User login
Catherine Cooper Nellist is editor of Pediatric News and Ob. Gyn. News. She has more than 30 years of experience reporting, writing, and editing stories about clinical medicine and the U.S. health care industry. Prior to taking the helm of these award-winning publications, Catherine covered major medical research meetings throughout the United States and Canada, and had been editor of Clinical Psychiatry News, and Dermatology News. She joined the company in 1984 after graduating magna cum laude from Dickinson College, Carlisle, Pa., with a BA in English.
Same-day consult, tympanostomy tube surgery improve efficiency of care
ATLANTA – Same-day surgery for children with otitis media who need tympanostomy tubes appears to improve access and efficiency of care, according to results of a small study presented at the annual meeting of the National Association of Pediatric Nurse Practitioners.
The Same-day Surgery Program allows consultation for tympanostomy tube placement and surgery to be completed in one extended appointment after referral from a primary care provider, said Allison Rose, a certified nurse practitioner at the Ann & Robert H. Lurie Children’s Hospital of Chicago.
In a retrospective, matched series of 30 children with a median age of 16 months enrolled in the program and 30 controls with a median age of 18 months, children in the same-day program had significantly shorter total overall clinical visit and surgical encounter time (151 minutes [135-169 minutes]), compared with controls (196 minutes [169-234 minutes]). The average number of days from scheduling the primary care office visit to surgery was 7 (4-11 days) for the same-day surgery patients and 14 (6-21 days) for controls. Eight patients in each group were enrolled in Medicaid, and 22 had private insurance or managed care.
Parents also cited multiple advantages of the program, including less missed work, less missed school/day care, quicker resolution of the medical problem, ease for the toddler, and appointment availability. Disadvantages mentioned were unclear expectations for the day of surgery and longer appointment duration.
The investigators remarked that according to one study, nearly 7% of children have tympanostomy tubes by the age of 3 years, and going to day care doubles the risk. They also emphasized that children in rural areas or those who are underinsured may have problems obtaining access to care for such surgical treatment when it is indicated – delaying treatment and putting them at risk for complications of otitis media.
“Lurie Children’s Hospital’s Same-day Surgery Program for children in need of tympanostomy tubes rethinks the referral, evaluation, and treatment process of a low-risk procedure for a common problem,” Ms. Rose said in a later interview. “This program can streamline subspecialty access to care with high family satisfaction.”
The authors said they had no relevant financial disclosures.
ATLANTA – Same-day surgery for children with otitis media who need tympanostomy tubes appears to improve access and efficiency of care, according to results of a small study presented at the annual meeting of the National Association of Pediatric Nurse Practitioners.
The Same-day Surgery Program allows consultation for tympanostomy tube placement and surgery to be completed in one extended appointment after referral from a primary care provider, said Allison Rose, a certified nurse practitioner at the Ann & Robert H. Lurie Children’s Hospital of Chicago.
In a retrospective, matched series of 30 children with a median age of 16 months enrolled in the program and 30 controls with a median age of 18 months, children in the same-day program had significantly shorter total overall clinical visit and surgical encounter time (151 minutes [135-169 minutes]), compared with controls (196 minutes [169-234 minutes]). The average number of days from scheduling the primary care office visit to surgery was 7 (4-11 days) for the same-day surgery patients and 14 (6-21 days) for controls. Eight patients in each group were enrolled in Medicaid, and 22 had private insurance or managed care.
Parents also cited multiple advantages of the program, including less missed work, less missed school/day care, quicker resolution of the medical problem, ease for the toddler, and appointment availability. Disadvantages mentioned were unclear expectations for the day of surgery and longer appointment duration.
The investigators remarked that according to one study, nearly 7% of children have tympanostomy tubes by the age of 3 years, and going to day care doubles the risk. They also emphasized that children in rural areas or those who are underinsured may have problems obtaining access to care for such surgical treatment when it is indicated – delaying treatment and putting them at risk for complications of otitis media.
“Lurie Children’s Hospital’s Same-day Surgery Program for children in need of tympanostomy tubes rethinks the referral, evaluation, and treatment process of a low-risk procedure for a common problem,” Ms. Rose said in a later interview. “This program can streamline subspecialty access to care with high family satisfaction.”
The authors said they had no relevant financial disclosures.
ATLANTA – Same-day surgery for children with otitis media who need tympanostomy tubes appears to improve access and efficiency of care, according to results of a small study presented at the annual meeting of the National Association of Pediatric Nurse Practitioners.
The Same-day Surgery Program allows consultation for tympanostomy tube placement and surgery to be completed in one extended appointment after referral from a primary care provider, said Allison Rose, a certified nurse practitioner at the Ann & Robert H. Lurie Children’s Hospital of Chicago.
In a retrospective, matched series of 30 children with a median age of 16 months enrolled in the program and 30 controls with a median age of 18 months, children in the same-day program had significantly shorter total overall clinical visit and surgical encounter time (151 minutes [135-169 minutes]), compared with controls (196 minutes [169-234 minutes]). The average number of days from scheduling the primary care office visit to surgery was 7 (4-11 days) for the same-day surgery patients and 14 (6-21 days) for controls. Eight patients in each group were enrolled in Medicaid, and 22 had private insurance or managed care.
Parents also cited multiple advantages of the program, including less missed work, less missed school/day care, quicker resolution of the medical problem, ease for the toddler, and appointment availability. Disadvantages mentioned were unclear expectations for the day of surgery and longer appointment duration.
The investigators remarked that according to one study, nearly 7% of children have tympanostomy tubes by the age of 3 years, and going to day care doubles the risk. They also emphasized that children in rural areas or those who are underinsured may have problems obtaining access to care for such surgical treatment when it is indicated – delaying treatment and putting them at risk for complications of otitis media.
“Lurie Children’s Hospital’s Same-day Surgery Program for children in need of tympanostomy tubes rethinks the referral, evaluation, and treatment process of a low-risk procedure for a common problem,” Ms. Rose said in a later interview. “This program can streamline subspecialty access to care with high family satisfaction.”
The authors said they had no relevant financial disclosures.
FROM THE NAPNAP ANNUAL MEETING
Key clinical point: A same-day surgery program allows consultation for tympanostomy tube placement and surgery to be completed in one extended appointment after referral from a primary care provider.
Major finding: Children in the Same-day Surgery Program had significantly shorter total overall clinical visit and surgical encounter time (151 minutes), compared with controls (196 minutes).
Data source: Retrospective study of 30 children in the Same-day Surgery Program undergoing tympanostomy tube placement matched for age, gender, and insurance with 30 control children.
Disclosures: The authors said they had no relevant financial disclosures.
Welcome Editorial Advisory Board member Dr. Stepien
We are pleased to welcome Dr. Kathy Stepien to the Pediatric News Editorial Advisory Board. Dr. Stepien practices general pediatrics in a private practice in Juneau, Alaska.
She graduated from the University of Washington, Seattle, and completed her pediatric residency at St. Joseph’s Hospital/Marshfield Clinic in Wisconsin. She received a Master of Arts Degree in Philosophy from Colorado State University and previously worked as a physical therapist for many years before studying medicine.
Dr. Stepien is board certified in pediatrics and is a fellow of the American Academy of Pediatrics. Her professional interests include physician wellness, medical humanities, and education.
We are pleased to welcome Dr. Kathy Stepien to the Pediatric News Editorial Advisory Board. Dr. Stepien practices general pediatrics in a private practice in Juneau, Alaska.
She graduated from the University of Washington, Seattle, and completed her pediatric residency at St. Joseph’s Hospital/Marshfield Clinic in Wisconsin. She received a Master of Arts Degree in Philosophy from Colorado State University and previously worked as a physical therapist for many years before studying medicine.
Dr. Stepien is board certified in pediatrics and is a fellow of the American Academy of Pediatrics. Her professional interests include physician wellness, medical humanities, and education.
We are pleased to welcome Dr. Kathy Stepien to the Pediatric News Editorial Advisory Board. Dr. Stepien practices general pediatrics in a private practice in Juneau, Alaska.
She graduated from the University of Washington, Seattle, and completed her pediatric residency at St. Joseph’s Hospital/Marshfield Clinic in Wisconsin. She received a Master of Arts Degree in Philosophy from Colorado State University and previously worked as a physical therapist for many years before studying medicine.
Dr. Stepien is board certified in pediatrics and is a fellow of the American Academy of Pediatrics. Her professional interests include physician wellness, medical humanities, and education.
Young Women Who Tan Indoors Are at Two- to Sixfold Increased Risk for Melanoma
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.
Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
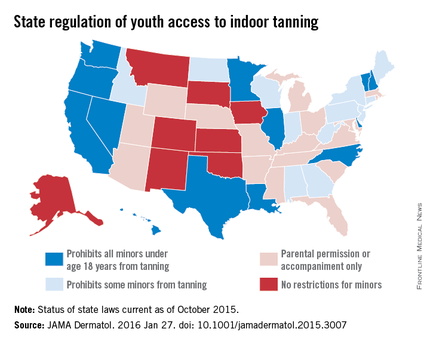
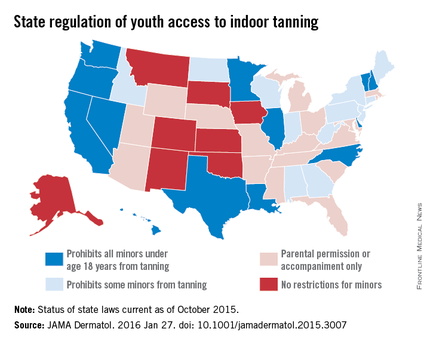
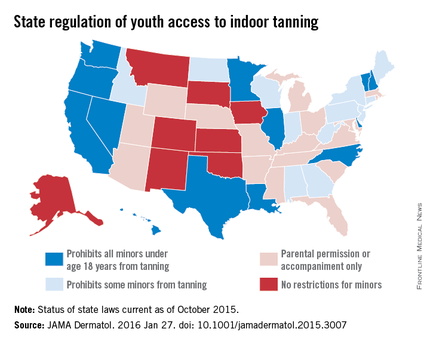
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.
Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.
Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
FROM JAMA DERMATOLOGY
Young women who tan indoors are at two- to sixfold increased risk of melanoma
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.

Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
In an accompanying editorial, the authors pointed out that the study found that “nearly all women in the study (96.8%) diagnosed with melanoma [while] younger than 30 years had engaged in indoor tanning, all initiating indoor tanning before age 25, and nearly all (90.5%) engaging in frequent indoor tanning,” and that the results build “on the previous literature and demonstrates the importance of public health efforts in reducing indoor tanning.”
By June 2015, “42 states had laws addressing youth access: 13 states restricted indoor tanning among minors (less than 18 years), 12 states prohibited minors at a younger age (e.g., 14-17 years), and 17 states required parents to give permission or to accompany minors while indoor tanning,” which have had some effect, they wrote.
“Indoor tanning among female high school students decreased from 25.4% in 2009 to 20.2% in 2013. Declines have also been noted among adults, with national rates decreasing from 8.6% to 6.5% among women and from 2.2% to 1.7% among men between 2010 and 2013. Despite these reductions, an estimated 11.3 million Americans continue to engage in indoor tanning each year, [more than] 85% (9.7 million) of whom are adults.”
Areas of concerns, however, are indoor tanning facilities available at college and university campuses, direct sale of indoor tanning devices to the public “and their use in unsupervised settings,” and deceptive advertising practices by the indoor tanning industry, they added.
These comments were excerpted from an editorial by Gery P. Guy Jr., Ph.D., of the division of cancer prevention and control, Centers for Disease Control and Prevention, and his associates (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermatol.2015.3007). The authors said they had no conflicts of interest.
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.

Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
Women under age 50 years who regularly tanned indoors were at a twofold to sixfold increased risk of melanoma, compared with age-matched women who had not engaged in indoor tanning, according to a population-based control study.
The 681 individuals with melanoma, drawn from the Skin Health Study, a population-based case-control study evaluating the indoor tanning and the risk of melanoma, conducted in Minnesota, were diagnosed during 2004-2007. Of these, 68% were women; of the 654 controls, 68% were women. For the women younger than 30 years who had ever tanned indoors, compared with controls, the crude odds ratio of developing melanoma was 6.0; for women aged 30-39 years, the adjusted odds ratio was 3.5; and for women aged 40-49 years, the adjusted odds ratio was 2.3.
Indoor tanning was most common in 95% of women in the case group who were younger than 40 years, compared with 81% of controls of the same age (P less than .001), although “The median hours of routine and recreational sun exposure were fairly similar among females in both groups.” Women younger than age 40 years at diagnosis or reference age started tanning indoors at a median age of 16 years, compared with 25 years among women aged 40 years and older (P less than .001). The results were reported on line on Jan. 27 (JAMA Dermatol. 2016 Jan 27. doi: 10.1001/jamadermaool.2015.2938).
“Given the substantial proportion of young women today who began indoor tanning as adolescents, this result is particularly concerning because their risk of developing melanoma in the future may be very high,” said DeAnn Lazovich, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
Nearly all women who developed melanoma who were younger than 30 at diagnosis reported tanning indoors more than 10 times. In the older age groups (30-50 years), women were nearly three to four times more likely to develop melanoma if they reported tanning indoors more than 10 times. The strongest association between use of indoor tanning and melanoma was observed among women who developed melanoma on their trunk, with an odds ratio of 3.7.
In men, the strength of the association between indoor tanning and melanoma was variable. This was likely because of the small sample size for some age groups, Dr. Lazovich and her associates said. There was no clear pattern between the age at initiation of indoor tanning or a dose response in relation to development of melanoma in men depending on their age at diagnosis.

Melanoma rates generally are higher in women than in men until about age 50 years, but rates have been increasing in both younger men and women. In 1995, the rising rates seemed to diverge by sex, but in 2006, the incidence of melanoma started to increase more steeply in younger women than men, according to some sources.
This current analysis “provides evidence that indoor tanning is likely driver of diverging trends in men and women younger than 50 years in the United States,” the authors wrote.
The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
FROM JAMA DERMATOLOGY
Key clinical point: Women under 50 years who regularly tan indoors are at a twofold to sixfold increased risk of melanoma, compared with women the same age who don’t tan indoors.
Major finding: For the women younger than 30 years who had ever tanned indoors, compared with controls, the adjusted odds ratio of developing melanoma was 6.0; for women aged 30-39 years, it was 3.5; and for women 40-49, it was 2.3.
Data source: Drawn from the Skin Health Study, 681 melanoma patients were age- and gender-matched with 654 controls.
Disclosures: The study was supported by National Institutes of Health grants. No conflicts of interest were reported.
Meningococcal B vaccine added to 2016 immunization schedule
The new 2016 recommended immunization schedule for children and adolescents reflects the addition of meningococcal B vaccine and various other changes.
Each year, a new immunization schedule is approved and published by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices, and the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Obstetricians and Gynecologists.
The addition of meningococcal B vaccine is shown by a blue bar indicating vaccination at 10 years for children at increased risk. Non–high-risk persons aged 16-18 years may be considered for vaccination, as indicated by a purple bar. The footnotes indicate that the two MenB vaccines “are not interchangeable; the same vaccine product must be used for all doses.” Also, Bexsero requires a two-dose series administered at least 1 month apart. Trumenba requires a three-dose series, with the second dose at least 2 months after the first and the third dose at least 6 months after the first.
Trumenba (Wyeth Pharmaceuticals) was licensed by the Food and Drug Administration in October 2014 and Bexsero (Novartis) was licensed in January 2015.
The human papillomavirus (HPV) vaccine is now referred to as 9vHPV, to reflect the availability of Merck’s Gardasil 9, which was licensed in December 2014 to replace the prior 4-valent version. A purple bar has been added to the HPV row for ages 9-10 years to indicate that children with a history of sexual abuse are at increased risk of HPV infection and should be vaccinated.
Other changes to the 2016 schedule and footnotes include:
• A change in the order of the vaccines to group vaccines according to the recommended ages of administration, as well as to the order of the footnotes
• The addition of a purple bar for Haemophilus influenzae type b (Hib) vaccine for children aged 5-18 years; this reflects a recommendation to vaccinate certain high-risk children in this age group who have not been immunized.
• A revision to the footnote for the hepatitis B vaccine to clarify the timing as well as the new CDC-recommended interval for postvaccination serologic testing of infants born to hepatitis B surface antigen (HBsAg)-positive mothers.
• A revision to the footnote for the DTaP vaccine to clarify recommendations to be taken after an inadvertently early administration of the fourth dose of that vaccine.
• An update to the footnote for the inactivated polio vaccine offering guidance on the vaccination of children who have received all doses of oral-only polio vaccine before age 4 years.
To see the immunization schedule, go to www.cdc.gov/vaccines.
The new 2016 recommended immunization schedule for children and adolescents reflects the addition of meningococcal B vaccine and various other changes.
Each year, a new immunization schedule is approved and published by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices, and the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Obstetricians and Gynecologists.
The addition of meningococcal B vaccine is shown by a blue bar indicating vaccination at 10 years for children at increased risk. Non–high-risk persons aged 16-18 years may be considered for vaccination, as indicated by a purple bar. The footnotes indicate that the two MenB vaccines “are not interchangeable; the same vaccine product must be used for all doses.” Also, Bexsero requires a two-dose series administered at least 1 month apart. Trumenba requires a three-dose series, with the second dose at least 2 months after the first and the third dose at least 6 months after the first.
Trumenba (Wyeth Pharmaceuticals) was licensed by the Food and Drug Administration in October 2014 and Bexsero (Novartis) was licensed in January 2015.
The human papillomavirus (HPV) vaccine is now referred to as 9vHPV, to reflect the availability of Merck’s Gardasil 9, which was licensed in December 2014 to replace the prior 4-valent version. A purple bar has been added to the HPV row for ages 9-10 years to indicate that children with a history of sexual abuse are at increased risk of HPV infection and should be vaccinated.
Other changes to the 2016 schedule and footnotes include:
• A change in the order of the vaccines to group vaccines according to the recommended ages of administration, as well as to the order of the footnotes
• The addition of a purple bar for Haemophilus influenzae type b (Hib) vaccine for children aged 5-18 years; this reflects a recommendation to vaccinate certain high-risk children in this age group who have not been immunized.
• A revision to the footnote for the hepatitis B vaccine to clarify the timing as well as the new CDC-recommended interval for postvaccination serologic testing of infants born to hepatitis B surface antigen (HBsAg)-positive mothers.
• A revision to the footnote for the DTaP vaccine to clarify recommendations to be taken after an inadvertently early administration of the fourth dose of that vaccine.
• An update to the footnote for the inactivated polio vaccine offering guidance on the vaccination of children who have received all doses of oral-only polio vaccine before age 4 years.
To see the immunization schedule, go to www.cdc.gov/vaccines.
The new 2016 recommended immunization schedule for children and adolescents reflects the addition of meningococcal B vaccine and various other changes.
Each year, a new immunization schedule is approved and published by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices, and the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Obstetricians and Gynecologists.
The addition of meningococcal B vaccine is shown by a blue bar indicating vaccination at 10 years for children at increased risk. Non–high-risk persons aged 16-18 years may be considered for vaccination, as indicated by a purple bar. The footnotes indicate that the two MenB vaccines “are not interchangeable; the same vaccine product must be used for all doses.” Also, Bexsero requires a two-dose series administered at least 1 month apart. Trumenba requires a three-dose series, with the second dose at least 2 months after the first and the third dose at least 6 months after the first.
Trumenba (Wyeth Pharmaceuticals) was licensed by the Food and Drug Administration in October 2014 and Bexsero (Novartis) was licensed in January 2015.
The human papillomavirus (HPV) vaccine is now referred to as 9vHPV, to reflect the availability of Merck’s Gardasil 9, which was licensed in December 2014 to replace the prior 4-valent version. A purple bar has been added to the HPV row for ages 9-10 years to indicate that children with a history of sexual abuse are at increased risk of HPV infection and should be vaccinated.
Other changes to the 2016 schedule and footnotes include:
• A change in the order of the vaccines to group vaccines according to the recommended ages of administration, as well as to the order of the footnotes
• The addition of a purple bar for Haemophilus influenzae type b (Hib) vaccine for children aged 5-18 years; this reflects a recommendation to vaccinate certain high-risk children in this age group who have not been immunized.
• A revision to the footnote for the hepatitis B vaccine to clarify the timing as well as the new CDC-recommended interval for postvaccination serologic testing of infants born to hepatitis B surface antigen (HBsAg)-positive mothers.
• A revision to the footnote for the DTaP vaccine to clarify recommendations to be taken after an inadvertently early administration of the fourth dose of that vaccine.
• An update to the footnote for the inactivated polio vaccine offering guidance on the vaccination of children who have received all doses of oral-only polio vaccine before age 4 years.
To see the immunization schedule, go to www.cdc.gov/vaccines.
Consider reimmunizing with MMR after HIV-infected children undergo antiretroviral treatment
Reimmunization with a single dose of MMR in children with HIV who have undergone antiretroviral therapy in most cases leads to seroconversion to the measles component, Dr. Anju Seth, professor of pediatrics at Lady Hardinge Medical College, New Delhi, and her associates found.
HIV-infected children don’t respond well to primary immunization with measles, mumps and rubella (MMR) vaccine, and those who do respond tend to lose a protective titer of measles antibodies by age 2-3 years. Revaccinating these children after they undergo antiretroviral therapy (ART) might result in good seroconversion, so Dr. Seth and her associates enrolled 66 children with HIV aged 5-18 years who had undergone antiretroviral therapy for a mean 3.4 years whose mean CD4 count was 716 mcg/L.
At enrollment, 16 children tested positive for measles antibodies, 8 were equivocal, and 42 tested negative. Testing 8-12 weeks after reimmmunization with a single dose of MMR, 62 tested positive, 1 equivocal, and 3 tested negative. Between the seropositive and seronegative children, there was no difference in age, gender, duration of ART, CD4 count, or clinical stage. There were no serious adverse reactions to reimmunizations, the investigators reported. Read the full study at the Pediatric Infectious Disease Journal (2016 Jan;35[1]:e8-11).
Reimmunization with a single dose of MMR in children with HIV who have undergone antiretroviral therapy in most cases leads to seroconversion to the measles component, Dr. Anju Seth, professor of pediatrics at Lady Hardinge Medical College, New Delhi, and her associates found.
HIV-infected children don’t respond well to primary immunization with measles, mumps and rubella (MMR) vaccine, and those who do respond tend to lose a protective titer of measles antibodies by age 2-3 years. Revaccinating these children after they undergo antiretroviral therapy (ART) might result in good seroconversion, so Dr. Seth and her associates enrolled 66 children with HIV aged 5-18 years who had undergone antiretroviral therapy for a mean 3.4 years whose mean CD4 count was 716 mcg/L.
At enrollment, 16 children tested positive for measles antibodies, 8 were equivocal, and 42 tested negative. Testing 8-12 weeks after reimmmunization with a single dose of MMR, 62 tested positive, 1 equivocal, and 3 tested negative. Between the seropositive and seronegative children, there was no difference in age, gender, duration of ART, CD4 count, or clinical stage. There were no serious adverse reactions to reimmunizations, the investigators reported. Read the full study at the Pediatric Infectious Disease Journal (2016 Jan;35[1]:e8-11).
Reimmunization with a single dose of MMR in children with HIV who have undergone antiretroviral therapy in most cases leads to seroconversion to the measles component, Dr. Anju Seth, professor of pediatrics at Lady Hardinge Medical College, New Delhi, and her associates found.
HIV-infected children don’t respond well to primary immunization with measles, mumps and rubella (MMR) vaccine, and those who do respond tend to lose a protective titer of measles antibodies by age 2-3 years. Revaccinating these children after they undergo antiretroviral therapy (ART) might result in good seroconversion, so Dr. Seth and her associates enrolled 66 children with HIV aged 5-18 years who had undergone antiretroviral therapy for a mean 3.4 years whose mean CD4 count was 716 mcg/L.
At enrollment, 16 children tested positive for measles antibodies, 8 were equivocal, and 42 tested negative. Testing 8-12 weeks after reimmmunization with a single dose of MMR, 62 tested positive, 1 equivocal, and 3 tested negative. Between the seropositive and seronegative children, there was no difference in age, gender, duration of ART, CD4 count, or clinical stage. There were no serious adverse reactions to reimmunizations, the investigators reported. Read the full study at the Pediatric Infectious Disease Journal (2016 Jan;35[1]:e8-11).
VIDEO: Transforming pediatric education to deal with mental health issues
WASHINGTON – Behavioral and mental health issues are the largest group of conditions that you see in your practice, but pediatric residency training does not adequately prepare you for this challenge, Dr. Julia A. McMillan said in a video roundtable at the annual meeting of the American Academy of Pediatrics.
Dr. John D. Duby, professor and chair of pediatrics at Wright State University, Dayton, Ohio, added, “as we think about the innovation and transformation in pediatric education, pediatricians alone can’t do this work. We need to think more about integrated models for training that bring in psychologists, licensed social workers, care coordinators, community health workers, maybe even child psychiatrists.”
Dr. McMillan, professor of pediatrics and associate dean for graduate medical education at the Johns Hopkins University, Baltimore, agreed, and said that training about behavioral and mental health issues needs to be reinforced throughout pediatric residency training, not just in a block rotation about mental health, but also during critical care or continuity clinic training.
Dr. Duby emphasized that although there are roadblocks to preparing pediatricians of the future to deal with children confronted with trauma or the most common mental health issues – attention-deficit/hyperactivity disorder, anxiety, depression, or disruptive behavior – the difficulty of handling these disorders in the pediatric medical home is not insurmountable. This really requires only about 10 skills, simple strategies that pediatricians can learn. One of these is assessing a patient’s readiness to change.
Dr. Michelle M. Macias, a professor of pediatrics and director of the division of developmental-behavioral pediatrics at the Medical University of South Carolina, Charleston, who also took part in the roundtable, added it is important to emphasize strength-based approaches, positive parenting, and preventive medicine to deal with behavioral and mental health issues in children.
For those already in practice, there also is help from the AAP. Dr. McMillan mentioned a 2009 article in Pediatrics (2009;124:410-21) written by the AAP Task Force on Mental Health and an online curriculum to aid residency continuity clinic preceptors in training residents to help children in their care with mental health issues.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Behavioral and mental health issues are the largest group of conditions that you see in your practice, but pediatric residency training does not adequately prepare you for this challenge, Dr. Julia A. McMillan said in a video roundtable at the annual meeting of the American Academy of Pediatrics.
Dr. John D. Duby, professor and chair of pediatrics at Wright State University, Dayton, Ohio, added, “as we think about the innovation and transformation in pediatric education, pediatricians alone can’t do this work. We need to think more about integrated models for training that bring in psychologists, licensed social workers, care coordinators, community health workers, maybe even child psychiatrists.”
Dr. McMillan, professor of pediatrics and associate dean for graduate medical education at the Johns Hopkins University, Baltimore, agreed, and said that training about behavioral and mental health issues needs to be reinforced throughout pediatric residency training, not just in a block rotation about mental health, but also during critical care or continuity clinic training.
Dr. Duby emphasized that although there are roadblocks to preparing pediatricians of the future to deal with children confronted with trauma or the most common mental health issues – attention-deficit/hyperactivity disorder, anxiety, depression, or disruptive behavior – the difficulty of handling these disorders in the pediatric medical home is not insurmountable. This really requires only about 10 skills, simple strategies that pediatricians can learn. One of these is assessing a patient’s readiness to change.
Dr. Michelle M. Macias, a professor of pediatrics and director of the division of developmental-behavioral pediatrics at the Medical University of South Carolina, Charleston, who also took part in the roundtable, added it is important to emphasize strength-based approaches, positive parenting, and preventive medicine to deal with behavioral and mental health issues in children.
For those already in practice, there also is help from the AAP. Dr. McMillan mentioned a 2009 article in Pediatrics (2009;124:410-21) written by the AAP Task Force on Mental Health and an online curriculum to aid residency continuity clinic preceptors in training residents to help children in their care with mental health issues.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Behavioral and mental health issues are the largest group of conditions that you see in your practice, but pediatric residency training does not adequately prepare you for this challenge, Dr. Julia A. McMillan said in a video roundtable at the annual meeting of the American Academy of Pediatrics.
Dr. John D. Duby, professor and chair of pediatrics at Wright State University, Dayton, Ohio, added, “as we think about the innovation and transformation in pediatric education, pediatricians alone can’t do this work. We need to think more about integrated models for training that bring in psychologists, licensed social workers, care coordinators, community health workers, maybe even child psychiatrists.”
Dr. McMillan, professor of pediatrics and associate dean for graduate medical education at the Johns Hopkins University, Baltimore, agreed, and said that training about behavioral and mental health issues needs to be reinforced throughout pediatric residency training, not just in a block rotation about mental health, but also during critical care or continuity clinic training.
Dr. Duby emphasized that although there are roadblocks to preparing pediatricians of the future to deal with children confronted with trauma or the most common mental health issues – attention-deficit/hyperactivity disorder, anxiety, depression, or disruptive behavior – the difficulty of handling these disorders in the pediatric medical home is not insurmountable. This really requires only about 10 skills, simple strategies that pediatricians can learn. One of these is assessing a patient’s readiness to change.
Dr. Michelle M. Macias, a professor of pediatrics and director of the division of developmental-behavioral pediatrics at the Medical University of South Carolina, Charleston, who also took part in the roundtable, added it is important to emphasize strength-based approaches, positive parenting, and preventive medicine to deal with behavioral and mental health issues in children.
For those already in practice, there also is help from the AAP. Dr. McMillan mentioned a 2009 article in Pediatrics (2009;124:410-21) written by the AAP Task Force on Mental Health and an online curriculum to aid residency continuity clinic preceptors in training residents to help children in their care with mental health issues.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Video roundtable - Next steps in quality improvement, part 2
WASHINGTON – Four experts explain what COQIPS, VIP, PEMCRC, and ALIIGN are all about.
These acronyms each concern pediatric quality improvement, and you can learn about them in part 2 of a video roundtable that took place at the annual meeting of the American Academy of Pediatrics.
Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the AAP Quality Improvement Innovation Networks (QUIIN), explains how Value in Inpatient Pediatrics (VIP) quality collaboratives involving a number of hospitals take guidelines that impact patient care, such as bronchiolitis, and create quality measures and toolkits, and try to implement what the guidelines are recommending. There also is an outpatient arm involving pediatric practices.
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore, New York, and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), described how COQIPS will serve as a clearinghouse for toolkits so pediatricians “don’t have to reinvent the wheel” when they want to do quality improvement projects. He emphasized that these toolkits are a quality improvement project-in-a-box.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, emphasized these guidelines and toolkits “apply to your patients, to the average pediatrician who wants to get involved.”
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP COQIPS, added that maintenance of certification is a perfect opportunity to do a quality improvement project, and not just that, to improve quality for your patients. Dr. Tieder is the author of the ALIIGN proposal, which is all about evaluating and implementing guidelines.
*This article was updated 11/3/2015.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Four experts explain what COQIPS, VIP, PEMCRC, and ALIIGN are all about.
These acronyms each concern pediatric quality improvement, and you can learn about them in part 2 of a video roundtable that took place at the annual meeting of the American Academy of Pediatrics.
Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the AAP Quality Improvement Innovation Networks (QUIIN), explains how Value in Inpatient Pediatrics (VIP) quality collaboratives involving a number of hospitals take guidelines that impact patient care, such as bronchiolitis, and create quality measures and toolkits, and try to implement what the guidelines are recommending. There also is an outpatient arm involving pediatric practices.
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore, New York, and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), described how COQIPS will serve as a clearinghouse for toolkits so pediatricians “don’t have to reinvent the wheel” when they want to do quality improvement projects. He emphasized that these toolkits are a quality improvement project-in-a-box.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, emphasized these guidelines and toolkits “apply to your patients, to the average pediatrician who wants to get involved.”
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP COQIPS, added that maintenance of certification is a perfect opportunity to do a quality improvement project, and not just that, to improve quality for your patients. Dr. Tieder is the author of the ALIIGN proposal, which is all about evaluating and implementing guidelines.
*This article was updated 11/3/2015.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Four experts explain what COQIPS, VIP, PEMCRC, and ALIIGN are all about.
These acronyms each concern pediatric quality improvement, and you can learn about them in part 2 of a video roundtable that took place at the annual meeting of the American Academy of Pediatrics.
Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the AAP Quality Improvement Innovation Networks (QUIIN), explains how Value in Inpatient Pediatrics (VIP) quality collaboratives involving a number of hospitals take guidelines that impact patient care, such as bronchiolitis, and create quality measures and toolkits, and try to implement what the guidelines are recommending. There also is an outpatient arm involving pediatric practices.
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore, New York, and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), described how COQIPS will serve as a clearinghouse for toolkits so pediatricians “don’t have to reinvent the wheel” when they want to do quality improvement projects. He emphasized that these toolkits are a quality improvement project-in-a-box.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, emphasized these guidelines and toolkits “apply to your patients, to the average pediatrician who wants to get involved.”
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP COQIPS, added that maintenance of certification is a perfect opportunity to do a quality improvement project, and not just that, to improve quality for your patients. Dr. Tieder is the author of the ALIIGN proposal, which is all about evaluating and implementing guidelines.
*This article was updated 11/3/2015.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Video roundtable - Next steps in quality improvement, Part 1
WASHINGTON – Experts in pediatric quality improvement convened at the annual meeting of the American Academy of Pediatrics to discuss important next steps that must occur for quality improvement to advance.
In part 1 of a video roundtable, they described how networks are being formed to spur data sharing and determination of benchmarks in a variety of pediatric conditions, such as urinary tract infections and asthma. Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the American Academy of Pediatrics Quality Improvement Innovation Networks (QUIIN), discussed how one such study on bronchiolitis guidelines enlisted the help of emergency physicians and inpatient physicians.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, questioned whether what third party payers want as benchmarks and what physicians, patients, and parents want in terms of quality of care are the same.
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP Council on Quality Improvement and Patient Safety (COQIPS), said, “With asthma, now we have a world where patient preferences matter, and they are hard to measure across this complicated health system.”
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore in New York and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), concurred.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Experts in pediatric quality improvement convened at the annual meeting of the American Academy of Pediatrics to discuss important next steps that must occur for quality improvement to advance.
In part 1 of a video roundtable, they described how networks are being formed to spur data sharing and determination of benchmarks in a variety of pediatric conditions, such as urinary tract infections and asthma. Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the American Academy of Pediatrics Quality Improvement Innovation Networks (QUIIN), discussed how one such study on bronchiolitis guidelines enlisted the help of emergency physicians and inpatient physicians.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, questioned whether what third party payers want as benchmarks and what physicians, patients, and parents want in terms of quality of care are the same.
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP Council on Quality Improvement and Patient Safety (COQIPS), said, “With asthma, now we have a world where patient preferences matter, and they are hard to measure across this complicated health system.”
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore in New York and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), concurred.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Experts in pediatric quality improvement convened at the annual meeting of the American Academy of Pediatrics to discuss important next steps that must occur for quality improvement to advance.
In part 1 of a video roundtable, they described how networks are being formed to spur data sharing and determination of benchmarks in a variety of pediatric conditions, such as urinary tract infections and asthma. Dr. Matt D. Garber, director of pediatric hospitalists and chief quality officer at Palmetto Health Children’s Hospital, Columbia, S.C., representing the American Academy of Pediatrics Quality Improvement Innovation Networks (QUIIN), discussed how one such study on bronchiolitis guidelines enlisted the help of emergency physicians and inpatient physicians.
Dr. Anupam B. Kharbanda, director of research for emergency services at Children’s Minnesota, Minneapolis, and chairman, AAP pediatric emergency medicine collaborative research committee of the section on emergency medicine, questioned whether what third party payers want as benchmarks and what physicians, patients, and parents want in terms of quality of care are the same.
Dr. Joel S. Tieder, a pediatric hospitalist and director of the maintenance of certification program at Seattle Children’s Hospital and vice-chair of the AAP Council on Quality Improvement and Patient Safety (COQIPS), said, “With asthma, now we have a world where patient preferences matter, and they are hard to measure across this complicated health system.”
Dr. Michael L. Rinke, a pediatric hospitalist who is medical director of quality at Children’s Hospital at Montefiore in New York and cochair of the implementation committee of the AAP Council on Quality Improvement and Patient Safety (COQIPS), concurred.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
Dr. Nathaniel Savio Beers joins Pediatric News board
We are pleased to welcome Dr. Nathaniel Savio Beers to the Pediatric News Editorial Advisory Board.
Dr. Beers is currently chief operating officer for the District of Columbia Public Schools and a general and developmental behavioral pediatrician at Children’s National Health System in Washington. At DCPS, he was previously the Chief of Specialized Instruction from 2011 to 2015. Previously, he was director of the Children’s Health Center, the largest provider of primary care in Washington, deputy director for the Community Health Administration in Washington, and Title V director for the D.C. Health Department.
He has served on the Washington Mayor’s Advisory Committee on Child Welfare, the Mayor’s Early Childhood Advisory Council, and the Children with Special Health Care Needs Advisory Board. Dr. Beers has served as president of the D.C. Chapter of the American Academy of Pediatrics, chair of the National AAP Committee on Membership, and chair of the AAP Section on Residents.
He is newly elected to the Council on School Health for the AAP. Dr. Beers graduated from George Washington University medical school and completed his pediatric residency at Children’s National. Dr. Beers was the Anne E. Dyson Child Advocacy Fellow at Children’s Hospital of Boston and Chief Fellow of General Pediatrics. He received a Master’s Degree of Public Administration at the Harvard Kennedy School, Boston.
We are pleased to welcome Dr. Nathaniel Savio Beers to the Pediatric News Editorial Advisory Board.
Dr. Beers is currently chief operating officer for the District of Columbia Public Schools and a general and developmental behavioral pediatrician at Children’s National Health System in Washington. At DCPS, he was previously the Chief of Specialized Instruction from 2011 to 2015. Previously, he was director of the Children’s Health Center, the largest provider of primary care in Washington, deputy director for the Community Health Administration in Washington, and Title V director for the D.C. Health Department.
He has served on the Washington Mayor’s Advisory Committee on Child Welfare, the Mayor’s Early Childhood Advisory Council, and the Children with Special Health Care Needs Advisory Board. Dr. Beers has served as president of the D.C. Chapter of the American Academy of Pediatrics, chair of the National AAP Committee on Membership, and chair of the AAP Section on Residents.
He is newly elected to the Council on School Health for the AAP. Dr. Beers graduated from George Washington University medical school and completed his pediatric residency at Children’s National. Dr. Beers was the Anne E. Dyson Child Advocacy Fellow at Children’s Hospital of Boston and Chief Fellow of General Pediatrics. He received a Master’s Degree of Public Administration at the Harvard Kennedy School, Boston.
We are pleased to welcome Dr. Nathaniel Savio Beers to the Pediatric News Editorial Advisory Board.
Dr. Beers is currently chief operating officer for the District of Columbia Public Schools and a general and developmental behavioral pediatrician at Children’s National Health System in Washington. At DCPS, he was previously the Chief of Specialized Instruction from 2011 to 2015. Previously, he was director of the Children’s Health Center, the largest provider of primary care in Washington, deputy director for the Community Health Administration in Washington, and Title V director for the D.C. Health Department.
He has served on the Washington Mayor’s Advisory Committee on Child Welfare, the Mayor’s Early Childhood Advisory Council, and the Children with Special Health Care Needs Advisory Board. Dr. Beers has served as president of the D.C. Chapter of the American Academy of Pediatrics, chair of the National AAP Committee on Membership, and chair of the AAP Section on Residents.
He is newly elected to the Council on School Health for the AAP. Dr. Beers graduated from George Washington University medical school and completed his pediatric residency at Children’s National. Dr. Beers was the Anne E. Dyson Child Advocacy Fellow at Children’s Hospital of Boston and Chief Fellow of General Pediatrics. He received a Master’s Degree of Public Administration at the Harvard Kennedy School, Boston.