User login
Prurigo nodularis has two disease endotypes, a cluster analysis shows
A cluster analysis of circulating plasma biomarkers in prurigo nodularis (PN) has identified two disease endotypes with inflammatory and noninflammatory biomarker profiles.
said senior author Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore. “This is the beginning of personalized medicine in prurigo nodularis.”
He and others have long observed significant clinical heterogeneity both in the presentation of PN – with the nodules in African American patients, for instance, appearing larger, thicker, and more fibrotic – and in patients’ response to immunomodulating and neuromodulating therapies.
To avoid the introduction of bias, the researchers used an unsupervised machine-learning approach to analyze the levels of 12 inflammatory biomarkers in 20 patients with PN and in matched healthy controls. The biomarkers were chosen based on their demonstrated dysregulation in PN and other inflammatory dermatoses.
The researchers then conducted a population-level analysis using multicenter electronic medical record data to explore inflammatory markers and verify findings from the cluster analysis. The study was published online Oct. 27, 2021, in the Journal of Investigative Dermatology.
One cluster of the 20 patients had higher levels of nine inflammatory biomarkers representing multiple immune axes: Higher interleukin-1 alpha, IL-4, IL-5, IL-6, IL-10, IL-17A, IL-22, and IL-25. This cluster had a higher percentage of Black patients, a higher severity of itch, and lower quality of life scores, the authors report in the preprint.
The other cluster – without such an inflammatory profile – had fewer Black patients and a higher percentage of patients with myelopathy (e.g. spinal stenosis, spinal trauma, degenerative disc disease). The rates of inflammatory comorbidities and of immune- and neuromodulating treatments at the time of blood draw were relatively equivalent between the two clusters.
In the subsequent population-level analysis, using data from a global health research network of EMRs from almost 50 health care organizations, Black patients with PN were found to have higher erythrocyte sedimentation rate, C-reactive protein, ferritin, and eosinophils, and lower transferrin, than White patients with PN. (The analysis included only Black and White patients.)
There are no Food and Drug Administration–approved therapies for PN, and “clinicians need to be really creative in managing these patients,” Dr. Kwatra said.
“There may be suggestions at the bedside that patients have more immune dysregulation, or maybe I’ll see increased circulating blood eosinophils,” he said. “And there are those who don’t seem to have any immune dysregulation and have more features of neurosensitization ... who may have a history of neck pain or back injury.”
The existence of endotypes in PN suggests that patients may benefit from personalized therapies with either immunomodulating or neuromodulating treatments, he and his colleagues wrote. “Further neuroimmune phenotyping studies of PN may pave the way for a future precision medicine management approach.”
Studies of PN conducted in Europe have been almost exclusively in White patients, Dr. Kwatra noted, even though PN has been shown to disproportionately affect Black and other racial/ethnic-minority patients.
Black patients with PN were found to have the highest all-cause mortality over 20 years post diagnosis in a separate analysis of over 22,000 patients with PN. Using data from the same health research network, Dr. Kwatra and coinvestigators stratified patients by race/ethnicity and compared each subgroup with a corresponding subgroup of similar race/ethnicity to control for inherent differences in mortality.
Overall, patients with PN had higher all-cause mortality than controls (hazard ratio, 1.70), likely because of a high comorbidity burden, they wrote in their research letter. Black patients with PN had the highest mortality (HR, 2.07), followed by White (HR, 1.74) and Hispanic (HR, 1.62) patients.
PN may exacerbate existing racial disparities in the social determinants of health, and Black patients may suffer from greater systemic inflammation, Dr. Kwatra and coauthors wrote. Certainly, he said, these findings, as well as the finding of a distinct inflammatory signature in Black patients with PN, support “that the disease burden is much higher” in these patients.
Dr Kwatra disclosed that he is an advisory board member/consultant for Celldex Therapeutics, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals and has received grant funding from several companies. His research is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Grants from the Dermatology Foundation and the Skin of Color Society also helped fund the cluster analysis.
A cluster analysis of circulating plasma biomarkers in prurigo nodularis (PN) has identified two disease endotypes with inflammatory and noninflammatory biomarker profiles.
said senior author Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore. “This is the beginning of personalized medicine in prurigo nodularis.”
He and others have long observed significant clinical heterogeneity both in the presentation of PN – with the nodules in African American patients, for instance, appearing larger, thicker, and more fibrotic – and in patients’ response to immunomodulating and neuromodulating therapies.
To avoid the introduction of bias, the researchers used an unsupervised machine-learning approach to analyze the levels of 12 inflammatory biomarkers in 20 patients with PN and in matched healthy controls. The biomarkers were chosen based on their demonstrated dysregulation in PN and other inflammatory dermatoses.
The researchers then conducted a population-level analysis using multicenter electronic medical record data to explore inflammatory markers and verify findings from the cluster analysis. The study was published online Oct. 27, 2021, in the Journal of Investigative Dermatology.
One cluster of the 20 patients had higher levels of nine inflammatory biomarkers representing multiple immune axes: Higher interleukin-1 alpha, IL-4, IL-5, IL-6, IL-10, IL-17A, IL-22, and IL-25. This cluster had a higher percentage of Black patients, a higher severity of itch, and lower quality of life scores, the authors report in the preprint.
The other cluster – without such an inflammatory profile – had fewer Black patients and a higher percentage of patients with myelopathy (e.g. spinal stenosis, spinal trauma, degenerative disc disease). The rates of inflammatory comorbidities and of immune- and neuromodulating treatments at the time of blood draw were relatively equivalent between the two clusters.
In the subsequent population-level analysis, using data from a global health research network of EMRs from almost 50 health care organizations, Black patients with PN were found to have higher erythrocyte sedimentation rate, C-reactive protein, ferritin, and eosinophils, and lower transferrin, than White patients with PN. (The analysis included only Black and White patients.)
There are no Food and Drug Administration–approved therapies for PN, and “clinicians need to be really creative in managing these patients,” Dr. Kwatra said.
“There may be suggestions at the bedside that patients have more immune dysregulation, or maybe I’ll see increased circulating blood eosinophils,” he said. “And there are those who don’t seem to have any immune dysregulation and have more features of neurosensitization ... who may have a history of neck pain or back injury.”
The existence of endotypes in PN suggests that patients may benefit from personalized therapies with either immunomodulating or neuromodulating treatments, he and his colleagues wrote. “Further neuroimmune phenotyping studies of PN may pave the way for a future precision medicine management approach.”
Studies of PN conducted in Europe have been almost exclusively in White patients, Dr. Kwatra noted, even though PN has been shown to disproportionately affect Black and other racial/ethnic-minority patients.
Black patients with PN were found to have the highest all-cause mortality over 20 years post diagnosis in a separate analysis of over 22,000 patients with PN. Using data from the same health research network, Dr. Kwatra and coinvestigators stratified patients by race/ethnicity and compared each subgroup with a corresponding subgroup of similar race/ethnicity to control for inherent differences in mortality.
Overall, patients with PN had higher all-cause mortality than controls (hazard ratio, 1.70), likely because of a high comorbidity burden, they wrote in their research letter. Black patients with PN had the highest mortality (HR, 2.07), followed by White (HR, 1.74) and Hispanic (HR, 1.62) patients.
PN may exacerbate existing racial disparities in the social determinants of health, and Black patients may suffer from greater systemic inflammation, Dr. Kwatra and coauthors wrote. Certainly, he said, these findings, as well as the finding of a distinct inflammatory signature in Black patients with PN, support “that the disease burden is much higher” in these patients.
Dr Kwatra disclosed that he is an advisory board member/consultant for Celldex Therapeutics, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals and has received grant funding from several companies. His research is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Grants from the Dermatology Foundation and the Skin of Color Society also helped fund the cluster analysis.
A cluster analysis of circulating plasma biomarkers in prurigo nodularis (PN) has identified two disease endotypes with inflammatory and noninflammatory biomarker profiles.
said senior author Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore. “This is the beginning of personalized medicine in prurigo nodularis.”
He and others have long observed significant clinical heterogeneity both in the presentation of PN – with the nodules in African American patients, for instance, appearing larger, thicker, and more fibrotic – and in patients’ response to immunomodulating and neuromodulating therapies.
To avoid the introduction of bias, the researchers used an unsupervised machine-learning approach to analyze the levels of 12 inflammatory biomarkers in 20 patients with PN and in matched healthy controls. The biomarkers were chosen based on their demonstrated dysregulation in PN and other inflammatory dermatoses.
The researchers then conducted a population-level analysis using multicenter electronic medical record data to explore inflammatory markers and verify findings from the cluster analysis. The study was published online Oct. 27, 2021, in the Journal of Investigative Dermatology.
One cluster of the 20 patients had higher levels of nine inflammatory biomarkers representing multiple immune axes: Higher interleukin-1 alpha, IL-4, IL-5, IL-6, IL-10, IL-17A, IL-22, and IL-25. This cluster had a higher percentage of Black patients, a higher severity of itch, and lower quality of life scores, the authors report in the preprint.
The other cluster – without such an inflammatory profile – had fewer Black patients and a higher percentage of patients with myelopathy (e.g. spinal stenosis, spinal trauma, degenerative disc disease). The rates of inflammatory comorbidities and of immune- and neuromodulating treatments at the time of blood draw were relatively equivalent between the two clusters.
In the subsequent population-level analysis, using data from a global health research network of EMRs from almost 50 health care organizations, Black patients with PN were found to have higher erythrocyte sedimentation rate, C-reactive protein, ferritin, and eosinophils, and lower transferrin, than White patients with PN. (The analysis included only Black and White patients.)
There are no Food and Drug Administration–approved therapies for PN, and “clinicians need to be really creative in managing these patients,” Dr. Kwatra said.
“There may be suggestions at the bedside that patients have more immune dysregulation, or maybe I’ll see increased circulating blood eosinophils,” he said. “And there are those who don’t seem to have any immune dysregulation and have more features of neurosensitization ... who may have a history of neck pain or back injury.”
The existence of endotypes in PN suggests that patients may benefit from personalized therapies with either immunomodulating or neuromodulating treatments, he and his colleagues wrote. “Further neuroimmune phenotyping studies of PN may pave the way for a future precision medicine management approach.”
Studies of PN conducted in Europe have been almost exclusively in White patients, Dr. Kwatra noted, even though PN has been shown to disproportionately affect Black and other racial/ethnic-minority patients.
Black patients with PN were found to have the highest all-cause mortality over 20 years post diagnosis in a separate analysis of over 22,000 patients with PN. Using data from the same health research network, Dr. Kwatra and coinvestigators stratified patients by race/ethnicity and compared each subgroup with a corresponding subgroup of similar race/ethnicity to control for inherent differences in mortality.
Overall, patients with PN had higher all-cause mortality than controls (hazard ratio, 1.70), likely because of a high comorbidity burden, they wrote in their research letter. Black patients with PN had the highest mortality (HR, 2.07), followed by White (HR, 1.74) and Hispanic (HR, 1.62) patients.
PN may exacerbate existing racial disparities in the social determinants of health, and Black patients may suffer from greater systemic inflammation, Dr. Kwatra and coauthors wrote. Certainly, he said, these findings, as well as the finding of a distinct inflammatory signature in Black patients with PN, support “that the disease burden is much higher” in these patients.
Dr Kwatra disclosed that he is an advisory board member/consultant for Celldex Therapeutics, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals and has received grant funding from several companies. His research is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Grants from the Dermatology Foundation and the Skin of Color Society also helped fund the cluster analysis.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Lung transplantation in the era of COVID-19: New issues and paradigms
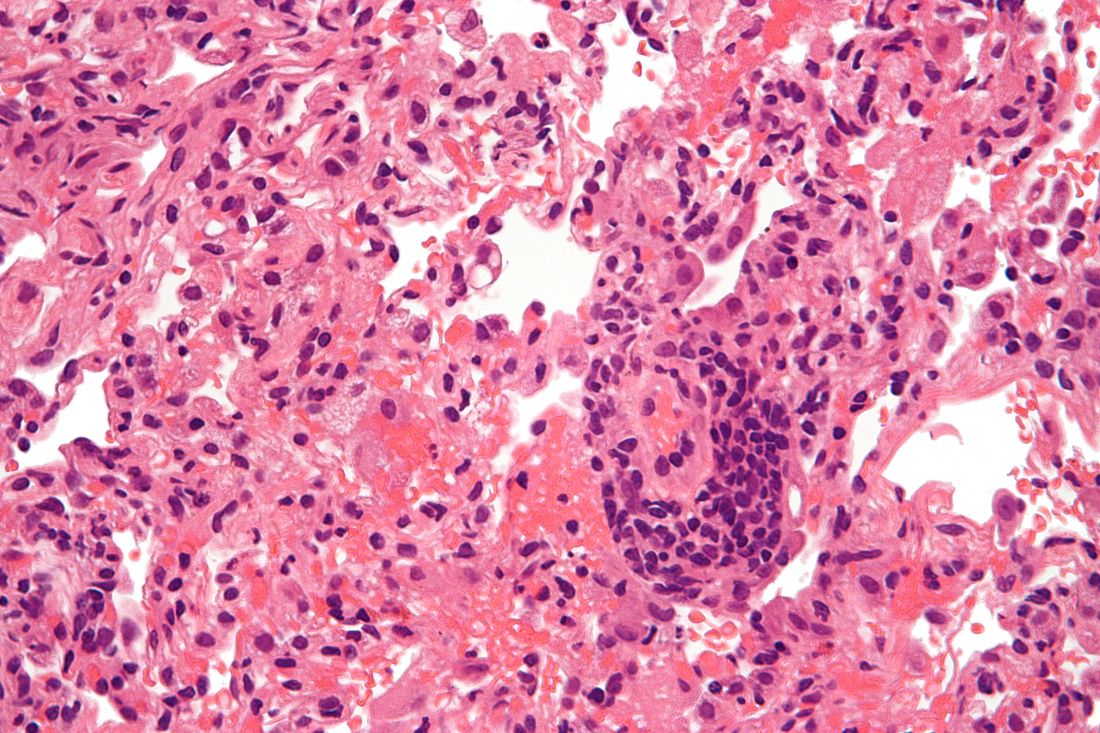
Data is sparse thus far, but there is concern in lung transplant medicine about the long-term risk of chronic lung allograft dysfunction (CLAD) and a potentially shortened longevity of transplanted lungs in recipients who become ill with COVID-19.
“My fear is that we’re potentially sitting on this iceberg worth of people who, come 6 months or a year from [the acute phase of] their COVID illness, will in fact have earlier and progressive, chronic rejection,” said Cameron R. Wolfe, MBBS, MPH, associate professor of medicine in transplant infectious disease at Duke University, Durham, N.C.
Lower respiratory viral infections have long been concerning for lung transplant recipients given their propensity to cause scarring, a decline in lung function, and a heightened risk of allograft rejection. Time will tell whether lung transplant recipients who survive COVID-19 follow a similar path, or one that is worse, he said.
Short-term data
Outcomes beyond hospitalization and acute illness for lung transplant recipients affected by COVID-19 have been reported in the literature by only a few lung transplant programs. These reports – as well as anecdotal experiences being informally shared among transplant programs – have raised the specter of more severe dysfunction following the acute phase and more early CLAD, said Tathagat Narula, MD, assistant professor of medicine at the Mayo Medical School, Rochester, Minn., and a consultant in lung transplantation at the Mayo Clinic’s Jacksonville program.
“The available data cover only 3-6 months out. We don’t know what will happen in the next 6 months and beyond,” Dr. Narula said in an interview.
The risks of COVID-19 in already-transplanted patients and issues relating to the inadequate antibody responses to vaccination are just some of the challenges of lung transplant medicine in the era of SARS-CoV-2. “COVID-19,” said Dr. Narula, “has completely changed the way we practice lung transplant medicine – the way we’re looking both at our recipients and our donors.”
Potential donors are being evaluated with lower respiratory SARS-CoV-2 testing and an abundance of caution. And patients with severe COVID-19 affecting their own lungs are roundly expected to drive up lung transplant volume in the near future. “The whole paradigm has changed,” Dr. Narula said.
Post-acute trajectories
A chart review study published in October by the lung transplant team at the University of Texas Southwestern Medical Center, Dallas, covered 44 consecutive survivors at a median follow-up of 4.5 months from hospital discharge or acute illness (the survival rate was 83.3%). Patients had significantly impaired functional status, and 18 of the 44 (40.9%) had a significant and persistent loss of forced vital capacity or forced expiratory volume in 1 second (>10% from pre–COVID-19 baseline).
Three patients met the criteria for new CLAD after COVID-19 infection, with all three classified as restrictive allograft syndrome (RAS) phenotype.
Moreover, the majority of COVID-19 survivors who had CT chest scans (22 of 28) showed persistent parenchymal opacities – a finding that, regardless of symptomatology, suggests persistent allograft injury, said Amit Banga, MD, associate professor of medicine and medical director of the ex vivo lung perfusion program in UT Southwestern’s lung transplant program.
“The implication is that there may be long-term consequences of COVID-19, perhaps related to some degree of ongoing inflammation and damage,” said Dr. Banga, a coauthor of the postinfection outcomes paper.
The UT Southwestern lung transplant program, which normally performs 60-80 transplants a year, began routine CT scanning 4-5 months into the pandemic, after “stumbling into a few patients who had no symptoms indicative of COVID pneumonia and no changes on an x-ray but significant involvement on a CT,” he said.
Without routine scanning in the general population of COVID-19 patients, Dr. Banga noted, “we’re limited in convincingly saying that COVID is uniquely doing this to lung transplant recipients.” Nor can they conclude that SARS-CoV-2 is unique from other respiratory viruses such as respiratory syncytial virus (RSV) in this regard. (The program has added CT scanning to its protocol for lung transplant recipients afflicted with other respiratory viruses to learn more.)
However, in the big picture, COVID-19 has proven to be far worse for lung transplant recipients than illness with other respiratory viruses, including RSV. “Patients have more frequent and greater loss of lung function, and worse debility from the acute illness,” Dr. Banga said.
“The cornerstones of treatment of both these viruses are very similar, but both the in-hospital course and the postdischarge outcomes are significantly different.”
In an initial paper published in September 2021, Dr. Banga and colleagues compared their first 25 lung transplant patients testing positive for SARS-CoV-2 with a historical cohort of 36 patients with RSV treated during 2016-2018.
Patients with COVID-19 had significantly worse morbidity and mortality, including worse postinfection lung function loss, functional decline, and 3-month survival.
More time, he said, will shed light on the risks of CLAD and the long-term potential for recovery of lung function. Currently, at UT Southwestern, it appears that patients who survive acute illness and the “first 3-6 months after COVID-19, when we’re seeing all the postinfection morbidity, may [enter] a period of stability,” Dr. Banga said.
Overall, he said, patients in their initial cohort are “holding steady” without unusual morbidity, readmissions, or “other setbacks to their allografts.”
At the Mayo Clinic in Jacksonville, which normally performs 40-50 lung transplants a year, transplant physicians have similarly observed significant declines in lung function beyond the acute phase of COVID-19. “Anecdotally, we’re seeing that some patients are beginning to recover some of their lung function, while others have not,” said Dr. Narula. “And we don’t have predictors as to who will progress to CLAD. It’s a big knowledge gap.”
Dr. Narula noted that patients with restrictive allograft syndrome, such as those reported by the UT Southwestern team, “have scarring of the lung and a much worse prognosis than the obstructive type of chronic rejection.” Whether there’s a role for antifibrotic therapy is a question worthy of research.
In UT Southwestern’s analysis, persistently lower absolute lymphocyte counts (< 600/dL) and higher ferritin levels (>150 ng/mL) at the time of hospital discharge were independently associated with significant lung function loss. This finding, reported in their October paper, has helped guide their management practices, Dr. Banga said.
“Persistently elevated ferritin may indicate ongoing inflammation at the allograft level,” he said. “We now send [such patients] home on a longer course of oral corticosteroids.”
At the front end of care for infected lung transplant recipients, Dr. Banga said that his team and physicians at other lung transplant programs are holding the cell-cycle inhibitor component of patients’ maintenance immunosuppression therapy (commonly mycophenolate or azathioprine) once infection is diagnosed to maximize chances of a better outcome.
“There may be variation on how long [the regimens are adjusted],” he said. “We changed our duration from 4 weeks to 2 due to patients developing a rebound worsening in the third and fourth week of acute illness.”
There is significant variation from institution to institution in how viral infections are managed in lung transplant recipients, he and Dr. Narula said. “Our numbers are so small in lung transplant, and we don’t have standardized protocols – it’s one of the biggest challenges in our field,” said Dr. Narula.
Vaccination issues, evaluation of donors
Whether or not immunosuppression regimens should be adjusted prior to vaccination is a controversial question, but is “an absolutely valid one” and is currently being studied in at least one National Institutes of Health–funded trial involving solid organ transplant recipients, said Dr. Wolfe.
“Some have jumped to the conclusion [based on some earlier data] that they should reduce immunosuppression regimens for everyone at the time of vaccination ... but I don’t know the answer yet,” he said. “Balancing staying rejection free with potentially gaining more immune response is complicated ... and it may depend on where the pandemic is going in your area and other factors.”
Reductions aside, Dr. Wolfe tells lung transplant recipients that, based on his approximation of a number of different studies in solid organ transplant recipients, approximately 40%-50% of patients who are immunized with two doses of the COVID-19 mRNA vaccines will develop meaningful antibody levels – and that this rises to 50%-60% after a third dose.
It is difficult to glean from available studies the level of vaccine response for lung transplant recipients specifically. But given that their level of maintenance immunosuppression is higher than for recipients of other donor organs, “as a broad sweep, lung transplant recipients tend to be lower in the pecking order of response,” he said.
Still, “there’s a lot to gain,” he said, pointing to a recent study from the Morbidity and Mortality Weekly Report (2021 Nov 5. doi: 10.15585/mmwr.mm7044e3) showing that effectiveness of mRNA vaccination against COVID-19–associated hospitalization was 77% among immunocompromised adults (compared with 90% in immunocompetent adults).
“This is good vindication to keep vaccinating,” he said, “and perhaps speaks to how difficult it is to assess the vaccine response [through measurement of antibody only].”
Neither Duke University’s transplant program, which performed 100-120 lung transplants a year pre-COVID, nor the programs at UT Southwestern or the Mayo Clinic in Jacksonville require that solid organ transplant candidates be vaccinated against SARS-CoV-2 in order to receive transplants, as some other transplant programs have done. (When asked about the issue, Dr. Banga and Dr. Narula each said that they have had no or little trouble convincing patients awaiting lung transplants of the need for COVID-19 vaccination.)
In an August statement, the American Society of Transplantation recommended vaccination for all solid organ transplant recipients, preferably prior to transplantation, and said that it “support[s] the development of institutional policies regarding pretransplant vaccination.”
The Society is not tracking centers’ vaccination policies. But Kaiser Health News reported in October that a growing number of transplant programs, such as UCHealth in Denver and UW Medicine in Seattle, have decided to either bar patients who refuse to be vaccinated from receiving transplants or give them lower priority on waitlists.
Potential lung donors, meanwhile, must be evaluated with lower respiratory COVID-19 testing, with results available prior to transplantation, according to policy developed by the Organ Procurement and Transplantation Network and effective in May 2021. The policy followed three published cases of donor-derived COVID-19 in lung transplant recipients, said Dr. Wolfe, who wrote about use of COVID-positive donors in an editorial published in October.
In each case, the donor had a negative COVID-19 nasopharyngeal swab at the time of organ procurement but was later found to have the virus on bronchoalveolar lavage, he said.
(The use of other organs from COVID-positive donors is appearing thus far to be safe, Dr. Wolfe noted. In the editorial, he references 13 cases of solid organ transplantation from SARS-CoV-2–infected donors into noninfected recipients; none of the 13 transplant recipients developed COVID-19).
Some questions remain, such as how many lower respiratory tests should be run, and how donors should be evaluated in cases of discordant results. Dr. Banga shared the case of a donor with one positive lower respiratory test result followed by two negative results. After internal debate, and consideration of potential false positives and other issues, the team at UT Southwestern decided to decline the donor, Dr. Banga said.
Other programs are likely making similar, appropriately cautious decisions, said Dr. Wolfe. “There’s no way in real-time donor evaluation to know whether the positive test is active virus that could infect the recipient and replicate ... or whether it’s [picking up] inactive or dead fragments of virus that was there several weeks ago. Our tests don’t differentiate that.”
Transplants in COVID-19 patients
Decision-making about lung transplant candidacy among patients with COVID-19 acute respiratory distress syndrome is complex and in need of a new paradigm.
“Some of these patients have the potential to recover, and they’re going to recover way later than what we’re used to,” said Dr. Banga. “We can’t extrapolate for COVID ARDS what we’ve learned for any other virus-related ARDS.”
Dr. Narula also has recently seen at least one COVID-19 patient on ECMO and under evaluation for transplantation recover. “We do not want to transplant too early,” he said, noting that there is consensus that lung transplant should be pursued only when the damage is deemed irreversible clinically and radiologically in the best judgment of the team. Still, “for many of these patients the only exit route will be lung transplants. For the next 12-24 months, a significant proportion of our lung transplant patients will have had post-COVID–related lung damage.”
As of October 2021, 233 lung transplants had been performed in the United States in recipients whose primary diagnosis was reported as COVID related, said Anne Paschke, media relations specialist with the United Network for Organ Sharing.
Dr. Banga, Dr. Wolfe, and Dr. Narula reported that they have no relevant disclosures.
Data is sparse thus far, but there is concern in lung transplant medicine about the long-term risk of chronic lung allograft dysfunction (CLAD) and a potentially shortened longevity of transplanted lungs in recipients who become ill with COVID-19.
“My fear is that we’re potentially sitting on this iceberg worth of people who, come 6 months or a year from [the acute phase of] their COVID illness, will in fact have earlier and progressive, chronic rejection,” said Cameron R. Wolfe, MBBS, MPH, associate professor of medicine in transplant infectious disease at Duke University, Durham, N.C.
Lower respiratory viral infections have long been concerning for lung transplant recipients given their propensity to cause scarring, a decline in lung function, and a heightened risk of allograft rejection. Time will tell whether lung transplant recipients who survive COVID-19 follow a similar path, or one that is worse, he said.
Short-term data
Outcomes beyond hospitalization and acute illness for lung transplant recipients affected by COVID-19 have been reported in the literature by only a few lung transplant programs. These reports – as well as anecdotal experiences being informally shared among transplant programs – have raised the specter of more severe dysfunction following the acute phase and more early CLAD, said Tathagat Narula, MD, assistant professor of medicine at the Mayo Medical School, Rochester, Minn., and a consultant in lung transplantation at the Mayo Clinic’s Jacksonville program.
“The available data cover only 3-6 months out. We don’t know what will happen in the next 6 months and beyond,” Dr. Narula said in an interview.
The risks of COVID-19 in already-transplanted patients and issues relating to the inadequate antibody responses to vaccination are just some of the challenges of lung transplant medicine in the era of SARS-CoV-2. “COVID-19,” said Dr. Narula, “has completely changed the way we practice lung transplant medicine – the way we’re looking both at our recipients and our donors.”
Potential donors are being evaluated with lower respiratory SARS-CoV-2 testing and an abundance of caution. And patients with severe COVID-19 affecting their own lungs are roundly expected to drive up lung transplant volume in the near future. “The whole paradigm has changed,” Dr. Narula said.
Post-acute trajectories
A chart review study published in October by the lung transplant team at the University of Texas Southwestern Medical Center, Dallas, covered 44 consecutive survivors at a median follow-up of 4.5 months from hospital discharge or acute illness (the survival rate was 83.3%). Patients had significantly impaired functional status, and 18 of the 44 (40.9%) had a significant and persistent loss of forced vital capacity or forced expiratory volume in 1 second (>10% from pre–COVID-19 baseline).
Three patients met the criteria for new CLAD after COVID-19 infection, with all three classified as restrictive allograft syndrome (RAS) phenotype.
Moreover, the majority of COVID-19 survivors who had CT chest scans (22 of 28) showed persistent parenchymal opacities – a finding that, regardless of symptomatology, suggests persistent allograft injury, said Amit Banga, MD, associate professor of medicine and medical director of the ex vivo lung perfusion program in UT Southwestern’s lung transplant program.
“The implication is that there may be long-term consequences of COVID-19, perhaps related to some degree of ongoing inflammation and damage,” said Dr. Banga, a coauthor of the postinfection outcomes paper.
The UT Southwestern lung transplant program, which normally performs 60-80 transplants a year, began routine CT scanning 4-5 months into the pandemic, after “stumbling into a few patients who had no symptoms indicative of COVID pneumonia and no changes on an x-ray but significant involvement on a CT,” he said.
Without routine scanning in the general population of COVID-19 patients, Dr. Banga noted, “we’re limited in convincingly saying that COVID is uniquely doing this to lung transplant recipients.” Nor can they conclude that SARS-CoV-2 is unique from other respiratory viruses such as respiratory syncytial virus (RSV) in this regard. (The program has added CT scanning to its protocol for lung transplant recipients afflicted with other respiratory viruses to learn more.)
However, in the big picture, COVID-19 has proven to be far worse for lung transplant recipients than illness with other respiratory viruses, including RSV. “Patients have more frequent and greater loss of lung function, and worse debility from the acute illness,” Dr. Banga said.
“The cornerstones of treatment of both these viruses are very similar, but both the in-hospital course and the postdischarge outcomes are significantly different.”
In an initial paper published in September 2021, Dr. Banga and colleagues compared their first 25 lung transplant patients testing positive for SARS-CoV-2 with a historical cohort of 36 patients with RSV treated during 2016-2018.
Patients with COVID-19 had significantly worse morbidity and mortality, including worse postinfection lung function loss, functional decline, and 3-month survival.
More time, he said, will shed light on the risks of CLAD and the long-term potential for recovery of lung function. Currently, at UT Southwestern, it appears that patients who survive acute illness and the “first 3-6 months after COVID-19, when we’re seeing all the postinfection morbidity, may [enter] a period of stability,” Dr. Banga said.
Overall, he said, patients in their initial cohort are “holding steady” without unusual morbidity, readmissions, or “other setbacks to their allografts.”
At the Mayo Clinic in Jacksonville, which normally performs 40-50 lung transplants a year, transplant physicians have similarly observed significant declines in lung function beyond the acute phase of COVID-19. “Anecdotally, we’re seeing that some patients are beginning to recover some of their lung function, while others have not,” said Dr. Narula. “And we don’t have predictors as to who will progress to CLAD. It’s a big knowledge gap.”
Dr. Narula noted that patients with restrictive allograft syndrome, such as those reported by the UT Southwestern team, “have scarring of the lung and a much worse prognosis than the obstructive type of chronic rejection.” Whether there’s a role for antifibrotic therapy is a question worthy of research.
In UT Southwestern’s analysis, persistently lower absolute lymphocyte counts (< 600/dL) and higher ferritin levels (>150 ng/mL) at the time of hospital discharge were independently associated with significant lung function loss. This finding, reported in their October paper, has helped guide their management practices, Dr. Banga said.
“Persistently elevated ferritin may indicate ongoing inflammation at the allograft level,” he said. “We now send [such patients] home on a longer course of oral corticosteroids.”
At the front end of care for infected lung transplant recipients, Dr. Banga said that his team and physicians at other lung transplant programs are holding the cell-cycle inhibitor component of patients’ maintenance immunosuppression therapy (commonly mycophenolate or azathioprine) once infection is diagnosed to maximize chances of a better outcome.
“There may be variation on how long [the regimens are adjusted],” he said. “We changed our duration from 4 weeks to 2 due to patients developing a rebound worsening in the third and fourth week of acute illness.”
There is significant variation from institution to institution in how viral infections are managed in lung transplant recipients, he and Dr. Narula said. “Our numbers are so small in lung transplant, and we don’t have standardized protocols – it’s one of the biggest challenges in our field,” said Dr. Narula.
Vaccination issues, evaluation of donors
Whether or not immunosuppression regimens should be adjusted prior to vaccination is a controversial question, but is “an absolutely valid one” and is currently being studied in at least one National Institutes of Health–funded trial involving solid organ transplant recipients, said Dr. Wolfe.
“Some have jumped to the conclusion [based on some earlier data] that they should reduce immunosuppression regimens for everyone at the time of vaccination ... but I don’t know the answer yet,” he said. “Balancing staying rejection free with potentially gaining more immune response is complicated ... and it may depend on where the pandemic is going in your area and other factors.”
Reductions aside, Dr. Wolfe tells lung transplant recipients that, based on his approximation of a number of different studies in solid organ transplant recipients, approximately 40%-50% of patients who are immunized with two doses of the COVID-19 mRNA vaccines will develop meaningful antibody levels – and that this rises to 50%-60% after a third dose.
It is difficult to glean from available studies the level of vaccine response for lung transplant recipients specifically. But given that their level of maintenance immunosuppression is higher than for recipients of other donor organs, “as a broad sweep, lung transplant recipients tend to be lower in the pecking order of response,” he said.
Still, “there’s a lot to gain,” he said, pointing to a recent study from the Morbidity and Mortality Weekly Report (2021 Nov 5. doi: 10.15585/mmwr.mm7044e3) showing that effectiveness of mRNA vaccination against COVID-19–associated hospitalization was 77% among immunocompromised adults (compared with 90% in immunocompetent adults).
“This is good vindication to keep vaccinating,” he said, “and perhaps speaks to how difficult it is to assess the vaccine response [through measurement of antibody only].”
Neither Duke University’s transplant program, which performed 100-120 lung transplants a year pre-COVID, nor the programs at UT Southwestern or the Mayo Clinic in Jacksonville require that solid organ transplant candidates be vaccinated against SARS-CoV-2 in order to receive transplants, as some other transplant programs have done. (When asked about the issue, Dr. Banga and Dr. Narula each said that they have had no or little trouble convincing patients awaiting lung transplants of the need for COVID-19 vaccination.)
In an August statement, the American Society of Transplantation recommended vaccination for all solid organ transplant recipients, preferably prior to transplantation, and said that it “support[s] the development of institutional policies regarding pretransplant vaccination.”
The Society is not tracking centers’ vaccination policies. But Kaiser Health News reported in October that a growing number of transplant programs, such as UCHealth in Denver and UW Medicine in Seattle, have decided to either bar patients who refuse to be vaccinated from receiving transplants or give them lower priority on waitlists.
Potential lung donors, meanwhile, must be evaluated with lower respiratory COVID-19 testing, with results available prior to transplantation, according to policy developed by the Organ Procurement and Transplantation Network and effective in May 2021. The policy followed three published cases of donor-derived COVID-19 in lung transplant recipients, said Dr. Wolfe, who wrote about use of COVID-positive donors in an editorial published in October.
In each case, the donor had a negative COVID-19 nasopharyngeal swab at the time of organ procurement but was later found to have the virus on bronchoalveolar lavage, he said.
(The use of other organs from COVID-positive donors is appearing thus far to be safe, Dr. Wolfe noted. In the editorial, he references 13 cases of solid organ transplantation from SARS-CoV-2–infected donors into noninfected recipients; none of the 13 transplant recipients developed COVID-19).
Some questions remain, such as how many lower respiratory tests should be run, and how donors should be evaluated in cases of discordant results. Dr. Banga shared the case of a donor with one positive lower respiratory test result followed by two negative results. After internal debate, and consideration of potential false positives and other issues, the team at UT Southwestern decided to decline the donor, Dr. Banga said.
Other programs are likely making similar, appropriately cautious decisions, said Dr. Wolfe. “There’s no way in real-time donor evaluation to know whether the positive test is active virus that could infect the recipient and replicate ... or whether it’s [picking up] inactive or dead fragments of virus that was there several weeks ago. Our tests don’t differentiate that.”
Transplants in COVID-19 patients
Decision-making about lung transplant candidacy among patients with COVID-19 acute respiratory distress syndrome is complex and in need of a new paradigm.
“Some of these patients have the potential to recover, and they’re going to recover way later than what we’re used to,” said Dr. Banga. “We can’t extrapolate for COVID ARDS what we’ve learned for any other virus-related ARDS.”
Dr. Narula also has recently seen at least one COVID-19 patient on ECMO and under evaluation for transplantation recover. “We do not want to transplant too early,” he said, noting that there is consensus that lung transplant should be pursued only when the damage is deemed irreversible clinically and radiologically in the best judgment of the team. Still, “for many of these patients the only exit route will be lung transplants. For the next 12-24 months, a significant proportion of our lung transplant patients will have had post-COVID–related lung damage.”
As of October 2021, 233 lung transplants had been performed in the United States in recipients whose primary diagnosis was reported as COVID related, said Anne Paschke, media relations specialist with the United Network for Organ Sharing.
Dr. Banga, Dr. Wolfe, and Dr. Narula reported that they have no relevant disclosures.
Data is sparse thus far, but there is concern in lung transplant medicine about the long-term risk of chronic lung allograft dysfunction (CLAD) and a potentially shortened longevity of transplanted lungs in recipients who become ill with COVID-19.
“My fear is that we’re potentially sitting on this iceberg worth of people who, come 6 months or a year from [the acute phase of] their COVID illness, will in fact have earlier and progressive, chronic rejection,” said Cameron R. Wolfe, MBBS, MPH, associate professor of medicine in transplant infectious disease at Duke University, Durham, N.C.
Lower respiratory viral infections have long been concerning for lung transplant recipients given their propensity to cause scarring, a decline in lung function, and a heightened risk of allograft rejection. Time will tell whether lung transplant recipients who survive COVID-19 follow a similar path, or one that is worse, he said.
Short-term data
Outcomes beyond hospitalization and acute illness for lung transplant recipients affected by COVID-19 have been reported in the literature by only a few lung transplant programs. These reports – as well as anecdotal experiences being informally shared among transplant programs – have raised the specter of more severe dysfunction following the acute phase and more early CLAD, said Tathagat Narula, MD, assistant professor of medicine at the Mayo Medical School, Rochester, Minn., and a consultant in lung transplantation at the Mayo Clinic’s Jacksonville program.
“The available data cover only 3-6 months out. We don’t know what will happen in the next 6 months and beyond,” Dr. Narula said in an interview.
The risks of COVID-19 in already-transplanted patients and issues relating to the inadequate antibody responses to vaccination are just some of the challenges of lung transplant medicine in the era of SARS-CoV-2. “COVID-19,” said Dr. Narula, “has completely changed the way we practice lung transplant medicine – the way we’re looking both at our recipients and our donors.”
Potential donors are being evaluated with lower respiratory SARS-CoV-2 testing and an abundance of caution. And patients with severe COVID-19 affecting their own lungs are roundly expected to drive up lung transplant volume in the near future. “The whole paradigm has changed,” Dr. Narula said.
Post-acute trajectories
A chart review study published in October by the lung transplant team at the University of Texas Southwestern Medical Center, Dallas, covered 44 consecutive survivors at a median follow-up of 4.5 months from hospital discharge or acute illness (the survival rate was 83.3%). Patients had significantly impaired functional status, and 18 of the 44 (40.9%) had a significant and persistent loss of forced vital capacity or forced expiratory volume in 1 second (>10% from pre–COVID-19 baseline).
Three patients met the criteria for new CLAD after COVID-19 infection, with all three classified as restrictive allograft syndrome (RAS) phenotype.
Moreover, the majority of COVID-19 survivors who had CT chest scans (22 of 28) showed persistent parenchymal opacities – a finding that, regardless of symptomatology, suggests persistent allograft injury, said Amit Banga, MD, associate professor of medicine and medical director of the ex vivo lung perfusion program in UT Southwestern’s lung transplant program.
“The implication is that there may be long-term consequences of COVID-19, perhaps related to some degree of ongoing inflammation and damage,” said Dr. Banga, a coauthor of the postinfection outcomes paper.
The UT Southwestern lung transplant program, which normally performs 60-80 transplants a year, began routine CT scanning 4-5 months into the pandemic, after “stumbling into a few patients who had no symptoms indicative of COVID pneumonia and no changes on an x-ray but significant involvement on a CT,” he said.
Without routine scanning in the general population of COVID-19 patients, Dr. Banga noted, “we’re limited in convincingly saying that COVID is uniquely doing this to lung transplant recipients.” Nor can they conclude that SARS-CoV-2 is unique from other respiratory viruses such as respiratory syncytial virus (RSV) in this regard. (The program has added CT scanning to its protocol for lung transplant recipients afflicted with other respiratory viruses to learn more.)
However, in the big picture, COVID-19 has proven to be far worse for lung transplant recipients than illness with other respiratory viruses, including RSV. “Patients have more frequent and greater loss of lung function, and worse debility from the acute illness,” Dr. Banga said.
“The cornerstones of treatment of both these viruses are very similar, but both the in-hospital course and the postdischarge outcomes are significantly different.”
In an initial paper published in September 2021, Dr. Banga and colleagues compared their first 25 lung transplant patients testing positive for SARS-CoV-2 with a historical cohort of 36 patients with RSV treated during 2016-2018.
Patients with COVID-19 had significantly worse morbidity and mortality, including worse postinfection lung function loss, functional decline, and 3-month survival.
More time, he said, will shed light on the risks of CLAD and the long-term potential for recovery of lung function. Currently, at UT Southwestern, it appears that patients who survive acute illness and the “first 3-6 months after COVID-19, when we’re seeing all the postinfection morbidity, may [enter] a period of stability,” Dr. Banga said.
Overall, he said, patients in their initial cohort are “holding steady” without unusual morbidity, readmissions, or “other setbacks to their allografts.”
At the Mayo Clinic in Jacksonville, which normally performs 40-50 lung transplants a year, transplant physicians have similarly observed significant declines in lung function beyond the acute phase of COVID-19. “Anecdotally, we’re seeing that some patients are beginning to recover some of their lung function, while others have not,” said Dr. Narula. “And we don’t have predictors as to who will progress to CLAD. It’s a big knowledge gap.”
Dr. Narula noted that patients with restrictive allograft syndrome, such as those reported by the UT Southwestern team, “have scarring of the lung and a much worse prognosis than the obstructive type of chronic rejection.” Whether there’s a role for antifibrotic therapy is a question worthy of research.
In UT Southwestern’s analysis, persistently lower absolute lymphocyte counts (< 600/dL) and higher ferritin levels (>150 ng/mL) at the time of hospital discharge were independently associated with significant lung function loss. This finding, reported in their October paper, has helped guide their management practices, Dr. Banga said.
“Persistently elevated ferritin may indicate ongoing inflammation at the allograft level,” he said. “We now send [such patients] home on a longer course of oral corticosteroids.”
At the front end of care for infected lung transplant recipients, Dr. Banga said that his team and physicians at other lung transplant programs are holding the cell-cycle inhibitor component of patients’ maintenance immunosuppression therapy (commonly mycophenolate or azathioprine) once infection is diagnosed to maximize chances of a better outcome.
“There may be variation on how long [the regimens are adjusted],” he said. “We changed our duration from 4 weeks to 2 due to patients developing a rebound worsening in the third and fourth week of acute illness.”
There is significant variation from institution to institution in how viral infections are managed in lung transplant recipients, he and Dr. Narula said. “Our numbers are so small in lung transplant, and we don’t have standardized protocols – it’s one of the biggest challenges in our field,” said Dr. Narula.
Vaccination issues, evaluation of donors
Whether or not immunosuppression regimens should be adjusted prior to vaccination is a controversial question, but is “an absolutely valid one” and is currently being studied in at least one National Institutes of Health–funded trial involving solid organ transplant recipients, said Dr. Wolfe.
“Some have jumped to the conclusion [based on some earlier data] that they should reduce immunosuppression regimens for everyone at the time of vaccination ... but I don’t know the answer yet,” he said. “Balancing staying rejection free with potentially gaining more immune response is complicated ... and it may depend on where the pandemic is going in your area and other factors.”
Reductions aside, Dr. Wolfe tells lung transplant recipients that, based on his approximation of a number of different studies in solid organ transplant recipients, approximately 40%-50% of patients who are immunized with two doses of the COVID-19 mRNA vaccines will develop meaningful antibody levels – and that this rises to 50%-60% after a third dose.
It is difficult to glean from available studies the level of vaccine response for lung transplant recipients specifically. But given that their level of maintenance immunosuppression is higher than for recipients of other donor organs, “as a broad sweep, lung transplant recipients tend to be lower in the pecking order of response,” he said.
Still, “there’s a lot to gain,” he said, pointing to a recent study from the Morbidity and Mortality Weekly Report (2021 Nov 5. doi: 10.15585/mmwr.mm7044e3) showing that effectiveness of mRNA vaccination against COVID-19–associated hospitalization was 77% among immunocompromised adults (compared with 90% in immunocompetent adults).
“This is good vindication to keep vaccinating,” he said, “and perhaps speaks to how difficult it is to assess the vaccine response [through measurement of antibody only].”
Neither Duke University’s transplant program, which performed 100-120 lung transplants a year pre-COVID, nor the programs at UT Southwestern or the Mayo Clinic in Jacksonville require that solid organ transplant candidates be vaccinated against SARS-CoV-2 in order to receive transplants, as some other transplant programs have done. (When asked about the issue, Dr. Banga and Dr. Narula each said that they have had no or little trouble convincing patients awaiting lung transplants of the need for COVID-19 vaccination.)
In an August statement, the American Society of Transplantation recommended vaccination for all solid organ transplant recipients, preferably prior to transplantation, and said that it “support[s] the development of institutional policies regarding pretransplant vaccination.”
The Society is not tracking centers’ vaccination policies. But Kaiser Health News reported in October that a growing number of transplant programs, such as UCHealth in Denver and UW Medicine in Seattle, have decided to either bar patients who refuse to be vaccinated from receiving transplants or give them lower priority on waitlists.
Potential lung donors, meanwhile, must be evaluated with lower respiratory COVID-19 testing, with results available prior to transplantation, according to policy developed by the Organ Procurement and Transplantation Network and effective in May 2021. The policy followed three published cases of donor-derived COVID-19 in lung transplant recipients, said Dr. Wolfe, who wrote about use of COVID-positive donors in an editorial published in October.
In each case, the donor had a negative COVID-19 nasopharyngeal swab at the time of organ procurement but was later found to have the virus on bronchoalveolar lavage, he said.
(The use of other organs from COVID-positive donors is appearing thus far to be safe, Dr. Wolfe noted. In the editorial, he references 13 cases of solid organ transplantation from SARS-CoV-2–infected donors into noninfected recipients; none of the 13 transplant recipients developed COVID-19).
Some questions remain, such as how many lower respiratory tests should be run, and how donors should be evaluated in cases of discordant results. Dr. Banga shared the case of a donor with one positive lower respiratory test result followed by two negative results. After internal debate, and consideration of potential false positives and other issues, the team at UT Southwestern decided to decline the donor, Dr. Banga said.
Other programs are likely making similar, appropriately cautious decisions, said Dr. Wolfe. “There’s no way in real-time donor evaluation to know whether the positive test is active virus that could infect the recipient and replicate ... or whether it’s [picking up] inactive or dead fragments of virus that was there several weeks ago. Our tests don’t differentiate that.”
Transplants in COVID-19 patients
Decision-making about lung transplant candidacy among patients with COVID-19 acute respiratory distress syndrome is complex and in need of a new paradigm.
“Some of these patients have the potential to recover, and they’re going to recover way later than what we’re used to,” said Dr. Banga. “We can’t extrapolate for COVID ARDS what we’ve learned for any other virus-related ARDS.”
Dr. Narula also has recently seen at least one COVID-19 patient on ECMO and under evaluation for transplantation recover. “We do not want to transplant too early,” he said, noting that there is consensus that lung transplant should be pursued only when the damage is deemed irreversible clinically and radiologically in the best judgment of the team. Still, “for many of these patients the only exit route will be lung transplants. For the next 12-24 months, a significant proportion of our lung transplant patients will have had post-COVID–related lung damage.”
As of October 2021, 233 lung transplants had been performed in the United States in recipients whose primary diagnosis was reported as COVID related, said Anne Paschke, media relations specialist with the United Network for Organ Sharing.
Dr. Banga, Dr. Wolfe, and Dr. Narula reported that they have no relevant disclosures.
Coping with a shattered immune system: COVID and beyond
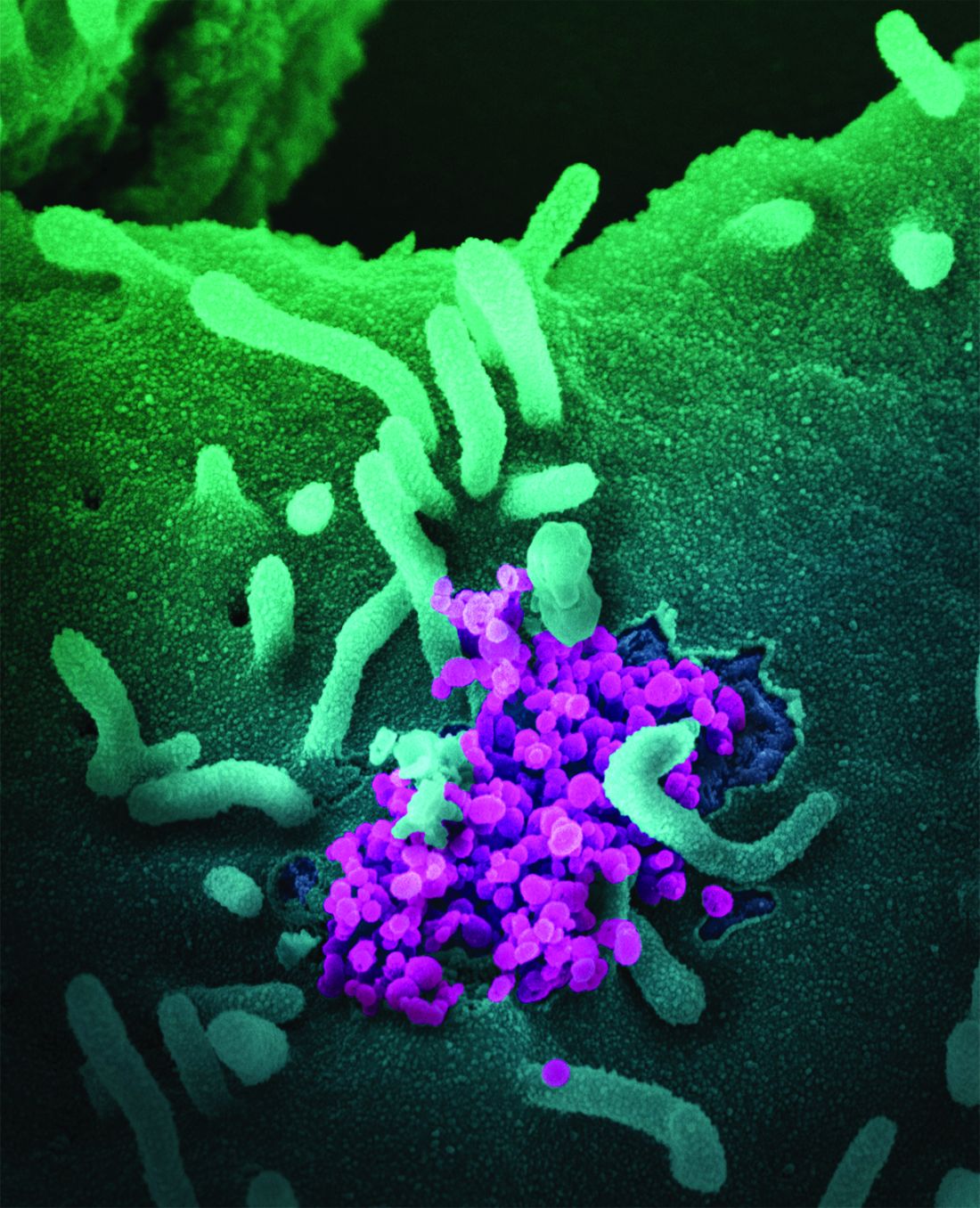
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
Hair follicle miniaturization common in persistent chemo-induced alopecia, case series suggests
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
FROM JAMA DERMATOLOGY
Dr. Judy C. Washington shows URM physicians how to lead
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
Western diet promoted skin, joint inflammation in preclinical study
A short-term Western diet facilitated the development of interleukin (IL)-23-mediated psoriasis-like skin and joint inflammation and caused shifts in the intestinal microbiota in a murine model – , say the investigators and other experts who reviewed the findings.
The mice did not become obese during the short duration of the multilayered study, which suggests that a Western diet (high sugar, moderate fat) can be impactful independent of obesity, Samuel T. Hwang, MD, PhD, professor and chair of dermatology at the University of California, Davis, and senior author of the study, said in an interview. The study was published in the Journal of Investigative Dermatology.
In an accompanying commentary, Renuka R. Nayak, MD, PhD, of the department of rheumatology at the University of California, San Francisco, wrote that the findings “add to the mounting evidence suggesting that diet has a prominent role in the treatment of psoriasis and [psoriatic arthritis] and raise the possibility that the microbiome may contribute to disease severity”.
Mice were fed a Western diet (WD) or conventional chow diet for 6 weeks and then injected with IL-23 minicircle (MC) DNA to induce systemic IL-23 overexpression – or a control minicircle DNA injection – and continued on these diets for another 4 weeks.
The mice in the WD/IL-23 MC DNA group developed erythema and scaling and increased epidermal thickness in the ears; such changes were “remarkably milder” or nonexistent in the other groups. Skin and joint immune cell populations, such as gamma delta T cells, neutrophils, and T helper type 17 cytokines were elevated in WD-fed mice, as were other markers of IL-23-mediated joint inflammation.
Recent research has suggested that the gut microbiota is dysbiotic in patients with psoriasis, and this new study found that WD-fed mice had less microbial diversity than that of mice fed a conventional diet. After IL-23 MC delivery, WD-fed reduced microbial diversity and pronounced dysbiosis.
“When we combined the Western diet and IL-23, we saw some very different microbes in abundance. The whole landscape changed,” Dr. Hwang said in the interview.
The data “suggest that WD and overexpression of IL-23 may contribute to gut microbiota dysbiosis in a synergistic and complex manner,” he and his coinvestigators wrote.
Treatment with broad-spectrum antibiotics suppressed IL-23-mediated skin and joint inflammation in the WD-fed mice – and moderately affected skin inflammation in conventionally-fed mice as well – which affirmed the role of dysbiosis.
And “notably,” in another layer of the study, mice that switched diets from a WD to a conventional diet had reduced skin and joint inflammation and increased diversity of gut microbiota. (Mice that were fed a WD for 6 weeks and given the IL-23 MC DNA were randomized to continue this diet for another 4 weeks or switch to a conventional diet.)
Commenting on the new research, Wilson Liao, MD, professor and vice chair of research in the department of dermatology at the University of California, San Francisco, said it “provides evidence” that diet can affect not only psoriasis, but psoriatic arthritis (PsA) as well, “through altering the ratio of good to bad bacteria in the gut.”
Going forward, better understanding “which specific gut bacteria and bacterial products lead to increased psoriatic inflammation, and the immunologic mechanism by which this occurs” will be important and could lead to novel treatments for psoriasis and PsA, said Dr. Liao, director of the UCSF Psoriasis and Skin Treatment Center.
Next on his research agenda, Dr. Hwang said, is the question of “how microbiota in the gut are actually able to influence inflammation at very distant sites in the joints and the skin.
“We want to understand the metabolic mechanisms,” he said, noting that “we invariably talk about cytokines, but there are other substances, like certain bile acids that are metabolized through the gut microbiome,” which may play a role.
The findings also offer a basis for treatment experiments in humans – of diet, probiotic therapy, or selective antibiotic modulation, for instance, Dr. Hwang said.
And in the meantime, the findings should encourage patients who are interested in making dietary changes, such as reducing sugar intake. “There’s wide interest – patients will ask, is there something I can change to make this better?” Dr. Hwang said. “Before, we could say it might be logical, but now we have some evidence. The message now is [high-sugar, moderate-fat] diets, apart from their ability to stimulate obesity, probably have some effects.”
Dietary change may not replace the need for other psoriasis treatments, he said, “but I think there’s good reason to believe that if you do change your diet, your treatment will be better than it would be without that dietary change,” he said.
In their discussion, Dr. Hwang and coauthors note that WD with IL-23 overexpression also decreased the mRNA expression of barrier-forming tight junction proteins, thus increasing intestinal permeability. This finding may be relevant, they wrote, because “leaky gut has been proposed as a pathogenic link between unhealthy diet, gut dysbiosis, and enhanced immune response,” and has been observed in a number of autoimmune diseases, including psoriasis.
Dr. Hwang, lead author Zhenrui Shi, MD, PhD, and coauthors reported no conflicts of interest. Their study was supported by the National Psoriasis Foundation, as well as the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the National Cancer Institute.
A short-term Western diet facilitated the development of interleukin (IL)-23-mediated psoriasis-like skin and joint inflammation and caused shifts in the intestinal microbiota in a murine model – , say the investigators and other experts who reviewed the findings.
The mice did not become obese during the short duration of the multilayered study, which suggests that a Western diet (high sugar, moderate fat) can be impactful independent of obesity, Samuel T. Hwang, MD, PhD, professor and chair of dermatology at the University of California, Davis, and senior author of the study, said in an interview. The study was published in the Journal of Investigative Dermatology.
In an accompanying commentary, Renuka R. Nayak, MD, PhD, of the department of rheumatology at the University of California, San Francisco, wrote that the findings “add to the mounting evidence suggesting that diet has a prominent role in the treatment of psoriasis and [psoriatic arthritis] and raise the possibility that the microbiome may contribute to disease severity”.
Mice were fed a Western diet (WD) or conventional chow diet for 6 weeks and then injected with IL-23 minicircle (MC) DNA to induce systemic IL-23 overexpression – or a control minicircle DNA injection – and continued on these diets for another 4 weeks.
The mice in the WD/IL-23 MC DNA group developed erythema and scaling and increased epidermal thickness in the ears; such changes were “remarkably milder” or nonexistent in the other groups. Skin and joint immune cell populations, such as gamma delta T cells, neutrophils, and T helper type 17 cytokines were elevated in WD-fed mice, as were other markers of IL-23-mediated joint inflammation.
Recent research has suggested that the gut microbiota is dysbiotic in patients with psoriasis, and this new study found that WD-fed mice had less microbial diversity than that of mice fed a conventional diet. After IL-23 MC delivery, WD-fed reduced microbial diversity and pronounced dysbiosis.
“When we combined the Western diet and IL-23, we saw some very different microbes in abundance. The whole landscape changed,” Dr. Hwang said in the interview.
The data “suggest that WD and overexpression of IL-23 may contribute to gut microbiota dysbiosis in a synergistic and complex manner,” he and his coinvestigators wrote.
Treatment with broad-spectrum antibiotics suppressed IL-23-mediated skin and joint inflammation in the WD-fed mice – and moderately affected skin inflammation in conventionally-fed mice as well – which affirmed the role of dysbiosis.
And “notably,” in another layer of the study, mice that switched diets from a WD to a conventional diet had reduced skin and joint inflammation and increased diversity of gut microbiota. (Mice that were fed a WD for 6 weeks and given the IL-23 MC DNA were randomized to continue this diet for another 4 weeks or switch to a conventional diet.)
Commenting on the new research, Wilson Liao, MD, professor and vice chair of research in the department of dermatology at the University of California, San Francisco, said it “provides evidence” that diet can affect not only psoriasis, but psoriatic arthritis (PsA) as well, “through altering the ratio of good to bad bacteria in the gut.”
Going forward, better understanding “which specific gut bacteria and bacterial products lead to increased psoriatic inflammation, and the immunologic mechanism by which this occurs” will be important and could lead to novel treatments for psoriasis and PsA, said Dr. Liao, director of the UCSF Psoriasis and Skin Treatment Center.
Next on his research agenda, Dr. Hwang said, is the question of “how microbiota in the gut are actually able to influence inflammation at very distant sites in the joints and the skin.
“We want to understand the metabolic mechanisms,” he said, noting that “we invariably talk about cytokines, but there are other substances, like certain bile acids that are metabolized through the gut microbiome,” which may play a role.
The findings also offer a basis for treatment experiments in humans – of diet, probiotic therapy, or selective antibiotic modulation, for instance, Dr. Hwang said.
And in the meantime, the findings should encourage patients who are interested in making dietary changes, such as reducing sugar intake. “There’s wide interest – patients will ask, is there something I can change to make this better?” Dr. Hwang said. “Before, we could say it might be logical, but now we have some evidence. The message now is [high-sugar, moderate-fat] diets, apart from their ability to stimulate obesity, probably have some effects.”
Dietary change may not replace the need for other psoriasis treatments, he said, “but I think there’s good reason to believe that if you do change your diet, your treatment will be better than it would be without that dietary change,” he said.
In their discussion, Dr. Hwang and coauthors note that WD with IL-23 overexpression also decreased the mRNA expression of barrier-forming tight junction proteins, thus increasing intestinal permeability. This finding may be relevant, they wrote, because “leaky gut has been proposed as a pathogenic link between unhealthy diet, gut dysbiosis, and enhanced immune response,” and has been observed in a number of autoimmune diseases, including psoriasis.
Dr. Hwang, lead author Zhenrui Shi, MD, PhD, and coauthors reported no conflicts of interest. Their study was supported by the National Psoriasis Foundation, as well as the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the National Cancer Institute.
A short-term Western diet facilitated the development of interleukin (IL)-23-mediated psoriasis-like skin and joint inflammation and caused shifts in the intestinal microbiota in a murine model – , say the investigators and other experts who reviewed the findings.
The mice did not become obese during the short duration of the multilayered study, which suggests that a Western diet (high sugar, moderate fat) can be impactful independent of obesity, Samuel T. Hwang, MD, PhD, professor and chair of dermatology at the University of California, Davis, and senior author of the study, said in an interview. The study was published in the Journal of Investigative Dermatology.
In an accompanying commentary, Renuka R. Nayak, MD, PhD, of the department of rheumatology at the University of California, San Francisco, wrote that the findings “add to the mounting evidence suggesting that diet has a prominent role in the treatment of psoriasis and [psoriatic arthritis] and raise the possibility that the microbiome may contribute to disease severity”.
Mice were fed a Western diet (WD) or conventional chow diet for 6 weeks and then injected with IL-23 minicircle (MC) DNA to induce systemic IL-23 overexpression – or a control minicircle DNA injection – and continued on these diets for another 4 weeks.
The mice in the WD/IL-23 MC DNA group developed erythema and scaling and increased epidermal thickness in the ears; such changes were “remarkably milder” or nonexistent in the other groups. Skin and joint immune cell populations, such as gamma delta T cells, neutrophils, and T helper type 17 cytokines were elevated in WD-fed mice, as were other markers of IL-23-mediated joint inflammation.
Recent research has suggested that the gut microbiota is dysbiotic in patients with psoriasis, and this new study found that WD-fed mice had less microbial diversity than that of mice fed a conventional diet. After IL-23 MC delivery, WD-fed reduced microbial diversity and pronounced dysbiosis.
“When we combined the Western diet and IL-23, we saw some very different microbes in abundance. The whole landscape changed,” Dr. Hwang said in the interview.
The data “suggest that WD and overexpression of IL-23 may contribute to gut microbiota dysbiosis in a synergistic and complex manner,” he and his coinvestigators wrote.
Treatment with broad-spectrum antibiotics suppressed IL-23-mediated skin and joint inflammation in the WD-fed mice – and moderately affected skin inflammation in conventionally-fed mice as well – which affirmed the role of dysbiosis.
And “notably,” in another layer of the study, mice that switched diets from a WD to a conventional diet had reduced skin and joint inflammation and increased diversity of gut microbiota. (Mice that were fed a WD for 6 weeks and given the IL-23 MC DNA were randomized to continue this diet for another 4 weeks or switch to a conventional diet.)
Commenting on the new research, Wilson Liao, MD, professor and vice chair of research in the department of dermatology at the University of California, San Francisco, said it “provides evidence” that diet can affect not only psoriasis, but psoriatic arthritis (PsA) as well, “through altering the ratio of good to bad bacteria in the gut.”
Going forward, better understanding “which specific gut bacteria and bacterial products lead to increased psoriatic inflammation, and the immunologic mechanism by which this occurs” will be important and could lead to novel treatments for psoriasis and PsA, said Dr. Liao, director of the UCSF Psoriasis and Skin Treatment Center.
Next on his research agenda, Dr. Hwang said, is the question of “how microbiota in the gut are actually able to influence inflammation at very distant sites in the joints and the skin.
“We want to understand the metabolic mechanisms,” he said, noting that “we invariably talk about cytokines, but there are other substances, like certain bile acids that are metabolized through the gut microbiome,” which may play a role.
The findings also offer a basis for treatment experiments in humans – of diet, probiotic therapy, or selective antibiotic modulation, for instance, Dr. Hwang said.
And in the meantime, the findings should encourage patients who are interested in making dietary changes, such as reducing sugar intake. “There’s wide interest – patients will ask, is there something I can change to make this better?” Dr. Hwang said. “Before, we could say it might be logical, but now we have some evidence. The message now is [high-sugar, moderate-fat] diets, apart from their ability to stimulate obesity, probably have some effects.”
Dietary change may not replace the need for other psoriasis treatments, he said, “but I think there’s good reason to believe that if you do change your diet, your treatment will be better than it would be without that dietary change,” he said.
In their discussion, Dr. Hwang and coauthors note that WD with IL-23 overexpression also decreased the mRNA expression of barrier-forming tight junction proteins, thus increasing intestinal permeability. This finding may be relevant, they wrote, because “leaky gut has been proposed as a pathogenic link between unhealthy diet, gut dysbiosis, and enhanced immune response,” and has been observed in a number of autoimmune diseases, including psoriasis.
Dr. Hwang, lead author Zhenrui Shi, MD, PhD, and coauthors reported no conflicts of interest. Their study was supported by the National Psoriasis Foundation, as well as the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the National Cancer Institute.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Study estimates carbon footprint reduction of virtual isotretinoin visits
: A reduction of 5,137 kg of greenhouse gas emissions in carbon dioxide equivalents.
In what they say is “one of the first studies to evaluate the environmental impact of any aspect of dermatology,” the authors of the retrospective cross-sectional study identified patients who had virtual visits for isotretinoin management between March 25 and May 29, 2020, – the period during which all such visits were conducted virtually in keeping with hospital recommendations to minimize the spread of COVID-19.
The investigators, from the department of dermatology and the department of civil and environmental engineering at West Virginia University, Morgantown, then counted the number of virtual visits that occurred during this period and through Dec. 1, 2020, (175 virtual visits), calculated the distance patients would have traveled round-trip had these visits been in-person, and converted miles saved into the environmental impact using U.S. Environmental Protection Agency and Federal Highway Administration data and relevant EPA standards.
Most patients had elected to continue virtual visits after May 29, the point at which patients were given the option to return to the WVUH clinic. (Patients who initiated treatment during the 2-month identification period were not included.)
The investigators determined that virtual management of isotretinoin saved a median of 37.8 miles per visit during the study period of March 25 to Dec. 1, and estimated that the virtual visits reduced total travel by 14,450 miles. For the analysis, patients were assumed to use light-duty vehicles.
In addition to calculating the reduction in emissions during the study period (5,137 kg of CO2equivalents) they used patient census data from 2019 to 2020 and data from the study period to project the mileage – and the associated emissions – that would be saved annually if all in-person visits for isotretinoin management occurred virtually.
Their calculation for a projected emissions reduction with 1 year of all-virtual isotretinoin management was 49,400 kg of greenhouse gas emissions in CO2equivalents. This is the emission load released when 24,690 kg of coal are burned or 6.3 million smartphones are charged, the researchers wrote.
“Considering that more than 1,000,000 prescriptions of isotretinoin are authorized annually in the United States, the environmental impact could be magnified if virtual delivery of isotretinoin care is adopted on a national scale,” they commented.“Given the serious consequences of global climate change, analysis of the environmental impact of all fields of medicine, including dermatology, is warranted,” they added.
The reduced greenhouse gas emissions are “definitely [being taken] into consideration for future decisions about virtual visits” in the department of dermatology, said Zachary Zinn, MD, residency director and associate professor in the department of dermatology at West Virginia University, Morgantown, who is the senior author of the study. “The main benefit of virtual care in my opinion,” he said in an interview, “is the potential to reduce our carbon footprint.”
Justin Lee, MD, an intern at WVU and the study’s first author, said that the research team was motivated to think about how they “could reduce the negative environmental impact of practicing dermatology” after they read a paper about the environmental impact of endoscopy, written by a gastroenterologist.
In the study, no pregnancies occurred and monthly tests were performed, but “formal assessment of pregnancy risk with virtual isotretinoin management would be warranted,” Dr. Lee and coauthors wrote, noting too that, while no differences were seen with respect to isotretinoin side effects, these were not formally analyzed.
Dr. Zinn said that he and colleagues at WVUH are currently conducting clinical trials to assess the quality and efficacy of virtual care for patients with acne, atopic dermatitis, and psoriasis. Delivering care virtually “will be easier to do if there are data supporting [its] quality and efficacy,” he said. Rosacea is another condition that may be amendable to virtual care, he noted.
Meanwhile, he said, isotretinoin management is “well suited” for virtual visits. When initiating isotretinoin treatment, Dr. Zinn now “proactively inquires” if patients would like to pursue their follow-up visits virtually. “I’ll note that it will save the time and decrease the burden of travel, including the financial cost as well as the environmental cost of travel,” he said, estimating that about half of their management visits are currently virtual.
Asked about the study, Misha Rosenbach, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said the reduced carbon footprint calculated by the researchers and its downstream health benefits “should be taken into consideration by [dermatology] departments, insurers and policymakers” when making decisions about teledermatology.
While environmental impact is “not something I think most institutions are considering for virtual versus in-person care, they should be. And some are,” said Dr. Rosenbach, a founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues.
Limitations of the study include the generalizability of the results. The impact of virtual isotretinoin management “may be less in predominantly urban areas” than it is in predominately rural West Virginia, the study authors note. And in the case of West Virginia, travel to a local laboratory and pharmacy offsets some of the environmental benefits for the virtual care, they noted. Such travel wasn’t accounted for in the study, but it was found to be a fraction of travel to the WVU hospital clinic. (Patients traveled a median of 5.8 miles to a lab 2.4 times from March 25 to Dec. 1, 2020.)
Dr. Lee will start his dermatology residency at WVU next year. The study was funded by a grant from the U.S. National Science Foundation. The authors have no relevant conflicts of interest, according to Dr. Lee.
: A reduction of 5,137 kg of greenhouse gas emissions in carbon dioxide equivalents.
In what they say is “one of the first studies to evaluate the environmental impact of any aspect of dermatology,” the authors of the retrospective cross-sectional study identified patients who had virtual visits for isotretinoin management between March 25 and May 29, 2020, – the period during which all such visits were conducted virtually in keeping with hospital recommendations to minimize the spread of COVID-19.
The investigators, from the department of dermatology and the department of civil and environmental engineering at West Virginia University, Morgantown, then counted the number of virtual visits that occurred during this period and through Dec. 1, 2020, (175 virtual visits), calculated the distance patients would have traveled round-trip had these visits been in-person, and converted miles saved into the environmental impact using U.S. Environmental Protection Agency and Federal Highway Administration data and relevant EPA standards.
Most patients had elected to continue virtual visits after May 29, the point at which patients were given the option to return to the WVUH clinic. (Patients who initiated treatment during the 2-month identification period were not included.)
The investigators determined that virtual management of isotretinoin saved a median of 37.8 miles per visit during the study period of March 25 to Dec. 1, and estimated that the virtual visits reduced total travel by 14,450 miles. For the analysis, patients were assumed to use light-duty vehicles.
In addition to calculating the reduction in emissions during the study period (5,137 kg of CO2equivalents) they used patient census data from 2019 to 2020 and data from the study period to project the mileage – and the associated emissions – that would be saved annually if all in-person visits for isotretinoin management occurred virtually.
Their calculation for a projected emissions reduction with 1 year of all-virtual isotretinoin management was 49,400 kg of greenhouse gas emissions in CO2equivalents. This is the emission load released when 24,690 kg of coal are burned or 6.3 million smartphones are charged, the researchers wrote.
“Considering that more than 1,000,000 prescriptions of isotretinoin are authorized annually in the United States, the environmental impact could be magnified if virtual delivery of isotretinoin care is adopted on a national scale,” they commented.“Given the serious consequences of global climate change, analysis of the environmental impact of all fields of medicine, including dermatology, is warranted,” they added.
The reduced greenhouse gas emissions are “definitely [being taken] into consideration for future decisions about virtual visits” in the department of dermatology, said Zachary Zinn, MD, residency director and associate professor in the department of dermatology at West Virginia University, Morgantown, who is the senior author of the study. “The main benefit of virtual care in my opinion,” he said in an interview, “is the potential to reduce our carbon footprint.”
Justin Lee, MD, an intern at WVU and the study’s first author, said that the research team was motivated to think about how they “could reduce the negative environmental impact of practicing dermatology” after they read a paper about the environmental impact of endoscopy, written by a gastroenterologist.
In the study, no pregnancies occurred and monthly tests were performed, but “formal assessment of pregnancy risk with virtual isotretinoin management would be warranted,” Dr. Lee and coauthors wrote, noting too that, while no differences were seen with respect to isotretinoin side effects, these were not formally analyzed.
Dr. Zinn said that he and colleagues at WVUH are currently conducting clinical trials to assess the quality and efficacy of virtual care for patients with acne, atopic dermatitis, and psoriasis. Delivering care virtually “will be easier to do if there are data supporting [its] quality and efficacy,” he said. Rosacea is another condition that may be amendable to virtual care, he noted.
Meanwhile, he said, isotretinoin management is “well suited” for virtual visits. When initiating isotretinoin treatment, Dr. Zinn now “proactively inquires” if patients would like to pursue their follow-up visits virtually. “I’ll note that it will save the time and decrease the burden of travel, including the financial cost as well as the environmental cost of travel,” he said, estimating that about half of their management visits are currently virtual.
Asked about the study, Misha Rosenbach, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said the reduced carbon footprint calculated by the researchers and its downstream health benefits “should be taken into consideration by [dermatology] departments, insurers and policymakers” when making decisions about teledermatology.
While environmental impact is “not something I think most institutions are considering for virtual versus in-person care, they should be. And some are,” said Dr. Rosenbach, a founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues.
Limitations of the study include the generalizability of the results. The impact of virtual isotretinoin management “may be less in predominantly urban areas” than it is in predominately rural West Virginia, the study authors note. And in the case of West Virginia, travel to a local laboratory and pharmacy offsets some of the environmental benefits for the virtual care, they noted. Such travel wasn’t accounted for in the study, but it was found to be a fraction of travel to the WVU hospital clinic. (Patients traveled a median of 5.8 miles to a lab 2.4 times from March 25 to Dec. 1, 2020.)
Dr. Lee will start his dermatology residency at WVU next year. The study was funded by a grant from the U.S. National Science Foundation. The authors have no relevant conflicts of interest, according to Dr. Lee.
: A reduction of 5,137 kg of greenhouse gas emissions in carbon dioxide equivalents.
In what they say is “one of the first studies to evaluate the environmental impact of any aspect of dermatology,” the authors of the retrospective cross-sectional study identified patients who had virtual visits for isotretinoin management between March 25 and May 29, 2020, – the period during which all such visits were conducted virtually in keeping with hospital recommendations to minimize the spread of COVID-19.
The investigators, from the department of dermatology and the department of civil and environmental engineering at West Virginia University, Morgantown, then counted the number of virtual visits that occurred during this period and through Dec. 1, 2020, (175 virtual visits), calculated the distance patients would have traveled round-trip had these visits been in-person, and converted miles saved into the environmental impact using U.S. Environmental Protection Agency and Federal Highway Administration data and relevant EPA standards.
Most patients had elected to continue virtual visits after May 29, the point at which patients were given the option to return to the WVUH clinic. (Patients who initiated treatment during the 2-month identification period were not included.)
The investigators determined that virtual management of isotretinoin saved a median of 37.8 miles per visit during the study period of March 25 to Dec. 1, and estimated that the virtual visits reduced total travel by 14,450 miles. For the analysis, patients were assumed to use light-duty vehicles.
In addition to calculating the reduction in emissions during the study period (5,137 kg of CO2equivalents) they used patient census data from 2019 to 2020 and data from the study period to project the mileage – and the associated emissions – that would be saved annually if all in-person visits for isotretinoin management occurred virtually.
Their calculation for a projected emissions reduction with 1 year of all-virtual isotretinoin management was 49,400 kg of greenhouse gas emissions in CO2equivalents. This is the emission load released when 24,690 kg of coal are burned or 6.3 million smartphones are charged, the researchers wrote.
“Considering that more than 1,000,000 prescriptions of isotretinoin are authorized annually in the United States, the environmental impact could be magnified if virtual delivery of isotretinoin care is adopted on a national scale,” they commented.“Given the serious consequences of global climate change, analysis of the environmental impact of all fields of medicine, including dermatology, is warranted,” they added.
The reduced greenhouse gas emissions are “definitely [being taken] into consideration for future decisions about virtual visits” in the department of dermatology, said Zachary Zinn, MD, residency director and associate professor in the department of dermatology at West Virginia University, Morgantown, who is the senior author of the study. “The main benefit of virtual care in my opinion,” he said in an interview, “is the potential to reduce our carbon footprint.”
Justin Lee, MD, an intern at WVU and the study’s first author, said that the research team was motivated to think about how they “could reduce the negative environmental impact of practicing dermatology” after they read a paper about the environmental impact of endoscopy, written by a gastroenterologist.
In the study, no pregnancies occurred and monthly tests were performed, but “formal assessment of pregnancy risk with virtual isotretinoin management would be warranted,” Dr. Lee and coauthors wrote, noting too that, while no differences were seen with respect to isotretinoin side effects, these were not formally analyzed.
Dr. Zinn said that he and colleagues at WVUH are currently conducting clinical trials to assess the quality and efficacy of virtual care for patients with acne, atopic dermatitis, and psoriasis. Delivering care virtually “will be easier to do if there are data supporting [its] quality and efficacy,” he said. Rosacea is another condition that may be amendable to virtual care, he noted.
Meanwhile, he said, isotretinoin management is “well suited” for virtual visits. When initiating isotretinoin treatment, Dr. Zinn now “proactively inquires” if patients would like to pursue their follow-up visits virtually. “I’ll note that it will save the time and decrease the burden of travel, including the financial cost as well as the environmental cost of travel,” he said, estimating that about half of their management visits are currently virtual.
Asked about the study, Misha Rosenbach, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said the reduced carbon footprint calculated by the researchers and its downstream health benefits “should be taken into consideration by [dermatology] departments, insurers and policymakers” when making decisions about teledermatology.
While environmental impact is “not something I think most institutions are considering for virtual versus in-person care, they should be. And some are,” said Dr. Rosenbach, a founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues.
Limitations of the study include the generalizability of the results. The impact of virtual isotretinoin management “may be less in predominantly urban areas” than it is in predominately rural West Virginia, the study authors note. And in the case of West Virginia, travel to a local laboratory and pharmacy offsets some of the environmental benefits for the virtual care, they noted. Such travel wasn’t accounted for in the study, but it was found to be a fraction of travel to the WVU hospital clinic. (Patients traveled a median of 5.8 miles to a lab 2.4 times from March 25 to Dec. 1, 2020.)
Dr. Lee will start his dermatology residency at WVU next year. The study was funded by a grant from the U.S. National Science Foundation. The authors have no relevant conflicts of interest, according to Dr. Lee.
FROM PEDIATRIC DERMATOLOGY
Dyspigmentation common in SOC patients with bullous pemphigoid
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
FROM SOC 2021
Political support of permanent DST concerns sleep scientists
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
FROM SLEEP 2021
OSA in women: Different symptoms, risks and consequences
The reported prevalence and severity of obstructive sleep apnea in women is lower, compared with men, but the consequences of the disease are “at least the same, if not worse,” with women appearing to have greater susceptibility to adverse OSA-related cardiovascular consequences – particularly as it pertains to endothelial dysfunction, Reena Mehra, MD, MS, said at the virtual annual meeting of the Associated Professional Sleep Societies.
Women more so than men have endothelial dysfunction associated with OSA, “suggesting there is an enhanced sensitivity of the female vascular endothelium to intermittent hypoxia,” said Dr. Mehra, director of sleep disorders research at the Cleveland Clinic and professor of medicine at Case Western Reserve University, also in Cleveland.
Sex-specific differences in the anatomic and physiological characteristics of the upper airway, in fat distribution and in respiratory stability as they relate to OSA have been documented for some time – and today, these and other differences relating to the diagnosis, treatment, and consequences of sleep apnea continue to be studied and elucidated, said Dr. Mehra, Anita Rajagopal, MD, and Chitra Lal, MD, in a session on OSA in women. Each spoke about the breath and implications of these differences, and of increasing recognition of the significance of OSA in women.
Likely underdiagnosis
Epidemiologic studies have suggested a three- to fivefold higher prevalence of OSA in men than in women in the general population. But it has also been estimated that 17%-25% of women have sleep apnea, and the prevalence reported in various studies has generally increased with time, said Dr. Rajagopal, department medical director for sleep medicine at Community Physician Network in Indianapolis, and medical director of the Community Health Network Sleep/Wake Disorders Center, also in Indianapolis.
One population-based study in Sweden, reported in 2013, found OSA (defined as an apnea-hypopnea index [AHI] ≥5) in 50% of women aged 20-70, she noted.
It’s quite possible women are being misdiagnosed or underdiagnosed because of their reporting of different symptoms, Dr. Rajagopal said. The Epworth Sleepiness Scale, commonly used to screen for OSA, has not been validated for use in women and has not been strongly associated with daytime sleepiness in women in population-based studies, she said, noting that women who report similar levels of daytime sleepiness to men are less likely to have an ESS score greater than 10.
“We shouldn’t rule out obstructive sleep apnea in women with a low ESS,” Dr. Rajagopal said in an interview after the meeting. Attentiveness to the symptoms more often reported by women – generalized daytime fatigue/lack of energy, insomnia, morning headaches, mood disturbances, and nightmares – is important, as is performance of overnight polysomnography when a home sleep study is negative and there is clinical suspicion of OSA.Respiratory disturbances in women are frequently associated with arousals – which induce less ventilatory instability in women than in men – rather than oxygen desaturations, leading to underestimation of OSA on home sleep testing. Insomnia associated with OSA in women may also increase the likelihood of a false negative result, Dr. Rajagopal said at the meeting.
“It’s really important [in sleep testing] to consider your AHI values in women,” she said. “The AHI value may not provide a true indication of the degree of sleep fragmentation being experienced by patients.” That OSA symptoms manifest in women with lower AHIs has been elucidated in research showing, for instance, that those with an AHI of 2-5 per hour have a similar level of symptoms to men with an AHI of at least 15 per hour, she said.
Women tend to have a clustering of apnea during REM sleep, and it’s possible that “the long-term effects of REM disruption contribute to greater symptomatology at lower AHI values in women compared to men,” Dr. Rajagopal said.
Also at play are when it comes to testing and diagnosis are several other key sex differences, she said. For one, the upper airways in women are less collapsible and more stable during sleep (most evident during non-REM sleep), and respiratory events during sleep are less frequently associated with complete upper airway collapse.
Women also have shorter apneic episodes, but “the longest apneas are associated with a more severe oxygen desaturation,” she said. Moreover, they have more episodes of upper airway resistance during sleep, which in and of itself “has been shown to produce clinical symptoms such as daytime fatigue and clinical depression.”
In her presentation, Dr. Mehra similarly commented on a likely underdiagnosis of OSA in women. In addition to differing symptoms, including palpitations, “women are less likely to have arousals, and have a lesser degree of nocturnal hypoxia compared to men ... perhaps leading to even more of an underdiagnosis.”
Unique consequences
Differences in upper airway physiology and other sex-specific differences impacting OSA susceptibility are at least partly attributable to sex hormones, said Dr. Mehra and Dr. Lal, associate professor of medicine at the Medical University of South Carolina, Charleston.
A significant increase in prevalence is seen after menopause, and research has shown that each additional year in menopause is associated with a greater AHI – a “dose-response effect,” Dr. Lal said. An inverse association between hormone replacement therapy and OSA severity has been seen in epidemiological studies including the Sleep Heart Health Study, Dr. Mehra said. But in prospective studies, Dr. Lal noted, hormone replacement therapy has not been shown to decrease AHI.
Experimental and clinical studies suggest that the vascular endothelium is influenced by sex hormones, Dr. Mehra said. Estrogen is known to improve endothelial function by inducing increased nitric oxide bioavailability – important in the setting of hypoxemia, which leads to reduced bioavailability of nitric oxide. “Alterations of sex-specific hormones in OSA may represent a key factor in increasing vulnerability to vascular dysfunction,” Dr. Mehra added.
The Sleep Heart Health Study also documented sex-specific differences, showing a graded increase of troponin with increasing OSA severity category as well as an increase in left ventricular mass thickness, and a 30% increased risk of heart failure or death in women with moderate/severe OSA, compared with women without OSA or with mild OSA, Dr. Mehra said. These findings were not observed in men.
The dominance of REM-related OSA in women raises risk because sleep disturbances during REM sleep are associated with adverse cardiometabolic outcomes including prevalent and incident hypertension, Dr. Mehra noted. “REM-related OSA may also adversely impact glucose metabolism,” she said, “even in the absence of non-REM obstructive sleep apnea.”
Regarding OSA treatment and responsivity, Dr. Mehra said that preliminary, post hoc data from a randomized, controlled trial of the impact of continuous positive airway pressure (CPAP) therapy on cardiovascular biomarkers showed a sex-specific effect. “There were differences in men versus women in terms of responsiveness with regards to biomarkers of inflammation and oxidative stress ... with reductions from CPAP observed in women but not in men,” said Dr. Mehra, a co-investigator of the study.
The data suggests, she said that “these biomarkers may be more responsive to treatment and a reversal of sleep apnea pathophysiology in women.”
Women also appear to respond better than men to upper airway nerve stimulation (UAS), she said, referring to an international registry study showing a 3.6-fold higher odds of responsiveness to the therapy relative to men. Women in the study were 60% less likely to be approved by insurance for UAS, however, making it “a public policy issue, said Dr. Mehra, a coinvestigator.
Dr. Rajagopal, Dr. Mehra, and Dr. Lal all reported that they had no potential conflicts of interest.
The reported prevalence and severity of obstructive sleep apnea in women is lower, compared with men, but the consequences of the disease are “at least the same, if not worse,” with women appearing to have greater susceptibility to adverse OSA-related cardiovascular consequences – particularly as it pertains to endothelial dysfunction, Reena Mehra, MD, MS, said at the virtual annual meeting of the Associated Professional Sleep Societies.
Women more so than men have endothelial dysfunction associated with OSA, “suggesting there is an enhanced sensitivity of the female vascular endothelium to intermittent hypoxia,” said Dr. Mehra, director of sleep disorders research at the Cleveland Clinic and professor of medicine at Case Western Reserve University, also in Cleveland.
Sex-specific differences in the anatomic and physiological characteristics of the upper airway, in fat distribution and in respiratory stability as they relate to OSA have been documented for some time – and today, these and other differences relating to the diagnosis, treatment, and consequences of sleep apnea continue to be studied and elucidated, said Dr. Mehra, Anita Rajagopal, MD, and Chitra Lal, MD, in a session on OSA in women. Each spoke about the breath and implications of these differences, and of increasing recognition of the significance of OSA in women.
Likely underdiagnosis
Epidemiologic studies have suggested a three- to fivefold higher prevalence of OSA in men than in women in the general population. But it has also been estimated that 17%-25% of women have sleep apnea, and the prevalence reported in various studies has generally increased with time, said Dr. Rajagopal, department medical director for sleep medicine at Community Physician Network in Indianapolis, and medical director of the Community Health Network Sleep/Wake Disorders Center, also in Indianapolis.
One population-based study in Sweden, reported in 2013, found OSA (defined as an apnea-hypopnea index [AHI] ≥5) in 50% of women aged 20-70, she noted.
It’s quite possible women are being misdiagnosed or underdiagnosed because of their reporting of different symptoms, Dr. Rajagopal said. The Epworth Sleepiness Scale, commonly used to screen for OSA, has not been validated for use in women and has not been strongly associated with daytime sleepiness in women in population-based studies, she said, noting that women who report similar levels of daytime sleepiness to men are less likely to have an ESS score greater than 10.
“We shouldn’t rule out obstructive sleep apnea in women with a low ESS,” Dr. Rajagopal said in an interview after the meeting. Attentiveness to the symptoms more often reported by women – generalized daytime fatigue/lack of energy, insomnia, morning headaches, mood disturbances, and nightmares – is important, as is performance of overnight polysomnography when a home sleep study is negative and there is clinical suspicion of OSA.Respiratory disturbances in women are frequently associated with arousals – which induce less ventilatory instability in women than in men – rather than oxygen desaturations, leading to underestimation of OSA on home sleep testing. Insomnia associated with OSA in women may also increase the likelihood of a false negative result, Dr. Rajagopal said at the meeting.
“It’s really important [in sleep testing] to consider your AHI values in women,” she said. “The AHI value may not provide a true indication of the degree of sleep fragmentation being experienced by patients.” That OSA symptoms manifest in women with lower AHIs has been elucidated in research showing, for instance, that those with an AHI of 2-5 per hour have a similar level of symptoms to men with an AHI of at least 15 per hour, she said.
Women tend to have a clustering of apnea during REM sleep, and it’s possible that “the long-term effects of REM disruption contribute to greater symptomatology at lower AHI values in women compared to men,” Dr. Rajagopal said.
Also at play are when it comes to testing and diagnosis are several other key sex differences, she said. For one, the upper airways in women are less collapsible and more stable during sleep (most evident during non-REM sleep), and respiratory events during sleep are less frequently associated with complete upper airway collapse.
Women also have shorter apneic episodes, but “the longest apneas are associated with a more severe oxygen desaturation,” she said. Moreover, they have more episodes of upper airway resistance during sleep, which in and of itself “has been shown to produce clinical symptoms such as daytime fatigue and clinical depression.”
In her presentation, Dr. Mehra similarly commented on a likely underdiagnosis of OSA in women. In addition to differing symptoms, including palpitations, “women are less likely to have arousals, and have a lesser degree of nocturnal hypoxia compared to men ... perhaps leading to even more of an underdiagnosis.”
Unique consequences
Differences in upper airway physiology and other sex-specific differences impacting OSA susceptibility are at least partly attributable to sex hormones, said Dr. Mehra and Dr. Lal, associate professor of medicine at the Medical University of South Carolina, Charleston.
A significant increase in prevalence is seen after menopause, and research has shown that each additional year in menopause is associated with a greater AHI – a “dose-response effect,” Dr. Lal said. An inverse association between hormone replacement therapy and OSA severity has been seen in epidemiological studies including the Sleep Heart Health Study, Dr. Mehra said. But in prospective studies, Dr. Lal noted, hormone replacement therapy has not been shown to decrease AHI.
Experimental and clinical studies suggest that the vascular endothelium is influenced by sex hormones, Dr. Mehra said. Estrogen is known to improve endothelial function by inducing increased nitric oxide bioavailability – important in the setting of hypoxemia, which leads to reduced bioavailability of nitric oxide. “Alterations of sex-specific hormones in OSA may represent a key factor in increasing vulnerability to vascular dysfunction,” Dr. Mehra added.
The Sleep Heart Health Study also documented sex-specific differences, showing a graded increase of troponin with increasing OSA severity category as well as an increase in left ventricular mass thickness, and a 30% increased risk of heart failure or death in women with moderate/severe OSA, compared with women without OSA or with mild OSA, Dr. Mehra said. These findings were not observed in men.
The dominance of REM-related OSA in women raises risk because sleep disturbances during REM sleep are associated with adverse cardiometabolic outcomes including prevalent and incident hypertension, Dr. Mehra noted. “REM-related OSA may also adversely impact glucose metabolism,” she said, “even in the absence of non-REM obstructive sleep apnea.”
Regarding OSA treatment and responsivity, Dr. Mehra said that preliminary, post hoc data from a randomized, controlled trial of the impact of continuous positive airway pressure (CPAP) therapy on cardiovascular biomarkers showed a sex-specific effect. “There were differences in men versus women in terms of responsiveness with regards to biomarkers of inflammation and oxidative stress ... with reductions from CPAP observed in women but not in men,” said Dr. Mehra, a co-investigator of the study.
The data suggests, she said that “these biomarkers may be more responsive to treatment and a reversal of sleep apnea pathophysiology in women.”
Women also appear to respond better than men to upper airway nerve stimulation (UAS), she said, referring to an international registry study showing a 3.6-fold higher odds of responsiveness to the therapy relative to men. Women in the study were 60% less likely to be approved by insurance for UAS, however, making it “a public policy issue, said Dr. Mehra, a coinvestigator.
Dr. Rajagopal, Dr. Mehra, and Dr. Lal all reported that they had no potential conflicts of interest.
The reported prevalence and severity of obstructive sleep apnea in women is lower, compared with men, but the consequences of the disease are “at least the same, if not worse,” with women appearing to have greater susceptibility to adverse OSA-related cardiovascular consequences – particularly as it pertains to endothelial dysfunction, Reena Mehra, MD, MS, said at the virtual annual meeting of the Associated Professional Sleep Societies.
Women more so than men have endothelial dysfunction associated with OSA, “suggesting there is an enhanced sensitivity of the female vascular endothelium to intermittent hypoxia,” said Dr. Mehra, director of sleep disorders research at the Cleveland Clinic and professor of medicine at Case Western Reserve University, also in Cleveland.
Sex-specific differences in the anatomic and physiological characteristics of the upper airway, in fat distribution and in respiratory stability as they relate to OSA have been documented for some time – and today, these and other differences relating to the diagnosis, treatment, and consequences of sleep apnea continue to be studied and elucidated, said Dr. Mehra, Anita Rajagopal, MD, and Chitra Lal, MD, in a session on OSA in women. Each spoke about the breath and implications of these differences, and of increasing recognition of the significance of OSA in women.
Likely underdiagnosis
Epidemiologic studies have suggested a three- to fivefold higher prevalence of OSA in men than in women in the general population. But it has also been estimated that 17%-25% of women have sleep apnea, and the prevalence reported in various studies has generally increased with time, said Dr. Rajagopal, department medical director for sleep medicine at Community Physician Network in Indianapolis, and medical director of the Community Health Network Sleep/Wake Disorders Center, also in Indianapolis.
One population-based study in Sweden, reported in 2013, found OSA (defined as an apnea-hypopnea index [AHI] ≥5) in 50% of women aged 20-70, she noted.
It’s quite possible women are being misdiagnosed or underdiagnosed because of their reporting of different symptoms, Dr. Rajagopal said. The Epworth Sleepiness Scale, commonly used to screen for OSA, has not been validated for use in women and has not been strongly associated with daytime sleepiness in women in population-based studies, she said, noting that women who report similar levels of daytime sleepiness to men are less likely to have an ESS score greater than 10.
“We shouldn’t rule out obstructive sleep apnea in women with a low ESS,” Dr. Rajagopal said in an interview after the meeting. Attentiveness to the symptoms more often reported by women – generalized daytime fatigue/lack of energy, insomnia, morning headaches, mood disturbances, and nightmares – is important, as is performance of overnight polysomnography when a home sleep study is negative and there is clinical suspicion of OSA.Respiratory disturbances in women are frequently associated with arousals – which induce less ventilatory instability in women than in men – rather than oxygen desaturations, leading to underestimation of OSA on home sleep testing. Insomnia associated with OSA in women may also increase the likelihood of a false negative result, Dr. Rajagopal said at the meeting.
“It’s really important [in sleep testing] to consider your AHI values in women,” she said. “The AHI value may not provide a true indication of the degree of sleep fragmentation being experienced by patients.” That OSA symptoms manifest in women with lower AHIs has been elucidated in research showing, for instance, that those with an AHI of 2-5 per hour have a similar level of symptoms to men with an AHI of at least 15 per hour, she said.
Women tend to have a clustering of apnea during REM sleep, and it’s possible that “the long-term effects of REM disruption contribute to greater symptomatology at lower AHI values in women compared to men,” Dr. Rajagopal said.
Also at play are when it comes to testing and diagnosis are several other key sex differences, she said. For one, the upper airways in women are less collapsible and more stable during sleep (most evident during non-REM sleep), and respiratory events during sleep are less frequently associated with complete upper airway collapse.
Women also have shorter apneic episodes, but “the longest apneas are associated with a more severe oxygen desaturation,” she said. Moreover, they have more episodes of upper airway resistance during sleep, which in and of itself “has been shown to produce clinical symptoms such as daytime fatigue and clinical depression.”
In her presentation, Dr. Mehra similarly commented on a likely underdiagnosis of OSA in women. In addition to differing symptoms, including palpitations, “women are less likely to have arousals, and have a lesser degree of nocturnal hypoxia compared to men ... perhaps leading to even more of an underdiagnosis.”
Unique consequences
Differences in upper airway physiology and other sex-specific differences impacting OSA susceptibility are at least partly attributable to sex hormones, said Dr. Mehra and Dr. Lal, associate professor of medicine at the Medical University of South Carolina, Charleston.
A significant increase in prevalence is seen after menopause, and research has shown that each additional year in menopause is associated with a greater AHI – a “dose-response effect,” Dr. Lal said. An inverse association between hormone replacement therapy and OSA severity has been seen in epidemiological studies including the Sleep Heart Health Study, Dr. Mehra said. But in prospective studies, Dr. Lal noted, hormone replacement therapy has not been shown to decrease AHI.
Experimental and clinical studies suggest that the vascular endothelium is influenced by sex hormones, Dr. Mehra said. Estrogen is known to improve endothelial function by inducing increased nitric oxide bioavailability – important in the setting of hypoxemia, which leads to reduced bioavailability of nitric oxide. “Alterations of sex-specific hormones in OSA may represent a key factor in increasing vulnerability to vascular dysfunction,” Dr. Mehra added.
The Sleep Heart Health Study also documented sex-specific differences, showing a graded increase of troponin with increasing OSA severity category as well as an increase in left ventricular mass thickness, and a 30% increased risk of heart failure or death in women with moderate/severe OSA, compared with women without OSA or with mild OSA, Dr. Mehra said. These findings were not observed in men.
The dominance of REM-related OSA in women raises risk because sleep disturbances during REM sleep are associated with adverse cardiometabolic outcomes including prevalent and incident hypertension, Dr. Mehra noted. “REM-related OSA may also adversely impact glucose metabolism,” she said, “even in the absence of non-REM obstructive sleep apnea.”
Regarding OSA treatment and responsivity, Dr. Mehra said that preliminary, post hoc data from a randomized, controlled trial of the impact of continuous positive airway pressure (CPAP) therapy on cardiovascular biomarkers showed a sex-specific effect. “There were differences in men versus women in terms of responsiveness with regards to biomarkers of inflammation and oxidative stress ... with reductions from CPAP observed in women but not in men,” said Dr. Mehra, a co-investigator of the study.
The data suggests, she said that “these biomarkers may be more responsive to treatment and a reversal of sleep apnea pathophysiology in women.”
Women also appear to respond better than men to upper airway nerve stimulation (UAS), she said, referring to an international registry study showing a 3.6-fold higher odds of responsiveness to the therapy relative to men. Women in the study were 60% less likely to be approved by insurance for UAS, however, making it “a public policy issue, said Dr. Mehra, a coinvestigator.
Dr. Rajagopal, Dr. Mehra, and Dr. Lal all reported that they had no potential conflicts of interest.
FROM SLEEP 2021