User login
In adults with prediabetes, vitamin D cuts diabetes risk
Results of the analysis, led by Anastassios G. Pittas, MD, MS, with the division of endocrinology, diabetes, and metabolism at Tufts Medical Center, in Boston, were published online in Annals of Internal Medicine (2023 Feb 7. doi: 10.7326/M22-3018).
All three eligible trials included in the analysis were randomized, double blinded, and placebo controlled. The three eligible trials tested three oral formulations of Vitamin D: cholecalciferol, 20,000 IU (500 mcg) weekly; cholecalciferol, 4,000 IU (100 mcg) daily; or eldecalcitol, 0.75 mcg daily, against placebos.
The authors of the new paper found that vitamin D reduced the risk for diabetes in people with prediabetes by a statistically significant 15% in adjusted analyses. The 3-year absolute risk reduction was 3.3%.
They found no difference in the rate ratios for adverse events (kidney stones, 1.17, 95% confidence interval, 0.69-1.99; hypercalcemia, 2.34; 95% CI, 0.83-6.66]; hypercalciuria, 1.65; 95% CI, 0.83-3.28]; death, 0.85; 95% CI, 0.31-2.36]) when study participants got vitamin D instead of placebo.
Differences from previous analyses
The relationship between vitamin D levels and risk for type 2 diabetes has been studied in previous trials and results have been mixed.
The authors note that two previous meta-analyses included trials “that had relatively short durations for assessment of diabetes risk (for example, ≤ 1 year), had high risk of bias (for example, open-label trials), or were not specifically designed and conducted for primary prevention of type 2 diabetes, potentially undermining the validity of the results.”
Each of the trials in this meta-analysis had a low risk of bias as determined by the Cochrane risk-of-bias tool, Dr. Pittas and colleagues said.
“The present study does not reach an opposite conclusion from the D2d study,” said Dr. Pittas, who coauthored that paper as well. “Rather, it confirms the results of the D2d study. In D2d and two other similar vitamin D and diabetes prevention trials (one in Norway and one in Japan), vitamin D reduced the rate of progression to diabetes in adults with prediabetes, but the observed differences were not statistically significant because the reported relative risk reductions (10%-13%) were smaller than each trial was powered to detect (25%-36%).”
“Individual participant data meta-analyses increase the statistical power to detect an effect. After combining data, we found that vitamin D reduced the risk of progression from prediabetes to diabetes by 15% and this result was statistically significant. So, the conclusion of the meta-analysis is essentially the same conclusion as in D2d and the other two trials. The difference is that the result is now statistically significant,” Dr. Pittas added.
Small reduction but large population
The authors acknowledged that the absolute risk reduction number is small, especially when compared with the risk reduction seen with intensive lifestyle changes (58%) and metformin (31%), as reported in an article published in the New England of Journal of Medicine (2002 Feb 7;346:393-403). But “extrapolating to the more than 374 million adults worldwide who have prediabetes suggests that inexpensive vitamin D supplementation could delay the development of diabetes in more than 10 million people,” they said.
As for how high vitamin D levels need to be, the authors write that their research indicates that the optimal level of vitamin D in the blood needed to reduce diabetes risk may be higher than an Institute of Medicine committee recommendation in 2011.
“The blood 25-hydroxy vitamin D level needed to optimally reduce diabetes risk may be near and possibly above the range of 125-150 nmol/L (50-60 ng/mL) that the 2011 Institute of Medicine Committee to Review Dietary Reference Intakes for Calcium and Vitamin D provided as the range corresponding to the tolerable upper intake level (UL) of 4,000 IU/d for vitamin D,” the authors of the new paper said.
Editorialists urge caution
In an accompanying editorial also published in the Annals of Internal Medicine, Malachi J. McKenna, MD, with the department of clinical chemistry, at St. Vincent’s University Hospital, and Mary A.T. Flynn, PhD, RD, with the Food Safety Authority of Ireland in Dublin, urge caution regarding vitamin D dosing.
They write that there are important distinctions between vitamin D supplements and vitamin D therapy, and the potential harms of high-dose vitamin D are still unclear.
“Vitamin D supplementation of 10 to 20 mcg (400 to 800 IU) daily can be applied safely at the population level to prevent skeletal and possibly nonskeletal disease. Very-high-dose vitamin D therapy might prevent type 2 diabetes in some patients but may also cause harm,” they note.
Dr. Pittas said in an interview that there have been some studies with high-dose vitamin D (up to 500,000 IU a year in one study) that reported an increased fall risk in older adults who had high fall risk. “However, these findings are not generalizable to other populations that are younger and at low or average fall risk, such as the prediabetes population to which the results of this meta-analysis apply,” he noted.
“The benefit-to-risk ratio for vitamin D depends on the target population and medical condition,” Dr. Pittas said. “The editorial refers to the NAM (National Academy of Medicine) vitamin D guidelines for the general, healthy population to promote bone health. The guidelines should not be extrapolated to specific populations, for example [patients with] prediabetes,” where the vitamin D benefit-to-risk ratio would be different from that in the general population.
Dr. Pittas and colleagues caution that the people studied in this meta-analysis were at high risk for type 2 diabetes, so these results do not apply to the general healthy population. The results also should not be extrapolated to people at average risk for any type of diabetes, they add.
Several physicians either declined to comment or did not respond to requests for comment on this research.
Dr. Pittas reports the National Institutes of Health and the American Diabetes Association made payments to his institution to conduct Vitamin D-related research. He is an unpaid cochair of the Endocrine Society’s Evaluation, Treatment and Prevention of Vitamin D Deficiency Clinical Practice Guideline team.
Coauthor Dr. Jorde reports grants from Novo Nordisk Foundation, North Norwegian Regional Health Authorities, and the Research Council of Norway.
Dr. Dawson-Hughes reports she is on the DSMB for AgNovos Healthcare. AgNovos is developing a bone implant to reduce hip fracture risk and she gets a stipend from the company. She reports Helsinn Therapeutics provided anamorelin and matching placebo for an NIH-funded clinical trial.
Dr. Trikalinos was supported by the D2d study. He is a technical methodological consultant to Latham and Watkins, who is retained by Pacira Pharmaceuticals.
Dr. Angellotti has been employed by Takeda and owns stock in the company.
The editorialists report no relevant financial relationships.
Results of the analysis, led by Anastassios G. Pittas, MD, MS, with the division of endocrinology, diabetes, and metabolism at Tufts Medical Center, in Boston, were published online in Annals of Internal Medicine (2023 Feb 7. doi: 10.7326/M22-3018).
All three eligible trials included in the analysis were randomized, double blinded, and placebo controlled. The three eligible trials tested three oral formulations of Vitamin D: cholecalciferol, 20,000 IU (500 mcg) weekly; cholecalciferol, 4,000 IU (100 mcg) daily; or eldecalcitol, 0.75 mcg daily, against placebos.
The authors of the new paper found that vitamin D reduced the risk for diabetes in people with prediabetes by a statistically significant 15% in adjusted analyses. The 3-year absolute risk reduction was 3.3%.
They found no difference in the rate ratios for adverse events (kidney stones, 1.17, 95% confidence interval, 0.69-1.99; hypercalcemia, 2.34; 95% CI, 0.83-6.66]; hypercalciuria, 1.65; 95% CI, 0.83-3.28]; death, 0.85; 95% CI, 0.31-2.36]) when study participants got vitamin D instead of placebo.
Differences from previous analyses
The relationship between vitamin D levels and risk for type 2 diabetes has been studied in previous trials and results have been mixed.
The authors note that two previous meta-analyses included trials “that had relatively short durations for assessment of diabetes risk (for example, ≤ 1 year), had high risk of bias (for example, open-label trials), or were not specifically designed and conducted for primary prevention of type 2 diabetes, potentially undermining the validity of the results.”
Each of the trials in this meta-analysis had a low risk of bias as determined by the Cochrane risk-of-bias tool, Dr. Pittas and colleagues said.
“The present study does not reach an opposite conclusion from the D2d study,” said Dr. Pittas, who coauthored that paper as well. “Rather, it confirms the results of the D2d study. In D2d and two other similar vitamin D and diabetes prevention trials (one in Norway and one in Japan), vitamin D reduced the rate of progression to diabetes in adults with prediabetes, but the observed differences were not statistically significant because the reported relative risk reductions (10%-13%) were smaller than each trial was powered to detect (25%-36%).”
“Individual participant data meta-analyses increase the statistical power to detect an effect. After combining data, we found that vitamin D reduced the risk of progression from prediabetes to diabetes by 15% and this result was statistically significant. So, the conclusion of the meta-analysis is essentially the same conclusion as in D2d and the other two trials. The difference is that the result is now statistically significant,” Dr. Pittas added.
Small reduction but large population
The authors acknowledged that the absolute risk reduction number is small, especially when compared with the risk reduction seen with intensive lifestyle changes (58%) and metformin (31%), as reported in an article published in the New England of Journal of Medicine (2002 Feb 7;346:393-403). But “extrapolating to the more than 374 million adults worldwide who have prediabetes suggests that inexpensive vitamin D supplementation could delay the development of diabetes in more than 10 million people,” they said.
As for how high vitamin D levels need to be, the authors write that their research indicates that the optimal level of vitamin D in the blood needed to reduce diabetes risk may be higher than an Institute of Medicine committee recommendation in 2011.
“The blood 25-hydroxy vitamin D level needed to optimally reduce diabetes risk may be near and possibly above the range of 125-150 nmol/L (50-60 ng/mL) that the 2011 Institute of Medicine Committee to Review Dietary Reference Intakes for Calcium and Vitamin D provided as the range corresponding to the tolerable upper intake level (UL) of 4,000 IU/d for vitamin D,” the authors of the new paper said.
Editorialists urge caution
In an accompanying editorial also published in the Annals of Internal Medicine, Malachi J. McKenna, MD, with the department of clinical chemistry, at St. Vincent’s University Hospital, and Mary A.T. Flynn, PhD, RD, with the Food Safety Authority of Ireland in Dublin, urge caution regarding vitamin D dosing.
They write that there are important distinctions between vitamin D supplements and vitamin D therapy, and the potential harms of high-dose vitamin D are still unclear.
“Vitamin D supplementation of 10 to 20 mcg (400 to 800 IU) daily can be applied safely at the population level to prevent skeletal and possibly nonskeletal disease. Very-high-dose vitamin D therapy might prevent type 2 diabetes in some patients but may also cause harm,” they note.
Dr. Pittas said in an interview that there have been some studies with high-dose vitamin D (up to 500,000 IU a year in one study) that reported an increased fall risk in older adults who had high fall risk. “However, these findings are not generalizable to other populations that are younger and at low or average fall risk, such as the prediabetes population to which the results of this meta-analysis apply,” he noted.
“The benefit-to-risk ratio for vitamin D depends on the target population and medical condition,” Dr. Pittas said. “The editorial refers to the NAM (National Academy of Medicine) vitamin D guidelines for the general, healthy population to promote bone health. The guidelines should not be extrapolated to specific populations, for example [patients with] prediabetes,” where the vitamin D benefit-to-risk ratio would be different from that in the general population.
Dr. Pittas and colleagues caution that the people studied in this meta-analysis were at high risk for type 2 diabetes, so these results do not apply to the general healthy population. The results also should not be extrapolated to people at average risk for any type of diabetes, they add.
Several physicians either declined to comment or did not respond to requests for comment on this research.
Dr. Pittas reports the National Institutes of Health and the American Diabetes Association made payments to his institution to conduct Vitamin D-related research. He is an unpaid cochair of the Endocrine Society’s Evaluation, Treatment and Prevention of Vitamin D Deficiency Clinical Practice Guideline team.
Coauthor Dr. Jorde reports grants from Novo Nordisk Foundation, North Norwegian Regional Health Authorities, and the Research Council of Norway.
Dr. Dawson-Hughes reports she is on the DSMB for AgNovos Healthcare. AgNovos is developing a bone implant to reduce hip fracture risk and she gets a stipend from the company. She reports Helsinn Therapeutics provided anamorelin and matching placebo for an NIH-funded clinical trial.
Dr. Trikalinos was supported by the D2d study. He is a technical methodological consultant to Latham and Watkins, who is retained by Pacira Pharmaceuticals.
Dr. Angellotti has been employed by Takeda and owns stock in the company.
The editorialists report no relevant financial relationships.
Results of the analysis, led by Anastassios G. Pittas, MD, MS, with the division of endocrinology, diabetes, and metabolism at Tufts Medical Center, in Boston, were published online in Annals of Internal Medicine (2023 Feb 7. doi: 10.7326/M22-3018).
All three eligible trials included in the analysis were randomized, double blinded, and placebo controlled. The three eligible trials tested three oral formulations of Vitamin D: cholecalciferol, 20,000 IU (500 mcg) weekly; cholecalciferol, 4,000 IU (100 mcg) daily; or eldecalcitol, 0.75 mcg daily, against placebos.
The authors of the new paper found that vitamin D reduced the risk for diabetes in people with prediabetes by a statistically significant 15% in adjusted analyses. The 3-year absolute risk reduction was 3.3%.
They found no difference in the rate ratios for adverse events (kidney stones, 1.17, 95% confidence interval, 0.69-1.99; hypercalcemia, 2.34; 95% CI, 0.83-6.66]; hypercalciuria, 1.65; 95% CI, 0.83-3.28]; death, 0.85; 95% CI, 0.31-2.36]) when study participants got vitamin D instead of placebo.
Differences from previous analyses
The relationship between vitamin D levels and risk for type 2 diabetes has been studied in previous trials and results have been mixed.
The authors note that two previous meta-analyses included trials “that had relatively short durations for assessment of diabetes risk (for example, ≤ 1 year), had high risk of bias (for example, open-label trials), or were not specifically designed and conducted for primary prevention of type 2 diabetes, potentially undermining the validity of the results.”
Each of the trials in this meta-analysis had a low risk of bias as determined by the Cochrane risk-of-bias tool, Dr. Pittas and colleagues said.
“The present study does not reach an opposite conclusion from the D2d study,” said Dr. Pittas, who coauthored that paper as well. “Rather, it confirms the results of the D2d study. In D2d and two other similar vitamin D and diabetes prevention trials (one in Norway and one in Japan), vitamin D reduced the rate of progression to diabetes in adults with prediabetes, but the observed differences were not statistically significant because the reported relative risk reductions (10%-13%) were smaller than each trial was powered to detect (25%-36%).”
“Individual participant data meta-analyses increase the statistical power to detect an effect. After combining data, we found that vitamin D reduced the risk of progression from prediabetes to diabetes by 15% and this result was statistically significant. So, the conclusion of the meta-analysis is essentially the same conclusion as in D2d and the other two trials. The difference is that the result is now statistically significant,” Dr. Pittas added.
Small reduction but large population
The authors acknowledged that the absolute risk reduction number is small, especially when compared with the risk reduction seen with intensive lifestyle changes (58%) and metformin (31%), as reported in an article published in the New England of Journal of Medicine (2002 Feb 7;346:393-403). But “extrapolating to the more than 374 million adults worldwide who have prediabetes suggests that inexpensive vitamin D supplementation could delay the development of diabetes in more than 10 million people,” they said.
As for how high vitamin D levels need to be, the authors write that their research indicates that the optimal level of vitamin D in the blood needed to reduce diabetes risk may be higher than an Institute of Medicine committee recommendation in 2011.
“The blood 25-hydroxy vitamin D level needed to optimally reduce diabetes risk may be near and possibly above the range of 125-150 nmol/L (50-60 ng/mL) that the 2011 Institute of Medicine Committee to Review Dietary Reference Intakes for Calcium and Vitamin D provided as the range corresponding to the tolerable upper intake level (UL) of 4,000 IU/d for vitamin D,” the authors of the new paper said.
Editorialists urge caution
In an accompanying editorial also published in the Annals of Internal Medicine, Malachi J. McKenna, MD, with the department of clinical chemistry, at St. Vincent’s University Hospital, and Mary A.T. Flynn, PhD, RD, with the Food Safety Authority of Ireland in Dublin, urge caution regarding vitamin D dosing.
They write that there are important distinctions between vitamin D supplements and vitamin D therapy, and the potential harms of high-dose vitamin D are still unclear.
“Vitamin D supplementation of 10 to 20 mcg (400 to 800 IU) daily can be applied safely at the population level to prevent skeletal and possibly nonskeletal disease. Very-high-dose vitamin D therapy might prevent type 2 diabetes in some patients but may also cause harm,” they note.
Dr. Pittas said in an interview that there have been some studies with high-dose vitamin D (up to 500,000 IU a year in one study) that reported an increased fall risk in older adults who had high fall risk. “However, these findings are not generalizable to other populations that are younger and at low or average fall risk, such as the prediabetes population to which the results of this meta-analysis apply,” he noted.
“The benefit-to-risk ratio for vitamin D depends on the target population and medical condition,” Dr. Pittas said. “The editorial refers to the NAM (National Academy of Medicine) vitamin D guidelines for the general, healthy population to promote bone health. The guidelines should not be extrapolated to specific populations, for example [patients with] prediabetes,” where the vitamin D benefit-to-risk ratio would be different from that in the general population.
Dr. Pittas and colleagues caution that the people studied in this meta-analysis were at high risk for type 2 diabetes, so these results do not apply to the general healthy population. The results also should not be extrapolated to people at average risk for any type of diabetes, they add.
Several physicians either declined to comment or did not respond to requests for comment on this research.
Dr. Pittas reports the National Institutes of Health and the American Diabetes Association made payments to his institution to conduct Vitamin D-related research. He is an unpaid cochair of the Endocrine Society’s Evaluation, Treatment and Prevention of Vitamin D Deficiency Clinical Practice Guideline team.
Coauthor Dr. Jorde reports grants from Novo Nordisk Foundation, North Norwegian Regional Health Authorities, and the Research Council of Norway.
Dr. Dawson-Hughes reports she is on the DSMB for AgNovos Healthcare. AgNovos is developing a bone implant to reduce hip fracture risk and she gets a stipend from the company. She reports Helsinn Therapeutics provided anamorelin and matching placebo for an NIH-funded clinical trial.
Dr. Trikalinos was supported by the D2d study. He is a technical methodological consultant to Latham and Watkins, who is retained by Pacira Pharmaceuticals.
Dr. Angellotti has been employed by Takeda and owns stock in the company.
The editorialists report no relevant financial relationships.
FROM ANNALS OF INTERNAL MEDICINE
‘Ozempic face’: Accepting wrinkles for improved health
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.
Longer diabetes duration links with increased heart failure
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Healthy habits lower T2D microvascular risks: Cohort study
People with diabetes who adhere to a healthy diet, exercise regularly, and follow other healthy lifestyle practices have a significantly lower risk of microvascular complications from the disease, such as diabetic neuropathy, retinopathy, and nephropathy, as well as foot disorders, than counterparts with diabetes who don’t, a prospective cohort study of more than 7,000 patients with type 2 diabetes has found.
“We believe this is one of the first large-scale analyses among diabetes patients that specifically examined an overall healthy lifestyle in relation to the risk of developing microvascular complications,” senior study author Qi Sun, MD, ScD, said in an interview. “The results are not surprising that the healthy lifestyle is associated with lower risk of developing these complications and the enhanced adherence to the healthy lifestyle is associated with lower risk as well. And these findings bear lots of public health significance as they suggest the important role of living a healthy lifestyle in the prevention of diabetes complications, on top of the clinical treatment.”
Dr. Sun is an associate professor of nutrition and epidemiology at the Harvard T.H. Chan School of Public Health, Boston.
The study stated that the findings “lend support” for the American Diabetes Association guidelines for healthy lifestyle practices in people with diabetes.
The study used a cohort from two large prospective cohort studies, the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS), comprising 4,982 women and 2,095 men who were diagnosed with type 2 diabetes during follow-up. They had no cardiovascular disease or cancer at the time of their diabetes diagnosis. Both NHS and HPFS used validated questionnaires to gather information on diet, lifestyle, medical history, and newly diagnosed diseases every 2-4 years. The latter study included NHS and HPFS participants who also completed supplementary questionnaires about their diabetes.
The latest study took into account five modifiable lifestyle-related factors: diet, body weight, smoking status, alcohol, and physical activity. For diet, both large studies used the 2010 Alternate Healthy Eating Index to assess diet quality; those in the upper 40th percentile of the study population were defined as healthy diet. Healthy body weight was defined at a body mass index of 18.5-25 kg/m2.
Among the latter study cohort, 2,878 incident cases of diabetic microvascular complications were documented during follow-up. Patients who adhered to a healthy lifestyle before their diabetes diagnosis, defined as having four or more low-risk lifestyle factors, had a 27% lower relative risk of developing any microvascular complication than counterparts with no low-risk lifestyle factors (relative risk, 0.73; 95% confidence interval, 0.35-1; P = .006).
The study found similar outcomes for those who adopted a healthy lifestyle after their diabetes diagnosis, with a 32% reduction in relative risk compared with those who didn’t adopt any healthy lifestyle practices (RR, 0.68; 95% CI, 0.55-0.83; P < .001).
Dr. Sun noted what was noteworthy about his group’s cohort study. “The unique design is truly the prospective follow-up over time so that we could examine the lifestyle at diabetes diagnosis as well as changes in lifestyle before and after diabetes in relation to the future risk of developing the complications,” he said.
A randomized trial would be a more rigorous way to evaluate the impact of a healthy lifestyle, he added, “although it’s much more expensive than a cohort study like what we did with this investigation.”
As for future research, Dr. Sun said, “It will be interesting to understand mechanisms underlying these observations. It’s also critical to understand why certain diabetes patients may not benefit from a healthy lifestyle, since some of them, even when living a healthy lifestyle, still develop the complications.”
This trial shows in a new light the benefits of healthy lifestyle practices on microvascular complications of type 2 diabetes, Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., and a professor at the University of Miami, said in a comment. “These benefits have always been surmised and demonstrated in a limited way in previous trials, but not subject to the level of analysis seen in this prospective cohort trial.”
He called the study design “excellent,” adding, “ ‘Validated’ self-reported questionnaires were used widely, although minimal detail is provided about the validation process.” One limitation, he noted, was “the homogeneity of the participants; all were health professionals.”
The study “affirms” and “quantitates” the benefits of a healthy lifestyle in type 2 diabetes. “The issue is not unawareness but rather application,” Dr. Jellinger said. “Modifying long-held lifestyle habits is a real challenge. Perhaps by ‘quantitating’ the benefit, as shown in this trial and hopefully additional studies, impetus will be provided to refocus on this approach, which is too often simply given lip service.”
The National Institutes of Health provided funding for the study. Dr. Sun has no relevant disclosures. Dr. Jellinger disclosed relationships with Amgen and Esperion.
People with diabetes who adhere to a healthy diet, exercise regularly, and follow other healthy lifestyle practices have a significantly lower risk of microvascular complications from the disease, such as diabetic neuropathy, retinopathy, and nephropathy, as well as foot disorders, than counterparts with diabetes who don’t, a prospective cohort study of more than 7,000 patients with type 2 diabetes has found.
“We believe this is one of the first large-scale analyses among diabetes patients that specifically examined an overall healthy lifestyle in relation to the risk of developing microvascular complications,” senior study author Qi Sun, MD, ScD, said in an interview. “The results are not surprising that the healthy lifestyle is associated with lower risk of developing these complications and the enhanced adherence to the healthy lifestyle is associated with lower risk as well. And these findings bear lots of public health significance as they suggest the important role of living a healthy lifestyle in the prevention of diabetes complications, on top of the clinical treatment.”
Dr. Sun is an associate professor of nutrition and epidemiology at the Harvard T.H. Chan School of Public Health, Boston.
The study stated that the findings “lend support” for the American Diabetes Association guidelines for healthy lifestyle practices in people with diabetes.
The study used a cohort from two large prospective cohort studies, the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS), comprising 4,982 women and 2,095 men who were diagnosed with type 2 diabetes during follow-up. They had no cardiovascular disease or cancer at the time of their diabetes diagnosis. Both NHS and HPFS used validated questionnaires to gather information on diet, lifestyle, medical history, and newly diagnosed diseases every 2-4 years. The latter study included NHS and HPFS participants who also completed supplementary questionnaires about their diabetes.
The latest study took into account five modifiable lifestyle-related factors: diet, body weight, smoking status, alcohol, and physical activity. For diet, both large studies used the 2010 Alternate Healthy Eating Index to assess diet quality; those in the upper 40th percentile of the study population were defined as healthy diet. Healthy body weight was defined at a body mass index of 18.5-25 kg/m2.
Among the latter study cohort, 2,878 incident cases of diabetic microvascular complications were documented during follow-up. Patients who adhered to a healthy lifestyle before their diabetes diagnosis, defined as having four or more low-risk lifestyle factors, had a 27% lower relative risk of developing any microvascular complication than counterparts with no low-risk lifestyle factors (relative risk, 0.73; 95% confidence interval, 0.35-1; P = .006).
The study found similar outcomes for those who adopted a healthy lifestyle after their diabetes diagnosis, with a 32% reduction in relative risk compared with those who didn’t adopt any healthy lifestyle practices (RR, 0.68; 95% CI, 0.55-0.83; P < .001).
Dr. Sun noted what was noteworthy about his group’s cohort study. “The unique design is truly the prospective follow-up over time so that we could examine the lifestyle at diabetes diagnosis as well as changes in lifestyle before and after diabetes in relation to the future risk of developing the complications,” he said.
A randomized trial would be a more rigorous way to evaluate the impact of a healthy lifestyle, he added, “although it’s much more expensive than a cohort study like what we did with this investigation.”
As for future research, Dr. Sun said, “It will be interesting to understand mechanisms underlying these observations. It’s also critical to understand why certain diabetes patients may not benefit from a healthy lifestyle, since some of them, even when living a healthy lifestyle, still develop the complications.”
This trial shows in a new light the benefits of healthy lifestyle practices on microvascular complications of type 2 diabetes, Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., and a professor at the University of Miami, said in a comment. “These benefits have always been surmised and demonstrated in a limited way in previous trials, but not subject to the level of analysis seen in this prospective cohort trial.”
He called the study design “excellent,” adding, “ ‘Validated’ self-reported questionnaires were used widely, although minimal detail is provided about the validation process.” One limitation, he noted, was “the homogeneity of the participants; all were health professionals.”
The study “affirms” and “quantitates” the benefits of a healthy lifestyle in type 2 diabetes. “The issue is not unawareness but rather application,” Dr. Jellinger said. “Modifying long-held lifestyle habits is a real challenge. Perhaps by ‘quantitating’ the benefit, as shown in this trial and hopefully additional studies, impetus will be provided to refocus on this approach, which is too often simply given lip service.”
The National Institutes of Health provided funding for the study. Dr. Sun has no relevant disclosures. Dr. Jellinger disclosed relationships with Amgen and Esperion.
People with diabetes who adhere to a healthy diet, exercise regularly, and follow other healthy lifestyle practices have a significantly lower risk of microvascular complications from the disease, such as diabetic neuropathy, retinopathy, and nephropathy, as well as foot disorders, than counterparts with diabetes who don’t, a prospective cohort study of more than 7,000 patients with type 2 diabetes has found.
“We believe this is one of the first large-scale analyses among diabetes patients that specifically examined an overall healthy lifestyle in relation to the risk of developing microvascular complications,” senior study author Qi Sun, MD, ScD, said in an interview. “The results are not surprising that the healthy lifestyle is associated with lower risk of developing these complications and the enhanced adherence to the healthy lifestyle is associated with lower risk as well. And these findings bear lots of public health significance as they suggest the important role of living a healthy lifestyle in the prevention of diabetes complications, on top of the clinical treatment.”
Dr. Sun is an associate professor of nutrition and epidemiology at the Harvard T.H. Chan School of Public Health, Boston.
The study stated that the findings “lend support” for the American Diabetes Association guidelines for healthy lifestyle practices in people with diabetes.
The study used a cohort from two large prospective cohort studies, the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS), comprising 4,982 women and 2,095 men who were diagnosed with type 2 diabetes during follow-up. They had no cardiovascular disease or cancer at the time of their diabetes diagnosis. Both NHS and HPFS used validated questionnaires to gather information on diet, lifestyle, medical history, and newly diagnosed diseases every 2-4 years. The latter study included NHS and HPFS participants who also completed supplementary questionnaires about their diabetes.
The latest study took into account five modifiable lifestyle-related factors: diet, body weight, smoking status, alcohol, and physical activity. For diet, both large studies used the 2010 Alternate Healthy Eating Index to assess diet quality; those in the upper 40th percentile of the study population were defined as healthy diet. Healthy body weight was defined at a body mass index of 18.5-25 kg/m2.
Among the latter study cohort, 2,878 incident cases of diabetic microvascular complications were documented during follow-up. Patients who adhered to a healthy lifestyle before their diabetes diagnosis, defined as having four or more low-risk lifestyle factors, had a 27% lower relative risk of developing any microvascular complication than counterparts with no low-risk lifestyle factors (relative risk, 0.73; 95% confidence interval, 0.35-1; P = .006).
The study found similar outcomes for those who adopted a healthy lifestyle after their diabetes diagnosis, with a 32% reduction in relative risk compared with those who didn’t adopt any healthy lifestyle practices (RR, 0.68; 95% CI, 0.55-0.83; P < .001).
Dr. Sun noted what was noteworthy about his group’s cohort study. “The unique design is truly the prospective follow-up over time so that we could examine the lifestyle at diabetes diagnosis as well as changes in lifestyle before and after diabetes in relation to the future risk of developing the complications,” he said.
A randomized trial would be a more rigorous way to evaluate the impact of a healthy lifestyle, he added, “although it’s much more expensive than a cohort study like what we did with this investigation.”
As for future research, Dr. Sun said, “It will be interesting to understand mechanisms underlying these observations. It’s also critical to understand why certain diabetes patients may not benefit from a healthy lifestyle, since some of them, even when living a healthy lifestyle, still develop the complications.”
This trial shows in a new light the benefits of healthy lifestyle practices on microvascular complications of type 2 diabetes, Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., and a professor at the University of Miami, said in a comment. “These benefits have always been surmised and demonstrated in a limited way in previous trials, but not subject to the level of analysis seen in this prospective cohort trial.”
He called the study design “excellent,” adding, “ ‘Validated’ self-reported questionnaires were used widely, although minimal detail is provided about the validation process.” One limitation, he noted, was “the homogeneity of the participants; all were health professionals.”
The study “affirms” and “quantitates” the benefits of a healthy lifestyle in type 2 diabetes. “The issue is not unawareness but rather application,” Dr. Jellinger said. “Modifying long-held lifestyle habits is a real challenge. Perhaps by ‘quantitating’ the benefit, as shown in this trial and hopefully additional studies, impetus will be provided to refocus on this approach, which is too often simply given lip service.”
The National Institutes of Health provided funding for the study. Dr. Sun has no relevant disclosures. Dr. Jellinger disclosed relationships with Amgen and Esperion.
FROM JAMA NETWORK OPEN
More type 2 diabetes deaths from cancer than heart disease
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
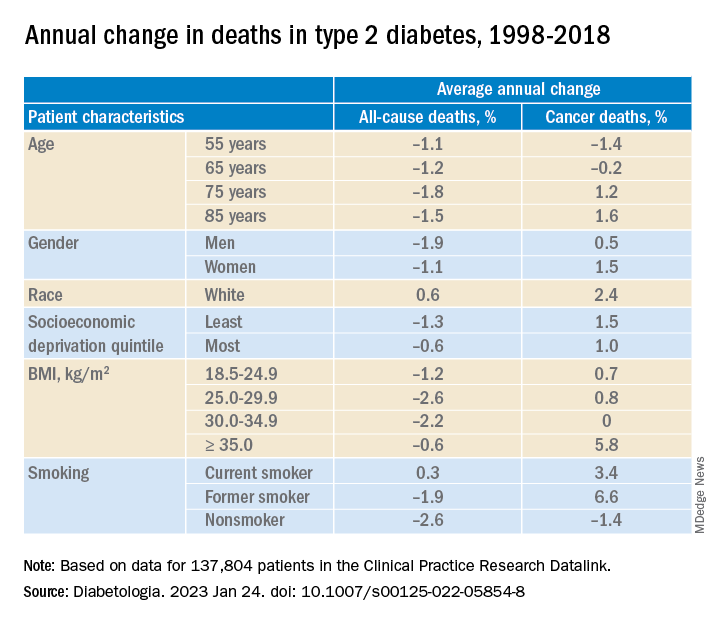
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
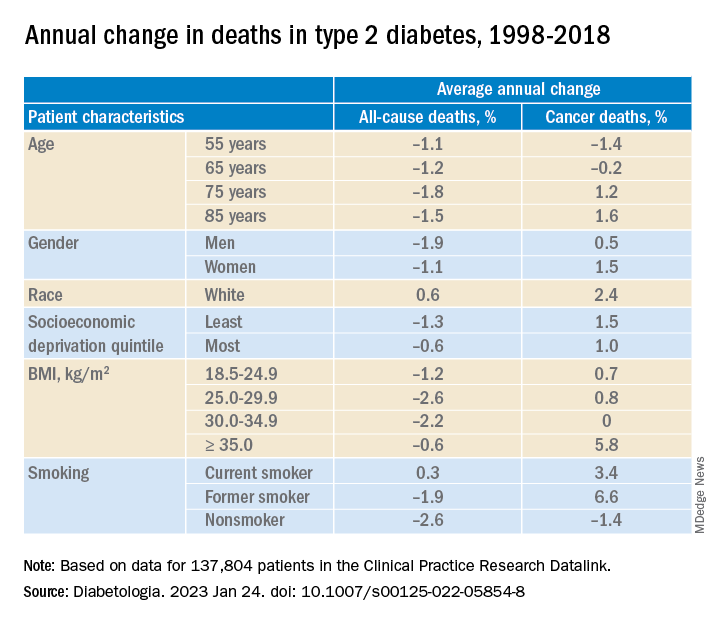
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
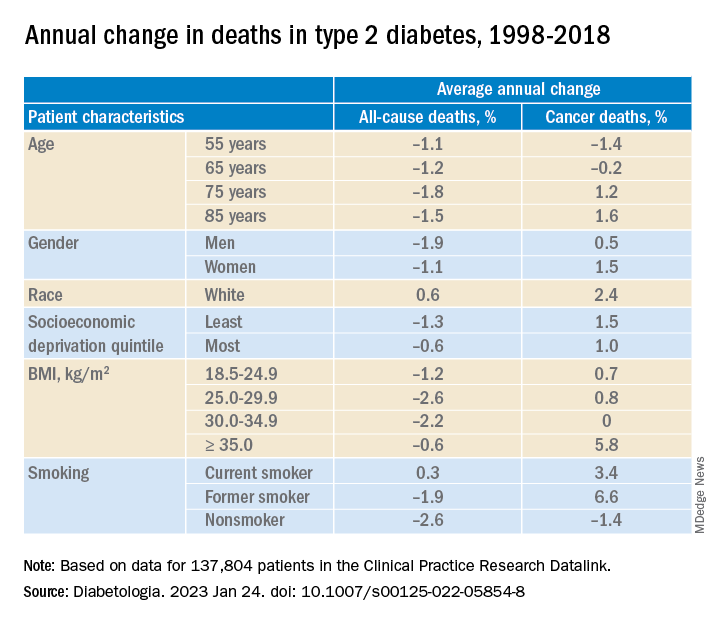
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DIABETOLOGIA
Eye check important before starting semaglutide for diabetes
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
FROM DIABETES & METABOLIC SYNDROME: CLINICAL RESEARCH & REVIEWS
EMR screening in emergency department tags undiagnosed diabetes
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
FROM JAMA NETWORK OPEN
High-deductible health plans detrimental for those with diabetes
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
FDA approves new type 2 diabetes drug bexagliflozin
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
Nitrite food additives may increase risk of type 2 diabetes
Consuming a large amount of nitrites from food additives versus none was associated with a greater risk of developing type 2 diabetes in the NutriNet-Santé study in France, researchers report.
However, a few experts who were not involved with this research question the strength of the findings because of study limitations.
The study involved more than 100,000 adults with a mean age of 43, and 79% were women.
Individuals with the highest intakes of nitrites from food additives (top third) had a 53% higher risk of developing type 2 diabetes during a median follow-up of 7 years compared with those with the lowest intake of this food additive after controlling for intake of sugars, red and processed meats, heme iron, salt, and saturated fatty acids. Consumption of nitrates from food additives was not associated with risk of type 2 diabetes.
“Our findings suggest a direct association between additives-originated nitrites and [type 2 diabetes] risk and corroborate previously suggested associations between total dietary nitrites and [type 2 diabetes],” the researchers report in an article published online in PLoS Medicine.
However, “as this is the first large-scale study finding these associations, these results need to be replicated in other large-scale cohorts,” senior author Mathilde Touvier, PhD, head of the Nutritional Epidemiology Research Team (EREN-CRESS), INSERM, INRAE, Sorbonne Paris Nord University, and lead author Bernard Srour, PhD, PharmD, a scientist at the same institution, said in a joint email to this news organization.
Short-term intervention studies to determine insulin resistance could also be tested, they add.
In the meantime, “this study adds further evidence to the existing strong link between nitrites and colorectal cancer risk, and supports the importance of further regulation of nitrites as food additives and nitrogen fertilizers,” they say.
According to Dr. Touvier and Dr. Srour, the takeaway message for clinicians is the finding that nitrites from food additives are associated with type 2 diabetes, “support existing guidelines recommending [limiting] the consumption of processed meats to prevent chronic diseases. However, the consumption of vegetables should be encouraged as they contain several beneficial compounds and contribute to chronic disease prevention.”
Some experts are skeptical
But three experts who were not involved with the research were skeptical about the conclusions, in comments made to the U.K. Science Media Centre.
“The fundamental weakness of this study is how the food additive intake was assessed,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London. “Estimates of intake were based on recalls of dietary intake on two separate occasions at the beginning of the study with no further estimates in the follow-up period of over 7 years,” he noted.
Other limitations include the relatively young age of the cohort and relatively low incidence of new cases of type 2 diabetes (about 1% of the study population over 7 years).
Moreover, the level of nitrite food additive ingestion is much lower than the acceptable daily intake. The findings would need to be replicated with appropriate adjustment for differences in body weight.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, said that “the study does not support the claim in the press release and paper that food additives are responsible for the increased risk.”
He pointed out that “nitrite from additives contributes only about 4%-6% of total nitrite intake in the population, and it is not clear why this should have a stronger impact on risk than nitrite from other sources,” such as nitrate found in food and water.
Duane Mellor, PhD, registered dietitian and senior lecturer, Aston University, Birmingham, England, said: “It could be questioned how accurate estimating intakes of individual additives like sodium nitrite, which was less than 1 mg per day from a record of just 2 days food intake per year, as it assumes people ate the same the other 363 days of the year.”
Moreover, “it is perhaps worth noting that the use of nitrites as an additive is often as sodium nitrite, which is used to cure meats like bacon, which if someone is seeking to reduce their risk of type 2 diabetes would be something people would be encouraged to eat less of [anyway].”
“The best way to reduce your risk of developing type 2 diabetes,” he said, “is to be physically active, maintain a healthy weight for you, and eat a varied diet based on vegetables, pulses, nuts, seeds, and fruit along with wholegrain and moderate intakes of dairy foods and meat (especially processed meats).”
Study details
Nitrites and nitrates are used as food additives to prevent bacterial growth, mainly in processed meats, and they are also found in foods (mainly green leafy vegetables) and water (nitrates from the use of nitrogen fertilizer can enter the water supply).
The researchers analyzed data from 104,168 participants in NutriNet-Santé who had no diabetes at baseline and who completed 24-hour dietary intake records. They investigated the association between exposure to nitrites and nitrates (in food and water or in additives) and incident type 2 diabetes.
Most nitrites came from food (95.3%), and less often from food additives (4.7%) and water (< 0.01%). The nitrites in foods were mainly from vegetables (60%) and seasonings (23%).
Most nitrates also came from food (93%), followed by water (6.9%) and food additives (0.1%). The nitrates in foods were mainly from vegetables (41%), processed meat (19%), and meat (17%).
During a median follow-up of 7.3 years, there were 969 incident cases of type 2 diabetes.
Compared with individuals in the lowest third of nitrites from food and water, those in the highest tertile had a 27% higher risk of incident type 2 diabetes, after adjusting for multiple variables (hazard ratio, 1.27; P = .009).
The risk of type 2 diabetes associated with the highest intake of nitrites from additives was as previously described, 53% higher, than that for those with the lowest intake.
There was no evidence of an association between nitrates and risk of type 2 diabetes.
The researchers acknowledge that study limitations include potential errors in assessment of nitrate and nitrate exposure, potential selection bias (participants in the web-based study may have had healthier behaviors than the general population), and potential unaccounted confounders (because it was an observational study).
A version of this article first appeared on Medscape.com.
Consuming a large amount of nitrites from food additives versus none was associated with a greater risk of developing type 2 diabetes in the NutriNet-Santé study in France, researchers report.
However, a few experts who were not involved with this research question the strength of the findings because of study limitations.
The study involved more than 100,000 adults with a mean age of 43, and 79% were women.
Individuals with the highest intakes of nitrites from food additives (top third) had a 53% higher risk of developing type 2 diabetes during a median follow-up of 7 years compared with those with the lowest intake of this food additive after controlling for intake of sugars, red and processed meats, heme iron, salt, and saturated fatty acids. Consumption of nitrates from food additives was not associated with risk of type 2 diabetes.
“Our findings suggest a direct association between additives-originated nitrites and [type 2 diabetes] risk and corroborate previously suggested associations between total dietary nitrites and [type 2 diabetes],” the researchers report in an article published online in PLoS Medicine.
However, “as this is the first large-scale study finding these associations, these results need to be replicated in other large-scale cohorts,” senior author Mathilde Touvier, PhD, head of the Nutritional Epidemiology Research Team (EREN-CRESS), INSERM, INRAE, Sorbonne Paris Nord University, and lead author Bernard Srour, PhD, PharmD, a scientist at the same institution, said in a joint email to this news organization.
Short-term intervention studies to determine insulin resistance could also be tested, they add.
In the meantime, “this study adds further evidence to the existing strong link between nitrites and colorectal cancer risk, and supports the importance of further regulation of nitrites as food additives and nitrogen fertilizers,” they say.
According to Dr. Touvier and Dr. Srour, the takeaway message for clinicians is the finding that nitrites from food additives are associated with type 2 diabetes, “support existing guidelines recommending [limiting] the consumption of processed meats to prevent chronic diseases. However, the consumption of vegetables should be encouraged as they contain several beneficial compounds and contribute to chronic disease prevention.”
Some experts are skeptical
But three experts who were not involved with the research were skeptical about the conclusions, in comments made to the U.K. Science Media Centre.
“The fundamental weakness of this study is how the food additive intake was assessed,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London. “Estimates of intake were based on recalls of dietary intake on two separate occasions at the beginning of the study with no further estimates in the follow-up period of over 7 years,” he noted.
Other limitations include the relatively young age of the cohort and relatively low incidence of new cases of type 2 diabetes (about 1% of the study population over 7 years).
Moreover, the level of nitrite food additive ingestion is much lower than the acceptable daily intake. The findings would need to be replicated with appropriate adjustment for differences in body weight.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, said that “the study does not support the claim in the press release and paper that food additives are responsible for the increased risk.”
He pointed out that “nitrite from additives contributes only about 4%-6% of total nitrite intake in the population, and it is not clear why this should have a stronger impact on risk than nitrite from other sources,” such as nitrate found in food and water.
Duane Mellor, PhD, registered dietitian and senior lecturer, Aston University, Birmingham, England, said: “It could be questioned how accurate estimating intakes of individual additives like sodium nitrite, which was less than 1 mg per day from a record of just 2 days food intake per year, as it assumes people ate the same the other 363 days of the year.”
Moreover, “it is perhaps worth noting that the use of nitrites as an additive is often as sodium nitrite, which is used to cure meats like bacon, which if someone is seeking to reduce their risk of type 2 diabetes would be something people would be encouraged to eat less of [anyway].”
“The best way to reduce your risk of developing type 2 diabetes,” he said, “is to be physically active, maintain a healthy weight for you, and eat a varied diet based on vegetables, pulses, nuts, seeds, and fruit along with wholegrain and moderate intakes of dairy foods and meat (especially processed meats).”
Study details
Nitrites and nitrates are used as food additives to prevent bacterial growth, mainly in processed meats, and they are also found in foods (mainly green leafy vegetables) and water (nitrates from the use of nitrogen fertilizer can enter the water supply).
The researchers analyzed data from 104,168 participants in NutriNet-Santé who had no diabetes at baseline and who completed 24-hour dietary intake records. They investigated the association between exposure to nitrites and nitrates (in food and water or in additives) and incident type 2 diabetes.
Most nitrites came from food (95.3%), and less often from food additives (4.7%) and water (< 0.01%). The nitrites in foods were mainly from vegetables (60%) and seasonings (23%).
Most nitrates also came from food (93%), followed by water (6.9%) and food additives (0.1%). The nitrates in foods were mainly from vegetables (41%), processed meat (19%), and meat (17%).
During a median follow-up of 7.3 years, there were 969 incident cases of type 2 diabetes.
Compared with individuals in the lowest third of nitrites from food and water, those in the highest tertile had a 27% higher risk of incident type 2 diabetes, after adjusting for multiple variables (hazard ratio, 1.27; P = .009).
The risk of type 2 diabetes associated with the highest intake of nitrites from additives was as previously described, 53% higher, than that for those with the lowest intake.
There was no evidence of an association between nitrates and risk of type 2 diabetes.
The researchers acknowledge that study limitations include potential errors in assessment of nitrate and nitrate exposure, potential selection bias (participants in the web-based study may have had healthier behaviors than the general population), and potential unaccounted confounders (because it was an observational study).
A version of this article first appeared on Medscape.com.
Consuming a large amount of nitrites from food additives versus none was associated with a greater risk of developing type 2 diabetes in the NutriNet-Santé study in France, researchers report.
However, a few experts who were not involved with this research question the strength of the findings because of study limitations.
The study involved more than 100,000 adults with a mean age of 43, and 79% were women.
Individuals with the highest intakes of nitrites from food additives (top third) had a 53% higher risk of developing type 2 diabetes during a median follow-up of 7 years compared with those with the lowest intake of this food additive after controlling for intake of sugars, red and processed meats, heme iron, salt, and saturated fatty acids. Consumption of nitrates from food additives was not associated with risk of type 2 diabetes.
“Our findings suggest a direct association between additives-originated nitrites and [type 2 diabetes] risk and corroborate previously suggested associations between total dietary nitrites and [type 2 diabetes],” the researchers report in an article published online in PLoS Medicine.
However, “as this is the first large-scale study finding these associations, these results need to be replicated in other large-scale cohorts,” senior author Mathilde Touvier, PhD, head of the Nutritional Epidemiology Research Team (EREN-CRESS), INSERM, INRAE, Sorbonne Paris Nord University, and lead author Bernard Srour, PhD, PharmD, a scientist at the same institution, said in a joint email to this news organization.
Short-term intervention studies to determine insulin resistance could also be tested, they add.
In the meantime, “this study adds further evidence to the existing strong link between nitrites and colorectal cancer risk, and supports the importance of further regulation of nitrites as food additives and nitrogen fertilizers,” they say.
According to Dr. Touvier and Dr. Srour, the takeaway message for clinicians is the finding that nitrites from food additives are associated with type 2 diabetes, “support existing guidelines recommending [limiting] the consumption of processed meats to prevent chronic diseases. However, the consumption of vegetables should be encouraged as they contain several beneficial compounds and contribute to chronic disease prevention.”
Some experts are skeptical
But three experts who were not involved with the research were skeptical about the conclusions, in comments made to the U.K. Science Media Centre.
“The fundamental weakness of this study is how the food additive intake was assessed,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London. “Estimates of intake were based on recalls of dietary intake on two separate occasions at the beginning of the study with no further estimates in the follow-up period of over 7 years,” he noted.
Other limitations include the relatively young age of the cohort and relatively low incidence of new cases of type 2 diabetes (about 1% of the study population over 7 years).
Moreover, the level of nitrite food additive ingestion is much lower than the acceptable daily intake. The findings would need to be replicated with appropriate adjustment for differences in body weight.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, said that “the study does not support the claim in the press release and paper that food additives are responsible for the increased risk.”
He pointed out that “nitrite from additives contributes only about 4%-6% of total nitrite intake in the population, and it is not clear why this should have a stronger impact on risk than nitrite from other sources,” such as nitrate found in food and water.
Duane Mellor, PhD, registered dietitian and senior lecturer, Aston University, Birmingham, England, said: “It could be questioned how accurate estimating intakes of individual additives like sodium nitrite, which was less than 1 mg per day from a record of just 2 days food intake per year, as it assumes people ate the same the other 363 days of the year.”
Moreover, “it is perhaps worth noting that the use of nitrites as an additive is often as sodium nitrite, which is used to cure meats like bacon, which if someone is seeking to reduce their risk of type 2 diabetes would be something people would be encouraged to eat less of [anyway].”
“The best way to reduce your risk of developing type 2 diabetes,” he said, “is to be physically active, maintain a healthy weight for you, and eat a varied diet based on vegetables, pulses, nuts, seeds, and fruit along with wholegrain and moderate intakes of dairy foods and meat (especially processed meats).”
Study details
Nitrites and nitrates are used as food additives to prevent bacterial growth, mainly in processed meats, and they are also found in foods (mainly green leafy vegetables) and water (nitrates from the use of nitrogen fertilizer can enter the water supply).
The researchers analyzed data from 104,168 participants in NutriNet-Santé who had no diabetes at baseline and who completed 24-hour dietary intake records. They investigated the association between exposure to nitrites and nitrates (in food and water or in additives) and incident type 2 diabetes.
Most nitrites came from food (95.3%), and less often from food additives (4.7%) and water (< 0.01%). The nitrites in foods were mainly from vegetables (60%) and seasonings (23%).
Most nitrates also came from food (93%), followed by water (6.9%) and food additives (0.1%). The nitrates in foods were mainly from vegetables (41%), processed meat (19%), and meat (17%).
During a median follow-up of 7.3 years, there were 969 incident cases of type 2 diabetes.
Compared with individuals in the lowest third of nitrites from food and water, those in the highest tertile had a 27% higher risk of incident type 2 diabetes, after adjusting for multiple variables (hazard ratio, 1.27; P = .009).
The risk of type 2 diabetes associated with the highest intake of nitrites from additives was as previously described, 53% higher, than that for those with the lowest intake.
There was no evidence of an association between nitrates and risk of type 2 diabetes.
The researchers acknowledge that study limitations include potential errors in assessment of nitrate and nitrate exposure, potential selection bias (participants in the web-based study may have had healthier behaviors than the general population), and potential unaccounted confounders (because it was an observational study).
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE