User login
Infectious Sacroiliitis in a Patient With a History of IV Drug Use
Case
A 29-year-old man presented to the ED with a 3-day history of constant left-sided low back pain that radiated to his left buttock and groin. The patient stated the pain worsened with movement, making it difficult for him to walk. He reported lifting heavy boxes at work, but denied any trauma. The patient also denied recent fevers, chills, chest pain, dyspnea, abdominal pain, urinary or fecal incontinence, weakness, numbness, or saddle anesthesia. Regarding his medical history, he had an appendectomy as a child, but reported no other surgeries or medical issues. His social history was significant for narcotic and inhalant use and daily tobacco use. The patient also reported taking heroin intravenously (IV) 6 months prior.
Vital signs at presentation were: heart rate (HR), 92 beats/min; respiratory rate, 15 breaths/min; blood pressure, 118/80 mm Hg; and temperature, 98.2°F. Oxygen saturation was 98% on room air.
The patient was a well-developed young man in no apparent distress. Dermatological examination showed bilateral track marks in the antecubital fossa. The musculoskeletal (MSK) examination demonstrated left gluteal tenderness to palpation and decreased active and passive range of motion of the left hip, especially with internal rotation and flexion. He had no midline tenderness, and the lower extremities had normal pulses and no motor or sensory deficits.
The patient’s pain improved with IV fluids, diazepam, and ketorolac, and he was able to ambulate with assistance. He was clinically diagnosed with sciatica, and discharged home with prescriptions for diazepam and ibuprofen. He was also instructed to follow-up with an orthopedist within 7 days from discharge.
The patient returned to the ED the following day with similar complaints of unabating left-sided pain and difficulty ambulating. His vital signs were notable for an elevated HR of 106 beats/min. Physical examination findings were unchanged from his presentation the previous day, and an X-ray of the lumbar spine showed no abnormalities.
After receiving IV analgesics, the patient’s pain improved and his tachycardia resolved. He was discharged home with instructions to continue taking diazepam, and was also given prescriptions for prednisone and oxycodone/acetaminophen. He was instructed to follow-up with an orthopedist within 24 hours.
Over the next 9 days, the patient was seen twice by an orthopedist, who ordered imaging of the lumbar spine, including a repeat X-ray and contrast-enhanced magnetic resonance imaging (MRI), both of which were unremarkable. The patient completed the prescribed course of diclofenac, oxycodone/acetaminophen, and prednisone, but experienced only minimal pain relief. The orthopedist prescribed the diclofenac to supplement the medication regimen that he was already on.
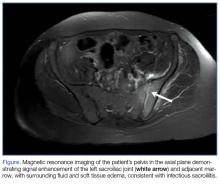
At the second follow-up visit, the orthopedist ordered an MRI of the patient’s left hip, which demonstrated inflammation of the left sacroiliac joint (SIJ) with effusion, and a 1-cm by 1-cm collection adjacent to the left psoas muscle; these findings were concerning for septic arthritis (Figure). Based on the MRI study, a computed tomography (CT)-guided arthrocentesis of the left SIJ was performed by an interventional radiologist.
Following the arthrocentesis, the orthopedist referred the patient to the ED. At this presentation, the emergency physician (EP) ordered blood cultures, blood work, urinalysis, and a urinary toxicology screen, and started the patient on IV ceftriaxone and vancomycin. The laboratory studies were significant for the following elevated inflammatory markers: erythrocyte sedimentation rate (ESR), 19 mm/h; C-reactive protein (CRP), 2.45 mg/L; white blood cell count (WBC), 13.6 K/uL with normal differential; and lactate level, 2.6 mg/dL. The toxicology screen was positive for opioids. The basic metabolic panel, chest X-ray, and urinalysis were all unremarkable. An electrocardiogram showed sinus tachycardia.
The patient was admitted to the hospital, and infectious disease services was contacted. While awaiting transport to the inpatient floor, the patient admitted to IV drug use 4 weeks prior to his initial presentation—not the 6 months he initially reported at the first ED visit.
The blood cultures grew Candida parapsilosis, and culture from the SIJ arthrocentesis grew Pseudomonas aeruginosa. The infectious disease physician switched the patient’s antibiotic therapy to IV cefepime and fluconazole. The patient also was seen by an orthopedist, who determined that no surgical intervention was required.
Follow-up laboratory studies showed inflammatory markers peaking at the following levels: ESR, 36 mm/h; CRP, 4.84 mg/L; and WBC, 32.1 K/uL with 90% neutrophils. These markers normalized throughout his hospital stay. The patient was also tested for hepatitis and human immunodeficiency virus, both of which were negative. A transesophageal echocardiogram showed no obvious masses or vegetations.
The patient had an uncomplicated hospital course, and was discharged home on hospital day 6 with a 4-week prescription of oral fluconazole and levofloxacin, and instructed to follow-up with both infectious disease and the orthopedist. To address his history of IV drug use, he also was given follow-up with pain management.
One month later, the patient returned a fourth time to the ED for evaluation of bilateral lower extremity pain and swelling. He stated that he had been mostly bed-bound at home since his discharge from the hospital due to continued pain with weight-bearing.
The patient’s vital signs were normal. The EP ordered a duplex ultrasound study, which showed extensive bilateral lower extremity deep vein thrombosis. He was started on subcutaneous therapeutic enoxaparin and admitted to the inpatient hospital. During admission, a left lower lobe pulmonary artery embolism was found on chest CT angiography, though he had no cardiac or respiratory symptoms. He was discharged home with a 3-month prescription for oral rivaroxaban.
At a 4-month follow-up visit, the patient reported minimal residual disability after completing the course of treatment. During the follow-up, the patient denied using IV heroin; he was referred to a pain management specialist, who placed the patient on methadone.
Discussion
Infectious sacroiliitis (ISI) is a rare form of infectious arthritis affecting the SIJ, with an incidence of 1 to 2 reported cases per year.1 The literature on ISI currently consists only of case reports and case series. This infection is often diagnosed after the disease has progressed, with a mean time to diagnosis of 43.3 days.2
Infectious arthritis of any joint has a prevalence of 2 to 10 per 100,000 people. In 50% of cases, the knee is the joint most commonly affected, followed by the hip, shoulder, and elbow.3 Regardless of location, infectious arthritis is associated with significant morbidity and mortality due to sepsis and irreversible loss of joint function.4
Risk factors for ISI include IV drug use, pregnancy, trauma, endocarditis, and immunosuppression.1 The decision to initiate the workup for ISI can be difficult to make because the condition may present without signs of an infectious etiology, such as toxic appearance, inflammatory changes surrounding the joint, or even fever—only 41% of affected patients in one case series were febrile.2 The workup is often time-consuming, invasive, and expensive.
Although delayed diagnosis and treatment of septic arthritis is associated with significant adverse effects, there is unfortunately no consensus to guide the workup for ISI. As opposed to Kocher’s criteria for the differentiation of septic hip arthritis from transient synovitis in pediatric patients or well-known red-flags for further evaluation of low back pain, physicians are left without much guidance when considering laboratory workup or imaging decisions to evaluate for ISI.
Sacroiliac Joint
As previously noted, the SIJ is not commonly affected by infection. It is a diarthrodial, L-shaped joint comprised of the posterior ilium and sacrum, and is a near-rigid structure with very limited movement that provides stability to the axial skeleton.5 The SIJ is often overlooked as a secondary cause of low back pain in younger patients with rheumatologic conditions (eg, ankylosing spondylitis, Reiter syndrome), pregnancy-associated ligamentous laxity, and osteoarthritis in elderly patients. In one study, 88.2% of sacroiliitis cases were inflammatory, 8.8% infectious, and 2.9% degenerative.6
Signs and Symptoms
As our case illustrates, ISI often presents with nonspecific symptoms and physical findings.7 Patients typically present with fever, painful manipulation of the SIJ, and unilateral lumbo-gluteal pain.2 The components of the history and physical examination suspicious for an infectious etiology include the subacute presentation; unresolved pain despite treatment; tenderness to palpation; decreased range of motion; and recent IV drug use, which increases the risk of infectious disease due to unsterile practices and direct inoculation of pathogens into the bloodstream8 and a further predilection into the axial skeleton. 9 It is important to obtain an accurate social history; however, patients may not be forthright about disclosing sensitive information such as sexual history and illicit drug use.
Physical Assessment
The SIJ is best appreciated in the seated patient by palpating one fingerbreadth medial to the posterior superior iliac spine as he or she slowly bends forward.10 Tenderness elicited while in this position is suggestive of SIJ inflammation. The area of tenderness may be lower than anticipated and lateral to the gluteal cleft, as synovial fluid is typically relegated to the lower half of the joint.
Several adjunctive physical examination maneuvers, such as the Gaenslen test and Flexion Abduction External Rotation test (FABER test or Patrick’s test) can isolate SIJ pathology or dysfunction. The Gaenslen test is performed by asking the patient to lie supine and flex the affected hip and knee, with the lumbar spine flat against the examination table. Hyperextending the contralateral thigh downward will reproduce pain in the affected SIJ.
The FABER test is a simple but less specific examination technique to assess joint pain in the hip, lumbar, and sacroiliac joints.11 In this assessment, the clinician flexes the patient’s affected knee to 90°, externally rotates the hip, and applies downward pressure on the knee. Pain reproduced in the affected SI region is sensitive for joint inflammation.
Laboratory and Imaging Studies
Laboratory studies typically show inconsistent and nonspecific findings, such as the elevated ESR and CRP levels seen in our patient.2,12 Imaging studies to assess the SIJ for signs of infection are therefore essential for confirming infection.
Magnetic resonance imaging is the preferred imaging modality to assess for ISI, since it has the highest sensitivity in visualizing joint effusion and bone marrow edema compared to other modalities. Computed tomography, however, can be helpful in visualizing associated abscesses and guiding arthrocentesis.12 Plain X-ray may not demonstrate early changes in bone.13 The confirmatory study for ISI is synovial fluid analysis and culture.7
Treatment
Infectious sacroiliitis secondary to P aeruginosa, a gram-negative bacillus, is difficult to treat because of the glycocalyx and slime production that protects the pathogen from antibiotics, the development of multiple-antimicrobial resistance, and poor drug penetration into bones and abscesses.14 Antibiotic treatment should cover Staphylococcus aureus and may be broadened to cover gram-negative bacilli. The recommended duration of treatment is at least a 2-week course of IV antibiotics, followed by a 6-week course of oral antibiotics.2 Therapy also includes pain control and surgical intervention for abscesses, osteomyelitis, and refractory cases.7
Complications
Complications and long-term sequelae are common in ISI, often due to late diagnosis of the condition. Our case illustrates the delayed diagnosis of Pseudomonas ISI with candidemia in a young man with a history of IV drug use presenting with atraumatic low back pain. His clinical course was complicated by a thromboembolic event, likely secondary to immobility and a hypercoagulable state from infection and inflammation.15 Infectious sacroiliitis secondary to P aeruginosa is most commonly seen in patients with immunosuppression, hospitalization, and IV drug use.2
Summary
Infectious sacroiliitis remains a diagnostic challenge for physicians due to its rare incidence and nonspecific clinical manifestations. Our case illustrates the importance of maintaining a high level of clinical suspicion for infectious arthritis in young patients presenting with common MSK complaints in the presence of infectious risk factors. Emergency physicians should consider red flags, abnormal vital signs, and patient recidivism when deciding on the most appropriate workup.
1. Mancarella L, De Santis M, Magarelli N, Ierardi AM, Bonomo L, Ferraccioli G. Septic sacroiliitis: an uncommon septic arthritis. Clin Exp Rheumatol. 2009;27(6):1004-1008.
2. Hermet M, Minichiello E, Flipo RM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC Infect Dis. 2012;12:305. doi:10.1186/1471-2334-12-305.
3. Abelson A. Septic Arthritis. Cleveland Clinic. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/rheumatology/septic-arthritis. Published August 2010. Accessed October 28, 2016.
4. Goldenberg DL. Septic arthritis. Lancet. 1998;351(9097):197-202. doi:10.1016/S0140-6736(97)09522-6.
5. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x.
6. Owlia MB, Danesh-Ardakani M. Frequency of sacroiliitis among patients with low back pain. Electron Physician. 2016;8(3):2094-2100. doi:10.19082/2094.
7. Zimmermann B 3rd, Mikolich DJ, Lally EV. Septic sacroiliitis. Semin Arthritis Rheum. 1996;26(3):592-604.
8. Brtalik D, Pariyadath M. A case report of infectious sacroiliitis in an adult presenting to the emergency department with inability to walk. J Emerg Med. 2017:52(3)e65-e68. doi:10.1016/j.jemermed.2016.10.022.
9. Ferraro K, Cohen MA. Acute septic sacroiliitis in an injection drug user. Am J Emerg Med. 2004;22(1):60-61.
10. Safran M, Botser IB. Hip anatomy and biomechanics. In: Miller MD, Thompson SR, eds. DeLee & Drez’s Orthopaedic Sports Medicine. Vol 2. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015:917-932.e1.
11. LeBlond RF, Brown DD, Suneja M, Szot JF. The spine, pelvic, and extremities. In: LeBlond RF, Brown DD, Suneja M, Szot JF. eds. DeGowin’s Diagnostic Examination. 10th ed. New York, NY: McGraw-Hill; 2015:508-576.
12. Scott KR, Rising KL, Conlon LW. Infectious sacroiliitis. J Emerg Med. 2014;47(3):83-84. doi:10.1016/j.jemermed.2014.05.001.
13. Cinar M, Sanal HT, Yilmaz S, et al. Radiological followup of the evolution of inflammatory process in sacroiliac joint with magnetic resonance imaging: a case with pyogenic sacroiliitis. Case Rep Rheumatol. 2012;2012:509136. doi:10.1155/2012/509136.
14. Calza L, Manfredi R, Marinacci G, Fortunato L, Chiodo F. Community-acquired Pseudomonas aeruginosa sacro-iliitis in a previously healthy patient. J Med Microbiol. 2002;51(7):620-622.
15. Levi M, Keller TT, van Gorp E, ten Cate H. Infection and inflammation and the coagulation system. Cardiovasc Res. 2003;60(1):26-39.
Case
A 29-year-old man presented to the ED with a 3-day history of constant left-sided low back pain that radiated to his left buttock and groin. The patient stated the pain worsened with movement, making it difficult for him to walk. He reported lifting heavy boxes at work, but denied any trauma. The patient also denied recent fevers, chills, chest pain, dyspnea, abdominal pain, urinary or fecal incontinence, weakness, numbness, or saddle anesthesia. Regarding his medical history, he had an appendectomy as a child, but reported no other surgeries or medical issues. His social history was significant for narcotic and inhalant use and daily tobacco use. The patient also reported taking heroin intravenously (IV) 6 months prior.
Vital signs at presentation were: heart rate (HR), 92 beats/min; respiratory rate, 15 breaths/min; blood pressure, 118/80 mm Hg; and temperature, 98.2°F. Oxygen saturation was 98% on room air.
The patient was a well-developed young man in no apparent distress. Dermatological examination showed bilateral track marks in the antecubital fossa. The musculoskeletal (MSK) examination demonstrated left gluteal tenderness to palpation and decreased active and passive range of motion of the left hip, especially with internal rotation and flexion. He had no midline tenderness, and the lower extremities had normal pulses and no motor or sensory deficits.
The patient’s pain improved with IV fluids, diazepam, and ketorolac, and he was able to ambulate with assistance. He was clinically diagnosed with sciatica, and discharged home with prescriptions for diazepam and ibuprofen. He was also instructed to follow-up with an orthopedist within 7 days from discharge.
The patient returned to the ED the following day with similar complaints of unabating left-sided pain and difficulty ambulating. His vital signs were notable for an elevated HR of 106 beats/min. Physical examination findings were unchanged from his presentation the previous day, and an X-ray of the lumbar spine showed no abnormalities.
After receiving IV analgesics, the patient’s pain improved and his tachycardia resolved. He was discharged home with instructions to continue taking diazepam, and was also given prescriptions for prednisone and oxycodone/acetaminophen. He was instructed to follow-up with an orthopedist within 24 hours.
Over the next 9 days, the patient was seen twice by an orthopedist, who ordered imaging of the lumbar spine, including a repeat X-ray and contrast-enhanced magnetic resonance imaging (MRI), both of which were unremarkable. The patient completed the prescribed course of diclofenac, oxycodone/acetaminophen, and prednisone, but experienced only minimal pain relief. The orthopedist prescribed the diclofenac to supplement the medication regimen that he was already on.
At the second follow-up visit, the orthopedist ordered an MRI of the patient’s left hip, which demonstrated inflammation of the left sacroiliac joint (SIJ) with effusion, and a 1-cm by 1-cm collection adjacent to the left psoas muscle; these findings were concerning for septic arthritis (Figure). Based on the MRI study, a computed tomography (CT)-guided arthrocentesis of the left SIJ was performed by an interventional radiologist.
Following the arthrocentesis, the orthopedist referred the patient to the ED. At this presentation, the emergency physician (EP) ordered blood cultures, blood work, urinalysis, and a urinary toxicology screen, and started the patient on IV ceftriaxone and vancomycin. The laboratory studies were significant for the following elevated inflammatory markers: erythrocyte sedimentation rate (ESR), 19 mm/h; C-reactive protein (CRP), 2.45 mg/L; white blood cell count (WBC), 13.6 K/uL with normal differential; and lactate level, 2.6 mg/dL. The toxicology screen was positive for opioids. The basic metabolic panel, chest X-ray, and urinalysis were all unremarkable. An electrocardiogram showed sinus tachycardia.
The patient was admitted to the hospital, and infectious disease services was contacted. While awaiting transport to the inpatient floor, the patient admitted to IV drug use 4 weeks prior to his initial presentation—not the 6 months he initially reported at the first ED visit.
The blood cultures grew Candida parapsilosis, and culture from the SIJ arthrocentesis grew Pseudomonas aeruginosa. The infectious disease physician switched the patient’s antibiotic therapy to IV cefepime and fluconazole. The patient also was seen by an orthopedist, who determined that no surgical intervention was required.
Follow-up laboratory studies showed inflammatory markers peaking at the following levels: ESR, 36 mm/h; CRP, 4.84 mg/L; and WBC, 32.1 K/uL with 90% neutrophils. These markers normalized throughout his hospital stay. The patient was also tested for hepatitis and human immunodeficiency virus, both of which were negative. A transesophageal echocardiogram showed no obvious masses or vegetations.
The patient had an uncomplicated hospital course, and was discharged home on hospital day 6 with a 4-week prescription of oral fluconazole and levofloxacin, and instructed to follow-up with both infectious disease and the orthopedist. To address his history of IV drug use, he also was given follow-up with pain management.
One month later, the patient returned a fourth time to the ED for evaluation of bilateral lower extremity pain and swelling. He stated that he had been mostly bed-bound at home since his discharge from the hospital due to continued pain with weight-bearing.
The patient’s vital signs were normal. The EP ordered a duplex ultrasound study, which showed extensive bilateral lower extremity deep vein thrombosis. He was started on subcutaneous therapeutic enoxaparin and admitted to the inpatient hospital. During admission, a left lower lobe pulmonary artery embolism was found on chest CT angiography, though he had no cardiac or respiratory symptoms. He was discharged home with a 3-month prescription for oral rivaroxaban.
At a 4-month follow-up visit, the patient reported minimal residual disability after completing the course of treatment. During the follow-up, the patient denied using IV heroin; he was referred to a pain management specialist, who placed the patient on methadone.
Discussion
Infectious sacroiliitis (ISI) is a rare form of infectious arthritis affecting the SIJ, with an incidence of 1 to 2 reported cases per year.1 The literature on ISI currently consists only of case reports and case series. This infection is often diagnosed after the disease has progressed, with a mean time to diagnosis of 43.3 days.2
Infectious arthritis of any joint has a prevalence of 2 to 10 per 100,000 people. In 50% of cases, the knee is the joint most commonly affected, followed by the hip, shoulder, and elbow.3 Regardless of location, infectious arthritis is associated with significant morbidity and mortality due to sepsis and irreversible loss of joint function.4
Risk factors for ISI include IV drug use, pregnancy, trauma, endocarditis, and immunosuppression.1 The decision to initiate the workup for ISI can be difficult to make because the condition may present without signs of an infectious etiology, such as toxic appearance, inflammatory changes surrounding the joint, or even fever—only 41% of affected patients in one case series were febrile.2 The workup is often time-consuming, invasive, and expensive.
Although delayed diagnosis and treatment of septic arthritis is associated with significant adverse effects, there is unfortunately no consensus to guide the workup for ISI. As opposed to Kocher’s criteria for the differentiation of septic hip arthritis from transient synovitis in pediatric patients or well-known red-flags for further evaluation of low back pain, physicians are left without much guidance when considering laboratory workup or imaging decisions to evaluate for ISI.
Sacroiliac Joint
As previously noted, the SIJ is not commonly affected by infection. It is a diarthrodial, L-shaped joint comprised of the posterior ilium and sacrum, and is a near-rigid structure with very limited movement that provides stability to the axial skeleton.5 The SIJ is often overlooked as a secondary cause of low back pain in younger patients with rheumatologic conditions (eg, ankylosing spondylitis, Reiter syndrome), pregnancy-associated ligamentous laxity, and osteoarthritis in elderly patients. In one study, 88.2% of sacroiliitis cases were inflammatory, 8.8% infectious, and 2.9% degenerative.6
Signs and Symptoms
As our case illustrates, ISI often presents with nonspecific symptoms and physical findings.7 Patients typically present with fever, painful manipulation of the SIJ, and unilateral lumbo-gluteal pain.2 The components of the history and physical examination suspicious for an infectious etiology include the subacute presentation; unresolved pain despite treatment; tenderness to palpation; decreased range of motion; and recent IV drug use, which increases the risk of infectious disease due to unsterile practices and direct inoculation of pathogens into the bloodstream8 and a further predilection into the axial skeleton. 9 It is important to obtain an accurate social history; however, patients may not be forthright about disclosing sensitive information such as sexual history and illicit drug use.
Physical Assessment
The SIJ is best appreciated in the seated patient by palpating one fingerbreadth medial to the posterior superior iliac spine as he or she slowly bends forward.10 Tenderness elicited while in this position is suggestive of SIJ inflammation. The area of tenderness may be lower than anticipated and lateral to the gluteal cleft, as synovial fluid is typically relegated to the lower half of the joint.
Several adjunctive physical examination maneuvers, such as the Gaenslen test and Flexion Abduction External Rotation test (FABER test or Patrick’s test) can isolate SIJ pathology or dysfunction. The Gaenslen test is performed by asking the patient to lie supine and flex the affected hip and knee, with the lumbar spine flat against the examination table. Hyperextending the contralateral thigh downward will reproduce pain in the affected SIJ.
The FABER test is a simple but less specific examination technique to assess joint pain in the hip, lumbar, and sacroiliac joints.11 In this assessment, the clinician flexes the patient’s affected knee to 90°, externally rotates the hip, and applies downward pressure on the knee. Pain reproduced in the affected SI region is sensitive for joint inflammation.
Laboratory and Imaging Studies
Laboratory studies typically show inconsistent and nonspecific findings, such as the elevated ESR and CRP levels seen in our patient.2,12 Imaging studies to assess the SIJ for signs of infection are therefore essential for confirming infection.
Magnetic resonance imaging is the preferred imaging modality to assess for ISI, since it has the highest sensitivity in visualizing joint effusion and bone marrow edema compared to other modalities. Computed tomography, however, can be helpful in visualizing associated abscesses and guiding arthrocentesis.12 Plain X-ray may not demonstrate early changes in bone.13 The confirmatory study for ISI is synovial fluid analysis and culture.7
Treatment
Infectious sacroiliitis secondary to P aeruginosa, a gram-negative bacillus, is difficult to treat because of the glycocalyx and slime production that protects the pathogen from antibiotics, the development of multiple-antimicrobial resistance, and poor drug penetration into bones and abscesses.14 Antibiotic treatment should cover Staphylococcus aureus and may be broadened to cover gram-negative bacilli. The recommended duration of treatment is at least a 2-week course of IV antibiotics, followed by a 6-week course of oral antibiotics.2 Therapy also includes pain control and surgical intervention for abscesses, osteomyelitis, and refractory cases.7
Complications
Complications and long-term sequelae are common in ISI, often due to late diagnosis of the condition. Our case illustrates the delayed diagnosis of Pseudomonas ISI with candidemia in a young man with a history of IV drug use presenting with atraumatic low back pain. His clinical course was complicated by a thromboembolic event, likely secondary to immobility and a hypercoagulable state from infection and inflammation.15 Infectious sacroiliitis secondary to P aeruginosa is most commonly seen in patients with immunosuppression, hospitalization, and IV drug use.2
Summary
Infectious sacroiliitis remains a diagnostic challenge for physicians due to its rare incidence and nonspecific clinical manifestations. Our case illustrates the importance of maintaining a high level of clinical suspicion for infectious arthritis in young patients presenting with common MSK complaints in the presence of infectious risk factors. Emergency physicians should consider red flags, abnormal vital signs, and patient recidivism when deciding on the most appropriate workup.
Case
A 29-year-old man presented to the ED with a 3-day history of constant left-sided low back pain that radiated to his left buttock and groin. The patient stated the pain worsened with movement, making it difficult for him to walk. He reported lifting heavy boxes at work, but denied any trauma. The patient also denied recent fevers, chills, chest pain, dyspnea, abdominal pain, urinary or fecal incontinence, weakness, numbness, or saddle anesthesia. Regarding his medical history, he had an appendectomy as a child, but reported no other surgeries or medical issues. His social history was significant for narcotic and inhalant use and daily tobacco use. The patient also reported taking heroin intravenously (IV) 6 months prior.
Vital signs at presentation were: heart rate (HR), 92 beats/min; respiratory rate, 15 breaths/min; blood pressure, 118/80 mm Hg; and temperature, 98.2°F. Oxygen saturation was 98% on room air.
The patient was a well-developed young man in no apparent distress. Dermatological examination showed bilateral track marks in the antecubital fossa. The musculoskeletal (MSK) examination demonstrated left gluteal tenderness to palpation and decreased active and passive range of motion of the left hip, especially with internal rotation and flexion. He had no midline tenderness, and the lower extremities had normal pulses and no motor or sensory deficits.
The patient’s pain improved with IV fluids, diazepam, and ketorolac, and he was able to ambulate with assistance. He was clinically diagnosed with sciatica, and discharged home with prescriptions for diazepam and ibuprofen. He was also instructed to follow-up with an orthopedist within 7 days from discharge.
The patient returned to the ED the following day with similar complaints of unabating left-sided pain and difficulty ambulating. His vital signs were notable for an elevated HR of 106 beats/min. Physical examination findings were unchanged from his presentation the previous day, and an X-ray of the lumbar spine showed no abnormalities.
After receiving IV analgesics, the patient’s pain improved and his tachycardia resolved. He was discharged home with instructions to continue taking diazepam, and was also given prescriptions for prednisone and oxycodone/acetaminophen. He was instructed to follow-up with an orthopedist within 24 hours.
Over the next 9 days, the patient was seen twice by an orthopedist, who ordered imaging of the lumbar spine, including a repeat X-ray and contrast-enhanced magnetic resonance imaging (MRI), both of which were unremarkable. The patient completed the prescribed course of diclofenac, oxycodone/acetaminophen, and prednisone, but experienced only minimal pain relief. The orthopedist prescribed the diclofenac to supplement the medication regimen that he was already on.
At the second follow-up visit, the orthopedist ordered an MRI of the patient’s left hip, which demonstrated inflammation of the left sacroiliac joint (SIJ) with effusion, and a 1-cm by 1-cm collection adjacent to the left psoas muscle; these findings were concerning for septic arthritis (Figure). Based on the MRI study, a computed tomography (CT)-guided arthrocentesis of the left SIJ was performed by an interventional radiologist.
Following the arthrocentesis, the orthopedist referred the patient to the ED. At this presentation, the emergency physician (EP) ordered blood cultures, blood work, urinalysis, and a urinary toxicology screen, and started the patient on IV ceftriaxone and vancomycin. The laboratory studies were significant for the following elevated inflammatory markers: erythrocyte sedimentation rate (ESR), 19 mm/h; C-reactive protein (CRP), 2.45 mg/L; white blood cell count (WBC), 13.6 K/uL with normal differential; and lactate level, 2.6 mg/dL. The toxicology screen was positive for opioids. The basic metabolic panel, chest X-ray, and urinalysis were all unremarkable. An electrocardiogram showed sinus tachycardia.
The patient was admitted to the hospital, and infectious disease services was contacted. While awaiting transport to the inpatient floor, the patient admitted to IV drug use 4 weeks prior to his initial presentation—not the 6 months he initially reported at the first ED visit.
The blood cultures grew Candida parapsilosis, and culture from the SIJ arthrocentesis grew Pseudomonas aeruginosa. The infectious disease physician switched the patient’s antibiotic therapy to IV cefepime and fluconazole. The patient also was seen by an orthopedist, who determined that no surgical intervention was required.
Follow-up laboratory studies showed inflammatory markers peaking at the following levels: ESR, 36 mm/h; CRP, 4.84 mg/L; and WBC, 32.1 K/uL with 90% neutrophils. These markers normalized throughout his hospital stay. The patient was also tested for hepatitis and human immunodeficiency virus, both of which were negative. A transesophageal echocardiogram showed no obvious masses or vegetations.
The patient had an uncomplicated hospital course, and was discharged home on hospital day 6 with a 4-week prescription of oral fluconazole and levofloxacin, and instructed to follow-up with both infectious disease and the orthopedist. To address his history of IV drug use, he also was given follow-up with pain management.
One month later, the patient returned a fourth time to the ED for evaluation of bilateral lower extremity pain and swelling. He stated that he had been mostly bed-bound at home since his discharge from the hospital due to continued pain with weight-bearing.
The patient’s vital signs were normal. The EP ordered a duplex ultrasound study, which showed extensive bilateral lower extremity deep vein thrombosis. He was started on subcutaneous therapeutic enoxaparin and admitted to the inpatient hospital. During admission, a left lower lobe pulmonary artery embolism was found on chest CT angiography, though he had no cardiac or respiratory symptoms. He was discharged home with a 3-month prescription for oral rivaroxaban.
At a 4-month follow-up visit, the patient reported minimal residual disability after completing the course of treatment. During the follow-up, the patient denied using IV heroin; he was referred to a pain management specialist, who placed the patient on methadone.
Discussion
Infectious sacroiliitis (ISI) is a rare form of infectious arthritis affecting the SIJ, with an incidence of 1 to 2 reported cases per year.1 The literature on ISI currently consists only of case reports and case series. This infection is often diagnosed after the disease has progressed, with a mean time to diagnosis of 43.3 days.2
Infectious arthritis of any joint has a prevalence of 2 to 10 per 100,000 people. In 50% of cases, the knee is the joint most commonly affected, followed by the hip, shoulder, and elbow.3 Regardless of location, infectious arthritis is associated with significant morbidity and mortality due to sepsis and irreversible loss of joint function.4
Risk factors for ISI include IV drug use, pregnancy, trauma, endocarditis, and immunosuppression.1 The decision to initiate the workup for ISI can be difficult to make because the condition may present without signs of an infectious etiology, such as toxic appearance, inflammatory changes surrounding the joint, or even fever—only 41% of affected patients in one case series were febrile.2 The workup is often time-consuming, invasive, and expensive.
Although delayed diagnosis and treatment of septic arthritis is associated with significant adverse effects, there is unfortunately no consensus to guide the workup for ISI. As opposed to Kocher’s criteria for the differentiation of septic hip arthritis from transient synovitis in pediatric patients or well-known red-flags for further evaluation of low back pain, physicians are left without much guidance when considering laboratory workup or imaging decisions to evaluate for ISI.
Sacroiliac Joint
As previously noted, the SIJ is not commonly affected by infection. It is a diarthrodial, L-shaped joint comprised of the posterior ilium and sacrum, and is a near-rigid structure with very limited movement that provides stability to the axial skeleton.5 The SIJ is often overlooked as a secondary cause of low back pain in younger patients with rheumatologic conditions (eg, ankylosing spondylitis, Reiter syndrome), pregnancy-associated ligamentous laxity, and osteoarthritis in elderly patients. In one study, 88.2% of sacroiliitis cases were inflammatory, 8.8% infectious, and 2.9% degenerative.6
Signs and Symptoms
As our case illustrates, ISI often presents with nonspecific symptoms and physical findings.7 Patients typically present with fever, painful manipulation of the SIJ, and unilateral lumbo-gluteal pain.2 The components of the history and physical examination suspicious for an infectious etiology include the subacute presentation; unresolved pain despite treatment; tenderness to palpation; decreased range of motion; and recent IV drug use, which increases the risk of infectious disease due to unsterile practices and direct inoculation of pathogens into the bloodstream8 and a further predilection into the axial skeleton. 9 It is important to obtain an accurate social history; however, patients may not be forthright about disclosing sensitive information such as sexual history and illicit drug use.
Physical Assessment
The SIJ is best appreciated in the seated patient by palpating one fingerbreadth medial to the posterior superior iliac spine as he or she slowly bends forward.10 Tenderness elicited while in this position is suggestive of SIJ inflammation. The area of tenderness may be lower than anticipated and lateral to the gluteal cleft, as synovial fluid is typically relegated to the lower half of the joint.
Several adjunctive physical examination maneuvers, such as the Gaenslen test and Flexion Abduction External Rotation test (FABER test or Patrick’s test) can isolate SIJ pathology or dysfunction. The Gaenslen test is performed by asking the patient to lie supine and flex the affected hip and knee, with the lumbar spine flat against the examination table. Hyperextending the contralateral thigh downward will reproduce pain in the affected SIJ.
The FABER test is a simple but less specific examination technique to assess joint pain in the hip, lumbar, and sacroiliac joints.11 In this assessment, the clinician flexes the patient’s affected knee to 90°, externally rotates the hip, and applies downward pressure on the knee. Pain reproduced in the affected SI region is sensitive for joint inflammation.
Laboratory and Imaging Studies
Laboratory studies typically show inconsistent and nonspecific findings, such as the elevated ESR and CRP levels seen in our patient.2,12 Imaging studies to assess the SIJ for signs of infection are therefore essential for confirming infection.
Magnetic resonance imaging is the preferred imaging modality to assess for ISI, since it has the highest sensitivity in visualizing joint effusion and bone marrow edema compared to other modalities. Computed tomography, however, can be helpful in visualizing associated abscesses and guiding arthrocentesis.12 Plain X-ray may not demonstrate early changes in bone.13 The confirmatory study for ISI is synovial fluid analysis and culture.7
Treatment
Infectious sacroiliitis secondary to P aeruginosa, a gram-negative bacillus, is difficult to treat because of the glycocalyx and slime production that protects the pathogen from antibiotics, the development of multiple-antimicrobial resistance, and poor drug penetration into bones and abscesses.14 Antibiotic treatment should cover Staphylococcus aureus and may be broadened to cover gram-negative bacilli. The recommended duration of treatment is at least a 2-week course of IV antibiotics, followed by a 6-week course of oral antibiotics.2 Therapy also includes pain control and surgical intervention for abscesses, osteomyelitis, and refractory cases.7
Complications
Complications and long-term sequelae are common in ISI, often due to late diagnosis of the condition. Our case illustrates the delayed diagnosis of Pseudomonas ISI with candidemia in a young man with a history of IV drug use presenting with atraumatic low back pain. His clinical course was complicated by a thromboembolic event, likely secondary to immobility and a hypercoagulable state from infection and inflammation.15 Infectious sacroiliitis secondary to P aeruginosa is most commonly seen in patients with immunosuppression, hospitalization, and IV drug use.2
Summary
Infectious sacroiliitis remains a diagnostic challenge for physicians due to its rare incidence and nonspecific clinical manifestations. Our case illustrates the importance of maintaining a high level of clinical suspicion for infectious arthritis in young patients presenting with common MSK complaints in the presence of infectious risk factors. Emergency physicians should consider red flags, abnormal vital signs, and patient recidivism when deciding on the most appropriate workup.
1. Mancarella L, De Santis M, Magarelli N, Ierardi AM, Bonomo L, Ferraccioli G. Septic sacroiliitis: an uncommon septic arthritis. Clin Exp Rheumatol. 2009;27(6):1004-1008.
2. Hermet M, Minichiello E, Flipo RM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC Infect Dis. 2012;12:305. doi:10.1186/1471-2334-12-305.
3. Abelson A. Septic Arthritis. Cleveland Clinic. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/rheumatology/septic-arthritis. Published August 2010. Accessed October 28, 2016.
4. Goldenberg DL. Septic arthritis. Lancet. 1998;351(9097):197-202. doi:10.1016/S0140-6736(97)09522-6.
5. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x.
6. Owlia MB, Danesh-Ardakani M. Frequency of sacroiliitis among patients with low back pain. Electron Physician. 2016;8(3):2094-2100. doi:10.19082/2094.
7. Zimmermann B 3rd, Mikolich DJ, Lally EV. Septic sacroiliitis. Semin Arthritis Rheum. 1996;26(3):592-604.
8. Brtalik D, Pariyadath M. A case report of infectious sacroiliitis in an adult presenting to the emergency department with inability to walk. J Emerg Med. 2017:52(3)e65-e68. doi:10.1016/j.jemermed.2016.10.022.
9. Ferraro K, Cohen MA. Acute septic sacroiliitis in an injection drug user. Am J Emerg Med. 2004;22(1):60-61.
10. Safran M, Botser IB. Hip anatomy and biomechanics. In: Miller MD, Thompson SR, eds. DeLee & Drez’s Orthopaedic Sports Medicine. Vol 2. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015:917-932.e1.
11. LeBlond RF, Brown DD, Suneja M, Szot JF. The spine, pelvic, and extremities. In: LeBlond RF, Brown DD, Suneja M, Szot JF. eds. DeGowin’s Diagnostic Examination. 10th ed. New York, NY: McGraw-Hill; 2015:508-576.
12. Scott KR, Rising KL, Conlon LW. Infectious sacroiliitis. J Emerg Med. 2014;47(3):83-84. doi:10.1016/j.jemermed.2014.05.001.
13. Cinar M, Sanal HT, Yilmaz S, et al. Radiological followup of the evolution of inflammatory process in sacroiliac joint with magnetic resonance imaging: a case with pyogenic sacroiliitis. Case Rep Rheumatol. 2012;2012:509136. doi:10.1155/2012/509136.
14. Calza L, Manfredi R, Marinacci G, Fortunato L, Chiodo F. Community-acquired Pseudomonas aeruginosa sacro-iliitis in a previously healthy patient. J Med Microbiol. 2002;51(7):620-622.
15. Levi M, Keller TT, van Gorp E, ten Cate H. Infection and inflammation and the coagulation system. Cardiovasc Res. 2003;60(1):26-39.
1. Mancarella L, De Santis M, Magarelli N, Ierardi AM, Bonomo L, Ferraccioli G. Septic sacroiliitis: an uncommon septic arthritis. Clin Exp Rheumatol. 2009;27(6):1004-1008.
2. Hermet M, Minichiello E, Flipo RM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC Infect Dis. 2012;12:305. doi:10.1186/1471-2334-12-305.
3. Abelson A. Septic Arthritis. Cleveland Clinic. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/rheumatology/septic-arthritis. Published August 2010. Accessed October 28, 2016.
4. Goldenberg DL. Septic arthritis. Lancet. 1998;351(9097):197-202. doi:10.1016/S0140-6736(97)09522-6.
5. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x.
6. Owlia MB, Danesh-Ardakani M. Frequency of sacroiliitis among patients with low back pain. Electron Physician. 2016;8(3):2094-2100. doi:10.19082/2094.
7. Zimmermann B 3rd, Mikolich DJ, Lally EV. Septic sacroiliitis. Semin Arthritis Rheum. 1996;26(3):592-604.
8. Brtalik D, Pariyadath M. A case report of infectious sacroiliitis in an adult presenting to the emergency department with inability to walk. J Emerg Med. 2017:52(3)e65-e68. doi:10.1016/j.jemermed.2016.10.022.
9. Ferraro K, Cohen MA. Acute septic sacroiliitis in an injection drug user. Am J Emerg Med. 2004;22(1):60-61.
10. Safran M, Botser IB. Hip anatomy and biomechanics. In: Miller MD, Thompson SR, eds. DeLee & Drez’s Orthopaedic Sports Medicine. Vol 2. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015:917-932.e1.
11. LeBlond RF, Brown DD, Suneja M, Szot JF. The spine, pelvic, and extremities. In: LeBlond RF, Brown DD, Suneja M, Szot JF. eds. DeGowin’s Diagnostic Examination. 10th ed. New York, NY: McGraw-Hill; 2015:508-576.
12. Scott KR, Rising KL, Conlon LW. Infectious sacroiliitis. J Emerg Med. 2014;47(3):83-84. doi:10.1016/j.jemermed.2014.05.001.
13. Cinar M, Sanal HT, Yilmaz S, et al. Radiological followup of the evolution of inflammatory process in sacroiliac joint with magnetic resonance imaging: a case with pyogenic sacroiliitis. Case Rep Rheumatol. 2012;2012:509136. doi:10.1155/2012/509136.
14. Calza L, Manfredi R, Marinacci G, Fortunato L, Chiodo F. Community-acquired Pseudomonas aeruginosa sacro-iliitis in a previously healthy patient. J Med Microbiol. 2002;51(7):620-622.
15. Levi M, Keller TT, van Gorp E, ten Cate H. Infection and inflammation and the coagulation system. Cardiovasc Res. 2003;60(1):26-39.
Prevention and treatment options for mTOR inhibitor-associated stomatitis
Mammalian target of rapamycin (mTOR), a serine–threonine protein kinase, operates in the phosphoinositide 3-kinase (PI3K)–protein kinase B (AKT)–mTOR signal transduction pathway regulating both normal and cancer cellular processes, including cell growth, proliferation, motility, survival, and protein and lipid synthesis.1 Genetic alterations affecting this pathway, including mutations in receptor tyrosine kinases PI3K and AKT, occur frequently in human cancers,2 supporting the rationale to develop drugs that target pathway components, such as mTOR inhibitors.
Two mTOR inhibitors are currently approved by the US Food and Drug Administration for cancer treatment: temsirolimus, for advanced renal cell carcinoma (RCC; approved 2007)3 and everolimus, for advanced RCC (approved 2009), advanced pancreatic neuroendocrine tumors (pNET; approved 2011), and hormone receptor-positive (HR-positive), human epidermal growth factor receptor-2 (HER2)-negative advanced breast cancer (approved 2012).4 Another mTOR inhibitor, sirolimus, is approved for use as an immunosuppressive agent and prophylactic against organ rejection after kidney transplant.5
Stomatitis, inflammation of the oral mucosa with contributing factors of genetic predisposition, nutritional deficiencies, infections, and immunological or hematologic dysfunction,6 occurs frequently as a side effect associated with mTOR inhibitor treatment.7-9 Left untreated or managed unsatisfactorily, mTOR inhibitor-associated stomatitis (mIAS) may cause patients discomfort and trouble with maintaining adequate nutritional intake and proper oral hygiene, as well as strict adherence to cancer treatment. It is therefore important for health care providers of cancer patients receiving mTOR inhibitor treatment to be knowledgeable about this side effect. The purpose of the present systematic review of published literature is to provide a better understanding of the differential diagnosis of mIAS, the pathophysiology of mIAS, preventive strategies for patients initiating mTOR inhibitor treatment, and treatment options available to manage mIAS.
Method
The PubMed database was searched with the terms mTOR inhibitor and stomatitis (no date restriction); 79 articles were retrieved, and all abstracts were reviewed to select those relevant to the aims of this review article. To understand future directions for management and prevention of mIAS, a search of clinicaltrials.gov was performed with the terms temsirolimus everolimus stomatitis yielding 12 clinical trials, of which 4 were excluded: 1 trial was terminated due to slow accrual, the status of 1 trial had not been verified in >2 years, and 2 studies focused on efficacy outcomes. A search of the American Society of Clinical Oncology (ASCO) meeting abstracts database was performed to assess the availability of clinical trial data; the search was limited to 2011-2016 and terms were stomatitis in the title and mTOR in the abstract or title. Seven abstracts were retrieved; 2 discussed stomatitis prevention (1 as a “trial-in-progress” and 1 presented results of the trial); the other 5 abstracts presented meta-analyses or reviews of previous clinical studies to assess the risk, incidence, management, and resolution of mIAS.
Review findings
Incidence of mIAS in patients treated for cancer
Two recent meta-analyses quantified the rate of mIAS in patients receiving mTOR inhibitors. Shameem and colleagues10 identified 9 randomized studies of everolimus (8 phase 3, 1 phase 2) and 2 of temsirolimus (1 each phase 2 and 3) involving a total of 4752 patients with a variety of tumor types including angiomyolipoma, breast, gastric, giant cell astrocytoma, pNET, and RCC. Patients received everolimus monotherapy (n = 1,075) or in combination with exemestane (n = 485), tamoxifen (n = 54), letrozole (n = 137), or octreotide (n = 216). Temsirolimus was administered as monotherapy (n = 208) or in combination with interferon
(n = 210) or letrozole (n = 550). The incidence of all-grade stomatitis in the 11 studies ranged from 11%-63%, and the overall incidence of any grade stomatitis was 33.5% (95% confidence interval [CI], 21.9%-47.6%). The concurrent use of a second agent may have confounded these findings because, for example, stomatitis has been reported in pooled analyses and in postmarketing experience with letrozole.11
Rugo and colleagues12 evaluated the incidence of stomatitis in 1455 patients participating in 5 phase 3 randomized clinical trials of everolimus in breast cancer, carcinoid tumor, pNET, and RCC. Patients received everolimus monotherapy
(n = 478) or in combination with exemestane (n = 482), trastuzumab plus vinorelbine (n = 280), or octreotide
(n = 215). The incidence of stomatitis in patients receiving everolimus was 59%-71%, compared with 19%-29% in 1,071 patients of the comparator arms (placebo, and placebo–trastuzumab–vinorelbine). The overall incidence of any grade stomatitis was 67%; most events were mild (grade 1/2); 9% of stomatitis events were moderate to severe (grade 3/4).
Differential clinical presentation of mIAS and severity
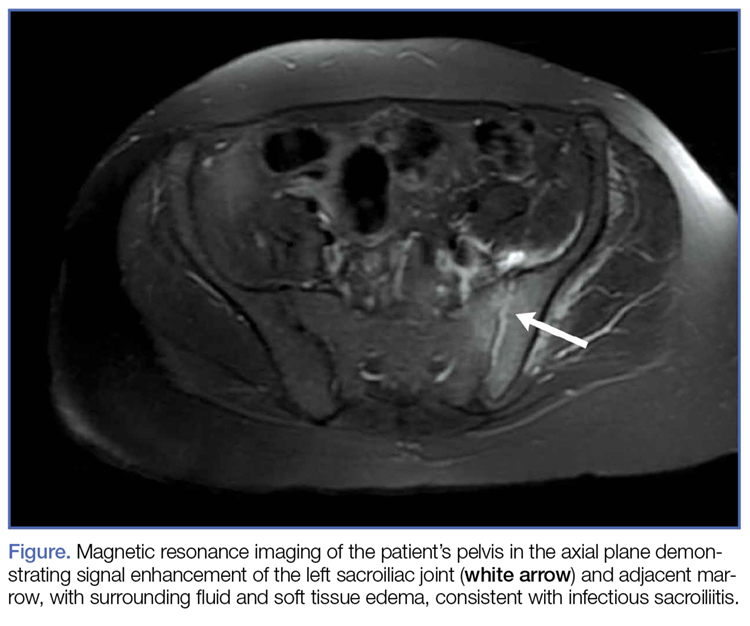
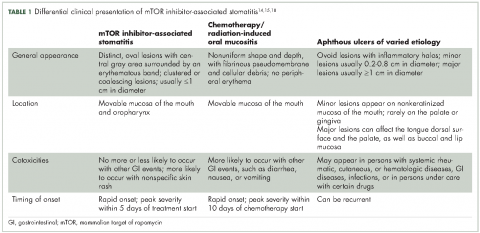
Oral mucositis is a common significant adverse event (AE) that occurs in patients with cancer who receive standard chemotherapy regimens and/or radiation therapy,13 so it is important to recognize that the clinical presentation of mIAS differs from that of oral mucositis (Table 1, Figure 14,15).16 mIAS shares some similarities with aphthous ulcers (also referred to as canker sores), a common oral condition with varied causes related to systemic disorders, gastrointestinal disorders, and infections, among others .17 In general, mIAS ulcers develop with a median onset of 10 days (range, 4-25 days) after initiation of mTOR inhibitor treatment and resolve in about 1-3 weeks after dose interruption/reduction of everolimus.16,18,19 mIAS ulcers appear as distinct, oval lesions with a central gray area surrounded by peripheral erythema. They are usually localized to the movable mucosa of the mouth and oropharynx. Although mIAS lesions are usually small, they are quite painful and may cluster.
Differential diagnosis of mIAS should be made based on physical examination and medical history, with consideration given to appearance of lesions (number, size, and location), current infection status, and current medications. Specific diagnostic testing should be conducted to confirm a coexisting or alternative cause of oral lesions.17
Although there are many different scales for grading mIAS severity, the most commonly used are the National Cancer Institute Common Terminology Criteria for Adverse Events (based on patient function, symptoms, and intervention needs) and the World Health Organization oral mucositis scales (based on symptoms, clinical presentation, and interference with patient function).20-22 These scales distinguish between mild lesions (grade 1/2) and moderate to severe lesions (grade 3/4) that cause significant pain or interfere with oral intake.
Pathophysiology of mIAS
The pathophysiology mIAS is incompletely understood. The ubiquitous role of the PI3K-AKT-mTOR pathway in regulating broad cellular functions suggests that mTOR inhibition is likely to have wide-ranging effects on many biological processes. It is not known whether disruption of one or more processes – or upsetting the balance of mTOR activities – underlies the formation of mIAS.
Differences between mIAS and oral mucositis, including clinical presentation and concomitant toxicities,16,23 suggest that the two types of oral lesions are fundamentally distinct. This distinction is supported by animal studies in which mTOR inhibition was found to almost completely prevent the appearance of oral mucositis in irradiated mice. The protective effect of mTOR inhibition is mediated through suppression of oxidative stress generated by radiation therapy.24
Although mIAS and recurrent aphthous ulcers share some similarities, it is not clear whether they also share a common pathophysiology. Recent studies suggest that patients with recurrent aphthous ulcers have immune dysfunction that leads to excessive immune response to normally innocuous substrates in the oral mucosa.25 mTOR inhibition can have proinflammatory activity by promoting autophagy, a process that stimulates antigen presentation and activation of T cells that produce proinflammatory cytokines.26 It is interesting to note that the incidence of stomatitis in patients receiving sirolimus after kidney transplant is relatively low, 3%-20%.5 Sirolimus is administered in combination with other immunosuppressants, namely cyclosporine and corticosteroids, so it suggests that concomitant use of a steroid-based regimen may have a preventive or therapeutic effect. However, posttransplant sirolimus is typically administered at relatively low doses, which might account in part for the lower incidence of mIAS observed. Ongoing clinical studies of steroid-based mouthwashes in patients receiving everolimus should shed light on this.
Other study findings have shown that inhibition of the PI3K-AKT-mTOR signaling pathway affects skin wound healing,27,28 which raises the possibility that mIAS may stem from a diminished capacity to repair physical injuries to the oral mucosa. More research is needed to elucidate the pathophysiology of mIAS.
Preventive measures for patients initiating mTOR inhibitor treatment
There are preventive measures for mIAS that have not yet been backed up with evidence-based findings, although several clinical studies that are underway aim to address this gap (Table 2). The hypotheses about the pathophysiology of mIAS suggest that certain preventive and therapeutic interventions might be effective against mIAS. For example, two studies are evaluating the use of steroid-based mouthwashes in patients receiving everolimus, based on the hypothesis that mIAS may arise from an inflammatory process; another study will evaluate a mucoadhesive oral wound rinse, based on the hypothesis that wound protection might prevent mIAS. Glutamine suspension is also under evaluation as it is understood to have wound-preventative and tissue-repair properties, and another study is focused on dentist-guided oral management. Recent results of one of these trials (SWISH),29 reported that preventative care with a dexamethasone mouthwash 3-4 times a day significantly minimized or prevented the incidence of all grades of stomatitis in women receiving everolimus plus exemestane therapy for advanced/metastatic breast cancer compared with the incidence of stomatitis observed in a previously published phase 3 trial (BOLERO-2)30,31 of everolimus plus exemestane in the same patient population. Results from several other studies are expected soon.
Current approaches to mIAS prevention are based largely on clinical experience with chemotherapy- or radiation-induced oral mucositis (Table 3).13,32 Preventive measures use three main strategies: establish and maintain good routine oral care; modify diet to avoid potentially damaging foods; and improve patient education about mIAS. In regard to patient education, numerous studies have reported that establishing an institutional protocol for oral care helped reduce the incidence of chemotherapy- or radiation-induced oral mucositis.33-40 An ongoing clinical study that will randomize patients to receive oral care education from oral surgeons or instruction on brushing only (NCT02376985) is investigating whether having an oral care protocol holds for patients with mIAS. The hypothesis is that focusing attention on oral care and educating patients to recognize the onset of mIAS facilitates early detection and promotes early intervention.
Therapeutic measures for patients with mIAS
Therapeutic measures for mIAS are based largely on experience with chemotherapy- or radiation-induced oral mucositis or recurrent aphthous ulcers (Table 3) and vary in part by the severity of lesions. Treatments for mild mIAS aim to ameliorate symptoms (eg, topical analgesics for pain), protect the oral mucosa (eg, mucoadhesive gels or viscous solutions that coat the oral cavity), prevent potential sequelae (eg, prophylactic antibiotics to avoid secondary infections), and reduce inflammation/immune response (eg, steroid-based mouth rinses, topical steroids, or topical anti-inflammatory agents). Treatments for mild mIAS are generally local rather than systemic.
Treatment options for moderate to severe mIAS include systemic approaches that generally carry increased risk of AEs and, therefore, should be reserved for patients with multiple lesions, uncontrolled or poorly controlled pain, or greatly diminished oral food intake (Table 3).41 When mIAS cannot be controlled with the interventions described, the dose of the mTOR inhibitor can be reduced with the recognition that dose modification of anticancer therapy may affect disease outcomes.29 The experience of reduction or interruption of treatment with everolimus in the BOLERO-2 trial as a strategy for management of AEs is discussed in a recent review.29 Prescribing information for both temsirolimus and everolimus specify that grade 3 AEs be treated with temporary dose interruption, and with resolution (temsirolimus: grade ≤2; everolimus: grade ≤1), treatment may be resumed at lower doses (temsirolimus: reduce by 5 mg/week; no lower than 15 mg/week; everolimus: reduce by half the previously administered dose).3,4 Grade 4 events due to treatment with temsirolimus may also be treated with dose interruption/reduction; the everolimus prescribing information advises treatment discontinuation for grade 4 stomatitis.
Summary and discussion
mTOR inhibitors can be effective treatments for patients with advanced cancer, specifically for advanced RCC, advanced pNET, and HR+, HER2-negative advanced breast cancer. Although mIAS may occur in many patients, it is usually grade 1 or 2 in severity. mIAS has an early onset, usually within the first 2 weeks of treatment16,19,42 and a relatively rapid resolution, usually within 3 weeks.16,19 Thus, most cases of mIAS are self-limiting.
The relatively recent emergence of mIAS poses short-term challenges regarding diagnosis, assessment, prevention, and treatment. Several clinical studies are underway to evaluate a range of interventions for their preventive and therapeutic efficacy in mIAS. Furthermore, our growing understanding of the underlying pathophysiology of mIAS can guide how mIAS is managed and what interventions patients receive.
Although mIAS is believed to differ from chemotherapy- or radiation-induced oral mucositis and aphthous ulcers, much can be learned from the treatment of both of these. Several strategies have been proposed to limit the occurrence of mIAS (Table 3). First, establish an oral care protocol. Educate patients who are initiating treatment with an mTOR inhibitor on implementation of the oral care protocol and emphasize adherence. Second, educate patients on the symptoms and timing of mIAS. Patients may hesitate to report mild symptoms or assume they are innocuous, so be clear that reporting all symptoms is important to allow timely clinical evaluation. Early recognition of mIAS facilitates early intervention and can prevent dose modification and interruption. Third, implement the preventive and treatment measures described. Many of the preventive measures can be incorporated into an oral care protocol.
The advent of mTOR inhibitors has clinically benefited many patients with cancer. Although side effects, like mIAS, may develop during treatment, they should not be considered insurmountable. Through education, vigilance, and aggressive management, health care providers and patients can work together to help patients maintain their quality of life while continuing to optimally address their disease.
Acknowledgment
The authors thank Anna Lau, PhD, and Patricia Segarini, PhD, of Percolation Communications LLC, for their editorial assistance. Funding for manuscript development was provided by Novartis Pharmaceuticals Corp.
1. Lauring J, Park BH, Wolff AC. The phosphoinositide-3-kinase-Akt-mTOR pathway as a therapeutic target in breast cancer. J Natl Compr Canc Netw. 2013;11:670-678.
2. Fruman DA, Rommel C. PI3K and cancer: lessons, challenges and opportunities. Nat Rev Drug Discov. 2014;13:140-156.
3. Torisel (temsirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2014.
4. Afinitor (everolimus) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
5. Rapamune (sirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2012.
6. Peterson DE, Boers-Doets CB, Bensadoun RJ, Herrstedt J, ESMO Guidelines Committee. Management of oral and gastrointestinal mucosal injury: ESMO Clinical Practice Guidelines for diagnosis, treatment, and follow-up. Ann Oncol. 2015;26 Suppl 5:v139-151.
7. Hidalgo M, Buckner JC, Erlichman C, et al. A phase I and pharmacokinetic study of temsirolimus (CCI-779) administered intravenously daily for 5 days every 2 weeks to patients with advanced cancer. Clin Cancer Res. 2006;12:5755-5763.
8. Martins F, de Oliveira MA, Wang Q, et al. A review of oral toxicity associated with mTOR inhibitor therapy in cancer patients. Oral Oncol. 2013;49:293-298.
9. O’Donnell A, Faivre S, Burris HA, 3rd, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol. 2008;26:1588-1595.
10. Shameem R, Lacouture M, Wu S. Incidence and risk of high-grade stomatitis with mTOR inhibitors in cancer patients. Cancer Invest. 2015;33:70-77.
11. Femara (letrozole) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2014.
12. Rugo HS, Hortobagyi GN, Yao J, et al. Meta-analysis of stomatitis in clinical studies of everolimus: incidence and relationship with efficacy. Ann Oncol. 2016;27:519-525.
13. Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109:820-831.
14. Sonis S, Treister N, Chawla S, Demetri G, Haluska F. Preliminary characterization of oral lesions associated with inhibitors of mammalian target of rapamycin in cancer patients. Cancer. 2010;116:210-215.
15. Scully C. Clinical practice. Aphthous ulceration. N Engl J Med. 2006;355:165-172.
16. Ferte C, Paci A, Zizi M, et al. Natural history, management and pharmacokinetics of everolimus-induced-oral ulcers: insights into compliance issues. Eur J Cancer. 2011;47:2249-2255.
17. Wong HM. Oral complications and management strategies for patients undergoing cancer therapy ScienceWorldJournal. 2014;581795.
18. de Oliveira MA, Martins EMF, Wang Q, et al. Clinical presentation and management of mTOR inhibitor-associated stomatitis. Oral Oncol. 2011;47:998-1003.
19. Rugo HS, Pritchard KI, Gnant M, et al. Incidence and time course of everolimus-related adverse events in postmenopausal women with hormone receptor-positive advanced breast cancer: insights from BOLERO-2. Ann Oncol. 2014;25:808-815.
20. National Cancer Institute. Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events v3.0 (CTCAE). http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed February 13, 2017.
21. National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v4.03. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed February 13, 2017.
22. World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment. Geneva, Switzerland: World Health Organization (WHO Offset Publication No. 48); 1979.
23. Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin. 2012;62:400-422.
24. Iglesias-Bartolome R, Patel V, Cotrim A, et al. mTOR inhibition prevents epithelial stem cell senescence and protects from radiation-induced mucositis. Cell Stem Cell. 2012;11:401-414.
25. Lewkowicz N, Lewkowicz P, Dzitko K, et al. Dysfunction of CD4+CD25high T regulatory cells in patients with recurrent aphthous stomatitis. J Oral Pathol Med. 2008;37:454-461.
26. Levine B, Deretic V. Unveiling the roles of autophagy in innate and adaptive immunity. Nat Rev Immunol. 2007;7:767-777.
27. Jin Y, Tymen SD, Chen D, et al. MicroRNA-99 family targets AKT/mTOR signaling pathway in dermal wound healing. PLoS One. 2013;8:e64434.
28. Rosselli-Murai LK, Almeida LO, Zagni C, et al. Periostin responds to mechanical stress and tension by activating the MTOR signaling pathway. PLoS One. 2013;8:e83580.
29. Rugo HS. Dosing and safety implications for oncologists when administering everolimus to patients with hormone receptor-positive breast cancer. Clin Breast Cancer. 2016;16:18-22.
30. Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520-529.
31. Yardley DA, Noguchi S, Pritchard KI, et al. Everolimus plus exemestane in postmenopausal patients with HR(+) breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30:870-884.
32. Rubenstein EB, Peterson DE, Schubert M, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004;100:2026-2046.
33. Borowski B, Benhamou E, Pico JL, Laplanche A, Margainaud JP, Hayat M. Prevention of oral mucositis in patients treated with high-dose chemotherapy and bone marrow transplantation: a randomised controlled trial comparing two protocols of dental care. Eur J Cancer B Oral Oncol. 1994;30B:93-97.
34. Cheng KK, Molassiotis A, Chang AM, Wai WC, Cheung SS. Evaluation of an oral care protocol intervention in the prevention of chemotherapy-induced oral mucositis in paediatric cancer patients. Eur J Cancer. 2001;37:2056-2063.
35. Dudjak LA. Mouth care for mucositis due to radiation therapy. Cancer Nurs. 1987;10:131-140.
36. Graham KM, Pecoraro DA, Ventura M, Meyer CC. Reducing the incidence of stomatitis using a quality assessment and improvement approach. Cancer Nurs. 1993;16:117-122.
37. Kenny SA. Effect of two oral care protocols on the incidence of stomatitis in hematology patients. Cancer Nurs. 1990;13:345-353.
38. Larson PJ, Miaskowski C, MacPhail L, et al. The PRO-SELF Mouth Aware program: an effective approach for reducing chemotherapy-induced mucositis. Cancer Nurs. 1998;21:263-268.
39. Levy-Polack MP, Sebelli P, Polack NL. Incidence of oral complications and application of a preventive protocol in children with acute leukemia. Spec Care Dentist. 1998;18:189-193.
40. Yeager KA, Webster J, Crain M, Kasow J, McGuire DB. Implementation of an oral care standard for leukemia and transplantation patients. Cancer Nurs. 2000;23:40-47; quiz 47-48.
41. Pilotte AP, Hohos MB, Polson KM, Huftalen TM, Treister N. Managing stomatitis in patients treated with mammalian target of rapamycin inhibitors. Clin J Oncol Nurs. 2011;15:E83-89.
42. Gomez-Fernandez C, Garden BC, Wu S, Feldman DR, Lacouture ME. The risk of skin rash and stomatitis with the mammalian target of rapamycin inhibitor temsirolimus: a systematic review of the literature and meta-analysis. Eur J Cancer. 2012;48:340-346.
43. Bonnaure-Mallet M, Bunetel L, Tricot-Doleux S, Guerin J, Bergeron C, LeGall E. Oral complications during treatment of malignant diseases in childhood: effects of tooth brushing. Eur J Cancer. 1998;34:1588-1591.
44. Chuang P, Langone AJ. Clobetasol ameliorates aphthous ulceration in renal transplant patients on sirolimus. Am J Transplant. 2007;7:714-717.
45. Femiano F, Buonaiuto C, Gombos F, Lanza A, Cirillo N. Pilot study on recurrent aphthous stomatitis (RAS): a randomized placebo-controlled trial for the comparative therapeutic effects of systemic prednisone and systemic montelukast in subjects unresponsive to topical therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:402-407.
Mammalian target of rapamycin (mTOR), a serine–threonine protein kinase, operates in the phosphoinositide 3-kinase (PI3K)–protein kinase B (AKT)–mTOR signal transduction pathway regulating both normal and cancer cellular processes, including cell growth, proliferation, motility, survival, and protein and lipid synthesis.1 Genetic alterations affecting this pathway, including mutations in receptor tyrosine kinases PI3K and AKT, occur frequently in human cancers,2 supporting the rationale to develop drugs that target pathway components, such as mTOR inhibitors.
Two mTOR inhibitors are currently approved by the US Food and Drug Administration for cancer treatment: temsirolimus, for advanced renal cell carcinoma (RCC; approved 2007)3 and everolimus, for advanced RCC (approved 2009), advanced pancreatic neuroendocrine tumors (pNET; approved 2011), and hormone receptor-positive (HR-positive), human epidermal growth factor receptor-2 (HER2)-negative advanced breast cancer (approved 2012).4 Another mTOR inhibitor, sirolimus, is approved for use as an immunosuppressive agent and prophylactic against organ rejection after kidney transplant.5
Stomatitis, inflammation of the oral mucosa with contributing factors of genetic predisposition, nutritional deficiencies, infections, and immunological or hematologic dysfunction,6 occurs frequently as a side effect associated with mTOR inhibitor treatment.7-9 Left untreated or managed unsatisfactorily, mTOR inhibitor-associated stomatitis (mIAS) may cause patients discomfort and trouble with maintaining adequate nutritional intake and proper oral hygiene, as well as strict adherence to cancer treatment. It is therefore important for health care providers of cancer patients receiving mTOR inhibitor treatment to be knowledgeable about this side effect. The purpose of the present systematic review of published literature is to provide a better understanding of the differential diagnosis of mIAS, the pathophysiology of mIAS, preventive strategies for patients initiating mTOR inhibitor treatment, and treatment options available to manage mIAS.
Method
The PubMed database was searched with the terms mTOR inhibitor and stomatitis (no date restriction); 79 articles were retrieved, and all abstracts were reviewed to select those relevant to the aims of this review article. To understand future directions for management and prevention of mIAS, a search of clinicaltrials.gov was performed with the terms temsirolimus everolimus stomatitis yielding 12 clinical trials, of which 4 were excluded: 1 trial was terminated due to slow accrual, the status of 1 trial had not been verified in >2 years, and 2 studies focused on efficacy outcomes. A search of the American Society of Clinical Oncology (ASCO) meeting abstracts database was performed to assess the availability of clinical trial data; the search was limited to 2011-2016 and terms were stomatitis in the title and mTOR in the abstract or title. Seven abstracts were retrieved; 2 discussed stomatitis prevention (1 as a “trial-in-progress” and 1 presented results of the trial); the other 5 abstracts presented meta-analyses or reviews of previous clinical studies to assess the risk, incidence, management, and resolution of mIAS.
Review findings
Incidence of mIAS in patients treated for cancer
Two recent meta-analyses quantified the rate of mIAS in patients receiving mTOR inhibitors. Shameem and colleagues10 identified 9 randomized studies of everolimus (8 phase 3, 1 phase 2) and 2 of temsirolimus (1 each phase 2 and 3) involving a total of 4752 patients with a variety of tumor types including angiomyolipoma, breast, gastric, giant cell astrocytoma, pNET, and RCC. Patients received everolimus monotherapy (n = 1,075) or in combination with exemestane (n = 485), tamoxifen (n = 54), letrozole (n = 137), or octreotide (n = 216). Temsirolimus was administered as monotherapy (n = 208) or in combination with interferon
(n = 210) or letrozole (n = 550). The incidence of all-grade stomatitis in the 11 studies ranged from 11%-63%, and the overall incidence of any grade stomatitis was 33.5% (95% confidence interval [CI], 21.9%-47.6%). The concurrent use of a second agent may have confounded these findings because, for example, stomatitis has been reported in pooled analyses and in postmarketing experience with letrozole.11
Rugo and colleagues12 evaluated the incidence of stomatitis in 1455 patients participating in 5 phase 3 randomized clinical trials of everolimus in breast cancer, carcinoid tumor, pNET, and RCC. Patients received everolimus monotherapy
(n = 478) or in combination with exemestane (n = 482), trastuzumab plus vinorelbine (n = 280), or octreotide
(n = 215). The incidence of stomatitis in patients receiving everolimus was 59%-71%, compared with 19%-29% in 1,071 patients of the comparator arms (placebo, and placebo–trastuzumab–vinorelbine). The overall incidence of any grade stomatitis was 67%; most events were mild (grade 1/2); 9% of stomatitis events were moderate to severe (grade 3/4).
Differential clinical presentation of mIAS and severity
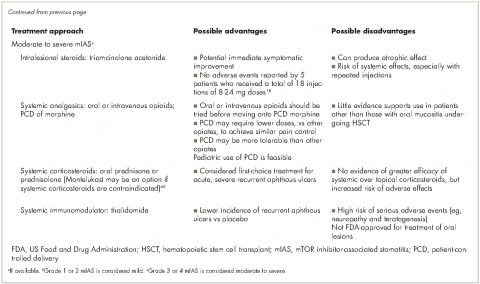
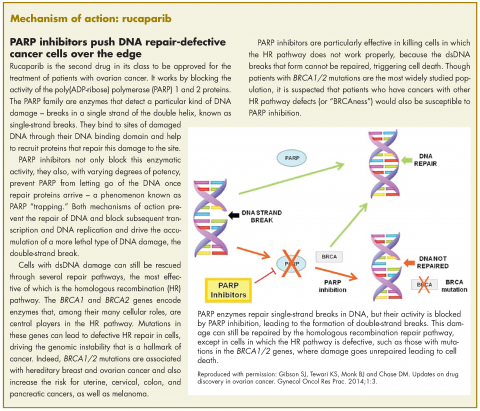
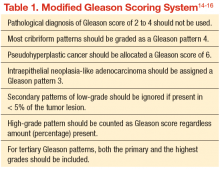
Oral mucositis is a common significant adverse event (AE) that occurs in patients with cancer who receive standard chemotherapy regimens and/or radiation therapy,13 so it is important to recognize that the clinical presentation of mIAS differs from that of oral mucositis (Table 1, Figure 14,15).16 mIAS shares some similarities with aphthous ulcers (also referred to as canker sores), a common oral condition with varied causes related to systemic disorders, gastrointestinal disorders, and infections, among others .17 In general, mIAS ulcers develop with a median onset of 10 days (range, 4-25 days) after initiation of mTOR inhibitor treatment and resolve in about 1-3 weeks after dose interruption/reduction of everolimus.16,18,19 mIAS ulcers appear as distinct, oval lesions with a central gray area surrounded by peripheral erythema. They are usually localized to the movable mucosa of the mouth and oropharynx. Although mIAS lesions are usually small, they are quite painful and may cluster.
Differential diagnosis of mIAS should be made based on physical examination and medical history, with consideration given to appearance of lesions (number, size, and location), current infection status, and current medications. Specific diagnostic testing should be conducted to confirm a coexisting or alternative cause of oral lesions.17
Although there are many different scales for grading mIAS severity, the most commonly used are the National Cancer Institute Common Terminology Criteria for Adverse Events (based on patient function, symptoms, and intervention needs) and the World Health Organization oral mucositis scales (based on symptoms, clinical presentation, and interference with patient function).20-22 These scales distinguish between mild lesions (grade 1/2) and moderate to severe lesions (grade 3/4) that cause significant pain or interfere with oral intake.
Pathophysiology of mIAS
The pathophysiology mIAS is incompletely understood. The ubiquitous role of the PI3K-AKT-mTOR pathway in regulating broad cellular functions suggests that mTOR inhibition is likely to have wide-ranging effects on many biological processes. It is not known whether disruption of one or more processes – or upsetting the balance of mTOR activities – underlies the formation of mIAS.
Differences between mIAS and oral mucositis, including clinical presentation and concomitant toxicities,16,23 suggest that the two types of oral lesions are fundamentally distinct. This distinction is supported by animal studies in which mTOR inhibition was found to almost completely prevent the appearance of oral mucositis in irradiated mice. The protective effect of mTOR inhibition is mediated through suppression of oxidative stress generated by radiation therapy.24
Although mIAS and recurrent aphthous ulcers share some similarities, it is not clear whether they also share a common pathophysiology. Recent studies suggest that patients with recurrent aphthous ulcers have immune dysfunction that leads to excessive immune response to normally innocuous substrates in the oral mucosa.25 mTOR inhibition can have proinflammatory activity by promoting autophagy, a process that stimulates antigen presentation and activation of T cells that produce proinflammatory cytokines.26 It is interesting to note that the incidence of stomatitis in patients receiving sirolimus after kidney transplant is relatively low, 3%-20%.5 Sirolimus is administered in combination with other immunosuppressants, namely cyclosporine and corticosteroids, so it suggests that concomitant use of a steroid-based regimen may have a preventive or therapeutic effect. However, posttransplant sirolimus is typically administered at relatively low doses, which might account in part for the lower incidence of mIAS observed. Ongoing clinical studies of steroid-based mouthwashes in patients receiving everolimus should shed light on this.
Other study findings have shown that inhibition of the PI3K-AKT-mTOR signaling pathway affects skin wound healing,27,28 which raises the possibility that mIAS may stem from a diminished capacity to repair physical injuries to the oral mucosa. More research is needed to elucidate the pathophysiology of mIAS.
Preventive measures for patients initiating mTOR inhibitor treatment
There are preventive measures for mIAS that have not yet been backed up with evidence-based findings, although several clinical studies that are underway aim to address this gap (Table 2). The hypotheses about the pathophysiology of mIAS suggest that certain preventive and therapeutic interventions might be effective against mIAS. For example, two studies are evaluating the use of steroid-based mouthwashes in patients receiving everolimus, based on the hypothesis that mIAS may arise from an inflammatory process; another study will evaluate a mucoadhesive oral wound rinse, based on the hypothesis that wound protection might prevent mIAS. Glutamine suspension is also under evaluation as it is understood to have wound-preventative and tissue-repair properties, and another study is focused on dentist-guided oral management. Recent results of one of these trials (SWISH),29 reported that preventative care with a dexamethasone mouthwash 3-4 times a day significantly minimized or prevented the incidence of all grades of stomatitis in women receiving everolimus plus exemestane therapy for advanced/metastatic breast cancer compared with the incidence of stomatitis observed in a previously published phase 3 trial (BOLERO-2)30,31 of everolimus plus exemestane in the same patient population. Results from several other studies are expected soon.
Current approaches to mIAS prevention are based largely on clinical experience with chemotherapy- or radiation-induced oral mucositis (Table 3).13,32 Preventive measures use three main strategies: establish and maintain good routine oral care; modify diet to avoid potentially damaging foods; and improve patient education about mIAS. In regard to patient education, numerous studies have reported that establishing an institutional protocol for oral care helped reduce the incidence of chemotherapy- or radiation-induced oral mucositis.33-40 An ongoing clinical study that will randomize patients to receive oral care education from oral surgeons or instruction on brushing only (NCT02376985) is investigating whether having an oral care protocol holds for patients with mIAS. The hypothesis is that focusing attention on oral care and educating patients to recognize the onset of mIAS facilitates early detection and promotes early intervention.
Therapeutic measures for patients with mIAS
Therapeutic measures for mIAS are based largely on experience with chemotherapy- or radiation-induced oral mucositis or recurrent aphthous ulcers (Table 3) and vary in part by the severity of lesions. Treatments for mild mIAS aim to ameliorate symptoms (eg, topical analgesics for pain), protect the oral mucosa (eg, mucoadhesive gels or viscous solutions that coat the oral cavity), prevent potential sequelae (eg, prophylactic antibiotics to avoid secondary infections), and reduce inflammation/immune response (eg, steroid-based mouth rinses, topical steroids, or topical anti-inflammatory agents). Treatments for mild mIAS are generally local rather than systemic.
Treatment options for moderate to severe mIAS include systemic approaches that generally carry increased risk of AEs and, therefore, should be reserved for patients with multiple lesions, uncontrolled or poorly controlled pain, or greatly diminished oral food intake (Table 3).41 When mIAS cannot be controlled with the interventions described, the dose of the mTOR inhibitor can be reduced with the recognition that dose modification of anticancer therapy may affect disease outcomes.29 The experience of reduction or interruption of treatment with everolimus in the BOLERO-2 trial as a strategy for management of AEs is discussed in a recent review.29 Prescribing information for both temsirolimus and everolimus specify that grade 3 AEs be treated with temporary dose interruption, and with resolution (temsirolimus: grade ≤2; everolimus: grade ≤1), treatment may be resumed at lower doses (temsirolimus: reduce by 5 mg/week; no lower than 15 mg/week; everolimus: reduce by half the previously administered dose).3,4 Grade 4 events due to treatment with temsirolimus may also be treated with dose interruption/reduction; the everolimus prescribing information advises treatment discontinuation for grade 4 stomatitis.
Summary and discussion
mTOR inhibitors can be effective treatments for patients with advanced cancer, specifically for advanced RCC, advanced pNET, and HR+, HER2-negative advanced breast cancer. Although mIAS may occur in many patients, it is usually grade 1 or 2 in severity. mIAS has an early onset, usually within the first 2 weeks of treatment16,19,42 and a relatively rapid resolution, usually within 3 weeks.16,19 Thus, most cases of mIAS are self-limiting.
The relatively recent emergence of mIAS poses short-term challenges regarding diagnosis, assessment, prevention, and treatment. Several clinical studies are underway to evaluate a range of interventions for their preventive and therapeutic efficacy in mIAS. Furthermore, our growing understanding of the underlying pathophysiology of mIAS can guide how mIAS is managed and what interventions patients receive.
Although mIAS is believed to differ from chemotherapy- or radiation-induced oral mucositis and aphthous ulcers, much can be learned from the treatment of both of these. Several strategies have been proposed to limit the occurrence of mIAS (Table 3). First, establish an oral care protocol. Educate patients who are initiating treatment with an mTOR inhibitor on implementation of the oral care protocol and emphasize adherence. Second, educate patients on the symptoms and timing of mIAS. Patients may hesitate to report mild symptoms or assume they are innocuous, so be clear that reporting all symptoms is important to allow timely clinical evaluation. Early recognition of mIAS facilitates early intervention and can prevent dose modification and interruption. Third, implement the preventive and treatment measures described. Many of the preventive measures can be incorporated into an oral care protocol.
The advent of mTOR inhibitors has clinically benefited many patients with cancer. Although side effects, like mIAS, may develop during treatment, they should not be considered insurmountable. Through education, vigilance, and aggressive management, health care providers and patients can work together to help patients maintain their quality of life while continuing to optimally address their disease.
Acknowledgment
The authors thank Anna Lau, PhD, and Patricia Segarini, PhD, of Percolation Communications LLC, for their editorial assistance. Funding for manuscript development was provided by Novartis Pharmaceuticals Corp.
Mammalian target of rapamycin (mTOR), a serine–threonine protein kinase, operates in the phosphoinositide 3-kinase (PI3K)–protein kinase B (AKT)–mTOR signal transduction pathway regulating both normal and cancer cellular processes, including cell growth, proliferation, motility, survival, and protein and lipid synthesis.1 Genetic alterations affecting this pathway, including mutations in receptor tyrosine kinases PI3K and AKT, occur frequently in human cancers,2 supporting the rationale to develop drugs that target pathway components, such as mTOR inhibitors.
Two mTOR inhibitors are currently approved by the US Food and Drug Administration for cancer treatment: temsirolimus, for advanced renal cell carcinoma (RCC; approved 2007)3 and everolimus, for advanced RCC (approved 2009), advanced pancreatic neuroendocrine tumors (pNET; approved 2011), and hormone receptor-positive (HR-positive), human epidermal growth factor receptor-2 (HER2)-negative advanced breast cancer (approved 2012).4 Another mTOR inhibitor, sirolimus, is approved for use as an immunosuppressive agent and prophylactic against organ rejection after kidney transplant.5
Stomatitis, inflammation of the oral mucosa with contributing factors of genetic predisposition, nutritional deficiencies, infections, and immunological or hematologic dysfunction,6 occurs frequently as a side effect associated with mTOR inhibitor treatment.7-9 Left untreated or managed unsatisfactorily, mTOR inhibitor-associated stomatitis (mIAS) may cause patients discomfort and trouble with maintaining adequate nutritional intake and proper oral hygiene, as well as strict adherence to cancer treatment. It is therefore important for health care providers of cancer patients receiving mTOR inhibitor treatment to be knowledgeable about this side effect. The purpose of the present systematic review of published literature is to provide a better understanding of the differential diagnosis of mIAS, the pathophysiology of mIAS, preventive strategies for patients initiating mTOR inhibitor treatment, and treatment options available to manage mIAS.
Method
The PubMed database was searched with the terms mTOR inhibitor and stomatitis (no date restriction); 79 articles were retrieved, and all abstracts were reviewed to select those relevant to the aims of this review article. To understand future directions for management and prevention of mIAS, a search of clinicaltrials.gov was performed with the terms temsirolimus everolimus stomatitis yielding 12 clinical trials, of which 4 were excluded: 1 trial was terminated due to slow accrual, the status of 1 trial had not been verified in >2 years, and 2 studies focused on efficacy outcomes. A search of the American Society of Clinical Oncology (ASCO) meeting abstracts database was performed to assess the availability of clinical trial data; the search was limited to 2011-2016 and terms were stomatitis in the title and mTOR in the abstract or title. Seven abstracts were retrieved; 2 discussed stomatitis prevention (1 as a “trial-in-progress” and 1 presented results of the trial); the other 5 abstracts presented meta-analyses or reviews of previous clinical studies to assess the risk, incidence, management, and resolution of mIAS.
Review findings
Incidence of mIAS in patients treated for cancer
Two recent meta-analyses quantified the rate of mIAS in patients receiving mTOR inhibitors. Shameem and colleagues10 identified 9 randomized studies of everolimus (8 phase 3, 1 phase 2) and 2 of temsirolimus (1 each phase 2 and 3) involving a total of 4752 patients with a variety of tumor types including angiomyolipoma, breast, gastric, giant cell astrocytoma, pNET, and RCC. Patients received everolimus monotherapy (n = 1,075) or in combination with exemestane (n = 485), tamoxifen (n = 54), letrozole (n = 137), or octreotide (n = 216). Temsirolimus was administered as monotherapy (n = 208) or in combination with interferon
(n = 210) or letrozole (n = 550). The incidence of all-grade stomatitis in the 11 studies ranged from 11%-63%, and the overall incidence of any grade stomatitis was 33.5% (95% confidence interval [CI], 21.9%-47.6%). The concurrent use of a second agent may have confounded these findings because, for example, stomatitis has been reported in pooled analyses and in postmarketing experience with letrozole.11
Rugo and colleagues12 evaluated the incidence of stomatitis in 1455 patients participating in 5 phase 3 randomized clinical trials of everolimus in breast cancer, carcinoid tumor, pNET, and RCC. Patients received everolimus monotherapy
(n = 478) or in combination with exemestane (n = 482), trastuzumab plus vinorelbine (n = 280), or octreotide
(n = 215). The incidence of stomatitis in patients receiving everolimus was 59%-71%, compared with 19%-29% in 1,071 patients of the comparator arms (placebo, and placebo–trastuzumab–vinorelbine). The overall incidence of any grade stomatitis was 67%; most events were mild (grade 1/2); 9% of stomatitis events were moderate to severe (grade 3/4).
Differential clinical presentation of mIAS and severity
Oral mucositis is a common significant adverse event (AE) that occurs in patients with cancer who receive standard chemotherapy regimens and/or radiation therapy,13 so it is important to recognize that the clinical presentation of mIAS differs from that of oral mucositis (Table 1, Figure 14,15).16 mIAS shares some similarities with aphthous ulcers (also referred to as canker sores), a common oral condition with varied causes related to systemic disorders, gastrointestinal disorders, and infections, among others .17 In general, mIAS ulcers develop with a median onset of 10 days (range, 4-25 days) after initiation of mTOR inhibitor treatment and resolve in about 1-3 weeks after dose interruption/reduction of everolimus.16,18,19 mIAS ulcers appear as distinct, oval lesions with a central gray area surrounded by peripheral erythema. They are usually localized to the movable mucosa of the mouth and oropharynx. Although mIAS lesions are usually small, they are quite painful and may cluster.
Differential diagnosis of mIAS should be made based on physical examination and medical history, with consideration given to appearance of lesions (number, size, and location), current infection status, and current medications. Specific diagnostic testing should be conducted to confirm a coexisting or alternative cause of oral lesions.17
Although there are many different scales for grading mIAS severity, the most commonly used are the National Cancer Institute Common Terminology Criteria for Adverse Events (based on patient function, symptoms, and intervention needs) and the World Health Organization oral mucositis scales (based on symptoms, clinical presentation, and interference with patient function).20-22 These scales distinguish between mild lesions (grade 1/2) and moderate to severe lesions (grade 3/4) that cause significant pain or interfere with oral intake.
Pathophysiology of mIAS
The pathophysiology mIAS is incompletely understood. The ubiquitous role of the PI3K-AKT-mTOR pathway in regulating broad cellular functions suggests that mTOR inhibition is likely to have wide-ranging effects on many biological processes. It is not known whether disruption of one or more processes – or upsetting the balance of mTOR activities – underlies the formation of mIAS.
Differences between mIAS and oral mucositis, including clinical presentation and concomitant toxicities,16,23 suggest that the two types of oral lesions are fundamentally distinct. This distinction is supported by animal studies in which mTOR inhibition was found to almost completely prevent the appearance of oral mucositis in irradiated mice. The protective effect of mTOR inhibition is mediated through suppression of oxidative stress generated by radiation therapy.24
Although mIAS and recurrent aphthous ulcers share some similarities, it is not clear whether they also share a common pathophysiology. Recent studies suggest that patients with recurrent aphthous ulcers have immune dysfunction that leads to excessive immune response to normally innocuous substrates in the oral mucosa.25 mTOR inhibition can have proinflammatory activity by promoting autophagy, a process that stimulates antigen presentation and activation of T cells that produce proinflammatory cytokines.26 It is interesting to note that the incidence of stomatitis in patients receiving sirolimus after kidney transplant is relatively low, 3%-20%.5 Sirolimus is administered in combination with other immunosuppressants, namely cyclosporine and corticosteroids, so it suggests that concomitant use of a steroid-based regimen may have a preventive or therapeutic effect. However, posttransplant sirolimus is typically administered at relatively low doses, which might account in part for the lower incidence of mIAS observed. Ongoing clinical studies of steroid-based mouthwashes in patients receiving everolimus should shed light on this.
Other study findings have shown that inhibition of the PI3K-AKT-mTOR signaling pathway affects skin wound healing,27,28 which raises the possibility that mIAS may stem from a diminished capacity to repair physical injuries to the oral mucosa. More research is needed to elucidate the pathophysiology of mIAS.
Preventive measures for patients initiating mTOR inhibitor treatment
There are preventive measures for mIAS that have not yet been backed up with evidence-based findings, although several clinical studies that are underway aim to address this gap (Table 2). The hypotheses about the pathophysiology of mIAS suggest that certain preventive and therapeutic interventions might be effective against mIAS. For example, two studies are evaluating the use of steroid-based mouthwashes in patients receiving everolimus, based on the hypothesis that mIAS may arise from an inflammatory process; another study will evaluate a mucoadhesive oral wound rinse, based on the hypothesis that wound protection might prevent mIAS. Glutamine suspension is also under evaluation as it is understood to have wound-preventative and tissue-repair properties, and another study is focused on dentist-guided oral management. Recent results of one of these trials (SWISH),29 reported that preventative care with a dexamethasone mouthwash 3-4 times a day significantly minimized or prevented the incidence of all grades of stomatitis in women receiving everolimus plus exemestane therapy for advanced/metastatic breast cancer compared with the incidence of stomatitis observed in a previously published phase 3 trial (BOLERO-2)30,31 of everolimus plus exemestane in the same patient population. Results from several other studies are expected soon.
Current approaches to mIAS prevention are based largely on clinical experience with chemotherapy- or radiation-induced oral mucositis (Table 3).13,32 Preventive measures use three main strategies: establish and maintain good routine oral care; modify diet to avoid potentially damaging foods; and improve patient education about mIAS. In regard to patient education, numerous studies have reported that establishing an institutional protocol for oral care helped reduce the incidence of chemotherapy- or radiation-induced oral mucositis.33-40 An ongoing clinical study that will randomize patients to receive oral care education from oral surgeons or instruction on brushing only (NCT02376985) is investigating whether having an oral care protocol holds for patients with mIAS. The hypothesis is that focusing attention on oral care and educating patients to recognize the onset of mIAS facilitates early detection and promotes early intervention.
Therapeutic measures for patients with mIAS
Therapeutic measures for mIAS are based largely on experience with chemotherapy- or radiation-induced oral mucositis or recurrent aphthous ulcers (Table 3) and vary in part by the severity of lesions. Treatments for mild mIAS aim to ameliorate symptoms (eg, topical analgesics for pain), protect the oral mucosa (eg, mucoadhesive gels or viscous solutions that coat the oral cavity), prevent potential sequelae (eg, prophylactic antibiotics to avoid secondary infections), and reduce inflammation/immune response (eg, steroid-based mouth rinses, topical steroids, or topical anti-inflammatory agents). Treatments for mild mIAS are generally local rather than systemic.
Treatment options for moderate to severe mIAS include systemic approaches that generally carry increased risk of AEs and, therefore, should be reserved for patients with multiple lesions, uncontrolled or poorly controlled pain, or greatly diminished oral food intake (Table 3).41 When mIAS cannot be controlled with the interventions described, the dose of the mTOR inhibitor can be reduced with the recognition that dose modification of anticancer therapy may affect disease outcomes.29 The experience of reduction or interruption of treatment with everolimus in the BOLERO-2 trial as a strategy for management of AEs is discussed in a recent review.29 Prescribing information for both temsirolimus and everolimus specify that grade 3 AEs be treated with temporary dose interruption, and with resolution (temsirolimus: grade ≤2; everolimus: grade ≤1), treatment may be resumed at lower doses (temsirolimus: reduce by 5 mg/week; no lower than 15 mg/week; everolimus: reduce by half the previously administered dose).3,4 Grade 4 events due to treatment with temsirolimus may also be treated with dose interruption/reduction; the everolimus prescribing information advises treatment discontinuation for grade 4 stomatitis.
Summary and discussion
mTOR inhibitors can be effective treatments for patients with advanced cancer, specifically for advanced RCC, advanced pNET, and HR+, HER2-negative advanced breast cancer. Although mIAS may occur in many patients, it is usually grade 1 or 2 in severity. mIAS has an early onset, usually within the first 2 weeks of treatment16,19,42 and a relatively rapid resolution, usually within 3 weeks.16,19 Thus, most cases of mIAS are self-limiting.
The relatively recent emergence of mIAS poses short-term challenges regarding diagnosis, assessment, prevention, and treatment. Several clinical studies are underway to evaluate a range of interventions for their preventive and therapeutic efficacy in mIAS. Furthermore, our growing understanding of the underlying pathophysiology of mIAS can guide how mIAS is managed and what interventions patients receive.
Although mIAS is believed to differ from chemotherapy- or radiation-induced oral mucositis and aphthous ulcers, much can be learned from the treatment of both of these. Several strategies have been proposed to limit the occurrence of mIAS (Table 3). First, establish an oral care protocol. Educate patients who are initiating treatment with an mTOR inhibitor on implementation of the oral care protocol and emphasize adherence. Second, educate patients on the symptoms and timing of mIAS. Patients may hesitate to report mild symptoms or assume they are innocuous, so be clear that reporting all symptoms is important to allow timely clinical evaluation. Early recognition of mIAS facilitates early intervention and can prevent dose modification and interruption. Third, implement the preventive and treatment measures described. Many of the preventive measures can be incorporated into an oral care protocol.
The advent of mTOR inhibitors has clinically benefited many patients with cancer. Although side effects, like mIAS, may develop during treatment, they should not be considered insurmountable. Through education, vigilance, and aggressive management, health care providers and patients can work together to help patients maintain their quality of life while continuing to optimally address their disease.
Acknowledgment
The authors thank Anna Lau, PhD, and Patricia Segarini, PhD, of Percolation Communications LLC, for their editorial assistance. Funding for manuscript development was provided by Novartis Pharmaceuticals Corp.
1. Lauring J, Park BH, Wolff AC. The phosphoinositide-3-kinase-Akt-mTOR pathway as a therapeutic target in breast cancer. J Natl Compr Canc Netw. 2013;11:670-678.
2. Fruman DA, Rommel C. PI3K and cancer: lessons, challenges and opportunities. Nat Rev Drug Discov. 2014;13:140-156.
3. Torisel (temsirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2014.
4. Afinitor (everolimus) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
5. Rapamune (sirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2012.
6. Peterson DE, Boers-Doets CB, Bensadoun RJ, Herrstedt J, ESMO Guidelines Committee. Management of oral and gastrointestinal mucosal injury: ESMO Clinical Practice Guidelines for diagnosis, treatment, and follow-up. Ann Oncol. 2015;26 Suppl 5:v139-151.
7. Hidalgo M, Buckner JC, Erlichman C, et al. A phase I and pharmacokinetic study of temsirolimus (CCI-779) administered intravenously daily for 5 days every 2 weeks to patients with advanced cancer. Clin Cancer Res. 2006;12:5755-5763.
8. Martins F, de Oliveira MA, Wang Q, et al. A review of oral toxicity associated with mTOR inhibitor therapy in cancer patients. Oral Oncol. 2013;49:293-298.
9. O’Donnell A, Faivre S, Burris HA, 3rd, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol. 2008;26:1588-1595.
10. Shameem R, Lacouture M, Wu S. Incidence and risk of high-grade stomatitis with mTOR inhibitors in cancer patients. Cancer Invest. 2015;33:70-77.
11. Femara (letrozole) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2014.
12. Rugo HS, Hortobagyi GN, Yao J, et al. Meta-analysis of stomatitis in clinical studies of everolimus: incidence and relationship with efficacy. Ann Oncol. 2016;27:519-525.
13. Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109:820-831.
14. Sonis S, Treister N, Chawla S, Demetri G, Haluska F. Preliminary characterization of oral lesions associated with inhibitors of mammalian target of rapamycin in cancer patients. Cancer. 2010;116:210-215.
15. Scully C. Clinical practice. Aphthous ulceration. N Engl J Med. 2006;355:165-172.
16. Ferte C, Paci A, Zizi M, et al. Natural history, management and pharmacokinetics of everolimus-induced-oral ulcers: insights into compliance issues. Eur J Cancer. 2011;47:2249-2255.
17. Wong HM. Oral complications and management strategies for patients undergoing cancer therapy ScienceWorldJournal. 2014;581795.
18. de Oliveira MA, Martins EMF, Wang Q, et al. Clinical presentation and management of mTOR inhibitor-associated stomatitis. Oral Oncol. 2011;47:998-1003.
19. Rugo HS, Pritchard KI, Gnant M, et al. Incidence and time course of everolimus-related adverse events in postmenopausal women with hormone receptor-positive advanced breast cancer: insights from BOLERO-2. Ann Oncol. 2014;25:808-815.
20. National Cancer Institute. Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events v3.0 (CTCAE). http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed February 13, 2017.
21. National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v4.03. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed February 13, 2017.
22. World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment. Geneva, Switzerland: World Health Organization (WHO Offset Publication No. 48); 1979.
23. Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin. 2012;62:400-422.
24. Iglesias-Bartolome R, Patel V, Cotrim A, et al. mTOR inhibition prevents epithelial stem cell senescence and protects from radiation-induced mucositis. Cell Stem Cell. 2012;11:401-414.
25. Lewkowicz N, Lewkowicz P, Dzitko K, et al. Dysfunction of CD4+CD25high T regulatory cells in patients with recurrent aphthous stomatitis. J Oral Pathol Med. 2008;37:454-461.
26. Levine B, Deretic V. Unveiling the roles of autophagy in innate and adaptive immunity. Nat Rev Immunol. 2007;7:767-777.
27. Jin Y, Tymen SD, Chen D, et al. MicroRNA-99 family targets AKT/mTOR signaling pathway in dermal wound healing. PLoS One. 2013;8:e64434.
28. Rosselli-Murai LK, Almeida LO, Zagni C, et al. Periostin responds to mechanical stress and tension by activating the MTOR signaling pathway. PLoS One. 2013;8:e83580.
29. Rugo HS. Dosing and safety implications for oncologists when administering everolimus to patients with hormone receptor-positive breast cancer. Clin Breast Cancer. 2016;16:18-22.
30. Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520-529.
31. Yardley DA, Noguchi S, Pritchard KI, et al. Everolimus plus exemestane in postmenopausal patients with HR(+) breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30:870-884.
32. Rubenstein EB, Peterson DE, Schubert M, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004;100:2026-2046.
33. Borowski B, Benhamou E, Pico JL, Laplanche A, Margainaud JP, Hayat M. Prevention of oral mucositis in patients treated with high-dose chemotherapy and bone marrow transplantation: a randomised controlled trial comparing two protocols of dental care. Eur J Cancer B Oral Oncol. 1994;30B:93-97.
34. Cheng KK, Molassiotis A, Chang AM, Wai WC, Cheung SS. Evaluation of an oral care protocol intervention in the prevention of chemotherapy-induced oral mucositis in paediatric cancer patients. Eur J Cancer. 2001;37:2056-2063.
35. Dudjak LA. Mouth care for mucositis due to radiation therapy. Cancer Nurs. 1987;10:131-140.
36. Graham KM, Pecoraro DA, Ventura M, Meyer CC. Reducing the incidence of stomatitis using a quality assessment and improvement approach. Cancer Nurs. 1993;16:117-122.
37. Kenny SA. Effect of two oral care protocols on the incidence of stomatitis in hematology patients. Cancer Nurs. 1990;13:345-353.
38. Larson PJ, Miaskowski C, MacPhail L, et al. The PRO-SELF Mouth Aware program: an effective approach for reducing chemotherapy-induced mucositis. Cancer Nurs. 1998;21:263-268.
39. Levy-Polack MP, Sebelli P, Polack NL. Incidence of oral complications and application of a preventive protocol in children with acute leukemia. Spec Care Dentist. 1998;18:189-193.
40. Yeager KA, Webster J, Crain M, Kasow J, McGuire DB. Implementation of an oral care standard for leukemia and transplantation patients. Cancer Nurs. 2000;23:40-47; quiz 47-48.
41. Pilotte AP, Hohos MB, Polson KM, Huftalen TM, Treister N. Managing stomatitis in patients treated with mammalian target of rapamycin inhibitors. Clin J Oncol Nurs. 2011;15:E83-89.
42. Gomez-Fernandez C, Garden BC, Wu S, Feldman DR, Lacouture ME. The risk of skin rash and stomatitis with the mammalian target of rapamycin inhibitor temsirolimus: a systematic review of the literature and meta-analysis. Eur J Cancer. 2012;48:340-346.
43. Bonnaure-Mallet M, Bunetel L, Tricot-Doleux S, Guerin J, Bergeron C, LeGall E. Oral complications during treatment of malignant diseases in childhood: effects of tooth brushing. Eur J Cancer. 1998;34:1588-1591.
44. Chuang P, Langone AJ. Clobetasol ameliorates aphthous ulceration in renal transplant patients on sirolimus. Am J Transplant. 2007;7:714-717.
45. Femiano F, Buonaiuto C, Gombos F, Lanza A, Cirillo N. Pilot study on recurrent aphthous stomatitis (RAS): a randomized placebo-controlled trial for the comparative therapeutic effects of systemic prednisone and systemic montelukast in subjects unresponsive to topical therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:402-407.
1. Lauring J, Park BH, Wolff AC. The phosphoinositide-3-kinase-Akt-mTOR pathway as a therapeutic target in breast cancer. J Natl Compr Canc Netw. 2013;11:670-678.
2. Fruman DA, Rommel C. PI3K and cancer: lessons, challenges and opportunities. Nat Rev Drug Discov. 2014;13:140-156.
3. Torisel (temsirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2014.
4. Afinitor (everolimus) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
5. Rapamune (sirolimus) [prescribing information]. Philadelphia, PA: Wyeth Pharmaceuticals; 2012.
6. Peterson DE, Boers-Doets CB, Bensadoun RJ, Herrstedt J, ESMO Guidelines Committee. Management of oral and gastrointestinal mucosal injury: ESMO Clinical Practice Guidelines for diagnosis, treatment, and follow-up. Ann Oncol. 2015;26 Suppl 5:v139-151.
7. Hidalgo M, Buckner JC, Erlichman C, et al. A phase I and pharmacokinetic study of temsirolimus (CCI-779) administered intravenously daily for 5 days every 2 weeks to patients with advanced cancer. Clin Cancer Res. 2006;12:5755-5763.
8. Martins F, de Oliveira MA, Wang Q, et al. A review of oral toxicity associated with mTOR inhibitor therapy in cancer patients. Oral Oncol. 2013;49:293-298.
9. O’Donnell A, Faivre S, Burris HA, 3rd, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol. 2008;26:1588-1595.
10. Shameem R, Lacouture M, Wu S. Incidence and risk of high-grade stomatitis with mTOR inhibitors in cancer patients. Cancer Invest. 2015;33:70-77.
11. Femara (letrozole) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2014.
12. Rugo HS, Hortobagyi GN, Yao J, et al. Meta-analysis of stomatitis in clinical studies of everolimus: incidence and relationship with efficacy. Ann Oncol. 2016;27:519-525.
13. Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109:820-831.
14. Sonis S, Treister N, Chawla S, Demetri G, Haluska F. Preliminary characterization of oral lesions associated with inhibitors of mammalian target of rapamycin in cancer patients. Cancer. 2010;116:210-215.
15. Scully C. Clinical practice. Aphthous ulceration. N Engl J Med. 2006;355:165-172.
16. Ferte C, Paci A, Zizi M, et al. Natural history, management and pharmacokinetics of everolimus-induced-oral ulcers: insights into compliance issues. Eur J Cancer. 2011;47:2249-2255.
17. Wong HM. Oral complications and management strategies for patients undergoing cancer therapy ScienceWorldJournal. 2014;581795.
18. de Oliveira MA, Martins EMF, Wang Q, et al. Clinical presentation and management of mTOR inhibitor-associated stomatitis. Oral Oncol. 2011;47:998-1003.
19. Rugo HS, Pritchard KI, Gnant M, et al. Incidence and time course of everolimus-related adverse events in postmenopausal women with hormone receptor-positive advanced breast cancer: insights from BOLERO-2. Ann Oncol. 2014;25:808-815.
20. National Cancer Institute. Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events v3.0 (CTCAE). http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed February 13, 2017.
21. National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v4.03. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed February 13, 2017.
22. World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment. Geneva, Switzerland: World Health Organization (WHO Offset Publication No. 48); 1979.
23. Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin. 2012;62:400-422.
24. Iglesias-Bartolome R, Patel V, Cotrim A, et al. mTOR inhibition prevents epithelial stem cell senescence and protects from radiation-induced mucositis. Cell Stem Cell. 2012;11:401-414.
25. Lewkowicz N, Lewkowicz P, Dzitko K, et al. Dysfunction of CD4+CD25high T regulatory cells in patients with recurrent aphthous stomatitis. J Oral Pathol Med. 2008;37:454-461.
26. Levine B, Deretic V. Unveiling the roles of autophagy in innate and adaptive immunity. Nat Rev Immunol. 2007;7:767-777.
27. Jin Y, Tymen SD, Chen D, et al. MicroRNA-99 family targets AKT/mTOR signaling pathway in dermal wound healing. PLoS One. 2013;8:e64434.
28. Rosselli-Murai LK, Almeida LO, Zagni C, et al. Periostin responds to mechanical stress and tension by activating the MTOR signaling pathway. PLoS One. 2013;8:e83580.
29. Rugo HS. Dosing and safety implications for oncologists when administering everolimus to patients with hormone receptor-positive breast cancer. Clin Breast Cancer. 2016;16:18-22.
30. Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520-529.
31. Yardley DA, Noguchi S, Pritchard KI, et al. Everolimus plus exemestane in postmenopausal patients with HR(+) breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30:870-884.
32. Rubenstein EB, Peterson DE, Schubert M, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004;100:2026-2046.
33. Borowski B, Benhamou E, Pico JL, Laplanche A, Margainaud JP, Hayat M. Prevention of oral mucositis in patients treated with high-dose chemotherapy and bone marrow transplantation: a randomised controlled trial comparing two protocols of dental care. Eur J Cancer B Oral Oncol. 1994;30B:93-97.
34. Cheng KK, Molassiotis A, Chang AM, Wai WC, Cheung SS. Evaluation of an oral care protocol intervention in the prevention of chemotherapy-induced oral mucositis in paediatric cancer patients. Eur J Cancer. 2001;37:2056-2063.
35. Dudjak LA. Mouth care for mucositis due to radiation therapy. Cancer Nurs. 1987;10:131-140.
36. Graham KM, Pecoraro DA, Ventura M, Meyer CC. Reducing the incidence of stomatitis using a quality assessment and improvement approach. Cancer Nurs. 1993;16:117-122.
37. Kenny SA. Effect of two oral care protocols on the incidence of stomatitis in hematology patients. Cancer Nurs. 1990;13:345-353.
38. Larson PJ, Miaskowski C, MacPhail L, et al. The PRO-SELF Mouth Aware program: an effective approach for reducing chemotherapy-induced mucositis. Cancer Nurs. 1998;21:263-268.
39. Levy-Polack MP, Sebelli P, Polack NL. Incidence of oral complications and application of a preventive protocol in children with acute leukemia. Spec Care Dentist. 1998;18:189-193.
40. Yeager KA, Webster J, Crain M, Kasow J, McGuire DB. Implementation of an oral care standard for leukemia and transplantation patients. Cancer Nurs. 2000;23:40-47; quiz 47-48.
41. Pilotte AP, Hohos MB, Polson KM, Huftalen TM, Treister N. Managing stomatitis in patients treated with mammalian target of rapamycin inhibitors. Clin J Oncol Nurs. 2011;15:E83-89.
42. Gomez-Fernandez C, Garden BC, Wu S, Feldman DR, Lacouture ME. The risk of skin rash and stomatitis with the mammalian target of rapamycin inhibitor temsirolimus: a systematic review of the literature and meta-analysis. Eur J Cancer. 2012;48:340-346.
43. Bonnaure-Mallet M, Bunetel L, Tricot-Doleux S, Guerin J, Bergeron C, LeGall E. Oral complications during treatment of malignant diseases in childhood: effects of tooth brushing. Eur J Cancer. 1998;34:1588-1591.
44. Chuang P, Langone AJ. Clobetasol ameliorates aphthous ulceration in renal transplant patients on sirolimus. Am J Transplant. 2007;7:714-717.
45. Femiano F, Buonaiuto C, Gombos F, Lanza A, Cirillo N. Pilot study on recurrent aphthous stomatitis (RAS): a randomized placebo-controlled trial for the comparative therapeutic effects of systemic prednisone and systemic montelukast in subjects unresponsive to topical therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:402-407.
Repeal and replace? How about retain, review, and refine?
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
Toxic abandonment: a case for non-participation in physician-assisted suicide
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
Rucaparib – second PARP inhibitor hits the market for ovarian cancer
Rucaparib was granted accelerated approval by the US Food and Drug Administration for the treatment of patients with BRCA1/2 mutant advanced ovarian cancer in January this year, making it the second drug in its class for this indication. It is a poly(ADP-ribose) polymerase inhibitor that works by blocking the repair of damaged DNA in cancer cells and triggering cell death.
The approval was based on findings from 2 single-arm clinical trials in which rucaparib led to complete or partial tumor shrinkage in more than half of the patients enrolled. A pooled analysis included 106 patients from the phase 2 trials, Study 10 (NCT01482715; N = 42) and ARIEL2 (NCT01891344; N = 64), in which patients with BRCA1/2 mutation-positive ovarian cancer who had progressed on 2 or more previous chemotherapy regimens, received 600 mg rucaparib twice daily.
Study 10 included only patients with platinum-sensitive disease and eligible patients were aged 18 years or older, with a known deleterious BRCA mutation, evidence of measurable disease as defined by Response Evaluation Criteria in Solid Tumors (version 1.1), sufficient archival tumor tissue, histologically confirmed high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer and relapsed disease confirmed by radiologic assessment. Meanwhile, ARIEL2 had similar eligibility criteria, except that patients with platinum-sensitive, resistant, and refractory disease were included.
Both studies excluded patients with active second malignancies, and for those with a history of prior cancer that had been curatively treated, no evidence of current disease was required and chemotherapy should have been completed more than 6 months or bone marrow transplant more than 2 years before the first dose of rucaparib. Patients who had previously been treated with a PARP inhibitor, with symptomatic and/or untreated central nervous system metastases, or who had been hospitalized for bowel obstruction within the previous 3 months, were also ineligible.
Across the 2 trials, the median age of trial participants was 59 years, 78% were white, and all had an Eastern Cooperative Oncology Group performance status of 0 (fully active, able to carry on all pre-disease performance without restriction) or 1 (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature). Both trials used a surrogate endpoint for approval, measuring the percentage of patients who experienced complete or partial tumor shrinkage, the overall response rate (ORR), while taking rucaparib.
In Study 10, the ORR was 60%, including a complete response (CR) rate of 10% and a partial response (PR) rate of 50%, over a median duration of response (DoR) of 7.9 months, while in ARIEL2, the ORR was 50%, including a CR of 8% and a PR of 42%, over a median DoR of 11.6 months. The pooled analysis demonstrated an ORR of 54%, CR of 9% and PR of 45%, over a median DoR of 9.2 months. In separate data reported in the prescribing information, the ORR as assessed by independent radiology review was 42%, with a median DoR of 6.7 months, while ORR according to investigator assessment was 66%. In all analyses, the response rate was similar for patients having BRCA1 versus BRCA2 gene mutations.
Safety analyses were performed in 377 patients across the 2 studies who received 600 mg rucaparib twice daily. The most common adverse events (AEs) of any grade included nausea, fatigue, vomiting, anemia, abdominal pain, dysgeusia, constipation, decreased appetite, diarrhea, thrombocytopenia, and dyspnea. The most common serious AEs (grade 3 or 4) were anemia (25%), fatigue/asthenia (11%), and increased alanine aminotransferase or aspartate aminotransferase levels (11%). Overall, 8% of patients discontinued treatment because of AEs.
The recommended dose according to the prescribing information is 600 mg, in the form of two 300-mg tablets taken orally twice daily with or without food. Phy
If hematologic toxicities occur while taking rucaparib, treatment should be interrupted and blood counts monitored until recovery and failure to recover to grade 1 or higher after 4 weeks should prompt referral to a hematologist for further investigation, while confirmed diagnosis of myelodysplastic syndromes or acute myeloid leukemia should lead to discontinuation of rucaparib. Pregnant women and those of reproductive potential should be advised of the potential risk to a fetus or the need for effective contraception during treatment and for 6 months after the last dose of rucaparib.
Rucaparib is indicated only for the treatment of patients with confirmed BRCA1/2 mutations, so the drug was approved in conjunction with a companion diagnostic. FoundationFocus CDxBRCA is the first next-generation sequencing-based test to receive FDA approval and detects the presence of deleterious BRCA gene mutations in tumor tissue samples. Rucaparib is marketed as Rubraca by Clovis Oncology Inc, and the companion diagnostic by Foundation Medicine Inc.
1. Rubraca (rucaparib) capsules, for oral use. Prescribing information. Clovis Oncology Inc. http://clovisoncology.com/files/rubraca-prescribing-info.pdf. Released December 2016. Accessed January 8th, 2017.
2. FDA grants accelerated approval to new treatment for advanced ovarian cancer. FDA News Release. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm533873.htm. Last updated December 19, 2016. Accessed January 8, 2017.
3. [No author listed.] Rucaparib approved for ovarian cancer. Cancer Discov. Epub ahead of print. January 5, 2017. doi: 10.1158/2159-8290. CD-NB2016-164.
Rucaparib was granted accelerated approval by the US Food and Drug Administration for the treatment of patients with BRCA1/2 mutant advanced ovarian cancer in January this year, making it the second drug in its class for this indication. It is a poly(ADP-ribose) polymerase inhibitor that works by blocking the repair of damaged DNA in cancer cells and triggering cell death.
The approval was based on findings from 2 single-arm clinical trials in which rucaparib led to complete or partial tumor shrinkage in more than half of the patients enrolled. A pooled analysis included 106 patients from the phase 2 trials, Study 10 (NCT01482715; N = 42) and ARIEL2 (NCT01891344; N = 64), in which patients with BRCA1/2 mutation-positive ovarian cancer who had progressed on 2 or more previous chemotherapy regimens, received 600 mg rucaparib twice daily.
Study 10 included only patients with platinum-sensitive disease and eligible patients were aged 18 years or older, with a known deleterious BRCA mutation, evidence of measurable disease as defined by Response Evaluation Criteria in Solid Tumors (version 1.1), sufficient archival tumor tissue, histologically confirmed high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer and relapsed disease confirmed by radiologic assessment. Meanwhile, ARIEL2 had similar eligibility criteria, except that patients with platinum-sensitive, resistant, and refractory disease were included.
Both studies excluded patients with active second malignancies, and for those with a history of prior cancer that had been curatively treated, no evidence of current disease was required and chemotherapy should have been completed more than 6 months or bone marrow transplant more than 2 years before the first dose of rucaparib. Patients who had previously been treated with a PARP inhibitor, with symptomatic and/or untreated central nervous system metastases, or who had been hospitalized for bowel obstruction within the previous 3 months, were also ineligible.
Across the 2 trials, the median age of trial participants was 59 years, 78% were white, and all had an Eastern Cooperative Oncology Group performance status of 0 (fully active, able to carry on all pre-disease performance without restriction) or 1 (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature). Both trials used a surrogate endpoint for approval, measuring the percentage of patients who experienced complete or partial tumor shrinkage, the overall response rate (ORR), while taking rucaparib.
In Study 10, the ORR was 60%, including a complete response (CR) rate of 10% and a partial response (PR) rate of 50%, over a median duration of response (DoR) of 7.9 months, while in ARIEL2, the ORR was 50%, including a CR of 8% and a PR of 42%, over a median DoR of 11.6 months. The pooled analysis demonstrated an ORR of 54%, CR of 9% and PR of 45%, over a median DoR of 9.2 months. In separate data reported in the prescribing information, the ORR as assessed by independent radiology review was 42%, with a median DoR of 6.7 months, while ORR according to investigator assessment was 66%. In all analyses, the response rate was similar for patients having BRCA1 versus BRCA2 gene mutations.
Safety analyses were performed in 377 patients across the 2 studies who received 600 mg rucaparib twice daily. The most common adverse events (AEs) of any grade included nausea, fatigue, vomiting, anemia, abdominal pain, dysgeusia, constipation, decreased appetite, diarrhea, thrombocytopenia, and dyspnea. The most common serious AEs (grade 3 or 4) were anemia (25%), fatigue/asthenia (11%), and increased alanine aminotransferase or aspartate aminotransferase levels (11%). Overall, 8% of patients discontinued treatment because of AEs.
The recommended dose according to the prescribing information is 600 mg, in the form of two 300-mg tablets taken orally twice daily with or without food. Phy
If hematologic toxicities occur while taking rucaparib, treatment should be interrupted and blood counts monitored until recovery and failure to recover to grade 1 or higher after 4 weeks should prompt referral to a hematologist for further investigation, while confirmed diagnosis of myelodysplastic syndromes or acute myeloid leukemia should lead to discontinuation of rucaparib. Pregnant women and those of reproductive potential should be advised of the potential risk to a fetus or the need for effective contraception during treatment and for 6 months after the last dose of rucaparib.
Rucaparib is indicated only for the treatment of patients with confirmed BRCA1/2 mutations, so the drug was approved in conjunction with a companion diagnostic. FoundationFocus CDxBRCA is the first next-generation sequencing-based test to receive FDA approval and detects the presence of deleterious BRCA gene mutations in tumor tissue samples. Rucaparib is marketed as Rubraca by Clovis Oncology Inc, and the companion diagnostic by Foundation Medicine Inc.
Rucaparib was granted accelerated approval by the US Food and Drug Administration for the treatment of patients with BRCA1/2 mutant advanced ovarian cancer in January this year, making it the second drug in its class for this indication. It is a poly(ADP-ribose) polymerase inhibitor that works by blocking the repair of damaged DNA in cancer cells and triggering cell death.
The approval was based on findings from 2 single-arm clinical trials in which rucaparib led to complete or partial tumor shrinkage in more than half of the patients enrolled. A pooled analysis included 106 patients from the phase 2 trials, Study 10 (NCT01482715; N = 42) and ARIEL2 (NCT01891344; N = 64), in which patients with BRCA1/2 mutation-positive ovarian cancer who had progressed on 2 or more previous chemotherapy regimens, received 600 mg rucaparib twice daily.
Study 10 included only patients with platinum-sensitive disease and eligible patients were aged 18 years or older, with a known deleterious BRCA mutation, evidence of measurable disease as defined by Response Evaluation Criteria in Solid Tumors (version 1.1), sufficient archival tumor tissue, histologically confirmed high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer and relapsed disease confirmed by radiologic assessment. Meanwhile, ARIEL2 had similar eligibility criteria, except that patients with platinum-sensitive, resistant, and refractory disease were included.
Both studies excluded patients with active second malignancies, and for those with a history of prior cancer that had been curatively treated, no evidence of current disease was required and chemotherapy should have been completed more than 6 months or bone marrow transplant more than 2 years before the first dose of rucaparib. Patients who had previously been treated with a PARP inhibitor, with symptomatic and/or untreated central nervous system metastases, or who had been hospitalized for bowel obstruction within the previous 3 months, were also ineligible.
Across the 2 trials, the median age of trial participants was 59 years, 78% were white, and all had an Eastern Cooperative Oncology Group performance status of 0 (fully active, able to carry on all pre-disease performance without restriction) or 1 (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature). Both trials used a surrogate endpoint for approval, measuring the percentage of patients who experienced complete or partial tumor shrinkage, the overall response rate (ORR), while taking rucaparib.
In Study 10, the ORR was 60%, including a complete response (CR) rate of 10% and a partial response (PR) rate of 50%, over a median duration of response (DoR) of 7.9 months, while in ARIEL2, the ORR was 50%, including a CR of 8% and a PR of 42%, over a median DoR of 11.6 months. The pooled analysis demonstrated an ORR of 54%, CR of 9% and PR of 45%, over a median DoR of 9.2 months. In separate data reported in the prescribing information, the ORR as assessed by independent radiology review was 42%, with a median DoR of 6.7 months, while ORR according to investigator assessment was 66%. In all analyses, the response rate was similar for patients having BRCA1 versus BRCA2 gene mutations.
Safety analyses were performed in 377 patients across the 2 studies who received 600 mg rucaparib twice daily. The most common adverse events (AEs) of any grade included nausea, fatigue, vomiting, anemia, abdominal pain, dysgeusia, constipation, decreased appetite, diarrhea, thrombocytopenia, and dyspnea. The most common serious AEs (grade 3 or 4) were anemia (25%), fatigue/asthenia (11%), and increased alanine aminotransferase or aspartate aminotransferase levels (11%). Overall, 8% of patients discontinued treatment because of AEs.
The recommended dose according to the prescribing information is 600 mg, in the form of two 300-mg tablets taken orally twice daily with or without food. Phy
If hematologic toxicities occur while taking rucaparib, treatment should be interrupted and blood counts monitored until recovery and failure to recover to grade 1 or higher after 4 weeks should prompt referral to a hematologist for further investigation, while confirmed diagnosis of myelodysplastic syndromes or acute myeloid leukemia should lead to discontinuation of rucaparib. Pregnant women and those of reproductive potential should be advised of the potential risk to a fetus or the need for effective contraception during treatment and for 6 months after the last dose of rucaparib.
Rucaparib is indicated only for the treatment of patients with confirmed BRCA1/2 mutations, so the drug was approved in conjunction with a companion diagnostic. FoundationFocus CDxBRCA is the first next-generation sequencing-based test to receive FDA approval and detects the presence of deleterious BRCA gene mutations in tumor tissue samples. Rucaparib is marketed as Rubraca by Clovis Oncology Inc, and the companion diagnostic by Foundation Medicine Inc.
1. Rubraca (rucaparib) capsules, for oral use. Prescribing information. Clovis Oncology Inc. http://clovisoncology.com/files/rubraca-prescribing-info.pdf. Released December 2016. Accessed January 8th, 2017.
2. FDA grants accelerated approval to new treatment for advanced ovarian cancer. FDA News Release. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm533873.htm. Last updated December 19, 2016. Accessed January 8, 2017.
3. [No author listed.] Rucaparib approved for ovarian cancer. Cancer Discov. Epub ahead of print. January 5, 2017. doi: 10.1158/2159-8290. CD-NB2016-164.
1. Rubraca (rucaparib) capsules, for oral use. Prescribing information. Clovis Oncology Inc. http://clovisoncology.com/files/rubraca-prescribing-info.pdf. Released December 2016. Accessed January 8th, 2017.
2. FDA grants accelerated approval to new treatment for advanced ovarian cancer. FDA News Release. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm533873.htm. Last updated December 19, 2016. Accessed January 8, 2017.
3. [No author listed.] Rucaparib approved for ovarian cancer. Cancer Discov. Epub ahead of print. January 5, 2017. doi: 10.1158/2159-8290. CD-NB2016-164.
End-of-life options and the legal pathways to physician aid in dying
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
Communicating Prognostic Information in Oncology
Study Overview
Objective. To assess the prevalence and determinants of patient–oncologist discordance in opinion of prognosis, and evaluate how often patients are aware of this discordance.
Design. Cross-sectional study.
Setting and participants. The study included 236 adult patients with advanced cancer and their 38 oncologists at academic and community oncology practices in Rochester, New York, and Sacramento, California. Inpatients and those already enrolled in hospice were excluded.
Main outcome measures. Patients and their oncologists independently reported their ratings of 2-year survival probability on a postindex visit multiple-choice questionnaire (response options included 100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). Prognostic discordance was defined as a more than 1 category difference between the patient and physician prognostic ratings. All patients were asked to report how they believed their oncologist would rate their 2-year survival probability. Those who correctly perceived their oncologist’s rating of their prognosis (within 1 category) were defined as knowing their oncologist’s opinion, and the rest were defined as not knowing their oncologist’s opinion. This distinction was used to categorize patients whose self-rating of their prognosis was discordant from their oncologist’s rating as either knowingly discordant or unknowingly discordant. Patient characteristics including age, sex, race/ethnicity, education, income, aggressiveness of cancer, self-efficacy with health care communication, recall of prognostic discussion with the oncologist, and end-of-life treatment preferences were evaluated as potential determinants of prognostic discordance.
Main results. 68% of patients rated their 2-year survival probability discordantly from their oncologists. Among these, 96% rated their prognosis more optimistically than their oncologists, and 89% were unaware that their opinions differed from that of their oncologists. Prognostic discordance was more common among nonwhite compared to white patients (95% versus 65%, P = 0.03). The prevalence of prognostic discordance did not significantly differ based on the other patient characteristics studied. Among patients whose prognostic ratings were discordant from their oncologist’s, 99% reported that they wanted to be involved in treatment decision making, and 70% were interested in involving palliative care when the end of life became near.
Conclusion. Patient–oncologist discordance about prognosis was common, particularly among nonwhite patients. In cases of prognostic discordance, patients rarely knew that their opinion differed from that of their oncologist, suggesting a lack of successful communication of prognostic information.
Commentary
Prior studies have noted that patients with advanced cancer perceive prognosis more optimistically than their physicians [1–3]. In a large national prospective observational study, the majority of patients receiving chemotherapy for metastatic (stage IV) lung or colorectal cancer inaccurately believed that chemotherapy was likely to be curative, potentially compromising their ability to make informed treatment decisions [4]. In the present study by Gramling et al, the authors confirm the observation that patients are more optimistic about prognosis than their oncologists, and furthermore demonstrate that most patients are unaware of the discrepancy, suggesting a failure of communication. As in prior studies, racial disparity in prognostic understanding was observed, with nonwhite patients being more likely to have overly optimistic views of their prognosis [4,5].
While the perceived 2-year survival probability is a somewhat arbitrary measure of prognostic opinion, it provides a useful representation of how one views the expected trajectory of disease. A high perceived likelihood of 2-year survival implies a view that long-term disease control can be achieved, whereas a low perceived likelihood of 2-year survival implies acknowledgement of terminal illness. This study effectively contrasts patient and physician opinions of 2-year survival probability, but it does not discriminate among clinically relevant differences in opinions within the 0–2 year prognostic range. For example, a patient whose oncologist believes his prognosis is < 6 months may be an appropriate candidate for hospice, but the patient may be unprepared to make the transition to hospice if he believes his prognosis is closer to a year or more. While the patient and oncologist may agree that 2-year survival is unlikely, they may have differing beliefs about the appropriateness of certain interventions based on their discrepant short-term prognostic views. Additional studies looking at perceived probabilities of short-term survival may be helpful in assessing patients’ readiness to transition to symptom-focused care when medically appropriate.
The authors designate 7 categories of 2-year survival probability (100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). The differences in percentage between prognostic categories are not evenly distributed, and therefore definition of discordance is non-uniform. The smaller percentage difference at the highest and lowest ends of the scale may result in overestimation of discordance at these extremes. For example, a patient rating her 2-year survival probability at 100% would be defined as having a discordant viewpoint from an oncologist rating her 2-year survival at 75% (as would be realistic for a diagnosis such as metastatic colon cancer). Given the imprecise nature of prognostication, the views of the patient and oncologist in this example are arguably similar, and perhaps should not be categorized as discordant.
As noted, patients already enrolled in hospice were excluded from the study, thus omitting a key group of patients whose prognostic views are more likely to be concordant with their physicians’ views. This group may be better captured in a prospective study of prognostic discordance among newly diagnosed advanced cancer patients after initial oncology consultation, allowing for inclusion of those who make an early transition to hospice.
Applications for Clinical Practice
Although clinicians tend to overestimate prognosis, their predictions correlate with outcomes in advanced cancer [6], and may therefore provide a useful framework for patients to understand the likely course of their disease. However, physicians often avoid explicit discussion of prognosis by shrouding prognostic information in discussions of radiographic findings, and quickly transitioning to discussion of treatment options [7]. Patients and families rarely inquire about prognosis, further limiting disclosure of prognostic information [7,8]. Even when prognostic information is explicitly stated, patients may misinterpret the information [4], potentially adversely affecting their ability to participate in shared decision making.
Some useful approaches for successfully communicating prognostic information may include asking patients what information they wish to hear before it is disclosed, providing prognostic data for patients with similar disease states while acknowledging individual variability, clearly defining the intent of proposed therapy (ie, curative versus noncurative), and asking the patient to restate information in order to assess understanding. Early involvement of palliative care specialists may help reinforce understanding about prognosis and goals of therapy, facilitate advance care planning, and reduce aggressive interventions at the end of life [2]. Ongoing research is directed at identifying effective interventions to improve communication between patients with advanced cancer and their oncologists [9].
—Irene M. Hutchins, MD
Scripps Cancer Center, La Jolla, CA
1. Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA 1998;279:1709–14.
2. Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–26.
3. Pronzato P, Bertelli G, Losardo P, Landucci M. What do advanced cancer patients know of their disease? A report from Italy. Support Care Cancer 1994;2:242–4.
4. Weeks JC, Catalano PJ, Cronin A, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–25.
5. Ford D, Zapka J, Gebregziabher M, et al. Factors associated with illness perception among critically ill patients and surrogates. Chest 2010;138:59–67.
6. Glare P, Virik K, Jones M, et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ 2003;327:195–8.
7. Singh S, Cortez D, Maynard D, et al. Characterizing the nature of scan results discussions: insights into why patients misunderstand their prognosis. J Oncol Pract 2017:JOP2016014621.
8. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909–13.
9. Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer 2013;13:188.
Study Overview
Objective. To assess the prevalence and determinants of patient–oncologist discordance in opinion of prognosis, and evaluate how often patients are aware of this discordance.
Design. Cross-sectional study.
Setting and participants. The study included 236 adult patients with advanced cancer and their 38 oncologists at academic and community oncology practices in Rochester, New York, and Sacramento, California. Inpatients and those already enrolled in hospice were excluded.
Main outcome measures. Patients and their oncologists independently reported their ratings of 2-year survival probability on a postindex visit multiple-choice questionnaire (response options included 100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). Prognostic discordance was defined as a more than 1 category difference between the patient and physician prognostic ratings. All patients were asked to report how they believed their oncologist would rate their 2-year survival probability. Those who correctly perceived their oncologist’s rating of their prognosis (within 1 category) were defined as knowing their oncologist’s opinion, and the rest were defined as not knowing their oncologist’s opinion. This distinction was used to categorize patients whose self-rating of their prognosis was discordant from their oncologist’s rating as either knowingly discordant or unknowingly discordant. Patient characteristics including age, sex, race/ethnicity, education, income, aggressiveness of cancer, self-efficacy with health care communication, recall of prognostic discussion with the oncologist, and end-of-life treatment preferences were evaluated as potential determinants of prognostic discordance.
Main results. 68% of patients rated their 2-year survival probability discordantly from their oncologists. Among these, 96% rated their prognosis more optimistically than their oncologists, and 89% were unaware that their opinions differed from that of their oncologists. Prognostic discordance was more common among nonwhite compared to white patients (95% versus 65%, P = 0.03). The prevalence of prognostic discordance did not significantly differ based on the other patient characteristics studied. Among patients whose prognostic ratings were discordant from their oncologist’s, 99% reported that they wanted to be involved in treatment decision making, and 70% were interested in involving palliative care when the end of life became near.
Conclusion. Patient–oncologist discordance about prognosis was common, particularly among nonwhite patients. In cases of prognostic discordance, patients rarely knew that their opinion differed from that of their oncologist, suggesting a lack of successful communication of prognostic information.
Commentary
Prior studies have noted that patients with advanced cancer perceive prognosis more optimistically than their physicians [1–3]. In a large national prospective observational study, the majority of patients receiving chemotherapy for metastatic (stage IV) lung or colorectal cancer inaccurately believed that chemotherapy was likely to be curative, potentially compromising their ability to make informed treatment decisions [4]. In the present study by Gramling et al, the authors confirm the observation that patients are more optimistic about prognosis than their oncologists, and furthermore demonstrate that most patients are unaware of the discrepancy, suggesting a failure of communication. As in prior studies, racial disparity in prognostic understanding was observed, with nonwhite patients being more likely to have overly optimistic views of their prognosis [4,5].
While the perceived 2-year survival probability is a somewhat arbitrary measure of prognostic opinion, it provides a useful representation of how one views the expected trajectory of disease. A high perceived likelihood of 2-year survival implies a view that long-term disease control can be achieved, whereas a low perceived likelihood of 2-year survival implies acknowledgement of terminal illness. This study effectively contrasts patient and physician opinions of 2-year survival probability, but it does not discriminate among clinically relevant differences in opinions within the 0–2 year prognostic range. For example, a patient whose oncologist believes his prognosis is < 6 months may be an appropriate candidate for hospice, but the patient may be unprepared to make the transition to hospice if he believes his prognosis is closer to a year or more. While the patient and oncologist may agree that 2-year survival is unlikely, they may have differing beliefs about the appropriateness of certain interventions based on their discrepant short-term prognostic views. Additional studies looking at perceived probabilities of short-term survival may be helpful in assessing patients’ readiness to transition to symptom-focused care when medically appropriate.
The authors designate 7 categories of 2-year survival probability (100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). The differences in percentage between prognostic categories are not evenly distributed, and therefore definition of discordance is non-uniform. The smaller percentage difference at the highest and lowest ends of the scale may result in overestimation of discordance at these extremes. For example, a patient rating her 2-year survival probability at 100% would be defined as having a discordant viewpoint from an oncologist rating her 2-year survival at 75% (as would be realistic for a diagnosis such as metastatic colon cancer). Given the imprecise nature of prognostication, the views of the patient and oncologist in this example are arguably similar, and perhaps should not be categorized as discordant.
As noted, patients already enrolled in hospice were excluded from the study, thus omitting a key group of patients whose prognostic views are more likely to be concordant with their physicians’ views. This group may be better captured in a prospective study of prognostic discordance among newly diagnosed advanced cancer patients after initial oncology consultation, allowing for inclusion of those who make an early transition to hospice.
Applications for Clinical Practice
Although clinicians tend to overestimate prognosis, their predictions correlate with outcomes in advanced cancer [6], and may therefore provide a useful framework for patients to understand the likely course of their disease. However, physicians often avoid explicit discussion of prognosis by shrouding prognostic information in discussions of radiographic findings, and quickly transitioning to discussion of treatment options [7]. Patients and families rarely inquire about prognosis, further limiting disclosure of prognostic information [7,8]. Even when prognostic information is explicitly stated, patients may misinterpret the information [4], potentially adversely affecting their ability to participate in shared decision making.
Some useful approaches for successfully communicating prognostic information may include asking patients what information they wish to hear before it is disclosed, providing prognostic data for patients with similar disease states while acknowledging individual variability, clearly defining the intent of proposed therapy (ie, curative versus noncurative), and asking the patient to restate information in order to assess understanding. Early involvement of palliative care specialists may help reinforce understanding about prognosis and goals of therapy, facilitate advance care planning, and reduce aggressive interventions at the end of life [2]. Ongoing research is directed at identifying effective interventions to improve communication between patients with advanced cancer and their oncologists [9].
—Irene M. Hutchins, MD
Scripps Cancer Center, La Jolla, CA
Study Overview
Objective. To assess the prevalence and determinants of patient–oncologist discordance in opinion of prognosis, and evaluate how often patients are aware of this discordance.
Design. Cross-sectional study.
Setting and participants. The study included 236 adult patients with advanced cancer and their 38 oncologists at academic and community oncology practices in Rochester, New York, and Sacramento, California. Inpatients and those already enrolled in hospice were excluded.
Main outcome measures. Patients and their oncologists independently reported their ratings of 2-year survival probability on a postindex visit multiple-choice questionnaire (response options included 100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). Prognostic discordance was defined as a more than 1 category difference between the patient and physician prognostic ratings. All patients were asked to report how they believed their oncologist would rate their 2-year survival probability. Those who correctly perceived their oncologist’s rating of their prognosis (within 1 category) were defined as knowing their oncologist’s opinion, and the rest were defined as not knowing their oncologist’s opinion. This distinction was used to categorize patients whose self-rating of their prognosis was discordant from their oncologist’s rating as either knowingly discordant or unknowingly discordant. Patient characteristics including age, sex, race/ethnicity, education, income, aggressiveness of cancer, self-efficacy with health care communication, recall of prognostic discussion with the oncologist, and end-of-life treatment preferences were evaluated as potential determinants of prognostic discordance.
Main results. 68% of patients rated their 2-year survival probability discordantly from their oncologists. Among these, 96% rated their prognosis more optimistically than their oncologists, and 89% were unaware that their opinions differed from that of their oncologists. Prognostic discordance was more common among nonwhite compared to white patients (95% versus 65%, P = 0.03). The prevalence of prognostic discordance did not significantly differ based on the other patient characteristics studied. Among patients whose prognostic ratings were discordant from their oncologist’s, 99% reported that they wanted to be involved in treatment decision making, and 70% were interested in involving palliative care when the end of life became near.
Conclusion. Patient–oncologist discordance about prognosis was common, particularly among nonwhite patients. In cases of prognostic discordance, patients rarely knew that their opinion differed from that of their oncologist, suggesting a lack of successful communication of prognostic information.
Commentary
Prior studies have noted that patients with advanced cancer perceive prognosis more optimistically than their physicians [1–3]. In a large national prospective observational study, the majority of patients receiving chemotherapy for metastatic (stage IV) lung or colorectal cancer inaccurately believed that chemotherapy was likely to be curative, potentially compromising their ability to make informed treatment decisions [4]. In the present study by Gramling et al, the authors confirm the observation that patients are more optimistic about prognosis than their oncologists, and furthermore demonstrate that most patients are unaware of the discrepancy, suggesting a failure of communication. As in prior studies, racial disparity in prognostic understanding was observed, with nonwhite patients being more likely to have overly optimistic views of their prognosis [4,5].
While the perceived 2-year survival probability is a somewhat arbitrary measure of prognostic opinion, it provides a useful representation of how one views the expected trajectory of disease. A high perceived likelihood of 2-year survival implies a view that long-term disease control can be achieved, whereas a low perceived likelihood of 2-year survival implies acknowledgement of terminal illness. This study effectively contrasts patient and physician opinions of 2-year survival probability, but it does not discriminate among clinically relevant differences in opinions within the 0–2 year prognostic range. For example, a patient whose oncologist believes his prognosis is < 6 months may be an appropriate candidate for hospice, but the patient may be unprepared to make the transition to hospice if he believes his prognosis is closer to a year or more. While the patient and oncologist may agree that 2-year survival is unlikely, they may have differing beliefs about the appropriateness of certain interventions based on their discrepant short-term prognostic views. Additional studies looking at perceived probabilities of short-term survival may be helpful in assessing patients’ readiness to transition to symptom-focused care when medically appropriate.
The authors designate 7 categories of 2-year survival probability (100%, about 90%, about 75%, about 50%, about 25%, about 10%, and 0%). The differences in percentage between prognostic categories are not evenly distributed, and therefore definition of discordance is non-uniform. The smaller percentage difference at the highest and lowest ends of the scale may result in overestimation of discordance at these extremes. For example, a patient rating her 2-year survival probability at 100% would be defined as having a discordant viewpoint from an oncologist rating her 2-year survival at 75% (as would be realistic for a diagnosis such as metastatic colon cancer). Given the imprecise nature of prognostication, the views of the patient and oncologist in this example are arguably similar, and perhaps should not be categorized as discordant.
As noted, patients already enrolled in hospice were excluded from the study, thus omitting a key group of patients whose prognostic views are more likely to be concordant with their physicians’ views. This group may be better captured in a prospective study of prognostic discordance among newly diagnosed advanced cancer patients after initial oncology consultation, allowing for inclusion of those who make an early transition to hospice.
Applications for Clinical Practice
Although clinicians tend to overestimate prognosis, their predictions correlate with outcomes in advanced cancer [6], and may therefore provide a useful framework for patients to understand the likely course of their disease. However, physicians often avoid explicit discussion of prognosis by shrouding prognostic information in discussions of radiographic findings, and quickly transitioning to discussion of treatment options [7]. Patients and families rarely inquire about prognosis, further limiting disclosure of prognostic information [7,8]. Even when prognostic information is explicitly stated, patients may misinterpret the information [4], potentially adversely affecting their ability to participate in shared decision making.
Some useful approaches for successfully communicating prognostic information may include asking patients what information they wish to hear before it is disclosed, providing prognostic data for patients with similar disease states while acknowledging individual variability, clearly defining the intent of proposed therapy (ie, curative versus noncurative), and asking the patient to restate information in order to assess understanding. Early involvement of palliative care specialists may help reinforce understanding about prognosis and goals of therapy, facilitate advance care planning, and reduce aggressive interventions at the end of life [2]. Ongoing research is directed at identifying effective interventions to improve communication between patients with advanced cancer and their oncologists [9].
—Irene M. Hutchins, MD
Scripps Cancer Center, La Jolla, CA
1. Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA 1998;279:1709–14.
2. Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–26.
3. Pronzato P, Bertelli G, Losardo P, Landucci M. What do advanced cancer patients know of their disease? A report from Italy. Support Care Cancer 1994;2:242–4.
4. Weeks JC, Catalano PJ, Cronin A, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–25.
5. Ford D, Zapka J, Gebregziabher M, et al. Factors associated with illness perception among critically ill patients and surrogates. Chest 2010;138:59–67.
6. Glare P, Virik K, Jones M, et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ 2003;327:195–8.
7. Singh S, Cortez D, Maynard D, et al. Characterizing the nature of scan results discussions: insights into why patients misunderstand their prognosis. J Oncol Pract 2017:JOP2016014621.
8. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909–13.
9. Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer 2013;13:188.
1. Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA 1998;279:1709–14.
2. Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–26.
3. Pronzato P, Bertelli G, Losardo P, Landucci M. What do advanced cancer patients know of their disease? A report from Italy. Support Care Cancer 1994;2:242–4.
4. Weeks JC, Catalano PJ, Cronin A, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–25.
5. Ford D, Zapka J, Gebregziabher M, et al. Factors associated with illness perception among critically ill patients and surrogates. Chest 2010;138:59–67.
6. Glare P, Virik K, Jones M, et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ 2003;327:195–8.
7. Singh S, Cortez D, Maynard D, et al. Characterizing the nature of scan results discussions: insights into why patients misunderstand their prognosis. J Oncol Pract 2017:JOP2016014621.
8. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909–13.
9. Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer 2013;13:188.
Prostate Cancer in Seniors Part 1: Epidemiology, Pathology, and Screening
Prostate cancer is the most common cancer and the second leading cause of cancer deaths in men. The incidence of prostate cancer continues to rise. Roughly 220,800 men were expected to be newly diagnosed with prostate cancer in 2015.1 As the population ages and overall life expectancy increases, prostate cancer is likely to become a growing health care burden, especially because prostate cancer is primarily a disease of elderly males.
There have been no specific practice guidelines for managing prostate cancer in older adults, and the current management of older patients with prostate cancer is often suboptimal. Fortunately, the International Society of Geriatric Oncology recently assembled a multidisciplinary prostate cancer working group, which has begun offering guidelines on evidence-based treatments of prostate cancer in the geriatric population.
This article (part 1 of 2) provides a brief overview of prostate cancer epidemiology, pathology and screening in senior patients. The second part (to be published in August 2015) will focus on treatment.
Epidemiology
Currently more than 2 million men are estimated to have prostate cancer in the U.S. About 18% to 20% of U.S. males have a lifetime risk of developing prostate
cancer. Prostate cancer is mainly a disease of seniors aged between 60 and 70 years—the median age of prostate cancer at diagnosis is about 65 to 68 years. About 65% of new prostate cancers are diagnosed in males aged 65 years and 25% in males > aged 75 years.2 Most older patients with prostate cancer do not die of prostate cancer.
As the life expectancy of the general population increases, the risk of developing prostate cancer among seniors is also expected to proportionally rise. Historically, the cancer-specific mortality rate of prostate cancer in patients aged > 70 years was only 29% if managed either with active surveillance or hormonal manipulation.
Prevalence of Incidental Prostate Cancer
There is an abrupt age-dependent increase of prostate cancer incidence from the 5th decade of life on. Furthermore, there is a 1 in 3 chance of incidental prostate cancer in men aged between 60 to 69 years and a 46% prevalence in men aged > 70 years. Yin and colleagues found that 12% of patients in their study group harbored incidental, preclinical prostate cancer.3-5 The increasing prostate cancer incidence showed a strong and clear correlation with advancing age (Figure 1).
The lifetime probability of being diagnosed with prostate cancer also increases significantly with age.6,7 Patients with a life expectancy of < 5 years are unlikely
to benefit from cancer screening and may be more likely to experience complications and potential treatment-related harm as a result of screening. Therefore, estimating the patient’s residual life expectancy is a critical factor in the decision-making process for patients with prostate cancer. Life expectancy can differ, depending on various factors besides age, such as health, functional status, and medical comorbidities. The estimated age-related life expectancy for seniors has gradually increased over the previous 5 decades.8
Risk Factors
There are several risk factors for prostate cancer: age, race, and ethnicity; genetic factors; environmental and socioeconomic status; dietary status; and others. However, these factors may play only a limited role in the risk of prostate cancer, and a cautious approach and careful interpretation are required for their application in clinical practice.9,10
- Age. There is a sudden and dramatic increase in the prevalence of prostate cancer with advancing age. Prostate cancer is rarely diagnosed in men aged < 40 years, but thereafter, the incidence of prostate cancer climbs steadily.11 Surprisingly, subclinical microscopic prostate cancer was found at autopsy (death from unrelated causes) in a majority of senior males in their eighth decade of life.3
- Race/ethnicity. Epidemiologic studies in the U.S. found the highest incidence of prostate cancer in African American men (incidence rate of 235 per 100,000 African American vs 150 per 100,000 white men). Also, African American men tended to present with higher grades and stages of prostate cancer. There were much lower incidence rates of prostate cancer in Asian Americans and Pacific Islanders, Hispanics, and American Indian and Alaska Natives (90 per 100,000, 126 per 100,000, and 78 per 100,000, respectively).9,10
- Diet. According to researchers, the western diet may be an important risk factors for prostate cancer. However, the actual relationship between obesity and prostate cancer is somewhat unclear, and any correlation is at present highly controversial. Some investigators have postulated that obesity can contribute to the development of prostate cancer; other studies have clearly established that obese patients, once diagnosed with prostate cancer, have inferior outcomes irrespective of the treatment modality used. Other studies, however, have suggested that certain hormonal profiles related to obesity may be protective against the development of prostate cancer.12,13
Pathologic Evaluation
The original Gleason Grading System was devised based on the careful analysis of the cellular pattern of tumor architecture, using a 5-point scale: Tumor cells similar to normal-appearing prostate tissue were designated Gleason 1, 2, and 3; whereas cells/glands appearing abnormal were designated Gleason 4 and 5. The total Gleason score is the sum of the 2 most representative patterns, applied to both prostatectomy and needle biopsy specimens. The main differences from the original Gleason system, proposed by the 2005 International Society of Urological Pathology Modified Gleason System, are summarized in Table 1.
Early Detection and Screening
Although prostate cancer screening with prostate-specific antigen (PSA) detects many prostate cancer cases, concerns surrounding universal screening include the potential for overdiagnosis and overtreatment, along with the real possibility for adverse effects and complications from treatment. In addition, the recommendations for prostate cancer screening are not consistent among the various national health organizations. The American Cancer Society (ACS) recommends having an informed discussion between the health care provider and patient about the possible benefits and harms of screening. The discussion should not be initiated in men aged < 50 years (or aged < 45 years in men with high-risk features), and there is no need for screening in men with a life expectancy of < 10 years.
Prostate cancer screening may detect cancers that would not have become clinically significant. This is even more likely to be true when life expectancy decreases. Informed screening decisions in senior adults should be made according to the individual’s values and preferences in addition to the estimated outcomes and possible harms as a result of screening. The National Comprehensive Cancer Network offers similar recommendation to the ACS Screening Guidelines (Table 2).
Screening Recommendations for Seniors
There have been no generally recognized guidelines on prostate cancer screening for seniors, although recently, Konety and colleagues published “The Iowa Prostate Cancer Consensus” for elderly prostate cancer patients (Table 3).17 The consensus includes:
- More prostate cancers are detected at an earlier stage, but many of them would never become clinically apparent in most patients’ life times
- A reduced mortality (either overall or disease specific) from screening is not proven during the course of 10-year follow-up
- Harms related to diagnostic and therapeutic procedures develop early and remain for an extended period, causing a negative impact on quality of life
- The small benefits of screening leading up to a prostatectomy are seen only after 12 years of follow-up and may be limited to a certain population group of
patients who are aged < 65 years - Current recommendations discourage the routine screening of seniors with short life expectancies (< 10 years) and depend on existing comorbidities and disease group risk
Conclusion
Prostate cancer is the most common cancer in American men and the second most common cause of cancer death. Prostate cancer is almost twice as common among African Americans vs whites, and much less common in Asian Americans and Pacific Islanders, Hispanics, American Indian and Alaska Natives. Prostate cancer is generally a cancer of older seniors, and nearly 80% of seniors are estimated to harbor subclinical prostate cancer by their eighth decade of life.8 Prostate cancer screening is not universally recommended, and major professional associations support an informed, evidence-based, shared decision-making process between medical professionals and patients. This decision should include the careful consideration of patients’ life expectancy and existing medical comorbidities, always weighing the potential benefits against the possible screening and treatment-related harms.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin.2015;65(1):5-29.
2. Fitzpatrick JM. Management of localized prostate cancer in senior adults: the crucial role of comorbidity. BJU Int. 2008;101(suppl 2):16-22.
3. Yin M, Bastacky S, Chandran U, Becich MJ, Dhir R. Prevalence of incidental prostate cancer in the general population: a study of healthy organ donors. J Urol. 2008;179(3):892-895.
4. Soos G, Tsakiris I, Szanto J, Turzo C, Haas PG, Dezso B.. The prevalence of prostate carcinoma and its precursor in Hungary: an autopsy study. Euro Urol. 2005;48(5):739-744.
5. Sánchez-Chapado M, Olmedilla G, Cabeza M, Donat E, Ruiz A. Prevalence of prostate cancer and prostatic intraepithelial neoplasia in Caucasian Mediterranean males: an autopsy study. Prostate. 2003;54(3):238-247.
6. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71-96.
7. Sun L, Caire AA, Robertson CN, et al. Men older than 70 years have higher risk prostate cancer and poorer survival in the early and late prostate specific antigen eras. J Urol. 2009;182(5):2242-2248.
8. Haas GP, Sakr WA. Epidemiology of prostate cancer. CA Cancer J Clin. 1997;47(5):273-287.
9. Miocinovic R. Epidemiology and risk factors. In: Klein EA, Jones JP, eds. Management of Prostate Cancer. 3rd ed. Totowa, NJ: Humana Press; 2013:1-11.
10. Crawford ED. Epidemiology of prostate cancer. Urology. 2003;62(6 suppl 1):3-12.
11. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277-300.
12. Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC. Height, body weight, and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev. 1997;6(8):557-563.
13. Gann PH, Hennekens CH, Ma J, Longcope C, Stampfer MJ. Prospective
study of sex hormone levels and risk of prostate cancer. J Natl Cancer Inst. 1996;88(16):1118-1126.
14. Epstein JI. An update of the Gleason grading system. J Urol. 2010;183(2):433-440.
15. Egevad L, Mazzucchelli R, Montironi R. Implications of the International Society of Urological Pathology modified Gleason grading system. Arch Pathol Lab Med. 2012;136(4):426-434.
16. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL; ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostate Carcinoma. Am J Surg Pathol. 2005;29(9): 1228-1242.
17. Konety BR, Sharp VJ, Raut H, Williams RD. Screening and management of prostate cancer in elderly men: the Iowa Prostate Cancer Consensus. Urology. 2008;71(3):511-514.
Prostate cancer is the most common cancer and the second leading cause of cancer deaths in men. The incidence of prostate cancer continues to rise. Roughly 220,800 men were expected to be newly diagnosed with prostate cancer in 2015.1 As the population ages and overall life expectancy increases, prostate cancer is likely to become a growing health care burden, especially because prostate cancer is primarily a disease of elderly males.
There have been no specific practice guidelines for managing prostate cancer in older adults, and the current management of older patients with prostate cancer is often suboptimal. Fortunately, the International Society of Geriatric Oncology recently assembled a multidisciplinary prostate cancer working group, which has begun offering guidelines on evidence-based treatments of prostate cancer in the geriatric population.
This article (part 1 of 2) provides a brief overview of prostate cancer epidemiology, pathology and screening in senior patients. The second part (to be published in August 2015) will focus on treatment.
Epidemiology
Currently more than 2 million men are estimated to have prostate cancer in the U.S. About 18% to 20% of U.S. males have a lifetime risk of developing prostate
cancer. Prostate cancer is mainly a disease of seniors aged between 60 and 70 years—the median age of prostate cancer at diagnosis is about 65 to 68 years. About 65% of new prostate cancers are diagnosed in males aged 65 years and 25% in males > aged 75 years.2 Most older patients with prostate cancer do not die of prostate cancer.
As the life expectancy of the general population increases, the risk of developing prostate cancer among seniors is also expected to proportionally rise. Historically, the cancer-specific mortality rate of prostate cancer in patients aged > 70 years was only 29% if managed either with active surveillance or hormonal manipulation.
Prevalence of Incidental Prostate Cancer
There is an abrupt age-dependent increase of prostate cancer incidence from the 5th decade of life on. Furthermore, there is a 1 in 3 chance of incidental prostate cancer in men aged between 60 to 69 years and a 46% prevalence in men aged > 70 years. Yin and colleagues found that 12% of patients in their study group harbored incidental, preclinical prostate cancer.3-5 The increasing prostate cancer incidence showed a strong and clear correlation with advancing age (Figure 1).
The lifetime probability of being diagnosed with prostate cancer also increases significantly with age.6,7 Patients with a life expectancy of < 5 years are unlikely
to benefit from cancer screening and may be more likely to experience complications and potential treatment-related harm as a result of screening. Therefore, estimating the patient’s residual life expectancy is a critical factor in the decision-making process for patients with prostate cancer. Life expectancy can differ, depending on various factors besides age, such as health, functional status, and medical comorbidities. The estimated age-related life expectancy for seniors has gradually increased over the previous 5 decades.8
Risk Factors
There are several risk factors for prostate cancer: age, race, and ethnicity; genetic factors; environmental and socioeconomic status; dietary status; and others. However, these factors may play only a limited role in the risk of prostate cancer, and a cautious approach and careful interpretation are required for their application in clinical practice.9,10
- Age. There is a sudden and dramatic increase in the prevalence of prostate cancer with advancing age. Prostate cancer is rarely diagnosed in men aged < 40 years, but thereafter, the incidence of prostate cancer climbs steadily.11 Surprisingly, subclinical microscopic prostate cancer was found at autopsy (death from unrelated causes) in a majority of senior males in their eighth decade of life.3
- Race/ethnicity. Epidemiologic studies in the U.S. found the highest incidence of prostate cancer in African American men (incidence rate of 235 per 100,000 African American vs 150 per 100,000 white men). Also, African American men tended to present with higher grades and stages of prostate cancer. There were much lower incidence rates of prostate cancer in Asian Americans and Pacific Islanders, Hispanics, and American Indian and Alaska Natives (90 per 100,000, 126 per 100,000, and 78 per 100,000, respectively).9,10
- Diet. According to researchers, the western diet may be an important risk factors for prostate cancer. However, the actual relationship between obesity and prostate cancer is somewhat unclear, and any correlation is at present highly controversial. Some investigators have postulated that obesity can contribute to the development of prostate cancer; other studies have clearly established that obese patients, once diagnosed with prostate cancer, have inferior outcomes irrespective of the treatment modality used. Other studies, however, have suggested that certain hormonal profiles related to obesity may be protective against the development of prostate cancer.12,13
Pathologic Evaluation
The original Gleason Grading System was devised based on the careful analysis of the cellular pattern of tumor architecture, using a 5-point scale: Tumor cells similar to normal-appearing prostate tissue were designated Gleason 1, 2, and 3; whereas cells/glands appearing abnormal were designated Gleason 4 and 5. The total Gleason score is the sum of the 2 most representative patterns, applied to both prostatectomy and needle biopsy specimens. The main differences from the original Gleason system, proposed by the 2005 International Society of Urological Pathology Modified Gleason System, are summarized in Table 1.
Early Detection and Screening
Although prostate cancer screening with prostate-specific antigen (PSA) detects many prostate cancer cases, concerns surrounding universal screening include the potential for overdiagnosis and overtreatment, along with the real possibility for adverse effects and complications from treatment. In addition, the recommendations for prostate cancer screening are not consistent among the various national health organizations. The American Cancer Society (ACS) recommends having an informed discussion between the health care provider and patient about the possible benefits and harms of screening. The discussion should not be initiated in men aged < 50 years (or aged < 45 years in men with high-risk features), and there is no need for screening in men with a life expectancy of < 10 years.
Prostate cancer screening may detect cancers that would not have become clinically significant. This is even more likely to be true when life expectancy decreases. Informed screening decisions in senior adults should be made according to the individual’s values and preferences in addition to the estimated outcomes and possible harms as a result of screening. The National Comprehensive Cancer Network offers similar recommendation to the ACS Screening Guidelines (Table 2).
Screening Recommendations for Seniors
There have been no generally recognized guidelines on prostate cancer screening for seniors, although recently, Konety and colleagues published “The Iowa Prostate Cancer Consensus” for elderly prostate cancer patients (Table 3).17 The consensus includes:
- More prostate cancers are detected at an earlier stage, but many of them would never become clinically apparent in most patients’ life times
- A reduced mortality (either overall or disease specific) from screening is not proven during the course of 10-year follow-up
- Harms related to diagnostic and therapeutic procedures develop early and remain for an extended period, causing a negative impact on quality of life
- The small benefits of screening leading up to a prostatectomy are seen only after 12 years of follow-up and may be limited to a certain population group of
patients who are aged < 65 years - Current recommendations discourage the routine screening of seniors with short life expectancies (< 10 years) and depend on existing comorbidities and disease group risk
Conclusion
Prostate cancer is the most common cancer in American men and the second most common cause of cancer death. Prostate cancer is almost twice as common among African Americans vs whites, and much less common in Asian Americans and Pacific Islanders, Hispanics, American Indian and Alaska Natives. Prostate cancer is generally a cancer of older seniors, and nearly 80% of seniors are estimated to harbor subclinical prostate cancer by their eighth decade of life.8 Prostate cancer screening is not universally recommended, and major professional associations support an informed, evidence-based, shared decision-making process between medical professionals and patients. This decision should include the careful consideration of patients’ life expectancy and existing medical comorbidities, always weighing the potential benefits against the possible screening and treatment-related harms.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
Prostate cancer is the most common cancer and the second leading cause of cancer deaths in men. The incidence of prostate cancer continues to rise. Roughly 220,800 men were expected to be newly diagnosed with prostate cancer in 2015.1 As the population ages and overall life expectancy increases, prostate cancer is likely to become a growing health care burden, especially because prostate cancer is primarily a disease of elderly males.
There have been no specific practice guidelines for managing prostate cancer in older adults, and the current management of older patients with prostate cancer is often suboptimal. Fortunately, the International Society of Geriatric Oncology recently assembled a multidisciplinary prostate cancer working group, which has begun offering guidelines on evidence-based treatments of prostate cancer in the geriatric population.
This article (part 1 of 2) provides a brief overview of prostate cancer epidemiology, pathology and screening in senior patients. The second part (to be published in August 2015) will focus on treatment.
Epidemiology
Currently more than 2 million men are estimated to have prostate cancer in the U.S. About 18% to 20% of U.S. males have a lifetime risk of developing prostate
cancer. Prostate cancer is mainly a disease of seniors aged between 60 and 70 years—the median age of prostate cancer at diagnosis is about 65 to 68 years. About 65% of new prostate cancers are diagnosed in males aged 65 years and 25% in males > aged 75 years.2 Most older patients with prostate cancer do not die of prostate cancer.
As the life expectancy of the general population increases, the risk of developing prostate cancer among seniors is also expected to proportionally rise. Historically, the cancer-specific mortality rate of prostate cancer in patients aged > 70 years was only 29% if managed either with active surveillance or hormonal manipulation.
Prevalence of Incidental Prostate Cancer
There is an abrupt age-dependent increase of prostate cancer incidence from the 5th decade of life on. Furthermore, there is a 1 in 3 chance of incidental prostate cancer in men aged between 60 to 69 years and a 46% prevalence in men aged > 70 years. Yin and colleagues found that 12% of patients in their study group harbored incidental, preclinical prostate cancer.3-5 The increasing prostate cancer incidence showed a strong and clear correlation with advancing age (Figure 1).
The lifetime probability of being diagnosed with prostate cancer also increases significantly with age.6,7 Patients with a life expectancy of < 5 years are unlikely
to benefit from cancer screening and may be more likely to experience complications and potential treatment-related harm as a result of screening. Therefore, estimating the patient’s residual life expectancy is a critical factor in the decision-making process for patients with prostate cancer. Life expectancy can differ, depending on various factors besides age, such as health, functional status, and medical comorbidities. The estimated age-related life expectancy for seniors has gradually increased over the previous 5 decades.8
Risk Factors
There are several risk factors for prostate cancer: age, race, and ethnicity; genetic factors; environmental and socioeconomic status; dietary status; and others. However, these factors may play only a limited role in the risk of prostate cancer, and a cautious approach and careful interpretation are required for their application in clinical practice.9,10
- Age. There is a sudden and dramatic increase in the prevalence of prostate cancer with advancing age. Prostate cancer is rarely diagnosed in men aged < 40 years, but thereafter, the incidence of prostate cancer climbs steadily.11 Surprisingly, subclinical microscopic prostate cancer was found at autopsy (death from unrelated causes) in a majority of senior males in their eighth decade of life.3
- Race/ethnicity. Epidemiologic studies in the U.S. found the highest incidence of prostate cancer in African American men (incidence rate of 235 per 100,000 African American vs 150 per 100,000 white men). Also, African American men tended to present with higher grades and stages of prostate cancer. There were much lower incidence rates of prostate cancer in Asian Americans and Pacific Islanders, Hispanics, and American Indian and Alaska Natives (90 per 100,000, 126 per 100,000, and 78 per 100,000, respectively).9,10
- Diet. According to researchers, the western diet may be an important risk factors for prostate cancer. However, the actual relationship between obesity and prostate cancer is somewhat unclear, and any correlation is at present highly controversial. Some investigators have postulated that obesity can contribute to the development of prostate cancer; other studies have clearly established that obese patients, once diagnosed with prostate cancer, have inferior outcomes irrespective of the treatment modality used. Other studies, however, have suggested that certain hormonal profiles related to obesity may be protective against the development of prostate cancer.12,13
Pathologic Evaluation
The original Gleason Grading System was devised based on the careful analysis of the cellular pattern of tumor architecture, using a 5-point scale: Tumor cells similar to normal-appearing prostate tissue were designated Gleason 1, 2, and 3; whereas cells/glands appearing abnormal were designated Gleason 4 and 5. The total Gleason score is the sum of the 2 most representative patterns, applied to both prostatectomy and needle biopsy specimens. The main differences from the original Gleason system, proposed by the 2005 International Society of Urological Pathology Modified Gleason System, are summarized in Table 1.
Early Detection and Screening
Although prostate cancer screening with prostate-specific antigen (PSA) detects many prostate cancer cases, concerns surrounding universal screening include the potential for overdiagnosis and overtreatment, along with the real possibility for adverse effects and complications from treatment. In addition, the recommendations for prostate cancer screening are not consistent among the various national health organizations. The American Cancer Society (ACS) recommends having an informed discussion between the health care provider and patient about the possible benefits and harms of screening. The discussion should not be initiated in men aged < 50 years (or aged < 45 years in men with high-risk features), and there is no need for screening in men with a life expectancy of < 10 years.
Prostate cancer screening may detect cancers that would not have become clinically significant. This is even more likely to be true when life expectancy decreases. Informed screening decisions in senior adults should be made according to the individual’s values and preferences in addition to the estimated outcomes and possible harms as a result of screening. The National Comprehensive Cancer Network offers similar recommendation to the ACS Screening Guidelines (Table 2).
Screening Recommendations for Seniors
There have been no generally recognized guidelines on prostate cancer screening for seniors, although recently, Konety and colleagues published “The Iowa Prostate Cancer Consensus” for elderly prostate cancer patients (Table 3).17 The consensus includes:
- More prostate cancers are detected at an earlier stage, but many of them would never become clinically apparent in most patients’ life times
- A reduced mortality (either overall or disease specific) from screening is not proven during the course of 10-year follow-up
- Harms related to diagnostic and therapeutic procedures develop early and remain for an extended period, causing a negative impact on quality of life
- The small benefits of screening leading up to a prostatectomy are seen only after 12 years of follow-up and may be limited to a certain population group of
patients who are aged < 65 years - Current recommendations discourage the routine screening of seniors with short life expectancies (< 10 years) and depend on existing comorbidities and disease group risk
Conclusion
Prostate cancer is the most common cancer in American men and the second most common cause of cancer death. Prostate cancer is almost twice as common among African Americans vs whites, and much less common in Asian Americans and Pacific Islanders, Hispanics, American Indian and Alaska Natives. Prostate cancer is generally a cancer of older seniors, and nearly 80% of seniors are estimated to harbor subclinical prostate cancer by their eighth decade of life.8 Prostate cancer screening is not universally recommended, and major professional associations support an informed, evidence-based, shared decision-making process between medical professionals and patients. This decision should include the careful consideration of patients’ life expectancy and existing medical comorbidities, always weighing the potential benefits against the possible screening and treatment-related harms.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin.2015;65(1):5-29.
2. Fitzpatrick JM. Management of localized prostate cancer in senior adults: the crucial role of comorbidity. BJU Int. 2008;101(suppl 2):16-22.
3. Yin M, Bastacky S, Chandran U, Becich MJ, Dhir R. Prevalence of incidental prostate cancer in the general population: a study of healthy organ donors. J Urol. 2008;179(3):892-895.
4. Soos G, Tsakiris I, Szanto J, Turzo C, Haas PG, Dezso B.. The prevalence of prostate carcinoma and its precursor in Hungary: an autopsy study. Euro Urol. 2005;48(5):739-744.
5. Sánchez-Chapado M, Olmedilla G, Cabeza M, Donat E, Ruiz A. Prevalence of prostate cancer and prostatic intraepithelial neoplasia in Caucasian Mediterranean males: an autopsy study. Prostate. 2003;54(3):238-247.
6. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71-96.
7. Sun L, Caire AA, Robertson CN, et al. Men older than 70 years have higher risk prostate cancer and poorer survival in the early and late prostate specific antigen eras. J Urol. 2009;182(5):2242-2248.
8. Haas GP, Sakr WA. Epidemiology of prostate cancer. CA Cancer J Clin. 1997;47(5):273-287.
9. Miocinovic R. Epidemiology and risk factors. In: Klein EA, Jones JP, eds. Management of Prostate Cancer. 3rd ed. Totowa, NJ: Humana Press; 2013:1-11.
10. Crawford ED. Epidemiology of prostate cancer. Urology. 2003;62(6 suppl 1):3-12.
11. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277-300.
12. Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC. Height, body weight, and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev. 1997;6(8):557-563.
13. Gann PH, Hennekens CH, Ma J, Longcope C, Stampfer MJ. Prospective
study of sex hormone levels and risk of prostate cancer. J Natl Cancer Inst. 1996;88(16):1118-1126.
14. Epstein JI. An update of the Gleason grading system. J Urol. 2010;183(2):433-440.
15. Egevad L, Mazzucchelli R, Montironi R. Implications of the International Society of Urological Pathology modified Gleason grading system. Arch Pathol Lab Med. 2012;136(4):426-434.
16. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL; ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostate Carcinoma. Am J Surg Pathol. 2005;29(9): 1228-1242.
17. Konety BR, Sharp VJ, Raut H, Williams RD. Screening and management of prostate cancer in elderly men: the Iowa Prostate Cancer Consensus. Urology. 2008;71(3):511-514.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin.2015;65(1):5-29.
2. Fitzpatrick JM. Management of localized prostate cancer in senior adults: the crucial role of comorbidity. BJU Int. 2008;101(suppl 2):16-22.
3. Yin M, Bastacky S, Chandran U, Becich MJ, Dhir R. Prevalence of incidental prostate cancer in the general population: a study of healthy organ donors. J Urol. 2008;179(3):892-895.
4. Soos G, Tsakiris I, Szanto J, Turzo C, Haas PG, Dezso B.. The prevalence of prostate carcinoma and its precursor in Hungary: an autopsy study. Euro Urol. 2005;48(5):739-744.
5. Sánchez-Chapado M, Olmedilla G, Cabeza M, Donat E, Ruiz A. Prevalence of prostate cancer and prostatic intraepithelial neoplasia in Caucasian Mediterranean males: an autopsy study. Prostate. 2003;54(3):238-247.
6. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71-96.
7. Sun L, Caire AA, Robertson CN, et al. Men older than 70 years have higher risk prostate cancer and poorer survival in the early and late prostate specific antigen eras. J Urol. 2009;182(5):2242-2248.
8. Haas GP, Sakr WA. Epidemiology of prostate cancer. CA Cancer J Clin. 1997;47(5):273-287.
9. Miocinovic R. Epidemiology and risk factors. In: Klein EA, Jones JP, eds. Management of Prostate Cancer. 3rd ed. Totowa, NJ: Humana Press; 2013:1-11.
10. Crawford ED. Epidemiology of prostate cancer. Urology. 2003;62(6 suppl 1):3-12.
11. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277-300.
12. Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC. Height, body weight, and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev. 1997;6(8):557-563.
13. Gann PH, Hennekens CH, Ma J, Longcope C, Stampfer MJ. Prospective
study of sex hormone levels and risk of prostate cancer. J Natl Cancer Inst. 1996;88(16):1118-1126.
14. Epstein JI. An update of the Gleason grading system. J Urol. 2010;183(2):433-440.
15. Egevad L, Mazzucchelli R, Montironi R. Implications of the International Society of Urological Pathology modified Gleason grading system. Arch Pathol Lab Med. 2012;136(4):426-434.
16. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL; ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostate Carcinoma. Am J Surg Pathol. 2005;29(9): 1228-1242.
17. Konety BR, Sharp VJ, Raut H, Williams RD. Screening and management of prostate cancer in elderly men: the Iowa Prostate Cancer Consensus. Urology. 2008;71(3):511-514.