User login
Official Newspaper of the American College of Surgeons
Postop surveillance sufficient for stage I testicular cancer
Surveillance is sufficient for most men with stage I seminoma after successful orchiectomy, according to the findings of the largest study ever performed to address the issue.
The 1,822 men followed only with surveillance in Denmark had an excellent disease-specific survival of 99.5%, Dr. Mette Saskø Mortensen said at a press briefing highlighting research to be presented at the upcoming American Society of Clinical Oncology annual meeting. Only 10 men died of testicular cancer or treatment-related causes during a median follow-up of 15.4 years.
This finding means that for every 1,000 men followed by a surveillance program, only 4 will die within 10 years, said incoming ASCO president Dr. Clifford Hudis, chief of breast cancer medicine service at Memorial Sloan-Kettering Cancer Center in New York.
He described the study as one of several recent reminders that sometimes "less is more" in patient care and noted that opting for surveillance spares patients from the harmful side effects of chemotherapy and radiation without diminishing their chances for long-term survival.
Seminoma is a relatively rare cancer, but it is the most common solid tumor among young men. Initial treatment is typically orchiectomy, but no standard postoperative management strategy has been established. The current results will likely accelerate the trend toward surveillance in the United States, where roughly 50% of men undergo either radiotherapy or chemotherapy with carboplatin after surgery.
Overall, 355 (19.5%) of the 1,822 men experienced a relapse during surveillance, said Dr. Mortensen, a PhD student in the oncology department at Copenhagen University Hospital.
The median time to relapse was 13.7 months, with the majority of patients (72.4%) relapsing within the first 2 years. Another 20.3% relapsed within years 2-5 and 7.3% after 5 years.
"With only 19.5% of the patients relapsing, the surveillance strategy spares the remaining 80% of patients from unnecessary treatment after orchiectomy," Dr. Mortensen said. "Surveillance is a safe strategy for stage I seminoma patients."
Surveillance has been the main follow-up strategy for stage I seminoma in Denmark since 1984, and consists of 5 years of scheduled clinical visits, computed tomography scans/chest x-rays, and blood measurements of tumor markers. Men in the analysis were diagnosed from 1984 to 2008, and their data were collected up to December 2012 from patient files and linked national registries.
As observed in other smaller studies, the risk for relapse was increased with elevated human chorionic gonadotropin levels of more than 200 IU/L, vascular invasion, and tumors larger than 4 cm, Dr. Mortensen said.
The study was supported in part by the Danish Cancer Society, Danish Research Foundation and the Preben and Anna Simonsen Foundation. Dr. Mortensen reported having no financial disclosures.
Surveillance is sufficient for most men with stage I seminoma after successful orchiectomy, according to the findings of the largest study ever performed to address the issue.
The 1,822 men followed only with surveillance in Denmark had an excellent disease-specific survival of 99.5%, Dr. Mette Saskø Mortensen said at a press briefing highlighting research to be presented at the upcoming American Society of Clinical Oncology annual meeting. Only 10 men died of testicular cancer or treatment-related causes during a median follow-up of 15.4 years.
This finding means that for every 1,000 men followed by a surveillance program, only 4 will die within 10 years, said incoming ASCO president Dr. Clifford Hudis, chief of breast cancer medicine service at Memorial Sloan-Kettering Cancer Center in New York.
He described the study as one of several recent reminders that sometimes "less is more" in patient care and noted that opting for surveillance spares patients from the harmful side effects of chemotherapy and radiation without diminishing their chances for long-term survival.
Seminoma is a relatively rare cancer, but it is the most common solid tumor among young men. Initial treatment is typically orchiectomy, but no standard postoperative management strategy has been established. The current results will likely accelerate the trend toward surveillance in the United States, where roughly 50% of men undergo either radiotherapy or chemotherapy with carboplatin after surgery.
Overall, 355 (19.5%) of the 1,822 men experienced a relapse during surveillance, said Dr. Mortensen, a PhD student in the oncology department at Copenhagen University Hospital.
The median time to relapse was 13.7 months, with the majority of patients (72.4%) relapsing within the first 2 years. Another 20.3% relapsed within years 2-5 and 7.3% after 5 years.
"With only 19.5% of the patients relapsing, the surveillance strategy spares the remaining 80% of patients from unnecessary treatment after orchiectomy," Dr. Mortensen said. "Surveillance is a safe strategy for stage I seminoma patients."
Surveillance has been the main follow-up strategy for stage I seminoma in Denmark since 1984, and consists of 5 years of scheduled clinical visits, computed tomography scans/chest x-rays, and blood measurements of tumor markers. Men in the analysis were diagnosed from 1984 to 2008, and their data were collected up to December 2012 from patient files and linked national registries.
As observed in other smaller studies, the risk for relapse was increased with elevated human chorionic gonadotropin levels of more than 200 IU/L, vascular invasion, and tumors larger than 4 cm, Dr. Mortensen said.
The study was supported in part by the Danish Cancer Society, Danish Research Foundation and the Preben and Anna Simonsen Foundation. Dr. Mortensen reported having no financial disclosures.
Surveillance is sufficient for most men with stage I seminoma after successful orchiectomy, according to the findings of the largest study ever performed to address the issue.
The 1,822 men followed only with surveillance in Denmark had an excellent disease-specific survival of 99.5%, Dr. Mette Saskø Mortensen said at a press briefing highlighting research to be presented at the upcoming American Society of Clinical Oncology annual meeting. Only 10 men died of testicular cancer or treatment-related causes during a median follow-up of 15.4 years.
This finding means that for every 1,000 men followed by a surveillance program, only 4 will die within 10 years, said incoming ASCO president Dr. Clifford Hudis, chief of breast cancer medicine service at Memorial Sloan-Kettering Cancer Center in New York.
He described the study as one of several recent reminders that sometimes "less is more" in patient care and noted that opting for surveillance spares patients from the harmful side effects of chemotherapy and radiation without diminishing their chances for long-term survival.
Seminoma is a relatively rare cancer, but it is the most common solid tumor among young men. Initial treatment is typically orchiectomy, but no standard postoperative management strategy has been established. The current results will likely accelerate the trend toward surveillance in the United States, where roughly 50% of men undergo either radiotherapy or chemotherapy with carboplatin after surgery.
Overall, 355 (19.5%) of the 1,822 men experienced a relapse during surveillance, said Dr. Mortensen, a PhD student in the oncology department at Copenhagen University Hospital.
The median time to relapse was 13.7 months, with the majority of patients (72.4%) relapsing within the first 2 years. Another 20.3% relapsed within years 2-5 and 7.3% after 5 years.
"With only 19.5% of the patients relapsing, the surveillance strategy spares the remaining 80% of patients from unnecessary treatment after orchiectomy," Dr. Mortensen said. "Surveillance is a safe strategy for stage I seminoma patients."
Surveillance has been the main follow-up strategy for stage I seminoma in Denmark since 1984, and consists of 5 years of scheduled clinical visits, computed tomography scans/chest x-rays, and blood measurements of tumor markers. Men in the analysis were diagnosed from 1984 to 2008, and their data were collected up to December 2012 from patient files and linked national registries.
As observed in other smaller studies, the risk for relapse was increased with elevated human chorionic gonadotropin levels of more than 200 IU/L, vascular invasion, and tumors larger than 4 cm, Dr. Mortensen said.
The study was supported in part by the Danish Cancer Society, Danish Research Foundation and the Preben and Anna Simonsen Foundation. Dr. Mortensen reported having no financial disclosures.
AT THE ASCO 2013 PRESSCAST
Major finding: The 10-year cancer-specific survival was 99.6%.
Data source: Retrospective, nationwide cohort study of surveillance in 1,822 men with stage I seminoma.
Disclosures: The study was supported in part by the Danish Cancer Society, Danish Research Foundation, and the Preben and Anna Simonsen Foundation. Dr. Mortensen reported having no financial disclosures.
Pulley stitch: A go-to for defects under tension
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ATLANTIC DERMATOLOGICAL CONFERENCE
Major finding: Key numerical finding (e.g., number needed to treat to prevent one death/event; number lived or died as result of intervention). Maximum 10 words/1 sentence.
Data source: Include type of study (e.g., randomized, placebo controlled trial; retrospective case-control study). Include number in the study.
Disclosures: Sponsor of study, funding source, relevant disclosures. If author has no relevant disclosures, "Dr. X reported having no financial disclosures." If necessary, "Meeting Y did not require reports of financial disclosures." Check meeting website because many list disclosures. Written in sentence form.
Standard-dose radiation bests high-dose radiation in advanced NSCLC
Standard-dose radiation produced better overall survival and locoregional control than did high-dose radiation when given with concurrent chemotherapy in patients with newly diagnosed stage III non–small cell lung cancer in the phase III, randomized RTOG 0617 trial.
Patients on the high dose had a 56% greater risk of death than those on a standard 60 Gy dose. Median overall survival times were 18.5 months with high-dose radiation and 28.7 months with a standard dose (hazard ratio, 1.56; P = .0007).
The risk of local failure also was increased by 37% in the high-dose arm (HR, 1.37; P = .03).
"At this point, there is no clear reason for the poor outcome we experienced on the high-dose arm," lead author Dr. Jeffrey Bradley said in a press briefing highlighting studies to be presented at the upcoming annual meeting of the American Society of Clinical Oncology (ASCO).
The most likely culprit is unreported toxicities, although other possible explanations are increased heart dose, longer duration of therapy, or a combination of these factors, he said.
The results are surprising because conventional thinking has been that higher doses of radiation would more effectively kill the tumor and thereby improve survival.
A phase-III trial in the 1970s established the standard radiation dose of 60 Gy in this setting but, over time, several radiation dose-ranging phase-II studies have reported promising results and improved median survival times with radiation doses up to 74 Gy, explained Dr. Bradley, professor of radiation oncology and chief of the thoracic service at Washington University, St. Louis.
At the same time, improvements in technology such as three-dimensional radiation therapy (RT) and intensity-modulated RT techniques have made RT delivery more precise, allowing organs and tissues sensitive to radiation to receive less radiation while the tumor receives more. This technique was explored in Radiation Therapy Oncology Group (RTOG) 0617.
"This is a very surprising result, especially when using these special radiation techniques that were designed to be more precise, you would expect that the outcome would be better," ASCO president Sandra Swain, medical director of the Washington (D.C.) Cancer Institute, told reporters. "This should really put an end to higher-dose treatments, given the better outcomes in the standard-dose arms."
Dr. Bradley said, "A lot of phase-III trials turn out negative when phase-II trials look good, so I think it was good to do a phase-III trial and get this answered."
RTOG 0617 randomly assigned 464 patients with newly diagnosed, unresected stage-III non–small cell lung cancer to conformal RT to 60 Gy, five times per week for 6 weeks or to 74 Gy five times per week for 7.5 weeks. All patients received concurrent chemotherapy with weekly paclitaxel (Taxol) and carboplatin, with a second randomization for patients to receive consolidation chemotherapy with or without cetuximab (Erbitux).
Among the 419 patients available for analysis at 18 months, local failure rates were 25% with standard-dose RT and 34.3% with high-dose RT (P = .03, as noted above), Dr. Bradley reported.
Median 18-month overall survival rates were 67% with the standard radiation dose vs. 54% with the high dose.
Median overall survival times in both groups were higher than expected, but "the overall survival benefit of 60 Gy is independent of the cetuximab question," he said. Data from that portion of the trial are expected to be reported in 2014.
Finally, the only significant difference in physician-reported side effects was a slightly higher rate of esophagitis in the high-dose arms (21% vs. 7%).
Full details of RTOG 0617 (abstract 7501) will be reported 10:15 a.m. on June 4 at ASCO’s annual meeting in Chicago.
The study was supported by the National Cancer Institute. Dr. Bradley reported having no relevant financial disclosures. A coauthor reported research funding from the NCI.
Standard-dose radiation produced better overall survival and locoregional control than did high-dose radiation when given with concurrent chemotherapy in patients with newly diagnosed stage III non–small cell lung cancer in the phase III, randomized RTOG 0617 trial.
Patients on the high dose had a 56% greater risk of death than those on a standard 60 Gy dose. Median overall survival times were 18.5 months with high-dose radiation and 28.7 months with a standard dose (hazard ratio, 1.56; P = .0007).
The risk of local failure also was increased by 37% in the high-dose arm (HR, 1.37; P = .03).
"At this point, there is no clear reason for the poor outcome we experienced on the high-dose arm," lead author Dr. Jeffrey Bradley said in a press briefing highlighting studies to be presented at the upcoming annual meeting of the American Society of Clinical Oncology (ASCO).
The most likely culprit is unreported toxicities, although other possible explanations are increased heart dose, longer duration of therapy, or a combination of these factors, he said.
The results are surprising because conventional thinking has been that higher doses of radiation would more effectively kill the tumor and thereby improve survival.
A phase-III trial in the 1970s established the standard radiation dose of 60 Gy in this setting but, over time, several radiation dose-ranging phase-II studies have reported promising results and improved median survival times with radiation doses up to 74 Gy, explained Dr. Bradley, professor of radiation oncology and chief of the thoracic service at Washington University, St. Louis.
At the same time, improvements in technology such as three-dimensional radiation therapy (RT) and intensity-modulated RT techniques have made RT delivery more precise, allowing organs and tissues sensitive to radiation to receive less radiation while the tumor receives more. This technique was explored in Radiation Therapy Oncology Group (RTOG) 0617.
"This is a very surprising result, especially when using these special radiation techniques that were designed to be more precise, you would expect that the outcome would be better," ASCO president Sandra Swain, medical director of the Washington (D.C.) Cancer Institute, told reporters. "This should really put an end to higher-dose treatments, given the better outcomes in the standard-dose arms."
Dr. Bradley said, "A lot of phase-III trials turn out negative when phase-II trials look good, so I think it was good to do a phase-III trial and get this answered."
RTOG 0617 randomly assigned 464 patients with newly diagnosed, unresected stage-III non–small cell lung cancer to conformal RT to 60 Gy, five times per week for 6 weeks or to 74 Gy five times per week for 7.5 weeks. All patients received concurrent chemotherapy with weekly paclitaxel (Taxol) and carboplatin, with a second randomization for patients to receive consolidation chemotherapy with or without cetuximab (Erbitux).
Among the 419 patients available for analysis at 18 months, local failure rates were 25% with standard-dose RT and 34.3% with high-dose RT (P = .03, as noted above), Dr. Bradley reported.
Median 18-month overall survival rates were 67% with the standard radiation dose vs. 54% with the high dose.
Median overall survival times in both groups were higher than expected, but "the overall survival benefit of 60 Gy is independent of the cetuximab question," he said. Data from that portion of the trial are expected to be reported in 2014.
Finally, the only significant difference in physician-reported side effects was a slightly higher rate of esophagitis in the high-dose arms (21% vs. 7%).
Full details of RTOG 0617 (abstract 7501) will be reported 10:15 a.m. on June 4 at ASCO’s annual meeting in Chicago.
The study was supported by the National Cancer Institute. Dr. Bradley reported having no relevant financial disclosures. A coauthor reported research funding from the NCI.
Standard-dose radiation produced better overall survival and locoregional control than did high-dose radiation when given with concurrent chemotherapy in patients with newly diagnosed stage III non–small cell lung cancer in the phase III, randomized RTOG 0617 trial.
Patients on the high dose had a 56% greater risk of death than those on a standard 60 Gy dose. Median overall survival times were 18.5 months with high-dose radiation and 28.7 months with a standard dose (hazard ratio, 1.56; P = .0007).
The risk of local failure also was increased by 37% in the high-dose arm (HR, 1.37; P = .03).
"At this point, there is no clear reason for the poor outcome we experienced on the high-dose arm," lead author Dr. Jeffrey Bradley said in a press briefing highlighting studies to be presented at the upcoming annual meeting of the American Society of Clinical Oncology (ASCO).
The most likely culprit is unreported toxicities, although other possible explanations are increased heart dose, longer duration of therapy, or a combination of these factors, he said.
The results are surprising because conventional thinking has been that higher doses of radiation would more effectively kill the tumor and thereby improve survival.
A phase-III trial in the 1970s established the standard radiation dose of 60 Gy in this setting but, over time, several radiation dose-ranging phase-II studies have reported promising results and improved median survival times with radiation doses up to 74 Gy, explained Dr. Bradley, professor of radiation oncology and chief of the thoracic service at Washington University, St. Louis.
At the same time, improvements in technology such as three-dimensional radiation therapy (RT) and intensity-modulated RT techniques have made RT delivery more precise, allowing organs and tissues sensitive to radiation to receive less radiation while the tumor receives more. This technique was explored in Radiation Therapy Oncology Group (RTOG) 0617.
"This is a very surprising result, especially when using these special radiation techniques that were designed to be more precise, you would expect that the outcome would be better," ASCO president Sandra Swain, medical director of the Washington (D.C.) Cancer Institute, told reporters. "This should really put an end to higher-dose treatments, given the better outcomes in the standard-dose arms."
Dr. Bradley said, "A lot of phase-III trials turn out negative when phase-II trials look good, so I think it was good to do a phase-III trial and get this answered."
RTOG 0617 randomly assigned 464 patients with newly diagnosed, unresected stage-III non–small cell lung cancer to conformal RT to 60 Gy, five times per week for 6 weeks or to 74 Gy five times per week for 7.5 weeks. All patients received concurrent chemotherapy with weekly paclitaxel (Taxol) and carboplatin, with a second randomization for patients to receive consolidation chemotherapy with or without cetuximab (Erbitux).
Among the 419 patients available for analysis at 18 months, local failure rates were 25% with standard-dose RT and 34.3% with high-dose RT (P = .03, as noted above), Dr. Bradley reported.
Median 18-month overall survival rates were 67% with the standard radiation dose vs. 54% with the high dose.
Median overall survival times in both groups were higher than expected, but "the overall survival benefit of 60 Gy is independent of the cetuximab question," he said. Data from that portion of the trial are expected to be reported in 2014.
Finally, the only significant difference in physician-reported side effects was a slightly higher rate of esophagitis in the high-dose arms (21% vs. 7%).
Full details of RTOG 0617 (abstract 7501) will be reported 10:15 a.m. on June 4 at ASCO’s annual meeting in Chicago.
The study was supported by the National Cancer Institute. Dr. Bradley reported having no relevant financial disclosures. A coauthor reported research funding from the NCI.
FROM THE ASCO 2013 PRESSCAST
Major finding: Patients with stage-III non–small cell lung cancer who received high-dose radiation had a 56% greater risk of death than those on a standard 60 Gy dose.
Data source: Phase-III randomized trial in 464 patients with stage-III non–small cell lung cancer.
Disclosures: The study was supported by the National Cancer Institute. Dr. Bradley reported having no relevant financial disclosures. A coauthor reported research funding from the NCI.
FDA approves radiotherapy for metastatic prostate cancer
Radium-223 dichloride, an alpha-particle–emitting radioactive agent, has been approved for treating men with castration-resistant prostate cancer that has spread to the bones, the Food and Drug Administration announced on May 15.
The agent "binds with minerals in the bone to deliver radiation directly to bone tumors," Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, noted in the statement.
Ra-223 is the second drug for prostate cancer approved by the FDA in the last year that has been shown to extend the survival of men with metastatic prostate cancer, Dr. Pazdur noted. Enzalutamide (Xtandi), an androgen receptor inhibitor, was approved in August 2012 for treating men with metastatic castration-resistant prostate cancer who were previously treated with docetaxel.
Approval of the radium-223 treatment, which will be marketed as Xofigo by Bayer Pharmaceuticals, was based on a phase III study of men with symptomatic castration-resistant prostate cancer with symptomatic bone metastases, and no other metastases, randomized to treatment with radium 233 (541 men) every 4 weeks for six cycles or placebo (268 men). All patients received best standard of care, which included external-beam radiation therapy, corticosteroids, antiandrogens, estrogens, estramustine, or ketoconazole.
In an interim analysis, overall survival, the primary endpoint, was a median of 14 months among those in the radiotherapy arm, compared with 11.2 months among those on placebo, a highly statistically significant improvement, with a hazard ratio of 0.695. An updated exploratory analysis conducted later in the trial "confirmed Xofigo’s ability to extend overall survival," the FDA statement noted.
(The prescribing information states that in the updated analysis, median survival was 14.9 months vs. 11.3 months among those on placebo, with a hazard ratio of 0.695).
The most common side effects reported during clinical trials in men receiving the treatment, in 10% or more of patients, were nausea, diarrhea, vomiting and peripheral edema. The most common laboratory abnormalities detected, in 10% or more of patients, were anemia, lymphocytopenia, leukopenia, thrombocytopenia, and neutropenia.
Xofigo comes in a solution and is administered at 4-week intervals for six injection cycles; it is slowly administered intravenously over 1 minute. Safety and efficacy of more than six injections has not been studied, according to the prescribing information.
Radium-223 dichloride, an alpha-particle–emitting radioactive agent, has been approved for treating men with castration-resistant prostate cancer that has spread to the bones, the Food and Drug Administration announced on May 15.
The agent "binds with minerals in the bone to deliver radiation directly to bone tumors," Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, noted in the statement.
Ra-223 is the second drug for prostate cancer approved by the FDA in the last year that has been shown to extend the survival of men with metastatic prostate cancer, Dr. Pazdur noted. Enzalutamide (Xtandi), an androgen receptor inhibitor, was approved in August 2012 for treating men with metastatic castration-resistant prostate cancer who were previously treated with docetaxel.
Approval of the radium-223 treatment, which will be marketed as Xofigo by Bayer Pharmaceuticals, was based on a phase III study of men with symptomatic castration-resistant prostate cancer with symptomatic bone metastases, and no other metastases, randomized to treatment with radium 233 (541 men) every 4 weeks for six cycles or placebo (268 men). All patients received best standard of care, which included external-beam radiation therapy, corticosteroids, antiandrogens, estrogens, estramustine, or ketoconazole.
In an interim analysis, overall survival, the primary endpoint, was a median of 14 months among those in the radiotherapy arm, compared with 11.2 months among those on placebo, a highly statistically significant improvement, with a hazard ratio of 0.695. An updated exploratory analysis conducted later in the trial "confirmed Xofigo’s ability to extend overall survival," the FDA statement noted.
(The prescribing information states that in the updated analysis, median survival was 14.9 months vs. 11.3 months among those on placebo, with a hazard ratio of 0.695).
The most common side effects reported during clinical trials in men receiving the treatment, in 10% or more of patients, were nausea, diarrhea, vomiting and peripheral edema. The most common laboratory abnormalities detected, in 10% or more of patients, were anemia, lymphocytopenia, leukopenia, thrombocytopenia, and neutropenia.
Xofigo comes in a solution and is administered at 4-week intervals for six injection cycles; it is slowly administered intravenously over 1 minute. Safety and efficacy of more than six injections has not been studied, according to the prescribing information.
Radium-223 dichloride, an alpha-particle–emitting radioactive agent, has been approved for treating men with castration-resistant prostate cancer that has spread to the bones, the Food and Drug Administration announced on May 15.
The agent "binds with minerals in the bone to deliver radiation directly to bone tumors," Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, noted in the statement.
Ra-223 is the second drug for prostate cancer approved by the FDA in the last year that has been shown to extend the survival of men with metastatic prostate cancer, Dr. Pazdur noted. Enzalutamide (Xtandi), an androgen receptor inhibitor, was approved in August 2012 for treating men with metastatic castration-resistant prostate cancer who were previously treated with docetaxel.
Approval of the radium-223 treatment, which will be marketed as Xofigo by Bayer Pharmaceuticals, was based on a phase III study of men with symptomatic castration-resistant prostate cancer with symptomatic bone metastases, and no other metastases, randomized to treatment with radium 233 (541 men) every 4 weeks for six cycles or placebo (268 men). All patients received best standard of care, which included external-beam radiation therapy, corticosteroids, antiandrogens, estrogens, estramustine, or ketoconazole.
In an interim analysis, overall survival, the primary endpoint, was a median of 14 months among those in the radiotherapy arm, compared with 11.2 months among those on placebo, a highly statistically significant improvement, with a hazard ratio of 0.695. An updated exploratory analysis conducted later in the trial "confirmed Xofigo’s ability to extend overall survival," the FDA statement noted.
(The prescribing information states that in the updated analysis, median survival was 14.9 months vs. 11.3 months among those on placebo, with a hazard ratio of 0.695).
The most common side effects reported during clinical trials in men receiving the treatment, in 10% or more of patients, were nausea, diarrhea, vomiting and peripheral edema. The most common laboratory abnormalities detected, in 10% or more of patients, were anemia, lymphocytopenia, leukopenia, thrombocytopenia, and neutropenia.
Xofigo comes in a solution and is administered at 4-week intervals for six injection cycles; it is slowly administered intravenously over 1 minute. Safety and efficacy of more than six injections has not been studied, according to the prescribing information.
Endovascular AAA repair superior for kidney disease patients
INDIANAPOLIS – Contrary to conventional wisdom, endovascular aneurysm repair (EVAR) provides outcomes superior to those achieved with open surgical repair of abdominal aortic aneurysm in patients with chronic renal insufficiency, a large study indicates.
"EVAR should be the first-line therapy in the patient with chronic renal insufficiency when the patient has the appropriate anatomy. However, in patients with severe renal impairment, a higher threshold should be applied for repair because the risks of both open repair and EVAR are significantly higher," Dr. Bao-Ngoc H. Nguyen declared at the annual meeting of the American Surgical Association.
"Chronic renal failure is quite prevalent in patients with abdominal aortic aneurysm: up to 30%. It is quite worrisome because any further decline in renal function in these patients could push them toward dialysis. More than that, postoperative renal failure is a predictor for early and late mortality," noted Dr. Nguyen of George Washington University, Washington.
She presented a retrospective study in patients with abdominal aortic aneurysm and chronic kidney disease. The aim, she explained, was to answer a key question: "Which one of these two treatment modalities is the lesser of two evils?"
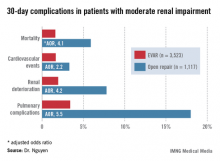
For answers, Dr. Nguyen and coinvestigators turned to the American College of Surgeons National Quality Improvement Program (NSQIP) database for 2005-2010. They identified 3,523 patients with moderate chronic renal insufficiency, defined as an estimated glomerular filtration rate (eGFR) of 30-60 mL/minute, who underwent EVAR for abdominal aortic aneurysm and 1,117 treated via open surgical repair. Another 363 EVAR patients had severe chronic renal insufficiency, with an eGFR of less than 30 mL/minute, as did 139 patients who underwent open repair. Vascular surgeons performed all procedures in this study.
Patients with moderate renal insufficiency who underwent EVAR had markedly lower 30-day rates of mortality, pulmonary complications, cardiovascular events, and postoperative renal dysfunction, including acute kidney injury, than did those who had open surgical repair. One or more adverse events occurred in 6% of the EVAR group, compared with 24.1% of open repair patients. In a multivariate analysis controlled for preoperative differences in the patient groups, those undergoing open repair had an adjusted 4.1-fold greater risk of mortality as well as a 2.2-fold increased risk of cardiovascular events, a 4.2-fold increased risk of renal deterioration including a 5.2-fold greater risk of dialysis, and additional hazards.
In contrast, among the much smaller population of patients with baseline severe chronic renal insufficiency, there was no significant difference between the two treatment groups in terms of 30-day mortality, postoperative renal deterioration, or cardiovascular complications, although pulmonary complications were an adjusted fivefold more likely in the open surgery than among EVAR patients. Of note, rates of all adverse outcomes were markedly higher in both groups than in those with moderate chronic renal insufficiency, such that one or more adverse events occurred in 16.9% of EVAR patients and 42.5% of the open repair patients with severe chronic renal insufficiency.
Discussant Dr. Michael Watkins commented that this study has one glaring shortcoming resulting from a limitation of the NSQIP database.
While NSQIP contains only validated data entered by unbiased, well-trained professionals and NSQIP is "far superior" to the various administrative databases commonly used in evaluating outcomes, it doesn’t include key details about patients’ presenting anatomy, observed Dr. Watkins, director of the vascular research laboratory at Massachusetts General Hospital, Boston.
"Was the anatomy really similar in the two groups, or were patients who underwent open repair not candidates for EVAR?" he asked.
Dr. Nguyen conceded that this constitutes a major study limitation, adding that she agrees with Dr. Watkins that anatomy should be the first and foremost factor considered in deciding upon the surgical approach in abdominal aortic aneurysm repair.
She reported having no financial conflicts.
INDIANAPOLIS – Contrary to conventional wisdom, endovascular aneurysm repair (EVAR) provides outcomes superior to those achieved with open surgical repair of abdominal aortic aneurysm in patients with chronic renal insufficiency, a large study indicates.
"EVAR should be the first-line therapy in the patient with chronic renal insufficiency when the patient has the appropriate anatomy. However, in patients with severe renal impairment, a higher threshold should be applied for repair because the risks of both open repair and EVAR are significantly higher," Dr. Bao-Ngoc H. Nguyen declared at the annual meeting of the American Surgical Association.
"Chronic renal failure is quite prevalent in patients with abdominal aortic aneurysm: up to 30%. It is quite worrisome because any further decline in renal function in these patients could push them toward dialysis. More than that, postoperative renal failure is a predictor for early and late mortality," noted Dr. Nguyen of George Washington University, Washington.
She presented a retrospective study in patients with abdominal aortic aneurysm and chronic kidney disease. The aim, she explained, was to answer a key question: "Which one of these two treatment modalities is the lesser of two evils?"
For answers, Dr. Nguyen and coinvestigators turned to the American College of Surgeons National Quality Improvement Program (NSQIP) database for 2005-2010. They identified 3,523 patients with moderate chronic renal insufficiency, defined as an estimated glomerular filtration rate (eGFR) of 30-60 mL/minute, who underwent EVAR for abdominal aortic aneurysm and 1,117 treated via open surgical repair. Another 363 EVAR patients had severe chronic renal insufficiency, with an eGFR of less than 30 mL/minute, as did 139 patients who underwent open repair. Vascular surgeons performed all procedures in this study.
Patients with moderate renal insufficiency who underwent EVAR had markedly lower 30-day rates of mortality, pulmonary complications, cardiovascular events, and postoperative renal dysfunction, including acute kidney injury, than did those who had open surgical repair. One or more adverse events occurred in 6% of the EVAR group, compared with 24.1% of open repair patients. In a multivariate analysis controlled for preoperative differences in the patient groups, those undergoing open repair had an adjusted 4.1-fold greater risk of mortality as well as a 2.2-fold increased risk of cardiovascular events, a 4.2-fold increased risk of renal deterioration including a 5.2-fold greater risk of dialysis, and additional hazards.
In contrast, among the much smaller population of patients with baseline severe chronic renal insufficiency, there was no significant difference between the two treatment groups in terms of 30-day mortality, postoperative renal deterioration, or cardiovascular complications, although pulmonary complications were an adjusted fivefold more likely in the open surgery than among EVAR patients. Of note, rates of all adverse outcomes were markedly higher in both groups than in those with moderate chronic renal insufficiency, such that one or more adverse events occurred in 16.9% of EVAR patients and 42.5% of the open repair patients with severe chronic renal insufficiency.
Discussant Dr. Michael Watkins commented that this study has one glaring shortcoming resulting from a limitation of the NSQIP database.
While NSQIP contains only validated data entered by unbiased, well-trained professionals and NSQIP is "far superior" to the various administrative databases commonly used in evaluating outcomes, it doesn’t include key details about patients’ presenting anatomy, observed Dr. Watkins, director of the vascular research laboratory at Massachusetts General Hospital, Boston.
"Was the anatomy really similar in the two groups, or were patients who underwent open repair not candidates for EVAR?" he asked.
Dr. Nguyen conceded that this constitutes a major study limitation, adding that she agrees with Dr. Watkins that anatomy should be the first and foremost factor considered in deciding upon the surgical approach in abdominal aortic aneurysm repair.
She reported having no financial conflicts.
INDIANAPOLIS – Contrary to conventional wisdom, endovascular aneurysm repair (EVAR) provides outcomes superior to those achieved with open surgical repair of abdominal aortic aneurysm in patients with chronic renal insufficiency, a large study indicates.
"EVAR should be the first-line therapy in the patient with chronic renal insufficiency when the patient has the appropriate anatomy. However, in patients with severe renal impairment, a higher threshold should be applied for repair because the risks of both open repair and EVAR are significantly higher," Dr. Bao-Ngoc H. Nguyen declared at the annual meeting of the American Surgical Association.
"Chronic renal failure is quite prevalent in patients with abdominal aortic aneurysm: up to 30%. It is quite worrisome because any further decline in renal function in these patients could push them toward dialysis. More than that, postoperative renal failure is a predictor for early and late mortality," noted Dr. Nguyen of George Washington University, Washington.
She presented a retrospective study in patients with abdominal aortic aneurysm and chronic kidney disease. The aim, she explained, was to answer a key question: "Which one of these two treatment modalities is the lesser of two evils?"
For answers, Dr. Nguyen and coinvestigators turned to the American College of Surgeons National Quality Improvement Program (NSQIP) database for 2005-2010. They identified 3,523 patients with moderate chronic renal insufficiency, defined as an estimated glomerular filtration rate (eGFR) of 30-60 mL/minute, who underwent EVAR for abdominal aortic aneurysm and 1,117 treated via open surgical repair. Another 363 EVAR patients had severe chronic renal insufficiency, with an eGFR of less than 30 mL/minute, as did 139 patients who underwent open repair. Vascular surgeons performed all procedures in this study.
Patients with moderate renal insufficiency who underwent EVAR had markedly lower 30-day rates of mortality, pulmonary complications, cardiovascular events, and postoperative renal dysfunction, including acute kidney injury, than did those who had open surgical repair. One or more adverse events occurred in 6% of the EVAR group, compared with 24.1% of open repair patients. In a multivariate analysis controlled for preoperative differences in the patient groups, those undergoing open repair had an adjusted 4.1-fold greater risk of mortality as well as a 2.2-fold increased risk of cardiovascular events, a 4.2-fold increased risk of renal deterioration including a 5.2-fold greater risk of dialysis, and additional hazards.
In contrast, among the much smaller population of patients with baseline severe chronic renal insufficiency, there was no significant difference between the two treatment groups in terms of 30-day mortality, postoperative renal deterioration, or cardiovascular complications, although pulmonary complications were an adjusted fivefold more likely in the open surgery than among EVAR patients. Of note, rates of all adverse outcomes were markedly higher in both groups than in those with moderate chronic renal insufficiency, such that one or more adverse events occurred in 16.9% of EVAR patients and 42.5% of the open repair patients with severe chronic renal insufficiency.
Discussant Dr. Michael Watkins commented that this study has one glaring shortcoming resulting from a limitation of the NSQIP database.
While NSQIP contains only validated data entered by unbiased, well-trained professionals and NSQIP is "far superior" to the various administrative databases commonly used in evaluating outcomes, it doesn’t include key details about patients’ presenting anatomy, observed Dr. Watkins, director of the vascular research laboratory at Massachusetts General Hospital, Boston.
"Was the anatomy really similar in the two groups, or were patients who underwent open repair not candidates for EVAR?" he asked.
Dr. Nguyen conceded that this constitutes a major study limitation, adding that she agrees with Dr. Watkins that anatomy should be the first and foremost factor considered in deciding upon the surgical approach in abdominal aortic aneurysm repair.
She reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major Finding: Patients with moderate chronic renal insufficiency who underwent open surgical repair of abdominal aortic aneurysm had a 4.2-fold greater risk of postoperative renal deterioration than did those who had an endovascular aneurysm repair.
Data Source: A retrospective study of a large national surgical database.
Disclosures: The presenter reported having no conflicts of interest.
Surgical educators flag training gaps
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
The source of their ire is a detailed new survey of the nation’s subspecialty fellowship program directors. Today 80% of graduating general surgery residents seek these year-long fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical areas. The surveyed program directors indicated many trainees arrive unprepared in essential areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Samer Mattar declared in presenting the survey results at the annual meeting of the American Surgical Association.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey and is an indication of the importance educators place on the subject matter, said Dr. Mattar of Indiana University, Indianapolis.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – academics and scholarship," Dr. Mattar noted in summarizing the survey results.
The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their residency rather than to push their skills to the next level. Among the key survey findings:
• Forty-three percent of program directors felt incoming fellows were unable to independently perform half an hour of a major procedure.
• Thirty percent of incoming fellows couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Fifty-six percent were unable to laparoscopically suture and tie knots properly, and 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter were deemed unable to recognize early signs of complications.
• Nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented.
• Only 51% of program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although fellows did show marked improvement in these areas as the year went on.
• A large majority of program directors thought their fellows were disinterested in research and advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
Discussant Dr. Michael G. Sarr was blunt: "This is a scary situation."
"There’s a clear message here from this study: We have a problem. I maintain that we have to stop being bullied by naive, public, politically driven agendas and by some of our own graybeard pundits – and I think we all know who those groups are – and once again take over the control of educating our successors," said Dr. Sarr, professor of surgery at the Mayo Medical School, Rochester, Minn.
He attributed the decline in graduating general surgery residents’ technical skills, patient ownership, and ability to function as trustworthy independent surgeons in large part to the mandated 80-hour maximum work week.
"We all admit and acknowledge that prior to the duty hours reduction of 2003, the expected duty hours most of us trained in were barbaric and often dangerous, and they involved too much scut work. But in the past the final product was superb," Dr. Sarr recalled.
He argued that while it would be folly to return to those days, some flexibility regarding the work hours limit would be beneficial.
"Should our politically driven ACGME [Accreditation Council for Graduate Medical Education] and our own RRC [Residency Review Committee] – yes, our own elected overseeing organization – liberalize its rigid, unbending, stringent rules to allow our residents to make more liberal decisions and to develop professionalism by exceeding their 80-hour work restriction when clinical situations demand their presence?" he asked.
Discussant Dr. Frank R. Lewis, executive director of the American Board of Surgery, said that even though the 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, he doesn’t believe this emotional and contentious issue is the main problem. He noted that at present the average number of operations done by a first-year resident is less than two per week, while second-year residents average only two to three per week.
"Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process," Dr. Lewis complained.
He added that nobody should be surprised by the Fellowship Council survey results. During the past decade the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present the percentage of examinees who fail either the oral or written ABS exam the first time around is in the mid-30s.
"That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject," the surgeon added.
He asserted that most of the factors responsible for the decline in the competence of graduating general surgery residents are beyond the control of academic surgeons. These factors include the gutting of surgical clerkship opportunities in the fourth year of medical school, along with changes in the surgical landscape that have caused once-popular operations to essentially go away due to technical advances or improved drug therapy.
Discussant Dr. Mark A. Malangoni, associate executive director of the ABS, noted that the more complex open surgery operations previously done by general surgery residents have in many cases been converted to complex laparoscopic procedures that have become the purview of the subspecialty fellowships. Why not abolish the fellowships and drive all those interesting cases and that dedicated training effort back into the residency years? he asked.
That’s not going to happen, Dr. Mattar replied, citing the huge market demand and need for these fellowships.
"They’re very rewarding to all stakeholders," he added.
But constructive changes are afoot, according to Dr. Mattar. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin to prepare for it then. And there are also efforts to custom-tailor the final year of general surgery residency so that residents can prepare for their fellowship year. Toward that end the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization with oversight over surgical subspecialty fellowships. Dr. Mattar reported having no financial conflicts.
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
The source of their ire is a detailed new survey of the nation’s subspecialty fellowship program directors. Today 80% of graduating general surgery residents seek these year-long fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical areas. The surveyed program directors indicated many trainees arrive unprepared in essential areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Samer Mattar declared in presenting the survey results at the annual meeting of the American Surgical Association.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey and is an indication of the importance educators place on the subject matter, said Dr. Mattar of Indiana University, Indianapolis.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – academics and scholarship," Dr. Mattar noted in summarizing the survey results.
The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their residency rather than to push their skills to the next level. Among the key survey findings:
• Forty-three percent of program directors felt incoming fellows were unable to independently perform half an hour of a major procedure.
• Thirty percent of incoming fellows couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Fifty-six percent were unable to laparoscopically suture and tie knots properly, and 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter were deemed unable to recognize early signs of complications.
• Nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented.
• Only 51% of program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although fellows did show marked improvement in these areas as the year went on.
• A large majority of program directors thought their fellows were disinterested in research and advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
Discussant Dr. Michael G. Sarr was blunt: "This is a scary situation."
"There’s a clear message here from this study: We have a problem. I maintain that we have to stop being bullied by naive, public, politically driven agendas and by some of our own graybeard pundits – and I think we all know who those groups are – and once again take over the control of educating our successors," said Dr. Sarr, professor of surgery at the Mayo Medical School, Rochester, Minn.
He attributed the decline in graduating general surgery residents’ technical skills, patient ownership, and ability to function as trustworthy independent surgeons in large part to the mandated 80-hour maximum work week.
"We all admit and acknowledge that prior to the duty hours reduction of 2003, the expected duty hours most of us trained in were barbaric and often dangerous, and they involved too much scut work. But in the past the final product was superb," Dr. Sarr recalled.
He argued that while it would be folly to return to those days, some flexibility regarding the work hours limit would be beneficial.
"Should our politically driven ACGME [Accreditation Council for Graduate Medical Education] and our own RRC [Residency Review Committee] – yes, our own elected overseeing organization – liberalize its rigid, unbending, stringent rules to allow our residents to make more liberal decisions and to develop professionalism by exceeding their 80-hour work restriction when clinical situations demand their presence?" he asked.
Discussant Dr. Frank R. Lewis, executive director of the American Board of Surgery, said that even though the 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, he doesn’t believe this emotional and contentious issue is the main problem. He noted that at present the average number of operations done by a first-year resident is less than two per week, while second-year residents average only two to three per week.
"Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process," Dr. Lewis complained.
He added that nobody should be surprised by the Fellowship Council survey results. During the past decade the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present the percentage of examinees who fail either the oral or written ABS exam the first time around is in the mid-30s.
"That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject," the surgeon added.
He asserted that most of the factors responsible for the decline in the competence of graduating general surgery residents are beyond the control of academic surgeons. These factors include the gutting of surgical clerkship opportunities in the fourth year of medical school, along with changes in the surgical landscape that have caused once-popular operations to essentially go away due to technical advances or improved drug therapy.
Discussant Dr. Mark A. Malangoni, associate executive director of the ABS, noted that the more complex open surgery operations previously done by general surgery residents have in many cases been converted to complex laparoscopic procedures that have become the purview of the subspecialty fellowships. Why not abolish the fellowships and drive all those interesting cases and that dedicated training effort back into the residency years? he asked.
That’s not going to happen, Dr. Mattar replied, citing the huge market demand and need for these fellowships.
"They’re very rewarding to all stakeholders," he added.
But constructive changes are afoot, according to Dr. Mattar. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin to prepare for it then. And there are also efforts to custom-tailor the final year of general surgery residency so that residents can prepare for their fellowship year. Toward that end the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization with oversight over surgical subspecialty fellowships. Dr. Mattar reported having no financial conflicts.
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
The source of their ire is a detailed new survey of the nation’s subspecialty fellowship program directors. Today 80% of graduating general surgery residents seek these year-long fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical areas. The surveyed program directors indicated many trainees arrive unprepared in essential areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Samer Mattar declared in presenting the survey results at the annual meeting of the American Surgical Association.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey and is an indication of the importance educators place on the subject matter, said Dr. Mattar of Indiana University, Indianapolis.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – academics and scholarship," Dr. Mattar noted in summarizing the survey results.
The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their residency rather than to push their skills to the next level. Among the key survey findings:
• Forty-three percent of program directors felt incoming fellows were unable to independently perform half an hour of a major procedure.
• Thirty percent of incoming fellows couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Fifty-six percent were unable to laparoscopically suture and tie knots properly, and 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter were deemed unable to recognize early signs of complications.
• Nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented.
• Only 51% of program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although fellows did show marked improvement in these areas as the year went on.
• A large majority of program directors thought their fellows were disinterested in research and advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
Discussant Dr. Michael G. Sarr was blunt: "This is a scary situation."
"There’s a clear message here from this study: We have a problem. I maintain that we have to stop being bullied by naive, public, politically driven agendas and by some of our own graybeard pundits – and I think we all know who those groups are – and once again take over the control of educating our successors," said Dr. Sarr, professor of surgery at the Mayo Medical School, Rochester, Minn.
He attributed the decline in graduating general surgery residents’ technical skills, patient ownership, and ability to function as trustworthy independent surgeons in large part to the mandated 80-hour maximum work week.
"We all admit and acknowledge that prior to the duty hours reduction of 2003, the expected duty hours most of us trained in were barbaric and often dangerous, and they involved too much scut work. But in the past the final product was superb," Dr. Sarr recalled.
He argued that while it would be folly to return to those days, some flexibility regarding the work hours limit would be beneficial.
"Should our politically driven ACGME [Accreditation Council for Graduate Medical Education] and our own RRC [Residency Review Committee] – yes, our own elected overseeing organization – liberalize its rigid, unbending, stringent rules to allow our residents to make more liberal decisions and to develop professionalism by exceeding their 80-hour work restriction when clinical situations demand their presence?" he asked.
Discussant Dr. Frank R. Lewis, executive director of the American Board of Surgery, said that even though the 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, he doesn’t believe this emotional and contentious issue is the main problem. He noted that at present the average number of operations done by a first-year resident is less than two per week, while second-year residents average only two to three per week.
"Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process," Dr. Lewis complained.
He added that nobody should be surprised by the Fellowship Council survey results. During the past decade the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present the percentage of examinees who fail either the oral or written ABS exam the first time around is in the mid-30s.
"That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject," the surgeon added.
He asserted that most of the factors responsible for the decline in the competence of graduating general surgery residents are beyond the control of academic surgeons. These factors include the gutting of surgical clerkship opportunities in the fourth year of medical school, along with changes in the surgical landscape that have caused once-popular operations to essentially go away due to technical advances or improved drug therapy.
Discussant Dr. Mark A. Malangoni, associate executive director of the ABS, noted that the more complex open surgery operations previously done by general surgery residents have in many cases been converted to complex laparoscopic procedures that have become the purview of the subspecialty fellowships. Why not abolish the fellowships and drive all those interesting cases and that dedicated training effort back into the residency years? he asked.
That’s not going to happen, Dr. Mattar replied, citing the huge market demand and need for these fellowships.
"They’re very rewarding to all stakeholders," he added.
But constructive changes are afoot, according to Dr. Mattar. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin to prepare for it then. And there are also efforts to custom-tailor the final year of general surgery residency so that residents can prepare for their fellowship year. Toward that end the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization with oversight over surgical subspecialty fellowships. Dr. Mattar reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major finding: Forty-three percent of incoming fellows in the nation’s surgical subspecialty programs were deemed by their program directors to be unable to independently perform half an hour of a major procedure.
Data source: A survey of the nation’s 145 surgical subspecialty program directors. It drew responses from 91 (63%).
Disclosures: The survey was conducted by the Fellowship Council, an umbrella organization with oversight over surgical subspecialty fellowships. Dr. Mattar reported having no financial conflicts.
Surgeons tackle readmission risk reduction
INDIANAPOLIS – Average 30-day readmission rates in a large national study varied widely by surgical specialty, ranging from 5% for general surgery patients to 12% for vascular surgery patients and 16% after hepato-pancreatic-biliary surgery.
This retrospective study was based upon American College of Surgeons National Surgical Quality Improvement Program (NSQIP) 2011 data on 240,125 patients discharged from 316 hospitals after these types of surgery. The results enabled investigators to identify the major risk factors for readmission. They used this information to generate a predictive model to identify patients at greatest risk with an eye toward introducing interventions to keep them out of the hospital, Dr. Timothy M. Pawlik said at the annual meeting of the American Surgical Association.
How effective such interventions will be in a surgical population is as yet unclear, he added.
The importance of this work lies in the growing emphasis health care payers are placing upon 30-day readmission as a quality-of-care indicator. In 2012, Medicare began cutting reimbursement by 1% to hospitals with above-average 30-day readmissions. Next year, this penalty is scheduled to increase to 3% under the Medicare Hospital Readmission Reduction Program. Prior research efforts to identify risk factors for readmission have focused chiefly on medical rather than surgical conditions, noted Dr. Pawlik, professor of surgery and chief of the division of surgical oncology at Johns Hopkins University, Baltimore.
The readmission risk predictive formula he and his coinvestigators developed is simple: American Society of Anesthesiologists physical status class + (length of stay/2). This number is rounded up to yield a risk score of 1-10. A patient with a readmission score of 1 has a 1% risk of readmission within 30 days of discharge. The risk climbs to 12% with a score of 5, 20% with a score of 8, and 40% with a score of 10.
"A score of 4 had an 8% readmission rate, with 77% sensitivity, 52% specificity, a low positive predictive value of 12%, but a high negative predictive value of 95%," the surgeon observed. "In essence, a score of 4 or higher was able to identify 80% of all readmissions, but it also included about half of all patients."
Because of a quirk in the NSQIP database – it records readmissions within 30 days of surgery instead of starting from discharge – the investigators had to limit the study population to surgery patients with a length of stay of 10 days or less and then apply statistical modeling. However, limiting the data set to patients with a maximum 10-day hospital stay only restricted the study cohort by 6%. Thus, the study results remain highly generalizable to U.S. surgery patients.
The area under the curve (AUC) of the receiver operating characteristic for the readmission risk formula was 0.70. Statisticians consider a test having an AUC of 0.50 to be worthless. An AUC of 1.0 would define a "perfect" test, while a test with an AUC in the 0.70-0.80 range is deemed of only "fair" accuracy.
The AUC for the readmission score varied considerably when applied to the various surgical subspecialties. For example, the AUC was 0.69 for general surgery patients but only 0.51 for thoracic surgery patients, 0.64 for vascular surgery patients, and 0.59 for colorectal surgery patients.
The fact that the predictive formula doesn’t perform any better than barely "fair" is testimony to the difficulty in identifying who will require readmission. That being said, the AUC for the readmission score after surgery compares favorably to published hospital readmission risk formulas developed for medical patients, which have similar and in many cases lower AUCs (JAMA 2011;306:1688-98), Dr. Pawlik observed.
At Johns Hopkins, the plan is to target surgery patients who have high readmission scores with interventions including more frequent follow-up phone calls and earlier scheduled postoperative clinic visits in an effort to keep them out of the hospital, he continued.
Discussant Dr. Keith D. Lillemoe was skeptical that this will result in reduced readmission rates. Indeed, he questioned whether the 30-day readmission rate is a legitimate quality measure for surgeons.
"I can look across the room and predict if a patient is going to come back in to the hospital. But what can we really do to keep such patients from being readmitted other than keeping them indeterminately long until we’ve passed that window? It seems like all the phone calls and early clinic visits in the world can’t stop the progression sometimes," reflected Dr. Lillemoe, professor and chairman of the department of surgery at Massachusetts General Hospital, Boston.
He noted with frustration that he had just stepped out of the lecture hall to arrange for readmission of a patient 1 week after discharge post pancreaticoduodenectomy.
"I made three phone calls myself to that guy trying to nurse him through his nausea and vomiting and other symptoms," the surgeon recalled.
Dr. Pawlik was sympathetic.
"It’s very hard to prevent readmissions. It’s a very complicated metric, and many would argue that it’s an inappropriate quality metric," he said. "Many things are outside our control before we even meet the patient, as are some things that occur in the hospital, and many things are beyond our control after discharge as far as where they live, their family structure, and their financial resources. In my opinion it’s a very problematic quality measure and I am not sure how we are going to tackle it."
He reported having no conflicts of interest.
INDIANAPOLIS – Average 30-day readmission rates in a large national study varied widely by surgical specialty, ranging from 5% for general surgery patients to 12% for vascular surgery patients and 16% after hepato-pancreatic-biliary surgery.
This retrospective study was based upon American College of Surgeons National Surgical Quality Improvement Program (NSQIP) 2011 data on 240,125 patients discharged from 316 hospitals after these types of surgery. The results enabled investigators to identify the major risk factors for readmission. They used this information to generate a predictive model to identify patients at greatest risk with an eye toward introducing interventions to keep them out of the hospital, Dr. Timothy M. Pawlik said at the annual meeting of the American Surgical Association.
How effective such interventions will be in a surgical population is as yet unclear, he added.
The importance of this work lies in the growing emphasis health care payers are placing upon 30-day readmission as a quality-of-care indicator. In 2012, Medicare began cutting reimbursement by 1% to hospitals with above-average 30-day readmissions. Next year, this penalty is scheduled to increase to 3% under the Medicare Hospital Readmission Reduction Program. Prior research efforts to identify risk factors for readmission have focused chiefly on medical rather than surgical conditions, noted Dr. Pawlik, professor of surgery and chief of the division of surgical oncology at Johns Hopkins University, Baltimore.
The readmission risk predictive formula he and his coinvestigators developed is simple: American Society of Anesthesiologists physical status class + (length of stay/2). This number is rounded up to yield a risk score of 1-10. A patient with a readmission score of 1 has a 1% risk of readmission within 30 days of discharge. The risk climbs to 12% with a score of 5, 20% with a score of 8, and 40% with a score of 10.
"A score of 4 had an 8% readmission rate, with 77% sensitivity, 52% specificity, a low positive predictive value of 12%, but a high negative predictive value of 95%," the surgeon observed. "In essence, a score of 4 or higher was able to identify 80% of all readmissions, but it also included about half of all patients."
Because of a quirk in the NSQIP database – it records readmissions within 30 days of surgery instead of starting from discharge – the investigators had to limit the study population to surgery patients with a length of stay of 10 days or less and then apply statistical modeling. However, limiting the data set to patients with a maximum 10-day hospital stay only restricted the study cohort by 6%. Thus, the study results remain highly generalizable to U.S. surgery patients.
The area under the curve (AUC) of the receiver operating characteristic for the readmission risk formula was 0.70. Statisticians consider a test having an AUC of 0.50 to be worthless. An AUC of 1.0 would define a "perfect" test, while a test with an AUC in the 0.70-0.80 range is deemed of only "fair" accuracy.
The AUC for the readmission score varied considerably when applied to the various surgical subspecialties. For example, the AUC was 0.69 for general surgery patients but only 0.51 for thoracic surgery patients, 0.64 for vascular surgery patients, and 0.59 for colorectal surgery patients.
The fact that the predictive formula doesn’t perform any better than barely "fair" is testimony to the difficulty in identifying who will require readmission. That being said, the AUC for the readmission score after surgery compares favorably to published hospital readmission risk formulas developed for medical patients, which have similar and in many cases lower AUCs (JAMA 2011;306:1688-98), Dr. Pawlik observed.
At Johns Hopkins, the plan is to target surgery patients who have high readmission scores with interventions including more frequent follow-up phone calls and earlier scheduled postoperative clinic visits in an effort to keep them out of the hospital, he continued.
Discussant Dr. Keith D. Lillemoe was skeptical that this will result in reduced readmission rates. Indeed, he questioned whether the 30-day readmission rate is a legitimate quality measure for surgeons.
"I can look across the room and predict if a patient is going to come back in to the hospital. But what can we really do to keep such patients from being readmitted other than keeping them indeterminately long until we’ve passed that window? It seems like all the phone calls and early clinic visits in the world can’t stop the progression sometimes," reflected Dr. Lillemoe, professor and chairman of the department of surgery at Massachusetts General Hospital, Boston.
He noted with frustration that he had just stepped out of the lecture hall to arrange for readmission of a patient 1 week after discharge post pancreaticoduodenectomy.
"I made three phone calls myself to that guy trying to nurse him through his nausea and vomiting and other symptoms," the surgeon recalled.
Dr. Pawlik was sympathetic.
"It’s very hard to prevent readmissions. It’s a very complicated metric, and many would argue that it’s an inappropriate quality metric," he said. "Many things are outside our control before we even meet the patient, as are some things that occur in the hospital, and many things are beyond our control after discharge as far as where they live, their family structure, and their financial resources. In my opinion it’s a very problematic quality measure and I am not sure how we are going to tackle it."
He reported having no conflicts of interest.
INDIANAPOLIS – Average 30-day readmission rates in a large national study varied widely by surgical specialty, ranging from 5% for general surgery patients to 12% for vascular surgery patients and 16% after hepato-pancreatic-biliary surgery.
This retrospective study was based upon American College of Surgeons National Surgical Quality Improvement Program (NSQIP) 2011 data on 240,125 patients discharged from 316 hospitals after these types of surgery. The results enabled investigators to identify the major risk factors for readmission. They used this information to generate a predictive model to identify patients at greatest risk with an eye toward introducing interventions to keep them out of the hospital, Dr. Timothy M. Pawlik said at the annual meeting of the American Surgical Association.
How effective such interventions will be in a surgical population is as yet unclear, he added.
The importance of this work lies in the growing emphasis health care payers are placing upon 30-day readmission as a quality-of-care indicator. In 2012, Medicare began cutting reimbursement by 1% to hospitals with above-average 30-day readmissions. Next year, this penalty is scheduled to increase to 3% under the Medicare Hospital Readmission Reduction Program. Prior research efforts to identify risk factors for readmission have focused chiefly on medical rather than surgical conditions, noted Dr. Pawlik, professor of surgery and chief of the division of surgical oncology at Johns Hopkins University, Baltimore.
The readmission risk predictive formula he and his coinvestigators developed is simple: American Society of Anesthesiologists physical status class + (length of stay/2). This number is rounded up to yield a risk score of 1-10. A patient with a readmission score of 1 has a 1% risk of readmission within 30 days of discharge. The risk climbs to 12% with a score of 5, 20% with a score of 8, and 40% with a score of 10.
"A score of 4 had an 8% readmission rate, with 77% sensitivity, 52% specificity, a low positive predictive value of 12%, but a high negative predictive value of 95%," the surgeon observed. "In essence, a score of 4 or higher was able to identify 80% of all readmissions, but it also included about half of all patients."
Because of a quirk in the NSQIP database – it records readmissions within 30 days of surgery instead of starting from discharge – the investigators had to limit the study population to surgery patients with a length of stay of 10 days or less and then apply statistical modeling. However, limiting the data set to patients with a maximum 10-day hospital stay only restricted the study cohort by 6%. Thus, the study results remain highly generalizable to U.S. surgery patients.
The area under the curve (AUC) of the receiver operating characteristic for the readmission risk formula was 0.70. Statisticians consider a test having an AUC of 0.50 to be worthless. An AUC of 1.0 would define a "perfect" test, while a test with an AUC in the 0.70-0.80 range is deemed of only "fair" accuracy.
The AUC for the readmission score varied considerably when applied to the various surgical subspecialties. For example, the AUC was 0.69 for general surgery patients but only 0.51 for thoracic surgery patients, 0.64 for vascular surgery patients, and 0.59 for colorectal surgery patients.
The fact that the predictive formula doesn’t perform any better than barely "fair" is testimony to the difficulty in identifying who will require readmission. That being said, the AUC for the readmission score after surgery compares favorably to published hospital readmission risk formulas developed for medical patients, which have similar and in many cases lower AUCs (JAMA 2011;306:1688-98), Dr. Pawlik observed.
At Johns Hopkins, the plan is to target surgery patients who have high readmission scores with interventions including more frequent follow-up phone calls and earlier scheduled postoperative clinic visits in an effort to keep them out of the hospital, he continued.
Discussant Dr. Keith D. Lillemoe was skeptical that this will result in reduced readmission rates. Indeed, he questioned whether the 30-day readmission rate is a legitimate quality measure for surgeons.
"I can look across the room and predict if a patient is going to come back in to the hospital. But what can we really do to keep such patients from being readmitted other than keeping them indeterminately long until we’ve passed that window? It seems like all the phone calls and early clinic visits in the world can’t stop the progression sometimes," reflected Dr. Lillemoe, professor and chairman of the department of surgery at Massachusetts General Hospital, Boston.
He noted with frustration that he had just stepped out of the lecture hall to arrange for readmission of a patient 1 week after discharge post pancreaticoduodenectomy.
"I made three phone calls myself to that guy trying to nurse him through his nausea and vomiting and other symptoms," the surgeon recalled.
Dr. Pawlik was sympathetic.
"It’s very hard to prevent readmissions. It’s a very complicated metric, and many would argue that it’s an inappropriate quality metric," he said. "Many things are outside our control before we even meet the patient, as are some things that occur in the hospital, and many things are beyond our control after discharge as far as where they live, their family structure, and their financial resources. In my opinion it’s a very problematic quality measure and I am not sure how we are going to tackle it."
He reported having no conflicts of interest.
AT THE ASA ANNUAL MEETING
Major Finding: The 30-day readmission rate following general, thoracic, and vascular surgery was 8%. It ranged from 5% to 16% depending upon the surgical subspecialty. The study led to generation of a simple readmission risk scoring system.
Data Source: A retrospective study of 240,125 patients in the American College of Surgeons National Surgical Quality Improvement Program who were discharged in 2011 following these types of surgery.
Disclosures: The presenter reported having no conflicts of interest.
Abdominal sacrocolpopexy 'less effective than desired' for POP
Abdominal sacrocolpopexy, with or without concomitant urethropexy, "is less effective than desired" for long-term treatment of pelvic organ prolapse, according to a report in the May 15 issue of JAMA.
In extended follow-up of 215 women who had undergone the surgery in 2001-2006 to correct pelvic organ prolapse (POP), nearly one-third of the procedures had failed at the 7-year mark. And for women whose surgery involved the placement of synthetic mesh, the estimated probability of mesh erosion was 10.5%, said Dr. Ingrid Nygaard of the University of Utah, Salt Lake City, and her associates.
Nevertheless, only 5% of the women in this study sought retreatment for POP – a result that the investigators interpreted to mean that the procedures had addressed their symptoms adequately.
"Based on our results, women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time," they said.
"Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly," the researchers noted (JAMA 2013;309:2016-24).
Even though some 225,000 women in the United States undergo POP surgeries every year, "little is known about long-term durability, complications, and pelvic floor symptoms" associated with the procedure. To examine the issue, Dr. Nygaard and her colleagues performed an extended follow-up of women who had participated in the CARE (Colpopexy and Urinary Reduction Efforts) trial, which concluded in 2006.
CARE was a multicenter trial funded by the National Institutes of Health in which 322 women who did not have stress urinary incontinence and were undergoing abdominal sacrocolpopexy were randomly assigned to concomitant Burch urethropexy (to prevent the common postoperative adverse effect of stress urinary incontinence) or to serve as controls. At 2 years, the incidence of stress urinary incontinence was 32.0% in women who had the prophylactic urethropexy, significantly lower than the 45.2% incidence in the control group.
Dr. Nygaard and her associates were able to follow up on 215 of these CARE participants up to 7 years later. "We were surprised by the magnitude of treatment failure rates," they said.
"By year 7, the estimated probabilities of treatment failure for the urethropexy group and the no urethropexy group, respectively, were 0.27 and 0.22 for anatomic pelvic organ prolapse, 0.29 and 0.24 for symptomatic pelvic organ prolapse, and 0.48 and 0.34 for composite pelvic organ prolapse," the investigators said.
The estimated probability that in a few years the women would develop stress urinary incontinence was 0.62 for those who had undergone urethropexy specifically to prevent that adverse effect and 0.77 for those who had not undergone urethropexy.
In addition, by year 7, 4 women had suture erosion and 23 had mesh erosion. Mesh erosion occurred with every type of mesh that had been placed.
"By year 7, at least 36 of 215 women (16.7%) ... had additional surgery related to pelvic floor disorders: 11 for recurrent POP, 14 for stress urinary incontinence, and 11 for mesh complications," the investigators said.
Their findings have three important implications.
"First, as a criterion standard for surgical treatment of POP, abdominal sacrocolpopexy is less effective than desired.
"For this study, we chose a clinically relevant definition of anatomic failure that some would argue is still not stringent enough, yet by 5 years, nearly one-third of women met our composite failure definition," they noted.
Nevertheless, the procedure generally appears to relieve POP symptoms, even though anatomic support wanes. Only 5% of the study population sought retreatment for POP, which "may imply that women found the treatment adequate," Dr. Nygaard and her colleagues said.
Second, "surgical prevention of stress urinary incontinence at the time of abdominal POP surgery involves no clinically significant trade-offs to date." Adding an anti–urinary-incontinence procedure to sacrocolpopexy decreases but does not eliminate the risk that such incontinence will develop.
And third, mesh-related complications continue to develop over time. "Long-term follow-up is mandatory to understand the long-term patient burden associated with surgical materials and devices," they said.
One limitation of this study was that participants at some sites could not be followed at all, and participants at other sites could only be followed by telephone interview rather than physical examination, because research funding for that purpose was not renewed over time.
The researchers added that clinical practice has shifted since the original CARE trial was conducted; midurethral slings are now more commonplace, and sacrocolpopexy now is often performed via laparoscopic or even robotic approaches. "It is unclear to what degree [our] results can be extrapolated to the newer procedures because we only evaluated open abdominal sacrocolpopexy and Burch urethropexy."
The extended CARE study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Research on Women’s Health at the National Institutes of Health. Dr. Nygaard reported no financial conflicts of interest; some of her associates reported ties to Johnson & Johnson, Key Tech, Pelvalon, Astellas, Pfizer, Warner Chilcott, GlaxoSmithKline, Uromedica, IDEO, Xanodyne, and Intuitive Surgical.
The findings of Nygaard and colleagues have important clinical implications and call into question "the designation of the abdominal sacrocolpopexy as the criterion standard procedure for prolapse repair," said Dr. Cheryl B. Iglesia.

|
|
Moreover, both clinicians and patients "may need to temper their expectations that pelvic floor surgery will last a lifetime. Not enough is known about the long-term outcomes of prolapse surgery; the natural history of prolapse; the effects of aging, hormonal, and weight changes; or the effects of straining and strenuous activity after prolapse repair," she said.
As with surgeries for face-lifts, which carry a 69% rate of partial relapse at 5.5 years, and for abdominal wall incisional hernia, which carry a 28% recurrence rate at 5 years, "operations for pelvic organ prolapse also may be vulnerable to the normal wear and tear of aging and activities of daily living," Dr. Iglesia said.
"Although imperfect, surgery for pelvic organ prolapse is generally safe and effective, and relief of bulge symptoms is associated with high patient satisfaction. Ultimately, patient-reported outcomes of symptom relief is the most important and fundamental goal of surgery," she said.
Dr. Iglesia is in the section of female pelvic medicine and reconstructive surgery at MedStar Washington (D.C.) Hospital Center and in the departments of obstetrics, gynecology, and urology at Georgetown University. She reported no financial conflicts of interest. These comments were taken from her remarks in an editorial accompanying Dr. Nygaard’s report (JAMA 2013;309:2045-6).
The findings of Nygaard and colleagues have important clinical implications and call into question "the designation of the abdominal sacrocolpopexy as the criterion standard procedure for prolapse repair," said Dr. Cheryl B. Iglesia.

|
|
Moreover, both clinicians and patients "may need to temper their expectations that pelvic floor surgery will last a lifetime. Not enough is known about the long-term outcomes of prolapse surgery; the natural history of prolapse; the effects of aging, hormonal, and weight changes; or the effects of straining and strenuous activity after prolapse repair," she said.
As with surgeries for face-lifts, which carry a 69% rate of partial relapse at 5.5 years, and for abdominal wall incisional hernia, which carry a 28% recurrence rate at 5 years, "operations for pelvic organ prolapse also may be vulnerable to the normal wear and tear of aging and activities of daily living," Dr. Iglesia said.
"Although imperfect, surgery for pelvic organ prolapse is generally safe and effective, and relief of bulge symptoms is associated with high patient satisfaction. Ultimately, patient-reported outcomes of symptom relief is the most important and fundamental goal of surgery," she said.
Dr. Iglesia is in the section of female pelvic medicine and reconstructive surgery at MedStar Washington (D.C.) Hospital Center and in the departments of obstetrics, gynecology, and urology at Georgetown University. She reported no financial conflicts of interest. These comments were taken from her remarks in an editorial accompanying Dr. Nygaard’s report (JAMA 2013;309:2045-6).
The findings of Nygaard and colleagues have important clinical implications and call into question "the designation of the abdominal sacrocolpopexy as the criterion standard procedure for prolapse repair," said Dr. Cheryl B. Iglesia.

|
|
Moreover, both clinicians and patients "may need to temper their expectations that pelvic floor surgery will last a lifetime. Not enough is known about the long-term outcomes of prolapse surgery; the natural history of prolapse; the effects of aging, hormonal, and weight changes; or the effects of straining and strenuous activity after prolapse repair," she said.
As with surgeries for face-lifts, which carry a 69% rate of partial relapse at 5.5 years, and for abdominal wall incisional hernia, which carry a 28% recurrence rate at 5 years, "operations for pelvic organ prolapse also may be vulnerable to the normal wear and tear of aging and activities of daily living," Dr. Iglesia said.
"Although imperfect, surgery for pelvic organ prolapse is generally safe and effective, and relief of bulge symptoms is associated with high patient satisfaction. Ultimately, patient-reported outcomes of symptom relief is the most important and fundamental goal of surgery," she said.
Dr. Iglesia is in the section of female pelvic medicine and reconstructive surgery at MedStar Washington (D.C.) Hospital Center and in the departments of obstetrics, gynecology, and urology at Georgetown University. She reported no financial conflicts of interest. These comments were taken from her remarks in an editorial accompanying Dr. Nygaard’s report (JAMA 2013;309:2045-6).
Abdominal sacrocolpopexy, with or without concomitant urethropexy, "is less effective than desired" for long-term treatment of pelvic organ prolapse, according to a report in the May 15 issue of JAMA.
In extended follow-up of 215 women who had undergone the surgery in 2001-2006 to correct pelvic organ prolapse (POP), nearly one-third of the procedures had failed at the 7-year mark. And for women whose surgery involved the placement of synthetic mesh, the estimated probability of mesh erosion was 10.5%, said Dr. Ingrid Nygaard of the University of Utah, Salt Lake City, and her associates.
Nevertheless, only 5% of the women in this study sought retreatment for POP – a result that the investigators interpreted to mean that the procedures had addressed their symptoms adequately.
"Based on our results, women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time," they said.
"Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly," the researchers noted (JAMA 2013;309:2016-24).
Even though some 225,000 women in the United States undergo POP surgeries every year, "little is known about long-term durability, complications, and pelvic floor symptoms" associated with the procedure. To examine the issue, Dr. Nygaard and her colleagues performed an extended follow-up of women who had participated in the CARE (Colpopexy and Urinary Reduction Efforts) trial, which concluded in 2006.
CARE was a multicenter trial funded by the National Institutes of Health in which 322 women who did not have stress urinary incontinence and were undergoing abdominal sacrocolpopexy were randomly assigned to concomitant Burch urethropexy (to prevent the common postoperative adverse effect of stress urinary incontinence) or to serve as controls. At 2 years, the incidence of stress urinary incontinence was 32.0% in women who had the prophylactic urethropexy, significantly lower than the 45.2% incidence in the control group.
Dr. Nygaard and her associates were able to follow up on 215 of these CARE participants up to 7 years later. "We were surprised by the magnitude of treatment failure rates," they said.
"By year 7, the estimated probabilities of treatment failure for the urethropexy group and the no urethropexy group, respectively, were 0.27 and 0.22 for anatomic pelvic organ prolapse, 0.29 and 0.24 for symptomatic pelvic organ prolapse, and 0.48 and 0.34 for composite pelvic organ prolapse," the investigators said.
The estimated probability that in a few years the women would develop stress urinary incontinence was 0.62 for those who had undergone urethropexy specifically to prevent that adverse effect and 0.77 for those who had not undergone urethropexy.
In addition, by year 7, 4 women had suture erosion and 23 had mesh erosion. Mesh erosion occurred with every type of mesh that had been placed.
"By year 7, at least 36 of 215 women (16.7%) ... had additional surgery related to pelvic floor disorders: 11 for recurrent POP, 14 for stress urinary incontinence, and 11 for mesh complications," the investigators said.
Their findings have three important implications.
"First, as a criterion standard for surgical treatment of POP, abdominal sacrocolpopexy is less effective than desired.
"For this study, we chose a clinically relevant definition of anatomic failure that some would argue is still not stringent enough, yet by 5 years, nearly one-third of women met our composite failure definition," they noted.
Nevertheless, the procedure generally appears to relieve POP symptoms, even though anatomic support wanes. Only 5% of the study population sought retreatment for POP, which "may imply that women found the treatment adequate," Dr. Nygaard and her colleagues said.
Second, "surgical prevention of stress urinary incontinence at the time of abdominal POP surgery involves no clinically significant trade-offs to date." Adding an anti–urinary-incontinence procedure to sacrocolpopexy decreases but does not eliminate the risk that such incontinence will develop.
And third, mesh-related complications continue to develop over time. "Long-term follow-up is mandatory to understand the long-term patient burden associated with surgical materials and devices," they said.
One limitation of this study was that participants at some sites could not be followed at all, and participants at other sites could only be followed by telephone interview rather than physical examination, because research funding for that purpose was not renewed over time.
The researchers added that clinical practice has shifted since the original CARE trial was conducted; midurethral slings are now more commonplace, and sacrocolpopexy now is often performed via laparoscopic or even robotic approaches. "It is unclear to what degree [our] results can be extrapolated to the newer procedures because we only evaluated open abdominal sacrocolpopexy and Burch urethropexy."
The extended CARE study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Research on Women’s Health at the National Institutes of Health. Dr. Nygaard reported no financial conflicts of interest; some of her associates reported ties to Johnson & Johnson, Key Tech, Pelvalon, Astellas, Pfizer, Warner Chilcott, GlaxoSmithKline, Uromedica, IDEO, Xanodyne, and Intuitive Surgical.
Abdominal sacrocolpopexy, with or without concomitant urethropexy, "is less effective than desired" for long-term treatment of pelvic organ prolapse, according to a report in the May 15 issue of JAMA.
In extended follow-up of 215 women who had undergone the surgery in 2001-2006 to correct pelvic organ prolapse (POP), nearly one-third of the procedures had failed at the 7-year mark. And for women whose surgery involved the placement of synthetic mesh, the estimated probability of mesh erosion was 10.5%, said Dr. Ingrid Nygaard of the University of Utah, Salt Lake City, and her associates.
Nevertheless, only 5% of the women in this study sought retreatment for POP – a result that the investigators interpreted to mean that the procedures had addressed their symptoms adequately.
"Based on our results, women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time," they said.
"Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly," the researchers noted (JAMA 2013;309:2016-24).
Even though some 225,000 women in the United States undergo POP surgeries every year, "little is known about long-term durability, complications, and pelvic floor symptoms" associated with the procedure. To examine the issue, Dr. Nygaard and her colleagues performed an extended follow-up of women who had participated in the CARE (Colpopexy and Urinary Reduction Efforts) trial, which concluded in 2006.
CARE was a multicenter trial funded by the National Institutes of Health in which 322 women who did not have stress urinary incontinence and were undergoing abdominal sacrocolpopexy were randomly assigned to concomitant Burch urethropexy (to prevent the common postoperative adverse effect of stress urinary incontinence) or to serve as controls. At 2 years, the incidence of stress urinary incontinence was 32.0% in women who had the prophylactic urethropexy, significantly lower than the 45.2% incidence in the control group.
Dr. Nygaard and her associates were able to follow up on 215 of these CARE participants up to 7 years later. "We were surprised by the magnitude of treatment failure rates," they said.
"By year 7, the estimated probabilities of treatment failure for the urethropexy group and the no urethropexy group, respectively, were 0.27 and 0.22 for anatomic pelvic organ prolapse, 0.29 and 0.24 for symptomatic pelvic organ prolapse, and 0.48 and 0.34 for composite pelvic organ prolapse," the investigators said.
The estimated probability that in a few years the women would develop stress urinary incontinence was 0.62 for those who had undergone urethropexy specifically to prevent that adverse effect and 0.77 for those who had not undergone urethropexy.
In addition, by year 7, 4 women had suture erosion and 23 had mesh erosion. Mesh erosion occurred with every type of mesh that had been placed.
"By year 7, at least 36 of 215 women (16.7%) ... had additional surgery related to pelvic floor disorders: 11 for recurrent POP, 14 for stress urinary incontinence, and 11 for mesh complications," the investigators said.
Their findings have three important implications.
"First, as a criterion standard for surgical treatment of POP, abdominal sacrocolpopexy is less effective than desired.
"For this study, we chose a clinically relevant definition of anatomic failure that some would argue is still not stringent enough, yet by 5 years, nearly one-third of women met our composite failure definition," they noted.
Nevertheless, the procedure generally appears to relieve POP symptoms, even though anatomic support wanes. Only 5% of the study population sought retreatment for POP, which "may imply that women found the treatment adequate," Dr. Nygaard and her colleagues said.
Second, "surgical prevention of stress urinary incontinence at the time of abdominal POP surgery involves no clinically significant trade-offs to date." Adding an anti–urinary-incontinence procedure to sacrocolpopexy decreases but does not eliminate the risk that such incontinence will develop.
And third, mesh-related complications continue to develop over time. "Long-term follow-up is mandatory to understand the long-term patient burden associated with surgical materials and devices," they said.
One limitation of this study was that participants at some sites could not be followed at all, and participants at other sites could only be followed by telephone interview rather than physical examination, because research funding for that purpose was not renewed over time.
The researchers added that clinical practice has shifted since the original CARE trial was conducted; midurethral slings are now more commonplace, and sacrocolpopexy now is often performed via laparoscopic or even robotic approaches. "It is unclear to what degree [our] results can be extrapolated to the newer procedures because we only evaluated open abdominal sacrocolpopexy and Burch urethropexy."
The extended CARE study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Research on Women’s Health at the National Institutes of Health. Dr. Nygaard reported no financial conflicts of interest; some of her associates reported ties to Johnson & Johnson, Key Tech, Pelvalon, Astellas, Pfizer, Warner Chilcott, GlaxoSmithKline, Uromedica, IDEO, Xanodyne, and Intuitive Surgical.
FROM JAMA
Major finding: The estimated probabilities of a composite of anatomic and symptomatic treatment failure were 0.48 for women who had concomitant urethropexy and 0.34 for those who had no urethropexy.
Data source: An extended (7-year) follow-up study involving 215 women who underwent abdominal sacrocolpopexy, with or without concomitant urethropexy, for pelvic organ prolapse.
Disclosures: The extended CARE study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Research on Women’s Health at the National Institutes of Health. Dr. Nygaard reported no financial conflicts of interest; some of her associates reported ties to Johnson & Johnson, Key Tech, Pelvalon, Astellas, Pfizer, Warner Chilcott, GlaxoSmithKline, Uromedica, IDEO, Xanodyne, and Intuitive Surgical.
Routine bilateral salpingectomy with hysterectomy gains acceptance
NEW ORLEANS – Acceptance is growing for routine bilateral salpingectomy at the time of hysterectomy to reduce the risk of ovarian serous carcinoma, based on findings from a retrospective cohort study.
The bilateral salpingectomy rates at a single institution increased from 3% in 2010 to 73% in the first 6 months of 2012 – a year after the center began offering the procedure to all women undergoing hysterectomy with ovarian preservation, Dr. Susan K. Park reported at the annual meeting of the American College of Obstetricians and Gynecologists.
"Across the board, patient acceptance of undergoing salpingectomy was very high," she said. Patients were counseled at a preoperative appointment that salpingectomy may reduce the risk of posthysterectomy pelvic adnexal masses and serous carcinomas.
Only two women who were offered the procedure declined, said Dr. Park of Olive View–UCLA Medical Center, Los Angeles.
Moreover, there was no difference in operating time or surgical morbidity in a case-control study involving 133 women who underwent hysterectomy with ovarian preservation and salpingectomy and in 433 controls who did not undergo salpingectomy.
Study subjects were women undergoing abdominal, laparoscopic, or vaginal hysterectomy with ovarian preservation. The salpingectomy rate was lowest for vaginal hysterectomy, as visualization of the fallopian tubes is often difficult with that approach. In fact, two of six women who were unable to undergo salpingectomy despite giving consent were unable to have the procedure because of poor visualization of the tubes, Dr. Park said.
The findings are important given that emerging research points to the fallopian tubes as the site of serous carcinogenesis, Dr. Park said.
Though limited by the retrospective, single-center design, this study is the largest known study to date to look at the feasibility and safety of performing salpingectomy at the time of hysterectomy with ovarian preservation, she said.
Long-term follow-up to evaluate the effects of routine bilateral salpingectomy in these subjects is underway, she noted.
Dr. Park reported having no disclosures.
NEW ORLEANS – Acceptance is growing for routine bilateral salpingectomy at the time of hysterectomy to reduce the risk of ovarian serous carcinoma, based on findings from a retrospective cohort study.
The bilateral salpingectomy rates at a single institution increased from 3% in 2010 to 73% in the first 6 months of 2012 – a year after the center began offering the procedure to all women undergoing hysterectomy with ovarian preservation, Dr. Susan K. Park reported at the annual meeting of the American College of Obstetricians and Gynecologists.
"Across the board, patient acceptance of undergoing salpingectomy was very high," she said. Patients were counseled at a preoperative appointment that salpingectomy may reduce the risk of posthysterectomy pelvic adnexal masses and serous carcinomas.
Only two women who were offered the procedure declined, said Dr. Park of Olive View–UCLA Medical Center, Los Angeles.
Moreover, there was no difference in operating time or surgical morbidity in a case-control study involving 133 women who underwent hysterectomy with ovarian preservation and salpingectomy and in 433 controls who did not undergo salpingectomy.
Study subjects were women undergoing abdominal, laparoscopic, or vaginal hysterectomy with ovarian preservation. The salpingectomy rate was lowest for vaginal hysterectomy, as visualization of the fallopian tubes is often difficult with that approach. In fact, two of six women who were unable to undergo salpingectomy despite giving consent were unable to have the procedure because of poor visualization of the tubes, Dr. Park said.
The findings are important given that emerging research points to the fallopian tubes as the site of serous carcinogenesis, Dr. Park said.
Though limited by the retrospective, single-center design, this study is the largest known study to date to look at the feasibility and safety of performing salpingectomy at the time of hysterectomy with ovarian preservation, she said.
Long-term follow-up to evaluate the effects of routine bilateral salpingectomy in these subjects is underway, she noted.
Dr. Park reported having no disclosures.
NEW ORLEANS – Acceptance is growing for routine bilateral salpingectomy at the time of hysterectomy to reduce the risk of ovarian serous carcinoma, based on findings from a retrospective cohort study.
The bilateral salpingectomy rates at a single institution increased from 3% in 2010 to 73% in the first 6 months of 2012 – a year after the center began offering the procedure to all women undergoing hysterectomy with ovarian preservation, Dr. Susan K. Park reported at the annual meeting of the American College of Obstetricians and Gynecologists.
"Across the board, patient acceptance of undergoing salpingectomy was very high," she said. Patients were counseled at a preoperative appointment that salpingectomy may reduce the risk of posthysterectomy pelvic adnexal masses and serous carcinomas.
Only two women who were offered the procedure declined, said Dr. Park of Olive View–UCLA Medical Center, Los Angeles.
Moreover, there was no difference in operating time or surgical morbidity in a case-control study involving 133 women who underwent hysterectomy with ovarian preservation and salpingectomy and in 433 controls who did not undergo salpingectomy.
Study subjects were women undergoing abdominal, laparoscopic, or vaginal hysterectomy with ovarian preservation. The salpingectomy rate was lowest for vaginal hysterectomy, as visualization of the fallopian tubes is often difficult with that approach. In fact, two of six women who were unable to undergo salpingectomy despite giving consent were unable to have the procedure because of poor visualization of the tubes, Dr. Park said.
The findings are important given that emerging research points to the fallopian tubes as the site of serous carcinogenesis, Dr. Park said.
Though limited by the retrospective, single-center design, this study is the largest known study to date to look at the feasibility and safety of performing salpingectomy at the time of hysterectomy with ovarian preservation, she said.
Long-term follow-up to evaluate the effects of routine bilateral salpingectomy in these subjects is underway, she noted.
Dr. Park reported having no disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Major finding: The bilateral salpingectomy rate increased from 3% in 2009 and 2010 to 73% in the first 6 months of 2012.
Data source: A retrospective cohort study of 133 women and 433 case-controls.
Disclosures: Dr. Park reported having no disclosures.
TAVR quickly dominates high-risk aortic stenosis
SAN FRANCISCO – It’s been barely half a year since U.S. cardiologists and cardiac surgeons first became able to routinely offer operable, high-risk patients with aortic stenosis the option of transcatheter valve replacement, yet in the first few months the transcatheter approach quickly rivaled open surgery.
But for the time being in U.S. practice, transcatheter aortic valve replacement (TAVR) remains boxed into the high-risk niche, along with the subgroup of patients who are not suitable for open surgery, king of a pair of relatively small hills.
And no matter how well TAVR performs in the current pair of trials that are comparing it with open surgical aortic valve replacement (SAVR) for intermediate-risk patients, it will remain relegated to niche status for years to come. That’s because roughly two-thirds of all operable patients with aortic stenosis who need valve replacement fall into the low-risk category, with a Society of Thoracic Surgeons (STS) risk score of less than 4%, which experts agree will remain SAVR’s exclusive territory for the foreseeable future.
The high-risk stratum of operable patients, which TAVR now dominates, constitutes about 10% of all patients who need a new aortic valve and can undergo open surgery, patients with an STS score greater than 8%. The intermediate-risk category – an STS score of 4%-8%, where TAVR now vies against open SAVR in two high-profile trials – makes up the final quarter of the operable-patient pie.
Within the high-risk and operable universe, TAVR’s rise has been meteoric, starting last October when the Food and Drug Administration gave Edwards, marketer of the SAPIEN valve system, approval for these patients. A small survey of operators from U.S. TAVR programs in March at the annual scientific session of the American College of Cardiology (ACC) revealed a uniform perception that by early 2013 a sizable majority of U.S. patients with severe aortic stenosis who are deemed operable and are at high surgical risk will wind up being treated by TAVR instead of SAVR. The cardiac surgeons who collaborate on TAVR seem to have fully conceded the advantages of TAVR for these patients.
"We generally go with TAVR. Most patients want it, and with the equivalence" in outcomes from the first PARTNER (Placement of Aortic Transcatheter Valves) cohort A (operable patients) trial (New Engl. J. Med. 2010:364:2187-98), "you usually go with the less invasive procedure," said Dr. Joseph E. Bavaria, professor of surgery and director of thoracic aortic surgery at the University of Pennsylvania in Philadelphia. The small number of high-risk patients who go to open surgery tend to be men, "because they do better with surgery, especially if their life expectancy is greater than 5-8 years," or patients with high stroke risk, Dr. Bavaria said in an interview at the annual meeting of the American College of Cardiology.
"Operable, high-risk patients get TAVR. I’m a surgeon saying that. I’ve already done the [PARTNER cohort A] trial, and I don’t want to do it again," said Dr. Michael Mack, a cardiothoracic surgeon at the Heart Hospital in Plano, Texas. "The results are the same [from TAVR and SAVR] at 30 days, 1 year, and 2 years, but boy do we beat up patients with open surgery. If it was my mom, she’d get TAVR," he said in an interview. "The tie goes to the less invasive treatment."
When high-risk, operable patients are seen by the heart team Dr. Mack works with, the only ones who go to SAVR are patients – generally men – who have a large aortic annulus and need a 29-mm-diameter valve, which is not available for the time being to U.S. TAVR patients; women with septal hypertrophy causing significant left ventricular outflow-tract obstruction; and the small percent of patients who opt for open surgery, usually because it’s the more established approach or because they fear a higher stroke risk from TAVR.
"The majority of high-risk, operable patients now go to TAVR; I think that’s pretty much true across the United States," said Dr. Jeffrey J. Popma, a cardiologist who does TAVR and is a professor of medicine at Harvard University in Boston.
Where TAVR stood in 2010 and 2011
How is TAVR performing? Performance can only be completely assessed months or years after the fact, so the impact that high-risk, operable U.S. patients received from TAVR’s use in routine practice in late 2012 and the first months of 2013 remains to be seen. The most recently treated patients now available for meaningful analysis in large numbers come from 2010 and 2011: new data reported at the ACC meeting from a U.S. program of continued TAVR access that began in late 2009 following the end of recruitment into the first PARTNER trial, and 1-year follow-up of nearly 14,000 patients who underwent TAVR in 2011 as part of routine practice in Germany and were entered into the country’s national TAVR registry.
Both databases had good news for high-risk or inoperable patients. TAVR outcomes in the first couple of years immediately following PARTNER in both the United States and Germany showed clinically meaningful improvements over the way TAVR performed during the first PARTNER trial. Less optimistic news for the low- and intermediate-risk patients who underwent TAVR in Germany, where wider device use is possible, was that in broad terms open surgery outperformed TAVR in these lower-risk patients, although TAVR’s defenders are quick to point out how tricky it is to make cross-treatment comparisons with registry data.
The nonrandomized, continued-access cohort that followed the first PARTNER trial at 22 U.S. centers, 3 sites in Canada, and 1 site in Germany included 1,017 inoperable or high-risk patients who had successful transfemoral TAVR between August 2009 and December 2011. When compared with the 415 inoperable or high-risk patients who underwent transfemoral TAVR in both cohorts of PARTNER, the more recently treated patients had a statistically significant decrease in all-cause 1-year mortality, from a 25% death rate in PARTNER to a 20% rate during the continued-access period, Dr. William F. Fearon reported at the meeting.
The continued-access patients also showed significant cuts in their rates of major vascular complications, which dropped from 15% of patients in PARTNER to 6% during continued access; and in rates of major bleeding complications, which fell from 15% in PARTNER to 7% during continued access. Strokes were also down during continued access, 5% compared with 7% during PARTNER, but this was not a statistically significant drop, reported Dr. Fearon, a cardiologist at Stanford (Calif.) University.
"Maybe these improvements are due to better patient selection, and maybe we have also gotten better at what we do," commented Dr. Popma.
The latest German experience
The 1-year German Aortic Valve Registry (GARY) results from 2011 show similar improvements compared with PARTNER. Among the 2,689 patients who underwent transvascular TAVR, the 1-year total mortality rate was 21%, and in the subset of patients with stroke data the combined rate of major and minor stroke was 5%.
But it was the way that transvascular TAVR (which includes both transfemoral and other vascular approaches but excludes the 1,181 patients who underwent transapical TAVR) stacked up against open surgical replacement that raised concern.
Of the 13,860 total patients entered into GARY during 2011, 9,985 underwent SAVR, with 6,523 of these patients undergoing an isolated procedure (the rest had valve replacement combined with coronary artery bypass). One-year mortality was 7% in patients who had isolated SAVR, dramatically below the 21% rate among the transvascular TAVR patients, Dr. Friedrich-Wilhelm Mohr reported at the meeting. The transapical TAVR patients had a 28% 1-year mortality rate.
To address the issue of between-treatment differences in patients’ underlying risk, Dr. Mohr presented two sets of analyses that stratified patients with two different risk-scoring systems, the EuroSCORE and the AKL (aortic valve surgery) score, also known as the German aortic valve score. The results showed how disparate the outcomes were when patients were subgrouped by their underlying risk. Among the patients who had lone SAVR, 80% fell into the lowest-risk level, with an AKL score of less than 3. Among the transvascular TAVR patients, only 17% had AKL scores below 3.
Among patients with AKL scores less than 3, those who underwent SAVR without bypass had a roughly 5% mortality rate after 1 year, compared with about a 15% mortality rate among the transvascular TAVR patients. Analyses in higher-risk patient subgroups showed that the survival gap between SAVR and TAVR patients progressively shrank, until in high-risk patients – as in those studied in PARTNER – the mortality rates were about the same in the SAVR and TAVR groups, said Dr. Mohr, professor and director of heart surgery at Leipzig University, Germany. He also reported similar findings when patients were stratified by their baseline EuroSCORE.
A big factor behind the worse survival among lower-risk TAVR patients is the problem of aortic regurgitation, Dr. Mohr said. Following valve replacement, 56% of the transvascular TAVR patients had grade 1 regurgitation, 7% had grade 2, and less than 1% had grade 3 leakage. These rates are way too high, he said. "Our major concern is the incidence of aortic regurgitation; more than half of the [TAVR] patients had some kind of regurgitation. Regurgitation matters whether it is mild or severe."
Despite his concern, TAVR use in Germany is accelerating. The total number of aortic valve replacements done in Germany jumped from just less than 14,000 in 2011 to more than 22,000 last year; TAVR cases more than doubled, from fewer than 4,000 in 2011 to nearly 10,000 in 2012, with a "move to intermediate-risk groups," said Dr. Mohr, who made it clear that he does not endorse this trend. "TAVR must be proven better than or equal to surgery before it’s used on a large scale," he said. The GARY results show "a clear difference [between TAVR and SAVR] in lower-risk patients. The GARY results do not support going into intermediate-risk patients."
Dr. Martin B. Leon agreed with Dr. Mohr that a definitive determination of whether TAVR is at least as good as SAVR in intermediate-risk patients must await results from the two major, ongoing multicenter trials testing this hypothesis, the PARTNER II trial, using the Edwards balloon-expandable SAPIEN XT valve system, and the SURTAVI (Safety and Efficacy Study of the Medtronic CoreValve System in the Treatment of Severe, Symptomatic Aortic Stenosis in Intermediate Risk Subjects Who Need Aortic Valve Replacement) trial. But Dr. Leon also cautioned that possible confounders might be distorting the GARY results, creating what he calls the "GARY Fallacy."
"The GARY Fallacy is the absurd notion that you can compare SAVR and TAVR in various risk strata without formal risk-adjustment methods to account for imbalances in baseline variables that are not captured in standard risk scores," he said in a talk at the meeting. "Aortic-stenosis patients were selected for TAVR based on their presumed increased risk, including many variables that are not represented in the risk algorithms, such as frailty, liver disease, porcelain aorta, a hostile chest, dementia, and severe chronic obstructive pulmonary disease. Therefore, the risk scores for TAVR patients underrepresent their true risk," Dr. Leon said.
But it’s also possible that TAVR needs more refinement before it completely catches up with SAVR, especially in patients who have the best outcomes from SAVR.
"I think SAVR outperforms TAVR in low-risk patients in the German registry because SAVR is a more mature procedure," said Dr. Raj R. Makkar, a TAVR operator and director of interventional cardiology at Cedars-Sinai Medical Center in Los Angeles. "Maybe this will change, as TAVR becomes safer with fewer valve leaks, strokes, and vascular complications."
Assessing patient risks
Experts also realize that the EuroSCORE, the AKL score, and the other risk-stratification tools now available have flaws when applied to TAVR patients. "Risk stratification for TAVR and SAVR is very problematic; the EuroSCORE has shown poor predictive value for mortality," Dr. Leon said. And while the AKL score was developed specifically for SAVR patients, its relevance to TAVR patients is suspect. In the first PARTNER trial, the multivariate predictors of mortality in the TAVR patients were "completely different" from the predictors in the SAVR patients, he noted.
"It’s tricky calculating scores," agreed Dr. Makkar. Both he and Dr. Mohr cited comorbidities such as pulmonary hypertension, cirrhosis, knee replacement producing impaired mobility, and porcelain aorta that each ratchet up a patient’s risk but have no effect whatsoever on a patient’s EuroSCORE or STS score.
The German cardiology and cardiac surgery societies recognize the limitations of current risk-scoring formulas and are developing a risk-stratification tool specifically designed for TAVR patients, Dr. Mohr said.
The way patients are assessed before, during, and after TAVR is receiving careful scrutiny from some investigators who reported their findings at the ACC meeting, with a particular focus on efforts to characterize and minimize aortic-valve regurgitation following TAVR.
One report, for example, reviewed 2,679 patients who underwent TAVR at any of 33 French centers and 1 in Monaco between January 2010 and October 2011, and were enrolled in the French Aortic National CoreValve and Edwards (FRANCE 2) Registry, established by the French cardiology and thoracic and cardiovascular surgery societies (N. Engl. J. Med. 2012;366:1705-15). FRANCE 2 includes nearly 1,900 patients who received the balloon-expandable Edwards SAPIEN valve, and nearly 900 treated with the self-expanding Medtronic CoreValve device.
Following TAVR, 60% of all patients in the registry had paravalvular aortic regurgitation: 45% with grade 1 regurgitation, 14% with grade 2, and 1% with grade 3 or 4. In a multivariate analysis, the self-expandable device was linked to twice the rate of higher-grade aortic regurgitation, grade 2 or higher, compared with the balloon-expandable valve; and TAVRs done via the femoral artery approach were also about twice as likely to result in higher-grade regurgitations compared with other catheterization routes, reported Dr. Eric Van Belle, a professor at the Cardiology Hospital in Lille, France.
Postprocedural paravalvular regurgitation of grade 2 or higher "was associated with a twofold increase in 1-year mortality, and was the strongest independent predictor of mortality," said Dr. Van Belle in his talk at the meeting. In addition, "annulus diameter and prosthesis diameter were major determinants of aortic regurgitation" in patients who received a balloon-expandable valve.
The FRANCE 2 results showed that postprocedural aortic regurgitation at grade 2 or higher "is a major issue and should be avoided, especially when there is no significant aortic regurgitation at baseline, or when a nonfemoral delivery approach is used." The link between nonfemoral delivery approaches and lower rates of aortic regurgitation suggests "good control of the depth of device delivery and improved catheter technology are key to reducing regurgitation rates," Dr. Van Belle said. "In addition, the prosthesis diameter relative to annulus diameter is key to preventing regurgitation with balloon-expandable devices. Prevention of aortic regurgitation is a major challenge for developing the next-generation device technology."
Minimizing aortic regurgitation
Two ways to cut aortic regurgitation rates following TAVR are to better match the valve to the annulus size, and when possible not finish a TAVR procedure until regurgitation has been minimized.
Two-dimensional transthoracic echocardiography had been the standard approach for annulus sizing as recently as 3 years ago, but it has been replaced with more accurate approaches, either three-dimensional transthoracic echo or CT. "Two-dimensional measurements are seriously limited due to variations and noncircular annular anatomy," Dr. Makkar said in a talk at the meeting. "CT provides the best overall assessment, because in addition to the cross-sectional measurement of the annulus it provides the best assessment of calcification," and three-dimensional transthoracic echo is now standard for intraprocedural assessments, he said.
The impact that a concerted effort to minimize aortic regurgitation can have on outcomes was examined in a single-center study reported by Dr. Jan-Malte Sinning, a cardiologist at University Hospital in Bonn, Germany. Last year, Dr. Sinning and his associates reported developing a quantitative measure of aortic regurgitation immediately following TAVR, the aortic regurgitation (AR) index, based on the difference between a patient’s diastolic blood pressure in the aorta and the left ventricular end-diastolic pressure (J. Am. Coll. Cardiol. 2012;59:1134-41). They then calculated the AR index immediately after TAVR in a prospective series of 167 patients, and set themselves the goal of immediately taking whatever steps were needed to bring the AR index above 25, a cutoff that seemed to correspond to no worse than mild regurgitation.
In their series, 62 patients underwent immediate post-TAVR corrective steps to reduce aortic regurgitation and bring their AR index above 25, most commonly additional balloon dilatation of the valve. The result was that while 16 patients had severe regurgitation before these steps, no patient had severe regurgitation following the corrective measures. The adjustments also cut the incidence of moderate regurgitations from 41 patients to 10, Dr. Sinning reported.
The consequence was that the 30-day stroke rate in the new cohort was 1%, compared with a 6% rate in a historical TAVR cohort at University Hospital in Bonn. The need for pacemaker implants was also cut in half by the intervention compared with the historical group, and 30-day mortality was 3% with these interventions, compared with 7% in the historical controls.
The results suggest that using the AR index as a trigger for taking corrective measures can help improve survival, and that post-TAVR dilatation can successfully decrease regurgitation without increasing patients’ stroke risk, Dr. Sinning concluded.
U.S. operators who perform TAVR say they take similar steps these days to deal with aortic regurgitation after TAVR. "We all understand that you don’t want patients to leave with a leak," said Dr. Popma. "We do everything we can to minimize leaks. When a patient leaves the lab with a moderate or severe leak, there wasn’t anything we could do about it."
Finding TAVR’s limits
Even as TAVR has become the go-to method for high-risk patients, operators have also tried to define the procedure’s outer limit, the point of disease severity when a patient is dying with aortic stenosis rather than because of aortic stenosis, and performing TAVR doesn’t make sense.
Dr. Makkar analyzed 369 inoperable patients who underwent TAVR in both the PARTNER I trial and the nonrandomized continued-access phase that followed. The patients fell into three groups: those who were inoperable because of technical reasons, such as a porcelain aorta or prior chest irradiation; patients who were inoperable because of comorbidities, such as frailty or severe lung disease; and those with both limitations. The 85 patients who were inoperable only because of a technical limitation had a 2-year mortality rate of 23% following TAVR; the other 284 patients who all had comorbidities had a 2-year mortality rate of about 43%.
Last year, Dr. Makkar reported that analysis of these 369 inoperable patients showed a 2-year mortality rate of 20% in the subgroup with an STS score of less than 5%, a mortality rate of 40% among those with a score of 5%-14.5% (but still significantly below the 60% 2-year mortality among similar inoperable patients managed by standard medical therapy only), and a 60% mortality rate among patients with a baseline STS score of 15% or more, an outcome that was no better than that of patients managed without TAVR (N. Engl. J. Med. 2012;366:1696-704).
In a multivariate analysis he recently ran on the data from these 369 patients, the likelihood of 2-year mortality rose by a statistically significant 3% for every 1% increase in the patient’s baseline STS risk score.
"It is important to remember that there are diminishing returns from TAVR in patients with more comorbidities, especially when their STS risk score is greater than 15%," said Dr. Makkar.
Dr. Sinning and Dr. Van Belle had no relevant disclosures. Dr. Mohr is a PARTNER investigator but had no other disclosures. Dr. Bavaria has been a speaker for Edwards and is a PARTNER investigator. Dr. Mack has received travel support from Edwards and is a PARTNER investigator. Dr. Popma has been a consultant to Boston Scientific, Abbott Vascular, and Covidien, and received research support from Boston Scientific, Abbott Vascular, Abiomed, Medtronic, and Cordis. Dr. Fearon has been a consultant to Heart Flow and received research support from St. Jude Medical. Dr. Leon has been a consultant to Symetis; has a major equity stake in Sadra, Claret, Valve Medical, and Apica; has received research support from Boston Scientific, Edwards, and Medtronic; and is a PARTNER investigator. Dr. Makkar has been a consultant to Cordis, Medtronic, Abbott, Entourage Medical, and Abiomed; has been a speaker for Lilly; has received research and travel support from Edwards; and is a PARTNER investigator.
On Twitter @mitchelzoler
SAN FRANCISCO – It’s been barely half a year since U.S. cardiologists and cardiac surgeons first became able to routinely offer operable, high-risk patients with aortic stenosis the option of transcatheter valve replacement, yet in the first few months the transcatheter approach quickly rivaled open surgery.
But for the time being in U.S. practice, transcatheter aortic valve replacement (TAVR) remains boxed into the high-risk niche, along with the subgroup of patients who are not suitable for open surgery, king of a pair of relatively small hills.
And no matter how well TAVR performs in the current pair of trials that are comparing it with open surgical aortic valve replacement (SAVR) for intermediate-risk patients, it will remain relegated to niche status for years to come. That’s because roughly two-thirds of all operable patients with aortic stenosis who need valve replacement fall into the low-risk category, with a Society of Thoracic Surgeons (STS) risk score of less than 4%, which experts agree will remain SAVR’s exclusive territory for the foreseeable future.
The high-risk stratum of operable patients, which TAVR now dominates, constitutes about 10% of all patients who need a new aortic valve and can undergo open surgery, patients with an STS score greater than 8%. The intermediate-risk category – an STS score of 4%-8%, where TAVR now vies against open SAVR in two high-profile trials – makes up the final quarter of the operable-patient pie.
Within the high-risk and operable universe, TAVR’s rise has been meteoric, starting last October when the Food and Drug Administration gave Edwards, marketer of the SAPIEN valve system, approval for these patients. A small survey of operators from U.S. TAVR programs in March at the annual scientific session of the American College of Cardiology (ACC) revealed a uniform perception that by early 2013 a sizable majority of U.S. patients with severe aortic stenosis who are deemed operable and are at high surgical risk will wind up being treated by TAVR instead of SAVR. The cardiac surgeons who collaborate on TAVR seem to have fully conceded the advantages of TAVR for these patients.
"We generally go with TAVR. Most patients want it, and with the equivalence" in outcomes from the first PARTNER (Placement of Aortic Transcatheter Valves) cohort A (operable patients) trial (New Engl. J. Med. 2010:364:2187-98), "you usually go with the less invasive procedure," said Dr. Joseph E. Bavaria, professor of surgery and director of thoracic aortic surgery at the University of Pennsylvania in Philadelphia. The small number of high-risk patients who go to open surgery tend to be men, "because they do better with surgery, especially if their life expectancy is greater than 5-8 years," or patients with high stroke risk, Dr. Bavaria said in an interview at the annual meeting of the American College of Cardiology.
"Operable, high-risk patients get TAVR. I’m a surgeon saying that. I’ve already done the [PARTNER cohort A] trial, and I don’t want to do it again," said Dr. Michael Mack, a cardiothoracic surgeon at the Heart Hospital in Plano, Texas. "The results are the same [from TAVR and SAVR] at 30 days, 1 year, and 2 years, but boy do we beat up patients with open surgery. If it was my mom, she’d get TAVR," he said in an interview. "The tie goes to the less invasive treatment."
When high-risk, operable patients are seen by the heart team Dr. Mack works with, the only ones who go to SAVR are patients – generally men – who have a large aortic annulus and need a 29-mm-diameter valve, which is not available for the time being to U.S. TAVR patients; women with septal hypertrophy causing significant left ventricular outflow-tract obstruction; and the small percent of patients who opt for open surgery, usually because it’s the more established approach or because they fear a higher stroke risk from TAVR.
"The majority of high-risk, operable patients now go to TAVR; I think that’s pretty much true across the United States," said Dr. Jeffrey J. Popma, a cardiologist who does TAVR and is a professor of medicine at Harvard University in Boston.
Where TAVR stood in 2010 and 2011
How is TAVR performing? Performance can only be completely assessed months or years after the fact, so the impact that high-risk, operable U.S. patients received from TAVR’s use in routine practice in late 2012 and the first months of 2013 remains to be seen. The most recently treated patients now available for meaningful analysis in large numbers come from 2010 and 2011: new data reported at the ACC meeting from a U.S. program of continued TAVR access that began in late 2009 following the end of recruitment into the first PARTNER trial, and 1-year follow-up of nearly 14,000 patients who underwent TAVR in 2011 as part of routine practice in Germany and were entered into the country’s national TAVR registry.
Both databases had good news for high-risk or inoperable patients. TAVR outcomes in the first couple of years immediately following PARTNER in both the United States and Germany showed clinically meaningful improvements over the way TAVR performed during the first PARTNER trial. Less optimistic news for the low- and intermediate-risk patients who underwent TAVR in Germany, where wider device use is possible, was that in broad terms open surgery outperformed TAVR in these lower-risk patients, although TAVR’s defenders are quick to point out how tricky it is to make cross-treatment comparisons with registry data.
The nonrandomized, continued-access cohort that followed the first PARTNER trial at 22 U.S. centers, 3 sites in Canada, and 1 site in Germany included 1,017 inoperable or high-risk patients who had successful transfemoral TAVR between August 2009 and December 2011. When compared with the 415 inoperable or high-risk patients who underwent transfemoral TAVR in both cohorts of PARTNER, the more recently treated patients had a statistically significant decrease in all-cause 1-year mortality, from a 25% death rate in PARTNER to a 20% rate during the continued-access period, Dr. William F. Fearon reported at the meeting.
The continued-access patients also showed significant cuts in their rates of major vascular complications, which dropped from 15% of patients in PARTNER to 6% during continued access; and in rates of major bleeding complications, which fell from 15% in PARTNER to 7% during continued access. Strokes were also down during continued access, 5% compared with 7% during PARTNER, but this was not a statistically significant drop, reported Dr. Fearon, a cardiologist at Stanford (Calif.) University.
"Maybe these improvements are due to better patient selection, and maybe we have also gotten better at what we do," commented Dr. Popma.
The latest German experience
The 1-year German Aortic Valve Registry (GARY) results from 2011 show similar improvements compared with PARTNER. Among the 2,689 patients who underwent transvascular TAVR, the 1-year total mortality rate was 21%, and in the subset of patients with stroke data the combined rate of major and minor stroke was 5%.
But it was the way that transvascular TAVR (which includes both transfemoral and other vascular approaches but excludes the 1,181 patients who underwent transapical TAVR) stacked up against open surgical replacement that raised concern.
Of the 13,860 total patients entered into GARY during 2011, 9,985 underwent SAVR, with 6,523 of these patients undergoing an isolated procedure (the rest had valve replacement combined with coronary artery bypass). One-year mortality was 7% in patients who had isolated SAVR, dramatically below the 21% rate among the transvascular TAVR patients, Dr. Friedrich-Wilhelm Mohr reported at the meeting. The transapical TAVR patients had a 28% 1-year mortality rate.
To address the issue of between-treatment differences in patients’ underlying risk, Dr. Mohr presented two sets of analyses that stratified patients with two different risk-scoring systems, the EuroSCORE and the AKL (aortic valve surgery) score, also known as the German aortic valve score. The results showed how disparate the outcomes were when patients were subgrouped by their underlying risk. Among the patients who had lone SAVR, 80% fell into the lowest-risk level, with an AKL score of less than 3. Among the transvascular TAVR patients, only 17% had AKL scores below 3.
Among patients with AKL scores less than 3, those who underwent SAVR without bypass had a roughly 5% mortality rate after 1 year, compared with about a 15% mortality rate among the transvascular TAVR patients. Analyses in higher-risk patient subgroups showed that the survival gap between SAVR and TAVR patients progressively shrank, until in high-risk patients – as in those studied in PARTNER – the mortality rates were about the same in the SAVR and TAVR groups, said Dr. Mohr, professor and director of heart surgery at Leipzig University, Germany. He also reported similar findings when patients were stratified by their baseline EuroSCORE.
A big factor behind the worse survival among lower-risk TAVR patients is the problem of aortic regurgitation, Dr. Mohr said. Following valve replacement, 56% of the transvascular TAVR patients had grade 1 regurgitation, 7% had grade 2, and less than 1% had grade 3 leakage. These rates are way too high, he said. "Our major concern is the incidence of aortic regurgitation; more than half of the [TAVR] patients had some kind of regurgitation. Regurgitation matters whether it is mild or severe."
Despite his concern, TAVR use in Germany is accelerating. The total number of aortic valve replacements done in Germany jumped from just less than 14,000 in 2011 to more than 22,000 last year; TAVR cases more than doubled, from fewer than 4,000 in 2011 to nearly 10,000 in 2012, with a "move to intermediate-risk groups," said Dr. Mohr, who made it clear that he does not endorse this trend. "TAVR must be proven better than or equal to surgery before it’s used on a large scale," he said. The GARY results show "a clear difference [between TAVR and SAVR] in lower-risk patients. The GARY results do not support going into intermediate-risk patients."
Dr. Martin B. Leon agreed with Dr. Mohr that a definitive determination of whether TAVR is at least as good as SAVR in intermediate-risk patients must await results from the two major, ongoing multicenter trials testing this hypothesis, the PARTNER II trial, using the Edwards balloon-expandable SAPIEN XT valve system, and the SURTAVI (Safety and Efficacy Study of the Medtronic CoreValve System in the Treatment of Severe, Symptomatic Aortic Stenosis in Intermediate Risk Subjects Who Need Aortic Valve Replacement) trial. But Dr. Leon also cautioned that possible confounders might be distorting the GARY results, creating what he calls the "GARY Fallacy."
"The GARY Fallacy is the absurd notion that you can compare SAVR and TAVR in various risk strata without formal risk-adjustment methods to account for imbalances in baseline variables that are not captured in standard risk scores," he said in a talk at the meeting. "Aortic-stenosis patients were selected for TAVR based on their presumed increased risk, including many variables that are not represented in the risk algorithms, such as frailty, liver disease, porcelain aorta, a hostile chest, dementia, and severe chronic obstructive pulmonary disease. Therefore, the risk scores for TAVR patients underrepresent their true risk," Dr. Leon said.
But it’s also possible that TAVR needs more refinement before it completely catches up with SAVR, especially in patients who have the best outcomes from SAVR.
"I think SAVR outperforms TAVR in low-risk patients in the German registry because SAVR is a more mature procedure," said Dr. Raj R. Makkar, a TAVR operator and director of interventional cardiology at Cedars-Sinai Medical Center in Los Angeles. "Maybe this will change, as TAVR becomes safer with fewer valve leaks, strokes, and vascular complications."
Assessing patient risks
Experts also realize that the EuroSCORE, the AKL score, and the other risk-stratification tools now available have flaws when applied to TAVR patients. "Risk stratification for TAVR and SAVR is very problematic; the EuroSCORE has shown poor predictive value for mortality," Dr. Leon said. And while the AKL score was developed specifically for SAVR patients, its relevance to TAVR patients is suspect. In the first PARTNER trial, the multivariate predictors of mortality in the TAVR patients were "completely different" from the predictors in the SAVR patients, he noted.
"It’s tricky calculating scores," agreed Dr. Makkar. Both he and Dr. Mohr cited comorbidities such as pulmonary hypertension, cirrhosis, knee replacement producing impaired mobility, and porcelain aorta that each ratchet up a patient’s risk but have no effect whatsoever on a patient’s EuroSCORE or STS score.
The German cardiology and cardiac surgery societies recognize the limitations of current risk-scoring formulas and are developing a risk-stratification tool specifically designed for TAVR patients, Dr. Mohr said.
The way patients are assessed before, during, and after TAVR is receiving careful scrutiny from some investigators who reported their findings at the ACC meeting, with a particular focus on efforts to characterize and minimize aortic-valve regurgitation following TAVR.
One report, for example, reviewed 2,679 patients who underwent TAVR at any of 33 French centers and 1 in Monaco between January 2010 and October 2011, and were enrolled in the French Aortic National CoreValve and Edwards (FRANCE 2) Registry, established by the French cardiology and thoracic and cardiovascular surgery societies (N. Engl. J. Med. 2012;366:1705-15). FRANCE 2 includes nearly 1,900 patients who received the balloon-expandable Edwards SAPIEN valve, and nearly 900 treated with the self-expanding Medtronic CoreValve device.
Following TAVR, 60% of all patients in the registry had paravalvular aortic regurgitation: 45% with grade 1 regurgitation, 14% with grade 2, and 1% with grade 3 or 4. In a multivariate analysis, the self-expandable device was linked to twice the rate of higher-grade aortic regurgitation, grade 2 or higher, compared with the balloon-expandable valve; and TAVRs done via the femoral artery approach were also about twice as likely to result in higher-grade regurgitations compared with other catheterization routes, reported Dr. Eric Van Belle, a professor at the Cardiology Hospital in Lille, France.
Postprocedural paravalvular regurgitation of grade 2 or higher "was associated with a twofold increase in 1-year mortality, and was the strongest independent predictor of mortality," said Dr. Van Belle in his talk at the meeting. In addition, "annulus diameter and prosthesis diameter were major determinants of aortic regurgitation" in patients who received a balloon-expandable valve.
The FRANCE 2 results showed that postprocedural aortic regurgitation at grade 2 or higher "is a major issue and should be avoided, especially when there is no significant aortic regurgitation at baseline, or when a nonfemoral delivery approach is used." The link between nonfemoral delivery approaches and lower rates of aortic regurgitation suggests "good control of the depth of device delivery and improved catheter technology are key to reducing regurgitation rates," Dr. Van Belle said. "In addition, the prosthesis diameter relative to annulus diameter is key to preventing regurgitation with balloon-expandable devices. Prevention of aortic regurgitation is a major challenge for developing the next-generation device technology."
Minimizing aortic regurgitation
Two ways to cut aortic regurgitation rates following TAVR are to better match the valve to the annulus size, and when possible not finish a TAVR procedure until regurgitation has been minimized.
Two-dimensional transthoracic echocardiography had been the standard approach for annulus sizing as recently as 3 years ago, but it has been replaced with more accurate approaches, either three-dimensional transthoracic echo or CT. "Two-dimensional measurements are seriously limited due to variations and noncircular annular anatomy," Dr. Makkar said in a talk at the meeting. "CT provides the best overall assessment, because in addition to the cross-sectional measurement of the annulus it provides the best assessment of calcification," and three-dimensional transthoracic echo is now standard for intraprocedural assessments, he said.
The impact that a concerted effort to minimize aortic regurgitation can have on outcomes was examined in a single-center study reported by Dr. Jan-Malte Sinning, a cardiologist at University Hospital in Bonn, Germany. Last year, Dr. Sinning and his associates reported developing a quantitative measure of aortic regurgitation immediately following TAVR, the aortic regurgitation (AR) index, based on the difference between a patient’s diastolic blood pressure in the aorta and the left ventricular end-diastolic pressure (J. Am. Coll. Cardiol. 2012;59:1134-41). They then calculated the AR index immediately after TAVR in a prospective series of 167 patients, and set themselves the goal of immediately taking whatever steps were needed to bring the AR index above 25, a cutoff that seemed to correspond to no worse than mild regurgitation.
In their series, 62 patients underwent immediate post-TAVR corrective steps to reduce aortic regurgitation and bring their AR index above 25, most commonly additional balloon dilatation of the valve. The result was that while 16 patients had severe regurgitation before these steps, no patient had severe regurgitation following the corrective measures. The adjustments also cut the incidence of moderate regurgitations from 41 patients to 10, Dr. Sinning reported.
The consequence was that the 30-day stroke rate in the new cohort was 1%, compared with a 6% rate in a historical TAVR cohort at University Hospital in Bonn. The need for pacemaker implants was also cut in half by the intervention compared with the historical group, and 30-day mortality was 3% with these interventions, compared with 7% in the historical controls.
The results suggest that using the AR index as a trigger for taking corrective measures can help improve survival, and that post-TAVR dilatation can successfully decrease regurgitation without increasing patients’ stroke risk, Dr. Sinning concluded.
U.S. operators who perform TAVR say they take similar steps these days to deal with aortic regurgitation after TAVR. "We all understand that you don’t want patients to leave with a leak," said Dr. Popma. "We do everything we can to minimize leaks. When a patient leaves the lab with a moderate or severe leak, there wasn’t anything we could do about it."
Finding TAVR’s limits
Even as TAVR has become the go-to method for high-risk patients, operators have also tried to define the procedure’s outer limit, the point of disease severity when a patient is dying with aortic stenosis rather than because of aortic stenosis, and performing TAVR doesn’t make sense.
Dr. Makkar analyzed 369 inoperable patients who underwent TAVR in both the PARTNER I trial and the nonrandomized continued-access phase that followed. The patients fell into three groups: those who were inoperable because of technical reasons, such as a porcelain aorta or prior chest irradiation; patients who were inoperable because of comorbidities, such as frailty or severe lung disease; and those with both limitations. The 85 patients who were inoperable only because of a technical limitation had a 2-year mortality rate of 23% following TAVR; the other 284 patients who all had comorbidities had a 2-year mortality rate of about 43%.
Last year, Dr. Makkar reported that analysis of these 369 inoperable patients showed a 2-year mortality rate of 20% in the subgroup with an STS score of less than 5%, a mortality rate of 40% among those with a score of 5%-14.5% (but still significantly below the 60% 2-year mortality among similar inoperable patients managed by standard medical therapy only), and a 60% mortality rate among patients with a baseline STS score of 15% or more, an outcome that was no better than that of patients managed without TAVR (N. Engl. J. Med. 2012;366:1696-704).
In a multivariate analysis he recently ran on the data from these 369 patients, the likelihood of 2-year mortality rose by a statistically significant 3% for every 1% increase in the patient’s baseline STS risk score.
"It is important to remember that there are diminishing returns from TAVR in patients with more comorbidities, especially when their STS risk score is greater than 15%," said Dr. Makkar.
Dr. Sinning and Dr. Van Belle had no relevant disclosures. Dr. Mohr is a PARTNER investigator but had no other disclosures. Dr. Bavaria has been a speaker for Edwards and is a PARTNER investigator. Dr. Mack has received travel support from Edwards and is a PARTNER investigator. Dr. Popma has been a consultant to Boston Scientific, Abbott Vascular, and Covidien, and received research support from Boston Scientific, Abbott Vascular, Abiomed, Medtronic, and Cordis. Dr. Fearon has been a consultant to Heart Flow and received research support from St. Jude Medical. Dr. Leon has been a consultant to Symetis; has a major equity stake in Sadra, Claret, Valve Medical, and Apica; has received research support from Boston Scientific, Edwards, and Medtronic; and is a PARTNER investigator. Dr. Makkar has been a consultant to Cordis, Medtronic, Abbott, Entourage Medical, and Abiomed; has been a speaker for Lilly; has received research and travel support from Edwards; and is a PARTNER investigator.
On Twitter @mitchelzoler
SAN FRANCISCO – It’s been barely half a year since U.S. cardiologists and cardiac surgeons first became able to routinely offer operable, high-risk patients with aortic stenosis the option of transcatheter valve replacement, yet in the first few months the transcatheter approach quickly rivaled open surgery.
But for the time being in U.S. practice, transcatheter aortic valve replacement (TAVR) remains boxed into the high-risk niche, along with the subgroup of patients who are not suitable for open surgery, king of a pair of relatively small hills.
And no matter how well TAVR performs in the current pair of trials that are comparing it with open surgical aortic valve replacement (SAVR) for intermediate-risk patients, it will remain relegated to niche status for years to come. That’s because roughly two-thirds of all operable patients with aortic stenosis who need valve replacement fall into the low-risk category, with a Society of Thoracic Surgeons (STS) risk score of less than 4%, which experts agree will remain SAVR’s exclusive territory for the foreseeable future.
The high-risk stratum of operable patients, which TAVR now dominates, constitutes about 10% of all patients who need a new aortic valve and can undergo open surgery, patients with an STS score greater than 8%. The intermediate-risk category – an STS score of 4%-8%, where TAVR now vies against open SAVR in two high-profile trials – makes up the final quarter of the operable-patient pie.
Within the high-risk and operable universe, TAVR’s rise has been meteoric, starting last October when the Food and Drug Administration gave Edwards, marketer of the SAPIEN valve system, approval for these patients. A small survey of operators from U.S. TAVR programs in March at the annual scientific session of the American College of Cardiology (ACC) revealed a uniform perception that by early 2013 a sizable majority of U.S. patients with severe aortic stenosis who are deemed operable and are at high surgical risk will wind up being treated by TAVR instead of SAVR. The cardiac surgeons who collaborate on TAVR seem to have fully conceded the advantages of TAVR for these patients.
"We generally go with TAVR. Most patients want it, and with the equivalence" in outcomes from the first PARTNER (Placement of Aortic Transcatheter Valves) cohort A (operable patients) trial (New Engl. J. Med. 2010:364:2187-98), "you usually go with the less invasive procedure," said Dr. Joseph E. Bavaria, professor of surgery and director of thoracic aortic surgery at the University of Pennsylvania in Philadelphia. The small number of high-risk patients who go to open surgery tend to be men, "because they do better with surgery, especially if their life expectancy is greater than 5-8 years," or patients with high stroke risk, Dr. Bavaria said in an interview at the annual meeting of the American College of Cardiology.
"Operable, high-risk patients get TAVR. I’m a surgeon saying that. I’ve already done the [PARTNER cohort A] trial, and I don’t want to do it again," said Dr. Michael Mack, a cardiothoracic surgeon at the Heart Hospital in Plano, Texas. "The results are the same [from TAVR and SAVR] at 30 days, 1 year, and 2 years, but boy do we beat up patients with open surgery. If it was my mom, she’d get TAVR," he said in an interview. "The tie goes to the less invasive treatment."
When high-risk, operable patients are seen by the heart team Dr. Mack works with, the only ones who go to SAVR are patients – generally men – who have a large aortic annulus and need a 29-mm-diameter valve, which is not available for the time being to U.S. TAVR patients; women with septal hypertrophy causing significant left ventricular outflow-tract obstruction; and the small percent of patients who opt for open surgery, usually because it’s the more established approach or because they fear a higher stroke risk from TAVR.
"The majority of high-risk, operable patients now go to TAVR; I think that’s pretty much true across the United States," said Dr. Jeffrey J. Popma, a cardiologist who does TAVR and is a professor of medicine at Harvard University in Boston.
Where TAVR stood in 2010 and 2011
How is TAVR performing? Performance can only be completely assessed months or years after the fact, so the impact that high-risk, operable U.S. patients received from TAVR’s use in routine practice in late 2012 and the first months of 2013 remains to be seen. The most recently treated patients now available for meaningful analysis in large numbers come from 2010 and 2011: new data reported at the ACC meeting from a U.S. program of continued TAVR access that began in late 2009 following the end of recruitment into the first PARTNER trial, and 1-year follow-up of nearly 14,000 patients who underwent TAVR in 2011 as part of routine practice in Germany and were entered into the country’s national TAVR registry.
Both databases had good news for high-risk or inoperable patients. TAVR outcomes in the first couple of years immediately following PARTNER in both the United States and Germany showed clinically meaningful improvements over the way TAVR performed during the first PARTNER trial. Less optimistic news for the low- and intermediate-risk patients who underwent TAVR in Germany, where wider device use is possible, was that in broad terms open surgery outperformed TAVR in these lower-risk patients, although TAVR’s defenders are quick to point out how tricky it is to make cross-treatment comparisons with registry data.
The nonrandomized, continued-access cohort that followed the first PARTNER trial at 22 U.S. centers, 3 sites in Canada, and 1 site in Germany included 1,017 inoperable or high-risk patients who had successful transfemoral TAVR between August 2009 and December 2011. When compared with the 415 inoperable or high-risk patients who underwent transfemoral TAVR in both cohorts of PARTNER, the more recently treated patients had a statistically significant decrease in all-cause 1-year mortality, from a 25% death rate in PARTNER to a 20% rate during the continued-access period, Dr. William F. Fearon reported at the meeting.
The continued-access patients also showed significant cuts in their rates of major vascular complications, which dropped from 15% of patients in PARTNER to 6% during continued access; and in rates of major bleeding complications, which fell from 15% in PARTNER to 7% during continued access. Strokes were also down during continued access, 5% compared with 7% during PARTNER, but this was not a statistically significant drop, reported Dr. Fearon, a cardiologist at Stanford (Calif.) University.
"Maybe these improvements are due to better patient selection, and maybe we have also gotten better at what we do," commented Dr. Popma.
The latest German experience
The 1-year German Aortic Valve Registry (GARY) results from 2011 show similar improvements compared with PARTNER. Among the 2,689 patients who underwent transvascular TAVR, the 1-year total mortality rate was 21%, and in the subset of patients with stroke data the combined rate of major and minor stroke was 5%.
But it was the way that transvascular TAVR (which includes both transfemoral and other vascular approaches but excludes the 1,181 patients who underwent transapical TAVR) stacked up against open surgical replacement that raised concern.
Of the 13,860 total patients entered into GARY during 2011, 9,985 underwent SAVR, with 6,523 of these patients undergoing an isolated procedure (the rest had valve replacement combined with coronary artery bypass). One-year mortality was 7% in patients who had isolated SAVR, dramatically below the 21% rate among the transvascular TAVR patients, Dr. Friedrich-Wilhelm Mohr reported at the meeting. The transapical TAVR patients had a 28% 1-year mortality rate.
To address the issue of between-treatment differences in patients’ underlying risk, Dr. Mohr presented two sets of analyses that stratified patients with two different risk-scoring systems, the EuroSCORE and the AKL (aortic valve surgery) score, also known as the German aortic valve score. The results showed how disparate the outcomes were when patients were subgrouped by their underlying risk. Among the patients who had lone SAVR, 80% fell into the lowest-risk level, with an AKL score of less than 3. Among the transvascular TAVR patients, only 17% had AKL scores below 3.
Among patients with AKL scores less than 3, those who underwent SAVR without bypass had a roughly 5% mortality rate after 1 year, compared with about a 15% mortality rate among the transvascular TAVR patients. Analyses in higher-risk patient subgroups showed that the survival gap between SAVR and TAVR patients progressively shrank, until in high-risk patients – as in those studied in PARTNER – the mortality rates were about the same in the SAVR and TAVR groups, said Dr. Mohr, professor and director of heart surgery at Leipzig University, Germany. He also reported similar findings when patients were stratified by their baseline EuroSCORE.
A big factor behind the worse survival among lower-risk TAVR patients is the problem of aortic regurgitation, Dr. Mohr said. Following valve replacement, 56% of the transvascular TAVR patients had grade 1 regurgitation, 7% had grade 2, and less than 1% had grade 3 leakage. These rates are way too high, he said. "Our major concern is the incidence of aortic regurgitation; more than half of the [TAVR] patients had some kind of regurgitation. Regurgitation matters whether it is mild or severe."
Despite his concern, TAVR use in Germany is accelerating. The total number of aortic valve replacements done in Germany jumped from just less than 14,000 in 2011 to more than 22,000 last year; TAVR cases more than doubled, from fewer than 4,000 in 2011 to nearly 10,000 in 2012, with a "move to intermediate-risk groups," said Dr. Mohr, who made it clear that he does not endorse this trend. "TAVR must be proven better than or equal to surgery before it’s used on a large scale," he said. The GARY results show "a clear difference [between TAVR and SAVR] in lower-risk patients. The GARY results do not support going into intermediate-risk patients."
Dr. Martin B. Leon agreed with Dr. Mohr that a definitive determination of whether TAVR is at least as good as SAVR in intermediate-risk patients must await results from the two major, ongoing multicenter trials testing this hypothesis, the PARTNER II trial, using the Edwards balloon-expandable SAPIEN XT valve system, and the SURTAVI (Safety and Efficacy Study of the Medtronic CoreValve System in the Treatment of Severe, Symptomatic Aortic Stenosis in Intermediate Risk Subjects Who Need Aortic Valve Replacement) trial. But Dr. Leon also cautioned that possible confounders might be distorting the GARY results, creating what he calls the "GARY Fallacy."
"The GARY Fallacy is the absurd notion that you can compare SAVR and TAVR in various risk strata without formal risk-adjustment methods to account for imbalances in baseline variables that are not captured in standard risk scores," he said in a talk at the meeting. "Aortic-stenosis patients were selected for TAVR based on their presumed increased risk, including many variables that are not represented in the risk algorithms, such as frailty, liver disease, porcelain aorta, a hostile chest, dementia, and severe chronic obstructive pulmonary disease. Therefore, the risk scores for TAVR patients underrepresent their true risk," Dr. Leon said.
But it’s also possible that TAVR needs more refinement before it completely catches up with SAVR, especially in patients who have the best outcomes from SAVR.
"I think SAVR outperforms TAVR in low-risk patients in the German registry because SAVR is a more mature procedure," said Dr. Raj R. Makkar, a TAVR operator and director of interventional cardiology at Cedars-Sinai Medical Center in Los Angeles. "Maybe this will change, as TAVR becomes safer with fewer valve leaks, strokes, and vascular complications."
Assessing patient risks
Experts also realize that the EuroSCORE, the AKL score, and the other risk-stratification tools now available have flaws when applied to TAVR patients. "Risk stratification for TAVR and SAVR is very problematic; the EuroSCORE has shown poor predictive value for mortality," Dr. Leon said. And while the AKL score was developed specifically for SAVR patients, its relevance to TAVR patients is suspect. In the first PARTNER trial, the multivariate predictors of mortality in the TAVR patients were "completely different" from the predictors in the SAVR patients, he noted.
"It’s tricky calculating scores," agreed Dr. Makkar. Both he and Dr. Mohr cited comorbidities such as pulmonary hypertension, cirrhosis, knee replacement producing impaired mobility, and porcelain aorta that each ratchet up a patient’s risk but have no effect whatsoever on a patient’s EuroSCORE or STS score.
The German cardiology and cardiac surgery societies recognize the limitations of current risk-scoring formulas and are developing a risk-stratification tool specifically designed for TAVR patients, Dr. Mohr said.
The way patients are assessed before, during, and after TAVR is receiving careful scrutiny from some investigators who reported their findings at the ACC meeting, with a particular focus on efforts to characterize and minimize aortic-valve regurgitation following TAVR.
One report, for example, reviewed 2,679 patients who underwent TAVR at any of 33 French centers and 1 in Monaco between January 2010 and October 2011, and were enrolled in the French Aortic National CoreValve and Edwards (FRANCE 2) Registry, established by the French cardiology and thoracic and cardiovascular surgery societies (N. Engl. J. Med. 2012;366:1705-15). FRANCE 2 includes nearly 1,900 patients who received the balloon-expandable Edwards SAPIEN valve, and nearly 900 treated with the self-expanding Medtronic CoreValve device.
Following TAVR, 60% of all patients in the registry had paravalvular aortic regurgitation: 45% with grade 1 regurgitation, 14% with grade 2, and 1% with grade 3 or 4. In a multivariate analysis, the self-expandable device was linked to twice the rate of higher-grade aortic regurgitation, grade 2 or higher, compared with the balloon-expandable valve; and TAVRs done via the femoral artery approach were also about twice as likely to result in higher-grade regurgitations compared with other catheterization routes, reported Dr. Eric Van Belle, a professor at the Cardiology Hospital in Lille, France.
Postprocedural paravalvular regurgitation of grade 2 or higher "was associated with a twofold increase in 1-year mortality, and was the strongest independent predictor of mortality," said Dr. Van Belle in his talk at the meeting. In addition, "annulus diameter and prosthesis diameter were major determinants of aortic regurgitation" in patients who received a balloon-expandable valve.
The FRANCE 2 results showed that postprocedural aortic regurgitation at grade 2 or higher "is a major issue and should be avoided, especially when there is no significant aortic regurgitation at baseline, or when a nonfemoral delivery approach is used." The link between nonfemoral delivery approaches and lower rates of aortic regurgitation suggests "good control of the depth of device delivery and improved catheter technology are key to reducing regurgitation rates," Dr. Van Belle said. "In addition, the prosthesis diameter relative to annulus diameter is key to preventing regurgitation with balloon-expandable devices. Prevention of aortic regurgitation is a major challenge for developing the next-generation device technology."
Minimizing aortic regurgitation
Two ways to cut aortic regurgitation rates following TAVR are to better match the valve to the annulus size, and when possible not finish a TAVR procedure until regurgitation has been minimized.
Two-dimensional transthoracic echocardiography had been the standard approach for annulus sizing as recently as 3 years ago, but it has been replaced with more accurate approaches, either three-dimensional transthoracic echo or CT. "Two-dimensional measurements are seriously limited due to variations and noncircular annular anatomy," Dr. Makkar said in a talk at the meeting. "CT provides the best overall assessment, because in addition to the cross-sectional measurement of the annulus it provides the best assessment of calcification," and three-dimensional transthoracic echo is now standard for intraprocedural assessments, he said.
The impact that a concerted effort to minimize aortic regurgitation can have on outcomes was examined in a single-center study reported by Dr. Jan-Malte Sinning, a cardiologist at University Hospital in Bonn, Germany. Last year, Dr. Sinning and his associates reported developing a quantitative measure of aortic regurgitation immediately following TAVR, the aortic regurgitation (AR) index, based on the difference between a patient’s diastolic blood pressure in the aorta and the left ventricular end-diastolic pressure (J. Am. Coll. Cardiol. 2012;59:1134-41). They then calculated the AR index immediately after TAVR in a prospective series of 167 patients, and set themselves the goal of immediately taking whatever steps were needed to bring the AR index above 25, a cutoff that seemed to correspond to no worse than mild regurgitation.
In their series, 62 patients underwent immediate post-TAVR corrective steps to reduce aortic regurgitation and bring their AR index above 25, most commonly additional balloon dilatation of the valve. The result was that while 16 patients had severe regurgitation before these steps, no patient had severe regurgitation following the corrective measures. The adjustments also cut the incidence of moderate regurgitations from 41 patients to 10, Dr. Sinning reported.
The consequence was that the 30-day stroke rate in the new cohort was 1%, compared with a 6% rate in a historical TAVR cohort at University Hospital in Bonn. The need for pacemaker implants was also cut in half by the intervention compared with the historical group, and 30-day mortality was 3% with these interventions, compared with 7% in the historical controls.
The results suggest that using the AR index as a trigger for taking corrective measures can help improve survival, and that post-TAVR dilatation can successfully decrease regurgitation without increasing patients’ stroke risk, Dr. Sinning concluded.
U.S. operators who perform TAVR say they take similar steps these days to deal with aortic regurgitation after TAVR. "We all understand that you don’t want patients to leave with a leak," said Dr. Popma. "We do everything we can to minimize leaks. When a patient leaves the lab with a moderate or severe leak, there wasn’t anything we could do about it."
Finding TAVR’s limits
Even as TAVR has become the go-to method for high-risk patients, operators have also tried to define the procedure’s outer limit, the point of disease severity when a patient is dying with aortic stenosis rather than because of aortic stenosis, and performing TAVR doesn’t make sense.
Dr. Makkar analyzed 369 inoperable patients who underwent TAVR in both the PARTNER I trial and the nonrandomized continued-access phase that followed. The patients fell into three groups: those who were inoperable because of technical reasons, such as a porcelain aorta or prior chest irradiation; patients who were inoperable because of comorbidities, such as frailty or severe lung disease; and those with both limitations. The 85 patients who were inoperable only because of a technical limitation had a 2-year mortality rate of 23% following TAVR; the other 284 patients who all had comorbidities had a 2-year mortality rate of about 43%.
Last year, Dr. Makkar reported that analysis of these 369 inoperable patients showed a 2-year mortality rate of 20% in the subgroup with an STS score of less than 5%, a mortality rate of 40% among those with a score of 5%-14.5% (but still significantly below the 60% 2-year mortality among similar inoperable patients managed by standard medical therapy only), and a 60% mortality rate among patients with a baseline STS score of 15% or more, an outcome that was no better than that of patients managed without TAVR (N. Engl. J. Med. 2012;366:1696-704).
In a multivariate analysis he recently ran on the data from these 369 patients, the likelihood of 2-year mortality rose by a statistically significant 3% for every 1% increase in the patient’s baseline STS risk score.
"It is important to remember that there are diminishing returns from TAVR in patients with more comorbidities, especially when their STS risk score is greater than 15%," said Dr. Makkar.
Dr. Sinning and Dr. Van Belle had no relevant disclosures. Dr. Mohr is a PARTNER investigator but had no other disclosures. Dr. Bavaria has been a speaker for Edwards and is a PARTNER investigator. Dr. Mack has received travel support from Edwards and is a PARTNER investigator. Dr. Popma has been a consultant to Boston Scientific, Abbott Vascular, and Covidien, and received research support from Boston Scientific, Abbott Vascular, Abiomed, Medtronic, and Cordis. Dr. Fearon has been a consultant to Heart Flow and received research support from St. Jude Medical. Dr. Leon has been a consultant to Symetis; has a major equity stake in Sadra, Claret, Valve Medical, and Apica; has received research support from Boston Scientific, Edwards, and Medtronic; and is a PARTNER investigator. Dr. Makkar has been a consultant to Cordis, Medtronic, Abbott, Entourage Medical, and Abiomed; has been a speaker for Lilly; has received research and travel support from Edwards; and is a PARTNER investigator.
On Twitter @mitchelzoler
AT ACC 13