User login
More restrictive hemoglobin threshold recommended for transfusion
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
FROM JAMA
Key clinical point: A restrictive threshold for red blood cell transfusion, in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL, is now recommended for most patients.
Major finding: A more restrictive threshold for red blood cell transfusion is not associated with an increased risk of mortality or other adverse outcomes from transfusion.
Data source: Updated guidelines from the AABB (formerly known as the American Association of Blood Banks).
Disclosures: Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies including CSL and Fresenius Kabi, but no other conflicts of interest were declared.
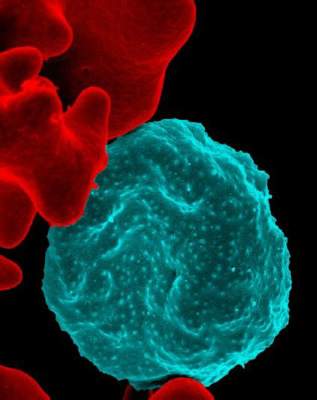
Donor NK cells elicited complete remissions in four of nine AML patients
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
FROM SCIENCE TRANSLATIONAL MEDICINE
Is stem-cell transplant curative for HIV infection?
DURBAN, SOUTH AFRICA – The 15 HIV-infected patients who have undergone allogeneic stem-cell transplant for life-threatening hematologic cancers under the auspices of the European EpiStem Consortium have uniformly demonstrated a profound and durable reduction in viral reservoir to a degree that hasn’t been approached by any other investigational cure strategy, Annemarie Wensing, MD, said at the 21st International AIDS Conference.
“We see an enormous reduction in the viral reservoir, and in two patients we cannot find any viable HIV in the blood using ultrasensitive tests. But we don’t know whether these patients are cured because they are still on antiretroviral therapy,” said Dr. Wensing of Utrecht (The Netherlands) University.
Non-Hodgkin’s lymphoma and Hodgkin’s lymphoma are 7-9 times more frequent in HIV-positive patients than in the general population. But allogeneic stem cell transplantation is an even higher-risk treatment in HIV-positive patients with life-threatening leukemia or lymphoma than in the HIV-negative population. Only 6 of the 15 EuroStem patients remain alive. Eight died within 4 months of the procedure and another died 2.5 years post-transplant, all from progression of their cancer or as a result of opportunistic infections arising during the immunosuppressive chemoablation that’s central to stem-cell transplantation. However, 3 of the 15 patients have survived longer than 3 years. In two of them, no HIV can be detected in blood or intestinal tissue using ultrasensitive tests, while in the third there is “only a slight trace,” according to Dr. Wensing, a clinical virologist.
EpiStem (the European Project to Guide and Investigate the Potential for HIV Cure by Stem-Cell Transplantation) is a multinational collaboration of European oncologists, infectious disease physicians, and other specialists. It was formed in response to the successful outcome of allogeneic stem cell transplantation for acute myeloid leukemia in HIV-positive Timothy Brown, more famously known as “the Berlin patient” (N Engl J Med. 2009 Feb 12;360(7):692-8). He has thus far survived 7 years off antiretroviral therapy.
Much has been made of the fact that Mr. Brown’s donor cells were homozygous for the CCR5 delta32 mutation, which confers natural resistance to HIV infection because it prevents the virus from infecting T cells. Only 1% or less of the population is homozygous for this mutation. But Dr. Wensing isn’t convinced that using donor cells with the mutation is a prerequisite for success. Indeed, while 4 of the 15 EpiStem patients received stem cells from donors homozygous for the mutation and another got donor cells heterozygous for the CCR5 delta32 mutation, the other 10 received stem cells capable of being infected by HIV – yet all 15 experienced an enormous reduction in their viral reservoir. And two of the three patients who have survived longer than 3 years got stem cells without the CCR5 delta32 mutation.
Dr. Wensing observed that a common denominator shared by Timothy Brown and the two EpiStem patients who have trace or undetectable HIV in blood or tissue samples more than 3 years post-transplant is that all three developed severe graft-versus-host disease in conjunction with their stem cell transplantation. She suspects this may have helped them to clear the infection, a hypothesis she intends to pursue further as EpiStem gathers more patients.
Eventually, if patients continue to test negative for HIV using ultrasensitive tests, it will be time to have a discussion with patients and their treating physicians as to whether they should continue on antiretroviral therapy.
“In the end it’s the patients’ decision, but they should be very well counseled because it can have medical and also psychological consequences if HIV returns,” she said.
EpiStem is funded by the American Foundation for AIDS Research Conssortium on HIV Eradication. Dr. Wensing reported having no financial conflicts regarding her presentation.
DURBAN, SOUTH AFRICA – The 15 HIV-infected patients who have undergone allogeneic stem-cell transplant for life-threatening hematologic cancers under the auspices of the European EpiStem Consortium have uniformly demonstrated a profound and durable reduction in viral reservoir to a degree that hasn’t been approached by any other investigational cure strategy, Annemarie Wensing, MD, said at the 21st International AIDS Conference.
“We see an enormous reduction in the viral reservoir, and in two patients we cannot find any viable HIV in the blood using ultrasensitive tests. But we don’t know whether these patients are cured because they are still on antiretroviral therapy,” said Dr. Wensing of Utrecht (The Netherlands) University.
Non-Hodgkin’s lymphoma and Hodgkin’s lymphoma are 7-9 times more frequent in HIV-positive patients than in the general population. But allogeneic stem cell transplantation is an even higher-risk treatment in HIV-positive patients with life-threatening leukemia or lymphoma than in the HIV-negative population. Only 6 of the 15 EuroStem patients remain alive. Eight died within 4 months of the procedure and another died 2.5 years post-transplant, all from progression of their cancer or as a result of opportunistic infections arising during the immunosuppressive chemoablation that’s central to stem-cell transplantation. However, 3 of the 15 patients have survived longer than 3 years. In two of them, no HIV can be detected in blood or intestinal tissue using ultrasensitive tests, while in the third there is “only a slight trace,” according to Dr. Wensing, a clinical virologist.
EpiStem (the European Project to Guide and Investigate the Potential for HIV Cure by Stem-Cell Transplantation) is a multinational collaboration of European oncologists, infectious disease physicians, and other specialists. It was formed in response to the successful outcome of allogeneic stem cell transplantation for acute myeloid leukemia in HIV-positive Timothy Brown, more famously known as “the Berlin patient” (N Engl J Med. 2009 Feb 12;360(7):692-8). He has thus far survived 7 years off antiretroviral therapy.
Much has been made of the fact that Mr. Brown’s donor cells were homozygous for the CCR5 delta32 mutation, which confers natural resistance to HIV infection because it prevents the virus from infecting T cells. Only 1% or less of the population is homozygous for this mutation. But Dr. Wensing isn’t convinced that using donor cells with the mutation is a prerequisite for success. Indeed, while 4 of the 15 EpiStem patients received stem cells from donors homozygous for the mutation and another got donor cells heterozygous for the CCR5 delta32 mutation, the other 10 received stem cells capable of being infected by HIV – yet all 15 experienced an enormous reduction in their viral reservoir. And two of the three patients who have survived longer than 3 years got stem cells without the CCR5 delta32 mutation.
Dr. Wensing observed that a common denominator shared by Timothy Brown and the two EpiStem patients who have trace or undetectable HIV in blood or tissue samples more than 3 years post-transplant is that all three developed severe graft-versus-host disease in conjunction with their stem cell transplantation. She suspects this may have helped them to clear the infection, a hypothesis she intends to pursue further as EpiStem gathers more patients.
Eventually, if patients continue to test negative for HIV using ultrasensitive tests, it will be time to have a discussion with patients and their treating physicians as to whether they should continue on antiretroviral therapy.
“In the end it’s the patients’ decision, but they should be very well counseled because it can have medical and also psychological consequences if HIV returns,” she said.
EpiStem is funded by the American Foundation for AIDS Research Conssortium on HIV Eradication. Dr. Wensing reported having no financial conflicts regarding her presentation.
DURBAN, SOUTH AFRICA – The 15 HIV-infected patients who have undergone allogeneic stem-cell transplant for life-threatening hematologic cancers under the auspices of the European EpiStem Consortium have uniformly demonstrated a profound and durable reduction in viral reservoir to a degree that hasn’t been approached by any other investigational cure strategy, Annemarie Wensing, MD, said at the 21st International AIDS Conference.
“We see an enormous reduction in the viral reservoir, and in two patients we cannot find any viable HIV in the blood using ultrasensitive tests. But we don’t know whether these patients are cured because they are still on antiretroviral therapy,” said Dr. Wensing of Utrecht (The Netherlands) University.
Non-Hodgkin’s lymphoma and Hodgkin’s lymphoma are 7-9 times more frequent in HIV-positive patients than in the general population. But allogeneic stem cell transplantation is an even higher-risk treatment in HIV-positive patients with life-threatening leukemia or lymphoma than in the HIV-negative population. Only 6 of the 15 EuroStem patients remain alive. Eight died within 4 months of the procedure and another died 2.5 years post-transplant, all from progression of their cancer or as a result of opportunistic infections arising during the immunosuppressive chemoablation that’s central to stem-cell transplantation. However, 3 of the 15 patients have survived longer than 3 years. In two of them, no HIV can be detected in blood or intestinal tissue using ultrasensitive tests, while in the third there is “only a slight trace,” according to Dr. Wensing, a clinical virologist.
EpiStem (the European Project to Guide and Investigate the Potential for HIV Cure by Stem-Cell Transplantation) is a multinational collaboration of European oncologists, infectious disease physicians, and other specialists. It was formed in response to the successful outcome of allogeneic stem cell transplantation for acute myeloid leukemia in HIV-positive Timothy Brown, more famously known as “the Berlin patient” (N Engl J Med. 2009 Feb 12;360(7):692-8). He has thus far survived 7 years off antiretroviral therapy.
Much has been made of the fact that Mr. Brown’s donor cells were homozygous for the CCR5 delta32 mutation, which confers natural resistance to HIV infection because it prevents the virus from infecting T cells. Only 1% or less of the population is homozygous for this mutation. But Dr. Wensing isn’t convinced that using donor cells with the mutation is a prerequisite for success. Indeed, while 4 of the 15 EpiStem patients received stem cells from donors homozygous for the mutation and another got donor cells heterozygous for the CCR5 delta32 mutation, the other 10 received stem cells capable of being infected by HIV – yet all 15 experienced an enormous reduction in their viral reservoir. And two of the three patients who have survived longer than 3 years got stem cells without the CCR5 delta32 mutation.
Dr. Wensing observed that a common denominator shared by Timothy Brown and the two EpiStem patients who have trace or undetectable HIV in blood or tissue samples more than 3 years post-transplant is that all three developed severe graft-versus-host disease in conjunction with their stem cell transplantation. She suspects this may have helped them to clear the infection, a hypothesis she intends to pursue further as EpiStem gathers more patients.
Eventually, if patients continue to test negative for HIV using ultrasensitive tests, it will be time to have a discussion with patients and their treating physicians as to whether they should continue on antiretroviral therapy.
“In the end it’s the patients’ decision, but they should be very well counseled because it can have medical and also psychological consequences if HIV returns,” she said.
EpiStem is funded by the American Foundation for AIDS Research Conssortium on HIV Eradication. Dr. Wensing reported having no financial conflicts regarding her presentation.
AT AIDS 2016
Key clinical point: It doesn’t appear to be necessary to use donor stem cells that are homozygous for the CCR5 delta32 mutation to achieve enormous sustained reductions in the viral reservoir in HIV-infected patients undergoing allogeneic stem cell transplantation for hematologic cancers.
Major finding: Two of three patients in a European series who have survived for longer than 3 years after stem-cell transplantation with undetectable or only trace HIV in their blood received donor cells lacking the rare CCR5 delta32 mutation.
Data source: EpiStem is an ongoing observational study of HIV-infected patients who undergo allogeneic stem cell transplantation for life-threatening hematologic cancers.
Disclosures: The EpiStem project is funded by the American Foundation for AIDS Research Conssortium on HIV Eradication. The presenter reported having no financial conflicts regarding her presentation.
New IDSA aspergillosis guidelines endorse galactomannan for diagnosis
New aspergillosis guidelines from the Infectious Diseases Society of America recommend serum and bronchoalveolar lavage galactomannan as a marker for the diagnosis of invasive Aspergillus in adult and pediatric patients who have hematologic malignancies or have undergone hematopoietic stem cell transplants.
Serial monitoring of serum galactomannan (GM) is also useful to monitor disease progression, therapeutic response, and prognosis in hematologic malignancy and hematopoietic stem cell transplant (HSCT) patients who have elevated baseline GM (Clin Infect Dis. 2016 Jun 29. doi: 10.1093/cid/ciw326).
Serum beta-D-glucan assays also are recommended for diagnosing invasive Aspergillus (IA) in high-risk hematologic malignancy and allogeneic HSCT patients, although these tests are not very specific for the infection.
The advice illustrates the Society’s emphasis on early diagnosis in its new guidelines, which supplant the group’s 2008 guidance. There are almost 100 recommendations covering – in depth – the management of invasive, allergic, and chronic Aspergillus infections in all their manifestations. It’s a step-by-step, how-to manual for handling the problem.
“Aspergillosis mortality rates have decreased significantly in recent years, but there is still significant mortality from the infection, and we have a ways to go. We felt that early diagnosis was key, which is why it’s such an important part of these guidelines,” said lead author Thomas Patterson, MD, chief of the Division of Infectious Diseases at the University of Texas Health Science Center, San Antonio. He highlighted the most important developments in a recent interview.
“We know a lot more since 2008 about the benefits of using biomarkers like GM in bronchoalveolar lavage samples, which could be highly useful for diagnosis. However, biomarkers have not been as well validated for biologic response and are not recommended” in most cases for monitoring how well patients are doing. Also, “biomarkers are not as useful in solid organ transplants; we discuss that” in the guidelines, Dr. Patterson said.
The society came out against routine polymerase chain reaction (PCR) testing of blood samples for diagnosis. Although there has been a lot of work on the technique, the evidence isn’t strong enough yet to establish overall clinical benefit, but there is emerging evidence for the diagnostic use of PCR in conjunction with radiologic findings.
For treatment, voriconazole remains the go-to drug, but the guidelines make room for more recently approved therapies. “We now have isavuconazole, which may be better tolerated,” but it’s recommended only as an alternative to voriconazole because evidence comes mostly from a single clinical trial, he said.
Posaconazole extended-release tablets are strongly recommended as prophylaxis based on high-quality evidence from studies in neutropenic patients. Posaconazole extended-release tablets result in significantly higher antifungal blood levels than those seen with voriconazole, and “it certainly has been useful in some patients”; however, posaconazole is not approved for primary therapy in the United States, Dr. Patterson said.
A large clinical trial that tested voriconazole plus an echinocandin against voriconazole alone found that in patients diagnosed using serum galactomannan – especially those with hematologic malignancies – outcomes were better with the combination. “The panel felt combinations could be considered in some patients” but didn’t recommend them for routine use because [again,] there’s not strong evidence,” he said.
For now, it seems that higher-risk patients with hematologic malignancies and those with more widespread disease might be the ones who benefit most from combination therapy.
“We also discussed allergic and saprophytic diseases. We know that some patients with allergic bronchopulmonary aspergillosis will respond to antifungal therapy, and perhaps reduce their need for steroids, so that’s now part of the suggestions, as well,” he said.
The IDSA funded the work. Dr. Patterson receives research funding from Astellas, Merck, and Revolution Medicines, and has been an adviser to numerous drug companies.
New aspergillosis guidelines from the Infectious Diseases Society of America recommend serum and bronchoalveolar lavage galactomannan as a marker for the diagnosis of invasive Aspergillus in adult and pediatric patients who have hematologic malignancies or have undergone hematopoietic stem cell transplants.
Serial monitoring of serum galactomannan (GM) is also useful to monitor disease progression, therapeutic response, and prognosis in hematologic malignancy and hematopoietic stem cell transplant (HSCT) patients who have elevated baseline GM (Clin Infect Dis. 2016 Jun 29. doi: 10.1093/cid/ciw326).
Serum beta-D-glucan assays also are recommended for diagnosing invasive Aspergillus (IA) in high-risk hematologic malignancy and allogeneic HSCT patients, although these tests are not very specific for the infection.
The advice illustrates the Society’s emphasis on early diagnosis in its new guidelines, which supplant the group’s 2008 guidance. There are almost 100 recommendations covering – in depth – the management of invasive, allergic, and chronic Aspergillus infections in all their manifestations. It’s a step-by-step, how-to manual for handling the problem.
“Aspergillosis mortality rates have decreased significantly in recent years, but there is still significant mortality from the infection, and we have a ways to go. We felt that early diagnosis was key, which is why it’s such an important part of these guidelines,” said lead author Thomas Patterson, MD, chief of the Division of Infectious Diseases at the University of Texas Health Science Center, San Antonio. He highlighted the most important developments in a recent interview.
“We know a lot more since 2008 about the benefits of using biomarkers like GM in bronchoalveolar lavage samples, which could be highly useful for diagnosis. However, biomarkers have not been as well validated for biologic response and are not recommended” in most cases for monitoring how well patients are doing. Also, “biomarkers are not as useful in solid organ transplants; we discuss that” in the guidelines, Dr. Patterson said.
The society came out against routine polymerase chain reaction (PCR) testing of blood samples for diagnosis. Although there has been a lot of work on the technique, the evidence isn’t strong enough yet to establish overall clinical benefit, but there is emerging evidence for the diagnostic use of PCR in conjunction with radiologic findings.
For treatment, voriconazole remains the go-to drug, but the guidelines make room for more recently approved therapies. “We now have isavuconazole, which may be better tolerated,” but it’s recommended only as an alternative to voriconazole because evidence comes mostly from a single clinical trial, he said.
Posaconazole extended-release tablets are strongly recommended as prophylaxis based on high-quality evidence from studies in neutropenic patients. Posaconazole extended-release tablets result in significantly higher antifungal blood levels than those seen with voriconazole, and “it certainly has been useful in some patients”; however, posaconazole is not approved for primary therapy in the United States, Dr. Patterson said.
A large clinical trial that tested voriconazole plus an echinocandin against voriconazole alone found that in patients diagnosed using serum galactomannan – especially those with hematologic malignancies – outcomes were better with the combination. “The panel felt combinations could be considered in some patients” but didn’t recommend them for routine use because [again,] there’s not strong evidence,” he said.
For now, it seems that higher-risk patients with hematologic malignancies and those with more widespread disease might be the ones who benefit most from combination therapy.
“We also discussed allergic and saprophytic diseases. We know that some patients with allergic bronchopulmonary aspergillosis will respond to antifungal therapy, and perhaps reduce their need for steroids, so that’s now part of the suggestions, as well,” he said.
The IDSA funded the work. Dr. Patterson receives research funding from Astellas, Merck, and Revolution Medicines, and has been an adviser to numerous drug companies.
New aspergillosis guidelines from the Infectious Diseases Society of America recommend serum and bronchoalveolar lavage galactomannan as a marker for the diagnosis of invasive Aspergillus in adult and pediatric patients who have hematologic malignancies or have undergone hematopoietic stem cell transplants.
Serial monitoring of serum galactomannan (GM) is also useful to monitor disease progression, therapeutic response, and prognosis in hematologic malignancy and hematopoietic stem cell transplant (HSCT) patients who have elevated baseline GM (Clin Infect Dis. 2016 Jun 29. doi: 10.1093/cid/ciw326).
Serum beta-D-glucan assays also are recommended for diagnosing invasive Aspergillus (IA) in high-risk hematologic malignancy and allogeneic HSCT patients, although these tests are not very specific for the infection.
The advice illustrates the Society’s emphasis on early diagnosis in its new guidelines, which supplant the group’s 2008 guidance. There are almost 100 recommendations covering – in depth – the management of invasive, allergic, and chronic Aspergillus infections in all their manifestations. It’s a step-by-step, how-to manual for handling the problem.
“Aspergillosis mortality rates have decreased significantly in recent years, but there is still significant mortality from the infection, and we have a ways to go. We felt that early diagnosis was key, which is why it’s such an important part of these guidelines,” said lead author Thomas Patterson, MD, chief of the Division of Infectious Diseases at the University of Texas Health Science Center, San Antonio. He highlighted the most important developments in a recent interview.
“We know a lot more since 2008 about the benefits of using biomarkers like GM in bronchoalveolar lavage samples, which could be highly useful for diagnosis. However, biomarkers have not been as well validated for biologic response and are not recommended” in most cases for monitoring how well patients are doing. Also, “biomarkers are not as useful in solid organ transplants; we discuss that” in the guidelines, Dr. Patterson said.
The society came out against routine polymerase chain reaction (PCR) testing of blood samples for diagnosis. Although there has been a lot of work on the technique, the evidence isn’t strong enough yet to establish overall clinical benefit, but there is emerging evidence for the diagnostic use of PCR in conjunction with radiologic findings.
For treatment, voriconazole remains the go-to drug, but the guidelines make room for more recently approved therapies. “We now have isavuconazole, which may be better tolerated,” but it’s recommended only as an alternative to voriconazole because evidence comes mostly from a single clinical trial, he said.
Posaconazole extended-release tablets are strongly recommended as prophylaxis based on high-quality evidence from studies in neutropenic patients. Posaconazole extended-release tablets result in significantly higher antifungal blood levels than those seen with voriconazole, and “it certainly has been useful in some patients”; however, posaconazole is not approved for primary therapy in the United States, Dr. Patterson said.
A large clinical trial that tested voriconazole plus an echinocandin against voriconazole alone found that in patients diagnosed using serum galactomannan – especially those with hematologic malignancies – outcomes were better with the combination. “The panel felt combinations could be considered in some patients” but didn’t recommend them for routine use because [again,] there’s not strong evidence,” he said.
For now, it seems that higher-risk patients with hematologic malignancies and those with more widespread disease might be the ones who benefit most from combination therapy.
“We also discussed allergic and saprophytic diseases. We know that some patients with allergic bronchopulmonary aspergillosis will respond to antifungal therapy, and perhaps reduce their need for steroids, so that’s now part of the suggestions, as well,” he said.
The IDSA funded the work. Dr. Patterson receives research funding from Astellas, Merck, and Revolution Medicines, and has been an adviser to numerous drug companies.
FROM CLINICAL INFECTIOUS DISEASES
Sex-mismatched RBCs associated with increased mortality after cardiac surgery
Transfusing sex-mismatched red blood cells (RBCs) was associated with an increased risk of death in people undergoing heart bypass surgery or aortic valve replacement, based on results of a retrospective single-center study of almost 10,000 transfusions in cardiac surgery patients.
Each unit of sex-mismatched red blood cells (RBCs) transfused was associated with an increased risk of death (hazard ratio, 1.083; 95% confidence interval, 1.028-1.140; P = .003). In addition, transfusing 1-2 units of non–leukocyte depleted RBCs was associated with a significant increase in the risk of death during the first year after surgery (HR, 1.426; 95% CI, 1.004-2.024; P = .047).
Transfusion of 1-2 units of leukocyte-depleted RBCs and the age of blood products was not associated with increased mortality (J Thorac Cardiovasc Surg. 2016;152:223-32.e1).
“Factors such as ABO group, Rh profile and sex of the PRBC [packed RBC] donor generally have been overlooked, as has the variation in postdonation treatment of blood,” in the outcomes of cardiac surgery patients, researchers led by Henrik Bjursten, MD, PhD, of Lund (Sweden) University, reported.
The study involved 9,907 patients at Lund University from 2002 to 2012: 7,696 had coronary artery bypass grafting (CABG); 1,216 had aortic valve replacement (AVR); and 995 concomitantly had both procedures. PRBC transfusions were given to nearly 51% of the patients. Compared with the group that did not receive PRBC transfusions, the transfused group had significantly higher rates of heart attack after surgery (1.5% vs. 0.6%), infection (0.6% vs. 0.3%), reoperation for bleeding (4.3% vs. 0.2%), 30-day death (0.7% vs. 0.2%), and overall death (25.9% vs. 12.6%).
Based on an analysis that factored in 24 different variables, transfusion of 1-2 units of non–leukocyte depleted PRBCs was associated with a HR of 1.426, but the same amount of leukocyte-depleted PRBCs did not increase risk (HR, 0.981). However, transfusion of 5-7 units of leukocyte-depleted RBCs was associated with decreased survival, as was transfusion of sex-mismatched PRBCs, associated with a HR of 1.046-1.133 per unit, Dr. Bjursten and colleagues wrote. “In this cohort, 58% of transfusions were sex mismatched, and thus we interpret the result as relatively robust and clinically relevant.”
Patients having combined CABG and AVR were more likely to have PRBC transfusions than patients who had a single procedure. Additionally, the increased death rate in the PRBC transfusion group may have been related to age and comorbidities such as diabetes, chronic obstructive pulmonary disease, and cardiac insufficiency. “Blood transfusion in part is a biomarker for advanced disease,” Dr. Bjursten and coauthors said. While patient who received PRBC transfusions may have been sicker, they did not require greater use of the ICU than patients who did not receive transfusions.
Dr. Bjursten disclosed receiving consulting fees from Boston Scientific. Coauthor Lars Algotsson, MD, PhD, disclosed receiving lecture fees from Abbott. All other authors had no financial disclosures.
The study results expand on the knowledge of potential sex-mismatch risks and reiterates the potential benefits of limiting transfusion to leukocyte-depleted PRBC.
Strengths of the study are its size and its use of the Swedish national tax registry to accurately count deaths. Weaknesses include its retrospective design and inherent issues with advanced statistical analysis, and the failure to address secondary morbidity outcomes. Cardiac surgery’s mortality is multifactorial and secondary outcomes would have strengthened the results.
Unlike previous studies, this study showed that 1 or 2 units of leukocyte-depleted PRBCs did not increase mortality.
This study suggests that sex-mismatched blood transfusions may create a high enough risk to necessitate a change in transfusion protocols. Further, many countries already have universal strategies to use leukocyte-depleted PRBC, and perhaps this study should call for the United States to pursue the same policy.
Jennifer Banayan, MD, and Mark Chaney, MD, of the University of Chicago made their remarks in a commentary (J Thorac Cardiovasc Surg. 2016;152:18-9) that accompanied the study.
The study results expand on the knowledge of potential sex-mismatch risks and reiterates the potential benefits of limiting transfusion to leukocyte-depleted PRBC.
Strengths of the study are its size and its use of the Swedish national tax registry to accurately count deaths. Weaknesses include its retrospective design and inherent issues with advanced statistical analysis, and the failure to address secondary morbidity outcomes. Cardiac surgery’s mortality is multifactorial and secondary outcomes would have strengthened the results.
Unlike previous studies, this study showed that 1 or 2 units of leukocyte-depleted PRBCs did not increase mortality.
This study suggests that sex-mismatched blood transfusions may create a high enough risk to necessitate a change in transfusion protocols. Further, many countries already have universal strategies to use leukocyte-depleted PRBC, and perhaps this study should call for the United States to pursue the same policy.
Jennifer Banayan, MD, and Mark Chaney, MD, of the University of Chicago made their remarks in a commentary (J Thorac Cardiovasc Surg. 2016;152:18-9) that accompanied the study.
The study results expand on the knowledge of potential sex-mismatch risks and reiterates the potential benefits of limiting transfusion to leukocyte-depleted PRBC.
Strengths of the study are its size and its use of the Swedish national tax registry to accurately count deaths. Weaknesses include its retrospective design and inherent issues with advanced statistical analysis, and the failure to address secondary morbidity outcomes. Cardiac surgery’s mortality is multifactorial and secondary outcomes would have strengthened the results.
Unlike previous studies, this study showed that 1 or 2 units of leukocyte-depleted PRBCs did not increase mortality.
This study suggests that sex-mismatched blood transfusions may create a high enough risk to necessitate a change in transfusion protocols. Further, many countries already have universal strategies to use leukocyte-depleted PRBC, and perhaps this study should call for the United States to pursue the same policy.
Jennifer Banayan, MD, and Mark Chaney, MD, of the University of Chicago made their remarks in a commentary (J Thorac Cardiovasc Surg. 2016;152:18-9) that accompanied the study.
Transfusing sex-mismatched red blood cells (RBCs) was associated with an increased risk of death in people undergoing heart bypass surgery or aortic valve replacement, based on results of a retrospective single-center study of almost 10,000 transfusions in cardiac surgery patients.
Each unit of sex-mismatched red blood cells (RBCs) transfused was associated with an increased risk of death (hazard ratio, 1.083; 95% confidence interval, 1.028-1.140; P = .003). In addition, transfusing 1-2 units of non–leukocyte depleted RBCs was associated with a significant increase in the risk of death during the first year after surgery (HR, 1.426; 95% CI, 1.004-2.024; P = .047).
Transfusion of 1-2 units of leukocyte-depleted RBCs and the age of blood products was not associated with increased mortality (J Thorac Cardiovasc Surg. 2016;152:223-32.e1).
“Factors such as ABO group, Rh profile and sex of the PRBC [packed RBC] donor generally have been overlooked, as has the variation in postdonation treatment of blood,” in the outcomes of cardiac surgery patients, researchers led by Henrik Bjursten, MD, PhD, of Lund (Sweden) University, reported.
The study involved 9,907 patients at Lund University from 2002 to 2012: 7,696 had coronary artery bypass grafting (CABG); 1,216 had aortic valve replacement (AVR); and 995 concomitantly had both procedures. PRBC transfusions were given to nearly 51% of the patients. Compared with the group that did not receive PRBC transfusions, the transfused group had significantly higher rates of heart attack after surgery (1.5% vs. 0.6%), infection (0.6% vs. 0.3%), reoperation for bleeding (4.3% vs. 0.2%), 30-day death (0.7% vs. 0.2%), and overall death (25.9% vs. 12.6%).
Based on an analysis that factored in 24 different variables, transfusion of 1-2 units of non–leukocyte depleted PRBCs was associated with a HR of 1.426, but the same amount of leukocyte-depleted PRBCs did not increase risk (HR, 0.981). However, transfusion of 5-7 units of leukocyte-depleted RBCs was associated with decreased survival, as was transfusion of sex-mismatched PRBCs, associated with a HR of 1.046-1.133 per unit, Dr. Bjursten and colleagues wrote. “In this cohort, 58% of transfusions were sex mismatched, and thus we interpret the result as relatively robust and clinically relevant.”
Patients having combined CABG and AVR were more likely to have PRBC transfusions than patients who had a single procedure. Additionally, the increased death rate in the PRBC transfusion group may have been related to age and comorbidities such as diabetes, chronic obstructive pulmonary disease, and cardiac insufficiency. “Blood transfusion in part is a biomarker for advanced disease,” Dr. Bjursten and coauthors said. While patient who received PRBC transfusions may have been sicker, they did not require greater use of the ICU than patients who did not receive transfusions.
Dr. Bjursten disclosed receiving consulting fees from Boston Scientific. Coauthor Lars Algotsson, MD, PhD, disclosed receiving lecture fees from Abbott. All other authors had no financial disclosures.
Transfusing sex-mismatched red blood cells (RBCs) was associated with an increased risk of death in people undergoing heart bypass surgery or aortic valve replacement, based on results of a retrospective single-center study of almost 10,000 transfusions in cardiac surgery patients.
Each unit of sex-mismatched red blood cells (RBCs) transfused was associated with an increased risk of death (hazard ratio, 1.083; 95% confidence interval, 1.028-1.140; P = .003). In addition, transfusing 1-2 units of non–leukocyte depleted RBCs was associated with a significant increase in the risk of death during the first year after surgery (HR, 1.426; 95% CI, 1.004-2.024; P = .047).
Transfusion of 1-2 units of leukocyte-depleted RBCs and the age of blood products was not associated with increased mortality (J Thorac Cardiovasc Surg. 2016;152:223-32.e1).
“Factors such as ABO group, Rh profile and sex of the PRBC [packed RBC] donor generally have been overlooked, as has the variation in postdonation treatment of blood,” in the outcomes of cardiac surgery patients, researchers led by Henrik Bjursten, MD, PhD, of Lund (Sweden) University, reported.
The study involved 9,907 patients at Lund University from 2002 to 2012: 7,696 had coronary artery bypass grafting (CABG); 1,216 had aortic valve replacement (AVR); and 995 concomitantly had both procedures. PRBC transfusions were given to nearly 51% of the patients. Compared with the group that did not receive PRBC transfusions, the transfused group had significantly higher rates of heart attack after surgery (1.5% vs. 0.6%), infection (0.6% vs. 0.3%), reoperation for bleeding (4.3% vs. 0.2%), 30-day death (0.7% vs. 0.2%), and overall death (25.9% vs. 12.6%).
Based on an analysis that factored in 24 different variables, transfusion of 1-2 units of non–leukocyte depleted PRBCs was associated with a HR of 1.426, but the same amount of leukocyte-depleted PRBCs did not increase risk (HR, 0.981). However, transfusion of 5-7 units of leukocyte-depleted RBCs was associated with decreased survival, as was transfusion of sex-mismatched PRBCs, associated with a HR of 1.046-1.133 per unit, Dr. Bjursten and colleagues wrote. “In this cohort, 58% of transfusions were sex mismatched, and thus we interpret the result as relatively robust and clinically relevant.”
Patients having combined CABG and AVR were more likely to have PRBC transfusions than patients who had a single procedure. Additionally, the increased death rate in the PRBC transfusion group may have been related to age and comorbidities such as diabetes, chronic obstructive pulmonary disease, and cardiac insufficiency. “Blood transfusion in part is a biomarker for advanced disease,” Dr. Bjursten and coauthors said. While patient who received PRBC transfusions may have been sicker, they did not require greater use of the ICU than patients who did not receive transfusions.
Dr. Bjursten disclosed receiving consulting fees from Boston Scientific. Coauthor Lars Algotsson, MD, PhD, disclosed receiving lecture fees from Abbott. All other authors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Transfusion of sex-mismatched and non–leukocyte depleted PRBCs may impact survival after cardiac surgery.
Major finding: Transfusion of 1-2 units of non–leukocyte depleted PRBCs has a hazard ratio of 1.426.
Data source: Single-center, retrospective study of 9,007 patients who had CABG or AVR, or both, from 2002 to 2012. The study used the Swedish national tax registry to track deaths.
Disclosures: Lead author Dr. Bjursten disclosed receiving consulting fees from Boston Scientific. Coauthor Lars Algotsson, MD, PhD, disclosed receiving lecture fees from Abbott. All other authors have nothing to disclose with regard to commercial support.
Cord blood cell infusions reduce cGVHD incidence
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Mesenchymal stromal cell infusions may reduce risk of chronic graft-versus-host disease following allogeneic stem cell transplants.
Major finding: The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27.4%, compared with 49% for placebo-treated controls.
Data source: Randomized, double-blind, controlled trial in 124 patients following HSCT for hematologic malignancies.
Disclosures: The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
FDA places CAR-T cell trial on hold following patient deaths
The Food and Drug Administration placed Juno Therapeutics’ phase II ROCKET trial, involving CAR-T cell therapy, on clinical hold following two treatment-related patient deaths caused by excess fluid accumulation in the brain.
The ROCKET trial is a single-arm, multicenter phase II study treating adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia with an infusion of the patient’s own T cells that have been genetically modified to express a chimeric antigen receptor (CAR) that will bind to CD19-expressing leukemia cells. This treatment is referred to as JCAR015, and the ROCKET trial is only one of three current clinical trials testing its safety and efficacy.
Just before the ROCKET trial commenced, researchers added the chemotherapy drug fludarabine, which was successful in improving the performance of other immunotherapies, to the JCAR015 infusion. Researchers involved in the trial reported that the addition of this drug was likely the cause of the patient deaths.
Juno Therapeuticswill submit a revised trial protocol and patient consent form to the FDA before the hold is lifted, Juno reported in a written statement. The other trials led by Juno Therapeutics involving CAR-T cell product candidates are not affected.
On Twitter @jessnicolecraig
The Food and Drug Administration placed Juno Therapeutics’ phase II ROCKET trial, involving CAR-T cell therapy, on clinical hold following two treatment-related patient deaths caused by excess fluid accumulation in the brain.
The ROCKET trial is a single-arm, multicenter phase II study treating adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia with an infusion of the patient’s own T cells that have been genetically modified to express a chimeric antigen receptor (CAR) that will bind to CD19-expressing leukemia cells. This treatment is referred to as JCAR015, and the ROCKET trial is only one of three current clinical trials testing its safety and efficacy.
Just before the ROCKET trial commenced, researchers added the chemotherapy drug fludarabine, which was successful in improving the performance of other immunotherapies, to the JCAR015 infusion. Researchers involved in the trial reported that the addition of this drug was likely the cause of the patient deaths.
Juno Therapeuticswill submit a revised trial protocol and patient consent form to the FDA before the hold is lifted, Juno reported in a written statement. The other trials led by Juno Therapeutics involving CAR-T cell product candidates are not affected.
On Twitter @jessnicolecraig
The Food and Drug Administration placed Juno Therapeutics’ phase II ROCKET trial, involving CAR-T cell therapy, on clinical hold following two treatment-related patient deaths caused by excess fluid accumulation in the brain.
The ROCKET trial is a single-arm, multicenter phase II study treating adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia with an infusion of the patient’s own T cells that have been genetically modified to express a chimeric antigen receptor (CAR) that will bind to CD19-expressing leukemia cells. This treatment is referred to as JCAR015, and the ROCKET trial is only one of three current clinical trials testing its safety and efficacy.
Just before the ROCKET trial commenced, researchers added the chemotherapy drug fludarabine, which was successful in improving the performance of other immunotherapies, to the JCAR015 infusion. Researchers involved in the trial reported that the addition of this drug was likely the cause of the patient deaths.
Juno Therapeuticswill submit a revised trial protocol and patient consent form to the FDA before the hold is lifted, Juno reported in a written statement. The other trials led by Juno Therapeutics involving CAR-T cell product candidates are not affected.
On Twitter @jessnicolecraig
Pathogen-reduced blood may cut transfusion-transmitted malaria
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
FROM THE LANCET
Key clinical point: The incidence of transfusion-transmitted malaria can be reduced by treating whole blood with a pathogen reduction system.
Major finding: Patients receiving pathogen-reduced whole blood had a lower incidence of transfusion-transmitted malaria (4%) than those who received standard treatment (22%).
Data source: Patients with anemia from a single center in Ghana being supported with whole blood transfusion.
Disclosures: Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed ties to the funding source.
ASH: HLA-identical sibling transplants “excellent” in eligble SCD patients
ORLANDO – For patients with severe sickle cell disease, stem cell transplants from an HLA identical sibling are associated with “excellent” 3-year overall and event-free survival, results of a retrospective analysis show.
Data on 1,000 hematopoietic stem cell transplants (HSCT) in children and adults with sickle-cell disease performed in 88 centers in 23 countries showed a 3-year event-free-survival (EFS) rate of 90%, and 3-year overall survival (OS) rate of 94%, reported Dr. Barbara Cappelli from the Eurocord International Registry in Paris, France.
“Early referral to transplant for patients with severe sickle-cell disease is warranted, as age is an independent predictor for both event-free survival and overall survival,” she said about the study at a briefing at the American Society of Hematology annual meeting.
Patients who received donor cord blood had the best 3-year OS, at 99%, compared with 94% for patients who received bone marrow grafts, and 80% for those who received peripheral blood stem cells (PBSC).
“Transplants from peripheral blood are not recommended, because the result that there is higher mortality with transplants with peripheral blood,” she said.
The findings provide further evidence that for patients with severe sickle-disease who have an HLA-identical sibling available as a donor, HSCT can be curative with good safety, commented Dr. Alexis Thompson, a professor of hematology at the Robert H. Lurie Children’s Hospital of Chicago, Illinois.
Dr. Thompson was not involved in the study, but moderated a briefing where the data were presented.
International Registries
HSCT is the only therapy currently known to be curative for sickle-cell disease, but due to the risk for early and late complications it is generally reserved for patients with the most severe anemia or most disabling symptoms.
To evaluate the efficacy and safety of HSCT for sickle-cell disease, the investigators took a retrospective look at data from bone marrow transplant registries covering Europe, Brazil, the United States, and other reporting centers.
They searched for data on all patients with sickle-cell disease, children and adults, who received a transplant from an HLA identical sibling from 1986 through 2013.
The majority of patients (85%) were younger than 16, with the median age at HSCT of 9 years (range 1 to 54 years). Stroke was the most common indication for HSCT.
In all, 87% of patients received a myeloablative conditioning regimen based on busulfan combined with either cyclophosphamide or fludarabine. The remaining 13% of patients underwent a reduced-intensity conditioning regimen, primarily with fludarabine and cyclophosphamide.
In vivo T-cell depletion was performed in 70% of patients, either with anti-thymocyte globulin (630 patients) or with alemtumumab (76).
Prophylaxis for graft vs. host disease (GVHD) was predominantly cyclosporine as monotherapy or in combination with methotrexate.
A large majority of patients (84%) received bone marrow grafts, 7% got PBSCs, and 9% received umbilical cord blood.
By 60 days, the cumulative incidence of engraftment was 98%, with a median cumulative incidence of platelet engraftment of 25 days.
The cumulative incidence of acute GVHD (within 100 days of transplant) 14.3%, and the cumulative incidence of chronic GVHD (out to 3 years) was 13.3%
In all, 71 patients (7%) required autologous reconstitution, 45 because of late graft failure, 31 patients (3%) underwent a second transplant and 67 patients (7%) died. Of the patients who died, 6% had received bone marrow, 1% had received cord blood, and 21% had received PBSC.
As noted before, respective EFS and OS 3 years after transplant were 90% and 94%.
In multivariate analysis controlled for transplant and demographic characteristics, the authors found that younger age at transplant and use of bone marrow or cord blood were independently associated with better EFS and OS. In addition, 3-year overall survival was significantly better among patients who received transplants from the year 2000 on.
The risk for acute GVHD was significantly associated with increasing age, but none of the variables tested were associated with chronic GVHD.
Dr. Cappelli said that ways to improve outcomes include performing pre-or post-natal diagnosis in at-risk families, performing HLA typing of all family members at the time of diagnosis, and going to transplant as soon as the criteria for severe sickle-cell disease are met.
The study was supported by Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR. Dr. Cappelli and Dr. Johnson reported having no conflicts of interest.
ORLANDO – For patients with severe sickle cell disease, stem cell transplants from an HLA identical sibling are associated with “excellent” 3-year overall and event-free survival, results of a retrospective analysis show.
Data on 1,000 hematopoietic stem cell transplants (HSCT) in children and adults with sickle-cell disease performed in 88 centers in 23 countries showed a 3-year event-free-survival (EFS) rate of 90%, and 3-year overall survival (OS) rate of 94%, reported Dr. Barbara Cappelli from the Eurocord International Registry in Paris, France.
“Early referral to transplant for patients with severe sickle-cell disease is warranted, as age is an independent predictor for both event-free survival and overall survival,” she said about the study at a briefing at the American Society of Hematology annual meeting.
Patients who received donor cord blood had the best 3-year OS, at 99%, compared with 94% for patients who received bone marrow grafts, and 80% for those who received peripheral blood stem cells (PBSC).
“Transplants from peripheral blood are not recommended, because the result that there is higher mortality with transplants with peripheral blood,” she said.
The findings provide further evidence that for patients with severe sickle-disease who have an HLA-identical sibling available as a donor, HSCT can be curative with good safety, commented Dr. Alexis Thompson, a professor of hematology at the Robert H. Lurie Children’s Hospital of Chicago, Illinois.
Dr. Thompson was not involved in the study, but moderated a briefing where the data were presented.
International Registries
HSCT is the only therapy currently known to be curative for sickle-cell disease, but due to the risk for early and late complications it is generally reserved for patients with the most severe anemia or most disabling symptoms.
To evaluate the efficacy and safety of HSCT for sickle-cell disease, the investigators took a retrospective look at data from bone marrow transplant registries covering Europe, Brazil, the United States, and other reporting centers.
They searched for data on all patients with sickle-cell disease, children and adults, who received a transplant from an HLA identical sibling from 1986 through 2013.
The majority of patients (85%) were younger than 16, with the median age at HSCT of 9 years (range 1 to 54 years). Stroke was the most common indication for HSCT.
In all, 87% of patients received a myeloablative conditioning regimen based on busulfan combined with either cyclophosphamide or fludarabine. The remaining 13% of patients underwent a reduced-intensity conditioning regimen, primarily with fludarabine and cyclophosphamide.
In vivo T-cell depletion was performed in 70% of patients, either with anti-thymocyte globulin (630 patients) or with alemtumumab (76).
Prophylaxis for graft vs. host disease (GVHD) was predominantly cyclosporine as monotherapy or in combination with methotrexate.
A large majority of patients (84%) received bone marrow grafts, 7% got PBSCs, and 9% received umbilical cord blood.
By 60 days, the cumulative incidence of engraftment was 98%, with a median cumulative incidence of platelet engraftment of 25 days.
The cumulative incidence of acute GVHD (within 100 days of transplant) 14.3%, and the cumulative incidence of chronic GVHD (out to 3 years) was 13.3%
In all, 71 patients (7%) required autologous reconstitution, 45 because of late graft failure, 31 patients (3%) underwent a second transplant and 67 patients (7%) died. Of the patients who died, 6% had received bone marrow, 1% had received cord blood, and 21% had received PBSC.
As noted before, respective EFS and OS 3 years after transplant were 90% and 94%.
In multivariate analysis controlled for transplant and demographic characteristics, the authors found that younger age at transplant and use of bone marrow or cord blood were independently associated with better EFS and OS. In addition, 3-year overall survival was significantly better among patients who received transplants from the year 2000 on.
The risk for acute GVHD was significantly associated with increasing age, but none of the variables tested were associated with chronic GVHD.
Dr. Cappelli said that ways to improve outcomes include performing pre-or post-natal diagnosis in at-risk families, performing HLA typing of all family members at the time of diagnosis, and going to transplant as soon as the criteria for severe sickle-cell disease are met.
The study was supported by Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR. Dr. Cappelli and Dr. Johnson reported having no conflicts of interest.
ORLANDO – For patients with severe sickle cell disease, stem cell transplants from an HLA identical sibling are associated with “excellent” 3-year overall and event-free survival, results of a retrospective analysis show.
Data on 1,000 hematopoietic stem cell transplants (HSCT) in children and adults with sickle-cell disease performed in 88 centers in 23 countries showed a 3-year event-free-survival (EFS) rate of 90%, and 3-year overall survival (OS) rate of 94%, reported Dr. Barbara Cappelli from the Eurocord International Registry in Paris, France.
“Early referral to transplant for patients with severe sickle-cell disease is warranted, as age is an independent predictor for both event-free survival and overall survival,” she said about the study at a briefing at the American Society of Hematology annual meeting.
Patients who received donor cord blood had the best 3-year OS, at 99%, compared with 94% for patients who received bone marrow grafts, and 80% for those who received peripheral blood stem cells (PBSC).
“Transplants from peripheral blood are not recommended, because the result that there is higher mortality with transplants with peripheral blood,” she said.
The findings provide further evidence that for patients with severe sickle-disease who have an HLA-identical sibling available as a donor, HSCT can be curative with good safety, commented Dr. Alexis Thompson, a professor of hematology at the Robert H. Lurie Children’s Hospital of Chicago, Illinois.
Dr. Thompson was not involved in the study, but moderated a briefing where the data were presented.
International Registries
HSCT is the only therapy currently known to be curative for sickle-cell disease, but due to the risk for early and late complications it is generally reserved for patients with the most severe anemia or most disabling symptoms.
To evaluate the efficacy and safety of HSCT for sickle-cell disease, the investigators took a retrospective look at data from bone marrow transplant registries covering Europe, Brazil, the United States, and other reporting centers.
They searched for data on all patients with sickle-cell disease, children and adults, who received a transplant from an HLA identical sibling from 1986 through 2013.
The majority of patients (85%) were younger than 16, with the median age at HSCT of 9 years (range 1 to 54 years). Stroke was the most common indication for HSCT.
In all, 87% of patients received a myeloablative conditioning regimen based on busulfan combined with either cyclophosphamide or fludarabine. The remaining 13% of patients underwent a reduced-intensity conditioning regimen, primarily with fludarabine and cyclophosphamide.
In vivo T-cell depletion was performed in 70% of patients, either with anti-thymocyte globulin (630 patients) or with alemtumumab (76).
Prophylaxis for graft vs. host disease (GVHD) was predominantly cyclosporine as monotherapy or in combination with methotrexate.
A large majority of patients (84%) received bone marrow grafts, 7% got PBSCs, and 9% received umbilical cord blood.
By 60 days, the cumulative incidence of engraftment was 98%, with a median cumulative incidence of platelet engraftment of 25 days.
The cumulative incidence of acute GVHD (within 100 days of transplant) 14.3%, and the cumulative incidence of chronic GVHD (out to 3 years) was 13.3%
In all, 71 patients (7%) required autologous reconstitution, 45 because of late graft failure, 31 patients (3%) underwent a second transplant and 67 patients (7%) died. Of the patients who died, 6% had received bone marrow, 1% had received cord blood, and 21% had received PBSC.
As noted before, respective EFS and OS 3 years after transplant were 90% and 94%.
In multivariate analysis controlled for transplant and demographic characteristics, the authors found that younger age at transplant and use of bone marrow or cord blood were independently associated with better EFS and OS. In addition, 3-year overall survival was significantly better among patients who received transplants from the year 2000 on.
The risk for acute GVHD was significantly associated with increasing age, but none of the variables tested were associated with chronic GVHD.
Dr. Cappelli said that ways to improve outcomes include performing pre-or post-natal diagnosis in at-risk families, performing HLA typing of all family members at the time of diagnosis, and going to transplant as soon as the criteria for severe sickle-cell disease are met.
The study was supported by Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR. Dr. Cappelli and Dr. Johnson reported having no conflicts of interest.
AT ASH 2015
Key clinical point: Bone marrow transplants from HLA-identical siblings are frequently curative of sickle-cell disease.
Major finding: Three-year event-free survival among 1000 patients was 90%, and 3-year overall survival was 94%.
Data source: Retrospective review of registry data on 1000 patients who underwent hematopoietic stem cell transplants with HLA-identical sibling donors.
Disclosures: The study was supported by Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR. Dr. Cappelli and Dr. Johnson reported having no conflicts of interest.
VIDEO: RBCs have extended shelf life, randomized trial shows
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015