User login
Tofacitinib and TNF inhibitors show similar VTE rates
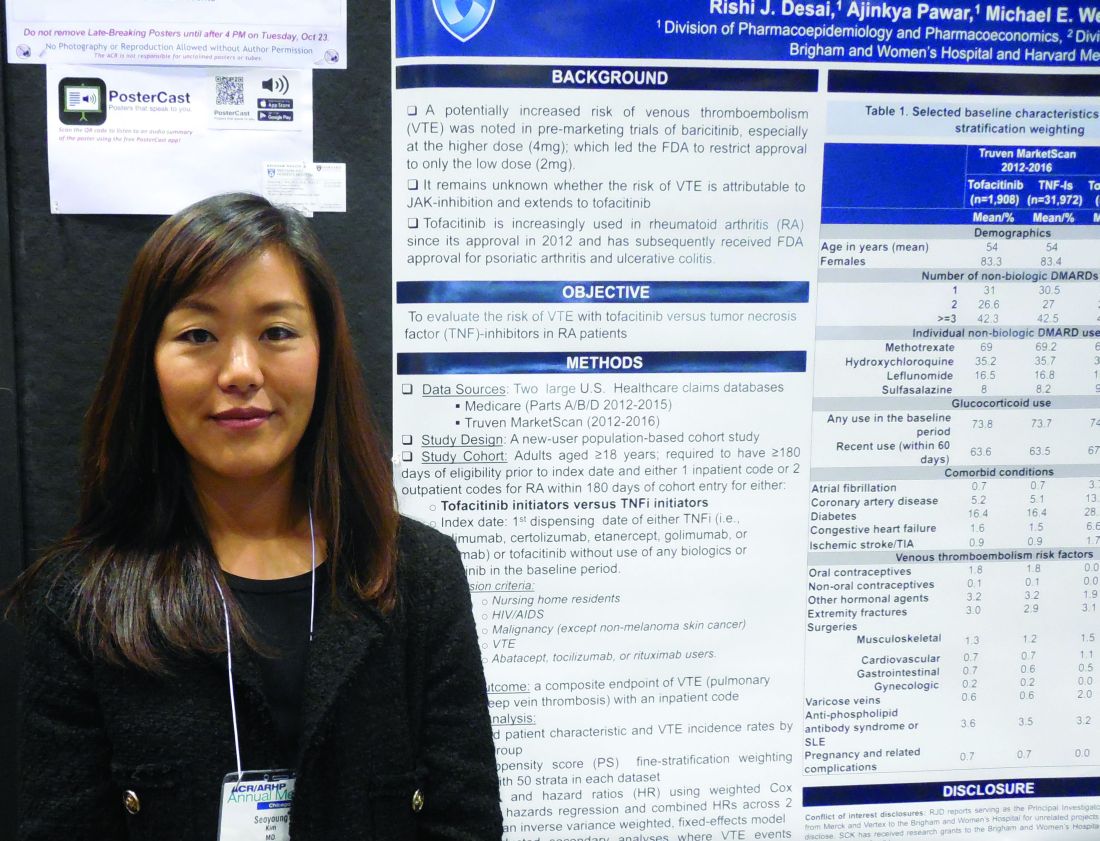
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Rheumatoid arthritis patients treated with tofacitinib showed no excess incidence of venous thromboembolism, compared with patients on a tumor necrosis factor inhibitor.
Major finding: Propensity score–adjusted rates of VTE were 33% higher with tofacitinib, compared with TNF inhibition, which was not a statistically significant difference.
Study details: Review of 51,160 rheumatoid arthritis patients from U.S. health insurance databases.
Disclosures: Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
Source: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
All patients with VTE have a high risk of recurrence
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
FROM THE AMERICAN JOURNAL OF MEDICINE
Key clinical point:
Major finding: At 10-year follow-up, recurrence rates per 100 person-years were 3.70 for patients with cancer-related VTE, 2.84 for patients with unprovoked VTE, and 2.22 for patients with provoked VTE.
Study details: An observational cohort study of 73,993 Danish patients with incident venous thromboembolism during January 2000–December 2015.
Disclosures: The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
Source: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Prolonged DAPT doesn’t help left main CAD
SAN DIEGO – Among patients who receive a drug-eluting stent (DES) in their left main coronary artery (LMCA), continuation of dual antiplatelet therapy (DAPT) past 1 year appears to provide no benefit.
The results come from a subanalysis of the EXCEL trial, which compared the Xience DES to coronary artery bypass graft (CABG) surgery in LMCA lesions.
The LMCA is worrisome to a lot of physicians because of the large amount of myocardial tissue it contains, and they often prescribe DAPT past the generally recommended 1 year. “It’s this magic thing, that ‘Well, it’s left main stenting, and you’d better protect the patient.’ But it turns out that it doesn’t,” said Sorin Brener, MD, director of the catheterization lab at New York Methodist Hospital, who presented the results of the study at the Transcatheter Cardiovascular Therapeutics annual meeting.
The researchers compared patients in both groups who opted to stop DAPT after 1 year versus those who continued therapy out to 3 years, and the news was not favorable for continuation. A composite of death, myocardial infarction, or stroke was higher among patients who continued DAPT, though the results did not reach statistical significance.
It’s possible that patients who continued DAPT were more ill on average. “Obviously, there could be cases where the doctor decided they deserved more prolonged therapy, but it’s not measurable, so I don’t think they were sicker,” said Dr. Brener.
The study was also underpowered. Those worse trends probably don’t represent a real signal, according to Dr. Brener. Rather, they suggest that there is no significant difference between the approaches. “The signal just tells you that there is no difference, and that prolonging DAPT probably just induces some minor bleeding, but it doesn’t protect you. So the message would be that you should treat all your patients the same way regardless of where you put the stent,” said Dr. Brener.
The researchers compared data from 497 patients in the EXCEL trial who continued DAPT out to 3 years with that from 136 who stopped DAPT early (115 stopped in year 1-2; 21 stopped in year 2-3). The baseline characteristics of the two groups were similar except for a higher incidence of recent MI in the group that stopped DAPT early (21.3% vs. 13.7%; P = .03).
At 3 years, death, MI, or stroke occurred in 7.8% of the continuation group and in 5.2% of the patients who stopped DAPT. All-cause mortality was 5.8% in the continuation group compared with 2.3% of those who stopped. When the researchers restricted the analysis to patients who presented with acute coronary syndrome, 7.6% and 3.6%, respectively, met the primary endpoint. None of these differences reached statistical significance.
The study was limited by a high dropout rate from DAPT in the first year: 152 patients stopped taking the medication even though they experienced no events, and they were excluded from the analysis.
The EXCEL trial was funded by Abbott. Dr. Brener has been a consultant or received honoraria or speaker’s fees for AstraZeneca.
SOURCE: Brener S. TCT 2018, Abstract TCT-1.
SAN DIEGO – Among patients who receive a drug-eluting stent (DES) in their left main coronary artery (LMCA), continuation of dual antiplatelet therapy (DAPT) past 1 year appears to provide no benefit.
The results come from a subanalysis of the EXCEL trial, which compared the Xience DES to coronary artery bypass graft (CABG) surgery in LMCA lesions.
The LMCA is worrisome to a lot of physicians because of the large amount of myocardial tissue it contains, and they often prescribe DAPT past the generally recommended 1 year. “It’s this magic thing, that ‘Well, it’s left main stenting, and you’d better protect the patient.’ But it turns out that it doesn’t,” said Sorin Brener, MD, director of the catheterization lab at New York Methodist Hospital, who presented the results of the study at the Transcatheter Cardiovascular Therapeutics annual meeting.
The researchers compared patients in both groups who opted to stop DAPT after 1 year versus those who continued therapy out to 3 years, and the news was not favorable for continuation. A composite of death, myocardial infarction, or stroke was higher among patients who continued DAPT, though the results did not reach statistical significance.
It’s possible that patients who continued DAPT were more ill on average. “Obviously, there could be cases where the doctor decided they deserved more prolonged therapy, but it’s not measurable, so I don’t think they were sicker,” said Dr. Brener.
The study was also underpowered. Those worse trends probably don’t represent a real signal, according to Dr. Brener. Rather, they suggest that there is no significant difference between the approaches. “The signal just tells you that there is no difference, and that prolonging DAPT probably just induces some minor bleeding, but it doesn’t protect you. So the message would be that you should treat all your patients the same way regardless of where you put the stent,” said Dr. Brener.
The researchers compared data from 497 patients in the EXCEL trial who continued DAPT out to 3 years with that from 136 who stopped DAPT early (115 stopped in year 1-2; 21 stopped in year 2-3). The baseline characteristics of the two groups were similar except for a higher incidence of recent MI in the group that stopped DAPT early (21.3% vs. 13.7%; P = .03).
At 3 years, death, MI, or stroke occurred in 7.8% of the continuation group and in 5.2% of the patients who stopped DAPT. All-cause mortality was 5.8% in the continuation group compared with 2.3% of those who stopped. When the researchers restricted the analysis to patients who presented with acute coronary syndrome, 7.6% and 3.6%, respectively, met the primary endpoint. None of these differences reached statistical significance.
The study was limited by a high dropout rate from DAPT in the first year: 152 patients stopped taking the medication even though they experienced no events, and they were excluded from the analysis.
The EXCEL trial was funded by Abbott. Dr. Brener has been a consultant or received honoraria or speaker’s fees for AstraZeneca.
SOURCE: Brener S. TCT 2018, Abstract TCT-1.
SAN DIEGO – Among patients who receive a drug-eluting stent (DES) in their left main coronary artery (LMCA), continuation of dual antiplatelet therapy (DAPT) past 1 year appears to provide no benefit.
The results come from a subanalysis of the EXCEL trial, which compared the Xience DES to coronary artery bypass graft (CABG) surgery in LMCA lesions.
The LMCA is worrisome to a lot of physicians because of the large amount of myocardial tissue it contains, and they often prescribe DAPT past the generally recommended 1 year. “It’s this magic thing, that ‘Well, it’s left main stenting, and you’d better protect the patient.’ But it turns out that it doesn’t,” said Sorin Brener, MD, director of the catheterization lab at New York Methodist Hospital, who presented the results of the study at the Transcatheter Cardiovascular Therapeutics annual meeting.
The researchers compared patients in both groups who opted to stop DAPT after 1 year versus those who continued therapy out to 3 years, and the news was not favorable for continuation. A composite of death, myocardial infarction, or stroke was higher among patients who continued DAPT, though the results did not reach statistical significance.
It’s possible that patients who continued DAPT were more ill on average. “Obviously, there could be cases where the doctor decided they deserved more prolonged therapy, but it’s not measurable, so I don’t think they were sicker,” said Dr. Brener.
The study was also underpowered. Those worse trends probably don’t represent a real signal, according to Dr. Brener. Rather, they suggest that there is no significant difference between the approaches. “The signal just tells you that there is no difference, and that prolonging DAPT probably just induces some minor bleeding, but it doesn’t protect you. So the message would be that you should treat all your patients the same way regardless of where you put the stent,” said Dr. Brener.
The researchers compared data from 497 patients in the EXCEL trial who continued DAPT out to 3 years with that from 136 who stopped DAPT early (115 stopped in year 1-2; 21 stopped in year 2-3). The baseline characteristics of the two groups were similar except for a higher incidence of recent MI in the group that stopped DAPT early (21.3% vs. 13.7%; P = .03).
At 3 years, death, MI, or stroke occurred in 7.8% of the continuation group and in 5.2% of the patients who stopped DAPT. All-cause mortality was 5.8% in the continuation group compared with 2.3% of those who stopped. When the researchers restricted the analysis to patients who presented with acute coronary syndrome, 7.6% and 3.6%, respectively, met the primary endpoint. None of these differences reached statistical significance.
The study was limited by a high dropout rate from DAPT in the first year: 152 patients stopped taking the medication even though they experienced no events, and they were excluded from the analysis.
The EXCEL trial was funded by Abbott. Dr. Brener has been a consultant or received honoraria or speaker’s fees for AstraZeneca.
SOURCE: Brener S. TCT 2018, Abstract TCT-1.
REPORTING FROM TCT 2018
Key clinical point: Prolonged DAPT was not associated with better outcomes.
Major finding: Composite death, myocardial infarction, and stroke was similar between the two groups.
Study details: A post hoc analysis of 633 patients in the EXCEL trial.
Disclosures: The EXCEL trial was funded by Abbott. Dr. Brener has been a consultant or received honoraria or speaker’s fees for AstraZeneca.
Source: Brener S. TCT 2018, Abstract TCT-1.
Risk score can predict thrombosis in ITP
Research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score was able to identify all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly, within a matter of days, suggesting they should be reevaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ont., and her colleagues reported their findings in Blood.
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome.
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L.
- Major bleeding (grade 2 bleeding that does not involve the skin) at the time of visit.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests an increased risk of thrombosis, and a negative score suggests an increased risk of bleeding.
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months. During that time, there were 41 encounters between patients and clinicians. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld during 22 encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
Three of the 13 patients continued on anticoagulation during 10 encounters. The patients received additional ITP treatments at 6 of these encounters.
Major bleeding was present at 2 of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
The TH2 score accurately predicted all seven thrombotic events. There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score – suggesting an increased risk of thrombosis – when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be reevaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number patients evaluated. The TH2 score should be validated in additional, larger studies, they advised.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma.
SOURCE: Balitsky AK et al. Blood. 2018 Nov 8. doi: 10.1182/blood-2018-08-868406.
Research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score was able to identify all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly, within a matter of days, suggesting they should be reevaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ont., and her colleagues reported their findings in Blood.
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome.
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L.
- Major bleeding (grade 2 bleeding that does not involve the skin) at the time of visit.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests an increased risk of thrombosis, and a negative score suggests an increased risk of bleeding.
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months. During that time, there were 41 encounters between patients and clinicians. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld during 22 encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
Three of the 13 patients continued on anticoagulation during 10 encounters. The patients received additional ITP treatments at 6 of these encounters.
Major bleeding was present at 2 of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
The TH2 score accurately predicted all seven thrombotic events. There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score – suggesting an increased risk of thrombosis – when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be reevaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number patients evaluated. The TH2 score should be validated in additional, larger studies, they advised.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma.
SOURCE: Balitsky AK et al. Blood. 2018 Nov 8. doi: 10.1182/blood-2018-08-868406.
Research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score was able to identify all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly, within a matter of days, suggesting they should be reevaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ont., and her colleagues reported their findings in Blood.
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome.
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L.
- Major bleeding (grade 2 bleeding that does not involve the skin) at the time of visit.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests an increased risk of thrombosis, and a negative score suggests an increased risk of bleeding.
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months. During that time, there were 41 encounters between patients and clinicians. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld during 22 encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
Three of the 13 patients continued on anticoagulation during 10 encounters. The patients received additional ITP treatments at 6 of these encounters.
Major bleeding was present at 2 of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
The TH2 score accurately predicted all seven thrombotic events. There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score – suggesting an increased risk of thrombosis – when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be reevaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number patients evaluated. The TH2 score should be validated in additional, larger studies, they advised.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma.
SOURCE: Balitsky AK et al. Blood. 2018 Nov 8. doi: 10.1182/blood-2018-08-868406.
FROM BLOOD
Key clinical point:
Major finding: The score predicted all seven thrombotic events in the study.
Study details: Retrospective study of 13 patients with ITP.
Disclosures: One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma.
Source: Balitsky AK et al. Blood. 2018 Nov 8. doi: 10.1182/blood-2018-08-868406.
Education can improve adherence to VTE prophylaxis
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Score can predict thrombosis in ITP
New research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score identified all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly—within a matter of days—which suggests they should be re-evaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues detailed this research in Blood.
About the score
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The resulting score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L
- Major bleeding (grade 2 bleeding that does not involve the skin) observed at a clinical encounter.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests a net increased risk of thrombosis, and a negative score suggests a net increased risk of bleeding.
Patient population
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months (interquartile range, 4.5 to 24 months). During that time, there were 41 clinical encounters. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld at some point during their 22 clinical encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
The remaining three patients (of the 13) did not stop anticoagulation. These patients received additional ITP treatments at six of their 10 clinical encounters.
Major bleeding was present at two of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
Testing the score
The TH2 score accurately predicted all seven thrombotic events.
There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score—suggesting an increased risk of thrombosis—when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be re-evaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number of patients evaluated. Therefore, the TH2 score should be validated in additional, larger studies.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma. The other researchers said they had no competing financial interests.
New research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score identified all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly—within a matter of days—which suggests they should be re-evaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues detailed this research in Blood.
About the score
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The resulting score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L
- Major bleeding (grade 2 bleeding that does not involve the skin) observed at a clinical encounter.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests a net increased risk of thrombosis, and a negative score suggests a net increased risk of bleeding.
Patient population
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months (interquartile range, 4.5 to 24 months). During that time, there were 41 clinical encounters. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld at some point during their 22 clinical encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
The remaining three patients (of the 13) did not stop anticoagulation. These patients received additional ITP treatments at six of their 10 clinical encounters.
Major bleeding was present at two of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
Testing the score
The TH2 score accurately predicted all seven thrombotic events.
There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score—suggesting an increased risk of thrombosis—when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be re-evaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number of patients evaluated. Therefore, the TH2 score should be validated in additional, larger studies.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma. The other researchers said they had no competing financial interests.
New research suggests a scoring system can predict the risk of thrombosis in patients with immune thrombocytopenia (ITP) who are taking anticoagulants.
Researchers tested their Thrombosis and Thrombocytopenia (TH2) risk assessment score in a small group of ITP patients on anticoagulants, and the score identified all seven patients who developed thrombosis.
The researchers also found that patients’ TH2 scores changed quickly—within a matter of days—which suggests they should be re-evaluated for thrombosis risk frequently.
Amaris K. Balitsky, MD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues detailed this research in Blood.
About the score
To develop the TH2 score, the researchers conducted a review of the literature and existing tools used to assess the risk of thrombosis and bleeding. The resulting score consists of two thrombosis items and two bleeding items.
The thrombosis items are:
- High thrombotic risk, which includes patients with atrial fibrillation and a CHA2DS2-VASc score greater than five; unprovoked, recurrent, or cancer-associated thrombosis; or antiphospholipid antibody syndrome
- Receipt of ITP therapies known to increase the risk of thrombosis in the previous 14 days or splenectomy in the previous 30 days.
The score’s bleeding items are:
- Platelet count less than 20 x 109/L
- Major bleeding (grade 2 bleeding that does not involve the skin) observed at a clinical encounter.
Each thrombosis item is assigned a score of +1, and each bleeding item is assigned a score of -1. A positive score or score of 0 suggests a net increased risk of thrombosis, and a negative score suggests a net increased risk of bleeding.
Patient population
The researchers tested the TH2 score in patients enrolled in the McMaster ITP Registry from 2010 to 2017.
There were 314 patients enrolled, but only 13 were receiving anticoagulation and had a platelet count less than 50 x 109/L. Six of these patients were receiving anticoagulation for atrial fibrillation and seven for venous thrombosis. Four patients were taking antiplatelet agents as well.
The median follow up was 9 months (interquartile range, 4.5 to 24 months). During that time, there were 41 clinical encounters. Data on treatment decisions and clinical outcomes were available for 32 of these encounters.
Ten of the 13 patients had anticoagulation withheld at some point during their 22 clinical encounters. Major bleeding was present at five of the encounters. At 17 encounters, patients received additional ITP treatments.
Six of the 10 patients who stopped anticoagulation had new thrombotic events, and two of these events were fatal. Three of the patients had thrombotic events even though they resumed anticoagulation.
The remaining three patients (of the 13) did not stop anticoagulation. These patients received additional ITP treatments at six of their 10 clinical encounters.
Major bleeding was present at two of the 10 encounters, and one new thrombotic event occurred in a patient with metastatic squamous cell cancer (despite continued treatment with warfarin).
Testing the score
The TH2 score accurately predicted all seven thrombotic events.
There were four patients who initially had a negative TH2 score, which suggested an increased risk of bleeding.
However, these patients had a positive or 0 score—suggesting an increased risk of thrombosis—when they were assessed again, after their platelet counts increased above 50 x 109/L.
The remaining three patients had initial scores of 0 and subsequent positive scores, both suggesting an increased risk of thrombosis.
The researchers said these findings suggest patients should be re-evaluated for thrombosis risk frequently, as ITP treatments are given and platelet counts increase.
“The results of our study suggest that the risk of thrombosis is high in patients with ITP who have a separate indication for anticoagulation, especially after ITP therapies are administered and the severe thrombocytopenia improves,” the researchers wrote. “Early resumption of anticoagulation should be considered in this population.”
The researchers also noted that this study was limited by its retrospective, single-center design and the small number of patients evaluated. Therefore, the TH2 score should be validated in additional, larger studies.
One researcher reported relationships with Amgen, Novartis, Rigel Pharmaceuticals, UCB, and Principia Biopharma. The other researchers said they had no competing financial interests.
Apixaban is safest effective DOAC for stroke prevention in Afib, per AHRQ report
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
Vaccine inhibits thrombus formation in mice
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
Test strips for warfarin monitoring recalled due to serious risks
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
CT opens extended window for stroke thrombolysis
MONTREAL – An extended time window for thrombolytic treatment of acute ischemic stroke patients using tissue plasminogen activator out to 9 hours from stroke onset was safe and effective using CT perfusion imaging and automated imaging processing software to select suitable patients in the EXTEND trial. This result matches the groundbreaking finding reported earlier in 2018 that used MRI to select patients for extended thrombolysis.
“To reproduce our results you need to set up CT perfusion” as well as the RAPID software for automated image processing to identify patients with a small infarct core and a large area of salvageable brain, said Henry Ma, MD, a stroke neurologist at Monash University, Melbourne, as he reported results from the trial at the World Stroke Congress. “EXTEND is the first positive thrombolysis trial in an extended time window using automated penumbral imaging.”
The new finding, from a trial with 225 randomized stroke patients, was especially notable because, by showing the validity of CT imaging for patient selection, it makes applying the extended time window for thrombolytic therapy more feasible for U.S. and Canadian stroke centers where CT imaging is much more common than MRI. A report from European investigators published in August 2018 from the WAKE-UP trial showed that thrombolysis with tissue plasminogen activator (tPA) was safe and effective when administered to patients who woke up with an acute ischemic stroke that had occurred more than 4.5 hours before treatment, but this study exclusively used MRI for patient selection (N Engl J Med. 2018 Aug 16;379[7]:611-22).
“In North America, our systems are more equipped for using CT,” commented Ashfaq Shuaib, MD, a professor of medicine and neurologist at the University of Alberta, Edmonton. Based on the WAKE-UP results, “MR would be preferred, but what we’ve been doing [since the WAKE-UP report] is if we see a CT scan that’s good we go ahead” with thrombolysis.
“Biologically, it doesn’t matter whether you use MR or CT; they both index the same underlying pathology. We’ve been hesitant to go beyond the MR finding from WAKE-UP, where there were data, but the findings from EXTEND were right in line with the WAKE-UP results, and that’s all we need to be reassured” that CT perfusion imaging also works for patient selection, commented Jeffrey L. Saver, MD, professor of medicine and director of the Comprehensive Stroke Center at the University of California, Los Angeles.
CT perfusion imaging and automated image processing “worked to select stroke patients” for an extended time window for treatment with mechanical thrombectomy in the DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Feb 22;378[8]:308-18) trials, a history that makes the new finding of successfully using CT imaging to select patients who qualify for extended use of thrombolysis “a convincing result,” Dr. Saver said in an interview. The new EXTEND findings “will have a major impact” on using an extended time window for thrombolysis in U.S. practice, he predicted.
The EXTEND trial (Int J Stroke. 2012 Jan 1;7[1]:74-80) ran at 22 sites in Australia, 11 sites in Taiwan, and 1 center in New Zealand. Recruitment of patients into the study stopped early, after enrolling 225 patients, in June 2018, when results from WAKE-UP came out.
The EXTEND investigators enrolled patients who were either 4.5-9 hours out from the onset of their stroke or patients with a wake-up stroke with an uncertain onset. Participating centers could use either CT perfusion or MRI to identify candidates for treatment, and all used the RAPID software for image processing to identify patients with a perfusion lesion of at least 10 mL and an ischemic core volume no greater than 70 mL. Dr. Ma did not report what percentage of patients underwent imaging with each of these methods, but hinted that clinicians had used CT for a majority of the cases. The study randomized patients to receive either 0.9 mg/kg tPA or placebo, and by the trial protocol none of the enrolled patients received treatment with mechanical thrombectomy.
The trial’s primary endpoint was the percentage of patients with a modified Rankin Scale score of 0 or 1 at 90 days after their stroke, which was achieved by 44% more patients in the tPA group relative to the placebo arm after adjustment for age and baseline stroke severity, a statistically significant difference. The results were also positive for several secondary endpoints, such as recanalization 24 hours after treatment, which occurred in 67% of patients treated with tPA and 37% of the control patients, a statistically significant 68% relative improvement with thrombolysis.
Mortality at 90 days was similar in the two arms – 9% among the placebo patients and 12% among those who received tPA. The rate of symptomatic intracranial hemorrhage 36 hours after treatment was significantly higher among patients treated with tPA at 6%, compared with 1% in the placebo group, but the magnitude of this adverse effect was consistent with rates of intracranial hemorrhages previously reported in other studies of thrombolytic treatment for acute ischemic stroke, Dr. Ma said. The small number of increased intracranial hemorrhages “was not associated with increased mortality, and did not negate the positive result of an improved rate of excellent functional outcomes.”
These findings will likely spur further adoption of imaging processing software of the type used in EXTEND by U.S. stroke centers, Dr. Saver predicted.
“More and more centers have been getting this [software], and now they have two reasons to have it: to identify patients for an extended window for mechanical thrombectomy and to identify patients for an extended window for thrombolysis. It is a compelling case to have the imaging software as widely disseminated as possible. Centers that want to do the best for patients should have this imaging-processing software,” Dr. Saver said.
Dr. Ma and Dr. Shuaib reported no disclosures. Dr. Saver has received research funding and personal fees from Medtronic-Abbott and Neuravia.
SOURCE: Ma H et al. Int J. Stroke. 2018 Oct;13(2S):235, Abstract 1014.
Ever since results from the WAKE-UP trial came out earlier in 2018, we at the University of Cincinnati have been imaging acute ischemic stroke patients who presented outside the standard 4.5-hour time limit for thrombolysis with MRI to see if they qualify for an extended window for thrombolysis. But this has been a cumbersome and redundant process because our default imaging method is CT, so we have been imaging potential candidates for an extended thrombolytic window twice, first with CT and then later with MRI.
The EXTEND findings also provide a further reason for U.S. stroke centers to purchase and use some type of imaging processing software if they don’t already have it, either the RAPID software that was used in EXTEND or one of the several similar software packages that are now available. Several primary stroke centers in my area still do not currently use this software, although its use has been quickly spreading and it will now be increasingly hard for these centers to hold off acquiring it. Fortunately the increased competition among software vendors who sell this type of software has meant that the price has been dropping.
Pooja Khatri, MD , is a professor of neurology and director of acute stroke at the University of Cincinnati. She has been a consultant to Biogen, Greenwich, and PTC Therapeutics. She made these comments in an interview.
Ever since results from the WAKE-UP trial came out earlier in 2018, we at the University of Cincinnati have been imaging acute ischemic stroke patients who presented outside the standard 4.5-hour time limit for thrombolysis with MRI to see if they qualify for an extended window for thrombolysis. But this has been a cumbersome and redundant process because our default imaging method is CT, so we have been imaging potential candidates for an extended thrombolytic window twice, first with CT and then later with MRI.
The EXTEND findings also provide a further reason for U.S. stroke centers to purchase and use some type of imaging processing software if they don’t already have it, either the RAPID software that was used in EXTEND or one of the several similar software packages that are now available. Several primary stroke centers in my area still do not currently use this software, although its use has been quickly spreading and it will now be increasingly hard for these centers to hold off acquiring it. Fortunately the increased competition among software vendors who sell this type of software has meant that the price has been dropping.
Pooja Khatri, MD , is a professor of neurology and director of acute stroke at the University of Cincinnati. She has been a consultant to Biogen, Greenwich, and PTC Therapeutics. She made these comments in an interview.
Ever since results from the WAKE-UP trial came out earlier in 2018, we at the University of Cincinnati have been imaging acute ischemic stroke patients who presented outside the standard 4.5-hour time limit for thrombolysis with MRI to see if they qualify for an extended window for thrombolysis. But this has been a cumbersome and redundant process because our default imaging method is CT, so we have been imaging potential candidates for an extended thrombolytic window twice, first with CT and then later with MRI.
The EXTEND findings also provide a further reason for U.S. stroke centers to purchase and use some type of imaging processing software if they don’t already have it, either the RAPID software that was used in EXTEND or one of the several similar software packages that are now available. Several primary stroke centers in my area still do not currently use this software, although its use has been quickly spreading and it will now be increasingly hard for these centers to hold off acquiring it. Fortunately the increased competition among software vendors who sell this type of software has meant that the price has been dropping.
Pooja Khatri, MD , is a professor of neurology and director of acute stroke at the University of Cincinnati. She has been a consultant to Biogen, Greenwich, and PTC Therapeutics. She made these comments in an interview.
MONTREAL – An extended time window for thrombolytic treatment of acute ischemic stroke patients using tissue plasminogen activator out to 9 hours from stroke onset was safe and effective using CT perfusion imaging and automated imaging processing software to select suitable patients in the EXTEND trial. This result matches the groundbreaking finding reported earlier in 2018 that used MRI to select patients for extended thrombolysis.
“To reproduce our results you need to set up CT perfusion” as well as the RAPID software for automated image processing to identify patients with a small infarct core and a large area of salvageable brain, said Henry Ma, MD, a stroke neurologist at Monash University, Melbourne, as he reported results from the trial at the World Stroke Congress. “EXTEND is the first positive thrombolysis trial in an extended time window using automated penumbral imaging.”
The new finding, from a trial with 225 randomized stroke patients, was especially notable because, by showing the validity of CT imaging for patient selection, it makes applying the extended time window for thrombolytic therapy more feasible for U.S. and Canadian stroke centers where CT imaging is much more common than MRI. A report from European investigators published in August 2018 from the WAKE-UP trial showed that thrombolysis with tissue plasminogen activator (tPA) was safe and effective when administered to patients who woke up with an acute ischemic stroke that had occurred more than 4.5 hours before treatment, but this study exclusively used MRI for patient selection (N Engl J Med. 2018 Aug 16;379[7]:611-22).
“In North America, our systems are more equipped for using CT,” commented Ashfaq Shuaib, MD, a professor of medicine and neurologist at the University of Alberta, Edmonton. Based on the WAKE-UP results, “MR would be preferred, but what we’ve been doing [since the WAKE-UP report] is if we see a CT scan that’s good we go ahead” with thrombolysis.
“Biologically, it doesn’t matter whether you use MR or CT; they both index the same underlying pathology. We’ve been hesitant to go beyond the MR finding from WAKE-UP, where there were data, but the findings from EXTEND were right in line with the WAKE-UP results, and that’s all we need to be reassured” that CT perfusion imaging also works for patient selection, commented Jeffrey L. Saver, MD, professor of medicine and director of the Comprehensive Stroke Center at the University of California, Los Angeles.
CT perfusion imaging and automated image processing “worked to select stroke patients” for an extended time window for treatment with mechanical thrombectomy in the DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Feb 22;378[8]:308-18) trials, a history that makes the new finding of successfully using CT imaging to select patients who qualify for extended use of thrombolysis “a convincing result,” Dr. Saver said in an interview. The new EXTEND findings “will have a major impact” on using an extended time window for thrombolysis in U.S. practice, he predicted.
The EXTEND trial (Int J Stroke. 2012 Jan 1;7[1]:74-80) ran at 22 sites in Australia, 11 sites in Taiwan, and 1 center in New Zealand. Recruitment of patients into the study stopped early, after enrolling 225 patients, in June 2018, when results from WAKE-UP came out.
The EXTEND investigators enrolled patients who were either 4.5-9 hours out from the onset of their stroke or patients with a wake-up stroke with an uncertain onset. Participating centers could use either CT perfusion or MRI to identify candidates for treatment, and all used the RAPID software for image processing to identify patients with a perfusion lesion of at least 10 mL and an ischemic core volume no greater than 70 mL. Dr. Ma did not report what percentage of patients underwent imaging with each of these methods, but hinted that clinicians had used CT for a majority of the cases. The study randomized patients to receive either 0.9 mg/kg tPA or placebo, and by the trial protocol none of the enrolled patients received treatment with mechanical thrombectomy.
The trial’s primary endpoint was the percentage of patients with a modified Rankin Scale score of 0 or 1 at 90 days after their stroke, which was achieved by 44% more patients in the tPA group relative to the placebo arm after adjustment for age and baseline stroke severity, a statistically significant difference. The results were also positive for several secondary endpoints, such as recanalization 24 hours after treatment, which occurred in 67% of patients treated with tPA and 37% of the control patients, a statistically significant 68% relative improvement with thrombolysis.
Mortality at 90 days was similar in the two arms – 9% among the placebo patients and 12% among those who received tPA. The rate of symptomatic intracranial hemorrhage 36 hours after treatment was significantly higher among patients treated with tPA at 6%, compared with 1% in the placebo group, but the magnitude of this adverse effect was consistent with rates of intracranial hemorrhages previously reported in other studies of thrombolytic treatment for acute ischemic stroke, Dr. Ma said. The small number of increased intracranial hemorrhages “was not associated with increased mortality, and did not negate the positive result of an improved rate of excellent functional outcomes.”
These findings will likely spur further adoption of imaging processing software of the type used in EXTEND by U.S. stroke centers, Dr. Saver predicted.
“More and more centers have been getting this [software], and now they have two reasons to have it: to identify patients for an extended window for mechanical thrombectomy and to identify patients for an extended window for thrombolysis. It is a compelling case to have the imaging software as widely disseminated as possible. Centers that want to do the best for patients should have this imaging-processing software,” Dr. Saver said.
Dr. Ma and Dr. Shuaib reported no disclosures. Dr. Saver has received research funding and personal fees from Medtronic-Abbott and Neuravia.
SOURCE: Ma H et al. Int J. Stroke. 2018 Oct;13(2S):235, Abstract 1014.
MONTREAL – An extended time window for thrombolytic treatment of acute ischemic stroke patients using tissue plasminogen activator out to 9 hours from stroke onset was safe and effective using CT perfusion imaging and automated imaging processing software to select suitable patients in the EXTEND trial. This result matches the groundbreaking finding reported earlier in 2018 that used MRI to select patients for extended thrombolysis.
“To reproduce our results you need to set up CT perfusion” as well as the RAPID software for automated image processing to identify patients with a small infarct core and a large area of salvageable brain, said Henry Ma, MD, a stroke neurologist at Monash University, Melbourne, as he reported results from the trial at the World Stroke Congress. “EXTEND is the first positive thrombolysis trial in an extended time window using automated penumbral imaging.”
The new finding, from a trial with 225 randomized stroke patients, was especially notable because, by showing the validity of CT imaging for patient selection, it makes applying the extended time window for thrombolytic therapy more feasible for U.S. and Canadian stroke centers where CT imaging is much more common than MRI. A report from European investigators published in August 2018 from the WAKE-UP trial showed that thrombolysis with tissue plasminogen activator (tPA) was safe and effective when administered to patients who woke up with an acute ischemic stroke that had occurred more than 4.5 hours before treatment, but this study exclusively used MRI for patient selection (N Engl J Med. 2018 Aug 16;379[7]:611-22).
“In North America, our systems are more equipped for using CT,” commented Ashfaq Shuaib, MD, a professor of medicine and neurologist at the University of Alberta, Edmonton. Based on the WAKE-UP results, “MR would be preferred, but what we’ve been doing [since the WAKE-UP report] is if we see a CT scan that’s good we go ahead” with thrombolysis.
“Biologically, it doesn’t matter whether you use MR or CT; they both index the same underlying pathology. We’ve been hesitant to go beyond the MR finding from WAKE-UP, where there were data, but the findings from EXTEND were right in line with the WAKE-UP results, and that’s all we need to be reassured” that CT perfusion imaging also works for patient selection, commented Jeffrey L. Saver, MD, professor of medicine and director of the Comprehensive Stroke Center at the University of California, Los Angeles.
CT perfusion imaging and automated image processing “worked to select stroke patients” for an extended time window for treatment with mechanical thrombectomy in the DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Feb 22;378[8]:308-18) trials, a history that makes the new finding of successfully using CT imaging to select patients who qualify for extended use of thrombolysis “a convincing result,” Dr. Saver said in an interview. The new EXTEND findings “will have a major impact” on using an extended time window for thrombolysis in U.S. practice, he predicted.
The EXTEND trial (Int J Stroke. 2012 Jan 1;7[1]:74-80) ran at 22 sites in Australia, 11 sites in Taiwan, and 1 center in New Zealand. Recruitment of patients into the study stopped early, after enrolling 225 patients, in June 2018, when results from WAKE-UP came out.
The EXTEND investigators enrolled patients who were either 4.5-9 hours out from the onset of their stroke or patients with a wake-up stroke with an uncertain onset. Participating centers could use either CT perfusion or MRI to identify candidates for treatment, and all used the RAPID software for image processing to identify patients with a perfusion lesion of at least 10 mL and an ischemic core volume no greater than 70 mL. Dr. Ma did not report what percentage of patients underwent imaging with each of these methods, but hinted that clinicians had used CT for a majority of the cases. The study randomized patients to receive either 0.9 mg/kg tPA or placebo, and by the trial protocol none of the enrolled patients received treatment with mechanical thrombectomy.
The trial’s primary endpoint was the percentage of patients with a modified Rankin Scale score of 0 or 1 at 90 days after their stroke, which was achieved by 44% more patients in the tPA group relative to the placebo arm after adjustment for age and baseline stroke severity, a statistically significant difference. The results were also positive for several secondary endpoints, such as recanalization 24 hours after treatment, which occurred in 67% of patients treated with tPA and 37% of the control patients, a statistically significant 68% relative improvement with thrombolysis.
Mortality at 90 days was similar in the two arms – 9% among the placebo patients and 12% among those who received tPA. The rate of symptomatic intracranial hemorrhage 36 hours after treatment was significantly higher among patients treated with tPA at 6%, compared with 1% in the placebo group, but the magnitude of this adverse effect was consistent with rates of intracranial hemorrhages previously reported in other studies of thrombolytic treatment for acute ischemic stroke, Dr. Ma said. The small number of increased intracranial hemorrhages “was not associated with increased mortality, and did not negate the positive result of an improved rate of excellent functional outcomes.”
These findings will likely spur further adoption of imaging processing software of the type used in EXTEND by U.S. stroke centers, Dr. Saver predicted.
“More and more centers have been getting this [software], and now they have two reasons to have it: to identify patients for an extended window for mechanical thrombectomy and to identify patients for an extended window for thrombolysis. It is a compelling case to have the imaging software as widely disseminated as possible. Centers that want to do the best for patients should have this imaging-processing software,” Dr. Saver said.
Dr. Ma and Dr. Shuaib reported no disclosures. Dr. Saver has received research funding and personal fees from Medtronic-Abbott and Neuravia.
SOURCE: Ma H et al. Int J. Stroke. 2018 Oct;13(2S):235, Abstract 1014.
REPORTING FROM THE WORLD STROKE CONGRESS
Key clinical point:
Major finding: Patients who received thrombolysis 4.5-9 hours after stroke onset had a 44% increased rate of good outcomes, compared with controls.
Study details: EXTEND, a multicenter, controlled trial with 225 patients.
Disclosures: Dr. Ma and Dr. Shuaib had no disclosures. Dr. Saver has received research funding and personal fees from Medtronic-Abbott and Neuravia.
Source: Ma H et al. Int J. Stroke. 2018 Oct;13(2S):235, Abstract 1014.