User login
Official Newspaper of the American College of Surgeons
Register now to activate your free JACS iPad app
American College of Surgeons (ACS) members and subscribers to the Journal of the American College of Surgeons (JACS) have free access to the JACS iPad® Edition. You need only register for the free app to activate access to JACS contents at http://www.journalacs.org/content/mobileaccessinstructions. The JACS iPad app and digital journals can then be downloaded at the iTunes® app store at https://itunes.apple.com/us/app/ jacs-official-scientific-journal/id491332618?mt=8 and accessed through the new iPad Newstand interface. The app allows users to access JACS content wherever and whenever it is needed.
The app automatically downloads new issues and allows users to interact with the Journal by tapping links to content. Users may bookmark their favorite articles, take notes and highlight items within articles, save the material to their favorite electronic reading device, and quickly access articles and issues.
American College of Surgeons (ACS) members and subscribers to the Journal of the American College of Surgeons (JACS) have free access to the JACS iPad® Edition. You need only register for the free app to activate access to JACS contents at http://www.journalacs.org/content/mobileaccessinstructions. The JACS iPad app and digital journals can then be downloaded at the iTunes® app store at https://itunes.apple.com/us/app/ jacs-official-scientific-journal/id491332618?mt=8 and accessed through the new iPad Newstand interface. The app allows users to access JACS content wherever and whenever it is needed.
The app automatically downloads new issues and allows users to interact with the Journal by tapping links to content. Users may bookmark their favorite articles, take notes and highlight items within articles, save the material to their favorite electronic reading device, and quickly access articles and issues.
American College of Surgeons (ACS) members and subscribers to the Journal of the American College of Surgeons (JACS) have free access to the JACS iPad® Edition. You need only register for the free app to activate access to JACS contents at http://www.journalacs.org/content/mobileaccessinstructions. The JACS iPad app and digital journals can then be downloaded at the iTunes® app store at https://itunes.apple.com/us/app/ jacs-official-scientific-journal/id491332618?mt=8 and accessed through the new iPad Newstand interface. The app allows users to access JACS content wherever and whenever it is needed.
The app automatically downloads new issues and allows users to interact with the Journal by tapping links to content. Users may bookmark their favorite articles, take notes and highlight items within articles, save the material to their favorite electronic reading device, and quickly access articles and issues.
International Guest Scholarships available for 2014
The American College of Surgeons (ACS) is offering International Guest Scholarships in 2014 to outstanding young surgeons from countries other than the U.S. or Canada who have demonstrated strong interests in teaching and research. The $10,000 scholarships will provide the International Guest Scholars with an opportunity to visit clinical, teaching, and research institutions in North America and to attend and participate fully in the educational opportunities and activities of the ACS Clinical Congress in San Francisco, CA, October 26-30, in 2014.
A legacy left to the College by Paul R. Hawley, MD, FACS (Hon), former Director of the College, originally funded the scholarship endowment. More recently, gifts from Fellows and their families and associates have expanded the roster of International Guest Scholarships. The ACS Foundation website features additional information about these benefactors and the awards they support.
The scholarship requirements are as follows:
• Applicants must be medical school graduates.
• Applicants must be at least 35 years of age, but younger than 45, on the filing date of the completed application.
• Applicants must submit their applications from their intended permanent location. The College will accept applications for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must have demonstrated a commitment to teaching and/or research in accordance with the standards of their respective home country.
• Applicants whose careers are in the developing stage are deemed more suitable for receipt of this scholarship than those who are serving in senior academic appointments.
• Applicants must submit a fully completed application form provided by the College on its website. The application and accompanying materials must be submitted in English. Submission of a curriculum vitae without a completed application is not acceptable.
• Applicants must provide a list of all of their publication credits and must submit three complete publications (reprints or manuscripts) of their choosing from that list.
• Applicants must submit letters of recommendation from three colleagues. One letter must be from the chair of the department in which the applicant holds academic appointment or a Fellow of the ACS residing in the applicant’s country. The letter from the chair or Fellow must include a specific statement detailing the nature and extent of the teaching and other academic involvement of the applicant.
• The International Guest Scholarships must be used in their designated year. Recipients cannot postpone the scholarship.
• Applicants who receive scholarships are expected to provide a full written report of the experiences provided through the scholarships upon completion of their tours.
• An unsuccessful applicant may reapply only twice, and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
International Guest Scholarships provide successful applicants with the privilege of participating in the College’s annual Clinical Congress in October, with public recognition of their presence. They will receive gratis admission to selected postgraduate courses, plus admission to all lectures, demonstrations, and exhibits, which are integral to the Clinical Congress. Assistance will be provided in arranging visits (following the Clinical Congress) to various clinics and universities of the scholars’ choosing.
To qualify for consideration by the selection committee, applicants must fulfill all of the requirements. The application form for the ACS International Guest Scholarship is available online on the College’s website at http://www.facs.org/memberservices/igs.html. Questions should be directed to:Kate Early, International Liaison, American College of Surgeons, 633 N. Saint Clair St., Chicago, IL 60611-3211 USA; [email protected].
The ACS must receive all completed applications, including all the supporting documentation for the 2013 International Guest Scholarships, no later than July 1, 2013. All applicants will be notified of the selection committee’s decision in November 2013. The College urges applicants to submit their completed application package as early as possible in order to provide sufficient time for processing.
The American College of Surgeons (ACS) is offering International Guest Scholarships in 2014 to outstanding young surgeons from countries other than the U.S. or Canada who have demonstrated strong interests in teaching and research. The $10,000 scholarships will provide the International Guest Scholars with an opportunity to visit clinical, teaching, and research institutions in North America and to attend and participate fully in the educational opportunities and activities of the ACS Clinical Congress in San Francisco, CA, October 26-30, in 2014.
A legacy left to the College by Paul R. Hawley, MD, FACS (Hon), former Director of the College, originally funded the scholarship endowment. More recently, gifts from Fellows and their families and associates have expanded the roster of International Guest Scholarships. The ACS Foundation website features additional information about these benefactors and the awards they support.
The scholarship requirements are as follows:
• Applicants must be medical school graduates.
• Applicants must be at least 35 years of age, but younger than 45, on the filing date of the completed application.
• Applicants must submit their applications from their intended permanent location. The College will accept applications for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must have demonstrated a commitment to teaching and/or research in accordance with the standards of their respective home country.
• Applicants whose careers are in the developing stage are deemed more suitable for receipt of this scholarship than those who are serving in senior academic appointments.
• Applicants must submit a fully completed application form provided by the College on its website. The application and accompanying materials must be submitted in English. Submission of a curriculum vitae without a completed application is not acceptable.
• Applicants must provide a list of all of their publication credits and must submit three complete publications (reprints or manuscripts) of their choosing from that list.
• Applicants must submit letters of recommendation from three colleagues. One letter must be from the chair of the department in which the applicant holds academic appointment or a Fellow of the ACS residing in the applicant’s country. The letter from the chair or Fellow must include a specific statement detailing the nature and extent of the teaching and other academic involvement of the applicant.
• The International Guest Scholarships must be used in their designated year. Recipients cannot postpone the scholarship.
• Applicants who receive scholarships are expected to provide a full written report of the experiences provided through the scholarships upon completion of their tours.
• An unsuccessful applicant may reapply only twice, and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
International Guest Scholarships provide successful applicants with the privilege of participating in the College’s annual Clinical Congress in October, with public recognition of their presence. They will receive gratis admission to selected postgraduate courses, plus admission to all lectures, demonstrations, and exhibits, which are integral to the Clinical Congress. Assistance will be provided in arranging visits (following the Clinical Congress) to various clinics and universities of the scholars’ choosing.
To qualify for consideration by the selection committee, applicants must fulfill all of the requirements. The application form for the ACS International Guest Scholarship is available online on the College’s website at http://www.facs.org/memberservices/igs.html. Questions should be directed to:Kate Early, International Liaison, American College of Surgeons, 633 N. Saint Clair St., Chicago, IL 60611-3211 USA; [email protected].
The ACS must receive all completed applications, including all the supporting documentation for the 2013 International Guest Scholarships, no later than July 1, 2013. All applicants will be notified of the selection committee’s decision in November 2013. The College urges applicants to submit their completed application package as early as possible in order to provide sufficient time for processing.
The American College of Surgeons (ACS) is offering International Guest Scholarships in 2014 to outstanding young surgeons from countries other than the U.S. or Canada who have demonstrated strong interests in teaching and research. The $10,000 scholarships will provide the International Guest Scholars with an opportunity to visit clinical, teaching, and research institutions in North America and to attend and participate fully in the educational opportunities and activities of the ACS Clinical Congress in San Francisco, CA, October 26-30, in 2014.
A legacy left to the College by Paul R. Hawley, MD, FACS (Hon), former Director of the College, originally funded the scholarship endowment. More recently, gifts from Fellows and their families and associates have expanded the roster of International Guest Scholarships. The ACS Foundation website features additional information about these benefactors and the awards they support.
The scholarship requirements are as follows:
• Applicants must be medical school graduates.
• Applicants must be at least 35 years of age, but younger than 45, on the filing date of the completed application.
• Applicants must submit their applications from their intended permanent location. The College will accept applications for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must have demonstrated a commitment to teaching and/or research in accordance with the standards of their respective home country.
• Applicants whose careers are in the developing stage are deemed more suitable for receipt of this scholarship than those who are serving in senior academic appointments.
• Applicants must submit a fully completed application form provided by the College on its website. The application and accompanying materials must be submitted in English. Submission of a curriculum vitae without a completed application is not acceptable.
• Applicants must provide a list of all of their publication credits and must submit three complete publications (reprints or manuscripts) of their choosing from that list.
• Applicants must submit letters of recommendation from three colleagues. One letter must be from the chair of the department in which the applicant holds academic appointment or a Fellow of the ACS residing in the applicant’s country. The letter from the chair or Fellow must include a specific statement detailing the nature and extent of the teaching and other academic involvement of the applicant.
• The International Guest Scholarships must be used in their designated year. Recipients cannot postpone the scholarship.
• Applicants who receive scholarships are expected to provide a full written report of the experiences provided through the scholarships upon completion of their tours.
• An unsuccessful applicant may reapply only twice, and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
International Guest Scholarships provide successful applicants with the privilege of participating in the College’s annual Clinical Congress in October, with public recognition of their presence. They will receive gratis admission to selected postgraduate courses, plus admission to all lectures, demonstrations, and exhibits, which are integral to the Clinical Congress. Assistance will be provided in arranging visits (following the Clinical Congress) to various clinics and universities of the scholars’ choosing.
To qualify for consideration by the selection committee, applicants must fulfill all of the requirements. The application form for the ACS International Guest Scholarship is available online on the College’s website at http://www.facs.org/memberservices/igs.html. Questions should be directed to:Kate Early, International Liaison, American College of Surgeons, 633 N. Saint Clair St., Chicago, IL 60611-3211 USA; [email protected].
The ACS must receive all completed applications, including all the supporting documentation for the 2013 International Guest Scholarships, no later than July 1, 2013. All applicants will be notified of the selection committee’s decision in November 2013. The College urges applicants to submit their completed application package as early as possible in order to provide sufficient time for processing.
Community Surgeons Travel Awards for 2014 now available
The International Relations Committee of the American College of Surgeons (ACS) announces two Community Surgeons Travel Awards for surgeons ages 30 to 50. These $4,000 awards allow international surgeons to participate in the annual ACS Clinical Congress. Surgeons who work in community or regional hospitals or clinics in countries other than the U.S. and Canada or who are from struggling academic departments of surgery in low- or middle-income countries are eligible for the awards. Candidates from Southeast Asia will receive preference in this cycle. The office of the International Liaison must receive all applications and supporting documents for these awards before July 1, 2013.
Each awardee will receive gratis registration to the Clinical Congress and to one available Clinical Congress postgraduate course. The College will help awardees find affordable hotel in the Clinical Congress host city. The 2014 Clinical Congress will take place in San Francisco, CA, October 26-30.The scholarship requirements are:
• Applicants must be graduates of medical schools.
• Age requirement refers to the date of the filing of the completed application.
• Applicants must submit their applications from their intended permanent location. Applications will be accepted for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must show evidence of commitment to high-quality surgery, surgical teaching, and improving access to surgical care in their community.
• Applicants must submit an online fully completed application form provided by the College. The application and accompanying materials must be typewritten and in English. Submission of a curriculum vitae only is insufficient
Preference will be given to applicants who have not already experienced training or surgical fellowships in North America.
Applicants must submit independently prepared letters of recommendation from three (3) of their colleagues. One letter must be from the chair of the department in which they hold a clinical or academic appointment or an ACS Fellow residing in their country. The letter from the chair or Fellow should directly address the applicant’s commitment to high-quality surgery, surgical teaching, improved access to surgical care locally. Letters of recommendation should be submitted by the persons making the recommendations.
The Community Surgeons Travel Awards must be used in the year for which they are designated. They cannot be postponed.
Awardees must provide a written report upon their return home, specifically focusing on the value of the visit to the awardee and the potential beneficial effect to patients in the country of origin.
Unsuccessful applicants may reapply only twice and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
To be considered by the selection committee, applicants must fulfill all requirements.
Find the application for the Community Surgeons Travel Award on the ACS website at http://www.facs.org/memberservices/community-travel.html.
Direct supporting materials and questions to:
Administrator
International Liaison Section
American College of Surgeons
633 N. Saint Clair St.
Chicago, IL 60611-3211
USA
[email protected] or 312-202-5021 (facsimile)
All applicants will be notified of the selection committee’s decision in November 2013. Please submit completed applications and supporting documents early to allow time for processing.
The International Relations Committee of the American College of Surgeons (ACS) announces two Community Surgeons Travel Awards for surgeons ages 30 to 50. These $4,000 awards allow international surgeons to participate in the annual ACS Clinical Congress. Surgeons who work in community or regional hospitals or clinics in countries other than the U.S. and Canada or who are from struggling academic departments of surgery in low- or middle-income countries are eligible for the awards. Candidates from Southeast Asia will receive preference in this cycle. The office of the International Liaison must receive all applications and supporting documents for these awards before July 1, 2013.
Each awardee will receive gratis registration to the Clinical Congress and to one available Clinical Congress postgraduate course. The College will help awardees find affordable hotel in the Clinical Congress host city. The 2014 Clinical Congress will take place in San Francisco, CA, October 26-30.The scholarship requirements are:
• Applicants must be graduates of medical schools.
• Age requirement refers to the date of the filing of the completed application.
• Applicants must submit their applications from their intended permanent location. Applications will be accepted for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must show evidence of commitment to high-quality surgery, surgical teaching, and improving access to surgical care in their community.
• Applicants must submit an online fully completed application form provided by the College. The application and accompanying materials must be typewritten and in English. Submission of a curriculum vitae only is insufficient
Preference will be given to applicants who have not already experienced training or surgical fellowships in North America.
Applicants must submit independently prepared letters of recommendation from three (3) of their colleagues. One letter must be from the chair of the department in which they hold a clinical or academic appointment or an ACS Fellow residing in their country. The letter from the chair or Fellow should directly address the applicant’s commitment to high-quality surgery, surgical teaching, improved access to surgical care locally. Letters of recommendation should be submitted by the persons making the recommendations.
The Community Surgeons Travel Awards must be used in the year for which they are designated. They cannot be postponed.
Awardees must provide a written report upon their return home, specifically focusing on the value of the visit to the awardee and the potential beneficial effect to patients in the country of origin.
Unsuccessful applicants may reapply only twice and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
To be considered by the selection committee, applicants must fulfill all requirements.
Find the application for the Community Surgeons Travel Award on the ACS website at http://www.facs.org/memberservices/community-travel.html.
Direct supporting materials and questions to:
Administrator
International Liaison Section
American College of Surgeons
633 N. Saint Clair St.
Chicago, IL 60611-3211
USA
[email protected] or 312-202-5021 (facsimile)
All applicants will be notified of the selection committee’s decision in November 2013. Please submit completed applications and supporting documents early to allow time for processing.
The International Relations Committee of the American College of Surgeons (ACS) announces two Community Surgeons Travel Awards for surgeons ages 30 to 50. These $4,000 awards allow international surgeons to participate in the annual ACS Clinical Congress. Surgeons who work in community or regional hospitals or clinics in countries other than the U.S. and Canada or who are from struggling academic departments of surgery in low- or middle-income countries are eligible for the awards. Candidates from Southeast Asia will receive preference in this cycle. The office of the International Liaison must receive all applications and supporting documents for these awards before July 1, 2013.
Each awardee will receive gratis registration to the Clinical Congress and to one available Clinical Congress postgraduate course. The College will help awardees find affordable hotel in the Clinical Congress host city. The 2014 Clinical Congress will take place in San Francisco, CA, October 26-30.The scholarship requirements are:
• Applicants must be graduates of medical schools.
• Age requirement refers to the date of the filing of the completed application.
• Applicants must submit their applications from their intended permanent location. Applications will be accepted for processing only when the applicants have been in surgical practice, teaching, or research for a minimum of one year at their intended permanent location, following completion of all formal training (including fellowships and scholarships).
• Applicants must show evidence of commitment to high-quality surgery, surgical teaching, and improving access to surgical care in their community.
• Applicants must submit an online fully completed application form provided by the College. The application and accompanying materials must be typewritten and in English. Submission of a curriculum vitae only is insufficient
Preference will be given to applicants who have not already experienced training or surgical fellowships in North America.
Applicants must submit independently prepared letters of recommendation from three (3) of their colleagues. One letter must be from the chair of the department in which they hold a clinical or academic appointment or an ACS Fellow residing in their country. The letter from the chair or Fellow should directly address the applicant’s commitment to high-quality surgery, surgical teaching, improved access to surgical care locally. Letters of recommendation should be submitted by the persons making the recommendations.
The Community Surgeons Travel Awards must be used in the year for which they are designated. They cannot be postponed.
Awardees must provide a written report upon their return home, specifically focusing on the value of the visit to the awardee and the potential beneficial effect to patients in the country of origin.
Unsuccessful applicants may reapply only twice and only by completing and submitting a current application form provided by the College, together with new supporting documentation.
To be considered by the selection committee, applicants must fulfill all requirements.
Find the application for the Community Surgeons Travel Award on the ACS website at http://www.facs.org/memberservices/community-travel.html.
Direct supporting materials and questions to:
Administrator
International Liaison Section
American College of Surgeons
633 N. Saint Clair St.
Chicago, IL 60611-3211
USA
[email protected] or 312-202-5021 (facsimile)
All applicants will be notified of the selection committee’s decision in November 2013. Please submit completed applications and supporting documents early to allow time for processing.
Osteoarthritis patients survive longer after hip resurfacing than replacement
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
AT RHEUMATOLOGY 2013
Major finding: The number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented total hip replacement, and it was 88 when compared to uncemented total hip replacement.
Data source: Retrospective, population-based, observational cohort study of 91,633 osteoarthritis patients who had metal-on-metal resurfacing or total hip replacement between April 1999 and March 2012.
Disclosures: Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
Prearthroplasty exercise benefits short lived
PHILADELPHIA – Preoperative neuromuscular exercise does not significantly improve function or pain 3 months after total hip or knee replacement, according to a randomized, controlled trial in 165 patients.
The study’s primary endpoint of self-reported activities of daily living (ADLs) at 3 months was similar in patients who exercised prior to surgery and those who did not (mean between-group difference 4.4 points; P = .096). The change from baseline in the group who exercised prior to surgery was 29 points vs. 25 points in the surgery-only group, on a 100-point, worst-to-best scale.
Joint-related quality of life (mean 4.5 points; P = .22) and pain (mean 3.6 points; P = .09) were also not significantly different between the two groups, Dr. Allan Villadsen said at the World Congress on Osteoarthritis Research Society.
The 8 weeks of twice-weekly exercise, however, was not for naught.
Patients improved immediately following exercise and this improvement carried over to 6 weeks after surgery, "indicating an earlier onset of recovery," he said. "Therefore, we believe exercise constitutes a viable treatment option for the individual patient who’s willing to engage in exercise prior to total hip or knee replacement and possibly obtain an earlier onset of recovery."
While preoperative exercise has been shown to improve function in other settings, little is known about its role in knee- and hip-replacement surgery for patients with severe osteoarthritis (OA). A meta-analysis of 23 randomized controlled trials involving 1,461 patients reported a small improvement in physical function and pain 3 weeks after total hip arthroscopy, but no effects in total knee replacement 3 months after surgery (Osteoarthritis Cartilage 2011;19:1381-95).A subsequent systematic review and meta-analysis, however, suggests that the therapeutic validity of the exercise programs used in the studies may have hampered the beneficial effects (PLos One 2012;7:e38031). In addition, the sample sizes were small, and the calculated effect sizes for pain and physical function were based on only two to four studies, observed Dr. Villadsen of the Institute of Sport Science and Clinical Biomechanics, University of Southern Denmark, Odense.
The current trial randomly assigned 165 patients with severe symptomatic hip or knee OA scheduled for unilateral primary total joint replacement to receive a brochure recommending exercise prior to surgery and a 3-hour information session with health professionals or the same intervention plus individualized group-based neuromuscular exercise guided by a physiotherapist. The sessions were designed to improve sensorimotor control and range of motion, and included warm up on a stationary bike, a circuit program, and a walking cool-down period, Dr. Villadsen said at the meeting, sponsored by Osteoarthritis Research Society International (OARSI).
Hip OA was present in 43 of the 84 patients in the exercise arm and 41 of the 81 controls. Their mean age was 67 years and mean ADL score on the 100-point Hip Disability and Osteoarthritis Outcome Score (HOOS) or Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaires was 50.6 and 45.6, respectively.
At 6 weeks, the between-group difference in activities of daily living on both the HOOS and KOOS questionnaires was 5.2, favoring the exercise group (P = .05), Dr. Villadsen said.
During a discussion of the results, an audience member asked whether the patients had tried exercise prior to joint replacement, which is the current recommendation. Dr. Villadsen said they did not track this, but that anecdotally, "Many of these patients are not offered what is recommended in the international guidelines, which is very disturbing ... if you asked them, many of them never even exercised before."
Session moderator and orthopedic surgeon Dr. Victor Goldberg, with Case Western Reserve University in Cleveland said it’s difficult to tease out the effects of surgery in analyses like these, but agreed that many patients are being sent to surgery without having been counseled to exercise. Part of the problem is that patients with mild to moderate OA are typically cared for by primary care physicians, who aren’t as well versed as rheumatologists and orthopedic surgeons are on the impairment, he said in an interview.
"That’s one of the charges of OARSI and our guidelines, is to really put it out in the community," he added.
"These kinds of studies, which point to the need for intervention in arthroplasty, particularly with well-done neuromuscular exercise programs, are very important to the overall management of these patients," Dr. Goldberg said. It’s needed because 15%-23% of patients after surgery say " ‘I’m not much better; I still hurt.’ "
Self-reported data at 1 year are currently being processed and will be included in a manuscript on the cost-effectiveness of the intervention, Dr. Villadsen said in an interview.
Dr. Villadsen reported having no financial disclosures.
PHILADELPHIA – Preoperative neuromuscular exercise does not significantly improve function or pain 3 months after total hip or knee replacement, according to a randomized, controlled trial in 165 patients.
The study’s primary endpoint of self-reported activities of daily living (ADLs) at 3 months was similar in patients who exercised prior to surgery and those who did not (mean between-group difference 4.4 points; P = .096). The change from baseline in the group who exercised prior to surgery was 29 points vs. 25 points in the surgery-only group, on a 100-point, worst-to-best scale.
Joint-related quality of life (mean 4.5 points; P = .22) and pain (mean 3.6 points; P = .09) were also not significantly different between the two groups, Dr. Allan Villadsen said at the World Congress on Osteoarthritis Research Society.
The 8 weeks of twice-weekly exercise, however, was not for naught.
Patients improved immediately following exercise and this improvement carried over to 6 weeks after surgery, "indicating an earlier onset of recovery," he said. "Therefore, we believe exercise constitutes a viable treatment option for the individual patient who’s willing to engage in exercise prior to total hip or knee replacement and possibly obtain an earlier onset of recovery."
While preoperative exercise has been shown to improve function in other settings, little is known about its role in knee- and hip-replacement surgery for patients with severe osteoarthritis (OA). A meta-analysis of 23 randomized controlled trials involving 1,461 patients reported a small improvement in physical function and pain 3 weeks after total hip arthroscopy, but no effects in total knee replacement 3 months after surgery (Osteoarthritis Cartilage 2011;19:1381-95).A subsequent systematic review and meta-analysis, however, suggests that the therapeutic validity of the exercise programs used in the studies may have hampered the beneficial effects (PLos One 2012;7:e38031). In addition, the sample sizes were small, and the calculated effect sizes for pain and physical function were based on only two to four studies, observed Dr. Villadsen of the Institute of Sport Science and Clinical Biomechanics, University of Southern Denmark, Odense.
The current trial randomly assigned 165 patients with severe symptomatic hip or knee OA scheduled for unilateral primary total joint replacement to receive a brochure recommending exercise prior to surgery and a 3-hour information session with health professionals or the same intervention plus individualized group-based neuromuscular exercise guided by a physiotherapist. The sessions were designed to improve sensorimotor control and range of motion, and included warm up on a stationary bike, a circuit program, and a walking cool-down period, Dr. Villadsen said at the meeting, sponsored by Osteoarthritis Research Society International (OARSI).
Hip OA was present in 43 of the 84 patients in the exercise arm and 41 of the 81 controls. Their mean age was 67 years and mean ADL score on the 100-point Hip Disability and Osteoarthritis Outcome Score (HOOS) or Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaires was 50.6 and 45.6, respectively.
At 6 weeks, the between-group difference in activities of daily living on both the HOOS and KOOS questionnaires was 5.2, favoring the exercise group (P = .05), Dr. Villadsen said.
During a discussion of the results, an audience member asked whether the patients had tried exercise prior to joint replacement, which is the current recommendation. Dr. Villadsen said they did not track this, but that anecdotally, "Many of these patients are not offered what is recommended in the international guidelines, which is very disturbing ... if you asked them, many of them never even exercised before."
Session moderator and orthopedic surgeon Dr. Victor Goldberg, with Case Western Reserve University in Cleveland said it’s difficult to tease out the effects of surgery in analyses like these, but agreed that many patients are being sent to surgery without having been counseled to exercise. Part of the problem is that patients with mild to moderate OA are typically cared for by primary care physicians, who aren’t as well versed as rheumatologists and orthopedic surgeons are on the impairment, he said in an interview.
"That’s one of the charges of OARSI and our guidelines, is to really put it out in the community," he added.
"These kinds of studies, which point to the need for intervention in arthroplasty, particularly with well-done neuromuscular exercise programs, are very important to the overall management of these patients," Dr. Goldberg said. It’s needed because 15%-23% of patients after surgery say " ‘I’m not much better; I still hurt.’ "
Self-reported data at 1 year are currently being processed and will be included in a manuscript on the cost-effectiveness of the intervention, Dr. Villadsen said in an interview.
Dr. Villadsen reported having no financial disclosures.
PHILADELPHIA – Preoperative neuromuscular exercise does not significantly improve function or pain 3 months after total hip or knee replacement, according to a randomized, controlled trial in 165 patients.
The study’s primary endpoint of self-reported activities of daily living (ADLs) at 3 months was similar in patients who exercised prior to surgery and those who did not (mean between-group difference 4.4 points; P = .096). The change from baseline in the group who exercised prior to surgery was 29 points vs. 25 points in the surgery-only group, on a 100-point, worst-to-best scale.
Joint-related quality of life (mean 4.5 points; P = .22) and pain (mean 3.6 points; P = .09) were also not significantly different between the two groups, Dr. Allan Villadsen said at the World Congress on Osteoarthritis Research Society.
The 8 weeks of twice-weekly exercise, however, was not for naught.
Patients improved immediately following exercise and this improvement carried over to 6 weeks after surgery, "indicating an earlier onset of recovery," he said. "Therefore, we believe exercise constitutes a viable treatment option for the individual patient who’s willing to engage in exercise prior to total hip or knee replacement and possibly obtain an earlier onset of recovery."
While preoperative exercise has been shown to improve function in other settings, little is known about its role in knee- and hip-replacement surgery for patients with severe osteoarthritis (OA). A meta-analysis of 23 randomized controlled trials involving 1,461 patients reported a small improvement in physical function and pain 3 weeks after total hip arthroscopy, but no effects in total knee replacement 3 months after surgery (Osteoarthritis Cartilage 2011;19:1381-95).A subsequent systematic review and meta-analysis, however, suggests that the therapeutic validity of the exercise programs used in the studies may have hampered the beneficial effects (PLos One 2012;7:e38031). In addition, the sample sizes were small, and the calculated effect sizes for pain and physical function were based on only two to four studies, observed Dr. Villadsen of the Institute of Sport Science and Clinical Biomechanics, University of Southern Denmark, Odense.
The current trial randomly assigned 165 patients with severe symptomatic hip or knee OA scheduled for unilateral primary total joint replacement to receive a brochure recommending exercise prior to surgery and a 3-hour information session with health professionals or the same intervention plus individualized group-based neuromuscular exercise guided by a physiotherapist. The sessions were designed to improve sensorimotor control and range of motion, and included warm up on a stationary bike, a circuit program, and a walking cool-down period, Dr. Villadsen said at the meeting, sponsored by Osteoarthritis Research Society International (OARSI).
Hip OA was present in 43 of the 84 patients in the exercise arm and 41 of the 81 controls. Their mean age was 67 years and mean ADL score on the 100-point Hip Disability and Osteoarthritis Outcome Score (HOOS) or Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaires was 50.6 and 45.6, respectively.
At 6 weeks, the between-group difference in activities of daily living on both the HOOS and KOOS questionnaires was 5.2, favoring the exercise group (P = .05), Dr. Villadsen said.
During a discussion of the results, an audience member asked whether the patients had tried exercise prior to joint replacement, which is the current recommendation. Dr. Villadsen said they did not track this, but that anecdotally, "Many of these patients are not offered what is recommended in the international guidelines, which is very disturbing ... if you asked them, many of them never even exercised before."
Session moderator and orthopedic surgeon Dr. Victor Goldberg, with Case Western Reserve University in Cleveland said it’s difficult to tease out the effects of surgery in analyses like these, but agreed that many patients are being sent to surgery without having been counseled to exercise. Part of the problem is that patients with mild to moderate OA are typically cared for by primary care physicians, who aren’t as well versed as rheumatologists and orthopedic surgeons are on the impairment, he said in an interview.
"That’s one of the charges of OARSI and our guidelines, is to really put it out in the community," he added.
"These kinds of studies, which point to the need for intervention in arthroplasty, particularly with well-done neuromuscular exercise programs, are very important to the overall management of these patients," Dr. Goldberg said. It’s needed because 15%-23% of patients after surgery say " ‘I’m not much better; I still hurt.’ "
Self-reported data at 1 year are currently being processed and will be included in a manuscript on the cost-effectiveness of the intervention, Dr. Villadsen said in an interview.
Dr. Villadsen reported having no financial disclosures.
AT OARSI
Major finding: Self-reported activities of daily living at 3 months was similar in patients who exercised prior to surgery and those who did not (mean between-group difference 4.4 points; P = .096).
Data source: Randomized, assessor-blinded trial in 165 patients undergoing total hip or knee replacement.
Disclosures: Dr. Villadsen reported having no financial disclosures.
Diabetes 'cure' holds up 6 years after bariatric surgery
INDIANAPOLIS – At 6 years of follow-up data, bariatric surgical cures of type 2 diabetes are holding steady in a single-center series of 217 patients.
"We see sustained weight loss, particularly in Roux-en-Y gastric bypass patients, 5-9 years after surgery." Diabetes remitted in 50% of patients, according to Dr. Stacy A. Brethauer of the Cleveland Clinic. "Bariatric surgery also achieved excellent long-term control of other cardiovascular risk factors; and diabetic nephropathy improved or stabilized."
Of 217 obese type 2 diabetic patients followed for a median of 6 years after bariatric surgery, 24% have been "cured." They have maintained a hemoglobin A1c level below 6% and fasting blood glucose values below 100 mg/dL for more than 5 years while off all antidiabetic medications, Dr. Brethauer reported at the annual meeting of the American Surgical Association.
Another 26% of patients have had partial remissions, meaning they maintained target HbA1c and fasting blood glucose levels off antidiabetic medications for more than 1 year but less than 5 years. In addition, 34% of patients were classified as "improved" based upon an absolute 1% or more reduction in HbA1c, a drop in fasting blood glucose in excess of 25 mg/dL, and a halving in the dose of antidiabetic medication for at least 1 year.
Diabetes recurred in 19% of subjects. Recurrence was defined as a return to an HbA1c of 6.5% or more or a fasting blood glucose level of at least 126 mg/dL.
The overall study population improved from a mean body mass index of 49 kg/m2 before surgery to 37 kg/m2 at 6 years after surgery. The mean HbA1c was 7.5% at baseline and 6.5% at 6 years. Fasting blood glucose at 6 years was a mean of 41.6 mg/dL lower than it was before surgery. LDL cholesterol levels were down by a mean of 10.1 mg/dL and HDL levels were up by 9.8 mg/dL. Systolic blood pressure was reduced by a mean of 10.9 mm Hg, with diastolic blood pressure was down by 3.2 mm Hg at 6 years after surgery.
Preoperatively, all but 5% of patients were on any antidiabetes medications; at 6 years after bariatric surgery, 54% were not on any antidiabetes drugs.
At baseline, 3% of subjects met all three key metabolic goals for diabetic patients as defined by the American Diabetes Association: an HbA1c below 7%, blood pressure below 130/80 mm Hg, and an LDL level below 100 mg/dL. At 6 years after surgery, 28% of patients met these goals. That result is particularly impressive in light of other studies that indicate 13% of the U.S. diabetic population as a whole meet all three goals.
The bariatric surgery group had a mean Framingham 10-year cardiovascular risk score of 28% preoperatively and of 22% at long-term followup.
The incidence of diabetic nephropathy among patients with type 2 diabetes is typically 2%-4% per year. Yet of 40 gastric bypass recipients known to have a normal urinary albumin-to-creatinine ratio preoperatively, only 1 developed macroalbuminuria and 1 microalbuminuria during a mean of 6 years postsurgical follow-up.
Also impressive, albuminuria regressed in 10 of the 19 gastric bypass recipients known to have the disorder at baseline. Albuminuria remained stable in the other 9 patients over the course of 6 years.
Mean excess weight loss at 1-2 years of follow-up was 61% in the 162 patients who underwent gastric bypass, 50% in the 23 with sleeve gastrectomy, and 30% in patients who had a gastric banding procedure.
In a multivariate analysis adjusted for baseline clinical characteristics, the significant predictors of diabetes remission following bariatric surgery were greater excess weight loss, preoperative diabetes duration of less than 5 years, and having a gastric bypass operation rather than sleeve gastrectomy or a gastric banding procedure.
Dr. Brethauer said this study, taken together with the findings of an earlier randomized clinical trial by the same investigators (N. Engl. J. Med. 2012;366:1567-76), conveys a clear message : "Bariatric surgery can induce a significant and sustainable remission of type 2 diabetes and other metabolic risk factors in obese patients and should be considered early in the course of the disease."
Discussant Dr. Walter J. Pories called Dr. Brethauer’s study "a really important contribution." He added that it’s high time for nonsurgeons to get on board.
"One in four adults over age 65 in this country has diabetes. One would have thought our medical colleagues would be ecstatic at the news that an operation on the gut – a safe procedure that can be done in about an hour – could produce full and durable remission of diabetes with complete prevention of amputations, blindness, and kidney failure. But that hasn’t been the case. All we’ve heard are cries for more and more evidence," said Dr. Pories, professor of surgery at East Carolina University, Greenville, N.C.
He added that in his view, Dr. Brethauer and his colleagues set the bar too high in requiring a sustained HbA1c below 6% as the definition of disease cure when the American Diabetes Association uses a figure of 7%. He noted that if the investigators had accepted the ADA metric, their combined cure/partial remission rate would have been considerably greater than the 50% figure they reported.
Dr. Brethauer replied that he and his coinvestigators chose a cutoff of 6% in order to make a point.
"When we raise this issue of ‘cure,’ which is still quite controversial and somewhat provocative, particularly with our endocrinology colleagues, I think we have to find the strictest and most conservative criteria that we can," he explained. "We continue to provide data in support of the concept that this is a surgically treated disease. It’s a major paradigm shift for our endocrinology colleagues to accept. I think it’s going to take a generation of endocrinologists before it’s embraced."
He reported that he serves as a consultant to Ethicon Endosurgery and Apollo Endosurgery.
INDIANAPOLIS – At 6 years of follow-up data, bariatric surgical cures of type 2 diabetes are holding steady in a single-center series of 217 patients.
"We see sustained weight loss, particularly in Roux-en-Y gastric bypass patients, 5-9 years after surgery." Diabetes remitted in 50% of patients, according to Dr. Stacy A. Brethauer of the Cleveland Clinic. "Bariatric surgery also achieved excellent long-term control of other cardiovascular risk factors; and diabetic nephropathy improved or stabilized."
Of 217 obese type 2 diabetic patients followed for a median of 6 years after bariatric surgery, 24% have been "cured." They have maintained a hemoglobin A1c level below 6% and fasting blood glucose values below 100 mg/dL for more than 5 years while off all antidiabetic medications, Dr. Brethauer reported at the annual meeting of the American Surgical Association.
Another 26% of patients have had partial remissions, meaning they maintained target HbA1c and fasting blood glucose levels off antidiabetic medications for more than 1 year but less than 5 years. In addition, 34% of patients were classified as "improved" based upon an absolute 1% or more reduction in HbA1c, a drop in fasting blood glucose in excess of 25 mg/dL, and a halving in the dose of antidiabetic medication for at least 1 year.
Diabetes recurred in 19% of subjects. Recurrence was defined as a return to an HbA1c of 6.5% or more or a fasting blood glucose level of at least 126 mg/dL.
The overall study population improved from a mean body mass index of 49 kg/m2 before surgery to 37 kg/m2 at 6 years after surgery. The mean HbA1c was 7.5% at baseline and 6.5% at 6 years. Fasting blood glucose at 6 years was a mean of 41.6 mg/dL lower than it was before surgery. LDL cholesterol levels were down by a mean of 10.1 mg/dL and HDL levels were up by 9.8 mg/dL. Systolic blood pressure was reduced by a mean of 10.9 mm Hg, with diastolic blood pressure was down by 3.2 mm Hg at 6 years after surgery.
Preoperatively, all but 5% of patients were on any antidiabetes medications; at 6 years after bariatric surgery, 54% were not on any antidiabetes drugs.
At baseline, 3% of subjects met all three key metabolic goals for diabetic patients as defined by the American Diabetes Association: an HbA1c below 7%, blood pressure below 130/80 mm Hg, and an LDL level below 100 mg/dL. At 6 years after surgery, 28% of patients met these goals. That result is particularly impressive in light of other studies that indicate 13% of the U.S. diabetic population as a whole meet all three goals.
The bariatric surgery group had a mean Framingham 10-year cardiovascular risk score of 28% preoperatively and of 22% at long-term followup.
The incidence of diabetic nephropathy among patients with type 2 diabetes is typically 2%-4% per year. Yet of 40 gastric bypass recipients known to have a normal urinary albumin-to-creatinine ratio preoperatively, only 1 developed macroalbuminuria and 1 microalbuminuria during a mean of 6 years postsurgical follow-up.
Also impressive, albuminuria regressed in 10 of the 19 gastric bypass recipients known to have the disorder at baseline. Albuminuria remained stable in the other 9 patients over the course of 6 years.
Mean excess weight loss at 1-2 years of follow-up was 61% in the 162 patients who underwent gastric bypass, 50% in the 23 with sleeve gastrectomy, and 30% in patients who had a gastric banding procedure.
In a multivariate analysis adjusted for baseline clinical characteristics, the significant predictors of diabetes remission following bariatric surgery were greater excess weight loss, preoperative diabetes duration of less than 5 years, and having a gastric bypass operation rather than sleeve gastrectomy or a gastric banding procedure.
Dr. Brethauer said this study, taken together with the findings of an earlier randomized clinical trial by the same investigators (N. Engl. J. Med. 2012;366:1567-76), conveys a clear message : "Bariatric surgery can induce a significant and sustainable remission of type 2 diabetes and other metabolic risk factors in obese patients and should be considered early in the course of the disease."
Discussant Dr. Walter J. Pories called Dr. Brethauer’s study "a really important contribution." He added that it’s high time for nonsurgeons to get on board.
"One in four adults over age 65 in this country has diabetes. One would have thought our medical colleagues would be ecstatic at the news that an operation on the gut – a safe procedure that can be done in about an hour – could produce full and durable remission of diabetes with complete prevention of amputations, blindness, and kidney failure. But that hasn’t been the case. All we’ve heard are cries for more and more evidence," said Dr. Pories, professor of surgery at East Carolina University, Greenville, N.C.
He added that in his view, Dr. Brethauer and his colleagues set the bar too high in requiring a sustained HbA1c below 6% as the definition of disease cure when the American Diabetes Association uses a figure of 7%. He noted that if the investigators had accepted the ADA metric, their combined cure/partial remission rate would have been considerably greater than the 50% figure they reported.
Dr. Brethauer replied that he and his coinvestigators chose a cutoff of 6% in order to make a point.
"When we raise this issue of ‘cure,’ which is still quite controversial and somewhat provocative, particularly with our endocrinology colleagues, I think we have to find the strictest and most conservative criteria that we can," he explained. "We continue to provide data in support of the concept that this is a surgically treated disease. It’s a major paradigm shift for our endocrinology colleagues to accept. I think it’s going to take a generation of endocrinologists before it’s embraced."
He reported that he serves as a consultant to Ethicon Endosurgery and Apollo Endosurgery.
INDIANAPOLIS – At 6 years of follow-up data, bariatric surgical cures of type 2 diabetes are holding steady in a single-center series of 217 patients.
"We see sustained weight loss, particularly in Roux-en-Y gastric bypass patients, 5-9 years after surgery." Diabetes remitted in 50% of patients, according to Dr. Stacy A. Brethauer of the Cleveland Clinic. "Bariatric surgery also achieved excellent long-term control of other cardiovascular risk factors; and diabetic nephropathy improved or stabilized."
Of 217 obese type 2 diabetic patients followed for a median of 6 years after bariatric surgery, 24% have been "cured." They have maintained a hemoglobin A1c level below 6% and fasting blood glucose values below 100 mg/dL for more than 5 years while off all antidiabetic medications, Dr. Brethauer reported at the annual meeting of the American Surgical Association.
Another 26% of patients have had partial remissions, meaning they maintained target HbA1c and fasting blood glucose levels off antidiabetic medications for more than 1 year but less than 5 years. In addition, 34% of patients were classified as "improved" based upon an absolute 1% or more reduction in HbA1c, a drop in fasting blood glucose in excess of 25 mg/dL, and a halving in the dose of antidiabetic medication for at least 1 year.
Diabetes recurred in 19% of subjects. Recurrence was defined as a return to an HbA1c of 6.5% or more or a fasting blood glucose level of at least 126 mg/dL.
The overall study population improved from a mean body mass index of 49 kg/m2 before surgery to 37 kg/m2 at 6 years after surgery. The mean HbA1c was 7.5% at baseline and 6.5% at 6 years. Fasting blood glucose at 6 years was a mean of 41.6 mg/dL lower than it was before surgery. LDL cholesterol levels were down by a mean of 10.1 mg/dL and HDL levels were up by 9.8 mg/dL. Systolic blood pressure was reduced by a mean of 10.9 mm Hg, with diastolic blood pressure was down by 3.2 mm Hg at 6 years after surgery.
Preoperatively, all but 5% of patients were on any antidiabetes medications; at 6 years after bariatric surgery, 54% were not on any antidiabetes drugs.
At baseline, 3% of subjects met all three key metabolic goals for diabetic patients as defined by the American Diabetes Association: an HbA1c below 7%, blood pressure below 130/80 mm Hg, and an LDL level below 100 mg/dL. At 6 years after surgery, 28% of patients met these goals. That result is particularly impressive in light of other studies that indicate 13% of the U.S. diabetic population as a whole meet all three goals.
The bariatric surgery group had a mean Framingham 10-year cardiovascular risk score of 28% preoperatively and of 22% at long-term followup.
The incidence of diabetic nephropathy among patients with type 2 diabetes is typically 2%-4% per year. Yet of 40 gastric bypass recipients known to have a normal urinary albumin-to-creatinine ratio preoperatively, only 1 developed macroalbuminuria and 1 microalbuminuria during a mean of 6 years postsurgical follow-up.
Also impressive, albuminuria regressed in 10 of the 19 gastric bypass recipients known to have the disorder at baseline. Albuminuria remained stable in the other 9 patients over the course of 6 years.
Mean excess weight loss at 1-2 years of follow-up was 61% in the 162 patients who underwent gastric bypass, 50% in the 23 with sleeve gastrectomy, and 30% in patients who had a gastric banding procedure.
In a multivariate analysis adjusted for baseline clinical characteristics, the significant predictors of diabetes remission following bariatric surgery were greater excess weight loss, preoperative diabetes duration of less than 5 years, and having a gastric bypass operation rather than sleeve gastrectomy or a gastric banding procedure.
Dr. Brethauer said this study, taken together with the findings of an earlier randomized clinical trial by the same investigators (N. Engl. J. Med. 2012;366:1567-76), conveys a clear message : "Bariatric surgery can induce a significant and sustainable remission of type 2 diabetes and other metabolic risk factors in obese patients and should be considered early in the course of the disease."
Discussant Dr. Walter J. Pories called Dr. Brethauer’s study "a really important contribution." He added that it’s high time for nonsurgeons to get on board.
"One in four adults over age 65 in this country has diabetes. One would have thought our medical colleagues would be ecstatic at the news that an operation on the gut – a safe procedure that can be done in about an hour – could produce full and durable remission of diabetes with complete prevention of amputations, blindness, and kidney failure. But that hasn’t been the case. All we’ve heard are cries for more and more evidence," said Dr. Pories, professor of surgery at East Carolina University, Greenville, N.C.
He added that in his view, Dr. Brethauer and his colleagues set the bar too high in requiring a sustained HbA1c below 6% as the definition of disease cure when the American Diabetes Association uses a figure of 7%. He noted that if the investigators had accepted the ADA metric, their combined cure/partial remission rate would have been considerably greater than the 50% figure they reported.
Dr. Brethauer replied that he and his coinvestigators chose a cutoff of 6% in order to make a point.
"When we raise this issue of ‘cure,’ which is still quite controversial and somewhat provocative, particularly with our endocrinology colleagues, I think we have to find the strictest and most conservative criteria that we can," he explained. "We continue to provide data in support of the concept that this is a surgically treated disease. It’s a major paradigm shift for our endocrinology colleagues to accept. I think it’s going to take a generation of endocrinologists before it’s embraced."
He reported that he serves as a consultant to Ethicon Endosurgery and Apollo Endosurgery.
AT THE ASA ANNUAL MEETING
Major finding: At a median of 6 years after bariatric surgery, 24% of patients have maintained an HbA1c below 6% and fasting blood glucose values below 100 mg/dL for more than 5 years while off all antidiabetic medications.
Data source: This is an ongoing retrospective single-center study in which 217 obese patients with type 2 diabetes have been followed for 5-9 years after bariatric surgery.
Disclosures: This study is sponsored by the Cleveland Clinic. The presenter reported serving as a consultant to Ethicon Endosurgery and Apollo Endosurgery.
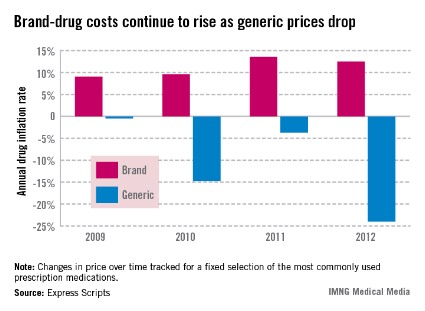
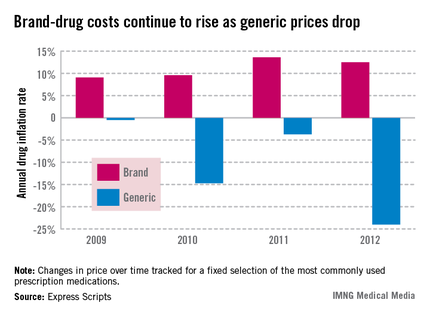
Brand-drug costs rising faster than inflation
The cost of brand drugs increased 12.5% last year, far outpacing inflation overall, Express Scripts said in its annual Drug Trend Report.
The overall U.S. inflation rate, according to the Bureau of Labor Statistics, was only 1.7% in 2012.
From January 2008 to December 2012, the cost of an "unchanged market basket of brand drugs rose from $100 to $165.44," Express Scripts said in the report, while the Consumer Price Index, which measures a broad selection of goods and services, went from $100 to $108.80.
The cost of an unchanged selection of generic drugs did the opposite over the same 5-year period, dropping to $57.38 by the end of 2012, according to the report. All dollar values have been adjusted to 2008 dollars.
In 2012 alone, the cost of generic drugs dropped by 24.4%, following decreases of 3.7% in 2011, 14.7% in 2010, and 0.5% in 2009. The price of brand drugs rose 13.6% in 2011, 9.6% in 2010, and 9.1% in 2009, the report noted.
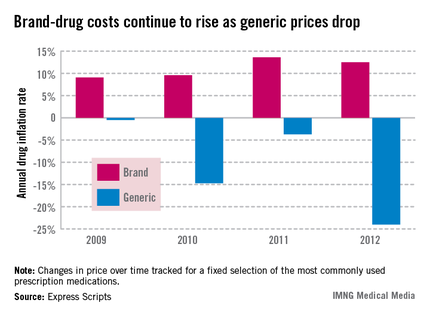
The cost of brand drugs increased 12.5% last year, far outpacing inflation overall, Express Scripts said in its annual Drug Trend Report.
The overall U.S. inflation rate, according to the Bureau of Labor Statistics, was only 1.7% in 2012.
From January 2008 to December 2012, the cost of an "unchanged market basket of brand drugs rose from $100 to $165.44," Express Scripts said in the report, while the Consumer Price Index, which measures a broad selection of goods and services, went from $100 to $108.80.
The cost of an unchanged selection of generic drugs did the opposite over the same 5-year period, dropping to $57.38 by the end of 2012, according to the report. All dollar values have been adjusted to 2008 dollars.
In 2012 alone, the cost of generic drugs dropped by 24.4%, following decreases of 3.7% in 2011, 14.7% in 2010, and 0.5% in 2009. The price of brand drugs rose 13.6% in 2011, 9.6% in 2010, and 9.1% in 2009, the report noted.
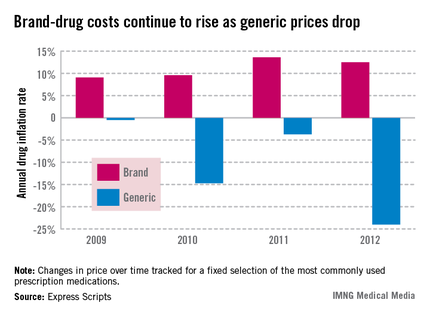
The cost of brand drugs increased 12.5% last year, far outpacing inflation overall, Express Scripts said in its annual Drug Trend Report.
The overall U.S. inflation rate, according to the Bureau of Labor Statistics, was only 1.7% in 2012.
From January 2008 to December 2012, the cost of an "unchanged market basket of brand drugs rose from $100 to $165.44," Express Scripts said in the report, while the Consumer Price Index, which measures a broad selection of goods and services, went from $100 to $108.80.
The cost of an unchanged selection of generic drugs did the opposite over the same 5-year period, dropping to $57.38 by the end of 2012, according to the report. All dollar values have been adjusted to 2008 dollars.
In 2012 alone, the cost of generic drugs dropped by 24.4%, following decreases of 3.7% in 2011, 14.7% in 2010, and 0.5% in 2009. The price of brand drugs rose 13.6% in 2011, 9.6% in 2010, and 9.1% in 2009, the report noted.
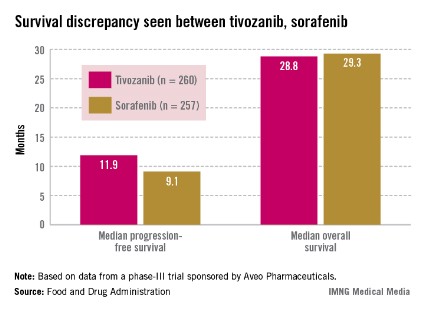
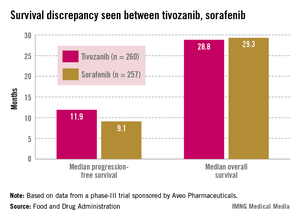
FDA advisory panel decides tivozanib falls short for advanced renal cell carcinoma
SILVER SPRING, MD. – Tivozanib’s risk-benefit profile fell short in a trial comparing the drug to sorafenib in patients with advanced renal cell carcinoma.
Citing a lower overall survival among patients in the tivozanib arm, despite a significant benefit in progression-free survival, the FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 13 to 1 at a May 2 meeting that the risk-benefit profile for tivozanib was not favorable.
Tivozanib appeared to be active in renal cell carcinoma (RCC) and had a manageable safety profile, the panelists said. But they had reservations about the design and patient demographics of the study; 88% of those enrolled in the trial were from Central and Eastern Europe. Only 8% of the patients in the study were enrolled in the United States and Western Europe, and only one black patient was enrolled, raising questions about the relevance of outcomes for a diversity of patients. Further, the trial’s comparator drug was sorafenib rather than a newer first-line tyrosine kinase inhibitor (TKI).
"While we are disappointed with the outcome of the ODAC vote, we remain confident in the efficacy, safety, and tolerability of tivozanib in RCC patients," Tuan Ha-Ngoc, president and chief executive officer of Aveo, the maker of tivozanib, said in a statement. "We are committed to the RCC patient community and will work closely with the FDA to address the issues discussed by the panel today as the agency continues its ongoing review of the New Drug Application for tivozanib."
Tivozanib, an oral capsule taken once a day, is a highly selective vascular endothelial growth factor (VEGF) TKI, according to Aveo. The company presented the results of the pivotal phase III study, the TIVO-1 (Tivozanib Versus Sorafenib in First-Line Advanced RCC) trial, which compared treatment with tivozanib in 260 patients with sorafenib in 257 patients. In 2005 sorafenib (Nexavar) became the first TKI approved for advanced RCC; several others have been approved since that time. In the United States, those newer drugs are considered before prescribing sorafenib in treating RCC.
Median progression-free survival (PFS), the primary endpoint of the study, was 11.9 months among those treated with tivozanib and 9.1 months among those on sorafenib, a significant difference that represented a 20% reduced risk (hazard ratio, 0.80).
Overall survival was poorer, however: 28.8 months in patients on tivozanib and 29.3 months in those on sorafenib (HR, 1.25). Overall, the safety profile of tivozanib was comparable to the profile of other VEGF inhibitors. Hypertension and dysphonia were more common with tivozanib, and diarrhea and plantar-palmar dysesthesia (hand-foot syndrome) were more common with sorafenib.
Aveo could not identify a safety signal to explain the lower overall survival. Company officials at the meeting said that more patients in the sorafenib arm (63%) crossed over to treatment with a targeted therapy, which in most cases was tivozanib. In the tivozanib arm, 16% crossed over to treatment with another therapy. The study’s protocol initially allowed crossover only in patients on sorafenib.
While there was a 20% improvement in PFS, there was "a potential 25% increase in the risk of death" compared with sorafenib, noted Dr. Jonathan Jarow, of the FDA’s Office of Hematology and Oncology Products. The company’s hypothesis regarding the crossover effect could not be proven with a post hoc analysis of the data "and remains just a hypothesis."
Approving a drug with a possible 25% increase in the risk of death was the FDA’s major concern and would set a precedent for approval of an oncology drug. The seven drugs approved for treating advanced RCC are thought to work by inhibiting VEGF or its receptor. Most of these approvals, except for temsirolimus, were based on improvements in PFS. Temsirolimus was additionally shown to improve overall survival in patients with a poor prognosis, according to the FDA.
Dr. Mikkael Sekeres, of the department of hematologic oncology and blood disorders at the Cleveland Clinic Taussig Cancer Institute, and the chair of the advisory panel to the FDA, expressed concern about the ethics of the study, which initially allowed crossover to another treatment in only one arm of the study and was conducted primarily in countries where other active RCC therapies are not readily available.
During the meeting, oncologists pointed out that treatments administered sequentially are associated with improved outcomes for patients with RCC.
"I cannot picture how I would be able to sit and talk with a patient about treating her or him with a drug that would allow that person to live without progression longer but possibly to die faster than if I treated that person with another available renal carcinoma drug, so I voted no," he added.
Aveo is developing tivozanib with Astellas Pharma. It is also being studied in combination with other targeted treatments or with chemotherapy regimens in patients with RCC, breast cancer, and colorectal cancer, according to Aveo. It has not been approved in any country.
The FDA usually follows the recommendations of its advisory panels. The deadline for the FDA review to be completed is July 28, according to Aveo. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at the tivozanib meeting.
SILVER SPRING, MD. – Tivozanib’s risk-benefit profile fell short in a trial comparing the drug to sorafenib in patients with advanced renal cell carcinoma.
Citing a lower overall survival among patients in the tivozanib arm, despite a significant benefit in progression-free survival, the FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 13 to 1 at a May 2 meeting that the risk-benefit profile for tivozanib was not favorable.
Tivozanib appeared to be active in renal cell carcinoma (RCC) and had a manageable safety profile, the panelists said. But they had reservations about the design and patient demographics of the study; 88% of those enrolled in the trial were from Central and Eastern Europe. Only 8% of the patients in the study were enrolled in the United States and Western Europe, and only one black patient was enrolled, raising questions about the relevance of outcomes for a diversity of patients. Further, the trial’s comparator drug was sorafenib rather than a newer first-line tyrosine kinase inhibitor (TKI).
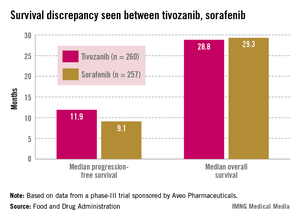
"While we are disappointed with the outcome of the ODAC vote, we remain confident in the efficacy, safety, and tolerability of tivozanib in RCC patients," Tuan Ha-Ngoc, president and chief executive officer of Aveo, the maker of tivozanib, said in a statement. "We are committed to the RCC patient community and will work closely with the FDA to address the issues discussed by the panel today as the agency continues its ongoing review of the New Drug Application for tivozanib."
Tivozanib, an oral capsule taken once a day, is a highly selective vascular endothelial growth factor (VEGF) TKI, according to Aveo. The company presented the results of the pivotal phase III study, the TIVO-1 (Tivozanib Versus Sorafenib in First-Line Advanced RCC) trial, which compared treatment with tivozanib in 260 patients with sorafenib in 257 patients. In 2005 sorafenib (Nexavar) became the first TKI approved for advanced RCC; several others have been approved since that time. In the United States, those newer drugs are considered before prescribing sorafenib in treating RCC.
Median progression-free survival (PFS), the primary endpoint of the study, was 11.9 months among those treated with tivozanib and 9.1 months among those on sorafenib, a significant difference that represented a 20% reduced risk (hazard ratio, 0.80).
Overall survival was poorer, however: 28.8 months in patients on tivozanib and 29.3 months in those on sorafenib (HR, 1.25). Overall, the safety profile of tivozanib was comparable to the profile of other VEGF inhibitors. Hypertension and dysphonia were more common with tivozanib, and diarrhea and plantar-palmar dysesthesia (hand-foot syndrome) were more common with sorafenib.
Aveo could not identify a safety signal to explain the lower overall survival. Company officials at the meeting said that more patients in the sorafenib arm (63%) crossed over to treatment with a targeted therapy, which in most cases was tivozanib. In the tivozanib arm, 16% crossed over to treatment with another therapy. The study’s protocol initially allowed crossover only in patients on sorafenib.
While there was a 20% improvement in PFS, there was "a potential 25% increase in the risk of death" compared with sorafenib, noted Dr. Jonathan Jarow, of the FDA’s Office of Hematology and Oncology Products. The company’s hypothesis regarding the crossover effect could not be proven with a post hoc analysis of the data "and remains just a hypothesis."
Approving a drug with a possible 25% increase in the risk of death was the FDA’s major concern and would set a precedent for approval of an oncology drug. The seven drugs approved for treating advanced RCC are thought to work by inhibiting VEGF or its receptor. Most of these approvals, except for temsirolimus, were based on improvements in PFS. Temsirolimus was additionally shown to improve overall survival in patients with a poor prognosis, according to the FDA.
Dr. Mikkael Sekeres, of the department of hematologic oncology and blood disorders at the Cleveland Clinic Taussig Cancer Institute, and the chair of the advisory panel to the FDA, expressed concern about the ethics of the study, which initially allowed crossover to another treatment in only one arm of the study and was conducted primarily in countries where other active RCC therapies are not readily available.
During the meeting, oncologists pointed out that treatments administered sequentially are associated with improved outcomes for patients with RCC.
"I cannot picture how I would be able to sit and talk with a patient about treating her or him with a drug that would allow that person to live without progression longer but possibly to die faster than if I treated that person with another available renal carcinoma drug, so I voted no," he added.
Aveo is developing tivozanib with Astellas Pharma. It is also being studied in combination with other targeted treatments or with chemotherapy regimens in patients with RCC, breast cancer, and colorectal cancer, according to Aveo. It has not been approved in any country.
The FDA usually follows the recommendations of its advisory panels. The deadline for the FDA review to be completed is July 28, according to Aveo. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at the tivozanib meeting.
SILVER SPRING, MD. – Tivozanib’s risk-benefit profile fell short in a trial comparing the drug to sorafenib in patients with advanced renal cell carcinoma.
Citing a lower overall survival among patients in the tivozanib arm, despite a significant benefit in progression-free survival, the FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 13 to 1 at a May 2 meeting that the risk-benefit profile for tivozanib was not favorable.
Tivozanib appeared to be active in renal cell carcinoma (RCC) and had a manageable safety profile, the panelists said. But they had reservations about the design and patient demographics of the study; 88% of those enrolled in the trial were from Central and Eastern Europe. Only 8% of the patients in the study were enrolled in the United States and Western Europe, and only one black patient was enrolled, raising questions about the relevance of outcomes for a diversity of patients. Further, the trial’s comparator drug was sorafenib rather than a newer first-line tyrosine kinase inhibitor (TKI).
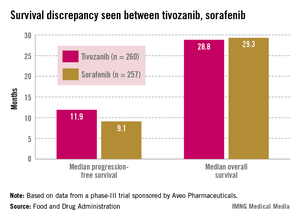
"While we are disappointed with the outcome of the ODAC vote, we remain confident in the efficacy, safety, and tolerability of tivozanib in RCC patients," Tuan Ha-Ngoc, president and chief executive officer of Aveo, the maker of tivozanib, said in a statement. "We are committed to the RCC patient community and will work closely with the FDA to address the issues discussed by the panel today as the agency continues its ongoing review of the New Drug Application for tivozanib."
Tivozanib, an oral capsule taken once a day, is a highly selective vascular endothelial growth factor (VEGF) TKI, according to Aveo. The company presented the results of the pivotal phase III study, the TIVO-1 (Tivozanib Versus Sorafenib in First-Line Advanced RCC) trial, which compared treatment with tivozanib in 260 patients with sorafenib in 257 patients. In 2005 sorafenib (Nexavar) became the first TKI approved for advanced RCC; several others have been approved since that time. In the United States, those newer drugs are considered before prescribing sorafenib in treating RCC.
Median progression-free survival (PFS), the primary endpoint of the study, was 11.9 months among those treated with tivozanib and 9.1 months among those on sorafenib, a significant difference that represented a 20% reduced risk (hazard ratio, 0.80).
Overall survival was poorer, however: 28.8 months in patients on tivozanib and 29.3 months in those on sorafenib (HR, 1.25). Overall, the safety profile of tivozanib was comparable to the profile of other VEGF inhibitors. Hypertension and dysphonia were more common with tivozanib, and diarrhea and plantar-palmar dysesthesia (hand-foot syndrome) were more common with sorafenib.
Aveo could not identify a safety signal to explain the lower overall survival. Company officials at the meeting said that more patients in the sorafenib arm (63%) crossed over to treatment with a targeted therapy, which in most cases was tivozanib. In the tivozanib arm, 16% crossed over to treatment with another therapy. The study’s protocol initially allowed crossover only in patients on sorafenib.
While there was a 20% improvement in PFS, there was "a potential 25% increase in the risk of death" compared with sorafenib, noted Dr. Jonathan Jarow, of the FDA’s Office of Hematology and Oncology Products. The company’s hypothesis regarding the crossover effect could not be proven with a post hoc analysis of the data "and remains just a hypothesis."
Approving a drug with a possible 25% increase in the risk of death was the FDA’s major concern and would set a precedent for approval of an oncology drug. The seven drugs approved for treating advanced RCC are thought to work by inhibiting VEGF or its receptor. Most of these approvals, except for temsirolimus, were based on improvements in PFS. Temsirolimus was additionally shown to improve overall survival in patients with a poor prognosis, according to the FDA.
Dr. Mikkael Sekeres, of the department of hematologic oncology and blood disorders at the Cleveland Clinic Taussig Cancer Institute, and the chair of the advisory panel to the FDA, expressed concern about the ethics of the study, which initially allowed crossover to another treatment in only one arm of the study and was conducted primarily in countries where other active RCC therapies are not readily available.
During the meeting, oncologists pointed out that treatments administered sequentially are associated with improved outcomes for patients with RCC.
"I cannot picture how I would be able to sit and talk with a patient about treating her or him with a drug that would allow that person to live without progression longer but possibly to die faster than if I treated that person with another available renal carcinoma drug, so I voted no," he added.
Aveo is developing tivozanib with Astellas Pharma. It is also being studied in combination with other targeted treatments or with chemotherapy regimens in patients with RCC, breast cancer, and colorectal cancer, according to Aveo. It has not been approved in any country.
The FDA usually follows the recommendations of its advisory panels. The deadline for the FDA review to be completed is July 28, according to Aveo. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. Occasionally, a panelist may be given a waiver, but not at the tivozanib meeting.
AT AN FDA ADVISORY PANEL MEETING
Know your values to achieve professional balance
SAN FRANCISCO – Maintaining balance and enthusiasm – at home and at your practice – can seem to be an impossible challenge. And yet, without it – in every aspect of your life – you will be a less-capable physician, a less-engaged and happy spouse or friend, a less satisfied person, and not on top of your game.
That’s according to Dr. Linda Clever, an internist who is president of Renew, a project of the Institute for Health & Healing at California Pacific Medical Center in San Francisco.
"It turns out that if we’re bored, if we’re sad, if we’re frightened, it leads to a loss of creativity, a loss of enthusiasm and engagement, and resilience and effectiveness, not just at work, but at home," Dr. Clever told attendees at the annual meeting of the American College of Physicians.
She was not discussing burnout, but something different. "If you’re rushing through the day just to get through the day, that’s an incipient sign of not being engaged," she said, calling that "a danger signal."
The key is to use your values as your foundation. "What gets you to happiness is living your values."
Dr. Clever said that people who are balanced, and at the top of their game:
• Have strong relationships.
• Have a religious or spiritual life of some sort, which might just be having a constant sense of wonder at the world.
• Take care of themselves.
• Like their work.
• Have the basic conviction that they can play the hand that’s dealt them. That is, the ways things are might not be the preferred way, but life is manageable.
During her presentation at the meeting, Dr. Clever led attendees through a variation on the workshops she gives at Renew. The program helps people identify and define their personal values, and offers ways to live out those values even while managing complex responsibilities and priorities. She asked attendees for their definition of success. Among the terms she collected: balance, happiness, peace, wellness, making a difference, money, and positive feedback. Control was also mentioned.
Dr. Clever said that control is a common term among physicians. Doctors "like to control things," she said. It’s not surprising, as they really have to be obsessive-compulsive, said Dr. Clever. "Who else is going to get a second creatinine? Who else is going to take a picture of that lesion and follow it for 3 days? Who else is going to draw a circle around that erythema and look at it again in 2 hours?" she asked.
But that creates what she called a "soft underbelly." The desire for control is a vulnerability because "when we aren’t perfect, it’s very hard on us, and it’s very disturbing," said Dr. Clever.
There are some things that physicians can control. The most important thing is to live your values. Values are what someone believes is good or bad, right or wrong, and what gives meaning, fuel, and joy. Once you know your values, then you can define success, and know how you will spend your time," she said.
When physician attendees were asked to share some of their values, they mentioned honesty, integrity, humor, empathy, compassion, self-sacrifice, tolerance, service, humility, charity, sustainability, spirituality, and respect for self and others. Values should be written down, discussed out loud and shared with loved ones, advised Dr. Clever.
Physicians, like anyone striving for balance, can also control their attitudes and how they respond and cope when faced with adversity. In that vein, she said, many people have been inspired by "Man's Search for Meaning," (Boston: Beacon Press, 2006) a memoir by psychiatrist Viktor Frankl, who spent several years in Nazi concentration camps.
"Frankl wrote that the last human freedom is the freedom to choose your attitude in a given set of circumstances," said Dr. Clever. She said that physicians could adopt this philosophy and talk to their patients, or to their teenagers, about this concept. "You can choose to be a victim and you can choose to be a winner."
If you’re feeling overwhelmed, get help, advised Dr. Clever, adding, "That’s what money is for." Consider a gardener or a housekeeper or even a life coach. And, if things aren’t going well, don’t just complain. Also, give up what Dr. Clever calls "BMW": bitching, moaning, and whining.
Learn new tricks, she advised, especially if the old way isn’t working. "We have to get more comfortable with change."
"One new trick is to learn how to say ‘no,’ " Dr. Clever said. Physicians like to please and "it turns out if we’re doing too much, we can’t do anything well."
One tip for saying no gracefully is to employ what she called the "no sandwich." On the top, you thank the person for asking you. In the middle is the "no," and on the bottom, you thank the person again and say that you are honored to have been asked.
On Twitter @aliciaault
SAN FRANCISCO – Maintaining balance and enthusiasm – at home and at your practice – can seem to be an impossible challenge. And yet, without it – in every aspect of your life – you will be a less-capable physician, a less-engaged and happy spouse or friend, a less satisfied person, and not on top of your game.
That’s according to Dr. Linda Clever, an internist who is president of Renew, a project of the Institute for Health & Healing at California Pacific Medical Center in San Francisco.
"It turns out that if we’re bored, if we’re sad, if we’re frightened, it leads to a loss of creativity, a loss of enthusiasm and engagement, and resilience and effectiveness, not just at work, but at home," Dr. Clever told attendees at the annual meeting of the American College of Physicians.
She was not discussing burnout, but something different. "If you’re rushing through the day just to get through the day, that’s an incipient sign of not being engaged," she said, calling that "a danger signal."
The key is to use your values as your foundation. "What gets you to happiness is living your values."
Dr. Clever said that people who are balanced, and at the top of their game:
• Have strong relationships.
• Have a religious or spiritual life of some sort, which might just be having a constant sense of wonder at the world.
• Take care of themselves.
• Like their work.
• Have the basic conviction that they can play the hand that’s dealt them. That is, the ways things are might not be the preferred way, but life is manageable.
During her presentation at the meeting, Dr. Clever led attendees through a variation on the workshops she gives at Renew. The program helps people identify and define their personal values, and offers ways to live out those values even while managing complex responsibilities and priorities. She asked attendees for their definition of success. Among the terms she collected: balance, happiness, peace, wellness, making a difference, money, and positive feedback. Control was also mentioned.
Dr. Clever said that control is a common term among physicians. Doctors "like to control things," she said. It’s not surprising, as they really have to be obsessive-compulsive, said Dr. Clever. "Who else is going to get a second creatinine? Who else is going to take a picture of that lesion and follow it for 3 days? Who else is going to draw a circle around that erythema and look at it again in 2 hours?" she asked.
But that creates what she called a "soft underbelly." The desire for control is a vulnerability because "when we aren’t perfect, it’s very hard on us, and it’s very disturbing," said Dr. Clever.
There are some things that physicians can control. The most important thing is to live your values. Values are what someone believes is good or bad, right or wrong, and what gives meaning, fuel, and joy. Once you know your values, then you can define success, and know how you will spend your time," she said.
When physician attendees were asked to share some of their values, they mentioned honesty, integrity, humor, empathy, compassion, self-sacrifice, tolerance, service, humility, charity, sustainability, spirituality, and respect for self and others. Values should be written down, discussed out loud and shared with loved ones, advised Dr. Clever.
Physicians, like anyone striving for balance, can also control their attitudes and how they respond and cope when faced with adversity. In that vein, she said, many people have been inspired by "Man's Search for Meaning," (Boston: Beacon Press, 2006) a memoir by psychiatrist Viktor Frankl, who spent several years in Nazi concentration camps.
"Frankl wrote that the last human freedom is the freedom to choose your attitude in a given set of circumstances," said Dr. Clever. She said that physicians could adopt this philosophy and talk to their patients, or to their teenagers, about this concept. "You can choose to be a victim and you can choose to be a winner."
If you’re feeling overwhelmed, get help, advised Dr. Clever, adding, "That’s what money is for." Consider a gardener or a housekeeper or even a life coach. And, if things aren’t going well, don’t just complain. Also, give up what Dr. Clever calls "BMW": bitching, moaning, and whining.
Learn new tricks, she advised, especially if the old way isn’t working. "We have to get more comfortable with change."
"One new trick is to learn how to say ‘no,’ " Dr. Clever said. Physicians like to please and "it turns out if we’re doing too much, we can’t do anything well."
One tip for saying no gracefully is to employ what she called the "no sandwich." On the top, you thank the person for asking you. In the middle is the "no," and on the bottom, you thank the person again and say that you are honored to have been asked.
On Twitter @aliciaault
SAN FRANCISCO – Maintaining balance and enthusiasm – at home and at your practice – can seem to be an impossible challenge. And yet, without it – in every aspect of your life – you will be a less-capable physician, a less-engaged and happy spouse or friend, a less satisfied person, and not on top of your game.
That’s according to Dr. Linda Clever, an internist who is president of Renew, a project of the Institute for Health & Healing at California Pacific Medical Center in San Francisco.
"It turns out that if we’re bored, if we’re sad, if we’re frightened, it leads to a loss of creativity, a loss of enthusiasm and engagement, and resilience and effectiveness, not just at work, but at home," Dr. Clever told attendees at the annual meeting of the American College of Physicians.
She was not discussing burnout, but something different. "If you’re rushing through the day just to get through the day, that’s an incipient sign of not being engaged," she said, calling that "a danger signal."
The key is to use your values as your foundation. "What gets you to happiness is living your values."
Dr. Clever said that people who are balanced, and at the top of their game:
• Have strong relationships.
• Have a religious or spiritual life of some sort, which might just be having a constant sense of wonder at the world.
• Take care of themselves.
• Like their work.
• Have the basic conviction that they can play the hand that’s dealt them. That is, the ways things are might not be the preferred way, but life is manageable.
During her presentation at the meeting, Dr. Clever led attendees through a variation on the workshops she gives at Renew. The program helps people identify and define their personal values, and offers ways to live out those values even while managing complex responsibilities and priorities. She asked attendees for their definition of success. Among the terms she collected: balance, happiness, peace, wellness, making a difference, money, and positive feedback. Control was also mentioned.
Dr. Clever said that control is a common term among physicians. Doctors "like to control things," she said. It’s not surprising, as they really have to be obsessive-compulsive, said Dr. Clever. "Who else is going to get a second creatinine? Who else is going to take a picture of that lesion and follow it for 3 days? Who else is going to draw a circle around that erythema and look at it again in 2 hours?" she asked.
But that creates what she called a "soft underbelly." The desire for control is a vulnerability because "when we aren’t perfect, it’s very hard on us, and it’s very disturbing," said Dr. Clever.
There are some things that physicians can control. The most important thing is to live your values. Values are what someone believes is good or bad, right or wrong, and what gives meaning, fuel, and joy. Once you know your values, then you can define success, and know how you will spend your time," she said.
When physician attendees were asked to share some of their values, they mentioned honesty, integrity, humor, empathy, compassion, self-sacrifice, tolerance, service, humility, charity, sustainability, spirituality, and respect for self and others. Values should be written down, discussed out loud and shared with loved ones, advised Dr. Clever.
Physicians, like anyone striving for balance, can also control their attitudes and how they respond and cope when faced with adversity. In that vein, she said, many people have been inspired by "Man's Search for Meaning," (Boston: Beacon Press, 2006) a memoir by psychiatrist Viktor Frankl, who spent several years in Nazi concentration camps.
"Frankl wrote that the last human freedom is the freedom to choose your attitude in a given set of circumstances," said Dr. Clever. She said that physicians could adopt this philosophy and talk to their patients, or to their teenagers, about this concept. "You can choose to be a victim and you can choose to be a winner."
If you’re feeling overwhelmed, get help, advised Dr. Clever, adding, "That’s what money is for." Consider a gardener or a housekeeper or even a life coach. And, if things aren’t going well, don’t just complain. Also, give up what Dr. Clever calls "BMW": bitching, moaning, and whining.
Learn new tricks, she advised, especially if the old way isn’t working. "We have to get more comfortable with change."
"One new trick is to learn how to say ‘no,’ " Dr. Clever said. Physicians like to please and "it turns out if we’re doing too much, we can’t do anything well."
One tip for saying no gracefully is to employ what she called the "no sandwich." On the top, you thank the person for asking you. In the middle is the "no," and on the bottom, you thank the person again and say that you are honored to have been asked.
On Twitter @aliciaault
EXPERT ANALYSIS FROM INTERNAL MEDICINE 2013
Elderly drive increase in U.K. aortic valve interventions
LOS ANGELES – Aortic valve interventions rose sharply in the United Kingdom during a recent 5-year period, largely due to a spike in procedures among elderly patients, researchers reported at the annual meeting of the Society of Thoracic Surgeons.
In the study, the combined U.K. Cardiac Surgical and Transcatheter Aortic Valve Implantation (TAVI) Registries – known as SATIRE for short – the team analyzed data from 37,020 patients nationwide who underwent aortic valve interventions (excluding balloon valvuloplasty) between 2006 and 2010.
Results showed that the annual number of these procedures increased by 32% over the course of the study, with about half of the increase due to procedures among patients aged 80 years and older, reported lead investigator Dr. Neil E. Moat, a cardiac surgeon and codirector of the Transcatheter Valve Programme at the Royal Brompton Hospital in London.
Overall, the annual number of aortic valve interventions increased during the study period, from 6,217 in 2006 to 8,201 in 2010. This was driven largely by a near doubling in interventions among patients aged 80 years or older, from 1,055 to 2,035.
"In 2010, 25% of all aortic valve interventions in the U.K. were performed in patients aged 80 or over," Dr. Moat noted.
By type of intervention, there was an increase in the annual number of TAVIs (from none to 749) and conventional surgeries (from 6,217 to 7,252), although the latter stabilized toward the end of the period.
"This is the first time in the whole history – 35 years of collecting U.K. cardiac surgical data – that these numbers have plateaued," he commented.
As of 2010, TAVIs accounted for 9% of all aortic valve interventions studied.
Not surprisingly, patients undergoing TAVI surgery were older than their counterparts undergoing conventional surgery, had a higher risk profile, and had poorer postoperative survival, but their lengths of hospital stay were statistically indistinguishable.
Importantly, two scores used in Europe to predict mortality after such interventions showed differential performance.
"The logistic EuroSCORE does not predict operative outcomes of surgery or TAVI" and should not be used, Dr. Moat advised. "The EuroSCORE II is probably quite good for conventional surgery but again is rather poor for predicting mortality outcomes from TAVI. And I suppose on this side of the pond, you will be pleased to hear that the STS [U.S. Society of Thoracic Surgeons] score is far better than either of these European scores in our population."
In the discussion after the presentation of the study, Dr. Paul A. Kurlansky, a cardiothoracic surgeon from Miami, remarked, "Maybe our risk score is better on this side of the pond, but we do not have the merging of databases that you guys have over there [in the U.K.], or the completion of them. One opportunity that I was wondering if you had taken or are planning to take advantage of is the ability to do propensity score matching or use other statistical tools in order to really match patients so that you can compare outcomes."
"That’s a very interesting question and something that we have debated long and hard," Dr. Moat replied, citing reservations given by the study’s statisticians. "They are very firm in their belief that whilst you can apply those statistical techniques, they are actually not valid because you have so much confounding by indication that [you are unable] to propensity-match populations. So it’s a deliberate decision not to pursue that."
Main analyses in the study used prospectively collected registry data for 35,392 patients undergoing conventional surgery – either aortic valve replacement (AVR) alone or combined with coronary artery bypass grafting (CABG) – and 1,628 TAVIs.
"Because [the registries] are national and publicly funded, they are free from any commercial bias. These are mandatory registries and therefore free of any selection bias," Dr. Moat pointed out. Furthermore, there is good standardization of definitions and long-term follow-up of mortality.
"All cardiac surgical procedures and all TAVIs in the U.K. are entered into national registries hosted by the National Institute for Cardiovascular Outcomes Research. The data set and databases of all of these registries are designed to be compatible and comparable," he added.
Overall, compared with patients undergoing surgery, patients undergoing TAVI were on average older and had a higher risk profile in terms of cardiovascular measures and comorbidities, although there was substantial overlap.
The median postoperative length of stay was 8 days after conventional surgery and 7 days after TAVI. "Despite the TAVI patients being older and at increased risk, there was no difference in postoperative length of stay. If anything, it was marginally lower in the TAVI group," Dr. Moat commented. The distribution of length of stay was also much the same. "You see a substantial numbers of these elderly, frail, and high-risk patients [in the TAVI group] being discharged before day 6," he added.
Actuarial analyses in the study population overall showed poorer survival after TAVI than after conventional surgery (whether AVR alone or combined with CABG), both in the first year and longer term. However, the gaps between curves were smaller among patients aged 80 years or older.
Among the patients undergoing TAVI, longer-term survival after aortic valve intervention did not differ according to the number of diseased vessels treated.
"An interesting observation worthy of further study is that we are well aware that patients having combined AVR and CABG have worse earlier and late survival than patients having isolated AVR. But it would seem that the presence of concomitant coronary artery disease – despite much of it being left untreated – did not affect early or late survival following TAVI," Dr. Moat commented.
The EuroSCORE was a poor predictor of mortality after both conventional surgery and TAVI, but the EuroSCORE II performed fairly well after conventional surgery, whether isolated AVR (observed:expected ratio, 0.87; area under the curve, 0.78) or AVR plus CABG (observed:expected ratio, 1.0; area under the curve, 0.73).
Dr. Moat disclosed that he is on the speakers bureau for, and receives honoraria from, Abbott Laboratories, and sits on the consultant/advisory board of Medtronic.
LOS ANGELES – Aortic valve interventions rose sharply in the United Kingdom during a recent 5-year period, largely due to a spike in procedures among elderly patients, researchers reported at the annual meeting of the Society of Thoracic Surgeons.
In the study, the combined U.K. Cardiac Surgical and Transcatheter Aortic Valve Implantation (TAVI) Registries – known as SATIRE for short – the team analyzed data from 37,020 patients nationwide who underwent aortic valve interventions (excluding balloon valvuloplasty) between 2006 and 2010.
Results showed that the annual number of these procedures increased by 32% over the course of the study, with about half of the increase due to procedures among patients aged 80 years and older, reported lead investigator Dr. Neil E. Moat, a cardiac surgeon and codirector of the Transcatheter Valve Programme at the Royal Brompton Hospital in London.
Overall, the annual number of aortic valve interventions increased during the study period, from 6,217 in 2006 to 8,201 in 2010. This was driven largely by a near doubling in interventions among patients aged 80 years or older, from 1,055 to 2,035.
"In 2010, 25% of all aortic valve interventions in the U.K. were performed in patients aged 80 or over," Dr. Moat noted.
By type of intervention, there was an increase in the annual number of TAVIs (from none to 749) and conventional surgeries (from 6,217 to 7,252), although the latter stabilized toward the end of the period.
"This is the first time in the whole history – 35 years of collecting U.K. cardiac surgical data – that these numbers have plateaued," he commented.
As of 2010, TAVIs accounted for 9% of all aortic valve interventions studied.
Not surprisingly, patients undergoing TAVI surgery were older than their counterparts undergoing conventional surgery, had a higher risk profile, and had poorer postoperative survival, but their lengths of hospital stay were statistically indistinguishable.
Importantly, two scores used in Europe to predict mortality after such interventions showed differential performance.
"The logistic EuroSCORE does not predict operative outcomes of surgery or TAVI" and should not be used, Dr. Moat advised. "The EuroSCORE II is probably quite good for conventional surgery but again is rather poor for predicting mortality outcomes from TAVI. And I suppose on this side of the pond, you will be pleased to hear that the STS [U.S. Society of Thoracic Surgeons] score is far better than either of these European scores in our population."
In the discussion after the presentation of the study, Dr. Paul A. Kurlansky, a cardiothoracic surgeon from Miami, remarked, "Maybe our risk score is better on this side of the pond, but we do not have the merging of databases that you guys have over there [in the U.K.], or the completion of them. One opportunity that I was wondering if you had taken or are planning to take advantage of is the ability to do propensity score matching or use other statistical tools in order to really match patients so that you can compare outcomes."
"That’s a very interesting question and something that we have debated long and hard," Dr. Moat replied, citing reservations given by the study’s statisticians. "They are very firm in their belief that whilst you can apply those statistical techniques, they are actually not valid because you have so much confounding by indication that [you are unable] to propensity-match populations. So it’s a deliberate decision not to pursue that."
Main analyses in the study used prospectively collected registry data for 35,392 patients undergoing conventional surgery – either aortic valve replacement (AVR) alone or combined with coronary artery bypass grafting (CABG) – and 1,628 TAVIs.
"Because [the registries] are national and publicly funded, they are free from any commercial bias. These are mandatory registries and therefore free of any selection bias," Dr. Moat pointed out. Furthermore, there is good standardization of definitions and long-term follow-up of mortality.
"All cardiac surgical procedures and all TAVIs in the U.K. are entered into national registries hosted by the National Institute for Cardiovascular Outcomes Research. The data set and databases of all of these registries are designed to be compatible and comparable," he added.
Overall, compared with patients undergoing surgery, patients undergoing TAVI were on average older and had a higher risk profile in terms of cardiovascular measures and comorbidities, although there was substantial overlap.
The median postoperative length of stay was 8 days after conventional surgery and 7 days after TAVI. "Despite the TAVI patients being older and at increased risk, there was no difference in postoperative length of stay. If anything, it was marginally lower in the TAVI group," Dr. Moat commented. The distribution of length of stay was also much the same. "You see a substantial numbers of these elderly, frail, and high-risk patients [in the TAVI group] being discharged before day 6," he added.
Actuarial analyses in the study population overall showed poorer survival after TAVI than after conventional surgery (whether AVR alone or combined with CABG), both in the first year and longer term. However, the gaps between curves were smaller among patients aged 80 years or older.
Among the patients undergoing TAVI, longer-term survival after aortic valve intervention did not differ according to the number of diseased vessels treated.
"An interesting observation worthy of further study is that we are well aware that patients having combined AVR and CABG have worse earlier and late survival than patients having isolated AVR. But it would seem that the presence of concomitant coronary artery disease – despite much of it being left untreated – did not affect early or late survival following TAVI," Dr. Moat commented.
The EuroSCORE was a poor predictor of mortality after both conventional surgery and TAVI, but the EuroSCORE II performed fairly well after conventional surgery, whether isolated AVR (observed:expected ratio, 0.87; area under the curve, 0.78) or AVR plus CABG (observed:expected ratio, 1.0; area under the curve, 0.73).
Dr. Moat disclosed that he is on the speakers bureau for, and receives honoraria from, Abbott Laboratories, and sits on the consultant/advisory board of Medtronic.
LOS ANGELES – Aortic valve interventions rose sharply in the United Kingdom during a recent 5-year period, largely due to a spike in procedures among elderly patients, researchers reported at the annual meeting of the Society of Thoracic Surgeons.
In the study, the combined U.K. Cardiac Surgical and Transcatheter Aortic Valve Implantation (TAVI) Registries – known as SATIRE for short – the team analyzed data from 37,020 patients nationwide who underwent aortic valve interventions (excluding balloon valvuloplasty) between 2006 and 2010.
Results showed that the annual number of these procedures increased by 32% over the course of the study, with about half of the increase due to procedures among patients aged 80 years and older, reported lead investigator Dr. Neil E. Moat, a cardiac surgeon and codirector of the Transcatheter Valve Programme at the Royal Brompton Hospital in London.
Overall, the annual number of aortic valve interventions increased during the study period, from 6,217 in 2006 to 8,201 in 2010. This was driven largely by a near doubling in interventions among patients aged 80 years or older, from 1,055 to 2,035.
"In 2010, 25% of all aortic valve interventions in the U.K. were performed in patients aged 80 or over," Dr. Moat noted.
By type of intervention, there was an increase in the annual number of TAVIs (from none to 749) and conventional surgeries (from 6,217 to 7,252), although the latter stabilized toward the end of the period.
"This is the first time in the whole history – 35 years of collecting U.K. cardiac surgical data – that these numbers have plateaued," he commented.
As of 2010, TAVIs accounted for 9% of all aortic valve interventions studied.
Not surprisingly, patients undergoing TAVI surgery were older than their counterparts undergoing conventional surgery, had a higher risk profile, and had poorer postoperative survival, but their lengths of hospital stay were statistically indistinguishable.
Importantly, two scores used in Europe to predict mortality after such interventions showed differential performance.
"The logistic EuroSCORE does not predict operative outcomes of surgery or TAVI" and should not be used, Dr. Moat advised. "The EuroSCORE II is probably quite good for conventional surgery but again is rather poor for predicting mortality outcomes from TAVI. And I suppose on this side of the pond, you will be pleased to hear that the STS [U.S. Society of Thoracic Surgeons] score is far better than either of these European scores in our population."
In the discussion after the presentation of the study, Dr. Paul A. Kurlansky, a cardiothoracic surgeon from Miami, remarked, "Maybe our risk score is better on this side of the pond, but we do not have the merging of databases that you guys have over there [in the U.K.], or the completion of them. One opportunity that I was wondering if you had taken or are planning to take advantage of is the ability to do propensity score matching or use other statistical tools in order to really match patients so that you can compare outcomes."
"That’s a very interesting question and something that we have debated long and hard," Dr. Moat replied, citing reservations given by the study’s statisticians. "They are very firm in their belief that whilst you can apply those statistical techniques, they are actually not valid because you have so much confounding by indication that [you are unable] to propensity-match populations. So it’s a deliberate decision not to pursue that."
Main analyses in the study used prospectively collected registry data for 35,392 patients undergoing conventional surgery – either aortic valve replacement (AVR) alone or combined with coronary artery bypass grafting (CABG) – and 1,628 TAVIs.
"Because [the registries] are national and publicly funded, they are free from any commercial bias. These are mandatory registries and therefore free of any selection bias," Dr. Moat pointed out. Furthermore, there is good standardization of definitions and long-term follow-up of mortality.
"All cardiac surgical procedures and all TAVIs in the U.K. are entered into national registries hosted by the National Institute for Cardiovascular Outcomes Research. The data set and databases of all of these registries are designed to be compatible and comparable," he added.
Overall, compared with patients undergoing surgery, patients undergoing TAVI were on average older and had a higher risk profile in terms of cardiovascular measures and comorbidities, although there was substantial overlap.
The median postoperative length of stay was 8 days after conventional surgery and 7 days after TAVI. "Despite the TAVI patients being older and at increased risk, there was no difference in postoperative length of stay. If anything, it was marginally lower in the TAVI group," Dr. Moat commented. The distribution of length of stay was also much the same. "You see a substantial numbers of these elderly, frail, and high-risk patients [in the TAVI group] being discharged before day 6," he added.
Actuarial analyses in the study population overall showed poorer survival after TAVI than after conventional surgery (whether AVR alone or combined with CABG), both in the first year and longer term. However, the gaps between curves were smaller among patients aged 80 years or older.
Among the patients undergoing TAVI, longer-term survival after aortic valve intervention did not differ according to the number of diseased vessels treated.
"An interesting observation worthy of further study is that we are well aware that patients having combined AVR and CABG have worse earlier and late survival than patients having isolated AVR. But it would seem that the presence of concomitant coronary artery disease – despite much of it being left untreated – did not affect early or late survival following TAVI," Dr. Moat commented.
The EuroSCORE was a poor predictor of mortality after both conventional surgery and TAVI, but the EuroSCORE II performed fairly well after conventional surgery, whether isolated AVR (observed:expected ratio, 0.87; area under the curve, 0.78) or AVR plus CABG (observed:expected ratio, 1.0; area under the curve, 0.73).
Dr. Moat disclosed that he is on the speakers bureau for, and receives honoraria from, Abbott Laboratories, and sits on the consultant/advisory board of Medtronic.
AT THE STS ANNUAL MEETING
Major Finding: There was a 32% increase in aortic valve interventions, driven in large part by an increase among patients aged 80 years or older.
Data Source: An analysis of pooled data from two U.K. population-based registries and 37,020 patients undergoing aortic valve interventions between 2006 and 2010.
Disclosures: Dr. Moat disclosed that he is on the speakers bureau for, and receives honoraria from, Abbott Laboratories, and sits on the consultant/advisory board of Medtronic.