User login
Catherine Cooper Nellist is editor of Pediatric News and Ob. Gyn. News. She has more than 30 years of experience reporting, writing, and editing stories about clinical medicine and the U.S. health care industry. Prior to taking the helm of these award-winning publications, Catherine covered major medical research meetings throughout the United States and Canada, and had been editor of Clinical Psychiatry News, and Dermatology News. She joined the company in 1984 after graduating magna cum laude from Dickinson College, Carlisle, Pa., with a BA in English.
Adolescents with an incarcerated parent at higher risk of mental health problems
Having or having had a parent in jail appears to be a risk factor for adolescent mental health problems, a Minnesota study found.
In a study of 122,180 children from the 8th, 9th, and 11th grades drawn from the 2013 Minnesota Student Survey, parental incarceration was strongly associated with higher rates of mental health problems such as internalizing, self-injury, suicidal ideation, and suicidal attempts. Children of currently incarcerated parents were two and a half to four times as likely to experience these mental health problems, and children of formerly incarcerated parents were roughly twice as likely to experience them, compared with children whose parents had not been jailed, said Laurel Davis, PhD, and Rebecca J. Shlafer, PhD, MPH, of the department of pediatrics at the University of Minnesota, Minneapolis.
For youth with currently incarcerated parents, almost half reported moderate symptoms of internalizing, and more than one-third reported at least one purposeful self-injury. However, only 30% reported any type of treatment for a mental health concern, the researchers said.
Parental closeness was protective against negative mental health outcomes, they noted. “Children of incarcerated parents are a vulnerable population and they should continue to be the targets of intervention efforts aiming to buttress their personal and social resources, including strong relationships with caregivers.”
Studies suggest that an estimated 1.9 million U.S. children have a parent in a state or federal prison, and millions more have a parent in county jails.
In Minnesota alone, 2,500 young people who had a parent in jail or whose parent had been in jail reported attempting suicide, and more than 5,000 children of incarcerated or formerly incarcerated parents had reported purposely having injured themselves in the last year. “This represents an enormous challenge to our systems of care,” said Dr. Davis and Dr. Shlafer. “Identifying and intervening with these youth should be a priority with governments and social service organizations.”
Read more at the Journal of Adolescence (2017;54:120-34).
Having or having had a parent in jail appears to be a risk factor for adolescent mental health problems, a Minnesota study found.
In a study of 122,180 children from the 8th, 9th, and 11th grades drawn from the 2013 Minnesota Student Survey, parental incarceration was strongly associated with higher rates of mental health problems such as internalizing, self-injury, suicidal ideation, and suicidal attempts. Children of currently incarcerated parents were two and a half to four times as likely to experience these mental health problems, and children of formerly incarcerated parents were roughly twice as likely to experience them, compared with children whose parents had not been jailed, said Laurel Davis, PhD, and Rebecca J. Shlafer, PhD, MPH, of the department of pediatrics at the University of Minnesota, Minneapolis.
For youth with currently incarcerated parents, almost half reported moderate symptoms of internalizing, and more than one-third reported at least one purposeful self-injury. However, only 30% reported any type of treatment for a mental health concern, the researchers said.
Parental closeness was protective against negative mental health outcomes, they noted. “Children of incarcerated parents are a vulnerable population and they should continue to be the targets of intervention efforts aiming to buttress their personal and social resources, including strong relationships with caregivers.”
Studies suggest that an estimated 1.9 million U.S. children have a parent in a state or federal prison, and millions more have a parent in county jails.
In Minnesota alone, 2,500 young people who had a parent in jail or whose parent had been in jail reported attempting suicide, and more than 5,000 children of incarcerated or formerly incarcerated parents had reported purposely having injured themselves in the last year. “This represents an enormous challenge to our systems of care,” said Dr. Davis and Dr. Shlafer. “Identifying and intervening with these youth should be a priority with governments and social service organizations.”
Read more at the Journal of Adolescence (2017;54:120-34).
Having or having had a parent in jail appears to be a risk factor for adolescent mental health problems, a Minnesota study found.
In a study of 122,180 children from the 8th, 9th, and 11th grades drawn from the 2013 Minnesota Student Survey, parental incarceration was strongly associated with higher rates of mental health problems such as internalizing, self-injury, suicidal ideation, and suicidal attempts. Children of currently incarcerated parents were two and a half to four times as likely to experience these mental health problems, and children of formerly incarcerated parents were roughly twice as likely to experience them, compared with children whose parents had not been jailed, said Laurel Davis, PhD, and Rebecca J. Shlafer, PhD, MPH, of the department of pediatrics at the University of Minnesota, Minneapolis.
For youth with currently incarcerated parents, almost half reported moderate symptoms of internalizing, and more than one-third reported at least one purposeful self-injury. However, only 30% reported any type of treatment for a mental health concern, the researchers said.
Parental closeness was protective against negative mental health outcomes, they noted. “Children of incarcerated parents are a vulnerable population and they should continue to be the targets of intervention efforts aiming to buttress their personal and social resources, including strong relationships with caregivers.”
Studies suggest that an estimated 1.9 million U.S. children have a parent in a state or federal prison, and millions more have a parent in county jails.
In Minnesota alone, 2,500 young people who had a parent in jail or whose parent had been in jail reported attempting suicide, and more than 5,000 children of incarcerated or formerly incarcerated parents had reported purposely having injured themselves in the last year. “This represents an enormous challenge to our systems of care,” said Dr. Davis and Dr. Shlafer. “Identifying and intervening with these youth should be a priority with governments and social service organizations.”
Read more at the Journal of Adolescence (2017;54:120-34).
FROM THE JOURNAL OF ADOLESCENCE
Picosecond alexandrite laser with lens modification effective for wrinkles
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
FROM LASERS IN SURGERY AND MEDICINE
A look back at 1967
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
Body-size awareness linked with BMI decrease in obese children, teens
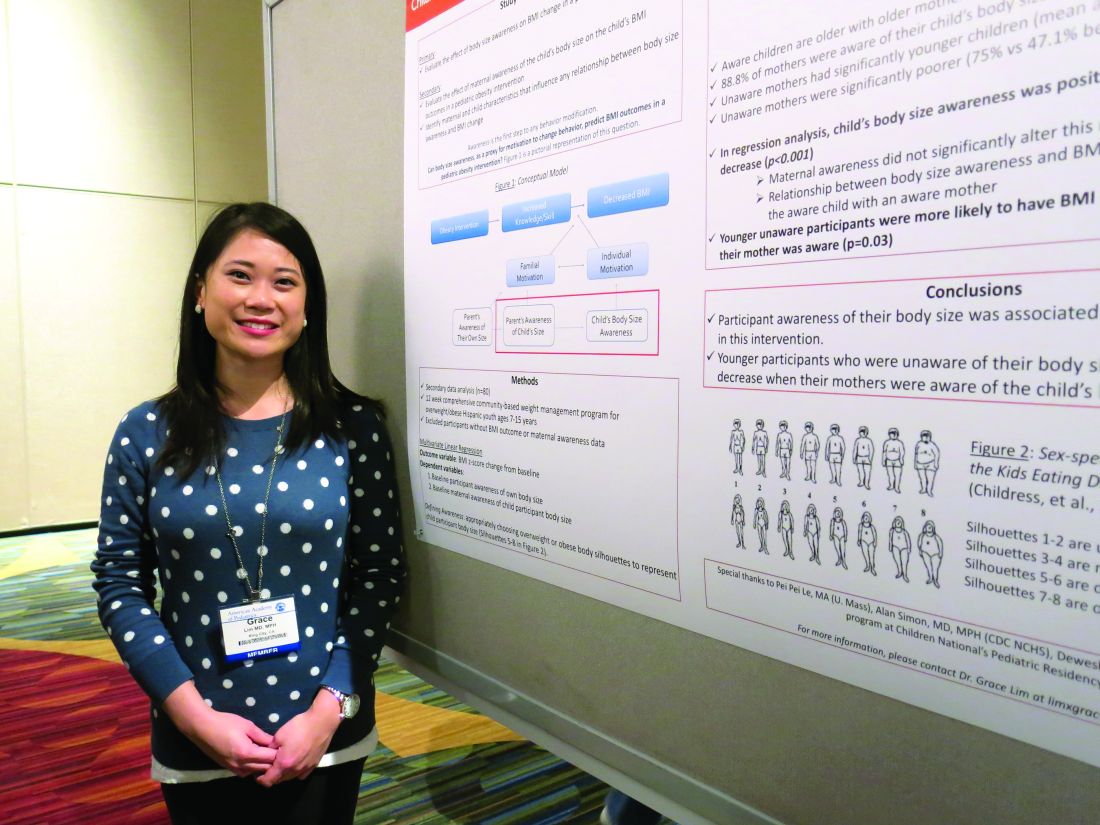
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
AT AAP 16
Key clinical point:
Major finding: 68% of 80 the children demonstrated awareness of overweight or obese body sizes and were more likely to drop their BMI.
Data source: A study of 80 overweight or obese Latino youths aged 7-15 years taking part in a 12-week, community-based weight management program.
Disclosures: Dr. Lim said she that had no relevant financial disclosures.
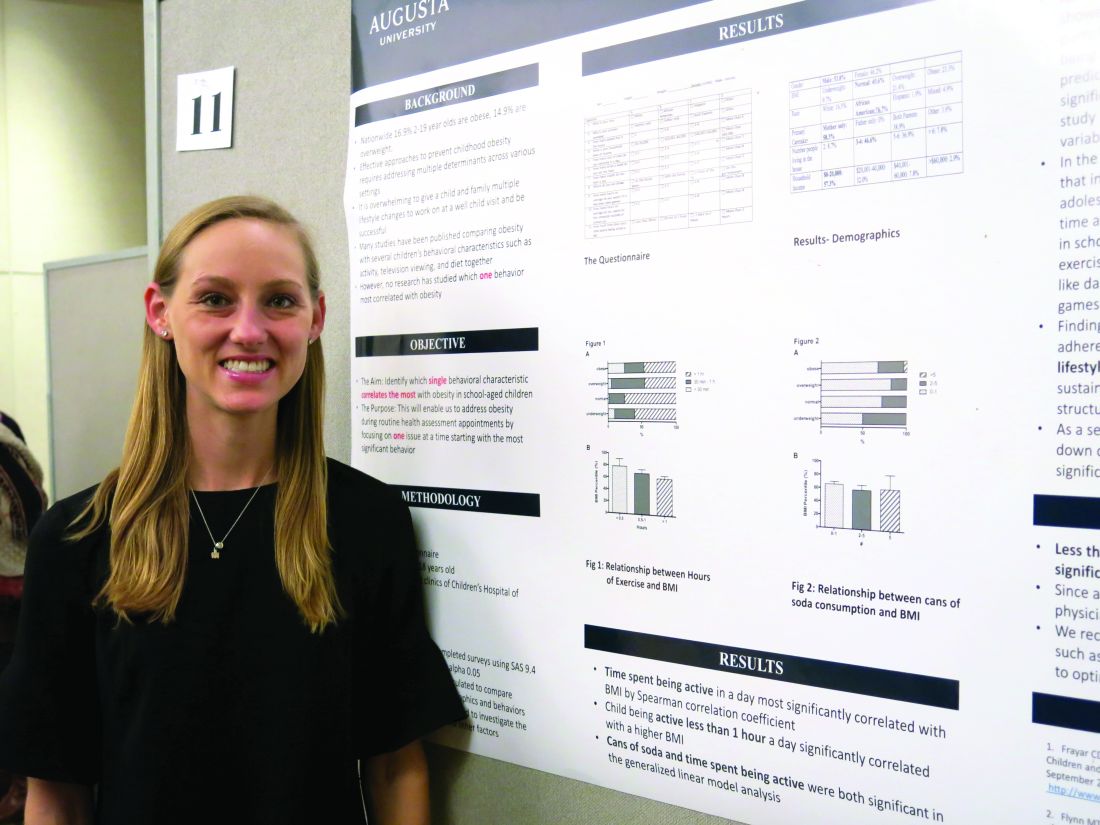
Obesity risk rises when kids aren’t active 1 hour a day
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
AT AAP 2016
Key clinical point:
Major finding: Being active less than 1 hour per day was significantly associated with a higher body mass index in children (P = .006 for 30 minutes to 1 hour, and P = .017 for less than 30 minutes).
Data source: A prospective, questionnaire-based study involving 103 children, aged 5-18 years, over a 6-month period.
Disclosures: Dr. Johnston said she had no relevant financial disclosures.
Children having an anaphylactic attack at school may not get proper treatment
Children experiencing an anaphylactic event at school may frequently encounter staff members who are not permitted to administer potentially life-saving epinephrine, according to recent survey study.
Of 6,574 surveys submitted by schools, there were 1,140 anaphylactic events reported in 736 schools.
A total of 6,088 schools provided data on staff training for recognizing anaphylaxis recognition: 30% provided training for all staff, 28% for most staff, 37% for the school nurse and select staff, and 2% for just the school nurse. Of 6,053 schools providing data on who is permitted to administer epinephrine to treat anaphylaxis, 22% permitted all staff, 16% permitted most staff, 55% permitted the school nurse and select trained staff, and 3% permitted the school nurse only, reported Martha V. White, MD, Institute for Asthma and Allergy, Wheaton, Md., and her associates (Pediatr Allerg Immunol Pulmonol. 2016. doi: 10.1089/ped.2016.0675).
These findings “suggest that there may be an opportunity to improve school staff training programs. Only 58.6% of schools surveyed trained all or most staff members to recognize the signs and symptoms of anaphylaxis. Similarly,only 37% of responding schools permitted all or most staff to administer epinephrine. ... School policies should be designed to allow for prompt administration of epinephrine during the early stages of an anaphylactic attack,” Dr. White and her associates concluded.
Among students having events for whom grade information was available, 33% occurred in elementary school students, 19% occurred in middle school students, and 45% occurred in high school students. In 1,049 anaphylactic events, the allergy history was known: 68% of events occurred in students with known allergies and 25% were in students with no known allergies.
When triggers were identified (in 78% of cases), food was the most common trigger, occurring in 60%, followed by insect bites or stings in 8%; environmental, medication, or health related triggers in 9%; and latex in 1%.
Data on use of epinephrine autoinjectors (EAIs) was available in 1,059 cases. EAIs were administered in 76% of anaphylactic events, were not administered in 23% cases, and it was unknown whether EAIs were given in the remaining 1%.
This study was supported by Mylan Specialty. Dr. White has served as a consultant for Mylan and Merck, and has received grants, fees, or support from numerous pharmaceutical companies. Christopher Herrem, PhD, is a paid employee of Mylan and may hold stock within the company. The remaining authors reported that they had no conflicts of interest.
Children experiencing an anaphylactic event at school may frequently encounter staff members who are not permitted to administer potentially life-saving epinephrine, according to recent survey study.
Of 6,574 surveys submitted by schools, there were 1,140 anaphylactic events reported in 736 schools.
A total of 6,088 schools provided data on staff training for recognizing anaphylaxis recognition: 30% provided training for all staff, 28% for most staff, 37% for the school nurse and select staff, and 2% for just the school nurse. Of 6,053 schools providing data on who is permitted to administer epinephrine to treat anaphylaxis, 22% permitted all staff, 16% permitted most staff, 55% permitted the school nurse and select trained staff, and 3% permitted the school nurse only, reported Martha V. White, MD, Institute for Asthma and Allergy, Wheaton, Md., and her associates (Pediatr Allerg Immunol Pulmonol. 2016. doi: 10.1089/ped.2016.0675).
These findings “suggest that there may be an opportunity to improve school staff training programs. Only 58.6% of schools surveyed trained all or most staff members to recognize the signs and symptoms of anaphylaxis. Similarly,only 37% of responding schools permitted all or most staff to administer epinephrine. ... School policies should be designed to allow for prompt administration of epinephrine during the early stages of an anaphylactic attack,” Dr. White and her associates concluded.
Among students having events for whom grade information was available, 33% occurred in elementary school students, 19% occurred in middle school students, and 45% occurred in high school students. In 1,049 anaphylactic events, the allergy history was known: 68% of events occurred in students with known allergies and 25% were in students with no known allergies.
When triggers were identified (in 78% of cases), food was the most common trigger, occurring in 60%, followed by insect bites or stings in 8%; environmental, medication, or health related triggers in 9%; and latex in 1%.
Data on use of epinephrine autoinjectors (EAIs) was available in 1,059 cases. EAIs were administered in 76% of anaphylactic events, were not administered in 23% cases, and it was unknown whether EAIs were given in the remaining 1%.
This study was supported by Mylan Specialty. Dr. White has served as a consultant for Mylan and Merck, and has received grants, fees, or support from numerous pharmaceutical companies. Christopher Herrem, PhD, is a paid employee of Mylan and may hold stock within the company. The remaining authors reported that they had no conflicts of interest.
Children experiencing an anaphylactic event at school may frequently encounter staff members who are not permitted to administer potentially life-saving epinephrine, according to recent survey study.
Of 6,574 surveys submitted by schools, there were 1,140 anaphylactic events reported in 736 schools.
A total of 6,088 schools provided data on staff training for recognizing anaphylaxis recognition: 30% provided training for all staff, 28% for most staff, 37% for the school nurse and select staff, and 2% for just the school nurse. Of 6,053 schools providing data on who is permitted to administer epinephrine to treat anaphylaxis, 22% permitted all staff, 16% permitted most staff, 55% permitted the school nurse and select trained staff, and 3% permitted the school nurse only, reported Martha V. White, MD, Institute for Asthma and Allergy, Wheaton, Md., and her associates (Pediatr Allerg Immunol Pulmonol. 2016. doi: 10.1089/ped.2016.0675).
These findings “suggest that there may be an opportunity to improve school staff training programs. Only 58.6% of schools surveyed trained all or most staff members to recognize the signs and symptoms of anaphylaxis. Similarly,only 37% of responding schools permitted all or most staff to administer epinephrine. ... School policies should be designed to allow for prompt administration of epinephrine during the early stages of an anaphylactic attack,” Dr. White and her associates concluded.
Among students having events for whom grade information was available, 33% occurred in elementary school students, 19% occurred in middle school students, and 45% occurred in high school students. In 1,049 anaphylactic events, the allergy history was known: 68% of events occurred in students with known allergies and 25% were in students with no known allergies.
When triggers were identified (in 78% of cases), food was the most common trigger, occurring in 60%, followed by insect bites or stings in 8%; environmental, medication, or health related triggers in 9%; and latex in 1%.
Data on use of epinephrine autoinjectors (EAIs) was available in 1,059 cases. EAIs were administered in 76% of anaphylactic events, were not administered in 23% cases, and it was unknown whether EAIs were given in the remaining 1%.
This study was supported by Mylan Specialty. Dr. White has served as a consultant for Mylan and Merck, and has received grants, fees, or support from numerous pharmaceutical companies. Christopher Herrem, PhD, is a paid employee of Mylan and may hold stock within the company. The remaining authors reported that they had no conflicts of interest.
FROM PEDIATRIC ALLERGY, IMMUNOLOGY, AND PULMONOLOGY
Key clinical point: School staff members are often not allowed to administer potentially life-saving epinephrine to children having an anaphylactic event.
Major finding: Of 6,053 schools providing data on who is permitted to administer epinephrine to treat anaphylaxis, 22% permitted all staff, 16% permitted most staff, 55% permitted the school nurse and select trained staff, and 3% permitted the school nurse only.
Data source: A survey of 6,574 schools.
Disclosures: This study was supported by Mylan Specialty. Dr. White has served as a consultant for Mylan and Merck and has received grants, fees, or support from numerous pharmaceutical companies. Christopher Herrem, PhD, is a paid employee of Mylan and may hold stock within the company. The remaining authors reported having no conflicts of interest.
New members welcomed to Consultant Board
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
Bill in Calif. seeks to ameliorate problem of finding scarce psychiatric hospital beds
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
Bill in Calif. seeks to ameliorate problem of finding scarce psychiatric hospital beds
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
It can be very difficult to find available inpatient psychiatric beds in California, leaving many teens or adults with acute psychiatric conditions waiting in hospital emergency rooms until a bed opens up – a problem shared by the other 49 states.
A bill in the California Assembly, backed by the California Psychiatric Association and the Steinberg Institute, a mental health policy organization, hopes to make the process easier by devising an online registry that collects and displays information so medical providers can find available psychiatric beds, Jenny Gold reported in an article published by Kaiser Health News.
However, the California Hospital Association doesn’t approve of the idea, saying that finding the right place for a psychiatric patient is a more complex process and such a registry could actually keep patients from getting the most appropriate treatment.
Read the whole article at http://tinyurl.com/jmvgz3g.
New Hampshire on the lookout for lead poisoning
The issue of lead poisoning is getting attention not just in Flint, Mich., but also in New Hampshire.
Dr. William Storo, president of the New Hampshire Pediatric Society, recently sent an email to all of the state’s pediatricians, reminding them that the state’s Department of Health and Human Services has found New Hampshire’s pediatric elevated blood lead level rates are 2.5 times the national average. Of the 10,281 children aged 5 years who were tested for lead at some point in their lives, 15% had an elevated blood lead level of 5 mcg/dL or higher in a 2014 New Hampshire study.
This is true because “more than half of the housing [was] built before lead paint was banned in 1978,” he said.
Yet, only 37% of the state’s 2-year-olds underwent blood lead testing in 2014. Dr. Storo’s email is a call for New Hampshire pediatricians to improve that percentage. The information-filled email – prepared by Gail Gettens of New Hampshire’s Healthy Homes and Lead Poisoning Prevention Program – is available at pediatricnews.com.
The Pediatric News website also includes links to information about lead poisoning testing and treatment from the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and several other states. Go to pediatricnews.com and scroll down the left side to click on Physician Resources; then look for Lead Poisoning.
The issue of lead poisoning is getting attention not just in Flint, Mich., but also in New Hampshire.
Dr. William Storo, president of the New Hampshire Pediatric Society, recently sent an email to all of the state’s pediatricians, reminding them that the state’s Department of Health and Human Services has found New Hampshire’s pediatric elevated blood lead level rates are 2.5 times the national average. Of the 10,281 children aged 5 years who were tested for lead at some point in their lives, 15% had an elevated blood lead level of 5 mcg/dL or higher in a 2014 New Hampshire study.
This is true because “more than half of the housing [was] built before lead paint was banned in 1978,” he said.
Yet, only 37% of the state’s 2-year-olds underwent blood lead testing in 2014. Dr. Storo’s email is a call for New Hampshire pediatricians to improve that percentage. The information-filled email – prepared by Gail Gettens of New Hampshire’s Healthy Homes and Lead Poisoning Prevention Program – is available at pediatricnews.com.
The Pediatric News website also includes links to information about lead poisoning testing and treatment from the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and several other states. Go to pediatricnews.com and scroll down the left side to click on Physician Resources; then look for Lead Poisoning.
The issue of lead poisoning is getting attention not just in Flint, Mich., but also in New Hampshire.
Dr. William Storo, president of the New Hampshire Pediatric Society, recently sent an email to all of the state’s pediatricians, reminding them that the state’s Department of Health and Human Services has found New Hampshire’s pediatric elevated blood lead level rates are 2.5 times the national average. Of the 10,281 children aged 5 years who were tested for lead at some point in their lives, 15% had an elevated blood lead level of 5 mcg/dL or higher in a 2014 New Hampshire study.
This is true because “more than half of the housing [was] built before lead paint was banned in 1978,” he said.
Yet, only 37% of the state’s 2-year-olds underwent blood lead testing in 2014. Dr. Storo’s email is a call for New Hampshire pediatricians to improve that percentage. The information-filled email – prepared by Gail Gettens of New Hampshire’s Healthy Homes and Lead Poisoning Prevention Program – is available at pediatricnews.com.
The Pediatric News website also includes links to information about lead poisoning testing and treatment from the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and several other states. Go to pediatricnews.com and scroll down the left side to click on Physician Resources; then look for Lead Poisoning.