User login
Official Newspaper of the American College of Surgeons
Vascular Surgery Chronicles: Charles Lindbergh and Alexis Carrel: Strange Bedfellows
How does one of the smartest and most well-known men of his time become almost forgotten in history? Dr. Alexis Carrel’s contributions to medicine brought him to the height of fame in the worlds of surgery and science. By designing a curved needle coated in Vaseline, Carrel developed a new method of blood-vessel anastomosis that created a new standard for vascular surgery. This development earned him the Nobel Prize in Medicine or Physiology in 1912, making Carrel the second surgeon and youngest scientist at that time to earn this recognition. The ability to repair, reconnect, or attach blood vessels to one another opened the door for open heart surgery, coronary artery bypass grafts, transplantation, and countless other procedures. He further gained respect while working with Henry Drysdale Dakin in the French Army Medical Corps by revolutionizing the treatment of major wounds with wound antisepsis in the form of Carrel-Dakin fluid. This contribution alone earned him the Cross of the Legion of Honor.
However, by the time of the 52nd Vascular Annual Meeting in 1998, Dr. William Abbott in his SVS Presidential Address would focus on Carrel as an example of a surgeon with vast achievements who had come to be underrecognized. Despite Carrel’s amazing accomplishments throughout his life, the choices he ultimately made later significantly affected his legacy. Dr. Abbott attributes this to Carrel’s “unfortunate leadership decisions, in both boldness and judgment.”
Similar issues affected the legacy of Carrel’s close friend and colleague, Charles Lindbergh. The relationship between these two legendary men demonstrates the serendipity of history, the power of partnerships, and the importance of one’s choices, as well as the fleeting nature of fame. Both men reached the heights of praise and public admiration, then tumbled in a downward spiral of public condemnation.
Lindbergh, America’s golden boy aviator, had won the hearts of the world after he became the first to fly solo from New York to Paris in 1927. On Nov. 28, 1930, the American hero met the pioneering scientist Carrel through the auspices of Dr. Charles Flagg, a caretaker for Elisabeth Morrow, Lindbergh’s chronically ill sister-in-law. He and Carrel met at the Rockefeller Institute for Medical Research and formed a quick bond of mutual respect and admiration. Lindbergh was interested in questioning Carrel on potential treatments for his sister-in-law’s diseased heart valves: “Why could not a part of the body be kept alive indefinitely if a mechanical heart was attached to it – an arm, or even a head?… Why would not a mechanical heart be valuable for certain surgical operations?”
For his part, Carrel, a firm believer in “physiognomy,” the assessment of a person’s character from their outer appearance, and eugenics, the science of improving a population through controlled breeding, viewed Lindbergh as the perfect human specimen.
He interpreted the tall and handsome American hero as one of the elite selected by nature to play a role in society by promoting the production of the fit.
It was after this meeting that Lindbergh was invited to work in Carrel’s lab at the Rockefeller Institute. Lindbergh was enthralled with Carrel’s intellect, stating that his friend’s “mind flashed with the speed of light in space between the logical world of science and the mystical world of God.” Through Carrel’s tutelage and supervision, Lindbergh became focused on research on organ preservation.
During the mid-1930s, Lindbergh’s contribution to Carrel’s laboratory culminated in the design and production of the first efficient perfusion pump. This pump was intended to perfuse organs with pulsatile flow while maintaining a sterile environment free from contamination. The two men coauthored a book, “The Culture of Organs,” which detailed the process and theories for allowing living organs to exist outside the body during surgery. Their combined work is said to have been a crucial step in the later development of open heart surgery and organ transplantation, as well as to have laid the groundwork for the development of the artificial heart. Their collaboration raised their combined fame to the point where both men appeared on the cover of Time magazine on June 13, 1938, highlighting their heart perfusion work.
However, the very ideas that bonded the two famed men in mutual admiration would come to be unpopular, if not reviled, and led to their mutual downfall. Carrel’s views stating the superiority of evolution, survival of the fittest, and thoughts of eugenics paralleled Lindbergh’s thoughts of heredity and evolution. Lindbergh grew up on a farm and knew about breeding livestock and was comfortable with Carrel’s philosophy of racial superiority.
Therefore, despite the incredible accomplishments of both men, these jointly held views and their later affiliation with Nazi Germany and its principles tarnished their legacy.
Lindbergh, one of the few men with his level of fame who had lived among people of all skin colors in many cultures, was constantly being charged with racism and antisemitism. And even though he had previously stated, “I can’t feel inferior or superior to another man because of race, or in any way antagonistic to him. I judge the individual not by his race, and have always done so,” he constantly spoke of the value of genetics in promoting individual importance. And this talk of race betterment was a concept synonymous with the growing Nazi movement in Germany.
To make matters worse, Lindbergh had openly admired the Third Reich after having received the German Medal of Honor in 1938, bestowed by Herman Goering. This combined with Lindbergh’s past appreciation of Germany and his well-known views on eugenics caused many to view him as a Nazi sympathizer. It didn’t help that Lindbergh was also a great isolationist during World War II and acted as a spokesperson for the “America First” committee, which believed that the United States should not intervene. The once great man was denounced within his own country in a manner that would parallel what would happen to Carrel.
During the same period, Carrel returned to France to display his patriotism. In support of the war effort, Carrel volunteered his time toward supporting and designing mobile military hospitals and combating malnutrition. However, in the early 1940s, Germany conquered France and set up a puppet French government at Vichy. The new government offered Carrel the opportunity to continue his research at his own “Institute of Man.” Because of his past sentiments and this relationship formed with the Nazi-supported Vichy government, Carrel would come to be seen as a Nazi collaborator as well.
After the liberation of France in 1944, Carrel was dismissed from the institute and placed under surveillance to investigate his collaboration with the Nazis. Although no conclusions were ever reached, Carrel’s reputation was further destroyed by the press; this left him depressed and ruined. He died later that year on Nov. 5 (J Vasc Surg. 1999;29[1]:1-7).
Through their similar political views, Lindbergh and Carrel became despised in their own countries. Lindbergh would later regain his stature as an American hero and icon after advising the Army and Navy in World War II and continuing his work in the aeronautics industry. But his reputation remained forever tarnished as a Nazi sympathizer, and he died with his legacy disgraced in the eyes of many.
Lindbergh and Carrel’s contributions, despite their personal choices and judgments throughout life, have not been forgotten. There are many who still appreciate and remember the advances that both brought to the fields of medicine and science. Their legacies remain linked through the Lindbergh-Carrel Prize, established at the Medical University of South Carolina in Charleston. The award celebrates their contributions to the “development of perfusion and bioreactor technologies for organ preservation and growth.”
Lindbergh and Carrel exemplify the idea that one must consider the legacy that individuals leave behind in the context of their overall interactions and influences on the society in which they lived. Both men had significant individual failings and made choices that tarnished their public image and affected their legacies. With regard to Carrel, his opinions regarding the superiority of the white man and his proclamation of his mystical views alienated him from the public and the scientific community. Lindbergh’s alleged racism and antisemitism tarnished his image as a true American hero. Whatever their personal failings, however, medicine was forever changed by the impact of the great surgeon and the pilot.
Sources:
Berg AS. Lindbergh, Putman Adult Press, 1998.
Friedman DM. The Immortalists: Charles Lindbergh, Dr. Alexis Carrel, and Their Daring Quest to Live Forever. Ecco Publishing, 2007.
Presidential address: Legend, leadership, legacy. Abbott WM. J Vasc Surg. 1999;29:1-7.
Chaudhuri J, Al-Rubeai M. Bioreactors for Tissue Engineering: Principles, Design and Operation. Springer Publishing, 2005.
Dr. Phair is at the Department of Cardiovascular and Thoracic Surgery, Division of Vascular and Endovascular Surgery, Montefiore Medical Center, Bronx, N.Y.
How does one of the smartest and most well-known men of his time become almost forgotten in history? Dr. Alexis Carrel’s contributions to medicine brought him to the height of fame in the worlds of surgery and science. By designing a curved needle coated in Vaseline, Carrel developed a new method of blood-vessel anastomosis that created a new standard for vascular surgery. This development earned him the Nobel Prize in Medicine or Physiology in 1912, making Carrel the second surgeon and youngest scientist at that time to earn this recognition. The ability to repair, reconnect, or attach blood vessels to one another opened the door for open heart surgery, coronary artery bypass grafts, transplantation, and countless other procedures. He further gained respect while working with Henry Drysdale Dakin in the French Army Medical Corps by revolutionizing the treatment of major wounds with wound antisepsis in the form of Carrel-Dakin fluid. This contribution alone earned him the Cross of the Legion of Honor.
However, by the time of the 52nd Vascular Annual Meeting in 1998, Dr. William Abbott in his SVS Presidential Address would focus on Carrel as an example of a surgeon with vast achievements who had come to be underrecognized. Despite Carrel’s amazing accomplishments throughout his life, the choices he ultimately made later significantly affected his legacy. Dr. Abbott attributes this to Carrel’s “unfortunate leadership decisions, in both boldness and judgment.”
Similar issues affected the legacy of Carrel’s close friend and colleague, Charles Lindbergh. The relationship between these two legendary men demonstrates the serendipity of history, the power of partnerships, and the importance of one’s choices, as well as the fleeting nature of fame. Both men reached the heights of praise and public admiration, then tumbled in a downward spiral of public condemnation.
Lindbergh, America’s golden boy aviator, had won the hearts of the world after he became the first to fly solo from New York to Paris in 1927. On Nov. 28, 1930, the American hero met the pioneering scientist Carrel through the auspices of Dr. Charles Flagg, a caretaker for Elisabeth Morrow, Lindbergh’s chronically ill sister-in-law. He and Carrel met at the Rockefeller Institute for Medical Research and formed a quick bond of mutual respect and admiration. Lindbergh was interested in questioning Carrel on potential treatments for his sister-in-law’s diseased heart valves: “Why could not a part of the body be kept alive indefinitely if a mechanical heart was attached to it – an arm, or even a head?… Why would not a mechanical heart be valuable for certain surgical operations?”
For his part, Carrel, a firm believer in “physiognomy,” the assessment of a person’s character from their outer appearance, and eugenics, the science of improving a population through controlled breeding, viewed Lindbergh as the perfect human specimen.
He interpreted the tall and handsome American hero as one of the elite selected by nature to play a role in society by promoting the production of the fit.
It was after this meeting that Lindbergh was invited to work in Carrel’s lab at the Rockefeller Institute. Lindbergh was enthralled with Carrel’s intellect, stating that his friend’s “mind flashed with the speed of light in space between the logical world of science and the mystical world of God.” Through Carrel’s tutelage and supervision, Lindbergh became focused on research on organ preservation.
During the mid-1930s, Lindbergh’s contribution to Carrel’s laboratory culminated in the design and production of the first efficient perfusion pump. This pump was intended to perfuse organs with pulsatile flow while maintaining a sterile environment free from contamination. The two men coauthored a book, “The Culture of Organs,” which detailed the process and theories for allowing living organs to exist outside the body during surgery. Their combined work is said to have been a crucial step in the later development of open heart surgery and organ transplantation, as well as to have laid the groundwork for the development of the artificial heart. Their collaboration raised their combined fame to the point where both men appeared on the cover of Time magazine on June 13, 1938, highlighting their heart perfusion work.
However, the very ideas that bonded the two famed men in mutual admiration would come to be unpopular, if not reviled, and led to their mutual downfall. Carrel’s views stating the superiority of evolution, survival of the fittest, and thoughts of eugenics paralleled Lindbergh’s thoughts of heredity and evolution. Lindbergh grew up on a farm and knew about breeding livestock and was comfortable with Carrel’s philosophy of racial superiority.
Therefore, despite the incredible accomplishments of both men, these jointly held views and their later affiliation with Nazi Germany and its principles tarnished their legacy.
Lindbergh, one of the few men with his level of fame who had lived among people of all skin colors in many cultures, was constantly being charged with racism and antisemitism. And even though he had previously stated, “I can’t feel inferior or superior to another man because of race, or in any way antagonistic to him. I judge the individual not by his race, and have always done so,” he constantly spoke of the value of genetics in promoting individual importance. And this talk of race betterment was a concept synonymous with the growing Nazi movement in Germany.
To make matters worse, Lindbergh had openly admired the Third Reich after having received the German Medal of Honor in 1938, bestowed by Herman Goering. This combined with Lindbergh’s past appreciation of Germany and his well-known views on eugenics caused many to view him as a Nazi sympathizer. It didn’t help that Lindbergh was also a great isolationist during World War II and acted as a spokesperson for the “America First” committee, which believed that the United States should not intervene. The once great man was denounced within his own country in a manner that would parallel what would happen to Carrel.
During the same period, Carrel returned to France to display his patriotism. In support of the war effort, Carrel volunteered his time toward supporting and designing mobile military hospitals and combating malnutrition. However, in the early 1940s, Germany conquered France and set up a puppet French government at Vichy. The new government offered Carrel the opportunity to continue his research at his own “Institute of Man.” Because of his past sentiments and this relationship formed with the Nazi-supported Vichy government, Carrel would come to be seen as a Nazi collaborator as well.
After the liberation of France in 1944, Carrel was dismissed from the institute and placed under surveillance to investigate his collaboration with the Nazis. Although no conclusions were ever reached, Carrel’s reputation was further destroyed by the press; this left him depressed and ruined. He died later that year on Nov. 5 (J Vasc Surg. 1999;29[1]:1-7).
Through their similar political views, Lindbergh and Carrel became despised in their own countries. Lindbergh would later regain his stature as an American hero and icon after advising the Army and Navy in World War II and continuing his work in the aeronautics industry. But his reputation remained forever tarnished as a Nazi sympathizer, and he died with his legacy disgraced in the eyes of many.
Lindbergh and Carrel’s contributions, despite their personal choices and judgments throughout life, have not been forgotten. There are many who still appreciate and remember the advances that both brought to the fields of medicine and science. Their legacies remain linked through the Lindbergh-Carrel Prize, established at the Medical University of South Carolina in Charleston. The award celebrates their contributions to the “development of perfusion and bioreactor technologies for organ preservation and growth.”
Lindbergh and Carrel exemplify the idea that one must consider the legacy that individuals leave behind in the context of their overall interactions and influences on the society in which they lived. Both men had significant individual failings and made choices that tarnished their public image and affected their legacies. With regard to Carrel, his opinions regarding the superiority of the white man and his proclamation of his mystical views alienated him from the public and the scientific community. Lindbergh’s alleged racism and antisemitism tarnished his image as a true American hero. Whatever their personal failings, however, medicine was forever changed by the impact of the great surgeon and the pilot.
Sources:
Berg AS. Lindbergh, Putman Adult Press, 1998.
Friedman DM. The Immortalists: Charles Lindbergh, Dr. Alexis Carrel, and Their Daring Quest to Live Forever. Ecco Publishing, 2007.
Presidential address: Legend, leadership, legacy. Abbott WM. J Vasc Surg. 1999;29:1-7.
Chaudhuri J, Al-Rubeai M. Bioreactors for Tissue Engineering: Principles, Design and Operation. Springer Publishing, 2005.
Dr. Phair is at the Department of Cardiovascular and Thoracic Surgery, Division of Vascular and Endovascular Surgery, Montefiore Medical Center, Bronx, N.Y.
How does one of the smartest and most well-known men of his time become almost forgotten in history? Dr. Alexis Carrel’s contributions to medicine brought him to the height of fame in the worlds of surgery and science. By designing a curved needle coated in Vaseline, Carrel developed a new method of blood-vessel anastomosis that created a new standard for vascular surgery. This development earned him the Nobel Prize in Medicine or Physiology in 1912, making Carrel the second surgeon and youngest scientist at that time to earn this recognition. The ability to repair, reconnect, or attach blood vessels to one another opened the door for open heart surgery, coronary artery bypass grafts, transplantation, and countless other procedures. He further gained respect while working with Henry Drysdale Dakin in the French Army Medical Corps by revolutionizing the treatment of major wounds with wound antisepsis in the form of Carrel-Dakin fluid. This contribution alone earned him the Cross of the Legion of Honor.
However, by the time of the 52nd Vascular Annual Meeting in 1998, Dr. William Abbott in his SVS Presidential Address would focus on Carrel as an example of a surgeon with vast achievements who had come to be underrecognized. Despite Carrel’s amazing accomplishments throughout his life, the choices he ultimately made later significantly affected his legacy. Dr. Abbott attributes this to Carrel’s “unfortunate leadership decisions, in both boldness and judgment.”
Similar issues affected the legacy of Carrel’s close friend and colleague, Charles Lindbergh. The relationship between these two legendary men demonstrates the serendipity of history, the power of partnerships, and the importance of one’s choices, as well as the fleeting nature of fame. Both men reached the heights of praise and public admiration, then tumbled in a downward spiral of public condemnation.
Lindbergh, America’s golden boy aviator, had won the hearts of the world after he became the first to fly solo from New York to Paris in 1927. On Nov. 28, 1930, the American hero met the pioneering scientist Carrel through the auspices of Dr. Charles Flagg, a caretaker for Elisabeth Morrow, Lindbergh’s chronically ill sister-in-law. He and Carrel met at the Rockefeller Institute for Medical Research and formed a quick bond of mutual respect and admiration. Lindbergh was interested in questioning Carrel on potential treatments for his sister-in-law’s diseased heart valves: “Why could not a part of the body be kept alive indefinitely if a mechanical heart was attached to it – an arm, or even a head?… Why would not a mechanical heart be valuable for certain surgical operations?”
For his part, Carrel, a firm believer in “physiognomy,” the assessment of a person’s character from their outer appearance, and eugenics, the science of improving a population through controlled breeding, viewed Lindbergh as the perfect human specimen.
He interpreted the tall and handsome American hero as one of the elite selected by nature to play a role in society by promoting the production of the fit.
It was after this meeting that Lindbergh was invited to work in Carrel’s lab at the Rockefeller Institute. Lindbergh was enthralled with Carrel’s intellect, stating that his friend’s “mind flashed with the speed of light in space between the logical world of science and the mystical world of God.” Through Carrel’s tutelage and supervision, Lindbergh became focused on research on organ preservation.
During the mid-1930s, Lindbergh’s contribution to Carrel’s laboratory culminated in the design and production of the first efficient perfusion pump. This pump was intended to perfuse organs with pulsatile flow while maintaining a sterile environment free from contamination. The two men coauthored a book, “The Culture of Organs,” which detailed the process and theories for allowing living organs to exist outside the body during surgery. Their combined work is said to have been a crucial step in the later development of open heart surgery and organ transplantation, as well as to have laid the groundwork for the development of the artificial heart. Their collaboration raised their combined fame to the point where both men appeared on the cover of Time magazine on June 13, 1938, highlighting their heart perfusion work.
However, the very ideas that bonded the two famed men in mutual admiration would come to be unpopular, if not reviled, and led to their mutual downfall. Carrel’s views stating the superiority of evolution, survival of the fittest, and thoughts of eugenics paralleled Lindbergh’s thoughts of heredity and evolution. Lindbergh grew up on a farm and knew about breeding livestock and was comfortable with Carrel’s philosophy of racial superiority.
Therefore, despite the incredible accomplishments of both men, these jointly held views and their later affiliation with Nazi Germany and its principles tarnished their legacy.
Lindbergh, one of the few men with his level of fame who had lived among people of all skin colors in many cultures, was constantly being charged with racism and antisemitism. And even though he had previously stated, “I can’t feel inferior or superior to another man because of race, or in any way antagonistic to him. I judge the individual not by his race, and have always done so,” he constantly spoke of the value of genetics in promoting individual importance. And this talk of race betterment was a concept synonymous with the growing Nazi movement in Germany.
To make matters worse, Lindbergh had openly admired the Third Reich after having received the German Medal of Honor in 1938, bestowed by Herman Goering. This combined with Lindbergh’s past appreciation of Germany and his well-known views on eugenics caused many to view him as a Nazi sympathizer. It didn’t help that Lindbergh was also a great isolationist during World War II and acted as a spokesperson for the “America First” committee, which believed that the United States should not intervene. The once great man was denounced within his own country in a manner that would parallel what would happen to Carrel.
During the same period, Carrel returned to France to display his patriotism. In support of the war effort, Carrel volunteered his time toward supporting and designing mobile military hospitals and combating malnutrition. However, in the early 1940s, Germany conquered France and set up a puppet French government at Vichy. The new government offered Carrel the opportunity to continue his research at his own “Institute of Man.” Because of his past sentiments and this relationship formed with the Nazi-supported Vichy government, Carrel would come to be seen as a Nazi collaborator as well.
After the liberation of France in 1944, Carrel was dismissed from the institute and placed under surveillance to investigate his collaboration with the Nazis. Although no conclusions were ever reached, Carrel’s reputation was further destroyed by the press; this left him depressed and ruined. He died later that year on Nov. 5 (J Vasc Surg. 1999;29[1]:1-7).
Through their similar political views, Lindbergh and Carrel became despised in their own countries. Lindbergh would later regain his stature as an American hero and icon after advising the Army and Navy in World War II and continuing his work in the aeronautics industry. But his reputation remained forever tarnished as a Nazi sympathizer, and he died with his legacy disgraced in the eyes of many.
Lindbergh and Carrel’s contributions, despite their personal choices and judgments throughout life, have not been forgotten. There are many who still appreciate and remember the advances that both brought to the fields of medicine and science. Their legacies remain linked through the Lindbergh-Carrel Prize, established at the Medical University of South Carolina in Charleston. The award celebrates their contributions to the “development of perfusion and bioreactor technologies for organ preservation and growth.”
Lindbergh and Carrel exemplify the idea that one must consider the legacy that individuals leave behind in the context of their overall interactions and influences on the society in which they lived. Both men had significant individual failings and made choices that tarnished their public image and affected their legacies. With regard to Carrel, his opinions regarding the superiority of the white man and his proclamation of his mystical views alienated him from the public and the scientific community. Lindbergh’s alleged racism and antisemitism tarnished his image as a true American hero. Whatever their personal failings, however, medicine was forever changed by the impact of the great surgeon and the pilot.
Sources:
Berg AS. Lindbergh, Putman Adult Press, 1998.
Friedman DM. The Immortalists: Charles Lindbergh, Dr. Alexis Carrel, and Their Daring Quest to Live Forever. Ecco Publishing, 2007.
Presidential address: Legend, leadership, legacy. Abbott WM. J Vasc Surg. 1999;29:1-7.
Chaudhuri J, Al-Rubeai M. Bioreactors for Tissue Engineering: Principles, Design and Operation. Springer Publishing, 2005.
Dr. Phair is at the Department of Cardiovascular and Thoracic Surgery, Division of Vascular and Endovascular Surgery, Montefiore Medical Center, Bronx, N.Y.
Feds: Major EHR companies will remove interoperability roadblocks
LAS VEGAS – Health care data interoperability should get a huge boost under a public-private effort announced Feb. 29 by U.S. Department of Health and Human Services Secretary Sylvia Burwell.
The nation’s top five health care systems and companies, which provide the electronic health record systems that cover more than 90% of U.S. hospital patients, have agreed to principles designed to improve patient access to health data and eliminate the practice of data blocking.
They also have agreed to adopt federally recognized, national interoperability standards, Ms. Burwell announced at the annual meeting of the Healthcare Information and Management Systems Society.
“Technology is not just one leg of our strategy to build a better health care system for our nation – it supports the entire effort,” Ms. Burwell said. “We are working to unlock health care data and information so that providers are better informed and patients and families can access their health care information, making them empowered, active participants in their own care.”
In a show of support, medical specialty societies including the American Academy of Family Physicians, the American College of Physicians, the American Society of Clinical Oncology, and the American Medical Association also signed on to the commitment.
“We have made tremendous progress to bring health care into the 21st century,” Ms. Burwell said. “In 6 short years, we have tripled the adoption of electronic health records. Today, three-quarters of physicians are using them. And nearly every hospital uses EHRs, meaning that there is now a digital care footprint for almost everyone in this country.”
To unlock all those data and make them useful to health care providers and patients, the health IT companies and health care systems have agreed to the following steps:
• Implement application programming interface (API) technology so that smartphone and tablet apps can be created, facilitating patient use and transfer of their health care data.
• Work so providers can share patient health care data with patients and other providers whenever permitted by law, while not blocking such sharing either intentionally or unintentionally.
• Use the federally recognized Fast Healthcare Interoperability Resources (FHIR) data standard.
This commitment is a “major step forward” to help patients “not just in one episode, but over the long term,” explained Dr. Karen DeSalvo, National Coordinator for Health Information Technology. The agreement means the health care system is “on the threshold of a truly historic opportunity to transform quality of care,” she added.
Federal officials have a timeline for progress toward these goals by 2018, Dr. DeSalvo noted. But “the private sector wants to pull that forward and be leaders with us,” she said. “So, our expectation is that the calls and the commitments and the associated actions that these developers have declared will be seeing some changes by the fall.”
To highlight health information technology’s promise, Ms. Burwell shared a story about electronic health records’ use to find children affected by lead pollution in the water supplies of Flint, Mich.
Alerted to the problem by a friend, pediatrician Mona Hanna-Attisha of Hurley Medical Center in Flint tried to determine whether pipe corrosion might leach dangerous levels of lead into the water supply, Ms. Burwell said.
“She knew the danger lead posed and began what she called a ‘crusade’ to find out if it was affecting children,” Ms. Burwell explained. Dr. Hanna-Attisha mined Hurley’s medical records to “compare blood test results from more than 700 children in the area and map home addresses for geographic variations.
“She quickly discovered that the percentage of children in Flint with lead poisoning had doubled, and even tripled, in some neighborhoods,” Burwell said.
If those results had still been on paper, “it would have taken forever to get these results,” she said.
“Dr. Hanna-Attisha’s story shows us the power of putting health care data to work,” Ms. Burwell noted. “It allows us to see the connections in our communities and helps us put patients in the center of their care.”
Dr. David Classen, chief information officer of the patient safety organization Pascal Metrics and an author of a 2011 Institute of Medicine report on health IT and patient safety, applauded the announcement and the commitment from major EHR vendors and hospital systems have signed on.
“That was one of the things [the IOM expert panel] envisioned – a public-private partnership that would really help this. That’s close to optimal in my view.”
But “the devil’s in the details,” said Dr. Classen, associate professor of medicine at the University of Utah. “When it comes to sharing safety information, it’s not just removal of the gag clauses, it’s also the confidentiality clauses, and the intellectual property protections. Those things too can inhibit sharing of safety information. The challenge here is that [EHR vendors] worry that if they’re so interoperable, they convert their proprietary technology into something that could virtually be open source...and everyone can look at it. Those are legitimate concerns.”
Another concern is agreeing on a common alphabet. “Without that, this is not going to work,” he said. “All these vendor products grew up in silos, without standards imposed on them. So naturally, they’re going to have a Tower of Babel, which means most of them aren’t going to be speaking the same language.”
LAS VEGAS – Health care data interoperability should get a huge boost under a public-private effort announced Feb. 29 by U.S. Department of Health and Human Services Secretary Sylvia Burwell.
The nation’s top five health care systems and companies, which provide the electronic health record systems that cover more than 90% of U.S. hospital patients, have agreed to principles designed to improve patient access to health data and eliminate the practice of data blocking.
They also have agreed to adopt federally recognized, national interoperability standards, Ms. Burwell announced at the annual meeting of the Healthcare Information and Management Systems Society.
“Technology is not just one leg of our strategy to build a better health care system for our nation – it supports the entire effort,” Ms. Burwell said. “We are working to unlock health care data and information so that providers are better informed and patients and families can access their health care information, making them empowered, active participants in their own care.”
In a show of support, medical specialty societies including the American Academy of Family Physicians, the American College of Physicians, the American Society of Clinical Oncology, and the American Medical Association also signed on to the commitment.
“We have made tremendous progress to bring health care into the 21st century,” Ms. Burwell said. “In 6 short years, we have tripled the adoption of electronic health records. Today, three-quarters of physicians are using them. And nearly every hospital uses EHRs, meaning that there is now a digital care footprint for almost everyone in this country.”
To unlock all those data and make them useful to health care providers and patients, the health IT companies and health care systems have agreed to the following steps:
• Implement application programming interface (API) technology so that smartphone and tablet apps can be created, facilitating patient use and transfer of their health care data.
• Work so providers can share patient health care data with patients and other providers whenever permitted by law, while not blocking such sharing either intentionally or unintentionally.
• Use the federally recognized Fast Healthcare Interoperability Resources (FHIR) data standard.
This commitment is a “major step forward” to help patients “not just in one episode, but over the long term,” explained Dr. Karen DeSalvo, National Coordinator for Health Information Technology. The agreement means the health care system is “on the threshold of a truly historic opportunity to transform quality of care,” she added.
Federal officials have a timeline for progress toward these goals by 2018, Dr. DeSalvo noted. But “the private sector wants to pull that forward and be leaders with us,” she said. “So, our expectation is that the calls and the commitments and the associated actions that these developers have declared will be seeing some changes by the fall.”
To highlight health information technology’s promise, Ms. Burwell shared a story about electronic health records’ use to find children affected by lead pollution in the water supplies of Flint, Mich.
Alerted to the problem by a friend, pediatrician Mona Hanna-Attisha of Hurley Medical Center in Flint tried to determine whether pipe corrosion might leach dangerous levels of lead into the water supply, Ms. Burwell said.
“She knew the danger lead posed and began what she called a ‘crusade’ to find out if it was affecting children,” Ms. Burwell explained. Dr. Hanna-Attisha mined Hurley’s medical records to “compare blood test results from more than 700 children in the area and map home addresses for geographic variations.
“She quickly discovered that the percentage of children in Flint with lead poisoning had doubled, and even tripled, in some neighborhoods,” Burwell said.
If those results had still been on paper, “it would have taken forever to get these results,” she said.
“Dr. Hanna-Attisha’s story shows us the power of putting health care data to work,” Ms. Burwell noted. “It allows us to see the connections in our communities and helps us put patients in the center of their care.”
Dr. David Classen, chief information officer of the patient safety organization Pascal Metrics and an author of a 2011 Institute of Medicine report on health IT and patient safety, applauded the announcement and the commitment from major EHR vendors and hospital systems have signed on.
“That was one of the things [the IOM expert panel] envisioned – a public-private partnership that would really help this. That’s close to optimal in my view.”
But “the devil’s in the details,” said Dr. Classen, associate professor of medicine at the University of Utah. “When it comes to sharing safety information, it’s not just removal of the gag clauses, it’s also the confidentiality clauses, and the intellectual property protections. Those things too can inhibit sharing of safety information. The challenge here is that [EHR vendors] worry that if they’re so interoperable, they convert their proprietary technology into something that could virtually be open source...and everyone can look at it. Those are legitimate concerns.”
Another concern is agreeing on a common alphabet. “Without that, this is not going to work,” he said. “All these vendor products grew up in silos, without standards imposed on them. So naturally, they’re going to have a Tower of Babel, which means most of them aren’t going to be speaking the same language.”
LAS VEGAS – Health care data interoperability should get a huge boost under a public-private effort announced Feb. 29 by U.S. Department of Health and Human Services Secretary Sylvia Burwell.
The nation’s top five health care systems and companies, which provide the electronic health record systems that cover more than 90% of U.S. hospital patients, have agreed to principles designed to improve patient access to health data and eliminate the practice of data blocking.
They also have agreed to adopt federally recognized, national interoperability standards, Ms. Burwell announced at the annual meeting of the Healthcare Information and Management Systems Society.
“Technology is not just one leg of our strategy to build a better health care system for our nation – it supports the entire effort,” Ms. Burwell said. “We are working to unlock health care data and information so that providers are better informed and patients and families can access their health care information, making them empowered, active participants in their own care.”
In a show of support, medical specialty societies including the American Academy of Family Physicians, the American College of Physicians, the American Society of Clinical Oncology, and the American Medical Association also signed on to the commitment.
“We have made tremendous progress to bring health care into the 21st century,” Ms. Burwell said. “In 6 short years, we have tripled the adoption of electronic health records. Today, three-quarters of physicians are using them. And nearly every hospital uses EHRs, meaning that there is now a digital care footprint for almost everyone in this country.”
To unlock all those data and make them useful to health care providers and patients, the health IT companies and health care systems have agreed to the following steps:
• Implement application programming interface (API) technology so that smartphone and tablet apps can be created, facilitating patient use and transfer of their health care data.
• Work so providers can share patient health care data with patients and other providers whenever permitted by law, while not blocking such sharing either intentionally or unintentionally.
• Use the federally recognized Fast Healthcare Interoperability Resources (FHIR) data standard.
This commitment is a “major step forward” to help patients “not just in one episode, but over the long term,” explained Dr. Karen DeSalvo, National Coordinator for Health Information Technology. The agreement means the health care system is “on the threshold of a truly historic opportunity to transform quality of care,” she added.
Federal officials have a timeline for progress toward these goals by 2018, Dr. DeSalvo noted. But “the private sector wants to pull that forward and be leaders with us,” she said. “So, our expectation is that the calls and the commitments and the associated actions that these developers have declared will be seeing some changes by the fall.”
To highlight health information technology’s promise, Ms. Burwell shared a story about electronic health records’ use to find children affected by lead pollution in the water supplies of Flint, Mich.
Alerted to the problem by a friend, pediatrician Mona Hanna-Attisha of Hurley Medical Center in Flint tried to determine whether pipe corrosion might leach dangerous levels of lead into the water supply, Ms. Burwell said.
“She knew the danger lead posed and began what she called a ‘crusade’ to find out if it was affecting children,” Ms. Burwell explained. Dr. Hanna-Attisha mined Hurley’s medical records to “compare blood test results from more than 700 children in the area and map home addresses for geographic variations.
“She quickly discovered that the percentage of children in Flint with lead poisoning had doubled, and even tripled, in some neighborhoods,” Burwell said.
If those results had still been on paper, “it would have taken forever to get these results,” she said.
“Dr. Hanna-Attisha’s story shows us the power of putting health care data to work,” Ms. Burwell noted. “It allows us to see the connections in our communities and helps us put patients in the center of their care.”
Dr. David Classen, chief information officer of the patient safety organization Pascal Metrics and an author of a 2011 Institute of Medicine report on health IT and patient safety, applauded the announcement and the commitment from major EHR vendors and hospital systems have signed on.
“That was one of the things [the IOM expert panel] envisioned – a public-private partnership that would really help this. That’s close to optimal in my view.”
But “the devil’s in the details,” said Dr. Classen, associate professor of medicine at the University of Utah. “When it comes to sharing safety information, it’s not just removal of the gag clauses, it’s also the confidentiality clauses, and the intellectual property protections. Those things too can inhibit sharing of safety information. The challenge here is that [EHR vendors] worry that if they’re so interoperable, they convert their proprietary technology into something that could virtually be open source...and everyone can look at it. Those are legitimate concerns.”
Another concern is agreeing on a common alphabet. “Without that, this is not going to work,” he said. “All these vendor products grew up in silos, without standards imposed on them. So naturally, they’re going to have a Tower of Babel, which means most of them aren’t going to be speaking the same language.”
AT HIMSS16
Occult micrometastases in N2 lymph nodes correlated with shorter survival in NSCLC
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
Key clinical point: Micrometastasis detected by immunohistochemistry (IHC) staining for cytokeratin (AE1/AE3) in the lymph nodes of patients with non–small cell lung cancer (NSCLC), designated stage I or N0 by standard techniques, correlated with decreased overall survival.
Major finding: Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017.
Data source: The Cancer and Leukemia Group B (CALGB) 9761 trial of 304 patients with stage 1A or 1B NSCLC.
Disclosures: Dr. Martin and coauthors had no disclosures.
Chronic pain among surgeons needs to be addressed
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.

|
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.

|
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.

|
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
HIV not a risk factor for postappendectomy complications
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients according to an analysis of cases in a national surgical database presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Michael C. Smith of the State University of New York, Brooklyn, explained why he and his colleagues felt it was time to update the literature on HIV and surgery. “Much of the literature on appendectomy in the setting of HIV is either from the early 1990s or elsewhere in the world, and it shows greatly increased complication rates in these patients,” he said.
The analysis queried the Nationwide Inpatient Sample (NIS) database for all patients who had acute appendicitis and appendectomy during 2005-2012. The analysis included patients who had both open and laparoscopic appendectomy, and compared the HIV group that did not have AIDS with the non-HIV group, Dr. Smith said. The population with AIDS, along with patients who had interval appendectomies after appendicitis, were excluded.
The study looked at 821 patients with HIV and 338,425 patients without HIV as controls.
“The only significant difference we found between the two groups was hospital length of stay, which differed by about three-quarters of a day,” Dr. Smith said. Patients with HIV spent on average 3.8 days in the hospital after appendectomy vs. 3 days for non-HIV patients. “Other complication rates were nonsignificant by our study,” he said.
The average total charge for HIV patients was also higher, $33,350 vs. $30,714, the analysis showed.
Dr. Smith acknowledged some limitations in using the NIS database, most notably that the data were from index hospitalizations only. “So we probably did not capture people who returned to the hospital on postoperative day 3, 4, and 5 after they were discharged home,” he said. “Therefore, prospective studies are needed to validate these results.”
He also said that the study did not differentiate between operations for perforated and nonperforated appendix, and he and his coresearchers could not determine why the HIV population had longer hospital stays.
Dr. Smith and coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Patients who have HIV are at no greater risk of complications from appendectomy than are non-HIV patients.
Major finding: Risk of death and complications were similar across both groups, although hospital stays were about 26% longer and cost about 10% more for patients with HIV.
Data source: Query of Nationwide Inpatient Sample (NIS) database during 2005-2012 of 812 HIV and 338,425 non-HIV patients who had appendectomy for acute appendicitis.
Disclosures: The study authors reported having no financial disclosures.
Smoking affects molecular profile of HPV-positive oropharyngeal cancer
SCOTTSDALE, ARIZ. – The human papillomavirus (HPV)–positive oropharyngeal cancers of heavy smokers and light smokers have distinctly different molecular profiles, which may have implications for treatment, according to a study presented at the Multidisciplinary Head and Neck Cancer Symposium.
The population-based cohort study of 66 patients found that mutations in certain genes associated with tobacco exposure and poorer survival – for example, NOTCH1, TP53, CDKN2A, and KRAS – were found almost exclusively in heavy smokers, investigators reported in a session and related press briefing. Also, the number of HPV reads detected in tumors was lower for heavy smokers as compared with light smokers.
Taken together, the findings suggest that although HPV-positive cancers in heavy smokers may be initiated through virus-related mutations, they go on to acquire tobacco-related mutations and become less dependent on the E6/E7 carcinogenesis mechanisms typically associated with the virus, said first author Dr. Jose P. Zevallos of the University of North Carolina, Chapel Hill.
“We think that this study and future studies based on this work will have important implications for personalizing treatment and decision making in HPV-positive oropharynx cancer, particularly in the era of less aggressive treatments for HPV-positive tumors because of their excellent prognosis,” he said. “As opposed to arbitrarily deciding that 10 pack-years [of smoking] is a number that we use to define more aggressive disease, we are trying to provide a molecular basis for more aggressive disease in order to decide who will benefit from less-aggressive versus more-aggressive treatment.”
Press briefing moderator Dr. Christine Gourin of Johns Hopkins University, Baltimore, said “This study is so important because we know that the molecular fingerprint of HPV-related oropharyngeal cancer is really different from anything that we have seen before – different patient population, different outcomes than when I was in training.”
“We don’t really understand fully why this fingerprint is so different and why tobacco affects the fingerprint,” she added. “The finding of differences in the molecular phenotypes of light smokers versus heavy smokers is something that we all appreciate clinically and we need to understand better to tailor treatment.”
Introducing the study, Dr. Zevallos noted that the HPV-positive cancers of smokers are known to have prognosis intermediate between those of the more favorable HPV-positive cancers of never smokers and the less favorable HPV-negative cancers. What remains unclear is the molecular basis for these differences.
Patients came from the population-based CHANCE (Carolina Head and Neck Cancer Epidemiology) study conducted during 2001-2006. The investigators performed targeted next-generation DNA sequencing in tumors with an assay for more than 700 genes associated with human cancers.
“We focused our attention on genes that overlap with those in COSMIC [the Catalogue of Somatic Mutations in Cancer] as well as on TCGA [The Cancer Genome Atlas] genes that were demonstrated to be significant in head and neck cancer,” Dr. Zevallos explained.
All 66 patients studied had HPV-positive tumors according to p16 expression or HPV polymerase chain reaction findings. Overall, 61% were heavy smokers, defined as having a greater than 10 pack-year history of smoking.
In terms of clinical outcome, the 5-year overall survival rate was 82% among the heavy smokers and 60% among the light or never smokers.
Mutations associated with tobacco use were found almost exclusively in the heavy smokers, Dr. Zevallos reported. For example, they had higher prevalences of mutations in NOTCH1 (18% vs. 0%), FAT1 (14% vs. 6%), and FGFR3 (10% vs. 0%), among others. On the other hand, the light and never smokers had a higher prevalence of mutations in PIK3CA (50% vs. 34%). Additionally, KRAS mutations were found only in the heavy smokers (4% vs. 0%), whereas HRAS mutations were found in the light and never smokers only (6% vs. 0%).
A pathway analysis incorporating the new information for HPV-positive heavy smokers confirmed that despite persistence of the HPV-related signature, these tumors also had signaling in several of the pathways typically associated with HPV-negative cancers, according to Dr. Zevallos.
HPV DNA was detected in all of the tumors, and in 95% of cases, the viral type was type 16. However, PCR for HPV was falsely negative in 9%. “This is a very important number as we rely on this as a surrogate for HPV status,” he commented. “p16 was the main inclusion criterion for this particular study, but this should be noted.”
Heavy smokers and patients who had died had a lower number of HPV reads per tumor. “This tells us that there are potentially subclones developing in these patients that are driven by tobacco-associated mutations, and this may explain worse outcomes in this patient population and warrants further exploration,” Dr. Zevallos elaborated.
SCOTTSDALE, ARIZ. – The human papillomavirus (HPV)–positive oropharyngeal cancers of heavy smokers and light smokers have distinctly different molecular profiles, which may have implications for treatment, according to a study presented at the Multidisciplinary Head and Neck Cancer Symposium.
The population-based cohort study of 66 patients found that mutations in certain genes associated with tobacco exposure and poorer survival – for example, NOTCH1, TP53, CDKN2A, and KRAS – were found almost exclusively in heavy smokers, investigators reported in a session and related press briefing. Also, the number of HPV reads detected in tumors was lower for heavy smokers as compared with light smokers.
Taken together, the findings suggest that although HPV-positive cancers in heavy smokers may be initiated through virus-related mutations, they go on to acquire tobacco-related mutations and become less dependent on the E6/E7 carcinogenesis mechanisms typically associated with the virus, said first author Dr. Jose P. Zevallos of the University of North Carolina, Chapel Hill.
“We think that this study and future studies based on this work will have important implications for personalizing treatment and decision making in HPV-positive oropharynx cancer, particularly in the era of less aggressive treatments for HPV-positive tumors because of their excellent prognosis,” he said. “As opposed to arbitrarily deciding that 10 pack-years [of smoking] is a number that we use to define more aggressive disease, we are trying to provide a molecular basis for more aggressive disease in order to decide who will benefit from less-aggressive versus more-aggressive treatment.”
Press briefing moderator Dr. Christine Gourin of Johns Hopkins University, Baltimore, said “This study is so important because we know that the molecular fingerprint of HPV-related oropharyngeal cancer is really different from anything that we have seen before – different patient population, different outcomes than when I was in training.”
“We don’t really understand fully why this fingerprint is so different and why tobacco affects the fingerprint,” she added. “The finding of differences in the molecular phenotypes of light smokers versus heavy smokers is something that we all appreciate clinically and we need to understand better to tailor treatment.”
Introducing the study, Dr. Zevallos noted that the HPV-positive cancers of smokers are known to have prognosis intermediate between those of the more favorable HPV-positive cancers of never smokers and the less favorable HPV-negative cancers. What remains unclear is the molecular basis for these differences.
Patients came from the population-based CHANCE (Carolina Head and Neck Cancer Epidemiology) study conducted during 2001-2006. The investigators performed targeted next-generation DNA sequencing in tumors with an assay for more than 700 genes associated with human cancers.
“We focused our attention on genes that overlap with those in COSMIC [the Catalogue of Somatic Mutations in Cancer] as well as on TCGA [The Cancer Genome Atlas] genes that were demonstrated to be significant in head and neck cancer,” Dr. Zevallos explained.
All 66 patients studied had HPV-positive tumors according to p16 expression or HPV polymerase chain reaction findings. Overall, 61% were heavy smokers, defined as having a greater than 10 pack-year history of smoking.
In terms of clinical outcome, the 5-year overall survival rate was 82% among the heavy smokers and 60% among the light or never smokers.
Mutations associated with tobacco use were found almost exclusively in the heavy smokers, Dr. Zevallos reported. For example, they had higher prevalences of mutations in NOTCH1 (18% vs. 0%), FAT1 (14% vs. 6%), and FGFR3 (10% vs. 0%), among others. On the other hand, the light and never smokers had a higher prevalence of mutations in PIK3CA (50% vs. 34%). Additionally, KRAS mutations were found only in the heavy smokers (4% vs. 0%), whereas HRAS mutations were found in the light and never smokers only (6% vs. 0%).
A pathway analysis incorporating the new information for HPV-positive heavy smokers confirmed that despite persistence of the HPV-related signature, these tumors also had signaling in several of the pathways typically associated with HPV-negative cancers, according to Dr. Zevallos.
HPV DNA was detected in all of the tumors, and in 95% of cases, the viral type was type 16. However, PCR for HPV was falsely negative in 9%. “This is a very important number as we rely on this as a surrogate for HPV status,” he commented. “p16 was the main inclusion criterion for this particular study, but this should be noted.”
Heavy smokers and patients who had died had a lower number of HPV reads per tumor. “This tells us that there are potentially subclones developing in these patients that are driven by tobacco-associated mutations, and this may explain worse outcomes in this patient population and warrants further exploration,” Dr. Zevallos elaborated.
SCOTTSDALE, ARIZ. – The human papillomavirus (HPV)–positive oropharyngeal cancers of heavy smokers and light smokers have distinctly different molecular profiles, which may have implications for treatment, according to a study presented at the Multidisciplinary Head and Neck Cancer Symposium.
The population-based cohort study of 66 patients found that mutations in certain genes associated with tobacco exposure and poorer survival – for example, NOTCH1, TP53, CDKN2A, and KRAS – were found almost exclusively in heavy smokers, investigators reported in a session and related press briefing. Also, the number of HPV reads detected in tumors was lower for heavy smokers as compared with light smokers.
Taken together, the findings suggest that although HPV-positive cancers in heavy smokers may be initiated through virus-related mutations, they go on to acquire tobacco-related mutations and become less dependent on the E6/E7 carcinogenesis mechanisms typically associated with the virus, said first author Dr. Jose P. Zevallos of the University of North Carolina, Chapel Hill.
“We think that this study and future studies based on this work will have important implications for personalizing treatment and decision making in HPV-positive oropharynx cancer, particularly in the era of less aggressive treatments for HPV-positive tumors because of their excellent prognosis,” he said. “As opposed to arbitrarily deciding that 10 pack-years [of smoking] is a number that we use to define more aggressive disease, we are trying to provide a molecular basis for more aggressive disease in order to decide who will benefit from less-aggressive versus more-aggressive treatment.”
Press briefing moderator Dr. Christine Gourin of Johns Hopkins University, Baltimore, said “This study is so important because we know that the molecular fingerprint of HPV-related oropharyngeal cancer is really different from anything that we have seen before – different patient population, different outcomes than when I was in training.”
“We don’t really understand fully why this fingerprint is so different and why tobacco affects the fingerprint,” she added. “The finding of differences in the molecular phenotypes of light smokers versus heavy smokers is something that we all appreciate clinically and we need to understand better to tailor treatment.”
Introducing the study, Dr. Zevallos noted that the HPV-positive cancers of smokers are known to have prognosis intermediate between those of the more favorable HPV-positive cancers of never smokers and the less favorable HPV-negative cancers. What remains unclear is the molecular basis for these differences.
Patients came from the population-based CHANCE (Carolina Head and Neck Cancer Epidemiology) study conducted during 2001-2006. The investigators performed targeted next-generation DNA sequencing in tumors with an assay for more than 700 genes associated with human cancers.
“We focused our attention on genes that overlap with those in COSMIC [the Catalogue of Somatic Mutations in Cancer] as well as on TCGA [The Cancer Genome Atlas] genes that were demonstrated to be significant in head and neck cancer,” Dr. Zevallos explained.
All 66 patients studied had HPV-positive tumors according to p16 expression or HPV polymerase chain reaction findings. Overall, 61% were heavy smokers, defined as having a greater than 10 pack-year history of smoking.
In terms of clinical outcome, the 5-year overall survival rate was 82% among the heavy smokers and 60% among the light or never smokers.
Mutations associated with tobacco use were found almost exclusively in the heavy smokers, Dr. Zevallos reported. For example, they had higher prevalences of mutations in NOTCH1 (18% vs. 0%), FAT1 (14% vs. 6%), and FGFR3 (10% vs. 0%), among others. On the other hand, the light and never smokers had a higher prevalence of mutations in PIK3CA (50% vs. 34%). Additionally, KRAS mutations were found only in the heavy smokers (4% vs. 0%), whereas HRAS mutations were found in the light and never smokers only (6% vs. 0%).
A pathway analysis incorporating the new information for HPV-positive heavy smokers confirmed that despite persistence of the HPV-related signature, these tumors also had signaling in several of the pathways typically associated with HPV-negative cancers, according to Dr. Zevallos.
HPV DNA was detected in all of the tumors, and in 95% of cases, the viral type was type 16. However, PCR for HPV was falsely negative in 9%. “This is a very important number as we rely on this as a surrogate for HPV status,” he commented. “p16 was the main inclusion criterion for this particular study, but this should be noted.”
Heavy smokers and patients who had died had a lower number of HPV reads per tumor. “This tells us that there are potentially subclones developing in these patients that are driven by tobacco-associated mutations, and this may explain worse outcomes in this patient population and warrants further exploration,” Dr. Zevallos elaborated.
AT THE MULTIDISCIPLINARY HEAD AND NECK CANCER SYMPOSIUM
Key clinical point: The molecular profile of HPV-positive oropharyngeal cancer differs distinctly between heavy and light smokers.
Major finding: Heavy smokers were more likely to have mutations of NOTCH1 (18% vs. 0%), TP53 (6% vs. 0%), and KRAS (4% vs. 0%), and they had fewer HPV reads in their tumors.
Data source: A population-based cohort study of 66 patients with HPV-positive oropharyngeal cancer.
Disclosures: Dr. Zevallos disclosed that he had no relevant conflicts of interest.
Periop statins don’t prevent acute kidney injury after cardiac surgery
ORLANDO – Statins administered perioperatively offered no protection against acute kidney injury following cardiac surgery, according to new results of a 5-year randomized clinical trial.
The findings held true whether or not patients were naive to statins; serum creatinine levels actually increased significantly more for statin-naive patients given atorvastatin than those given placebo.
The study was stopped early for patients naive to statins because increased acute kidney injury was seen in those patients who had chronic kidney disease (eGFR less than 60 mL/min/1.73 m2), and was subsequently stopped early for futility for all patients.
“De novo initiation of daily perioperative atorvastatin treatment did not reduce the incidence of AKI or reduce the increase in serum creatinine concentration associated with cardiac surgery,” wrote Dr. Frederic T. Billings IV, professor of medicine at Vanderbilt University, Nashville, Tenn., and his collaborators. The findings (JAMA 2016 Feb 23. doi: 10.1001/jama.2016.0548) were published concurrently with his presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In what Dr. Phil B. Fontanarosa, executive editor of JAMA and comoderator of the late-breaking trials session at the meeting, described as “really an elegant clinical trial,” Dr. Billings and his collaborators enrolled 615 patients over 5 years at Vanderbilt University Medical Center.
Patients undergoing elective coronary artery bypass grafting, valvular heart surgery, or ascending aortic surgery were eligible. Patients were excluded if they had prior statin intolerance, acute coronary syndrome, or liver dysfunction; were taking potent CYP3A4 inhibitors or cyclosporine; were receiving renal replacement therapy or had a kidney transplant; or were pregnant.
Both patients currently on a statin and patients naive to statins were recruited. Statin-naive patients received 80 mg atorvastatin the day before surgery, and then 40 mg of atorvastatin on the day of surgery and daily following surgery, or a matched placebo regimen.
Patients who were already on a statin received the study drug only on days that they would not have received a statin if treated according to the current standard of care. It was deemed unethical to allow those patients to receive placebo during and after surgery, since observational studies suggested that doing so might increase their potential for AKI.
For those patients already on a statin, this meant that they stayed on their usual regimen until the day of surgery, and then were randomized to receive either 80 mg of atorvastatin on the day of surgery and 40 mg of atorvastatin the day after surgery, or a matching placebo regimen.
For both groups, the study drug was given at least 3 hours before surgery on the day of surgery.
Randomization was stratified for prior statin use, for chronic kidney disease, and by history of diabetes. The 199 patients naive to statins and the 416 already on a statin were similar in demographic and health characteristics. Median age was 67 years, 188 (30.6%) were women; 202 participants (32.8%) had diabetes.
The primary outcome measure was diagnosis of AKI, defined as an increase of 0.3 mg/dL in serum creatinine, or beginning renal replacement therapy within 48 hours of surgery. Baseline serum creatinine was measured no more than 7 days prior to surgery.
AKI occurred in 64 of 308 patients (20.8%) in the atorvastatin group, and in 60 of 307 patients (19.5%) receiving placebo overall (P = .75). For those naive to statins, 21.6% of the atorvastatin group and 13.4% of the placebo group developed AKI (P = .15). Overall, 179 enrolled patients had CKD, and the incidence of AKI did not significantly differ in the atorvastatin and the placebo arms of this subgroup.
The subpopulation of participants with CKD who were statin naive (n = 36), however, saw an increased incidence of AKI with atorvastatin compared to placebo. AKI occurred in 9 of 17 patients (52.9%) given atorvastatin, and in 3 of 19 (15.8%) given placebo group (RR, 3.35[95% confidence interval 0.12 to 10.05]; P = .03). “It should be noted that the number of patients in this subgroup was particularly small, leading to a wide confidence interval and an increased chance of type 1 error,” said Dr. Billings.
Secondary outcome measures were maximum increase in creatinine concentration from baseline through postop day 2, delirium in the ICU, degree of myocardial injury, and incidence of postoperative pneumonia, atrial fibrillation, or stroke. Perioperative atorvastatin administration did not affect any of these endpoints.
The safety analysis showed no indications of increased risk of skeletal muscle or liver injury with perioperative atorvastatin use.
In the real world, “Most patients presenting for cardiac surgery … are already taking statins, and in the current study there was little evidence that continuation or withdrawal from statin treatment on the day of surgery and postoperative day 1 affects AKI,” wrote Dr. Billings and his coauthors.
Study limitations included its single-center design, and the use of AKI criteria that may not be sensitive to late-developing AKI. Also, for enrolled patients who were already on statins, statin exposure was not reduced in comparison with usual care.
After the presentation, Dr. Billings reported that the researchers also collected information about other biomarkers that may signal AKI, including IgM. He and his collaborators plan later publication of those data after a full analysis.
The National Institutes of Health and the Vanderbilt University Medical Center department of anesthesiology funded the study. Dr. Brown reported receiving grants from Shire Pharmaceuticals and New Haven Pharmaceuticals, and personal fees from Novartis Pharmaceuticals and Alnylam Pharmaceuticals. The other authors reported no conflicts of interest.
On Twitter @karioakes
ORLANDO – Statins administered perioperatively offered no protection against acute kidney injury following cardiac surgery, according to new results of a 5-year randomized clinical trial.
The findings held true whether or not patients were naive to statins; serum creatinine levels actually increased significantly more for statin-naive patients given atorvastatin than those given placebo.
The study was stopped early for patients naive to statins because increased acute kidney injury was seen in those patients who had chronic kidney disease (eGFR less than 60 mL/min/1.73 m2), and was subsequently stopped early for futility for all patients.
“De novo initiation of daily perioperative atorvastatin treatment did not reduce the incidence of AKI or reduce the increase in serum creatinine concentration associated with cardiac surgery,” wrote Dr. Frederic T. Billings IV, professor of medicine at Vanderbilt University, Nashville, Tenn., and his collaborators. The findings (JAMA 2016 Feb 23. doi: 10.1001/jama.2016.0548) were published concurrently with his presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In what Dr. Phil B. Fontanarosa, executive editor of JAMA and comoderator of the late-breaking trials session at the meeting, described as “really an elegant clinical trial,” Dr. Billings and his collaborators enrolled 615 patients over 5 years at Vanderbilt University Medical Center.
Patients undergoing elective coronary artery bypass grafting, valvular heart surgery, or ascending aortic surgery were eligible. Patients were excluded if they had prior statin intolerance, acute coronary syndrome, or liver dysfunction; were taking potent CYP3A4 inhibitors or cyclosporine; were receiving renal replacement therapy or had a kidney transplant; or were pregnant.
Both patients currently on a statin and patients naive to statins were recruited. Statin-naive patients received 80 mg atorvastatin the day before surgery, and then 40 mg of atorvastatin on the day of surgery and daily following surgery, or a matched placebo regimen.
Patients who were already on a statin received the study drug only on days that they would not have received a statin if treated according to the current standard of care. It was deemed unethical to allow those patients to receive placebo during and after surgery, since observational studies suggested that doing so might increase their potential for AKI.
For those patients already on a statin, this meant that they stayed on their usual regimen until the day of surgery, and then were randomized to receive either 80 mg of atorvastatin on the day of surgery and 40 mg of atorvastatin the day after surgery, or a matching placebo regimen.
For both groups, the study drug was given at least 3 hours before surgery on the day of surgery.
Randomization was stratified for prior statin use, for chronic kidney disease, and by history of diabetes. The 199 patients naive to statins and the 416 already on a statin were similar in demographic and health characteristics. Median age was 67 years, 188 (30.6%) were women; 202 participants (32.8%) had diabetes.
The primary outcome measure was diagnosis of AKI, defined as an increase of 0.3 mg/dL in serum creatinine, or beginning renal replacement therapy within 48 hours of surgery. Baseline serum creatinine was measured no more than 7 days prior to surgery.
AKI occurred in 64 of 308 patients (20.8%) in the atorvastatin group, and in 60 of 307 patients (19.5%) receiving placebo overall (P = .75). For those naive to statins, 21.6% of the atorvastatin group and 13.4% of the placebo group developed AKI (P = .15). Overall, 179 enrolled patients had CKD, and the incidence of AKI did not significantly differ in the atorvastatin and the placebo arms of this subgroup.
The subpopulation of participants with CKD who were statin naive (n = 36), however, saw an increased incidence of AKI with atorvastatin compared to placebo. AKI occurred in 9 of 17 patients (52.9%) given atorvastatin, and in 3 of 19 (15.8%) given placebo group (RR, 3.35[95% confidence interval 0.12 to 10.05]; P = .03). “It should be noted that the number of patients in this subgroup was particularly small, leading to a wide confidence interval and an increased chance of type 1 error,” said Dr. Billings.
Secondary outcome measures were maximum increase in creatinine concentration from baseline through postop day 2, delirium in the ICU, degree of myocardial injury, and incidence of postoperative pneumonia, atrial fibrillation, or stroke. Perioperative atorvastatin administration did not affect any of these endpoints.
The safety analysis showed no indications of increased risk of skeletal muscle or liver injury with perioperative atorvastatin use.
In the real world, “Most patients presenting for cardiac surgery … are already taking statins, and in the current study there was little evidence that continuation or withdrawal from statin treatment on the day of surgery and postoperative day 1 affects AKI,” wrote Dr. Billings and his coauthors.
Study limitations included its single-center design, and the use of AKI criteria that may not be sensitive to late-developing AKI. Also, for enrolled patients who were already on statins, statin exposure was not reduced in comparison with usual care.
After the presentation, Dr. Billings reported that the researchers also collected information about other biomarkers that may signal AKI, including IgM. He and his collaborators plan later publication of those data after a full analysis.
The National Institutes of Health and the Vanderbilt University Medical Center department of anesthesiology funded the study. Dr. Brown reported receiving grants from Shire Pharmaceuticals and New Haven Pharmaceuticals, and personal fees from Novartis Pharmaceuticals and Alnylam Pharmaceuticals. The other authors reported no conflicts of interest.
On Twitter @karioakes
ORLANDO – Statins administered perioperatively offered no protection against acute kidney injury following cardiac surgery, according to new results of a 5-year randomized clinical trial.
The findings held true whether or not patients were naive to statins; serum creatinine levels actually increased significantly more for statin-naive patients given atorvastatin than those given placebo.
The study was stopped early for patients naive to statins because increased acute kidney injury was seen in those patients who had chronic kidney disease (eGFR less than 60 mL/min/1.73 m2), and was subsequently stopped early for futility for all patients.
“De novo initiation of daily perioperative atorvastatin treatment did not reduce the incidence of AKI or reduce the increase in serum creatinine concentration associated with cardiac surgery,” wrote Dr. Frederic T. Billings IV, professor of medicine at Vanderbilt University, Nashville, Tenn., and his collaborators. The findings (JAMA 2016 Feb 23. doi: 10.1001/jama.2016.0548) were published concurrently with his presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In what Dr. Phil B. Fontanarosa, executive editor of JAMA and comoderator of the late-breaking trials session at the meeting, described as “really an elegant clinical trial,” Dr. Billings and his collaborators enrolled 615 patients over 5 years at Vanderbilt University Medical Center.
Patients undergoing elective coronary artery bypass grafting, valvular heart surgery, or ascending aortic surgery were eligible. Patients were excluded if they had prior statin intolerance, acute coronary syndrome, or liver dysfunction; were taking potent CYP3A4 inhibitors or cyclosporine; were receiving renal replacement therapy or had a kidney transplant; or were pregnant.
Both patients currently on a statin and patients naive to statins were recruited. Statin-naive patients received 80 mg atorvastatin the day before surgery, and then 40 mg of atorvastatin on the day of surgery and daily following surgery, or a matched placebo regimen.
Patients who were already on a statin received the study drug only on days that they would not have received a statin if treated according to the current standard of care. It was deemed unethical to allow those patients to receive placebo during and after surgery, since observational studies suggested that doing so might increase their potential for AKI.
For those patients already on a statin, this meant that they stayed on their usual regimen until the day of surgery, and then were randomized to receive either 80 mg of atorvastatin on the day of surgery and 40 mg of atorvastatin the day after surgery, or a matching placebo regimen.
For both groups, the study drug was given at least 3 hours before surgery on the day of surgery.
Randomization was stratified for prior statin use, for chronic kidney disease, and by history of diabetes. The 199 patients naive to statins and the 416 already on a statin were similar in demographic and health characteristics. Median age was 67 years, 188 (30.6%) were women; 202 participants (32.8%) had diabetes.
The primary outcome measure was diagnosis of AKI, defined as an increase of 0.3 mg/dL in serum creatinine, or beginning renal replacement therapy within 48 hours of surgery. Baseline serum creatinine was measured no more than 7 days prior to surgery.
AKI occurred in 64 of 308 patients (20.8%) in the atorvastatin group, and in 60 of 307 patients (19.5%) receiving placebo overall (P = .75). For those naive to statins, 21.6% of the atorvastatin group and 13.4% of the placebo group developed AKI (P = .15). Overall, 179 enrolled patients had CKD, and the incidence of AKI did not significantly differ in the atorvastatin and the placebo arms of this subgroup.
The subpopulation of participants with CKD who were statin naive (n = 36), however, saw an increased incidence of AKI with atorvastatin compared to placebo. AKI occurred in 9 of 17 patients (52.9%) given atorvastatin, and in 3 of 19 (15.8%) given placebo group (RR, 3.35[95% confidence interval 0.12 to 10.05]; P = .03). “It should be noted that the number of patients in this subgroup was particularly small, leading to a wide confidence interval and an increased chance of type 1 error,” said Dr. Billings.
Secondary outcome measures were maximum increase in creatinine concentration from baseline through postop day 2, delirium in the ICU, degree of myocardial injury, and incidence of postoperative pneumonia, atrial fibrillation, or stroke. Perioperative atorvastatin administration did not affect any of these endpoints.
The safety analysis showed no indications of increased risk of skeletal muscle or liver injury with perioperative atorvastatin use.
In the real world, “Most patients presenting for cardiac surgery … are already taking statins, and in the current study there was little evidence that continuation or withdrawal from statin treatment on the day of surgery and postoperative day 1 affects AKI,” wrote Dr. Billings and his coauthors.
Study limitations included its single-center design, and the use of AKI criteria that may not be sensitive to late-developing AKI. Also, for enrolled patients who were already on statins, statin exposure was not reduced in comparison with usual care.
After the presentation, Dr. Billings reported that the researchers also collected information about other biomarkers that may signal AKI, including IgM. He and his collaborators plan later publication of those data after a full analysis.
The National Institutes of Health and the Vanderbilt University Medical Center department of anesthesiology funded the study. Dr. Brown reported receiving grants from Shire Pharmaceuticals and New Haven Pharmaceuticals, and personal fees from Novartis Pharmaceuticals and Alnylam Pharmaceuticals. The other authors reported no conflicts of interest.
On Twitter @karioakes
AT THE CRITICAL CARE CONGRESS
Key clinical point: Perioperative atorvastatin did not protect against acute kidney injury after cardiac surgery.
Major finding: Acute kidney injury occurred in 64 of 308 patients (20.8%) in the atorvastatin group, and in 60 of 307 patients (19.5%) receiving placebo overall, a nonsignificant difference (P = .75).
Data source: Randomized, double-blinded, placebo-controlled trial of 615 adults who underwent cardiac surgery.
Disclosures: The National Institutes of Health and the Vanderbilt University Medical Center department of anesthesiology funded the study. Dr. Brown reported receiving grants from Shire Pharmaceuticals and New Haven Pharmaceuticals, and personal fees from Novartis Pharmaceuticals and Alnylam Pharmaceuticals. The other authors reported no conflicts of interest.
Adding azithromycin cuts postcesarean maternal infections
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Prophylactic azithromycin added to standard antibiotics decreased maternal infections after cesarean.
Major finding: The number needed to treat to prevent one postsurgical infection was 17.
Data source: The randomized, placebo-controlled trial comprised 2,013 women.
Disclosures: The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
VIDEO: Beware legal land mines when working with PAs, NPs
AUSTIN, TEX. – As use of mid-level providers grows, legal risks for practices also can rise.
In this video interview at an American Health Lawyers Association conference, attorney Alex T. Krouse discusses common liability dangers that arise when working with physician assistants and nurse practitioners. Mr. Krouse also speaks about frequent billing errors that can happen within provider teams and breaks down the difference between physician supervision and physician collaboration.
On Twitter @legal_med
AUSTIN, TEX. – As use of mid-level providers grows, legal risks for practices also can rise.
In this video interview at an American Health Lawyers Association conference, attorney Alex T. Krouse discusses common liability dangers that arise when working with physician assistants and nurse practitioners. Mr. Krouse also speaks about frequent billing errors that can happen within provider teams and breaks down the difference between physician supervision and physician collaboration.
On Twitter @legal_med
AUSTIN, TEX. – As use of mid-level providers grows, legal risks for practices also can rise.
In this video interview at an American Health Lawyers Association conference, attorney Alex T. Krouse discusses common liability dangers that arise when working with physician assistants and nurse practitioners. Mr. Krouse also speaks about frequent billing errors that can happen within provider teams and breaks down the difference between physician supervision and physician collaboration.
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS & HOSPITALS LAW INSTITUTE
Prevention driving increase in mastectomies
The overall mastectomy rate rose 36% from 2005 to 2013, even though “the incidence of breast cancer overall remained stable,” according to the Agency for Healthcare Research and Quality (AHRQ).
The rate of bilateral mastectomies jumped 226% over that time period, going from 9.1 per 100,000 adult women in 2005 to 29.7 per 100,000 in 2013. The unilateral mastectomy rate, starting at 57.3 per 100,000 women in 2005, rose to 69.8 in 2009 and then fell to 60.6 in 2013, for an increase of 6% overall, the AHRQ reported.
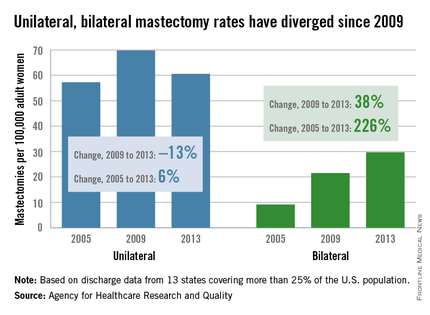
The rate of bilateral mastectomies without any cancer diagnosis increased from 2.0 to 4.4 per 100,000 from 2005 to 2013, and the unilateral rate rose from 2.7 to 3.7 per 100,000, the report noted.
Both unilateral and bilateral mastectomies are increasingly performed as outpatient procedures. The rate done in hospital-based ambulatory surgery settings nearly doubled from 16.1 to 31 per 100,000 women, and the overall proportion performed in ambulatory settings reached 45% in 2013, the AHRQ said.
The analysis shows that “more women are opting for mastectomies, particularly preventive double mastectomies, and more of those surgeries are being done as outpatient procedures,” AHRQ Director Rick Kronick, Ph.D., said in a written statement. These “changing patterns of care for breast cancer [highlight] the need for further evidence about the effects of choices women are making on their health, well-being, and safety.”
The analysis of the State Inpatient Databases and the State Ambulatory Surgery and Services Databases involved data from 13 states that had cases in both databases and used coding that allowed identification of unilateral versus bilateral mastectomies. Those 13 states represent more than 25% of the U.S. population.
The overall mastectomy rate rose 36% from 2005 to 2013, even though “the incidence of breast cancer overall remained stable,” according to the Agency for Healthcare Research and Quality (AHRQ).
The rate of bilateral mastectomies jumped 226% over that time period, going from 9.1 per 100,000 adult women in 2005 to 29.7 per 100,000 in 2013. The unilateral mastectomy rate, starting at 57.3 per 100,000 women in 2005, rose to 69.8 in 2009 and then fell to 60.6 in 2013, for an increase of 6% overall, the AHRQ reported.
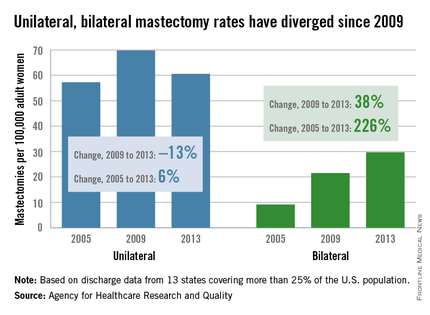
The rate of bilateral mastectomies without any cancer diagnosis increased from 2.0 to 4.4 per 100,000 from 2005 to 2013, and the unilateral rate rose from 2.7 to 3.7 per 100,000, the report noted.
Both unilateral and bilateral mastectomies are increasingly performed as outpatient procedures. The rate done in hospital-based ambulatory surgery settings nearly doubled from 16.1 to 31 per 100,000 women, and the overall proportion performed in ambulatory settings reached 45% in 2013, the AHRQ said.
The analysis shows that “more women are opting for mastectomies, particularly preventive double mastectomies, and more of those surgeries are being done as outpatient procedures,” AHRQ Director Rick Kronick, Ph.D., said in a written statement. These “changing patterns of care for breast cancer [highlight] the need for further evidence about the effects of choices women are making on their health, well-being, and safety.”
The analysis of the State Inpatient Databases and the State Ambulatory Surgery and Services Databases involved data from 13 states that had cases in both databases and used coding that allowed identification of unilateral versus bilateral mastectomies. Those 13 states represent more than 25% of the U.S. population.
The overall mastectomy rate rose 36% from 2005 to 2013, even though “the incidence of breast cancer overall remained stable,” according to the Agency for Healthcare Research and Quality (AHRQ).
The rate of bilateral mastectomies jumped 226% over that time period, going from 9.1 per 100,000 adult women in 2005 to 29.7 per 100,000 in 2013. The unilateral mastectomy rate, starting at 57.3 per 100,000 women in 2005, rose to 69.8 in 2009 and then fell to 60.6 in 2013, for an increase of 6% overall, the AHRQ reported.
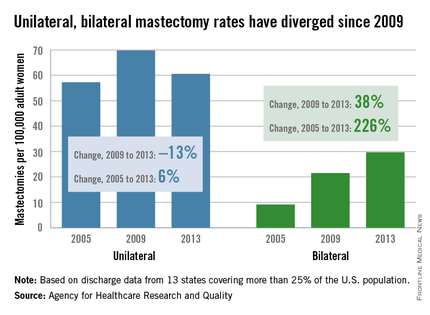
The rate of bilateral mastectomies without any cancer diagnosis increased from 2.0 to 4.4 per 100,000 from 2005 to 2013, and the unilateral rate rose from 2.7 to 3.7 per 100,000, the report noted.
Both unilateral and bilateral mastectomies are increasingly performed as outpatient procedures. The rate done in hospital-based ambulatory surgery settings nearly doubled from 16.1 to 31 per 100,000 women, and the overall proportion performed in ambulatory settings reached 45% in 2013, the AHRQ said.
The analysis shows that “more women are opting for mastectomies, particularly preventive double mastectomies, and more of those surgeries are being done as outpatient procedures,” AHRQ Director Rick Kronick, Ph.D., said in a written statement. These “changing patterns of care for breast cancer [highlight] the need for further evidence about the effects of choices women are making on their health, well-being, and safety.”
The analysis of the State Inpatient Databases and the State Ambulatory Surgery and Services Databases involved data from 13 states that had cases in both databases and used coding that allowed identification of unilateral versus bilateral mastectomies. Those 13 states represent more than 25% of the U.S. population.