User login
Diet and Skin: A Primer
Dermatologists frequently learn about skin conditions that are directly linked to diet. For example, we know that nutritional deficiencies can impact the hair, skin, and nails, and that celiac disease manifests with dermatitis herpetiformis of the skin. Patients commonly ask their dermatologists about the impact of diet on their skin. There are many outdated myths, but research on the subject is increasingly demonstrating important associations. Dermatologists must become familiar with the data on this topic so that we can provide informed counseling for our patients. This article reviews the current literature on associations between diet and 3 common cutaneous conditions—acne, psoriasis, and atopic dermatitis [AD]—and provides tips on how to best address our patients’ questions on this topic.
Acne
Studies increasingly support an association between a high glycemic diet (foods that lead to a spike in serum glucose) and acne; Bowe et al1 provided an excellent summary of the topic in 2010. This year, a large prospective cohort study of more than 24,000 participants demonstrated an association between adult acne and a diet high in milk, sugary beverages and foods, and fatty foods.2 In prospective cohort studies of more than 6000 adolescent girls and 4000 adolescent boys, Adebamowo et al3,4 demonstrated a correlation between skim milk consumption and acne. Whey protein supplementation also has been implicated in acne flares.5,6 The biological mechanism of the impact of high glycemic index foods and acne is believed to be mainly via activation of the insulinlike growth factor 1 (IGF-1) pathway, which promotes androgen synthesis and increases androgen bioavailability via decreased synthesis of sex hormone binding globulin.1,2 Insulinlike growth factor 1 also stimulates its downstream target, mammalian target of rapamycin (mTOR), leading to activation of antiapoptotic and proliferation signaling, ultimately resulting in oxidative stress and inflammation causing acne.2 Penso et al2 noted that patients with IGF-1 deficiency (Laron syndrome) never develop acne unless treated with exogenous IGF-1, further supporting its role in acne formation.7 There currently is a paucity of randomized controlled trials assessing the impact of diet on acne.
Psoriasis
The literature consistently shows that obesity is a predisposing factor for psoriasis. Additionally, weight gain may cause flares of existing psoriasis.8 Promotion of a healthy diet is an important factor in the management of obesity, alongside physical activity and, in some cases, medication and bariatric surgery.9 Patients with psoriasis who are overweight have been shown to experience improvement in their psoriasis after weight loss secondary to diet and exercise.8,10 The joint American Academy of Dermatology and National Psoriasis Foundation guidelines recommend that dermatologists advise patients to practice a healthy lifestyle including a healthy diet and communicate with a patient’s primary care provider so they can be appropriately evaluated and treated for comorbidities including metabolic syndrome, diabetes, and hyperlipidemia.11 In the NutriNet-Santé cohort study, investigators found an inverse correlation between psoriasis severity and adherence to a Mediterranean diet, which the authors conclude supports the hypothesis that this may slow the progression of psoriasis.12 In a single meta-analysis, it was reported that patients with psoriasis have a 3-fold increased risk for celiac disease compared to the general population.13 It remains unknown if these data are generalizable to the US population. Dermatologists should consider screening patients with psoriasis for celiac disease based on reported symptoms. When suspected, it is necessary to order appropriate serologies and consider referral to gastroenterology prior to recommending a gluten-free diet, as elimination of gluten prior to testing may lead to false-negative results.
Atopic Dermatitis
Patients and parents/guardians of children with AD often ask about the impact of diet on the condition. A small minority of patients may experience flares of AD due to ongoing, non–IgE-mediated allergen exposure.14 Diet as a trigger for flares should be suspected in children with persistent, moderate to severe AD. In these patients, allergen avoidance may lead to improvement but not resolution of AD. Allergens ordered from most common to least common are the following: eggs, milk, peanuts/tree nuts, shellfish, soy, and wheat.15 Additionally, it is important to note that children with AD are at higher risk for developing life-threatening, IgE-mediated food allergies compared to the general population (37% vs 6.8%).16,17 The LEAP (Learning Early about Peanut Allergy) study led to a paradigm shift in prevention of peanut allergies in high-risk children (ie, those with severe AD and/or egg allergy), providing data to support the idea that early introduction of allergenic foods such as peanuts may prevent severe allergies.18 Further studies are necessary to clarify the population in which allergen testing and recommendations on food avoidance are warranted vs early introduction.19
Conclusion
Early data support the relationship between diet and many common dermatologic conditions, including acne, psoriasis, and AD. Dermatologists should be familiar with the evidence supporting the relationship between diet and various skin conditions to best answer patients’ questions and counsel as appropriate. It is important for dermatologists to continue to stay up-to-date on the literature on this subject as new data emerge. Knowledge about the relationship between diet and skin allows dermatologists to not only support our patients’ skin health but their overall health as well.
- Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63:124-141.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in teenaged boys. J Am Acad Dermatol. 2008;58:787-793.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in adolescent girls. Dermatol Online J. 2006;12:1.
- Silverberg NB. Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes. Cutis. 2012;90:70-72.
- Cengiz FP, Cemil BC, Emiroglu N, et al. Acne located on the trunk, whey protein supplementation: is there any association? Health Promot Perspect. 2017;7:106-108.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Jensen P, Skov L. Psoriasis and obesity [published online February 23, 2017]. Dermatology. 2016;232:633-639.
- Extreme obesity, and what you can do. American Heart Association website. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight/extreme-obesity-and-what-you-can-do. Updated April 18, 2014. Accessed November 30, 2020.
- Naldi L, Conti A, Cazzaniga S, et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol. 2014;170:634-642.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Silverberg NB, Lee-Wong M, Yosipovitch G. Diet and atopic dermatitis. Cutis. 2016;97:227-232.
- Bieber T, Bussmann C. Atopic dermatitis. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:203-218.
- Eigenmann PA, Sicherer SH, Borkowski TA, et al. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998;101:E8.
- Age-adjusted percentages (with standard errors) of hay fever, respiratory allergies, food allergies, and skin allergies in the past 12 months for children under age 18 years, by selected characteristics: United States, 2016. CDC website. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_C-2.pdf. Accessed December 8, 2020.
- Du Toit G, Roberts G, Sayre PH, et al; LEAP study team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Sugita K, Akdis CA. Recent developments and advances in atopic dermatitis and food allergy [published online October 22, 2019]. Allergol Int. 2020;69:204-214.
Dermatologists frequently learn about skin conditions that are directly linked to diet. For example, we know that nutritional deficiencies can impact the hair, skin, and nails, and that celiac disease manifests with dermatitis herpetiformis of the skin. Patients commonly ask their dermatologists about the impact of diet on their skin. There are many outdated myths, but research on the subject is increasingly demonstrating important associations. Dermatologists must become familiar with the data on this topic so that we can provide informed counseling for our patients. This article reviews the current literature on associations between diet and 3 common cutaneous conditions—acne, psoriasis, and atopic dermatitis [AD]—and provides tips on how to best address our patients’ questions on this topic.
Acne
Studies increasingly support an association between a high glycemic diet (foods that lead to a spike in serum glucose) and acne; Bowe et al1 provided an excellent summary of the topic in 2010. This year, a large prospective cohort study of more than 24,000 participants demonstrated an association between adult acne and a diet high in milk, sugary beverages and foods, and fatty foods.2 In prospective cohort studies of more than 6000 adolescent girls and 4000 adolescent boys, Adebamowo et al3,4 demonstrated a correlation between skim milk consumption and acne. Whey protein supplementation also has been implicated in acne flares.5,6 The biological mechanism of the impact of high glycemic index foods and acne is believed to be mainly via activation of the insulinlike growth factor 1 (IGF-1) pathway, which promotes androgen synthesis and increases androgen bioavailability via decreased synthesis of sex hormone binding globulin.1,2 Insulinlike growth factor 1 also stimulates its downstream target, mammalian target of rapamycin (mTOR), leading to activation of antiapoptotic and proliferation signaling, ultimately resulting in oxidative stress and inflammation causing acne.2 Penso et al2 noted that patients with IGF-1 deficiency (Laron syndrome) never develop acne unless treated with exogenous IGF-1, further supporting its role in acne formation.7 There currently is a paucity of randomized controlled trials assessing the impact of diet on acne.
Psoriasis
The literature consistently shows that obesity is a predisposing factor for psoriasis. Additionally, weight gain may cause flares of existing psoriasis.8 Promotion of a healthy diet is an important factor in the management of obesity, alongside physical activity and, in some cases, medication and bariatric surgery.9 Patients with psoriasis who are overweight have been shown to experience improvement in their psoriasis after weight loss secondary to diet and exercise.8,10 The joint American Academy of Dermatology and National Psoriasis Foundation guidelines recommend that dermatologists advise patients to practice a healthy lifestyle including a healthy diet and communicate with a patient’s primary care provider so they can be appropriately evaluated and treated for comorbidities including metabolic syndrome, diabetes, and hyperlipidemia.11 In the NutriNet-Santé cohort study, investigators found an inverse correlation between psoriasis severity and adherence to a Mediterranean diet, which the authors conclude supports the hypothesis that this may slow the progression of psoriasis.12 In a single meta-analysis, it was reported that patients with psoriasis have a 3-fold increased risk for celiac disease compared to the general population.13 It remains unknown if these data are generalizable to the US population. Dermatologists should consider screening patients with psoriasis for celiac disease based on reported symptoms. When suspected, it is necessary to order appropriate serologies and consider referral to gastroenterology prior to recommending a gluten-free diet, as elimination of gluten prior to testing may lead to false-negative results.
Atopic Dermatitis
Patients and parents/guardians of children with AD often ask about the impact of diet on the condition. A small minority of patients may experience flares of AD due to ongoing, non–IgE-mediated allergen exposure.14 Diet as a trigger for flares should be suspected in children with persistent, moderate to severe AD. In these patients, allergen avoidance may lead to improvement but not resolution of AD. Allergens ordered from most common to least common are the following: eggs, milk, peanuts/tree nuts, shellfish, soy, and wheat.15 Additionally, it is important to note that children with AD are at higher risk for developing life-threatening, IgE-mediated food allergies compared to the general population (37% vs 6.8%).16,17 The LEAP (Learning Early about Peanut Allergy) study led to a paradigm shift in prevention of peanut allergies in high-risk children (ie, those with severe AD and/or egg allergy), providing data to support the idea that early introduction of allergenic foods such as peanuts may prevent severe allergies.18 Further studies are necessary to clarify the population in which allergen testing and recommendations on food avoidance are warranted vs early introduction.19
Conclusion
Early data support the relationship between diet and many common dermatologic conditions, including acne, psoriasis, and AD. Dermatologists should be familiar with the evidence supporting the relationship between diet and various skin conditions to best answer patients’ questions and counsel as appropriate. It is important for dermatologists to continue to stay up-to-date on the literature on this subject as new data emerge. Knowledge about the relationship between diet and skin allows dermatologists to not only support our patients’ skin health but their overall health as well.
Dermatologists frequently learn about skin conditions that are directly linked to diet. For example, we know that nutritional deficiencies can impact the hair, skin, and nails, and that celiac disease manifests with dermatitis herpetiformis of the skin. Patients commonly ask their dermatologists about the impact of diet on their skin. There are many outdated myths, but research on the subject is increasingly demonstrating important associations. Dermatologists must become familiar with the data on this topic so that we can provide informed counseling for our patients. This article reviews the current literature on associations between diet and 3 common cutaneous conditions—acne, psoriasis, and atopic dermatitis [AD]—and provides tips on how to best address our patients’ questions on this topic.
Acne
Studies increasingly support an association between a high glycemic diet (foods that lead to a spike in serum glucose) and acne; Bowe et al1 provided an excellent summary of the topic in 2010. This year, a large prospective cohort study of more than 24,000 participants demonstrated an association between adult acne and a diet high in milk, sugary beverages and foods, and fatty foods.2 In prospective cohort studies of more than 6000 adolescent girls and 4000 adolescent boys, Adebamowo et al3,4 demonstrated a correlation between skim milk consumption and acne. Whey protein supplementation also has been implicated in acne flares.5,6 The biological mechanism of the impact of high glycemic index foods and acne is believed to be mainly via activation of the insulinlike growth factor 1 (IGF-1) pathway, which promotes androgen synthesis and increases androgen bioavailability via decreased synthesis of sex hormone binding globulin.1,2 Insulinlike growth factor 1 also stimulates its downstream target, mammalian target of rapamycin (mTOR), leading to activation of antiapoptotic and proliferation signaling, ultimately resulting in oxidative stress and inflammation causing acne.2 Penso et al2 noted that patients with IGF-1 deficiency (Laron syndrome) never develop acne unless treated with exogenous IGF-1, further supporting its role in acne formation.7 There currently is a paucity of randomized controlled trials assessing the impact of diet on acne.
Psoriasis
The literature consistently shows that obesity is a predisposing factor for psoriasis. Additionally, weight gain may cause flares of existing psoriasis.8 Promotion of a healthy diet is an important factor in the management of obesity, alongside physical activity and, in some cases, medication and bariatric surgery.9 Patients with psoriasis who are overweight have been shown to experience improvement in their psoriasis after weight loss secondary to diet and exercise.8,10 The joint American Academy of Dermatology and National Psoriasis Foundation guidelines recommend that dermatologists advise patients to practice a healthy lifestyle including a healthy diet and communicate with a patient’s primary care provider so they can be appropriately evaluated and treated for comorbidities including metabolic syndrome, diabetes, and hyperlipidemia.11 In the NutriNet-Santé cohort study, investigators found an inverse correlation between psoriasis severity and adherence to a Mediterranean diet, which the authors conclude supports the hypothesis that this may slow the progression of psoriasis.12 In a single meta-analysis, it was reported that patients with psoriasis have a 3-fold increased risk for celiac disease compared to the general population.13 It remains unknown if these data are generalizable to the US population. Dermatologists should consider screening patients with psoriasis for celiac disease based on reported symptoms. When suspected, it is necessary to order appropriate serologies and consider referral to gastroenterology prior to recommending a gluten-free diet, as elimination of gluten prior to testing may lead to false-negative results.
Atopic Dermatitis
Patients and parents/guardians of children with AD often ask about the impact of diet on the condition. A small minority of patients may experience flares of AD due to ongoing, non–IgE-mediated allergen exposure.14 Diet as a trigger for flares should be suspected in children with persistent, moderate to severe AD. In these patients, allergen avoidance may lead to improvement but not resolution of AD. Allergens ordered from most common to least common are the following: eggs, milk, peanuts/tree nuts, shellfish, soy, and wheat.15 Additionally, it is important to note that children with AD are at higher risk for developing life-threatening, IgE-mediated food allergies compared to the general population (37% vs 6.8%).16,17 The LEAP (Learning Early about Peanut Allergy) study led to a paradigm shift in prevention of peanut allergies in high-risk children (ie, those with severe AD and/or egg allergy), providing data to support the idea that early introduction of allergenic foods such as peanuts may prevent severe allergies.18 Further studies are necessary to clarify the population in which allergen testing and recommendations on food avoidance are warranted vs early introduction.19
Conclusion
Early data support the relationship between diet and many common dermatologic conditions, including acne, psoriasis, and AD. Dermatologists should be familiar with the evidence supporting the relationship between diet and various skin conditions to best answer patients’ questions and counsel as appropriate. It is important for dermatologists to continue to stay up-to-date on the literature on this subject as new data emerge. Knowledge about the relationship between diet and skin allows dermatologists to not only support our patients’ skin health but their overall health as well.
- Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63:124-141.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in teenaged boys. J Am Acad Dermatol. 2008;58:787-793.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in adolescent girls. Dermatol Online J. 2006;12:1.
- Silverberg NB. Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes. Cutis. 2012;90:70-72.
- Cengiz FP, Cemil BC, Emiroglu N, et al. Acne located on the trunk, whey protein supplementation: is there any association? Health Promot Perspect. 2017;7:106-108.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Jensen P, Skov L. Psoriasis and obesity [published online February 23, 2017]. Dermatology. 2016;232:633-639.
- Extreme obesity, and what you can do. American Heart Association website. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight/extreme-obesity-and-what-you-can-do. Updated April 18, 2014. Accessed November 30, 2020.
- Naldi L, Conti A, Cazzaniga S, et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol. 2014;170:634-642.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Silverberg NB, Lee-Wong M, Yosipovitch G. Diet and atopic dermatitis. Cutis. 2016;97:227-232.
- Bieber T, Bussmann C. Atopic dermatitis. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:203-218.
- Eigenmann PA, Sicherer SH, Borkowski TA, et al. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998;101:E8.
- Age-adjusted percentages (with standard errors) of hay fever, respiratory allergies, food allergies, and skin allergies in the past 12 months for children under age 18 years, by selected characteristics: United States, 2016. CDC website. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_C-2.pdf. Accessed December 8, 2020.
- Du Toit G, Roberts G, Sayre PH, et al; LEAP study team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Sugita K, Akdis CA. Recent developments and advances in atopic dermatitis and food allergy [published online October 22, 2019]. Allergol Int. 2020;69:204-214.
- Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63:124-141.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in teenaged boys. J Am Acad Dermatol. 2008;58:787-793.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in adolescent girls. Dermatol Online J. 2006;12:1.
- Silverberg NB. Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes. Cutis. 2012;90:70-72.
- Cengiz FP, Cemil BC, Emiroglu N, et al. Acne located on the trunk, whey protein supplementation: is there any association? Health Promot Perspect. 2017;7:106-108.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Jensen P, Skov L. Psoriasis and obesity [published online February 23, 2017]. Dermatology. 2016;232:633-639.
- Extreme obesity, and what you can do. American Heart Association website. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight/extreme-obesity-and-what-you-can-do. Updated April 18, 2014. Accessed November 30, 2020.
- Naldi L, Conti A, Cazzaniga S, et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol. 2014;170:634-642.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Silverberg NB, Lee-Wong M, Yosipovitch G. Diet and atopic dermatitis. Cutis. 2016;97:227-232.
- Bieber T, Bussmann C. Atopic dermatitis. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:203-218.
- Eigenmann PA, Sicherer SH, Borkowski TA, et al. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998;101:E8.
- Age-adjusted percentages (with standard errors) of hay fever, respiratory allergies, food allergies, and skin allergies in the past 12 months for children under age 18 years, by selected characteristics: United States, 2016. CDC website. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_C-2.pdf. Accessed December 8, 2020.
- Du Toit G, Roberts G, Sayre PH, et al; LEAP study team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Sugita K, Akdis CA. Recent developments and advances in atopic dermatitis and food allergy [published online October 22, 2019]. Allergol Int. 2020;69:204-214.
Resident Pearls
- There are strong data on the relationship between dietary patterns and skin conditions.
- High glycemic index foods (eg, skim milk, whey protein, sugary beverages, fatty foods) are associated with acne vulgaris.
- Obesity is a risk factor for psoriasis; weight loss interventions such as improved dietary patterns can improve psoriasis.
- Children with atopic dermatitis (AD) are at higher risk for food allergies (both IgE and non–IgE-mediated allergies). A small subset may experience flares in their AD in relation to non–IgE-mediated food allergies.
Studying in Dermatology Residency
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
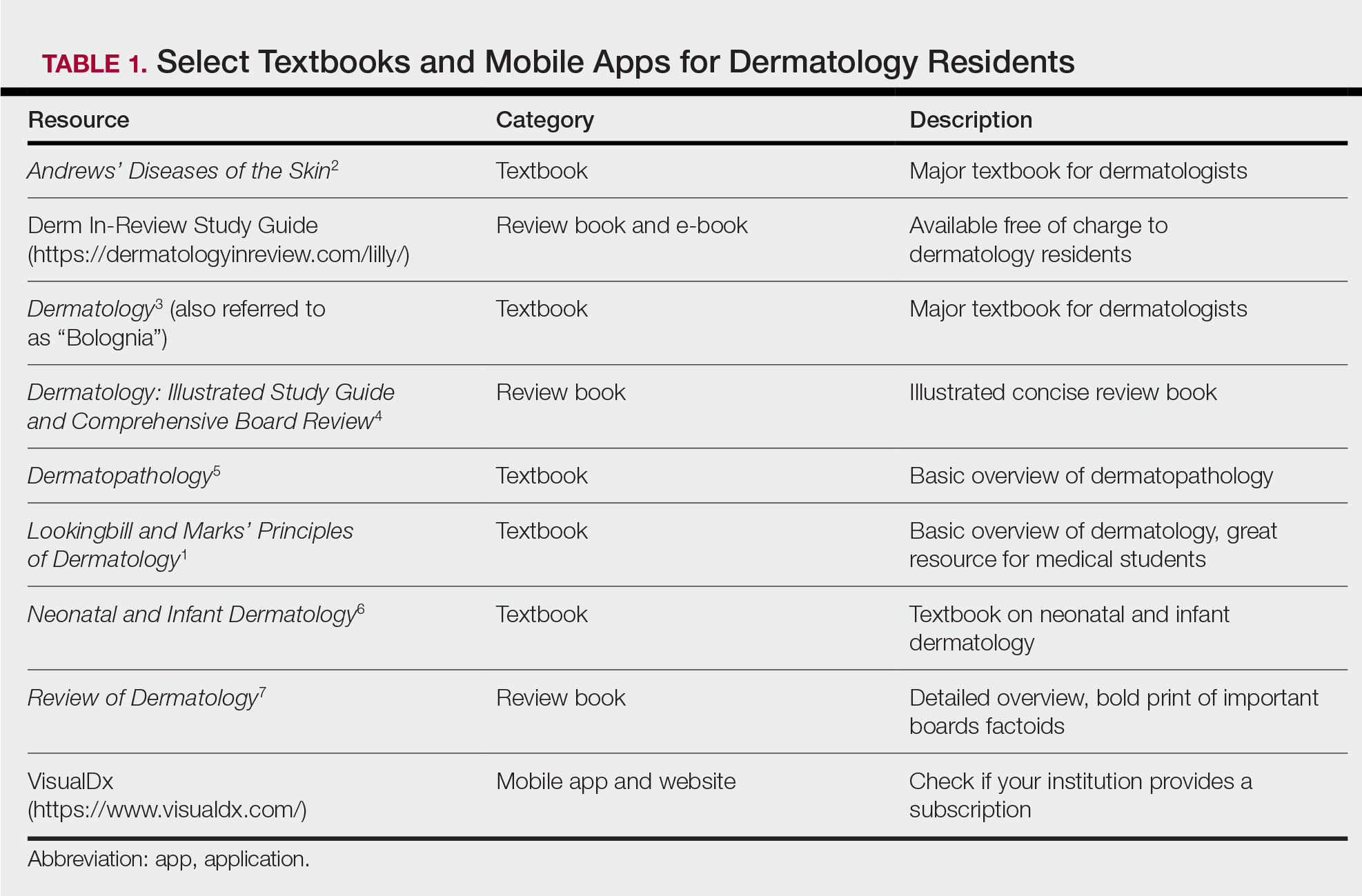
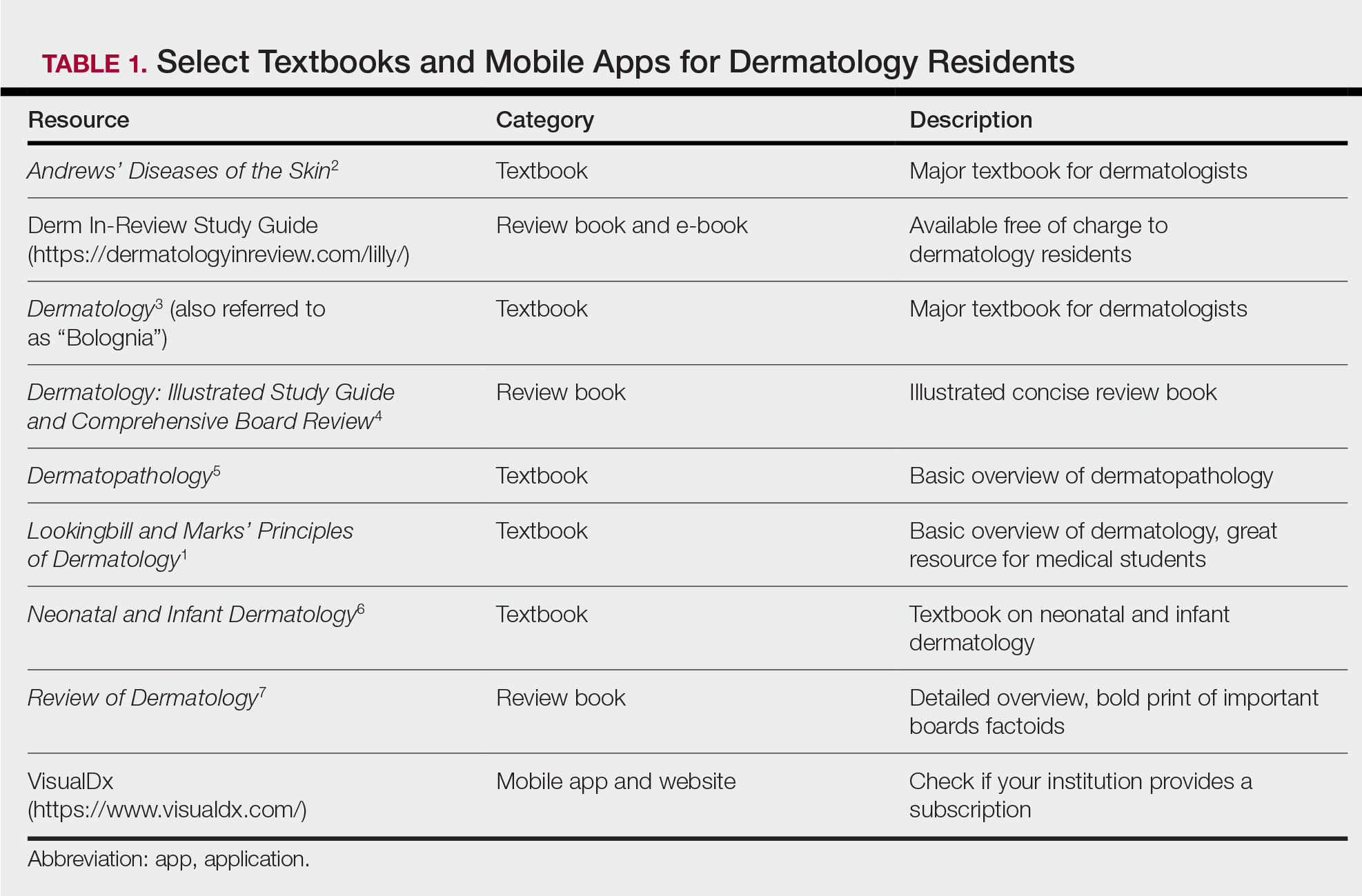
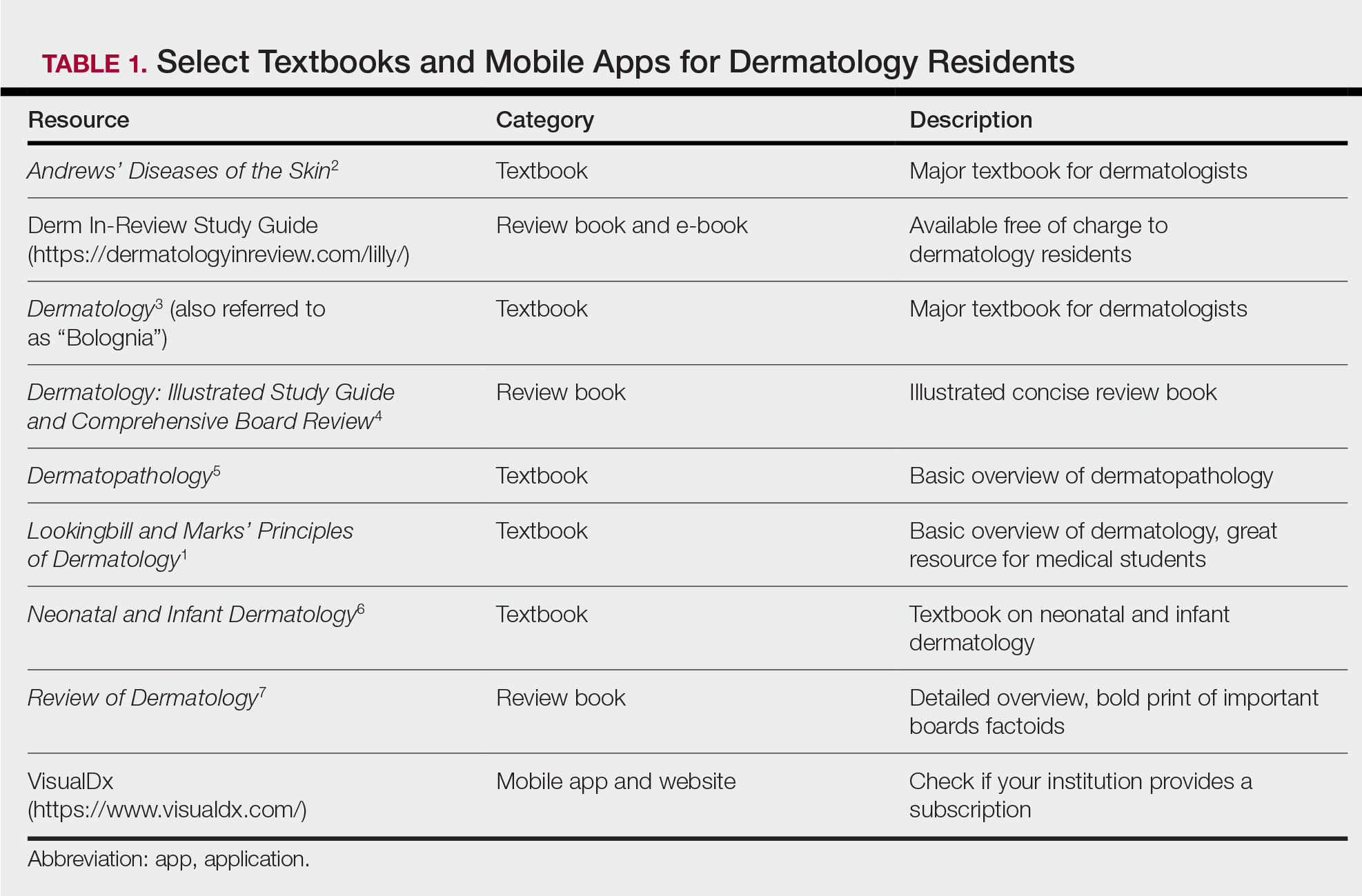
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
Second Year
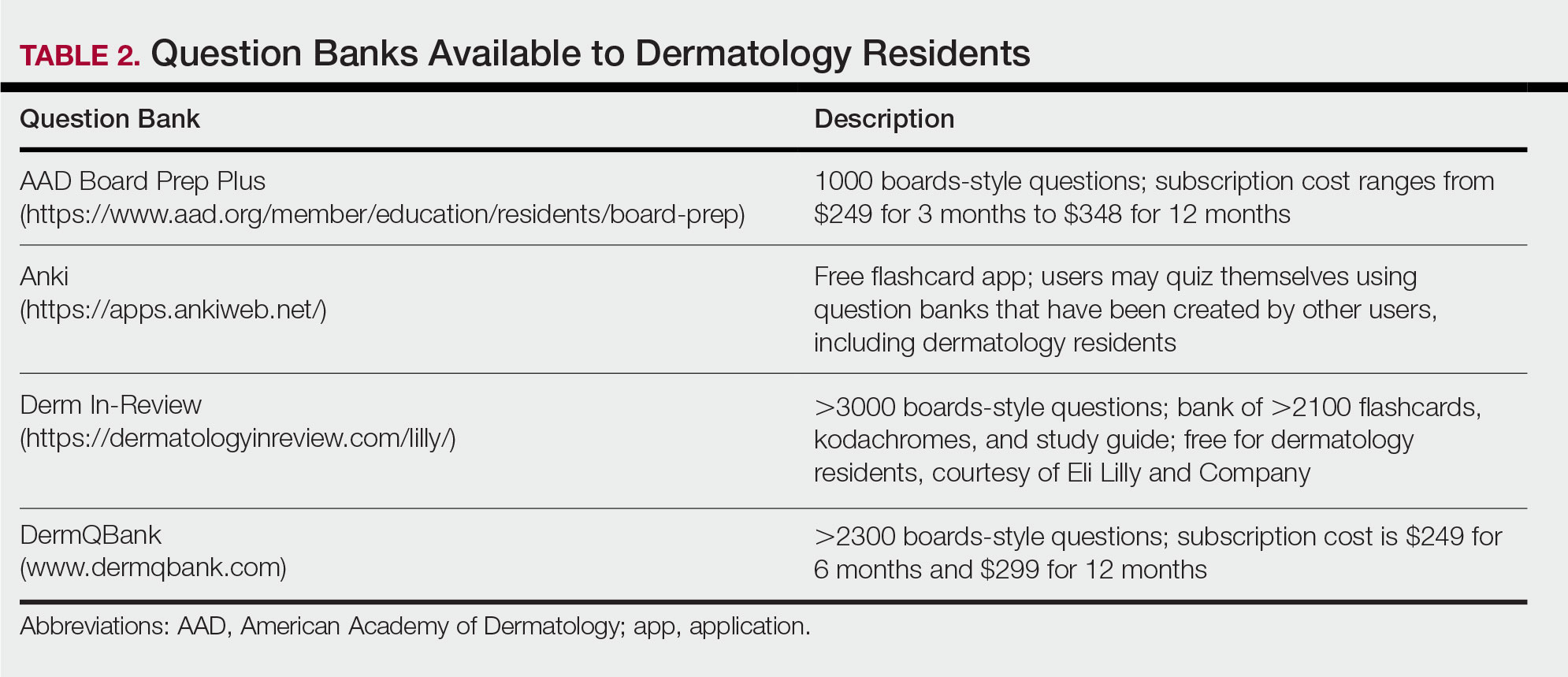
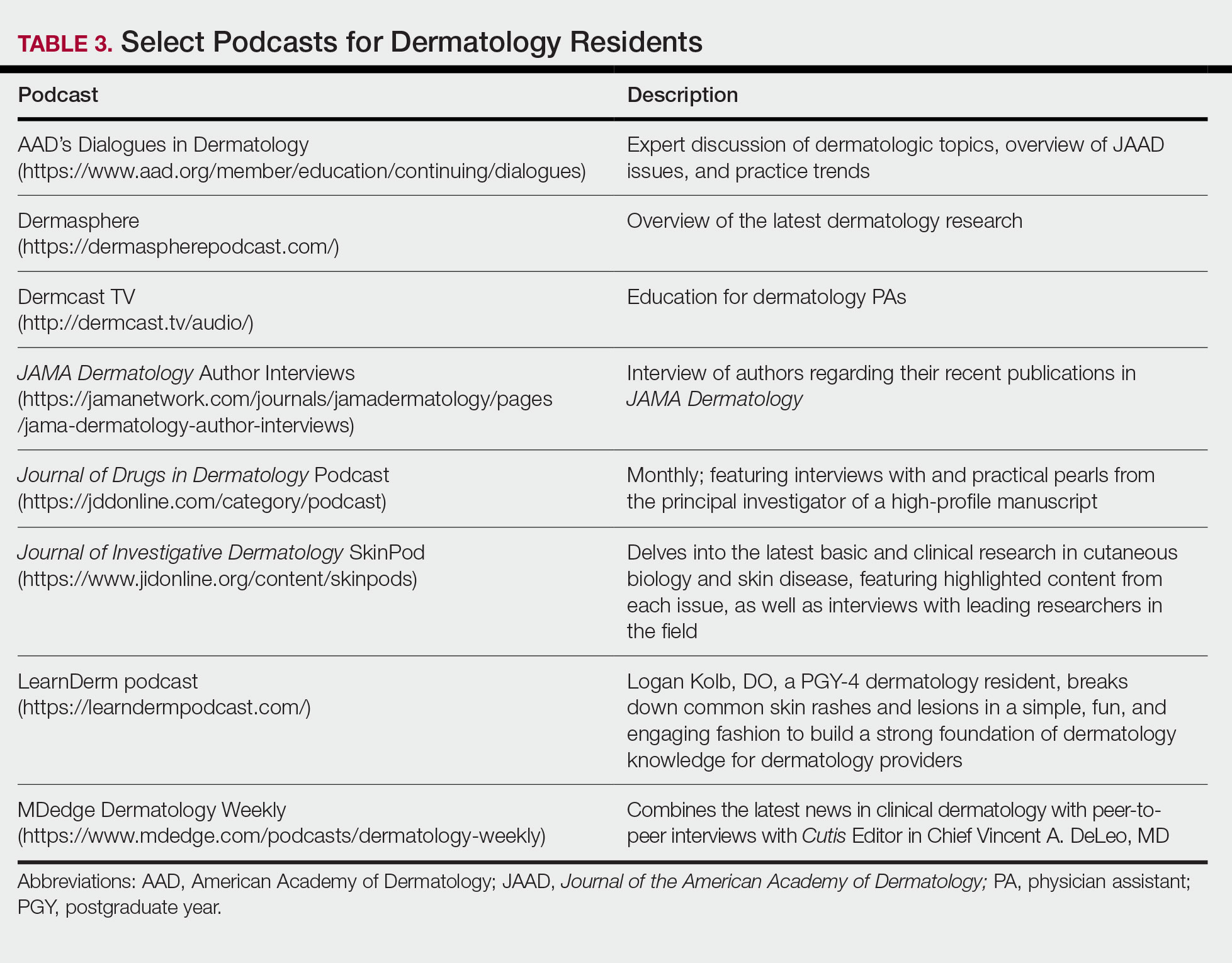
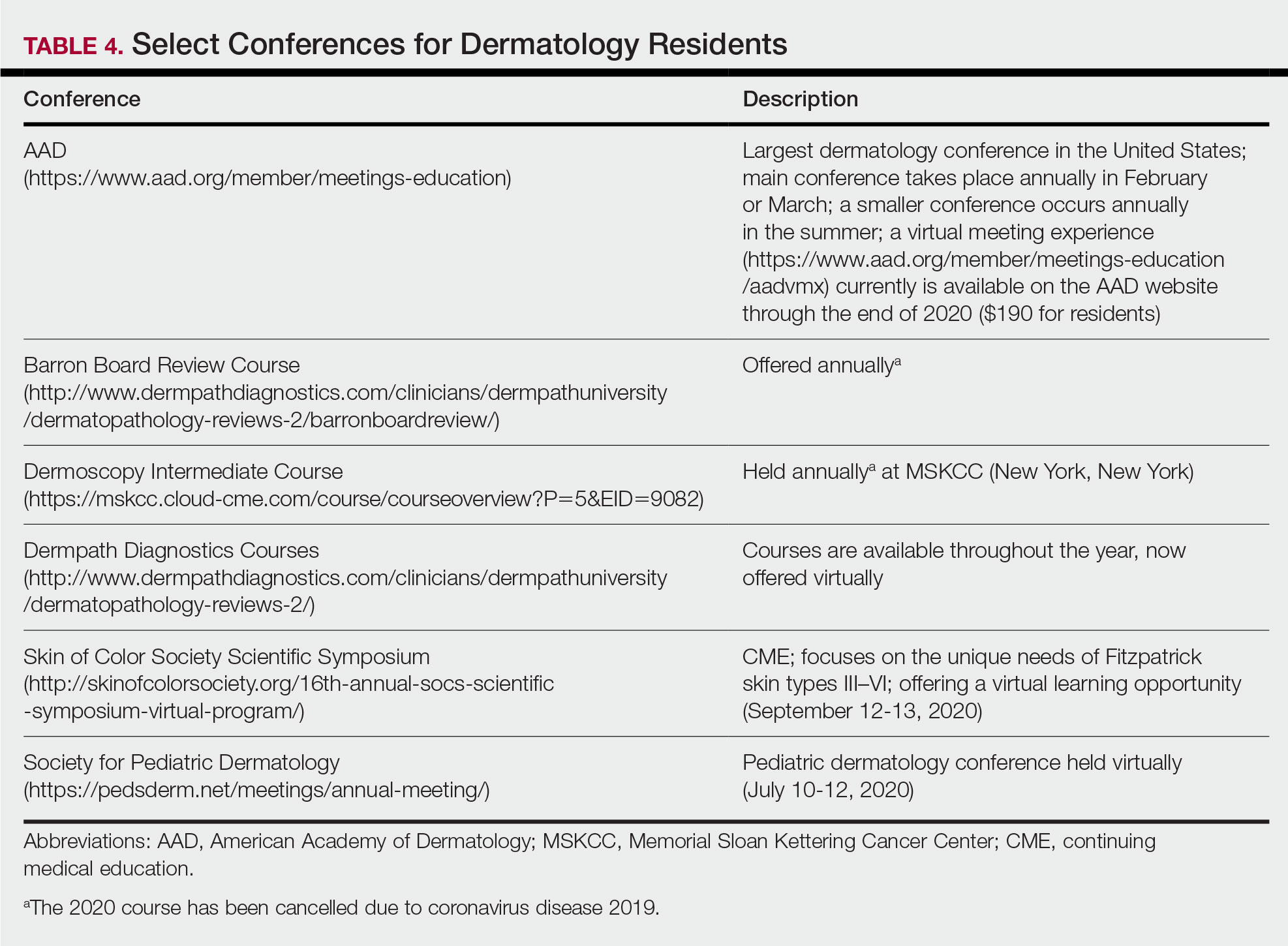
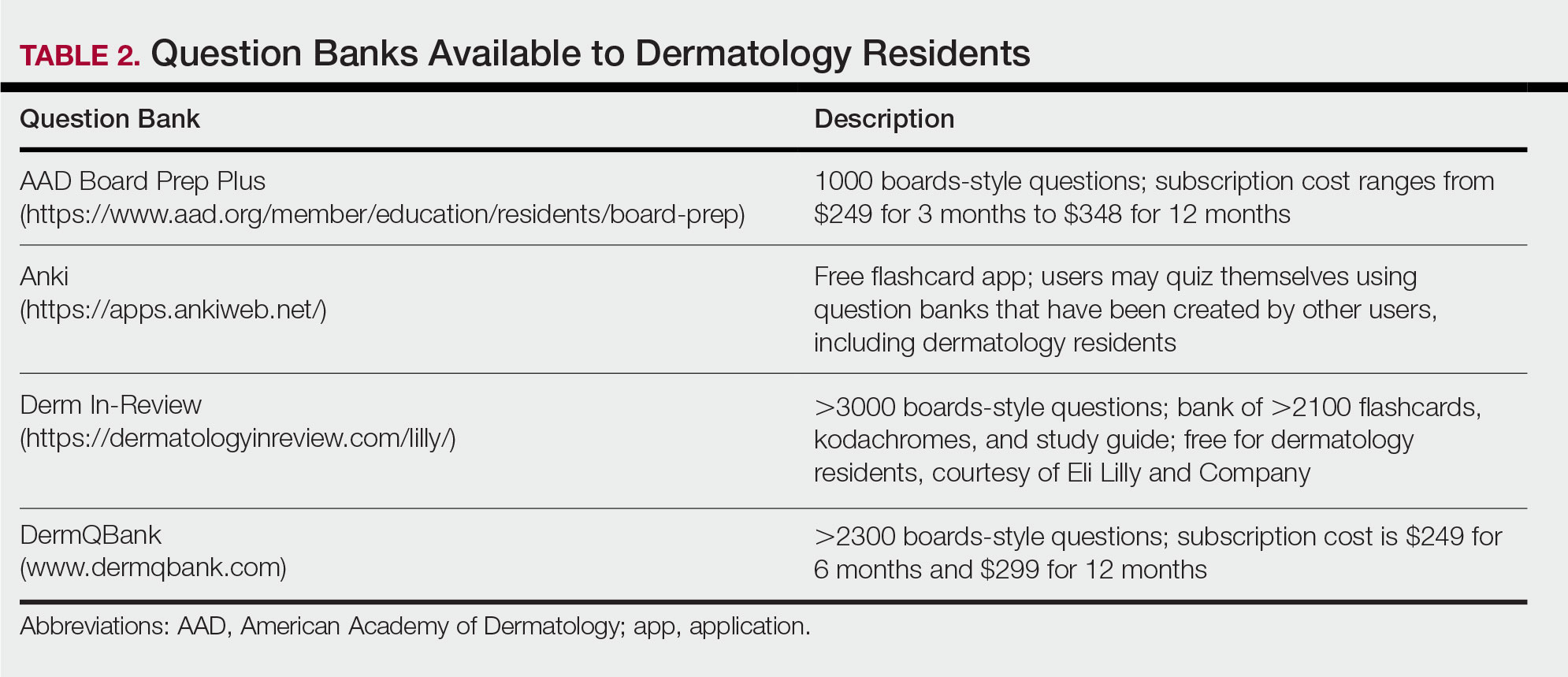
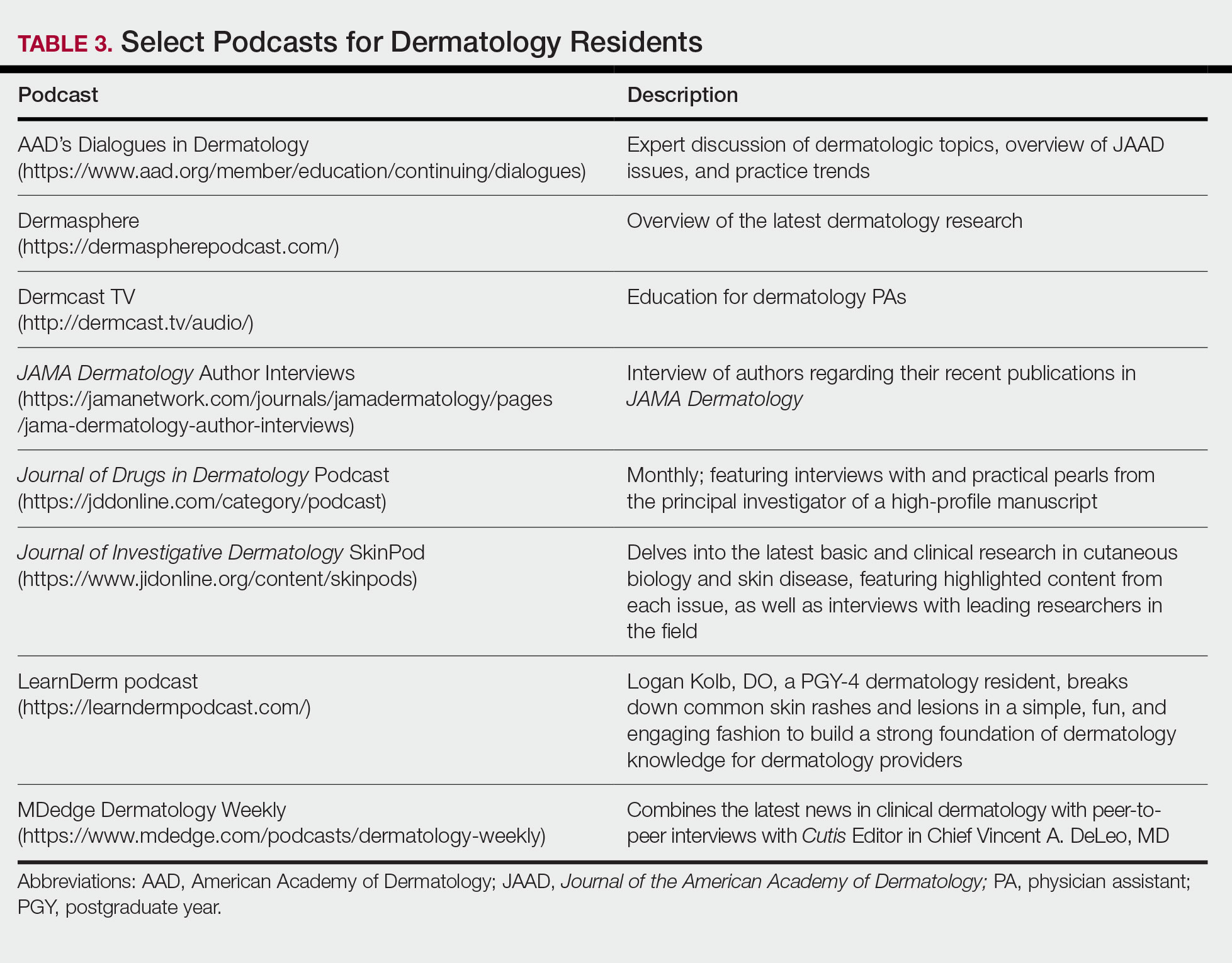
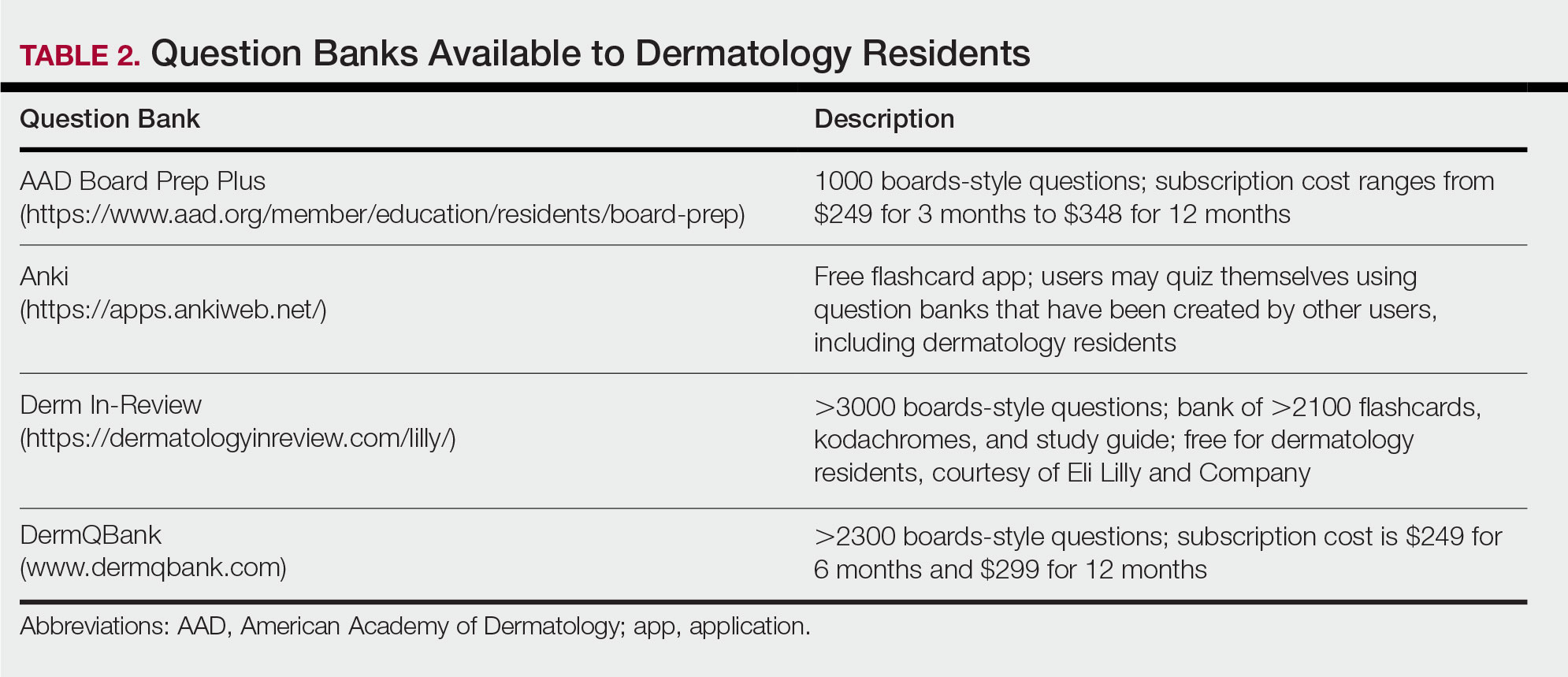
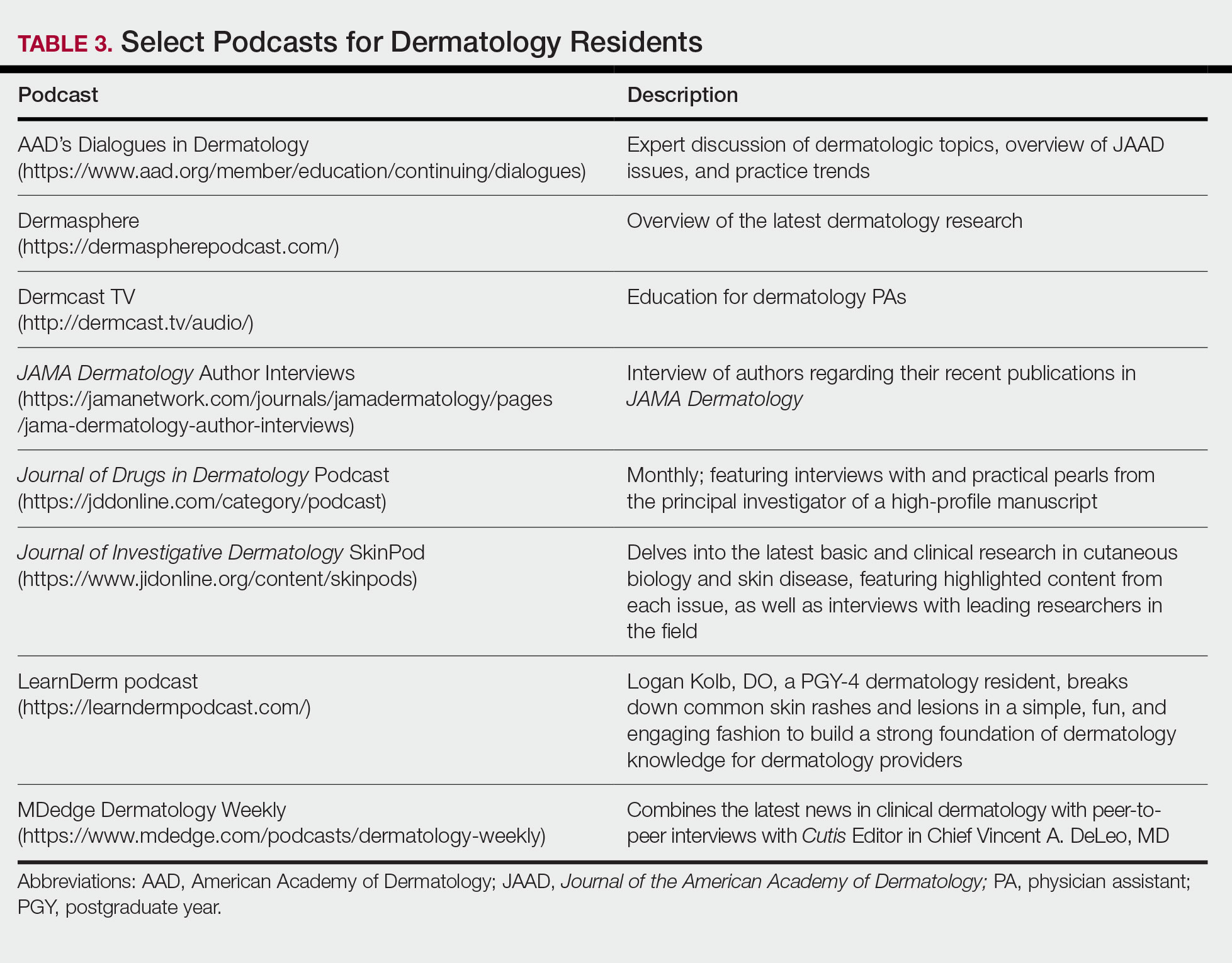
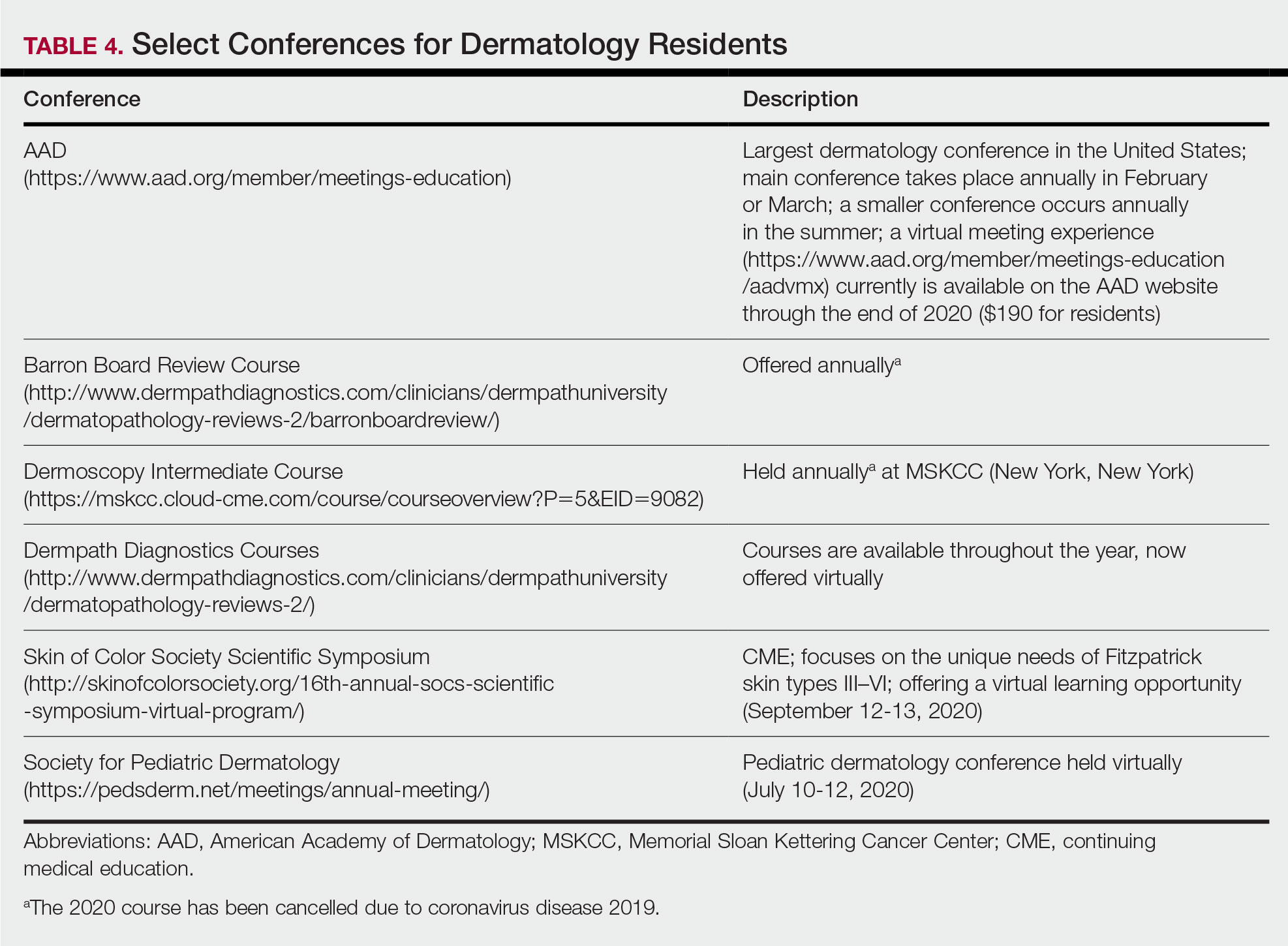
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
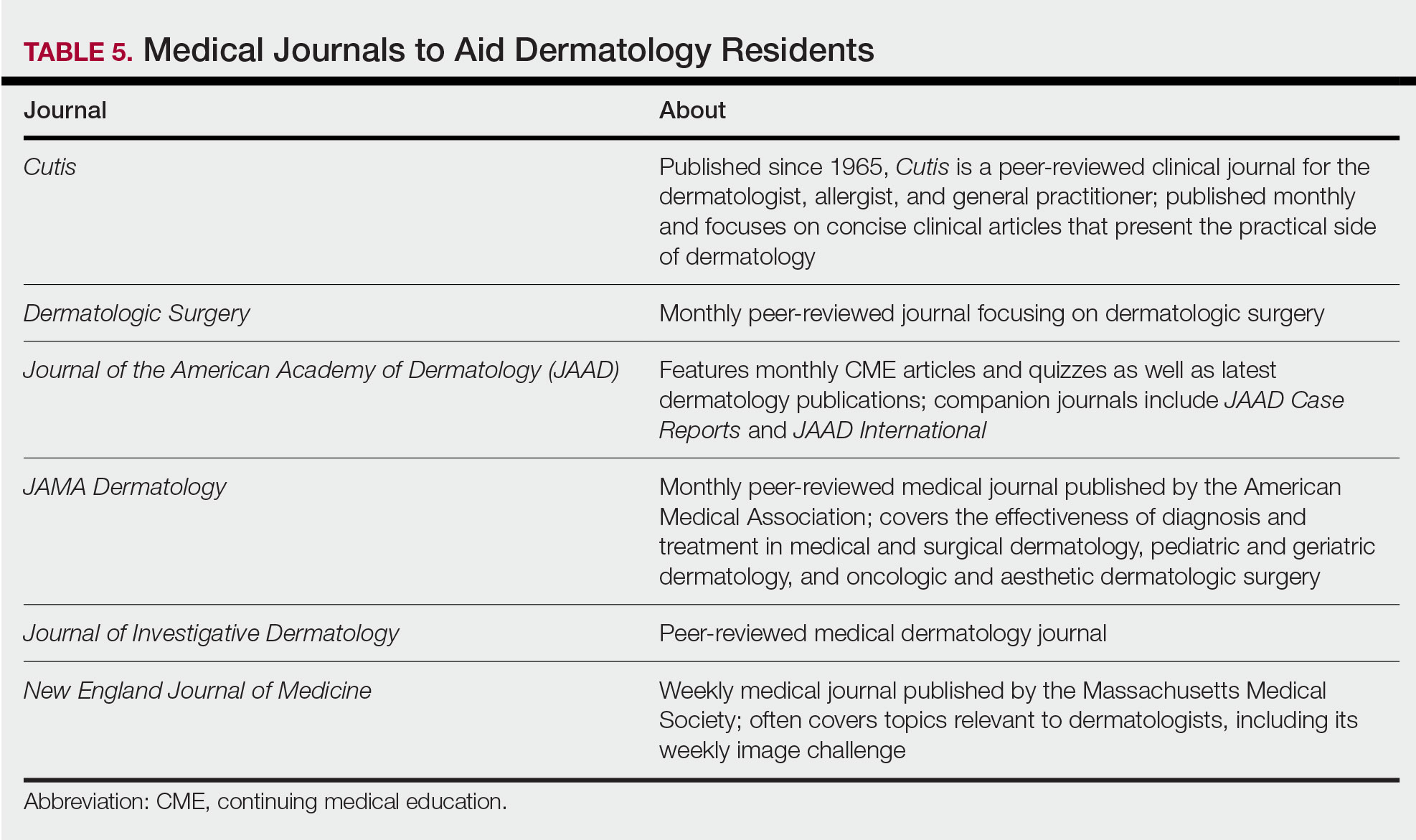
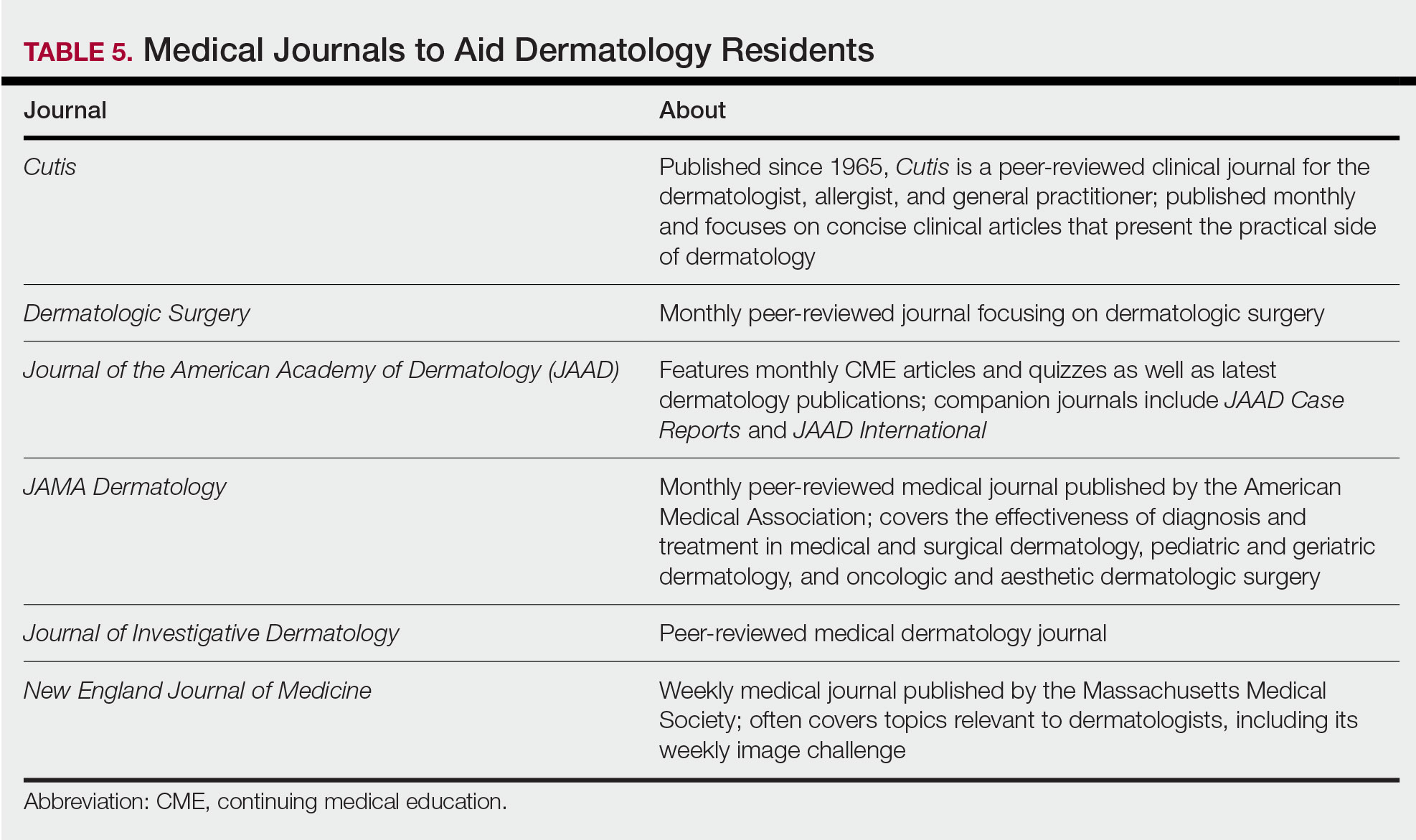
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
Second Year
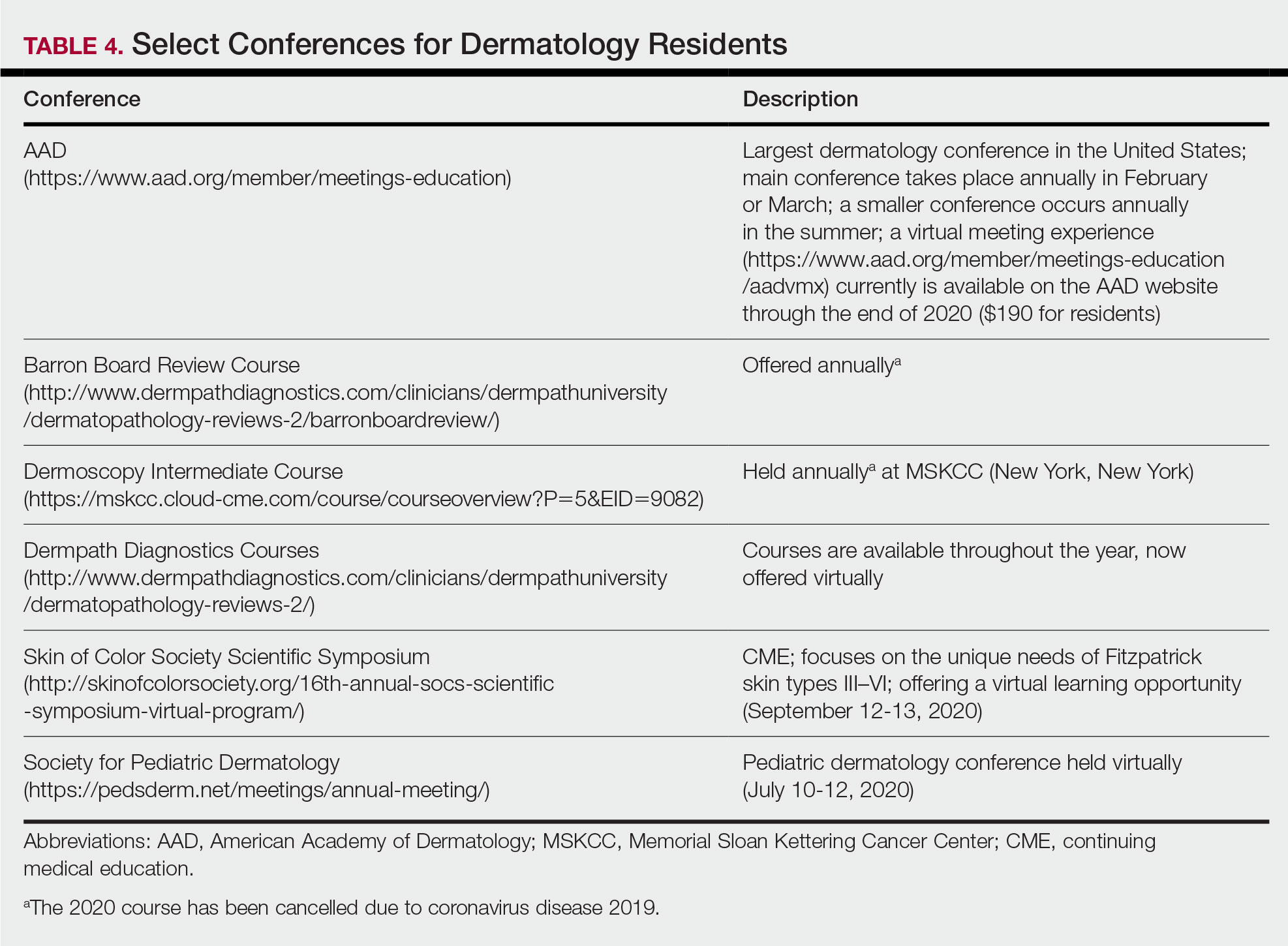
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
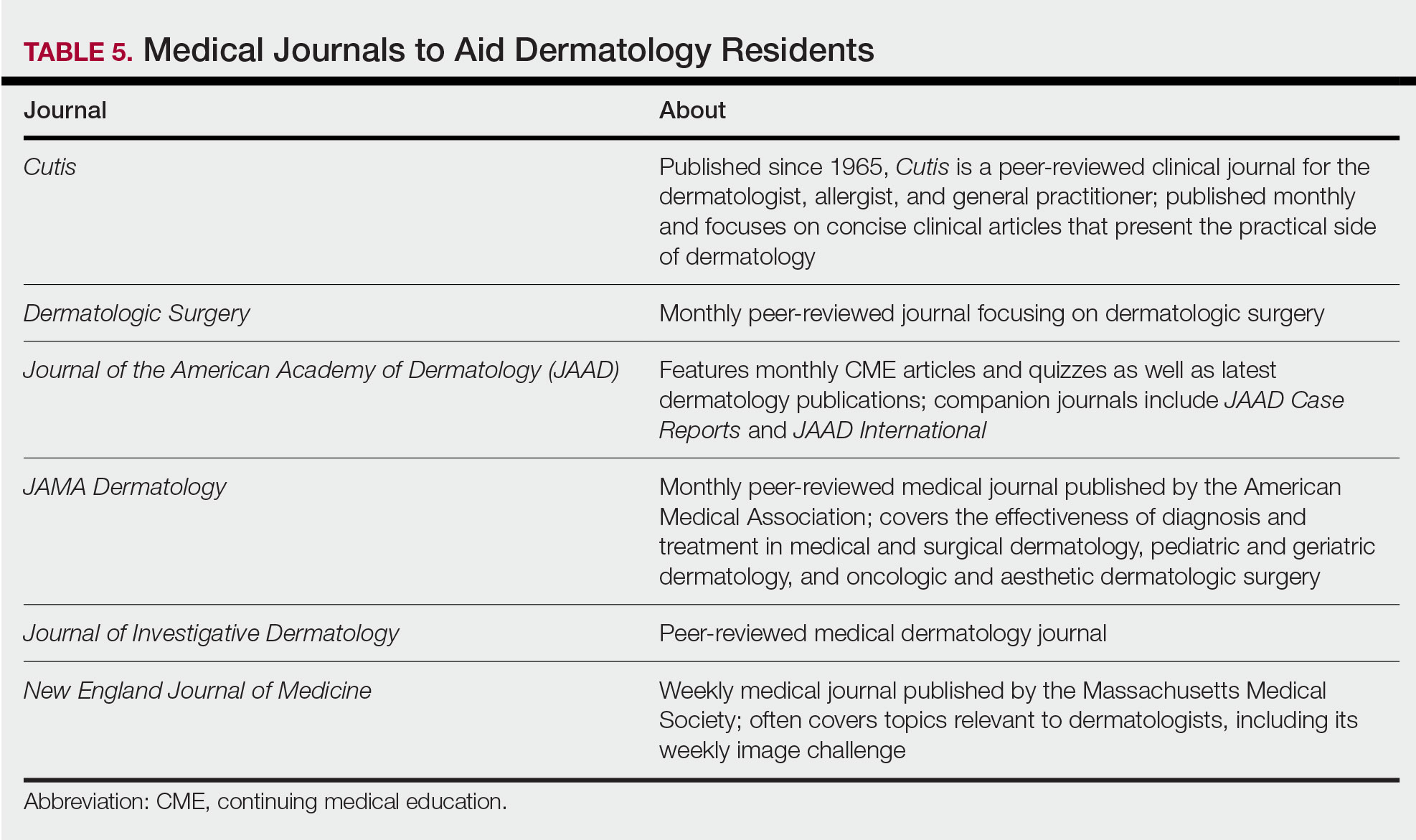
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
Second Year
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
Resident Pearls
- Independent study is a large component of dermatology residency.
- Consistent habits and a tailored approach will support optimal learning for each dermatology resident.
- The beginning of residency is a good time to explore a variety of resources to see what works best. Toward the end of residency, as studying becomes more targeted, residents may benefit from sticking to the resources with which they are most comfortable.
Over-the-counter Topical Products in Dermatology
Over-the-counter (OTC) topical products commonly are discussed during dermatology encounters. Unsurprisingly, dermatologists recommend OTC topical formulations at the highest rate of all medical specialists.1,2 These products may aid in the treatment of skin disease and include shampoo for seborrheic dermatitis, moisturizer for atopic dermatitis, and an armamentarium of products for acne. Conversely, an incorrect selection of OTC topicals can cause or exacerbate skin conditions or result in systemic toxicity. This article addresses how dermatology residents may become familiar with the safety, utility, and tolerability of these products.
Safety and Regulation
Over-the-counter products fall into one or more US Food and Drug Administration (FDA) categories, each of which is subject to a unique set of regulations. The FDA website (www.fda.gov/cosmetics and www.fda.gov/drugs) is an excellent resource for comprehensive and up-to-date information about categorization, safety, and regulation of these products.
Many OTC products are categorized as drugs, including topical steroids, antimicrobials, and sunscreens.3 Most of these products previously were available by prescription and became available OTC after sufficient postmarketing safety information.4 Once a drug becomes available OTC, monitoring relies on reporting from health care professionals.5 Notably, the safety of chemical sunscreens is being re-evaluated in light of recent data demonstrating serum levels in humans above the FDA limit for drugs exempt from further testing for carcinogenicity and reproductive and developmental effects.6-8
The FDA has the authority to regulate imported cosmetic products.
Another category relevant to dermatologists includes dietary supplements. The FDA is responsible for evaluating safety and labeling of products before marketing and taking action against any adulterated or misbranded dietary supplement.14 The FDA does not directly test products, though third-party agencies including NSF International and United States Pharmacopeia impart certification after verification that labeled ingredients are present in the product and test for contaminants.15,16
Utility and Pharmacology
Dermatology residents may have less experience and comfort with the safety profiles and indications of nondrug ingredients in topical products. The textbook Comprehensive Dermatologic Drug Therapy17 is an excellent initial resource for learning about the mechanism of action, efficacy, pharmacology, and side effects of such ingredients, including hydroxy acids, shampoos, cleansers, sunscreens, insect repellents, and topical antioxidants. Dermatology residents also need to be familiar with ingredients causing allergic contact dermatitis, and Fisher’s Contact Dermatitis18 is an excellent resource.
When patients indicate use of a particular product, clinicians may not be certain about specific ingredients. In this case, they may refer to the Walgreens website (www.walgreens.com), which provides an ingredient list for all products that they sell. Additionally, the Environmental Working Group’s Skin Deep program (www.ewg.org/skindeep) maintains a database of more than 85,000 personal care products, which may be accessed online or using their mobile application (Healthy Living), which allows one to scan a product’s barcode.
Trying Them Out
Lastly, it is helpful for dermatologists to be personally familiar with a variety of products to address patients’ concerns regarding tolerability of products (eg, greasiness, inability to “rub in,” sunscreens leaving a white cast, drying effect of cleansers). Samples at conferences including the annual meeting of the American Academy of Dermatology provide a cost-effective way for residents to try out a variety of products. Additionally, residents may purchase different products each time they restock their own supply of personal care products to sample a variety.
Final Thoughts
The FDA website contains up-to-date information on the safety of OTC products, which is constantly in flux. This article provides additional references for dermatology residents to begin to learn about the safety, utility, and pharmacology of topical OTC products. Firsthand experience by sampling products helps dermatologists
- Vogel CA, Balkrishnan R, Fleischer AB, et al. Over-the-counter topical skin products—a common component of skin disease management. Cutis. 2004;74:55-67.
- Nolan BV, Levender MM, Davis SA, et al. Trends in the use of topical over the counter products in the management of dermatologic disease in the United States. Dermatol Online J. 2012;18:1.
- Is it a cosmetic, a drug, or both? (or is it soap?). US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/it-cosmetic-drug-or-both-or-it-soap. Updated August 2, 2018. Accessed April 30, 2020.
- Clarke P. How FDA strives to ensure safety of OTC products. US Food and Drug Administration website. https://www.fda.gov/drugs/special-features/how-fda-strives-ensure-safety-otc-products. Updated March 10, 2016. Accessed April 30, 2020.
- Bond C, Hannaford P. Issues related to monitoring the safety of over-the-counter (OTC) medicines. Drug Saf. 2003;26:1065-1074.
- Matta MK, Zusterzeel R, Pilli NR, et al. Effect of sunscreen application under maximal use conditions on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2019;321:2082-2091.
- Matta MK, Florian J, Zusterzeel R, et al. Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2020;323:256-267.
- FDA advances new proposed regulation to make sure that sunscreens are safe and effective. US Food and Drug Administration website. https://www.fda.gov/news-events/press-announcements/fda-advances-new-proposed-regulation-make-sure-sunscreens-are-safe-and-effective. Published February 21, 2019. Accessed May 1, 2020.
- FDA authority over cosmetics: how cosmetics are not FDA-approved, but are FDA-regulated. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/fda-authority-over-cosmetics-how-cosmetics-are-not-fda-approved-are-fda-regulated. Updated July 24, 2018. Accessed May 1, 2020.
- Inspection of cosmetics. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-compliance-enforcement/inspection-cosmetics. Updated November 3, 2017. Accessed May 1, 2020.
- Cosmetics imports. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-international-activities/cosmetics-importers. Updated September 14, 2018. Accessed May 1, 2020.
- Mercury poisoning linked to use of skin-lightening creams from Mexico. California Department of Health website. https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/CDPH%20Document%20Library/Mercury%20in%20Skin%20Creams_HealthAlert%202019.pdf. Accessed May 1, 2020.
- Otley CC, Sober A. Over-the-counter clobetasol propionate. Arch Dermatol. 1994;130:121.
- Dietary supplements. US Food and Drug Administration website. https://www.fda.gov/food/dietary-supplements. Updated August 16, 2019. Accessed May 1, 2020.
- Supplement and vitamin certification. NSF website. https://www.nsf.org/consumer-resources/health-beauty/supplements-vitamins/supplement-vitamin-certification. Accessed May 1, 2020.
- USP Verified Mark. The United States Pharmacopeial Convention website. https://www.usp.org/verification-services/verified-mark. Accessed May 1, 2020.
- Wolverton SE. Comprehensive Dermatologic Drug Therapy. 3rd ed. New York, NY: Elsevier Saunders; 2013.
- Fowler JF, Zirwas MJ, eds. Fisher’s Contact Dermatitis. 7th ed. Phoenix, AZ: Contact Dermatitis Institute; 2019.
Over-the-counter (OTC) topical products commonly are discussed during dermatology encounters. Unsurprisingly, dermatologists recommend OTC topical formulations at the highest rate of all medical specialists.1,2 These products may aid in the treatment of skin disease and include shampoo for seborrheic dermatitis, moisturizer for atopic dermatitis, and an armamentarium of products for acne. Conversely, an incorrect selection of OTC topicals can cause or exacerbate skin conditions or result in systemic toxicity. This article addresses how dermatology residents may become familiar with the safety, utility, and tolerability of these products.
Safety and Regulation
Over-the-counter products fall into one or more US Food and Drug Administration (FDA) categories, each of which is subject to a unique set of regulations. The FDA website (www.fda.gov/cosmetics and www.fda.gov/drugs) is an excellent resource for comprehensive and up-to-date information about categorization, safety, and regulation of these products.
Many OTC products are categorized as drugs, including topical steroids, antimicrobials, and sunscreens.3 Most of these products previously were available by prescription and became available OTC after sufficient postmarketing safety information.4 Once a drug becomes available OTC, monitoring relies on reporting from health care professionals.5 Notably, the safety of chemical sunscreens is being re-evaluated in light of recent data demonstrating serum levels in humans above the FDA limit for drugs exempt from further testing for carcinogenicity and reproductive and developmental effects.6-8
The FDA has the authority to regulate imported cosmetic products.
Another category relevant to dermatologists includes dietary supplements. The FDA is responsible for evaluating safety and labeling of products before marketing and taking action against any adulterated or misbranded dietary supplement.14 The FDA does not directly test products, though third-party agencies including NSF International and United States Pharmacopeia impart certification after verification that labeled ingredients are present in the product and test for contaminants.15,16
Utility and Pharmacology
Dermatology residents may have less experience and comfort with the safety profiles and indications of nondrug ingredients in topical products. The textbook Comprehensive Dermatologic Drug Therapy17 is an excellent initial resource for learning about the mechanism of action, efficacy, pharmacology, and side effects of such ingredients, including hydroxy acids, shampoos, cleansers, sunscreens, insect repellents, and topical antioxidants. Dermatology residents also need to be familiar with ingredients causing allergic contact dermatitis, and Fisher’s Contact Dermatitis18 is an excellent resource.
When patients indicate use of a particular product, clinicians may not be certain about specific ingredients. In this case, they may refer to the Walgreens website (www.walgreens.com), which provides an ingredient list for all products that they sell. Additionally, the Environmental Working Group’s Skin Deep program (www.ewg.org/skindeep) maintains a database of more than 85,000 personal care products, which may be accessed online or using their mobile application (Healthy Living), which allows one to scan a product’s barcode.
Trying Them Out
Lastly, it is helpful for dermatologists to be personally familiar with a variety of products to address patients’ concerns regarding tolerability of products (eg, greasiness, inability to “rub in,” sunscreens leaving a white cast, drying effect of cleansers). Samples at conferences including the annual meeting of the American Academy of Dermatology provide a cost-effective way for residents to try out a variety of products. Additionally, residents may purchase different products each time they restock their own supply of personal care products to sample a variety.
Final Thoughts
The FDA website contains up-to-date information on the safety of OTC products, which is constantly in flux. This article provides additional references for dermatology residents to begin to learn about the safety, utility, and pharmacology of topical OTC products. Firsthand experience by sampling products helps dermatologists
Over-the-counter (OTC) topical products commonly are discussed during dermatology encounters. Unsurprisingly, dermatologists recommend OTC topical formulations at the highest rate of all medical specialists.1,2 These products may aid in the treatment of skin disease and include shampoo for seborrheic dermatitis, moisturizer for atopic dermatitis, and an armamentarium of products for acne. Conversely, an incorrect selection of OTC topicals can cause or exacerbate skin conditions or result in systemic toxicity. This article addresses how dermatology residents may become familiar with the safety, utility, and tolerability of these products.
Safety and Regulation
Over-the-counter products fall into one or more US Food and Drug Administration (FDA) categories, each of which is subject to a unique set of regulations. The FDA website (www.fda.gov/cosmetics and www.fda.gov/drugs) is an excellent resource for comprehensive and up-to-date information about categorization, safety, and regulation of these products.
Many OTC products are categorized as drugs, including topical steroids, antimicrobials, and sunscreens.3 Most of these products previously were available by prescription and became available OTC after sufficient postmarketing safety information.4 Once a drug becomes available OTC, monitoring relies on reporting from health care professionals.5 Notably, the safety of chemical sunscreens is being re-evaluated in light of recent data demonstrating serum levels in humans above the FDA limit for drugs exempt from further testing for carcinogenicity and reproductive and developmental effects.6-8
The FDA has the authority to regulate imported cosmetic products.
Another category relevant to dermatologists includes dietary supplements. The FDA is responsible for evaluating safety and labeling of products before marketing and taking action against any adulterated or misbranded dietary supplement.14 The FDA does not directly test products, though third-party agencies including NSF International and United States Pharmacopeia impart certification after verification that labeled ingredients are present in the product and test for contaminants.15,16
Utility and Pharmacology
Dermatology residents may have less experience and comfort with the safety profiles and indications of nondrug ingredients in topical products. The textbook Comprehensive Dermatologic Drug Therapy17 is an excellent initial resource for learning about the mechanism of action, efficacy, pharmacology, and side effects of such ingredients, including hydroxy acids, shampoos, cleansers, sunscreens, insect repellents, and topical antioxidants. Dermatology residents also need to be familiar with ingredients causing allergic contact dermatitis, and Fisher’s Contact Dermatitis18 is an excellent resource.
When patients indicate use of a particular product, clinicians may not be certain about specific ingredients. In this case, they may refer to the Walgreens website (www.walgreens.com), which provides an ingredient list for all products that they sell. Additionally, the Environmental Working Group’s Skin Deep program (www.ewg.org/skindeep) maintains a database of more than 85,000 personal care products, which may be accessed online or using their mobile application (Healthy Living), which allows one to scan a product’s barcode.
Trying Them Out
Lastly, it is helpful for dermatologists to be personally familiar with a variety of products to address patients’ concerns regarding tolerability of products (eg, greasiness, inability to “rub in,” sunscreens leaving a white cast, drying effect of cleansers). Samples at conferences including the annual meeting of the American Academy of Dermatology provide a cost-effective way for residents to try out a variety of products. Additionally, residents may purchase different products each time they restock their own supply of personal care products to sample a variety.
Final Thoughts
The FDA website contains up-to-date information on the safety of OTC products, which is constantly in flux. This article provides additional references for dermatology residents to begin to learn about the safety, utility, and pharmacology of topical OTC products. Firsthand experience by sampling products helps dermatologists
- Vogel CA, Balkrishnan R, Fleischer AB, et al. Over-the-counter topical skin products—a common component of skin disease management. Cutis. 2004;74:55-67.
- Nolan BV, Levender MM, Davis SA, et al. Trends in the use of topical over the counter products in the management of dermatologic disease in the United States. Dermatol Online J. 2012;18:1.
- Is it a cosmetic, a drug, or both? (or is it soap?). US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/it-cosmetic-drug-or-both-or-it-soap. Updated August 2, 2018. Accessed April 30, 2020.
- Clarke P. How FDA strives to ensure safety of OTC products. US Food and Drug Administration website. https://www.fda.gov/drugs/special-features/how-fda-strives-ensure-safety-otc-products. Updated March 10, 2016. Accessed April 30, 2020.
- Bond C, Hannaford P. Issues related to monitoring the safety of over-the-counter (OTC) medicines. Drug Saf. 2003;26:1065-1074.
- Matta MK, Zusterzeel R, Pilli NR, et al. Effect of sunscreen application under maximal use conditions on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2019;321:2082-2091.
- Matta MK, Florian J, Zusterzeel R, et al. Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2020;323:256-267.
- FDA advances new proposed regulation to make sure that sunscreens are safe and effective. US Food and Drug Administration website. https://www.fda.gov/news-events/press-announcements/fda-advances-new-proposed-regulation-make-sure-sunscreens-are-safe-and-effective. Published February 21, 2019. Accessed May 1, 2020.
- FDA authority over cosmetics: how cosmetics are not FDA-approved, but are FDA-regulated. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/fda-authority-over-cosmetics-how-cosmetics-are-not-fda-approved-are-fda-regulated. Updated July 24, 2018. Accessed May 1, 2020.
- Inspection of cosmetics. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-compliance-enforcement/inspection-cosmetics. Updated November 3, 2017. Accessed May 1, 2020.
- Cosmetics imports. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-international-activities/cosmetics-importers. Updated September 14, 2018. Accessed May 1, 2020.
- Mercury poisoning linked to use of skin-lightening creams from Mexico. California Department of Health website. https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/CDPH%20Document%20Library/Mercury%20in%20Skin%20Creams_HealthAlert%202019.pdf. Accessed May 1, 2020.
- Otley CC, Sober A. Over-the-counter clobetasol propionate. Arch Dermatol. 1994;130:121.
- Dietary supplements. US Food and Drug Administration website. https://www.fda.gov/food/dietary-supplements. Updated August 16, 2019. Accessed May 1, 2020.
- Supplement and vitamin certification. NSF website. https://www.nsf.org/consumer-resources/health-beauty/supplements-vitamins/supplement-vitamin-certification. Accessed May 1, 2020.
- USP Verified Mark. The United States Pharmacopeial Convention website. https://www.usp.org/verification-services/verified-mark. Accessed May 1, 2020.
- Wolverton SE. Comprehensive Dermatologic Drug Therapy. 3rd ed. New York, NY: Elsevier Saunders; 2013.
- Fowler JF, Zirwas MJ, eds. Fisher’s Contact Dermatitis. 7th ed. Phoenix, AZ: Contact Dermatitis Institute; 2019.
- Vogel CA, Balkrishnan R, Fleischer AB, et al. Over-the-counter topical skin products—a common component of skin disease management. Cutis. 2004;74:55-67.
- Nolan BV, Levender MM, Davis SA, et al. Trends in the use of topical over the counter products in the management of dermatologic disease in the United States. Dermatol Online J. 2012;18:1.
- Is it a cosmetic, a drug, or both? (or is it soap?). US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/it-cosmetic-drug-or-both-or-it-soap. Updated August 2, 2018. Accessed April 30, 2020.
- Clarke P. How FDA strives to ensure safety of OTC products. US Food and Drug Administration website. https://www.fda.gov/drugs/special-features/how-fda-strives-ensure-safety-otc-products. Updated March 10, 2016. Accessed April 30, 2020.
- Bond C, Hannaford P. Issues related to monitoring the safety of over-the-counter (OTC) medicines. Drug Saf. 2003;26:1065-1074.
- Matta MK, Zusterzeel R, Pilli NR, et al. Effect of sunscreen application under maximal use conditions on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2019;321:2082-2091.
- Matta MK, Florian J, Zusterzeel R, et al. Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA. 2020;323:256-267.
- FDA advances new proposed regulation to make sure that sunscreens are safe and effective. US Food and Drug Administration website. https://www.fda.gov/news-events/press-announcements/fda-advances-new-proposed-regulation-make-sure-sunscreens-are-safe-and-effective. Published February 21, 2019. Accessed May 1, 2020.
- FDA authority over cosmetics: how cosmetics are not FDA-approved, but are FDA-regulated. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-laws-regulations/fda-authority-over-cosmetics-how-cosmetics-are-not-fda-approved-are-fda-regulated. Updated July 24, 2018. Accessed May 1, 2020.
- Inspection of cosmetics. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-compliance-enforcement/inspection-cosmetics. Updated November 3, 2017. Accessed May 1, 2020.
- Cosmetics imports. US Food and Drug Administration website. https://www.fda.gov/cosmetics/cosmetics-international-activities/cosmetics-importers. Updated September 14, 2018. Accessed May 1, 2020.
- Mercury poisoning linked to use of skin-lightening creams from Mexico. California Department of Health website. https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/CDPH%20Document%20Library/Mercury%20in%20Skin%20Creams_HealthAlert%202019.pdf. Accessed May 1, 2020.
- Otley CC, Sober A. Over-the-counter clobetasol propionate. Arch Dermatol. 1994;130:121.
- Dietary supplements. US Food and Drug Administration website. https://www.fda.gov/food/dietary-supplements. Updated August 16, 2019. Accessed May 1, 2020.
- Supplement and vitamin certification. NSF website. https://www.nsf.org/consumer-resources/health-beauty/supplements-vitamins/supplement-vitamin-certification. Accessed May 1, 2020.
- USP Verified Mark. The United States Pharmacopeial Convention website. https://www.usp.org/verification-services/verified-mark. Accessed May 1, 2020.
- Wolverton SE. Comprehensive Dermatologic Drug Therapy. 3rd ed. New York, NY: Elsevier Saunders; 2013.
- Fowler JF, Zirwas MJ, eds. Fisher’s Contact Dermatitis. 7th ed. Phoenix, AZ: Contact Dermatitis Institute; 2019.
Resident Pearls
- Several branches of the US Food and Drug Administration are responsible for regulation of overthe-counter (OTC) topical products with both direct and indirect oversight.
- There are several excellent resources available to dermatologists in training who are interested in learning about pharmacology and tolerability of OTC products.
- Firsthand experience in personally sampling a variety of products also helps clinicians provide practical recommendations to patients.
Coronavirus and Dermatology: A Resident’s Perspective
On January 30, 2020, the World Health Organization declared the outbreak of coronavirus disease 2019 (COVID-19) a public health emergency of international concern.1 Severe acute respiratory syndrome–associated coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, is an enveloped, single-stranded RNA virus. It is the seventh known coronavirus to infect humans and third zoonotic Coronaviridae to cause fatal respiratory illness, along with SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV).2 There has been a rapid shift in the geographic center of the outbreak as well as the numbers of confirmed cases and deaths. Although the first cases in late 2019 and early 2020 were in China, by mid-March Italy became the center of the pandemic, with a steep increase in the number of cases in other European countries and the United States.3 Although COVID-19 does not have known dermatologic manifestations, it has the potential for wide-reaching impact on our field.
Strained Resources
In the United States, COVID-19 initially was associated with international travel but is now rapidly spreading throughout the community. I am currently a dermatology resident at New York-Presbyterian, Columbia campus, in New York, New York, a city that unfortunately finds itself underprepared to handle this unprecedented crisis. As of Monday, March 16, 2020, New York-Presbyterian made the decision to postpone all elective procedures, including Mohs micrographic surgery, to preserve hospital resources, including trained personnel, personal protective equipment, ventilators, and hospital beds. There have not been clear-cut guidelines regarding how to approach other dermatologic care for our patients, including routine clinic visits and inpatient dermatology consultations, leaving decisions up to individual departments and providers.
It would be prudent to learn from our colleagues in China who report steps that have been successful in preventing nosocomial spread of COVID-19 in the dermatologic setting. Tao et al4 described their protocols in both the outpatient and inpatient dermatologic setting, beginning with strict triage before patients can even enter a clinic building for their outpatient appointment. Those who screen positive are sent to a fever clinic for further evaluation, which may include a rapid computed tomography scan (using a machine that may perform 200 chest computed tomography scans per day) and SARS-CoV-2 polymerase chain reaction.5 For inpatient dermatologic consultation of patients with known COVID-19, telehealth and multidisciplinary meetings are first and second line, respectively, with bedside dermatologic consultation as a last resort.4 Chen et al6 described similarly strict triage protocols as well as physician use of full-body personal protective equipment during all patient encounters. These measures are taken in light of the well-documented phenomenon of asymptomatic carriage and transmission, as all patients entering their dermatologic clinics have screened negative for symptomatic SARS-CoV-2 infection.6
Conferences and Education
Coronavirus is impacting the education of millions of individuals worldwide, including that of dermatology residents. The Annual Meeting of the American Academy of Dermatology, which was scheduled to take place in March 2020, was canceled due to COVID-19.7 The American Board of Dermatology has released a statement indicating that for all dermatology residents, time spent in COVID-19–mandated quarantine will count as clinical education if residents are able to work with their program to complete independent structured academic activity during that time.8 We also must consider the possibility that dermatology residents are reassigned to work outside of our specialty, resulting in less time and experience caring for patients with dermatologic conditions. Dermatologists in other countries have been called upon to care for COVID-19 patients, even reported to be working in intensive care units in Italy.9 Virtual technologies may be used in novel ways to support dermatology resident education throughout this process.
Final Thoughts
As physicians, dermatologists are in the position to educate their patients regarding prevention strategies, especially given that the lay press disseminates confusing and inaccurate information. The World Health Organization provides specific guidance, focusing on handwashing, respiratory hygiene, social distancing, and encouraging symptomatic patients to seek remote care whenever possible.10 Many of our patients are at high risk of complications due to COVID-19, whether due to their age or because they are immunocompromised. As the situation unfolds, the impact on and role of dermatology in this crisis will continue to evolve.
- Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)[news release]. Geneva, Switzerland: World Health Organization; January 30, 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-%282005%29-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-%282019-ncov%29. Accessed March 16, 2020.
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273.
- World Health Organization. Coronavirus disease 2019: Situation Report—58. March 18, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200318-sitrep-58-covid-19.pdf?sfvrsn=20876712_2. Accessed March 19, 2020.
- Tao J, Song Z, Yang L, et al. Emergency management for preventing and controlling nosocomial infection of 2019 novel coronavirus: implications for the dermatology department [published online March 5, 2020]. Br J Dermatol. doi:10.1111/bjd.19011.
- McNeil DG. Jr. Inside China’s all out war on the coronavirus. The New York Times. March 4, 2020. https://www.nytimes.com/2020/03/04/health/coronavirus-china-aylward.html?smid=tw-nytimes&smtyp=cur. Accessed March 19, 2020.
- Chen Y, Pradhan S, Xue S. What are we doing in the dermatology outpatient department amidst the raging of the 2019 novel coronavirus? J Am Acad Dermatol. 2020;82:1034.
- Hruza GJ. 2020 annual AAD meeting is canceled due to COVID-19 outbreak. American Academy of Dermatology website. https://www.aad.org/member/meetings/am2020/faqs/coronavirus. Accessed March 16, 2020.
- American Board of Dermatology. Impact of COVID-19 on dermatology resident education. March 6, 2020. https://www.abderm.org/2978.aspx. Accessed March 16, 2020.
- “It’s Like a War” [podcast]. The Daily. March 17, 2020. https://www.nytimes.com/2020/03/17/podcasts/the-daily/italy-coronavirus.html?action=click&module=audio-series-bar®ion=header&pgtype=Article. Accessed March 20, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for public. March 18, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed March 19, 2020.
On January 30, 2020, the World Health Organization declared the outbreak of coronavirus disease 2019 (COVID-19) a public health emergency of international concern.1 Severe acute respiratory syndrome–associated coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, is an enveloped, single-stranded RNA virus. It is the seventh known coronavirus to infect humans and third zoonotic Coronaviridae to cause fatal respiratory illness, along with SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV).2 There has been a rapid shift in the geographic center of the outbreak as well as the numbers of confirmed cases and deaths. Although the first cases in late 2019 and early 2020 were in China, by mid-March Italy became the center of the pandemic, with a steep increase in the number of cases in other European countries and the United States.3 Although COVID-19 does not have known dermatologic manifestations, it has the potential for wide-reaching impact on our field.
Strained Resources
In the United States, COVID-19 initially was associated with international travel but is now rapidly spreading throughout the community. I am currently a dermatology resident at New York-Presbyterian, Columbia campus, in New York, New York, a city that unfortunately finds itself underprepared to handle this unprecedented crisis. As of Monday, March 16, 2020, New York-Presbyterian made the decision to postpone all elective procedures, including Mohs micrographic surgery, to preserve hospital resources, including trained personnel, personal protective equipment, ventilators, and hospital beds. There have not been clear-cut guidelines regarding how to approach other dermatologic care for our patients, including routine clinic visits and inpatient dermatology consultations, leaving decisions up to individual departments and providers.
It would be prudent to learn from our colleagues in China who report steps that have been successful in preventing nosocomial spread of COVID-19 in the dermatologic setting. Tao et al4 described their protocols in both the outpatient and inpatient dermatologic setting, beginning with strict triage before patients can even enter a clinic building for their outpatient appointment. Those who screen positive are sent to a fever clinic for further evaluation, which may include a rapid computed tomography scan (using a machine that may perform 200 chest computed tomography scans per day) and SARS-CoV-2 polymerase chain reaction.5 For inpatient dermatologic consultation of patients with known COVID-19, telehealth and multidisciplinary meetings are first and second line, respectively, with bedside dermatologic consultation as a last resort.4 Chen et al6 described similarly strict triage protocols as well as physician use of full-body personal protective equipment during all patient encounters. These measures are taken in light of the well-documented phenomenon of asymptomatic carriage and transmission, as all patients entering their dermatologic clinics have screened negative for symptomatic SARS-CoV-2 infection.6
Conferences and Education
Coronavirus is impacting the education of millions of individuals worldwide, including that of dermatology residents. The Annual Meeting of the American Academy of Dermatology, which was scheduled to take place in March 2020, was canceled due to COVID-19.7 The American Board of Dermatology has released a statement indicating that for all dermatology residents, time spent in COVID-19–mandated quarantine will count as clinical education if residents are able to work with their program to complete independent structured academic activity during that time.8 We also must consider the possibility that dermatology residents are reassigned to work outside of our specialty, resulting in less time and experience caring for patients with dermatologic conditions. Dermatologists in other countries have been called upon to care for COVID-19 patients, even reported to be working in intensive care units in Italy.9 Virtual technologies may be used in novel ways to support dermatology resident education throughout this process.
Final Thoughts
As physicians, dermatologists are in the position to educate their patients regarding prevention strategies, especially given that the lay press disseminates confusing and inaccurate information. The World Health Organization provides specific guidance, focusing on handwashing, respiratory hygiene, social distancing, and encouraging symptomatic patients to seek remote care whenever possible.10 Many of our patients are at high risk of complications due to COVID-19, whether due to their age or because they are immunocompromised. As the situation unfolds, the impact on and role of dermatology in this crisis will continue to evolve.
On January 30, 2020, the World Health Organization declared the outbreak of coronavirus disease 2019 (COVID-19) a public health emergency of international concern.1 Severe acute respiratory syndrome–associated coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, is an enveloped, single-stranded RNA virus. It is the seventh known coronavirus to infect humans and third zoonotic Coronaviridae to cause fatal respiratory illness, along with SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV).2 There has been a rapid shift in the geographic center of the outbreak as well as the numbers of confirmed cases and deaths. Although the first cases in late 2019 and early 2020 were in China, by mid-March Italy became the center of the pandemic, with a steep increase in the number of cases in other European countries and the United States.3 Although COVID-19 does not have known dermatologic manifestations, it has the potential for wide-reaching impact on our field.
Strained Resources
In the United States, COVID-19 initially was associated with international travel but is now rapidly spreading throughout the community. I am currently a dermatology resident at New York-Presbyterian, Columbia campus, in New York, New York, a city that unfortunately finds itself underprepared to handle this unprecedented crisis. As of Monday, March 16, 2020, New York-Presbyterian made the decision to postpone all elective procedures, including Mohs micrographic surgery, to preserve hospital resources, including trained personnel, personal protective equipment, ventilators, and hospital beds. There have not been clear-cut guidelines regarding how to approach other dermatologic care for our patients, including routine clinic visits and inpatient dermatology consultations, leaving decisions up to individual departments and providers.
It would be prudent to learn from our colleagues in China who report steps that have been successful in preventing nosocomial spread of COVID-19 in the dermatologic setting. Tao et al4 described their protocols in both the outpatient and inpatient dermatologic setting, beginning with strict triage before patients can even enter a clinic building for their outpatient appointment. Those who screen positive are sent to a fever clinic for further evaluation, which may include a rapid computed tomography scan (using a machine that may perform 200 chest computed tomography scans per day) and SARS-CoV-2 polymerase chain reaction.5 For inpatient dermatologic consultation of patients with known COVID-19, telehealth and multidisciplinary meetings are first and second line, respectively, with bedside dermatologic consultation as a last resort.4 Chen et al6 described similarly strict triage protocols as well as physician use of full-body personal protective equipment during all patient encounters. These measures are taken in light of the well-documented phenomenon of asymptomatic carriage and transmission, as all patients entering their dermatologic clinics have screened negative for symptomatic SARS-CoV-2 infection.6
Conferences and Education
Coronavirus is impacting the education of millions of individuals worldwide, including that of dermatology residents. The Annual Meeting of the American Academy of Dermatology, which was scheduled to take place in March 2020, was canceled due to COVID-19.7 The American Board of Dermatology has released a statement indicating that for all dermatology residents, time spent in COVID-19–mandated quarantine will count as clinical education if residents are able to work with their program to complete independent structured academic activity during that time.8 We also must consider the possibility that dermatology residents are reassigned to work outside of our specialty, resulting in less time and experience caring for patients with dermatologic conditions. Dermatologists in other countries have been called upon to care for COVID-19 patients, even reported to be working in intensive care units in Italy.9 Virtual technologies may be used in novel ways to support dermatology resident education throughout this process.
Final Thoughts
As physicians, dermatologists are in the position to educate their patients regarding prevention strategies, especially given that the lay press disseminates confusing and inaccurate information. The World Health Organization provides specific guidance, focusing on handwashing, respiratory hygiene, social distancing, and encouraging symptomatic patients to seek remote care whenever possible.10 Many of our patients are at high risk of complications due to COVID-19, whether due to their age or because they are immunocompromised. As the situation unfolds, the impact on and role of dermatology in this crisis will continue to evolve.
- Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)[news release]. Geneva, Switzerland: World Health Organization; January 30, 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-%282005%29-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-%282019-ncov%29. Accessed March 16, 2020.
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273.
- World Health Organization. Coronavirus disease 2019: Situation Report—58. March 18, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200318-sitrep-58-covid-19.pdf?sfvrsn=20876712_2. Accessed March 19, 2020.
- Tao J, Song Z, Yang L, et al. Emergency management for preventing and controlling nosocomial infection of 2019 novel coronavirus: implications for the dermatology department [published online March 5, 2020]. Br J Dermatol. doi:10.1111/bjd.19011.
- McNeil DG. Jr. Inside China’s all out war on the coronavirus. The New York Times. March 4, 2020. https://www.nytimes.com/2020/03/04/health/coronavirus-china-aylward.html?smid=tw-nytimes&smtyp=cur. Accessed March 19, 2020.
- Chen Y, Pradhan S, Xue S. What are we doing in the dermatology outpatient department amidst the raging of the 2019 novel coronavirus? J Am Acad Dermatol. 2020;82:1034.
- Hruza GJ. 2020 annual AAD meeting is canceled due to COVID-19 outbreak. American Academy of Dermatology website. https://www.aad.org/member/meetings/am2020/faqs/coronavirus. Accessed March 16, 2020.
- American Board of Dermatology. Impact of COVID-19 on dermatology resident education. March 6, 2020. https://www.abderm.org/2978.aspx. Accessed March 16, 2020.
- “It’s Like a War” [podcast]. The Daily. March 17, 2020. https://www.nytimes.com/2020/03/17/podcasts/the-daily/italy-coronavirus.html?action=click&module=audio-series-bar®ion=header&pgtype=Article. Accessed March 20, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for public. March 18, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed March 19, 2020.
- Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)[news release]. Geneva, Switzerland: World Health Organization; January 30, 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-%282005%29-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-%282019-ncov%29. Accessed March 16, 2020.
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273.
- World Health Organization. Coronavirus disease 2019: Situation Report—58. March 18, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200318-sitrep-58-covid-19.pdf?sfvrsn=20876712_2. Accessed March 19, 2020.
- Tao J, Song Z, Yang L, et al. Emergency management for preventing and controlling nosocomial infection of 2019 novel coronavirus: implications for the dermatology department [published online March 5, 2020]. Br J Dermatol. doi:10.1111/bjd.19011.
- McNeil DG. Jr. Inside China’s all out war on the coronavirus. The New York Times. March 4, 2020. https://www.nytimes.com/2020/03/04/health/coronavirus-china-aylward.html?smid=tw-nytimes&smtyp=cur. Accessed March 19, 2020.
- Chen Y, Pradhan S, Xue S. What are we doing in the dermatology outpatient department amidst the raging of the 2019 novel coronavirus? J Am Acad Dermatol. 2020;82:1034.
- Hruza GJ. 2020 annual AAD meeting is canceled due to COVID-19 outbreak. American Academy of Dermatology website. https://www.aad.org/member/meetings/am2020/faqs/coronavirus. Accessed March 16, 2020.
- American Board of Dermatology. Impact of COVID-19 on dermatology resident education. March 6, 2020. https://www.abderm.org/2978.aspx. Accessed March 16, 2020.
- “It’s Like a War” [podcast]. The Daily. March 17, 2020. https://www.nytimes.com/2020/03/17/podcasts/the-daily/italy-coronavirus.html?action=click&module=audio-series-bar®ion=header&pgtype=Article. Accessed March 20, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for public. March 18, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed March 19, 2020.
Handoffs in Dermatology Residency
As a dermatologist, there are innumerable items to track after each patient encounter, such as results from biopsies, laboratory tests, cultures, and imaging, as well as ensuring follow-up with providers in other specialties. In residency, there is the complicating factor of switching rotations and therefore transitioning care to different providers (Figure). Ensuring organized handoff practices is especially important in residency. In a study of malpractice claims involving residents, handoff problems were a notable contributing factor in 19% of malpractice cases involving residents vs 13% of cases involving attending physicians.1 There still is a high percentage of malpractice cases involving handoff problems among attending physicians, highlighting the fact that these issues persist beyond residency.

This article will review a variety of handoff and organizational practices that dermatology residents currently use, discuss the evidence behind best practices, and highlight additional considerations relevant when selecting organizational tools.
Varied Practices
Based on personal discussions with residents from 7 dermatology residency programs across the country, there is marked variability in both the frequency of handoffs and organizational methods utilized. Two major factors that dictate these practices are the structure of the residency program and electronic health record (EHR) capacities.
Program structure and allocation of resident responsibilities affect the frequency of handoffs in the outpatient dermatology residency setting. In some programs, residents are responsible for all pending studies for patients they have seen, even after switching clinical sites. In other programs, residents sign out patients, including pending test results, when transitioning from one clinical rotation to another. The frequency of these handoffs varies, ranging from every few weeks to every 4 months.
Many dermatology residents report utilizing features in the EHR to organize outstanding tasks and results, obviating the need for additional documentation. Some EHRs have the capacity to assign proxies, which allows for a seamless transition to another provider. When the EHR lacks these capabilities, organization of outstanding tasks relies more heavily on supplemental documentation. Residents noted using spreadsheets, typed documents, electronic applications designed to organize handoffs outside of the EHR, and handwritten notes.
There is room for formal education on the best handoff and organizational practices in dermatology residency. A study of anesthesiology residents at a major academic institution suggested that education regarding sign-out practices is most effective when it is multimodal, using both formal and informal methods.2 Based on my discussions with other dermatology residents, these practices generally are informally learned; often, dermatology residents did not realize that organization practices varied so widely at other institutions.
Evidence Behind Handoff Practices
There are data in the dermatology literature to support utilizing electronic means for handoff practices. At a tertiary dermatology department in Melbourne, Australia, providers created a novel electronic handover system using Microsoft programs to be used alongside the main hospital EHR to help practitioners keep track of outpatient studies.3 An audit of this system demonstrated that its use provided a reliable system for follow-up on all outpatient results, with benefits in clinical, organizational, and health research domains.4 The investigators noted that residents, registrars, nurses, and consultants utilized the electronic handover system, with residents completing 90% of all tasks.3 Similarly, several residents I spoke with personally cited using Listrunner (www.listrunnerapp.com), a Health Insurance Portability and Accountability Act–compliant electronic tool outside of the EHR designed for collaborative management of patient lists.
Outside of the dermatology literature, resident handoff in the outpatient setting mainly has been studied in the primary care year-end transition of care, with findings that are certainly relevant to dermatology residency. Pincavage et al5 performed a targeted literature search on year-end handoff practices, and Donnelly et al6 studied internal medicine residents in an outpatient ambulatory clinic; both supported implementing a standardized process for sign-out. Pincavage et al5 also recommended focusing on high-risk patients, educating residents on handoff practices, preparing patients for the transition, and performing safety audits. Donnelly et al6 found that providing time dedicated to patient handoff and clear expectations improved handoff practices.
There is extensive literature on handoff practices in the inpatient setting sparked by an increasing number of handoffs after the implementation of Accreditation Council for Graduate Medical Education duty hour restrictions in 1989. Some of the guiding principles may be applied to the outpatient dermatology setting. Many residents may be familiar with mnemonics that have been developed to organize content during sign-out, which have been s
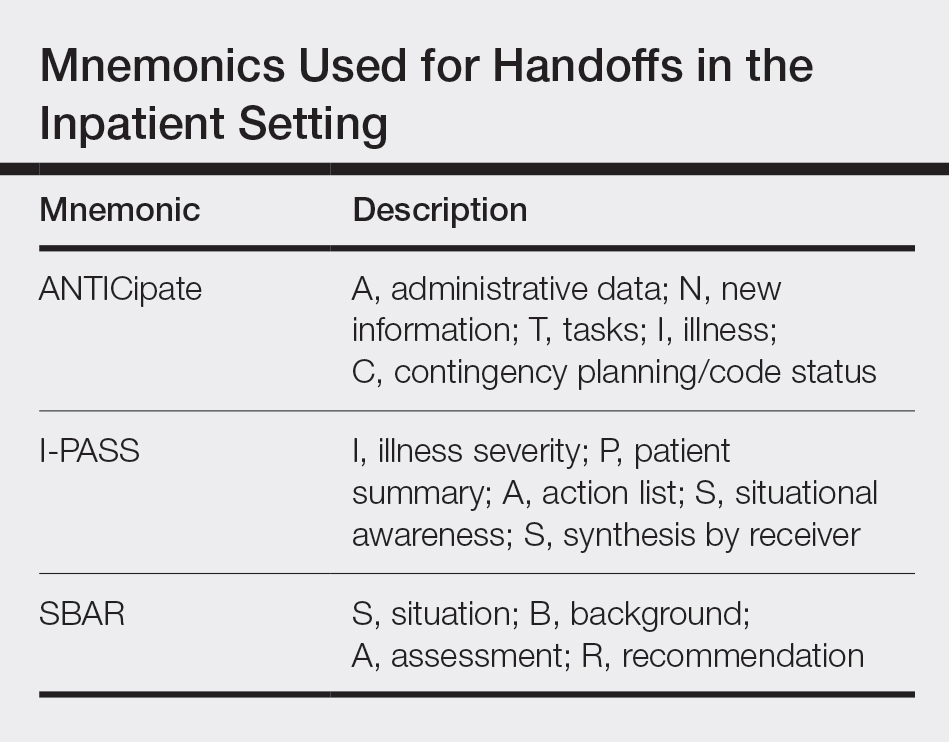
Other Considerations
An important consideration during patient handoffs is security, especially when implementing documentation and tools outside of the EHR. It is important for providers to be compliant with institutional policies as well as the Health Insurance Portability and Accountability Act and ensure protection against cyberattacks, which have been on the rise; 83% of 1300 physicians surveyed have been the victim of a cyberattack.9 Providers also should be mindful of redundancies in organizational and handoff practices. Multiple methods for keeping track of information helps ensure that important results do not fall through the cracks. However, too many redundancies may be wasteful of a practice’s resources and providers’ time.
Final Thoughts
There are varied practices regarding organization of handoff and follow-up. Residency should serve as an opportunity for physicians to become familiar with different practices. Becoming familiar with the varied options may be helpful to take forward in one’s career, especially given that dermatologists may enter a work setting postresidency with practices that are different from where they trained. Additionally, given rapid shifts in technologies, providers must change how they stay organized. This evolving landscape provides an opportunity for the next generation of dermatologists to take leadership to shape the future of organizational practices.
- Singh H, Thomas EJ, Petersen LA, et al. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030-2036.
- Muralidharan M, Clapp JT, Pulos BP, et al. How does training in anesthesia residency shape residents’ approaches to patient care handoffs? a single-center qualitative interview study. BMC Med Educ. 2018;18:271.
- Poon F, Martyres R, Denahy A, et al. Improving patient safety: the impact of an outpatients’ electronic handover system in a tertiary dermatology department. Australas J Dermatol. 2018;59:E183-E188.
- Listrunner website. https://www.listrunnerapp.com. Accessed January 30, 2020.
- Pincavage AT, Donnelly MJ, Young JQ, et al. Year-end resident clinic handoffs: narrative review and recommendations for improvement. Jt Comm J Qual Patient Saf. 2017;43:71-79.
- Donnelly MJ, Clauser JM, Weissman NJ. An intervention to improve ambulatory care handoffs at the end of residency. J Grad Med Educ. 2012;4:381-384.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257-266.
- Breaux J, Mclendon R, Stedman RB, et al. Developing a standardized and sustainable resident sign-out process: an AIAMC National Initiative IV Project. Ochsner J. 2014;14:563-568.
- American Medical Association and Accenture. Taking the physician’s pulse: tackling cyber threats in healthcare. https://www.accenture.com/_acnmedia/accenture/conversion-assets/dotcom/documents/local/en/accenture-health-taking-the-physicians-pulse.pdf. Accessed January 30, 2020.
As a dermatologist, there are innumerable items to track after each patient encounter, such as results from biopsies, laboratory tests, cultures, and imaging, as well as ensuring follow-up with providers in other specialties. In residency, there is the complicating factor of switching rotations and therefore transitioning care to different providers (Figure). Ensuring organized handoff practices is especially important in residency. In a study of malpractice claims involving residents, handoff problems were a notable contributing factor in 19% of malpractice cases involving residents vs 13% of cases involving attending physicians.1 There still is a high percentage of malpractice cases involving handoff problems among attending physicians, highlighting the fact that these issues persist beyond residency.

This article will review a variety of handoff and organizational practices that dermatology residents currently use, discuss the evidence behind best practices, and highlight additional considerations relevant when selecting organizational tools.
Varied Practices
Based on personal discussions with residents from 7 dermatology residency programs across the country, there is marked variability in both the frequency of handoffs and organizational methods utilized. Two major factors that dictate these practices are the structure of the residency program and electronic health record (EHR) capacities.
Program structure and allocation of resident responsibilities affect the frequency of handoffs in the outpatient dermatology residency setting. In some programs, residents are responsible for all pending studies for patients they have seen, even after switching clinical sites. In other programs, residents sign out patients, including pending test results, when transitioning from one clinical rotation to another. The frequency of these handoffs varies, ranging from every few weeks to every 4 months.
Many dermatology residents report utilizing features in the EHR to organize outstanding tasks and results, obviating the need for additional documentation. Some EHRs have the capacity to assign proxies, which allows for a seamless transition to another provider. When the EHR lacks these capabilities, organization of outstanding tasks relies more heavily on supplemental documentation. Residents noted using spreadsheets, typed documents, electronic applications designed to organize handoffs outside of the EHR, and handwritten notes.
There is room for formal education on the best handoff and organizational practices in dermatology residency. A study of anesthesiology residents at a major academic institution suggested that education regarding sign-out practices is most effective when it is multimodal, using both formal and informal methods.2 Based on my discussions with other dermatology residents, these practices generally are informally learned; often, dermatology residents did not realize that organization practices varied so widely at other institutions.
Evidence Behind Handoff Practices
There are data in the dermatology literature to support utilizing electronic means for handoff practices. At a tertiary dermatology department in Melbourne, Australia, providers created a novel electronic handover system using Microsoft programs to be used alongside the main hospital EHR to help practitioners keep track of outpatient studies.3 An audit of this system demonstrated that its use provided a reliable system for follow-up on all outpatient results, with benefits in clinical, organizational, and health research domains.4 The investigators noted that residents, registrars, nurses, and consultants utilized the electronic handover system, with residents completing 90% of all tasks.3 Similarly, several residents I spoke with personally cited using Listrunner (www.listrunnerapp.com), a Health Insurance Portability and Accountability Act–compliant electronic tool outside of the EHR designed for collaborative management of patient lists.
Outside of the dermatology literature, resident handoff in the outpatient setting mainly has been studied in the primary care year-end transition of care, with findings that are certainly relevant to dermatology residency. Pincavage et al5 performed a targeted literature search on year-end handoff practices, and Donnelly et al6 studied internal medicine residents in an outpatient ambulatory clinic; both supported implementing a standardized process for sign-out. Pincavage et al5 also recommended focusing on high-risk patients, educating residents on handoff practices, preparing patients for the transition, and performing safety audits. Donnelly et al6 found that providing time dedicated to patient handoff and clear expectations improved handoff practices.
There is extensive literature on handoff practices in the inpatient setting sparked by an increasing number of handoffs after the implementation of Accreditation Council for Graduate Medical Education duty hour restrictions in 1989. Some of the guiding principles may be applied to the outpatient dermatology setting. Many residents may be familiar with mnemonics that have been developed to organize content during sign-out, which have been s
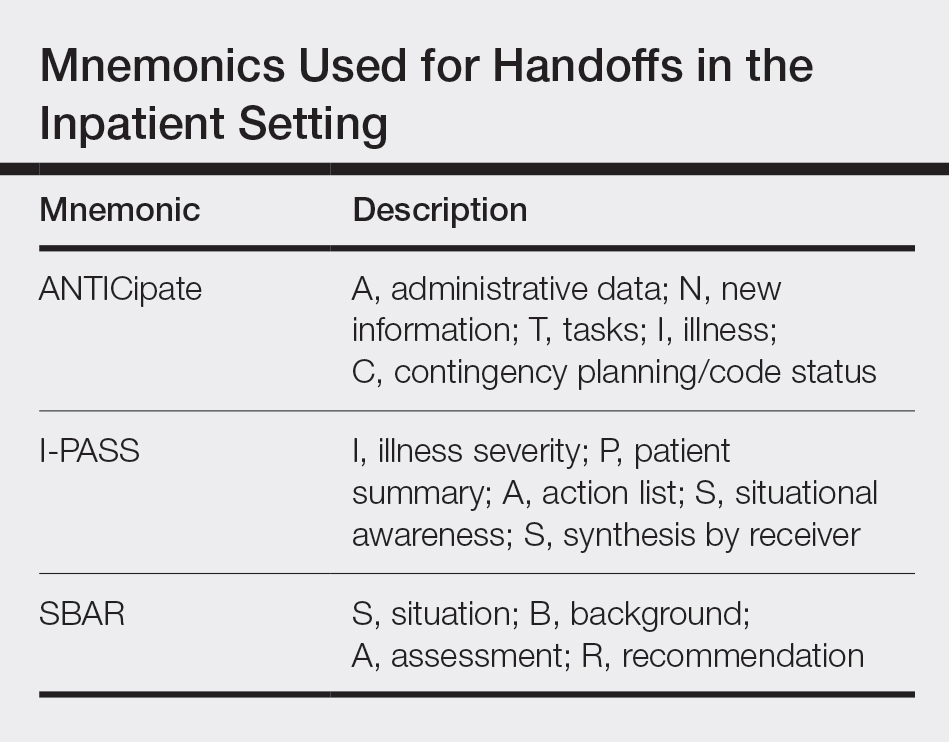
Other Considerations
An important consideration during patient handoffs is security, especially when implementing documentation and tools outside of the EHR. It is important for providers to be compliant with institutional policies as well as the Health Insurance Portability and Accountability Act and ensure protection against cyberattacks, which have been on the rise; 83% of 1300 physicians surveyed have been the victim of a cyberattack.9 Providers also should be mindful of redundancies in organizational and handoff practices. Multiple methods for keeping track of information helps ensure that important results do not fall through the cracks. However, too many redundancies may be wasteful of a practice’s resources and providers’ time.
Final Thoughts
There are varied practices regarding organization of handoff and follow-up. Residency should serve as an opportunity for physicians to become familiar with different practices. Becoming familiar with the varied options may be helpful to take forward in one’s career, especially given that dermatologists may enter a work setting postresidency with practices that are different from where they trained. Additionally, given rapid shifts in technologies, providers must change how they stay organized. This evolving landscape provides an opportunity for the next generation of dermatologists to take leadership to shape the future of organizational practices.
As a dermatologist, there are innumerable items to track after each patient encounter, such as results from biopsies, laboratory tests, cultures, and imaging, as well as ensuring follow-up with providers in other specialties. In residency, there is the complicating factor of switching rotations and therefore transitioning care to different providers (Figure). Ensuring organized handoff practices is especially important in residency. In a study of malpractice claims involving residents, handoff problems were a notable contributing factor in 19% of malpractice cases involving residents vs 13% of cases involving attending physicians.1 There still is a high percentage of malpractice cases involving handoff problems among attending physicians, highlighting the fact that these issues persist beyond residency.

This article will review a variety of handoff and organizational practices that dermatology residents currently use, discuss the evidence behind best practices, and highlight additional considerations relevant when selecting organizational tools.
Varied Practices
Based on personal discussions with residents from 7 dermatology residency programs across the country, there is marked variability in both the frequency of handoffs and organizational methods utilized. Two major factors that dictate these practices are the structure of the residency program and electronic health record (EHR) capacities.
Program structure and allocation of resident responsibilities affect the frequency of handoffs in the outpatient dermatology residency setting. In some programs, residents are responsible for all pending studies for patients they have seen, even after switching clinical sites. In other programs, residents sign out patients, including pending test results, when transitioning from one clinical rotation to another. The frequency of these handoffs varies, ranging from every few weeks to every 4 months.
Many dermatology residents report utilizing features in the EHR to organize outstanding tasks and results, obviating the need for additional documentation. Some EHRs have the capacity to assign proxies, which allows for a seamless transition to another provider. When the EHR lacks these capabilities, organization of outstanding tasks relies more heavily on supplemental documentation. Residents noted using spreadsheets, typed documents, electronic applications designed to organize handoffs outside of the EHR, and handwritten notes.
There is room for formal education on the best handoff and organizational practices in dermatology residency. A study of anesthesiology residents at a major academic institution suggested that education regarding sign-out practices is most effective when it is multimodal, using both formal and informal methods.2 Based on my discussions with other dermatology residents, these practices generally are informally learned; often, dermatology residents did not realize that organization practices varied so widely at other institutions.
Evidence Behind Handoff Practices
There are data in the dermatology literature to support utilizing electronic means for handoff practices. At a tertiary dermatology department in Melbourne, Australia, providers created a novel electronic handover system using Microsoft programs to be used alongside the main hospital EHR to help practitioners keep track of outpatient studies.3 An audit of this system demonstrated that its use provided a reliable system for follow-up on all outpatient results, with benefits in clinical, organizational, and health research domains.4 The investigators noted that residents, registrars, nurses, and consultants utilized the electronic handover system, with residents completing 90% of all tasks.3 Similarly, several residents I spoke with personally cited using Listrunner (www.listrunnerapp.com), a Health Insurance Portability and Accountability Act–compliant electronic tool outside of the EHR designed for collaborative management of patient lists.
Outside of the dermatology literature, resident handoff in the outpatient setting mainly has been studied in the primary care year-end transition of care, with findings that are certainly relevant to dermatology residency. Pincavage et al5 performed a targeted literature search on year-end handoff practices, and Donnelly et al6 studied internal medicine residents in an outpatient ambulatory clinic; both supported implementing a standardized process for sign-out. Pincavage et al5 also recommended focusing on high-risk patients, educating residents on handoff practices, preparing patients for the transition, and performing safety audits. Donnelly et al6 found that providing time dedicated to patient handoff and clear expectations improved handoff practices.
There is extensive literature on handoff practices in the inpatient setting sparked by an increasing number of handoffs after the implementation of Accreditation Council for Graduate Medical Education duty hour restrictions in 1989. Some of the guiding principles may be applied to the outpatient dermatology setting. Many residents may be familiar with mnemonics that have been developed to organize content during sign-out, which have been s
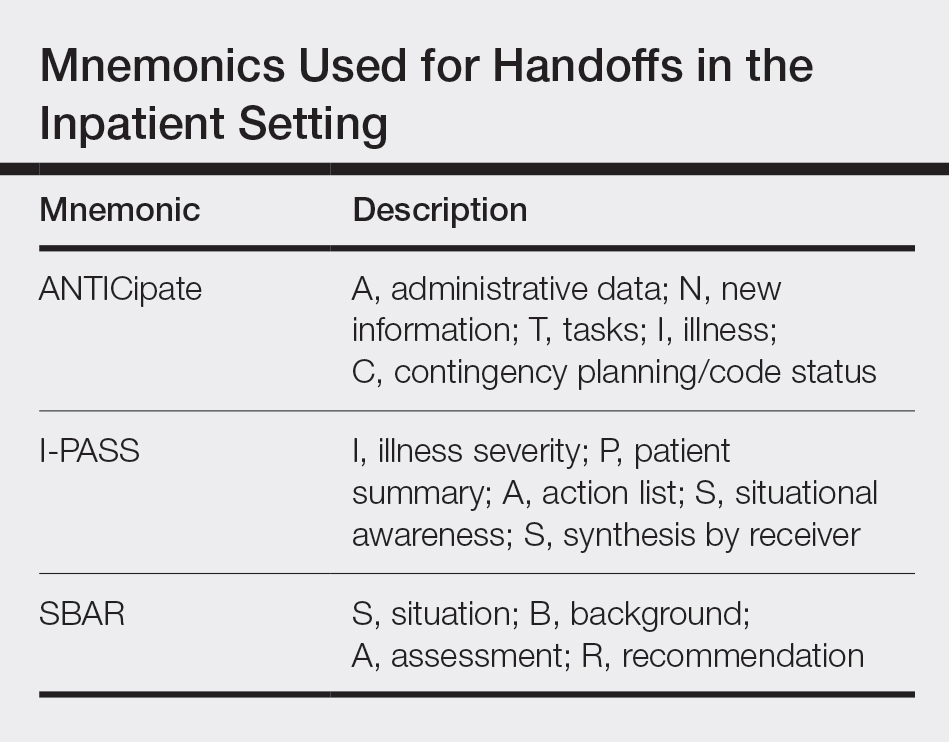
Other Considerations
An important consideration during patient handoffs is security, especially when implementing documentation and tools outside of the EHR. It is important for providers to be compliant with institutional policies as well as the Health Insurance Portability and Accountability Act and ensure protection against cyberattacks, which have been on the rise; 83% of 1300 physicians surveyed have been the victim of a cyberattack.9 Providers also should be mindful of redundancies in organizational and handoff practices. Multiple methods for keeping track of information helps ensure that important results do not fall through the cracks. However, too many redundancies may be wasteful of a practice’s resources and providers’ time.
Final Thoughts
There are varied practices regarding organization of handoff and follow-up. Residency should serve as an opportunity for physicians to become familiar with different practices. Becoming familiar with the varied options may be helpful to take forward in one’s career, especially given that dermatologists may enter a work setting postresidency with practices that are different from where they trained. Additionally, given rapid shifts in technologies, providers must change how they stay organized. This evolving landscape provides an opportunity for the next generation of dermatologists to take leadership to shape the future of organizational practices.
- Singh H, Thomas EJ, Petersen LA, et al. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030-2036.
- Muralidharan M, Clapp JT, Pulos BP, et al. How does training in anesthesia residency shape residents’ approaches to patient care handoffs? a single-center qualitative interview study. BMC Med Educ. 2018;18:271.
- Poon F, Martyres R, Denahy A, et al. Improving patient safety: the impact of an outpatients’ electronic handover system in a tertiary dermatology department. Australas J Dermatol. 2018;59:E183-E188.
- Listrunner website. https://www.listrunnerapp.com. Accessed January 30, 2020.
- Pincavage AT, Donnelly MJ, Young JQ, et al. Year-end resident clinic handoffs: narrative review and recommendations for improvement. Jt Comm J Qual Patient Saf. 2017;43:71-79.
- Donnelly MJ, Clauser JM, Weissman NJ. An intervention to improve ambulatory care handoffs at the end of residency. J Grad Med Educ. 2012;4:381-384.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257-266.
- Breaux J, Mclendon R, Stedman RB, et al. Developing a standardized and sustainable resident sign-out process: an AIAMC National Initiative IV Project. Ochsner J. 2014;14:563-568.
- American Medical Association and Accenture. Taking the physician’s pulse: tackling cyber threats in healthcare. https://www.accenture.com/_acnmedia/accenture/conversion-assets/dotcom/documents/local/en/accenture-health-taking-the-physicians-pulse.pdf. Accessed January 30, 2020.
- Singh H, Thomas EJ, Petersen LA, et al. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030-2036.
- Muralidharan M, Clapp JT, Pulos BP, et al. How does training in anesthesia residency shape residents’ approaches to patient care handoffs? a single-center qualitative interview study. BMC Med Educ. 2018;18:271.
- Poon F, Martyres R, Denahy A, et al. Improving patient safety: the impact of an outpatients’ electronic handover system in a tertiary dermatology department. Australas J Dermatol. 2018;59:E183-E188.
- Listrunner website. https://www.listrunnerapp.com. Accessed January 30, 2020.
- Pincavage AT, Donnelly MJ, Young JQ, et al. Year-end resident clinic handoffs: narrative review and recommendations for improvement. Jt Comm J Qual Patient Saf. 2017;43:71-79.
- Donnelly MJ, Clauser JM, Weissman NJ. An intervention to improve ambulatory care handoffs at the end of residency. J Grad Med Educ. 2012;4:381-384.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257-266.
- Breaux J, Mclendon R, Stedman RB, et al. Developing a standardized and sustainable resident sign-out process: an AIAMC National Initiative IV Project. Ochsner J. 2014;14:563-568.
- American Medical Association and Accenture. Taking the physician’s pulse: tackling cyber threats in healthcare. https://www.accenture.com/_acnmedia/accenture/conversion-assets/dotcom/documents/local/en/accenture-health-taking-the-physicians-pulse.pdf. Accessed January 30, 2020.
Resident Pearl
- For dermatology residents, ensuring organized handoff and follow-up practices is essential. Residency provides an opportunity to become familiar with different practices to take forward in one’s career.


