant women with coagulation disorders is a concern. However, the herb has been used for thousands of years, so the risk of harm, at least from occasional use, must be very rare.
• Echinacea. This herb is used topically to enhance wound healing and systemically as an immunostimulant. An IV formulation is used in Germany but is not available in the United States. It also has been recommended to assist in the prevention or treatment of viral upper respiratory tract infections. Its use in pregnancy is limited to one small study.
• Evening primrose oil. The oil contains two essential fatty acids: cis-linoleic and gamma-linolenic acid. In a national survey of nurse-midwives, it was the most frequently used herbal preparation for the induction of labor. No adverse effects have been reported in the fetus or newborn from this use. The doses used varied widely and included both oral and vaginal routes of administration. In addition, the oil has been used for rheumatoid arthritis and diabetic neuropathy, but there are no reports of these uses in pregnancy.
• Garlic. Garlic has been used for food flavoring since ancient times and appears to be safe during pregnancy. Some components cross the placenta, as shown by garlic odor in the amniotic fluid and on the newborn’s breath. Very high doses have the potential to induce menstruation or uterine contractions, but apparently these effects have not been reported.
• Ginger. No reports of ginger-induced developmental toxicity have been located. Ginger has been used as antiemetic for nausea and vomiting of pregnancy.
• Ginseng. The root is the most important part of this plant that is found throughout the world and has been used in medicine for more than 2,000 years. The herb has been promoted for multiple pharmacologic effects, including adaptogenic, CNS, cardiovascular, endocrine, ergogenic, antineoplastic, and immunomodulatory effects.
Hypertension and hypoglycemia have been reported in nonpregnant patients, but not in the limited human pregnancy data. A brief 1991 study compared 88 women who took the herb during pregnancy with 88 controls. No differences between the groups were found with regard to the mode of delivery, birth weight, low birth weight (< 2,500 ), preterm delivery (< 37 weeks), low Apgar score (< 7), stillbirths, neonatal deaths, or maternal complications (Asia Oceania J. Obstet. Gynaecol. 1991;17:379-80).
• Ginkgo biloba. The limited animal reproduction data suggest low risk, but there is no reported human pregnancy experience. Nevertheless, it is an ancient herbal preparation that is commonly used for organic brain syndrome, circulatory disorders, asthma, vertigo, and tinnitus. Because of its widespread use, it is doubtful that a major teratogenic effect would have escaped notice, but more subtle or low-incidence toxic effects may not have been detected.
• Kudzu. No human or animal data regarding pregnancy have been located. The herb has been used for more than 2,500 years for the treatment of alcohol hangover, drunkenness, alcoholism, muscle pain, and measles. Many of its chemical constituents can be found in foods. Nevertheless, high, frequent doses should be avoided.
• Nutmeg. This is a commonly used spice but, as with any herb, high doses can produce toxicity. The toxicity is caused by a chemical in the seeds, myristicin, which has anticholinergic properties. A woman at 30 weeks’ gestation misread a recipe and used a whole grated nutmeg rather than 1/8 teaspoon when making cookies. When she ate a cookie, she experienced sinus tachycardia, hypertension, and a sensation of impending doom. The fetus had tachycardia, and atropine-like poisoning was diagnosed. After about 12 hours, both mother and fetus made an uneventful recovery and a healthy infant was born at term.
• Passion flower. The name of this herb may refer to about 400 species of the genus Passiflora. It is available in both oral and topical forms and is used for nervousness, neuralgia, insomnia, pain, asthma, seizures, burns, hemorrhoids, and menopausal complaints. As with many herbs, it contains a large number of chemicals, none of which have undergone reproductive testing. No reports describing the use of this herb in human pregnancy have been located. However, because it has uterine stimulant properties, the oral formulation is best avoided in pregnancy.
• Peppermint. This popular flavoring appears to be harmless for the mother and developing baby when low, recommended doses are ingested. Peppermint oil is available in numerous topical and oral formulations. High oral doses, however, can cause significant toxicity, including death. During pregnancy, ingestion of more than the recommended doses is unsafe because of possible emmenagogic and abortifacient properties.
• Pumpkin seed. This herb, when used as a food, appears to be harmless for the mother and embryo-fetus, but no reports describing its use in pregnancy have been located. High doses, such as those used in traditional medicine or in eating disorders, should be avoided because of the potential for toxic effects from the many chemicals these seeds contain.
• Raspberry leaf. Raspberry leaf tea is commonly used by pregnant women. Nurse-midwives often prescribe the tea to treat nausea and vomiting and as a uterine tonic to shorten labor. A double-blind, randomized, placebo-controlled study evaluated the effect of raspberry leaf tablets (2 tablets/day) on pregnancy outcomes. Compared with controls, no differences were found for length of labor or stages of labor, mode of delivery, admission to the neonatal intensive care unit, Apgar score, and birth weight (J. Midwifery Womens Health 2001;46:51-9).
• Safflower. Safflower oil is commonly used in cooking and has been given for its laxative action. There are no reports describing the use of the herb in pregnancy. It is doubtful if such use would have any adverse effect on a pregnancy. Although abortifacient and emmenagogic effects have been suggested, there is no evidence supporting these effects when used as a food.
• St. John’s wort. No toxicity in pregnant humans has been reported. The use of the herb is widespread and dates back thousands of years. Thus, it is doubtful that the herb is a major teratogen or causes other elements of developmental toxicity. The herb has been used for the management of anxiety, depression, insomnia, inflammation, and gastritis. It is also used as a diuretic and, topically, for the treatment of hemorrhoids and enhanced wound healing.
• Yohimbine. The use of this herb in human pregnancies has not been reported. It has been used as an aphrodisiac and for weight loss, sexual dysfunction, and the treatment of orthostatic hypotension. Although it has no Food and Drug Administration–sanctioned indications, it is also available by prescription for male erectile dysfunction. Due to the lack of data regarding pregnancy, the herb is best avoided during pregnancy.
There are few data regarding the effects of the above herbs on a breast-feeding infant. Depending upon the herb, nursing infants will be exposed to many chemical compounds. For those herbs used as food, nursing is probably safe. The safety of the other herbs during lactation is unknown. However, toxicity has been reported in a 9-day-old term infant whose mother was taking arnica (Clin. Toxicol. 2009;47:726, abstract 120). The infant presented with lethargy, decreased milk intake, anemia, and jaundice but recovered with treatment. After the mother stopped the herb and resumed nursing, no further problems were noted in the infant.
Mr. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; clinical professor of pharmacy at the University of California, San Francisco; and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He had no relevant financial disclosures. Contact him at [email protected].
Herbs are commonly consumed by pregnant and breast-feeding women, possibly because they believe that “natural products” are safer than drugs. However, even though some have been available for hundreds or thousands of years, little is known about their effects on the embryo, fetus, newborn, or nursing infant. Moreover, as unregulated products, the concentration, contents, and presence of contaminants cannot be easily determined. Detailed reviews of the 22 most commonly used herbs discussed here can be found in “Drugs in Pregnancy and Lactation,” Briggs GG, Freeman RK, 10th ed., Philadelphia: Wolters Kluwer Health, 2014).
In the following discussions, dose, one of the two key factors that determine the risk of developmental toxicity (abnormal growth, structural anomalies, functional and/or neurobehavioral deficits, or death), is rarely reported. In addition, all herbs contain multiple chemical compounds, few of which have been studied during pregnancy or lactation. Thus, with few exceptions, a woman who takes an herb in pregnancy should be informed that the risk to her developing baby is unknown.
Six herbs are considered contraindicated in pregnancy: arnica, black seed /kalanji, blue cohosh, feverfew, salvia divinorum, and valerian.
• Arnica. The dried flowers, and sometimes the roots and rhizomes, are the parts of this perennial plant that are used topically for their anti-inflammatory and analgesic effects. There is no clinical evidence to support this use. Occasional topical use probably represents a low risk, but absorption may occur when it is applied to broken skin. The Food and Drug Administration has classified arnica as an unsafe herb and, when used orally, it is considered a poison. It is a uterine stimulant and an abortifacient. Nevertheless, in homeopathic formulations, it has been promoted for use before and during labor for internal and external bruising of the mother and newborn. In Italy, it is one of the top 10 herbs taken by women (Pharmacoepidemiol. Drug Saf. 2006;15:354-9).
• Black seed/kalanji. This herb has been used for thousands of year as a medicine, food, or spice. Because of this, it is unlikely that it causes teratogenesis. Nevertheless, its use to stimulate menstruation and its potential contraceptive properties suggest that it is contraindicated in pregnancy.
• Blue cohosh. Some of the components of this herb have been shown to be teratogenic and toxic in various animal species, so it should be avoided in the first trimester. The herb has uterine stimulant properties that are used by nurse-midwives to stimulate labor. Blue cohosh was the most frequently used herbal preparation for this purpose. However, some sources believe that the potential fetal and newborn toxicity may outweigh any medical benefit (“PDR for Herbal Medicine,” 2nd ed., Montvale, N.J.: Medical Economics, 2000:109-10; “The Review of Natural Products,” St. Louis, MO: Facts and Comparisons, 2000).
• Feverfew. This herb has been used for labor, menstrual disorders, potential miscarriage, and morning sickness; as an abortifacient; and for several other indications. Because of its antipyretic properties, it has been known as “medieval aspirin.” The doses used for these indications have not been quantified. Because of its emmenagogic (capable of provoking menstruation) activity, the herb should not be used in pregnancy.
• Salvia divinorum. This herb has hallucinogenic effects and is used in certain regions of Mexico for healing and divinatory rituals. It is also thought to have antidiarrheal properties. The herb is either smoked or chewed, or its juices are ingested. When taken orally, systemic effects are dependent upon absorption across the oral mucosa as the active ingredient is destroyed in the GI tract. Persistent psychosis has been observed in people who smoked the herb, so it is contraindicated in pregnancy.
• Valerian. A large number of preparations containing valerian are available. It has been used as a sedative and hypnotic for anxiety, restlessness, and sleep disturbances, as well as several other pharmacologic claims. Because of the risk of cytotoxicity in the fetus and hepatotoxicity in the mother, the herb should be avoided during gestation.
For the remaining 16 herbs, small, infrequent doses probably cause no harm to the mother, embryo, fetus, or newborn. Nevertheless, as noted below, some of these herbs are best avoided during pregnancy.
• Chamomile. Excessive use of this herb should be avoided because it is thought to have uterine stimulant, emmenagogic, and abortifacient properties. Although controversial, some nurse-midwives prescribe chamomile teas for the treatment of morning sickness. Because the plant sources of the herb contain coumarin compounds, ingesting chamomile by pregnant women with coagulation disorders is a concern. However, the herb has been used for thousands of years, so the risk of harm, at least from occasional use, must be very rare.
• Echinacea. This herb is used topically to enhance wound healing and systemically as an immunostimulant. An IV formulation is used in Germany but is not available in the United States. It also has been recommended to assist in the prevention or treatment of viral upper respiratory tract infections. Its use in pregnancy is limited to one small study.
• Evening primrose oil. The oil contains two essential fatty acids: cis-linoleic and gamma-linolenic acid. In a national survey of nurse-midwives, it was the most frequently used herbal preparation for the induction of labor. No adverse effects have been reported in the fetus or newborn from this use. The doses used varied widely and included both oral and vaginal routes of administration. In addition, the oil has been used for rheumatoid arthritis and diabetic neuropathy, but there are no reports of these uses in pregnancy.
• Garlic. Garlic has been used for food flavoring since ancient times and appears to be safe during pregnancy. Some components cross the placenta, as shown by garlic odor in the amniotic fluid and on the newborn’s breath. Very high doses have the potential to induce menstruation or uterine contractions, but apparently these effects have not been reported.
• Ginger. No reports of ginger-induced developmental toxicity have been located. Ginger has been used as antiemetic for nausea and vomiting of pregnancy.
• Ginseng. The root is the most important part of this plant that is found throughout the world and has been used in medicine for more than 2,000 years. The herb has been promoted for multiple pharmacologic effects, including adaptogenic, CNS, cardiovascular, endocrine, ergogenic, antineoplastic, and immunomodulatory effects.
Hypertension and hypoglycemia have been reported in nonpregnant patients, but not in the limited human pregnancy data. A brief 1991 study compared 88 women who took the herb during pregnancy with 88 controls. No differences between the groups were found with regard to the mode of delivery, birth weight, low birth weight (< 2,500 ), preterm delivery (< 37 weeks), low Apgar score (< 7), stillbirths, neonatal deaths, or maternal complications (Asia Oceania J. Obstet. Gynaecol. 1991;17:379-80).
• Ginkgo biloba. The limited animal reproduction data suggest low risk, but there is no reported human pregnancy experience. Nevertheless, it is an ancient herbal preparation that is commonly used for organic brain syndrome, circulatory disorders, asthma, vertigo, and tinnitus. Because of its widespread use, it is doubtful that a major teratogenic effect would have escaped notice, but more subtle or low-incidence toxic effects may not have been detected.
• Kudzu. No human or animal data regarding pregnancy have been located. The herb has been used for more than 2,500 years for the treatment of alcohol hangover, drunkenness, alcoholism, muscle pain, and measles. Many of its chemical constituents can be found in foods. Nevertheless, high, frequent doses should be avoided.
• Nutmeg. This is a commonly used spice but, as with any herb, high doses can produce toxicity. The toxicity is caused by a chemical in the seeds, myristicin, which has anticholinergic properties. A woman at 30 weeks’ gestation misread a recipe and used a whole grated nutmeg rather than 1/8 teaspoon when making cookies. When she ate a cookie, she experienced sinus tachycardia, hypertension, and a sensation of impending doom. The fetus had tachycardia, and atropine-like poisoning was diagnosed. After about 12 hours, both mother and fetus made an uneventful recovery and a healthy infant was born at term.
• Passion flower. The name of this herb may refer to about 400 species of the genus Passiflora. It is available in both oral and topical forms and is used for nervousness, neuralgia, insomnia, pain, asthma, seizures, burns, hemorrhoids, and menopausal complaints. As with many herbs, it contains a large number of chemicals, none of which have undergone reproductive testing. No reports describing the use of this herb in human pregnancy have been located. However, because it has uterine stimulant properties, the oral formulation is best avoided in pregnancy.
• Peppermint. This popular flavoring appears to be harmless for the mother and developing baby when low, recommended doses are ingested. Peppermint oil is available in numerous topical and oral formulations. High oral doses, however, can cause significant toxicity, including death. During pregnancy, ingestion of more than the recommended doses is unsafe because of possible emmenagogic and abortifacient properties.
• Pumpkin seed. This herb, when used as a food, appears to be harmless for the mother and embryo-fetus, but no reports describing its use in pregnancy have been located. High doses, such as those used in traditional medicine or in eating disorders, should be avoided because of the potential for toxic effects from the many chemicals these seeds contain.
• Raspberry leaf. Raspberry leaf tea is commonly used by pregnant women. Nurse-midwives often prescribe the tea to treat nausea and vomiting and as a uterine tonic to shorten labor. A double-blind, randomized, placebo-controlled study evaluated the effect of raspberry leaf tablets (2 tablets/day) on pregnancy outcomes. Compared with controls, no differences were found for length of labor or stages of labor, mode of delivery, admission to the neonatal intensive care unit, Apgar score, and birth weight (J. Midwifery Womens Health 2001;46:51-9).
• Safflower. Safflower oil is commonly used in cooking and has been given for its laxative action. There are no reports describing the use of the herb in pregnancy. It is doubtful if such use would have any adverse effect on a pregnancy. Although abortifacient and emmenagogic effects have been suggested, there is no evidence supporting these effects when used as a food.
• St. John’s wort. No toxicity in pregnant humans has been reported. The use of the herb is widespread and dates back thousands of years. Thus, it is doubtful that the herb is a major teratogen or causes other elements of developmental toxicity. The herb has been used for the management of anxiety, depression, insomnia, inflammation, and gastritis. It is also used as a diuretic and, topically, for the treatment of hemorrhoids and enhanced wound healing.
• Yohimbine. The use of this herb in human pregnancies has not been reported. It has been used as an aphrodisiac and for weight loss, sexual dysfunction, and the treatment of orthostatic hypotension. Although it has no Food and Drug Administration–sanctioned indications, it is also available by prescription for male erectile dysfunction. Due to the lack of data regarding pregnancy, the herb is best avoided during pregnancy.
There are few data regarding the effects of the above herbs on a breast-feeding infant. Depending upon the herb, nursing infants will be exposed to many chemical compounds. For those herbs used as food, nursing is probably safe. The safety of the other herbs during lactation is unknown. However, toxicity has been reported in a 9-day-old term infant whose mother was taking arnica (Clin. Toxicol. 2009;47:726, abstract 120). The infant presented with lethargy, decreased milk intake, anemia, and jaundice but recovered with treatment. After the mother stopped the herb and resumed nursing, no further problems were noted in the infant.
Mr. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; clinical professor of pharmacy at the University of California, San Francisco; and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He had no relevant financial disclosures. Contact him at [email protected].
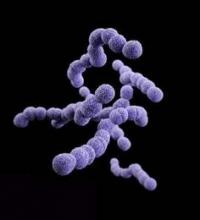
Questions raised over intrapartum antibiotics to prevent neonatal streptococcus B
The introduction of antibiotic prophylaxis in the Netherlands to prevent invasive neonatal group B streptococcus infection has failed to achieve a decrease in the incidence of infection, prompting calls for guidelines to be reassessed and alternative prevention methods considered.
Analysis of nationwide surveillance data from 1987 to 2011 showed that the incidence of invasive group B streptococcus in infants aged 3 months and under actually increased from 0.20 per 1,000 live births to 0.32 per 1,000 (P < .0001), while the incidence of early-onset disease increased from 0.11 per 1,000 live births to 0.19 per 1,000 (P < .0001).
Researchers also noted an increase in cases of disease caused by clonal complex 17 – which has been associated with invasive disease in neonates – and fewer cases caused by clonal complex 19, as well as a nonsignificant increase in the incidence of invasive Escherichia coli infection after the 1999 implementation of intravenous antibiotic prophylaxis during labor.
“Our findings offer no explanation for the increase in incidence over the past 25 years in Netherlands, [however] possible explanations include changes in the host, medical practice, increased submission of isolates to the National Laboratory, or the pathogen itself,” wrote Dr. Vincent Bekker, from the Emma Children’s Hospital, Academic Medical Center, Amsterdam, and colleagues (Lancet Infect. Dis. 2014 Oct. 19).
In an accompanying editorial, Dr. Shannon D. Manning of Michigan State University, East Lansing, pointed out that the results ran counter to those of other studies, such as one from the United States which showed that intrapartum antibiotic prophylaxis was associated with a 65% reduction in early-onset disease.
“The findings of Bekker and colleagues confirm that group B streptococcus disease in babies remains a global public health concern and show the importance of continuous surveillance in different geographic locations,” Dr. Manning noted.
The study was supported by the National Institute of Public Health and the Environment. There were no other conflicts of interest declared.
The introduction of antibiotic prophylaxis in the Netherlands to prevent invasive neonatal group B streptococcus infection has failed to achieve a decrease in the incidence of infection, prompting calls for guidelines to be reassessed and alternative prevention methods considered.
Analysis of nationwide surveillance data from 1987 to 2011 showed that the incidence of invasive group B streptococcus in infants aged 3 months and under actually increased from 0.20 per 1,000 live births to 0.32 per 1,000 (P < .0001), while the incidence of early-onset disease increased from 0.11 per 1,000 live births to 0.19 per 1,000 (P < .0001).
Researchers also noted an increase in cases of disease caused by clonal complex 17 – which has been associated with invasive disease in neonates – and fewer cases caused by clonal complex 19, as well as a nonsignificant increase in the incidence of invasive Escherichia coli infection after the 1999 implementation of intravenous antibiotic prophylaxis during labor.
“Our findings offer no explanation for the increase in incidence over the past 25 years in Netherlands, [however] possible explanations include changes in the host, medical practice, increased submission of isolates to the National Laboratory, or the pathogen itself,” wrote Dr. Vincent Bekker, from the Emma Children’s Hospital, Academic Medical Center, Amsterdam, and colleagues (Lancet Infect. Dis. 2014 Oct. 19).
In an accompanying editorial, Dr. Shannon D. Manning of Michigan State University, East Lansing, pointed out that the results ran counter to those of other studies, such as one from the United States which showed that intrapartum antibiotic prophylaxis was associated with a 65% reduction in early-onset disease.
“The findings of Bekker and colleagues confirm that group B streptococcus disease in babies remains a global public health concern and show the importance of continuous surveillance in different geographic locations,” Dr. Manning noted.
The study was supported by the National Institute of Public Health and the Environment. There were no other conflicts of interest declared.
The introduction of antibiotic prophylaxis in the Netherlands to prevent invasive neonatal group B streptococcus infection has failed to achieve a decrease in the incidence of infection, prompting calls for guidelines to be reassessed and alternative prevention methods considered.
Analysis of nationwide surveillance data from 1987 to 2011 showed that the incidence of invasive group B streptococcus in infants aged 3 months and under actually increased from 0.20 per 1,000 live births to 0.32 per 1,000 (P < .0001), while the incidence of early-onset disease increased from 0.11 per 1,000 live births to 0.19 per 1,000 (P < .0001).
Researchers also noted an increase in cases of disease caused by clonal complex 17 – which has been associated with invasive disease in neonates – and fewer cases caused by clonal complex 19, as well as a nonsignificant increase in the incidence of invasive Escherichia coli infection after the 1999 implementation of intravenous antibiotic prophylaxis during labor.
“Our findings offer no explanation for the increase in incidence over the past 25 years in Netherlands, [however] possible explanations include changes in the host, medical practice, increased submission of isolates to the National Laboratory, or the pathogen itself,” wrote Dr. Vincent Bekker, from the Emma Children’s Hospital, Academic Medical Center, Amsterdam, and colleagues (Lancet Infect. Dis. 2014 Oct. 19).
In an accompanying editorial, Dr. Shannon D. Manning of Michigan State University, East Lansing, pointed out that the results ran counter to those of other studies, such as one from the United States which showed that intrapartum antibiotic prophylaxis was associated with a 65% reduction in early-onset disease.
“The findings of Bekker and colleagues confirm that group B streptococcus disease in babies remains a global public health concern and show the importance of continuous surveillance in different geographic locations,” Dr. Manning noted.
The study was supported by the National Institute of Public Health and the Environment. There were no other conflicts of interest declared.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Dutch data show an increase in the incidence of invasive neonatal group B streptococcus infection despite intrapartum antibiotic prophylaxis.
Major finding: The incidence of invasive neonatal group B streptococcus infection has increased in the Netherlands since the introduction of intrapartum antibiotic prophylaxis.
Data source: Analysis of population-wide surveillance data.
Disclosures: The study was supported by the National Institute of Public Health and the Environment. There were no other conflicts of interest declared.
Obstetrics measures fail to capture quality of care
Hospital quality measures aimed at decreasing elective early deliveries and cesarean deliveries in low-risk women were not linked with declines in serious maternal or neonatal complications, according to a study published Oct. 15 in JAMA.
Data on more than 100,000 babies born at term in 2010 in New York City hospitals showed that there was wide variation in both maternal and neonatal complications between hospitals, but there was no association between the morbidity rates and the quality metrics studied (JAMA. 2014; 312:1531-41).
Dr. Elizabeth A. Howell of the Icahn School of Medicine at Mount Sinai in New York, and her colleagues, looked at two Joint Commission perinatal quality measures: elective deliveries performed prior to 39 weeks of gestation and cesarean deliveries performed in low-risk nulliparous women.
The rates for elective deliveries before 39 weeks ranged from 15.5 to 41.9 per 100 deliveries among the 41 hospitals studied. For cesarean deliveries in low-risk women, the rates range from 11.7 to 39.3 per 100 deliveries.
There was also a wide range in maternal and neonatal morbidity. Maternal morbidity rates ranged from 0.9 to 5.7 mothers with complications per 100 deliveries, while neonatal morbidity ranged from 3.1 to 21.3 infants with complications per 100 births. Neither of the Joint Commission quality measures was associated with severe complications.
Dr. Howell and her colleagues concluded that while overutilization measures may be important, they aren’t comprehensive enough to reflect the actual quality of care.
These perinatal measures are not the only hospital-level quality measures not linked to decreases in the outcomes they are designed to influence, the investigators noted. They cited examples where quality measures for heart failure, pneumonia, acute MI, and infection control were not associated with improved outcomes or predicted only small improvements.
Quality measures often “capture only a narrow slice of hospital quality,” Dr. Howell wrote. “There is a need to reassess how these measures are designed and implemented and to think more broadly about constructing meaningful quality measures tightly linked with patient outcomes.”
The researchers called for the development of other quality measures such as metrics aimed at identifying whether hemorrhage and preeclampsia protocols are being used in the delivery suite.
The study was funded by a grant from the National Institute of Child Health and Human Development and a fellowship grant from the European Commission. The researchers reported having no financial disclosures.
On Twitter @maryellenny
Hospital quality measures aimed at decreasing elective early deliveries and cesarean deliveries in low-risk women were not linked with declines in serious maternal or neonatal complications, according to a study published Oct. 15 in JAMA.
Data on more than 100,000 babies born at term in 2010 in New York City hospitals showed that there was wide variation in both maternal and neonatal complications between hospitals, but there was no association between the morbidity rates and the quality metrics studied (JAMA. 2014; 312:1531-41).
Dr. Elizabeth A. Howell of the Icahn School of Medicine at Mount Sinai in New York, and her colleagues, looked at two Joint Commission perinatal quality measures: elective deliveries performed prior to 39 weeks of gestation and cesarean deliveries performed in low-risk nulliparous women.
The rates for elective deliveries before 39 weeks ranged from 15.5 to 41.9 per 100 deliveries among the 41 hospitals studied. For cesarean deliveries in low-risk women, the rates range from 11.7 to 39.3 per 100 deliveries.
There was also a wide range in maternal and neonatal morbidity. Maternal morbidity rates ranged from 0.9 to 5.7 mothers with complications per 100 deliveries, while neonatal morbidity ranged from 3.1 to 21.3 infants with complications per 100 births. Neither of the Joint Commission quality measures was associated with severe complications.
Dr. Howell and her colleagues concluded that while overutilization measures may be important, they aren’t comprehensive enough to reflect the actual quality of care.
These perinatal measures are not the only hospital-level quality measures not linked to decreases in the outcomes they are designed to influence, the investigators noted. They cited examples where quality measures for heart failure, pneumonia, acute MI, and infection control were not associated with improved outcomes or predicted only small improvements.
Quality measures often “capture only a narrow slice of hospital quality,” Dr. Howell wrote. “There is a need to reassess how these measures are designed and implemented and to think more broadly about constructing meaningful quality measures tightly linked with patient outcomes.”
The researchers called for the development of other quality measures such as metrics aimed at identifying whether hemorrhage and preeclampsia protocols are being used in the delivery suite.
The study was funded by a grant from the National Institute of Child Health and Human Development and a fellowship grant from the European Commission. The researchers reported having no financial disclosures.
On Twitter @maryellenny
Hospital quality measures aimed at decreasing elective early deliveries and cesarean deliveries in low-risk women were not linked with declines in serious maternal or neonatal complications, according to a study published Oct. 15 in JAMA.
Data on more than 100,000 babies born at term in 2010 in New York City hospitals showed that there was wide variation in both maternal and neonatal complications between hospitals, but there was no association between the morbidity rates and the quality metrics studied (JAMA. 2014; 312:1531-41).
Dr. Elizabeth A. Howell of the Icahn School of Medicine at Mount Sinai in New York, and her colleagues, looked at two Joint Commission perinatal quality measures: elective deliveries performed prior to 39 weeks of gestation and cesarean deliveries performed in low-risk nulliparous women.
The rates for elective deliveries before 39 weeks ranged from 15.5 to 41.9 per 100 deliveries among the 41 hospitals studied. For cesarean deliveries in low-risk women, the rates range from 11.7 to 39.3 per 100 deliveries.
There was also a wide range in maternal and neonatal morbidity. Maternal morbidity rates ranged from 0.9 to 5.7 mothers with complications per 100 deliveries, while neonatal morbidity ranged from 3.1 to 21.3 infants with complications per 100 births. Neither of the Joint Commission quality measures was associated with severe complications.
Dr. Howell and her colleagues concluded that while overutilization measures may be important, they aren’t comprehensive enough to reflect the actual quality of care.
These perinatal measures are not the only hospital-level quality measures not linked to decreases in the outcomes they are designed to influence, the investigators noted. They cited examples where quality measures for heart failure, pneumonia, acute MI, and infection control were not associated with improved outcomes or predicted only small improvements.
Quality measures often “capture only a narrow slice of hospital quality,” Dr. Howell wrote. “There is a need to reassess how these measures are designed and implemented and to think more broadly about constructing meaningful quality measures tightly linked with patient outcomes.”
The researchers called for the development of other quality measures such as metrics aimed at identifying whether hemorrhage and preeclampsia protocols are being used in the delivery suite.
The study was funded by a grant from the National Institute of Child Health and Human Development and a fellowship grant from the European Commission. The researchers reported having no financial disclosures.
On Twitter @maryellenny
FROM JAMA
Key clinical point: Existing obstetrics measures may not help improve quality of care.
Major finding: There was a four- to fivefold variation in severe maternal morbidity rates and a sevenfold variation in neonatal morbidity, but no correlation to the obstetric performance measures studied.
Data source: Birth certificate data linked with New York State discharge abstract data for all delivery and newborn hospitalizations in New York City in 2010. The final sample included 103,416 newborns.
Disclosures:The study was funded by a grant from the National Institute of Child Health and Human Development and a fellowship grant from the European Commission. The researchers reported having no financial disclosures.
Retinopathy screening during gestational diabetes may be lacking
VIENNA – A concerning number of women with gestational diabetes may not be getting optimal retinal care during their pregnancy.
About 11% of women in an Irish observational cohort study received just one retinal exam of the two that are recommended during pregnancy and 29% received no exam, Dr. Aoife Maria Egan said at the annual meeting of the European Association for the Study of Diabetes.
Women who attended prepregnancy care clinics were most likely to get appropriate screening. “This is probably because they had been made aware of what would be expected for them during pregnancy,” said Dr. Egan of the University Hospital Galway (Ireland).
The study was an offshoot of the ongoing Atlantic Diabetes in Pregnancy (DIP) project, which examines the outcomes of pregnancy for women with type 1 and type 2 diabetes and the factors influencing these outcomes. It was created in 2005 and provides universal screening for gestational diabetes as part of its outcomes research. The retinopathy study covered 2006-2012.
Adequate retinopathy evaluation was considered to be at least two retinal exams conducted in separate trimesters. Each exam consisted of tests of visual acuity, dilation, and opthalmologic exams and retinal images that were reviewed by an accredited retinal grader.
DIP considered four grades of retinopathy, which have been defined by the National Screening Committee in the United Kingdom: none (R0), background (R1), preproliferative (R2), and proliferative (R3). Additionally, macular edema is graded as present or absent. Progression was considered to be a change from one retinopathy grade to the next or the development of new macular edema.
The study group consisted of 341 women with gestational diabetes (68% type 1). Most of these (90%) were white. They averaged 31 years of age, with a history of two pregnancies. There were 296 live births (87%). The final analysis included 307 women who delivered after 22 weeks.
Most of the women (60%) did have an adequate evaluation. However, 11% had only one exam and 29% had no exam, Dr. Egan said.
There were a few significant differences between those who had adequate retinal exams and those who did not. Women who had two exams were more likely to have type 1 diabetes (72% vs. 61% without adequate exams) and white (94% vs. 85%). They had a longer duration of diabetics (11 vs. 9 years). More of them had attended a prepregnancy center (56% vs. 17%) and were taking folic acid (70% vs. 54%), she reported.
A multivariate analysis determined that attending the prepregnancy clinic was the strongest predictive factor, increasing the likelihood of adequate screening by more than six times.
Of those who had an adequate exam, 74% did not progress during their pregnancy and 26% did. Of those 48 who progressed, the largest portion (26) went from R0 to R1. R1 to R2 progression occurred in seven patients, and R1/R2 to R3 in six. Six patients developed a new maculopathy and three had worsening maculopathy.
Several significant differences emerged when comparing those who progressed with those who did not. The women with worsening retinopathy had a longer duration of diabetes (14 vs. 10 years) and higher systolic blood pressure at baseline (129 vs. 122 mm Hg).
They also had higher baseline hemoglobin A1c (7.7% vs. 7%) and a greater change in HbA1cduring the pregnancy (1.38% vs. 0.74%). An HbA1creduction between the first and third trimester was associated with a doubling in the risk of progression. Those who had a higher reduction of HbA1cbetween trimesters one and three were more than twice as likely to have retinopathy progression.
This highlights the dilemma clinicians face when trying to balance maternal and fetal risks of glycemic control, Dr. Egan said. Women who present with poor glycemic control should moderate that to optimize fetal health, but lowering HbA1ccan predispose the mother to retinopathic changes.
“We try and target tight control and monitor the ones we know are at risk for retinopathy progression very closely,” she said.
Whether that makes any long-term difference is still an unknown. “Some studies have shown that, while pregnancy might accelerate retinopathy, in the long run women end up even in that regard. Six or seven years down the road, everyone looks the same,” she noted.
The DIP program is funded by the Health Research Board of Ireland. Dr. Egan had no financial disclosures.
On Twitter @alz_gal
VIENNA – A concerning number of women with gestational diabetes may not be getting optimal retinal care during their pregnancy.
About 11% of women in an Irish observational cohort study received just one retinal exam of the two that are recommended during pregnancy and 29% received no exam, Dr. Aoife Maria Egan said at the annual meeting of the European Association for the Study of Diabetes.
Women who attended prepregnancy care clinics were most likely to get appropriate screening. “This is probably because they had been made aware of what would be expected for them during pregnancy,” said Dr. Egan of the University Hospital Galway (Ireland).
The study was an offshoot of the ongoing Atlantic Diabetes in Pregnancy (DIP) project, which examines the outcomes of pregnancy for women with type 1 and type 2 diabetes and the factors influencing these outcomes. It was created in 2005 and provides universal screening for gestational diabetes as part of its outcomes research. The retinopathy study covered 2006-2012.
Adequate retinopathy evaluation was considered to be at least two retinal exams conducted in separate trimesters. Each exam consisted of tests of visual acuity, dilation, and opthalmologic exams and retinal images that were reviewed by an accredited retinal grader.
DIP considered four grades of retinopathy, which have been defined by the National Screening Committee in the United Kingdom: none (R0), background (R1), preproliferative (R2), and proliferative (R3). Additionally, macular edema is graded as present or absent. Progression was considered to be a change from one retinopathy grade to the next or the development of new macular edema.
The study group consisted of 341 women with gestational diabetes (68% type 1). Most of these (90%) were white. They averaged 31 years of age, with a history of two pregnancies. There were 296 live births (87%). The final analysis included 307 women who delivered after 22 weeks.
Most of the women (60%) did have an adequate evaluation. However, 11% had only one exam and 29% had no exam, Dr. Egan said.
There were a few significant differences between those who had adequate retinal exams and those who did not. Women who had two exams were more likely to have type 1 diabetes (72% vs. 61% without adequate exams) and white (94% vs. 85%). They had a longer duration of diabetics (11 vs. 9 years). More of them had attended a prepregnancy center (56% vs. 17%) and were taking folic acid (70% vs. 54%), she reported.
A multivariate analysis determined that attending the prepregnancy clinic was the strongest predictive factor, increasing the likelihood of adequate screening by more than six times.
Of those who had an adequate exam, 74% did not progress during their pregnancy and 26% did. Of those 48 who progressed, the largest portion (26) went from R0 to R1. R1 to R2 progression occurred in seven patients, and R1/R2 to R3 in six. Six patients developed a new maculopathy and three had worsening maculopathy.
Several significant differences emerged when comparing those who progressed with those who did not. The women with worsening retinopathy had a longer duration of diabetes (14 vs. 10 years) and higher systolic blood pressure at baseline (129 vs. 122 mm Hg).
They also had higher baseline hemoglobin A1c (7.7% vs. 7%) and a greater change in HbA1cduring the pregnancy (1.38% vs. 0.74%). An HbA1creduction between the first and third trimester was associated with a doubling in the risk of progression. Those who had a higher reduction of HbA1cbetween trimesters one and three were more than twice as likely to have retinopathy progression.
This highlights the dilemma clinicians face when trying to balance maternal and fetal risks of glycemic control, Dr. Egan said. Women who present with poor glycemic control should moderate that to optimize fetal health, but lowering HbA1ccan predispose the mother to retinopathic changes.
“We try and target tight control and monitor the ones we know are at risk for retinopathy progression very closely,” she said.
Whether that makes any long-term difference is still an unknown. “Some studies have shown that, while pregnancy might accelerate retinopathy, in the long run women end up even in that regard. Six or seven years down the road, everyone looks the same,” she noted.
The DIP program is funded by the Health Research Board of Ireland. Dr. Egan had no financial disclosures.
On Twitter @alz_gal
VIENNA – A concerning number of women with gestational diabetes may not be getting optimal retinal care during their pregnancy.
About 11% of women in an Irish observational cohort study received just one retinal exam of the two that are recommended during pregnancy and 29% received no exam, Dr. Aoife Maria Egan said at the annual meeting of the European Association for the Study of Diabetes.
Women who attended prepregnancy care clinics were most likely to get appropriate screening. “This is probably because they had been made aware of what would be expected for them during pregnancy,” said Dr. Egan of the University Hospital Galway (Ireland).
The study was an offshoot of the ongoing Atlantic Diabetes in Pregnancy (DIP) project, which examines the outcomes of pregnancy for women with type 1 and type 2 diabetes and the factors influencing these outcomes. It was created in 2005 and provides universal screening for gestational diabetes as part of its outcomes research. The retinopathy study covered 2006-2012.
Adequate retinopathy evaluation was considered to be at least two retinal exams conducted in separate trimesters. Each exam consisted of tests of visual acuity, dilation, and opthalmologic exams and retinal images that were reviewed by an accredited retinal grader.
DIP considered four grades of retinopathy, which have been defined by the National Screening Committee in the United Kingdom: none (R0), background (R1), preproliferative (R2), and proliferative (R3). Additionally, macular edema is graded as present or absent. Progression was considered to be a change from one retinopathy grade to the next or the development of new macular edema.
The study group consisted of 341 women with gestational diabetes (68% type 1). Most of these (90%) were white. They averaged 31 years of age, with a history of two pregnancies. There were 296 live births (87%). The final analysis included 307 women who delivered after 22 weeks.
Most of the women (60%) did have an adequate evaluation. However, 11% had only one exam and 29% had no exam, Dr. Egan said.
There were a few significant differences between those who had adequate retinal exams and those who did not. Women who had two exams were more likely to have type 1 diabetes (72% vs. 61% without adequate exams) and white (94% vs. 85%). They had a longer duration of diabetics (11 vs. 9 years). More of them had attended a prepregnancy center (56% vs. 17%) and were taking folic acid (70% vs. 54%), she reported.
A multivariate analysis determined that attending the prepregnancy clinic was the strongest predictive factor, increasing the likelihood of adequate screening by more than six times.
Of those who had an adequate exam, 74% did not progress during their pregnancy and 26% did. Of those 48 who progressed, the largest portion (26) went from R0 to R1. R1 to R2 progression occurred in seven patients, and R1/R2 to R3 in six. Six patients developed a new maculopathy and three had worsening maculopathy.
Several significant differences emerged when comparing those who progressed with those who did not. The women with worsening retinopathy had a longer duration of diabetes (14 vs. 10 years) and higher systolic blood pressure at baseline (129 vs. 122 mm Hg).
They also had higher baseline hemoglobin A1c (7.7% vs. 7%) and a greater change in HbA1cduring the pregnancy (1.38% vs. 0.74%). An HbA1creduction between the first and third trimester was associated with a doubling in the risk of progression. Those who had a higher reduction of HbA1cbetween trimesters one and three were more than twice as likely to have retinopathy progression.
This highlights the dilemma clinicians face when trying to balance maternal and fetal risks of glycemic control, Dr. Egan said. Women who present with poor glycemic control should moderate that to optimize fetal health, but lowering HbA1ccan predispose the mother to retinopathic changes.
“We try and target tight control and monitor the ones we know are at risk for retinopathy progression very closely,” she said.
Whether that makes any long-term difference is still an unknown. “Some studies have shown that, while pregnancy might accelerate retinopathy, in the long run women end up even in that regard. Six or seven years down the road, everyone looks the same,” she noted.
The DIP program is funded by the Health Research Board of Ireland. Dr. Egan had no financial disclosures.
On Twitter @alz_gal
AT EASD 2014
Key clinical point: Women with gestational diabetes may not get adequate evaluation for retinopathy.
Major finding: About 40% of women with gestational diabetes didn’t receive adequate evaluation for retinopathy during their pregnancy.
Data source: The prospective observational cohort comprised 307 women.
Disclosures: The DIP program is funded by the Health Research Board of Ireland. Dr. Egan had no financial disclosures.
Maternal weight before pregnancy linked to children’s cognition
VIENNA – By age 4 years, the children of women who were overweight or obese before their pregnancy scored 3-4 points below normal on measures of neurocognitive development.
The children showed deficits in motor and memory scales, as well as in general cognition, Dr. Leda Chatzi said at the annual meeting of the European Association for the Study of Diabetes.
Children whose mothers had gestational diabetes did not exhibit similar decreased cognitive scores. They were, however, significantly more likely to exhibit symptoms of attention-deficit/hyperactivity disorder, said Dr. Chatzi of the University of Crete, Heraklion, Greece.
“These findings have important public health implications, given the increasing prevalence of maternal obesity and gestational diabetes worldwide,” she said.
Dr. Chatzi presented a subanalysis of the Rhea Study, a mother-child birth cohort that began in Crete in 2007 with the aim of investigating the potential risks maternal environment and lifestyle might exert upon offspring – including maternal obesity. It comprises about 1,300 live singleton births. At entry, mothers give urine and blood samples and undergo anthropometric measurements. Cord blood is collected at birth. Mothers and children are followed from birth onward with anthropometrics, psychological and clinical exams, neurodevelopmental testing, and further biological samples. The oldest children in the cohort are now 7 years old; follow-up continues.
Dr. Chatzi’s study comprised 707 mother-child pairs; the children were 4 years old at the time of this analysis. Maternal factors considered in the analysis included fasting glucose and insulin levels at gestational weeks 10-14, body mass index before pregnancy and at the end of the first trimester, and the development of gestational diabetes.
The children underwent several tests of neurocognition, including the McCarthy Scales of Children’s Abilities; the Attentional Deficit Hyperactivity Disorder Test; and the Strengths and Difficulties Questionnaire.
The McCarthy scale includes several subscales: perceptual, quantitative, motor, verbal, memory, and general cognition. A multivariate analysis controlled for the child’s gender, body mass index (BMI), and preschool attendance; maternal demographics and smoking; and the duration of breastfeeding.
At delivery, mothers had a mean age of 30 years; 32% smoked during pregnancy. The infants’ mean gestational age was 38 weeks. Breastfeeding lasted a mean of 4 months.
About one-third of the mothers were either overweight (21%) or obese (13%). Most of those (92%) developed gestational diabetes.
As maternal prepregnancy BMI increased, child scores on general cognition, memory, and motor subscales decreased. The break point for decline below population norms seemed to be between 25 and 30 kg/m2. The children of women whose prepregnancy BMI approached 40 kg/m2 scored a mean of 3-4 points lower on general cognition and the subscales of memory, quantitative, perceptual, and motor performance.
Prepregnancy BMI had no effect on attention-deficit/hyperactivity disorder scores. However, ADHD scores increased significantly in the children of mothers who developed gestational diabetes.
The pathophysiologic link between gestational diabetes and ADHD has never been elucidated, Dr. Chatzi noted. It’s something she intends to investigate. “We’re planning to evaluate these children at later ages, including studying inflammatory markers and potential genetic markers of DNA methylation,” she said.
Dr. Chatzi had no financial disclosures.
On Twitter @alz_gal
VIENNA – By age 4 years, the children of women who were overweight or obese before their pregnancy scored 3-4 points below normal on measures of neurocognitive development.
The children showed deficits in motor and memory scales, as well as in general cognition, Dr. Leda Chatzi said at the annual meeting of the European Association for the Study of Diabetes.
Children whose mothers had gestational diabetes did not exhibit similar decreased cognitive scores. They were, however, significantly more likely to exhibit symptoms of attention-deficit/hyperactivity disorder, said Dr. Chatzi of the University of Crete, Heraklion, Greece.
“These findings have important public health implications, given the increasing prevalence of maternal obesity and gestational diabetes worldwide,” she said.
Dr. Chatzi presented a subanalysis of the Rhea Study, a mother-child birth cohort that began in Crete in 2007 with the aim of investigating the potential risks maternal environment and lifestyle might exert upon offspring – including maternal obesity. It comprises about 1,300 live singleton births. At entry, mothers give urine and blood samples and undergo anthropometric measurements. Cord blood is collected at birth. Mothers and children are followed from birth onward with anthropometrics, psychological and clinical exams, neurodevelopmental testing, and further biological samples. The oldest children in the cohort are now 7 years old; follow-up continues.
Dr. Chatzi’s study comprised 707 mother-child pairs; the children were 4 years old at the time of this analysis. Maternal factors considered in the analysis included fasting glucose and insulin levels at gestational weeks 10-14, body mass index before pregnancy and at the end of the first trimester, and the development of gestational diabetes.
The children underwent several tests of neurocognition, including the McCarthy Scales of Children’s Abilities; the Attentional Deficit Hyperactivity Disorder Test; and the Strengths and Difficulties Questionnaire.
The McCarthy scale includes several subscales: perceptual, quantitative, motor, verbal, memory, and general cognition. A multivariate analysis controlled for the child’s gender, body mass index (BMI), and preschool attendance; maternal demographics and smoking; and the duration of breastfeeding.
At delivery, mothers had a mean age of 30 years; 32% smoked during pregnancy. The infants’ mean gestational age was 38 weeks. Breastfeeding lasted a mean of 4 months.
About one-third of the mothers were either overweight (21%) or obese (13%). Most of those (92%) developed gestational diabetes.
As maternal prepregnancy BMI increased, child scores on general cognition, memory, and motor subscales decreased. The break point for decline below population norms seemed to be between 25 and 30 kg/m2. The children of women whose prepregnancy BMI approached 40 kg/m2 scored a mean of 3-4 points lower on general cognition and the subscales of memory, quantitative, perceptual, and motor performance.
Prepregnancy BMI had no effect on attention-deficit/hyperactivity disorder scores. However, ADHD scores increased significantly in the children of mothers who developed gestational diabetes.
The pathophysiologic link between gestational diabetes and ADHD has never been elucidated, Dr. Chatzi noted. It’s something she intends to investigate. “We’re planning to evaluate these children at later ages, including studying inflammatory markers and potential genetic markers of DNA methylation,” she said.
Dr. Chatzi had no financial disclosures.
On Twitter @alz_gal
VIENNA – By age 4 years, the children of women who were overweight or obese before their pregnancy scored 3-4 points below normal on measures of neurocognitive development.
The children showed deficits in motor and memory scales, as well as in general cognition, Dr. Leda Chatzi said at the annual meeting of the European Association for the Study of Diabetes.
Children whose mothers had gestational diabetes did not exhibit similar decreased cognitive scores. They were, however, significantly more likely to exhibit symptoms of attention-deficit/hyperactivity disorder, said Dr. Chatzi of the University of Crete, Heraklion, Greece.
“These findings have important public health implications, given the increasing prevalence of maternal obesity and gestational diabetes worldwide,” she said.
Dr. Chatzi presented a subanalysis of the Rhea Study, a mother-child birth cohort that began in Crete in 2007 with the aim of investigating the potential risks maternal environment and lifestyle might exert upon offspring – including maternal obesity. It comprises about 1,300 live singleton births. At entry, mothers give urine and blood samples and undergo anthropometric measurements. Cord blood is collected at birth. Mothers and children are followed from birth onward with anthropometrics, psychological and clinical exams, neurodevelopmental testing, and further biological samples. The oldest children in the cohort are now 7 years old; follow-up continues.
Dr. Chatzi’s study comprised 707 mother-child pairs; the children were 4 years old at the time of this analysis. Maternal factors considered in the analysis included fasting glucose and insulin levels at gestational weeks 10-14, body mass index before pregnancy and at the end of the first trimester, and the development of gestational diabetes.
The children underwent several tests of neurocognition, including the McCarthy Scales of Children’s Abilities; the Attentional Deficit Hyperactivity Disorder Test; and the Strengths and Difficulties Questionnaire.
The McCarthy scale includes several subscales: perceptual, quantitative, motor, verbal, memory, and general cognition. A multivariate analysis controlled for the child’s gender, body mass index (BMI), and preschool attendance; maternal demographics and smoking; and the duration of breastfeeding.
At delivery, mothers had a mean age of 30 years; 32% smoked during pregnancy. The infants’ mean gestational age was 38 weeks. Breastfeeding lasted a mean of 4 months.
About one-third of the mothers were either overweight (21%) or obese (13%). Most of those (92%) developed gestational diabetes.
As maternal prepregnancy BMI increased, child scores on general cognition, memory, and motor subscales decreased. The break point for decline below population norms seemed to be between 25 and 30 kg/m2. The children of women whose prepregnancy BMI approached 40 kg/m2 scored a mean of 3-4 points lower on general cognition and the subscales of memory, quantitative, perceptual, and motor performance.
Prepregnancy BMI had no effect on attention-deficit/hyperactivity disorder scores. However, ADHD scores increased significantly in the children of mothers who developed gestational diabetes.
The pathophysiologic link between gestational diabetes and ADHD has never been elucidated, Dr. Chatzi noted. It’s something she intends to investigate. “We’re planning to evaluate these children at later ages, including studying inflammatory markers and potential genetic markers of DNA methylation,” she said.
Dr. Chatzi had no financial disclosures.
On Twitter @alz_gal
At EASD 2014
Key clinical point: Maternal prepregnancy weight may influence child cognition by 4 years.
Major finding: The children of women who were overweight or obese before pregnancy scored three-four points lower than normal on neurocognitive tests.
Data source: The prospective observational cohort comprised 707 mother-child pairs.
Disclosures: Dr. Chatzi had no financial disclosures.
Mother’s preference should determine epidural timing
The best time to offer pain relief to a woman in labor is when she requests it, according to a study.
“The evidence we have does not provide a compelling reason why this [request] should be refused,” Dr. Ban Leong Sng, head of women’s anesthesia at KK Women’s and Children’s Hospital in Singapore, said in a statement, speaking about mothers who ask for an epidural early in their labor. “The right time to give the epidural is when the woman requests pain relief.”
Although previous studies indicated that early initiation of an epidural correlated with longer labors and increased risk of cesarean delivery, Dr. Sng and his colleagues did not find clinically significant support for this in their meta-analysis of nine randomized, controlled studies of 15,752 pregnant women who received epidural at various times during their labor. The finding appears online in the Cochrane Library.
“There is predominantly high-quality evidence that early or late initiation of epidural analgesia for labor have similar effects on all measured outcomes,” Dr. Sng and his associates wrote.
The risk ratio for cesarean delivery with early vs. late initiation of epidural was 1.02 (95% confidence interval, 0.96 to 1.08). Similarly, there was no notable difference in the risk for instrumental birth correlative to the timing of the epidural (relative risk 0.93%; 95% CI 0.86 to 1.01).
The mean difference between early or late epidural when it came to the duration of the second stage of labor was about three and a half minutes (95% CI, -6.71 to 0.27). The authors noted that there was “significant heterogeneity” in the duration of the first stage of labor, and that their data were not pooled.
As for fetal outcomes, results were similar. The differences in Apgar scores of less than 7 at 1 minute post partum in infants born to mothers who’d had early or late initiation of pain relief was negligible (RR 0.96; 95% CI 0.84 to 1.10). There also were no clinically significant differences in Apgar scores less than 7 at 5 minutes post partum (RR 0.96; 95% CI, 0.69 to 1.33).
In addition, the difference in umbilical arterial pH in infants born to mothers with early or late epidural was negligible (mean difference, 0.01; 95% CI -0.01 to 0.03).
The authors noted the studies they analyzed varied in their definition of “early” and “late” epidural; however, early initiation was typically defined as when there was cervical dilation of less than 4-5 cm. Late initiation typically was considered to be when there was cervical dilation of 4-5 cm or more. Analgesic doses also varied across the studies, as did pain relief administered before initiation of the epidural.
On Twitter @whitneymcknight
The best time to offer pain relief to a woman in labor is when she requests it, according to a study.
“The evidence we have does not provide a compelling reason why this [request] should be refused,” Dr. Ban Leong Sng, head of women’s anesthesia at KK Women’s and Children’s Hospital in Singapore, said in a statement, speaking about mothers who ask for an epidural early in their labor. “The right time to give the epidural is when the woman requests pain relief.”
Although previous studies indicated that early initiation of an epidural correlated with longer labors and increased risk of cesarean delivery, Dr. Sng and his colleagues did not find clinically significant support for this in their meta-analysis of nine randomized, controlled studies of 15,752 pregnant women who received epidural at various times during their labor. The finding appears online in the Cochrane Library.
“There is predominantly high-quality evidence that early or late initiation of epidural analgesia for labor have similar effects on all measured outcomes,” Dr. Sng and his associates wrote.
The risk ratio for cesarean delivery with early vs. late initiation of epidural was 1.02 (95% confidence interval, 0.96 to 1.08). Similarly, there was no notable difference in the risk for instrumental birth correlative to the timing of the epidural (relative risk 0.93%; 95% CI 0.86 to 1.01).
The mean difference between early or late epidural when it came to the duration of the second stage of labor was about three and a half minutes (95% CI, -6.71 to 0.27). The authors noted that there was “significant heterogeneity” in the duration of the first stage of labor, and that their data were not pooled.
As for fetal outcomes, results were similar. The differences in Apgar scores of less than 7 at 1 minute post partum in infants born to mothers who’d had early or late initiation of pain relief was negligible (RR 0.96; 95% CI 0.84 to 1.10). There also were no clinically significant differences in Apgar scores less than 7 at 5 minutes post partum (RR 0.96; 95% CI, 0.69 to 1.33).
In addition, the difference in umbilical arterial pH in infants born to mothers with early or late epidural was negligible (mean difference, 0.01; 95% CI -0.01 to 0.03).
The authors noted the studies they analyzed varied in their definition of “early” and “late” epidural; however, early initiation was typically defined as when there was cervical dilation of less than 4-5 cm. Late initiation typically was considered to be when there was cervical dilation of 4-5 cm or more. Analgesic doses also varied across the studies, as did pain relief administered before initiation of the epidural.
On Twitter @whitneymcknight
The best time to offer pain relief to a woman in labor is when she requests it, according to a study.
“The evidence we have does not provide a compelling reason why this [request] should be refused,” Dr. Ban Leong Sng, head of women’s anesthesia at KK Women’s and Children’s Hospital in Singapore, said in a statement, speaking about mothers who ask for an epidural early in their labor. “The right time to give the epidural is when the woman requests pain relief.”
Although previous studies indicated that early initiation of an epidural correlated with longer labors and increased risk of cesarean delivery, Dr. Sng and his colleagues did not find clinically significant support for this in their meta-analysis of nine randomized, controlled studies of 15,752 pregnant women who received epidural at various times during their labor. The finding appears online in the Cochrane Library.
“There is predominantly high-quality evidence that early or late initiation of epidural analgesia for labor have similar effects on all measured outcomes,” Dr. Sng and his associates wrote.
The risk ratio for cesarean delivery with early vs. late initiation of epidural was 1.02 (95% confidence interval, 0.96 to 1.08). Similarly, there was no notable difference in the risk for instrumental birth correlative to the timing of the epidural (relative risk 0.93%; 95% CI 0.86 to 1.01).
The mean difference between early or late epidural when it came to the duration of the second stage of labor was about three and a half minutes (95% CI, -6.71 to 0.27). The authors noted that there was “significant heterogeneity” in the duration of the first stage of labor, and that their data were not pooled.
As for fetal outcomes, results were similar. The differences in Apgar scores of less than 7 at 1 minute post partum in infants born to mothers who’d had early or late initiation of pain relief was negligible (RR 0.96; 95% CI 0.84 to 1.10). There also were no clinically significant differences in Apgar scores less than 7 at 5 minutes post partum (RR 0.96; 95% CI, 0.69 to 1.33).
In addition, the difference in umbilical arterial pH in infants born to mothers with early or late epidural was negligible (mean difference, 0.01; 95% CI -0.01 to 0.03).
The authors noted the studies they analyzed varied in their definition of “early” and “late” epidural; however, early initiation was typically defined as when there was cervical dilation of less than 4-5 cm. Late initiation typically was considered to be when there was cervical dilation of 4-5 cm or more. Analgesic doses also varied across the studies, as did pain relief administered before initiation of the epidural.
On Twitter @whitneymcknight
FROM THE COCHRANE LIBRARY
Key clinical point: The best time for an epidural is when the mother requests it.
Major finding: No clinically significant difference was found in maternal or fetal outcomes between early or late initiation of epidural.
Data source: Meta-analysis of data from nine randomized controlled studies of early or late epidurals in 15,752 women.
Disclosures: Dr. Sng and his colleagues said they had no relevant disclosures.
Eating fried food before pregnancy may increase risk of gestational diabetes
Even moderate consumption of fried foods before pregnancy can significantly increase the risk of gestational diabetes, a large retrospective study has determined.
Depending on how often fried foods were consumed each week, the risk increased anywhere from 13% to more than double, compared with those who abstained from fried foods. The risks were relatively stable when body weight was controlled for, and higher for foods eaten away from home than in-home. These findings seem to support the authors’ conjecture that chemical changes, rather than calories, may be the root problem.
“The potential detrimental effects may result from the modification of foods and frying medium, and generation of harmful by-products during the frying process,” especially because frying oils in restaurants are generally reused, increasing degradation, Dr. Wei Bao, of the National Institutes of Health, and his associates wrote in the Oct. 8 issue of Diabetologia (2014 [doi: 10.1007/s00125-014-3382-x]). “Frying deteriorates oils through the processes of oxidation and hydrogenation, leading to an increase in the absorption of oil degradation products by the foods being fried, and also a loss of unsaturated fatty acids ... and an increase in the corresponding trans-fatty acids.”
Frying also results in the production of advanced glycation end products, which, because they increase oxidative stress and inflammation, have been implicated in insulin resistance, beta-cell damage, and diabetes.
The team used data from the Nurses’ Health Study to examine the relationship between consuming fried foods and the development of gestational diabetes. The cohort included 21,079 singleton pregnancies. Among these, there were 847 (4%) incident cases of gestational diabetes. The analysis compared fried foods consumed 1-3, 4-6, and 7 or more times per week, to consumption less than once per week.
The relative risks were significantly increased for each of these consumption patterns (1.13, 1.31, and 2.18, respectively). The significant association was somewhat attenuated, but remained significant, after adjustment for body mass index.
However, the results were altered when the authors broke their general analysis down into consumption of fried foods up to four times weekly, either away from or at home. Only consumption away from home remained significantly associated with gestational diabetes (relative risk, 1.63)
The National Institutes of Health funded the study. The authors had no financial disclosures.
On Twitter @alz_gal
Even moderate consumption of fried foods before pregnancy can significantly increase the risk of gestational diabetes, a large retrospective study has determined.
Depending on how often fried foods were consumed each week, the risk increased anywhere from 13% to more than double, compared with those who abstained from fried foods. The risks were relatively stable when body weight was controlled for, and higher for foods eaten away from home than in-home. These findings seem to support the authors’ conjecture that chemical changes, rather than calories, may be the root problem.
“The potential detrimental effects may result from the modification of foods and frying medium, and generation of harmful by-products during the frying process,” especially because frying oils in restaurants are generally reused, increasing degradation, Dr. Wei Bao, of the National Institutes of Health, and his associates wrote in the Oct. 8 issue of Diabetologia (2014 [doi: 10.1007/s00125-014-3382-x]). “Frying deteriorates oils through the processes of oxidation and hydrogenation, leading to an increase in the absorption of oil degradation products by the foods being fried, and also a loss of unsaturated fatty acids ... and an increase in the corresponding trans-fatty acids.”
Frying also results in the production of advanced glycation end products, which, because they increase oxidative stress and inflammation, have been implicated in insulin resistance, beta-cell damage, and diabetes.
The team used data from the Nurses’ Health Study to examine the relationship between consuming fried foods and the development of gestational diabetes. The cohort included 21,079 singleton pregnancies. Among these, there were 847 (4%) incident cases of gestational diabetes. The analysis compared fried foods consumed 1-3, 4-6, and 7 or more times per week, to consumption less than once per week.
The relative risks were significantly increased for each of these consumption patterns (1.13, 1.31, and 2.18, respectively). The significant association was somewhat attenuated, but remained significant, after adjustment for body mass index.
However, the results were altered when the authors broke their general analysis down into consumption of fried foods up to four times weekly, either away from or at home. Only consumption away from home remained significantly associated with gestational diabetes (relative risk, 1.63)
The National Institutes of Health funded the study. The authors had no financial disclosures.
On Twitter @alz_gal
Even moderate consumption of fried foods before pregnancy can significantly increase the risk of gestational diabetes, a large retrospective study has determined.
Depending on how often fried foods were consumed each week, the risk increased anywhere from 13% to more than double, compared with those who abstained from fried foods. The risks were relatively stable when body weight was controlled for, and higher for foods eaten away from home than in-home. These findings seem to support the authors’ conjecture that chemical changes, rather than calories, may be the root problem.
“The potential detrimental effects may result from the modification of foods and frying medium, and generation of harmful by-products during the frying process,” especially because frying oils in restaurants are generally reused, increasing degradation, Dr. Wei Bao, of the National Institutes of Health, and his associates wrote in the Oct. 8 issue of Diabetologia (2014 [doi: 10.1007/s00125-014-3382-x]). “Frying deteriorates oils through the processes of oxidation and hydrogenation, leading to an increase in the absorption of oil degradation products by the foods being fried, and also a loss of unsaturated fatty acids ... and an increase in the corresponding trans-fatty acids.”
Frying also results in the production of advanced glycation end products, which, because they increase oxidative stress and inflammation, have been implicated in insulin resistance, beta-cell damage, and diabetes.
The team used data from the Nurses’ Health Study to examine the relationship between consuming fried foods and the development of gestational diabetes. The cohort included 21,079 singleton pregnancies. Among these, there were 847 (4%) incident cases of gestational diabetes. The analysis compared fried foods consumed 1-3, 4-6, and 7 or more times per week, to consumption less than once per week.
The relative risks were significantly increased for each of these consumption patterns (1.13, 1.31, and 2.18, respectively). The significant association was somewhat attenuated, but remained significant, after adjustment for body mass index.
However, the results were altered when the authors broke their general analysis down into consumption of fried foods up to four times weekly, either away from or at home. Only consumption away from home remained significantly associated with gestational diabetes (relative risk, 1.63)
The National Institutes of Health funded the study. The authors had no financial disclosures.
On Twitter @alz_gal
FROM DIABETOLOGIA
Key clinical point: Eating fried foods before pregnancy is associated with an increased risk of gestational diabetes.
Major finding: Eating such foods could almost double the risk, depending on how frequently they were consumed.
Data source: The cohort comprised more than 21,000 women who were enrolled in the Nurses’ Health Study.
Disclosures: The National Institutes of Health funded the study. The authors had no financial disclosures.
Second child tests positive for HIV infection after apparent viral remission
An HIV-positive child, who was thought to have been cured of the virus after receiving intensive antiretroviral treatment for 3 years starting at birth, exhibited detectable signs of HIV infection just 2 weeks after termination of treatment.
The child, born to an HIV-positive mother from whom the infection was contracted, is the second reported instance of apparent HIV remission in a child after receiving early antiretroviral treatment (ART) at birth, following the case of the Mississippi infant. In both cases, intense ART was administered to the babies for prolonged periods of time beginning at birth, and traces of HIV were no longer evident in blood samples, only for the virus to return later.
“The so-called Mississippi child was believed to be cured thanks to early initiation of ART [which] raised the possibility of achieving a cure without procedures such as bone marrow transplant with CCR5-delta 32 cells,” according to a case report penned by Dr. Vania Giacomet and associates at the Luigi Sacco Hospital in Milan, Italy, where the most recent child was treated. “However, recent evidence of viral rebound in the Mississippi child shattered this hope.”
According to the case report published by The Lancet (Lancet 2014;384:1320), the latest child was born to an HIV-positive mother, who went into labor in December 2009 after 41 weeks’ gestation. HIV 1-2 antibody western blot and HIV-1 antigen p24 were positive in the newborn, who also had an HIV-RNA viral load of 152,560 copies per mL.
The infant was placed on a regimen of prophylaxis with zidovudine and nevirapine within 12 hours of birth, resulting in a viral load of 13,530 copies per mL after 4 days. Doctors then began a triple ART with ritonavir-boosted lopinavir, zidovudine, and lamivudine, which drastically decreased the infant’s viral load to 3,971 copies per mL at day 15, 49 copies per mL after 3 months, and “below assay detection” just 6 months after birth.
Doctors continued administering ART to the child for 3 years, reporting that the viral load remained undetectable and that CD4 T-cell counts were higher than usual. Furthermore, HIV antibodies also had vanished from the infant’s blood work, indicating that the infant was no longer seropositive. With the permission of the child’s mother, doctors terminated the treatment.
Two weeks after treatment ended, however, HIV tests on the child’s blood work came back positive, indicating that viral remission was no longer occurring. Because of this, doctors concluded that the ART was not sufficient to eliminate viral reservoirs within the child, thus allowing the disease to reemerge.
“The availability of many classes of potent antiretroviral drugs has substantially decreased HIV morbidity and mortality, but these drugs cannot eradicate the virus because they do not eliminate viral reservoirs,” the investigators said.
The case report also says that the infant’s in utero infection, low birth weight, and unusually high viral load likely “precluded long-lasting viral remission.” The authors note that the child’s case was not identical to that of the infant in Mississippi, namely because the Italian child’s immune system continued to show signs of responding to HIV infection even when viral load was undetectable; the Mississippi infant’s immune system did not.
No financial disclosures were reported.
An HIV-positive child, who was thought to have been cured of the virus after receiving intensive antiretroviral treatment for 3 years starting at birth, exhibited detectable signs of HIV infection just 2 weeks after termination of treatment.
The child, born to an HIV-positive mother from whom the infection was contracted, is the second reported instance of apparent HIV remission in a child after receiving early antiretroviral treatment (ART) at birth, following the case of the Mississippi infant. In both cases, intense ART was administered to the babies for prolonged periods of time beginning at birth, and traces of HIV were no longer evident in blood samples, only for the virus to return later.
“The so-called Mississippi child was believed to be cured thanks to early initiation of ART [which] raised the possibility of achieving a cure without procedures such as bone marrow transplant with CCR5-delta 32 cells,” according to a case report penned by Dr. Vania Giacomet and associates at the Luigi Sacco Hospital in Milan, Italy, where the most recent child was treated. “However, recent evidence of viral rebound in the Mississippi child shattered this hope.”
According to the case report published by The Lancet (Lancet 2014;384:1320), the latest child was born to an HIV-positive mother, who went into labor in December 2009 after 41 weeks’ gestation. HIV 1-2 antibody western blot and HIV-1 antigen p24 were positive in the newborn, who also had an HIV-RNA viral load of 152,560 copies per mL.
The infant was placed on a regimen of prophylaxis with zidovudine and nevirapine within 12 hours of birth, resulting in a viral load of 13,530 copies per mL after 4 days. Doctors then began a triple ART with ritonavir-boosted lopinavir, zidovudine, and lamivudine, which drastically decreased the infant’s viral load to 3,971 copies per mL at day 15, 49 copies per mL after 3 months, and “below assay detection” just 6 months after birth.
Doctors continued administering ART to the child for 3 years, reporting that the viral load remained undetectable and that CD4 T-cell counts were higher than usual. Furthermore, HIV antibodies also had vanished from the infant’s blood work, indicating that the infant was no longer seropositive. With the permission of the child’s mother, doctors terminated the treatment.
Two weeks after treatment ended, however, HIV tests on the child’s blood work came back positive, indicating that viral remission was no longer occurring. Because of this, doctors concluded that the ART was not sufficient to eliminate viral reservoirs within the child, thus allowing the disease to reemerge.
“The availability of many classes of potent antiretroviral drugs has substantially decreased HIV morbidity and mortality, but these drugs cannot eradicate the virus because they do not eliminate viral reservoirs,” the investigators said.
The case report also says that the infant’s in utero infection, low birth weight, and unusually high viral load likely “precluded long-lasting viral remission.” The authors note that the child’s case was not identical to that of the infant in Mississippi, namely because the Italian child’s immune system continued to show signs of responding to HIV infection even when viral load was undetectable; the Mississippi infant’s immune system did not.
No financial disclosures were reported.
An HIV-positive child, who was thought to have been cured of the virus after receiving intensive antiretroviral treatment for 3 years starting at birth, exhibited detectable signs of HIV infection just 2 weeks after termination of treatment.
The child, born to an HIV-positive mother from whom the infection was contracted, is the second reported instance of apparent HIV remission in a child after receiving early antiretroviral treatment (ART) at birth, following the case of the Mississippi infant. In both cases, intense ART was administered to the babies for prolonged periods of time beginning at birth, and traces of HIV were no longer evident in blood samples, only for the virus to return later.
“The so-called Mississippi child was believed to be cured thanks to early initiation of ART [which] raised the possibility of achieving a cure without procedures such as bone marrow transplant with CCR5-delta 32 cells,” according to a case report penned by Dr. Vania Giacomet and associates at the Luigi Sacco Hospital in Milan, Italy, where the most recent child was treated. “However, recent evidence of viral rebound in the Mississippi child shattered this hope.”
According to the case report published by The Lancet (Lancet 2014;384:1320), the latest child was born to an HIV-positive mother, who went into labor in December 2009 after 41 weeks’ gestation. HIV 1-2 antibody western blot and HIV-1 antigen p24 were positive in the newborn, who also had an HIV-RNA viral load of 152,560 copies per mL.
The infant was placed on a regimen of prophylaxis with zidovudine and nevirapine within 12 hours of birth, resulting in a viral load of 13,530 copies per mL after 4 days. Doctors then began a triple ART with ritonavir-boosted lopinavir, zidovudine, and lamivudine, which drastically decreased the infant’s viral load to 3,971 copies per mL at day 15, 49 copies per mL after 3 months, and “below assay detection” just 6 months after birth.
Doctors continued administering ART to the child for 3 years, reporting that the viral load remained undetectable and that CD4 T-cell counts were higher than usual. Furthermore, HIV antibodies also had vanished from the infant’s blood work, indicating that the infant was no longer seropositive. With the permission of the child’s mother, doctors terminated the treatment.
Two weeks after treatment ended, however, HIV tests on the child’s blood work came back positive, indicating that viral remission was no longer occurring. Because of this, doctors concluded that the ART was not sufficient to eliminate viral reservoirs within the child, thus allowing the disease to reemerge.
“The availability of many classes of potent antiretroviral drugs has substantially decreased HIV morbidity and mortality, but these drugs cannot eradicate the virus because they do not eliminate viral reservoirs,” the investigators said.
The case report also says that the infant’s in utero infection, low birth weight, and unusually high viral load likely “precluded long-lasting viral remission.” The authors note that the child’s case was not identical to that of the infant in Mississippi, namely because the Italian child’s immune system continued to show signs of responding to HIV infection even when viral load was undetectable; the Mississippi infant’s immune system did not.
No financial disclosures were reported.
FROM THE LANCET
Key clinical point: Early antiretroviral treatment did not eliminate viral reservoirs, leading to remeergence of HIV.
Major finding: Child began ART at birth and continued for 3 years, but showed detectable signs of HIV infection 2 weeks after termination of treatment.
Data source: Case report published in The Lancet.
Disclosures: No financial disclosures were reported.
Dutch study clarifies risk of attempted vaginal birth of breech fetus
Should a baby that presents breech at term be delivered vaginally or by cesarean delivery? In October 2000, results of the Term Breech Trial (TBT), the largest randomized controlled trial to investigate the effect of delivery mode for term breech deliveries on neonatal and maternal outcomes, essentially answered this question, showing that planned cesarean delivery was safer than planned vaginal delivery (with combined perinatal morbidity and mortality scores of 5% vs 16%, respectively).1 These study results affected national guidelines for choosing delivery mode in the Netherlands as well as other countries around the world.
What has been the impact on mode of delivery and neonatal outcome in the Netherlands since the TBT’s publication? Furthermore, are there antepartum parameters that can distinguish which women are at high risk versus low risk for adverse neonatal outcomes when presenting breech at delivery? Vlemmix and colleagues sought to answer these questions, using retrospective data from the Netherlands Perinatal Registry (PRN) from 1999 through 2007.1
Perinatal death decreased over time—but only for women electing cesarean
During the study period, approximately 4% of all births were breech. The researchers studied 58,320 women with term breech delivery, using the PRN. They noted an increase in the elective cesarean delivery (ECD) rate for these women, from 24% before October 2000 to 60% after December 2000, and as a consequence, found that overall perinatal mortality decreased from 1.3% to 0.7% (odds ratio [OR] 0.51; 95% confidence interval [CI] 0.28–0.93).1
However, among the women who underwent planned vaginal delivery, the overall perinatal mortality remained stable (1.7% vs 1.6%; OR, 0.96; 95% CI, 0.52–1.76). “Despite the lower percentage of women opting for or offered a vaginal delivery, and despite a higher emergency cesarean rate during vaginal breech birth, neonatal outcome within the planned vaginal birth group did not improve,” state the authors.1
Putting the results in absolute numbers
The investigators say that the 40% of Dutch women with breech presentation at term who still attempt vaginal birth do so without improved neonatal outcome; these deliveries generate a 10-fold higher fetal mortality rate compared with ECD. Further, no subgroup of women, when evaluating parity, onset of labor, type of breech presentation, and birthweight, could be identified with a low risk of poor neonatal outcome during planned vaginal delivery compared with ECD.1
Since the TBT, 1,692 more combined elective and emergency cesarean deliveries were performed annually, leading to five less neonatal deaths per year (number needed to treat, 338). If all women who still undergo planned vaginal birth receive ECD, 6,490 more ECDs would be performed, with 10 less neonatal deaths, 116 less neonates with low Apgar score, and 20 less neonates with birth trauma per year, according to the researchers.1
They suggest that clinicians use the results of this study when counseling women with a term breech presentation on mode of delivery. “To properly inform patients, a combination of risk presentation (absolute risks, relative risks and figures) is necessary to enable individual informed decision making.”1
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
Reference
- Vlemmix F, Bergenhenegouwen L, Schaaf JM, et al. Term breech deliveries in the Netherlands: did the increased cesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet Gynecol Scand. 2014;93:888–896.
Should a baby that presents breech at term be delivered vaginally or by cesarean delivery? In October 2000, results of the Term Breech Trial (TBT), the largest randomized controlled trial to investigate the effect of delivery mode for term breech deliveries on neonatal and maternal outcomes, essentially answered this question, showing that planned cesarean delivery was safer than planned vaginal delivery (with combined perinatal morbidity and mortality scores of 5% vs 16%, respectively).1 These study results affected national guidelines for choosing delivery mode in the Netherlands as well as other countries around the world.
What has been the impact on mode of delivery and neonatal outcome in the Netherlands since the TBT’s publication? Furthermore, are there antepartum parameters that can distinguish which women are at high risk versus low risk for adverse neonatal outcomes when presenting breech at delivery? Vlemmix and colleagues sought to answer these questions, using retrospective data from the Netherlands Perinatal Registry (PRN) from 1999 through 2007.1
Perinatal death decreased over time—but only for women electing cesarean
During the study period, approximately 4% of all births were breech. The researchers studied 58,320 women with term breech delivery, using the PRN. They noted an increase in the elective cesarean delivery (ECD) rate for these women, from 24% before October 2000 to 60% after December 2000, and as a consequence, found that overall perinatal mortality decreased from 1.3% to 0.7% (odds ratio [OR] 0.51; 95% confidence interval [CI] 0.28–0.93).1
However, among the women who underwent planned vaginal delivery, the overall perinatal mortality remained stable (1.7% vs 1.6%; OR, 0.96; 95% CI, 0.52–1.76). “Despite the lower percentage of women opting for or offered a vaginal delivery, and despite a higher emergency cesarean rate during vaginal breech birth, neonatal outcome within the planned vaginal birth group did not improve,” state the authors.1
Putting the results in absolute numbers
The investigators say that the 40% of Dutch women with breech presentation at term who still attempt vaginal birth do so without improved neonatal outcome; these deliveries generate a 10-fold higher fetal mortality rate compared with ECD. Further, no subgroup of women, when evaluating parity, onset of labor, type of breech presentation, and birthweight, could be identified with a low risk of poor neonatal outcome during planned vaginal delivery compared with ECD.1
Since the TBT, 1,692 more combined elective and emergency cesarean deliveries were performed annually, leading to five less neonatal deaths per year (number needed to treat, 338). If all women who still undergo planned vaginal birth receive ECD, 6,490 more ECDs would be performed, with 10 less neonatal deaths, 116 less neonates with low Apgar score, and 20 less neonates with birth trauma per year, according to the researchers.1
They suggest that clinicians use the results of this study when counseling women with a term breech presentation on mode of delivery. “To properly inform patients, a combination of risk presentation (absolute risks, relative risks and figures) is necessary to enable individual informed decision making.”1
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
Should a baby that presents breech at term be delivered vaginally or by cesarean delivery? In October 2000, results of the Term Breech Trial (TBT), the largest randomized controlled trial to investigate the effect of delivery mode for term breech deliveries on neonatal and maternal outcomes, essentially answered this question, showing that planned cesarean delivery was safer than planned vaginal delivery (with combined perinatal morbidity and mortality scores of 5% vs 16%, respectively).1 These study results affected national guidelines for choosing delivery mode in the Netherlands as well as other countries around the world.
What has been the impact on mode of delivery and neonatal outcome in the Netherlands since the TBT’s publication? Furthermore, are there antepartum parameters that can distinguish which women are at high risk versus low risk for adverse neonatal outcomes when presenting breech at delivery? Vlemmix and colleagues sought to answer these questions, using retrospective data from the Netherlands Perinatal Registry (PRN) from 1999 through 2007.1
Perinatal death decreased over time—but only for women electing cesarean
During the study period, approximately 4% of all births were breech. The researchers studied 58,320 women with term breech delivery, using the PRN. They noted an increase in the elective cesarean delivery (ECD) rate for these women, from 24% before October 2000 to 60% after December 2000, and as a consequence, found that overall perinatal mortality decreased from 1.3% to 0.7% (odds ratio [OR] 0.51; 95% confidence interval [CI] 0.28–0.93).1
However, among the women who underwent planned vaginal delivery, the overall perinatal mortality remained stable (1.7% vs 1.6%; OR, 0.96; 95% CI, 0.52–1.76). “Despite the lower percentage of women opting for or offered a vaginal delivery, and despite a higher emergency cesarean rate during vaginal breech birth, neonatal outcome within the planned vaginal birth group did not improve,” state the authors.1
Putting the results in absolute numbers
The investigators say that the 40% of Dutch women with breech presentation at term who still attempt vaginal birth do so without improved neonatal outcome; these deliveries generate a 10-fold higher fetal mortality rate compared with ECD. Further, no subgroup of women, when evaluating parity, onset of labor, type of breech presentation, and birthweight, could be identified with a low risk of poor neonatal outcome during planned vaginal delivery compared with ECD.1
Since the TBT, 1,692 more combined elective and emergency cesarean deliveries were performed annually, leading to five less neonatal deaths per year (number needed to treat, 338). If all women who still undergo planned vaginal birth receive ECD, 6,490 more ECDs would be performed, with 10 less neonatal deaths, 116 less neonates with low Apgar score, and 20 less neonates with birth trauma per year, according to the researchers.1
They suggest that clinicians use the results of this study when counseling women with a term breech presentation on mode of delivery. “To properly inform patients, a combination of risk presentation (absolute risks, relative risks and figures) is necessary to enable individual informed decision making.”1
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
Reference
- Vlemmix F, Bergenhenegouwen L, Schaaf JM, et al. Term breech deliveries in the Netherlands: did the increased cesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet Gynecol Scand. 2014;93:888–896.
Reference
- Vlemmix F, Bergenhenegouwen L, Schaaf JM, et al. Term breech deliveries in the Netherlands: did the increased cesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet Gynecol Scand. 2014;93:888–896.
ACOG issues guidelines for managing listeriosis during pregnancy
The first medical management guidelines for treating the bacteria listeria during pregnancy were recently released by the American College of Obstetricians and Gynecologists (ACOG).1
The new guidelines were developed in response to recent reports of recalls of listeria-contaminated food and concern because data show the incidence of listeriosis among pregnant women is approximately 13 times higher than in the general population.1 Maternal listeriosis can cause significant fetal and perinatal complications, including miscarriage, preterm labor, stillbirth, as well as neonatal listeriosis and neonatal death.2
“It is essential for ObGyns not only to be aware of the best ways to manage the care of a pregnant patient who has been exposed to listeria bacteria, but, just as important, to counsel pregnant women regarding how to avoid potential exposure,” said Jeffrey L. Ecker, MD, chair of the ACOG Committee on Obstetric Practice.2
Symptoms of listeriosis are similar to a flu-like infection and can include fever, muscle pain, backache, headache, and gastrointestinal symptoms, including diarrhea.2
The Committee Opinion offers management recommendations for three scenarios1:
- Asymptomatic women who have been exposed to listeria: No testing is necessary unless symptoms develop within 2 months of exposure. Listeriosis-related fetal surveillance is unnecessary.
- No fever, with mild symptoms consistent with listeriosis: A pregnant woman who has been exposed to a listeria-containing food and is displaying mild symptoms, but does not have a fever, does not require culture testing (although it may be done). If her blood is tested, the laboratory should be informed about the listeriosis threat so that the bacteria is not confused with a contaminant.
- Fever, with or without symptoms consistent with listeriosis: A pregnant woman who has been exposed and has a fever exceeding 100.6°F should undergo blood culture testing. Because results will not be available for several days, the Committee Opinion recommends simultaneous listeriosis treatment for the patient and surveillance of the fetus.
Preventive measures to avoid listeria exposure include not eating the following foods1:
- hot dogs, lunch meats, cold cuts served cold or heated to less than 165°F
- refrigerated pate and meat spreads
- refrigerated smoked seafood
- raw (unpasteurized) milk
- unpasteurized soft cheese (feta, queso blanco, Brie, blue-veined cheeses)
- unwashed raw produce (when eating raw fruits and vegetables, skin should be washed thoroughly in running tap water, even if it will be peeled or cut).
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
- American College of Obstetricians and Gynecologists. Committee Opinion. Management of pregnant women with presumptive exposure to Listeria monocytogenes [published online ahead of print August 5, 2014]. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Management-of-Pregnant-Women-With-Presumptive-Exposure-to-Listeria-monocytogenes. Accessed September 29, 2014.
- American College of Obstetricians and Gynecologists. Ob-Gyns address management of listeria during pregnancy [press release]. http://www.acog.org/About-ACOG/News-Room/News-Releases/2014/Ob-Gyns-Address-Management-of-Listeria-During-Pregnancy. Published August 6, 2014. Accessed September 29, 2014.
The first medical management guidelines for treating the bacteria listeria during pregnancy were recently released by the American College of Obstetricians and Gynecologists (ACOG).1
The new guidelines were developed in response to recent reports of recalls of listeria-contaminated food and concern because data show the incidence of listeriosis among pregnant women is approximately 13 times higher than in the general population.1 Maternal listeriosis can cause significant fetal and perinatal complications, including miscarriage, preterm labor, stillbirth, as well as neonatal listeriosis and neonatal death.2
“It is essential for ObGyns not only to be aware of the best ways to manage the care of a pregnant patient who has been exposed to listeria bacteria, but, just as important, to counsel pregnant women regarding how to avoid potential exposure,” said Jeffrey L. Ecker, MD, chair of the ACOG Committee on Obstetric Practice.2
Symptoms of listeriosis are similar to a flu-like infection and can include fever, muscle pain, backache, headache, and gastrointestinal symptoms, including diarrhea.2
The Committee Opinion offers management recommendations for three scenarios1:
- Asymptomatic women who have been exposed to listeria: No testing is necessary unless symptoms develop within 2 months of exposure. Listeriosis-related fetal surveillance is unnecessary.
- No fever, with mild symptoms consistent with listeriosis: A pregnant woman who has been exposed to a listeria-containing food and is displaying mild symptoms, but does not have a fever, does not require culture testing (although it may be done). If her blood is tested, the laboratory should be informed about the listeriosis threat so that the bacteria is not confused with a contaminant.
- Fever, with or without symptoms consistent with listeriosis: A pregnant woman who has been exposed and has a fever exceeding 100.6°F should undergo blood culture testing. Because results will not be available for several days, the Committee Opinion recommends simultaneous listeriosis treatment for the patient and surveillance of the fetus.
Preventive measures to avoid listeria exposure include not eating the following foods1:
- hot dogs, lunch meats, cold cuts served cold or heated to less than 165°F
- refrigerated pate and meat spreads
- refrigerated smoked seafood
- raw (unpasteurized) milk
- unpasteurized soft cheese (feta, queso blanco, Brie, blue-veined cheeses)
- unwashed raw produce (when eating raw fruits and vegetables, skin should be washed thoroughly in running tap water, even if it will be peeled or cut).
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
The first medical management guidelines for treating the bacteria listeria during pregnancy were recently released by the American College of Obstetricians and Gynecologists (ACOG).1
The new guidelines were developed in response to recent reports of recalls of listeria-contaminated food and concern because data show the incidence of listeriosis among pregnant women is approximately 13 times higher than in the general population.1 Maternal listeriosis can cause significant fetal and perinatal complications, including miscarriage, preterm labor, stillbirth, as well as neonatal listeriosis and neonatal death.2
“It is essential for ObGyns not only to be aware of the best ways to manage the care of a pregnant patient who has been exposed to listeria bacteria, but, just as important, to counsel pregnant women regarding how to avoid potential exposure,” said Jeffrey L. Ecker, MD, chair of the ACOG Committee on Obstetric Practice.2
Symptoms of listeriosis are similar to a flu-like infection and can include fever, muscle pain, backache, headache, and gastrointestinal symptoms, including diarrhea.2
The Committee Opinion offers management recommendations for three scenarios1:
- Asymptomatic women who have been exposed to listeria: No testing is necessary unless symptoms develop within 2 months of exposure. Listeriosis-related fetal surveillance is unnecessary.
- No fever, with mild symptoms consistent with listeriosis: A pregnant woman who has been exposed to a listeria-containing food and is displaying mild symptoms, but does not have a fever, does not require culture testing (although it may be done). If her blood is tested, the laboratory should be informed about the listeriosis threat so that the bacteria is not confused with a contaminant.
- Fever, with or without symptoms consistent with listeriosis: A pregnant woman who has been exposed and has a fever exceeding 100.6°F should undergo blood culture testing. Because results will not be available for several days, the Committee Opinion recommends simultaneous listeriosis treatment for the patient and surveillance of the fetus.
Preventive measures to avoid listeria exposure include not eating the following foods1:
- hot dogs, lunch meats, cold cuts served cold or heated to less than 165°F
- refrigerated pate and meat spreads
- refrigerated smoked seafood
- raw (unpasteurized) milk
- unpasteurized soft cheese (feta, queso blanco, Brie, blue-veined cheeses)
- unwashed raw produce (when eating raw fruits and vegetables, skin should be washed thoroughly in running tap water, even if it will be peeled or cut).
Share your thoughts on this news! Send your Letter to the Editor to [email protected]. Please include your name, and the city and state in which you practice.
- American College of Obstetricians and Gynecologists. Committee Opinion. Management of pregnant women with presumptive exposure to Listeria monocytogenes [published online ahead of print August 5, 2014]. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Management-of-Pregnant-Women-With-Presumptive-Exposure-to-Listeria-monocytogenes. Accessed September 29, 2014.
- American College of Obstetricians and Gynecologists. Ob-Gyns address management of listeria during pregnancy [press release]. http://www.acog.org/About-ACOG/News-Room/News-Releases/2014/Ob-Gyns-Address-Management-of-Listeria-During-Pregnancy. Published August 6, 2014. Accessed September 29, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion. Management of pregnant women with presumptive exposure to Listeria monocytogenes [published online ahead of print August 5, 2014]. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Management-of-Pregnant-Women-With-Presumptive-Exposure-to-Listeria-monocytogenes. Accessed September 29, 2014.
- American College of Obstetricians and Gynecologists. Ob-Gyns address management of listeria during pregnancy [press release]. http://www.acog.org/About-ACOG/News-Room/News-Releases/2014/Ob-Gyns-Address-Management-of-Listeria-During-Pregnancy. Published August 6, 2014. Accessed September 29, 2014.