User login
Tennessee Hospitals Cut Costs While Improving Outcomes
HOT SPRINGS, VA. – A collaboration among 10 hospitals in Tennessee has produced a boost in quality of care while also saving millions of dollars.
The collaboration first got started in 2005, when the three initial participants – Erlanger Medical Center in Chattanooga, Vanderbilt University Medical Center in Nashville, and St. Francis Hospital–Memphis – took inspiration from the rollout of the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP), said Dr. Joseph B. Cofer, a professor of surgery at the University of Tennessee, Chattanooga.
A successful run so far has led BlueCross Blue Shield of Tennessee (which has bankrolled the operation) to extend its funding through 2012 for the 10 hospitals that are currently participating, said Dr. Cofer. And it made funds available for an additional 11 hospitals to join, which would bring the total to 21.
With data now complete for 2009 and 2010, the Tennessee Surgical Quality Collaborative reported that postoperative mortality was not statistically significantly different from the first year (2.32%, or 232/10,000) to the second year (2.38%, or 237/10,000).
However, significant declines in postoperative complications in five areas – acute renal failure (25% drop), graft/flap failure (60% drop), ventilation for more than 48 hours (15% drop), superficial incisional surgical-site infection (19% drop), and wound disruption (34% drop) – resulted in total savings of $4.47 million.
At the same time, increases in postoperative complications in three areas – urinary tract infection (42% rise), pneumonia (23% rise), and deep vein thrombosis (35% rise) – cost $2.1 million.
Overall, the savings were at least $2 million for the 10 participating hospitals, said Dr. Cofer. But that number reflects only a sampling of cases from the 10 hospitals; if all the cases had been included, "we can reliably say we probably avoided about $8 million in costs over this year," Dr. Cofer said.
"Why this happened, we don’t know," he added. It’s possible that just being part of the NSQIP process improves monitoring and outcomes.
The Tennessee collaborative is now identifying exemplar hospitals and "sending out teams to dissect how they did it so well," Dr. Cofer said. Then, those best practices will be disseminated to other hospitals in the collaborative.
The collaboration would not likely have been possible without the participation of BlueCross BlueShield of Tennessee. Dr. Cofer spearheaded the talks with the insurer, which began in 2006 and culminated in a three-way partnership among the Blues, the Tennessee chapter of the ACS, and the Tennessee Hospital Association. In 2008, the Blues announced that it was giving the collaboration $2.5 million over the next 3 years to fund the collaborative.
Another crucial element was the leadership committee, said Dr. Cofer. Of the seven committee members, four are surgeons, two are hospital CEOs, and one is a staff person from the Tennessee Hospital Association. Data cannot be released without permission of the committee, and, so far, specific data are not being shared.
Dr. J. David Richardson, a discussant and chairman of the NSQIP committee at ACS, said, "it takes a tremendous effort to put a group like this together," adding that "within the ACS, I think we’ve all been heartened by the initiative taken by the Tennessee chapter in developing this program." The ACS is looking to expand the program, particularly beyond Veterans Affairs hospitals, said Dr. Richardson, professor and vice chairman of surgery at the University of Louisville (Ky.). The collaborative model is a way to spread the cost, so it may entice more participants, he said.
"This is a provocative paper because it should provoke us to follow suit," Dr. Joseph J. Tepas III, professor of surgery at the University of Florida, Jacksonville, said in his discussion of the paper. "This report demonstrates that this engine of quality, fueled by real-time clinical data, produces results that are understandable to the nonphysician public."
He added that just participating in NSQIP likely improved the hospitals’ quality. "The power of NSQIP is, first, in its surveillance, and this is what’s so well demonstrated here," he said.
Dr. Tepas, Dr. Richardson, and several other discussants asked why there had been improvement in some clinical areas but not in others. Was this perhaps a change in surgical leadership, or – as Dr. Cofer suggested – the Hawthorne effect (that is, the tendency of outcomes to improve when participants – in this case, hospitals and surgeons – know they are being monitored)?
Lead author Dr. Oscar Guillamondegui had an answer: "There have been no real changes in leadership at any of these hospitals, but if you think about the cost of putting together a NSQIP program – other than for the large hospitals – for many of these hospitals, it’s a bottom-line item that’s not insubstantial," he said. "Most hospitals will push to have improvement of care just based on the fact they’re putting that kind of funding into a system," said Dr. Guillamondegui of the division of trauma and surgical critical care at Vanderbilt University Medical Center. He also surmised that the Hawthorne effect may have played a part.
Some outcomes got worse, likely because of natural variations, but also because NSQIP definitions are strict and include a 30-day window, he said. For instance, more than half of urinary tract infections happen outside the hospital, but if they occur within 30 days of admission, they fall within the NSQIP 30-day morbidity outcome window.
Going forward, sustaining such collaboratives could be difficult, said Dr. Guillamondegui. "If you have a weak surgeon champion, then the program does nothing," especially if data are not being shared with other surgeons or the hospital administration. "If your culture isn’t capable of sustaining this, it will fail."
Dr. Cofer, Dr. Tepas, and Dr. Guillamondegui reported no conflicts. Dr. Richardson chairs the ACS NSQIP committee.
HOT SPRINGS, VA. – A collaboration among 10 hospitals in Tennessee has produced a boost in quality of care while also saving millions of dollars.
The collaboration first got started in 2005, when the three initial participants – Erlanger Medical Center in Chattanooga, Vanderbilt University Medical Center in Nashville, and St. Francis Hospital–Memphis – took inspiration from the rollout of the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP), said Dr. Joseph B. Cofer, a professor of surgery at the University of Tennessee, Chattanooga.
A successful run so far has led BlueCross Blue Shield of Tennessee (which has bankrolled the operation) to extend its funding through 2012 for the 10 hospitals that are currently participating, said Dr. Cofer. And it made funds available for an additional 11 hospitals to join, which would bring the total to 21.
With data now complete for 2009 and 2010, the Tennessee Surgical Quality Collaborative reported that postoperative mortality was not statistically significantly different from the first year (2.32%, or 232/10,000) to the second year (2.38%, or 237/10,000).
However, significant declines in postoperative complications in five areas – acute renal failure (25% drop), graft/flap failure (60% drop), ventilation for more than 48 hours (15% drop), superficial incisional surgical-site infection (19% drop), and wound disruption (34% drop) – resulted in total savings of $4.47 million.
At the same time, increases in postoperative complications in three areas – urinary tract infection (42% rise), pneumonia (23% rise), and deep vein thrombosis (35% rise) – cost $2.1 million.
Overall, the savings were at least $2 million for the 10 participating hospitals, said Dr. Cofer. But that number reflects only a sampling of cases from the 10 hospitals; if all the cases had been included, "we can reliably say we probably avoided about $8 million in costs over this year," Dr. Cofer said.
"Why this happened, we don’t know," he added. It’s possible that just being part of the NSQIP process improves monitoring and outcomes.
The Tennessee collaborative is now identifying exemplar hospitals and "sending out teams to dissect how they did it so well," Dr. Cofer said. Then, those best practices will be disseminated to other hospitals in the collaborative.
The collaboration would not likely have been possible without the participation of BlueCross BlueShield of Tennessee. Dr. Cofer spearheaded the talks with the insurer, which began in 2006 and culminated in a three-way partnership among the Blues, the Tennessee chapter of the ACS, and the Tennessee Hospital Association. In 2008, the Blues announced that it was giving the collaboration $2.5 million over the next 3 years to fund the collaborative.
Another crucial element was the leadership committee, said Dr. Cofer. Of the seven committee members, four are surgeons, two are hospital CEOs, and one is a staff person from the Tennessee Hospital Association. Data cannot be released without permission of the committee, and, so far, specific data are not being shared.
Dr. J. David Richardson, a discussant and chairman of the NSQIP committee at ACS, said, "it takes a tremendous effort to put a group like this together," adding that "within the ACS, I think we’ve all been heartened by the initiative taken by the Tennessee chapter in developing this program." The ACS is looking to expand the program, particularly beyond Veterans Affairs hospitals, said Dr. Richardson, professor and vice chairman of surgery at the University of Louisville (Ky.). The collaborative model is a way to spread the cost, so it may entice more participants, he said.
"This is a provocative paper because it should provoke us to follow suit," Dr. Joseph J. Tepas III, professor of surgery at the University of Florida, Jacksonville, said in his discussion of the paper. "This report demonstrates that this engine of quality, fueled by real-time clinical data, produces results that are understandable to the nonphysician public."
He added that just participating in NSQIP likely improved the hospitals’ quality. "The power of NSQIP is, first, in its surveillance, and this is what’s so well demonstrated here," he said.
Dr. Tepas, Dr. Richardson, and several other discussants asked why there had been improvement in some clinical areas but not in others. Was this perhaps a change in surgical leadership, or – as Dr. Cofer suggested – the Hawthorne effect (that is, the tendency of outcomes to improve when participants – in this case, hospitals and surgeons – know they are being monitored)?
Lead author Dr. Oscar Guillamondegui had an answer: "There have been no real changes in leadership at any of these hospitals, but if you think about the cost of putting together a NSQIP program – other than for the large hospitals – for many of these hospitals, it’s a bottom-line item that’s not insubstantial," he said. "Most hospitals will push to have improvement of care just based on the fact they’re putting that kind of funding into a system," said Dr. Guillamondegui of the division of trauma and surgical critical care at Vanderbilt University Medical Center. He also surmised that the Hawthorne effect may have played a part.
Some outcomes got worse, likely because of natural variations, but also because NSQIP definitions are strict and include a 30-day window, he said. For instance, more than half of urinary tract infections happen outside the hospital, but if they occur within 30 days of admission, they fall within the NSQIP 30-day morbidity outcome window.
Going forward, sustaining such collaboratives could be difficult, said Dr. Guillamondegui. "If you have a weak surgeon champion, then the program does nothing," especially if data are not being shared with other surgeons or the hospital administration. "If your culture isn’t capable of sustaining this, it will fail."
Dr. Cofer, Dr. Tepas, and Dr. Guillamondegui reported no conflicts. Dr. Richardson chairs the ACS NSQIP committee.
HOT SPRINGS, VA. – A collaboration among 10 hospitals in Tennessee has produced a boost in quality of care while also saving millions of dollars.
The collaboration first got started in 2005, when the three initial participants – Erlanger Medical Center in Chattanooga, Vanderbilt University Medical Center in Nashville, and St. Francis Hospital–Memphis – took inspiration from the rollout of the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP), said Dr. Joseph B. Cofer, a professor of surgery at the University of Tennessee, Chattanooga.
A successful run so far has led BlueCross Blue Shield of Tennessee (which has bankrolled the operation) to extend its funding through 2012 for the 10 hospitals that are currently participating, said Dr. Cofer. And it made funds available for an additional 11 hospitals to join, which would bring the total to 21.
With data now complete for 2009 and 2010, the Tennessee Surgical Quality Collaborative reported that postoperative mortality was not statistically significantly different from the first year (2.32%, or 232/10,000) to the second year (2.38%, or 237/10,000).
However, significant declines in postoperative complications in five areas – acute renal failure (25% drop), graft/flap failure (60% drop), ventilation for more than 48 hours (15% drop), superficial incisional surgical-site infection (19% drop), and wound disruption (34% drop) – resulted in total savings of $4.47 million.
At the same time, increases in postoperative complications in three areas – urinary tract infection (42% rise), pneumonia (23% rise), and deep vein thrombosis (35% rise) – cost $2.1 million.
Overall, the savings were at least $2 million for the 10 participating hospitals, said Dr. Cofer. But that number reflects only a sampling of cases from the 10 hospitals; if all the cases had been included, "we can reliably say we probably avoided about $8 million in costs over this year," Dr. Cofer said.
"Why this happened, we don’t know," he added. It’s possible that just being part of the NSQIP process improves monitoring and outcomes.
The Tennessee collaborative is now identifying exemplar hospitals and "sending out teams to dissect how they did it so well," Dr. Cofer said. Then, those best practices will be disseminated to other hospitals in the collaborative.
The collaboration would not likely have been possible without the participation of BlueCross BlueShield of Tennessee. Dr. Cofer spearheaded the talks with the insurer, which began in 2006 and culminated in a three-way partnership among the Blues, the Tennessee chapter of the ACS, and the Tennessee Hospital Association. In 2008, the Blues announced that it was giving the collaboration $2.5 million over the next 3 years to fund the collaborative.
Another crucial element was the leadership committee, said Dr. Cofer. Of the seven committee members, four are surgeons, two are hospital CEOs, and one is a staff person from the Tennessee Hospital Association. Data cannot be released without permission of the committee, and, so far, specific data are not being shared.
Dr. J. David Richardson, a discussant and chairman of the NSQIP committee at ACS, said, "it takes a tremendous effort to put a group like this together," adding that "within the ACS, I think we’ve all been heartened by the initiative taken by the Tennessee chapter in developing this program." The ACS is looking to expand the program, particularly beyond Veterans Affairs hospitals, said Dr. Richardson, professor and vice chairman of surgery at the University of Louisville (Ky.). The collaborative model is a way to spread the cost, so it may entice more participants, he said.
"This is a provocative paper because it should provoke us to follow suit," Dr. Joseph J. Tepas III, professor of surgery at the University of Florida, Jacksonville, said in his discussion of the paper. "This report demonstrates that this engine of quality, fueled by real-time clinical data, produces results that are understandable to the nonphysician public."
He added that just participating in NSQIP likely improved the hospitals’ quality. "The power of NSQIP is, first, in its surveillance, and this is what’s so well demonstrated here," he said.
Dr. Tepas, Dr. Richardson, and several other discussants asked why there had been improvement in some clinical areas but not in others. Was this perhaps a change in surgical leadership, or – as Dr. Cofer suggested – the Hawthorne effect (that is, the tendency of outcomes to improve when participants – in this case, hospitals and surgeons – know they are being monitored)?
Lead author Dr. Oscar Guillamondegui had an answer: "There have been no real changes in leadership at any of these hospitals, but if you think about the cost of putting together a NSQIP program – other than for the large hospitals – for many of these hospitals, it’s a bottom-line item that’s not insubstantial," he said. "Most hospitals will push to have improvement of care just based on the fact they’re putting that kind of funding into a system," said Dr. Guillamondegui of the division of trauma and surgical critical care at Vanderbilt University Medical Center. He also surmised that the Hawthorne effect may have played a part.
Some outcomes got worse, likely because of natural variations, but also because NSQIP definitions are strict and include a 30-day window, he said. For instance, more than half of urinary tract infections happen outside the hospital, but if they occur within 30 days of admission, they fall within the NSQIP 30-day morbidity outcome window.
Going forward, sustaining such collaboratives could be difficult, said Dr. Guillamondegui. "If you have a weak surgeon champion, then the program does nothing," especially if data are not being shared with other surgeons or the hospital administration. "If your culture isn’t capable of sustaining this, it will fail."
Dr. Cofer, Dr. Tepas, and Dr. Guillamondegui reported no conflicts. Dr. Richardson chairs the ACS NSQIP committee.
FROM THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: The Tennessee Surgical Quality Collaborative saw significant improvements in some patient outcomes, and saved as much as $8 million in its first year.
Data Source: Data collected from the 10 hospitals participating in the collaborative.
Disclosures: Dr. Cofer, Dr. Tepas, and Dr. Guillamondegui reported no conflicts. Dr. Richardson chairs the ACS NSQIP committee.
Iron Deficiency Anemia 'Unintended Consequence' of Gastric Bypass
SAN DIEGO – About one-quarter of patients referred to a private hematology practice had iron deficiency associated with gastric bypass surgery.
In addition, 57% demonstrated symptoms of pica syndrome – a craving for and compulsive eating of non-food substances such as ice and starch.
"As morbid obesity has become a large problem in this country and more and more people are undergoing gastric bypass surgery, iron deficiency anemia is an unintended consequence," Dr. Thomas A. Bensinger said at the annual meeting of the American Society of Hematology. "Some of these patients get very severely anemic."
Dr. Bensinger and his associates at Maryland Oncology Hematology in Greenbelt reviewed the medical records of 300 adults referred to the practice between March and November of 2010 with a diagnosis of anemia. Of the total, 130 demonstrated iron deficiency anemia after undergoing laboratory studies that included complete blood count, ferritin, iron/total iron-binding capacity, reticulocyte count and review of the peripheral blood film.
Of the 130 patients, 122 (94%) were women, 4 of whom were pregnant. Heavy menstrual bleeding was the most common cause of iron deficiency anemia (62%), followed by gastric bypass surgery (24%), gastrointestinal abnormalities (6%), and heavy menstrual bleeding associated with the presence of uterine fibroid (5%). In addition, 12% of patients had both heavy menstrual bleeding and had undergone gastric bypass surgery. The remaining 3% of patients were male.
More than half of patients (57%) demonstrated symptoms of pica syndrome, primarily the urge to eat ice. Two patients reported an urge to eat toilet paper while one patient reported eating leaves that were stripped from a plant in her garden. Such symptoms "were often not reported by the patient unless the patient was questioned in detail with the exception of a small subset of patients who had performed an internet search and found pica for ice to be associated with iron deficiency anemia," Dr. Bensinger said.
Pica syndrome symptoms typically resolved within 7-21 days of intravenous iron administration. "I speculate that the craving for ice is related to enzymes that are in the oral cavity in the mucosa," he said. "They get iron depleted and somehow the ice makes them feel better. When you give them the iron, those enzymes get repleted. It’s a very interesting phenomenon. Some of our patients know when they start to get iron deficient again because they realize they’re eating ice."
The study’s overall findings underscore the importance of paying close attention to key indicators of iron deficiency anemia, including low mean corpuscular volume and various forms of pica syndrome.
"You have to keep paying attention to the causes of anemia," he said.
Dr. Bensinger reported having no relevant financial disclosures.
SAN DIEGO – About one-quarter of patients referred to a private hematology practice had iron deficiency associated with gastric bypass surgery.
In addition, 57% demonstrated symptoms of pica syndrome – a craving for and compulsive eating of non-food substances such as ice and starch.
"As morbid obesity has become a large problem in this country and more and more people are undergoing gastric bypass surgery, iron deficiency anemia is an unintended consequence," Dr. Thomas A. Bensinger said at the annual meeting of the American Society of Hematology. "Some of these patients get very severely anemic."
Dr. Bensinger and his associates at Maryland Oncology Hematology in Greenbelt reviewed the medical records of 300 adults referred to the practice between March and November of 2010 with a diagnosis of anemia. Of the total, 130 demonstrated iron deficiency anemia after undergoing laboratory studies that included complete blood count, ferritin, iron/total iron-binding capacity, reticulocyte count and review of the peripheral blood film.
Of the 130 patients, 122 (94%) were women, 4 of whom were pregnant. Heavy menstrual bleeding was the most common cause of iron deficiency anemia (62%), followed by gastric bypass surgery (24%), gastrointestinal abnormalities (6%), and heavy menstrual bleeding associated with the presence of uterine fibroid (5%). In addition, 12% of patients had both heavy menstrual bleeding and had undergone gastric bypass surgery. The remaining 3% of patients were male.
More than half of patients (57%) demonstrated symptoms of pica syndrome, primarily the urge to eat ice. Two patients reported an urge to eat toilet paper while one patient reported eating leaves that were stripped from a plant in her garden. Such symptoms "were often not reported by the patient unless the patient was questioned in detail with the exception of a small subset of patients who had performed an internet search and found pica for ice to be associated with iron deficiency anemia," Dr. Bensinger said.
Pica syndrome symptoms typically resolved within 7-21 days of intravenous iron administration. "I speculate that the craving for ice is related to enzymes that are in the oral cavity in the mucosa," he said. "They get iron depleted and somehow the ice makes them feel better. When you give them the iron, those enzymes get repleted. It’s a very interesting phenomenon. Some of our patients know when they start to get iron deficient again because they realize they’re eating ice."
The study’s overall findings underscore the importance of paying close attention to key indicators of iron deficiency anemia, including low mean corpuscular volume and various forms of pica syndrome.
"You have to keep paying attention to the causes of anemia," he said.
Dr. Bensinger reported having no relevant financial disclosures.
SAN DIEGO – About one-quarter of patients referred to a private hematology practice had iron deficiency associated with gastric bypass surgery.
In addition, 57% demonstrated symptoms of pica syndrome – a craving for and compulsive eating of non-food substances such as ice and starch.
"As morbid obesity has become a large problem in this country and more and more people are undergoing gastric bypass surgery, iron deficiency anemia is an unintended consequence," Dr. Thomas A. Bensinger said at the annual meeting of the American Society of Hematology. "Some of these patients get very severely anemic."
Dr. Bensinger and his associates at Maryland Oncology Hematology in Greenbelt reviewed the medical records of 300 adults referred to the practice between March and November of 2010 with a diagnosis of anemia. Of the total, 130 demonstrated iron deficiency anemia after undergoing laboratory studies that included complete blood count, ferritin, iron/total iron-binding capacity, reticulocyte count and review of the peripheral blood film.
Of the 130 patients, 122 (94%) were women, 4 of whom were pregnant. Heavy menstrual bleeding was the most common cause of iron deficiency anemia (62%), followed by gastric bypass surgery (24%), gastrointestinal abnormalities (6%), and heavy menstrual bleeding associated with the presence of uterine fibroid (5%). In addition, 12% of patients had both heavy menstrual bleeding and had undergone gastric bypass surgery. The remaining 3% of patients were male.
More than half of patients (57%) demonstrated symptoms of pica syndrome, primarily the urge to eat ice. Two patients reported an urge to eat toilet paper while one patient reported eating leaves that were stripped from a plant in her garden. Such symptoms "were often not reported by the patient unless the patient was questioned in detail with the exception of a small subset of patients who had performed an internet search and found pica for ice to be associated with iron deficiency anemia," Dr. Bensinger said.
Pica syndrome symptoms typically resolved within 7-21 days of intravenous iron administration. "I speculate that the craving for ice is related to enzymes that are in the oral cavity in the mucosa," he said. "They get iron depleted and somehow the ice makes them feel better. When you give them the iron, those enzymes get repleted. It’s a very interesting phenomenon. Some of our patients know when they start to get iron deficient again because they realize they’re eating ice."
The study’s overall findings underscore the importance of paying close attention to key indicators of iron deficiency anemia, including low mean corpuscular volume and various forms of pica syndrome.
"You have to keep paying attention to the causes of anemia," he said.
Dr. Bensinger reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY
Major Finding: Gastric bypass surgery was determined to be the cause of iron deficiency anemia in 24% of cases.
Data Source: A study of 130 patients referred to a private hematology practice who, following referral, demonstrated iron deficiency anemia after numerous laboratory studies.
Disclosures: Dr. Bensinger said that he had no relevant financial disclosures.
Low-Volume Transfusion Safe for Some Elderly Patients
Elderly hip surgery patients with cardiovascular disease do equally well whether they receive transfusions to maintain a hemoglobin level of 8 g/dL or more than 10 g/dL, a randomized trial has found.
Neither the restrictive nor the liberal transfusion protocol significantly altered the primary outcomes of mortality or functional status, or any of the prespecified secondary outcomes, Dr. Jeffrey L. Carson and his colleagues wrote in the Dec. 14 issue of the New England Journal of Medicine.
"Our findings suggest that it is reasonable to withhold transfusion in patients who have undergone surgery in the absence of symptoms of anemia or a decline in the hemoglobin level below 8 g/dL, even in elderly patients with underlying cardiovascular disease or risk factors," Dr. Carson, of the University of Medicine and Dentistry of New Jersey, Piscataway, and his coauthors wrote (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMoa1012452]).
The investigators randomized 2,016 patients undergoing hip fracture surgery to either a liberal or restrictive transfusion protocol. The liberal protocol called for 1 unit of packed red cells and additional blood to maintain a hemoglobin level of more than 10 g/dL, whereas the restrictive one called for transfusions at the physician’s discretion or when hemoglobin levels fell to below 8 g/dL.
The study’s primary end points were death or an inability to walk 10 feet without assistance by 60 days after surgery. The secondary outcomes were in-hospital heart attack, unstable angina, or death for any reason.
The patients’ mean age was 82 years; 63% had cardiovascular disease. Women made up 75.2% of the liberal strategy group and 76.3% of the restrictive group. Postoperative hemoglobin before transfusion was 1.3 g/dL higher in the liberal protocol group than in the restrictive group – a significant difference.
Those in the liberal group also received significantly more blood than did those in the restrictive group (median 2 vs. 0 units). A total of 59% of patients in the restrictive group did not receive any blood, compared with only 3% in the liberal group.
Despite the differences in transfusion volume, the study found no significant differences in any primary or secondary outcomes. The 60-day rate of mortality or the inability to walk 10 feet unassisted was 35% in each group. At 60 days, 8% of the liberal protocol group and 7% of the restrictive group had died, a nonsignificant 1% absolute risk reduction.
Nor were the combined secondary end points significantly different. In-hospital heart attack, unstable angina, or death within 30 days occurred in 4% of the restrictive group and in 5% of the liberal group. There were no significant differences in adverse events or length of hospital stay.
Men in the liberal protocol group were significantly more likely than women to achieve the primary end point (odds ratio, 1.45 vs. 0.74). The investigators said this was an unexpected finding that could have been due to chance. Interactions based on age, race, or cardiovascular disease were not significant.
FOCUS (Transfusion Trigger Trial for Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair) was sponsored by the National Institutes of Health. Dr. Carson reported that he had received NIH funding for the study. Two other authors reported multiple financial relationships with pharmaceutical and medical device companies.
FOCUS should give some reassurance that a more restrictive postsurgical transfusion protocol is a reasonable option for elderly patents at risk for cardiovascular events, Paul J. Barr, Ph.D., and Dr. Karen E.M. Bailie wrote in an accompanying editorial (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMe111087]).
Such a strategy not only conserves the limited blood supply, but helps protect these patients from the hazards of transfusion, they wrote.
"Even though red-cell transfusion is an accepted and widely used intervention, questions regarding which patients should receive transfusions and under what circumstances continue to spark debate. Meanwhile, concern about potential risks of blood transfusion and the costs of maintaining an adequate and safe blood supply have heightened interest in strategies to reduce the risk of red-cell transfusions."
FOCUS provides some insight into the matter for one high-risk group: elderly patients with cardiovascular disease or risk factors who undergo hip fracture surgery. "The study population is an important one in which to pose this question, since such patients are likely to be transfused because of surgical blood loss and their age, and it is plausible that they may be compromised at lower hemoglobin levels."
The trial was well conducted and had excellent statistical power, noted Dr. Barr and Dr. Bailie. But although statistically significant, the small between-group hemoglobin difference (1 g/dL) might have not been clinically relevant.
"This difference may not have been clinically significant in this group of elderly patients and may, therefore, have contributed to the lack of detectable difference in the primary outcome between the groups."
The authors cautioned, however, against applying the trial’s positive results to all patients similar to those in the FOCUS study. Despite the apparent advantages of receiving less blood, "the risks of under-transfusion should not be overlooked. The decision to transfuse should be guided by an assessment of individual patients on the basis of a combination of signs, symptoms, and laboratory measures, and not by a single hemoglobin measure."
Dr. Barr is from Queen’s University Belfast, Ireland. Dr. Barrie is from the West of Scotland Blood Transfusion Center, Glasgow. Neither disclosed any financial conflicts with the work.
FOCUS should give some reassurance that a more restrictive postsurgical transfusion protocol is a reasonable option for elderly patents at risk for cardiovascular events, Paul J. Barr, Ph.D., and Dr. Karen E.M. Bailie wrote in an accompanying editorial (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMe111087]).
Such a strategy not only conserves the limited blood supply, but helps protect these patients from the hazards of transfusion, they wrote.
"Even though red-cell transfusion is an accepted and widely used intervention, questions regarding which patients should receive transfusions and under what circumstances continue to spark debate. Meanwhile, concern about potential risks of blood transfusion and the costs of maintaining an adequate and safe blood supply have heightened interest in strategies to reduce the risk of red-cell transfusions."
FOCUS provides some insight into the matter for one high-risk group: elderly patients with cardiovascular disease or risk factors who undergo hip fracture surgery. "The study population is an important one in which to pose this question, since such patients are likely to be transfused because of surgical blood loss and their age, and it is plausible that they may be compromised at lower hemoglobin levels."
The trial was well conducted and had excellent statistical power, noted Dr. Barr and Dr. Bailie. But although statistically significant, the small between-group hemoglobin difference (1 g/dL) might have not been clinically relevant.
"This difference may not have been clinically significant in this group of elderly patients and may, therefore, have contributed to the lack of detectable difference in the primary outcome between the groups."
The authors cautioned, however, against applying the trial’s positive results to all patients similar to those in the FOCUS study. Despite the apparent advantages of receiving less blood, "the risks of under-transfusion should not be overlooked. The decision to transfuse should be guided by an assessment of individual patients on the basis of a combination of signs, symptoms, and laboratory measures, and not by a single hemoglobin measure."
Dr. Barr is from Queen’s University Belfast, Ireland. Dr. Barrie is from the West of Scotland Blood Transfusion Center, Glasgow. Neither disclosed any financial conflicts with the work.
FOCUS should give some reassurance that a more restrictive postsurgical transfusion protocol is a reasonable option for elderly patents at risk for cardiovascular events, Paul J. Barr, Ph.D., and Dr. Karen E.M. Bailie wrote in an accompanying editorial (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMe111087]).
Such a strategy not only conserves the limited blood supply, but helps protect these patients from the hazards of transfusion, they wrote.
"Even though red-cell transfusion is an accepted and widely used intervention, questions regarding which patients should receive transfusions and under what circumstances continue to spark debate. Meanwhile, concern about potential risks of blood transfusion and the costs of maintaining an adequate and safe blood supply have heightened interest in strategies to reduce the risk of red-cell transfusions."
FOCUS provides some insight into the matter for one high-risk group: elderly patients with cardiovascular disease or risk factors who undergo hip fracture surgery. "The study population is an important one in which to pose this question, since such patients are likely to be transfused because of surgical blood loss and their age, and it is plausible that they may be compromised at lower hemoglobin levels."
The trial was well conducted and had excellent statistical power, noted Dr. Barr and Dr. Bailie. But although statistically significant, the small between-group hemoglobin difference (1 g/dL) might have not been clinically relevant.
"This difference may not have been clinically significant in this group of elderly patients and may, therefore, have contributed to the lack of detectable difference in the primary outcome between the groups."
The authors cautioned, however, against applying the trial’s positive results to all patients similar to those in the FOCUS study. Despite the apparent advantages of receiving less blood, "the risks of under-transfusion should not be overlooked. The decision to transfuse should be guided by an assessment of individual patients on the basis of a combination of signs, symptoms, and laboratory measures, and not by a single hemoglobin measure."
Dr. Barr is from Queen’s University Belfast, Ireland. Dr. Barrie is from the West of Scotland Blood Transfusion Center, Glasgow. Neither disclosed any financial conflicts with the work.
Elderly hip surgery patients with cardiovascular disease do equally well whether they receive transfusions to maintain a hemoglobin level of 8 g/dL or more than 10 g/dL, a randomized trial has found.
Neither the restrictive nor the liberal transfusion protocol significantly altered the primary outcomes of mortality or functional status, or any of the prespecified secondary outcomes, Dr. Jeffrey L. Carson and his colleagues wrote in the Dec. 14 issue of the New England Journal of Medicine.
"Our findings suggest that it is reasonable to withhold transfusion in patients who have undergone surgery in the absence of symptoms of anemia or a decline in the hemoglobin level below 8 g/dL, even in elderly patients with underlying cardiovascular disease or risk factors," Dr. Carson, of the University of Medicine and Dentistry of New Jersey, Piscataway, and his coauthors wrote (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMoa1012452]).
The investigators randomized 2,016 patients undergoing hip fracture surgery to either a liberal or restrictive transfusion protocol. The liberal protocol called for 1 unit of packed red cells and additional blood to maintain a hemoglobin level of more than 10 g/dL, whereas the restrictive one called for transfusions at the physician’s discretion or when hemoglobin levels fell to below 8 g/dL.
The study’s primary end points were death or an inability to walk 10 feet without assistance by 60 days after surgery. The secondary outcomes were in-hospital heart attack, unstable angina, or death for any reason.
The patients’ mean age was 82 years; 63% had cardiovascular disease. Women made up 75.2% of the liberal strategy group and 76.3% of the restrictive group. Postoperative hemoglobin before transfusion was 1.3 g/dL higher in the liberal protocol group than in the restrictive group – a significant difference.
Those in the liberal group also received significantly more blood than did those in the restrictive group (median 2 vs. 0 units). A total of 59% of patients in the restrictive group did not receive any blood, compared with only 3% in the liberal group.
Despite the differences in transfusion volume, the study found no significant differences in any primary or secondary outcomes. The 60-day rate of mortality or the inability to walk 10 feet unassisted was 35% in each group. At 60 days, 8% of the liberal protocol group and 7% of the restrictive group had died, a nonsignificant 1% absolute risk reduction.
Nor were the combined secondary end points significantly different. In-hospital heart attack, unstable angina, or death within 30 days occurred in 4% of the restrictive group and in 5% of the liberal group. There were no significant differences in adverse events or length of hospital stay.
Men in the liberal protocol group were significantly more likely than women to achieve the primary end point (odds ratio, 1.45 vs. 0.74). The investigators said this was an unexpected finding that could have been due to chance. Interactions based on age, race, or cardiovascular disease were not significant.
FOCUS (Transfusion Trigger Trial for Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair) was sponsored by the National Institutes of Health. Dr. Carson reported that he had received NIH funding for the study. Two other authors reported multiple financial relationships with pharmaceutical and medical device companies.
Elderly hip surgery patients with cardiovascular disease do equally well whether they receive transfusions to maintain a hemoglobin level of 8 g/dL or more than 10 g/dL, a randomized trial has found.
Neither the restrictive nor the liberal transfusion protocol significantly altered the primary outcomes of mortality or functional status, or any of the prespecified secondary outcomes, Dr. Jeffrey L. Carson and his colleagues wrote in the Dec. 14 issue of the New England Journal of Medicine.
"Our findings suggest that it is reasonable to withhold transfusion in patients who have undergone surgery in the absence of symptoms of anemia or a decline in the hemoglobin level below 8 g/dL, even in elderly patients with underlying cardiovascular disease or risk factors," Dr. Carson, of the University of Medicine and Dentistry of New Jersey, Piscataway, and his coauthors wrote (N. Engl. J. Med. 2011 Dec. 14 [doi:10.1056/NEJMoa1012452]).
The investigators randomized 2,016 patients undergoing hip fracture surgery to either a liberal or restrictive transfusion protocol. The liberal protocol called for 1 unit of packed red cells and additional blood to maintain a hemoglobin level of more than 10 g/dL, whereas the restrictive one called for transfusions at the physician’s discretion or when hemoglobin levels fell to below 8 g/dL.
The study’s primary end points were death or an inability to walk 10 feet without assistance by 60 days after surgery. The secondary outcomes were in-hospital heart attack, unstable angina, or death for any reason.
The patients’ mean age was 82 years; 63% had cardiovascular disease. Women made up 75.2% of the liberal strategy group and 76.3% of the restrictive group. Postoperative hemoglobin before transfusion was 1.3 g/dL higher in the liberal protocol group than in the restrictive group – a significant difference.
Those in the liberal group also received significantly more blood than did those in the restrictive group (median 2 vs. 0 units). A total of 59% of patients in the restrictive group did not receive any blood, compared with only 3% in the liberal group.
Despite the differences in transfusion volume, the study found no significant differences in any primary or secondary outcomes. The 60-day rate of mortality or the inability to walk 10 feet unassisted was 35% in each group. At 60 days, 8% of the liberal protocol group and 7% of the restrictive group had died, a nonsignificant 1% absolute risk reduction.
Nor were the combined secondary end points significantly different. In-hospital heart attack, unstable angina, or death within 30 days occurred in 4% of the restrictive group and in 5% of the liberal group. There were no significant differences in adverse events or length of hospital stay.
Men in the liberal protocol group were significantly more likely than women to achieve the primary end point (odds ratio, 1.45 vs. 0.74). The investigators said this was an unexpected finding that could have been due to chance. Interactions based on age, race, or cardiovascular disease were not significant.
FOCUS (Transfusion Trigger Trial for Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair) was sponsored by the National Institutes of Health. Dr. Carson reported that he had received NIH funding for the study. Two other authors reported multiple financial relationships with pharmaceutical and medical device companies.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: Among 2,016 elderly patients undergoing hip fracture surgery, clinical end points did not vary between those in a restricted transfusion protocol and those in a liberal transfusion protocol. Both groups had a 35% rate of death or inability to ambulate unassisted.
Data Source: A randomized study comparing two transfusion triggers: a hemoglobin drop to 8 g/dL or maintaining the hemoglobin at 10 g/dL.
Disclosures: FOCUS (Transfusion Trigger Trial for Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair) was sponsored by the National Institutes of Health. Dr. Carson reported that he had received NIH funding for the study. Two other authors reported multiple financial relationships with pharmaceutical and medical device companies.
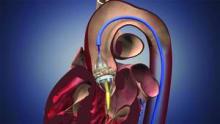
New-Onset AF Seen in One-Third of TAVI Patients
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Major Finding: NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% (odds ratio 4.79) in those who did not experience NOAF; the rate was 15.9% vs. 3.2% at 12 months (odds ratio 5.0).
Data Source: A prospective study of 138 patients undergoing TAVI.
Disclosures: Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed that they have consulted for Edwards Lifesciences Inc., and/or St. Jude Medical.
Aspirin Reduces Risk of Recurrent Blood Clots
SAN DIEGO – Aspirin reduced the risk of recurrent symptomatic venous thromboembolism by about 40% when given over a 2-year period following 6-12 months of warfarin therapy, with no apparent increase in major bleeding.
The findings, presented during a press briefing at the annual meeting of the American Society of Hematology, suggest that aspirin is a valid alternative to oral anticoagulants in the extended treatment of venous thromboembolism (VTE).
"This has great implications for clinical practice because many patients on anticoagulant treatment after a first-ever VTE are stopped after the initial 6 months of therapy and then they receive nothing for secondary prevention," lead author Dr. Cecilia Becattini, an internist in the stroke unit at the University of Perugia (Italy), said in an interview. "Maybe aspirin is a great opportunity [for VTE prevention] instead of nothing, because warfarin has the complication of major bleeding."
For the multicenter study known as WARFASA, 402 patients with a first-ever unprovoked VTE who had completed 6-12 months of oral anticoagulant treatment were randomized to receive aspirin 100 mg daily (aspirin group) or placebo for at least 2 years (placebo group).
The primary efficacy outcome was objectively confirmed recurrent symptomatic VTE and VTE-related death. Clinically relevant (major and nonmajor) bleeding were the main safety outcomes. Bleeding was considered major if it was fatal, occurred in a critical organ, or was associated with a decrease in hemoglobin of greater than 2.0 g/dL or led to a transfusion of two units or greater of whole blood or red cells.
The mean age of patients was 64 years and 56% were male. Of the 402 patients, 205 were randomized to the aspirin group while 197 were randomized to the placebo group. During the study period, which was a mean 25 months, Dr. Becattini reported that a VTE recurrence occurred in 28 patients in the aspirin group (6.6% per patient-year) and in 43 patients in the placebo group (11.0% per patient-year). This translated into a hazard ratio of 0.58.
During the on-treatment study period, which was a mean of 22 months, a VTE recurrence occurred in 23 patients in the aspirin group (5.9% per patient-year) and in 39 patients in the placebo group (11% per patient-year). This translated into a hazard ratio of 0.55.
There was one case of major bleeding in each group and three cases of clinically relevant nonmajor bleeding in each group. There were six deaths in the aspirin group (1.4% per patient-year) and five deaths in the placebo group (1.3% per patient-year), a difference that was not statistically significant (HR 1.04).
In an interview, Dr. Charles S. Abrams, professor of medicine at the University of Pennsylvania, Philadelphia, called the study findings "intriguing" and said that a larger trial will be needed to confirm the findings. "I’m not sure what the reason for the difference [between the placebo and aspiring groups] is," said Dr. Abrams.
"One possibility is that it’s a relatively small trial. If you look at the incidence of recurrent clots in most circumstances, it’s usually about 8% per year when you stop that anticoagulant." In the WARFASA trial, he continued, the incidence of recurrent clots in the placebo and aspirin groups "flanked what you would normally expect. It makes you worry that’s some sort of a fluke."
For her part, Dr. Becattini acknowledged that a larger confirmatory trial is needed before the use of aspirin for extended treatment of VTE can be recommended. She said that she discusses the option with patients who are candidates for aspirin therapy. With aspirin, she said, "we can have an alternative to nothing. It is not just an alternative, but it is a safe alternative."
The study was supported by a grant-in-aid from Bayer Pharma to the University of Perugia. Dr. Becattini and her coauthors said they had no relevant conflicts of interest to declare.
SAN DIEGO – Aspirin reduced the risk of recurrent symptomatic venous thromboembolism by about 40% when given over a 2-year period following 6-12 months of warfarin therapy, with no apparent increase in major bleeding.
The findings, presented during a press briefing at the annual meeting of the American Society of Hematology, suggest that aspirin is a valid alternative to oral anticoagulants in the extended treatment of venous thromboembolism (VTE).
"This has great implications for clinical practice because many patients on anticoagulant treatment after a first-ever VTE are stopped after the initial 6 months of therapy and then they receive nothing for secondary prevention," lead author Dr. Cecilia Becattini, an internist in the stroke unit at the University of Perugia (Italy), said in an interview. "Maybe aspirin is a great opportunity [for VTE prevention] instead of nothing, because warfarin has the complication of major bleeding."
For the multicenter study known as WARFASA, 402 patients with a first-ever unprovoked VTE who had completed 6-12 months of oral anticoagulant treatment were randomized to receive aspirin 100 mg daily (aspirin group) or placebo for at least 2 years (placebo group).
The primary efficacy outcome was objectively confirmed recurrent symptomatic VTE and VTE-related death. Clinically relevant (major and nonmajor) bleeding were the main safety outcomes. Bleeding was considered major if it was fatal, occurred in a critical organ, or was associated with a decrease in hemoglobin of greater than 2.0 g/dL or led to a transfusion of two units or greater of whole blood or red cells.
The mean age of patients was 64 years and 56% were male. Of the 402 patients, 205 were randomized to the aspirin group while 197 were randomized to the placebo group. During the study period, which was a mean 25 months, Dr. Becattini reported that a VTE recurrence occurred in 28 patients in the aspirin group (6.6% per patient-year) and in 43 patients in the placebo group (11.0% per patient-year). This translated into a hazard ratio of 0.58.
During the on-treatment study period, which was a mean of 22 months, a VTE recurrence occurred in 23 patients in the aspirin group (5.9% per patient-year) and in 39 patients in the placebo group (11% per patient-year). This translated into a hazard ratio of 0.55.
There was one case of major bleeding in each group and three cases of clinically relevant nonmajor bleeding in each group. There were six deaths in the aspirin group (1.4% per patient-year) and five deaths in the placebo group (1.3% per patient-year), a difference that was not statistically significant (HR 1.04).
In an interview, Dr. Charles S. Abrams, professor of medicine at the University of Pennsylvania, Philadelphia, called the study findings "intriguing" and said that a larger trial will be needed to confirm the findings. "I’m not sure what the reason for the difference [between the placebo and aspiring groups] is," said Dr. Abrams.
"One possibility is that it’s a relatively small trial. If you look at the incidence of recurrent clots in most circumstances, it’s usually about 8% per year when you stop that anticoagulant." In the WARFASA trial, he continued, the incidence of recurrent clots in the placebo and aspirin groups "flanked what you would normally expect. It makes you worry that’s some sort of a fluke."
For her part, Dr. Becattini acknowledged that a larger confirmatory trial is needed before the use of aspirin for extended treatment of VTE can be recommended. She said that she discusses the option with patients who are candidates for aspirin therapy. With aspirin, she said, "we can have an alternative to nothing. It is not just an alternative, but it is a safe alternative."
The study was supported by a grant-in-aid from Bayer Pharma to the University of Perugia. Dr. Becattini and her coauthors said they had no relevant conflicts of interest to declare.
SAN DIEGO – Aspirin reduced the risk of recurrent symptomatic venous thromboembolism by about 40% when given over a 2-year period following 6-12 months of warfarin therapy, with no apparent increase in major bleeding.
The findings, presented during a press briefing at the annual meeting of the American Society of Hematology, suggest that aspirin is a valid alternative to oral anticoagulants in the extended treatment of venous thromboembolism (VTE).
"This has great implications for clinical practice because many patients on anticoagulant treatment after a first-ever VTE are stopped after the initial 6 months of therapy and then they receive nothing for secondary prevention," lead author Dr. Cecilia Becattini, an internist in the stroke unit at the University of Perugia (Italy), said in an interview. "Maybe aspirin is a great opportunity [for VTE prevention] instead of nothing, because warfarin has the complication of major bleeding."
For the multicenter study known as WARFASA, 402 patients with a first-ever unprovoked VTE who had completed 6-12 months of oral anticoagulant treatment were randomized to receive aspirin 100 mg daily (aspirin group) or placebo for at least 2 years (placebo group).
The primary efficacy outcome was objectively confirmed recurrent symptomatic VTE and VTE-related death. Clinically relevant (major and nonmajor) bleeding were the main safety outcomes. Bleeding was considered major if it was fatal, occurred in a critical organ, or was associated with a decrease in hemoglobin of greater than 2.0 g/dL or led to a transfusion of two units or greater of whole blood or red cells.
The mean age of patients was 64 years and 56% were male. Of the 402 patients, 205 were randomized to the aspirin group while 197 were randomized to the placebo group. During the study period, which was a mean 25 months, Dr. Becattini reported that a VTE recurrence occurred in 28 patients in the aspirin group (6.6% per patient-year) and in 43 patients in the placebo group (11.0% per patient-year). This translated into a hazard ratio of 0.58.
During the on-treatment study period, which was a mean of 22 months, a VTE recurrence occurred in 23 patients in the aspirin group (5.9% per patient-year) and in 39 patients in the placebo group (11% per patient-year). This translated into a hazard ratio of 0.55.
There was one case of major bleeding in each group and three cases of clinically relevant nonmajor bleeding in each group. There were six deaths in the aspirin group (1.4% per patient-year) and five deaths in the placebo group (1.3% per patient-year), a difference that was not statistically significant (HR 1.04).
In an interview, Dr. Charles S. Abrams, professor of medicine at the University of Pennsylvania, Philadelphia, called the study findings "intriguing" and said that a larger trial will be needed to confirm the findings. "I’m not sure what the reason for the difference [between the placebo and aspiring groups] is," said Dr. Abrams.
"One possibility is that it’s a relatively small trial. If you look at the incidence of recurrent clots in most circumstances, it’s usually about 8% per year when you stop that anticoagulant." In the WARFASA trial, he continued, the incidence of recurrent clots in the placebo and aspirin groups "flanked what you would normally expect. It makes you worry that’s some sort of a fluke."
For her part, Dr. Becattini acknowledged that a larger confirmatory trial is needed before the use of aspirin for extended treatment of VTE can be recommended. She said that she discusses the option with patients who are candidates for aspirin therapy. With aspirin, she said, "we can have an alternative to nothing. It is not just an alternative, but it is a safe alternative."
The study was supported by a grant-in-aid from Bayer Pharma to the University of Perugia. Dr. Becattini and her coauthors said they had no relevant conflicts of interest to declare.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY
Major Finding: In a population of patients with unprovoked venous thromboembolism who had completed 6-12 months of oral anticoagulant treatment, aspirin reduced the incidence of recurrent VTE by about 40%, compared with placebo.
Data Source: A multicenter study of 402 patients with a mean age of 64 years who were randomized to receive to receive aspirin, 100 mg daily, or placebo for at least 2 years.
Disclosures: The study was supported by a grant-in-aid from Bayer Pharma to the University of Perugia, Italy. Dr. Becattini and her coauthors said they had no relevant conflicts of interest to declare.
Early Thrombolysis Improves Long-term Outcomes After DVT
SAN DIEGO – Catheter-directed thrombolysis added to standard therapy for deep vein thrombosis reduced the risk of post-thrombotic syndrome by 14.5%, but at an increased cost of bleeding among 209 patients in a randomized, controlled trial.
At 2 years, 55.6% of patients receiving standard treatment with anticoagulation and compression stockings developed post-thrombotic syndrome (PTS), compared with 41.1% receiving catheter-directed thrombolysis (CDT) plus standard therapy (P = .047) in the multicenter CaVenT study.
The number needed to treat to prevent one PTS was seven, Dr. Per Morten Sandset and his colleagues will report in a late-breaking abstract to be presented Dec. 13 at the annual meeting of the American Society of Hematology. About one in four patients is still at risk for developing PTS after adequate treatment with anticoagulation and compression stockings.
The CaVenT (Catheter-Directed Thrombolysis for Acute Iliofemoral Deep Vein Thrombosis) trial provides much-needed prospective, randomized data on CDT, and is unique in that it focuses on functional rather than surrogate outcomes used in previous trials and case series, Dr. Sandset said at a press briefing in which he discussed the findings.
Still, the study is small and unlikely to change practice or resolve the controversy that has surrounded the use of early fibrinolysis since systemic thrombolytic therapy was introduced decades ago.
"For the first time, we have the evidence to support this type of treatment for centers that have developed this methodology, but I also believe we need further study," said Dr. Sandset, a professor in the division of specialized medicine and surgery at Oslo University in Norway.
Briefing moderator Dr. Charles Abrams, associate chief of hematology-oncology at the University of Pennsylvania School of Medicine in Philadelphia, said CaVenT provides the best randomized data to date, but that many clinicians, particularly in the United States, have been hesitant to adopt early fibrinolysis because of the increased risk of a serious bleeding complication.
"This is a tantalizing trial, but I don’t think ... when I’m back at my own institution that the next patient I see with a deep vein thrombosis is probably going to get it," he said.
Both men said results are eagerly awaited from the ongoing phase III, randomized ATTRACT trial evaluating CDT with blood-thinning drugs in 692 patients with proximal DVT. The cohort is three times larger than that of the CaVenT trial, but results from the North American trial are not expected possibly until 2015.
CaVenT randomized 209 patients who presented at 20 hospitals in Norway with their first acute iliofemoral DVT and symptoms present for up to 21 days to CDT with alteplase (Activase) followed by standard treatment or standard treatment alone. In all, 189 patients were evaluable for analysis. Their average age was 51.5 years (range 18-75 years), and 36% were women.
CDT significantly increased the rate of iliofemoral patency at six months from 47.4% with standard therapy to 65.9% (P = .012), Dr. Sandset said.
Importantly, patients who regained iliofemoral patency at six months had significantly less PTS at 2 years than those who experienced insufficient recanalization (36.9% vs. 61.3%, P less than .001). In all, 80 of the 90 patients in the CDT arm had successful lysis.
Bleeding complications were reported in 20 patients in the CDT arm and none in the control arm. Five bleeding events were clinically relevant and three were major, including compartment syndrome of the calf requiring surgery, abdominal wall hematoma requiring transfusion, and an inguinal puncture site hematoma.
No deaths, pulmonary embolisms, strokes or other complications with a permanently reduced outcome were reported, Dr. Sandset said.
"CDT should be considered in patients with acute iliofemoral DVT and no apparent risk of bleeding," he said, adding that the results should be taken into account when guidelines are revised.
One of the problems for clinicians managing patients with DVT is that PTS can vary from simple heaviness in the leg to a constantly swollen leg that can impair the patient’s ability to walk or hold a steady job, Dr. Abrams said.
"Patients with bigger clots and clots higher up in their thigh get more persistent symptoms, but you really can’t predict all that well who will have a bad long-term complication," he said in an interview. "And the downside of this is that the administration of this drug in other trials has led to bleeding complications in 5% of patients, and 2% of that 5% are either strokes or retroperitoneal bleeding."
Dr. Abrams noted that older patients are also at greater risk of a bleeding complication than younger patients, and that clinicians will have to weigh the pros and cons of the current findings in this context with their patients.
Dr. Sandset and Dr. Abrams reported no conflicts of interest.
SAN DIEGO – Catheter-directed thrombolysis added to standard therapy for deep vein thrombosis reduced the risk of post-thrombotic syndrome by 14.5%, but at an increased cost of bleeding among 209 patients in a randomized, controlled trial.
At 2 years, 55.6% of patients receiving standard treatment with anticoagulation and compression stockings developed post-thrombotic syndrome (PTS), compared with 41.1% receiving catheter-directed thrombolysis (CDT) plus standard therapy (P = .047) in the multicenter CaVenT study.
The number needed to treat to prevent one PTS was seven, Dr. Per Morten Sandset and his colleagues will report in a late-breaking abstract to be presented Dec. 13 at the annual meeting of the American Society of Hematology. About one in four patients is still at risk for developing PTS after adequate treatment with anticoagulation and compression stockings.
The CaVenT (Catheter-Directed Thrombolysis for Acute Iliofemoral Deep Vein Thrombosis) trial provides much-needed prospective, randomized data on CDT, and is unique in that it focuses on functional rather than surrogate outcomes used in previous trials and case series, Dr. Sandset said at a press briefing in which he discussed the findings.
Still, the study is small and unlikely to change practice or resolve the controversy that has surrounded the use of early fibrinolysis since systemic thrombolytic therapy was introduced decades ago.
"For the first time, we have the evidence to support this type of treatment for centers that have developed this methodology, but I also believe we need further study," said Dr. Sandset, a professor in the division of specialized medicine and surgery at Oslo University in Norway.
Briefing moderator Dr. Charles Abrams, associate chief of hematology-oncology at the University of Pennsylvania School of Medicine in Philadelphia, said CaVenT provides the best randomized data to date, but that many clinicians, particularly in the United States, have been hesitant to adopt early fibrinolysis because of the increased risk of a serious bleeding complication.
"This is a tantalizing trial, but I don’t think ... when I’m back at my own institution that the next patient I see with a deep vein thrombosis is probably going to get it," he said.
Both men said results are eagerly awaited from the ongoing phase III, randomized ATTRACT trial evaluating CDT with blood-thinning drugs in 692 patients with proximal DVT. The cohort is three times larger than that of the CaVenT trial, but results from the North American trial are not expected possibly until 2015.
CaVenT randomized 209 patients who presented at 20 hospitals in Norway with their first acute iliofemoral DVT and symptoms present for up to 21 days to CDT with alteplase (Activase) followed by standard treatment or standard treatment alone. In all, 189 patients were evaluable for analysis. Their average age was 51.5 years (range 18-75 years), and 36% were women.
CDT significantly increased the rate of iliofemoral patency at six months from 47.4% with standard therapy to 65.9% (P = .012), Dr. Sandset said.
Importantly, patients who regained iliofemoral patency at six months had significantly less PTS at 2 years than those who experienced insufficient recanalization (36.9% vs. 61.3%, P less than .001). In all, 80 of the 90 patients in the CDT arm had successful lysis.
Bleeding complications were reported in 20 patients in the CDT arm and none in the control arm. Five bleeding events were clinically relevant and three were major, including compartment syndrome of the calf requiring surgery, abdominal wall hematoma requiring transfusion, and an inguinal puncture site hematoma.
No deaths, pulmonary embolisms, strokes or other complications with a permanently reduced outcome were reported, Dr. Sandset said.
"CDT should be considered in patients with acute iliofemoral DVT and no apparent risk of bleeding," he said, adding that the results should be taken into account when guidelines are revised.
One of the problems for clinicians managing patients with DVT is that PTS can vary from simple heaviness in the leg to a constantly swollen leg that can impair the patient’s ability to walk or hold a steady job, Dr. Abrams said.
"Patients with bigger clots and clots higher up in their thigh get more persistent symptoms, but you really can’t predict all that well who will have a bad long-term complication," he said in an interview. "And the downside of this is that the administration of this drug in other trials has led to bleeding complications in 5% of patients, and 2% of that 5% are either strokes or retroperitoneal bleeding."
Dr. Abrams noted that older patients are also at greater risk of a bleeding complication than younger patients, and that clinicians will have to weigh the pros and cons of the current findings in this context with their patients.
Dr. Sandset and Dr. Abrams reported no conflicts of interest.
SAN DIEGO – Catheter-directed thrombolysis added to standard therapy for deep vein thrombosis reduced the risk of post-thrombotic syndrome by 14.5%, but at an increased cost of bleeding among 209 patients in a randomized, controlled trial.
At 2 years, 55.6% of patients receiving standard treatment with anticoagulation and compression stockings developed post-thrombotic syndrome (PTS), compared with 41.1% receiving catheter-directed thrombolysis (CDT) plus standard therapy (P = .047) in the multicenter CaVenT study.
The number needed to treat to prevent one PTS was seven, Dr. Per Morten Sandset and his colleagues will report in a late-breaking abstract to be presented Dec. 13 at the annual meeting of the American Society of Hematology. About one in four patients is still at risk for developing PTS after adequate treatment with anticoagulation and compression stockings.
The CaVenT (Catheter-Directed Thrombolysis for Acute Iliofemoral Deep Vein Thrombosis) trial provides much-needed prospective, randomized data on CDT, and is unique in that it focuses on functional rather than surrogate outcomes used in previous trials and case series, Dr. Sandset said at a press briefing in which he discussed the findings.
Still, the study is small and unlikely to change practice or resolve the controversy that has surrounded the use of early fibrinolysis since systemic thrombolytic therapy was introduced decades ago.
"For the first time, we have the evidence to support this type of treatment for centers that have developed this methodology, but I also believe we need further study," said Dr. Sandset, a professor in the division of specialized medicine and surgery at Oslo University in Norway.
Briefing moderator Dr. Charles Abrams, associate chief of hematology-oncology at the University of Pennsylvania School of Medicine in Philadelphia, said CaVenT provides the best randomized data to date, but that many clinicians, particularly in the United States, have been hesitant to adopt early fibrinolysis because of the increased risk of a serious bleeding complication.
"This is a tantalizing trial, but I don’t think ... when I’m back at my own institution that the next patient I see with a deep vein thrombosis is probably going to get it," he said.
Both men said results are eagerly awaited from the ongoing phase III, randomized ATTRACT trial evaluating CDT with blood-thinning drugs in 692 patients with proximal DVT. The cohort is three times larger than that of the CaVenT trial, but results from the North American trial are not expected possibly until 2015.
CaVenT randomized 209 patients who presented at 20 hospitals in Norway with their first acute iliofemoral DVT and symptoms present for up to 21 days to CDT with alteplase (Activase) followed by standard treatment or standard treatment alone. In all, 189 patients were evaluable for analysis. Their average age was 51.5 years (range 18-75 years), and 36% were women.
CDT significantly increased the rate of iliofemoral patency at six months from 47.4% with standard therapy to 65.9% (P = .012), Dr. Sandset said.
Importantly, patients who regained iliofemoral patency at six months had significantly less PTS at 2 years than those who experienced insufficient recanalization (36.9% vs. 61.3%, P less than .001). In all, 80 of the 90 patients in the CDT arm had successful lysis.
Bleeding complications were reported in 20 patients in the CDT arm and none in the control arm. Five bleeding events were clinically relevant and three were major, including compartment syndrome of the calf requiring surgery, abdominal wall hematoma requiring transfusion, and an inguinal puncture site hematoma.
No deaths, pulmonary embolisms, strokes or other complications with a permanently reduced outcome were reported, Dr. Sandset said.
"CDT should be considered in patients with acute iliofemoral DVT and no apparent risk of bleeding," he said, adding that the results should be taken into account when guidelines are revised.
One of the problems for clinicians managing patients with DVT is that PTS can vary from simple heaviness in the leg to a constantly swollen leg that can impair the patient’s ability to walk or hold a steady job, Dr. Abrams said.
"Patients with bigger clots and clots higher up in their thigh get more persistent symptoms, but you really can’t predict all that well who will have a bad long-term complication," he said in an interview. "And the downside of this is that the administration of this drug in other trials has led to bleeding complications in 5% of patients, and 2% of that 5% are either strokes or retroperitoneal bleeding."
Dr. Abrams noted that older patients are also at greater risk of a bleeding complication than younger patients, and that clinicians will have to weigh the pros and cons of the current findings in this context with their patients.
Dr. Sandset and Dr. Abrams reported no conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY
Major Finding: At 2 years, 55.6% of patients receiving standard DVT treatment developed post-thrombotic syndrome vs. 41.1% receiving catheter-directed thrombolysis plus standard therapy (P = .047).
Data Source: Prospective, randomized trial in 209 patients with an acute iliofemoral deep vein thrombosis.
Disclosures: Dr. Sandset and Dr. Abrams reported no conflicts of interest.
Contralateral Prophylactic Mastectomy Ups Surgical Risk
SAN ANTONIO – Contralateral prophylactic mastectomy – in comparison to unilateral mastectomy – was associated with a significantly increased rate of major postoperative surgical complications in a 470-patient study.
Physicians therefore must provide appropriate information about these risks to patients who are considering the contralateral procedure, according to lead investigator Allison C. Stover, M.P.H. Major complications often require numerous unplanned procedures, which increase patient burden and treatment costs.
To assess the impact of the contralateral procedure on surgical outcomes, Ms. Stover of the University of California, San Francisco, and her colleagues identified patients who underwent unilateral or bilateral mastectomy with immediate reconstruction at her institution between 2005 and 2010. A minimum of 1 year of follow-up data was available for each study participant. Patients with bilateral cancer or bilateral prophylactic surgery were excluded from the analysis.
The investigators grouped the patients by unilateral or contralateral mastectomy status. They also prospectively captured complications, including infection with use of oral or intravenous antibiotics; implant exposure, loss, or removal; seroma; hematoma; delayed wound healing; necrosis; readmission; and return to the operating room.
Among the 470 patients (665 breasts) who met the study criteria, the mean follow-up time was 22 months. There were no differences between the groups in tumor grade, stage, follow-up time, smoking history, or radiation, either prior to or post surgery, Ms. Stover said in a poster presentation at the San Antonio Breast Cancer Symposium.
Significant between-group differences were observed in age and the number of skin-sparing mastectomies, she said, noting that the contralateral group was younger than the unilateral group (mean age 46.04 years vs. 50.55 years, respectively), and had a larger proportion of skin-sparing mastectomies.
The rate of any major complication was 1.5 times higher in the contralateral group compared with the unilateral group, Ms. Stover stated. "There were significant between-group differences in the number of severe infections requiring IV antibiotics and return to the operating room, as well as the overall rate of any major complication," she said.
A comparison of the complication rate by index vs. prophylactic breast within the contralateral group showed a significantly higher rate of implant loss in the index breast, but no significant differences in any other measure, Ms. Stover noted.
Because many contralateral cases are not at sufficiently high risk for a second breast cancer to meet clinical criteria for prophylactic surgery, the increased complication rate should be taken into consideration when counseling women who are contemplating contralateral mastectomy, Ms. Stover said, adding that they should also be incorporated into guidelines and clinical recommendations.
The poster discussant, Dr. Ismail Jatoi of the University of Texas Health Sciences Center in San Antonio, pointed out that the study’s mean follow-up of 22 months may be insufficient to adequately compare the complication rates. "There are long-term implications that may increase the value [of the contralateral procedure]. For example, patients who undergo the procedure no longer undergo mammograms and thus are not subject to false-positive reports and the subsequent associated testing. They may have lower morbidity over time," he said. "The long-term impact may be less dire than the short-term impact."
It is also possible that the results could be attributed to a "multiplicity of testing," Dr. Jatoi said. "When you test for a lot of bad outcomes, you’re likely to find one."
Despite these concerns, "there clearly are some risks, which point to the need for proper, thorough informed consent," said Dr. Jatoi. "The possible increased complication risks are definitely points to be made when we provide informed consent."
Ms. Stover and Dr. Jatoi reported that they had no relevant financial conflicts.
SAN ANTONIO – Contralateral prophylactic mastectomy – in comparison to unilateral mastectomy – was associated with a significantly increased rate of major postoperative surgical complications in a 470-patient study.
Physicians therefore must provide appropriate information about these risks to patients who are considering the contralateral procedure, according to lead investigator Allison C. Stover, M.P.H. Major complications often require numerous unplanned procedures, which increase patient burden and treatment costs.
To assess the impact of the contralateral procedure on surgical outcomes, Ms. Stover of the University of California, San Francisco, and her colleagues identified patients who underwent unilateral or bilateral mastectomy with immediate reconstruction at her institution between 2005 and 2010. A minimum of 1 year of follow-up data was available for each study participant. Patients with bilateral cancer or bilateral prophylactic surgery were excluded from the analysis.
The investigators grouped the patients by unilateral or contralateral mastectomy status. They also prospectively captured complications, including infection with use of oral or intravenous antibiotics; implant exposure, loss, or removal; seroma; hematoma; delayed wound healing; necrosis; readmission; and return to the operating room.
Among the 470 patients (665 breasts) who met the study criteria, the mean follow-up time was 22 months. There were no differences between the groups in tumor grade, stage, follow-up time, smoking history, or radiation, either prior to or post surgery, Ms. Stover said in a poster presentation at the San Antonio Breast Cancer Symposium.
Significant between-group differences were observed in age and the number of skin-sparing mastectomies, she said, noting that the contralateral group was younger than the unilateral group (mean age 46.04 years vs. 50.55 years, respectively), and had a larger proportion of skin-sparing mastectomies.
The rate of any major complication was 1.5 times higher in the contralateral group compared with the unilateral group, Ms. Stover stated. "There were significant between-group differences in the number of severe infections requiring IV antibiotics and return to the operating room, as well as the overall rate of any major complication," she said.
A comparison of the complication rate by index vs. prophylactic breast within the contralateral group showed a significantly higher rate of implant loss in the index breast, but no significant differences in any other measure, Ms. Stover noted.
Because many contralateral cases are not at sufficiently high risk for a second breast cancer to meet clinical criteria for prophylactic surgery, the increased complication rate should be taken into consideration when counseling women who are contemplating contralateral mastectomy, Ms. Stover said, adding that they should also be incorporated into guidelines and clinical recommendations.
The poster discussant, Dr. Ismail Jatoi of the University of Texas Health Sciences Center in San Antonio, pointed out that the study’s mean follow-up of 22 months may be insufficient to adequately compare the complication rates. "There are long-term implications that may increase the value [of the contralateral procedure]. For example, patients who undergo the procedure no longer undergo mammograms and thus are not subject to false-positive reports and the subsequent associated testing. They may have lower morbidity over time," he said. "The long-term impact may be less dire than the short-term impact."
It is also possible that the results could be attributed to a "multiplicity of testing," Dr. Jatoi said. "When you test for a lot of bad outcomes, you’re likely to find one."
Despite these concerns, "there clearly are some risks, which point to the need for proper, thorough informed consent," said Dr. Jatoi. "The possible increased complication risks are definitely points to be made when we provide informed consent."
Ms. Stover and Dr. Jatoi reported that they had no relevant financial conflicts.
SAN ANTONIO – Contralateral prophylactic mastectomy – in comparison to unilateral mastectomy – was associated with a significantly increased rate of major postoperative surgical complications in a 470-patient study.
Physicians therefore must provide appropriate information about these risks to patients who are considering the contralateral procedure, according to lead investigator Allison C. Stover, M.P.H. Major complications often require numerous unplanned procedures, which increase patient burden and treatment costs.
To assess the impact of the contralateral procedure on surgical outcomes, Ms. Stover of the University of California, San Francisco, and her colleagues identified patients who underwent unilateral or bilateral mastectomy with immediate reconstruction at her institution between 2005 and 2010. A minimum of 1 year of follow-up data was available for each study participant. Patients with bilateral cancer or bilateral prophylactic surgery were excluded from the analysis.
The investigators grouped the patients by unilateral or contralateral mastectomy status. They also prospectively captured complications, including infection with use of oral or intravenous antibiotics; implant exposure, loss, or removal; seroma; hematoma; delayed wound healing; necrosis; readmission; and return to the operating room.
Among the 470 patients (665 breasts) who met the study criteria, the mean follow-up time was 22 months. There were no differences between the groups in tumor grade, stage, follow-up time, smoking history, or radiation, either prior to or post surgery, Ms. Stover said in a poster presentation at the San Antonio Breast Cancer Symposium.
Significant between-group differences were observed in age and the number of skin-sparing mastectomies, she said, noting that the contralateral group was younger than the unilateral group (mean age 46.04 years vs. 50.55 years, respectively), and had a larger proportion of skin-sparing mastectomies.
The rate of any major complication was 1.5 times higher in the contralateral group compared with the unilateral group, Ms. Stover stated. "There were significant between-group differences in the number of severe infections requiring IV antibiotics and return to the operating room, as well as the overall rate of any major complication," she said.
A comparison of the complication rate by index vs. prophylactic breast within the contralateral group showed a significantly higher rate of implant loss in the index breast, but no significant differences in any other measure, Ms. Stover noted.
Because many contralateral cases are not at sufficiently high risk for a second breast cancer to meet clinical criteria for prophylactic surgery, the increased complication rate should be taken into consideration when counseling women who are contemplating contralateral mastectomy, Ms. Stover said, adding that they should also be incorporated into guidelines and clinical recommendations.
The poster discussant, Dr. Ismail Jatoi of the University of Texas Health Sciences Center in San Antonio, pointed out that the study’s mean follow-up of 22 months may be insufficient to adequately compare the complication rates. "There are long-term implications that may increase the value [of the contralateral procedure]. For example, patients who undergo the procedure no longer undergo mammograms and thus are not subject to false-positive reports and the subsequent associated testing. They may have lower morbidity over time," he said. "The long-term impact may be less dire than the short-term impact."
It is also possible that the results could be attributed to a "multiplicity of testing," Dr. Jatoi said. "When you test for a lot of bad outcomes, you’re likely to find one."
Despite these concerns, "there clearly are some risks, which point to the need for proper, thorough informed consent," said Dr. Jatoi. "The possible increased complication risks are definitely points to be made when we provide informed consent."
Ms. Stover and Dr. Jatoi reported that they had no relevant financial conflicts.
FROM THE SAN ANTONIO BREAST CANCER SYMPOSIUM
Major Finding: Unilateral breast cancer patients undergoing contralateral prophylactic mastectomy were 1.5 times more likely to experience postsurgical complications than those undergoing unilateral mastectomy.
Data Source: Comparison of postsurgical outcomes among 470 breast cancer patients entered into a prospective database who underwent unilateral or bilateral mastectomy with immediate reconstruction.
Disclosures: Ms. Stover and Dr. Jatoi reported that they had no relevant financial conflicts.
Older Age, Comorbidities Raise Readmission Risk After Colectomy
HOT SPRINGS, VA. – A shorter length of stay appears to be associated with a higher risk of readmission after colectomy, but only in patients who are older and have more preoperative comorbidities and perioperative complications, results of a large database review demonstrate.
Dr. Timothy Pawlik and his colleagues from Johns Hopkins Hospital, Baltimore, conducted a retrospective study of the Surveillance, Epidemiology, and End Results (SEER) database of 149,622 Medicare patients with a primary diagnosis of colorectal cancer who underwent colectomy from 1986 to 2005. The goal was to determine trends in readmission rates during the first 30 days.
"How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?"
Increasingly, payers – especially Medicare – are penalizing hospitals for failing to prevent readmissions, which cost about $40 billion annually. Moreover, up to three-quarters of readmissions may be avoidable. In the meantime, many hospitals are fast-tracking patients for discharge after colorectal surgery.
In the SEER data, the mean age was 75 years in the 1986-1990 period and 77 years in the later period of 2001-2005. Patients were sicker in the later time period, with 63% having a Charlson comorbidity score of 3 or greater, compared with only 53% in the earlier time frame.
Most patients (38%) had a right colectomy; 23% had a sigmoid procedure, 13% had a rectal procedure, and 11% had a left colectomy. Forty-six percent of patients had lymph node metastasis, and 17% had an emergent procedure.
Morbidity for the entire study period was 37%; most complications were gastrointestinal or related to bleeding or postoperative infection. Again, there was a significant difference between the earlier and the later time frames. Perioperative morbidity was 27% in the 1986-1990 time frame, vs. 40% in 2001-2005. Mortality, at 4%, remained stable over time.
The mean length of stay decreased from 14 to 10 days from the early time to the later time period. And, over time, the percentage of patients discharged to home decreased, while discharges to skilled nursing facilities increased.
Overall, there were 17,000 readmissions, for a rate of 11%. Readmissions also increased, from 10% early on to 14% in 2001-2005. During that later time frame, patients had a 46% increased risk of readmission. Almost half of the readmissions occurred within the first 7 days after surgery, primarily for complications, dehydration, or infection. The mortality rate associated with readmission was 8%.
Multivariate analysis showed that the factors most likely to impact readmission were multiple comorbidities or a history of any perioperative complication, said Dr. Pawlik. Early discharge alone was not associated with a higher risk of readmission.
The study shows that "ongoing initiatives to reduce risk of readmissions and the associated costs, morbidity, and mortality are needed," said Dr. Pawlik.
It also "provides data that we all know to be true: namely, that the patients we are operating on have more comorbidities and that length of stay increases the rate of readmissions," said Dr. Susan Galandiuk, the discussant at the meeting. However, payers have been using length of stay and readmissions as quality surrogates, said Dr. Galandiuk, professor of surgery at the University of Louisville, Ky.
Not readmitting an elderly patient with many comorbidities and complications "would be a quality of care issue, and not the other way around," she added. The problem now is, "How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?" asked Dr. Galandiuk.
Dr. Pawlik agreed that readmissions should not necessarily be held to be all bad. "Blaming readmissions on length of stay is a gross oversimplification of what’s going on," he added. Surgeons are clearly operating on older and sicker patients, and are doing more complicated operations that may result in a higher rate of morbidity – all this "in a culture of being asked to send people home earlier," he said.
"Our data clearly show that early discharge is feasible in some patients, but it needs to be used judiciously, especially in an older population," said Dr. Pawlik.
Dr. Pawlik and Dr. Galandiuk reported no conflicts.
HOT SPRINGS, VA. – A shorter length of stay appears to be associated with a higher risk of readmission after colectomy, but only in patients who are older and have more preoperative comorbidities and perioperative complications, results of a large database review demonstrate.
Dr. Timothy Pawlik and his colleagues from Johns Hopkins Hospital, Baltimore, conducted a retrospective study of the Surveillance, Epidemiology, and End Results (SEER) database of 149,622 Medicare patients with a primary diagnosis of colorectal cancer who underwent colectomy from 1986 to 2005. The goal was to determine trends in readmission rates during the first 30 days.
"How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?"
Increasingly, payers – especially Medicare – are penalizing hospitals for failing to prevent readmissions, which cost about $40 billion annually. Moreover, up to three-quarters of readmissions may be avoidable. In the meantime, many hospitals are fast-tracking patients for discharge after colorectal surgery.
In the SEER data, the mean age was 75 years in the 1986-1990 period and 77 years in the later period of 2001-2005. Patients were sicker in the later time period, with 63% having a Charlson comorbidity score of 3 or greater, compared with only 53% in the earlier time frame.
Most patients (38%) had a right colectomy; 23% had a sigmoid procedure, 13% had a rectal procedure, and 11% had a left colectomy. Forty-six percent of patients had lymph node metastasis, and 17% had an emergent procedure.
Morbidity for the entire study period was 37%; most complications were gastrointestinal or related to bleeding or postoperative infection. Again, there was a significant difference between the earlier and the later time frames. Perioperative morbidity was 27% in the 1986-1990 time frame, vs. 40% in 2001-2005. Mortality, at 4%, remained stable over time.
The mean length of stay decreased from 14 to 10 days from the early time to the later time period. And, over time, the percentage of patients discharged to home decreased, while discharges to skilled nursing facilities increased.
Overall, there were 17,000 readmissions, for a rate of 11%. Readmissions also increased, from 10% early on to 14% in 2001-2005. During that later time frame, patients had a 46% increased risk of readmission. Almost half of the readmissions occurred within the first 7 days after surgery, primarily for complications, dehydration, or infection. The mortality rate associated with readmission was 8%.
Multivariate analysis showed that the factors most likely to impact readmission were multiple comorbidities or a history of any perioperative complication, said Dr. Pawlik. Early discharge alone was not associated with a higher risk of readmission.
The study shows that "ongoing initiatives to reduce risk of readmissions and the associated costs, morbidity, and mortality are needed," said Dr. Pawlik.
It also "provides data that we all know to be true: namely, that the patients we are operating on have more comorbidities and that length of stay increases the rate of readmissions," said Dr. Susan Galandiuk, the discussant at the meeting. However, payers have been using length of stay and readmissions as quality surrogates, said Dr. Galandiuk, professor of surgery at the University of Louisville, Ky.
Not readmitting an elderly patient with many comorbidities and complications "would be a quality of care issue, and not the other way around," she added. The problem now is, "How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?" asked Dr. Galandiuk.
Dr. Pawlik agreed that readmissions should not necessarily be held to be all bad. "Blaming readmissions on length of stay is a gross oversimplification of what’s going on," he added. Surgeons are clearly operating on older and sicker patients, and are doing more complicated operations that may result in a higher rate of morbidity – all this "in a culture of being asked to send people home earlier," he said.
"Our data clearly show that early discharge is feasible in some patients, but it needs to be used judiciously, especially in an older population," said Dr. Pawlik.
Dr. Pawlik and Dr. Galandiuk reported no conflicts.
HOT SPRINGS, VA. – A shorter length of stay appears to be associated with a higher risk of readmission after colectomy, but only in patients who are older and have more preoperative comorbidities and perioperative complications, results of a large database review demonstrate.
Dr. Timothy Pawlik and his colleagues from Johns Hopkins Hospital, Baltimore, conducted a retrospective study of the Surveillance, Epidemiology, and End Results (SEER) database of 149,622 Medicare patients with a primary diagnosis of colorectal cancer who underwent colectomy from 1986 to 2005. The goal was to determine trends in readmission rates during the first 30 days.
"How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?"
Increasingly, payers – especially Medicare – are penalizing hospitals for failing to prevent readmissions, which cost about $40 billion annually. Moreover, up to three-quarters of readmissions may be avoidable. In the meantime, many hospitals are fast-tracking patients for discharge after colorectal surgery.
In the SEER data, the mean age was 75 years in the 1986-1990 period and 77 years in the later period of 2001-2005. Patients were sicker in the later time period, with 63% having a Charlson comorbidity score of 3 or greater, compared with only 53% in the earlier time frame.
Most patients (38%) had a right colectomy; 23% had a sigmoid procedure, 13% had a rectal procedure, and 11% had a left colectomy. Forty-six percent of patients had lymph node metastasis, and 17% had an emergent procedure.
Morbidity for the entire study period was 37%; most complications were gastrointestinal or related to bleeding or postoperative infection. Again, there was a significant difference between the earlier and the later time frames. Perioperative morbidity was 27% in the 1986-1990 time frame, vs. 40% in 2001-2005. Mortality, at 4%, remained stable over time.
The mean length of stay decreased from 14 to 10 days from the early time to the later time period. And, over time, the percentage of patients discharged to home decreased, while discharges to skilled nursing facilities increased.
Overall, there were 17,000 readmissions, for a rate of 11%. Readmissions also increased, from 10% early on to 14% in 2001-2005. During that later time frame, patients had a 46% increased risk of readmission. Almost half of the readmissions occurred within the first 7 days after surgery, primarily for complications, dehydration, or infection. The mortality rate associated with readmission was 8%.
Multivariate analysis showed that the factors most likely to impact readmission were multiple comorbidities or a history of any perioperative complication, said Dr. Pawlik. Early discharge alone was not associated with a higher risk of readmission.
The study shows that "ongoing initiatives to reduce risk of readmissions and the associated costs, morbidity, and mortality are needed," said Dr. Pawlik.
It also "provides data that we all know to be true: namely, that the patients we are operating on have more comorbidities and that length of stay increases the rate of readmissions," said Dr. Susan Galandiuk, the discussant at the meeting. However, payers have been using length of stay and readmissions as quality surrogates, said Dr. Galandiuk, professor of surgery at the University of Louisville, Ky.
Not readmitting an elderly patient with many comorbidities and complications "would be a quality of care issue, and not the other way around," she added. The problem now is, "How do we begin to remedy the demonization of legitimate readmissions either politically, medically, or both?" asked Dr. Galandiuk.
Dr. Pawlik agreed that readmissions should not necessarily be held to be all bad. "Blaming readmissions on length of stay is a gross oversimplification of what’s going on," he added. Surgeons are clearly operating on older and sicker patients, and are doing more complicated operations that may result in a higher rate of morbidity – all this "in a culture of being asked to send people home earlier," he said.
"Our data clearly show that early discharge is feasible in some patients, but it needs to be used judiciously, especially in an older population," said Dr. Pawlik.
Dr. Pawlik and Dr. Galandiuk reported no conflicts.
FROM THE SOUTHERN SURGICAL ASSOCIATION ANNUAL MEETING
Major Finding: An increase in readmissions from 10% in 1986-1990 to 14% in 2001-2005 corresponded to older age and higher comorbidities in the later time period.
Data Source: Retrospective study of the SEER database of 149,622 Medicare patients with a primary diagnosis of colorectal cancer.
Disclosures: Dr. Pawlik and Dr. Galandiuk reported no conflicts.
Undiagnosed Diabetes Common in Women With Acute MI
ORLANDO – A fifth of women with an acute myocardial infarction have previously undiagnosed diabetes, according to results from a German registry that included 706 women.
The registry analysis also showed that prevalence of previously undiagnosed diabetes in women with a recent MI significantly exceeded the rate in men, Dr. Anselm K. Gitt said at the annual scientific sessions of the American Heart Association. And the 3-year outcome of women with an acute MI and newly diagnosed diabetes closely tracked the outcomes of women who survived an acute MI and had previously diagnosed diabetes. The 3-year mortality rate in both groups of women was about 30%, reported Dr. Gitt, a cardiologist at the Heart Center in Ludwigshafen, Germany, and vice director of the Myocardial Infarction Research Institute in Ludwigshafen.
Guidelines issued in 2007 by the European Society of Cardiology and the European Association for the Study of Diabetes recommended that physicians routinely perform an oral glucose tolerance test on patients following a MI who had not previously been diagnosed with diabetes (Eur. Heart J. 2007;28:88-136). "We started this study to see whether the recommendation had value in clinical practice. I think our new data confirm the recommendation," Dr. Gitt said.
However, because of results from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trial, simply focusing on intensive glycemic control in post-MI patients with newly diagnosed diabetes is probably not an ideal management approach, he acknowledged. Although study results have not clearly established an optimal strategy, he suggested "good glycemic control with attention to avoiding hypoglycemia, along with aggressively treating cardiovascular risk factors such as lipids and hypertension."
Dr. Gitt and his associates tallied the prevalence of diabetes in acute MI patients with data collected in the SWEETHEART registry, which enrolled 2,767 patients within 24 hours of either an ST-elevation MI or non ST-elevation MI at 30 German centers, and then followed the patients for 3 years. The group included 706 women (26%), with an average age of 71 years, compared with an average age of 64 among the 2,061 enrolled men. The prevalence of previously diagnosed diabetes was 30% among the women, and 23% among the men.
All patients without a prior diagnosis of diabetes underwent assessment with an oral glucose tolerance test, following the recommendation made by the ESC and EASD in 2007. This identified an additional 20% of the women and 15% of the men with diabetes (a blood glucose level greater than 200 mg/dL 2 hours following the oral glucose challenge), as well as 18% of the women and 23% of the men with impaired glucose tolerance. The total 50% prevalence of both newly and previously diagnosed diabetes among the women who entered the study was significantly higher than the combined 38% prevalence rate among the men, Dr. Gitt said.
During hospitalization for the index acute MI, the mortality rate among both the women and men newly diagnosed with diabetes was about 3%, similar to the rate among those with previously diagnosed diabetes. Mortality among the women and men with newly identified impaired glucose tolerance ran 0.8% and 0.4%, respectively, while mortality among those with no diabetes or glucose impairment was 1.2% among women and 1.3% among men.
During the 3-year follow-up, mortality in the newly diagnosed women was 31%, and it was 22% among the men. This finding is "important," because it shows that once physicians diagnose diabetes in a recent MI patient "their risk is very high," Dr. Gitt said. In women with a prior diabetes diagnosis the 3-year mortality rate was 30%, while in men with previously identified diabetes the mortality rate was 35%. Men and women with either impaired glucose tolerance or no identified glucose metabolism disorder had substantially lower 3-year mortality rates than ranged from 11% to 13%.
Dr. Gitt has received research grants from, and has been a consultant to or served on the speakers bureau for, AstraZeneca, Bristol Myers Squibb, Essex, GlaxoSmithKline, Merck, MSD, Pfizer, Roche, Eli Lilly, Sanofi-Aventis, Schering Plough, and Servier. He said that he has received research grants from Abbott and Hexal, and that he has been a consultant to or served on a speakers bureau for Amgen, Daiichi Sankyo, Iroko, and Novo Nordisk.
ORLANDO – A fifth of women with an acute myocardial infarction have previously undiagnosed diabetes, according to results from a German registry that included 706 women.
The registry analysis also showed that prevalence of previously undiagnosed diabetes in women with a recent MI significantly exceeded the rate in men, Dr. Anselm K. Gitt said at the annual scientific sessions of the American Heart Association. And the 3-year outcome of women with an acute MI and newly diagnosed diabetes closely tracked the outcomes of women who survived an acute MI and had previously diagnosed diabetes. The 3-year mortality rate in both groups of women was about 30%, reported Dr. Gitt, a cardiologist at the Heart Center in Ludwigshafen, Germany, and vice director of the Myocardial Infarction Research Institute in Ludwigshafen.
Guidelines issued in 2007 by the European Society of Cardiology and the European Association for the Study of Diabetes recommended that physicians routinely perform an oral glucose tolerance test on patients following a MI who had not previously been diagnosed with diabetes (Eur. Heart J. 2007;28:88-136). "We started this study to see whether the recommendation had value in clinical practice. I think our new data confirm the recommendation," Dr. Gitt said.
However, because of results from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trial, simply focusing on intensive glycemic control in post-MI patients with newly diagnosed diabetes is probably not an ideal management approach, he acknowledged. Although study results have not clearly established an optimal strategy, he suggested "good glycemic control with attention to avoiding hypoglycemia, along with aggressively treating cardiovascular risk factors such as lipids and hypertension."
Dr. Gitt and his associates tallied the prevalence of diabetes in acute MI patients with data collected in the SWEETHEART registry, which enrolled 2,767 patients within 24 hours of either an ST-elevation MI or non ST-elevation MI at 30 German centers, and then followed the patients for 3 years. The group included 706 women (26%), with an average age of 71 years, compared with an average age of 64 among the 2,061 enrolled men. The prevalence of previously diagnosed diabetes was 30% among the women, and 23% among the men.
All patients without a prior diagnosis of diabetes underwent assessment with an oral glucose tolerance test, following the recommendation made by the ESC and EASD in 2007. This identified an additional 20% of the women and 15% of the men with diabetes (a blood glucose level greater than 200 mg/dL 2 hours following the oral glucose challenge), as well as 18% of the women and 23% of the men with impaired glucose tolerance. The total 50% prevalence of both newly and previously diagnosed diabetes among the women who entered the study was significantly higher than the combined 38% prevalence rate among the men, Dr. Gitt said.
During hospitalization for the index acute MI, the mortality rate among both the women and men newly diagnosed with diabetes was about 3%, similar to the rate among those with previously diagnosed diabetes. Mortality among the women and men with newly identified impaired glucose tolerance ran 0.8% and 0.4%, respectively, while mortality among those with no diabetes or glucose impairment was 1.2% among women and 1.3% among men.
During the 3-year follow-up, mortality in the newly diagnosed women was 31%, and it was 22% among the men. This finding is "important," because it shows that once physicians diagnose diabetes in a recent MI patient "their risk is very high," Dr. Gitt said. In women with a prior diabetes diagnosis the 3-year mortality rate was 30%, while in men with previously identified diabetes the mortality rate was 35%. Men and women with either impaired glucose tolerance or no identified glucose metabolism disorder had substantially lower 3-year mortality rates than ranged from 11% to 13%.
Dr. Gitt has received research grants from, and has been a consultant to or served on the speakers bureau for, AstraZeneca, Bristol Myers Squibb, Essex, GlaxoSmithKline, Merck, MSD, Pfizer, Roche, Eli Lilly, Sanofi-Aventis, Schering Plough, and Servier. He said that he has received research grants from Abbott and Hexal, and that he has been a consultant to or served on a speakers bureau for Amgen, Daiichi Sankyo, Iroko, and Novo Nordisk.
ORLANDO – A fifth of women with an acute myocardial infarction have previously undiagnosed diabetes, according to results from a German registry that included 706 women.
The registry analysis also showed that prevalence of previously undiagnosed diabetes in women with a recent MI significantly exceeded the rate in men, Dr. Anselm K. Gitt said at the annual scientific sessions of the American Heart Association. And the 3-year outcome of women with an acute MI and newly diagnosed diabetes closely tracked the outcomes of women who survived an acute MI and had previously diagnosed diabetes. The 3-year mortality rate in both groups of women was about 30%, reported Dr. Gitt, a cardiologist at the Heart Center in Ludwigshafen, Germany, and vice director of the Myocardial Infarction Research Institute in Ludwigshafen.
Guidelines issued in 2007 by the European Society of Cardiology and the European Association for the Study of Diabetes recommended that physicians routinely perform an oral glucose tolerance test on patients following a MI who had not previously been diagnosed with diabetes (Eur. Heart J. 2007;28:88-136). "We started this study to see whether the recommendation had value in clinical practice. I think our new data confirm the recommendation," Dr. Gitt said.
However, because of results from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trial, simply focusing on intensive glycemic control in post-MI patients with newly diagnosed diabetes is probably not an ideal management approach, he acknowledged. Although study results have not clearly established an optimal strategy, he suggested "good glycemic control with attention to avoiding hypoglycemia, along with aggressively treating cardiovascular risk factors such as lipids and hypertension."
Dr. Gitt and his associates tallied the prevalence of diabetes in acute MI patients with data collected in the SWEETHEART registry, which enrolled 2,767 patients within 24 hours of either an ST-elevation MI or non ST-elevation MI at 30 German centers, and then followed the patients for 3 years. The group included 706 women (26%), with an average age of 71 years, compared with an average age of 64 among the 2,061 enrolled men. The prevalence of previously diagnosed diabetes was 30% among the women, and 23% among the men.
All patients without a prior diagnosis of diabetes underwent assessment with an oral glucose tolerance test, following the recommendation made by the ESC and EASD in 2007. This identified an additional 20% of the women and 15% of the men with diabetes (a blood glucose level greater than 200 mg/dL 2 hours following the oral glucose challenge), as well as 18% of the women and 23% of the men with impaired glucose tolerance. The total 50% prevalence of both newly and previously diagnosed diabetes among the women who entered the study was significantly higher than the combined 38% prevalence rate among the men, Dr. Gitt said.
During hospitalization for the index acute MI, the mortality rate among both the women and men newly diagnosed with diabetes was about 3%, similar to the rate among those with previously diagnosed diabetes. Mortality among the women and men with newly identified impaired glucose tolerance ran 0.8% and 0.4%, respectively, while mortality among those with no diabetes or glucose impairment was 1.2% among women and 1.3% among men.
During the 3-year follow-up, mortality in the newly diagnosed women was 31%, and it was 22% among the men. This finding is "important," because it shows that once physicians diagnose diabetes in a recent MI patient "their risk is very high," Dr. Gitt said. In women with a prior diabetes diagnosis the 3-year mortality rate was 30%, while in men with previously identified diabetes the mortality rate was 35%. Men and women with either impaired glucose tolerance or no identified glucose metabolism disorder had substantially lower 3-year mortality rates than ranged from 11% to 13%.
Dr. Gitt has received research grants from, and has been a consultant to or served on the speakers bureau for, AstraZeneca, Bristol Myers Squibb, Essex, GlaxoSmithKline, Merck, MSD, Pfizer, Roche, Eli Lilly, Sanofi-Aventis, Schering Plough, and Servier. He said that he has received research grants from Abbott and Hexal, and that he has been a consultant to or served on a speakers bureau for Amgen, Daiichi Sankyo, Iroko, and Novo Nordisk.
FROM THE ANNUAL SCIENTIFIC SESSIONS OF THE AMERICAN HEART ASSOCIATION
Major Finding: Following an acute myocardial infarction, the prevalence of previously undiagnosed diabetes was 20% in women, 15% in men.
Data Source: Review of 706 women and 2,061 men with an acute myocardial infarction enrolled into the SWEETHEART registry at 30 centers in Germany.
Disclosures: Dr. Gitt has received research grants from, and has been a consultant to or served on the speakers bureau for, AstraZeneca, Bristol Myers Squibb, Essex, GlaxoSmithKline, Merck, MSD, Pfizer, Roche, Eli Lilly, Sanofi-Aventis, Schering Plough, and Servier. He said that he has received research grants from Abbott and Hexal, and that he has been a consultant to or served on a speakers bureau for Amgen, Daiichi Sankyo, Iroko, and Novo Nordisk.
Think Smart to Improve the Safety of Patient-Controlled Analgesia
How often do errors with patient-controlled analgesia occur? More often than we know, research suggests.
Researchers who studied more than 900,000 medication record errors say that the 1% of errors related to patient-controlled analgesia (PCA) is probably just the tip of the iceberg. Although 1% may seem insignificant, this analysis was based on the voluntary medication error reporting, says lead researcher Rodney Hicks, Ph.D., who at that time of the study was manager, patient safety research and practice, U.S. Pharmacopeia.
"Although generalization of voluntary reported findings to the general population should be done cautiously," he points out, that "the general rule of thumb is that for every reported event, there can be between 300-1,000 unreported events."
This rule of thumb, based on 9,571 reported events, would mean that between 2.8 million and 9.6 million total events (unreported & reported) occurred over the 5-year period from July 1, 2000, to June 30, 2005. On an annualized basis, this would mean that about 600,000-2 million events/year could involve PCA.
These numbers are unacceptable in what should be an era of increasing patient safety. Says Dr. Hicks, "Further study would need to be done to ascertain the total number of PCA events, but the problem is extensive in my opinion." The picture is already pretty clear, but there is more to the data.
When the study looked at the number of events that caused harm, there were 624 records of PCA associated with harm, corresponding to 6.5% of the patients. Again, while 6.5% may seem small, as the study found, "By comparison, during the same period, only 1.5% of all other errors reported to MedMarx led to harm. This represents a fourfold higher relative risk of harm for PCA events."
"All health care disciplines were implicated in the errors, including physicians, pharmacists, and nurses" he said. "Therefore, it will take an interdisciplinary team to resolve the problems."
Dr. Hicks’ retrospective study of the magnitude, frequency, and nature of nonharmful and harmful medication errors associated with patient-controlled analgesia covered a 5-year review period with 919,241 medication errors records from 801 reporting health care facilities. The analysis was based on the international voluntary medication error reporting program, MedMarx. Dr. Hicks is now a professor a Western University College of Graduate Nursing, Pomona, Calif.
"Our analysis was in no means trying to discourage the use of PCA pumps. Many studies have shown the benefits of using PCA, including improved pain management, better utilization of nursing resources, increased patient satisfaction, and improved pulmonary function.
"However, this is clearly an indication that standardization needs to occur and organizations should invest in training and policies and procedures as well as equipment – all areas to promote safety."
Moreover, although elimination of error is critical, studies have shown even a correctly programmed PCA pump poses patient safety risks.
Appropriate doses of opiates can suppress respiration and decrease heart rate and blood pressure. Episodes of bradypnea and desaturation can escalate to respiratory depression requiring rescue, according to come via Ray Maddox, Pharm. D., of St. Joseph’s/Candler Health System and his colleagues, who studied an intravenous infusion safety initiative at the 644-bed, tertiary-care, magnet system to evaluate how "smart" technology can help avert high-risk adverse drug events and improve patient outcomes.
These investigators further point out that the success rate for in-hospital cardiopulmonary resuscitation remains less than one in five patients. If detected early, most cases of opioid-induced respiratory depression can be treated with naloxone. However, severe cases can be fatal. The risk of patient harm from medication errors with PCA pumps is 3.5 times the risk from any other type of medication administration error.
The researchers recommend the following: "Capnographic monitoring – measurements of ventilation using respiration and exhaled carbon dioxide – is particularly important because it can provide an earlier warning of respiratory depression than pulse oximetry in some patient populations."
In short, although there are many benefits to PCA usage, for improved patient safety, reduce the risks and monitor continuously to detect respiratory depression events.
With the desire to reduce errors and improve patient safety with the use of patient-controlled analgesia, a safety checklist is being developed by the Physician-Patient Alliance for Health and Safety. For more on this initiative, contact Michael Wong [email protected].
The Physician-Patient Alliance for Health & Safety is an advocacy group devoted to improving patient health and safety. PPAHS comprises physicians, patients, individuals, and organizations. PPAHS reports having no financial conflicts of interest and not having received funding or grants. It recently conducted a survey on the American Society of Anesthesiologists Standards & Anesthesia Patient Safety Foundation Recommendations, available online. PPAHS welcomes inquiries regarding financial assistance to implement the safety checklist initiative.
How often do errors with patient-controlled analgesia occur? More often than we know, research suggests.
Researchers who studied more than 900,000 medication record errors say that the 1% of errors related to patient-controlled analgesia (PCA) is probably just the tip of the iceberg. Although 1% may seem insignificant, this analysis was based on the voluntary medication error reporting, says lead researcher Rodney Hicks, Ph.D., who at that time of the study was manager, patient safety research and practice, U.S. Pharmacopeia.
"Although generalization of voluntary reported findings to the general population should be done cautiously," he points out, that "the general rule of thumb is that for every reported event, there can be between 300-1,000 unreported events."
This rule of thumb, based on 9,571 reported events, would mean that between 2.8 million and 9.6 million total events (unreported & reported) occurred over the 5-year period from July 1, 2000, to June 30, 2005. On an annualized basis, this would mean that about 600,000-2 million events/year could involve PCA.
These numbers are unacceptable in what should be an era of increasing patient safety. Says Dr. Hicks, "Further study would need to be done to ascertain the total number of PCA events, but the problem is extensive in my opinion." The picture is already pretty clear, but there is more to the data.
When the study looked at the number of events that caused harm, there were 624 records of PCA associated with harm, corresponding to 6.5% of the patients. Again, while 6.5% may seem small, as the study found, "By comparison, during the same period, only 1.5% of all other errors reported to MedMarx led to harm. This represents a fourfold higher relative risk of harm for PCA events."
"All health care disciplines were implicated in the errors, including physicians, pharmacists, and nurses" he said. "Therefore, it will take an interdisciplinary team to resolve the problems."
Dr. Hicks’ retrospective study of the magnitude, frequency, and nature of nonharmful and harmful medication errors associated with patient-controlled analgesia covered a 5-year review period with 919,241 medication errors records from 801 reporting health care facilities. The analysis was based on the international voluntary medication error reporting program, MedMarx. Dr. Hicks is now a professor a Western University College of Graduate Nursing, Pomona, Calif.
"Our analysis was in no means trying to discourage the use of PCA pumps. Many studies have shown the benefits of using PCA, including improved pain management, better utilization of nursing resources, increased patient satisfaction, and improved pulmonary function.
"However, this is clearly an indication that standardization needs to occur and organizations should invest in training and policies and procedures as well as equipment – all areas to promote safety."
Moreover, although elimination of error is critical, studies have shown even a correctly programmed PCA pump poses patient safety risks.
Appropriate doses of opiates can suppress respiration and decrease heart rate and blood pressure. Episodes of bradypnea and desaturation can escalate to respiratory depression requiring rescue, according to come via Ray Maddox, Pharm. D., of St. Joseph’s/Candler Health System and his colleagues, who studied an intravenous infusion safety initiative at the 644-bed, tertiary-care, magnet system to evaluate how "smart" technology can help avert high-risk adverse drug events and improve patient outcomes.
These investigators further point out that the success rate for in-hospital cardiopulmonary resuscitation remains less than one in five patients. If detected early, most cases of opioid-induced respiratory depression can be treated with naloxone. However, severe cases can be fatal. The risk of patient harm from medication errors with PCA pumps is 3.5 times the risk from any other type of medication administration error.
The researchers recommend the following: "Capnographic monitoring – measurements of ventilation using respiration and exhaled carbon dioxide – is particularly important because it can provide an earlier warning of respiratory depression than pulse oximetry in some patient populations."
In short, although there are many benefits to PCA usage, for improved patient safety, reduce the risks and monitor continuously to detect respiratory depression events.
With the desire to reduce errors and improve patient safety with the use of patient-controlled analgesia, a safety checklist is being developed by the Physician-Patient Alliance for Health and Safety. For more on this initiative, contact Michael Wong [email protected].
The Physician-Patient Alliance for Health & Safety is an advocacy group devoted to improving patient health and safety. PPAHS comprises physicians, patients, individuals, and organizations. PPAHS reports having no financial conflicts of interest and not having received funding or grants. It recently conducted a survey on the American Society of Anesthesiologists Standards & Anesthesia Patient Safety Foundation Recommendations, available online. PPAHS welcomes inquiries regarding financial assistance to implement the safety checklist initiative.
How often do errors with patient-controlled analgesia occur? More often than we know, research suggests.
Researchers who studied more than 900,000 medication record errors say that the 1% of errors related to patient-controlled analgesia (PCA) is probably just the tip of the iceberg. Although 1% may seem insignificant, this analysis was based on the voluntary medication error reporting, says lead researcher Rodney Hicks, Ph.D., who at that time of the study was manager, patient safety research and practice, U.S. Pharmacopeia.
"Although generalization of voluntary reported findings to the general population should be done cautiously," he points out, that "the general rule of thumb is that for every reported event, there can be between 300-1,000 unreported events."
This rule of thumb, based on 9,571 reported events, would mean that between 2.8 million and 9.6 million total events (unreported & reported) occurred over the 5-year period from July 1, 2000, to June 30, 2005. On an annualized basis, this would mean that about 600,000-2 million events/year could involve PCA.
These numbers are unacceptable in what should be an era of increasing patient safety. Says Dr. Hicks, "Further study would need to be done to ascertain the total number of PCA events, but the problem is extensive in my opinion." The picture is already pretty clear, but there is more to the data.
When the study looked at the number of events that caused harm, there were 624 records of PCA associated with harm, corresponding to 6.5% of the patients. Again, while 6.5% may seem small, as the study found, "By comparison, during the same period, only 1.5% of all other errors reported to MedMarx led to harm. This represents a fourfold higher relative risk of harm for PCA events."
"All health care disciplines were implicated in the errors, including physicians, pharmacists, and nurses" he said. "Therefore, it will take an interdisciplinary team to resolve the problems."
Dr. Hicks’ retrospective study of the magnitude, frequency, and nature of nonharmful and harmful medication errors associated with patient-controlled analgesia covered a 5-year review period with 919,241 medication errors records from 801 reporting health care facilities. The analysis was based on the international voluntary medication error reporting program, MedMarx. Dr. Hicks is now a professor a Western University College of Graduate Nursing, Pomona, Calif.
"Our analysis was in no means trying to discourage the use of PCA pumps. Many studies have shown the benefits of using PCA, including improved pain management, better utilization of nursing resources, increased patient satisfaction, and improved pulmonary function.
"However, this is clearly an indication that standardization needs to occur and organizations should invest in training and policies and procedures as well as equipment – all areas to promote safety."
Moreover, although elimination of error is critical, studies have shown even a correctly programmed PCA pump poses patient safety risks.
Appropriate doses of opiates can suppress respiration and decrease heart rate and blood pressure. Episodes of bradypnea and desaturation can escalate to respiratory depression requiring rescue, according to come via Ray Maddox, Pharm. D., of St. Joseph’s/Candler Health System and his colleagues, who studied an intravenous infusion safety initiative at the 644-bed, tertiary-care, magnet system to evaluate how "smart" technology can help avert high-risk adverse drug events and improve patient outcomes.
These investigators further point out that the success rate for in-hospital cardiopulmonary resuscitation remains less than one in five patients. If detected early, most cases of opioid-induced respiratory depression can be treated with naloxone. However, severe cases can be fatal. The risk of patient harm from medication errors with PCA pumps is 3.5 times the risk from any other type of medication administration error.
The researchers recommend the following: "Capnographic monitoring – measurements of ventilation using respiration and exhaled carbon dioxide – is particularly important because it can provide an earlier warning of respiratory depression than pulse oximetry in some patient populations."
In short, although there are many benefits to PCA usage, for improved patient safety, reduce the risks and monitor continuously to detect respiratory depression events.
With the desire to reduce errors and improve patient safety with the use of patient-controlled analgesia, a safety checklist is being developed by the Physician-Patient Alliance for Health and Safety. For more on this initiative, contact Michael Wong [email protected].
The Physician-Patient Alliance for Health & Safety is an advocacy group devoted to improving patient health and safety. PPAHS comprises physicians, patients, individuals, and organizations. PPAHS reports having no financial conflicts of interest and not having received funding or grants. It recently conducted a survey on the American Society of Anesthesiologists Standards & Anesthesia Patient Safety Foundation Recommendations, available online. PPAHS welcomes inquiries regarding financial assistance to implement the safety checklist initiative.