User login
Ibrutinib bodes well for relapsed mantle-cell lymphoma
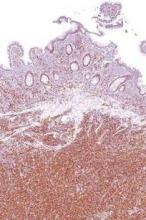
Progression-free survival was significantly better when patients with relapsed or refractory mantle-cell lymphoma were treated with oral ibrutinib than with intravenous temsirolimus, based on results from 280 patients in an international, randomized, open-label phase III trial.
Study subjects had undergone one or more previous rituximab-containing chemotherapy regimens to receive intravenous temsirolimus or oral ibrutinib at a daily dose of 560 mg.
Compared with temsirolimus, ibrutinib resulted in a 57% reduction in the risk of disease progression or death at a median follow-up of 20 months. Median progression-free survival – the trial’s primary endpoint – was 14.6 months for the ibrutinib group and 6.2 months for the temsirolimus group.
Ibrutinib was also better tolerated, with 68% of patients having grade 3 or higher treatment-emergent adverse events as compared to 87% of patients in the temsirolimus group, despite a median 4-fold longer treatment duration for the ibrutinib group than the temsirolimus group. Additionally, 6% of patients discontinued ibrutinib because of adverse events versus 26% in the temsirolimus group, reported Dr. Martin Dreyling of Klinikum der Universität in Munich, Germany, and his associates.
Based on results of the Functional Assessment of Cancer Therapy-Lymphoma (FACT-Lym) questionnaire, ibrutinib was associated with greater and more rapid improvements, and also with less worsening in lymphoma symptoms, as measured by the lymphoma subscale of the FACT-Lym (Lancet. 2016;387:770-78).
Ibrutinib, a first-in-class oral inhibitor of Bruton’s tyrosine kinase, is approved in the United States and the European Union at a dose of 560 mg per day for patients with mantle cell lymphoma who have received at least one previous line of therapy.
The mammalian target of rapamycin (mTOR) inhibitor temsirolimus is approved in the European Union for relapsed or refractory mantle-cell lymphoma, but does not have FDA approval for this indication.
The study, funded by Janssen, is ongoing. Future research, the investigators say, should examine ibrutinib-based combination approaches for patients with relapsed or refractory mantle-cell lymphoma and in front-line therapy.
Dr. Dreyling reported grants and personal fees from Janssen and Pfizer outside of the study. Several other authors reported grants from Janssen during the study and financial ties to the company.
The findings from this phase III trial clearly establish ibrutinib as a new standard for treatment of relapsed mantle-cell lymphoma. Within the next 2 years, many expect the agent will find its way into the frontline setting for treatment of mantle cell lymphoma in combination with standard chemotherapy, based on results of another already completed phase III trial (the SHINE trial).
Despite this remarkable progress, however, mantle-cell lymphoma remains incurable. Roughly 30%-40% of people with the disease will not respond to ibrutinib, and even among responders relapse seems inevitable.
Mantle-cell lymphoma has been a model for accelerated development of novel drugs. Ibrutinib was developed with tremendous speed, and the FDA’s approval of the agent in 2013 based on findings from a non-pivotal phase II trial was surprising to everyone other than the participating patients and physicians. Hopefully the resources mobilized to bring ibrutinib so far, so fast, will continue to be available to help us learn how best to use the drug.
Dr. Peter Martin is with the department of medicine at Weill Cornell Medical College in New York. His comments are excerpted from an editorial that accompanied the study in The Lancet. Dr. Martin reported that he is a consultant for Janssen and has received honoraria from the company for speaking.
The findings from this phase III trial clearly establish ibrutinib as a new standard for treatment of relapsed mantle-cell lymphoma. Within the next 2 years, many expect the agent will find its way into the frontline setting for treatment of mantle cell lymphoma in combination with standard chemotherapy, based on results of another already completed phase III trial (the SHINE trial).
Despite this remarkable progress, however, mantle-cell lymphoma remains incurable. Roughly 30%-40% of people with the disease will not respond to ibrutinib, and even among responders relapse seems inevitable.
Mantle-cell lymphoma has been a model for accelerated development of novel drugs. Ibrutinib was developed with tremendous speed, and the FDA’s approval of the agent in 2013 based on findings from a non-pivotal phase II trial was surprising to everyone other than the participating patients and physicians. Hopefully the resources mobilized to bring ibrutinib so far, so fast, will continue to be available to help us learn how best to use the drug.
Dr. Peter Martin is with the department of medicine at Weill Cornell Medical College in New York. His comments are excerpted from an editorial that accompanied the study in The Lancet. Dr. Martin reported that he is a consultant for Janssen and has received honoraria from the company for speaking.
The findings from this phase III trial clearly establish ibrutinib as a new standard for treatment of relapsed mantle-cell lymphoma. Within the next 2 years, many expect the agent will find its way into the frontline setting for treatment of mantle cell lymphoma in combination with standard chemotherapy, based on results of another already completed phase III trial (the SHINE trial).
Despite this remarkable progress, however, mantle-cell lymphoma remains incurable. Roughly 30%-40% of people with the disease will not respond to ibrutinib, and even among responders relapse seems inevitable.
Mantle-cell lymphoma has been a model for accelerated development of novel drugs. Ibrutinib was developed with tremendous speed, and the FDA’s approval of the agent in 2013 based on findings from a non-pivotal phase II trial was surprising to everyone other than the participating patients and physicians. Hopefully the resources mobilized to bring ibrutinib so far, so fast, will continue to be available to help us learn how best to use the drug.
Dr. Peter Martin is with the department of medicine at Weill Cornell Medical College in New York. His comments are excerpted from an editorial that accompanied the study in The Lancet. Dr. Martin reported that he is a consultant for Janssen and has received honoraria from the company for speaking.
Progression-free survival was significantly better when patients with relapsed or refractory mantle-cell lymphoma were treated with oral ibrutinib than with intravenous temsirolimus, based on results from 280 patients in an international, randomized, open-label phase III trial.
Study subjects had undergone one or more previous rituximab-containing chemotherapy regimens to receive intravenous temsirolimus or oral ibrutinib at a daily dose of 560 mg.
Compared with temsirolimus, ibrutinib resulted in a 57% reduction in the risk of disease progression or death at a median follow-up of 20 months. Median progression-free survival – the trial’s primary endpoint – was 14.6 months for the ibrutinib group and 6.2 months for the temsirolimus group.
Ibrutinib was also better tolerated, with 68% of patients having grade 3 or higher treatment-emergent adverse events as compared to 87% of patients in the temsirolimus group, despite a median 4-fold longer treatment duration for the ibrutinib group than the temsirolimus group. Additionally, 6% of patients discontinued ibrutinib because of adverse events versus 26% in the temsirolimus group, reported Dr. Martin Dreyling of Klinikum der Universität in Munich, Germany, and his associates.
Based on results of the Functional Assessment of Cancer Therapy-Lymphoma (FACT-Lym) questionnaire, ibrutinib was associated with greater and more rapid improvements, and also with less worsening in lymphoma symptoms, as measured by the lymphoma subscale of the FACT-Lym (Lancet. 2016;387:770-78).
Ibrutinib, a first-in-class oral inhibitor of Bruton’s tyrosine kinase, is approved in the United States and the European Union at a dose of 560 mg per day for patients with mantle cell lymphoma who have received at least one previous line of therapy.
The mammalian target of rapamycin (mTOR) inhibitor temsirolimus is approved in the European Union for relapsed or refractory mantle-cell lymphoma, but does not have FDA approval for this indication.
The study, funded by Janssen, is ongoing. Future research, the investigators say, should examine ibrutinib-based combination approaches for patients with relapsed or refractory mantle-cell lymphoma and in front-line therapy.
Dr. Dreyling reported grants and personal fees from Janssen and Pfizer outside of the study. Several other authors reported grants from Janssen during the study and financial ties to the company.
Progression-free survival was significantly better when patients with relapsed or refractory mantle-cell lymphoma were treated with oral ibrutinib than with intravenous temsirolimus, based on results from 280 patients in an international, randomized, open-label phase III trial.
Study subjects had undergone one or more previous rituximab-containing chemotherapy regimens to receive intravenous temsirolimus or oral ibrutinib at a daily dose of 560 mg.
Compared with temsirolimus, ibrutinib resulted in a 57% reduction in the risk of disease progression or death at a median follow-up of 20 months. Median progression-free survival – the trial’s primary endpoint – was 14.6 months for the ibrutinib group and 6.2 months for the temsirolimus group.
Ibrutinib was also better tolerated, with 68% of patients having grade 3 or higher treatment-emergent adverse events as compared to 87% of patients in the temsirolimus group, despite a median 4-fold longer treatment duration for the ibrutinib group than the temsirolimus group. Additionally, 6% of patients discontinued ibrutinib because of adverse events versus 26% in the temsirolimus group, reported Dr. Martin Dreyling of Klinikum der Universität in Munich, Germany, and his associates.
Based on results of the Functional Assessment of Cancer Therapy-Lymphoma (FACT-Lym) questionnaire, ibrutinib was associated with greater and more rapid improvements, and also with less worsening in lymphoma symptoms, as measured by the lymphoma subscale of the FACT-Lym (Lancet. 2016;387:770-78).
Ibrutinib, a first-in-class oral inhibitor of Bruton’s tyrosine kinase, is approved in the United States and the European Union at a dose of 560 mg per day for patients with mantle cell lymphoma who have received at least one previous line of therapy.
The mammalian target of rapamycin (mTOR) inhibitor temsirolimus is approved in the European Union for relapsed or refractory mantle-cell lymphoma, but does not have FDA approval for this indication.
The study, funded by Janssen, is ongoing. Future research, the investigators say, should examine ibrutinib-based combination approaches for patients with relapsed or refractory mantle-cell lymphoma and in front-line therapy.
Dr. Dreyling reported grants and personal fees from Janssen and Pfizer outside of the study. Several other authors reported grants from Janssen during the study and financial ties to the company.
FROM THE LANCET
Key clinical point: Ibrutinib significantly improved progression-free survival, compared with temsirolimus in patients with relapsed or refractory mantle-cell lymphoma.
Major finding: Median progression-free survival was 14.6 months with ibrutinib and 6.2 months with temsirolimus.
Data source: A randomized open-label phase III trial (ongoing) that randomized 280 patients to each treatment group.
Disclosures: The study was funded by Janssen. Dr. Dreyling reported grants and personal fees from Janssen and Pfizer outside of the study, and other authors reported grants from Janssen during the study and financial ties to the company.
Good Samaritan protection should ease pediatricians’ hesitations
“If there is a doctor or nurse on board, please identify yourself by pushing the attendant call button.”
For pediatricians, such calls for voluntary emergency help can be simple and ethically clear on one hand, but legally worrisome and uncomfortable on the other.
“We’ve all hesitated,” Dr. Steven M. Donn, former chair of the American Academy of Pediatrics’ Committee on Medical Liability & Risk Management, said at the AAP’s annual meeting in Washington. “We often find ourselves in various scenarios, not with our pediatric population, but with elderly and younger adults, when we feel like we may be in over our heads. And we’re also afraid we’ll get sued.”
Good Samaritan laws in all 50 states, however, provide legal protection for good faith attempts to help, even if such attempts are technically “negligent.”
“The goal of these laws is to strike the right balance … to reduce liability enough to motivate volunteerism, but to preserve enough liability to prevent reckless or harmful interactions,” said Dr. Dunn, a professor of pediatrics at the University of Michigan, Ann Arbor.
While the laws provide legal immunity against ordinary negligence (doing something that an average, reasonable person would not do), there is not generally no immunity provided for “gross negligence,” which is defined as reckless and willful disregard for the safety of others.
He urged pediatricians to remember three criteria for immunity: That it is an emergency situation, where failure to intervene could result in death or severe bodily harm; that the responder acts without compensation; and that the responder acts rationally, in good faith, and without gross negligence.
“Don’t be afraid to get involved,” Dr. Dunn said. “Just keep within the limits of your abilities and provide help in good faith. Do the Heimlich maneuver, for instance, but don’t ask for a dinner knife to do a tracheotomy.”
And with regards to compensation, it’s fine to accept a free drink on an airplane, but not to accept free airline tickets, he said.
A case scenario: An elderly woman falls on an escalator in a shopping mall, sustaining an apparent head and neck injury. You offer assistance, stabilize the head and neck, and request a call to 911. The woman is taken to the emergency room, and the store manager gives you a $500 gift certificate in gratitude. Unfortunately, however, the woman has a bad outcome and sues you for negligence. “By accepting the gift certificate, you’ve [in all likelihood] lost your [Good Samaritan] protection,” he said.
Patients and parents can refuse help, and helping despite refusal is usually deemed to be not in “good faith.” There may be exceptions, however. “Say you’re waiting for your child in the middle school parking lot when you see another child struck by lightning. You initiate CPR, and as you’re administering CPR the father of the child arrives and greets you with ‘If anything happens to my child, I am going to sue you,’ “ Dr. Dunn said. “What are the risks of continuing care?”
“You’d just need to be aware that there could be a separate charge for care without consent, or even assault and battery,” Dr. Dunn said. “But I think it’s one you could probably win since you were acting in good faith to provide lifesaving attention.”
Good Samaritan laws generally do not apply to medical professionals while “on the job,” but some states extend protection to medical professionals who render emergency assistance in a hospital or other “health care setting” when such assistance is beyond the scope of their work duties.
“So if you’re walking down the hallway, and someone collapses and you offer assistance, even though you’re not the patient’s physician, in some states you’ll be covered by the Good Samaritan law,” Dr. Dunn said. “So it’s helpful to know your state’s laws.”
Good Samaritan assistance during commercial flights is governed by the federal Aviation Medical Assistance Act of 1998; the law protects providers who respond to in-flight medical emergencies against liability for negligence. Medical emergencies occur in about 1 of every 600 flights, and physicians assist in nearly half of these cases, according to a 2013 study (N Engl J Med. 2013 Aug 29;369[9]:877).
“If there is a doctor or nurse on board, please identify yourself by pushing the attendant call button.”
For pediatricians, such calls for voluntary emergency help can be simple and ethically clear on one hand, but legally worrisome and uncomfortable on the other.
“We’ve all hesitated,” Dr. Steven M. Donn, former chair of the American Academy of Pediatrics’ Committee on Medical Liability & Risk Management, said at the AAP’s annual meeting in Washington. “We often find ourselves in various scenarios, not with our pediatric population, but with elderly and younger adults, when we feel like we may be in over our heads. And we’re also afraid we’ll get sued.”
Good Samaritan laws in all 50 states, however, provide legal protection for good faith attempts to help, even if such attempts are technically “negligent.”
“The goal of these laws is to strike the right balance … to reduce liability enough to motivate volunteerism, but to preserve enough liability to prevent reckless or harmful interactions,” said Dr. Dunn, a professor of pediatrics at the University of Michigan, Ann Arbor.
While the laws provide legal immunity against ordinary negligence (doing something that an average, reasonable person would not do), there is not generally no immunity provided for “gross negligence,” which is defined as reckless and willful disregard for the safety of others.
He urged pediatricians to remember three criteria for immunity: That it is an emergency situation, where failure to intervene could result in death or severe bodily harm; that the responder acts without compensation; and that the responder acts rationally, in good faith, and without gross negligence.
“Don’t be afraid to get involved,” Dr. Dunn said. “Just keep within the limits of your abilities and provide help in good faith. Do the Heimlich maneuver, for instance, but don’t ask for a dinner knife to do a tracheotomy.”
And with regards to compensation, it’s fine to accept a free drink on an airplane, but not to accept free airline tickets, he said.
A case scenario: An elderly woman falls on an escalator in a shopping mall, sustaining an apparent head and neck injury. You offer assistance, stabilize the head and neck, and request a call to 911. The woman is taken to the emergency room, and the store manager gives you a $500 gift certificate in gratitude. Unfortunately, however, the woman has a bad outcome and sues you for negligence. “By accepting the gift certificate, you’ve [in all likelihood] lost your [Good Samaritan] protection,” he said.
Patients and parents can refuse help, and helping despite refusal is usually deemed to be not in “good faith.” There may be exceptions, however. “Say you’re waiting for your child in the middle school parking lot when you see another child struck by lightning. You initiate CPR, and as you’re administering CPR the father of the child arrives and greets you with ‘If anything happens to my child, I am going to sue you,’ “ Dr. Dunn said. “What are the risks of continuing care?”
“You’d just need to be aware that there could be a separate charge for care without consent, or even assault and battery,” Dr. Dunn said. “But I think it’s one you could probably win since you were acting in good faith to provide lifesaving attention.”
Good Samaritan laws generally do not apply to medical professionals while “on the job,” but some states extend protection to medical professionals who render emergency assistance in a hospital or other “health care setting” when such assistance is beyond the scope of their work duties.
“So if you’re walking down the hallway, and someone collapses and you offer assistance, even though you’re not the patient’s physician, in some states you’ll be covered by the Good Samaritan law,” Dr. Dunn said. “So it’s helpful to know your state’s laws.”
Good Samaritan assistance during commercial flights is governed by the federal Aviation Medical Assistance Act of 1998; the law protects providers who respond to in-flight medical emergencies against liability for negligence. Medical emergencies occur in about 1 of every 600 flights, and physicians assist in nearly half of these cases, according to a 2013 study (N Engl J Med. 2013 Aug 29;369[9]:877).
“If there is a doctor or nurse on board, please identify yourself by pushing the attendant call button.”
For pediatricians, such calls for voluntary emergency help can be simple and ethically clear on one hand, but legally worrisome and uncomfortable on the other.
“We’ve all hesitated,” Dr. Steven M. Donn, former chair of the American Academy of Pediatrics’ Committee on Medical Liability & Risk Management, said at the AAP’s annual meeting in Washington. “We often find ourselves in various scenarios, not with our pediatric population, but with elderly and younger adults, when we feel like we may be in over our heads. And we’re also afraid we’ll get sued.”
Good Samaritan laws in all 50 states, however, provide legal protection for good faith attempts to help, even if such attempts are technically “negligent.”
“The goal of these laws is to strike the right balance … to reduce liability enough to motivate volunteerism, but to preserve enough liability to prevent reckless or harmful interactions,” said Dr. Dunn, a professor of pediatrics at the University of Michigan, Ann Arbor.
While the laws provide legal immunity against ordinary negligence (doing something that an average, reasonable person would not do), there is not generally no immunity provided for “gross negligence,” which is defined as reckless and willful disregard for the safety of others.
He urged pediatricians to remember three criteria for immunity: That it is an emergency situation, where failure to intervene could result in death or severe bodily harm; that the responder acts without compensation; and that the responder acts rationally, in good faith, and without gross negligence.
“Don’t be afraid to get involved,” Dr. Dunn said. “Just keep within the limits of your abilities and provide help in good faith. Do the Heimlich maneuver, for instance, but don’t ask for a dinner knife to do a tracheotomy.”
And with regards to compensation, it’s fine to accept a free drink on an airplane, but not to accept free airline tickets, he said.
A case scenario: An elderly woman falls on an escalator in a shopping mall, sustaining an apparent head and neck injury. You offer assistance, stabilize the head and neck, and request a call to 911. The woman is taken to the emergency room, and the store manager gives you a $500 gift certificate in gratitude. Unfortunately, however, the woman has a bad outcome and sues you for negligence. “By accepting the gift certificate, you’ve [in all likelihood] lost your [Good Samaritan] protection,” he said.
Patients and parents can refuse help, and helping despite refusal is usually deemed to be not in “good faith.” There may be exceptions, however. “Say you’re waiting for your child in the middle school parking lot when you see another child struck by lightning. You initiate CPR, and as you’re administering CPR the father of the child arrives and greets you with ‘If anything happens to my child, I am going to sue you,’ “ Dr. Dunn said. “What are the risks of continuing care?”
“You’d just need to be aware that there could be a separate charge for care without consent, or even assault and battery,” Dr. Dunn said. “But I think it’s one you could probably win since you were acting in good faith to provide lifesaving attention.”
Good Samaritan laws generally do not apply to medical professionals while “on the job,” but some states extend protection to medical professionals who render emergency assistance in a hospital or other “health care setting” when such assistance is beyond the scope of their work duties.
“So if you’re walking down the hallway, and someone collapses and you offer assistance, even though you’re not the patient’s physician, in some states you’ll be covered by the Good Samaritan law,” Dr. Dunn said. “So it’s helpful to know your state’s laws.”
Good Samaritan assistance during commercial flights is governed by the federal Aviation Medical Assistance Act of 1998; the law protects providers who respond to in-flight medical emergencies against liability for negligence. Medical emergencies occur in about 1 of every 600 flights, and physicians assist in nearly half of these cases, according to a 2013 study (N Engl J Med. 2013 Aug 29;369[9]:877).
Pregnancy did not increase Hodgkin lymphoma relapse rate
Women who become pregnant while in remission from Hodgkin lymphoma were not at increased risk for cancer relapse, according to an analysis of data from Swedish health care registries combined with medical records.
Of 449 women who were diagnosed with Hodgkin lymphoma between 1992 and 2009, 144 (32%) became pregnant during follow-up, which started 6 months after diagnosis, when the disease was assumed to be in remission. Only one of these women experienced a pregnancy-associated relapse, which was defined as a relapse occurring during pregnancy or within 5 years of delivery. Of the women who did not become pregnant, 46 had a relapse.
The effect of pregnancy on relapse has been a concern of patients and clinicians, but “our findings suggest that the risk of pregnancy-associated relapse does not need to be taken into account in family planning for women whose Hodgkin lymphoma is in remission,” said Caroline E. Weibull of Karolinska Institutet in Stockholm, and her associates.
The researchers used the nationwide “Swedish Cancer Register” to identify all cases of Hodgkin lymphoma (reporting is mandatory) and merged this data with clinical information from other registries and medical records.
The pregnancy rates were similar among women who had limited- and advanced-stage disease and among women with and without B symptoms at diagnosis – a finding that negates consideration of a so-called “healthy mother effect” in protecting against relapse, they wrote (J Clin Onc. 2015 Dec. 14 [doi:10.1200/JCO.2015.63.3446]).
The researchers also found that the absolute risk for relapse was highest in the first 2-3 years after diagnosis, which suggests that women should be advised, “if possible, to wait 2 years after cessation of treatment before becoming pregnant.” Additionally, the relapse rate more than doubled in women aged 30 years or older at diagnosis, compared with women aged 18-24 years at diagnosis – a finding consistent with previous research, they noted.
Women in the study were aged 18-40 at diagnosis. Follow-up ended on the date of relapse, the date of death, or at the end of 2010, whichever came first.
Women who become pregnant while in remission from Hodgkin lymphoma were not at increased risk for cancer relapse, according to an analysis of data from Swedish health care registries combined with medical records.
Of 449 women who were diagnosed with Hodgkin lymphoma between 1992 and 2009, 144 (32%) became pregnant during follow-up, which started 6 months after diagnosis, when the disease was assumed to be in remission. Only one of these women experienced a pregnancy-associated relapse, which was defined as a relapse occurring during pregnancy or within 5 years of delivery. Of the women who did not become pregnant, 46 had a relapse.
The effect of pregnancy on relapse has been a concern of patients and clinicians, but “our findings suggest that the risk of pregnancy-associated relapse does not need to be taken into account in family planning for women whose Hodgkin lymphoma is in remission,” said Caroline E. Weibull of Karolinska Institutet in Stockholm, and her associates.
The researchers used the nationwide “Swedish Cancer Register” to identify all cases of Hodgkin lymphoma (reporting is mandatory) and merged this data with clinical information from other registries and medical records.
The pregnancy rates were similar among women who had limited- and advanced-stage disease and among women with and without B symptoms at diagnosis – a finding that negates consideration of a so-called “healthy mother effect” in protecting against relapse, they wrote (J Clin Onc. 2015 Dec. 14 [doi:10.1200/JCO.2015.63.3446]).
The researchers also found that the absolute risk for relapse was highest in the first 2-3 years after diagnosis, which suggests that women should be advised, “if possible, to wait 2 years after cessation of treatment before becoming pregnant.” Additionally, the relapse rate more than doubled in women aged 30 years or older at diagnosis, compared with women aged 18-24 years at diagnosis – a finding consistent with previous research, they noted.
Women in the study were aged 18-40 at diagnosis. Follow-up ended on the date of relapse, the date of death, or at the end of 2010, whichever came first.
Women who become pregnant while in remission from Hodgkin lymphoma were not at increased risk for cancer relapse, according to an analysis of data from Swedish health care registries combined with medical records.
Of 449 women who were diagnosed with Hodgkin lymphoma between 1992 and 2009, 144 (32%) became pregnant during follow-up, which started 6 months after diagnosis, when the disease was assumed to be in remission. Only one of these women experienced a pregnancy-associated relapse, which was defined as a relapse occurring during pregnancy or within 5 years of delivery. Of the women who did not become pregnant, 46 had a relapse.
The effect of pregnancy on relapse has been a concern of patients and clinicians, but “our findings suggest that the risk of pregnancy-associated relapse does not need to be taken into account in family planning for women whose Hodgkin lymphoma is in remission,” said Caroline E. Weibull of Karolinska Institutet in Stockholm, and her associates.
The researchers used the nationwide “Swedish Cancer Register” to identify all cases of Hodgkin lymphoma (reporting is mandatory) and merged this data with clinical information from other registries and medical records.
The pregnancy rates were similar among women who had limited- and advanced-stage disease and among women with and without B symptoms at diagnosis – a finding that negates consideration of a so-called “healthy mother effect” in protecting against relapse, they wrote (J Clin Onc. 2015 Dec. 14 [doi:10.1200/JCO.2015.63.3446]).
The researchers also found that the absolute risk for relapse was highest in the first 2-3 years after diagnosis, which suggests that women should be advised, “if possible, to wait 2 years after cessation of treatment before becoming pregnant.” Additionally, the relapse rate more than doubled in women aged 30 years or older at diagnosis, compared with women aged 18-24 years at diagnosis – a finding consistent with previous research, they noted.
Women in the study were aged 18-40 at diagnosis. Follow-up ended on the date of relapse, the date of death, or at the end of 2010, whichever came first.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Pregnancy did not increase the risk of relapse of Hodgkin lymphoma in a population-based study.
Major finding: Of 144 women who became pregnant 6 months or longer after diagnosis of Hodgkin lymphoma, 1 experienced a pregnancy-associated relapse.
Data source: Population-based study utilizing Swedish health care registries and medical records, in which 449 women with Hodgkin lymphoma diagnoses, and 47 relapses, were identified.
Disclosures: The study was supported by the Swedish Cancer Society, the Strategic Research Program in Epidemiology at Karolinska Institutet, the Swedish Society for Medicine, and the Swedish Society for Medical Research.
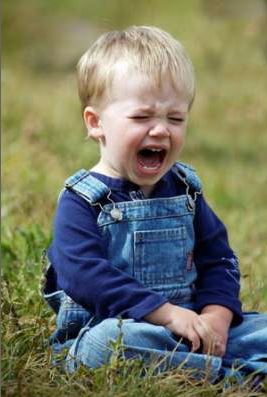
Changes in AAP periodicity schedule include several new screenings
An updated version of the American Academy of Pediatrics’ Recommendations for Preventive Pediatric Health Care, published in the January 2016 issue of Pediatrics, includes screening recommendations that may still be slow on the uptake in pediatric practices since being approved by the AAP 2 years ago.
Depression screening is “starting to improve,” but lipid screening and HIV screening have been “harder to implement,” said Dr. Geoffrey R. Simon, chair of the AAP’s Committee on Practice and Ambulatory Medicine, which works with the Bright Futures Periodicity Schedule Workgroup to keep the schedule up to date.
Publication of the schedule in Pediatrics (2016 Jan. doi: 10.1542/peds.2015-3908), as has been done every 3-5 years, is in many ways a formality this time around. Two years ago, the AAP began updating the schedule in real time to immediately reflect new recommendations and guidelines endorsed or produced by the Academy for comprehensive health supervision.
“The goal has been to shorten the time frame for incorporating new evidence, including removing screening items that research has demonstrated aren’t useful,” Dr. Simon, a pediatrician in Wilmington, Del., said in an interview.
Each of these screenings, however, like the other recommended services listed in the Periodicity Schedule, is backed by evidence and is required under the Affordable Care Act to be covered by insurers without any cost sharing. Other recommendations include a call for fluoride varnish applications from 6 months through 5 years.
“These aren’t just good ideas. There is strong evidence for [every recommendation] on the Periodicity Schedule,” Dr. Joseph F. Hagan Jr., a member of the Bright Futures Periodicity Schedule Workgroup and a pediatrician in Burlington, Vt., said in an interview.
The updated schedule no longer recommends vision screening at age 18 years, based on evidence showing that far fewer new vision problems develop in low-risk young adults as younger children. It also omits routine screening for cervical dysplasia until age 21 years.
The change from vision screening to risk-based assessment at age 18 coincides with publication – also in the January issue of Pediatrics – of an AAP policy statement on Visual System Assessment in Infants, Children, and Young Adults (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-35970.) and an accompanying clinical report titled Procedures for the Evaluation of the Visual System by Pediatricians (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-3597).
Screening for depression is recommended annually from ages 11-21 years, as suicide is now a leading cause of death among adolescents. And HIV screening is recommended for adolescents aged 16-18 years to address federal statistics showing that 1 in 4 new HIV infections occurs in youth aged 13-24 years, and that about 60% of all youth with HIV do not know they are infected, according to the AAP.
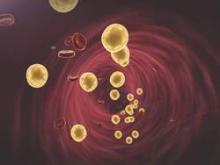
The recommendation for dyslipidemia screening covers patients aged 9-11 years, in addition to those aged 18-21 years. The recommendation to screen once during each of these two windows of times is based on guidelines from the National Heart, Lung, and Blood Institute on cardiovascular risk reduction in childhood and adolescence, Dr. Simon said.
“It was an attempt to make it easier and more effective by replacing an ineffective and cumbersome two-step screening process using risk assessment with lab testing if needed,” he said.
At the annual meeting of the AAP in October 2015, pediatric cardiologist Dr. Sarah de Ferranti said in a packed sessionon lipid screening that getting a family history of cardiovascular disease has proven unreliable for identifying children at high risk of disease – even those with familial hypercholesterolemia. This disorder affects 1 in 250 individuals, she said, and is usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as adults.”
Dr. Karalyn Kinsella, a pediatrician in Cheshire, Conn., is among those pediatricians who have found lipid screening and HIV screening to be particularly challenging. “The difficulty [with lipid screening in my practice] is with those children who are already physically active, have healthy diets, and a normal BMI,” said Dr. Kinsella, who was asked to comment on the current periodicity schedule. “When they have elevated lipid levels, what is our next step? For those not high enough to treat, it can create unnecessary anxiety in families.”
With respect to HIV screening, payment issues can impede confidentiality. “We’re obligated to maintain confidentiality with the teen, but parents sometimes see the bill,” she said, adding that many her adolescents’ families “have health savings accounts with high deductibles and have to pay out of pocket.”
Coverage of point-of-care testing still is inadequate, Dr. Simon said. “It’s a payer barrier to delivering care in a timely manner,” he said.
Another recommendation made in 2014 and reflected in the newly published schedule advises pediatricians to use the CRAFFT (Car, Relax, Forget, Friends, Trouble) screening questionnaire as a tool to screen adolescents for drug and alcohol use. Specific tools are not usually recommended, Dr. Hagan said, but the CRAFFT screen “is validated and has been sufficiently widely used that we recommend it.”
One challenge, Dr. Kinsella said, is allowing enough time for the teen patient to fill out two screens – CRAFFT and a depression screening tool. “Ideally,” she added, “patients could fill them out on an [EHR] patient portal,” with confidentiality ensured.
The upcoming revised edition of the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents – expected in late spring or early summer of 2016 – will offer more guidance on previsit screening, which is valuable because “it moves some of this time away from the [limited] face-to-face time that you have, so you know where to focus your time in the visit,” said Dr. Hagan, coeditor of Bright Futures.
“We’re looking at making these visits efficient, efficacious, and most importantly, doable,” he emphasized.
The 4th edition of Bright Futures will include another freshly updated periodicity schedule that likely will include maternal depression screening and a recommendation for developmental screening at 4 years, as well as an expanded window for HIV testing from the current 16-18 years to 15-21 years, said Dr. Hagan, who previewed the new edition at the AAP annual meeting.
As Bright Futures and the Committee on Practice and Ambulatory Medicine deliberate these potential additions to the schedule, “we [will consider] how much these screening recommendations can impact and improve child health, and if a busy pediatrician can perform them in a time and cost-effective manner,” Dr. Simon said.
An up-to-date periodicity schedule can be accessed here.
An updated version of the American Academy of Pediatrics’ Recommendations for Preventive Pediatric Health Care, published in the January 2016 issue of Pediatrics, includes screening recommendations that may still be slow on the uptake in pediatric practices since being approved by the AAP 2 years ago.
Depression screening is “starting to improve,” but lipid screening and HIV screening have been “harder to implement,” said Dr. Geoffrey R. Simon, chair of the AAP’s Committee on Practice and Ambulatory Medicine, which works with the Bright Futures Periodicity Schedule Workgroup to keep the schedule up to date.
Publication of the schedule in Pediatrics (2016 Jan. doi: 10.1542/peds.2015-3908), as has been done every 3-5 years, is in many ways a formality this time around. Two years ago, the AAP began updating the schedule in real time to immediately reflect new recommendations and guidelines endorsed or produced by the Academy for comprehensive health supervision.
“The goal has been to shorten the time frame for incorporating new evidence, including removing screening items that research has demonstrated aren’t useful,” Dr. Simon, a pediatrician in Wilmington, Del., said in an interview.
Each of these screenings, however, like the other recommended services listed in the Periodicity Schedule, is backed by evidence and is required under the Affordable Care Act to be covered by insurers without any cost sharing. Other recommendations include a call for fluoride varnish applications from 6 months through 5 years.
“These aren’t just good ideas. There is strong evidence for [every recommendation] on the Periodicity Schedule,” Dr. Joseph F. Hagan Jr., a member of the Bright Futures Periodicity Schedule Workgroup and a pediatrician in Burlington, Vt., said in an interview.
The updated schedule no longer recommends vision screening at age 18 years, based on evidence showing that far fewer new vision problems develop in low-risk young adults as younger children. It also omits routine screening for cervical dysplasia until age 21 years.
The change from vision screening to risk-based assessment at age 18 coincides with publication – also in the January issue of Pediatrics – of an AAP policy statement on Visual System Assessment in Infants, Children, and Young Adults (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-35970.) and an accompanying clinical report titled Procedures for the Evaluation of the Visual System by Pediatricians (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-3597).
Screening for depression is recommended annually from ages 11-21 years, as suicide is now a leading cause of death among adolescents. And HIV screening is recommended for adolescents aged 16-18 years to address federal statistics showing that 1 in 4 new HIV infections occurs in youth aged 13-24 years, and that about 60% of all youth with HIV do not know they are infected, according to the AAP.
The recommendation for dyslipidemia screening covers patients aged 9-11 years, in addition to those aged 18-21 years. The recommendation to screen once during each of these two windows of times is based on guidelines from the National Heart, Lung, and Blood Institute on cardiovascular risk reduction in childhood and adolescence, Dr. Simon said.
“It was an attempt to make it easier and more effective by replacing an ineffective and cumbersome two-step screening process using risk assessment with lab testing if needed,” he said.
At the annual meeting of the AAP in October 2015, pediatric cardiologist Dr. Sarah de Ferranti said in a packed sessionon lipid screening that getting a family history of cardiovascular disease has proven unreliable for identifying children at high risk of disease – even those with familial hypercholesterolemia. This disorder affects 1 in 250 individuals, she said, and is usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as adults.”
Dr. Karalyn Kinsella, a pediatrician in Cheshire, Conn., is among those pediatricians who have found lipid screening and HIV screening to be particularly challenging. “The difficulty [with lipid screening in my practice] is with those children who are already physically active, have healthy diets, and a normal BMI,” said Dr. Kinsella, who was asked to comment on the current periodicity schedule. “When they have elevated lipid levels, what is our next step? For those not high enough to treat, it can create unnecessary anxiety in families.”
With respect to HIV screening, payment issues can impede confidentiality. “We’re obligated to maintain confidentiality with the teen, but parents sometimes see the bill,” she said, adding that many her adolescents’ families “have health savings accounts with high deductibles and have to pay out of pocket.”
Coverage of point-of-care testing still is inadequate, Dr. Simon said. “It’s a payer barrier to delivering care in a timely manner,” he said.
Another recommendation made in 2014 and reflected in the newly published schedule advises pediatricians to use the CRAFFT (Car, Relax, Forget, Friends, Trouble) screening questionnaire as a tool to screen adolescents for drug and alcohol use. Specific tools are not usually recommended, Dr. Hagan said, but the CRAFFT screen “is validated and has been sufficiently widely used that we recommend it.”
One challenge, Dr. Kinsella said, is allowing enough time for the teen patient to fill out two screens – CRAFFT and a depression screening tool. “Ideally,” she added, “patients could fill them out on an [EHR] patient portal,” with confidentiality ensured.
The upcoming revised edition of the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents – expected in late spring or early summer of 2016 – will offer more guidance on previsit screening, which is valuable because “it moves some of this time away from the [limited] face-to-face time that you have, so you know where to focus your time in the visit,” said Dr. Hagan, coeditor of Bright Futures.
“We’re looking at making these visits efficient, efficacious, and most importantly, doable,” he emphasized.
The 4th edition of Bright Futures will include another freshly updated periodicity schedule that likely will include maternal depression screening and a recommendation for developmental screening at 4 years, as well as an expanded window for HIV testing from the current 16-18 years to 15-21 years, said Dr. Hagan, who previewed the new edition at the AAP annual meeting.
As Bright Futures and the Committee on Practice and Ambulatory Medicine deliberate these potential additions to the schedule, “we [will consider] how much these screening recommendations can impact and improve child health, and if a busy pediatrician can perform them in a time and cost-effective manner,” Dr. Simon said.
An up-to-date periodicity schedule can be accessed here.
An updated version of the American Academy of Pediatrics’ Recommendations for Preventive Pediatric Health Care, published in the January 2016 issue of Pediatrics, includes screening recommendations that may still be slow on the uptake in pediatric practices since being approved by the AAP 2 years ago.
Depression screening is “starting to improve,” but lipid screening and HIV screening have been “harder to implement,” said Dr. Geoffrey R. Simon, chair of the AAP’s Committee on Practice and Ambulatory Medicine, which works with the Bright Futures Periodicity Schedule Workgroup to keep the schedule up to date.
Publication of the schedule in Pediatrics (2016 Jan. doi: 10.1542/peds.2015-3908), as has been done every 3-5 years, is in many ways a formality this time around. Two years ago, the AAP began updating the schedule in real time to immediately reflect new recommendations and guidelines endorsed or produced by the Academy for comprehensive health supervision.
“The goal has been to shorten the time frame for incorporating new evidence, including removing screening items that research has demonstrated aren’t useful,” Dr. Simon, a pediatrician in Wilmington, Del., said in an interview.
Each of these screenings, however, like the other recommended services listed in the Periodicity Schedule, is backed by evidence and is required under the Affordable Care Act to be covered by insurers without any cost sharing. Other recommendations include a call for fluoride varnish applications from 6 months through 5 years.
“These aren’t just good ideas. There is strong evidence for [every recommendation] on the Periodicity Schedule,” Dr. Joseph F. Hagan Jr., a member of the Bright Futures Periodicity Schedule Workgroup and a pediatrician in Burlington, Vt., said in an interview.
The updated schedule no longer recommends vision screening at age 18 years, based on evidence showing that far fewer new vision problems develop in low-risk young adults as younger children. It also omits routine screening for cervical dysplasia until age 21 years.
The change from vision screening to risk-based assessment at age 18 coincides with publication – also in the January issue of Pediatrics – of an AAP policy statement on Visual System Assessment in Infants, Children, and Young Adults (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-35970.) and an accompanying clinical report titled Procedures for the Evaluation of the Visual System by Pediatricians (Pediatrics. 2016 Jan. doi: 10.1542/peds.2015-3597).
Screening for depression is recommended annually from ages 11-21 years, as suicide is now a leading cause of death among adolescents. And HIV screening is recommended for adolescents aged 16-18 years to address federal statistics showing that 1 in 4 new HIV infections occurs in youth aged 13-24 years, and that about 60% of all youth with HIV do not know they are infected, according to the AAP.
The recommendation for dyslipidemia screening covers patients aged 9-11 years, in addition to those aged 18-21 years. The recommendation to screen once during each of these two windows of times is based on guidelines from the National Heart, Lung, and Blood Institute on cardiovascular risk reduction in childhood and adolescence, Dr. Simon said.
“It was an attempt to make it easier and more effective by replacing an ineffective and cumbersome two-step screening process using risk assessment with lab testing if needed,” he said.
At the annual meeting of the AAP in October 2015, pediatric cardiologist Dr. Sarah de Ferranti said in a packed sessionon lipid screening that getting a family history of cardiovascular disease has proven unreliable for identifying children at high risk of disease – even those with familial hypercholesterolemia. This disorder affects 1 in 250 individuals, she said, and is usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as adults.”
Dr. Karalyn Kinsella, a pediatrician in Cheshire, Conn., is among those pediatricians who have found lipid screening and HIV screening to be particularly challenging. “The difficulty [with lipid screening in my practice] is with those children who are already physically active, have healthy diets, and a normal BMI,” said Dr. Kinsella, who was asked to comment on the current periodicity schedule. “When they have elevated lipid levels, what is our next step? For those not high enough to treat, it can create unnecessary anxiety in families.”
With respect to HIV screening, payment issues can impede confidentiality. “We’re obligated to maintain confidentiality with the teen, but parents sometimes see the bill,” she said, adding that many her adolescents’ families “have health savings accounts with high deductibles and have to pay out of pocket.”
Coverage of point-of-care testing still is inadequate, Dr. Simon said. “It’s a payer barrier to delivering care in a timely manner,” he said.
Another recommendation made in 2014 and reflected in the newly published schedule advises pediatricians to use the CRAFFT (Car, Relax, Forget, Friends, Trouble) screening questionnaire as a tool to screen adolescents for drug and alcohol use. Specific tools are not usually recommended, Dr. Hagan said, but the CRAFFT screen “is validated and has been sufficiently widely used that we recommend it.”
One challenge, Dr. Kinsella said, is allowing enough time for the teen patient to fill out two screens – CRAFFT and a depression screening tool. “Ideally,” she added, “patients could fill them out on an [EHR] patient portal,” with confidentiality ensured.
The upcoming revised edition of the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents – expected in late spring or early summer of 2016 – will offer more guidance on previsit screening, which is valuable because “it moves some of this time away from the [limited] face-to-face time that you have, so you know where to focus your time in the visit,” said Dr. Hagan, coeditor of Bright Futures.
“We’re looking at making these visits efficient, efficacious, and most importantly, doable,” he emphasized.
The 4th edition of Bright Futures will include another freshly updated periodicity schedule that likely will include maternal depression screening and a recommendation for developmental screening at 4 years, as well as an expanded window for HIV testing from the current 16-18 years to 15-21 years, said Dr. Hagan, who previewed the new edition at the AAP annual meeting.
As Bright Futures and the Committee on Practice and Ambulatory Medicine deliberate these potential additions to the schedule, “we [will consider] how much these screening recommendations can impact and improve child health, and if a busy pediatrician can perform them in a time and cost-effective manner,” Dr. Simon said.
An up-to-date periodicity schedule can be accessed here.
FROM PEDIATRICS
AAP: New Bright Futures edition coming with added screenings
WASHINGTON – A new edition of the Bright Futures guidelines is scheduled for release in 2016, and among the expected changes are a recommendation for developmental screening at 4 years and an increased emphasis on the “social determinants of health.”
Revisions planned for the 4th edition of the Bright Futures Health Supervision Guidelines for Infants, Children, and Adolescents, including the American Academy of Pediatrics Periodicity Schedule, are notable not only because they reflect new evidence, but because the services recommended in the guidelines are required by the Affordable Care Act to be covered by insurers without any cost sharing, Dr. Joseph F. Hagan Jr., a pediatrician in Burlington, Vt., and coeditor of Bright Futures, said at the annual meeting of the American Academy of Pediatrics.
The current Recommendations for Preventive Pediatric Health Care – Periodicity Schedule – which represents a consensus of the Bright Futures advisory committee and the AAP – recommends standardized developmental screening at ages 9, 18, and 30 months, and autism screening at ages 18 and 24 months.
The expected addition of developmental screening to the 4-year health supervision visit will be in keeping with the tools most often utilized in pediatric practices, such as the Ages & Stages Questionnaires, which are validated for screening in children up to 5 years of age. “A lot can happen in 18 months [since the 30-month visit],” Dr. Hagan said.
In 2015 the U.S. Preventive Services Task Force assigned a “I” evidence rating to screening for speech and language delays and disorders in children aged 5 and younger, which means it found insufficient evidence to recommend for or against screening. Still, developmental screening meets a minimum standard for Bright Futures of being “evidence informed” in its recommendations for services and screening, Dr. Hagan said.
“We have tried to provide at least evidence-informed recommendations for the content each of the 31 visits you provide from birth to age 21,” he emphasized. Evidence was “important in the 3rd edition and it’s essential in the 4th. We must have a strong evidence base when we make a recommendation for something new that insurance companies will need to pay for.”
Outside of the Periodicity Schedule, Bright Futures offers recommendations for health promotion and anticipatory guidance, and some of these recommendations are consensus based rather than evidence based or evidence informed. However, a lack of evidence “doesn’t necessarily mean lack of efficacy,” he said at the meeting. “It usually reflects a lack of study in children.”
The updated guidelines – which, like previous versions, have been funded by the U.S. Department of Health and Human Services and will be published by the AAP – will include an expanded chapter on rationale and evidence for each recommendation so that “you can see transparently what we chose and why,” Dr. Hagan told this newspaper.
The social components of health have been a core component of the Bright Futures guidelines since their inception in 1994, but the upcoming 4th edition will more specifically incorporate social determinants of health as a visit priority for most of the recommended health supervision visits, he said.
Some of the other expected changes to Bright Futures address the following areas:
• Motor screening. Recommended developmental surveillance in the updated Bright Futures guidelines will for the first time include evaluation for motor delays, the importance of which was described in a 2013 AAP clinical report (Pediatrics. 2013 Jun;131[6]:e2016-27).
• Maternal depression screening. This was included in the 3rd edition as a selective screen, and was recommended by the AAP in a 2010 clinical report on recognition and management of perinatal and postpartum depression (Pediatrics. 2010 Nov;126[5]:1032-9). Finalization of a draft USPSTF statement recommending depression screening in mothers will give Bright Futures and the AAP the evidence it needs to incorporate this screening into the periodicity schedule.
• Safe sleep. Sleep in the parents’ room “for at least 6 months” will be recommended, as well as a move away from swaddling by 2 months of age. The latter is based on consensus opinion. “There’s no evidence, but there’s concern about safety [of swaddling],” Dr. Hagan said. “By the 1-month visit, we should be encouraging parents not to swaddle for sleep.”
• Iron supplementation. The AAP recommended in 2011 that exclusively breastfed infants should receive an iron supplement starting at 4 months, and the 4th edition of Bright Futures will highlight this. And as a reflection of “current best thinking,” the new edition will recommend advising parents that meat is a better source of iron than iron-fortified cereal. “We want to move it earlier in the nutritional schema,” Dr. Hagan said.
• Fluoride varnish. This procedure was integrated into the Periodicity Schedule in September 2015, with a recommendation from 6 months through 5 years of age, after having received a B-level recommendation by the USPSTF in 2014. The new Bright Futures edition will provide detail and guidance on this oral health service.
• HIV screening. The recommended window for universal one-time screening will be expanded from 16-18 years to 15-21 years, with the current recommendation for annual selective screening and an opt-out option remaining as is. The new window will be more consistent with recommendations of the Centers for Disease Control and Prevention and will better cover the middle-adolescent period of 15-17 years of age, Dr. Hagan said.
WASHINGTON – A new edition of the Bright Futures guidelines is scheduled for release in 2016, and among the expected changes are a recommendation for developmental screening at 4 years and an increased emphasis on the “social determinants of health.”
Revisions planned for the 4th edition of the Bright Futures Health Supervision Guidelines for Infants, Children, and Adolescents, including the American Academy of Pediatrics Periodicity Schedule, are notable not only because they reflect new evidence, but because the services recommended in the guidelines are required by the Affordable Care Act to be covered by insurers without any cost sharing, Dr. Joseph F. Hagan Jr., a pediatrician in Burlington, Vt., and coeditor of Bright Futures, said at the annual meeting of the American Academy of Pediatrics.
The current Recommendations for Preventive Pediatric Health Care – Periodicity Schedule – which represents a consensus of the Bright Futures advisory committee and the AAP – recommends standardized developmental screening at ages 9, 18, and 30 months, and autism screening at ages 18 and 24 months.
The expected addition of developmental screening to the 4-year health supervision visit will be in keeping with the tools most often utilized in pediatric practices, such as the Ages & Stages Questionnaires, which are validated for screening in children up to 5 years of age. “A lot can happen in 18 months [since the 30-month visit],” Dr. Hagan said.
In 2015 the U.S. Preventive Services Task Force assigned a “I” evidence rating to screening for speech and language delays and disorders in children aged 5 and younger, which means it found insufficient evidence to recommend for or against screening. Still, developmental screening meets a minimum standard for Bright Futures of being “evidence informed” in its recommendations for services and screening, Dr. Hagan said.
“We have tried to provide at least evidence-informed recommendations for the content each of the 31 visits you provide from birth to age 21,” he emphasized. Evidence was “important in the 3rd edition and it’s essential in the 4th. We must have a strong evidence base when we make a recommendation for something new that insurance companies will need to pay for.”
Outside of the Periodicity Schedule, Bright Futures offers recommendations for health promotion and anticipatory guidance, and some of these recommendations are consensus based rather than evidence based or evidence informed. However, a lack of evidence “doesn’t necessarily mean lack of efficacy,” he said at the meeting. “It usually reflects a lack of study in children.”
The updated guidelines – which, like previous versions, have been funded by the U.S. Department of Health and Human Services and will be published by the AAP – will include an expanded chapter on rationale and evidence for each recommendation so that “you can see transparently what we chose and why,” Dr. Hagan told this newspaper.
The social components of health have been a core component of the Bright Futures guidelines since their inception in 1994, but the upcoming 4th edition will more specifically incorporate social determinants of health as a visit priority for most of the recommended health supervision visits, he said.
Some of the other expected changes to Bright Futures address the following areas:
• Motor screening. Recommended developmental surveillance in the updated Bright Futures guidelines will for the first time include evaluation for motor delays, the importance of which was described in a 2013 AAP clinical report (Pediatrics. 2013 Jun;131[6]:e2016-27).
• Maternal depression screening. This was included in the 3rd edition as a selective screen, and was recommended by the AAP in a 2010 clinical report on recognition and management of perinatal and postpartum depression (Pediatrics. 2010 Nov;126[5]:1032-9). Finalization of a draft USPSTF statement recommending depression screening in mothers will give Bright Futures and the AAP the evidence it needs to incorporate this screening into the periodicity schedule.
• Safe sleep. Sleep in the parents’ room “for at least 6 months” will be recommended, as well as a move away from swaddling by 2 months of age. The latter is based on consensus opinion. “There’s no evidence, but there’s concern about safety [of swaddling],” Dr. Hagan said. “By the 1-month visit, we should be encouraging parents not to swaddle for sleep.”
• Iron supplementation. The AAP recommended in 2011 that exclusively breastfed infants should receive an iron supplement starting at 4 months, and the 4th edition of Bright Futures will highlight this. And as a reflection of “current best thinking,” the new edition will recommend advising parents that meat is a better source of iron than iron-fortified cereal. “We want to move it earlier in the nutritional schema,” Dr. Hagan said.
• Fluoride varnish. This procedure was integrated into the Periodicity Schedule in September 2015, with a recommendation from 6 months through 5 years of age, after having received a B-level recommendation by the USPSTF in 2014. The new Bright Futures edition will provide detail and guidance on this oral health service.
• HIV screening. The recommended window for universal one-time screening will be expanded from 16-18 years to 15-21 years, with the current recommendation for annual selective screening and an opt-out option remaining as is. The new window will be more consistent with recommendations of the Centers for Disease Control and Prevention and will better cover the middle-adolescent period of 15-17 years of age, Dr. Hagan said.
WASHINGTON – A new edition of the Bright Futures guidelines is scheduled for release in 2016, and among the expected changes are a recommendation for developmental screening at 4 years and an increased emphasis on the “social determinants of health.”
Revisions planned for the 4th edition of the Bright Futures Health Supervision Guidelines for Infants, Children, and Adolescents, including the American Academy of Pediatrics Periodicity Schedule, are notable not only because they reflect new evidence, but because the services recommended in the guidelines are required by the Affordable Care Act to be covered by insurers without any cost sharing, Dr. Joseph F. Hagan Jr., a pediatrician in Burlington, Vt., and coeditor of Bright Futures, said at the annual meeting of the American Academy of Pediatrics.
The current Recommendations for Preventive Pediatric Health Care – Periodicity Schedule – which represents a consensus of the Bright Futures advisory committee and the AAP – recommends standardized developmental screening at ages 9, 18, and 30 months, and autism screening at ages 18 and 24 months.
The expected addition of developmental screening to the 4-year health supervision visit will be in keeping with the tools most often utilized in pediatric practices, such as the Ages & Stages Questionnaires, which are validated for screening in children up to 5 years of age. “A lot can happen in 18 months [since the 30-month visit],” Dr. Hagan said.
In 2015 the U.S. Preventive Services Task Force assigned a “I” evidence rating to screening for speech and language delays and disorders in children aged 5 and younger, which means it found insufficient evidence to recommend for or against screening. Still, developmental screening meets a minimum standard for Bright Futures of being “evidence informed” in its recommendations for services and screening, Dr. Hagan said.
“We have tried to provide at least evidence-informed recommendations for the content each of the 31 visits you provide from birth to age 21,” he emphasized. Evidence was “important in the 3rd edition and it’s essential in the 4th. We must have a strong evidence base when we make a recommendation for something new that insurance companies will need to pay for.”
Outside of the Periodicity Schedule, Bright Futures offers recommendations for health promotion and anticipatory guidance, and some of these recommendations are consensus based rather than evidence based or evidence informed. However, a lack of evidence “doesn’t necessarily mean lack of efficacy,” he said at the meeting. “It usually reflects a lack of study in children.”
The updated guidelines – which, like previous versions, have been funded by the U.S. Department of Health and Human Services and will be published by the AAP – will include an expanded chapter on rationale and evidence for each recommendation so that “you can see transparently what we chose and why,” Dr. Hagan told this newspaper.
The social components of health have been a core component of the Bright Futures guidelines since their inception in 1994, but the upcoming 4th edition will more specifically incorporate social determinants of health as a visit priority for most of the recommended health supervision visits, he said.
Some of the other expected changes to Bright Futures address the following areas:
• Motor screening. Recommended developmental surveillance in the updated Bright Futures guidelines will for the first time include evaluation for motor delays, the importance of which was described in a 2013 AAP clinical report (Pediatrics. 2013 Jun;131[6]:e2016-27).
• Maternal depression screening. This was included in the 3rd edition as a selective screen, and was recommended by the AAP in a 2010 clinical report on recognition and management of perinatal and postpartum depression (Pediatrics. 2010 Nov;126[5]:1032-9). Finalization of a draft USPSTF statement recommending depression screening in mothers will give Bright Futures and the AAP the evidence it needs to incorporate this screening into the periodicity schedule.
• Safe sleep. Sleep in the parents’ room “for at least 6 months” will be recommended, as well as a move away from swaddling by 2 months of age. The latter is based on consensus opinion. “There’s no evidence, but there’s concern about safety [of swaddling],” Dr. Hagan said. “By the 1-month visit, we should be encouraging parents not to swaddle for sleep.”
• Iron supplementation. The AAP recommended in 2011 that exclusively breastfed infants should receive an iron supplement starting at 4 months, and the 4th edition of Bright Futures will highlight this. And as a reflection of “current best thinking,” the new edition will recommend advising parents that meat is a better source of iron than iron-fortified cereal. “We want to move it earlier in the nutritional schema,” Dr. Hagan said.
• Fluoride varnish. This procedure was integrated into the Periodicity Schedule in September 2015, with a recommendation from 6 months through 5 years of age, after having received a B-level recommendation by the USPSTF in 2014. The new Bright Futures edition will provide detail and guidance on this oral health service.
• HIV screening. The recommended window for universal one-time screening will be expanded from 16-18 years to 15-21 years, with the current recommendation for annual selective screening and an opt-out option remaining as is. The new window will be more consistent with recommendations of the Centers for Disease Control and Prevention and will better cover the middle-adolescent period of 15-17 years of age, Dr. Hagan said.
EXPERT ANALYSIS FROM THE AAP ANNUAL MEETING
AAP: Fluoride varnish is billable and implementable
WASHINGTON – With fluoride varnish treatments now on the Bright Futures periodicity schedule, reimbursement is attainable, and pediatricians can focus on integrating the 45- to 60-second procedure into their practices and strengthening their oral health messaging to families.
Pediatrician Melinda Clark and pediatric dentist Rocio B. Quiñonez teamed up at the annual meeting of the American Academy of Pediatrics to deliver this message and to show pediatricians through a hands-on workshop how simple and important fluoride varnishing and oral health counseling are to pediatric preventive care.
“We have to own a part of this,” said Dr. Clark of the Albany (N.Y.) Medical Center Pediatric Group. With the dental community overloaded and dental caries the most common chronic childhood disease, “we cannot just cut out the teeth from our medical prevention paradigm.”
Dental caries is five times more common than asthma and seven times more common than hay fever. One in four children begin kindergarten with a history of early childhood caries, and children with the disease are three times as likely to miss school. The disease can progress to local infections, systemic infection, and in rare cases, death.
In 2014, the U.S. Preventive Services Task Force (USPSTF) recommended that primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption. The USPSTF did not specifically recommend the frequency of application, but in a clinical report published later in 2014 on “Fluoride Use in Caries Prevention in the Primary Care Setting,” the American Academy of Pediatrics recommended fluoride varnish at least once every 6 months – and preferably every 3 months – starting at tooth emergence (Pediatrics. 2014 Sep;134[3]:626-33).
And in September 2015, fluoride varnish was added to the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents and integrated into the Bright Futures–AAP periodicity schedule.
Both the B recommendation given by the USPSTF to fluoride varnish application and inclusion in the Bright Futures periodicity schedule mean that it is required by the Affordable Care Act to be covered by insurers without out of pocket costs to the patient. Currently, 49 states are reimbursing physicians for fluoride varnish in the Medicaid population.
“It’s become the standard of care,” said Dr. Quiñonez of the division of pediatric dentistry at the University of North Carolina at Chapel Hill.
Fluoride varnish is a concentrated topical fluoride that sets on contact with saliva and helps prevent caries by enhancing remineralization and inhibiting bacterial enzymes. It has been shown to reduce decay by 30%-63%, depending on whether it is coupled with dental health counseling. The treatment has its greatest effect when applied before the onset of caries, but it also may help halt or reverse early carious lesions, which present as decalcified “white spot lesions” along the gum line.
“We have months, often times many months, to prevent disease and to intervene in the earliest stages [of childhood caries] … before children end up in the hospital or operating room,” said Dr. Clark, a former member of the AAP’s Section on Oral Health Executive Committee and a lead author of the AAP’s report on fluoride use.
She advised taking a systematic approach to applying the varnish. “I often apply it by arches [upper and lower, one dab per arch], as opposed to quadrants,” she said. “As long as you’re painting all the surfaces of every tooth with a thin layer of fluoride varnish, it’s an incredibly safe and effective procedure.”
“And you’ll get good at keeping the tongue out of the way using the gauze,” she said.
Varnish is best applied in infants and toddlers in a knee-to-knee format [provider-to-parent] with the child facing the parent and holding the parent’s hands, and the provider tipping the child into his or her lap. The teeth are dried first with a 2-inch gauze square. The fluoride is painted on with a brush provided with the varnish. Dr. Clark uses a head lamp as a light source so she has full use of both hands. Some providers use a dental mirror to increase visibility, but “I don’t find this necessary for most young children,” she said.
Questions about the safety of fluoride overall and fluoride varnish specifically “will come up” during discussions of oral health, Dr. Clark said. The only scientifically proven risk of fluoride is the development of fluorosis, which may occur if too much fluoride is ingested during the period of tooth and bone development, she said.
The small rise in plasma fluoride levels that can follow an application of fluoride varnish is comparable to ingesting a 1 mg fluoride tablet or brushing with fluoridated toothpaste, Dr. Clark said. Parents should be instructed not to brush the child’s teeth that evening or give any fluoride supplementation that day, if supplements are being used.
Not brushing teeth until the next morning also allows the varnish to stay on and continue depositing fluoride, she said. The child may eat, drink, and use a pacifier immediately after a varnish application. Hot, sticky, and crunchy foods should be avoided the same day.
The only contraindications to fluoride varnish are allergy to colophony/pine rosin, allergy to pine nuts, and ulcerative gingivitis/stomatitis or other open lesions. There are only three cases in the literature of side effects: one case of contact dermatitis and two cases of stomatitis. Colophony-free versions of fluoride varnish are available, Dr. Clark said.
Fluoride varnish is approved by the Food and Drug Administration as a cavity liner – not as a cavity prevention agent – but more than 110 studies and 40 clinical trials have documented its safety and effectiveness for cavity prevention, Dr. Clark reported. The 0.25 ml dose of varnish, which costs between $1 and $2, is the appropriate dose for children aged 4 years and under.Fluoride varnish is part of a bigger picture of oral health care in pediatrics – one that, first and foremost, involves “routinely asking if your patients have a dental home,” Dr. Clark said. The effectiveness of fluoride varnish is enhanced by regular discussions of oral health and counseling about risk factors for early childhood caries, such as frequent snacking and continual bottle or sippy cup use with fluid other than water.
Both Dr. Clark and Dr. Quiñonez urged pediatricians to take advantage of the parallels between obesity prevention and early childhood caries prevention nutritional messages (such as the risks of frequent juice and soda). And Dr. Clark suggested talking about bacteria and not just hygiene. “It sounds better to blame the evil bacteria than it does to blame poor hygiene, and that’s fine,” she said. “We can talk about how we’re going to keep the bacteria at bay.”
Dr. Quiñonez pointed out that children who were born premature or with low birth weights tend to have a higher prevalence of enamel defects and therefore are at greater risk of developing early childhood caries.
The AAP successfully advocated that fluoride varnish application be reimbursed as a separately reported service with use of the medical CPT code 99188. Use of the code to report fluoride varnish application by a physician or other qualified health professional took effect in January 2015. In some states, the dental code D1206 has been used with a V modifier specific to prophylactic fluoride administration for reimbursement through Medicaid and managed care. The modifier for use in ICD-10 is Z41.8.
“I’m in New York state, and we’ve been reimbursed $30 per fluoride varnish application (since 2009), and this includes risk assessment and counseling,” said Dr. Clark. “Some states pay in the single digits, and some pay in the high $50s.”
State by state information on payment and a host of practice tools and information on fluoride, fluoride varnish, and oral health risk assessment and counseling are available at the AAP’s Oral Health website. The site also provides links to each state’s AAP Chapter Oral Health Advocate who provides or coordinates education and training.
WASHINGTON – With fluoride varnish treatments now on the Bright Futures periodicity schedule, reimbursement is attainable, and pediatricians can focus on integrating the 45- to 60-second procedure into their practices and strengthening their oral health messaging to families.
Pediatrician Melinda Clark and pediatric dentist Rocio B. Quiñonez teamed up at the annual meeting of the American Academy of Pediatrics to deliver this message and to show pediatricians through a hands-on workshop how simple and important fluoride varnishing and oral health counseling are to pediatric preventive care.
“We have to own a part of this,” said Dr. Clark of the Albany (N.Y.) Medical Center Pediatric Group. With the dental community overloaded and dental caries the most common chronic childhood disease, “we cannot just cut out the teeth from our medical prevention paradigm.”
Dental caries is five times more common than asthma and seven times more common than hay fever. One in four children begin kindergarten with a history of early childhood caries, and children with the disease are three times as likely to miss school. The disease can progress to local infections, systemic infection, and in rare cases, death.
In 2014, the U.S. Preventive Services Task Force (USPSTF) recommended that primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption. The USPSTF did not specifically recommend the frequency of application, but in a clinical report published later in 2014 on “Fluoride Use in Caries Prevention in the Primary Care Setting,” the American Academy of Pediatrics recommended fluoride varnish at least once every 6 months – and preferably every 3 months – starting at tooth emergence (Pediatrics. 2014 Sep;134[3]:626-33).
And in September 2015, fluoride varnish was added to the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents and integrated into the Bright Futures–AAP periodicity schedule.
Both the B recommendation given by the USPSTF to fluoride varnish application and inclusion in the Bright Futures periodicity schedule mean that it is required by the Affordable Care Act to be covered by insurers without out of pocket costs to the patient. Currently, 49 states are reimbursing physicians for fluoride varnish in the Medicaid population.
“It’s become the standard of care,” said Dr. Quiñonez of the division of pediatric dentistry at the University of North Carolina at Chapel Hill.
Fluoride varnish is a concentrated topical fluoride that sets on contact with saliva and helps prevent caries by enhancing remineralization and inhibiting bacterial enzymes. It has been shown to reduce decay by 30%-63%, depending on whether it is coupled with dental health counseling. The treatment has its greatest effect when applied before the onset of caries, but it also may help halt or reverse early carious lesions, which present as decalcified “white spot lesions” along the gum line.
“We have months, often times many months, to prevent disease and to intervene in the earliest stages [of childhood caries] … before children end up in the hospital or operating room,” said Dr. Clark, a former member of the AAP’s Section on Oral Health Executive Committee and a lead author of the AAP’s report on fluoride use.
She advised taking a systematic approach to applying the varnish. “I often apply it by arches [upper and lower, one dab per arch], as opposed to quadrants,” she said. “As long as you’re painting all the surfaces of every tooth with a thin layer of fluoride varnish, it’s an incredibly safe and effective procedure.”
“And you’ll get good at keeping the tongue out of the way using the gauze,” she said.
Varnish is best applied in infants and toddlers in a knee-to-knee format [provider-to-parent] with the child facing the parent and holding the parent’s hands, and the provider tipping the child into his or her lap. The teeth are dried first with a 2-inch gauze square. The fluoride is painted on with a brush provided with the varnish. Dr. Clark uses a head lamp as a light source so she has full use of both hands. Some providers use a dental mirror to increase visibility, but “I don’t find this necessary for most young children,” she said.
Questions about the safety of fluoride overall and fluoride varnish specifically “will come up” during discussions of oral health, Dr. Clark said. The only scientifically proven risk of fluoride is the development of fluorosis, which may occur if too much fluoride is ingested during the period of tooth and bone development, she said.
The small rise in plasma fluoride levels that can follow an application of fluoride varnish is comparable to ingesting a 1 mg fluoride tablet or brushing with fluoridated toothpaste, Dr. Clark said. Parents should be instructed not to brush the child’s teeth that evening or give any fluoride supplementation that day, if supplements are being used.
Not brushing teeth until the next morning also allows the varnish to stay on and continue depositing fluoride, she said. The child may eat, drink, and use a pacifier immediately after a varnish application. Hot, sticky, and crunchy foods should be avoided the same day.
The only contraindications to fluoride varnish are allergy to colophony/pine rosin, allergy to pine nuts, and ulcerative gingivitis/stomatitis or other open lesions. There are only three cases in the literature of side effects: one case of contact dermatitis and two cases of stomatitis. Colophony-free versions of fluoride varnish are available, Dr. Clark said.
Fluoride varnish is approved by the Food and Drug Administration as a cavity liner – not as a cavity prevention agent – but more than 110 studies and 40 clinical trials have documented its safety and effectiveness for cavity prevention, Dr. Clark reported. The 0.25 ml dose of varnish, which costs between $1 and $2, is the appropriate dose for children aged 4 years and under.Fluoride varnish is part of a bigger picture of oral health care in pediatrics – one that, first and foremost, involves “routinely asking if your patients have a dental home,” Dr. Clark said. The effectiveness of fluoride varnish is enhanced by regular discussions of oral health and counseling about risk factors for early childhood caries, such as frequent snacking and continual bottle or sippy cup use with fluid other than water.
Both Dr. Clark and Dr. Quiñonez urged pediatricians to take advantage of the parallels between obesity prevention and early childhood caries prevention nutritional messages (such as the risks of frequent juice and soda). And Dr. Clark suggested talking about bacteria and not just hygiene. “It sounds better to blame the evil bacteria than it does to blame poor hygiene, and that’s fine,” she said. “We can talk about how we’re going to keep the bacteria at bay.”
Dr. Quiñonez pointed out that children who were born premature or with low birth weights tend to have a higher prevalence of enamel defects and therefore are at greater risk of developing early childhood caries.
The AAP successfully advocated that fluoride varnish application be reimbursed as a separately reported service with use of the medical CPT code 99188. Use of the code to report fluoride varnish application by a physician or other qualified health professional took effect in January 2015. In some states, the dental code D1206 has been used with a V modifier specific to prophylactic fluoride administration for reimbursement through Medicaid and managed care. The modifier for use in ICD-10 is Z41.8.
“I’m in New York state, and we’ve been reimbursed $30 per fluoride varnish application (since 2009), and this includes risk assessment and counseling,” said Dr. Clark. “Some states pay in the single digits, and some pay in the high $50s.”
State by state information on payment and a host of practice tools and information on fluoride, fluoride varnish, and oral health risk assessment and counseling are available at the AAP’s Oral Health website. The site also provides links to each state’s AAP Chapter Oral Health Advocate who provides or coordinates education and training.
WASHINGTON – With fluoride varnish treatments now on the Bright Futures periodicity schedule, reimbursement is attainable, and pediatricians can focus on integrating the 45- to 60-second procedure into their practices and strengthening their oral health messaging to families.
Pediatrician Melinda Clark and pediatric dentist Rocio B. Quiñonez teamed up at the annual meeting of the American Academy of Pediatrics to deliver this message and to show pediatricians through a hands-on workshop how simple and important fluoride varnishing and oral health counseling are to pediatric preventive care.
“We have to own a part of this,” said Dr. Clark of the Albany (N.Y.) Medical Center Pediatric Group. With the dental community overloaded and dental caries the most common chronic childhood disease, “we cannot just cut out the teeth from our medical prevention paradigm.”
Dental caries is five times more common than asthma and seven times more common than hay fever. One in four children begin kindergarten with a history of early childhood caries, and children with the disease are three times as likely to miss school. The disease can progress to local infections, systemic infection, and in rare cases, death.
In 2014, the U.S. Preventive Services Task Force (USPSTF) recommended that primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption. The USPSTF did not specifically recommend the frequency of application, but in a clinical report published later in 2014 on “Fluoride Use in Caries Prevention in the Primary Care Setting,” the American Academy of Pediatrics recommended fluoride varnish at least once every 6 months – and preferably every 3 months – starting at tooth emergence (Pediatrics. 2014 Sep;134[3]:626-33).
And in September 2015, fluoride varnish was added to the Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents and integrated into the Bright Futures–AAP periodicity schedule.
Both the B recommendation given by the USPSTF to fluoride varnish application and inclusion in the Bright Futures periodicity schedule mean that it is required by the Affordable Care Act to be covered by insurers without out of pocket costs to the patient. Currently, 49 states are reimbursing physicians for fluoride varnish in the Medicaid population.
“It’s become the standard of care,” said Dr. Quiñonez of the division of pediatric dentistry at the University of North Carolina at Chapel Hill.
Fluoride varnish is a concentrated topical fluoride that sets on contact with saliva and helps prevent caries by enhancing remineralization and inhibiting bacterial enzymes. It has been shown to reduce decay by 30%-63%, depending on whether it is coupled with dental health counseling. The treatment has its greatest effect when applied before the onset of caries, but it also may help halt or reverse early carious lesions, which present as decalcified “white spot lesions” along the gum line.
“We have months, often times many months, to prevent disease and to intervene in the earliest stages [of childhood caries] … before children end up in the hospital or operating room,” said Dr. Clark, a former member of the AAP’s Section on Oral Health Executive Committee and a lead author of the AAP’s report on fluoride use.
She advised taking a systematic approach to applying the varnish. “I often apply it by arches [upper and lower, one dab per arch], as opposed to quadrants,” she said. “As long as you’re painting all the surfaces of every tooth with a thin layer of fluoride varnish, it’s an incredibly safe and effective procedure.”
“And you’ll get good at keeping the tongue out of the way using the gauze,” she said.
Varnish is best applied in infants and toddlers in a knee-to-knee format [provider-to-parent] with the child facing the parent and holding the parent’s hands, and the provider tipping the child into his or her lap. The teeth are dried first with a 2-inch gauze square. The fluoride is painted on with a brush provided with the varnish. Dr. Clark uses a head lamp as a light source so she has full use of both hands. Some providers use a dental mirror to increase visibility, but “I don’t find this necessary for most young children,” she said.
Questions about the safety of fluoride overall and fluoride varnish specifically “will come up” during discussions of oral health, Dr. Clark said. The only scientifically proven risk of fluoride is the development of fluorosis, which may occur if too much fluoride is ingested during the period of tooth and bone development, she said.
The small rise in plasma fluoride levels that can follow an application of fluoride varnish is comparable to ingesting a 1 mg fluoride tablet or brushing with fluoridated toothpaste, Dr. Clark said. Parents should be instructed not to brush the child’s teeth that evening or give any fluoride supplementation that day, if supplements are being used.
Not brushing teeth until the next morning also allows the varnish to stay on and continue depositing fluoride, she said. The child may eat, drink, and use a pacifier immediately after a varnish application. Hot, sticky, and crunchy foods should be avoided the same day.
The only contraindications to fluoride varnish are allergy to colophony/pine rosin, allergy to pine nuts, and ulcerative gingivitis/stomatitis or other open lesions. There are only three cases in the literature of side effects: one case of contact dermatitis and two cases of stomatitis. Colophony-free versions of fluoride varnish are available, Dr. Clark said.
Fluoride varnish is approved by the Food and Drug Administration as a cavity liner – not as a cavity prevention agent – but more than 110 studies and 40 clinical trials have documented its safety and effectiveness for cavity prevention, Dr. Clark reported. The 0.25 ml dose of varnish, which costs between $1 and $2, is the appropriate dose for children aged 4 years and under.Fluoride varnish is part of a bigger picture of oral health care in pediatrics – one that, first and foremost, involves “routinely asking if your patients have a dental home,” Dr. Clark said. The effectiveness of fluoride varnish is enhanced by regular discussions of oral health and counseling about risk factors for early childhood caries, such as frequent snacking and continual bottle or sippy cup use with fluid other than water.
Both Dr. Clark and Dr. Quiñonez urged pediatricians to take advantage of the parallels between obesity prevention and early childhood caries prevention nutritional messages (such as the risks of frequent juice and soda). And Dr. Clark suggested talking about bacteria and not just hygiene. “It sounds better to blame the evil bacteria than it does to blame poor hygiene, and that’s fine,” she said. “We can talk about how we’re going to keep the bacteria at bay.”
Dr. Quiñonez pointed out that children who were born premature or with low birth weights tend to have a higher prevalence of enamel defects and therefore are at greater risk of developing early childhood caries.
The AAP successfully advocated that fluoride varnish application be reimbursed as a separately reported service with use of the medical CPT code 99188. Use of the code to report fluoride varnish application by a physician or other qualified health professional took effect in January 2015. In some states, the dental code D1206 has been used with a V modifier specific to prophylactic fluoride administration for reimbursement through Medicaid and managed care. The modifier for use in ICD-10 is Z41.8.
“I’m in New York state, and we’ve been reimbursed $30 per fluoride varnish application (since 2009), and this includes risk assessment and counseling,” said Dr. Clark. “Some states pay in the single digits, and some pay in the high $50s.”
State by state information on payment and a host of practice tools and information on fluoride, fluoride varnish, and oral health risk assessment and counseling are available at the AAP’s Oral Health website. The site also provides links to each state’s AAP Chapter Oral Health Advocate who provides or coordinates education and training.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Use ‘multiple layers’ to combat intimate partner violence
WASHINGTON – Pediatric practices can combat the toxic stress created by intimate partner violence – and often prevent child maltreatment – by providing “multiple layers of opportunity” for disclosure and access to resources, Dr. Kimberly Randell said at the annual meeting of the American Academy of Pediatrics.
Each year, approximately 15.5 million children – disproportionately younger children – are exposed to intimate partner violence (IPV) (J Fam Psychol. 2006;20[1]:137-42). Their mothers, IPV victims, will seek care for their children when they don’t seek care for themselves, and they will address IPV for their children, she said.
“These are women who are coming in for the 2-, 4-, 6-month visits, but haven’t seen their ob for the postpartum visit ,and they may not see their primary care physician for several more years,” said Dr. Randell, who coordinates the IPV program at Children’s Mercy Hospital in Kansas City, Mo. “They’ll address IPV in the context of how it affects their kids.”
Between 1 in 3 women and 1 in 4 men will experience intimate partner violence (IPV) at some point in their lifetime, according to The National Intimate Partner and Sexual Violence Survey 2010 Summary Report by the Centers for Disease Control and Prevention. Families experiencing IPV “look no different from families who aren’t,” making it worthwhile to universally screen for the problem as part of anticipatory guidance. There is no hard evidence favoring written or verbal assessment – “it all depends on what works best for your practice,” Dr. Randell said.
However, she implored pediatricians to line up advocacy resources, educate staff, and develop processes for intervention. “We know that if you just hand someone a pamphlet or a help line number and say ‘call when you’re ready,’ the odds are they’re not going to call,” Dr. Randell said.
Instead, tell the mother you would like to connect her with a community partner who specializes in IVP and can help her figure out a plan for her and her child’s safety. Ideally, a nurse or staff member in the pediatric office who is educated about IVP could be the initial link – someone “to whom you can make a warm hand-off.”
In this case, she explained, the pediatrician can “say something like, ‘I’d like you to talk with Jennifer. She knows a lot about situations like these and can offer some resources. We can even make the call from the office today.’ ”
Phone calls made from the office, when agreed to, are “very safe calls,” Dr. Randell emphasized.
Ideally, pediatric offices can partner with a local IPV agency for education and referrals. Other possibilities are the social work department at a local children’s hospital or the National Domestic Violence hot line (1-800-799-7233, 1-800-787-3224 TTY). Dr. Randell advised using the term “help line” instead of “hotline” because, in her experience, families associate a “hotline” with children “being taken away.”
Physicians worry about damaging trust by asking about IPV, but numerous studies show most mothers agree that pediatric health care providers should ask.
Introducing questions about IPV with a “framing statement” can minimize any perception of judgment. An example: “Because violence at home is common and affects children’s health and safety, I now ask all families in my practice about exposure to violence.”
The framing statement can then be followed with an indirect question such as “Do you feel safe at home and in your relationship?” or a more direct question, such as:
• “Has your child ever seen a violent or frightening event at home or in your neighborhood?”
• “Have you ever been hurt or threatened by your partner?”
• “Do you ever feel afraid of or controlled by or isolated by your partner?”
IPV is an adverse childhood experience that not only creates toxic stress, but puts children at significantly higher risk – up to 15 times the risk – for all forms of childhood maltreatment. Men also experience IPV, but women are most frequently the nonoffenders, she noted.
Pediatricians should know their states’ child abuse and IVP reporting laws, and inform the nonoffending parent of any limits on confidentiality. “If your state has mandatory reporting for exposure to IVP, you need to let the parent know,” she said. “They need to be able to take this into consideration when they’re deciding if it’s safe or the right time to disclose.”
Dr. Randell advised physicians to try to involve the parent when reporting IPV, either per mandatory reporting laws or per results of a child safety assessment. Explain that you’d like them to make the report with you,” she said. “This can be an important step in maintaining a trusting relationship and empowering her.”
Care must be taken in documenting IPV disclosure because the abusive parent often has access to the child’s chart and/or receives insurance statements. Dr. Randell offered several tips:
Use limited, coded documentation in the chart.
• Do not use IPV-related billing codes or mention the terms “domestic violence” or “IPV.”
• Do not use the word shelter or include notes about safety plans.
• Do not screen in the presence of verbal children, or children aged 3 years and older.
Children may inadvertently tell the abuser that mom has been talking to someone, she explained. “And it’s also probably bad for kids to hear mom denying [IPV] because it reinforces that this is a behavior that we keep secret and don’t talk about.”
Posters, pamphlets, and other environmental cues are an important layer for helping families who are experiencing IPV, largely because these items provide women with the opportunity to access resources without having to disclose IPV.
In focus groups at Children’s Mercy, mothers who had experienced or were experiencing IPV said they wanted information “not only on what IPV looks like … but about how it impacts kids, about resources, and about safety planning,” Dr. Randell said. “And they wanted things that are hopeful ... They don’t want to be labeled [as victims].”
There are several validated screening instruments for IPV (such as the Partner Violence Screen and the Woman Abuse Screening Tool), but the tools have significantly variable sensitivities and specificities and have not been studied in pediatric settings. General psychosocial screening tools used in pediatrics, such as the Pediatric Symptom Checklist and the Strengths and Difficulties Questionnaire, may provide clues of possible trauma, including IPV, she noted.
Among the resources recommended by Dr. Randell:
• The Harvard Center for the Developing Child (www.developingchild.harvard.edu).
• Futures Without Violence (www.futureswithoutviolence.org).
• AAP’s policy statement on IPV: pediatrics.aappublications.org/content/125/5/1094).
WASHINGTON – Pediatric practices can combat the toxic stress created by intimate partner violence – and often prevent child maltreatment – by providing “multiple layers of opportunity” for disclosure and access to resources, Dr. Kimberly Randell said at the annual meeting of the American Academy of Pediatrics.
Each year, approximately 15.5 million children – disproportionately younger children – are exposed to intimate partner violence (IPV) (J Fam Psychol. 2006;20[1]:137-42). Their mothers, IPV victims, will seek care for their children when they don’t seek care for themselves, and they will address IPV for their children, she said.
“These are women who are coming in for the 2-, 4-, 6-month visits, but haven’t seen their ob for the postpartum visit ,and they may not see their primary care physician for several more years,” said Dr. Randell, who coordinates the IPV program at Children’s Mercy Hospital in Kansas City, Mo. “They’ll address IPV in the context of how it affects their kids.”
Between 1 in 3 women and 1 in 4 men will experience intimate partner violence (IPV) at some point in their lifetime, according to The National Intimate Partner and Sexual Violence Survey 2010 Summary Report by the Centers for Disease Control and Prevention. Families experiencing IPV “look no different from families who aren’t,” making it worthwhile to universally screen for the problem as part of anticipatory guidance. There is no hard evidence favoring written or verbal assessment – “it all depends on what works best for your practice,” Dr. Randell said.
However, she implored pediatricians to line up advocacy resources, educate staff, and develop processes for intervention. “We know that if you just hand someone a pamphlet or a help line number and say ‘call when you’re ready,’ the odds are they’re not going to call,” Dr. Randell said.
Instead, tell the mother you would like to connect her with a community partner who specializes in IVP and can help her figure out a plan for her and her child’s safety. Ideally, a nurse or staff member in the pediatric office who is educated about IVP could be the initial link – someone “to whom you can make a warm hand-off.”
In this case, she explained, the pediatrician can “say something like, ‘I’d like you to talk with Jennifer. She knows a lot about situations like these and can offer some resources. We can even make the call from the office today.’ ”
Phone calls made from the office, when agreed to, are “very safe calls,” Dr. Randell emphasized.
Ideally, pediatric offices can partner with a local IPV agency for education and referrals. Other possibilities are the social work department at a local children’s hospital or the National Domestic Violence hot line (1-800-799-7233, 1-800-787-3224 TTY). Dr. Randell advised using the term “help line” instead of “hotline” because, in her experience, families associate a “hotline” with children “being taken away.”
Physicians worry about damaging trust by asking about IPV, but numerous studies show most mothers agree that pediatric health care providers should ask.
Introducing questions about IPV with a “framing statement” can minimize any perception of judgment. An example: “Because violence at home is common and affects children’s health and safety, I now ask all families in my practice about exposure to violence.”
The framing statement can then be followed with an indirect question such as “Do you feel safe at home and in your relationship?” or a more direct question, such as:
• “Has your child ever seen a violent or frightening event at home or in your neighborhood?”
• “Have you ever been hurt or threatened by your partner?”
• “Do you ever feel afraid of or controlled by or isolated by your partner?”
IPV is an adverse childhood experience that not only creates toxic stress, but puts children at significantly higher risk – up to 15 times the risk – for all forms of childhood maltreatment. Men also experience IPV, but women are most frequently the nonoffenders, she noted.
Pediatricians should know their states’ child abuse and IVP reporting laws, and inform the nonoffending parent of any limits on confidentiality. “If your state has mandatory reporting for exposure to IVP, you need to let the parent know,” she said. “They need to be able to take this into consideration when they’re deciding if it’s safe or the right time to disclose.”
Dr. Randell advised physicians to try to involve the parent when reporting IPV, either per mandatory reporting laws or per results of a child safety assessment. Explain that you’d like them to make the report with you,” she said. “This can be an important step in maintaining a trusting relationship and empowering her.”
Care must be taken in documenting IPV disclosure because the abusive parent often has access to the child’s chart and/or receives insurance statements. Dr. Randell offered several tips:
Use limited, coded documentation in the chart.
• Do not use IPV-related billing codes or mention the terms “domestic violence” or “IPV.”
• Do not use the word shelter or include notes about safety plans.
• Do not screen in the presence of verbal children, or children aged 3 years and older.
Children may inadvertently tell the abuser that mom has been talking to someone, she explained. “And it’s also probably bad for kids to hear mom denying [IPV] because it reinforces that this is a behavior that we keep secret and don’t talk about.”
Posters, pamphlets, and other environmental cues are an important layer for helping families who are experiencing IPV, largely because these items provide women with the opportunity to access resources without having to disclose IPV.
In focus groups at Children’s Mercy, mothers who had experienced or were experiencing IPV said they wanted information “not only on what IPV looks like … but about how it impacts kids, about resources, and about safety planning,” Dr. Randell said. “And they wanted things that are hopeful ... They don’t want to be labeled [as victims].”
There are several validated screening instruments for IPV (such as the Partner Violence Screen and the Woman Abuse Screening Tool), but the tools have significantly variable sensitivities and specificities and have not been studied in pediatric settings. General psychosocial screening tools used in pediatrics, such as the Pediatric Symptom Checklist and the Strengths and Difficulties Questionnaire, may provide clues of possible trauma, including IPV, she noted.
Among the resources recommended by Dr. Randell:
• The Harvard Center for the Developing Child (www.developingchild.harvard.edu).
• Futures Without Violence (www.futureswithoutviolence.org).
• AAP’s policy statement on IPV: pediatrics.aappublications.org/content/125/5/1094).
WASHINGTON – Pediatric practices can combat the toxic stress created by intimate partner violence – and often prevent child maltreatment – by providing “multiple layers of opportunity” for disclosure and access to resources, Dr. Kimberly Randell said at the annual meeting of the American Academy of Pediatrics.
Each year, approximately 15.5 million children – disproportionately younger children – are exposed to intimate partner violence (IPV) (J Fam Psychol. 2006;20[1]:137-42). Their mothers, IPV victims, will seek care for their children when they don’t seek care for themselves, and they will address IPV for their children, she said.
“These are women who are coming in for the 2-, 4-, 6-month visits, but haven’t seen their ob for the postpartum visit ,and they may not see their primary care physician for several more years,” said Dr. Randell, who coordinates the IPV program at Children’s Mercy Hospital in Kansas City, Mo. “They’ll address IPV in the context of how it affects their kids.”
Between 1 in 3 women and 1 in 4 men will experience intimate partner violence (IPV) at some point in their lifetime, according to The National Intimate Partner and Sexual Violence Survey 2010 Summary Report by the Centers for Disease Control and Prevention. Families experiencing IPV “look no different from families who aren’t,” making it worthwhile to universally screen for the problem as part of anticipatory guidance. There is no hard evidence favoring written or verbal assessment – “it all depends on what works best for your practice,” Dr. Randell said.
However, she implored pediatricians to line up advocacy resources, educate staff, and develop processes for intervention. “We know that if you just hand someone a pamphlet or a help line number and say ‘call when you’re ready,’ the odds are they’re not going to call,” Dr. Randell said.
Instead, tell the mother you would like to connect her with a community partner who specializes in IVP and can help her figure out a plan for her and her child’s safety. Ideally, a nurse or staff member in the pediatric office who is educated about IVP could be the initial link – someone “to whom you can make a warm hand-off.”
In this case, she explained, the pediatrician can “say something like, ‘I’d like you to talk with Jennifer. She knows a lot about situations like these and can offer some resources. We can even make the call from the office today.’ ”
Phone calls made from the office, when agreed to, are “very safe calls,” Dr. Randell emphasized.
Ideally, pediatric offices can partner with a local IPV agency for education and referrals. Other possibilities are the social work department at a local children’s hospital or the National Domestic Violence hot line (1-800-799-7233, 1-800-787-3224 TTY). Dr. Randell advised using the term “help line” instead of “hotline” because, in her experience, families associate a “hotline” with children “being taken away.”
Physicians worry about damaging trust by asking about IPV, but numerous studies show most mothers agree that pediatric health care providers should ask.
Introducing questions about IPV with a “framing statement” can minimize any perception of judgment. An example: “Because violence at home is common and affects children’s health and safety, I now ask all families in my practice about exposure to violence.”
The framing statement can then be followed with an indirect question such as “Do you feel safe at home and in your relationship?” or a more direct question, such as:
• “Has your child ever seen a violent or frightening event at home or in your neighborhood?”
• “Have you ever been hurt or threatened by your partner?”
• “Do you ever feel afraid of or controlled by or isolated by your partner?”
IPV is an adverse childhood experience that not only creates toxic stress, but puts children at significantly higher risk – up to 15 times the risk – for all forms of childhood maltreatment. Men also experience IPV, but women are most frequently the nonoffenders, she noted.
Pediatricians should know their states’ child abuse and IVP reporting laws, and inform the nonoffending parent of any limits on confidentiality. “If your state has mandatory reporting for exposure to IVP, you need to let the parent know,” she said. “They need to be able to take this into consideration when they’re deciding if it’s safe or the right time to disclose.”
Dr. Randell advised physicians to try to involve the parent when reporting IPV, either per mandatory reporting laws or per results of a child safety assessment. Explain that you’d like them to make the report with you,” she said. “This can be an important step in maintaining a trusting relationship and empowering her.”
Care must be taken in documenting IPV disclosure because the abusive parent often has access to the child’s chart and/or receives insurance statements. Dr. Randell offered several tips:
Use limited, coded documentation in the chart.
• Do not use IPV-related billing codes or mention the terms “domestic violence” or “IPV.”
• Do not use the word shelter or include notes about safety plans.
• Do not screen in the presence of verbal children, or children aged 3 years and older.
Children may inadvertently tell the abuser that mom has been talking to someone, she explained. “And it’s also probably bad for kids to hear mom denying [IPV] because it reinforces that this is a behavior that we keep secret and don’t talk about.”
Posters, pamphlets, and other environmental cues are an important layer for helping families who are experiencing IPV, largely because these items provide women with the opportunity to access resources without having to disclose IPV.
In focus groups at Children’s Mercy, mothers who had experienced or were experiencing IPV said they wanted information “not only on what IPV looks like … but about how it impacts kids, about resources, and about safety planning,” Dr. Randell said. “And they wanted things that are hopeful ... They don’t want to be labeled [as victims].”
There are several validated screening instruments for IPV (such as the Partner Violence Screen and the Woman Abuse Screening Tool), but the tools have significantly variable sensitivities and specificities and have not been studied in pediatric settings. General psychosocial screening tools used in pediatrics, such as the Pediatric Symptom Checklist and the Strengths and Difficulties Questionnaire, may provide clues of possible trauma, including IPV, she noted.
Among the resources recommended by Dr. Randell:
• The Harvard Center for the Developing Child (www.developingchild.harvard.edu).
• Futures Without Violence (www.futureswithoutviolence.org).
• AAP’s policy statement on IPV: pediatrics.aappublications.org/content/125/5/1094).
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Creating safe environment aids recovery from trauma disorders
WASHINGTON – Maintaining safety and helping to ensure caregiver well-being are critical interventions for children with posttraumatic stress disorder (PTSD) and other trauma syndromes, Dr. Mary Margaret Gleason said at the annual meeting of the American Academy of Pediatrics.
“Talk a lot [with caregivers] about safety, meaning the [importance of a] lack of violence in the home and the lack of corporal punishment,” said Dr. Gleason, a pediatrician and child and adolescent psychiatrist at Tulane University in New Orleans. “And equally important, make sure that parents are taking care of themselves and are getting treatment [if they’ve also experienced trauma].”
PTSD must be treated with evidence-based therapy or it will become more entrenched with time, she said. Both child-parent psychotherapy in toddlers and preschool-aged children, and cognitive behavioral therapy (CBT) in children of preschool age and up, lead to short-term and sustained reductions in children’s symptoms.
In communities without treatment specialists and resources, stressing safety becomes even more important. Help children with PTSD and other trauma disorders to learn to recognize and label their feelings, manage emotional dysregulation, learn the principles of CBT, and achieve deep relaxation. “You can put a pulse oximeter on a child and teach them how to do deep relaxation,” she said. “You can challenge them to bring down the numbers.”
Books on CBT for general anxiety – and, increasingly, online CBT tools – can be helpful for some families, as can the National Child Traumatic Stress Network’s online resources (www.nctsn.org).
Dr. Gleason advised looking for a broad range of disorders in children who have experienced trauma – whether the trauma is acute or chronic, and whether it involves personal or community events. “You need to be thinking about PTSD, certainly, but also attention-deficit/hyperactivity disorder (ADHD), disruptive behaviors, mood disorders, separation anxiety disorders, and sleep disorders,” she said. Conversely, “if a child develops another disorder after a traumatic event, look for signs of PTSD.”
A study of children living in and around New Orleans when Hurricane Katrina struck in 2005 found a wide range of disorders as well as high prevalence of PTSD. “There were [few] children who developed new diagnoses who didn’t also have some symptoms of PTSD,” Dr. Gleason said.
The Diagnostic and Statistical Manual of Mental Disorders–5 placed PTSD in the diagnostic category of trauma- and stressor-related disorders and included separate criteria for PTSD in preschool children. PTSD broadly involves symptoms of at least 1-month duration from four symptom clusters: Intrusive thoughts (e.g. distressing dreams), avoidance, negative alterations in cognition and mood, and changed arousal and reactivity.
Preschool PTSD applies to children ages 6 years and younger, and requires fewer symptoms to be present. The arousal/reactivity symptoms cluster includes irritability and extreme tantrums, she noted.
For children of any age, it is important to note that distressing dreams do not have to involve content specific to the traumatic event to meet diagnostic criteria, Dr. Gleason said.
Compared with PTSD, less is known about the presentation in school-age children and adolescents of reactive attachment disorder (RAD) and disinhibited social engagement disorder (DSED) – two other trauma-related disorders in DSM-5. Both are related to the attachment system and require a developmental age of at least 9 months, and both involve “pathogenic care,” which can mean emotional neglect and/or persistent disregard of the child’s basic physical needs.
The child with RAD “rarely seeks comfort” when distressed, has a limited response to comfort, and has limited positive affect, Dr. Gleason explained.
“When they fall and hurt their knee, or when they build a tower and it falls over, they don’t look for anyone to help them organize their feelings. And when someone tries to help them, this doesn’t reduce their distress,” she said.
There is some overlap with the clinical presentation of autism spectrum disorder, so it is important to rule out ASD in diagnosing RAD.
Treatment, she said, entails placement in an adequate caregiving environment. “What’s really important to know about RAD is that it’s really a reflection of the current caregiving environment,” Dr. Gleason said. “It’s not about the history. It’s about the [trauma] of what’s happening now.”
DSED is quite different in its clinical construct and course. “These children are indiscriminately social,” she said. “They’ll go off with a stranger … off into new situations without ever looking back to see if their caregiver is there.”
Unlike RAD, this disorder is not associated with current caregiving quality. “It’s important for caregivers to know that this syndrome is a reflection of what happened earlier and not what’s happening now,” Dr. Gleason said. “And it does respond to quality caregiving, but very, very slowly. It can take years.”
Dr. Gleason reported that she has no relevant financial disclosures.
WASHINGTON – Maintaining safety and helping to ensure caregiver well-being are critical interventions for children with posttraumatic stress disorder (PTSD) and other trauma syndromes, Dr. Mary Margaret Gleason said at the annual meeting of the American Academy of Pediatrics.
“Talk a lot [with caregivers] about safety, meaning the [importance of a] lack of violence in the home and the lack of corporal punishment,” said Dr. Gleason, a pediatrician and child and adolescent psychiatrist at Tulane University in New Orleans. “And equally important, make sure that parents are taking care of themselves and are getting treatment [if they’ve also experienced trauma].”
PTSD must be treated with evidence-based therapy or it will become more entrenched with time, she said. Both child-parent psychotherapy in toddlers and preschool-aged children, and cognitive behavioral therapy (CBT) in children of preschool age and up, lead to short-term and sustained reductions in children’s symptoms.
In communities without treatment specialists and resources, stressing safety becomes even more important. Help children with PTSD and other trauma disorders to learn to recognize and label their feelings, manage emotional dysregulation, learn the principles of CBT, and achieve deep relaxation. “You can put a pulse oximeter on a child and teach them how to do deep relaxation,” she said. “You can challenge them to bring down the numbers.”
Books on CBT for general anxiety – and, increasingly, online CBT tools – can be helpful for some families, as can the National Child Traumatic Stress Network’s online resources (www.nctsn.org).
Dr. Gleason advised looking for a broad range of disorders in children who have experienced trauma – whether the trauma is acute or chronic, and whether it involves personal or community events. “You need to be thinking about PTSD, certainly, but also attention-deficit/hyperactivity disorder (ADHD), disruptive behaviors, mood disorders, separation anxiety disorders, and sleep disorders,” she said. Conversely, “if a child develops another disorder after a traumatic event, look for signs of PTSD.”
A study of children living in and around New Orleans when Hurricane Katrina struck in 2005 found a wide range of disorders as well as high prevalence of PTSD. “There were [few] children who developed new diagnoses who didn’t also have some symptoms of PTSD,” Dr. Gleason said.
The Diagnostic and Statistical Manual of Mental Disorders–5 placed PTSD in the diagnostic category of trauma- and stressor-related disorders and included separate criteria for PTSD in preschool children. PTSD broadly involves symptoms of at least 1-month duration from four symptom clusters: Intrusive thoughts (e.g. distressing dreams), avoidance, negative alterations in cognition and mood, and changed arousal and reactivity.
Preschool PTSD applies to children ages 6 years and younger, and requires fewer symptoms to be present. The arousal/reactivity symptoms cluster includes irritability and extreme tantrums, she noted.
For children of any age, it is important to note that distressing dreams do not have to involve content specific to the traumatic event to meet diagnostic criteria, Dr. Gleason said.
Compared with PTSD, less is known about the presentation in school-age children and adolescents of reactive attachment disorder (RAD) and disinhibited social engagement disorder (DSED) – two other trauma-related disorders in DSM-5. Both are related to the attachment system and require a developmental age of at least 9 months, and both involve “pathogenic care,” which can mean emotional neglect and/or persistent disregard of the child’s basic physical needs.
The child with RAD “rarely seeks comfort” when distressed, has a limited response to comfort, and has limited positive affect, Dr. Gleason explained.
“When they fall and hurt their knee, or when they build a tower and it falls over, they don’t look for anyone to help them organize their feelings. And when someone tries to help them, this doesn’t reduce their distress,” she said.
There is some overlap with the clinical presentation of autism spectrum disorder, so it is important to rule out ASD in diagnosing RAD.
Treatment, she said, entails placement in an adequate caregiving environment. “What’s really important to know about RAD is that it’s really a reflection of the current caregiving environment,” Dr. Gleason said. “It’s not about the history. It’s about the [trauma] of what’s happening now.”
DSED is quite different in its clinical construct and course. “These children are indiscriminately social,” she said. “They’ll go off with a stranger … off into new situations without ever looking back to see if their caregiver is there.”
Unlike RAD, this disorder is not associated with current caregiving quality. “It’s important for caregivers to know that this syndrome is a reflection of what happened earlier and not what’s happening now,” Dr. Gleason said. “And it does respond to quality caregiving, but very, very slowly. It can take years.”
Dr. Gleason reported that she has no relevant financial disclosures.
WASHINGTON – Maintaining safety and helping to ensure caregiver well-being are critical interventions for children with posttraumatic stress disorder (PTSD) and other trauma syndromes, Dr. Mary Margaret Gleason said at the annual meeting of the American Academy of Pediatrics.
“Talk a lot [with caregivers] about safety, meaning the [importance of a] lack of violence in the home and the lack of corporal punishment,” said Dr. Gleason, a pediatrician and child and adolescent psychiatrist at Tulane University in New Orleans. “And equally important, make sure that parents are taking care of themselves and are getting treatment [if they’ve also experienced trauma].”
PTSD must be treated with evidence-based therapy or it will become more entrenched with time, she said. Both child-parent psychotherapy in toddlers and preschool-aged children, and cognitive behavioral therapy (CBT) in children of preschool age and up, lead to short-term and sustained reductions in children’s symptoms.
In communities without treatment specialists and resources, stressing safety becomes even more important. Help children with PTSD and other trauma disorders to learn to recognize and label their feelings, manage emotional dysregulation, learn the principles of CBT, and achieve deep relaxation. “You can put a pulse oximeter on a child and teach them how to do deep relaxation,” she said. “You can challenge them to bring down the numbers.”
Books on CBT for general anxiety – and, increasingly, online CBT tools – can be helpful for some families, as can the National Child Traumatic Stress Network’s online resources (www.nctsn.org).
Dr. Gleason advised looking for a broad range of disorders in children who have experienced trauma – whether the trauma is acute or chronic, and whether it involves personal or community events. “You need to be thinking about PTSD, certainly, but also attention-deficit/hyperactivity disorder (ADHD), disruptive behaviors, mood disorders, separation anxiety disorders, and sleep disorders,” she said. Conversely, “if a child develops another disorder after a traumatic event, look for signs of PTSD.”
A study of children living in and around New Orleans when Hurricane Katrina struck in 2005 found a wide range of disorders as well as high prevalence of PTSD. “There were [few] children who developed new diagnoses who didn’t also have some symptoms of PTSD,” Dr. Gleason said.
The Diagnostic and Statistical Manual of Mental Disorders–5 placed PTSD in the diagnostic category of trauma- and stressor-related disorders and included separate criteria for PTSD in preschool children. PTSD broadly involves symptoms of at least 1-month duration from four symptom clusters: Intrusive thoughts (e.g. distressing dreams), avoidance, negative alterations in cognition and mood, and changed arousal and reactivity.
Preschool PTSD applies to children ages 6 years and younger, and requires fewer symptoms to be present. The arousal/reactivity symptoms cluster includes irritability and extreme tantrums, she noted.
For children of any age, it is important to note that distressing dreams do not have to involve content specific to the traumatic event to meet diagnostic criteria, Dr. Gleason said.
Compared with PTSD, less is known about the presentation in school-age children and adolescents of reactive attachment disorder (RAD) and disinhibited social engagement disorder (DSED) – two other trauma-related disorders in DSM-5. Both are related to the attachment system and require a developmental age of at least 9 months, and both involve “pathogenic care,” which can mean emotional neglect and/or persistent disregard of the child’s basic physical needs.
The child with RAD “rarely seeks comfort” when distressed, has a limited response to comfort, and has limited positive affect, Dr. Gleason explained.
“When they fall and hurt their knee, or when they build a tower and it falls over, they don’t look for anyone to help them organize their feelings. And when someone tries to help them, this doesn’t reduce their distress,” she said.
There is some overlap with the clinical presentation of autism spectrum disorder, so it is important to rule out ASD in diagnosing RAD.
Treatment, she said, entails placement in an adequate caregiving environment. “What’s really important to know about RAD is that it’s really a reflection of the current caregiving environment,” Dr. Gleason said. “It’s not about the history. It’s about the [trauma] of what’s happening now.”
DSED is quite different in its clinical construct and course. “These children are indiscriminately social,” she said. “They’ll go off with a stranger … off into new situations without ever looking back to see if their caregiver is there.”
Unlike RAD, this disorder is not associated with current caregiving quality. “It’s important for caregivers to know that this syndrome is a reflection of what happened earlier and not what’s happening now,” Dr. Gleason said. “And it does respond to quality caregiving, but very, very slowly. It can take years.”
Dr. Gleason reported that she has no relevant financial disclosures.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Treat corporal punishment as a risk factor
WASHINGTON – The legal definition of what constitutes “reasonable” corporal punishment is contracting, making it more critical than ever to inquire about discipline, provide alternatives to corporal punishment, and address religious objections with culturally sensitive responses.
In delivering this message, Victor I. Vieth, J.D., founder and senior director of the Gundersen National Child Protection Training Center in La Crosse, Wisc., stressed that spanking and other forms of corporal punishment are still widely practiced, and that the many parents who employ this form of discipline are open to considering alternatives that they can learn and believe in.
“The vast majority of parents are doing the best they know how. … They don’t know the alternatives,” Mr. Vieth said.
“Reasonable” corporal punishment is lawful in all 50 states, but the definition of reasonable is narrowing. Courts now will consider the child’s size, frowning upon such punishment for children under the age of 2 years. They will consider where on the body the child is hit, generally viewing anything but the buttocks as unreasonable, and they’ll look at whether objects have been used.
Courts even appear willing today to consider the “nature of the child’s misbehavior,” which “opens the door to even mild corporal punishment cases sometimes being considered unlawful,” such as a parent hitting a child on the buttocks once or twice after milk is spilled, said Mr. Vieth, whose training center oversees a Center for Effective Discipline.
“Think about this as a mandatory reporter,” he said at the annual meeting of the American Academy of Pediatrics. “The vast majority of corporal punishment cases we see probably are running afoul of criminal or civil codes today.”
Shifts in case law are likely being driven by research showing that corporal punishment is a risk factor for both short-term and long-term physical and mental injury, he said. It has long been known that even mild forms of physical abuse – what’s been called “ordinary” physical punishment – can cause negative behavioral and psychological outcomes such as alcohol abuse, depression, behavioral problems, and low achievement.
More recent research has expanded the toll, linking acts such as pushing, grabbing, shoving, slapping, and hitting not only with higher risks of mental disorders and family dysfunction, but with higher risks of cardiovascular disease, arthritis, and obesity.
Ask parents about what form of discipline they’re using, and educate parents who indicate using corporal punishment about the medical risks and mental health risks in the short and long term. It’s important to then give parents “practical, concrete” tools that model alternative methods. Vanderbilt University’s Play Nicely free online parenting program is one that Mr. Vieth often recommends.
The parental response of “my parents hit me and I turned out just fine” is not uncommon, and it can be handled in various ways, he said.
You could segue into a discussion of risks by saying, for example, “Well, let’s explore that. I’ve known you for a long time, and I think you did turn out well. And that’s consistent with the research because the research doesn’t show that if you receive corporal punishment, you’re going to grow up to have negative outcomes. The research says that it’s a risk factor, and the more you hit and the longer you hit, the greater the risk will be.”
You also could compare corporal punishment research to research on smoking, Mr. Vieth said, by saying, “It’s not that different from smoking. One cigarette in the back of the school house won’t kill you, but two packs a day will dramatically increase the risk.”
Religion is a top reason – if not the No. 1 reason – for the use of corporal punishment, and it’s important to understand its influence on discipline and to develop culturally sensitive responses to parents who object for religious reasons to alternative approaches, Mr. Vieth said.
He recommended the following strategies when a parent cites religious grounds for physical discipline:
• Be aware of your own biases. Do not automatically label parents as neglectful or abusive.
• Refrain from pastoral work. “Assure the parent that you’re not trying to take away her religious beliefs, that you’re discussing religion because she’s speaking about discipline that must fit within her belief system.”
• Ask if the belief system “authorizes” or “requires” corporal punishment. If it is authorized, there’s a clear basis for working together.
• Try to distinguish between parents who need education and those who should be prosecuted. Some parents may accept and use corporal punishment, but may be amenable to discussion and education.
• Emphasize the patient’s strengths. Parental warmth, for instance, does not negate the risks of corporal punishment, but it can be a good foundation.
• Acknowledge the benefits of religion, such as its promotion of well-being and healthy behavior.
• Recognize the value of discipline and emphasize that you’re advocating for “effective” discipline with the fewest risk factors.
• “Play in the parent’s ball field.” If the parent believes she is God’s representative to the child, consider asking questions such as “What is your child learning about God when you hit her? What did you learn about God from being physically disciplined?” Parents often will pause and reflect.
Mr. Vieth told the story of Carol, a deeply religious single mother who was raised in a home with corporal discipline and who believed that God’s word in her Protestant faith told her that she must sometimes hit her 3-year-old son with an object. She confessed to a coworker that she was paddling her son on the buttocks, but did not like doing so and was scared of hurting him.
Carol’s coworker called Child Protective Services. The subsequent multidisciplinary team investigation chose not to file criminal charges, but to file a civil child protection petition. Carol pledged to improve her parenting, but was unwilling to forgo the practice altogether. Over time, it became apparent to the team working with Carol that she was heavily influenced by James Dobson, Ph.D., the founder of an organization called Focus on the Family. Unlike other more extreme advocates of corporal punishment, Dr. Dobson caps the number of spanks at two, with one for lesser infractions, and says spanking must never leave a bruise or injury (“From Sticks to Flowers: Guidelines for Child Protection Professionals Working with Parents Using Scripture to Justify Corporal Punishment,” [St. Paul, Minn.: William Mitchell Law Review, 2014, p. 923]), Mr. Vieth noted.
“For Carol, his views trumped all medical and health research,” Mr. Vieth said. “We had to figure out a way to play in her court.” Working with a social worker, he found passages in Dobson’s writing that conveyed the message that not every child needs corporal punishment.
“Once I started quoting Dobson, it changed the dynamic” and the team was able to work with her on embracing and learning alternative approaches. The petition was dropped, and Carol now is an advocate in her church for discipline methods other than corporal punishment.
Mr. Vieth reported having no relevant financial disclosures.
WASHINGTON – The legal definition of what constitutes “reasonable” corporal punishment is contracting, making it more critical than ever to inquire about discipline, provide alternatives to corporal punishment, and address religious objections with culturally sensitive responses.
In delivering this message, Victor I. Vieth, J.D., founder and senior director of the Gundersen National Child Protection Training Center in La Crosse, Wisc., stressed that spanking and other forms of corporal punishment are still widely practiced, and that the many parents who employ this form of discipline are open to considering alternatives that they can learn and believe in.
“The vast majority of parents are doing the best they know how. … They don’t know the alternatives,” Mr. Vieth said.
“Reasonable” corporal punishment is lawful in all 50 states, but the definition of reasonable is narrowing. Courts now will consider the child’s size, frowning upon such punishment for children under the age of 2 years. They will consider where on the body the child is hit, generally viewing anything but the buttocks as unreasonable, and they’ll look at whether objects have been used.
Courts even appear willing today to consider the “nature of the child’s misbehavior,” which “opens the door to even mild corporal punishment cases sometimes being considered unlawful,” such as a parent hitting a child on the buttocks once or twice after milk is spilled, said Mr. Vieth, whose training center oversees a Center for Effective Discipline.
“Think about this as a mandatory reporter,” he said at the annual meeting of the American Academy of Pediatrics. “The vast majority of corporal punishment cases we see probably are running afoul of criminal or civil codes today.”
Shifts in case law are likely being driven by research showing that corporal punishment is a risk factor for both short-term and long-term physical and mental injury, he said. It has long been known that even mild forms of physical abuse – what’s been called “ordinary” physical punishment – can cause negative behavioral and psychological outcomes such as alcohol abuse, depression, behavioral problems, and low achievement.
More recent research has expanded the toll, linking acts such as pushing, grabbing, shoving, slapping, and hitting not only with higher risks of mental disorders and family dysfunction, but with higher risks of cardiovascular disease, arthritis, and obesity.
Ask parents about what form of discipline they’re using, and educate parents who indicate using corporal punishment about the medical risks and mental health risks in the short and long term. It’s important to then give parents “practical, concrete” tools that model alternative methods. Vanderbilt University’s Play Nicely free online parenting program is one that Mr. Vieth often recommends.
The parental response of “my parents hit me and I turned out just fine” is not uncommon, and it can be handled in various ways, he said.
You could segue into a discussion of risks by saying, for example, “Well, let’s explore that. I’ve known you for a long time, and I think you did turn out well. And that’s consistent with the research because the research doesn’t show that if you receive corporal punishment, you’re going to grow up to have negative outcomes. The research says that it’s a risk factor, and the more you hit and the longer you hit, the greater the risk will be.”
You also could compare corporal punishment research to research on smoking, Mr. Vieth said, by saying, “It’s not that different from smoking. One cigarette in the back of the school house won’t kill you, but two packs a day will dramatically increase the risk.”
Religion is a top reason – if not the No. 1 reason – for the use of corporal punishment, and it’s important to understand its influence on discipline and to develop culturally sensitive responses to parents who object for religious reasons to alternative approaches, Mr. Vieth said.
He recommended the following strategies when a parent cites religious grounds for physical discipline:
• Be aware of your own biases. Do not automatically label parents as neglectful or abusive.
• Refrain from pastoral work. “Assure the parent that you’re not trying to take away her religious beliefs, that you’re discussing religion because she’s speaking about discipline that must fit within her belief system.”
• Ask if the belief system “authorizes” or “requires” corporal punishment. If it is authorized, there’s a clear basis for working together.
• Try to distinguish between parents who need education and those who should be prosecuted. Some parents may accept and use corporal punishment, but may be amenable to discussion and education.
• Emphasize the patient’s strengths. Parental warmth, for instance, does not negate the risks of corporal punishment, but it can be a good foundation.
• Acknowledge the benefits of religion, such as its promotion of well-being and healthy behavior.
• Recognize the value of discipline and emphasize that you’re advocating for “effective” discipline with the fewest risk factors.
• “Play in the parent’s ball field.” If the parent believes she is God’s representative to the child, consider asking questions such as “What is your child learning about God when you hit her? What did you learn about God from being physically disciplined?” Parents often will pause and reflect.
Mr. Vieth told the story of Carol, a deeply religious single mother who was raised in a home with corporal discipline and who believed that God’s word in her Protestant faith told her that she must sometimes hit her 3-year-old son with an object. She confessed to a coworker that she was paddling her son on the buttocks, but did not like doing so and was scared of hurting him.
Carol’s coworker called Child Protective Services. The subsequent multidisciplinary team investigation chose not to file criminal charges, but to file a civil child protection petition. Carol pledged to improve her parenting, but was unwilling to forgo the practice altogether. Over time, it became apparent to the team working with Carol that she was heavily influenced by James Dobson, Ph.D., the founder of an organization called Focus on the Family. Unlike other more extreme advocates of corporal punishment, Dr. Dobson caps the number of spanks at two, with one for lesser infractions, and says spanking must never leave a bruise or injury (“From Sticks to Flowers: Guidelines for Child Protection Professionals Working with Parents Using Scripture to Justify Corporal Punishment,” [St. Paul, Minn.: William Mitchell Law Review, 2014, p. 923]), Mr. Vieth noted.
“For Carol, his views trumped all medical and health research,” Mr. Vieth said. “We had to figure out a way to play in her court.” Working with a social worker, he found passages in Dobson’s writing that conveyed the message that not every child needs corporal punishment.
“Once I started quoting Dobson, it changed the dynamic” and the team was able to work with her on embracing and learning alternative approaches. The petition was dropped, and Carol now is an advocate in her church for discipline methods other than corporal punishment.
Mr. Vieth reported having no relevant financial disclosures.
WASHINGTON – The legal definition of what constitutes “reasonable” corporal punishment is contracting, making it more critical than ever to inquire about discipline, provide alternatives to corporal punishment, and address religious objections with culturally sensitive responses.
In delivering this message, Victor I. Vieth, J.D., founder and senior director of the Gundersen National Child Protection Training Center in La Crosse, Wisc., stressed that spanking and other forms of corporal punishment are still widely practiced, and that the many parents who employ this form of discipline are open to considering alternatives that they can learn and believe in.
“The vast majority of parents are doing the best they know how. … They don’t know the alternatives,” Mr. Vieth said.
“Reasonable” corporal punishment is lawful in all 50 states, but the definition of reasonable is narrowing. Courts now will consider the child’s size, frowning upon such punishment for children under the age of 2 years. They will consider where on the body the child is hit, generally viewing anything but the buttocks as unreasonable, and they’ll look at whether objects have been used.
Courts even appear willing today to consider the “nature of the child’s misbehavior,” which “opens the door to even mild corporal punishment cases sometimes being considered unlawful,” such as a parent hitting a child on the buttocks once or twice after milk is spilled, said Mr. Vieth, whose training center oversees a Center for Effective Discipline.
“Think about this as a mandatory reporter,” he said at the annual meeting of the American Academy of Pediatrics. “The vast majority of corporal punishment cases we see probably are running afoul of criminal or civil codes today.”
Shifts in case law are likely being driven by research showing that corporal punishment is a risk factor for both short-term and long-term physical and mental injury, he said. It has long been known that even mild forms of physical abuse – what’s been called “ordinary” physical punishment – can cause negative behavioral and psychological outcomes such as alcohol abuse, depression, behavioral problems, and low achievement.
More recent research has expanded the toll, linking acts such as pushing, grabbing, shoving, slapping, and hitting not only with higher risks of mental disorders and family dysfunction, but with higher risks of cardiovascular disease, arthritis, and obesity.
Ask parents about what form of discipline they’re using, and educate parents who indicate using corporal punishment about the medical risks and mental health risks in the short and long term. It’s important to then give parents “practical, concrete” tools that model alternative methods. Vanderbilt University’s Play Nicely free online parenting program is one that Mr. Vieth often recommends.
The parental response of “my parents hit me and I turned out just fine” is not uncommon, and it can be handled in various ways, he said.
You could segue into a discussion of risks by saying, for example, “Well, let’s explore that. I’ve known you for a long time, and I think you did turn out well. And that’s consistent with the research because the research doesn’t show that if you receive corporal punishment, you’re going to grow up to have negative outcomes. The research says that it’s a risk factor, and the more you hit and the longer you hit, the greater the risk will be.”
You also could compare corporal punishment research to research on smoking, Mr. Vieth said, by saying, “It’s not that different from smoking. One cigarette in the back of the school house won’t kill you, but two packs a day will dramatically increase the risk.”
Religion is a top reason – if not the No. 1 reason – for the use of corporal punishment, and it’s important to understand its influence on discipline and to develop culturally sensitive responses to parents who object for religious reasons to alternative approaches, Mr. Vieth said.
He recommended the following strategies when a parent cites religious grounds for physical discipline:
• Be aware of your own biases. Do not automatically label parents as neglectful or abusive.
• Refrain from pastoral work. “Assure the parent that you’re not trying to take away her religious beliefs, that you’re discussing religion because she’s speaking about discipline that must fit within her belief system.”
• Ask if the belief system “authorizes” or “requires” corporal punishment. If it is authorized, there’s a clear basis for working together.
• Try to distinguish between parents who need education and those who should be prosecuted. Some parents may accept and use corporal punishment, but may be amenable to discussion and education.
• Emphasize the patient’s strengths. Parental warmth, for instance, does not negate the risks of corporal punishment, but it can be a good foundation.
• Acknowledge the benefits of religion, such as its promotion of well-being and healthy behavior.
• Recognize the value of discipline and emphasize that you’re advocating for “effective” discipline with the fewest risk factors.
• “Play in the parent’s ball field.” If the parent believes she is God’s representative to the child, consider asking questions such as “What is your child learning about God when you hit her? What did you learn about God from being physically disciplined?” Parents often will pause and reflect.
Mr. Vieth told the story of Carol, a deeply religious single mother who was raised in a home with corporal discipline and who believed that God’s word in her Protestant faith told her that she must sometimes hit her 3-year-old son with an object. She confessed to a coworker that she was paddling her son on the buttocks, but did not like doing so and was scared of hurting him.
Carol’s coworker called Child Protective Services. The subsequent multidisciplinary team investigation chose not to file criminal charges, but to file a civil child protection petition. Carol pledged to improve her parenting, but was unwilling to forgo the practice altogether. Over time, it became apparent to the team working with Carol that she was heavily influenced by James Dobson, Ph.D., the founder of an organization called Focus on the Family. Unlike other more extreme advocates of corporal punishment, Dr. Dobson caps the number of spanks at two, with one for lesser infractions, and says spanking must never leave a bruise or injury (“From Sticks to Flowers: Guidelines for Child Protection Professionals Working with Parents Using Scripture to Justify Corporal Punishment,” [St. Paul, Minn.: William Mitchell Law Review, 2014, p. 923]), Mr. Vieth noted.
“For Carol, his views trumped all medical and health research,” Mr. Vieth said. “We had to figure out a way to play in her court.” Working with a social worker, he found passages in Dobson’s writing that conveyed the message that not every child needs corporal punishment.
“Once I started quoting Dobson, it changed the dynamic” and the team was able to work with her on embracing and learning alternative approaches. The petition was dropped, and Carol now is an advocate in her church for discipline methods other than corporal punishment.
Mr. Vieth reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
AAP: Screen for lipids with nonfasting total cholesterol and HDL
WASHINGTON – Recommendations for universal lipid screening between 9 and 11 years and again between ages 17 and 21 – and selective screening of children with risk factors starting at age 2 years – may best be heeded by measuring nonfasting total cholesterol and high-density lipoprotein, pediatric cardiologist Dr. Sarah de Ferranti told a packed room at the annual meeting of the American Academy of Pediatrics.
The difference of the two values is the non-HDL cholesterol level (total cholesterol minus HDL) and represents the atherogenic portion of the lipid profile. It is a “valid” initial result, she assured pediatricians.
Non-HDL values of 145 mg/dL and over should then be further explored through a complete fasting lipid profile, said Dr. de Ferranti, who directs the preventive cardiology program at Boston Children’s Hospital.
While the nonfasting, non-HDL approach has been deemed acceptable for universal screening, national guidelines endorsed by the AAP recommend that selective testing of high-risk children be done with a fasting profile. “But I think people find that onerous,” Dr. de Ferranti said. “Doing a nonfasting test initially [in any pediatric case] is quite reasonable. It’s more convenient, and it may help us to better implement the guidelines and not lose families.”
In 2011, the National Heart, Lung, and Blood Institute (NHLBI) called on physicians not only to selectively screen children with risk factors for cardiovascular disease, but to screen their healthy 9- to 11- and 17- to 21-year-old patients, and to provide lifestyle therapy for patients who have high LDL cholesterol readings on follow-up testing, and then statin treatment for those who don’t respond.
Surveys have shown that fewer than half of pediatricians do routine screening, however, and that many are frustrated with the limitations of lifestyle interventions and at least somewhat uncomfortable with the concept of statin treatment.
The AAP’s own recommendations for lipid screening, issued in 2008, were confined to selective screening of children with risk factors such as obesity, diabetes, or hypertension, or a family history of heart attack, stroke, and high cholesterol. But in 2011, the academy endorsed the NHLBI’s Integrated Guidelines for Cardiovascular Risk Reduction in Childhood and Adolescence, embracing its additional call for screening healthy children during two windows of time.
Both guidelines – the AAP’s and the NHLBI’s – recommend statin treatment for patients whose LDL remains at 190 mg/dL or above after 6 months of lifestyle therapy, and for patients whose LDL is 160 mg/dL or above after lifestyle therapy when additional risk factors are present.
Dr. de Ferranti acknowledged gaps in research on the benefits of early treatment and said that, personally, she is “not sure that [universal screening] will definitely be the right approach for the future.”
She implored pediatricians, however, to remember when making practice decisions that universal screening “has attempted to address the fact that getting a family history [of cardiovascular disease] isn’t always helpful or reliable” for identifying children at high risk of cardiovascular disease, even those with familial hypercholesterolemia.
Familiar hypercholesterolemia is a disorder of LDL cholesterol processing estimated to affect 1 in 250 individuals. It’s usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as young adults,” said de Ferranti, assistant professor of medicine at Harvard Medical School, Boston.
Studies have shown that individuals aged 20-39 years who have the disorder are almost 90 times as likely to die from coronary heart disease as is the general population in that age group, she noted.
Available data on the impact of treating familiar hypercholesterolemia in childhood is “relatively scant” but “convincing,” she said. One randomized controlled study of statin treatment in children with the disorder used vascular thickness as a proxy for cardiovascular events. Children who took pravastatin for 2 years had a lower mean carotid intima media thickness, and lower LDL levels, compared with children assigned to placebo (JAMA 2004 Jul 21;292[3]:331-7).
Further follow-up of these children has suggested delayed atherosclerotic disease and prevention of cardiac events in the statin group, Dr. de Ferranti noted. And separate observational research shows a significant reduction in cardiovascular disease events in affected adults taking statins.
Not all pediatricians are convinced that screening is justified. A 2013 electronic survey of pediatric providers in Minnesota showed that while 77% supported the concept of lipid screening, 33% performed no screening, 50% screened selectively, and only 16% performed universal screening. (J. Pediatr. 2014 Mar;164[3]:572-6).
In a recent national survey of randomly selected, practicing AAP members, at least two-thirds indicated that they screen based on family history, high-risk conditions, and obesity. Fewer than half said they perform universal age-based screening.
Obtaining labs appears to be a major barrier, Dr. de Ferranti pointed out. Nearly half of the pediatricians who responded to the survey, which was presented at the 2015 annual meeting of the Pediatric Academic Societies, reported problems with patients not returning for a fasting test, she said.
Dr. de Ferranti and her colleagues at Boston Children’s Hospital recently led a quality improvement project to implement lipid screening in their center’s urban primary care practice. Provider adherence to recommended screening, which resembled the NHLBI recommendations, was high. Almost a quarter of the approximately 1,200 patients who received test orders, however, did not complete the ordered screening test, even though it entailed nonfasting non-HDL testing.
And patients screened based on their age alone (the universal screening component) had a low rate of abnormal findings: Only 2.7% were found to have non-HDL of 145 mg/dL or greater, which was surprising to Dr. de Ferranti given the high rate of obesity (45%) in the practice’s population.
“Age-only screening, at least from our data so far, is not very productive,” she said. Only one patient had a clinical picture consistent with familial hyperlipidemia, and this patient was identified based on risk factors and not age alone.
On the other hand, mild abnormalities (non-HDL of 120-145 mg/dL) – the kind that often prompt Dr. de Ferranti to advise lifestyle modification, including a low saturated fat intake of 12-15 g/day with no trans fat, high fiber, and high intake of fresh fruits and vegetables – were common across the board.
Asked about the safety of statins in children, Dr. de Ferranti said there appears to be a 1%-2% rate of side effects in the pediatric population. “My patients have done well,” she said. “Remember, initiation of statins (involves) a discussion – it’s not an emergency. We usually don’t decide in one visit.”
Low-dose statin therapy is an option starting at age 10 years, but Dr. de Ferranti said she sometimes will start “very high risk” patients earlier, between 8 and 10 years of age.
Many of the AAP survey participants believed that statins were appropriate for patients with confirmed high LDL unresponsive to lifestyle change; about 62% agreed with statin use for young children in such situations and almost 90% for older children. Significantly fewer started statin therapy themselves (about 8% for young children and 21% for older children). About half said they refer these patients to lipid specialists, but almost a third reported limited local access.
These low rates of statin treatment or referral for those with severe LDL elevations are concerning and “suggest a missed opportunity for cardiovascular risk reduction in these high-risk children,” Dr. de Ferranti said.
Pediatricians should soon receive more guidance on lipid screening from the U.S. Preventive Services Task Force. In 2007, the task force was unable to determine the balance between potential harms and benefits for routinely screening children and adolescents for dyslipidemia, and issued an “indeterminate” recommendation. It is now reviewing the evidence and is expected to release new guidelines in the near future, she said.
Dr. de Ferranti disclosed that she has current research funding from the Patient Centered Research Institute, the New England Congenital Cardiology Research Foundation, and the Pediatric Heart Network. She also receives royalties from UptoDate, an online clinical decision support resource.
WASHINGTON – Recommendations for universal lipid screening between 9 and 11 years and again between ages 17 and 21 – and selective screening of children with risk factors starting at age 2 years – may best be heeded by measuring nonfasting total cholesterol and high-density lipoprotein, pediatric cardiologist Dr. Sarah de Ferranti told a packed room at the annual meeting of the American Academy of Pediatrics.
The difference of the two values is the non-HDL cholesterol level (total cholesterol minus HDL) and represents the atherogenic portion of the lipid profile. It is a “valid” initial result, she assured pediatricians.
Non-HDL values of 145 mg/dL and over should then be further explored through a complete fasting lipid profile, said Dr. de Ferranti, who directs the preventive cardiology program at Boston Children’s Hospital.
While the nonfasting, non-HDL approach has been deemed acceptable for universal screening, national guidelines endorsed by the AAP recommend that selective testing of high-risk children be done with a fasting profile. “But I think people find that onerous,” Dr. de Ferranti said. “Doing a nonfasting test initially [in any pediatric case] is quite reasonable. It’s more convenient, and it may help us to better implement the guidelines and not lose families.”
In 2011, the National Heart, Lung, and Blood Institute (NHLBI) called on physicians not only to selectively screen children with risk factors for cardiovascular disease, but to screen their healthy 9- to 11- and 17- to 21-year-old patients, and to provide lifestyle therapy for patients who have high LDL cholesterol readings on follow-up testing, and then statin treatment for those who don’t respond.
Surveys have shown that fewer than half of pediatricians do routine screening, however, and that many are frustrated with the limitations of lifestyle interventions and at least somewhat uncomfortable with the concept of statin treatment.
The AAP’s own recommendations for lipid screening, issued in 2008, were confined to selective screening of children with risk factors such as obesity, diabetes, or hypertension, or a family history of heart attack, stroke, and high cholesterol. But in 2011, the academy endorsed the NHLBI’s Integrated Guidelines for Cardiovascular Risk Reduction in Childhood and Adolescence, embracing its additional call for screening healthy children during two windows of time.
Both guidelines – the AAP’s and the NHLBI’s – recommend statin treatment for patients whose LDL remains at 190 mg/dL or above after 6 months of lifestyle therapy, and for patients whose LDL is 160 mg/dL or above after lifestyle therapy when additional risk factors are present.
Dr. de Ferranti acknowledged gaps in research on the benefits of early treatment and said that, personally, she is “not sure that [universal screening] will definitely be the right approach for the future.”
She implored pediatricians, however, to remember when making practice decisions that universal screening “has attempted to address the fact that getting a family history [of cardiovascular disease] isn’t always helpful or reliable” for identifying children at high risk of cardiovascular disease, even those with familial hypercholesterolemia.
Familiar hypercholesterolemia is a disorder of LDL cholesterol processing estimated to affect 1 in 250 individuals. It’s usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as young adults,” said de Ferranti, assistant professor of medicine at Harvard Medical School, Boston.
Studies have shown that individuals aged 20-39 years who have the disorder are almost 90 times as likely to die from coronary heart disease as is the general population in that age group, she noted.
Available data on the impact of treating familiar hypercholesterolemia in childhood is “relatively scant” but “convincing,” she said. One randomized controlled study of statin treatment in children with the disorder used vascular thickness as a proxy for cardiovascular events. Children who took pravastatin for 2 years had a lower mean carotid intima media thickness, and lower LDL levels, compared with children assigned to placebo (JAMA 2004 Jul 21;292[3]:331-7).
Further follow-up of these children has suggested delayed atherosclerotic disease and prevention of cardiac events in the statin group, Dr. de Ferranti noted. And separate observational research shows a significant reduction in cardiovascular disease events in affected adults taking statins.
Not all pediatricians are convinced that screening is justified. A 2013 electronic survey of pediatric providers in Minnesota showed that while 77% supported the concept of lipid screening, 33% performed no screening, 50% screened selectively, and only 16% performed universal screening. (J. Pediatr. 2014 Mar;164[3]:572-6).
In a recent national survey of randomly selected, practicing AAP members, at least two-thirds indicated that they screen based on family history, high-risk conditions, and obesity. Fewer than half said they perform universal age-based screening.
Obtaining labs appears to be a major barrier, Dr. de Ferranti pointed out. Nearly half of the pediatricians who responded to the survey, which was presented at the 2015 annual meeting of the Pediatric Academic Societies, reported problems with patients not returning for a fasting test, she said.
Dr. de Ferranti and her colleagues at Boston Children’s Hospital recently led a quality improvement project to implement lipid screening in their center’s urban primary care practice. Provider adherence to recommended screening, which resembled the NHLBI recommendations, was high. Almost a quarter of the approximately 1,200 patients who received test orders, however, did not complete the ordered screening test, even though it entailed nonfasting non-HDL testing.
And patients screened based on their age alone (the universal screening component) had a low rate of abnormal findings: Only 2.7% were found to have non-HDL of 145 mg/dL or greater, which was surprising to Dr. de Ferranti given the high rate of obesity (45%) in the practice’s population.
“Age-only screening, at least from our data so far, is not very productive,” she said. Only one patient had a clinical picture consistent with familial hyperlipidemia, and this patient was identified based on risk factors and not age alone.
On the other hand, mild abnormalities (non-HDL of 120-145 mg/dL) – the kind that often prompt Dr. de Ferranti to advise lifestyle modification, including a low saturated fat intake of 12-15 g/day with no trans fat, high fiber, and high intake of fresh fruits and vegetables – were common across the board.
Asked about the safety of statins in children, Dr. de Ferranti said there appears to be a 1%-2% rate of side effects in the pediatric population. “My patients have done well,” she said. “Remember, initiation of statins (involves) a discussion – it’s not an emergency. We usually don’t decide in one visit.”
Low-dose statin therapy is an option starting at age 10 years, but Dr. de Ferranti said she sometimes will start “very high risk” patients earlier, between 8 and 10 years of age.
Many of the AAP survey participants believed that statins were appropriate for patients with confirmed high LDL unresponsive to lifestyle change; about 62% agreed with statin use for young children in such situations and almost 90% for older children. Significantly fewer started statin therapy themselves (about 8% for young children and 21% for older children). About half said they refer these patients to lipid specialists, but almost a third reported limited local access.
These low rates of statin treatment or referral for those with severe LDL elevations are concerning and “suggest a missed opportunity for cardiovascular risk reduction in these high-risk children,” Dr. de Ferranti said.
Pediatricians should soon receive more guidance on lipid screening from the U.S. Preventive Services Task Force. In 2007, the task force was unable to determine the balance between potential harms and benefits for routinely screening children and adolescents for dyslipidemia, and issued an “indeterminate” recommendation. It is now reviewing the evidence and is expected to release new guidelines in the near future, she said.
Dr. de Ferranti disclosed that she has current research funding from the Patient Centered Research Institute, the New England Congenital Cardiology Research Foundation, and the Pediatric Heart Network. She also receives royalties from UptoDate, an online clinical decision support resource.
WASHINGTON – Recommendations for universal lipid screening between 9 and 11 years and again between ages 17 and 21 – and selective screening of children with risk factors starting at age 2 years – may best be heeded by measuring nonfasting total cholesterol and high-density lipoprotein, pediatric cardiologist Dr. Sarah de Ferranti told a packed room at the annual meeting of the American Academy of Pediatrics.
The difference of the two values is the non-HDL cholesterol level (total cholesterol minus HDL) and represents the atherogenic portion of the lipid profile. It is a “valid” initial result, she assured pediatricians.
Non-HDL values of 145 mg/dL and over should then be further explored through a complete fasting lipid profile, said Dr. de Ferranti, who directs the preventive cardiology program at Boston Children’s Hospital.
While the nonfasting, non-HDL approach has been deemed acceptable for universal screening, national guidelines endorsed by the AAP recommend that selective testing of high-risk children be done with a fasting profile. “But I think people find that onerous,” Dr. de Ferranti said. “Doing a nonfasting test initially [in any pediatric case] is quite reasonable. It’s more convenient, and it may help us to better implement the guidelines and not lose families.”
In 2011, the National Heart, Lung, and Blood Institute (NHLBI) called on physicians not only to selectively screen children with risk factors for cardiovascular disease, but to screen their healthy 9- to 11- and 17- to 21-year-old patients, and to provide lifestyle therapy for patients who have high LDL cholesterol readings on follow-up testing, and then statin treatment for those who don’t respond.
Surveys have shown that fewer than half of pediatricians do routine screening, however, and that many are frustrated with the limitations of lifestyle interventions and at least somewhat uncomfortable with the concept of statin treatment.
The AAP’s own recommendations for lipid screening, issued in 2008, were confined to selective screening of children with risk factors such as obesity, diabetes, or hypertension, or a family history of heart attack, stroke, and high cholesterol. But in 2011, the academy endorsed the NHLBI’s Integrated Guidelines for Cardiovascular Risk Reduction in Childhood and Adolescence, embracing its additional call for screening healthy children during two windows of time.
Both guidelines – the AAP’s and the NHLBI’s – recommend statin treatment for patients whose LDL remains at 190 mg/dL or above after 6 months of lifestyle therapy, and for patients whose LDL is 160 mg/dL or above after lifestyle therapy when additional risk factors are present.
Dr. de Ferranti acknowledged gaps in research on the benefits of early treatment and said that, personally, she is “not sure that [universal screening] will definitely be the right approach for the future.”
She implored pediatricians, however, to remember when making practice decisions that universal screening “has attempted to address the fact that getting a family history [of cardiovascular disease] isn’t always helpful or reliable” for identifying children at high risk of cardiovascular disease, even those with familial hypercholesterolemia.
Familiar hypercholesterolemia is a disorder of LDL cholesterol processing estimated to affect 1 in 250 individuals. It’s usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as young adults,” said de Ferranti, assistant professor of medicine at Harvard Medical School, Boston.
Studies have shown that individuals aged 20-39 years who have the disorder are almost 90 times as likely to die from coronary heart disease as is the general population in that age group, she noted.
Available data on the impact of treating familiar hypercholesterolemia in childhood is “relatively scant” but “convincing,” she said. One randomized controlled study of statin treatment in children with the disorder used vascular thickness as a proxy for cardiovascular events. Children who took pravastatin for 2 years had a lower mean carotid intima media thickness, and lower LDL levels, compared with children assigned to placebo (JAMA 2004 Jul 21;292[3]:331-7).
Further follow-up of these children has suggested delayed atherosclerotic disease and prevention of cardiac events in the statin group, Dr. de Ferranti noted. And separate observational research shows a significant reduction in cardiovascular disease events in affected adults taking statins.
Not all pediatricians are convinced that screening is justified. A 2013 electronic survey of pediatric providers in Minnesota showed that while 77% supported the concept of lipid screening, 33% performed no screening, 50% screened selectively, and only 16% performed universal screening. (J. Pediatr. 2014 Mar;164[3]:572-6).
In a recent national survey of randomly selected, practicing AAP members, at least two-thirds indicated that they screen based on family history, high-risk conditions, and obesity. Fewer than half said they perform universal age-based screening.
Obtaining labs appears to be a major barrier, Dr. de Ferranti pointed out. Nearly half of the pediatricians who responded to the survey, which was presented at the 2015 annual meeting of the Pediatric Academic Societies, reported problems with patients not returning for a fasting test, she said.
Dr. de Ferranti and her colleagues at Boston Children’s Hospital recently led a quality improvement project to implement lipid screening in their center’s urban primary care practice. Provider adherence to recommended screening, which resembled the NHLBI recommendations, was high. Almost a quarter of the approximately 1,200 patients who received test orders, however, did not complete the ordered screening test, even though it entailed nonfasting non-HDL testing.
And patients screened based on their age alone (the universal screening component) had a low rate of abnormal findings: Only 2.7% were found to have non-HDL of 145 mg/dL or greater, which was surprising to Dr. de Ferranti given the high rate of obesity (45%) in the practice’s population.
“Age-only screening, at least from our data so far, is not very productive,” she said. Only one patient had a clinical picture consistent with familial hyperlipidemia, and this patient was identified based on risk factors and not age alone.
On the other hand, mild abnormalities (non-HDL of 120-145 mg/dL) – the kind that often prompt Dr. de Ferranti to advise lifestyle modification, including a low saturated fat intake of 12-15 g/day with no trans fat, high fiber, and high intake of fresh fruits and vegetables – were common across the board.
Asked about the safety of statins in children, Dr. de Ferranti said there appears to be a 1%-2% rate of side effects in the pediatric population. “My patients have done well,” she said. “Remember, initiation of statins (involves) a discussion – it’s not an emergency. We usually don’t decide in one visit.”
Low-dose statin therapy is an option starting at age 10 years, but Dr. de Ferranti said she sometimes will start “very high risk” patients earlier, between 8 and 10 years of age.
Many of the AAP survey participants believed that statins were appropriate for patients with confirmed high LDL unresponsive to lifestyle change; about 62% agreed with statin use for young children in such situations and almost 90% for older children. Significantly fewer started statin therapy themselves (about 8% for young children and 21% for older children). About half said they refer these patients to lipid specialists, but almost a third reported limited local access.
These low rates of statin treatment or referral for those with severe LDL elevations are concerning and “suggest a missed opportunity for cardiovascular risk reduction in these high-risk children,” Dr. de Ferranti said.
Pediatricians should soon receive more guidance on lipid screening from the U.S. Preventive Services Task Force. In 2007, the task force was unable to determine the balance between potential harms and benefits for routinely screening children and adolescents for dyslipidemia, and issued an “indeterminate” recommendation. It is now reviewing the evidence and is expected to release new guidelines in the near future, she said.
Dr. de Ferranti disclosed that she has current research funding from the Patient Centered Research Institute, the New England Congenital Cardiology Research Foundation, and the Pediatric Heart Network. She also receives royalties from UptoDate, an online clinical decision support resource.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE