User login
CT findings identify COPD phenotype with high risk for exacerbations
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
FROM THE ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point: COPD patients with both airway thickening and emphysema have more hospitalizations and more severe dyspnea.
Major finding: Patients with mixed phenotype COPD had 2.0 to 3.6 more COPD exacerbation hospitalizations (P<0.05) and more severe dyspnea (P<0.01).
Data source: A cross-sectional study using pulmonary function testing (PFTs), medical interviews, and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD.
Disclosures: Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Mobile health technology may encourage behavioral change
Mobile health technology such as wearable monitors, applications, and text-messaging programs may encourage behavioral change, according to a scientific statement by the American Heart Association published Aug. 13.
With cardiovascular disease, heart disease, and stroke remaining a major cause of morbidity and mortality, the AHA has identified four behaviors as part of its 2020 Strategic Impact Goals: promoting physical activity and healthful eating, and reducing weight and tobacco abuse. The AHA included blood pressure, cholesterol, and glucose as health indicators. Together these make up the AHA’s Life’s Simple 7. When taking into account these seven factors, 32% of Americans have a normal body mass index, less than 1% eat healthfully, and more than 30% have not achieved blood pressure or lipid goals.
Therefore, Lora Burke, Ph.D., of the School of Nursing at the University of Pittsburgh, and her colleagues sought to review the studies looking at mobile health interventions’ impact on the CV health indicators and targeted behaviors.
The researchers conducted an English language literature search focused on various mobile health terms and clinical diagnoses and limited to the period of 2004-2014.
Mobile health technology is beneficial for short-term weight loss when included with comprehensive lifestyle interventions. For patients who need to lose weight, physicians should consider recommending mobile health programs that are evidence based and take into account behavioral approaches, healthful eating, and physical activity. Likewise, feedback, social support, and self-monitoring capabilities should be available in the mobile health program.
More than 20% of American adults are using a form of health tracking, but there are not enough data to know if wearable tracking devices are effective at increasing physical activity. Likewise, the associated applications lack studies on their efficacy. The authors note that combining group behavioral interventions with activity trackers may result in more weight loss than with either the group intervention or tracking device alone.
Smoking cessation guidelines encourage the five As: ask, advise, assess, assist, and arrange, but clinicians are providing assessment of tobacco abuse, assistance in cessation, and arrangement for follow-up of the cessation program less often.
Several studies have shown nearly twice the abstinence rates with use of text messaging programs, but most were unsuccessful after 6 months, despite the mobile health device. Therefore, text messaging smoking cessation programs should be considered only if combined with another proven cessation intervention, the researchers noted.
In terms of the use of mobile health technology in improving glucose, blood pressure, and lipids, the data are limited.
Addressing cardiovascular disease risk factors before the development of CVD is associated with reduced CVD mortality. Given the limited face-to-face time physicians have with patients, mobile health technologies have the potential to expand the options to encourage behavioral change in patients.
“Using mHealth tools for monitoring provides the clinician data that far exceed what can be measured in the brief clinical encounter and reflect the status of physiological or behavioral measures in the person’s natural setting,” the authors concluded (Circulation. 2015 Aug. 13. doi: 10.1161/CIR.0000000000000232.)
The authors reported multiple disclosures including involvement with Scale Down, Coeus Health, Actigraph, Open mHealth, and WellDoc which are health technology companies.
Mobile health technology such as wearable monitors, applications, and text-messaging programs may encourage behavioral change, according to a scientific statement by the American Heart Association published Aug. 13.
With cardiovascular disease, heart disease, and stroke remaining a major cause of morbidity and mortality, the AHA has identified four behaviors as part of its 2020 Strategic Impact Goals: promoting physical activity and healthful eating, and reducing weight and tobacco abuse. The AHA included blood pressure, cholesterol, and glucose as health indicators. Together these make up the AHA’s Life’s Simple 7. When taking into account these seven factors, 32% of Americans have a normal body mass index, less than 1% eat healthfully, and more than 30% have not achieved blood pressure or lipid goals.
Therefore, Lora Burke, Ph.D., of the School of Nursing at the University of Pittsburgh, and her colleagues sought to review the studies looking at mobile health interventions’ impact on the CV health indicators and targeted behaviors.
The researchers conducted an English language literature search focused on various mobile health terms and clinical diagnoses and limited to the period of 2004-2014.
Mobile health technology is beneficial for short-term weight loss when included with comprehensive lifestyle interventions. For patients who need to lose weight, physicians should consider recommending mobile health programs that are evidence based and take into account behavioral approaches, healthful eating, and physical activity. Likewise, feedback, social support, and self-monitoring capabilities should be available in the mobile health program.
More than 20% of American adults are using a form of health tracking, but there are not enough data to know if wearable tracking devices are effective at increasing physical activity. Likewise, the associated applications lack studies on their efficacy. The authors note that combining group behavioral interventions with activity trackers may result in more weight loss than with either the group intervention or tracking device alone.
Smoking cessation guidelines encourage the five As: ask, advise, assess, assist, and arrange, but clinicians are providing assessment of tobacco abuse, assistance in cessation, and arrangement for follow-up of the cessation program less often.
Several studies have shown nearly twice the abstinence rates with use of text messaging programs, but most were unsuccessful after 6 months, despite the mobile health device. Therefore, text messaging smoking cessation programs should be considered only if combined with another proven cessation intervention, the researchers noted.
In terms of the use of mobile health technology in improving glucose, blood pressure, and lipids, the data are limited.
Addressing cardiovascular disease risk factors before the development of CVD is associated with reduced CVD mortality. Given the limited face-to-face time physicians have with patients, mobile health technologies have the potential to expand the options to encourage behavioral change in patients.
“Using mHealth tools for monitoring provides the clinician data that far exceed what can be measured in the brief clinical encounter and reflect the status of physiological or behavioral measures in the person’s natural setting,” the authors concluded (Circulation. 2015 Aug. 13. doi: 10.1161/CIR.0000000000000232.)
The authors reported multiple disclosures including involvement with Scale Down, Coeus Health, Actigraph, Open mHealth, and WellDoc which are health technology companies.
Mobile health technology such as wearable monitors, applications, and text-messaging programs may encourage behavioral change, according to a scientific statement by the American Heart Association published Aug. 13.
With cardiovascular disease, heart disease, and stroke remaining a major cause of morbidity and mortality, the AHA has identified four behaviors as part of its 2020 Strategic Impact Goals: promoting physical activity and healthful eating, and reducing weight and tobacco abuse. The AHA included blood pressure, cholesterol, and glucose as health indicators. Together these make up the AHA’s Life’s Simple 7. When taking into account these seven factors, 32% of Americans have a normal body mass index, less than 1% eat healthfully, and more than 30% have not achieved blood pressure or lipid goals.
Therefore, Lora Burke, Ph.D., of the School of Nursing at the University of Pittsburgh, and her colleagues sought to review the studies looking at mobile health interventions’ impact on the CV health indicators and targeted behaviors.
The researchers conducted an English language literature search focused on various mobile health terms and clinical diagnoses and limited to the period of 2004-2014.
Mobile health technology is beneficial for short-term weight loss when included with comprehensive lifestyle interventions. For patients who need to lose weight, physicians should consider recommending mobile health programs that are evidence based and take into account behavioral approaches, healthful eating, and physical activity. Likewise, feedback, social support, and self-monitoring capabilities should be available in the mobile health program.
More than 20% of American adults are using a form of health tracking, but there are not enough data to know if wearable tracking devices are effective at increasing physical activity. Likewise, the associated applications lack studies on their efficacy. The authors note that combining group behavioral interventions with activity trackers may result in more weight loss than with either the group intervention or tracking device alone.
Smoking cessation guidelines encourage the five As: ask, advise, assess, assist, and arrange, but clinicians are providing assessment of tobacco abuse, assistance in cessation, and arrangement for follow-up of the cessation program less often.
Several studies have shown nearly twice the abstinence rates with use of text messaging programs, but most were unsuccessful after 6 months, despite the mobile health device. Therefore, text messaging smoking cessation programs should be considered only if combined with another proven cessation intervention, the researchers noted.
In terms of the use of mobile health technology in improving glucose, blood pressure, and lipids, the data are limited.
Addressing cardiovascular disease risk factors before the development of CVD is associated with reduced CVD mortality. Given the limited face-to-face time physicians have with patients, mobile health technologies have the potential to expand the options to encourage behavioral change in patients.
“Using mHealth tools for monitoring provides the clinician data that far exceed what can be measured in the brief clinical encounter and reflect the status of physiological or behavioral measures in the person’s natural setting,” the authors concluded (Circulation. 2015 Aug. 13. doi: 10.1161/CIR.0000000000000232.)
The authors reported multiple disclosures including involvement with Scale Down, Coeus Health, Actigraph, Open mHealth, and WellDoc which are health technology companies.
FROM CIRCULATION
One-third of organ donations after circulatory death are unsuccessful
Despite the increase in donation of organs for transplant after circulatory death, many of these donations fail, according to a new study.
Dr. Joseph Scalea of the division of transplantation at the University of Wisconsin in Madison and his colleagues sought to explicate the process resulting in unsuccessful donation after circulatory death (DCD) and to explore the factors contributing to time to death in donors with successful organ donation. They conducted a retrospective study of data obtained from all organ donors at a single transplant center during January 2011-September 2014 (Ann Surg. 2015 Jul 15. doi: 10.1097/SLA.0000000000001298). A total of 506 organ donation procedures were studied, 169 of which were DCD. Time of death and outcomes data was obtained in 99.4% of the cases
The reasons for DCD failure appear to be rooted in the timing of support removal and the progression to death of these potential organ donors. A study of transplantation in the United Kingdom has shown that organs are less likely to be viable for transplantation if the donor does not progress to death within the first hour of withdrawal of support (Curr Opin Organ Transplant. 2013;18:133-9).
“People need to be aware that when folks have agreed to donate organs of a loved one and it is going to be a [circulatory death donation], that there is roughly a one in three chance, at least, that organ donation won’t come to fruition,” Dr. Jeffrey D. Punch, a transplant specialist at the University of Michigan in Ann Arbor, said in an interview.
Protocols vary by organization, but DCD typically involves the surgical team withdrawing life support in the absence of the organ recovery team. If circulatory death occurs within the time determined by the protocol, the organs are recovered for transplantation. Studies have indicated since the general acceptance of DCD since the 1990s, these donations account for as much as a 30% increase in donation rates in the United States and abroad (Am J Transplant. 2006 Feb;6(2):281-91; N Engl J Med. 2007;357:209-13).
The University of Wisconsin’s DCD protocol involved waiting up to 30 minutes after withdrawal of support (WOS) to recover pancreas and liver and up to 2 hours to recover kidneys.
During the study period, 33.4% (n = 169/506) of the organ donations were DCD. At least one organ was successfully donated in 72.8% of cases (n = 123), whereas in 27.2% (n = 46), the patient did not progress to death in the protocol time frame to be considered for donation. Head trauma (21.9%), cerebrovascular accident (23.7%), and anoxia (47.3%) were the most common diagnosis leading to DCD; however, success of DCD donation was not associated with the diagnosis. But if withdrawal of support was initiated in the OR, successful donation was more likely (P = .006).
“Those patients who underwent WOS in the ICU successfully donated organs less frequently. This difference is hard to interpret, as there may be different techniques of withdrawal in the ICU, or a selection bias (i.e., deemed less likely to die quickly) with which patients are considered for an ICU withdrawal,” the researchers wrote.
Dr. Punch, the Jeremiah and Claire Turcotte Professor of Surgery at the University of Michigan added, “It certainly makes more sense for withdrawal of support to happen in the operating room. It is more effective and they are more likely to be able to donate organs.”
The mean time from WOS to death was 28 minutes and 35 seconds for successful donations and 33 hours, 37 minutes, and 15 seconds for unsuccessful donations. In patients that successfully donated, 90.2% died less than an hour after WOS.
The investigators point out, “the ability to donate organs from a family member or loved one is often the only positive memory of an otherwise devastating experience. Unfortunately, not all donors successfully donate after attempted DCD.”
The authors reported no conflicts of interests.
Despite the increase in donation of organs for transplant after circulatory death, many of these donations fail, according to a new study.
Dr. Joseph Scalea of the division of transplantation at the University of Wisconsin in Madison and his colleagues sought to explicate the process resulting in unsuccessful donation after circulatory death (DCD) and to explore the factors contributing to time to death in donors with successful organ donation. They conducted a retrospective study of data obtained from all organ donors at a single transplant center during January 2011-September 2014 (Ann Surg. 2015 Jul 15. doi: 10.1097/SLA.0000000000001298). A total of 506 organ donation procedures were studied, 169 of which were DCD. Time of death and outcomes data was obtained in 99.4% of the cases
The reasons for DCD failure appear to be rooted in the timing of support removal and the progression to death of these potential organ donors. A study of transplantation in the United Kingdom has shown that organs are less likely to be viable for transplantation if the donor does not progress to death within the first hour of withdrawal of support (Curr Opin Organ Transplant. 2013;18:133-9).
“People need to be aware that when folks have agreed to donate organs of a loved one and it is going to be a [circulatory death donation], that there is roughly a one in three chance, at least, that organ donation won’t come to fruition,” Dr. Jeffrey D. Punch, a transplant specialist at the University of Michigan in Ann Arbor, said in an interview.
Protocols vary by organization, but DCD typically involves the surgical team withdrawing life support in the absence of the organ recovery team. If circulatory death occurs within the time determined by the protocol, the organs are recovered for transplantation. Studies have indicated since the general acceptance of DCD since the 1990s, these donations account for as much as a 30% increase in donation rates in the United States and abroad (Am J Transplant. 2006 Feb;6(2):281-91; N Engl J Med. 2007;357:209-13).
The University of Wisconsin’s DCD protocol involved waiting up to 30 minutes after withdrawal of support (WOS) to recover pancreas and liver and up to 2 hours to recover kidneys.
During the study period, 33.4% (n = 169/506) of the organ donations were DCD. At least one organ was successfully donated in 72.8% of cases (n = 123), whereas in 27.2% (n = 46), the patient did not progress to death in the protocol time frame to be considered for donation. Head trauma (21.9%), cerebrovascular accident (23.7%), and anoxia (47.3%) were the most common diagnosis leading to DCD; however, success of DCD donation was not associated with the diagnosis. But if withdrawal of support was initiated in the OR, successful donation was more likely (P = .006).
“Those patients who underwent WOS in the ICU successfully donated organs less frequently. This difference is hard to interpret, as there may be different techniques of withdrawal in the ICU, or a selection bias (i.e., deemed less likely to die quickly) with which patients are considered for an ICU withdrawal,” the researchers wrote.
Dr. Punch, the Jeremiah and Claire Turcotte Professor of Surgery at the University of Michigan added, “It certainly makes more sense for withdrawal of support to happen in the operating room. It is more effective and they are more likely to be able to donate organs.”
The mean time from WOS to death was 28 minutes and 35 seconds for successful donations and 33 hours, 37 minutes, and 15 seconds for unsuccessful donations. In patients that successfully donated, 90.2% died less than an hour after WOS.
The investigators point out, “the ability to donate organs from a family member or loved one is often the only positive memory of an otherwise devastating experience. Unfortunately, not all donors successfully donate after attempted DCD.”
The authors reported no conflicts of interests.
Despite the increase in donation of organs for transplant after circulatory death, many of these donations fail, according to a new study.
Dr. Joseph Scalea of the division of transplantation at the University of Wisconsin in Madison and his colleagues sought to explicate the process resulting in unsuccessful donation after circulatory death (DCD) and to explore the factors contributing to time to death in donors with successful organ donation. They conducted a retrospective study of data obtained from all organ donors at a single transplant center during January 2011-September 2014 (Ann Surg. 2015 Jul 15. doi: 10.1097/SLA.0000000000001298). A total of 506 organ donation procedures were studied, 169 of which were DCD. Time of death and outcomes data was obtained in 99.4% of the cases
The reasons for DCD failure appear to be rooted in the timing of support removal and the progression to death of these potential organ donors. A study of transplantation in the United Kingdom has shown that organs are less likely to be viable for transplantation if the donor does not progress to death within the first hour of withdrawal of support (Curr Opin Organ Transplant. 2013;18:133-9).
“People need to be aware that when folks have agreed to donate organs of a loved one and it is going to be a [circulatory death donation], that there is roughly a one in three chance, at least, that organ donation won’t come to fruition,” Dr. Jeffrey D. Punch, a transplant specialist at the University of Michigan in Ann Arbor, said in an interview.
Protocols vary by organization, but DCD typically involves the surgical team withdrawing life support in the absence of the organ recovery team. If circulatory death occurs within the time determined by the protocol, the organs are recovered for transplantation. Studies have indicated since the general acceptance of DCD since the 1990s, these donations account for as much as a 30% increase in donation rates in the United States and abroad (Am J Transplant. 2006 Feb;6(2):281-91; N Engl J Med. 2007;357:209-13).
The University of Wisconsin’s DCD protocol involved waiting up to 30 minutes after withdrawal of support (WOS) to recover pancreas and liver and up to 2 hours to recover kidneys.
During the study period, 33.4% (n = 169/506) of the organ donations were DCD. At least one organ was successfully donated in 72.8% of cases (n = 123), whereas in 27.2% (n = 46), the patient did not progress to death in the protocol time frame to be considered for donation. Head trauma (21.9%), cerebrovascular accident (23.7%), and anoxia (47.3%) were the most common diagnosis leading to DCD; however, success of DCD donation was not associated with the diagnosis. But if withdrawal of support was initiated in the OR, successful donation was more likely (P = .006).
“Those patients who underwent WOS in the ICU successfully donated organs less frequently. This difference is hard to interpret, as there may be different techniques of withdrawal in the ICU, or a selection bias (i.e., deemed less likely to die quickly) with which patients are considered for an ICU withdrawal,” the researchers wrote.
Dr. Punch, the Jeremiah and Claire Turcotte Professor of Surgery at the University of Michigan added, “It certainly makes more sense for withdrawal of support to happen in the operating room. It is more effective and they are more likely to be able to donate organs.”
The mean time from WOS to death was 28 minutes and 35 seconds for successful donations and 33 hours, 37 minutes, and 15 seconds for unsuccessful donations. In patients that successfully donated, 90.2% died less than an hour after WOS.
The investigators point out, “the ability to donate organs from a family member or loved one is often the only positive memory of an otherwise devastating experience. Unfortunately, not all donors successfully donate after attempted DCD.”
The authors reported no conflicts of interests.
FROM ANNALS OF SURGERY
Key clinical point: Some abdominal transplants are not possible because of failed DCD donation.
Major finding: At least one organ was successfully donated in 72.8% (n = 123), whereas 27.2% (n = 46) did not progress to death in the protocol time frame to be considered for donation.
Data source: Retrospective study of data obtained from all organ donors from a single transplant center during January 2011-September 2014.
Disclosures: The authors reported no conflicts of interests.
Schizophrenia decreases hippocampal and prefrontal cortex activity
Schizophrenia is associated with memory deficits and decreased hippocampal and dorsolateral prefrontal cortex activation, according to a study recently published in JAMA Psychiatry.
Concentrating on relationships between objects (relational encoding) or specific features of objects (item-specific encoding) may help long-term memory. The prefrontal cortex (PFC) and medial temporal lobe (MTL) are involved with these types of memory encoding. But relational memory may be impaired in individuals with schizophrenia.
The researchers, led by J. Daniel Ragland, Ph.D., from the department of psychiatry at the University of California, Davis, sought to use an adapted Relational and Item-Specific Encoding (RiSE) paradigm with functional MRI (fMRI) with the goal of highlighting the role of MTL subregions in retrieval and PFC subregions in encoding. Likewise, the investigators sought to test whether MTL and PFC subregions are affected in schizophrenia with impairment in relational memory but not item-specific memory.
In a multicenter study, data was obtained from November 1, 2010 through May 30, 2012. After excluding patients for excess movement, image acquisition errors, and below-chance performance, data was obtained from 52 schizophrenic outpatients and 57 healthy controls (JAMA Psychiatry 2015, July 22 [doi:10.1001/jamapsychiatry.2015.0276].
Patients with schizophrenia were characterized as having less education but were clinically stable with only mild symptoms and were on a fixed medication dose. Study participants were randomly presented with pictures of paired objects and asked questions to assess item-specific encoding, relational encoding, recognition, and associative recognition. The participants were scanned using fMRI for about 22 minutes.
Compared to the healthy controls, the schizophrenic patients demonstrated impairment in item recognition (P < 0.03). Likewise, during relational encoding, schizophrenic patients were found to have reduced activation in the dorsolateral PFC (P < 0.05) compared to healthy controls.
Hippocampal (HI) activation was demonstrated during retrieval success while healthy controls were completing associative recognition and relational item recognition activities. However, schizophrenic participants demonstrated reduced HI activation during relational item recognition activities. This association was not observed in item-specific activities (P < 0.05).
The results highlight memory deficits for relational versus item-specific tasks with deficits in HI and dorsolateral PCF activation in schizophrenic study participants, according to the researchers.
They suggested “that distinct PFC and HI subregions and mnemonic processes may be disrupted” rather than “solely attributing episodic memory deficits in schizophrenia to failed memory consolidation and retrieval in the HI or to disrupted strategic memory control in the PFC.”
Possible approaches to improve memory in patients with schizophrenia include training in relational processing, possibly in combination with neurostimulation, phamacologic, or other mechanistic interventions, the researchers wrote.
One limitation of the study noted was use of medication by most of the schizophrenic participants.
The study was funded by grants from the National Institutes of Health. The researchers reported multiple disclosures including research grants and participation as consultants for pharmaceutical companies.
Schizophrenia is associated with memory deficits and decreased hippocampal and dorsolateral prefrontal cortex activation, according to a study recently published in JAMA Psychiatry.
Concentrating on relationships between objects (relational encoding) or specific features of objects (item-specific encoding) may help long-term memory. The prefrontal cortex (PFC) and medial temporal lobe (MTL) are involved with these types of memory encoding. But relational memory may be impaired in individuals with schizophrenia.
The researchers, led by J. Daniel Ragland, Ph.D., from the department of psychiatry at the University of California, Davis, sought to use an adapted Relational and Item-Specific Encoding (RiSE) paradigm with functional MRI (fMRI) with the goal of highlighting the role of MTL subregions in retrieval and PFC subregions in encoding. Likewise, the investigators sought to test whether MTL and PFC subregions are affected in schizophrenia with impairment in relational memory but not item-specific memory.
In a multicenter study, data was obtained from November 1, 2010 through May 30, 2012. After excluding patients for excess movement, image acquisition errors, and below-chance performance, data was obtained from 52 schizophrenic outpatients and 57 healthy controls (JAMA Psychiatry 2015, July 22 [doi:10.1001/jamapsychiatry.2015.0276].
Patients with schizophrenia were characterized as having less education but were clinically stable with only mild symptoms and were on a fixed medication dose. Study participants were randomly presented with pictures of paired objects and asked questions to assess item-specific encoding, relational encoding, recognition, and associative recognition. The participants were scanned using fMRI for about 22 minutes.
Compared to the healthy controls, the schizophrenic patients demonstrated impairment in item recognition (P < 0.03). Likewise, during relational encoding, schizophrenic patients were found to have reduced activation in the dorsolateral PFC (P < 0.05) compared to healthy controls.
Hippocampal (HI) activation was demonstrated during retrieval success while healthy controls were completing associative recognition and relational item recognition activities. However, schizophrenic participants demonstrated reduced HI activation during relational item recognition activities. This association was not observed in item-specific activities (P < 0.05).
The results highlight memory deficits for relational versus item-specific tasks with deficits in HI and dorsolateral PCF activation in schizophrenic study participants, according to the researchers.
They suggested “that distinct PFC and HI subregions and mnemonic processes may be disrupted” rather than “solely attributing episodic memory deficits in schizophrenia to failed memory consolidation and retrieval in the HI or to disrupted strategic memory control in the PFC.”
Possible approaches to improve memory in patients with schizophrenia include training in relational processing, possibly in combination with neurostimulation, phamacologic, or other mechanistic interventions, the researchers wrote.
One limitation of the study noted was use of medication by most of the schizophrenic participants.
The study was funded by grants from the National Institutes of Health. The researchers reported multiple disclosures including research grants and participation as consultants for pharmaceutical companies.
Schizophrenia is associated with memory deficits and decreased hippocampal and dorsolateral prefrontal cortex activation, according to a study recently published in JAMA Psychiatry.
Concentrating on relationships between objects (relational encoding) or specific features of objects (item-specific encoding) may help long-term memory. The prefrontal cortex (PFC) and medial temporal lobe (MTL) are involved with these types of memory encoding. But relational memory may be impaired in individuals with schizophrenia.
The researchers, led by J. Daniel Ragland, Ph.D., from the department of psychiatry at the University of California, Davis, sought to use an adapted Relational and Item-Specific Encoding (RiSE) paradigm with functional MRI (fMRI) with the goal of highlighting the role of MTL subregions in retrieval and PFC subregions in encoding. Likewise, the investigators sought to test whether MTL and PFC subregions are affected in schizophrenia with impairment in relational memory but not item-specific memory.
In a multicenter study, data was obtained from November 1, 2010 through May 30, 2012. After excluding patients for excess movement, image acquisition errors, and below-chance performance, data was obtained from 52 schizophrenic outpatients and 57 healthy controls (JAMA Psychiatry 2015, July 22 [doi:10.1001/jamapsychiatry.2015.0276].
Patients with schizophrenia were characterized as having less education but were clinically stable with only mild symptoms and were on a fixed medication dose. Study participants were randomly presented with pictures of paired objects and asked questions to assess item-specific encoding, relational encoding, recognition, and associative recognition. The participants were scanned using fMRI for about 22 minutes.
Compared to the healthy controls, the schizophrenic patients demonstrated impairment in item recognition (P < 0.03). Likewise, during relational encoding, schizophrenic patients were found to have reduced activation in the dorsolateral PFC (P < 0.05) compared to healthy controls.
Hippocampal (HI) activation was demonstrated during retrieval success while healthy controls were completing associative recognition and relational item recognition activities. However, schizophrenic participants demonstrated reduced HI activation during relational item recognition activities. This association was not observed in item-specific activities (P < 0.05).
The results highlight memory deficits for relational versus item-specific tasks with deficits in HI and dorsolateral PCF activation in schizophrenic study participants, according to the researchers.
They suggested “that distinct PFC and HI subregions and mnemonic processes may be disrupted” rather than “solely attributing episodic memory deficits in schizophrenia to failed memory consolidation and retrieval in the HI or to disrupted strategic memory control in the PFC.”
Possible approaches to improve memory in patients with schizophrenia include training in relational processing, possibly in combination with neurostimulation, phamacologic, or other mechanistic interventions, the researchers wrote.
One limitation of the study noted was use of medication by most of the schizophrenic participants.
The study was funded by grants from the National Institutes of Health. The researchers reported multiple disclosures including research grants and participation as consultants for pharmaceutical companies.
FROM JAMA PSYCHIATRY
Key clinical point: Schizophrenia is associated with decreased hippocampal (HI) and dorsolateral prefrontal cortex activation (PFC) activation and memory deficits.
Major finding: Schizophrenic participants had impairment in item recognition, reduced activation in the dorsolateral PFC, and reduced HI activation during relational item recognition activities.
Data source: A multicenter study, from November 1, 2010 through May 30, 2012, using the RiSE paradigm with fMRI, comparing 52 schizophrenia patients with 57 healthy controls.
Disclosures: The study was funded by grants from the National Institutes of Health. The researchers reported multiple disclosures including research grants and participation as consultants for pharmaceutical companies.
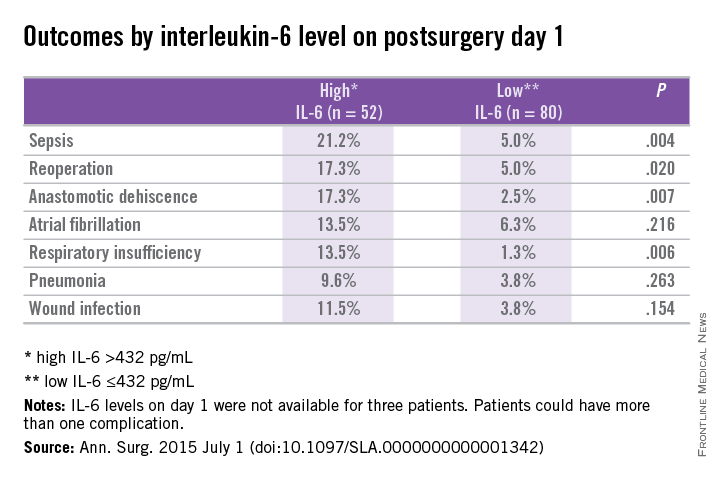
Elevated IL-6 linked to complications after major abdominal surgery
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
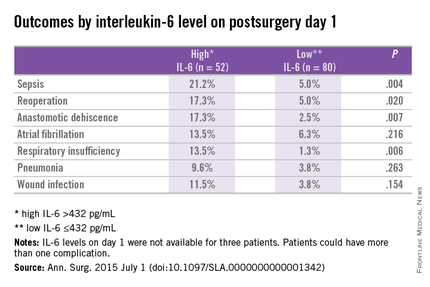
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Postoperative complications after major abdominal surgery are associated with elevated IL-6.
Major finding: Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (P < .02).
Data source: Prospective cohort study at a single center using data from the Myocardial Injury and Postoperative Complications after major abdominal surgery (MICOLON) study.
Disclosures: The authors reported no conflicts of interest.
TEP inguinal hernia repairs have low incidence of chronic pain
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
FROM ANNALS OF SURGERY
Key clinical point: TEP inguinal hernia repair is associated with a low incidence of chronic pain.
Major finding: Utilizing the IPQ questionnaire, 7.7% of patients reported having “pain that could not be ignored” in the last week with no difference between the two groups (P < .462).
Data source: Prospective data obtained from the Swedish Hernia Registry, IPQ, and SF-36 questionnaires.
Disclosures: The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Early intervention in autism may have sustained benefits
Children with autism spectrum disorder (ASD) who participated in an early intervention program showed sustained improvement in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity at 2 years’ follow-up, according to a prospective study.
“These findings demonstrate how early identification and intensive, early ASD-specific intervention can improve long-term outcomes for children with ASD,” noted Dr. Annette Estes of the University of Washington Autism Center in Seattle and her colleagues (J. Am. Acad. Child Adolesc. Psychiatry 2015;54:580-7).
A prospective 2-year follow-up study was conducted involving 39 6-year-old children with ASD who participated in the randomized clinical trial of the Early Start Denver Model (ESDM). Participants were initially enrolled at 18-30 months and were randomized to intensive interventions at home (ESDM) or treatment-as-usual in the community (COM) for 2 years. The ESDM group was offered 2-hour intervention sessions twice per day, 5 days per week, for 2 years by therapists. The number of hours of therapist-delivered interventions did not differ significantly between the ESDM and COM groups.
Supervised doctoral students or a clinical psychologist who was not aware of the participant’s intervention status assessed the children. Parent questionnaires or interviews were obtained to assess peer relationships, challenging behavior, adaptive behavior, and repetitive behavior.
Two years after intervention, differences in intellectual functioning were not found to be significantly different between the ESDM and COM groups. After initial treatment, the researchers noted there were not differences in core autism symptoms. However, the ESDM group demonstrated improvement in adaptive behavior and core autism symptoms at the 2-year follow-up, compared with the COM group. Improvements in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity on average were sustained in the 2 years after ESDM.
Dr. Estes and her associates pointed out that the generalizability of the findings may be limited by the amount of intervention hours the COM group received, and suggested they may have had greater access to intervention than typical families. Furthermore, the mothers of the study subjects were more highly educated, compared with average U.S. women.
The researchers concluded, “This provides direct evidence that these children did not exhibit a developmental regression, lose skills, or, in the case of standardized tests, slow their rate of development after withdrawal of early intensive services.”
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Estes reported multiple disclosures for grants and funding. Dr. Rogers and Dr. Dawson reported receiving royalties from books on early intervention they coauthored, and Dr. Rogers also reported receiving royalties, material fees, and honoraria related to the ESDM. The remaining coauthors reported no relevant financial disclosures.
Children with autism spectrum disorder (ASD) who participated in an early intervention program showed sustained improvement in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity at 2 years’ follow-up, according to a prospective study.
“These findings demonstrate how early identification and intensive, early ASD-specific intervention can improve long-term outcomes for children with ASD,” noted Dr. Annette Estes of the University of Washington Autism Center in Seattle and her colleagues (J. Am. Acad. Child Adolesc. Psychiatry 2015;54:580-7).
A prospective 2-year follow-up study was conducted involving 39 6-year-old children with ASD who participated in the randomized clinical trial of the Early Start Denver Model (ESDM). Participants were initially enrolled at 18-30 months and were randomized to intensive interventions at home (ESDM) or treatment-as-usual in the community (COM) for 2 years. The ESDM group was offered 2-hour intervention sessions twice per day, 5 days per week, for 2 years by therapists. The number of hours of therapist-delivered interventions did not differ significantly between the ESDM and COM groups.
Supervised doctoral students or a clinical psychologist who was not aware of the participant’s intervention status assessed the children. Parent questionnaires or interviews were obtained to assess peer relationships, challenging behavior, adaptive behavior, and repetitive behavior.
Two years after intervention, differences in intellectual functioning were not found to be significantly different between the ESDM and COM groups. After initial treatment, the researchers noted there were not differences in core autism symptoms. However, the ESDM group demonstrated improvement in adaptive behavior and core autism symptoms at the 2-year follow-up, compared with the COM group. Improvements in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity on average were sustained in the 2 years after ESDM.
Dr. Estes and her associates pointed out that the generalizability of the findings may be limited by the amount of intervention hours the COM group received, and suggested they may have had greater access to intervention than typical families. Furthermore, the mothers of the study subjects were more highly educated, compared with average U.S. women.
The researchers concluded, “This provides direct evidence that these children did not exhibit a developmental regression, lose skills, or, in the case of standardized tests, slow their rate of development after withdrawal of early intensive services.”
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Estes reported multiple disclosures for grants and funding. Dr. Rogers and Dr. Dawson reported receiving royalties from books on early intervention they coauthored, and Dr. Rogers also reported receiving royalties, material fees, and honoraria related to the ESDM. The remaining coauthors reported no relevant financial disclosures.
Children with autism spectrum disorder (ASD) who participated in an early intervention program showed sustained improvement in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity at 2 years’ follow-up, according to a prospective study.
“These findings demonstrate how early identification and intensive, early ASD-specific intervention can improve long-term outcomes for children with ASD,” noted Dr. Annette Estes of the University of Washington Autism Center in Seattle and her colleagues (J. Am. Acad. Child Adolesc. Psychiatry 2015;54:580-7).
A prospective 2-year follow-up study was conducted involving 39 6-year-old children with ASD who participated in the randomized clinical trial of the Early Start Denver Model (ESDM). Participants were initially enrolled at 18-30 months and were randomized to intensive interventions at home (ESDM) or treatment-as-usual in the community (COM) for 2 years. The ESDM group was offered 2-hour intervention sessions twice per day, 5 days per week, for 2 years by therapists. The number of hours of therapist-delivered interventions did not differ significantly between the ESDM and COM groups.
Supervised doctoral students or a clinical psychologist who was not aware of the participant’s intervention status assessed the children. Parent questionnaires or interviews were obtained to assess peer relationships, challenging behavior, adaptive behavior, and repetitive behavior.
Two years after intervention, differences in intellectual functioning were not found to be significantly different between the ESDM and COM groups. After initial treatment, the researchers noted there were not differences in core autism symptoms. However, the ESDM group demonstrated improvement in adaptive behavior and core autism symptoms at the 2-year follow-up, compared with the COM group. Improvements in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity on average were sustained in the 2 years after ESDM.
Dr. Estes and her associates pointed out that the generalizability of the findings may be limited by the amount of intervention hours the COM group received, and suggested they may have had greater access to intervention than typical families. Furthermore, the mothers of the study subjects were more highly educated, compared with average U.S. women.
The researchers concluded, “This provides direct evidence that these children did not exhibit a developmental regression, lose skills, or, in the case of standardized tests, slow their rate of development after withdrawal of early intensive services.”
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Estes reported multiple disclosures for grants and funding. Dr. Rogers and Dr. Dawson reported receiving royalties from books on early intervention they coauthored, and Dr. Rogers also reported receiving royalties, material fees, and honoraria related to the ESDM. The remaining coauthors reported no relevant financial disclosures.
FROM JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
Key clinical point: Early intervention in autism at ages 18-30 months showed sustained benefits at age 6 years.
Major finding: Two years after completing early intervention for autism spectrum disorders, children showed sustained improvement in adaptive behavior, challenging behavior, overall intellectual ability, and symptom severity.
Data source: A prospective 2-year follow-up of 39 6-year-old children initially enrolled in a randomized clinical trial of the Early Start Denver Model for autism intervention.
Disclosures: The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Estes reported multiple disclosures for grants and funding. Dr. Rogers and Dr. Dawson reported receiving royalties from books on early intervention they coauthored, and Dr. Rogers also reported receiving royalty, material fees, and honoraria related to the ESDM. The remaining coauthors reported no relevant financial disclosures.
Delivery mortality and complications higher in epileptic women
Pregnant women with a history of epilepsy are at increased risk for death and complications during delivery, according to a new study.
It is estimated that women with a history of epilepsy comprise 0.3%-0.5% of all pregnancies, but there are limited data on the risk of death and complications in the pregnant epileptic patient, Sarah MacDonald of Harvard T.H. Chan School of Public Health, Boston, and her colleagues wrote in their paper published online July 6 in JAMA Neurology.
Ms. MacDonald and her associates sought to determine if patients with a history of epilepsy are at increased risk for morbidity and mortality during delivery by conducting a retrospective cohort study of a weighted sample of 20,449,532 women without and 69,385 women with epilepsy in the Nationwide Inpatient Sample from 2007 to 2011. They obtained epilepsy diagnoses and baseline characteristics from ICD-9-CM codes. To limit the possibility of nonepileptic or eclampsia seizures being recorded as epilepsy, patients in the cohort were restricted to those without a history of hypertensive disorders and the ICD-9-CM code for “epilepsy, unspecified” was removed (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1017]).
Patients with a history of epilepsy had a frequency of death of 80 per 100,000 pregnancies, versus 6 deaths per 100,000 pregnancies without a history of epilepsy. The researchers noted a greater than 10-fold higher odds of death for epileptic patients (adjusted odds ratio, 11.46; 95% confidence interval, 8.64-15.19) when accounting for age, income, location, year, and race.
Pregnant women with a history of epilepsy were found to have higher rates of labor induction, cesarean section delivery, longer hospital stays, pregnancy-related hypertension, preeclampsia, and hemorrhage. Likewise, the researchers noted increased rates of gestational diabetes, premature rupture of membranes, chorioamnionitis, and premature delivery in patients with epilepsy. Furthermore, the newborns of epileptic mothers had higher rates of stillbirth, fetal distress, and poor growth. Overall, pregnant women with a history of epilepsy had significantly greater odds of severe morbidity (adjusted OR, 2.53; 95% CI, 2.44-2.63).
“However, despite their heightened risk of complications, we did not observe evidence that women with epilepsy are routinely triaged to high-risk medical centers,” the authors noted. But even though “the risk is substantially heightened on the multiplicative scale,” they said that the absolute rate of maternal death during delivery “is still very rare even among women with epilepsy.”
“Why did WWE [women with epilepsy] die at a higher rate in the MacDonald et al study? The authors suggested a number of possibilities, ranging from obstetrical complications, complications resulting from seizures (aspiration or status epilepticus), and a high rate of SUDEP (sudden unexplained death in epilepsy).”
“The MacDonald et al study provides important new information and demonstrates several risks associated with pregnancy in WWE. However, it raises far more questions than it answers. Most WWE have uncomplicated pregnancies. We need to understand the mechanisms underlying these risks, including death, so that we can identify the specific population at risk and devise interventions to reduce these risks.”
Dr. Jacqueline French is with the Comprehensive Epilepsy Center at New York University, New York. Dr. Kimford Meador is with the Stanford Comprehensive Epilepsy Center at Stanford University in Palo Alto, Calif. Dr. French reported receiving research support from multiple sources, including pharmceutical companies developing epilepsy drugs, the National Institutes of Health, the Epilepsy Therapy Project, the Epilepsy Research Foundation, and the Epilepsy Study Consortium. Dr. Meador reported receiving research support from UCB and other sources, including the National Institutes of Health, the Patient-Centered Outcomes Research Institute, and the Epilepsy Study Consortium. They made these comments in an editorial accompanying the study by Ms. MacDonald and her associates (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1356]).
“Why did WWE [women with epilepsy] die at a higher rate in the MacDonald et al study? The authors suggested a number of possibilities, ranging from obstetrical complications, complications resulting from seizures (aspiration or status epilepticus), and a high rate of SUDEP (sudden unexplained death in epilepsy).”
“The MacDonald et al study provides important new information and demonstrates several risks associated with pregnancy in WWE. However, it raises far more questions than it answers. Most WWE have uncomplicated pregnancies. We need to understand the mechanisms underlying these risks, including death, so that we can identify the specific population at risk and devise interventions to reduce these risks.”
Dr. Jacqueline French is with the Comprehensive Epilepsy Center at New York University, New York. Dr. Kimford Meador is with the Stanford Comprehensive Epilepsy Center at Stanford University in Palo Alto, Calif. Dr. French reported receiving research support from multiple sources, including pharmceutical companies developing epilepsy drugs, the National Institutes of Health, the Epilepsy Therapy Project, the Epilepsy Research Foundation, and the Epilepsy Study Consortium. Dr. Meador reported receiving research support from UCB and other sources, including the National Institutes of Health, the Patient-Centered Outcomes Research Institute, and the Epilepsy Study Consortium. They made these comments in an editorial accompanying the study by Ms. MacDonald and her associates (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1356]).
“Why did WWE [women with epilepsy] die at a higher rate in the MacDonald et al study? The authors suggested a number of possibilities, ranging from obstetrical complications, complications resulting from seizures (aspiration or status epilepticus), and a high rate of SUDEP (sudden unexplained death in epilepsy).”
“The MacDonald et al study provides important new information and demonstrates several risks associated with pregnancy in WWE. However, it raises far more questions than it answers. Most WWE have uncomplicated pregnancies. We need to understand the mechanisms underlying these risks, including death, so that we can identify the specific population at risk and devise interventions to reduce these risks.”
Dr. Jacqueline French is with the Comprehensive Epilepsy Center at New York University, New York. Dr. Kimford Meador is with the Stanford Comprehensive Epilepsy Center at Stanford University in Palo Alto, Calif. Dr. French reported receiving research support from multiple sources, including pharmceutical companies developing epilepsy drugs, the National Institutes of Health, the Epilepsy Therapy Project, the Epilepsy Research Foundation, and the Epilepsy Study Consortium. Dr. Meador reported receiving research support from UCB and other sources, including the National Institutes of Health, the Patient-Centered Outcomes Research Institute, and the Epilepsy Study Consortium. They made these comments in an editorial accompanying the study by Ms. MacDonald and her associates (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1356]).
Pregnant women with a history of epilepsy are at increased risk for death and complications during delivery, according to a new study.
It is estimated that women with a history of epilepsy comprise 0.3%-0.5% of all pregnancies, but there are limited data on the risk of death and complications in the pregnant epileptic patient, Sarah MacDonald of Harvard T.H. Chan School of Public Health, Boston, and her colleagues wrote in their paper published online July 6 in JAMA Neurology.
Ms. MacDonald and her associates sought to determine if patients with a history of epilepsy are at increased risk for morbidity and mortality during delivery by conducting a retrospective cohort study of a weighted sample of 20,449,532 women without and 69,385 women with epilepsy in the Nationwide Inpatient Sample from 2007 to 2011. They obtained epilepsy diagnoses and baseline characteristics from ICD-9-CM codes. To limit the possibility of nonepileptic or eclampsia seizures being recorded as epilepsy, patients in the cohort were restricted to those without a history of hypertensive disorders and the ICD-9-CM code for “epilepsy, unspecified” was removed (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1017]).
Patients with a history of epilepsy had a frequency of death of 80 per 100,000 pregnancies, versus 6 deaths per 100,000 pregnancies without a history of epilepsy. The researchers noted a greater than 10-fold higher odds of death for epileptic patients (adjusted odds ratio, 11.46; 95% confidence interval, 8.64-15.19) when accounting for age, income, location, year, and race.
Pregnant women with a history of epilepsy were found to have higher rates of labor induction, cesarean section delivery, longer hospital stays, pregnancy-related hypertension, preeclampsia, and hemorrhage. Likewise, the researchers noted increased rates of gestational diabetes, premature rupture of membranes, chorioamnionitis, and premature delivery in patients with epilepsy. Furthermore, the newborns of epileptic mothers had higher rates of stillbirth, fetal distress, and poor growth. Overall, pregnant women with a history of epilepsy had significantly greater odds of severe morbidity (adjusted OR, 2.53; 95% CI, 2.44-2.63).
“However, despite their heightened risk of complications, we did not observe evidence that women with epilepsy are routinely triaged to high-risk medical centers,” the authors noted. But even though “the risk is substantially heightened on the multiplicative scale,” they said that the absolute rate of maternal death during delivery “is still very rare even among women with epilepsy.”
Pregnant women with a history of epilepsy are at increased risk for death and complications during delivery, according to a new study.
It is estimated that women with a history of epilepsy comprise 0.3%-0.5% of all pregnancies, but there are limited data on the risk of death and complications in the pregnant epileptic patient, Sarah MacDonald of Harvard T.H. Chan School of Public Health, Boston, and her colleagues wrote in their paper published online July 6 in JAMA Neurology.
Ms. MacDonald and her associates sought to determine if patients with a history of epilepsy are at increased risk for morbidity and mortality during delivery by conducting a retrospective cohort study of a weighted sample of 20,449,532 women without and 69,385 women with epilepsy in the Nationwide Inpatient Sample from 2007 to 2011. They obtained epilepsy diagnoses and baseline characteristics from ICD-9-CM codes. To limit the possibility of nonepileptic or eclampsia seizures being recorded as epilepsy, patients in the cohort were restricted to those without a history of hypertensive disorders and the ICD-9-CM code for “epilepsy, unspecified” was removed (JAMA Neurol. 2015 July 6 [doi:10.1001/jamaneurol.2015.1017]).
Patients with a history of epilepsy had a frequency of death of 80 per 100,000 pregnancies, versus 6 deaths per 100,000 pregnancies without a history of epilepsy. The researchers noted a greater than 10-fold higher odds of death for epileptic patients (adjusted odds ratio, 11.46; 95% confidence interval, 8.64-15.19) when accounting for age, income, location, year, and race.
Pregnant women with a history of epilepsy were found to have higher rates of labor induction, cesarean section delivery, longer hospital stays, pregnancy-related hypertension, preeclampsia, and hemorrhage. Likewise, the researchers noted increased rates of gestational diabetes, premature rupture of membranes, chorioamnionitis, and premature delivery in patients with epilepsy. Furthermore, the newborns of epileptic mothers had higher rates of stillbirth, fetal distress, and poor growth. Overall, pregnant women with a history of epilepsy had significantly greater odds of severe morbidity (adjusted OR, 2.53; 95% CI, 2.44-2.63).
“However, despite their heightened risk of complications, we did not observe evidence that women with epilepsy are routinely triaged to high-risk medical centers,” the authors noted. But even though “the risk is substantially heightened on the multiplicative scale,” they said that the absolute rate of maternal death during delivery “is still very rare even among women with epilepsy.”
FROM JAMA NEUROLOGY
Key clinical point: Epilepsy is associated with increased risk of maternal death and complications surrounding delivery.
Major finding: Pregnant women with a history of epilepsy had a 10-fold increased likelihood of death (adjusted OR, 11.46; 95% CI, 8.64-15.19) and higher rates of complications.
Data source: A retrospective cohort study of pregnant women using data obtained from the Nationwide Inpatient Sample from 2007 to 2011.
Disclosures: The authors reported no conflicts of interest. The study was supported by a grant from the National Institute of Mental Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Researchers pin down possible cause, source for narcolepsy associated with flu vaccine
Patients with a history of vaccination with the pandemic influenza vaccine Pandemrix and narcolepsy were found to have antibodies to hypocretin receptor 2, possibly explaining this association after the 2009 (H1N1) pandemic.
The development of narcolepsy is associated with HLA-DQB1*0602 haplotype, loss of hypothalamic cells, and decrease production of hypocretin, a neuropeptide also known as orexin.
After the 2009 H1N1 influenza pandemic, there were increased reports of narcolepsy associated with the Pandemrix vaccine in Europe. Studies of this association found a 12.7-fold increased risk of narcolepsy within 8 months of Pandemrix vaccination. However, Focetria, the other H1N1 vaccine used in Europe in the 2009 pandemic, does not currently have a reported increased risk. Likewise, studies in China indicate an increased risk of narcolepsy after infection with the 2009 pandemic H1N1 influenza virus.
“We hypothesized that differences between the ‘adjuvanted’ A(H1N1)pdm09 vaccines Pandemrix and Focetria explain the association of narcolepsy with Pandemrix vaccinated subjects,” Dr. Syed Ahmed of Novartis Vaccines, Siena, Italy, and colleagues reported (Sci. Transl. Med. 2015;7:294ra105).
The researchers conducted a retrospective analysis of sera from narcoleptic individuals vaccinated with Pandemrix and a history of H1N1 infection as well as children from Finland without a history of narcolepsy and a history of Focetria vaccination. The samples were randomized and the investigators were blinded.
By aligning protein sequences of influenza strains, the researchers were able to identify an influenza nucleoprotein peptide similar to the hypocretin receptor. ELISA assays detected antibodies to hypocretin receptor 2 in a significantly higher percentage of sera samples from patients with a history of Pandemrix vaccination, HLA-DQB1*0602 haplotype, and narcolepsy (17 of 20), compared with patients with a history of Focetria vaccination (0 of 6; P < .001) or H1N1 infection (5 of 20; P < .001).
Furthermore, mass spectrometry indicated Focetria contained 72.7% less nucleoprotein than did Pandemrix. ELISA assays detected fewer nucleoprotein antibodies in individuals vaccinated with Focetria than in those infected with H1N1. Dr. Ahmed and his colleagues concluded that a possible mechanism for influenza and vaccine associated narcolepsy involves nucleoprotein antigen development after vaccination or infection and cross reaction with the hypocretin receptor 2. Furthermore, the difference in nucleoprotein content of the two vaccine types may further explain the association of Pandemrix vaccination with narcolepsy.
“The implications of the new work are important but specific. First of all, the findings show that in rare cases, vaccines can accidentally trigger autoimmunelike brain disease. The anti-H1N1 vaccine Pandemrix appears to make the case, stimulating in some individuals the production of hypocretin receptor cross-binding antibodies as a result of its high content of influenza [nucleoprotein].”
“Last, the work elegantly provides insight into vaccine-related narcolepsy but does not directly disclose whether similar mechanisms (autoimmune, parainfectious, etc.) contribute to sporadic narcolepsy. To settle this question definitively will require additional data from immune therapies, neuropathology, and much-needed narcolepsy animal models.”
Dr. Hartmut Wekerle is affiliated with the Max-Planck Institute of Neurobiology, Martinsried, Germany. These comments are taken from an editorial accompanying Dr. Ahmed and his colleagues’ report (Sci. Transl. Med. 2015;7:294fs27).
“The implications of the new work are important but specific. First of all, the findings show that in rare cases, vaccines can accidentally trigger autoimmunelike brain disease. The anti-H1N1 vaccine Pandemrix appears to make the case, stimulating in some individuals the production of hypocretin receptor cross-binding antibodies as a result of its high content of influenza [nucleoprotein].”
“Last, the work elegantly provides insight into vaccine-related narcolepsy but does not directly disclose whether similar mechanisms (autoimmune, parainfectious, etc.) contribute to sporadic narcolepsy. To settle this question definitively will require additional data from immune therapies, neuropathology, and much-needed narcolepsy animal models.”
Dr. Hartmut Wekerle is affiliated with the Max-Planck Institute of Neurobiology, Martinsried, Germany. These comments are taken from an editorial accompanying Dr. Ahmed and his colleagues’ report (Sci. Transl. Med. 2015;7:294fs27).
“The implications of the new work are important but specific. First of all, the findings show that in rare cases, vaccines can accidentally trigger autoimmunelike brain disease. The anti-H1N1 vaccine Pandemrix appears to make the case, stimulating in some individuals the production of hypocretin receptor cross-binding antibodies as a result of its high content of influenza [nucleoprotein].”
“Last, the work elegantly provides insight into vaccine-related narcolepsy but does not directly disclose whether similar mechanisms (autoimmune, parainfectious, etc.) contribute to sporadic narcolepsy. To settle this question definitively will require additional data from immune therapies, neuropathology, and much-needed narcolepsy animal models.”
Dr. Hartmut Wekerle is affiliated with the Max-Planck Institute of Neurobiology, Martinsried, Germany. These comments are taken from an editorial accompanying Dr. Ahmed and his colleagues’ report (Sci. Transl. Med. 2015;7:294fs27).
Patients with a history of vaccination with the pandemic influenza vaccine Pandemrix and narcolepsy were found to have antibodies to hypocretin receptor 2, possibly explaining this association after the 2009 (H1N1) pandemic.
The development of narcolepsy is associated with HLA-DQB1*0602 haplotype, loss of hypothalamic cells, and decrease production of hypocretin, a neuropeptide also known as orexin.
After the 2009 H1N1 influenza pandemic, there were increased reports of narcolepsy associated with the Pandemrix vaccine in Europe. Studies of this association found a 12.7-fold increased risk of narcolepsy within 8 months of Pandemrix vaccination. However, Focetria, the other H1N1 vaccine used in Europe in the 2009 pandemic, does not currently have a reported increased risk. Likewise, studies in China indicate an increased risk of narcolepsy after infection with the 2009 pandemic H1N1 influenza virus.
“We hypothesized that differences between the ‘adjuvanted’ A(H1N1)pdm09 vaccines Pandemrix and Focetria explain the association of narcolepsy with Pandemrix vaccinated subjects,” Dr. Syed Ahmed of Novartis Vaccines, Siena, Italy, and colleagues reported (Sci. Transl. Med. 2015;7:294ra105).
The researchers conducted a retrospective analysis of sera from narcoleptic individuals vaccinated with Pandemrix and a history of H1N1 infection as well as children from Finland without a history of narcolepsy and a history of Focetria vaccination. The samples were randomized and the investigators were blinded.
By aligning protein sequences of influenza strains, the researchers were able to identify an influenza nucleoprotein peptide similar to the hypocretin receptor. ELISA assays detected antibodies to hypocretin receptor 2 in a significantly higher percentage of sera samples from patients with a history of Pandemrix vaccination, HLA-DQB1*0602 haplotype, and narcolepsy (17 of 20), compared with patients with a history of Focetria vaccination (0 of 6; P < .001) or H1N1 infection (5 of 20; P < .001).
Furthermore, mass spectrometry indicated Focetria contained 72.7% less nucleoprotein than did Pandemrix. ELISA assays detected fewer nucleoprotein antibodies in individuals vaccinated with Focetria than in those infected with H1N1. Dr. Ahmed and his colleagues concluded that a possible mechanism for influenza and vaccine associated narcolepsy involves nucleoprotein antigen development after vaccination or infection and cross reaction with the hypocretin receptor 2. Furthermore, the difference in nucleoprotein content of the two vaccine types may further explain the association of Pandemrix vaccination with narcolepsy.
Patients with a history of vaccination with the pandemic influenza vaccine Pandemrix and narcolepsy were found to have antibodies to hypocretin receptor 2, possibly explaining this association after the 2009 (H1N1) pandemic.
The development of narcolepsy is associated with HLA-DQB1*0602 haplotype, loss of hypothalamic cells, and decrease production of hypocretin, a neuropeptide also known as orexin.
After the 2009 H1N1 influenza pandemic, there were increased reports of narcolepsy associated with the Pandemrix vaccine in Europe. Studies of this association found a 12.7-fold increased risk of narcolepsy within 8 months of Pandemrix vaccination. However, Focetria, the other H1N1 vaccine used in Europe in the 2009 pandemic, does not currently have a reported increased risk. Likewise, studies in China indicate an increased risk of narcolepsy after infection with the 2009 pandemic H1N1 influenza virus.
“We hypothesized that differences between the ‘adjuvanted’ A(H1N1)pdm09 vaccines Pandemrix and Focetria explain the association of narcolepsy with Pandemrix vaccinated subjects,” Dr. Syed Ahmed of Novartis Vaccines, Siena, Italy, and colleagues reported (Sci. Transl. Med. 2015;7:294ra105).
The researchers conducted a retrospective analysis of sera from narcoleptic individuals vaccinated with Pandemrix and a history of H1N1 infection as well as children from Finland without a history of narcolepsy and a history of Focetria vaccination. The samples were randomized and the investigators were blinded.
By aligning protein sequences of influenza strains, the researchers were able to identify an influenza nucleoprotein peptide similar to the hypocretin receptor. ELISA assays detected antibodies to hypocretin receptor 2 in a significantly higher percentage of sera samples from patients with a history of Pandemrix vaccination, HLA-DQB1*0602 haplotype, and narcolepsy (17 of 20), compared with patients with a history of Focetria vaccination (0 of 6; P < .001) or H1N1 infection (5 of 20; P < .001).
Furthermore, mass spectrometry indicated Focetria contained 72.7% less nucleoprotein than did Pandemrix. ELISA assays detected fewer nucleoprotein antibodies in individuals vaccinated with Focetria than in those infected with H1N1. Dr. Ahmed and his colleagues concluded that a possible mechanism for influenza and vaccine associated narcolepsy involves nucleoprotein antigen development after vaccination or infection and cross reaction with the hypocretin receptor 2. Furthermore, the difference in nucleoprotein content of the two vaccine types may further explain the association of Pandemrix vaccination with narcolepsy.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:Nucleoprotein antibodies possibly explain influenza vaccine associated narcolepsy.
Major finding: Patients with a history of Pandemrix vaccination, HLA-DQB1*0602 haplotype, and narcolepsy had detectable antibodies to hypocretin receptor 2.
Data source: Retrospective analysis of sera from the 2009 H1N1 pandemic.
Disclosures: The authors note no funding sources for the study, but an award from the National Center for Research Resources helped provide the mass spectrometer used during the study. Multiple authors disclosed employment and stock holdings in Novartis and Atreca. There were also authors who reported receiving honoraria and holding patents.
Rise in Bordetella pertussis associated with asymptomatic transmission
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
FROM BMC MEDICINE
Key clinical point: Asymptomatic transmission of B. pertussis by vaccinated individuals may explain rise in whooping cough.
Major finding: Phylodynamic and wavelet analyses of data are consistent with asymptomatic transmission of B. pertussis.
Data source: Data of reported cases of B. pertussis was obtained from the Centers for Disease Control and Prevention and Public Health England and analysis of 36 U.S. isolates from 1935 to 2005.
Disclosures: The researchers report no competing interests and were supported by the Omidyar Group and the Santa Fe Institute.