User login
Ulipristal reduces bleeding with contraceptive implant
Ulipristal acetate reduces breakthrough bleeding in women with etonogestrel implants, according to new findings.
After 30 days, patients treated with ulipristal were more satisfied with their bleeding profiles than were those given placebo, reported Rachel E. Zigler, MD, of the department of obstetrics and gynecology at Washington University in St. Louis and her colleagues.
About half of women experience unscheduled bleeding within the first 6 months of etonogestrel implantation, causing many to discontinue treatment. The etiology of this phenomenon is poorly understood.
“One leading theory is that sustained exposure to a progestin can lead to endometrial angiogenesis disruption, resulting in the development of a dense venous network that is fragile and prone to bleeding,” the researchers wrote in Obstetrics & Gynecology.
Ulipristal acetate is a selective progesterone receptor modulator approved for emergency contraception in the United States. Outside the United States, it is used to treat abnormal uterine bleeding in cases of uterine leiomyoma. Ulipristal acts directly upon myometrial and endometrial tissue and “may also displace local progestin within the uterus to counteract bleeding secondary to … a dense, fragile venous network.”
The double-blind, placebo-controlled study included 65 women aged 18-45 years with etonogestrel implants. Eligibility required that implants be in place for more than 90 days and less than 3 years and that participants experienced more than one bleeding episode over a 24-day time frame.
Patients received either 15 mg ulipristal (n = 32) or placebo (n = 33) daily for 7 days. From the first day of treatment until 30 days, patients self-reported bleeding events. Weekly phone questionnaires also were conducted to determine satisfaction with medication and side effects.
Ten days after starting treatment, bleeding resolved in 34% of patients treated with ulipristal versus 10% of patients given placebo (P = .03).
The ulipristal group reported a median of 5 fewer bleeding days, compared with the placebo group, over the month-long evaluation (7 vs. 12; P = .002). Treatment satisfaction rates were also better in the ulipristal group, with nearly three-quarters (72%) “very happy” with results versus about one-quarter (27%) of women who received placebo.
Consequently, more ulipristal patients desired to keep their implants, compared with placebo patients. All patients receiving ulipristal would consider ulipristal for breakthrough bleeding in the future, compared with two-thirds of patients in the placebo group.
Side effects were uncommon for both groups; the most common side effect was headache, reported in 9% in the ulipristal group and 19% in the placebo group.
“Increased satisfaction with the etonogestrel implant may lead to a decrease in discontinuation rates and potentially a decrease in unintended pregnancy rates in this population,” the researchers wrote.
Study funding was provided by the Society of Family Planning Research Fund, the Washington University Institute of Clinical and Translational Sciences, and the National Center for Advancing Translational Sciences. The authors reported financial disclosures related to Bayer and Merck.
SOURCE: Zigler RE et al. Obstet Gynecol. 2018;132:888-94.
The recent trial by Zigler et al. showed that ulipristal acetate may reduce bleeding days in contraceptive implant users, but larger studies are needed, and concerns about logistics, dose, and toxicity must be addressed before clinical roll out, according to Eve Espey, MD.
The FDA halted the present trial after another ulipristal study overseas detected liver toxicity. The overseas study (for uterine leiomyoma) involved daily administration of ulipristal (5 mg) for 3 months, which is significantly longer than the present study for breakthrough bleeding. The European Medicines Agency has since determined that women with liver issues should not receive ulipristal and that others should have close liver monitoring before, during, and after ulipristal therapy.
Despite the above concerns, ulipristal still holds promise for a common clinical problem.
“This study contributes to the literature on management of bothersome bleeding with the contraceptive implant,” Dr. Espey said. “It is an important area because bothersome bleeding leads both to dissatisfaction and method discontinuation. As a recent Cochrane review pointed out, although several different medications have been used, studies are small and not yet conclusive. Despite these caveats, the findings were promising, similar to findings of prior work with a similar compound, mifepristone. Future directions would include clinical trials utilizing ulipristal acetate in a larger population powered for discontinuation.”
Dr. Espey is a professor in and chair of the department of obstetrics and gynecology and the family planning fellowship director at the University of New Mexico, Albuquerque. These comments are adapted from an interview. Dr. Espey said she had no relevant financial disclosures.
The recent trial by Zigler et al. showed that ulipristal acetate may reduce bleeding days in contraceptive implant users, but larger studies are needed, and concerns about logistics, dose, and toxicity must be addressed before clinical roll out, according to Eve Espey, MD.
The FDA halted the present trial after another ulipristal study overseas detected liver toxicity. The overseas study (for uterine leiomyoma) involved daily administration of ulipristal (5 mg) for 3 months, which is significantly longer than the present study for breakthrough bleeding. The European Medicines Agency has since determined that women with liver issues should not receive ulipristal and that others should have close liver monitoring before, during, and after ulipristal therapy.
Despite the above concerns, ulipristal still holds promise for a common clinical problem.
“This study contributes to the literature on management of bothersome bleeding with the contraceptive implant,” Dr. Espey said. “It is an important area because bothersome bleeding leads both to dissatisfaction and method discontinuation. As a recent Cochrane review pointed out, although several different medications have been used, studies are small and not yet conclusive. Despite these caveats, the findings were promising, similar to findings of prior work with a similar compound, mifepristone. Future directions would include clinical trials utilizing ulipristal acetate in a larger population powered for discontinuation.”
Dr. Espey is a professor in and chair of the department of obstetrics and gynecology and the family planning fellowship director at the University of New Mexico, Albuquerque. These comments are adapted from an interview. Dr. Espey said she had no relevant financial disclosures.
The recent trial by Zigler et al. showed that ulipristal acetate may reduce bleeding days in contraceptive implant users, but larger studies are needed, and concerns about logistics, dose, and toxicity must be addressed before clinical roll out, according to Eve Espey, MD.
The FDA halted the present trial after another ulipristal study overseas detected liver toxicity. The overseas study (for uterine leiomyoma) involved daily administration of ulipristal (5 mg) for 3 months, which is significantly longer than the present study for breakthrough bleeding. The European Medicines Agency has since determined that women with liver issues should not receive ulipristal and that others should have close liver monitoring before, during, and after ulipristal therapy.
Despite the above concerns, ulipristal still holds promise for a common clinical problem.
“This study contributes to the literature on management of bothersome bleeding with the contraceptive implant,” Dr. Espey said. “It is an important area because bothersome bleeding leads both to dissatisfaction and method discontinuation. As a recent Cochrane review pointed out, although several different medications have been used, studies are small and not yet conclusive. Despite these caveats, the findings were promising, similar to findings of prior work with a similar compound, mifepristone. Future directions would include clinical trials utilizing ulipristal acetate in a larger population powered for discontinuation.”
Dr. Espey is a professor in and chair of the department of obstetrics and gynecology and the family planning fellowship director at the University of New Mexico, Albuquerque. These comments are adapted from an interview. Dr. Espey said she had no relevant financial disclosures.
Ulipristal acetate reduces breakthrough bleeding in women with etonogestrel implants, according to new findings.
After 30 days, patients treated with ulipristal were more satisfied with their bleeding profiles than were those given placebo, reported Rachel E. Zigler, MD, of the department of obstetrics and gynecology at Washington University in St. Louis and her colleagues.
About half of women experience unscheduled bleeding within the first 6 months of etonogestrel implantation, causing many to discontinue treatment. The etiology of this phenomenon is poorly understood.
“One leading theory is that sustained exposure to a progestin can lead to endometrial angiogenesis disruption, resulting in the development of a dense venous network that is fragile and prone to bleeding,” the researchers wrote in Obstetrics & Gynecology.
Ulipristal acetate is a selective progesterone receptor modulator approved for emergency contraception in the United States. Outside the United States, it is used to treat abnormal uterine bleeding in cases of uterine leiomyoma. Ulipristal acts directly upon myometrial and endometrial tissue and “may also displace local progestin within the uterus to counteract bleeding secondary to … a dense, fragile venous network.”
The double-blind, placebo-controlled study included 65 women aged 18-45 years with etonogestrel implants. Eligibility required that implants be in place for more than 90 days and less than 3 years and that participants experienced more than one bleeding episode over a 24-day time frame.
Patients received either 15 mg ulipristal (n = 32) or placebo (n = 33) daily for 7 days. From the first day of treatment until 30 days, patients self-reported bleeding events. Weekly phone questionnaires also were conducted to determine satisfaction with medication and side effects.
Ten days after starting treatment, bleeding resolved in 34% of patients treated with ulipristal versus 10% of patients given placebo (P = .03).
The ulipristal group reported a median of 5 fewer bleeding days, compared with the placebo group, over the month-long evaluation (7 vs. 12; P = .002). Treatment satisfaction rates were also better in the ulipristal group, with nearly three-quarters (72%) “very happy” with results versus about one-quarter (27%) of women who received placebo.
Consequently, more ulipristal patients desired to keep their implants, compared with placebo patients. All patients receiving ulipristal would consider ulipristal for breakthrough bleeding in the future, compared with two-thirds of patients in the placebo group.
Side effects were uncommon for both groups; the most common side effect was headache, reported in 9% in the ulipristal group and 19% in the placebo group.
“Increased satisfaction with the etonogestrel implant may lead to a decrease in discontinuation rates and potentially a decrease in unintended pregnancy rates in this population,” the researchers wrote.
Study funding was provided by the Society of Family Planning Research Fund, the Washington University Institute of Clinical and Translational Sciences, and the National Center for Advancing Translational Sciences. The authors reported financial disclosures related to Bayer and Merck.
SOURCE: Zigler RE et al. Obstet Gynecol. 2018;132:888-94.
Ulipristal acetate reduces breakthrough bleeding in women with etonogestrel implants, according to new findings.
After 30 days, patients treated with ulipristal were more satisfied with their bleeding profiles than were those given placebo, reported Rachel E. Zigler, MD, of the department of obstetrics and gynecology at Washington University in St. Louis and her colleagues.
About half of women experience unscheduled bleeding within the first 6 months of etonogestrel implantation, causing many to discontinue treatment. The etiology of this phenomenon is poorly understood.
“One leading theory is that sustained exposure to a progestin can lead to endometrial angiogenesis disruption, resulting in the development of a dense venous network that is fragile and prone to bleeding,” the researchers wrote in Obstetrics & Gynecology.
Ulipristal acetate is a selective progesterone receptor modulator approved for emergency contraception in the United States. Outside the United States, it is used to treat abnormal uterine bleeding in cases of uterine leiomyoma. Ulipristal acts directly upon myometrial and endometrial tissue and “may also displace local progestin within the uterus to counteract bleeding secondary to … a dense, fragile venous network.”
The double-blind, placebo-controlled study included 65 women aged 18-45 years with etonogestrel implants. Eligibility required that implants be in place for more than 90 days and less than 3 years and that participants experienced more than one bleeding episode over a 24-day time frame.
Patients received either 15 mg ulipristal (n = 32) or placebo (n = 33) daily for 7 days. From the first day of treatment until 30 days, patients self-reported bleeding events. Weekly phone questionnaires also were conducted to determine satisfaction with medication and side effects.
Ten days after starting treatment, bleeding resolved in 34% of patients treated with ulipristal versus 10% of patients given placebo (P = .03).
The ulipristal group reported a median of 5 fewer bleeding days, compared with the placebo group, over the month-long evaluation (7 vs. 12; P = .002). Treatment satisfaction rates were also better in the ulipristal group, with nearly three-quarters (72%) “very happy” with results versus about one-quarter (27%) of women who received placebo.
Consequently, more ulipristal patients desired to keep their implants, compared with placebo patients. All patients receiving ulipristal would consider ulipristal for breakthrough bleeding in the future, compared with two-thirds of patients in the placebo group.
Side effects were uncommon for both groups; the most common side effect was headache, reported in 9% in the ulipristal group and 19% in the placebo group.
“Increased satisfaction with the etonogestrel implant may lead to a decrease in discontinuation rates and potentially a decrease in unintended pregnancy rates in this population,” the researchers wrote.
Study funding was provided by the Society of Family Planning Research Fund, the Washington University Institute of Clinical and Translational Sciences, and the National Center for Advancing Translational Sciences. The authors reported financial disclosures related to Bayer and Merck.
SOURCE: Zigler RE et al. Obstet Gynecol. 2018;132:888-94.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Treatment with ulipristal was associated with 5 fewer bleeding days per month, compared with placebo (P = .002).
Study details: The double-blind, placebo-controlled trial involved 65 women with etonogestrel implants who reported more than one bleeding episode in a 24-day time frame.
Disclosures: The study was funded by the Society of Family Planning Research Fund, the Washington University Institute of Clinical and Translational Sciences, and the National Center for Advancing Translational Sciences (NCATS). The authors reported financial disclosures related to Bayer and Merck.
Source: Zigler RE et al. Obstet Gynecol. 2018;132:888-94.
Pregnancy registries are a valuable resource
Pregnancy registries are valuable sources of information. For many drugs, they are the primary source of the human pregnancy experience. However, although most of the registries use the word “pregnancy,” it is important to note that many also enroll women who took the target drug shortly before conception.
The strengths of these registries are their prospective nature (enrolled before the outcome is known) and enrollment over a wide geographical area. Typically, two types of pregnancy outcomes are obtained: those with birth defects and those without known birth defects (classified as live births, fetal deaths, and spontaneous abortions). Registries can identify early signals of teratogenicity, but they have several limitations: selection bias that results from voluntary reporting; target populations that are not representative; lost-to-follow-up pregnancies that may have had different outcomes than those with documented outcomes; elective terminations and fetal deaths without birth defects and spontaneous abortions, all of which may lack details; the lack of control groups (with some exceptions); and the publication of results that may be delayed or not be in a peer-reviewed journal. Because the total number of exposed pregnancies is unknown, the data cannot be used to calculate prevalences, but they can be used to estimate the proportion of birth defects. Some registries also collect data on retrospective reports (reported after outcome is known). Such reports are less representative of the target population because they can be biased toward the reporting of more unusual and severe outcomes. But they may be helpful in detecting unusual patterns of birth defects.
For the following drugs, web addresses can be obtained from the Food and Drug Administration website, List of Pregnancy Exposure Registries.
MotherToBaby
A large registry, the MotherToBaby Organization of Teratology Information Specialists (OTIS) (877-311-8972), involves patients in several different categories and the effects of the drugs on the embryo-fetus: autoimmune diseases (ankylosing spondylitis, rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, psoriasis, Crohn’s disease, and multiple sclerosis); asthma at less than 20 weeks’ gestation; vaccines; and heterozygous or homozygous familial hypercholesterolemia.
For the autoimmune diseases, the drugs and trade names are abatacept (Orencia), adalimumab (Humira), certolizumab pegol (Cimzia), etanercept (Enbrel), infliximab (Remicade), leflunomide (Arava), otezla (Apremilast), teriflunomide (Aubagio), tocilizumab (Actemra), tofacitinib (Xeljanz), and ustekinumab (Stelara).
For the asthma group, the drug being investigated is mepolizumab (Nucala).
Two vaccines – for tetanus, diphtheria, and pertussis (Tdap) and meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menveo) – are being studied.
The last category is heterozygous or homozygous familial hypercholesterolemia. The two agents in this category are alirocumab (Praluent) and evolocumab (Repatha).
Other registries
Breast cancer
The Mother Pregnancy Registry, INC Research (800-690-6720), is enrolling breast cancer patients who have been treated during pregnancy with ado-trastuzumab emtansine (Kadcyla), pertuzumab (Perjeta), or trastuzumab (Herceptin).
Epilepsy
The Antiepileptic Drug Pregnancy registry (888-233-2334) is studying eslicarbazepine (Aptiom) and pregabalin (Lyrica).
Fabry disease
The Fabry Registry, Genzyme Corp (617-591-5500) is studying the use in pregnancy of agalsidase beta (Fabrazyme) for Fabry disease.
Fibromyalgia
The Savella Pregnancy Registry (877-643-3010) is looking for patients with fibromyalgia who are being treated with milnacipran (Savella).
Hepatitis B
The Ribavirin Pregnancy Registry, INC Research (800-593-2214) is looking for subjects with hepatitis C who have been treated with ribavirin (Copegus).
Hypercholesterolemia
Lomitapide (Juxtapid) is being studied by the Global Lomitapide Pregnancy Exposure Registry managed by Aegerion (877-902-4099). The drug is used for homozygous familial hypercholesterolemia.
Mucopolysaccharidosis
The Mucopolysaccharidosis I (MPS I) registry, Genzyme (617-591-5500) is studying the use of laronidase (Aldurazyme) for Hurler syndrome, Scheie syndrome, and Hurler-Scheie syndrome.
The use of galsulfase (Naglazyme) for Maroteaux-Lamy syndrome during pregnancy is under study by the Mucopolysaccharidosis VI (MPS VI), clinical surveillance program (BioMarin Pharmaceutical) (415-506-6849 or 415-506-6703).
Multiple sclerosis
Novartis is conducting the Gilenya Pregnancy Registry (877-598-7237) for patients with multiple sclerosis who are taking fingolimod (Gilenya).
Alemtuzumab (Lemtrada), also indicated for multiple sclerosis, is the target agent for the LEMTRADA Pregnancy Exposure Registry (866-758-2990).
Narcolepsy and other sleep disorders
Armodafinil (Nuvigil), used for excessive sleepiness associated with narcolepsy and other sleep disorders, is being studied in the Nuvigil Pregnancy Registry (866-404-4106). A second drug with the same indication and telephone number, modafinil (Provigil), is in the Provigil Pregnancy Registry.
Osteoporosis
Amgen’s Pregnancy Surveillance Program (800-772-6436) is enrolling pregnant subjects with osteoporosis who are being treated with denosumab (Prolia).
Others
Two Merck pregnancy registries (800-986-8999) cover the following conditions: type 2 diabetes sitagliptin+metformin (Janumet) or sitagliptin (Januvia); and migraine headaches rizatriptan (Maxalt).
GlaxoSmithKline is conducting two registries: the Belimumab Pregnancy Registry for patients with systemic lupus erythematosus treated with belimumab (Benlysta) (877-681-6296); and Promacta Pregnancy Registry for women treated for thrombocytopenia with eltrombopag (Promacta) (888-825-5249).
Psychiatric Drugs
The National Pregnancy Registry for Atypical Antipsychotics (866-961-2388) is studying 10 drugs: aripiprazole (Abilify), asenapine (Saphris), clozapine (Clozaril), iloperidone (Fanapt), lurasidone (Latuda), olanzapine (Zyprexa), paliperidone (Invega), quetiapine (Seroquel), risperidone (Risperdal), and ziprasidone (Geodon).
The National Pregnancy Registry for Antidepressants (844-405-6185) is studying amitriptyline (Elavil), amoxapine (Asendin), bupropion (Forfivo XL and Wellbutrin), citalopram (Celexa), clomipramine (Anafranil), desipramine (Norpramin), desvenlafaxine (Prisiq), doxepin (Sinequan), escitalopram (Lexapro), fluvoxamine (Luvox), fluoxetine (Prozac), imipramine (Tofranil), isocarboxazid (Marplan), levomilnacipran (Fetzima), maprotiline (Ludiomil), mirtazapine (Remeron), nefazodone (Serzone), nortriptyline (Pamelor), paroxetine (Paxil), phenelzine (Nardill), protriptyline (Vivactil), selegiline (Emsam), sertraline (Zoloft), tranylcypromine (Pamate), trazodone (Desyrel), trimipramine (Surmontil), venlafaxine (Effexor), and vilazodone (Viibryd).
The National Pregnancy Registry of Psychostimulants (866-961-2388) is studying amphetamine (Adderall), dextroamphetamine (Dexedrine and Focalin), lisdexamfetamine (Vyvanse), methylphenidate (Concerta, Daytrana, Desoxyn, Ritalin), and modafinil (Provigil).
The antidepressant duloxetine (Cymbalta) is being studied by the Cymbalta Pregnancy Registry (866-814-6975).
Transplant patients
Renal transplant patients exposed to mycophenolate (CellCept) can be enrolled in the Transplantation Pregnancy Registry International (877-955-6877) or the Mycophenolate Pregnancy Registry (800-617-8191). The Transplantation Pregnancy Registry International also is enrolling renal transplant patients exposed to belatacept (Nulojix).
Vaccines
A quadrivalent influenza vaccine (Afluria) is being studied by the Seqirus Influenza Vaccine Pregnancy Registry (855-358-8972). A second vaccine for meningococcal disease meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menactra) is under study by the Menactra Vaccine Pregnancy Registry (800-822-2463). The Bexsero Pregnancy Registry (877-413-4759) is open to patients who have received the meningococcal group B vaccine (Bexsero). The Hepatitis B Vaccine [Recombinant] Adjuvanted Pregnancy Registry, also listed as HEPLISAV-B, is enrolling patients who have received that vaccine (844-443-7734); it is supported by the Dynavax Technologies Corporation.
Because the strength of a registry is based on numbers, health care professionals are encouraged to enroll potential subjects or have their patients call to enroll themselves.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Pregnancy registries are valuable sources of information. For many drugs, they are the primary source of the human pregnancy experience. However, although most of the registries use the word “pregnancy,” it is important to note that many also enroll women who took the target drug shortly before conception.
The strengths of these registries are their prospective nature (enrolled before the outcome is known) and enrollment over a wide geographical area. Typically, two types of pregnancy outcomes are obtained: those with birth defects and those without known birth defects (classified as live births, fetal deaths, and spontaneous abortions). Registries can identify early signals of teratogenicity, but they have several limitations: selection bias that results from voluntary reporting; target populations that are not representative; lost-to-follow-up pregnancies that may have had different outcomes than those with documented outcomes; elective terminations and fetal deaths without birth defects and spontaneous abortions, all of which may lack details; the lack of control groups (with some exceptions); and the publication of results that may be delayed or not be in a peer-reviewed journal. Because the total number of exposed pregnancies is unknown, the data cannot be used to calculate prevalences, but they can be used to estimate the proportion of birth defects. Some registries also collect data on retrospective reports (reported after outcome is known). Such reports are less representative of the target population because they can be biased toward the reporting of more unusual and severe outcomes. But they may be helpful in detecting unusual patterns of birth defects.
For the following drugs, web addresses can be obtained from the Food and Drug Administration website, List of Pregnancy Exposure Registries.
MotherToBaby
A large registry, the MotherToBaby Organization of Teratology Information Specialists (OTIS) (877-311-8972), involves patients in several different categories and the effects of the drugs on the embryo-fetus: autoimmune diseases (ankylosing spondylitis, rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, psoriasis, Crohn’s disease, and multiple sclerosis); asthma at less than 20 weeks’ gestation; vaccines; and heterozygous or homozygous familial hypercholesterolemia.
For the autoimmune diseases, the drugs and trade names are abatacept (Orencia), adalimumab (Humira), certolizumab pegol (Cimzia), etanercept (Enbrel), infliximab (Remicade), leflunomide (Arava), otezla (Apremilast), teriflunomide (Aubagio), tocilizumab (Actemra), tofacitinib (Xeljanz), and ustekinumab (Stelara).
For the asthma group, the drug being investigated is mepolizumab (Nucala).
Two vaccines – for tetanus, diphtheria, and pertussis (Tdap) and meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menveo) – are being studied.
The last category is heterozygous or homozygous familial hypercholesterolemia. The two agents in this category are alirocumab (Praluent) and evolocumab (Repatha).
Other registries
Breast cancer
The Mother Pregnancy Registry, INC Research (800-690-6720), is enrolling breast cancer patients who have been treated during pregnancy with ado-trastuzumab emtansine (Kadcyla), pertuzumab (Perjeta), or trastuzumab (Herceptin).
Epilepsy
The Antiepileptic Drug Pregnancy registry (888-233-2334) is studying eslicarbazepine (Aptiom) and pregabalin (Lyrica).
Fabry disease
The Fabry Registry, Genzyme Corp (617-591-5500) is studying the use in pregnancy of agalsidase beta (Fabrazyme) for Fabry disease.
Fibromyalgia
The Savella Pregnancy Registry (877-643-3010) is looking for patients with fibromyalgia who are being treated with milnacipran (Savella).
Hepatitis B
The Ribavirin Pregnancy Registry, INC Research (800-593-2214) is looking for subjects with hepatitis C who have been treated with ribavirin (Copegus).
Hypercholesterolemia
Lomitapide (Juxtapid) is being studied by the Global Lomitapide Pregnancy Exposure Registry managed by Aegerion (877-902-4099). The drug is used for homozygous familial hypercholesterolemia.
Mucopolysaccharidosis
The Mucopolysaccharidosis I (MPS I) registry, Genzyme (617-591-5500) is studying the use of laronidase (Aldurazyme) for Hurler syndrome, Scheie syndrome, and Hurler-Scheie syndrome.
The use of galsulfase (Naglazyme) for Maroteaux-Lamy syndrome during pregnancy is under study by the Mucopolysaccharidosis VI (MPS VI), clinical surveillance program (BioMarin Pharmaceutical) (415-506-6849 or 415-506-6703).
Multiple sclerosis
Novartis is conducting the Gilenya Pregnancy Registry (877-598-7237) for patients with multiple sclerosis who are taking fingolimod (Gilenya).
Alemtuzumab (Lemtrada), also indicated for multiple sclerosis, is the target agent for the LEMTRADA Pregnancy Exposure Registry (866-758-2990).
Narcolepsy and other sleep disorders
Armodafinil (Nuvigil), used for excessive sleepiness associated with narcolepsy and other sleep disorders, is being studied in the Nuvigil Pregnancy Registry (866-404-4106). A second drug with the same indication and telephone number, modafinil (Provigil), is in the Provigil Pregnancy Registry.
Osteoporosis
Amgen’s Pregnancy Surveillance Program (800-772-6436) is enrolling pregnant subjects with osteoporosis who are being treated with denosumab (Prolia).
Others
Two Merck pregnancy registries (800-986-8999) cover the following conditions: type 2 diabetes sitagliptin+metformin (Janumet) or sitagliptin (Januvia); and migraine headaches rizatriptan (Maxalt).
GlaxoSmithKline is conducting two registries: the Belimumab Pregnancy Registry for patients with systemic lupus erythematosus treated with belimumab (Benlysta) (877-681-6296); and Promacta Pregnancy Registry for women treated for thrombocytopenia with eltrombopag (Promacta) (888-825-5249).
Psychiatric Drugs
The National Pregnancy Registry for Atypical Antipsychotics (866-961-2388) is studying 10 drugs: aripiprazole (Abilify), asenapine (Saphris), clozapine (Clozaril), iloperidone (Fanapt), lurasidone (Latuda), olanzapine (Zyprexa), paliperidone (Invega), quetiapine (Seroquel), risperidone (Risperdal), and ziprasidone (Geodon).
The National Pregnancy Registry for Antidepressants (844-405-6185) is studying amitriptyline (Elavil), amoxapine (Asendin), bupropion (Forfivo XL and Wellbutrin), citalopram (Celexa), clomipramine (Anafranil), desipramine (Norpramin), desvenlafaxine (Prisiq), doxepin (Sinequan), escitalopram (Lexapro), fluvoxamine (Luvox), fluoxetine (Prozac), imipramine (Tofranil), isocarboxazid (Marplan), levomilnacipran (Fetzima), maprotiline (Ludiomil), mirtazapine (Remeron), nefazodone (Serzone), nortriptyline (Pamelor), paroxetine (Paxil), phenelzine (Nardill), protriptyline (Vivactil), selegiline (Emsam), sertraline (Zoloft), tranylcypromine (Pamate), trazodone (Desyrel), trimipramine (Surmontil), venlafaxine (Effexor), and vilazodone (Viibryd).
The National Pregnancy Registry of Psychostimulants (866-961-2388) is studying amphetamine (Adderall), dextroamphetamine (Dexedrine and Focalin), lisdexamfetamine (Vyvanse), methylphenidate (Concerta, Daytrana, Desoxyn, Ritalin), and modafinil (Provigil).
The antidepressant duloxetine (Cymbalta) is being studied by the Cymbalta Pregnancy Registry (866-814-6975).
Transplant patients
Renal transplant patients exposed to mycophenolate (CellCept) can be enrolled in the Transplantation Pregnancy Registry International (877-955-6877) or the Mycophenolate Pregnancy Registry (800-617-8191). The Transplantation Pregnancy Registry International also is enrolling renal transplant patients exposed to belatacept (Nulojix).
Vaccines
A quadrivalent influenza vaccine (Afluria) is being studied by the Seqirus Influenza Vaccine Pregnancy Registry (855-358-8972). A second vaccine for meningococcal disease meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menactra) is under study by the Menactra Vaccine Pregnancy Registry (800-822-2463). The Bexsero Pregnancy Registry (877-413-4759) is open to patients who have received the meningococcal group B vaccine (Bexsero). The Hepatitis B Vaccine [Recombinant] Adjuvanted Pregnancy Registry, also listed as HEPLISAV-B, is enrolling patients who have received that vaccine (844-443-7734); it is supported by the Dynavax Technologies Corporation.
Because the strength of a registry is based on numbers, health care professionals are encouraged to enroll potential subjects or have their patients call to enroll themselves.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Pregnancy registries are valuable sources of information. For many drugs, they are the primary source of the human pregnancy experience. However, although most of the registries use the word “pregnancy,” it is important to note that many also enroll women who took the target drug shortly before conception.
The strengths of these registries are their prospective nature (enrolled before the outcome is known) and enrollment over a wide geographical area. Typically, two types of pregnancy outcomes are obtained: those with birth defects and those without known birth defects (classified as live births, fetal deaths, and spontaneous abortions). Registries can identify early signals of teratogenicity, but they have several limitations: selection bias that results from voluntary reporting; target populations that are not representative; lost-to-follow-up pregnancies that may have had different outcomes than those with documented outcomes; elective terminations and fetal deaths without birth defects and spontaneous abortions, all of which may lack details; the lack of control groups (with some exceptions); and the publication of results that may be delayed or not be in a peer-reviewed journal. Because the total number of exposed pregnancies is unknown, the data cannot be used to calculate prevalences, but they can be used to estimate the proportion of birth defects. Some registries also collect data on retrospective reports (reported after outcome is known). Such reports are less representative of the target population because they can be biased toward the reporting of more unusual and severe outcomes. But they may be helpful in detecting unusual patterns of birth defects.
For the following drugs, web addresses can be obtained from the Food and Drug Administration website, List of Pregnancy Exposure Registries.
MotherToBaby
A large registry, the MotherToBaby Organization of Teratology Information Specialists (OTIS) (877-311-8972), involves patients in several different categories and the effects of the drugs on the embryo-fetus: autoimmune diseases (ankylosing spondylitis, rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, psoriasis, Crohn’s disease, and multiple sclerosis); asthma at less than 20 weeks’ gestation; vaccines; and heterozygous or homozygous familial hypercholesterolemia.
For the autoimmune diseases, the drugs and trade names are abatacept (Orencia), adalimumab (Humira), certolizumab pegol (Cimzia), etanercept (Enbrel), infliximab (Remicade), leflunomide (Arava), otezla (Apremilast), teriflunomide (Aubagio), tocilizumab (Actemra), tofacitinib (Xeljanz), and ustekinumab (Stelara).
For the asthma group, the drug being investigated is mepolizumab (Nucala).
Two vaccines – for tetanus, diphtheria, and pertussis (Tdap) and meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menveo) – are being studied.
The last category is heterozygous or homozygous familial hypercholesterolemia. The two agents in this category are alirocumab (Praluent) and evolocumab (Repatha).
Other registries
Breast cancer
The Mother Pregnancy Registry, INC Research (800-690-6720), is enrolling breast cancer patients who have been treated during pregnancy with ado-trastuzumab emtansine (Kadcyla), pertuzumab (Perjeta), or trastuzumab (Herceptin).
Epilepsy
The Antiepileptic Drug Pregnancy registry (888-233-2334) is studying eslicarbazepine (Aptiom) and pregabalin (Lyrica).
Fabry disease
The Fabry Registry, Genzyme Corp (617-591-5500) is studying the use in pregnancy of agalsidase beta (Fabrazyme) for Fabry disease.
Fibromyalgia
The Savella Pregnancy Registry (877-643-3010) is looking for patients with fibromyalgia who are being treated with milnacipran (Savella).
Hepatitis B
The Ribavirin Pregnancy Registry, INC Research (800-593-2214) is looking for subjects with hepatitis C who have been treated with ribavirin (Copegus).
Hypercholesterolemia
Lomitapide (Juxtapid) is being studied by the Global Lomitapide Pregnancy Exposure Registry managed by Aegerion (877-902-4099). The drug is used for homozygous familial hypercholesterolemia.
Mucopolysaccharidosis
The Mucopolysaccharidosis I (MPS I) registry, Genzyme (617-591-5500) is studying the use of laronidase (Aldurazyme) for Hurler syndrome, Scheie syndrome, and Hurler-Scheie syndrome.
The use of galsulfase (Naglazyme) for Maroteaux-Lamy syndrome during pregnancy is under study by the Mucopolysaccharidosis VI (MPS VI), clinical surveillance program (BioMarin Pharmaceutical) (415-506-6849 or 415-506-6703).
Multiple sclerosis
Novartis is conducting the Gilenya Pregnancy Registry (877-598-7237) for patients with multiple sclerosis who are taking fingolimod (Gilenya).
Alemtuzumab (Lemtrada), also indicated for multiple sclerosis, is the target agent for the LEMTRADA Pregnancy Exposure Registry (866-758-2990).
Narcolepsy and other sleep disorders
Armodafinil (Nuvigil), used for excessive sleepiness associated with narcolepsy and other sleep disorders, is being studied in the Nuvigil Pregnancy Registry (866-404-4106). A second drug with the same indication and telephone number, modafinil (Provigil), is in the Provigil Pregnancy Registry.
Osteoporosis
Amgen’s Pregnancy Surveillance Program (800-772-6436) is enrolling pregnant subjects with osteoporosis who are being treated with denosumab (Prolia).
Others
Two Merck pregnancy registries (800-986-8999) cover the following conditions: type 2 diabetes sitagliptin+metformin (Janumet) or sitagliptin (Januvia); and migraine headaches rizatriptan (Maxalt).
GlaxoSmithKline is conducting two registries: the Belimumab Pregnancy Registry for patients with systemic lupus erythematosus treated with belimumab (Benlysta) (877-681-6296); and Promacta Pregnancy Registry for women treated for thrombocytopenia with eltrombopag (Promacta) (888-825-5249).
Psychiatric Drugs
The National Pregnancy Registry for Atypical Antipsychotics (866-961-2388) is studying 10 drugs: aripiprazole (Abilify), asenapine (Saphris), clozapine (Clozaril), iloperidone (Fanapt), lurasidone (Latuda), olanzapine (Zyprexa), paliperidone (Invega), quetiapine (Seroquel), risperidone (Risperdal), and ziprasidone (Geodon).
The National Pregnancy Registry for Antidepressants (844-405-6185) is studying amitriptyline (Elavil), amoxapine (Asendin), bupropion (Forfivo XL and Wellbutrin), citalopram (Celexa), clomipramine (Anafranil), desipramine (Norpramin), desvenlafaxine (Prisiq), doxepin (Sinequan), escitalopram (Lexapro), fluvoxamine (Luvox), fluoxetine (Prozac), imipramine (Tofranil), isocarboxazid (Marplan), levomilnacipran (Fetzima), maprotiline (Ludiomil), mirtazapine (Remeron), nefazodone (Serzone), nortriptyline (Pamelor), paroxetine (Paxil), phenelzine (Nardill), protriptyline (Vivactil), selegiline (Emsam), sertraline (Zoloft), tranylcypromine (Pamate), trazodone (Desyrel), trimipramine (Surmontil), venlafaxine (Effexor), and vilazodone (Viibryd).
The National Pregnancy Registry of Psychostimulants (866-961-2388) is studying amphetamine (Adderall), dextroamphetamine (Dexedrine and Focalin), lisdexamfetamine (Vyvanse), methylphenidate (Concerta, Daytrana, Desoxyn, Ritalin), and modafinil (Provigil).
The antidepressant duloxetine (Cymbalta) is being studied by the Cymbalta Pregnancy Registry (866-814-6975).
Transplant patients
Renal transplant patients exposed to mycophenolate (CellCept) can be enrolled in the Transplantation Pregnancy Registry International (877-955-6877) or the Mycophenolate Pregnancy Registry (800-617-8191). The Transplantation Pregnancy Registry International also is enrolling renal transplant patients exposed to belatacept (Nulojix).
Vaccines
A quadrivalent influenza vaccine (Afluria) is being studied by the Seqirus Influenza Vaccine Pregnancy Registry (855-358-8972). A second vaccine for meningococcal disease meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y and W-135 (Menactra) is under study by the Menactra Vaccine Pregnancy Registry (800-822-2463). The Bexsero Pregnancy Registry (877-413-4759) is open to patients who have received the meningococcal group B vaccine (Bexsero). The Hepatitis B Vaccine [Recombinant] Adjuvanted Pregnancy Registry, also listed as HEPLISAV-B, is enrolling patients who have received that vaccine (844-443-7734); it is supported by the Dynavax Technologies Corporation.
Because the strength of a registry is based on numbers, health care professionals are encouraged to enroll potential subjects or have their patients call to enroll themselves.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Clearance rates for some antiepileptic drugs rise during pregnancy
Certain antiepileptic drugs show significant increases in clearance rates during pregnancy, which may be associated with increased seizure rates, research suggests.
Paula E. Voinescu, MD, PhD, of Brigham and Women’s Hospital, Boston, and her coauthors conducted a prospective, observational study of 44 pregnancies in 40 women with epilepsy who were treated with antiepileptic drugs. The women were enrolled preconception or in early pregnancy, then kept daily diaries of medication doses, adherence, and seizures, while antiepileptic drug concentrations were measured every 1-3 months.
The investigators found that levetiracetam reached a mean maximal clearance during the first trimester that was 71% higher than baseline clearance (P = .0001), and its clearance level remained high throughout pregnancy.
“This is important information for clinicians who manage women on levetiracetam as they may opt to begin TDM [therapeutic drug monitoring] as early as possible in pregnancy,” the investigators wrote. The report was published online Sept. 5 in Neurology.
The authors noted that there was significant variability between participants in clearance rates of levetiracetam, ranging from 1.42-fold to 2.02-fold baseline clearance, and they suggested that pharmacogenetic differences may play a role.
“Levetiracetam is mainly excreted unchanged by the kidneys, and the changes in clearance are consistent with the time course of increased glomerular filtration rate during pregnancy,” they wrote. “The pathophysiology of the interparticipant variability in clearance fluctuation during pregnancy and of the race influence observed for levetiracetam are difficult to explain with the known pharmacokinetic data.”
Both oxcarbazepine and topiramate also reached significantly higher mean maximal clearances during the second trimester than at baseline (63% and 39% higher, respectively), and their elevated clearance persisted into the third trimester.
However, there were no significant changes in clearance rates of total or free phenytoin or valproic acid during pregnancy.
Among the 15 women for whom researchers had complete seizure history and antiepileptic drug concentrations, 40% experienced a worsening of seizure frequency during at least one trimester.
Overall, lower individualized ratio-to-target concentrations of drug were associated with increased seizure frequency in the first and second trimester, but not in the third trimester.
While the study did not compare seizure outcomes between patients who were managed with TDM and those who were not, the authors suggested that their data supported the use of TDM during pregnancy.
“The finding of lower AED RTC [antiepileptic drug ratio to concentration] at different trimesters suggests that in outpatient clinical practice, possible changes in AED dosing varied by trimester may be clinically important for patient care.”
The study was supported by the National Institutes of Health, the American Brain Foundation, the American Epilepsy Society, the Epilepsy Foundation, and the Karger Fund. Four authors declared support, honoraria, and/or other funding from the pharmaceutical industry, and five also declared support from the study funding bodies.
SOURCE: Voinescu P et al. Neurology. 2018 Sep 5. doi: 10.1212/WNL.0000000000006240.
Certain antiepileptic drugs show significant increases in clearance rates during pregnancy, which may be associated with increased seizure rates, research suggests.
Paula E. Voinescu, MD, PhD, of Brigham and Women’s Hospital, Boston, and her coauthors conducted a prospective, observational study of 44 pregnancies in 40 women with epilepsy who were treated with antiepileptic drugs. The women were enrolled preconception or in early pregnancy, then kept daily diaries of medication doses, adherence, and seizures, while antiepileptic drug concentrations were measured every 1-3 months.
The investigators found that levetiracetam reached a mean maximal clearance during the first trimester that was 71% higher than baseline clearance (P = .0001), and its clearance level remained high throughout pregnancy.
“This is important information for clinicians who manage women on levetiracetam as they may opt to begin TDM [therapeutic drug monitoring] as early as possible in pregnancy,” the investigators wrote. The report was published online Sept. 5 in Neurology.
The authors noted that there was significant variability between participants in clearance rates of levetiracetam, ranging from 1.42-fold to 2.02-fold baseline clearance, and they suggested that pharmacogenetic differences may play a role.
“Levetiracetam is mainly excreted unchanged by the kidneys, and the changes in clearance are consistent with the time course of increased glomerular filtration rate during pregnancy,” they wrote. “The pathophysiology of the interparticipant variability in clearance fluctuation during pregnancy and of the race influence observed for levetiracetam are difficult to explain with the known pharmacokinetic data.”
Both oxcarbazepine and topiramate also reached significantly higher mean maximal clearances during the second trimester than at baseline (63% and 39% higher, respectively), and their elevated clearance persisted into the third trimester.
However, there were no significant changes in clearance rates of total or free phenytoin or valproic acid during pregnancy.
Among the 15 women for whom researchers had complete seizure history and antiepileptic drug concentrations, 40% experienced a worsening of seizure frequency during at least one trimester.
Overall, lower individualized ratio-to-target concentrations of drug were associated with increased seizure frequency in the first and second trimester, but not in the third trimester.
While the study did not compare seizure outcomes between patients who were managed with TDM and those who were not, the authors suggested that their data supported the use of TDM during pregnancy.
“The finding of lower AED RTC [antiepileptic drug ratio to concentration] at different trimesters suggests that in outpatient clinical practice, possible changes in AED dosing varied by trimester may be clinically important for patient care.”
The study was supported by the National Institutes of Health, the American Brain Foundation, the American Epilepsy Society, the Epilepsy Foundation, and the Karger Fund. Four authors declared support, honoraria, and/or other funding from the pharmaceutical industry, and five also declared support from the study funding bodies.
SOURCE: Voinescu P et al. Neurology. 2018 Sep 5. doi: 10.1212/WNL.0000000000006240.
Certain antiepileptic drugs show significant increases in clearance rates during pregnancy, which may be associated with increased seizure rates, research suggests.
Paula E. Voinescu, MD, PhD, of Brigham and Women’s Hospital, Boston, and her coauthors conducted a prospective, observational study of 44 pregnancies in 40 women with epilepsy who were treated with antiepileptic drugs. The women were enrolled preconception or in early pregnancy, then kept daily diaries of medication doses, adherence, and seizures, while antiepileptic drug concentrations were measured every 1-3 months.
The investigators found that levetiracetam reached a mean maximal clearance during the first trimester that was 71% higher than baseline clearance (P = .0001), and its clearance level remained high throughout pregnancy.
“This is important information for clinicians who manage women on levetiracetam as they may opt to begin TDM [therapeutic drug monitoring] as early as possible in pregnancy,” the investigators wrote. The report was published online Sept. 5 in Neurology.
The authors noted that there was significant variability between participants in clearance rates of levetiracetam, ranging from 1.42-fold to 2.02-fold baseline clearance, and they suggested that pharmacogenetic differences may play a role.
“Levetiracetam is mainly excreted unchanged by the kidneys, and the changes in clearance are consistent with the time course of increased glomerular filtration rate during pregnancy,” they wrote. “The pathophysiology of the interparticipant variability in clearance fluctuation during pregnancy and of the race influence observed for levetiracetam are difficult to explain with the known pharmacokinetic data.”
Both oxcarbazepine and topiramate also reached significantly higher mean maximal clearances during the second trimester than at baseline (63% and 39% higher, respectively), and their elevated clearance persisted into the third trimester.
However, there were no significant changes in clearance rates of total or free phenytoin or valproic acid during pregnancy.
Among the 15 women for whom researchers had complete seizure history and antiepileptic drug concentrations, 40% experienced a worsening of seizure frequency during at least one trimester.
Overall, lower individualized ratio-to-target concentrations of drug were associated with increased seizure frequency in the first and second trimester, but not in the third trimester.
While the study did not compare seizure outcomes between patients who were managed with TDM and those who were not, the authors suggested that their data supported the use of TDM during pregnancy.
“The finding of lower AED RTC [antiepileptic drug ratio to concentration] at different trimesters suggests that in outpatient clinical practice, possible changes in AED dosing varied by trimester may be clinically important for patient care.”
The study was supported by the National Institutes of Health, the American Brain Foundation, the American Epilepsy Society, the Epilepsy Foundation, and the Karger Fund. Four authors declared support, honoraria, and/or other funding from the pharmaceutical industry, and five also declared support from the study funding bodies.
SOURCE: Voinescu P et al. Neurology. 2018 Sep 5. doi: 10.1212/WNL.0000000000006240.
FROM NEUROLOGY
Key clinical point: Some antiepileptic drugs show higher clearance rates during pregnancy, which could increase seizure risk.
Major finding: The mean maximal clearance rate of levetiracetam in the first trimester is 71% higher than baseline.
Study details: Prospective observational study in 40 women with 44 pregnancies.
Disclosures: The study was supported by the National Institutes of Health, the American Brain Foundation, the American Epilepsy Society, the Epilepsy Foundation, and the Karger Fund. Four authors declared support, honoraria, and/or other funding from the pharmaceutical industry, and five also declared support from the study funding bodies.
Source: Voinescu P et al. Neurology. 2018 Sep 5. doi: 10.1212/WNL.0000000000006240
Age, risk factors should guide chlamydia, gonorrhea screening of HIV-infected women
WASHINGTON – Among HIV-infected women, those aged 18-29 years had the highest rates of gonorrhea and chlamydia. These results suggest that screening for these sexually transmitted infections (STIs) should be based on age and risk in HIV-infected women, said Jodie Dionne-Odom, MD, of the University of Alabama at Birmingham.
Annual screening for gonorrhea and chlamydia is recommended for all sexually active adults with HIV, but prevalence varies by gender, age, and risk behavior, Dr. Dionne-Odom said at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Dr. Odom and her colleagues calculated annual testing and positivity rates during 2007-2016 for chlamydia and gonorrhea among women engaged in HIV care in eight U.S. cities as part of the Centers for AIDS Research (CFAR) Clinical Networks and Integrated Clinical Services (CNICS) longitudinal cohort.
They assessed demographic data based on the most recent year the patient was in care and used validated surveys (AUDIT-C and ASSIST) to assess risk behaviors in the past 3-6 months. They collected information from 5,084 women and 158,745 HIV primary care and women’s health visits.
The median patient age was 47 years; 62.1% of the patients were black; 70% had CD4 counts greater than 350; and 73.6% had HIV viral loads of less than 500 copies/mL. In terms of reported risk, 60.6% of the women were sexually active, (85.5% of whom reported monogamy); 13.1% had problem alcohol use, and 11.6% had active drug use.
Sampling for gonorrhea and chlamydia were mostly from urogenital sites (86.6%), 6.6% were extragenital, and 6.8% were “other.” Nearly all (98.5%) of 23,492 chlamydia tests and 95.7% of 23,324 gonorrhea tests used nucleic acid amplification, Dr. Dionne-Odom said.
During the most recent year in care, 42.7% of women were tested for gonorrhea and chlamydia, and 3.4% were positive, with the annual positivity rates over the study ranging from 1.5% to 3.2% for chlamydia and 0.9% to 1.5% for gonorrhea. However, Dr. Dionne-Odom and her colleagues found that the prevalence of STIs was inversely related to patient age, with gonorrhea and chlamydia positivity in 2016 being 16% for chlamydia and 3.9% for gonorrhea among women aged 18-24 years, compared with 1.1% and 0.7%, respectively, for women older than 50 years.
“As with national data on women, HIV-infected women aged 18-29 years had the highest rates of gonorrhea and chlamydia. Our results show that targeted screening for chlamydia and gonorrhea in women with HIV based on age and risk is warranted,” Dr. Dionne-Odom concluded.
Dr. Dionne-Odom reported that she had no relevant disclosures.
WASHINGTON – Among HIV-infected women, those aged 18-29 years had the highest rates of gonorrhea and chlamydia. These results suggest that screening for these sexually transmitted infections (STIs) should be based on age and risk in HIV-infected women, said Jodie Dionne-Odom, MD, of the University of Alabama at Birmingham.
Annual screening for gonorrhea and chlamydia is recommended for all sexually active adults with HIV, but prevalence varies by gender, age, and risk behavior, Dr. Dionne-Odom said at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Dr. Odom and her colleagues calculated annual testing and positivity rates during 2007-2016 for chlamydia and gonorrhea among women engaged in HIV care in eight U.S. cities as part of the Centers for AIDS Research (CFAR) Clinical Networks and Integrated Clinical Services (CNICS) longitudinal cohort.
They assessed demographic data based on the most recent year the patient was in care and used validated surveys (AUDIT-C and ASSIST) to assess risk behaviors in the past 3-6 months. They collected information from 5,084 women and 158,745 HIV primary care and women’s health visits.
The median patient age was 47 years; 62.1% of the patients were black; 70% had CD4 counts greater than 350; and 73.6% had HIV viral loads of less than 500 copies/mL. In terms of reported risk, 60.6% of the women were sexually active, (85.5% of whom reported monogamy); 13.1% had problem alcohol use, and 11.6% had active drug use.
Sampling for gonorrhea and chlamydia were mostly from urogenital sites (86.6%), 6.6% were extragenital, and 6.8% were “other.” Nearly all (98.5%) of 23,492 chlamydia tests and 95.7% of 23,324 gonorrhea tests used nucleic acid amplification, Dr. Dionne-Odom said.
During the most recent year in care, 42.7% of women were tested for gonorrhea and chlamydia, and 3.4% were positive, with the annual positivity rates over the study ranging from 1.5% to 3.2% for chlamydia and 0.9% to 1.5% for gonorrhea. However, Dr. Dionne-Odom and her colleagues found that the prevalence of STIs was inversely related to patient age, with gonorrhea and chlamydia positivity in 2016 being 16% for chlamydia and 3.9% for gonorrhea among women aged 18-24 years, compared with 1.1% and 0.7%, respectively, for women older than 50 years.
“As with national data on women, HIV-infected women aged 18-29 years had the highest rates of gonorrhea and chlamydia. Our results show that targeted screening for chlamydia and gonorrhea in women with HIV based on age and risk is warranted,” Dr. Dionne-Odom concluded.
Dr. Dionne-Odom reported that she had no relevant disclosures.
WASHINGTON – Among HIV-infected women, those aged 18-29 years had the highest rates of gonorrhea and chlamydia. These results suggest that screening for these sexually transmitted infections (STIs) should be based on age and risk in HIV-infected women, said Jodie Dionne-Odom, MD, of the University of Alabama at Birmingham.
Annual screening for gonorrhea and chlamydia is recommended for all sexually active adults with HIV, but prevalence varies by gender, age, and risk behavior, Dr. Dionne-Odom said at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Dr. Odom and her colleagues calculated annual testing and positivity rates during 2007-2016 for chlamydia and gonorrhea among women engaged in HIV care in eight U.S. cities as part of the Centers for AIDS Research (CFAR) Clinical Networks and Integrated Clinical Services (CNICS) longitudinal cohort.
They assessed demographic data based on the most recent year the patient was in care and used validated surveys (AUDIT-C and ASSIST) to assess risk behaviors in the past 3-6 months. They collected information from 5,084 women and 158,745 HIV primary care and women’s health visits.
The median patient age was 47 years; 62.1% of the patients were black; 70% had CD4 counts greater than 350; and 73.6% had HIV viral loads of less than 500 copies/mL. In terms of reported risk, 60.6% of the women were sexually active, (85.5% of whom reported monogamy); 13.1% had problem alcohol use, and 11.6% had active drug use.
Sampling for gonorrhea and chlamydia were mostly from urogenital sites (86.6%), 6.6% were extragenital, and 6.8% were “other.” Nearly all (98.5%) of 23,492 chlamydia tests and 95.7% of 23,324 gonorrhea tests used nucleic acid amplification, Dr. Dionne-Odom said.
During the most recent year in care, 42.7% of women were tested for gonorrhea and chlamydia, and 3.4% were positive, with the annual positivity rates over the study ranging from 1.5% to 3.2% for chlamydia and 0.9% to 1.5% for gonorrhea. However, Dr. Dionne-Odom and her colleagues found that the prevalence of STIs was inversely related to patient age, with gonorrhea and chlamydia positivity in 2016 being 16% for chlamydia and 3.9% for gonorrhea among women aged 18-24 years, compared with 1.1% and 0.7%, respectively, for women older than 50 years.
“As with national data on women, HIV-infected women aged 18-29 years had the highest rates of gonorrhea and chlamydia. Our results show that targeted screening for chlamydia and gonorrhea in women with HIV based on age and risk is warranted,” Dr. Dionne-Odom concluded.
Dr. Dionne-Odom reported that she had no relevant disclosures.
REPORTING FROM THE 2018 STD PREVENTION CONFERENCE
Key clinical point: Targeted screening for chlamydia and gonorrhea in women with HIV based on age, risk is warranted.
Major finding: Chlamydia infections were seen in 16% and gonorrhea in 3.9% of HIV-infected women aged 18-24 years and in 1.1% and 0.7%, respectively, in women over age 50.
Study details: Data analysis of 5,084 women in 8 U.S. cities during 2007-2016.
Disclosures: Dr. Dionne-Odom reported that she had no relevant disclosures.
Two red flags spell trouble ahead in spontaneous coronary artery dissection
MUNICH –
Women whose spontaneous coronary artery dissection (SCAD) occurred during the peripartum period were at 2.8-fold increased risk of in-hospital major adverse events in a multivariate analysis, while those with a background connective tissue disorder were at 8.7-fold increased risk for major adverse cardiovascular events within 30 days of hospitalization in the Canadian SCAD (CanSCAD) study, Jacqueline Saw, MD, reported at the annual congress of the European Society of Cardiology.
CanSCAD is an ongoing, rigorous, prospective, multicenter, observational study of 750 patients with SCAD documented on angiography and confirmed in a core lab. To put the study in perspective, the worldwide medical literature published over the last decade contains fewer than 1,300 other cases of this seriously underdiagnosed, poorly understood disorder, noted Dr. Saw, CanSCAD principal investigator and a cardiologist at the University of British Columbia, Vancouver. Because much remains unclear about SCAD, a condition mistakenly considered to be rare in the past, the Canadian study was undertaken to shed light on predisposing and precipitating factors, optimal management, and clinical outcomes. Although Dr. Saw could present only the in-hospital and 30-day outcomes, follow-up will continue at 6, 12, 24, and 36 months.
SCAD is a nontraumatic, noniatrogenic, nonatherosclerotic separation of the coronary artery wall by intramural hematoma, creating a false lumen which compresses the true arterial lumen. This compromises blood flow with resultant myocardial ischemia or infarction. Intimal tear may or may not be present.
CanSCAD underscored that this is predominantly a disease affecting relatively young women: 89% of SCAD participants were female, 55% of whom were postmenopausal. The mean age at presentation was 52 years, and only 9% of subjects were older than age 65. Seventy percent of subjects presented with non–ST-elevation MI, the other 30% with STEMI. The predominant symptom was chest pain in 92% of patients. The average length of hospital stay was 4 days.
In terms of precipitating factors, half of patients cited high or severe emotional stress, with 41% of subjects scoring 20 or higher on the Perceived Stress Scale. About 30% of patients cited unusually intense physical stress, such as lifting more than 50 pounds, as a precipitating factor.
Of note, one-third of patients had no cardiovascular risk factors.
The in-hospital major adverse event rate – a composite of all-cause mortality, stroke, recurrent MI, cardiogenic shock, heart failure, cardiac arrest, repeat or unplanned revascularization, and heart transplantation – was 8.8%. Mortality through 1 month was reassuringly low, at 0.1%. Nonetheless, 4.9% of patients experienced recurrent symptoms necessitating emergency room visits within 30 days post discharge, and 2.5% required hospitalization because of their chest pain.
Patients who presented with SCAD during the peripartum period were more severely affected. Although they accounted for only 4.5% of subjects, their in-hospital major adverse event rate was 20.6%, compared with 8.2% in the others. They had a 17.6% prevalence of a left ventricular ejection fraction below 35%, as did only 3.1% of patients without peripartum SCAD. They were more than twice as likely to have elevated cardiac troponin levels. Moreover, peripartum SCAD was independently associated with a 2.9-fold increased risk of major adverse cardiovascular events at 30 days, a composite of all-cause mortality, stroke, recurrent MI, heart failure, or revascularization.
The other independent predictor of 30-day major adverse cardiovascular events in a multivariate logistic regression analysis was having a connective tissue disorder, present in 3.6% of participants.
Management was conservative, with no percutaneous coronary intervention used in 84% of patients. Outcomes were worse in the subgroup who underwent PCI, but Dr. Saw cautioned against making much of that.
“Keep in mind that the patients who undergo PCI are typically the higher-risk cohort with ongoing ischemia and chest pain, so there will be some bias there,” according to the cardiologist.
Session chair Patrick W. Serruys, MD, of Erasmus University, Rotterdam, the Netherlands, commented, “It seems like there is a critical period of 30 days, more or less, and beyond that time the situation can be considered as settled and a wait-and-see attitude is fine. It looked like patients with peripartum dissection or connective tissue disease should potentially be kept in hospital for at least 15 days, and maybe 30 days, because I see your cumulative adverse event curve plateauing around 15 days.”
“Are you doing that in your practice?” asked Dr. Serruys.
“It’s true that conservatively managed patients should remain in hospital for typically about 4 days. For patients with a high-risk presentation we do advocate staying in hospital for longer periods,” Dr. Saw replied. “It would be great to keep them for 15 days, although typically if their chest pain has settled by 10 days they can be discharged home.”
Audience members were eager to hear her recommendations regarding dual-antiplatelet therapy. She explained that in her practice patients are generally discharged on aspirin and clopidogrel and typically continue the clopidogrel for at least a month.
“When we follow them in the office at 1 month, if their chest pain has settled, we would discontinue DAPT,” Dr. Saw said.
The ongoing CanSCAD study is sponsored by the Canadian Institutes of Health Research, the Stroke Foundation of Canada, the National Institutes of Health, Abbott Vascular, Boston Scientific, AstraZeneca, and Servier. Dr. Saw reported serving as a consultant to Abbott Vascular and Boston Scientific.
MUNICH –
Women whose spontaneous coronary artery dissection (SCAD) occurred during the peripartum period were at 2.8-fold increased risk of in-hospital major adverse events in a multivariate analysis, while those with a background connective tissue disorder were at 8.7-fold increased risk for major adverse cardiovascular events within 30 days of hospitalization in the Canadian SCAD (CanSCAD) study, Jacqueline Saw, MD, reported at the annual congress of the European Society of Cardiology.
CanSCAD is an ongoing, rigorous, prospective, multicenter, observational study of 750 patients with SCAD documented on angiography and confirmed in a core lab. To put the study in perspective, the worldwide medical literature published over the last decade contains fewer than 1,300 other cases of this seriously underdiagnosed, poorly understood disorder, noted Dr. Saw, CanSCAD principal investigator and a cardiologist at the University of British Columbia, Vancouver. Because much remains unclear about SCAD, a condition mistakenly considered to be rare in the past, the Canadian study was undertaken to shed light on predisposing and precipitating factors, optimal management, and clinical outcomes. Although Dr. Saw could present only the in-hospital and 30-day outcomes, follow-up will continue at 6, 12, 24, and 36 months.
SCAD is a nontraumatic, noniatrogenic, nonatherosclerotic separation of the coronary artery wall by intramural hematoma, creating a false lumen which compresses the true arterial lumen. This compromises blood flow with resultant myocardial ischemia or infarction. Intimal tear may or may not be present.
CanSCAD underscored that this is predominantly a disease affecting relatively young women: 89% of SCAD participants were female, 55% of whom were postmenopausal. The mean age at presentation was 52 years, and only 9% of subjects were older than age 65. Seventy percent of subjects presented with non–ST-elevation MI, the other 30% with STEMI. The predominant symptom was chest pain in 92% of patients. The average length of hospital stay was 4 days.
In terms of precipitating factors, half of patients cited high or severe emotional stress, with 41% of subjects scoring 20 or higher on the Perceived Stress Scale. About 30% of patients cited unusually intense physical stress, such as lifting more than 50 pounds, as a precipitating factor.
Of note, one-third of patients had no cardiovascular risk factors.
The in-hospital major adverse event rate – a composite of all-cause mortality, stroke, recurrent MI, cardiogenic shock, heart failure, cardiac arrest, repeat or unplanned revascularization, and heart transplantation – was 8.8%. Mortality through 1 month was reassuringly low, at 0.1%. Nonetheless, 4.9% of patients experienced recurrent symptoms necessitating emergency room visits within 30 days post discharge, and 2.5% required hospitalization because of their chest pain.
Patients who presented with SCAD during the peripartum period were more severely affected. Although they accounted for only 4.5% of subjects, their in-hospital major adverse event rate was 20.6%, compared with 8.2% in the others. They had a 17.6% prevalence of a left ventricular ejection fraction below 35%, as did only 3.1% of patients without peripartum SCAD. They were more than twice as likely to have elevated cardiac troponin levels. Moreover, peripartum SCAD was independently associated with a 2.9-fold increased risk of major adverse cardiovascular events at 30 days, a composite of all-cause mortality, stroke, recurrent MI, heart failure, or revascularization.
The other independent predictor of 30-day major adverse cardiovascular events in a multivariate logistic regression analysis was having a connective tissue disorder, present in 3.6% of participants.
Management was conservative, with no percutaneous coronary intervention used in 84% of patients. Outcomes were worse in the subgroup who underwent PCI, but Dr. Saw cautioned against making much of that.
“Keep in mind that the patients who undergo PCI are typically the higher-risk cohort with ongoing ischemia and chest pain, so there will be some bias there,” according to the cardiologist.
Session chair Patrick W. Serruys, MD, of Erasmus University, Rotterdam, the Netherlands, commented, “It seems like there is a critical period of 30 days, more or less, and beyond that time the situation can be considered as settled and a wait-and-see attitude is fine. It looked like patients with peripartum dissection or connective tissue disease should potentially be kept in hospital for at least 15 days, and maybe 30 days, because I see your cumulative adverse event curve plateauing around 15 days.”
“Are you doing that in your practice?” asked Dr. Serruys.
“It’s true that conservatively managed patients should remain in hospital for typically about 4 days. For patients with a high-risk presentation we do advocate staying in hospital for longer periods,” Dr. Saw replied. “It would be great to keep them for 15 days, although typically if their chest pain has settled by 10 days they can be discharged home.”
Audience members were eager to hear her recommendations regarding dual-antiplatelet therapy. She explained that in her practice patients are generally discharged on aspirin and clopidogrel and typically continue the clopidogrel for at least a month.
“When we follow them in the office at 1 month, if their chest pain has settled, we would discontinue DAPT,” Dr. Saw said.
The ongoing CanSCAD study is sponsored by the Canadian Institutes of Health Research, the Stroke Foundation of Canada, the National Institutes of Health, Abbott Vascular, Boston Scientific, AstraZeneca, and Servier. Dr. Saw reported serving as a consultant to Abbott Vascular and Boston Scientific.
MUNICH –
Women whose spontaneous coronary artery dissection (SCAD) occurred during the peripartum period were at 2.8-fold increased risk of in-hospital major adverse events in a multivariate analysis, while those with a background connective tissue disorder were at 8.7-fold increased risk for major adverse cardiovascular events within 30 days of hospitalization in the Canadian SCAD (CanSCAD) study, Jacqueline Saw, MD, reported at the annual congress of the European Society of Cardiology.
CanSCAD is an ongoing, rigorous, prospective, multicenter, observational study of 750 patients with SCAD documented on angiography and confirmed in a core lab. To put the study in perspective, the worldwide medical literature published over the last decade contains fewer than 1,300 other cases of this seriously underdiagnosed, poorly understood disorder, noted Dr. Saw, CanSCAD principal investigator and a cardiologist at the University of British Columbia, Vancouver. Because much remains unclear about SCAD, a condition mistakenly considered to be rare in the past, the Canadian study was undertaken to shed light on predisposing and precipitating factors, optimal management, and clinical outcomes. Although Dr. Saw could present only the in-hospital and 30-day outcomes, follow-up will continue at 6, 12, 24, and 36 months.
SCAD is a nontraumatic, noniatrogenic, nonatherosclerotic separation of the coronary artery wall by intramural hematoma, creating a false lumen which compresses the true arterial lumen. This compromises blood flow with resultant myocardial ischemia or infarction. Intimal tear may or may not be present.
CanSCAD underscored that this is predominantly a disease affecting relatively young women: 89% of SCAD participants were female, 55% of whom were postmenopausal. The mean age at presentation was 52 years, and only 9% of subjects were older than age 65. Seventy percent of subjects presented with non–ST-elevation MI, the other 30% with STEMI. The predominant symptom was chest pain in 92% of patients. The average length of hospital stay was 4 days.
In terms of precipitating factors, half of patients cited high or severe emotional stress, with 41% of subjects scoring 20 or higher on the Perceived Stress Scale. About 30% of patients cited unusually intense physical stress, such as lifting more than 50 pounds, as a precipitating factor.
Of note, one-third of patients had no cardiovascular risk factors.
The in-hospital major adverse event rate – a composite of all-cause mortality, stroke, recurrent MI, cardiogenic shock, heart failure, cardiac arrest, repeat or unplanned revascularization, and heart transplantation – was 8.8%. Mortality through 1 month was reassuringly low, at 0.1%. Nonetheless, 4.9% of patients experienced recurrent symptoms necessitating emergency room visits within 30 days post discharge, and 2.5% required hospitalization because of their chest pain.
Patients who presented with SCAD during the peripartum period were more severely affected. Although they accounted for only 4.5% of subjects, their in-hospital major adverse event rate was 20.6%, compared with 8.2% in the others. They had a 17.6% prevalence of a left ventricular ejection fraction below 35%, as did only 3.1% of patients without peripartum SCAD. They were more than twice as likely to have elevated cardiac troponin levels. Moreover, peripartum SCAD was independently associated with a 2.9-fold increased risk of major adverse cardiovascular events at 30 days, a composite of all-cause mortality, stroke, recurrent MI, heart failure, or revascularization.
The other independent predictor of 30-day major adverse cardiovascular events in a multivariate logistic regression analysis was having a connective tissue disorder, present in 3.6% of participants.
Management was conservative, with no percutaneous coronary intervention used in 84% of patients. Outcomes were worse in the subgroup who underwent PCI, but Dr. Saw cautioned against making much of that.
“Keep in mind that the patients who undergo PCI are typically the higher-risk cohort with ongoing ischemia and chest pain, so there will be some bias there,” according to the cardiologist.
Session chair Patrick W. Serruys, MD, of Erasmus University, Rotterdam, the Netherlands, commented, “It seems like there is a critical period of 30 days, more or less, and beyond that time the situation can be considered as settled and a wait-and-see attitude is fine. It looked like patients with peripartum dissection or connective tissue disease should potentially be kept in hospital for at least 15 days, and maybe 30 days, because I see your cumulative adverse event curve plateauing around 15 days.”
“Are you doing that in your practice?” asked Dr. Serruys.
“It’s true that conservatively managed patients should remain in hospital for typically about 4 days. For patients with a high-risk presentation we do advocate staying in hospital for longer periods,” Dr. Saw replied. “It would be great to keep them for 15 days, although typically if their chest pain has settled by 10 days they can be discharged home.”
Audience members were eager to hear her recommendations regarding dual-antiplatelet therapy. She explained that in her practice patients are generally discharged on aspirin and clopidogrel and typically continue the clopidogrel for at least a month.
“When we follow them in the office at 1 month, if their chest pain has settled, we would discontinue DAPT,” Dr. Saw said.
The ongoing CanSCAD study is sponsored by the Canadian Institutes of Health Research, the Stroke Foundation of Canada, the National Institutes of Health, Abbott Vascular, Boston Scientific, AstraZeneca, and Servier. Dr. Saw reported serving as a consultant to Abbott Vascular and Boston Scientific.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: SCAD occurring during the peripartum period or in patients with connective tissue disease identifies subgroups at high risk for major adverse cardiovascular events within 30 days.
Major finding: Patients with spontaneous coronary artery dissection and comorbid connective tissue disease were at 8.7-fold increased risk of major adverse cardiovascular events within 30 days.
Study details: CanSCAD is an ongoing, prospective, multicenter, observational study in 750 patients with confirmed spontaneous coronary artery dissection.
Disclosures: CanSCAD is sponsored by the Canadian Institutes of Health Research, the Stroke Foundation of Canada, the National Institutes of Health, Abbott Vascular, Boston Scientific, AstraZeneca, and Servier.
Vaginal intraepithelial neoplasia: What to do when dysplasia persists after hysterectomy
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
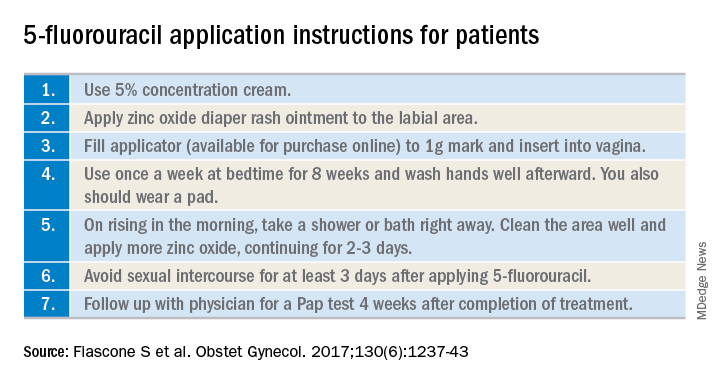
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
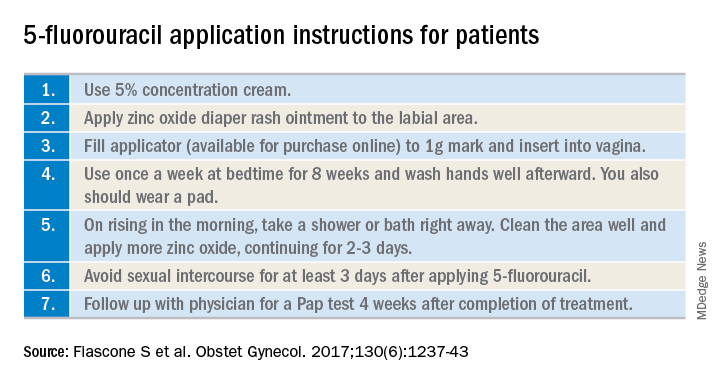
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
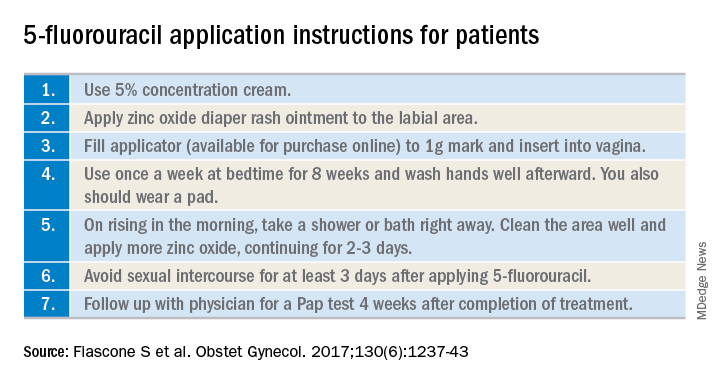
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
One-step gestational diabetes screening doesn’t improve outcomes
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Increased diagnoses of gestational diabetes did not significantly improve maternal or fetal outcomes.
Major finding: Adoption of a one-step screening process for gestational diabetes increased diagnoses by 41%.
Study details: The data come from a before-and-after cohort study with a population of 23,257 women.
Disclosures: Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
Source: Pocobelli G et al. Obstet Gynecol. 2018;132:859-67.
Opioid Use Disorder Numbers Among Pregnant Women Are on the Rise
The number of women with opioid use disorder (OUD) at labor and delivery more than quadrupled between 1999 and 2014, according to a first-ever multistate analysis of trends by the CDC.
Researchers found that the national prevalence rate of OUD rose from 1.5 per 1,000 delivery hospitalizations in 1999 to 6.5 in 2014. On average, the national prevalence rate grew by 0.39 cases per 1,000 each year.
The increases were significant and seen in all of the 28 states with at least 3 years of data available for analysis. The average increases were lowest in California and Hawaii and highest in Maine, New Mexico, Vermont, and West Virginia.
Opioid use disorder during pregnancy has been associated with a range of negative health outcomes, including maternal death, preterm birth, stillbirth, and neonatal abstinence syndrome (NAS).
The CDC’s recommended strategies include:
- Implementing universal substance use screening at the first prenatal visit;
- Ensuring pregnant women with OUD have access to medication-assisted therapy and related addiction services; and
- Ensuring that mothers with OUD receive adequate patient-centered postpartum care, including mental health and substance use treatment, relapse-prevention programs, and family planning services
The CDC also is supporting state-based perinatal quality cooperatives, networks of teams working to better identify women with OUD during pregnancy and to standardize care for mothers and NAS-affected infants.
The number of women with opioid use disorder (OUD) at labor and delivery more than quadrupled between 1999 and 2014, according to a first-ever multistate analysis of trends by the CDC.
Researchers found that the national prevalence rate of OUD rose from 1.5 per 1,000 delivery hospitalizations in 1999 to 6.5 in 2014. On average, the national prevalence rate grew by 0.39 cases per 1,000 each year.
The increases were significant and seen in all of the 28 states with at least 3 years of data available for analysis. The average increases were lowest in California and Hawaii and highest in Maine, New Mexico, Vermont, and West Virginia.
Opioid use disorder during pregnancy has been associated with a range of negative health outcomes, including maternal death, preterm birth, stillbirth, and neonatal abstinence syndrome (NAS).
The CDC’s recommended strategies include:
- Implementing universal substance use screening at the first prenatal visit;
- Ensuring pregnant women with OUD have access to medication-assisted therapy and related addiction services; and
- Ensuring that mothers with OUD receive adequate patient-centered postpartum care, including mental health and substance use treatment, relapse-prevention programs, and family planning services
The CDC also is supporting state-based perinatal quality cooperatives, networks of teams working to better identify women with OUD during pregnancy and to standardize care for mothers and NAS-affected infants.
The number of women with opioid use disorder (OUD) at labor and delivery more than quadrupled between 1999 and 2014, according to a first-ever multistate analysis of trends by the CDC.
Researchers found that the national prevalence rate of OUD rose from 1.5 per 1,000 delivery hospitalizations in 1999 to 6.5 in 2014. On average, the national prevalence rate grew by 0.39 cases per 1,000 each year.
The increases were significant and seen in all of the 28 states with at least 3 years of data available for analysis. The average increases were lowest in California and Hawaii and highest in Maine, New Mexico, Vermont, and West Virginia.
Opioid use disorder during pregnancy has been associated with a range of negative health outcomes, including maternal death, preterm birth, stillbirth, and neonatal abstinence syndrome (NAS).
The CDC’s recommended strategies include:
- Implementing universal substance use screening at the first prenatal visit;
- Ensuring pregnant women with OUD have access to medication-assisted therapy and related addiction services; and
- Ensuring that mothers with OUD receive adequate patient-centered postpartum care, including mental health and substance use treatment, relapse-prevention programs, and family planning services
The CDC also is supporting state-based perinatal quality cooperatives, networks of teams working to better identify women with OUD during pregnancy and to standardize care for mothers and NAS-affected infants.
Severe maternal morbidity climbs; racial disparities persist
The rate of severe maternal morbidity in the United States has climbed steadily since 2006, increasing 45% overall in the decade ending in 2015, according to a new report from the Agency for Healthcare Research and Quality that also found large ethnic and racial, geographic, and socioeconomic variation in rates of severe maternal morbidity.
The longstanding increased risk for severe maternal morbidity for black women, compared with white women, continued essentially unchanged, with black women 112%-115% more likely to experience any of 21 conditions and procedures that defined severe maternal morbidity in the report. Disparities also existed between white women and those of Hispanic or Asian/Pacific Islander origin, but those gaps are narrowing, according to the report.
“Black women, Hispanic women, and women of other races/ethnicities were overrepresented among deliveries involving severe maternal morbidity, as compared with white women,” wrote Kathryn Fingar, PhD, and her coauthors. “White women constituted a lower percentage of deliveries with any severe maternal morbidity than they did other deliveries” – 23% lower.
The 21 indicators, developed by the Centers for Disease Control and Prevention, range from conditions such as renal failure and sepsis to in-hospital procedures such as blood transfusion and hysterectomy. Women were considered to have severe maternal morbidity if any of the indicators were present, regardless of whether in-hospital death occurred.

Dr. Fingar of IBM Watson Health, Cambridge, Mass., and her collaborators summarized data from AHRQ’s Healthcare Cost and Utilization Project (H-CUP) in the statistical brief. The two most common procedures that indicate severe maternal morbidity are blood transfusion and hysterectomy, and these indicators were tracked in deliveries where women had a condition that served as one of the severe maternal morbidity indicators.
Dr. Fingar and her colleagues noted that they excluded data for the final quarter of 2015, because that is when the transition from the 9th to the 10th edition of the International Classifications of Diseases was made.
In addition to the overall increase from 101.3 to 146.6 women per 10,000 experiencing any severe maternal morbidity, the incidence of blood transfusion during a delivery hospitalization, either alone or in conjunction with other indicators, rose from 78.9 to 121.1 women per 10,000, an increase of 54%.
Showing that increased blood transfusions were a major driver of the jump in severe maternal morbidity, the composite increase in the rates of all other indicators went from 34 to 42 per delivery hospitalization, an increase of just 24%, or less than half the increase in blood transfusions.
There was significant variation in trends over time for the rates of the other indicators: acute renal failure, shock, the need for mechanical ventilation, and sepsis all increased by at least 100% (range, 104%-134%), and the rates of aneurysm increased by 99%. Rates of other indicators fell; pulmonary edema, embolism, eclampsia, myocardial infarction, cerebrovascular disorders, serious anesthesia complications, and intraoperative heart failure and arrest all declined by 25%-53% during the data-gathering period.
Looking at the data another way, 78% of cases of severe maternal morbidity in 2006 and 83% in 2015 involved a blood transfusion, making it the most common indicator. Far fewer delivery hospitalizations involved disseminated intravascular coagulation (DIC) and hysterectomy, the next most common indicators, which were seen in just 8% of cases.
Blood transfusions were most likely in women with shock (72%), amniotic fluid embolism (63%), sickle cell disease with crisis (54%), and DIC (51%).
One in three women who experienced shock during delivery had a hysterectomy, as did more than 20% of women who experienced adult respiratory distress syndrome or cardiac arrest (or ventricular fibrillation).
Women delivering at the youngest and oldest ends of the age spectrum were more likely to experience severe maternal morbidity. For women younger than 20 years of age, the rate was 206 per 10,000. In the group of women aged 40 years and over, the rate of any severe maternal morbidity was 248 per 10,000 delivery hospitalizations. Women in their 20s and 30s had rates of 136 and 143 per 10,000, respectively.
Besides race/ethnicity and age, a variety of other patient characteristics were associated with increased rates of severe maternal morbidity and mortality, with higher rates seen in women from the poorest quartile than the wealthiest (177 versus 122 per 10,000, respectively). Women with Medicaid were more likely than those with private insurance to experience severe maternal morbidity during a delivery hospitalization (175 versus 121 per 10,000, respectively).
Similarly, severe maternal morbidity was more common in safety net hospitals and in minority-serving hospitals (182 versus 128 and 176 versus 123 per 10,000, respectively) than other hospitals.
Regionally, severe maternal morbidity was most common in the Northeast and the South, at 165 and 164 per 10,000, respectively, compared with rates of 132 and 116 in the West and Midwest, respectively.
Hospital deaths per 100,000 delivery hospitalizations were 248% higher for black than white women in 2006. By the end of 2015, that figure declined modestly to 193%, with absolute rates of 19 versus 5.5 deaths per 100,000 delivery hospitalizations for black versus white women in 2006. In 2015, the absolute rates were 11 versus 4 per 100,000.
The study was conducted by the Agency for Healthcare Research and Quality. There were no reported conflicts of interest.
SOURCE: Fingar K et al. Agency for Healthcare Research and Quality Statistical Brief #243.
The data here confirm, again, that we have a crisis in maternal health care in the United States. Not only is severe maternal morbidity increasing, but disparities in outcomes between white and black women persist, such that severe maternal morbidity is twice as common among black women as it is among white women.
It’s tempting to attribute the gap to social determinants of health that are outside the control of the obstetrician-gynecologist. But education doesn’t protect black women: the New York City Department of Health and Mental Hygiene found that non-Hispanic black women with a college degree have higher rates of severe maternal morbidity than women of other race/ethnicities who never graduated high school. It’s a stark finding that’s illustrated by the heartbreaking story of Shalon Irving, a PhD epidemiologist at the Centers for Disease Control and Prevention, whose postpartum death was reported by ProPublica last winter.
One contributing factor is likely to be implicit biases that affect how well we see and hear patients who are different from us. I was mortified to see my own implicit biases when I took the Project Implicit Social Attitudes test (https://implicit.harvard.edu/implicit/). These aren’t the beliefs that we choose – they are the patterns that we absorb from our day-to-day lives. If you search Google images for “pregnancy,” “motherhood,” or “breastfeeding,” the overwhelming majority of images feature white women, whereas the phrase “welfare queen” is used to denigrate the reproduction of women of color. That’s the world we live in, and these patterns reinforce mental short cuts that are more likely to drive our behavior when we’re pressed for time, as we are every day in clinical practice. In one study in a pediatric emergency department, the busier the shift, the higher the providers’ implicit bias at the end of the shift.
We might start by looking at the images on our web sites and hanging in our offices and hospital corridors – do they look like the women we care for? Do they celebrate pregnancy and parenthood for diverse families? And how can we make sure that we pause, before we walk into a patient’s room, so that we can be fully present to her individual strengths and vulnerabilities, and tailor our care to her as an individual?
Alison Stuebe, MD, of the University of North Carolina, Chapel Hill, is medical director of lactation services and on the steering committee for Moms Rising North Carolina, the Breastfeeding Expert Work Group for the American College of Obstetricians and Gynecologists, and a board member of the Society for Maternal-Fetal Medicine. She was asked to comment on the AHRQ report by this newspaper.
The data here confirm, again, that we have a crisis in maternal health care in the United States. Not only is severe maternal morbidity increasing, but disparities in outcomes between white and black women persist, such that severe maternal morbidity is twice as common among black women as it is among white women.
It’s tempting to attribute the gap to social determinants of health that are outside the control of the obstetrician-gynecologist. But education doesn’t protect black women: the New York City Department of Health and Mental Hygiene found that non-Hispanic black women with a college degree have higher rates of severe maternal morbidity than women of other race/ethnicities who never graduated high school. It’s a stark finding that’s illustrated by the heartbreaking story of Shalon Irving, a PhD epidemiologist at the Centers for Disease Control and Prevention, whose postpartum death was reported by ProPublica last winter.
One contributing factor is likely to be implicit biases that affect how well we see and hear patients who are different from us. I was mortified to see my own implicit biases when I took the Project Implicit Social Attitudes test (https://implicit.harvard.edu/implicit/). These aren’t the beliefs that we choose – they are the patterns that we absorb from our day-to-day lives. If you search Google images for “pregnancy,” “motherhood,” or “breastfeeding,” the overwhelming majority of images feature white women, whereas the phrase “welfare queen” is used to denigrate the reproduction of women of color. That’s the world we live in, and these patterns reinforce mental short cuts that are more likely to drive our behavior when we’re pressed for time, as we are every day in clinical practice. In one study in a pediatric emergency department, the busier the shift, the higher the providers’ implicit bias at the end of the shift.
We might start by looking at the images on our web sites and hanging in our offices and hospital corridors – do they look like the women we care for? Do they celebrate pregnancy and parenthood for diverse families? And how can we make sure that we pause, before we walk into a patient’s room, so that we can be fully present to her individual strengths and vulnerabilities, and tailor our care to her as an individual?
Alison Stuebe, MD, of the University of North Carolina, Chapel Hill, is medical director of lactation services and on the steering committee for Moms Rising North Carolina, the Breastfeeding Expert Work Group for the American College of Obstetricians and Gynecologists, and a board member of the Society for Maternal-Fetal Medicine. She was asked to comment on the AHRQ report by this newspaper.
The data here confirm, again, that we have a crisis in maternal health care in the United States. Not only is severe maternal morbidity increasing, but disparities in outcomes between white and black women persist, such that severe maternal morbidity is twice as common among black women as it is among white women.
It’s tempting to attribute the gap to social determinants of health that are outside the control of the obstetrician-gynecologist. But education doesn’t protect black women: the New York City Department of Health and Mental Hygiene found that non-Hispanic black women with a college degree have higher rates of severe maternal morbidity than women of other race/ethnicities who never graduated high school. It’s a stark finding that’s illustrated by the heartbreaking story of Shalon Irving, a PhD epidemiologist at the Centers for Disease Control and Prevention, whose postpartum death was reported by ProPublica last winter.
One contributing factor is likely to be implicit biases that affect how well we see and hear patients who are different from us. I was mortified to see my own implicit biases when I took the Project Implicit Social Attitudes test (https://implicit.harvard.edu/implicit/). These aren’t the beliefs that we choose – they are the patterns that we absorb from our day-to-day lives. If you search Google images for “pregnancy,” “motherhood,” or “breastfeeding,” the overwhelming majority of images feature white women, whereas the phrase “welfare queen” is used to denigrate the reproduction of women of color. That’s the world we live in, and these patterns reinforce mental short cuts that are more likely to drive our behavior when we’re pressed for time, as we are every day in clinical practice. In one study in a pediatric emergency department, the busier the shift, the higher the providers’ implicit bias at the end of the shift.
We might start by looking at the images on our web sites and hanging in our offices and hospital corridors – do they look like the women we care for? Do they celebrate pregnancy and parenthood for diverse families? And how can we make sure that we pause, before we walk into a patient’s room, so that we can be fully present to her individual strengths and vulnerabilities, and tailor our care to her as an individual?
Alison Stuebe, MD, of the University of North Carolina, Chapel Hill, is medical director of lactation services and on the steering committee for Moms Rising North Carolina, the Breastfeeding Expert Work Group for the American College of Obstetricians and Gynecologists, and a board member of the Society for Maternal-Fetal Medicine. She was asked to comment on the AHRQ report by this newspaper.
The rate of severe maternal morbidity in the United States has climbed steadily since 2006, increasing 45% overall in the decade ending in 2015, according to a new report from the Agency for Healthcare Research and Quality that also found large ethnic and racial, geographic, and socioeconomic variation in rates of severe maternal morbidity.
The longstanding increased risk for severe maternal morbidity for black women, compared with white women, continued essentially unchanged, with black women 112%-115% more likely to experience any of 21 conditions and procedures that defined severe maternal morbidity in the report. Disparities also existed between white women and those of Hispanic or Asian/Pacific Islander origin, but those gaps are narrowing, according to the report.
“Black women, Hispanic women, and women of other races/ethnicities were overrepresented among deliveries involving severe maternal morbidity, as compared with white women,” wrote Kathryn Fingar, PhD, and her coauthors. “White women constituted a lower percentage of deliveries with any severe maternal morbidity than they did other deliveries” – 23% lower.
The 21 indicators, developed by the Centers for Disease Control and Prevention, range from conditions such as renal failure and sepsis to in-hospital procedures such as blood transfusion and hysterectomy. Women were considered to have severe maternal morbidity if any of the indicators were present, regardless of whether in-hospital death occurred.

Dr. Fingar of IBM Watson Health, Cambridge, Mass., and her collaborators summarized data from AHRQ’s Healthcare Cost and Utilization Project (H-CUP) in the statistical brief. The two most common procedures that indicate severe maternal morbidity are blood transfusion and hysterectomy, and these indicators were tracked in deliveries where women had a condition that served as one of the severe maternal morbidity indicators.
Dr. Fingar and her colleagues noted that they excluded data for the final quarter of 2015, because that is when the transition from the 9th to the 10th edition of the International Classifications of Diseases was made.
In addition to the overall increase from 101.3 to 146.6 women per 10,000 experiencing any severe maternal morbidity, the incidence of blood transfusion during a delivery hospitalization, either alone or in conjunction with other indicators, rose from 78.9 to 121.1 women per 10,000, an increase of 54%.
Showing that increased blood transfusions were a major driver of the jump in severe maternal morbidity, the composite increase in the rates of all other indicators went from 34 to 42 per delivery hospitalization, an increase of just 24%, or less than half the increase in blood transfusions.
There was significant variation in trends over time for the rates of the other indicators: acute renal failure, shock, the need for mechanical ventilation, and sepsis all increased by at least 100% (range, 104%-134%), and the rates of aneurysm increased by 99%. Rates of other indicators fell; pulmonary edema, embolism, eclampsia, myocardial infarction, cerebrovascular disorders, serious anesthesia complications, and intraoperative heart failure and arrest all declined by 25%-53% during the data-gathering period.
Looking at the data another way, 78% of cases of severe maternal morbidity in 2006 and 83% in 2015 involved a blood transfusion, making it the most common indicator. Far fewer delivery hospitalizations involved disseminated intravascular coagulation (DIC) and hysterectomy, the next most common indicators, which were seen in just 8% of cases.
Blood transfusions were most likely in women with shock (72%), amniotic fluid embolism (63%), sickle cell disease with crisis (54%), and DIC (51%).
One in three women who experienced shock during delivery had a hysterectomy, as did more than 20% of women who experienced adult respiratory distress syndrome or cardiac arrest (or ventricular fibrillation).
Women delivering at the youngest and oldest ends of the age spectrum were more likely to experience severe maternal morbidity. For women younger than 20 years of age, the rate was 206 per 10,000. In the group of women aged 40 years and over, the rate of any severe maternal morbidity was 248 per 10,000 delivery hospitalizations. Women in their 20s and 30s had rates of 136 and 143 per 10,000, respectively.
Besides race/ethnicity and age, a variety of other patient characteristics were associated with increased rates of severe maternal morbidity and mortality, with higher rates seen in women from the poorest quartile than the wealthiest (177 versus 122 per 10,000, respectively). Women with Medicaid were more likely than those with private insurance to experience severe maternal morbidity during a delivery hospitalization (175 versus 121 per 10,000, respectively).
Similarly, severe maternal morbidity was more common in safety net hospitals and in minority-serving hospitals (182 versus 128 and 176 versus 123 per 10,000, respectively) than other hospitals.
Regionally, severe maternal morbidity was most common in the Northeast and the South, at 165 and 164 per 10,000, respectively, compared with rates of 132 and 116 in the West and Midwest, respectively.
Hospital deaths per 100,000 delivery hospitalizations were 248% higher for black than white women in 2006. By the end of 2015, that figure declined modestly to 193%, with absolute rates of 19 versus 5.5 deaths per 100,000 delivery hospitalizations for black versus white women in 2006. In 2015, the absolute rates were 11 versus 4 per 100,000.
The study was conducted by the Agency for Healthcare Research and Quality. There were no reported conflicts of interest.
SOURCE: Fingar K et al. Agency for Healthcare Research and Quality Statistical Brief #243.
The rate of severe maternal morbidity in the United States has climbed steadily since 2006, increasing 45% overall in the decade ending in 2015, according to a new report from the Agency for Healthcare Research and Quality that also found large ethnic and racial, geographic, and socioeconomic variation in rates of severe maternal morbidity.
The longstanding increased risk for severe maternal morbidity for black women, compared with white women, continued essentially unchanged, with black women 112%-115% more likely to experience any of 21 conditions and procedures that defined severe maternal morbidity in the report. Disparities also existed between white women and those of Hispanic or Asian/Pacific Islander origin, but those gaps are narrowing, according to the report.
“Black women, Hispanic women, and women of other races/ethnicities were overrepresented among deliveries involving severe maternal morbidity, as compared with white women,” wrote Kathryn Fingar, PhD, and her coauthors. “White women constituted a lower percentage of deliveries with any severe maternal morbidity than they did other deliveries” – 23% lower.
The 21 indicators, developed by the Centers for Disease Control and Prevention, range from conditions such as renal failure and sepsis to in-hospital procedures such as blood transfusion and hysterectomy. Women were considered to have severe maternal morbidity if any of the indicators were present, regardless of whether in-hospital death occurred.

Dr. Fingar of IBM Watson Health, Cambridge, Mass., and her collaborators summarized data from AHRQ’s Healthcare Cost and Utilization Project (H-CUP) in the statistical brief. The two most common procedures that indicate severe maternal morbidity are blood transfusion and hysterectomy, and these indicators were tracked in deliveries where women had a condition that served as one of the severe maternal morbidity indicators.
Dr. Fingar and her colleagues noted that they excluded data for the final quarter of 2015, because that is when the transition from the 9th to the 10th edition of the International Classifications of Diseases was made.
In addition to the overall increase from 101.3 to 146.6 women per 10,000 experiencing any severe maternal morbidity, the incidence of blood transfusion during a delivery hospitalization, either alone or in conjunction with other indicators, rose from 78.9 to 121.1 women per 10,000, an increase of 54%.
Showing that increased blood transfusions were a major driver of the jump in severe maternal morbidity, the composite increase in the rates of all other indicators went from 34 to 42 per delivery hospitalization, an increase of just 24%, or less than half the increase in blood transfusions.
There was significant variation in trends over time for the rates of the other indicators: acute renal failure, shock, the need for mechanical ventilation, and sepsis all increased by at least 100% (range, 104%-134%), and the rates of aneurysm increased by 99%. Rates of other indicators fell; pulmonary edema, embolism, eclampsia, myocardial infarction, cerebrovascular disorders, serious anesthesia complications, and intraoperative heart failure and arrest all declined by 25%-53% during the data-gathering period.
Looking at the data another way, 78% of cases of severe maternal morbidity in 2006 and 83% in 2015 involved a blood transfusion, making it the most common indicator. Far fewer delivery hospitalizations involved disseminated intravascular coagulation (DIC) and hysterectomy, the next most common indicators, which were seen in just 8% of cases.
Blood transfusions were most likely in women with shock (72%), amniotic fluid embolism (63%), sickle cell disease with crisis (54%), and DIC (51%).
One in three women who experienced shock during delivery had a hysterectomy, as did more than 20% of women who experienced adult respiratory distress syndrome or cardiac arrest (or ventricular fibrillation).
Women delivering at the youngest and oldest ends of the age spectrum were more likely to experience severe maternal morbidity. For women younger than 20 years of age, the rate was 206 per 10,000. In the group of women aged 40 years and over, the rate of any severe maternal morbidity was 248 per 10,000 delivery hospitalizations. Women in their 20s and 30s had rates of 136 and 143 per 10,000, respectively.
Besides race/ethnicity and age, a variety of other patient characteristics were associated with increased rates of severe maternal morbidity and mortality, with higher rates seen in women from the poorest quartile than the wealthiest (177 versus 122 per 10,000, respectively). Women with Medicaid were more likely than those with private insurance to experience severe maternal morbidity during a delivery hospitalization (175 versus 121 per 10,000, respectively).
Similarly, severe maternal morbidity was more common in safety net hospitals and in minority-serving hospitals (182 versus 128 and 176 versus 123 per 10,000, respectively) than other hospitals.
Regionally, severe maternal morbidity was most common in the Northeast and the South, at 165 and 164 per 10,000, respectively, compared with rates of 132 and 116 in the West and Midwest, respectively.
Hospital deaths per 100,000 delivery hospitalizations were 248% higher for black than white women in 2006. By the end of 2015, that figure declined modestly to 193%, with absolute rates of 19 versus 5.5 deaths per 100,000 delivery hospitalizations for black versus white women in 2006. In 2015, the absolute rates were 11 versus 4 per 100,000.
The study was conducted by the Agency for Healthcare Research and Quality. There were no reported conflicts of interest.
SOURCE: Fingar K et al. Agency for Healthcare Research and Quality Statistical Brief #243.
FROM AN AHRQ STATISTICAL BRIEF
Key clinical point:
Major finding: Black women were over 100% more likely to experience severe maternal morbidity, compared with white women.
Study details: Statistical analysis of Healthcare Cost and Utilization Project (H-CUP) data.
Disclosures: The study was funded by the Agency for Healthcare Research and Quality. The authors reported no conflicts of interest.
Source: Fingar K et al. Agency for Healthcare Research and Quality Statistical Brief #243.
Guidelines released for perimenopausal depression
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
FROM THE JOURNAL OF WOMEN’S HEALTH