User login
Cardiovascular cost of smoking may last up to 25 years
Quitting smoking significantly reduces the risk of cardiovascular disease, but past smokers are still at elevated cardiovascular risk, compared with nonsmokers, for up to 25 years after smoking cessation, research in JAMA suggests.
A retrospective analysis of data from 8,770 individuals in the Framingham Heart Study compared the incidence of myocardial infarction, stroke, heart failure, or cardiovascular death in ever-smokers with that of never smokers.
Only 40% of the total cohort had never smoked. Of the 4,115 current smokers at baseline, 38.6% quit during the course of the study and did not relapse but 51.4% continued to smoke until they developed cardiovascular disease or dropped out of the study.
Current smokers had a significant 4.68-fold higher incidence of cardiovascular disease, compared with those who had never smoked, but those who stopped smoking showed a 39% decline in their risk of cardiovascular disease within 5 years of cessation.
However, individuals who were formerly heavy smokers – defined as at least 20 pack-years of smoking – retained a risk of cardiovascular disease 25% higher than that of never smokers until 10-15 years after quitting smoking. At 16 years, the 95% confidence interval for cardiovascular disease risk among former smokers versus that of never smokers finally and consistently included the null value of 1.
The study pooled two cohorts; the original cohort, who attended their fourth examination during 1954-1958 and an offspring cohort who attended their first examination during 1971-1975. The authors saw a difference between the two cohorts in the time course of cardiovascular disease risk in heavy smokers.
In the original cohort, former heavy smoking ceased to be significantly associated with increased cardiovascular disease risk within 5-10 years of cessation, but in the offspring cohort, it took 25 years after cessation for the incidence to decline to the same level of risk seen in never smokers.
“The upper estimate of this time course is a decade longer than that of the Nurses’ Health Study results for coronary heart disease and cardiovascular death and more than 20 years longer than in some prior reports for coronary heart disease and stroke,” wrote Meredith S. Duncan from the division of cardiovascular medicine at the Vanderbilt University Medical Center, Nashville, Tenn., and coauthors. “Although the exact amount of time after quitting at which former smokers’ CVD risk ceases to differ significantly from that of never smokers is unknown (and may further depend on cumulative exposure), these findings support a longer time course of risk reduction than was previously thought, yielding implications for CVD risk stratification of former smokers.”
However, they did note that the study could not account for environmental tobacco smoke exposure and that the participants were mostly of white European ancestry, which limited the generalizability of the findings to other populations.
The Framingham Health Study was supported by the National Heart, Lung, and Blood Institute. One author declared a consultancy with a pharmaceutical company on a proposed clinical trial. No other conflicts of interest were declared.
SOURCE: Duncan M et al. JAMA 2019. doi: 10.1001/jama.2019.10298.
Quitting smoking significantly reduces the risk of cardiovascular disease, but past smokers are still at elevated cardiovascular risk, compared with nonsmokers, for up to 25 years after smoking cessation, research in JAMA suggests.
A retrospective analysis of data from 8,770 individuals in the Framingham Heart Study compared the incidence of myocardial infarction, stroke, heart failure, or cardiovascular death in ever-smokers with that of never smokers.
Only 40% of the total cohort had never smoked. Of the 4,115 current smokers at baseline, 38.6% quit during the course of the study and did not relapse but 51.4% continued to smoke until they developed cardiovascular disease or dropped out of the study.
Current smokers had a significant 4.68-fold higher incidence of cardiovascular disease, compared with those who had never smoked, but those who stopped smoking showed a 39% decline in their risk of cardiovascular disease within 5 years of cessation.
However, individuals who were formerly heavy smokers – defined as at least 20 pack-years of smoking – retained a risk of cardiovascular disease 25% higher than that of never smokers until 10-15 years after quitting smoking. At 16 years, the 95% confidence interval for cardiovascular disease risk among former smokers versus that of never smokers finally and consistently included the null value of 1.
The study pooled two cohorts; the original cohort, who attended their fourth examination during 1954-1958 and an offspring cohort who attended their first examination during 1971-1975. The authors saw a difference between the two cohorts in the time course of cardiovascular disease risk in heavy smokers.
In the original cohort, former heavy smoking ceased to be significantly associated with increased cardiovascular disease risk within 5-10 years of cessation, but in the offspring cohort, it took 25 years after cessation for the incidence to decline to the same level of risk seen in never smokers.
“The upper estimate of this time course is a decade longer than that of the Nurses’ Health Study results for coronary heart disease and cardiovascular death and more than 20 years longer than in some prior reports for coronary heart disease and stroke,” wrote Meredith S. Duncan from the division of cardiovascular medicine at the Vanderbilt University Medical Center, Nashville, Tenn., and coauthors. “Although the exact amount of time after quitting at which former smokers’ CVD risk ceases to differ significantly from that of never smokers is unknown (and may further depend on cumulative exposure), these findings support a longer time course of risk reduction than was previously thought, yielding implications for CVD risk stratification of former smokers.”
However, they did note that the study could not account for environmental tobacco smoke exposure and that the participants were mostly of white European ancestry, which limited the generalizability of the findings to other populations.
The Framingham Health Study was supported by the National Heart, Lung, and Blood Institute. One author declared a consultancy with a pharmaceutical company on a proposed clinical trial. No other conflicts of interest were declared.
SOURCE: Duncan M et al. JAMA 2019. doi: 10.1001/jama.2019.10298.
Quitting smoking significantly reduces the risk of cardiovascular disease, but past smokers are still at elevated cardiovascular risk, compared with nonsmokers, for up to 25 years after smoking cessation, research in JAMA suggests.
A retrospective analysis of data from 8,770 individuals in the Framingham Heart Study compared the incidence of myocardial infarction, stroke, heart failure, or cardiovascular death in ever-smokers with that of never smokers.
Only 40% of the total cohort had never smoked. Of the 4,115 current smokers at baseline, 38.6% quit during the course of the study and did not relapse but 51.4% continued to smoke until they developed cardiovascular disease or dropped out of the study.
Current smokers had a significant 4.68-fold higher incidence of cardiovascular disease, compared with those who had never smoked, but those who stopped smoking showed a 39% decline in their risk of cardiovascular disease within 5 years of cessation.
However, individuals who were formerly heavy smokers – defined as at least 20 pack-years of smoking – retained a risk of cardiovascular disease 25% higher than that of never smokers until 10-15 years after quitting smoking. At 16 years, the 95% confidence interval for cardiovascular disease risk among former smokers versus that of never smokers finally and consistently included the null value of 1.
The study pooled two cohorts; the original cohort, who attended their fourth examination during 1954-1958 and an offspring cohort who attended their first examination during 1971-1975. The authors saw a difference between the two cohorts in the time course of cardiovascular disease risk in heavy smokers.
In the original cohort, former heavy smoking ceased to be significantly associated with increased cardiovascular disease risk within 5-10 years of cessation, but in the offspring cohort, it took 25 years after cessation for the incidence to decline to the same level of risk seen in never smokers.
“The upper estimate of this time course is a decade longer than that of the Nurses’ Health Study results for coronary heart disease and cardiovascular death and more than 20 years longer than in some prior reports for coronary heart disease and stroke,” wrote Meredith S. Duncan from the division of cardiovascular medicine at the Vanderbilt University Medical Center, Nashville, Tenn., and coauthors. “Although the exact amount of time after quitting at which former smokers’ CVD risk ceases to differ significantly from that of never smokers is unknown (and may further depend on cumulative exposure), these findings support a longer time course of risk reduction than was previously thought, yielding implications for CVD risk stratification of former smokers.”
However, they did note that the study could not account for environmental tobacco smoke exposure and that the participants were mostly of white European ancestry, which limited the generalizability of the findings to other populations.
The Framingham Health Study was supported by the National Heart, Lung, and Blood Institute. One author declared a consultancy with a pharmaceutical company on a proposed clinical trial. No other conflicts of interest were declared.
SOURCE: Duncan M et al. JAMA 2019. doi: 10.1001/jama.2019.10298.
FROM JAMA
Key clinical point:
Major finding: In the offspring cohort, heavy smokers showed elevated incidence of CVD for up to 25 years after quitting smoking.
Study details: A retrospective analysis of data from 8,770 individuals in the Framingham Heart Study.
Disclosures: The Framingham Health Study was supported by the National Heart, Lung, and Blood Institute. One author declared a consultancy with a pharmaceutical company on a proposed clinical trial. No other conflicts of interest were declared.
Source: Duncan M et al. JAMA. 2019. doi: 10.1001/jama.2019.10298.
FDA approves Xenleta for community-acquired bacterial pneumonia treatment
The Food and Drug Administration has announced its approval of lefamulin (Xenleta) for the treatment of community-acquired bacterial pneumonia in adults.
Approval was based on results of two clinical trials assessing a total of 1,289 people with community-acquired bacterial pneumonia. In these trials, lefamulin was compared with moxifloxacin with and without linezolid. Patients who received lefamulin had similar rates of treatment success as those taking moxifloxacin alone or moxifloxacin plus linezolid.
The most common adverse reactions associated with lefamulin include diarrhea, nausea, reactions at the injection site, elevated liver enzymes, and vomiting. Patients with prolonged QT interval, patients with arrhythmias, patients receiving treatment with antiarrhythmic agents, and patients receiving other drugs that prolong the QT interval are contraindicated. In addition, because of evidence of fetal harm in animal studies, pregnant women should be advised of potential risks before receiving lefamulin.
“This new drug provides another option for the treatment of patients with community-acquired bacterial pneumonia, a serious disease. For managing this serious disease, it is important for physicians and patients to have treatment options,” Ed Cox, MD, MPH, director of the FDA’s Office of Antimicrobial Products, said in the press release.
The Food and Drug Administration has announced its approval of lefamulin (Xenleta) for the treatment of community-acquired bacterial pneumonia in adults.
Approval was based on results of two clinical trials assessing a total of 1,289 people with community-acquired bacterial pneumonia. In these trials, lefamulin was compared with moxifloxacin with and without linezolid. Patients who received lefamulin had similar rates of treatment success as those taking moxifloxacin alone or moxifloxacin plus linezolid.
The most common adverse reactions associated with lefamulin include diarrhea, nausea, reactions at the injection site, elevated liver enzymes, and vomiting. Patients with prolonged QT interval, patients with arrhythmias, patients receiving treatment with antiarrhythmic agents, and patients receiving other drugs that prolong the QT interval are contraindicated. In addition, because of evidence of fetal harm in animal studies, pregnant women should be advised of potential risks before receiving lefamulin.
“This new drug provides another option for the treatment of patients with community-acquired bacterial pneumonia, a serious disease. For managing this serious disease, it is important for physicians and patients to have treatment options,” Ed Cox, MD, MPH, director of the FDA’s Office of Antimicrobial Products, said in the press release.
The Food and Drug Administration has announced its approval of lefamulin (Xenleta) for the treatment of community-acquired bacterial pneumonia in adults.
Approval was based on results of two clinical trials assessing a total of 1,289 people with community-acquired bacterial pneumonia. In these trials, lefamulin was compared with moxifloxacin with and without linezolid. Patients who received lefamulin had similar rates of treatment success as those taking moxifloxacin alone or moxifloxacin plus linezolid.
The most common adverse reactions associated with lefamulin include diarrhea, nausea, reactions at the injection site, elevated liver enzymes, and vomiting. Patients with prolonged QT interval, patients with arrhythmias, patients receiving treatment with antiarrhythmic agents, and patients receiving other drugs that prolong the QT interval are contraindicated. In addition, because of evidence of fetal harm in animal studies, pregnant women should be advised of potential risks before receiving lefamulin.
“This new drug provides another option for the treatment of patients with community-acquired bacterial pneumonia, a serious disease. For managing this serious disease, it is important for physicians and patients to have treatment options,” Ed Cox, MD, MPH, director of the FDA’s Office of Antimicrobial Products, said in the press release.
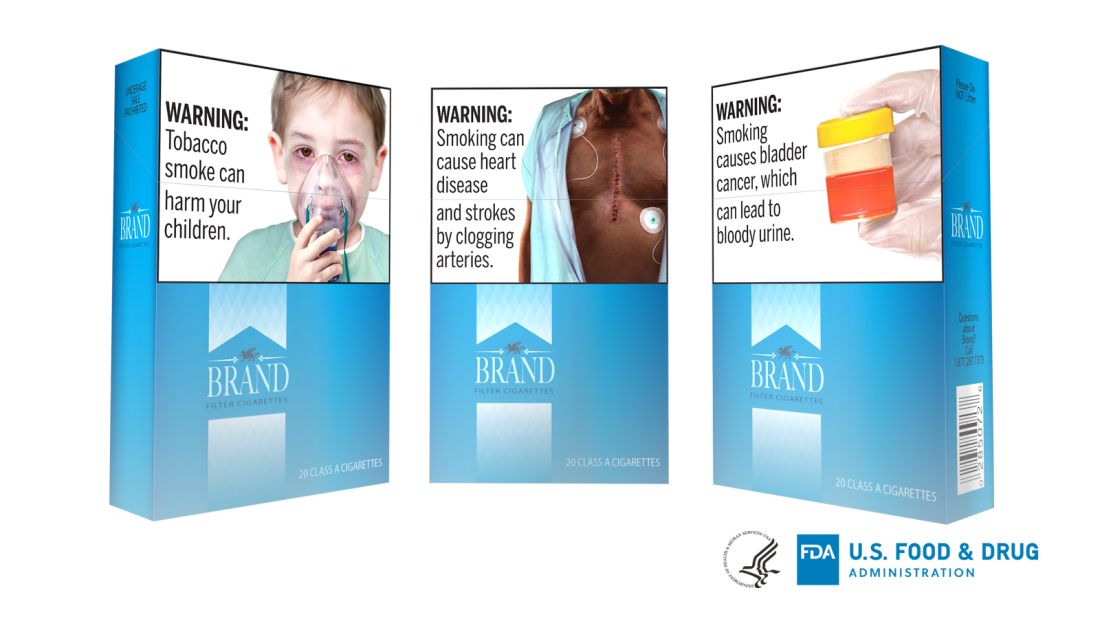
FDA takes another swing at updating cigarette pack warnings
illustrating the harms of smoking, but this could be subjected to legal challenge.
Several years ago, tobacco companies filed a lawsuit, which ultimately shut down a similar proposal.
The warnings focus on lesser-known complications – including diabetes, cataracts, gangrene, stroke, bladder cancer, erectile dysfunction, and obstructive pulmonary disease – and would take up the top half of the front and back of cigarette packs, and at least the top 20% of print advertisements. Each pack and ad would be required to carry 1 of the 13 proposed warnings, according to the announcement.
The approach would be similar to, but not as aggressive as Canada’s. For years, cigarettes packs sold in Canada have included disturbing photographs of diseased lungs, rotted teeth, and dying patients. The lasting impact of such imagery has been demonstrated in the literature (for example, Am J Prev Med. 2007 Mar;32[3]:202-9).
The new proposal is the FDA’s second attempt to enact something comparable in the United States, after being directed to do so by the Tobacco Control Act of 2009.
The first effort to add strong, illustrated warnings to cigarette packs was widely backed by medical groups, but challenged in the courts by R.J. Reynolds and other tobacco companies, and blocked on appeal in 2012 as an abridgment of commercial free speech. The federal government dropped the case in 2013.
The American Lung Association and other public health groups subsequently sued the FDA in 2016 to enact the Tobacco Act mandate. Subsequently, a federal judge ordered the agency to publish a new rule by August 2019, and issue a final rule in March 2020.
This time around, the FDA “took the necessary time to get these new proposed warnings right ... based on – and within the limits of – both science and the law,” the agency said. The new images, though graphic, are less disturbing than those used in Canada and the agency’s previous proposals, which included an apparent corpse with a sternotomy. The 1-800-Quit-Now cessation hotline number, which was a sticking point in the 2012 ruling, has also been dropped.
When asked about the new efforts, R.J. Reynolds spokesperson Kaelan Hollon said, “We are carefully reviewing FDA’s latest proposal for graphic warnings on cigarettes. We firmly support public awareness of the harms of smoking cigarettes, but the manner in which those messages are delivered to the public cannot run afoul of the First Amendment protections that apply to all speakers, including cigarette manufacturers.”
Warnings on U.S. cigarettes haven’t changed since 1984, when the risks of lung cancer, heart disease, emphysema, and pregnancy complications were added to the side of cigarette packs. With time, the FDA said the surgeon general’s warnings have become “virtually invisible” to consumers.
The American Lung Association, American Academy of Pediatrics, and other plaintiffs in the 2016 suit called the new proposal a “dramatic improvement” over the current situation and “long overdue” in a joint statement on Aug. 15.
Although rates have declined substantially in recent decades, about 34.3 million U.S. adults and almost 1.4 million teenagers still smoke. The habit kills about a half million Americans every year, at a health cost of more than $300 billion, the FDA said.
Comments on the proposed rule are being accepted through Oct. 15. The agency is open to suggestions for alternative text and images.
illustrating the harms of smoking, but this could be subjected to legal challenge.
Several years ago, tobacco companies filed a lawsuit, which ultimately shut down a similar proposal.
The warnings focus on lesser-known complications – including diabetes, cataracts, gangrene, stroke, bladder cancer, erectile dysfunction, and obstructive pulmonary disease – and would take up the top half of the front and back of cigarette packs, and at least the top 20% of print advertisements. Each pack and ad would be required to carry 1 of the 13 proposed warnings, according to the announcement.
The approach would be similar to, but not as aggressive as Canada’s. For years, cigarettes packs sold in Canada have included disturbing photographs of diseased lungs, rotted teeth, and dying patients. The lasting impact of such imagery has been demonstrated in the literature (for example, Am J Prev Med. 2007 Mar;32[3]:202-9).
The new proposal is the FDA’s second attempt to enact something comparable in the United States, after being directed to do so by the Tobacco Control Act of 2009.
The first effort to add strong, illustrated warnings to cigarette packs was widely backed by medical groups, but challenged in the courts by R.J. Reynolds and other tobacco companies, and blocked on appeal in 2012 as an abridgment of commercial free speech. The federal government dropped the case in 2013.
The American Lung Association and other public health groups subsequently sued the FDA in 2016 to enact the Tobacco Act mandate. Subsequently, a federal judge ordered the agency to publish a new rule by August 2019, and issue a final rule in March 2020.
This time around, the FDA “took the necessary time to get these new proposed warnings right ... based on – and within the limits of – both science and the law,” the agency said. The new images, though graphic, are less disturbing than those used in Canada and the agency’s previous proposals, which included an apparent corpse with a sternotomy. The 1-800-Quit-Now cessation hotline number, which was a sticking point in the 2012 ruling, has also been dropped.
When asked about the new efforts, R.J. Reynolds spokesperson Kaelan Hollon said, “We are carefully reviewing FDA’s latest proposal for graphic warnings on cigarettes. We firmly support public awareness of the harms of smoking cigarettes, but the manner in which those messages are delivered to the public cannot run afoul of the First Amendment protections that apply to all speakers, including cigarette manufacturers.”
Warnings on U.S. cigarettes haven’t changed since 1984, when the risks of lung cancer, heart disease, emphysema, and pregnancy complications were added to the side of cigarette packs. With time, the FDA said the surgeon general’s warnings have become “virtually invisible” to consumers.
The American Lung Association, American Academy of Pediatrics, and other plaintiffs in the 2016 suit called the new proposal a “dramatic improvement” over the current situation and “long overdue” in a joint statement on Aug. 15.
Although rates have declined substantially in recent decades, about 34.3 million U.S. adults and almost 1.4 million teenagers still smoke. The habit kills about a half million Americans every year, at a health cost of more than $300 billion, the FDA said.
Comments on the proposed rule are being accepted through Oct. 15. The agency is open to suggestions for alternative text and images.
illustrating the harms of smoking, but this could be subjected to legal challenge.
Several years ago, tobacco companies filed a lawsuit, which ultimately shut down a similar proposal.
The warnings focus on lesser-known complications – including diabetes, cataracts, gangrene, stroke, bladder cancer, erectile dysfunction, and obstructive pulmonary disease – and would take up the top half of the front and back of cigarette packs, and at least the top 20% of print advertisements. Each pack and ad would be required to carry 1 of the 13 proposed warnings, according to the announcement.
The approach would be similar to, but not as aggressive as Canada’s. For years, cigarettes packs sold in Canada have included disturbing photographs of diseased lungs, rotted teeth, and dying patients. The lasting impact of such imagery has been demonstrated in the literature (for example, Am J Prev Med. 2007 Mar;32[3]:202-9).
The new proposal is the FDA’s second attempt to enact something comparable in the United States, after being directed to do so by the Tobacco Control Act of 2009.
The first effort to add strong, illustrated warnings to cigarette packs was widely backed by medical groups, but challenged in the courts by R.J. Reynolds and other tobacco companies, and blocked on appeal in 2012 as an abridgment of commercial free speech. The federal government dropped the case in 2013.
The American Lung Association and other public health groups subsequently sued the FDA in 2016 to enact the Tobacco Act mandate. Subsequently, a federal judge ordered the agency to publish a new rule by August 2019, and issue a final rule in March 2020.
This time around, the FDA “took the necessary time to get these new proposed warnings right ... based on – and within the limits of – both science and the law,” the agency said. The new images, though graphic, are less disturbing than those used in Canada and the agency’s previous proposals, which included an apparent corpse with a sternotomy. The 1-800-Quit-Now cessation hotline number, which was a sticking point in the 2012 ruling, has also been dropped.
When asked about the new efforts, R.J. Reynolds spokesperson Kaelan Hollon said, “We are carefully reviewing FDA’s latest proposal for graphic warnings on cigarettes. We firmly support public awareness of the harms of smoking cigarettes, but the manner in which those messages are delivered to the public cannot run afoul of the First Amendment protections that apply to all speakers, including cigarette manufacturers.”
Warnings on U.S. cigarettes haven’t changed since 1984, when the risks of lung cancer, heart disease, emphysema, and pregnancy complications were added to the side of cigarette packs. With time, the FDA said the surgeon general’s warnings have become “virtually invisible” to consumers.
The American Lung Association, American Academy of Pediatrics, and other plaintiffs in the 2016 suit called the new proposal a “dramatic improvement” over the current situation and “long overdue” in a joint statement on Aug. 15.
Although rates have declined substantially in recent decades, about 34.3 million U.S. adults and almost 1.4 million teenagers still smoke. The habit kills about a half million Americans every year, at a health cost of more than $300 billion, the FDA said.
Comments on the proposed rule are being accepted through Oct. 15. The agency is open to suggestions for alternative text and images.
FDA approves drug combo to treat highly resistant TB
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
NEWS FROM THE FDA
Asthma hospitalization in kids linked with doubled migraine incidence
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
REPORTING FROM AHS 2019
Study: Cardiac biomarkers predicted CV events in CAP
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
FROM CHEST
Exposure to outdoor air pollutants linked to increased emphysema
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
FROM JAMA
Procalcitonin advocated to help rule out bacterial infections
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
EXPERT ANALYSIS FROM PHM 2019
Vaping in 2019: Risk vs. reward
The prevalence and popularity of electronic cigarettes or “vaping” have grown dramatically over the last several years in the United States. Although new studies targeting these products are being done at increasing frequency, there remains a relative paucity of data regarding the long-term risks. Proponents argue that they can be used as a cessation tool for smokers, or failing that, a safer replacement for traditional cigarettes. Opponents make the case that the perception of safety could contribute to increased use in people who may have otherwise never smoked, leading to an overall increase in nicotine use and addiction. This is most readily seen in the adolescent population, where use has skyrocketed, leading to concerns about how electronic cigarettes are marketed to youth, as well as the ease of access.
Basics of vaping (devices)
In its most basic form, an electronic cigarette consists of a battery that powers a heating coil. This heating coil applies heat to a wick, which is soaked in liquid, “vape juice,” converting it into a vapor that is then directly inhaled. However, there can be many variations on this simple theme. Early generation products resembled traditional cigarettes in size and shape and were marketed as smoking cessation aids. Newer devices have abandoned this look and strategy. Preloaded cartridges have been replaced by large tanks that the user can fill with the liquid of their choosing. Multiple tanks can be purchased for a single device, enabling the user to have multiple flavors or various levels of nicotine dosing on hand for quick changing, depending on user preference or mood. Additionally, there are variable voltage settings, resulting in different styles of vapor and/or “throat hit” (the description of the desired burning vs smooth effect of the vapor on the oropharynx). This type of device invites experimentation. Multiple flavors can be used in isolation or mixed together at various temperatures. It no longer resembles classic cigarettes, and the flavor and experience are more prominently promoted. One can see that this device has more appeal to a “never smoker” than the original products, and there is concern that it is being marketed as such with some success (Dinakar C, et al. N Engl J Med. 2016;375[14]:1372).
E-liquid
Perhaps more important than the devices themselves is an understanding of the components of the liquid used to generate the inhaled aerosol.
Typically, four components are present:
• Propylene glycol
• Vegetable glycerin
• Flavoring
• Nicotine
The first two components are generally considered nontoxic, based on their use as food additives. However, inhalation is a novel route of entry and the long-term effects on the respiratory tract are unclear.
The third component, “flavorings,” is a catch-all term for the hundreds of different flavors and styles of e-liquids available today, ranging from menthol to fruit or candy and everything in between. It is difficult to account for all the potential effects of the numerous flavorings being used, especially when some are combined by the end user to various degrees.
Nicotine is present, specified in varying doses. However, vaping style, experience, and type of device used can dramatically affect how much is absorbed, making dosages difficult to predict. Additionally, labeled doses are prone to wide ranges of error (Schraufnagel DE, et al. Am J Respir Crit Care Med. 2014;190[6]:611).
What are the risks?
Cancer
A handful of known carcinogens can be found in inhaled vapor, including formaldehyde, acetaldehyde, acrolein, toluene, and nitrosamines. However, they are present in far lower concentrations than in traditional cigarettes (Goniewicz ML, et al. JAMA Netw Open. 2018;1[8]e185937). This leads to the natural assumption that vaping, while not benign, poses a much lower cancer risk when compared with smoking. Whether that is borne out in the long term remains to be seen.
Pulmonary function
The long-term effect on pulmonary function is not known. Small studies have shown no significant changes to spirometry after acute exposure to vapor. More data are needed in this area (Palazzolo DL. Frontiers Public Health. 2013;1[56]1-20).
Wound healing
An animal study has shown evidence of poor wound healing extrapolated from skin flap necrosis in rats. Exposure to vapor vs smoke yielded similar results, and both were worse than the sham arm (Troiano C, et al. JAMA Facial Plast Surg. 2019;21[1]:5). While it is difficult to know how to apply this clinically, it may be prudent to advise patients to abstain while in preparation for elective surgery.
Cardiovascular/stroke
Much of the cardiovascular toxicity from cigarette use is tied to the myriad of complex toxic particles produced in inhaled smoke, the vast majority of which are not present in e-cigarette vapor. While nicotine itself has known acute cardiovascular effects, including tachycardia and vasoconstriction, a tolerance to these effects occurs over time. Previous evaluations of nicotine replacement therapies and smokeless tobacco for their cardiovascular effects have had mixed results. But, there appears to be a trend toward minimal cardiovascular risk when using “cleaner” products, such as nicotine replacement therapy compared with smokeless tobacco (Benowitz NL, et al. Nature Rev Cardiol. 2017;14[8]:447). Whether this can be extrapolated to electronic cigarette use is unknown but is encouraging.
Alternative toxicity
In addition to the above risks that are in comparison to traditional smoking, vaping also introduces novel toxicities. There are case reports of lipoid pneumonia, ARDS, hypersensitivity pneumonitis, eosinophilic pneumonia, and diffuse alveola hemorrhage. Burns from malfunctioning devices must also be considered, as there is a wide array of products available, at differing levels of build quality.
Toxic oral ingestion of nicotine, especially by children, has led to increased calls to poison centers. For a small child, this can be fatal. Regulation of labels and containers could curtail this issue. But, public education regarding the toxicity of these substances when ingested in large quantities is also important. If there is a lack of understanding about this danger, then typical safeguards are easily overlooked by individual users.
Are there benefits?
Smoking cessation
Compared with other products, such as nicotine patches, gum, and pharmaceutical methods, e-cigarettes most closely mimic the actual experience of smoking. For some, the habit and ritual of smoking is as much a part of the addiction as nicotine. Vaping has the potential to help alleviate this difficult aspect of cessation. Data involving early generation products failed to show a significant advantage. Newer devices that are more pleasurable to use and offer more efficient nicotine delivery may be more effective. Indeed, a recent study in the New England Journal of Medicine from this year demonstrated improved smoking cessation compared with traditional methods, using second generation vape devices (Hajek P, et al. N Engl J Med. 2019;380[7]629). It will be interesting to see if this can be repeatable going forward and if protocols can be established to maximize effectiveness.
As outlined above, it is difficult to make definitive conclusions or recommendations regarding electronic cigarette use at the present time. The risk of cancer and cardiopulmonary disease is likely to be significantly lower but not eliminated. Use as a smoking cessation aid is starting to show promise. Even without cessation, ongoing vaping is likely to be safer than ongoing smoking. Two caveats to this remain: some patients, in an effort to quit smoking, may take up vaping but eventually become “dual users.” This scenario has been associated with higher toxic exposure and possibly worse outcomes. The second caveat is that while there is promise to using this as a cessation tool, it should not yet replace other more well-studied, first-line agents in this regard. It should, perhaps, target patients who are motivated to quit but have failed more traditional methods. Finally, there continues to be concern that vaping could appeal to never smokers, given its perceived safety profile and ease of use in public places. This could lead to an overall increase in nicotine addiction, which could be a significant step backwards.
Dr. Clark is Assistant Professor, Pulmonary and Critical Care Medicine, UT Southwestern Medical Center, Dallas, Texas.
The prevalence and popularity of electronic cigarettes or “vaping” have grown dramatically over the last several years in the United States. Although new studies targeting these products are being done at increasing frequency, there remains a relative paucity of data regarding the long-term risks. Proponents argue that they can be used as a cessation tool for smokers, or failing that, a safer replacement for traditional cigarettes. Opponents make the case that the perception of safety could contribute to increased use in people who may have otherwise never smoked, leading to an overall increase in nicotine use and addiction. This is most readily seen in the adolescent population, where use has skyrocketed, leading to concerns about how electronic cigarettes are marketed to youth, as well as the ease of access.
Basics of vaping (devices)
In its most basic form, an electronic cigarette consists of a battery that powers a heating coil. This heating coil applies heat to a wick, which is soaked in liquid, “vape juice,” converting it into a vapor that is then directly inhaled. However, there can be many variations on this simple theme. Early generation products resembled traditional cigarettes in size and shape and were marketed as smoking cessation aids. Newer devices have abandoned this look and strategy. Preloaded cartridges have been replaced by large tanks that the user can fill with the liquid of their choosing. Multiple tanks can be purchased for a single device, enabling the user to have multiple flavors or various levels of nicotine dosing on hand for quick changing, depending on user preference or mood. Additionally, there are variable voltage settings, resulting in different styles of vapor and/or “throat hit” (the description of the desired burning vs smooth effect of the vapor on the oropharynx). This type of device invites experimentation. Multiple flavors can be used in isolation or mixed together at various temperatures. It no longer resembles classic cigarettes, and the flavor and experience are more prominently promoted. One can see that this device has more appeal to a “never smoker” than the original products, and there is concern that it is being marketed as such with some success (Dinakar C, et al. N Engl J Med. 2016;375[14]:1372).
E-liquid
Perhaps more important than the devices themselves is an understanding of the components of the liquid used to generate the inhaled aerosol.
Typically, four components are present:
• Propylene glycol
• Vegetable glycerin
• Flavoring
• Nicotine
The first two components are generally considered nontoxic, based on their use as food additives. However, inhalation is a novel route of entry and the long-term effects on the respiratory tract are unclear.
The third component, “flavorings,” is a catch-all term for the hundreds of different flavors and styles of e-liquids available today, ranging from menthol to fruit or candy and everything in between. It is difficult to account for all the potential effects of the numerous flavorings being used, especially when some are combined by the end user to various degrees.
Nicotine is present, specified in varying doses. However, vaping style, experience, and type of device used can dramatically affect how much is absorbed, making dosages difficult to predict. Additionally, labeled doses are prone to wide ranges of error (Schraufnagel DE, et al. Am J Respir Crit Care Med. 2014;190[6]:611).
What are the risks?
Cancer
A handful of known carcinogens can be found in inhaled vapor, including formaldehyde, acetaldehyde, acrolein, toluene, and nitrosamines. However, they are present in far lower concentrations than in traditional cigarettes (Goniewicz ML, et al. JAMA Netw Open. 2018;1[8]e185937). This leads to the natural assumption that vaping, while not benign, poses a much lower cancer risk when compared with smoking. Whether that is borne out in the long term remains to be seen.
Pulmonary function
The long-term effect on pulmonary function is not known. Small studies have shown no significant changes to spirometry after acute exposure to vapor. More data are needed in this area (Palazzolo DL. Frontiers Public Health. 2013;1[56]1-20).
Wound healing
An animal study has shown evidence of poor wound healing extrapolated from skin flap necrosis in rats. Exposure to vapor vs smoke yielded similar results, and both were worse than the sham arm (Troiano C, et al. JAMA Facial Plast Surg. 2019;21[1]:5). While it is difficult to know how to apply this clinically, it may be prudent to advise patients to abstain while in preparation for elective surgery.
Cardiovascular/stroke
Much of the cardiovascular toxicity from cigarette use is tied to the myriad of complex toxic particles produced in inhaled smoke, the vast majority of which are not present in e-cigarette vapor. While nicotine itself has known acute cardiovascular effects, including tachycardia and vasoconstriction, a tolerance to these effects occurs over time. Previous evaluations of nicotine replacement therapies and smokeless tobacco for their cardiovascular effects have had mixed results. But, there appears to be a trend toward minimal cardiovascular risk when using “cleaner” products, such as nicotine replacement therapy compared with smokeless tobacco (Benowitz NL, et al. Nature Rev Cardiol. 2017;14[8]:447). Whether this can be extrapolated to electronic cigarette use is unknown but is encouraging.
Alternative toxicity
In addition to the above risks that are in comparison to traditional smoking, vaping also introduces novel toxicities. There are case reports of lipoid pneumonia, ARDS, hypersensitivity pneumonitis, eosinophilic pneumonia, and diffuse alveola hemorrhage. Burns from malfunctioning devices must also be considered, as there is a wide array of products available, at differing levels of build quality.
Toxic oral ingestion of nicotine, especially by children, has led to increased calls to poison centers. For a small child, this can be fatal. Regulation of labels and containers could curtail this issue. But, public education regarding the toxicity of these substances when ingested in large quantities is also important. If there is a lack of understanding about this danger, then typical safeguards are easily overlooked by individual users.
Are there benefits?
Smoking cessation
Compared with other products, such as nicotine patches, gum, and pharmaceutical methods, e-cigarettes most closely mimic the actual experience of smoking. For some, the habit and ritual of smoking is as much a part of the addiction as nicotine. Vaping has the potential to help alleviate this difficult aspect of cessation. Data involving early generation products failed to show a significant advantage. Newer devices that are more pleasurable to use and offer more efficient nicotine delivery may be more effective. Indeed, a recent study in the New England Journal of Medicine from this year demonstrated improved smoking cessation compared with traditional methods, using second generation vape devices (Hajek P, et al. N Engl J Med. 2019;380[7]629). It will be interesting to see if this can be repeatable going forward and if protocols can be established to maximize effectiveness.
As outlined above, it is difficult to make definitive conclusions or recommendations regarding electronic cigarette use at the present time. The risk of cancer and cardiopulmonary disease is likely to be significantly lower but not eliminated. Use as a smoking cessation aid is starting to show promise. Even without cessation, ongoing vaping is likely to be safer than ongoing smoking. Two caveats to this remain: some patients, in an effort to quit smoking, may take up vaping but eventually become “dual users.” This scenario has been associated with higher toxic exposure and possibly worse outcomes. The second caveat is that while there is promise to using this as a cessation tool, it should not yet replace other more well-studied, first-line agents in this regard. It should, perhaps, target patients who are motivated to quit but have failed more traditional methods. Finally, there continues to be concern that vaping could appeal to never smokers, given its perceived safety profile and ease of use in public places. This could lead to an overall increase in nicotine addiction, which could be a significant step backwards.
Dr. Clark is Assistant Professor, Pulmonary and Critical Care Medicine, UT Southwestern Medical Center, Dallas, Texas.
The prevalence and popularity of electronic cigarettes or “vaping” have grown dramatically over the last several years in the United States. Although new studies targeting these products are being done at increasing frequency, there remains a relative paucity of data regarding the long-term risks. Proponents argue that they can be used as a cessation tool for smokers, or failing that, a safer replacement for traditional cigarettes. Opponents make the case that the perception of safety could contribute to increased use in people who may have otherwise never smoked, leading to an overall increase in nicotine use and addiction. This is most readily seen in the adolescent population, where use has skyrocketed, leading to concerns about how electronic cigarettes are marketed to youth, as well as the ease of access.
Basics of vaping (devices)
In its most basic form, an electronic cigarette consists of a battery that powers a heating coil. This heating coil applies heat to a wick, which is soaked in liquid, “vape juice,” converting it into a vapor that is then directly inhaled. However, there can be many variations on this simple theme. Early generation products resembled traditional cigarettes in size and shape and were marketed as smoking cessation aids. Newer devices have abandoned this look and strategy. Preloaded cartridges have been replaced by large tanks that the user can fill with the liquid of their choosing. Multiple tanks can be purchased for a single device, enabling the user to have multiple flavors or various levels of nicotine dosing on hand for quick changing, depending on user preference or mood. Additionally, there are variable voltage settings, resulting in different styles of vapor and/or “throat hit” (the description of the desired burning vs smooth effect of the vapor on the oropharynx). This type of device invites experimentation. Multiple flavors can be used in isolation or mixed together at various temperatures. It no longer resembles classic cigarettes, and the flavor and experience are more prominently promoted. One can see that this device has more appeal to a “never smoker” than the original products, and there is concern that it is being marketed as such with some success (Dinakar C, et al. N Engl J Med. 2016;375[14]:1372).
E-liquid
Perhaps more important than the devices themselves is an understanding of the components of the liquid used to generate the inhaled aerosol.
Typically, four components are present:
• Propylene glycol
• Vegetable glycerin
• Flavoring
• Nicotine
The first two components are generally considered nontoxic, based on their use as food additives. However, inhalation is a novel route of entry and the long-term effects on the respiratory tract are unclear.
The third component, “flavorings,” is a catch-all term for the hundreds of different flavors and styles of e-liquids available today, ranging from menthol to fruit or candy and everything in between. It is difficult to account for all the potential effects of the numerous flavorings being used, especially when some are combined by the end user to various degrees.
Nicotine is present, specified in varying doses. However, vaping style, experience, and type of device used can dramatically affect how much is absorbed, making dosages difficult to predict. Additionally, labeled doses are prone to wide ranges of error (Schraufnagel DE, et al. Am J Respir Crit Care Med. 2014;190[6]:611).
What are the risks?
Cancer
A handful of known carcinogens can be found in inhaled vapor, including formaldehyde, acetaldehyde, acrolein, toluene, and nitrosamines. However, they are present in far lower concentrations than in traditional cigarettes (Goniewicz ML, et al. JAMA Netw Open. 2018;1[8]e185937). This leads to the natural assumption that vaping, while not benign, poses a much lower cancer risk when compared with smoking. Whether that is borne out in the long term remains to be seen.
Pulmonary function
The long-term effect on pulmonary function is not known. Small studies have shown no significant changes to spirometry after acute exposure to vapor. More data are needed in this area (Palazzolo DL. Frontiers Public Health. 2013;1[56]1-20).
Wound healing
An animal study has shown evidence of poor wound healing extrapolated from skin flap necrosis in rats. Exposure to vapor vs smoke yielded similar results, and both were worse than the sham arm (Troiano C, et al. JAMA Facial Plast Surg. 2019;21[1]:5). While it is difficult to know how to apply this clinically, it may be prudent to advise patients to abstain while in preparation for elective surgery.
Cardiovascular/stroke
Much of the cardiovascular toxicity from cigarette use is tied to the myriad of complex toxic particles produced in inhaled smoke, the vast majority of which are not present in e-cigarette vapor. While nicotine itself has known acute cardiovascular effects, including tachycardia and vasoconstriction, a tolerance to these effects occurs over time. Previous evaluations of nicotine replacement therapies and smokeless tobacco for their cardiovascular effects have had mixed results. But, there appears to be a trend toward minimal cardiovascular risk when using “cleaner” products, such as nicotine replacement therapy compared with smokeless tobacco (Benowitz NL, et al. Nature Rev Cardiol. 2017;14[8]:447). Whether this can be extrapolated to electronic cigarette use is unknown but is encouraging.
Alternative toxicity
In addition to the above risks that are in comparison to traditional smoking, vaping also introduces novel toxicities. There are case reports of lipoid pneumonia, ARDS, hypersensitivity pneumonitis, eosinophilic pneumonia, and diffuse alveola hemorrhage. Burns from malfunctioning devices must also be considered, as there is a wide array of products available, at differing levels of build quality.
Toxic oral ingestion of nicotine, especially by children, has led to increased calls to poison centers. For a small child, this can be fatal. Regulation of labels and containers could curtail this issue. But, public education regarding the toxicity of these substances when ingested in large quantities is also important. If there is a lack of understanding about this danger, then typical safeguards are easily overlooked by individual users.
Are there benefits?
Smoking cessation
Compared with other products, such as nicotine patches, gum, and pharmaceutical methods, e-cigarettes most closely mimic the actual experience of smoking. For some, the habit and ritual of smoking is as much a part of the addiction as nicotine. Vaping has the potential to help alleviate this difficult aspect of cessation. Data involving early generation products failed to show a significant advantage. Newer devices that are more pleasurable to use and offer more efficient nicotine delivery may be more effective. Indeed, a recent study in the New England Journal of Medicine from this year demonstrated improved smoking cessation compared with traditional methods, using second generation vape devices (Hajek P, et al. N Engl J Med. 2019;380[7]629). It will be interesting to see if this can be repeatable going forward and if protocols can be established to maximize effectiveness.
As outlined above, it is difficult to make definitive conclusions or recommendations regarding electronic cigarette use at the present time. The risk of cancer and cardiopulmonary disease is likely to be significantly lower but not eliminated. Use as a smoking cessation aid is starting to show promise. Even without cessation, ongoing vaping is likely to be safer than ongoing smoking. Two caveats to this remain: some patients, in an effort to quit smoking, may take up vaping but eventually become “dual users.” This scenario has been associated with higher toxic exposure and possibly worse outcomes. The second caveat is that while there is promise to using this as a cessation tool, it should not yet replace other more well-studied, first-line agents in this regard. It should, perhaps, target patients who are motivated to quit but have failed more traditional methods. Finally, there continues to be concern that vaping could appeal to never smokers, given its perceived safety profile and ease of use in public places. This could lead to an overall increase in nicotine addiction, which could be a significant step backwards.
Dr. Clark is Assistant Professor, Pulmonary and Critical Care Medicine, UT Southwestern Medical Center, Dallas, Texas.
Sepsis survivors’ persistent immunosuppression raises mortality risk
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
FROM JAMA NETWORK OPEN
Key clinical point: Markers of inflammation and immunosuppression persist in over two-thirds of patients hospitalized for sepsis, which could explain worsened outcomes and mortality up to 1 year after hospitalization.
Major finding: Patients with signs of hyperinflammation and immunosuppression had significantly increased mortality after 1 year and were significantly more likely to be readmitted or die because of cardiovascular disease or cancer.
Study details: A prospective cohort study of 483 patients who were hospitalized because of sepsis at 12 different centers between January 2012 and May 2017.
Disclosures: This study was funded by grants from National Institutes of Health and resources from the Veterans Affairs Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
Source: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.