User login
Study: Quality of care may not determine pneumonia readmissions
Lower quality of care was not associated with pneumonia readmissions, according to a study using a commercially available software program to examine possibly preventable readmissions.
Rates of hospital readmission are now being used to demonstrate hospital performance and the Centers for Medicare & Medicaid Services may even penalize hospitals with high rates of readmissions. As a result, it has become increasingly important to recognize clinical situations that may lead to a potentially preventable readmission.
The Potentially Preventable Readmission (PPRs) software was developed by 3M Health Information Systems to identify such cases and is being adopted by some state Medicaid programs for hospital payment and reporting. Dr. Ann M. Borzecki of the Center for Healthcare Organization and Implementation Research in Bedford, Mass., and her colleagues sought to understand if patients with pneumonia flagged by the PPR software as preventable readmissions were associated with failures in the process of care.
The investigators conducted a cross-sectional retrospective observational study with Veterans Affairs electronic medical record (EMR) data from October 2005 to September 2010. Patients with diagnoses of pneumonia and a 30-day readmission were identified and then flagged as PPR-yes (for example, readmissions associated with quality of care problems) vs. PPR-no, using the 3M PPR software. A tool to measure quality of care was applied to 100 random readmissions abstracted for full review. The study was published online Sept. 14 in BMJ Quality and Safety. (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-003911).
Of all the pneumonia readmission cases, 72% were PPR-yes vs.77% of the 100 abstracted cases. There were no significant differences between the groups other than a trend toward more comorbidity in the PPR-yes group.
After researchers adjusted for comorbidities and demographics, they noted no significant difference in quality of care between the PPR-yes and PPR-no groups. Interestingly, the PPR-yes group had slightly higher quality scores than did the PPR-no group (total scores, 71.2 vs. 65.8 respectively, P = .14).
The authors write, “Among veterans readmitted after a pneumonia discharge, we found no significant difference in quality of care, as measured by processes of care received during the index admission and after discharge, between cases flagged as PPRs and nonflagged cases. Indeed, contrary to our hypothesis, quality scores were slightly higher among PPR-flagged cases.”
The authors emphasized that causes of readmissions are multifaceted and many aspects may be out of the control of the hospital. However, they noted a concern for a lack of postdischarge documentation and emphasized the need for thorough documentation at all levels of care.
The authors report no competing interest. The study was funded by the U.S. Department of Veterans Affairs Health Service Research and Development Service.
Even with potentially preventable readmissions having a slightly higher, although not significant, quality score, the question remains: Do the flagged cases actually represent avoidable readmissions? The results bring up further questions on including preventable readmissions in quality measures.
Rates of readmission may reflect several aspects of care including the patient’s financial, environmental, and psychosocial factors. Furthermore, failure to address patient factors that contribute to readmission rates may abate hospital interventions to prevent those readmissions.
Dr. Christine Soong is affiliated with Mount Sinai Hospital in Toronto. These comments are taken from an accompanying editorial (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-004484). No competing interests were declared.
Even with potentially preventable readmissions having a slightly higher, although not significant, quality score, the question remains: Do the flagged cases actually represent avoidable readmissions? The results bring up further questions on including preventable readmissions in quality measures.
Rates of readmission may reflect several aspects of care including the patient’s financial, environmental, and psychosocial factors. Furthermore, failure to address patient factors that contribute to readmission rates may abate hospital interventions to prevent those readmissions.
Dr. Christine Soong is affiliated with Mount Sinai Hospital in Toronto. These comments are taken from an accompanying editorial (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-004484). No competing interests were declared.
Even with potentially preventable readmissions having a slightly higher, although not significant, quality score, the question remains: Do the flagged cases actually represent avoidable readmissions? The results bring up further questions on including preventable readmissions in quality measures.
Rates of readmission may reflect several aspects of care including the patient’s financial, environmental, and psychosocial factors. Furthermore, failure to address patient factors that contribute to readmission rates may abate hospital interventions to prevent those readmissions.
Dr. Christine Soong is affiliated with Mount Sinai Hospital in Toronto. These comments are taken from an accompanying editorial (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-004484). No competing interests were declared.
Lower quality of care was not associated with pneumonia readmissions, according to a study using a commercially available software program to examine possibly preventable readmissions.
Rates of hospital readmission are now being used to demonstrate hospital performance and the Centers for Medicare & Medicaid Services may even penalize hospitals with high rates of readmissions. As a result, it has become increasingly important to recognize clinical situations that may lead to a potentially preventable readmission.
The Potentially Preventable Readmission (PPRs) software was developed by 3M Health Information Systems to identify such cases and is being adopted by some state Medicaid programs for hospital payment and reporting. Dr. Ann M. Borzecki of the Center for Healthcare Organization and Implementation Research in Bedford, Mass., and her colleagues sought to understand if patients with pneumonia flagged by the PPR software as preventable readmissions were associated with failures in the process of care.
The investigators conducted a cross-sectional retrospective observational study with Veterans Affairs electronic medical record (EMR) data from October 2005 to September 2010. Patients with diagnoses of pneumonia and a 30-day readmission were identified and then flagged as PPR-yes (for example, readmissions associated with quality of care problems) vs. PPR-no, using the 3M PPR software. A tool to measure quality of care was applied to 100 random readmissions abstracted for full review. The study was published online Sept. 14 in BMJ Quality and Safety. (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-003911).
Of all the pneumonia readmission cases, 72% were PPR-yes vs.77% of the 100 abstracted cases. There were no significant differences between the groups other than a trend toward more comorbidity in the PPR-yes group.
After researchers adjusted for comorbidities and demographics, they noted no significant difference in quality of care between the PPR-yes and PPR-no groups. Interestingly, the PPR-yes group had slightly higher quality scores than did the PPR-no group (total scores, 71.2 vs. 65.8 respectively, P = .14).
The authors write, “Among veterans readmitted after a pneumonia discharge, we found no significant difference in quality of care, as measured by processes of care received during the index admission and after discharge, between cases flagged as PPRs and nonflagged cases. Indeed, contrary to our hypothesis, quality scores were slightly higher among PPR-flagged cases.”
The authors emphasized that causes of readmissions are multifaceted and many aspects may be out of the control of the hospital. However, they noted a concern for a lack of postdischarge documentation and emphasized the need for thorough documentation at all levels of care.
The authors report no competing interest. The study was funded by the U.S. Department of Veterans Affairs Health Service Research and Development Service.
Lower quality of care was not associated with pneumonia readmissions, according to a study using a commercially available software program to examine possibly preventable readmissions.
Rates of hospital readmission are now being used to demonstrate hospital performance and the Centers for Medicare & Medicaid Services may even penalize hospitals with high rates of readmissions. As a result, it has become increasingly important to recognize clinical situations that may lead to a potentially preventable readmission.
The Potentially Preventable Readmission (PPRs) software was developed by 3M Health Information Systems to identify such cases and is being adopted by some state Medicaid programs for hospital payment and reporting. Dr. Ann M. Borzecki of the Center for Healthcare Organization and Implementation Research in Bedford, Mass., and her colleagues sought to understand if patients with pneumonia flagged by the PPR software as preventable readmissions were associated with failures in the process of care.
The investigators conducted a cross-sectional retrospective observational study with Veterans Affairs electronic medical record (EMR) data from October 2005 to September 2010. Patients with diagnoses of pneumonia and a 30-day readmission were identified and then flagged as PPR-yes (for example, readmissions associated with quality of care problems) vs. PPR-no, using the 3M PPR software. A tool to measure quality of care was applied to 100 random readmissions abstracted for full review. The study was published online Sept. 14 in BMJ Quality and Safety. (http://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2015-003911).
Of all the pneumonia readmission cases, 72% were PPR-yes vs.77% of the 100 abstracted cases. There were no significant differences between the groups other than a trend toward more comorbidity in the PPR-yes group.
After researchers adjusted for comorbidities and demographics, they noted no significant difference in quality of care between the PPR-yes and PPR-no groups. Interestingly, the PPR-yes group had slightly higher quality scores than did the PPR-no group (total scores, 71.2 vs. 65.8 respectively, P = .14).
The authors write, “Among veterans readmitted after a pneumonia discharge, we found no significant difference in quality of care, as measured by processes of care received during the index admission and after discharge, between cases flagged as PPRs and nonflagged cases. Indeed, contrary to our hypothesis, quality scores were slightly higher among PPR-flagged cases.”
The authors emphasized that causes of readmissions are multifaceted and many aspects may be out of the control of the hospital. However, they noted a concern for a lack of postdischarge documentation and emphasized the need for thorough documentation at all levels of care.
The authors report no competing interest. The study was funded by the U.S. Department of Veterans Affairs Health Service Research and Development Service.
BMJ QUALITY AND SAFETY
Key clinical point: A commercially available software program used to highlight possible preventable readmissions did not indicate cases with a lower quality of care in pneumonia readmissions.
Major finding: There was no significant difference in quality of care between groups of cases flagged by the software (PPR-yes) and groups not flagged (PPR-no), and the PPR-yes group actually had a slightly higher quality scores (total scores, 71.2 vs. 65.8 respectively, P = .14).
Data source: A cross-sectional retrospective observational study with Veterans Health Administration EMR data from October 2005 to September 2010.
Disclosures: The authors report no competing interest. The study was funded by the U.S. Department of Veterans Affairs Health Service Research and Development Service.
HbA1c aids prediction of atherosclerotic CVD
When combined with conventional risk factors, hemoglobin A1c modestly aids in prediction of atherosclerotic cardiovascular disease risk, according to a retrospective analysis published online Sept. 8 in Circulation: Cardiovascular Quality and Outcomes.
Conventional risk factors for CVD such as sex, age, blood pressure, smoking, or lipid level are important tools used to aid in clinical decision making. However, there is current debate about whether to include hemoglobin A1c in the algorithms, despite the clear association of CVD with glucose levels, said Jamie A. Jarmul of the University of North Carolina in Chapel Hill, and colleagues.
They used data from the 2011-2012 National Health and Nutrition Examination Survey (NHANES) to analyze CVD risk factors and HbA1c in 2,000 individuals aged 40-79 years without a history of diabetes or CVD. Utilizing a regression model, the distribution of HbA1c based on patient characteristics was predicted. The impact of the predicted HbA1c on the 10-year atherosclerotic CVD risk was calculated with the use of example clinical scenarios.
Factors considered significant predictors of HbA1c were HDL-cholesterol, total cholesterol, current smoking, sex, age, race/ethnicity, and systolic blood pressure. Further, individuals who were of black, Asian, or Hispanic race/ethnicity were associated with prediction of higher HbA1c.
The investigators noted that by using the final model, they found a modest effect of HbA1c on post-test atherosclerotic CVD risk in participants with intermediate risk. In the example clinical scenarios, an HbA1c of more than 6.5% was associated with increase in posttest atherosclerotic CVD risk by 1.0%-2.5% points. An HbA1c less than 5.7% was associated with a lowering of posttest atherosclerotic CVD risk by 0.4%-2.0% points (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.001639). The authors note the posttest atherosclerotic CVD risk of having an elevated HbA1c (greater than 6.5%) is similar to being 5 years older.
“The results we have presented here represent a necessary intermediate step before conducting these more comprehensive analyses assessing the utility of HbA1c testing in ASCVD [atherosclerotic cardiovascular disease] primary prevention and the larger question of universal screening for abnormal blood glucose levels,” the authors noted.
The National Institutes of Health supported the study. Dr. Pignone reports being a member of the U.S. Preventive Services Task Force (USPSTF).
With the modest effects of HbA1c on risk classification combined with its low cost, wide availability, and low risk, even a small improvement in cardiovascular disease risk prediction may add value to the current models.
However, utilizing biomarkers to create personalized risk prediction models has not seemed to return great results for CVD risk reclassification. Therefore, it may be time to consider alternative methods based on expert consensus.
Furthermore, it may be reasonable to move away from markers of the disease to detection with methods such as coronary artery calcium by noncontrast CT scan to detect the presence or, perhaps just as importantly, the absence of atherosclerosis.
Dr. Khurram Nasir is director of the Center for Healthcare Advancement and Outcomes in Coral Gables, Fla. These comments are taken from an accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.002207). Dr. Nasir reported consulting for Regeneron and being on the advisory board for Quest Diagnostic.
With the modest effects of HbA1c on risk classification combined with its low cost, wide availability, and low risk, even a small improvement in cardiovascular disease risk prediction may add value to the current models.
However, utilizing biomarkers to create personalized risk prediction models has not seemed to return great results for CVD risk reclassification. Therefore, it may be time to consider alternative methods based on expert consensus.
Furthermore, it may be reasonable to move away from markers of the disease to detection with methods such as coronary artery calcium by noncontrast CT scan to detect the presence or, perhaps just as importantly, the absence of atherosclerosis.
Dr. Khurram Nasir is director of the Center for Healthcare Advancement and Outcomes in Coral Gables, Fla. These comments are taken from an accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.002207). Dr. Nasir reported consulting for Regeneron and being on the advisory board for Quest Diagnostic.
With the modest effects of HbA1c on risk classification combined with its low cost, wide availability, and low risk, even a small improvement in cardiovascular disease risk prediction may add value to the current models.
However, utilizing biomarkers to create personalized risk prediction models has not seemed to return great results for CVD risk reclassification. Therefore, it may be time to consider alternative methods based on expert consensus.
Furthermore, it may be reasonable to move away from markers of the disease to detection with methods such as coronary artery calcium by noncontrast CT scan to detect the presence or, perhaps just as importantly, the absence of atherosclerosis.
Dr. Khurram Nasir is director of the Center for Healthcare Advancement and Outcomes in Coral Gables, Fla. These comments are taken from an accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.002207). Dr. Nasir reported consulting for Regeneron and being on the advisory board for Quest Diagnostic.
When combined with conventional risk factors, hemoglobin A1c modestly aids in prediction of atherosclerotic cardiovascular disease risk, according to a retrospective analysis published online Sept. 8 in Circulation: Cardiovascular Quality and Outcomes.
Conventional risk factors for CVD such as sex, age, blood pressure, smoking, or lipid level are important tools used to aid in clinical decision making. However, there is current debate about whether to include hemoglobin A1c in the algorithms, despite the clear association of CVD with glucose levels, said Jamie A. Jarmul of the University of North Carolina in Chapel Hill, and colleagues.
They used data from the 2011-2012 National Health and Nutrition Examination Survey (NHANES) to analyze CVD risk factors and HbA1c in 2,000 individuals aged 40-79 years without a history of diabetes or CVD. Utilizing a regression model, the distribution of HbA1c based on patient characteristics was predicted. The impact of the predicted HbA1c on the 10-year atherosclerotic CVD risk was calculated with the use of example clinical scenarios.
Factors considered significant predictors of HbA1c were HDL-cholesterol, total cholesterol, current smoking, sex, age, race/ethnicity, and systolic blood pressure. Further, individuals who were of black, Asian, or Hispanic race/ethnicity were associated with prediction of higher HbA1c.
The investigators noted that by using the final model, they found a modest effect of HbA1c on post-test atherosclerotic CVD risk in participants with intermediate risk. In the example clinical scenarios, an HbA1c of more than 6.5% was associated with increase in posttest atherosclerotic CVD risk by 1.0%-2.5% points. An HbA1c less than 5.7% was associated with a lowering of posttest atherosclerotic CVD risk by 0.4%-2.0% points (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.001639). The authors note the posttest atherosclerotic CVD risk of having an elevated HbA1c (greater than 6.5%) is similar to being 5 years older.
“The results we have presented here represent a necessary intermediate step before conducting these more comprehensive analyses assessing the utility of HbA1c testing in ASCVD [atherosclerotic cardiovascular disease] primary prevention and the larger question of universal screening for abnormal blood glucose levels,” the authors noted.
The National Institutes of Health supported the study. Dr. Pignone reports being a member of the U.S. Preventive Services Task Force (USPSTF).
When combined with conventional risk factors, hemoglobin A1c modestly aids in prediction of atherosclerotic cardiovascular disease risk, according to a retrospective analysis published online Sept. 8 in Circulation: Cardiovascular Quality and Outcomes.
Conventional risk factors for CVD such as sex, age, blood pressure, smoking, or lipid level are important tools used to aid in clinical decision making. However, there is current debate about whether to include hemoglobin A1c in the algorithms, despite the clear association of CVD with glucose levels, said Jamie A. Jarmul of the University of North Carolina in Chapel Hill, and colleagues.
They used data from the 2011-2012 National Health and Nutrition Examination Survey (NHANES) to analyze CVD risk factors and HbA1c in 2,000 individuals aged 40-79 years without a history of diabetes or CVD. Utilizing a regression model, the distribution of HbA1c based on patient characteristics was predicted. The impact of the predicted HbA1c on the 10-year atherosclerotic CVD risk was calculated with the use of example clinical scenarios.
Factors considered significant predictors of HbA1c were HDL-cholesterol, total cholesterol, current smoking, sex, age, race/ethnicity, and systolic blood pressure. Further, individuals who were of black, Asian, or Hispanic race/ethnicity were associated with prediction of higher HbA1c.
The investigators noted that by using the final model, they found a modest effect of HbA1c on post-test atherosclerotic CVD risk in participants with intermediate risk. In the example clinical scenarios, an HbA1c of more than 6.5% was associated with increase in posttest atherosclerotic CVD risk by 1.0%-2.5% points. An HbA1c less than 5.7% was associated with a lowering of posttest atherosclerotic CVD risk by 0.4%-2.0% points (Circ Cardiovasc Qual Outcomes. 2015 Sep 8. doi:10.1161/CIRCOUTCOMES.115.001639). The authors note the posttest atherosclerotic CVD risk of having an elevated HbA1c (greater than 6.5%) is similar to being 5 years older.
“The results we have presented here represent a necessary intermediate step before conducting these more comprehensive analyses assessing the utility of HbA1c testing in ASCVD [atherosclerotic cardiovascular disease] primary prevention and the larger question of universal screening for abnormal blood glucose levels,” the authors noted.
The National Institutes of Health supported the study. Dr. Pignone reports being a member of the U.S. Preventive Services Task Force (USPSTF).
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Hemoglobin A1c modestly aids in prediction of atherosclerotic CVD.
Major finding: In the example clinical scenarios, an HbA1c of greater than 6.5% was associated with increase in post-test atherosclerotic CVD risk by 1.0%-2.5% points and an HbA1c less than 5.7% was associated with a lowering of posttest atherosclerotic CVD risk by 0.4%-2.0% points.
Data source: The 2011-2012 National Health and Nutrition Examination Survey (NHANES).
Disclosures: The National Institutes of Health funded the study. Dr. Pignone reports being a member of the U.S. Preventive Services Task Force (USPSTF).
Diabetes Prevalence Rising, Especially in Black, Asian, and Hispanic Populations
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
FROM JAMA
Diabetes prevalence rising, especially in black, Asian, and Hispanic populations
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The decrease in amount of total diabetes that was undiagnosed may suggest that initiatives to encourage behavior changes in physical activity and diet may have started to impact the prevalence of obesity and secondarily the prevalence of diabetes.

|
Dr. William H. Herman |
Although the higher prevalence of undiagnosed diabetes in Asian Americans, younger patients, and Hispanic patients highlights disparities that exist, efforts to promote screening, identification of at-risk people, development of prevention programs, encouraging behavior change, and these data provide some hope.
The prevalence of total diabetes remained stable from 2008 to 2012. What explains the recent change in the upward trend? Perhaps it is this: “Providing insurance coverage for intensive behavioral therapies for obesity and using behavioral economic approaches to encourage their uptake are further removing barriers to patient engagement and are providing strong incentives for individual behavioral change.”
Dr. William H. Herman is affiliated with the department of internal medicine at the University of Michigan in Ann Arbor. These comments are taken from an accompanying editorial. Dr. Herman reported receiving personal fees from Merck Sharp & Dohme, Lexicon Pharmaceuticals, and Profil Institute for Clinical Research.
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
The prevalence of diabetes in the United States was 12% to 14% in 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Over the past decade, the prevalence of diabetes has increased, placing it as a major cause of mortality and morbidity in the United States.
Andy Menke, Ph.D., of Social & Scientific Systems, a biotechnology company in Silver Spring, Md., and his colleagues sought to estimate the U.S. trends and prevalence of prediabetes, total diabetes, diagnosed diabetes, and undiagnosed diabetes using data from the National Health and Nutrition Examination Survey (NHANES). Their results were published in the Journal of the American Medical Association online Sept. 8.
NHANES is a cross-sectional survey, conducted from 1988 to 1994 and 1999 to 2012. To estimate the most recent prevalence, the investigators sampled 2,781 adults from the 2011-2012 data and included 23,634 adults to estimate the trends from 1988 to 2010.
The prevalence of diabetes was determined based on a diagnosis of diabetes or evidence of based on fasting plasma glucose greater than 126 mg/dL, hemoglobin A1c of 6.5% or more, or 2-hour post prandial glucose greater than 200 mg/dL. Prediabetes was noted to be based on 2-hour post prandial glucose of 140-199 mg/dL, fasting plasma glucose of 100-125 mg/dL, or hemoglobin A1c of 5.7%-6.4%.
During 2011-2012, the prevalence of diabetes based on 2-hour post prandial glucose, fasting plasma glucose, or hemoglobin A1c was 14.3% for total diabetes (diagnosed and undiagnosed). Furthermore, the prevalence was 9.1% for diagnosed, 5.2% for undiagnosed, and 38% for prediabetes.
When compared to white individuals (11.3%), the age-standardized prevalence of diabetes was higher in Hispanic (22.6%, P less than .001), Asian (20.6%, P = .007), and black (21.8%, P less than .001) individuals. Likewise, Hispanics (29.7%, P = .003) and blacks (30.8%, P less than .001) tended to have higher BMIs compared to whites (28.4%). Asians tended to have lower BMIs (24.6%, P less than .001).
The age-standardized prevalence of undiagnosed diabetes was higher in Hispanic (49%, P = .02) and Asian (50.9%, P = .004) individuals than in other groups. However, the age-standardized prevalence of prediabetes was higher in blacks (39.6%) than in Asians (32.2%, P = .05).
When defining diabetes based on hemoglobin A1c or fasting plasma glucose alone, the authors found fewer people with undiagnosed diabetes. For example, the prevalence was 12.3% for total diabetes with 3.1% undiagnosed and 9.2% diagnosed. Furthermore, 36.5% of the study subjects qualified as prediabetic based on these definitions.
The age-standardized prevalance of diabetes increased from 9.8% to 12.4% during the 1988-1994 and 2011-2012 periods (P less than .001 trend). However, there was not much change in prevalence from 2007-2008 to 2011-2012 (12.5% to 12.4%).
The prevalence of diabetes significantly increased during the study time period in both sexes, all racial groups, education levels, incomes, and ages.
The amount of total diabetes that was undiagnosed decreased in most groups, including sex, racial groups, and most age groups. However, in Mexican American subjects the rate of undiagnosed diabetes actually increased over the study period (5.6% to 5.9%, P = .01). The increased prevalence of diabetes was due to increases in the amount of diagnosed diabetes, the authors wrote.
Finally, the age-standardized prevalence of total diabetes for subjects aged 40-74 years was 15.9%, 18.1%, and 18% during 1988-1994, 2005-2006, and 2011-2012, respectively (P = .01 for trend).
“Between 1988-1994 and 2011-2012, the prevalence of diabetes increased significantly among the overall population and among each age group, both sexes, every racial/ethnic group, every education level, and every income level, with a particularly rapid increase among non-Hispanic black and Mexican American participants. The proportion of people who had undiagnosed diabetes significantly decreased,” the authors noted.
The authors further clarified that the lower rates of undiagnosed diabetes over time may be secondary to improved survival in patients with diabetes and better screening.
The National Institute of Diabetes and Digestive and Kidney Diseases supported the study. The authors reported no conflicts of interests.
FROM JAMA
Key clinical point: The prevalence of diabetes is rising, especially among black, Asian, and Hispanic populations.
Major finding: The prevalence of diabetes was between 12% and 14% during 2011-2012 with higher rates in black, Asian, and Hispanic populations.
Data source: A cross-sectional survey with data from NHANES from 1988 to 1994 and 1999 to 2012.
Disclosures: The National Institute of Diabetes and Digestive and Kidney Diseases funded the study. The authors reported no conflicts of interests.
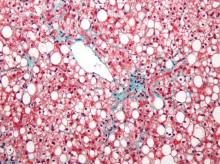
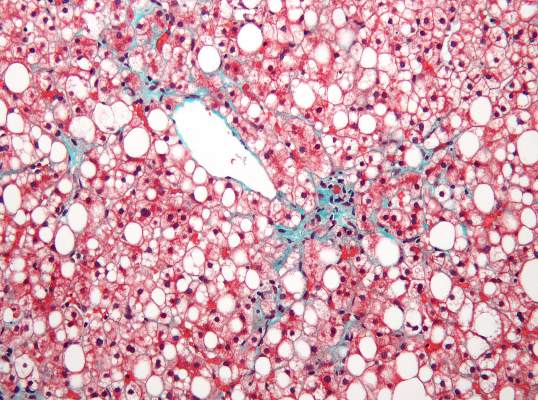
Subclinical Heart Dysfunction, Fatty Liver Linked
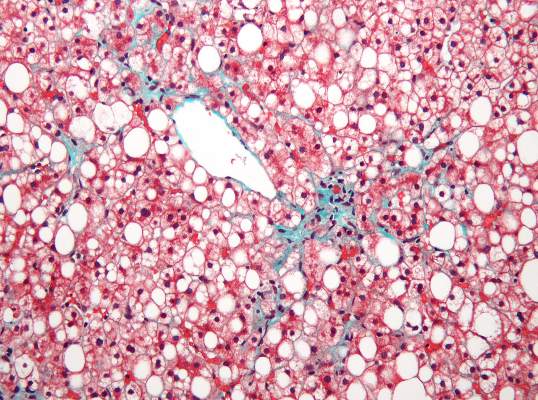
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
FROM HEPATOLOGY
Subclinical heart dysfunction, fatty liver linked
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
FROM HEPATOLOGY
Key clinical point: Researchers found an association between nonalcoholic fatty liver disease and myocardial dysfunction and remodeling.
Major finding: Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (P less than .0001), and elevated LV filling pressures (P less than .001) was more common in participants with NAFLD than in those without.
Data source: A cross-sectional study of 2,713 patients from the CARDIA study using CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study.
Disclosures: The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Alcohol, Marijuana Use Common in Youth With Chronic Disease
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
FROM PEDIATRICS
Alcohol, marijuana use common in youth with chronic disease
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment, according to a new study published in Pediatrics.
Approximately 1 in 4 American youths are living with a chronic medical condition. The most common substance abused by young people is alcohol, which can lead to adverse medication interactions and difficulty with treatment adherence and self-care. As with healthy youth, alcohol abuse may be associated with poor sleep, smoke exposure, and unprotected or unplanned sex. Marijuana use can lead to airway inflammation, treatment nonadherence, and sleep disturbances. Currently, there are no studies that indicate marijuana has therapeutic utility in young people.
Elissa Weitzman of Harvard Medical School in Boston, and colleagues sought to fill in knowledge gaps on the prevalence of substance use in chronically ill youths, which may lead to development of preventative strategies.
The investigators conducted a cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease (IBD). The questionnaire assessed alcohol use, behaviors, marijuana use, and health care interactions (Pediatrics 2015. doi: 10.1542/peds.2015-0722).
Of the 532 youths invited to participate in the study, 403 consented to participate; 51.6% were female, and 75.1% where white. The average age of participants was 15.6 years, and overall they were in good mental health.
Alcohol use within the past year was reported in 30.8%, and older age correlated to alcohol use (P less than .001). Binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year, and 10.4% in the total group. Binge drinking was reported more often in older (P less than .001) and white (P less than .01) chronically ill youth. Better mental health scores were associated with binge drinking (P less than .01).
Marijuana use was reported in 17.2% of the study group and 20.6% of the high school–aged group. Furthermore, marijuana use in chronically ill youth was associated with males, older age, lower socioeconomic status (P less than .01), and poorer mental health (P less than .01). Participants with IBD had higher rates of marijuana use than participants with arthritis or asthma. Almost all youth who reported past-year marijuana use also reported past-year alcohol use, the investigators noted.
Knowledge of alcohol’s potential effects with medications and laboratory results was low, with only 53.1% and 37.2% of high school students answering correctly, respectively. Those who answered incorrectly were 8.53 and 4.46 times more likely to drink and binge drink (P less than .001).
Approximately 8.3% and 32% of the high school–aged participants reported skipping or forgetting to take prescription medications within the past 30 days, respectively. Intentional nonadherence was associated with lower mental health scores (P less than .001). High school–aged youth who admitted to alcohol use within the past year were 1.61 times and 1.79 times more likely to skip and forget their medications, respectively.
Ms. Weitzman and her associates noted that the association of better mental health scores with binge drinking may be related to the social aspect, whereas the association of poorer mental health scores with marijuana may be related to its possible use to improve symptoms.
The authors also pointed out that although nonadherence was associated with alcohol use and poorer mental health scores, it also may be related to health-risking behaviors, poor self-regulation, and the feeling of invulnerability associated with adolescent development.
“Alcohol and marijuana use are prevalent among youth with chronic medical conditions, and drinking is associated with treatment nonadherence. Education and screening of medically vulnerable youth are warranted to ameliorate risk,” they concluded.
The authors reported no disclosures, and the study was supported by an NIH grant.
FROM PEDIATRICS
Key clinical point: Alcohol and marijuana use is common in youth with chronic disease, and alcohol use is associated with nonadherence to treatment.
Major finding: Alcohol was reported in 30.8%, and binge drinking was reported in 37.7% of respondents who reported alcohol use within the past year. Marijuana use was reported in 17.2% of the study group and associated with lower socioeconomic status (P less than .01) and poorer mental health (P less than .01).
Data source: A cross-sectional web-based assessment of youth aged 9-18 years who were being treated for cystic fibrosis, asthma, arthritis, type 1 diabetes, or inflammatory bowel disease.
Disclosures: The authors report no disclosures and the study was supported by an NIH grant.
Hydroxyurea boosts O2 saturations in children with sickle cell disease
Nocturnal and awake oxygen saturations are higher in children whose sickle cell disease (SCD) is treated with hydroxyurea, according to the results of a study by Dr. Indra Narang of the Hospital for Sick Children in Toronto and her colleagues.
“Improving SaO2 [oxygen saturation] may be an important mechanism of action of hydroxyurea therapy. As such, improving SaO2 across the severity spectrum of SCD may be beneficial in decreasing SCD morbidities with an overall improvement in long-term health,” the researchers wrote.
Sickle cell disease is characterized by development of rigid and sickled cells when deoxygenated, which may result in vasoocclusive injury to organs. Hydroxyurea enhances the production of fetal hemoglobin and can lead to less acute chest syndrome and vasoocclusive crises. Furthermore, children with sickle cell disease have a high prevalence of obstructive sleep apnea, which is associated with nocturnal desaturations and may be related to morbidity in SCD.
To evaluate the role of hydroxyurea in nocturnal oxygen saturations in pediatric patients, the researchers conducted a cross-sectional review of pediatric SCD patients referred for polysomnograms at the Hospital for Sick Children in Toronto from May 2007 to May 2014. Polysomnography data were analyzed on 37 children with SCD on hydroxyurea and matched with 104 children with SCD not treated with hydroxyurea. SAO2 was assessed using the Masimo oximeter (Ann Am Thorac Soc. 2015 July;12[7]1044-9).
Obstructive sleep apnea was found in 38% (n = 14) of subjects treated with hydroxyurea versus 52% (n = 54) in the nonhydroxyurea group. In the hydroxyurea group, the median obstructive apnea-hypopnea index was 0.9 events/hr vs. 1.9 events/hr in the nonhydroxyurea group, Dr. Narang and her associates reported.
Compared with the nonhydroxyurea SCD group, the hydroxyurea SCD group had significantly higher median awake (98.6% vs. 96.2%; P less than .0001) and sleep oxygen saturations (98.4% vs. 96.1%; P less than .0001). Likewise, treatment with hydroxyurea was associated with a significantly higher sleep oxygen saturation nadir when compared with the nonhydroxyurea group (91.4% vs. 85%; P = .0002), the investigators said.
Finally, treatment with hydroxyurea was associated with higher hemoglobin levels than no hydroxyurea treatment (P less than .0001) and the hemoglobin levels significantly correlated with sleep, awake, and lowest nocturnal oxygen saturation (P less than .0001).
The authors said that they had no conflicts to disclose.
Nocturnal and awake oxygen saturations are higher in children whose sickle cell disease (SCD) is treated with hydroxyurea, according to the results of a study by Dr. Indra Narang of the Hospital for Sick Children in Toronto and her colleagues.
“Improving SaO2 [oxygen saturation] may be an important mechanism of action of hydroxyurea therapy. As such, improving SaO2 across the severity spectrum of SCD may be beneficial in decreasing SCD morbidities with an overall improvement in long-term health,” the researchers wrote.
Sickle cell disease is characterized by development of rigid and sickled cells when deoxygenated, which may result in vasoocclusive injury to organs. Hydroxyurea enhances the production of fetal hemoglobin and can lead to less acute chest syndrome and vasoocclusive crises. Furthermore, children with sickle cell disease have a high prevalence of obstructive sleep apnea, which is associated with nocturnal desaturations and may be related to morbidity in SCD.
To evaluate the role of hydroxyurea in nocturnal oxygen saturations in pediatric patients, the researchers conducted a cross-sectional review of pediatric SCD patients referred for polysomnograms at the Hospital for Sick Children in Toronto from May 2007 to May 2014. Polysomnography data were analyzed on 37 children with SCD on hydroxyurea and matched with 104 children with SCD not treated with hydroxyurea. SAO2 was assessed using the Masimo oximeter (Ann Am Thorac Soc. 2015 July;12[7]1044-9).
Obstructive sleep apnea was found in 38% (n = 14) of subjects treated with hydroxyurea versus 52% (n = 54) in the nonhydroxyurea group. In the hydroxyurea group, the median obstructive apnea-hypopnea index was 0.9 events/hr vs. 1.9 events/hr in the nonhydroxyurea group, Dr. Narang and her associates reported.
Compared with the nonhydroxyurea SCD group, the hydroxyurea SCD group had significantly higher median awake (98.6% vs. 96.2%; P less than .0001) and sleep oxygen saturations (98.4% vs. 96.1%; P less than .0001). Likewise, treatment with hydroxyurea was associated with a significantly higher sleep oxygen saturation nadir when compared with the nonhydroxyurea group (91.4% vs. 85%; P = .0002), the investigators said.
Finally, treatment with hydroxyurea was associated with higher hemoglobin levels than no hydroxyurea treatment (P less than .0001) and the hemoglobin levels significantly correlated with sleep, awake, and lowest nocturnal oxygen saturation (P less than .0001).
The authors said that they had no conflicts to disclose.
Nocturnal and awake oxygen saturations are higher in children whose sickle cell disease (SCD) is treated with hydroxyurea, according to the results of a study by Dr. Indra Narang of the Hospital for Sick Children in Toronto and her colleagues.
“Improving SaO2 [oxygen saturation] may be an important mechanism of action of hydroxyurea therapy. As such, improving SaO2 across the severity spectrum of SCD may be beneficial in decreasing SCD morbidities with an overall improvement in long-term health,” the researchers wrote.
Sickle cell disease is characterized by development of rigid and sickled cells when deoxygenated, which may result in vasoocclusive injury to organs. Hydroxyurea enhances the production of fetal hemoglobin and can lead to less acute chest syndrome and vasoocclusive crises. Furthermore, children with sickle cell disease have a high prevalence of obstructive sleep apnea, which is associated with nocturnal desaturations and may be related to morbidity in SCD.
To evaluate the role of hydroxyurea in nocturnal oxygen saturations in pediatric patients, the researchers conducted a cross-sectional review of pediatric SCD patients referred for polysomnograms at the Hospital for Sick Children in Toronto from May 2007 to May 2014. Polysomnography data were analyzed on 37 children with SCD on hydroxyurea and matched with 104 children with SCD not treated with hydroxyurea. SAO2 was assessed using the Masimo oximeter (Ann Am Thorac Soc. 2015 July;12[7]1044-9).
Obstructive sleep apnea was found in 38% (n = 14) of subjects treated with hydroxyurea versus 52% (n = 54) in the nonhydroxyurea group. In the hydroxyurea group, the median obstructive apnea-hypopnea index was 0.9 events/hr vs. 1.9 events/hr in the nonhydroxyurea group, Dr. Narang and her associates reported.
Compared with the nonhydroxyurea SCD group, the hydroxyurea SCD group had significantly higher median awake (98.6% vs. 96.2%; P less than .0001) and sleep oxygen saturations (98.4% vs. 96.1%; P less than .0001). Likewise, treatment with hydroxyurea was associated with a significantly higher sleep oxygen saturation nadir when compared with the nonhydroxyurea group (91.4% vs. 85%; P = .0002), the investigators said.
Finally, treatment with hydroxyurea was associated with higher hemoglobin levels than no hydroxyurea treatment (P less than .0001) and the hemoglobin levels significantly correlated with sleep, awake, and lowest nocturnal oxygen saturation (P less than .0001).
The authors said that they had no conflicts to disclose.
FROM ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point: Nocturnal and awake oxygen saturations are higher in patients treated with hydroxyurea.
Major finding: The hydroxyurea SCD group was found to have significantly higher median awake (P less than .0001) and sleep (P less than .0001) oxygen saturation vs. the nonhydroxyurea SCD group and significantly higher sleep oxygen saturation nadir vs. the nonhydroxyurea group (P = .0002).
Data source: A cross-sectional review of 141 pediatric SCD patients referred for polysomnography from May 2007 to May 2014.
Disclosures: The authors said that they had no conflicts to disclose.
Evidence of a respiratory virus does not exclude Kawasaki disease
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
FROM PEDIATRICS
Key clinical point: A positive respiratory viral PCR does not exclude Kawasaki disease.
Major finding: There were no significant differences in clinical presentation, laboratory results, coronary artery lesions, or frequency of PICU admission between the viral-positive and viral-negative groups.
Data source: A chart review of 192 patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado, Aurora.
Disclosures: The authors report no external funding sources or disclosures.