User login
ED care pathway hastens febrile neutropenia therapy
Cancer patients who arrive in the emergency department with febrile neutropenia (FN) received antibiotics much more quickly when their condition was identified as a medical emergency and a care pathway was used to guide treatment. The set of simple interventions slashed average time to antibiotics from about 4 hours to less than 1.5 hours, compared with a historical cohort, and the inexpensive interventions have had durable results.
Dr. Michael Keng and his coinvestigators at the Cleveland Clinic reported the results of a single-center prospective analysis that targeted FN, a common and serious chemotherapy complication with a mortality rate that can exceed 50% in medically fragile individuals [doi:10.1200/JOP.2014.002733].
“With an increasing number of outpatient chemotherapy regimens, more patients are likely to present to the emergency department (ED) with FN,” wrote Dr. Keng. The FN pathway devised by Dr. Keng and his associates implemented key changes designed to identify FN as an emergency and guide prompt triage, assessment, and treatment.
Study coauthor Dr. Mikkael Sekeres said, “The interventions were not complicated. We standardized our definition of fever; provided patients with wallet-sized cards alerting emergency departments to the potential of this serious condition; worked with our emergency department staff to change the triage level of fever and neutropenia to be equivalent to that observed for heart attack or stroke; designed standard febrile neutropenia order sets for our electronic medical record; and relocated the antibiotics used to treat febrile neutropenia to our emergency department.”
Febrile patients with cancer in the prospective cohort (n = 223) were compared with a historical cohort of patients presenting to the ED who received usual care (n = 87), as well as to a concurrent cohort of patients who were directly admitted to the hospital (n = 114). The total number of FN episodes for the cohorts was 276, 107, and 114, respectively. Multivariable analysis was used to account for some differences in patient characteristics across cohorts.
Time to antibiotics for the pathway was a median 81 minutes, compared with 225 minutes for the historical cohort and 169 minutes for the direct-admission cohort (P less than .001 for both). Only two patients in the combined comparison cohorts received antibiotics within 60 minutes, while almost one-third of the prospective cohort receiving the protocol was treated within 60 minutes.
Using the order set in the EHR also made a difference: for those treated per the order set (n = 103), median time to antibiotics was 68 minutes, compared with 96 minutes when the order set was not used.
Secondary outcome measures included times to physician assessment, blood draw, and antibiotic order placement. All measures except time to physician assessment were significantly shorter for the FN pathway group than for the comparison cohorts (P less than .001 for all).
Since so many changes were made at once, Dr. Keng and his coauthors noted, “it is difficult to determine the impact of any one change.” Some institutions may have difficulty implementing all the interventions, but immediate triage, automated antibiotic ordering, and EHR use were the changes that had the most impact, he wrote.
“Instituting these changes took less than half a year, and the benefits have persisted for years afterward,” Dr. Sekeres said in an interview.
No study authors reported conflicts of interest.
Cancer patients who arrive in the emergency department with febrile neutropenia (FN) received antibiotics much more quickly when their condition was identified as a medical emergency and a care pathway was used to guide treatment. The set of simple interventions slashed average time to antibiotics from about 4 hours to less than 1.5 hours, compared with a historical cohort, and the inexpensive interventions have had durable results.
Dr. Michael Keng and his coinvestigators at the Cleveland Clinic reported the results of a single-center prospective analysis that targeted FN, a common and serious chemotherapy complication with a mortality rate that can exceed 50% in medically fragile individuals [doi:10.1200/JOP.2014.002733].
“With an increasing number of outpatient chemotherapy regimens, more patients are likely to present to the emergency department (ED) with FN,” wrote Dr. Keng. The FN pathway devised by Dr. Keng and his associates implemented key changes designed to identify FN as an emergency and guide prompt triage, assessment, and treatment.
Study coauthor Dr. Mikkael Sekeres said, “The interventions were not complicated. We standardized our definition of fever; provided patients with wallet-sized cards alerting emergency departments to the potential of this serious condition; worked with our emergency department staff to change the triage level of fever and neutropenia to be equivalent to that observed for heart attack or stroke; designed standard febrile neutropenia order sets for our electronic medical record; and relocated the antibiotics used to treat febrile neutropenia to our emergency department.”
Febrile patients with cancer in the prospective cohort (n = 223) were compared with a historical cohort of patients presenting to the ED who received usual care (n = 87), as well as to a concurrent cohort of patients who were directly admitted to the hospital (n = 114). The total number of FN episodes for the cohorts was 276, 107, and 114, respectively. Multivariable analysis was used to account for some differences in patient characteristics across cohorts.
Time to antibiotics for the pathway was a median 81 minutes, compared with 225 minutes for the historical cohort and 169 minutes for the direct-admission cohort (P less than .001 for both). Only two patients in the combined comparison cohorts received antibiotics within 60 minutes, while almost one-third of the prospective cohort receiving the protocol was treated within 60 minutes.
Using the order set in the EHR also made a difference: for those treated per the order set (n = 103), median time to antibiotics was 68 minutes, compared with 96 minutes when the order set was not used.
Secondary outcome measures included times to physician assessment, blood draw, and antibiotic order placement. All measures except time to physician assessment were significantly shorter for the FN pathway group than for the comparison cohorts (P less than .001 for all).
Since so many changes were made at once, Dr. Keng and his coauthors noted, “it is difficult to determine the impact of any one change.” Some institutions may have difficulty implementing all the interventions, but immediate triage, automated antibiotic ordering, and EHR use were the changes that had the most impact, he wrote.
“Instituting these changes took less than half a year, and the benefits have persisted for years afterward,” Dr. Sekeres said in an interview.
No study authors reported conflicts of interest.
Cancer patients who arrive in the emergency department with febrile neutropenia (FN) received antibiotics much more quickly when their condition was identified as a medical emergency and a care pathway was used to guide treatment. The set of simple interventions slashed average time to antibiotics from about 4 hours to less than 1.5 hours, compared with a historical cohort, and the inexpensive interventions have had durable results.
Dr. Michael Keng and his coinvestigators at the Cleveland Clinic reported the results of a single-center prospective analysis that targeted FN, a common and serious chemotherapy complication with a mortality rate that can exceed 50% in medically fragile individuals [doi:10.1200/JOP.2014.002733].
“With an increasing number of outpatient chemotherapy regimens, more patients are likely to present to the emergency department (ED) with FN,” wrote Dr. Keng. The FN pathway devised by Dr. Keng and his associates implemented key changes designed to identify FN as an emergency and guide prompt triage, assessment, and treatment.
Study coauthor Dr. Mikkael Sekeres said, “The interventions were not complicated. We standardized our definition of fever; provided patients with wallet-sized cards alerting emergency departments to the potential of this serious condition; worked with our emergency department staff to change the triage level of fever and neutropenia to be equivalent to that observed for heart attack or stroke; designed standard febrile neutropenia order sets for our electronic medical record; and relocated the antibiotics used to treat febrile neutropenia to our emergency department.”
Febrile patients with cancer in the prospective cohort (n = 223) were compared with a historical cohort of patients presenting to the ED who received usual care (n = 87), as well as to a concurrent cohort of patients who were directly admitted to the hospital (n = 114). The total number of FN episodes for the cohorts was 276, 107, and 114, respectively. Multivariable analysis was used to account for some differences in patient characteristics across cohorts.
Time to antibiotics for the pathway was a median 81 minutes, compared with 225 minutes for the historical cohort and 169 minutes for the direct-admission cohort (P less than .001 for both). Only two patients in the combined comparison cohorts received antibiotics within 60 minutes, while almost one-third of the prospective cohort receiving the protocol was treated within 60 minutes.
Using the order set in the EHR also made a difference: for those treated per the order set (n = 103), median time to antibiotics was 68 minutes, compared with 96 minutes when the order set was not used.
Secondary outcome measures included times to physician assessment, blood draw, and antibiotic order placement. All measures except time to physician assessment were significantly shorter for the FN pathway group than for the comparison cohorts (P less than .001 for all).
Since so many changes were made at once, Dr. Keng and his coauthors noted, “it is difficult to determine the impact of any one change.” Some institutions may have difficulty implementing all the interventions, but immediate triage, automated antibiotic ordering, and EHR use were the changes that had the most impact, he wrote.
“Instituting these changes took less than half a year, and the benefits have persisted for years afterward,” Dr. Sekeres said in an interview.
No study authors reported conflicts of interest.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Key clinical point: Instituting a care pathway hastened antibiotic administration in cancer patients with fever in the emergency department.
Major finding: Cancer patients treated according to a febrile neutropenia care pathway in the emergency department received antibiotics in 81 minutes, significantly sooner than did historical and direct admission comparison cohorts at 235 and 169 minutes, respectively (P less than .001 for both differences).
Data source: Prospective study of 276 FN episodes in 223 patients, compared with 107 episodes in 87 historical patients and 114 episodes in 101 direct admission cohort patients.
Disclosures: The authors reported no relevant financial disclosures.
Quit smoking for less chest pain, better mental health after MI
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
FROM CIRCULATION CARDIOVASCULAR QUALITY OUTCOMES
Key clinical point: Patients who quit smoking after acute myocardial infarction had better health-related quality of life and less chest pain than those who continued smoking.
Major finding: One year after acute MI, those who stopped smoking had similar mental health scores and angina levels to never-smokers.
Data source: 4,003 patients in two U.S., multicenter, prospective AMI registries who were assessed for smoking status, HRQOL, and angina at 1, 6, and 12 months post MI.
Disclosures: The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
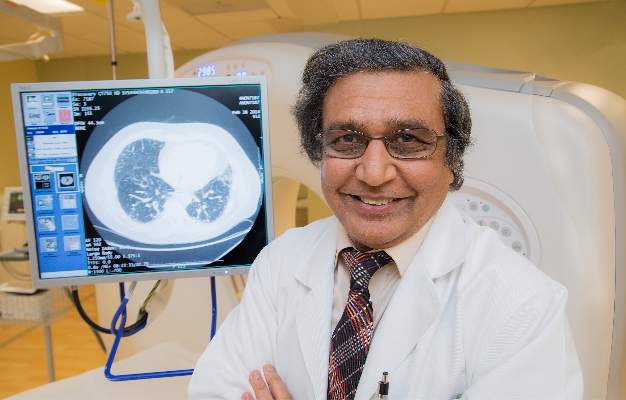
New IPF guidelines limit treatment choices
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Picato Adverse Events Prompt FDA Warning
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
FROM AN FDA MEDWATCH ALERT
Picato adverse events prompt FDA warning
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
On Twitter @karioakes
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
On Twitter @karioakes
The Food and Drug Administration has issued a Drug Safety Communication warning for the potential for severe allergic reactions, shingles, and severe eye injuries from incorrect application of Picato (ingenol mebutate), a topical gel used to treat actinic keratosis.
Picato’s manufacurer, Leo Pharma Inc., will be required to change the drug’s labeling to reflect the risk for these adverse events and provide more information about safe application of Picato gel.
In the data summary accompanying the announcement, the FDA noted that some of the incorrect use of Picato gel was related either to inaccurate prescribing or dispensing. Adverse events reported were associated with incorrect application of Picato gel, which is to be used on no more than 25 cm2 of skin at a time, and for no more than 3 consecutive days.
Some of the adverse events reports describe mixing Picato with other products, occluding the skin after applying Picato gel, washing it off before the recommended 6 hours, or applying at bedtime.
Additionally, some adverse events occurred when the stronger 0.05% formulation, intended for use on the extremities and trunk, was applied to the face. Facial actinic keratoses are to be treated with the 0.015% formulation.
Adverse events described included severe allergic reactions ranging from significant contact dermatitis to anaphylaxis. Reactivation of herpes zoster was also reported; some of these cases were associated with applying Picato gel to a larger-than-recommended area, or with using an incorrect dose strength.
Another class of adverse events involved accidental transfer of Picato gel, often to the eyes. This occurred even after handwashing. In addition to eyelid swelling and irritation, cases of chemical conjunctivitis and corneal ulceration were reported. Lips, tongue, and rectum were other areas affected by accidental transfer of Picato gel.
On Twitter @karioakes
FROM AN FDA MEDWATCH ALERT
FDA approves flibanserin for low female sexual desire
The Food and Drug Administration has approved flibanserin as the first drug treatment for acquired, generalized hypoactive sexual desire disorder in premenopausal women. The drug – marketed as Addyi – is expected to be available by Oct. 17.
Conditions of the drug’s third – and successful – bid for approval, however, include a risk evaluation and mitigation strategy (REMS), post-marketing research, and a boxed warning to highlight the risk of severe hypotension and syncope for some patients.
The decision adheres to the recommendations of two FDA advisory panels – the Bone, Reproductive and Urologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee – which met jointly on June 4 and voted 18-6 for approval of the non-hormonal, centrally-acting drug. The panels advised that additional measures beyond labeling language be put in place to address concerns about serious adverse events associated with flibanserin. Unpredictable episodes of syncope have been reported, and significant interactions with alcohol can worsen the hypotension and syncope flibanserin can cause.
Flibanserin is a mixed agonist/antagonist for serotonin and dopamine receptors. It is meant to be taken orally at bedtime on a chronic basis; the dose is 100mg. Previous applications for approval in 2009 by then-manufacturer Boehringer Ingelheim, and in 2013 by current manufacturer Sprout Pharmaceuticals, were denied.
The REMS requires that prescribers of flibanserin complete training about the risks of severe hypotension and syncope when the drug is taken with alcohol, and that a patient-provider agreement form about these risks be signed. Pharmacies must also certify with the REMS program.
The black box warning will state that the use of alcohol is contraindicated when taking flibanserin, that it should not be taken with moderate or strong CYP3A4 inhibitors, and that it is contraindicated for those with liver impairment. The FDA is also requiring more study of flibanserin and alcohol in women.
In a series of three phase III clinical trials in North America, premenopausal women who met the DSM-IV diagnostic criteria for hypoactive sexual desire disorder (HSDD) and who were in a stable monogamous relationship took flibanserin or placebo. Of the more than 1,200 women in each study arm, those taking flibanserin had a statistically significant improvement in the number of satisfying sexual events (SSEs) per month, and also showed a significant increase in sexual desire, though overall effect sizes were modest. Women on placebo experienced an increase of 1.5 SSEs per month, compared to 2.5 SSEs per month in those taking flibanserin.
The primary endpoint for sexual desire in the first two studies was a response on an electronic diary reporting the highest level of desire over the last 24 hours. For the final study, the primary desire endpoint was the desire domain of the Female Sexual Function Index, which asked respondents to reflect on their desire over the previous 28 days. In the third clinical trial, women taking flibanserin showed a significantly greater increase in desire than those taking placebo.
Side effects and adverse events associated with flibanserin included drowsiness, hypotension, and syncope. Since the drug is metabolized through the CYP3A4 system, potential for drug-drug and drug-alcohol interaction exists.
Dr. Walid Gellad, co-director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh, was on the FDA panel that voted in favor of flibanserin’s approval. In an interview, he explained that he attempted to balance the need for the medication against both the very real safety concerns and the relatively modest effect size.
As flibanserin hits the market, he said, “there is no doubt that the adverse events are going to be worse in real life than we saw in the trials.” Off-label use and drinking while taking the drug in spite of warnings are the likely contributors, he said.
On the other hand, “biology is important,” said Deborah Arrindell, vice president for health policy for the American Sexual Health Association, a supporter of Even the Score, a coalition of groups that includes Sprout Pharmaceuticals and that has pushed for approval of the drug. Having a medical treatment for women with HSDD, she said, represents real progress.
“We recognize that medical and biological factors are at play in human sexuality,” she said.
Women who have concerns about their level of sexual desire will be able to work with their providers to determine if flibanserin is a medication that could help them. Approval of flibanserin, Ms. Arrindell said, signals further acknowledgement that “women have a right to sexual pleasure, and that sexual health is part of one’s overall health and well-being.”
Dr. Lisa Larkin, scientific co-chair of Even the Score, and director of the UC Women’s Center in Cincinnati, applauded the FDA’s decision, saying that she hopes the approval will open the pipeline to research and development for more medications for women’s sexual health. Dr. Larkin, an internist with a special interest in women’s health, does not receive compensation for her position with Even the Score.
“This is a landmark day,” she said, even with the physician education and post-marketing requirements imposed by the FDA. “The patients I see are very distressed. These are real women suffering from a real medical condition.”
But Leonore Tiefer, Ph.D., clinical associate professor of psychiatry at New York University, expressed her disappointment in what she characterized as the FDA’s failure to adhere to its core mission. The FDA, she said, has become “too porous to external influences. To yield to pressure from industry was a mistake.”
She explained that as a sexologist, she has many non-pharmacologic treatments in her toolkit to help women with low sexual desire.
“I don’t think this is going to help women,” Dr. Tiefer said.
On Twitter @karioakes
The Food and Drug Administration has approved flibanserin as the first drug treatment for acquired, generalized hypoactive sexual desire disorder in premenopausal women. The drug – marketed as Addyi – is expected to be available by Oct. 17.
Conditions of the drug’s third – and successful – bid for approval, however, include a risk evaluation and mitigation strategy (REMS), post-marketing research, and a boxed warning to highlight the risk of severe hypotension and syncope for some patients.
The decision adheres to the recommendations of two FDA advisory panels – the Bone, Reproductive and Urologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee – which met jointly on June 4 and voted 18-6 for approval of the non-hormonal, centrally-acting drug. The panels advised that additional measures beyond labeling language be put in place to address concerns about serious adverse events associated with flibanserin. Unpredictable episodes of syncope have been reported, and significant interactions with alcohol can worsen the hypotension and syncope flibanserin can cause.
Flibanserin is a mixed agonist/antagonist for serotonin and dopamine receptors. It is meant to be taken orally at bedtime on a chronic basis; the dose is 100mg. Previous applications for approval in 2009 by then-manufacturer Boehringer Ingelheim, and in 2013 by current manufacturer Sprout Pharmaceuticals, were denied.
The REMS requires that prescribers of flibanserin complete training about the risks of severe hypotension and syncope when the drug is taken with alcohol, and that a patient-provider agreement form about these risks be signed. Pharmacies must also certify with the REMS program.
The black box warning will state that the use of alcohol is contraindicated when taking flibanserin, that it should not be taken with moderate or strong CYP3A4 inhibitors, and that it is contraindicated for those with liver impairment. The FDA is also requiring more study of flibanserin and alcohol in women.
In a series of three phase III clinical trials in North America, premenopausal women who met the DSM-IV diagnostic criteria for hypoactive sexual desire disorder (HSDD) and who were in a stable monogamous relationship took flibanserin or placebo. Of the more than 1,200 women in each study arm, those taking flibanserin had a statistically significant improvement in the number of satisfying sexual events (SSEs) per month, and also showed a significant increase in sexual desire, though overall effect sizes were modest. Women on placebo experienced an increase of 1.5 SSEs per month, compared to 2.5 SSEs per month in those taking flibanserin.
The primary endpoint for sexual desire in the first two studies was a response on an electronic diary reporting the highest level of desire over the last 24 hours. For the final study, the primary desire endpoint was the desire domain of the Female Sexual Function Index, which asked respondents to reflect on their desire over the previous 28 days. In the third clinical trial, women taking flibanserin showed a significantly greater increase in desire than those taking placebo.
Side effects and adverse events associated with flibanserin included drowsiness, hypotension, and syncope. Since the drug is metabolized through the CYP3A4 system, potential for drug-drug and drug-alcohol interaction exists.
Dr. Walid Gellad, co-director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh, was on the FDA panel that voted in favor of flibanserin’s approval. In an interview, he explained that he attempted to balance the need for the medication against both the very real safety concerns and the relatively modest effect size.
As flibanserin hits the market, he said, “there is no doubt that the adverse events are going to be worse in real life than we saw in the trials.” Off-label use and drinking while taking the drug in spite of warnings are the likely contributors, he said.
On the other hand, “biology is important,” said Deborah Arrindell, vice president for health policy for the American Sexual Health Association, a supporter of Even the Score, a coalition of groups that includes Sprout Pharmaceuticals and that has pushed for approval of the drug. Having a medical treatment for women with HSDD, she said, represents real progress.
“We recognize that medical and biological factors are at play in human sexuality,” she said.
Women who have concerns about their level of sexual desire will be able to work with their providers to determine if flibanserin is a medication that could help them. Approval of flibanserin, Ms. Arrindell said, signals further acknowledgement that “women have a right to sexual pleasure, and that sexual health is part of one’s overall health and well-being.”
Dr. Lisa Larkin, scientific co-chair of Even the Score, and director of the UC Women’s Center in Cincinnati, applauded the FDA’s decision, saying that she hopes the approval will open the pipeline to research and development for more medications for women’s sexual health. Dr. Larkin, an internist with a special interest in women’s health, does not receive compensation for her position with Even the Score.
“This is a landmark day,” she said, even with the physician education and post-marketing requirements imposed by the FDA. “The patients I see are very distressed. These are real women suffering from a real medical condition.”
But Leonore Tiefer, Ph.D., clinical associate professor of psychiatry at New York University, expressed her disappointment in what she characterized as the FDA’s failure to adhere to its core mission. The FDA, she said, has become “too porous to external influences. To yield to pressure from industry was a mistake.”
She explained that as a sexologist, she has many non-pharmacologic treatments in her toolkit to help women with low sexual desire.
“I don’t think this is going to help women,” Dr. Tiefer said.
On Twitter @karioakes
The Food and Drug Administration has approved flibanserin as the first drug treatment for acquired, generalized hypoactive sexual desire disorder in premenopausal women. The drug – marketed as Addyi – is expected to be available by Oct. 17.
Conditions of the drug’s third – and successful – bid for approval, however, include a risk evaluation and mitigation strategy (REMS), post-marketing research, and a boxed warning to highlight the risk of severe hypotension and syncope for some patients.
The decision adheres to the recommendations of two FDA advisory panels – the Bone, Reproductive and Urologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee – which met jointly on June 4 and voted 18-6 for approval of the non-hormonal, centrally-acting drug. The panels advised that additional measures beyond labeling language be put in place to address concerns about serious adverse events associated with flibanserin. Unpredictable episodes of syncope have been reported, and significant interactions with alcohol can worsen the hypotension and syncope flibanserin can cause.
Flibanserin is a mixed agonist/antagonist for serotonin and dopamine receptors. It is meant to be taken orally at bedtime on a chronic basis; the dose is 100mg. Previous applications for approval in 2009 by then-manufacturer Boehringer Ingelheim, and in 2013 by current manufacturer Sprout Pharmaceuticals, were denied.
The REMS requires that prescribers of flibanserin complete training about the risks of severe hypotension and syncope when the drug is taken with alcohol, and that a patient-provider agreement form about these risks be signed. Pharmacies must also certify with the REMS program.
The black box warning will state that the use of alcohol is contraindicated when taking flibanserin, that it should not be taken with moderate or strong CYP3A4 inhibitors, and that it is contraindicated for those with liver impairment. The FDA is also requiring more study of flibanserin and alcohol in women.
In a series of three phase III clinical trials in North America, premenopausal women who met the DSM-IV diagnostic criteria for hypoactive sexual desire disorder (HSDD) and who were in a stable monogamous relationship took flibanserin or placebo. Of the more than 1,200 women in each study arm, those taking flibanserin had a statistically significant improvement in the number of satisfying sexual events (SSEs) per month, and also showed a significant increase in sexual desire, though overall effect sizes were modest. Women on placebo experienced an increase of 1.5 SSEs per month, compared to 2.5 SSEs per month in those taking flibanserin.
The primary endpoint for sexual desire in the first two studies was a response on an electronic diary reporting the highest level of desire over the last 24 hours. For the final study, the primary desire endpoint was the desire domain of the Female Sexual Function Index, which asked respondents to reflect on their desire over the previous 28 days. In the third clinical trial, women taking flibanserin showed a significantly greater increase in desire than those taking placebo.
Side effects and adverse events associated with flibanserin included drowsiness, hypotension, and syncope. Since the drug is metabolized through the CYP3A4 system, potential for drug-drug and drug-alcohol interaction exists.
Dr. Walid Gellad, co-director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh, was on the FDA panel that voted in favor of flibanserin’s approval. In an interview, he explained that he attempted to balance the need for the medication against both the very real safety concerns and the relatively modest effect size.
As flibanserin hits the market, he said, “there is no doubt that the adverse events are going to be worse in real life than we saw in the trials.” Off-label use and drinking while taking the drug in spite of warnings are the likely contributors, he said.
On the other hand, “biology is important,” said Deborah Arrindell, vice president for health policy for the American Sexual Health Association, a supporter of Even the Score, a coalition of groups that includes Sprout Pharmaceuticals and that has pushed for approval of the drug. Having a medical treatment for women with HSDD, she said, represents real progress.
“We recognize that medical and biological factors are at play in human sexuality,” she said.
Women who have concerns about their level of sexual desire will be able to work with their providers to determine if flibanserin is a medication that could help them. Approval of flibanserin, Ms. Arrindell said, signals further acknowledgement that “women have a right to sexual pleasure, and that sexual health is part of one’s overall health and well-being.”
Dr. Lisa Larkin, scientific co-chair of Even the Score, and director of the UC Women’s Center in Cincinnati, applauded the FDA’s decision, saying that she hopes the approval will open the pipeline to research and development for more medications for women’s sexual health. Dr. Larkin, an internist with a special interest in women’s health, does not receive compensation for her position with Even the Score.
“This is a landmark day,” she said, even with the physician education and post-marketing requirements imposed by the FDA. “The patients I see are very distressed. These are real women suffering from a real medical condition.”
But Leonore Tiefer, Ph.D., clinical associate professor of psychiatry at New York University, expressed her disappointment in what she characterized as the FDA’s failure to adhere to its core mission. The FDA, she said, has become “too porous to external influences. To yield to pressure from industry was a mistake.”
She explained that as a sexologist, she has many non-pharmacologic treatments in her toolkit to help women with low sexual desire.
“I don’t think this is going to help women,” Dr. Tiefer said.
On Twitter @karioakes
FIRE-3: Drug sequence plays role in mCRC outcomes
The sequence of antibody agents may affect overall survival for individuals with metastatic colorectal cancer (mCRC) according to new analysis of data from a large clinical trial comparing two antibody therapies used in conjunction with a standard systemic regime.
Tumor biology may be modified when antibody therapies are used, affecting the tumor’s susceptibility to later therapies, said Dr. Dominik Modest of the University Hospital Grosshadern (Munich), and his coauthors.
Individuals with mCRC were studied in the FIRE-3 trial, an open-label, randomized phase III clinical trial of cetuximab or bevacizumab in combination with FOLFIRI (fluorouracil plus folinic acid in combination with irinotecan) for patients with metastatic colorectal cancer (n = 592, KRAS exon 2 wild-type and n = 400, RAS wild-type). First-line use of cetuximab, an anti–epidermal growth factor receptor (anti-EGFR) agent, was compared head-to-head with first-line use of bevacizumab, an anti–vascular endothelial growth factor (anti-VEGF) agent.
For this population with advanced disease, the study protocol permitted use of an extensive array of second-, third-, and later-line therapies, as well as tumor-directed surgery and radiation therapy. Thus, a subset of FIRE-3 patients in each arm received first one antibody therapy, then the other, allowing investigators to explore the effect of agent sequence.
Though the analysis was predetermined, investigators were interested in explaining an earlier finding from FIRE-3: The cetuximab arm patients had significantly prolonged overall survival (OS) compared with the bevacizumab arm, despite no significant difference in progression-free survival (PFS) or response rate between the treatment arms in either the KRAS exon 2 wild-type intention-to-treat population, or the RAS wild-type group.
On analysis, patients who crossed over to receive oxaliplatin-based chemotherapy plus cetuximab or panitumumab after initial bevacizumab (n = 38) were compared with those who received oxaliplatin-based chemotherapy in combination with bevacizumab after initial cetuximab (n = 67). PFS after second-line therapy was slightly longer for patients who received initial cetuximab (6.3 vs. 5.7 months for KRAS exon 2 wild-type group and 7.3 vs. 5.8 months for RAS wild-type group), though the differences were not statistically significant.
However, overall survival after second-line therapy was significantly longer for the intention-to-treat population when cetuximab was the initial treatment (16.3 months vs. 13.2 months, P = .0021), as was PFS after second line therapy (6.5 vs. 4.7 months, P less than 0.001).
“Taken together, it seems that the sequential application of anti-EGFR agents followed by second-line anti-VEGF therapy achieves more favorable results than the reverse sequence,” said Dr. Modest and his associates. Particularly for patients witth RAS wild-type tumors, “first-line application of anti EGFR–directed therapy may therefore represent an optimal condition for effective subsequent therapy including antiangiogenic agents,” they said.
Dr. Modest and his coauthors cautioned that although poststudy treatment analysis was predefined for FIRE-3, their findings are observational and should not replace prospectively randomized trials designed to compare cancer therapy sequences.
The study was sponsored by Merck KGaA. The study authors report multiple financial disclosures for various pharmaceutical companies.
On Twitter @karioakes
The sequence of antibody agents may affect overall survival for individuals with metastatic colorectal cancer (mCRC) according to new analysis of data from a large clinical trial comparing two antibody therapies used in conjunction with a standard systemic regime.
Tumor biology may be modified when antibody therapies are used, affecting the tumor’s susceptibility to later therapies, said Dr. Dominik Modest of the University Hospital Grosshadern (Munich), and his coauthors.
Individuals with mCRC were studied in the FIRE-3 trial, an open-label, randomized phase III clinical trial of cetuximab or bevacizumab in combination with FOLFIRI (fluorouracil plus folinic acid in combination with irinotecan) for patients with metastatic colorectal cancer (n = 592, KRAS exon 2 wild-type and n = 400, RAS wild-type). First-line use of cetuximab, an anti–epidermal growth factor receptor (anti-EGFR) agent, was compared head-to-head with first-line use of bevacizumab, an anti–vascular endothelial growth factor (anti-VEGF) agent.
For this population with advanced disease, the study protocol permitted use of an extensive array of second-, third-, and later-line therapies, as well as tumor-directed surgery and radiation therapy. Thus, a subset of FIRE-3 patients in each arm received first one antibody therapy, then the other, allowing investigators to explore the effect of agent sequence.
Though the analysis was predetermined, investigators were interested in explaining an earlier finding from FIRE-3: The cetuximab arm patients had significantly prolonged overall survival (OS) compared with the bevacizumab arm, despite no significant difference in progression-free survival (PFS) or response rate between the treatment arms in either the KRAS exon 2 wild-type intention-to-treat population, or the RAS wild-type group.
On analysis, patients who crossed over to receive oxaliplatin-based chemotherapy plus cetuximab or panitumumab after initial bevacizumab (n = 38) were compared with those who received oxaliplatin-based chemotherapy in combination with bevacizumab after initial cetuximab (n = 67). PFS after second-line therapy was slightly longer for patients who received initial cetuximab (6.3 vs. 5.7 months for KRAS exon 2 wild-type group and 7.3 vs. 5.8 months for RAS wild-type group), though the differences were not statistically significant.
However, overall survival after second-line therapy was significantly longer for the intention-to-treat population when cetuximab was the initial treatment (16.3 months vs. 13.2 months, P = .0021), as was PFS after second line therapy (6.5 vs. 4.7 months, P less than 0.001).
“Taken together, it seems that the sequential application of anti-EGFR agents followed by second-line anti-VEGF therapy achieves more favorable results than the reverse sequence,” said Dr. Modest and his associates. Particularly for patients witth RAS wild-type tumors, “first-line application of anti EGFR–directed therapy may therefore represent an optimal condition for effective subsequent therapy including antiangiogenic agents,” they said.
Dr. Modest and his coauthors cautioned that although poststudy treatment analysis was predefined for FIRE-3, their findings are observational and should not replace prospectively randomized trials designed to compare cancer therapy sequences.
The study was sponsored by Merck KGaA. The study authors report multiple financial disclosures for various pharmaceutical companies.
On Twitter @karioakes
The sequence of antibody agents may affect overall survival for individuals with metastatic colorectal cancer (mCRC) according to new analysis of data from a large clinical trial comparing two antibody therapies used in conjunction with a standard systemic regime.
Tumor biology may be modified when antibody therapies are used, affecting the tumor’s susceptibility to later therapies, said Dr. Dominik Modest of the University Hospital Grosshadern (Munich), and his coauthors.
Individuals with mCRC were studied in the FIRE-3 trial, an open-label, randomized phase III clinical trial of cetuximab or bevacizumab in combination with FOLFIRI (fluorouracil plus folinic acid in combination with irinotecan) for patients with metastatic colorectal cancer (n = 592, KRAS exon 2 wild-type and n = 400, RAS wild-type). First-line use of cetuximab, an anti–epidermal growth factor receptor (anti-EGFR) agent, was compared head-to-head with first-line use of bevacizumab, an anti–vascular endothelial growth factor (anti-VEGF) agent.
For this population with advanced disease, the study protocol permitted use of an extensive array of second-, third-, and later-line therapies, as well as tumor-directed surgery and radiation therapy. Thus, a subset of FIRE-3 patients in each arm received first one antibody therapy, then the other, allowing investigators to explore the effect of agent sequence.
Though the analysis was predetermined, investigators were interested in explaining an earlier finding from FIRE-3: The cetuximab arm patients had significantly prolonged overall survival (OS) compared with the bevacizumab arm, despite no significant difference in progression-free survival (PFS) or response rate between the treatment arms in either the KRAS exon 2 wild-type intention-to-treat population, or the RAS wild-type group.
On analysis, patients who crossed over to receive oxaliplatin-based chemotherapy plus cetuximab or panitumumab after initial bevacizumab (n = 38) were compared with those who received oxaliplatin-based chemotherapy in combination with bevacizumab after initial cetuximab (n = 67). PFS after second-line therapy was slightly longer for patients who received initial cetuximab (6.3 vs. 5.7 months for KRAS exon 2 wild-type group and 7.3 vs. 5.8 months for RAS wild-type group), though the differences were not statistically significant.
However, overall survival after second-line therapy was significantly longer for the intention-to-treat population when cetuximab was the initial treatment (16.3 months vs. 13.2 months, P = .0021), as was PFS after second line therapy (6.5 vs. 4.7 months, P less than 0.001).
“Taken together, it seems that the sequential application of anti-EGFR agents followed by second-line anti-VEGF therapy achieves more favorable results than the reverse sequence,” said Dr. Modest and his associates. Particularly for patients witth RAS wild-type tumors, “first-line application of anti EGFR–directed therapy may therefore represent an optimal condition for effective subsequent therapy including antiangiogenic agents,” they said.
Dr. Modest and his coauthors cautioned that although poststudy treatment analysis was predefined for FIRE-3, their findings are observational and should not replace prospectively randomized trials designed to compare cancer therapy sequences.
The study was sponsored by Merck KGaA. The study authors report multiple financial disclosures for various pharmaceutical companies.
On Twitter @karioakes
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: First-line use of anti-EGFR agents, followed by subsequent antiangiogenic agents, resulted in better survival for patients with metastatic colorectal cancer (mCRC) than the reverse order.
Major finding: Patients who received initial cetuximab, compared with bevacizumab had longer overall survival after second-line therapy (16.3 months vs. 13.2 months, P = .0021).
Data source: Retrospective, exploratory analyses from FIRE-3, an open-label, randomized phase III clinical trial of cetuximab or bevacizumab in combination with FOLFIRI (fluorouracil plus folinic acid in combination with irinotecan) for patients with metastatic colorectal cancer (n = 592, KRAS exon 2 wild-type and n = 400, RAS wild-type).
Disclosures: The study was sponsored by Merck KGaA. The study authors report multiple financial disclosures for various pharmaceutical companies.
Solid histology predicts poor survival in resected lung adenocarcinoma
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Predominantly solid tumor histology predicted earlier recurrence and poorer postrecurrence survival (PRS) in surgically resected stage I lung adenocarcinoma.
Major finding: Lung adenocarcinoma patients with predominantly solid tumor subtype had worse PRS than did those with other subtypes after surgical resection (HR, 1.76, P = .016).
Data source: Retrospective, single-site medical record review of 1,120 patients undergoing complete resection for stage I lung adenocarcinoma from 1999 to 2009.
Disclosures: The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
New Cushing’s guidelines emphasize team approach
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Percutaneous thrombectomy reduces risk of postthrombotic syndrome
Adding a mechanical suction technique to local thrombolysis to break up and remove blood clots reduced postthrombotic syndrome (PTS) after deep vein thrombosis (DVT) without causing increased complications, according to a small retrospective study.
Dr. Chun-Yang Huang of the National Yang Ming University (Taipei, Taiwan) and colleagues examined patients diagnosed with acute proximal lower limb DVT. Patients received either thrombolysis alone via a catheter-directed thrombolysis (CDT), or percutaneous mechanical thrombectomy (PMT) by a combination of pharmacologic thrombolysis and suction; both techniques were accompanied by systemic anticoagulation. Though both treatment groups fared well during treatment and for the 12-month follow-up period, the PMT group had a significantly lower incidence of PTS 1 year after treatment (Ann. Vascular Surg. 2015. doi: 10.1016/j.avsg.2015.01.014).
For those with DVT, parenteral anticoagulation prevents propagation of the clot and minimizes risk of pulmonary embolism (PE); however, anticoagulation does not accelerate dissolution of the existing clot. According to study authors, 30%-40% of those with proximal leg DVTs will go on to develop PTS, with the prolonged distal venous stasis from an undisturbed clot causing loss of valvular competence and resultant chronic venous insufficiency. PTS can involve leg swelling, discomfort, skin changes, and ulceration, with significant impact on quality of life and health care costs.
Techniques such as CDT and PMT can increase the rate of clot dissolution, thus restoring patency sooner and minimizing risk for PTS. However, these methods also can carry increased risk of bleeding and infection, considerations that must be balanced against potential benefit.
Investigators reviewed records for 39 patients who were diagnosed with ultrasound- or CT-confirmed acute proximal lower limb DVT and received either CDT or PMT during the period from November 2010 to November 2013. Patients were not randomized to treatment arms but were assigned using clinical judgment and patient preference. During the 12-month follow-up, three participants died of malignancy and two were lost to follow-up. Analysis was completed for the remaining 34 patients.
Overall, patient characteristics did not differ significantly between groups, with mean ages of 62.75 for the PMT group (n = 16) and 64.17 for the CDT group (n = 18). In all, 13/34 participants were female. Patients in both treatment groups fared well, with no 30-day mortality, and no episodes of major bleeding, PE, or renal failure. Ten patients in the PMT group and six in the CDT group required stenting of the common iliac vein to maintain patency, a nonsignificant difference. Just one participant in the CDE group experienced a minor bleeding event.
Turning to outcomes, study authors assessed postprocedure patency, finding improved patency for both procedures (P less than .001 for both, compared with preoperation patency scores), with no significant difference between the two groups post procedure. Thrombus scores were also significantly better for both treatment arms post procedure (P less than .001). Clot burden tended to improve more rapidly over the 12-month follow-up period for the PMT group, though the difference between groups was just short of statistically significant.
At 12 months, though the amount of venous reflux did not differ significantly between groups, those who had received PMT had significantly fewer signs and symptoms of PTS. This assessment used the Villalta scale, a standardized assessment and scoring system for PTS, where higher numbers indicate worse PTS. The PMT group’s Villalta score was 2.06 +/–2.95, compared with 5.06 +/–4.07 for the CDT group (P = .030).
Study limitations included the small study size, retrospective study design, and lack of randomization. Acknowledging these limitations, Dr. Huang and coauthors called for larger, multicenter, randomized controlled studies of PMT. The personal and economic costs of PTS, they argue, warrant exploring whether PMT may help minimize total thrombolysis dose, reduce hospital stays, and decrease costs while minimizing the risks of chronic venous insufficiency post DVT.
Dr. Huang and coauthors reported no conflicts of interest.
Adding a mechanical suction technique to local thrombolysis to break up and remove blood clots reduced postthrombotic syndrome (PTS) after deep vein thrombosis (DVT) without causing increased complications, according to a small retrospective study.
Dr. Chun-Yang Huang of the National Yang Ming University (Taipei, Taiwan) and colleagues examined patients diagnosed with acute proximal lower limb DVT. Patients received either thrombolysis alone via a catheter-directed thrombolysis (CDT), or percutaneous mechanical thrombectomy (PMT) by a combination of pharmacologic thrombolysis and suction; both techniques were accompanied by systemic anticoagulation. Though both treatment groups fared well during treatment and for the 12-month follow-up period, the PMT group had a significantly lower incidence of PTS 1 year after treatment (Ann. Vascular Surg. 2015. doi: 10.1016/j.avsg.2015.01.014).
For those with DVT, parenteral anticoagulation prevents propagation of the clot and minimizes risk of pulmonary embolism (PE); however, anticoagulation does not accelerate dissolution of the existing clot. According to study authors, 30%-40% of those with proximal leg DVTs will go on to develop PTS, with the prolonged distal venous stasis from an undisturbed clot causing loss of valvular competence and resultant chronic venous insufficiency. PTS can involve leg swelling, discomfort, skin changes, and ulceration, with significant impact on quality of life and health care costs.
Techniques such as CDT and PMT can increase the rate of clot dissolution, thus restoring patency sooner and minimizing risk for PTS. However, these methods also can carry increased risk of bleeding and infection, considerations that must be balanced against potential benefit.
Investigators reviewed records for 39 patients who were diagnosed with ultrasound- or CT-confirmed acute proximal lower limb DVT and received either CDT or PMT during the period from November 2010 to November 2013. Patients were not randomized to treatment arms but were assigned using clinical judgment and patient preference. During the 12-month follow-up, three participants died of malignancy and two were lost to follow-up. Analysis was completed for the remaining 34 patients.
Overall, patient characteristics did not differ significantly between groups, with mean ages of 62.75 for the PMT group (n = 16) and 64.17 for the CDT group (n = 18). In all, 13/34 participants were female. Patients in both treatment groups fared well, with no 30-day mortality, and no episodes of major bleeding, PE, or renal failure. Ten patients in the PMT group and six in the CDT group required stenting of the common iliac vein to maintain patency, a nonsignificant difference. Just one participant in the CDE group experienced a minor bleeding event.
Turning to outcomes, study authors assessed postprocedure patency, finding improved patency for both procedures (P less than .001 for both, compared with preoperation patency scores), with no significant difference between the two groups post procedure. Thrombus scores were also significantly better for both treatment arms post procedure (P less than .001). Clot burden tended to improve more rapidly over the 12-month follow-up period for the PMT group, though the difference between groups was just short of statistically significant.
At 12 months, though the amount of venous reflux did not differ significantly between groups, those who had received PMT had significantly fewer signs and symptoms of PTS. This assessment used the Villalta scale, a standardized assessment and scoring system for PTS, where higher numbers indicate worse PTS. The PMT group’s Villalta score was 2.06 +/–2.95, compared with 5.06 +/–4.07 for the CDT group (P = .030).
Study limitations included the small study size, retrospective study design, and lack of randomization. Acknowledging these limitations, Dr. Huang and coauthors called for larger, multicenter, randomized controlled studies of PMT. The personal and economic costs of PTS, they argue, warrant exploring whether PMT may help minimize total thrombolysis dose, reduce hospital stays, and decrease costs while minimizing the risks of chronic venous insufficiency post DVT.
Dr. Huang and coauthors reported no conflicts of interest.
Adding a mechanical suction technique to local thrombolysis to break up and remove blood clots reduced postthrombotic syndrome (PTS) after deep vein thrombosis (DVT) without causing increased complications, according to a small retrospective study.
Dr. Chun-Yang Huang of the National Yang Ming University (Taipei, Taiwan) and colleagues examined patients diagnosed with acute proximal lower limb DVT. Patients received either thrombolysis alone via a catheter-directed thrombolysis (CDT), or percutaneous mechanical thrombectomy (PMT) by a combination of pharmacologic thrombolysis and suction; both techniques were accompanied by systemic anticoagulation. Though both treatment groups fared well during treatment and for the 12-month follow-up period, the PMT group had a significantly lower incidence of PTS 1 year after treatment (Ann. Vascular Surg. 2015. doi: 10.1016/j.avsg.2015.01.014).
For those with DVT, parenteral anticoagulation prevents propagation of the clot and minimizes risk of pulmonary embolism (PE); however, anticoagulation does not accelerate dissolution of the existing clot. According to study authors, 30%-40% of those with proximal leg DVTs will go on to develop PTS, with the prolonged distal venous stasis from an undisturbed clot causing loss of valvular competence and resultant chronic venous insufficiency. PTS can involve leg swelling, discomfort, skin changes, and ulceration, with significant impact on quality of life and health care costs.
Techniques such as CDT and PMT can increase the rate of clot dissolution, thus restoring patency sooner and minimizing risk for PTS. However, these methods also can carry increased risk of bleeding and infection, considerations that must be balanced against potential benefit.
Investigators reviewed records for 39 patients who were diagnosed with ultrasound- or CT-confirmed acute proximal lower limb DVT and received either CDT or PMT during the period from November 2010 to November 2013. Patients were not randomized to treatment arms but were assigned using clinical judgment and patient preference. During the 12-month follow-up, three participants died of malignancy and two were lost to follow-up. Analysis was completed for the remaining 34 patients.
Overall, patient characteristics did not differ significantly between groups, with mean ages of 62.75 for the PMT group (n = 16) and 64.17 for the CDT group (n = 18). In all, 13/34 participants were female. Patients in both treatment groups fared well, with no 30-day mortality, and no episodes of major bleeding, PE, or renal failure. Ten patients in the PMT group and six in the CDT group required stenting of the common iliac vein to maintain patency, a nonsignificant difference. Just one participant in the CDE group experienced a minor bleeding event.
Turning to outcomes, study authors assessed postprocedure patency, finding improved patency for both procedures (P less than .001 for both, compared with preoperation patency scores), with no significant difference between the two groups post procedure. Thrombus scores were also significantly better for both treatment arms post procedure (P less than .001). Clot burden tended to improve more rapidly over the 12-month follow-up period for the PMT group, though the difference between groups was just short of statistically significant.
At 12 months, though the amount of venous reflux did not differ significantly between groups, those who had received PMT had significantly fewer signs and symptoms of PTS. This assessment used the Villalta scale, a standardized assessment and scoring system for PTS, where higher numbers indicate worse PTS. The PMT group’s Villalta score was 2.06 +/–2.95, compared with 5.06 +/–4.07 for the CDT group (P = .030).
Study limitations included the small study size, retrospective study design, and lack of randomization. Acknowledging these limitations, Dr. Huang and coauthors called for larger, multicenter, randomized controlled studies of PMT. The personal and economic costs of PTS, they argue, warrant exploring whether PMT may help minimize total thrombolysis dose, reduce hospital stays, and decrease costs while minimizing the risks of chronic venous insufficiency post DVT.
Dr. Huang and coauthors reported no conflicts of interest.
Key clinical point: Both percutaneous PMT and catheter-directed thrombolysis (CDT) were safe and effective, but PMT reduced risk of postthrombotic syndrome.
Major finding: In a small retrospective analysis of patients with deep vein thrombosis (DVT), both PMT and CDT were safe and effective when used in combination with systemic anticoagulation; however, postthrombotic syndrome (PTS) scoring was significantly better for those receiving PMT (Villalta score 2.1 +/- 3.0 vs. 5.1 +/- 4.1, P = .030).
Data source: Retrospective study of 39 patients who were diagnosed with acute proximal DVT of the lower limb between November 2010 and November 2013 at a Taiwanese hospital.
Disclosures: The authors reported that they had no conflicts of interest; funding source was not provided.