User login
Prediction of Semitendinosus and Gracilis Tendon Lengths and Diameters for Double Bundle ACL Reconstruction
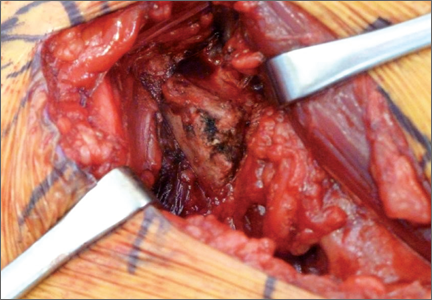
Low Velocity Gunshot Wounds Result in Significant Contamination Regardless of Ballistic Characteristics
Family or Career—Must We Choose?
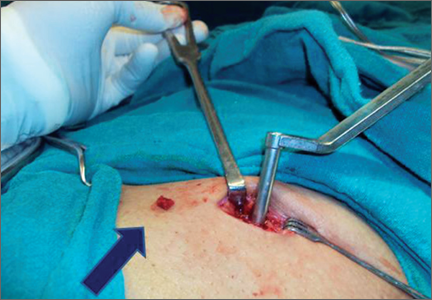
Minimally-Invasive Bone Graft Harvesting Technique Without Sophisticated Instruments
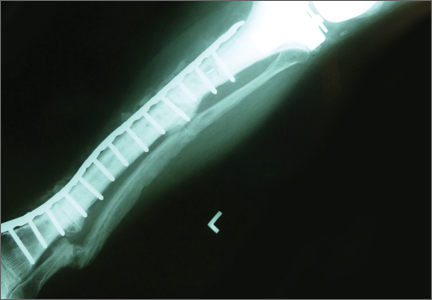
Total Knee Arthroplasty With Concurrent Femoral and Tibial Osteotomies in Osteogenesis Imperfecta
Symptomatic Hip Impingement Due to Exostosis Associated With Supra-Acetabular Pelvic External Fixator Pin
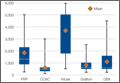
Cost Estimates of Biologic Implants Among Orthopedic Surgeons
All-Polyethylene Tibial Components in Octogenarians: Survivorship, Performance, and Cost
Children Are Not Small Adults
"Children are not small adults” is a common saying among pediatric care providers across all specialties, including pediatric orthopedics. In addition to obvious size differences, children have physical features that are different from those in adults, such as growth plates, increased ligamentous laxity, and different levels of cognitive ability and neuromuscular control. In addition, growth can lead to progression of deformities (neuromuscular disease) or can be used to correct deformities (remodeling of fractures). Awareness of these factors, as well as emotional and social issues, is critical to provide the best outcome to pediatric patients.
The past decade has led to tremendous advances in pediatric orthopedics, including the development of highly specialized children’s hospitals with comprehensive multispecialty clinics, the use of genetic testing, and the use of computer-assisted technologies for deformity-correction and intraoperative navigation. While tremendous advances have been made, one area that has been lagging is the
development of pediatric-specific orthopedic implants. This problem is multifactorial and not unique to pediatric orthopedics. Adult devices such as defibrillators, pacemakers, heart valves, dialysis catheters/ports, and orthopedic implants are commonly used in children in an off-label fashion. For example, up to 60% of procedures performed in pediatric interventional cardiology are off-label.1 Common
off-label uses in pediatric orthopedics involve the use of adult pedicle screws and trauma implants in skeletally immature patients.
Most experts say the biggest driver behind this lag is economics. The pediatric market is smaller than the adult market. Some pediatric conditions, such as genetic disorders, early onset scoliosis, and hip dysplasia are rare relative to adult musculoskeletal conditions such as osteoarthritis.
This makes it more difficult for companies to recover money spent on research and development. Probably the best example of this is in the joint arthroplasty market.
According to the CDC, in 2009, 676,000 and 327,000 total hip and knee replacements, respectively, were done in the US alone. This tremendous volume, and potential revenue for the manufacturers, has led to a host of innovations such as gender and activity-specific implants. An interesting contrast to this is the cast saw. Fracture care is one of the most common pediatric orthopedic procedures performed world-wide. Despite studies regarding cast saw complications,
including burns, patient/parental anxiety, and increased medico-legal risk when complications occur, little change has occurred to these devices since their invention by Dr. Homer Stryker in 1943.
In addition, it is becoming much more difficult and expensive to bring new products to market. Obtaining FDA approval usually requires large multicenter trials, which
are not possible given the rarity of some of the pediatric orthopedic conditions, as well as the reluctance of patients, parents, physicians, and institutions to enroll children in clinical trials. Some devices for rare conditions such as the VEPTR (vertical expandable prosthetic titanium rib) have been FDA-approved, but as a humanitarian device exemption.
In addition to off-label use, devices often are modified to provide a better fit. Some devices are available for children as a custom order, but they are not readily available when needed. In addition, only 30% of pediatric care in the US is provided in children’s hospitals where pediatric implants, if they even exist, as well as people experienced in their use, are most likely to be available.
To address this problem, Congress passed the Pediatric Device Safety and Improvement Act in 2007, which authorized the FDA to issue grants to stimulate the development of pediatric-specific devices. So far, approximately $11 million
has been awarded to 220 projects in various stages of completion across all areas of pediatric care, not just orthopedics. While a good first step, the overall amount spent is dwarfed by the amount spent on adults.
Despite these challenges, patient- and market-driven factors are increasing interest in the development of pediatric orthopedic devices. With increasing parental
demand for specialized pediatric care grows, so does the demand for pediatric-specific implants. Increased competition among device companies to be “full-service” to hospital systems has led to increased interest in developing pediatric-specific implants. While the implants themselves may not be profit leaders, their ability to make an implant company full-service to a hospital system may make it cost-effective, similar to the way retail companies use “loss leaders” to drive store traffic. Even now, there is only one pediatric specific orthopedic device company in
the marketplace.
Pediatric orthopedists have long recognized that children are not small adults, and it is time that the medical device manufacturers and regulatory agencies recognize it as well.
Reference
1. Sutherell JS, Hirsch R, Beekman RH 3rd. Pediatric interventional cardiology
in the United States is dependent on the off-label use of medical
devices. Congenit Heart Dis. 2010;5(1):2-7.
"Children are not small adults” is a common saying among pediatric care providers across all specialties, including pediatric orthopedics. In addition to obvious size differences, children have physical features that are different from those in adults, such as growth plates, increased ligamentous laxity, and different levels of cognitive ability and neuromuscular control. In addition, growth can lead to progression of deformities (neuromuscular disease) or can be used to correct deformities (remodeling of fractures). Awareness of these factors, as well as emotional and social issues, is critical to provide the best outcome to pediatric patients.
The past decade has led to tremendous advances in pediatric orthopedics, including the development of highly specialized children’s hospitals with comprehensive multispecialty clinics, the use of genetic testing, and the use of computer-assisted technologies for deformity-correction and intraoperative navigation. While tremendous advances have been made, one area that has been lagging is the
development of pediatric-specific orthopedic implants. This problem is multifactorial and not unique to pediatric orthopedics. Adult devices such as defibrillators, pacemakers, heart valves, dialysis catheters/ports, and orthopedic implants are commonly used in children in an off-label fashion. For example, up to 60% of procedures performed in pediatric interventional cardiology are off-label.1 Common
off-label uses in pediatric orthopedics involve the use of adult pedicle screws and trauma implants in skeletally immature patients.
Most experts say the biggest driver behind this lag is economics. The pediatric market is smaller than the adult market. Some pediatric conditions, such as genetic disorders, early onset scoliosis, and hip dysplasia are rare relative to adult musculoskeletal conditions such as osteoarthritis.
This makes it more difficult for companies to recover money spent on research and development. Probably the best example of this is in the joint arthroplasty market.
According to the CDC, in 2009, 676,000 and 327,000 total hip and knee replacements, respectively, were done in the US alone. This tremendous volume, and potential revenue for the manufacturers, has led to a host of innovations such as gender and activity-specific implants. An interesting contrast to this is the cast saw. Fracture care is one of the most common pediatric orthopedic procedures performed world-wide. Despite studies regarding cast saw complications,
including burns, patient/parental anxiety, and increased medico-legal risk when complications occur, little change has occurred to these devices since their invention by Dr. Homer Stryker in 1943.
In addition, it is becoming much more difficult and expensive to bring new products to market. Obtaining FDA approval usually requires large multicenter trials, which
are not possible given the rarity of some of the pediatric orthopedic conditions, as well as the reluctance of patients, parents, physicians, and institutions to enroll children in clinical trials. Some devices for rare conditions such as the VEPTR (vertical expandable prosthetic titanium rib) have been FDA-approved, but as a humanitarian device exemption.
In addition to off-label use, devices often are modified to provide a better fit. Some devices are available for children as a custom order, but they are not readily available when needed. In addition, only 30% of pediatric care in the US is provided in children’s hospitals where pediatric implants, if they even exist, as well as people experienced in their use, are most likely to be available.
To address this problem, Congress passed the Pediatric Device Safety and Improvement Act in 2007, which authorized the FDA to issue grants to stimulate the development of pediatric-specific devices. So far, approximately $11 million
has been awarded to 220 projects in various stages of completion across all areas of pediatric care, not just orthopedics. While a good first step, the overall amount spent is dwarfed by the amount spent on adults.
Despite these challenges, patient- and market-driven factors are increasing interest in the development of pediatric orthopedic devices. With increasing parental
demand for specialized pediatric care grows, so does the demand for pediatric-specific implants. Increased competition among device companies to be “full-service” to hospital systems has led to increased interest in developing pediatric-specific implants. While the implants themselves may not be profit leaders, their ability to make an implant company full-service to a hospital system may make it cost-effective, similar to the way retail companies use “loss leaders” to drive store traffic. Even now, there is only one pediatric specific orthopedic device company in
the marketplace.
Pediatric orthopedists have long recognized that children are not small adults, and it is time that the medical device manufacturers and regulatory agencies recognize it as well.
Reference
1. Sutherell JS, Hirsch R, Beekman RH 3rd. Pediatric interventional cardiology
in the United States is dependent on the off-label use of medical
devices. Congenit Heart Dis. 2010;5(1):2-7.
"Children are not small adults” is a common saying among pediatric care providers across all specialties, including pediatric orthopedics. In addition to obvious size differences, children have physical features that are different from those in adults, such as growth plates, increased ligamentous laxity, and different levels of cognitive ability and neuromuscular control. In addition, growth can lead to progression of deformities (neuromuscular disease) or can be used to correct deformities (remodeling of fractures). Awareness of these factors, as well as emotional and social issues, is critical to provide the best outcome to pediatric patients.
The past decade has led to tremendous advances in pediatric orthopedics, including the development of highly specialized children’s hospitals with comprehensive multispecialty clinics, the use of genetic testing, and the use of computer-assisted technologies for deformity-correction and intraoperative navigation. While tremendous advances have been made, one area that has been lagging is the
development of pediatric-specific orthopedic implants. This problem is multifactorial and not unique to pediatric orthopedics. Adult devices such as defibrillators, pacemakers, heart valves, dialysis catheters/ports, and orthopedic implants are commonly used in children in an off-label fashion. For example, up to 60% of procedures performed in pediatric interventional cardiology are off-label.1 Common
off-label uses in pediatric orthopedics involve the use of adult pedicle screws and trauma implants in skeletally immature patients.
Most experts say the biggest driver behind this lag is economics. The pediatric market is smaller than the adult market. Some pediatric conditions, such as genetic disorders, early onset scoliosis, and hip dysplasia are rare relative to adult musculoskeletal conditions such as osteoarthritis.
This makes it more difficult for companies to recover money spent on research and development. Probably the best example of this is in the joint arthroplasty market.
According to the CDC, in 2009, 676,000 and 327,000 total hip and knee replacements, respectively, were done in the US alone. This tremendous volume, and potential revenue for the manufacturers, has led to a host of innovations such as gender and activity-specific implants. An interesting contrast to this is the cast saw. Fracture care is one of the most common pediatric orthopedic procedures performed world-wide. Despite studies regarding cast saw complications,
including burns, patient/parental anxiety, and increased medico-legal risk when complications occur, little change has occurred to these devices since their invention by Dr. Homer Stryker in 1943.
In addition, it is becoming much more difficult and expensive to bring new products to market. Obtaining FDA approval usually requires large multicenter trials, which
are not possible given the rarity of some of the pediatric orthopedic conditions, as well as the reluctance of patients, parents, physicians, and institutions to enroll children in clinical trials. Some devices for rare conditions such as the VEPTR (vertical expandable prosthetic titanium rib) have been FDA-approved, but as a humanitarian device exemption.
In addition to off-label use, devices often are modified to provide a better fit. Some devices are available for children as a custom order, but they are not readily available when needed. In addition, only 30% of pediatric care in the US is provided in children’s hospitals where pediatric implants, if they even exist, as well as people experienced in their use, are most likely to be available.
To address this problem, Congress passed the Pediatric Device Safety and Improvement Act in 2007, which authorized the FDA to issue grants to stimulate the development of pediatric-specific devices. So far, approximately $11 million
has been awarded to 220 projects in various stages of completion across all areas of pediatric care, not just orthopedics. While a good first step, the overall amount spent is dwarfed by the amount spent on adults.
Despite these challenges, patient- and market-driven factors are increasing interest in the development of pediatric orthopedic devices. With increasing parental
demand for specialized pediatric care grows, so does the demand for pediatric-specific implants. Increased competition among device companies to be “full-service” to hospital systems has led to increased interest in developing pediatric-specific implants. While the implants themselves may not be profit leaders, their ability to make an implant company full-service to a hospital system may make it cost-effective, similar to the way retail companies use “loss leaders” to drive store traffic. Even now, there is only one pediatric specific orthopedic device company in
the marketplace.
Pediatric orthopedists have long recognized that children are not small adults, and it is time that the medical device manufacturers and regulatory agencies recognize it as well.
Reference
1. Sutherell JS, Hirsch R, Beekman RH 3rd. Pediatric interventional cardiology
in the United States is dependent on the off-label use of medical
devices. Congenit Heart Dis. 2010;5(1):2-7.