User login
Some Sports Injuries Greater for Girls
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
OCD Commonly Precedes Schizophrenia in Men With Both
Symptoms of obsessive-compulsive disorder preceded symptoms of schizophrenia in 48% of 133 patients hospitalized over an 11-year period who had both disorders.
The obsessive-compulsive symptoms and psychotic symptoms occurred simultaneously in 24% of patients, and the obsessive-compulsive symptoms followed the first occurrence of psychotic symptoms in 28%. The first clinically significant symptoms of obsessive-compulsive disorder (OCD) appeared at a mean age of 19.1 years, compared with a mean age of onset of 20.4 years for first psychotic symptoms, Sarit Faragian, Ph.D., and associates reported.
The difference in age of onset of the two disorders was significant in men (who accounted for 73% of the cohort) but not in women. Also, both disorders appeared earlier in men than in women. The men first developed OCD at a mean age of 18.3 years and schizophrenic symptoms at a mean of 19.8 years. The women first developed OCD at a mean age of 21.2 years and schizophrenic symptoms at a mean of 22.1 years, reported Dr. Faragian, a researcher at Tirat Carmel (Israel) Mental Health Center.
The study included consecutive patients admitted to the center with schizo-obsessive disorder from 1999 through 2010 (Psychiatry Res. 2012;197:19-22).
A considerable gap was found, however, between the mean ages of symptom onset and that of diagnostic assessment (mean age, 30 years), so the investigators also analyzed a subgroup of 52 patients with a first episode of schizophrenia (mean age at assessment, 22 years) in order to minimize recall bias. The findings reinforced those from the larger cohort: Clinically significant OCD symptoms emerged about 3 years earlier than schizophrenia symptoms in the subgroup, at ages 18.2 and 21.6 years, respectively.
The OCD symptoms came first in 26 (50%) of the patients with first-episode schizophrenia, simultaneously in 14 patients (27%), and after schizophrenia symptoms in 12 patients (23%).
The findings imply that obsessive-compulsive symptoms are independent of psychosis and not a result of schizophrenia in a substantial proportion of patients with schizo-obsessive disorder, the investigators suggested. It’s still true, however, that antipsychotic drug treatment or unknown schizophrenia-related causes triggered secondary OCD symptoms in a subset of patients with schizophrenia, as previous studies have shown.
In the current study, the investigators also compared the 133 patients with schizo-obsessive disorder with 113 matched patients admitted during the same time period who had schizophrenia but not OCD. Symptoms appeared significantly earlier in the schizo-obsessive group (20.4 years), compared with the schizophrenia group (23.4 years).
Patients in the schizo-obsessive group were significantly more likely to report that psychotic symptoms started before age 18 (46.6%), compared with patients in the schizophrenia-only group (21.2%), or that symptoms started before age 22 (69.9% vs. 52.2%, respectively).
Because OCD symptoms started before psychotic symptoms in so many schizo-obsessive patients, OCD might be useful to identify youths at high risk for progression to schizophrenia, Dr. Faragian suggested. The same might be said of OCD and bipolar disorder, based on previous studies showing that bipolar disorder started at a younger age in patients with anxiety disorders, particularly OCD, he added.
Among other limitations to the current study, the number of women in the study might have been too small to show a significant difference in temporal onset of OCD and psychotic symptoms. Both schizophrenia and OCD are heterogeneous disorders, however, and early-onset OCD is known to be familial and more common in boys. Future studies should focus on the familial influences on age of onset of schizo-obsessive disorder, Dr. Faragian suggested.
The study appears to be the largest so far to analyze age of onset of symptoms in patients with schizo-obsessive disorder. It excluded patients with affective and organic mental disorders or drug-induced or alcohol-induced psychoses.
Dr. Faragian and colleagues have no disclosures of financial conflicts of interest to report.
Symptoms of obsessive-compulsive disorder preceded symptoms of schizophrenia in 48% of 133 patients hospitalized over an 11-year period who had both disorders.
The obsessive-compulsive symptoms and psychotic symptoms occurred simultaneously in 24% of patients, and the obsessive-compulsive symptoms followed the first occurrence of psychotic symptoms in 28%. The first clinically significant symptoms of obsessive-compulsive disorder (OCD) appeared at a mean age of 19.1 years, compared with a mean age of onset of 20.4 years for first psychotic symptoms, Sarit Faragian, Ph.D., and associates reported.
The difference in age of onset of the two disorders was significant in men (who accounted for 73% of the cohort) but not in women. Also, both disorders appeared earlier in men than in women. The men first developed OCD at a mean age of 18.3 years and schizophrenic symptoms at a mean of 19.8 years. The women first developed OCD at a mean age of 21.2 years and schizophrenic symptoms at a mean of 22.1 years, reported Dr. Faragian, a researcher at Tirat Carmel (Israel) Mental Health Center.
The study included consecutive patients admitted to the center with schizo-obsessive disorder from 1999 through 2010 (Psychiatry Res. 2012;197:19-22).
A considerable gap was found, however, between the mean ages of symptom onset and that of diagnostic assessment (mean age, 30 years), so the investigators also analyzed a subgroup of 52 patients with a first episode of schizophrenia (mean age at assessment, 22 years) in order to minimize recall bias. The findings reinforced those from the larger cohort: Clinically significant OCD symptoms emerged about 3 years earlier than schizophrenia symptoms in the subgroup, at ages 18.2 and 21.6 years, respectively.
The OCD symptoms came first in 26 (50%) of the patients with first-episode schizophrenia, simultaneously in 14 patients (27%), and after schizophrenia symptoms in 12 patients (23%).
The findings imply that obsessive-compulsive symptoms are independent of psychosis and not a result of schizophrenia in a substantial proportion of patients with schizo-obsessive disorder, the investigators suggested. It’s still true, however, that antipsychotic drug treatment or unknown schizophrenia-related causes triggered secondary OCD symptoms in a subset of patients with schizophrenia, as previous studies have shown.
In the current study, the investigators also compared the 133 patients with schizo-obsessive disorder with 113 matched patients admitted during the same time period who had schizophrenia but not OCD. Symptoms appeared significantly earlier in the schizo-obsessive group (20.4 years), compared with the schizophrenia group (23.4 years).
Patients in the schizo-obsessive group were significantly more likely to report that psychotic symptoms started before age 18 (46.6%), compared with patients in the schizophrenia-only group (21.2%), or that symptoms started before age 22 (69.9% vs. 52.2%, respectively).
Because OCD symptoms started before psychotic symptoms in so many schizo-obsessive patients, OCD might be useful to identify youths at high risk for progression to schizophrenia, Dr. Faragian suggested. The same might be said of OCD and bipolar disorder, based on previous studies showing that bipolar disorder started at a younger age in patients with anxiety disorders, particularly OCD, he added.
Among other limitations to the current study, the number of women in the study might have been too small to show a significant difference in temporal onset of OCD and psychotic symptoms. Both schizophrenia and OCD are heterogeneous disorders, however, and early-onset OCD is known to be familial and more common in boys. Future studies should focus on the familial influences on age of onset of schizo-obsessive disorder, Dr. Faragian suggested.
The study appears to be the largest so far to analyze age of onset of symptoms in patients with schizo-obsessive disorder. It excluded patients with affective and organic mental disorders or drug-induced or alcohol-induced psychoses.
Dr. Faragian and colleagues have no disclosures of financial conflicts of interest to report.
Symptoms of obsessive-compulsive disorder preceded symptoms of schizophrenia in 48% of 133 patients hospitalized over an 11-year period who had both disorders.
The obsessive-compulsive symptoms and psychotic symptoms occurred simultaneously in 24% of patients, and the obsessive-compulsive symptoms followed the first occurrence of psychotic symptoms in 28%. The first clinically significant symptoms of obsessive-compulsive disorder (OCD) appeared at a mean age of 19.1 years, compared with a mean age of onset of 20.4 years for first psychotic symptoms, Sarit Faragian, Ph.D., and associates reported.
The difference in age of onset of the two disorders was significant in men (who accounted for 73% of the cohort) but not in women. Also, both disorders appeared earlier in men than in women. The men first developed OCD at a mean age of 18.3 years and schizophrenic symptoms at a mean of 19.8 years. The women first developed OCD at a mean age of 21.2 years and schizophrenic symptoms at a mean of 22.1 years, reported Dr. Faragian, a researcher at Tirat Carmel (Israel) Mental Health Center.
The study included consecutive patients admitted to the center with schizo-obsessive disorder from 1999 through 2010 (Psychiatry Res. 2012;197:19-22).
A considerable gap was found, however, between the mean ages of symptom onset and that of diagnostic assessment (mean age, 30 years), so the investigators also analyzed a subgroup of 52 patients with a first episode of schizophrenia (mean age at assessment, 22 years) in order to minimize recall bias. The findings reinforced those from the larger cohort: Clinically significant OCD symptoms emerged about 3 years earlier than schizophrenia symptoms in the subgroup, at ages 18.2 and 21.6 years, respectively.
The OCD symptoms came first in 26 (50%) of the patients with first-episode schizophrenia, simultaneously in 14 patients (27%), and after schizophrenia symptoms in 12 patients (23%).
The findings imply that obsessive-compulsive symptoms are independent of psychosis and not a result of schizophrenia in a substantial proportion of patients with schizo-obsessive disorder, the investigators suggested. It’s still true, however, that antipsychotic drug treatment or unknown schizophrenia-related causes triggered secondary OCD symptoms in a subset of patients with schizophrenia, as previous studies have shown.
In the current study, the investigators also compared the 133 patients with schizo-obsessive disorder with 113 matched patients admitted during the same time period who had schizophrenia but not OCD. Symptoms appeared significantly earlier in the schizo-obsessive group (20.4 years), compared with the schizophrenia group (23.4 years).
Patients in the schizo-obsessive group were significantly more likely to report that psychotic symptoms started before age 18 (46.6%), compared with patients in the schizophrenia-only group (21.2%), or that symptoms started before age 22 (69.9% vs. 52.2%, respectively).
Because OCD symptoms started before psychotic symptoms in so many schizo-obsessive patients, OCD might be useful to identify youths at high risk for progression to schizophrenia, Dr. Faragian suggested. The same might be said of OCD and bipolar disorder, based on previous studies showing that bipolar disorder started at a younger age in patients with anxiety disorders, particularly OCD, he added.
Among other limitations to the current study, the number of women in the study might have been too small to show a significant difference in temporal onset of OCD and psychotic symptoms. Both schizophrenia and OCD are heterogeneous disorders, however, and early-onset OCD is known to be familial and more common in boys. Future studies should focus on the familial influences on age of onset of schizo-obsessive disorder, Dr. Faragian suggested.
The study appears to be the largest so far to analyze age of onset of symptoms in patients with schizo-obsessive disorder. It excluded patients with affective and organic mental disorders or drug-induced or alcohol-induced psychoses.
Dr. Faragian and colleagues have no disclosures of financial conflicts of interest to report.
FROM PSYCHIATRY RESEARCH
Major Finding: Obsessive-compulsive symptoms started earlier than schizophrenia symptoms in 48% of patients with both disorders. The difference in age of onset was significant in men but not women.
Data Source: This was a prospective study of 133 patients with schizo-obsessive disorder who were admitted consecutively to one institution from 1999 through 2010.
Disclosures: Neither Dr. Faragian nor colleagues listed disclosures of financial conflicts of interest.
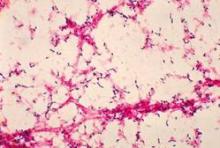
Infant Invasive Pneumococcal Disease Tanked in 2011
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
AT A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Modified Bariatric Surgery Tames Diabetes in Small Series
HOUSTON (IMNG) – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
Dr. Kirtikumar D. Modi
HOUSTON (IMNG) – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
Dr. Kirtikumar D. Modi
HOUSTON (IMNG) – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
Dr. Kirtikumar D. Modi
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Diabetes went into remission in 20 of 43 adults after laparoscopic sleeve gastrectomy with ileal interposition; the procedure also reduced the need for medications in the other 23 patients.
Data Source: The study is based on a case series at one institution.
Disclosures: Dr. Modi reported having no financial disclosures.
More Than Half of Diabetic Men Are Aspirin Resistant
HOUSTON (IMNG) – In all, 53% of 142 young men with type 2 diabetes were resistant to the anticlotting effects of aspirin in a retrospective analysis, suggesting that they may need higher-than-usual doses of prophylactic aspirin to prevent heart attacks and strokes.
The study shows that aspirin resistance is common in men with type 2 diabetes, even in those with good glycemic control, Dr. Subhashini Yaturu and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The investigators combined test results and information that had been gathered at one institution for a previous study with supplemental analyses of urine samples in order to measure concentrations of 11-dehydro-thromboxane beta-2 (11-DH-TXB2), a major urinary metabolite of thromboxane that is formed during blood clotting. High urinary levels of 11-DH-TXB2, measured using an enzyme immunoassay kit, indicate resistance to aspirin. Aspirin resistance was defined as a urine level of at least 1,500 pg 11-DH-TXB2 per mg of creatinine.
The men had a mean age of 49 years and a mean body mass index of 34 kg/m2. They’d had diabetes for a mean of 8 years; 88% of them had hypertension, and 23% had a history of coronary artery disease.
The investigators had hypothesized that aspirin resistance might be associated with high insulin levels and inflammatory markers. They found that 11-DH-TXB2 per creatinine levels correlated with a history of coronary artery disease, abdominal fat content, and interleukin-6 levels. Levels were highest in patients with a longer duration of diabetes and increased urinary microalbumin levels, an indicator of early kidney disease in diabetes, said Dr. Yaturu, section chief of the endocrinology and metabolism department at the Albany (N.Y.) Stratton Veterans Affairs Medical Center.
Although high blood pressure and greater abdominal-fat distribution conventionally are associated with increased risk of cardiovascular disease, these were not associated with aspirin resistance in this study. Patients with or without aspirin resistance did not differ significantly in age, BMI, history of hypertension, or waist-to-hip ratio. They also did not differ significantly in biochemical parameters such as creatinine, thyroid function tests, lipid parameters, or glycosylated hemoglobin (HbA1C) measurements.
Patients with aspirin resistance had a mean HbA1c of 8.1%, compared with 7.7% in those without aspirin resistance.
Knowing that aspirin resistance is so common is important clinically because it may allow for additional measures. Giving patients higher medication doses or additional prophylactic therapy might be considered to prevent heart attacks and strokes, Dr. Yaturu said.
Identifying patients with aspirin resistance isn’t easy, however, given the lack of correlation with obvious clinical markers, she said in an interview. The measures used in the study are still a research tool. But if aspirin resistance is identified in a patient, consider doubling the standard low dose of aspirin, she suggested.
Cardiovascular risk in patients with type 2 diabetes is equivalent to that of patients without diabetes who have had a coronary event, she noted. The American Diabetes Association recommends enteric-coated aspirin at a dosage of 81-325 mg/day for the prevention of cardiovascular events in high-risk patients with diabetes, including those older than 40 years or patients with risk factors other than diabetes, such as hypertension, smoking, dyslipidemia, albuminuria, or a family history of cardiovascular disease.
Causes of aspirin resistance include concurrent use of NSAIDs that may compete with aspirin at the cyclooxygenase-1 receptor site; polymorphisms in the COX1 gene; poor glucose control; body weight; and conditions associated with a high turnover of platelets, she said.
Dr. Yaturu reported having no financial disclosures.
Dr. Subhashini Yaturu
HOUSTON (IMNG) – In all, 53% of 142 young men with type 2 diabetes were resistant to the anticlotting effects of aspirin in a retrospective analysis, suggesting that they may need higher-than-usual doses of prophylactic aspirin to prevent heart attacks and strokes.
The study shows that aspirin resistance is common in men with type 2 diabetes, even in those with good glycemic control, Dr. Subhashini Yaturu and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The investigators combined test results and information that had been gathered at one institution for a previous study with supplemental analyses of urine samples in order to measure concentrations of 11-dehydro-thromboxane beta-2 (11-DH-TXB2), a major urinary metabolite of thromboxane that is formed during blood clotting. High urinary levels of 11-DH-TXB2, measured using an enzyme immunoassay kit, indicate resistance to aspirin. Aspirin resistance was defined as a urine level of at least 1,500 pg 11-DH-TXB2 per mg of creatinine.
The men had a mean age of 49 years and a mean body mass index of 34 kg/m2. They’d had diabetes for a mean of 8 years; 88% of them had hypertension, and 23% had a history of coronary artery disease.
The investigators had hypothesized that aspirin resistance might be associated with high insulin levels and inflammatory markers. They found that 11-DH-TXB2 per creatinine levels correlated with a history of coronary artery disease, abdominal fat content, and interleukin-6 levels. Levels were highest in patients with a longer duration of diabetes and increased urinary microalbumin levels, an indicator of early kidney disease in diabetes, said Dr. Yaturu, section chief of the endocrinology and metabolism department at the Albany (N.Y.) Stratton Veterans Affairs Medical Center.
Although high blood pressure and greater abdominal-fat distribution conventionally are associated with increased risk of cardiovascular disease, these were not associated with aspirin resistance in this study. Patients with or without aspirin resistance did not differ significantly in age, BMI, history of hypertension, or waist-to-hip ratio. They also did not differ significantly in biochemical parameters such as creatinine, thyroid function tests, lipid parameters, or glycosylated hemoglobin (HbA1C) measurements.
Patients with aspirin resistance had a mean HbA1c of 8.1%, compared with 7.7% in those without aspirin resistance.
Knowing that aspirin resistance is so common is important clinically because it may allow for additional measures. Giving patients higher medication doses or additional prophylactic therapy might be considered to prevent heart attacks and strokes, Dr. Yaturu said.
Identifying patients with aspirin resistance isn’t easy, however, given the lack of correlation with obvious clinical markers, she said in an interview. The measures used in the study are still a research tool. But if aspirin resistance is identified in a patient, consider doubling the standard low dose of aspirin, she suggested.
Cardiovascular risk in patients with type 2 diabetes is equivalent to that of patients without diabetes who have had a coronary event, she noted. The American Diabetes Association recommends enteric-coated aspirin at a dosage of 81-325 mg/day for the prevention of cardiovascular events in high-risk patients with diabetes, including those older than 40 years or patients with risk factors other than diabetes, such as hypertension, smoking, dyslipidemia, albuminuria, or a family history of cardiovascular disease.
Causes of aspirin resistance include concurrent use of NSAIDs that may compete with aspirin at the cyclooxygenase-1 receptor site; polymorphisms in the COX1 gene; poor glucose control; body weight; and conditions associated with a high turnover of platelets, she said.
Dr. Yaturu reported having no financial disclosures.
Dr. Subhashini Yaturu
HOUSTON (IMNG) – In all, 53% of 142 young men with type 2 diabetes were resistant to the anticlotting effects of aspirin in a retrospective analysis, suggesting that they may need higher-than-usual doses of prophylactic aspirin to prevent heart attacks and strokes.
The study shows that aspirin resistance is common in men with type 2 diabetes, even in those with good glycemic control, Dr. Subhashini Yaturu and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The investigators combined test results and information that had been gathered at one institution for a previous study with supplemental analyses of urine samples in order to measure concentrations of 11-dehydro-thromboxane beta-2 (11-DH-TXB2), a major urinary metabolite of thromboxane that is formed during blood clotting. High urinary levels of 11-DH-TXB2, measured using an enzyme immunoassay kit, indicate resistance to aspirin. Aspirin resistance was defined as a urine level of at least 1,500 pg 11-DH-TXB2 per mg of creatinine.
The men had a mean age of 49 years and a mean body mass index of 34 kg/m2. They’d had diabetes for a mean of 8 years; 88% of them had hypertension, and 23% had a history of coronary artery disease.
The investigators had hypothesized that aspirin resistance might be associated with high insulin levels and inflammatory markers. They found that 11-DH-TXB2 per creatinine levels correlated with a history of coronary artery disease, abdominal fat content, and interleukin-6 levels. Levels were highest in patients with a longer duration of diabetes and increased urinary microalbumin levels, an indicator of early kidney disease in diabetes, said Dr. Yaturu, section chief of the endocrinology and metabolism department at the Albany (N.Y.) Stratton Veterans Affairs Medical Center.
Although high blood pressure and greater abdominal-fat distribution conventionally are associated with increased risk of cardiovascular disease, these were not associated with aspirin resistance in this study. Patients with or without aspirin resistance did not differ significantly in age, BMI, history of hypertension, or waist-to-hip ratio. They also did not differ significantly in biochemical parameters such as creatinine, thyroid function tests, lipid parameters, or glycosylated hemoglobin (HbA1C) measurements.
Patients with aspirin resistance had a mean HbA1c of 8.1%, compared with 7.7% in those without aspirin resistance.
Knowing that aspirin resistance is so common is important clinically because it may allow for additional measures. Giving patients higher medication doses or additional prophylactic therapy might be considered to prevent heart attacks and strokes, Dr. Yaturu said.
Identifying patients with aspirin resistance isn’t easy, however, given the lack of correlation with obvious clinical markers, she said in an interview. The measures used in the study are still a research tool. But if aspirin resistance is identified in a patient, consider doubling the standard low dose of aspirin, she suggested.
Cardiovascular risk in patients with type 2 diabetes is equivalent to that of patients without diabetes who have had a coronary event, she noted. The American Diabetes Association recommends enteric-coated aspirin at a dosage of 81-325 mg/day for the prevention of cardiovascular events in high-risk patients with diabetes, including those older than 40 years or patients with risk factors other than diabetes, such as hypertension, smoking, dyslipidemia, albuminuria, or a family history of cardiovascular disease.
Causes of aspirin resistance include concurrent use of NSAIDs that may compete with aspirin at the cyclooxygenase-1 receptor site; polymorphisms in the COX1 gene; poor glucose control; body weight; and conditions associated with a high turnover of platelets, she said.
Dr. Yaturu reported having no financial disclosures.
Dr. Subhashini Yaturu
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Some 53% of 142 men with type 2 diabetes had aspirin resistance.
Data Source: Findings are based on a supplementary analysis of urine samples from a prior study at one institution; aspirin resistance was defined as at least 1,500 pg 11-DH-TXB2 per mg of creatinine.
Disclosures: Dr. Yaturu reported having no financial disclosures.
Younger Age for Measles Vaccine Debated
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
AT A PEDIATRIC UPDATE SPONOSORED BY STANFORD UNIVERSITY
Diabetes Drug Eased Postprandial Hypoglycemia
HOUSTON – Off-label use of sitagliptin to treat patients with postprandial hypoglycemia significantly reduced the symptoms of reactive hypoglycemia in a preliminary randomized, controlled, double-blind trial of 28 adults.
The 13 patients who took 100 mg/day of sitagliptin (Januvia) for 2 weeks and the 15 control patients on an identical placebo did not differ in baseline characteristics or in prerandomization measures of insulin and blood sugar levels from 5-hour meal tolerance tests. The 440-calorie meal contained 100 g of carbohydrates, which usually would trigger reactive hypoglycemia symptoms in these patients.
After treatment, the sitagliptin group rated the intensity of reactive hypoglycemia symptoms significantly lower than did the control group – 2 vs. 5 – on a visual analog scale of 1-10, in which 0 represented no symptoms and 10 was greatest symptom intensity, Dr. Paloma Almeda-Valdés and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
Patients in the sitagliptin group reported significant reductions in the symptoms of anxiety, palpitations, shakiness (tremor), diaphoresis, dizziness, tingling, difficulty concentrating, and weakness, said Dr. Almeda-Valdés of Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Mexico City.
Sitagliptin is approved to lower glucose levels in adults with type 2 diabetes. It increases glucagon-like peptide1 circulating levels, which improves the early-phase secretion of insulin.
Meal tolerance tests after 2 weeks of treatment showed that the sitagliptin group had significantly higher levels of insulin within 30 minutes of the test, with areas under the curve of 2,278 mcU/mL per minute compared with 2,106 mcU/mL per minute in the control group.
The increased insulin concentration in this early phase after the meal was associated with significantly higher glucose concentrations later on, 1-5 hours after the meal. The glucose areas under the curve in the late phase of the meal tolerance test were 90,030 mg/dL per minute in the sitagliptin group and 84,165 mg/dL per minute in the control group.
These biochemical changes were associated with the reductions in symptom severity in the sitagliptin group, Dr. Almeda-Valdés said.
"The hypothesis is that sitagliptin restores insulin secretion in these patients, and this was associated with higher glucose levels in the late phase" and thus less hypoglycemia, she said in an interview.
The study defined symptomatic reactive hypoglycemia as the presence of symptoms associated with a 2- to 4-hour postprandial capillary glucose less than 65 mg/dL that disappeared with carbohydrate ingestion.
Merck, which markets sitagliptin, provided funding, the drug, and the placebo for the study. Dr. Almeda-Valdés reported having no other disclosures.
HOUSTON – Off-label use of sitagliptin to treat patients with postprandial hypoglycemia significantly reduced the symptoms of reactive hypoglycemia in a preliminary randomized, controlled, double-blind trial of 28 adults.
The 13 patients who took 100 mg/day of sitagliptin (Januvia) for 2 weeks and the 15 control patients on an identical placebo did not differ in baseline characteristics or in prerandomization measures of insulin and blood sugar levels from 5-hour meal tolerance tests. The 440-calorie meal contained 100 g of carbohydrates, which usually would trigger reactive hypoglycemia symptoms in these patients.
After treatment, the sitagliptin group rated the intensity of reactive hypoglycemia symptoms significantly lower than did the control group – 2 vs. 5 – on a visual analog scale of 1-10, in which 0 represented no symptoms and 10 was greatest symptom intensity, Dr. Paloma Almeda-Valdés and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
Patients in the sitagliptin group reported significant reductions in the symptoms of anxiety, palpitations, shakiness (tremor), diaphoresis, dizziness, tingling, difficulty concentrating, and weakness, said Dr. Almeda-Valdés of Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Mexico City.
Sitagliptin is approved to lower glucose levels in adults with type 2 diabetes. It increases glucagon-like peptide1 circulating levels, which improves the early-phase secretion of insulin.
Meal tolerance tests after 2 weeks of treatment showed that the sitagliptin group had significantly higher levels of insulin within 30 minutes of the test, with areas under the curve of 2,278 mcU/mL per minute compared with 2,106 mcU/mL per minute in the control group.
The increased insulin concentration in this early phase after the meal was associated with significantly higher glucose concentrations later on, 1-5 hours after the meal. The glucose areas under the curve in the late phase of the meal tolerance test were 90,030 mg/dL per minute in the sitagliptin group and 84,165 mg/dL per minute in the control group.
These biochemical changes were associated with the reductions in symptom severity in the sitagliptin group, Dr. Almeda-Valdés said.
"The hypothesis is that sitagliptin restores insulin secretion in these patients, and this was associated with higher glucose levels in the late phase" and thus less hypoglycemia, she said in an interview.
The study defined symptomatic reactive hypoglycemia as the presence of symptoms associated with a 2- to 4-hour postprandial capillary glucose less than 65 mg/dL that disappeared with carbohydrate ingestion.
Merck, which markets sitagliptin, provided funding, the drug, and the placebo for the study. Dr. Almeda-Valdés reported having no other disclosures.
HOUSTON – Off-label use of sitagliptin to treat patients with postprandial hypoglycemia significantly reduced the symptoms of reactive hypoglycemia in a preliminary randomized, controlled, double-blind trial of 28 adults.
The 13 patients who took 100 mg/day of sitagliptin (Januvia) for 2 weeks and the 15 control patients on an identical placebo did not differ in baseline characteristics or in prerandomization measures of insulin and blood sugar levels from 5-hour meal tolerance tests. The 440-calorie meal contained 100 g of carbohydrates, which usually would trigger reactive hypoglycemia symptoms in these patients.
After treatment, the sitagliptin group rated the intensity of reactive hypoglycemia symptoms significantly lower than did the control group – 2 vs. 5 – on a visual analog scale of 1-10, in which 0 represented no symptoms and 10 was greatest symptom intensity, Dr. Paloma Almeda-Valdés and her associates reported in a poster presentation at the annual meeting of the Endocrine Society.
Patients in the sitagliptin group reported significant reductions in the symptoms of anxiety, palpitations, shakiness (tremor), diaphoresis, dizziness, tingling, difficulty concentrating, and weakness, said Dr. Almeda-Valdés of Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Mexico City.
Sitagliptin is approved to lower glucose levels in adults with type 2 diabetes. It increases glucagon-like peptide1 circulating levels, which improves the early-phase secretion of insulin.
Meal tolerance tests after 2 weeks of treatment showed that the sitagliptin group had significantly higher levels of insulin within 30 minutes of the test, with areas under the curve of 2,278 mcU/mL per minute compared with 2,106 mcU/mL per minute in the control group.
The increased insulin concentration in this early phase after the meal was associated with significantly higher glucose concentrations later on, 1-5 hours after the meal. The glucose areas under the curve in the late phase of the meal tolerance test were 90,030 mg/dL per minute in the sitagliptin group and 84,165 mg/dL per minute in the control group.
These biochemical changes were associated with the reductions in symptom severity in the sitagliptin group, Dr. Almeda-Valdés said.
"The hypothesis is that sitagliptin restores insulin secretion in these patients, and this was associated with higher glucose levels in the late phase" and thus less hypoglycemia, she said in an interview.
The study defined symptomatic reactive hypoglycemia as the presence of symptoms associated with a 2- to 4-hour postprandial capillary glucose less than 65 mg/dL that disappeared with carbohydrate ingestion.
Merck, which markets sitagliptin, provided funding, the drug, and the placebo for the study. Dr. Almeda-Valdés reported having no other disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Two weeks of 100 mg/day of sitagliptin increased postprandial insulin and glucose levels and significantly reduced patient ratings of the intensity of reactive hypoglycemia symptoms to 2 (on a scale of 1-10) compared with a rating of 5 in patients on placebo.
Data Source: This was a randomized, double-blind, controlled trial of 28 adults with reactive hypoglycemia.
Disclosures: Merck, which markets sitagliptin, provided funding, the drug, and the placebo for the study. Dr. Almeda-Valdés reported having no other disclosures.
Modified Bariatric Surgery Tames Diabetes in Small Series
HOUSTON – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
HOUSTON – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
HOUSTON – Laparoscopic sleeve gastrectomy with ileal interposition sent diabetes into remission in 20 of 43 adults and reduced the need for diabetes medications in the other 23 patients during an average of 20 months of follow-up.
Among the 30 obese (defined as having a body mass index greater than 27 kg/m2) patients in the study, 26 showed remission of diabetes – an 86% success rate that’s similar to results reported for gastric bypass surgery, Dr. Kirtikumar D. Modi said in a press briefing at the annual meeting of the Endocrine Society.
Patients had an average disease duration of 10 years and an average BMI of 33. In laparoscopic sleeve gastrectomy with ileal interposition, stapling reduces the size of the stomach, and a segment of the ileum is shifted to the jejunal area closer to the stomach. The average BMI fell to 26 after surgery. Among 30 patients who had hypertension before surgery, 27 had no hypertension postoperatively.
The surgery seemed to have no significant effect on lipid levels, "maybe because [the patients] were already on lipid-lowering drugs," said Dr. Modi, chief endocrinologist at Medwin Hospital in Hyderabad, India.
There were few complications; approximately 25% of patients had nausea and loss of appetite during the first postoperative month. Difficulty with rapid swallowing in six patients subsided over 2 weeks.
In a second series, Dr. Modi and his associates performed a laparoscopic diverted sleeve gastrectomy with ileal interposition on 17 additional patients who were not obese and had had diabetes longer than 10 years – the characteristics of patients who responded less well to the sleeve gastrectomy with ileal interposition in the first series.
Laparoscopic diverted sleeve gastrectomy diverts food away from parts of the small intestine, including the duodenum, where the absorption of nutrients begins, and the ileal segment is shifted more proximally. Patients who underwent this procedure had had diabetes for 15 years on average, and they had an average BMI of 29 as well as stimulated C-peptide levels greater than 4 ng/mL.
As expected, the mean BMI decreased to 23 over 18 months, he said. Of the eight patients who had hypertension before surgery, seven (88%) had no hypertension afterward. This time, treatment produced significant decreases in glycemic, lipid, and microalbuminuria levels.
At 9 months after surgery, diabetes was in remission in 12 (70%) of the 17 patients, and the other 5 patients needed fewer oral hyperglycemic medications than did those in the first series.
All patients in both studies had poorly controlled diabetes. The investigators defined diabetes remission as a hemoglobin A1c level less than 6.5% and no further need for insulin or oral hypoglycemic agents.
The reduction in hemoglobin A1c was disproportionately greater than the decline in BMI, suggesting benefits that are "much more than the weight improvement," he said.
More complications were seen in the second series, including three patients with minor intraoperative complications. Another patient developed ileus with ileal perforation 2 weeks after surgery and underwent laparotomy for repair. Three patients experienced nausea and anorexia for 2 weeks. Two patients developed vitamin B12 deficiency at 12 months.
A previous study of 150 patients with uncontrolled type 2 diabetes reported better glycemic control in patients who were randomized to 12 months of medical therapy plus bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass), compared with those on medical treatment alone, Dr. Modi noted (N. Engl. J. Med. 2012;366:1567-76).
A separate retrospective study of 271,726 patients in the Bariatric Outcomes Longitudinal Database found that the efficacy and safety of laparoscopic sleeve gastrectomy fell between those of gastric banding and laparoscopic gastric bypass.
Dr. Modi reported having no financial disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Diabetes went into remission in 20 of 43 adults after laparoscopic sleeve gastrectomy with ileal interposition; the procedure also reduced the need for medications in the other 23 patients.
Data Source: The study is based on a case series at one institution.
Disclosures: Dr. Modi reported having no financial disclosures.
Fitness Curbs Mortality in Men With Diabetes
HOUSTON – Physical fitness nearly halved the risk of death in men with type 2 diabetes, regardless of whether they had left ventricular hypertrophy, a longitudinal study of 866 patients found.
During a follow-up period as long as 24 years (with a median 9-year follow-up), 236 men who had left ventricular hypertrophy and were within the lower 50th percentile of physical fitness were 20% more likely to die, compared with 225 men in a reference group who did not have left ventricular hypertrophy and also had a low level of fitness. The difference in mortality risk between these two groups did not reach statistical significance.
In contrast, compared with the reference group, the risk of death was 41% lower in 218 men who were physically fit (in the upper 50th percentile) and did not have left ventricular hypertrophy and 43% lower in 187 men who were fit and did have left ventricular hypertrophy, Dr. Khaled Alswat and his associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The risk reductions in the two fit groups were statistically significant.
"We, as doctors, do a lot of testing, and one of those tests should be an exercise test" for patients with diabetes who have an increased risk for heart disease, said Dr. Alswat, an endocrinology fellow at Veterans Affairs Medical Center and George Washington University, Washington. An exercise stress test provides objective measures that physicians can use to work with patients on improving their physical fitness, he said in an interview.
The patients underwent a standardized exercise stress test and echocardiographic evaluation at the VA Medical Center during 1986-2011. Those who had a peak exercise capacity of at least six metabolic equivalence tasks (METs) were considered fit, and the rest were defined as having a low level of fitness (within the lower 50th percentile).
Left ventricular hypertrophy was defined by a left ventricular mass index, calculated by dividing left ventricular mass by height in meters to the power of 2.7. A left ventricular mass index greater than 48 g/m2.7 indicated left ventricular hypertrophy.
During follow-up, 346 patients died, for an annual death rate of 4%.
Smoking significantly increased mortality risk by 54%, a multivariate Cox proportional hazards analysis showed. The study controlled for the potential influences of age, body mass index, hypertension, smoking, and medications.
The adjusted mortality risk declined by 17% for every one-MET increase in fitness, Dr. Alswat reported.
Previous studies had shown that higher exercise capacity was associated with lower mortality risk in people with diabetes, but it had not been clear whether this applies to people with diabetes and left ventricular hypertrophy, he said.
Dr. Alswat reported having no relevant financial disclosures.
HOUSTON – Physical fitness nearly halved the risk of death in men with type 2 diabetes, regardless of whether they had left ventricular hypertrophy, a longitudinal study of 866 patients found.
During a follow-up period as long as 24 years (with a median 9-year follow-up), 236 men who had left ventricular hypertrophy and were within the lower 50th percentile of physical fitness were 20% more likely to die, compared with 225 men in a reference group who did not have left ventricular hypertrophy and also had a low level of fitness. The difference in mortality risk between these two groups did not reach statistical significance.
In contrast, compared with the reference group, the risk of death was 41% lower in 218 men who were physically fit (in the upper 50th percentile) and did not have left ventricular hypertrophy and 43% lower in 187 men who were fit and did have left ventricular hypertrophy, Dr. Khaled Alswat and his associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The risk reductions in the two fit groups were statistically significant.
"We, as doctors, do a lot of testing, and one of those tests should be an exercise test" for patients with diabetes who have an increased risk for heart disease, said Dr. Alswat, an endocrinology fellow at Veterans Affairs Medical Center and George Washington University, Washington. An exercise stress test provides objective measures that physicians can use to work with patients on improving their physical fitness, he said in an interview.
The patients underwent a standardized exercise stress test and echocardiographic evaluation at the VA Medical Center during 1986-2011. Those who had a peak exercise capacity of at least six metabolic equivalence tasks (METs) were considered fit, and the rest were defined as having a low level of fitness (within the lower 50th percentile).
Left ventricular hypertrophy was defined by a left ventricular mass index, calculated by dividing left ventricular mass by height in meters to the power of 2.7. A left ventricular mass index greater than 48 g/m2.7 indicated left ventricular hypertrophy.
During follow-up, 346 patients died, for an annual death rate of 4%.
Smoking significantly increased mortality risk by 54%, a multivariate Cox proportional hazards analysis showed. The study controlled for the potential influences of age, body mass index, hypertension, smoking, and medications.
The adjusted mortality risk declined by 17% for every one-MET increase in fitness, Dr. Alswat reported.
Previous studies had shown that higher exercise capacity was associated with lower mortality risk in people with diabetes, but it had not been clear whether this applies to people with diabetes and left ventricular hypertrophy, he said.
Dr. Alswat reported having no relevant financial disclosures.
HOUSTON – Physical fitness nearly halved the risk of death in men with type 2 diabetes, regardless of whether they had left ventricular hypertrophy, a longitudinal study of 866 patients found.
During a follow-up period as long as 24 years (with a median 9-year follow-up), 236 men who had left ventricular hypertrophy and were within the lower 50th percentile of physical fitness were 20% more likely to die, compared with 225 men in a reference group who did not have left ventricular hypertrophy and also had a low level of fitness. The difference in mortality risk between these two groups did not reach statistical significance.
In contrast, compared with the reference group, the risk of death was 41% lower in 218 men who were physically fit (in the upper 50th percentile) and did not have left ventricular hypertrophy and 43% lower in 187 men who were fit and did have left ventricular hypertrophy, Dr. Khaled Alswat and his associates reported in a poster presentation at the annual meeting of the Endocrine Society.
The risk reductions in the two fit groups were statistically significant.
"We, as doctors, do a lot of testing, and one of those tests should be an exercise test" for patients with diabetes who have an increased risk for heart disease, said Dr. Alswat, an endocrinology fellow at Veterans Affairs Medical Center and George Washington University, Washington. An exercise stress test provides objective measures that physicians can use to work with patients on improving their physical fitness, he said in an interview.
The patients underwent a standardized exercise stress test and echocardiographic evaluation at the VA Medical Center during 1986-2011. Those who had a peak exercise capacity of at least six metabolic equivalence tasks (METs) were considered fit, and the rest were defined as having a low level of fitness (within the lower 50th percentile).
Left ventricular hypertrophy was defined by a left ventricular mass index, calculated by dividing left ventricular mass by height in meters to the power of 2.7. A left ventricular mass index greater than 48 g/m2.7 indicated left ventricular hypertrophy.
During follow-up, 346 patients died, for an annual death rate of 4%.
Smoking significantly increased mortality risk by 54%, a multivariate Cox proportional hazards analysis showed. The study controlled for the potential influences of age, body mass index, hypertension, smoking, and medications.
The adjusted mortality risk declined by 17% for every one-MET increase in fitness, Dr. Alswat reported.
Previous studies had shown that higher exercise capacity was associated with lower mortality risk in people with diabetes, but it had not been clear whether this applies to people with diabetes and left ventricular hypertrophy, he said.
Dr. Alswat reported having no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Among men with diabetes, physical fitness decreased mortality risk by 43% in those with (and by 41% in those without) left ventricular hypertrophy compared with men without left ventricular hypertrophy who had a low level of fitness.
Data Source: Longitudinal study of 866 men who underwent exercise stress tests and echocardiographic evaluations at one institution from 1986 to 2011 and were followed for a median of 9 years.
Disclosures: Dr. Alswat reported having no relevant financial disclosures.
Overcome Problem Behavior by Using 'Reflective' Relationships
BELLEVUE, WASH. – Dr. Claudia M. Gold spent 17 years in general and behavioral pediatrics being frustrated time and again by a familiar cycle: A parent would ask for help with a child’s problematic behavior, Dr. Gold’s "bag of behavioral tricks" wouldn’t help, the parent would begin to speak in increasingly negative terms about the child, and Dr. Gold would feel increasingly negative about the parent.
At a loss, she would recommend that the parent take the child to a therapist, the parent usually would not, and eventually the child would end up with a psychiatric diagnosis and on medication. Those years paralleled an explosion in diagnoses of pediatric bipolar disorder in the United States and the use of atypical antipsychotics in children with explosive behavior.
Then Dr. Gold took classes to learn more about infant mental health and attachment theory. She incorporated an emphasis on reflective relationships in her work, which "transformed my practice. Suddenly children were getting better. Amazing things were happening," said Dr. Gold, director of the Early Childhood Social Emotional Health Program at Newton-Wellesley Hospital, Newton, Mass.
The key to this change was implementing principles of reflective functioning, also known as "mentalization," which Dr. Gold calls "holding the child in mind." She and other speakers at a conference sponsored by the North Pacific Pediatric Society said that applying these principles to the pediatrician-parent relationship, and helping parents use them in the parent-child relationship, makes all the difference.
"Behavior problems" are problems of self-regulation of intense emotion, and self-regulation develops through coregulation in relationships with primary caregivers, Dr. Gold explained.
She starts by helping the parent reflect on the meaning of the child’s behavior, the child’s wants and needs, instead of just focusing on the behavior itself. "Even for a moment, reflect on the child’s experience. The child feels that, and calms down or begins to calm down. Parents begin to feel better," she said.
Dr. Gold outlined four essential components of reflective functioning in her book, "Keeping Your Child in Mind: Overcoming Defiance, Tantrums, and Other Everyday Behavior Problems by Seeing the World Through Your Child’s Eyes" (Boston: Da Capo Press, 2011):
1. Curiosity about the meaning of behavior. This means considering the thoughts and feelings driving a child’s behavior.
2. Empathy. This means reframing "difficult" behavior as "stressed" behavior.
3. Containing and regulating the child’s experience. This step can involve setting limits.
4. Self-regulation. This step involves the parent or pediatrician managing their own feelings.
When the pediatrician uses these same principles to reflect on the parent’s experience, that supports the parent’s efforts to reflect on the child’s experience, Paula D. Zeanah, Ph.D., said in a separate presentation.
Just as infants and young children in distress rely on the parental relationship, the pediatrician is "functioning as that go-to figure when the parent is in distress," said Dr. Zeanah, professor of clinical psychiatry at Tulane University and interim chief of pediatrics at Tulane Hospital for Children, both in New Orleans.
And just as a child’s behavior can trigger emotions and frustrations in the parent, the parent’s actions do the same for pediatricians. "We don’t spend enough time reflecting on how parents make us feel," she said.
Studies have shown that patients often provide clues to aspects of their inner lives that primary clinicians usually don’t recognize or acknowledge, missing opportunities for empathy and personal connection that are key to building the physician-patient relationship.
Dr. Zeanah recommended "really basic stuff that seems to make a difference," such as active listening, fewer interruptions, sitting so you’re face-to-face and making eye contact, and tailoring short-term and long-term goals according to the child’s and family’s needs.
Ask open-ended questions: "Is this what you expected?" of parenting. About social support: "Who helps you with the baby?" About mood: "Being a new parent can be exhausting. How are you doing?" About work: "How much time off do you have from work for the new baby?" About behavior: "What upsets you most about your baby?"
Notice parent-infant interactions and support parents by acknowledging the relationship. Especially during times of distress, say something supportive like, "Your baby turns to you when he’s upset."
Dr. Nancy Thordarson, codirector of the meeting, used to follow a typical pediatrician’s impulse to show parents how to calm a child and be a better parent. Things have really shifted for the better in her practice since she started pointing out the relationship to parents with comments like, "I notice he turns to you for comfort when he’s stressed. He looks to you for support. Your relationship is helping him grow his brain."
Sometimes those simple sentences move a parent to tears, said Dr. Thordarson, a pediatrician in Marysville, Wash.
She teaches parents to first calm themselves, then calm the child. "Notice your feelings, take a breath," then try some specific suggestion for the particular behavior, she said. "Once they get that, you often don’t need to show them, ‘This is how you do it.’ "
Dr. Thordarson and other meeting organizers said interest is growing in promoting first relationships and reflective functioning. "We’re really hoping this will catch fire," she said.
Dr. Gold added that the 2013 meeting of the American Academy of Pediatrics will feature an emphasis on infant mental health.
The speakers reported having no financial disclosures.
BELLEVUE, WASH. – Dr. Claudia M. Gold spent 17 years in general and behavioral pediatrics being frustrated time and again by a familiar cycle: A parent would ask for help with a child’s problematic behavior, Dr. Gold’s "bag of behavioral tricks" wouldn’t help, the parent would begin to speak in increasingly negative terms about the child, and Dr. Gold would feel increasingly negative about the parent.
At a loss, she would recommend that the parent take the child to a therapist, the parent usually would not, and eventually the child would end up with a psychiatric diagnosis and on medication. Those years paralleled an explosion in diagnoses of pediatric bipolar disorder in the United States and the use of atypical antipsychotics in children with explosive behavior.
Then Dr. Gold took classes to learn more about infant mental health and attachment theory. She incorporated an emphasis on reflective relationships in her work, which "transformed my practice. Suddenly children were getting better. Amazing things were happening," said Dr. Gold, director of the Early Childhood Social Emotional Health Program at Newton-Wellesley Hospital, Newton, Mass.
The key to this change was implementing principles of reflective functioning, also known as "mentalization," which Dr. Gold calls "holding the child in mind." She and other speakers at a conference sponsored by the North Pacific Pediatric Society said that applying these principles to the pediatrician-parent relationship, and helping parents use them in the parent-child relationship, makes all the difference.
"Behavior problems" are problems of self-regulation of intense emotion, and self-regulation develops through coregulation in relationships with primary caregivers, Dr. Gold explained.
She starts by helping the parent reflect on the meaning of the child’s behavior, the child’s wants and needs, instead of just focusing on the behavior itself. "Even for a moment, reflect on the child’s experience. The child feels that, and calms down or begins to calm down. Parents begin to feel better," she said.
Dr. Gold outlined four essential components of reflective functioning in her book, "Keeping Your Child in Mind: Overcoming Defiance, Tantrums, and Other Everyday Behavior Problems by Seeing the World Through Your Child’s Eyes" (Boston: Da Capo Press, 2011):
1. Curiosity about the meaning of behavior. This means considering the thoughts and feelings driving a child’s behavior.
2. Empathy. This means reframing "difficult" behavior as "stressed" behavior.
3. Containing and regulating the child’s experience. This step can involve setting limits.
4. Self-regulation. This step involves the parent or pediatrician managing their own feelings.
When the pediatrician uses these same principles to reflect on the parent’s experience, that supports the parent’s efforts to reflect on the child’s experience, Paula D. Zeanah, Ph.D., said in a separate presentation.
Just as infants and young children in distress rely on the parental relationship, the pediatrician is "functioning as that go-to figure when the parent is in distress," said Dr. Zeanah, professor of clinical psychiatry at Tulane University and interim chief of pediatrics at Tulane Hospital for Children, both in New Orleans.
And just as a child’s behavior can trigger emotions and frustrations in the parent, the parent’s actions do the same for pediatricians. "We don’t spend enough time reflecting on how parents make us feel," she said.
Studies have shown that patients often provide clues to aspects of their inner lives that primary clinicians usually don’t recognize or acknowledge, missing opportunities for empathy and personal connection that are key to building the physician-patient relationship.
Dr. Zeanah recommended "really basic stuff that seems to make a difference," such as active listening, fewer interruptions, sitting so you’re face-to-face and making eye contact, and tailoring short-term and long-term goals according to the child’s and family’s needs.
Ask open-ended questions: "Is this what you expected?" of parenting. About social support: "Who helps you with the baby?" About mood: "Being a new parent can be exhausting. How are you doing?" About work: "How much time off do you have from work for the new baby?" About behavior: "What upsets you most about your baby?"
Notice parent-infant interactions and support parents by acknowledging the relationship. Especially during times of distress, say something supportive like, "Your baby turns to you when he’s upset."
Dr. Nancy Thordarson, codirector of the meeting, used to follow a typical pediatrician’s impulse to show parents how to calm a child and be a better parent. Things have really shifted for the better in her practice since she started pointing out the relationship to parents with comments like, "I notice he turns to you for comfort when he’s stressed. He looks to you for support. Your relationship is helping him grow his brain."
Sometimes those simple sentences move a parent to tears, said Dr. Thordarson, a pediatrician in Marysville, Wash.
She teaches parents to first calm themselves, then calm the child. "Notice your feelings, take a breath," then try some specific suggestion for the particular behavior, she said. "Once they get that, you often don’t need to show them, ‘This is how you do it.’ "
Dr. Thordarson and other meeting organizers said interest is growing in promoting first relationships and reflective functioning. "We’re really hoping this will catch fire," she said.
Dr. Gold added that the 2013 meeting of the American Academy of Pediatrics will feature an emphasis on infant mental health.
The speakers reported having no financial disclosures.
BELLEVUE, WASH. – Dr. Claudia M. Gold spent 17 years in general and behavioral pediatrics being frustrated time and again by a familiar cycle: A parent would ask for help with a child’s problematic behavior, Dr. Gold’s "bag of behavioral tricks" wouldn’t help, the parent would begin to speak in increasingly negative terms about the child, and Dr. Gold would feel increasingly negative about the parent.
At a loss, she would recommend that the parent take the child to a therapist, the parent usually would not, and eventually the child would end up with a psychiatric diagnosis and on medication. Those years paralleled an explosion in diagnoses of pediatric bipolar disorder in the United States and the use of atypical antipsychotics in children with explosive behavior.
Then Dr. Gold took classes to learn more about infant mental health and attachment theory. She incorporated an emphasis on reflective relationships in her work, which "transformed my practice. Suddenly children were getting better. Amazing things were happening," said Dr. Gold, director of the Early Childhood Social Emotional Health Program at Newton-Wellesley Hospital, Newton, Mass.
The key to this change was implementing principles of reflective functioning, also known as "mentalization," which Dr. Gold calls "holding the child in mind." She and other speakers at a conference sponsored by the North Pacific Pediatric Society said that applying these principles to the pediatrician-parent relationship, and helping parents use them in the parent-child relationship, makes all the difference.
"Behavior problems" are problems of self-regulation of intense emotion, and self-regulation develops through coregulation in relationships with primary caregivers, Dr. Gold explained.
She starts by helping the parent reflect on the meaning of the child’s behavior, the child’s wants and needs, instead of just focusing on the behavior itself. "Even for a moment, reflect on the child’s experience. The child feels that, and calms down or begins to calm down. Parents begin to feel better," she said.
Dr. Gold outlined four essential components of reflective functioning in her book, "Keeping Your Child in Mind: Overcoming Defiance, Tantrums, and Other Everyday Behavior Problems by Seeing the World Through Your Child’s Eyes" (Boston: Da Capo Press, 2011):
1. Curiosity about the meaning of behavior. This means considering the thoughts and feelings driving a child’s behavior.
2. Empathy. This means reframing "difficult" behavior as "stressed" behavior.
3. Containing and regulating the child’s experience. This step can involve setting limits.
4. Self-regulation. This step involves the parent or pediatrician managing their own feelings.
When the pediatrician uses these same principles to reflect on the parent’s experience, that supports the parent’s efforts to reflect on the child’s experience, Paula D. Zeanah, Ph.D., said in a separate presentation.
Just as infants and young children in distress rely on the parental relationship, the pediatrician is "functioning as that go-to figure when the parent is in distress," said Dr. Zeanah, professor of clinical psychiatry at Tulane University and interim chief of pediatrics at Tulane Hospital for Children, both in New Orleans.
And just as a child’s behavior can trigger emotions and frustrations in the parent, the parent’s actions do the same for pediatricians. "We don’t spend enough time reflecting on how parents make us feel," she said.
Studies have shown that patients often provide clues to aspects of their inner lives that primary clinicians usually don’t recognize or acknowledge, missing opportunities for empathy and personal connection that are key to building the physician-patient relationship.
Dr. Zeanah recommended "really basic stuff that seems to make a difference," such as active listening, fewer interruptions, sitting so you’re face-to-face and making eye contact, and tailoring short-term and long-term goals according to the child’s and family’s needs.
Ask open-ended questions: "Is this what you expected?" of parenting. About social support: "Who helps you with the baby?" About mood: "Being a new parent can be exhausting. How are you doing?" About work: "How much time off do you have from work for the new baby?" About behavior: "What upsets you most about your baby?"
Notice parent-infant interactions and support parents by acknowledging the relationship. Especially during times of distress, say something supportive like, "Your baby turns to you when he’s upset."
Dr. Nancy Thordarson, codirector of the meeting, used to follow a typical pediatrician’s impulse to show parents how to calm a child and be a better parent. Things have really shifted for the better in her practice since she started pointing out the relationship to parents with comments like, "I notice he turns to you for comfort when he’s stressed. He looks to you for support. Your relationship is helping him grow his brain."
Sometimes those simple sentences move a parent to tears, said Dr. Thordarson, a pediatrician in Marysville, Wash.
She teaches parents to first calm themselves, then calm the child. "Notice your feelings, take a breath," then try some specific suggestion for the particular behavior, she said. "Once they get that, you often don’t need to show them, ‘This is how you do it.’ "
Dr. Thordarson and other meeting organizers said interest is growing in promoting first relationships and reflective functioning. "We’re really hoping this will catch fire," she said.
Dr. Gold added that the 2013 meeting of the American Academy of Pediatrics will feature an emphasis on infant mental health.
The speakers reported having no financial disclosures.
AT A CONFERENCE SPONSORED BY THE NORTH PACIFIC PEDIATRIC SOCIETY