User login
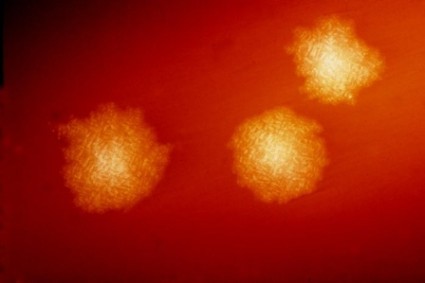
Promising C. difficile Antibiotic in Pipeline
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men to either the drug (single or multiple doses of cadazolid) or placebo. All subjects remained in the clinic for observation for 120 hours after the last dose.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
Negligible recovery of unchanged cadazolid in urine samples and the fact that most of the dose was recovered in feces suggests that treatment produced high concentrations at the colon. In fecal samples collected during days 6 and 10 of treatment, the mean cumulative recovery of unchanged cadazolid in feces was between 87% and 94%.
There were no significant changes in vital signs, ECG results, or laboratory parameters compared with baseline measurements, and no drug-related serious adverse events. All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
The dose or duration of treatment did not seem to affect the number of adverse events.
In the single-dose group, 8 of 30 subjects on cadazolid (27%) and 4 of 10 on placebo (40%) reported adverse events, most commonly headache and diarrhea. Four subjects on cadazolid (13%) and two on placebo (20%) reported headache, and three subjects on cadazolid (10%) and one on placebo (10%) reported diarrhea.
In the twice-a-day dosing group, 7 of 18 subjects on cadazolid (39%) and 1 of 6 subjects on placebo (17%) reported adverse events, most commonly headache in 5 subjects on cadazolid (28%) and 1 subject on placebo (17%).
Subjects were aged 45-60 years and had a body mass index of 18-32 kg/m2.
C. difficile is the most common cause of antibiotic-associated infectious diarrhea, especially among the elderly. The mainstays of treating C. difficile–associated infection, metronidazole or vancomycin, fail in approximately 20%-45% of patients.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men to either the drug (single or multiple doses of cadazolid) or placebo. All subjects remained in the clinic for observation for 120 hours after the last dose.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
Negligible recovery of unchanged cadazolid in urine samples and the fact that most of the dose was recovered in feces suggests that treatment produced high concentrations at the colon. In fecal samples collected during days 6 and 10 of treatment, the mean cumulative recovery of unchanged cadazolid in feces was between 87% and 94%.
There were no significant changes in vital signs, ECG results, or laboratory parameters compared with baseline measurements, and no drug-related serious adverse events. All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
The dose or duration of treatment did not seem to affect the number of adverse events.
In the single-dose group, 8 of 30 subjects on cadazolid (27%) and 4 of 10 on placebo (40%) reported adverse events, most commonly headache and diarrhea. Four subjects on cadazolid (13%) and two on placebo (20%) reported headache, and three subjects on cadazolid (10%) and one on placebo (10%) reported diarrhea.
In the twice-a-day dosing group, 7 of 18 subjects on cadazolid (39%) and 1 of 6 subjects on placebo (17%) reported adverse events, most commonly headache in 5 subjects on cadazolid (28%) and 1 subject on placebo (17%).
Subjects were aged 45-60 years and had a body mass index of 18-32 kg/m2.
C. difficile is the most common cause of antibiotic-associated infectious diarrhea, especially among the elderly. The mainstays of treating C. difficile–associated infection, metronidazole or vancomycin, fail in approximately 20%-45% of patients.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men to either the drug (single or multiple doses of cadazolid) or placebo. All subjects remained in the clinic for observation for 120 hours after the last dose.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
Negligible recovery of unchanged cadazolid in urine samples and the fact that most of the dose was recovered in feces suggests that treatment produced high concentrations at the colon. In fecal samples collected during days 6 and 10 of treatment, the mean cumulative recovery of unchanged cadazolid in feces was between 87% and 94%.
There were no significant changes in vital signs, ECG results, or laboratory parameters compared with baseline measurements, and no drug-related serious adverse events. All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
The dose or duration of treatment did not seem to affect the number of adverse events.
In the single-dose group, 8 of 30 subjects on cadazolid (27%) and 4 of 10 on placebo (40%) reported adverse events, most commonly headache and diarrhea. Four subjects on cadazolid (13%) and two on placebo (20%) reported headache, and three subjects on cadazolid (10%) and one on placebo (10%) reported diarrhea.
In the twice-a-day dosing group, 7 of 18 subjects on cadazolid (39%) and 1 of 6 subjects on placebo (17%) reported adverse events, most commonly headache in 5 subjects on cadazolid (28%) and 1 subject on placebo (17%).
Subjects were aged 45-60 years and had a body mass index of 18-32 kg/m2.
C. difficile is the most common cause of antibiotic-associated infectious diarrhea, especially among the elderly. The mainstays of treating C. difficile–associated infection, metronidazole or vancomycin, fail in approximately 20%-45% of patients.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: The experimental antibiotic cadazolid concentrated in feces with low systemic exposure and few side effects after single doses or twice-a-day dosing for 10 days.
Data Source: Data are from a randomized, placebo-controlled study in 64 healthy, nonsmoking men.
Disclosures: Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
Rifampin Combinations May Protect Against C. difficile Colitis
SAN FRANCISCO – The addition of rifampin to long-term antibiotic regimens significantly lowers the risk for Clostridium difficile–associated colitis in patients being treated for osteoarticular infections.
The retrospective cohort study comprised 393 treatment episodes – 55% of them for infections subsequent to arthroplasty – among patients admitted to a Swiss orthopedic surgery unit from 1996 to 2012. The ribotype 027 was not endemic in the region.
The 42% of patients who were treated with combination therapy that included oral rifampin (600 mg/day) were significantly less like to develop C. difficile colitis despite being on the antibiotics for a median of 63 days (ranging from 20-294 days), Caroline Landelle, Pharm.D., Ph.D. and her associates reported at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
Rifampin use was inversely associated with C. difficile colitis, with an adjusted hazard ratio of 0.18, Dr. Landelle reported in a poster presentation.
In general, longer duration of antibiotics treatment was associated with C. difficile colitis, with an adjusted hazard ratio of 1.01, said Dr. Landelle of the University of Geneva.
Factors not associated with colitis risk (either positively or negatively) included the use of antianaerobic antibiotics (in 38% of patients), treatment with intravenous vancomycin (in 45%, for a median of 13 days), age, or sex.
Fourteen patients (4%) developed symptomatic C. difficile colitis after a median of 14 days of antibiotic treatment (ranging from 8-193 days). Of these, six patients were on vancomycin (43%) and two patients were receiving rifampin (14%) prior to development of the colitis, Dr. Landelle reported at the meeting, sponsored by the American Society for Microbiology.
"C. difficile colitis was rare despite long-term antibiotic use among patients with osteoarticular infection. In contrast to intravenous vancomycin, combination antibiotic therapy with oral rifampin might protect against C. difficile–associated colitis," the investigators suggested.
The cohort had a median age of 69 years; 41% was female, and 31% of patients were immunosuppressed.
Of the 401 microorganisms isolated from the osteoarticular infections, 32% were methicillin-sensitive Staphylococcus aureus, 16% were methicillin-resistant S. aureus, 17% each were coagulase-negative Staphylococcus or gram-negative bacilli, and 18% were other organisms.
The investigators hypothesized that combination therapy with rifampin or derivative medications might protect against C. difficile colitis because very few cases have been reported of rifampin-associated pseudomembranous colitis, and patients undergoing treatment with long-term antibiotic combination therapy for osteoarticular infections rarely develop symptomatic C. difficile–associated disease.
Rifaximin and other antibiotics belonging to the macrocyclic family are being investigated as alternative therapies for C. difficile–associated disease, Dr. Landelle said. Some studies have shown high rates of C. difficile resistance to rifampin in Europe, but the rate of resistance at her institution was low. In Switzerland, rifamycin antibiotics have been used for decades, but rifaximin is not licensed for the treatment of hepatic encephalopathy, diarrhea, and traveler’s diarrhea or for prophylaxis in patients undergoing GI surgery, which may explain the low rate of resistance there.
The study excluded patients with prior episodes of C. difficile–associated disease, patients being treated with metronidazole, and patients with septic arthritis.
Dr. Landelle did not provide her financial disclosures.
SAN FRANCISCO – The addition of rifampin to long-term antibiotic regimens significantly lowers the risk for Clostridium difficile–associated colitis in patients being treated for osteoarticular infections.
The retrospective cohort study comprised 393 treatment episodes – 55% of them for infections subsequent to arthroplasty – among patients admitted to a Swiss orthopedic surgery unit from 1996 to 2012. The ribotype 027 was not endemic in the region.
The 42% of patients who were treated with combination therapy that included oral rifampin (600 mg/day) were significantly less like to develop C. difficile colitis despite being on the antibiotics for a median of 63 days (ranging from 20-294 days), Caroline Landelle, Pharm.D., Ph.D. and her associates reported at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
Rifampin use was inversely associated with C. difficile colitis, with an adjusted hazard ratio of 0.18, Dr. Landelle reported in a poster presentation.
In general, longer duration of antibiotics treatment was associated with C. difficile colitis, with an adjusted hazard ratio of 1.01, said Dr. Landelle of the University of Geneva.
Factors not associated with colitis risk (either positively or negatively) included the use of antianaerobic antibiotics (in 38% of patients), treatment with intravenous vancomycin (in 45%, for a median of 13 days), age, or sex.
Fourteen patients (4%) developed symptomatic C. difficile colitis after a median of 14 days of antibiotic treatment (ranging from 8-193 days). Of these, six patients were on vancomycin (43%) and two patients were receiving rifampin (14%) prior to development of the colitis, Dr. Landelle reported at the meeting, sponsored by the American Society for Microbiology.
"C. difficile colitis was rare despite long-term antibiotic use among patients with osteoarticular infection. In contrast to intravenous vancomycin, combination antibiotic therapy with oral rifampin might protect against C. difficile–associated colitis," the investigators suggested.
The cohort had a median age of 69 years; 41% was female, and 31% of patients were immunosuppressed.
Of the 401 microorganisms isolated from the osteoarticular infections, 32% were methicillin-sensitive Staphylococcus aureus, 16% were methicillin-resistant S. aureus, 17% each were coagulase-negative Staphylococcus or gram-negative bacilli, and 18% were other organisms.
The investigators hypothesized that combination therapy with rifampin or derivative medications might protect against C. difficile colitis because very few cases have been reported of rifampin-associated pseudomembranous colitis, and patients undergoing treatment with long-term antibiotic combination therapy for osteoarticular infections rarely develop symptomatic C. difficile–associated disease.
Rifaximin and other antibiotics belonging to the macrocyclic family are being investigated as alternative therapies for C. difficile–associated disease, Dr. Landelle said. Some studies have shown high rates of C. difficile resistance to rifampin in Europe, but the rate of resistance at her institution was low. In Switzerland, rifamycin antibiotics have been used for decades, but rifaximin is not licensed for the treatment of hepatic encephalopathy, diarrhea, and traveler’s diarrhea or for prophylaxis in patients undergoing GI surgery, which may explain the low rate of resistance there.
The study excluded patients with prior episodes of C. difficile–associated disease, patients being treated with metronidazole, and patients with septic arthritis.
Dr. Landelle did not provide her financial disclosures.
SAN FRANCISCO – The addition of rifampin to long-term antibiotic regimens significantly lowers the risk for Clostridium difficile–associated colitis in patients being treated for osteoarticular infections.
The retrospective cohort study comprised 393 treatment episodes – 55% of them for infections subsequent to arthroplasty – among patients admitted to a Swiss orthopedic surgery unit from 1996 to 2012. The ribotype 027 was not endemic in the region.
The 42% of patients who were treated with combination therapy that included oral rifampin (600 mg/day) were significantly less like to develop C. difficile colitis despite being on the antibiotics for a median of 63 days (ranging from 20-294 days), Caroline Landelle, Pharm.D., Ph.D. and her associates reported at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
Rifampin use was inversely associated with C. difficile colitis, with an adjusted hazard ratio of 0.18, Dr. Landelle reported in a poster presentation.
In general, longer duration of antibiotics treatment was associated with C. difficile colitis, with an adjusted hazard ratio of 1.01, said Dr. Landelle of the University of Geneva.
Factors not associated with colitis risk (either positively or negatively) included the use of antianaerobic antibiotics (in 38% of patients), treatment with intravenous vancomycin (in 45%, for a median of 13 days), age, or sex.
Fourteen patients (4%) developed symptomatic C. difficile colitis after a median of 14 days of antibiotic treatment (ranging from 8-193 days). Of these, six patients were on vancomycin (43%) and two patients were receiving rifampin (14%) prior to development of the colitis, Dr. Landelle reported at the meeting, sponsored by the American Society for Microbiology.
"C. difficile colitis was rare despite long-term antibiotic use among patients with osteoarticular infection. In contrast to intravenous vancomycin, combination antibiotic therapy with oral rifampin might protect against C. difficile–associated colitis," the investigators suggested.
The cohort had a median age of 69 years; 41% was female, and 31% of patients were immunosuppressed.
Of the 401 microorganisms isolated from the osteoarticular infections, 32% were methicillin-sensitive Staphylococcus aureus, 16% were methicillin-resistant S. aureus, 17% each were coagulase-negative Staphylococcus or gram-negative bacilli, and 18% were other organisms.
The investigators hypothesized that combination therapy with rifampin or derivative medications might protect against C. difficile colitis because very few cases have been reported of rifampin-associated pseudomembranous colitis, and patients undergoing treatment with long-term antibiotic combination therapy for osteoarticular infections rarely develop symptomatic C. difficile–associated disease.
Rifaximin and other antibiotics belonging to the macrocyclic family are being investigated as alternative therapies for C. difficile–associated disease, Dr. Landelle said. Some studies have shown high rates of C. difficile resistance to rifampin in Europe, but the rate of resistance at her institution was low. In Switzerland, rifamycin antibiotics have been used for decades, but rifaximin is not licensed for the treatment of hepatic encephalopathy, diarrhea, and traveler’s diarrhea or for prophylaxis in patients undergoing GI surgery, which may explain the low rate of resistance there.
The study excluded patients with prior episodes of C. difficile–associated disease, patients being treated with metronidazole, and patients with septic arthritis.
Dr. Landelle did not provide her financial disclosures.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Among 14 patients who developed C. difficile colitis during long-term antibiotic treatment for osteoarticular infections, 2 were on combination regimens including rifampin (14%), compared with 6 who were on vancomycin (43%).
Data Source: Results were taken from a Swiss retrospective cohort study of 393 treatment episodes for osteoarticular infections at one institution, 42% of which used combination rifampin regimens and 45% of which used vancomycin.
Disclosures: Dr. Landelle did not provide her financial disclosures.
Glycemic Variation Increased in Nondiabetic Obese People
HOUSTON – Data from 42 morbidly obese people who applied to be on the television show "The Biggest Loser" showed significantly greater glycemic variability even without diabetes, compared with previous data on nondiabetic, normal-weight adults.
Oxidative stress from the glycemic variability may contribute to microvascular and macrovascular changes in obese people and help explain why some obese people develop advanced cardiovascular disease and increased risk for cardiovascular events, investigators said at the annual meeting of the Endocrine Society.
"The Biggest Loser" applicants wore a masked continuous glucose monitor for 3-8 days as part of the application process. Four patients with type 1 or type 2 diabetes were excluded from the analysis, leaving 23 people with normal glucose tolerance and 15 who were classified as having prediabetes. The investigators compared the swings between high and low glucose readings in these 38 patients with historic data on 37 age-matched, nondiabetic, normal-weight people from the Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (Diabetes Care 33;6:1297-9).
The average hemoglobin A1c was 5.3% in the normoglycemic but obese applicants and 5.4% in the nonobese control group, compared with 5.8% in the obese applicants.
The standard deviation in glucose measures was 24 mg/dL in both the normoglycemic applicants and the prediabetic applicants, compared with 12 mg/dL in the nonobese control group, Sara J. Salkind and her associates reported. Other standard measures of glycemic variability showed similar trends. The mean amplitude of glycemic excursion was 48 mg/dL in the normoglycemic applicants and 50 mg/dL in the prediabetic group, compared with 27 mg/dL the control group.
The percentage of glucose values that fell within the range of 81-139 mg/dL was 77% in the normoglycemic applicants and 78% in the prediabetic group, compared with 99% in the control group. Glucose values below 80 mg/dL comprised 11% of values in the "normal" obese group and 5% of values in the prediabetes group, compared with 0.3% of values in the control group. Glucose values higher than 140 mg/dL comprised 12% of measures in the "normal" obese group, 18% of measures in the prediabetes group, and 0.3% of values in the control group.
If "normal" glycemic status is defined as a HbA1c less than 5.7%, a fasting glucose level less than 100 mg/dL, and a 2-hour postprandial glucose load of less than 140 mg/dL, then "these obese people, who by almost all the traditional measures have normal glycemia, have increased variability and much greater variability than normals of similar age" who are not obese, coinvestigator Robert A. Vigersky, Col., MC, USA, said in an interview.
Both Ms. Salkind and Dr. Vigersky are with the endocrinology service at Walter Reed National Military Medical Center, Bethesda, Md. The investigators’ report reflects the personal views of the authors and not the official views of the United States Army or the Department of Defense.
People with diabetes are known to have glycemic variability, but there are few previous data on glycemic variability in people without diabetes. The current findings have implications for the pathophysiology of microvascular disease and, combined with previous studies suggesting that obese people have increased carotid intima-media thickness, compared with normal-weight people, may increase understanding of cardiovascular risk from obesity.
Measures of glycemic variability also may have a more practical application as a behavior-modification tool to help obese people understand the effects of their eating habits on their bodies. The investigators said they will pursue studies to see if continuous glucose monitoring might help obese patients lose weight and avoid converting to prediabetes or diabetes.
The average age in the current study was 32 years in the "normal" group and 34 years in the prediabetes group. The average body mass index was 50 and 51 kg/m2, respectively. The 2-hour post-glucose load averaged 107 mg/dL for normoglycemic applicants and 145 mg/dL in the prediabetes group. The fasting plasma glucose averaged 89 mg/dL in the "normal" group and 97 mg/dL in the prediabetes group. Hypertension was present in 76% and 93%, respectively.
Dexcom, which makes continuous glucose meters, funded the study. The investigators reported having no other financial disclosures.
HOUSTON – Data from 42 morbidly obese people who applied to be on the television show "The Biggest Loser" showed significantly greater glycemic variability even without diabetes, compared with previous data on nondiabetic, normal-weight adults.
Oxidative stress from the glycemic variability may contribute to microvascular and macrovascular changes in obese people and help explain why some obese people develop advanced cardiovascular disease and increased risk for cardiovascular events, investigators said at the annual meeting of the Endocrine Society.
"The Biggest Loser" applicants wore a masked continuous glucose monitor for 3-8 days as part of the application process. Four patients with type 1 or type 2 diabetes were excluded from the analysis, leaving 23 people with normal glucose tolerance and 15 who were classified as having prediabetes. The investigators compared the swings between high and low glucose readings in these 38 patients with historic data on 37 age-matched, nondiabetic, normal-weight people from the Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (Diabetes Care 33;6:1297-9).
The average hemoglobin A1c was 5.3% in the normoglycemic but obese applicants and 5.4% in the nonobese control group, compared with 5.8% in the obese applicants.
The standard deviation in glucose measures was 24 mg/dL in both the normoglycemic applicants and the prediabetic applicants, compared with 12 mg/dL in the nonobese control group, Sara J. Salkind and her associates reported. Other standard measures of glycemic variability showed similar trends. The mean amplitude of glycemic excursion was 48 mg/dL in the normoglycemic applicants and 50 mg/dL in the prediabetic group, compared with 27 mg/dL the control group.
The percentage of glucose values that fell within the range of 81-139 mg/dL was 77% in the normoglycemic applicants and 78% in the prediabetic group, compared with 99% in the control group. Glucose values below 80 mg/dL comprised 11% of values in the "normal" obese group and 5% of values in the prediabetes group, compared with 0.3% of values in the control group. Glucose values higher than 140 mg/dL comprised 12% of measures in the "normal" obese group, 18% of measures in the prediabetes group, and 0.3% of values in the control group.
If "normal" glycemic status is defined as a HbA1c less than 5.7%, a fasting glucose level less than 100 mg/dL, and a 2-hour postprandial glucose load of less than 140 mg/dL, then "these obese people, who by almost all the traditional measures have normal glycemia, have increased variability and much greater variability than normals of similar age" who are not obese, coinvestigator Robert A. Vigersky, Col., MC, USA, said in an interview.
Both Ms. Salkind and Dr. Vigersky are with the endocrinology service at Walter Reed National Military Medical Center, Bethesda, Md. The investigators’ report reflects the personal views of the authors and not the official views of the United States Army or the Department of Defense.
People with diabetes are known to have glycemic variability, but there are few previous data on glycemic variability in people without diabetes. The current findings have implications for the pathophysiology of microvascular disease and, combined with previous studies suggesting that obese people have increased carotid intima-media thickness, compared with normal-weight people, may increase understanding of cardiovascular risk from obesity.
Measures of glycemic variability also may have a more practical application as a behavior-modification tool to help obese people understand the effects of their eating habits on their bodies. The investigators said they will pursue studies to see if continuous glucose monitoring might help obese patients lose weight and avoid converting to prediabetes or diabetes.
The average age in the current study was 32 years in the "normal" group and 34 years in the prediabetes group. The average body mass index was 50 and 51 kg/m2, respectively. The 2-hour post-glucose load averaged 107 mg/dL for normoglycemic applicants and 145 mg/dL in the prediabetes group. The fasting plasma glucose averaged 89 mg/dL in the "normal" group and 97 mg/dL in the prediabetes group. Hypertension was present in 76% and 93%, respectively.
Dexcom, which makes continuous glucose meters, funded the study. The investigators reported having no other financial disclosures.
HOUSTON – Data from 42 morbidly obese people who applied to be on the television show "The Biggest Loser" showed significantly greater glycemic variability even without diabetes, compared with previous data on nondiabetic, normal-weight adults.
Oxidative stress from the glycemic variability may contribute to microvascular and macrovascular changes in obese people and help explain why some obese people develop advanced cardiovascular disease and increased risk for cardiovascular events, investigators said at the annual meeting of the Endocrine Society.
"The Biggest Loser" applicants wore a masked continuous glucose monitor for 3-8 days as part of the application process. Four patients with type 1 or type 2 diabetes were excluded from the analysis, leaving 23 people with normal glucose tolerance and 15 who were classified as having prediabetes. The investigators compared the swings between high and low glucose readings in these 38 patients with historic data on 37 age-matched, nondiabetic, normal-weight people from the Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (Diabetes Care 33;6:1297-9).
The average hemoglobin A1c was 5.3% in the normoglycemic but obese applicants and 5.4% in the nonobese control group, compared with 5.8% in the obese applicants.
The standard deviation in glucose measures was 24 mg/dL in both the normoglycemic applicants and the prediabetic applicants, compared with 12 mg/dL in the nonobese control group, Sara J. Salkind and her associates reported. Other standard measures of glycemic variability showed similar trends. The mean amplitude of glycemic excursion was 48 mg/dL in the normoglycemic applicants and 50 mg/dL in the prediabetic group, compared with 27 mg/dL the control group.
The percentage of glucose values that fell within the range of 81-139 mg/dL was 77% in the normoglycemic applicants and 78% in the prediabetic group, compared with 99% in the control group. Glucose values below 80 mg/dL comprised 11% of values in the "normal" obese group and 5% of values in the prediabetes group, compared with 0.3% of values in the control group. Glucose values higher than 140 mg/dL comprised 12% of measures in the "normal" obese group, 18% of measures in the prediabetes group, and 0.3% of values in the control group.
If "normal" glycemic status is defined as a HbA1c less than 5.7%, a fasting glucose level less than 100 mg/dL, and a 2-hour postprandial glucose load of less than 140 mg/dL, then "these obese people, who by almost all the traditional measures have normal glycemia, have increased variability and much greater variability than normals of similar age" who are not obese, coinvestigator Robert A. Vigersky, Col., MC, USA, said in an interview.
Both Ms. Salkind and Dr. Vigersky are with the endocrinology service at Walter Reed National Military Medical Center, Bethesda, Md. The investigators’ report reflects the personal views of the authors and not the official views of the United States Army or the Department of Defense.
People with diabetes are known to have glycemic variability, but there are few previous data on glycemic variability in people without diabetes. The current findings have implications for the pathophysiology of microvascular disease and, combined with previous studies suggesting that obese people have increased carotid intima-media thickness, compared with normal-weight people, may increase understanding of cardiovascular risk from obesity.
Measures of glycemic variability also may have a more practical application as a behavior-modification tool to help obese people understand the effects of their eating habits on their bodies. The investigators said they will pursue studies to see if continuous glucose monitoring might help obese patients lose weight and avoid converting to prediabetes or diabetes.
The average age in the current study was 32 years in the "normal" group and 34 years in the prediabetes group. The average body mass index was 50 and 51 kg/m2, respectively. The 2-hour post-glucose load averaged 107 mg/dL for normoglycemic applicants and 145 mg/dL in the prediabetes group. The fasting plasma glucose averaged 89 mg/dL in the "normal" group and 97 mg/dL in the prediabetes group. Hypertension was present in 76% and 93%, respectively.
Dexcom, which makes continuous glucose meters, funded the study. The investigators reported having no other financial disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Continuous glucose meter readings showed a standard deviation of 24 mg/dL in obese people with normal glycemic status or prediabetes, compared with 12 mg/dL in normal-weight healthy controls.
Data Source: Prospective continuous glucose monitoring in 38 nondiabetic obese people, compared with historical data on 37 nonobese, nondiabetic people of similar age.
Disclosures: Dexcom, which makes continuous glucose meters, funded the study. The investigators reported having no other financial disclosures.
Computer Algorithm Improved ICU Glucose Control
HOUSTON – Nurses using a computerized algorithm maintained better glycemic control, compared with expert nursing care without the algorithm, in a prospective, randomized study of 300 patients in one institution’s ICU.
Baseline characteristics did not differ between the 151 patients randomized to nursing care and the 149 patients cared for by nurses using the LOGIC-Insulin computerized algorithm developed by Dr. Dieter Mesotten and his associates at Catholic University of Leuven, Belgium. Mean blood glucose levels during ICU care also were similar between groups: 106 mg/dL in both groups.
On other measures of glycemic control, however, the LOGIC group scored significantly better than did the nurses group, he reported in a poster presentation at the annual meeting of the Endocrine Society. The LOGIC group had a significantly lower mean score on the Glycemic Penalty Index, a marker of efficacy of blood glucose control that was the primary outcome measure of efficacy in the study: 9.8 vs. 12.4 in the nurses group.
Patients in the LOGIC group were less likely to develop critically low glucose levels, they spent more time in the study’s target range of 80-110mg/dL, and they had narrower swings between minimum and maximum blood-sugar measurements, indicating less blood glucose variability.
Mean scores on the Hyperglycemic Index were significantly lower in the LOGIC group (2.5 mg/dL), compared with the nurses group (4.2 mg/dL). Patients in the LOGIC group reached the target range of 80-110 mg/dL faster (in 2 hours on average instead of 3 hours in the nurses group) and were within the target range 69% of the time while in the ICU, compared with 60% of the time for patients in the nurses group. The mean daily difference between minimum and maximum blood glucose levels was 31 mg/dL in the LOGIC group and 37 mg/dL in the nurses group, Dr. Mesotten reported.
The patients had been admitted to the ICU after cardiac surgery (49% in the nurses group and 51% in the LOGIC group), following transplantation (17% and 13%, respectively), because of medical problems (15% and 17%), respectively, or for other reasons.
In general, maintaining tight blood control in critically ill patients is labor intensive and difficult. The LOGIC algorithm may have made this task more successful but also appeared to add a bit to the nursing team’s workload by increasing the frequency of glucose measurements. Nurses in the LOGIC group measured blood glucose levels every 2.2 hours on average, compared with every 2.5 hours in the nursing-only group, a statistically significant difference.
Patients averaged 64 years in age, 60% were male, and 21% had diabetes when admitted to the ICU.
Dr. Mesotten reported having no financial disclosures. Belgian public agencies funded the study.
nursing care, LOGIC-Insulin computerized algorithm, Dr. Dieter Mesotten, Glycemic Penalty Index, Hyperglycemic Index,
HOUSTON – Nurses using a computerized algorithm maintained better glycemic control, compared with expert nursing care without the algorithm, in a prospective, randomized study of 300 patients in one institution’s ICU.
Baseline characteristics did not differ between the 151 patients randomized to nursing care and the 149 patients cared for by nurses using the LOGIC-Insulin computerized algorithm developed by Dr. Dieter Mesotten and his associates at Catholic University of Leuven, Belgium. Mean blood glucose levels during ICU care also were similar between groups: 106 mg/dL in both groups.
On other measures of glycemic control, however, the LOGIC group scored significantly better than did the nurses group, he reported in a poster presentation at the annual meeting of the Endocrine Society. The LOGIC group had a significantly lower mean score on the Glycemic Penalty Index, a marker of efficacy of blood glucose control that was the primary outcome measure of efficacy in the study: 9.8 vs. 12.4 in the nurses group.
Patients in the LOGIC group were less likely to develop critically low glucose levels, they spent more time in the study’s target range of 80-110mg/dL, and they had narrower swings between minimum and maximum blood-sugar measurements, indicating less blood glucose variability.
Mean scores on the Hyperglycemic Index were significantly lower in the LOGIC group (2.5 mg/dL), compared with the nurses group (4.2 mg/dL). Patients in the LOGIC group reached the target range of 80-110 mg/dL faster (in 2 hours on average instead of 3 hours in the nurses group) and were within the target range 69% of the time while in the ICU, compared with 60% of the time for patients in the nurses group. The mean daily difference between minimum and maximum blood glucose levels was 31 mg/dL in the LOGIC group and 37 mg/dL in the nurses group, Dr. Mesotten reported.
The patients had been admitted to the ICU after cardiac surgery (49% in the nurses group and 51% in the LOGIC group), following transplantation (17% and 13%, respectively), because of medical problems (15% and 17%), respectively, or for other reasons.
In general, maintaining tight blood control in critically ill patients is labor intensive and difficult. The LOGIC algorithm may have made this task more successful but also appeared to add a bit to the nursing team’s workload by increasing the frequency of glucose measurements. Nurses in the LOGIC group measured blood glucose levels every 2.2 hours on average, compared with every 2.5 hours in the nursing-only group, a statistically significant difference.
Patients averaged 64 years in age, 60% were male, and 21% had diabetes when admitted to the ICU.
Dr. Mesotten reported having no financial disclosures. Belgian public agencies funded the study.
HOUSTON – Nurses using a computerized algorithm maintained better glycemic control, compared with expert nursing care without the algorithm, in a prospective, randomized study of 300 patients in one institution’s ICU.
Baseline characteristics did not differ between the 151 patients randomized to nursing care and the 149 patients cared for by nurses using the LOGIC-Insulin computerized algorithm developed by Dr. Dieter Mesotten and his associates at Catholic University of Leuven, Belgium. Mean blood glucose levels during ICU care also were similar between groups: 106 mg/dL in both groups.
On other measures of glycemic control, however, the LOGIC group scored significantly better than did the nurses group, he reported in a poster presentation at the annual meeting of the Endocrine Society. The LOGIC group had a significantly lower mean score on the Glycemic Penalty Index, a marker of efficacy of blood glucose control that was the primary outcome measure of efficacy in the study: 9.8 vs. 12.4 in the nurses group.
Patients in the LOGIC group were less likely to develop critically low glucose levels, they spent more time in the study’s target range of 80-110mg/dL, and they had narrower swings between minimum and maximum blood-sugar measurements, indicating less blood glucose variability.
Mean scores on the Hyperglycemic Index were significantly lower in the LOGIC group (2.5 mg/dL), compared with the nurses group (4.2 mg/dL). Patients in the LOGIC group reached the target range of 80-110 mg/dL faster (in 2 hours on average instead of 3 hours in the nurses group) and were within the target range 69% of the time while in the ICU, compared with 60% of the time for patients in the nurses group. The mean daily difference between minimum and maximum blood glucose levels was 31 mg/dL in the LOGIC group and 37 mg/dL in the nurses group, Dr. Mesotten reported.
The patients had been admitted to the ICU after cardiac surgery (49% in the nurses group and 51% in the LOGIC group), following transplantation (17% and 13%, respectively), because of medical problems (15% and 17%), respectively, or for other reasons.
In general, maintaining tight blood control in critically ill patients is labor intensive and difficult. The LOGIC algorithm may have made this task more successful but also appeared to add a bit to the nursing team’s workload by increasing the frequency of glucose measurements. Nurses in the LOGIC group measured blood glucose levels every 2.2 hours on average, compared with every 2.5 hours in the nursing-only group, a statistically significant difference.
Patients averaged 64 years in age, 60% were male, and 21% had diabetes when admitted to the ICU.
Dr. Mesotten reported having no financial disclosures. Belgian public agencies funded the study.
nursing care, LOGIC-Insulin computerized algorithm, Dr. Dieter Mesotten, Glycemic Penalty Index, Hyperglycemic Index,
nursing care, LOGIC-Insulin computerized algorithm, Dr. Dieter Mesotten, Glycemic Penalty Index, Hyperglycemic Index,
FROM THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: Use of the LOGIC computerized algorithm improved scores on the Glycemic Penalty Index to a mean of 9.8 during ICU care, compared with a mean score of 12.4 under expert nursing care alone.
Data Source: Prospective, randomized, single-blind study in 300 patients managed in one institution’s ICU.
Disclosures: Dr. Mesotten reported having no financial disclosures. Belgian public agencies funded the study.
Therapy-Resistant Asthma May Be Neither
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
X-Ray Illustrates Constipation Pain for Parents
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Partner Violence, Reproductive Coercion Are Teen Problems
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
Include 'Legal Highs,' Designer Drugs in Screening
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC CONFERENCE
Fight Obesity with Specific, Countable Goals
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Experimental Drug Improves Muscle Strength in Cancer
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: The experimental drug enobosarm significantly improved physical function on a stair-climb test by 17% in hypogonadal men with cancer and by 12% in eugonadal men with cancer, compared with nonsignificant improvements in men on placebo.
Data Source: Data are from an analysis of data on a secondary end point (physical function) in 93 men from a randomized, double-blind, multicenter trial in 159 cancer patients.
Disclosures: GTx, the company that is developing enobosarm, funded the study. Dr. Dobs reported having no other financial disclosures.