User login
75-year-old man • fatigue • unintentional weight loss • anemia • Dx?
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
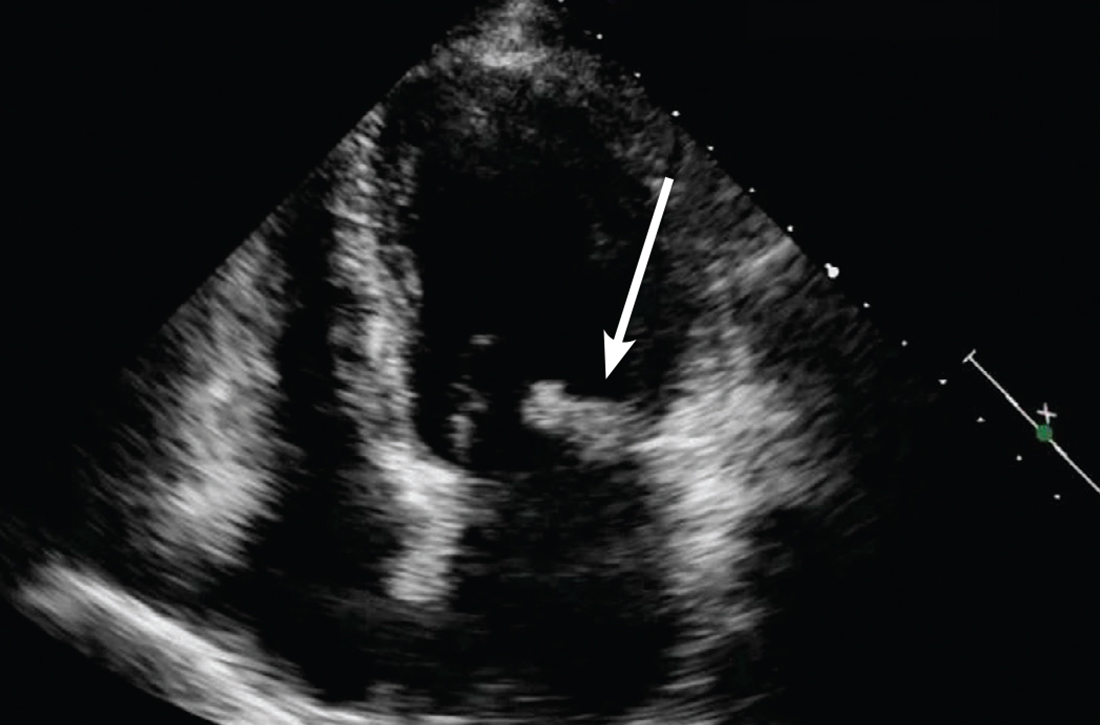
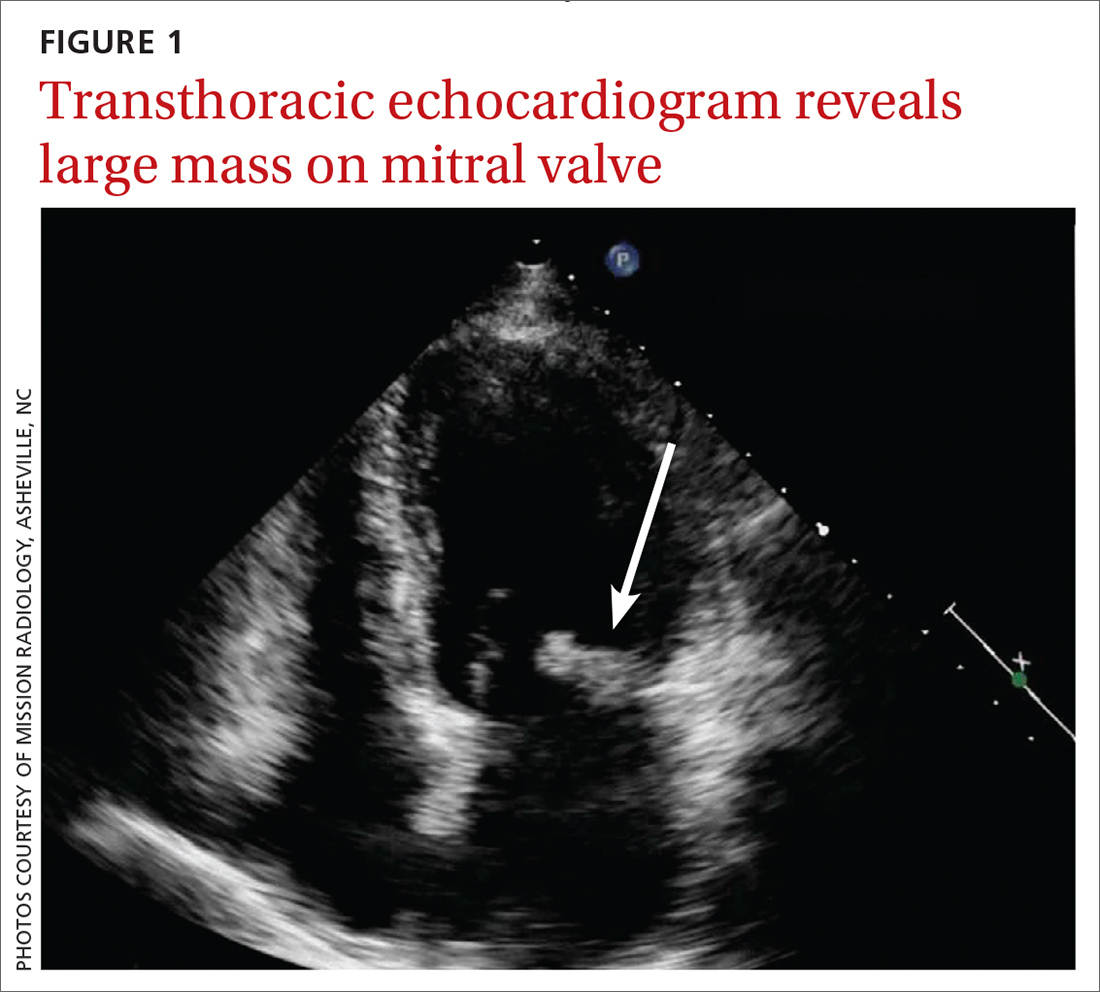
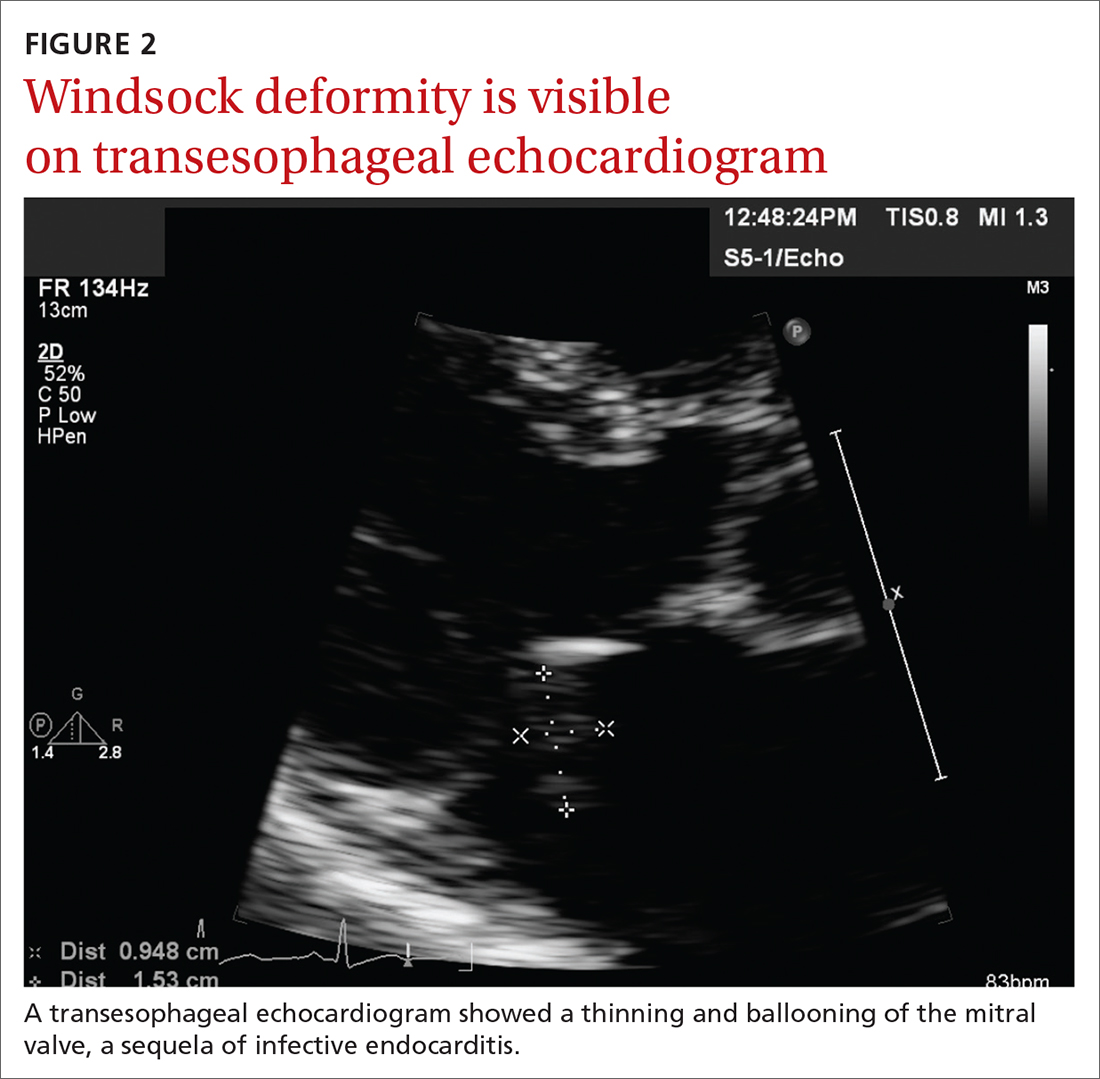
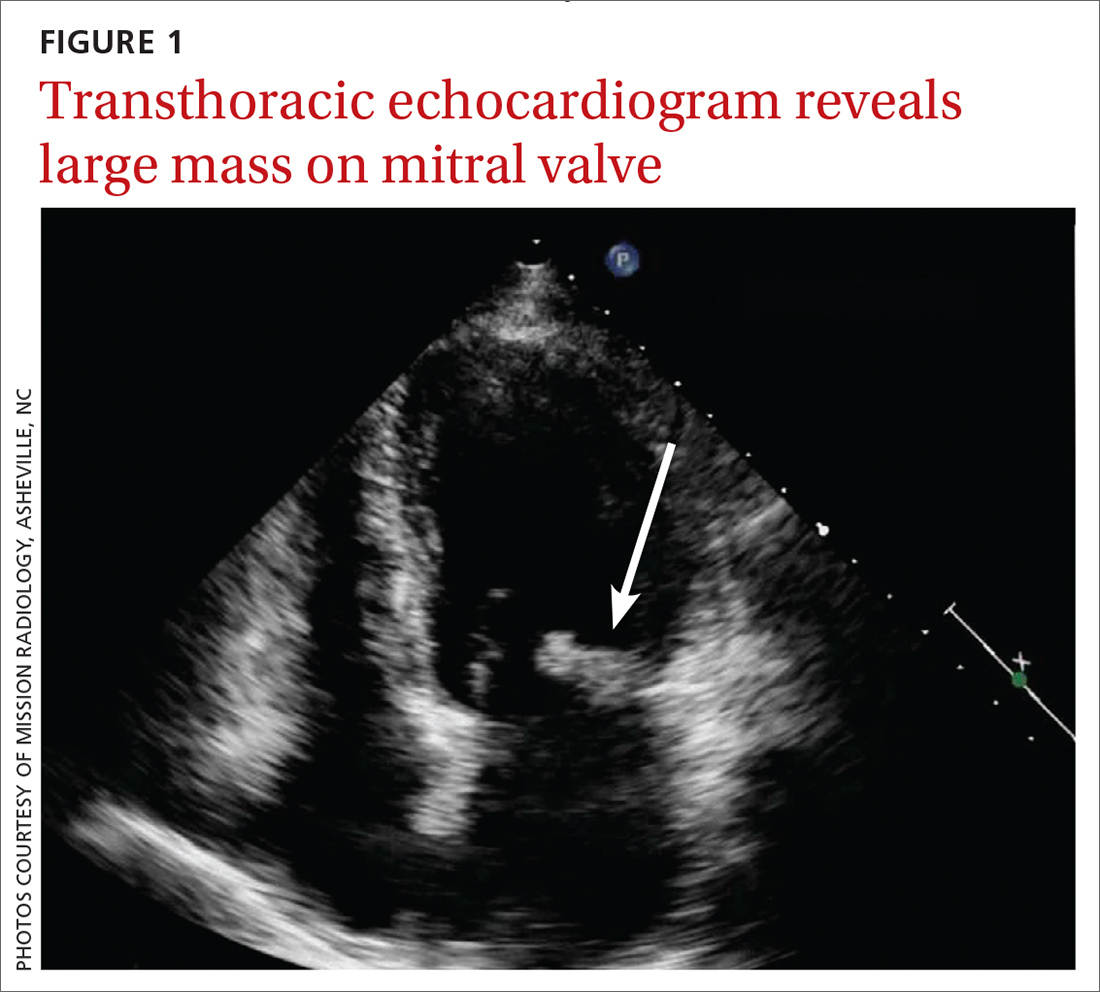
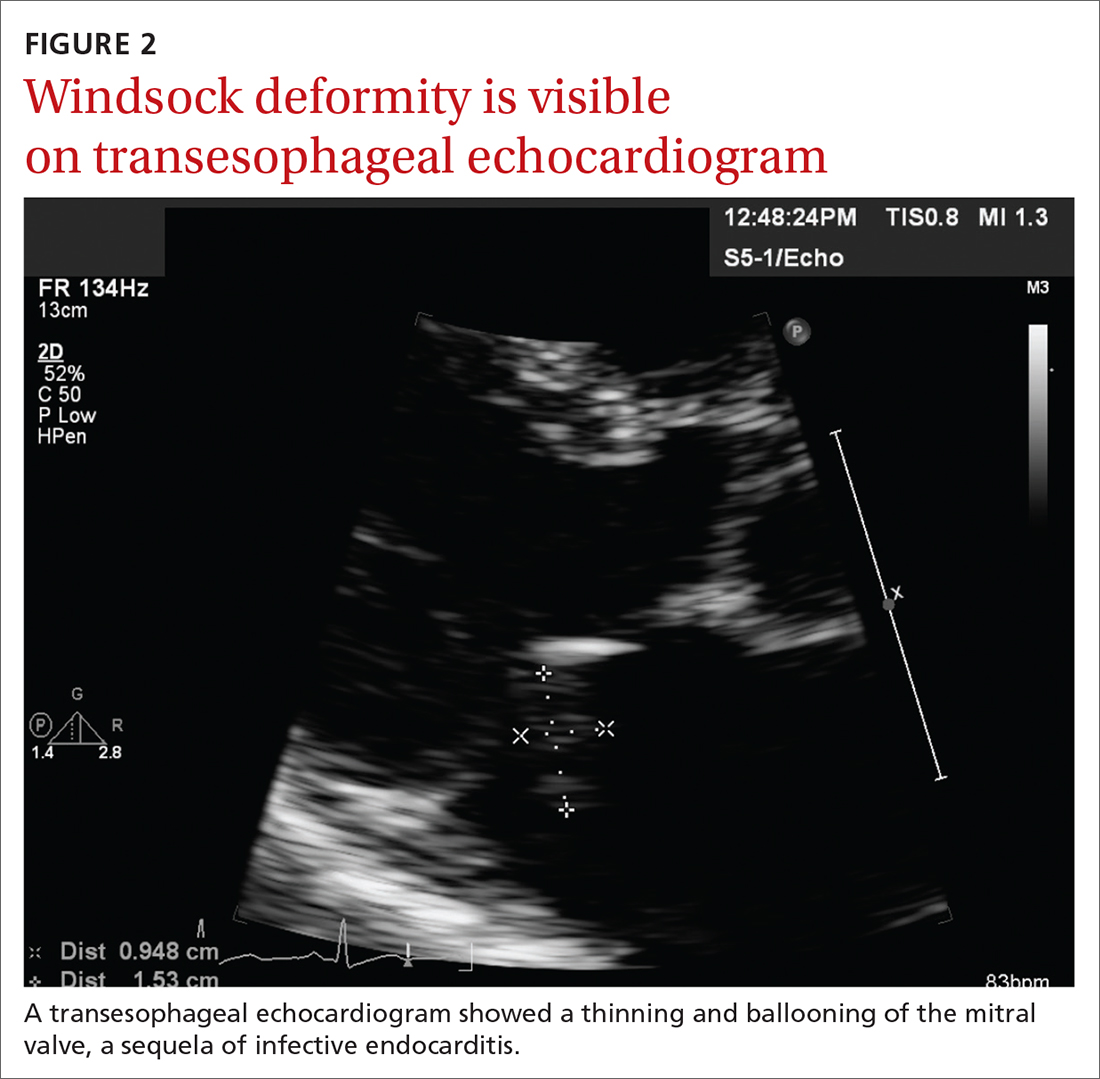
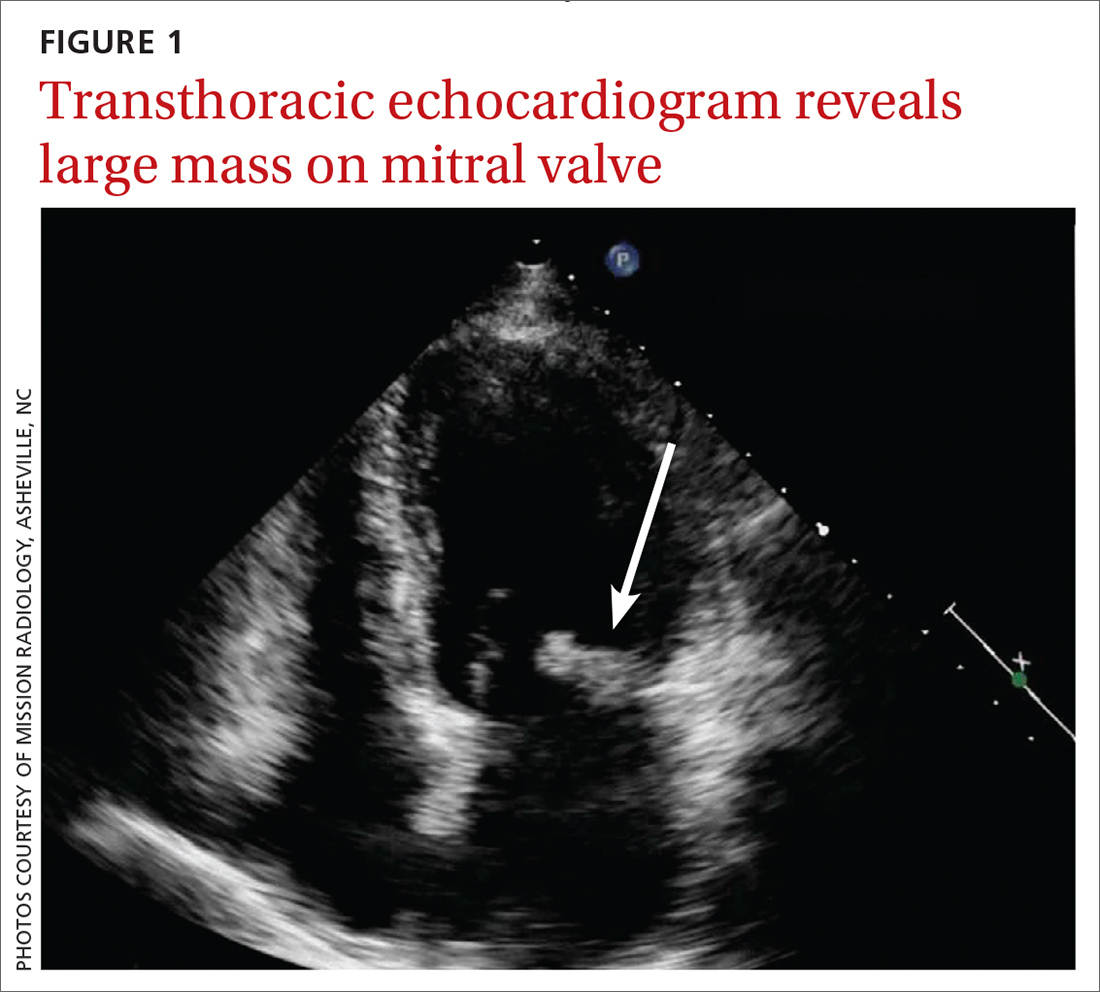
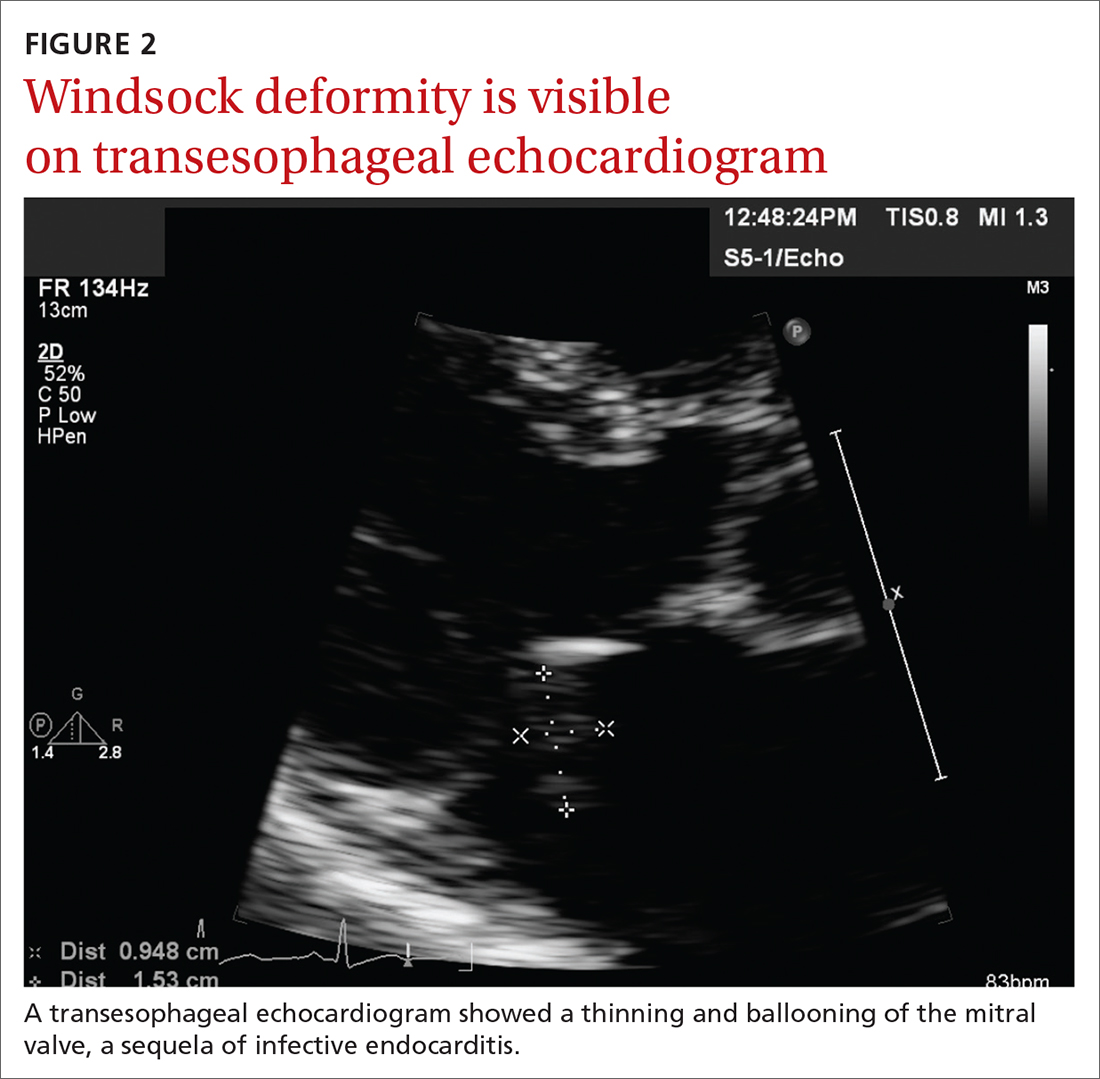
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603
Does XR injectable naltrexone prevent relapse as effectively as daily sublingual buprenorphine-naloxone?
EVIDENCE SUMMARY
Two recent multicenter, open-label RCTs, 1 in the United States and 1 in Norway, compared monthly XR-NTX with daily BUP-NX.1,2 Both studies evaluated effectiveness (defined by either the number of people who relapsed or self-reported opioid use), cravings, and safety (defined as the absence of serious adverse events such as medically complex withdrawal or fatal overdose).
The participant populations were similar in both mean age and mean age of onset of opioid use. Duration of opioid use was reported differently (total duration or years of heavy heroin or other opioid use) and couldn’t be compared directly.
Naltrexone and buprenorphine-naloxone are similarly effective
The US study enrolled 570 opioid-dependent participants in a 24-week comparative effectiveness trial.1 The 8 study sites were community treatment programs, and the participants were recruited during voluntary inpatient detoxification admissions. Some participants were randomized while on methadone or buprenorphine tapers and some after complete detoxification.
The intention-to-treat analysis included 283 patients in the XR-NTX group and 287 in the BUP-NX group. At 24 weeks, the number of participants who’d had a relapse event (self-reported use or positive urine drug test for nonstudy opioids or refusal to provide a urine sample) was 185 (65%) for XR-NTX compared with 163 (57%) for BUP-NX (odds ratio [OR] = 1.44, 95% confidence interval [CI], 1.02 to 2.01; P = .036).
The 12-week Norwegian noninferiority trial enrolled 159 participants.2 In contrast to the US study, all participants were required to complete inpatient detoxification before randomization and induction onto the study medication.
Patients on BUP-NX reported 3.6 more days of heroin use within the previous 28 days than patients in the XR-NTX group (95% CI, 1.2 to 6; P = .003). For other illicit opioids, self-reported use was 2.4 days greater in the BUP-NX group (95% CI, −0.1 to 4.9; P = .06). Retention with XR-NTX was noninferior to BUP-NX (mean days in therapy [standard deviation], 69.3 [25.9] and 63.7 [29.9]; P = .33).
Randomizing after complete detox reduces induction failures
Naltrexone, a full opioid antagonist, precipitates withdrawal when a full or partial opioid agonist is engaging the opioid receptor. For this reason, an opioid-free interval of 7 to 10 days is generally recommended before initiating naltrexone, raising the risk for relapse during the induction process.
Continue to: The Norwegian trial...
The Norwegian trial randomized participants after detoxification. The US trial, in which some participants were randomized before completing detoxification, reported 79 (28%) induction failures for XR-NTX and 17 (6%) for BUP-NX.1 As a result, a per protocol analysis was completed with the 204 patients on XR-NTX and 270 patients on BUP-NX who were successfully inducted onto a study medication. The 24-week relapse rate was 52% (106) for XR-NTX and 56% (150) for BUP-NX (OR = 0.87; 95% CI, 0.60 to 1.25; P = .44).
Cravings, adverse events, and cost considerations
Patients reported cravings using a visual analog scale. At 12 weeks in both studies, the XR-NTX groups reported fewer cravings than the BUP-NX groups, although by the end of the 24-week US trial, no statistically significant difference in cravings was found between the 2 groups.1,2
The Norwegian trial found a difference between the XR-NTX and the BUP-NX groups in the percentage of nonserious adverse events such as nausea or chills (60.6% in the XR-NTX group vs 30.6% in the BUP-NX group; P < .001), and the US trial found a difference in total number of overdoses (64% of the total overdoses were in the XR-NTX group). Neither trial, however, reported a statistically significant difference in serious adverse events or fatal overdoses between the 2 groups.1,2
The price for naltrexone is $1665.06 per monthly injection.3 The price for buprenorphine-naloxone varies depending on dose and formulation, with a general range of $527 to $600 per month at 16 mg/d.4
Editor’s takeaway
Two higher-quality RCTs show similar but imperfect effectiveness for both XR-NTX and daily sublingual BUP-NX. Injectable naltrexone’s higher cost may influence medication choice.
1. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391:309-318.
2. Tanum L, Solli KK, Latif ZE, et al. Effectiveness of injectable extended-release naltrexone vs daily buprenorphine-naloxone for opioid dependence: a randomized clinical noninferiority trial. JAMA Psychiatry. 2017;74:1197-1205.
3. Naltrexone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
4. Buprenorphine and naloxone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
EVIDENCE SUMMARY
Two recent multicenter, open-label RCTs, 1 in the United States and 1 in Norway, compared monthly XR-NTX with daily BUP-NX.1,2 Both studies evaluated effectiveness (defined by either the number of people who relapsed or self-reported opioid use), cravings, and safety (defined as the absence of serious adverse events such as medically complex withdrawal or fatal overdose).
The participant populations were similar in both mean age and mean age of onset of opioid use. Duration of opioid use was reported differently (total duration or years of heavy heroin or other opioid use) and couldn’t be compared directly.
Naltrexone and buprenorphine-naloxone are similarly effective
The US study enrolled 570 opioid-dependent participants in a 24-week comparative effectiveness trial.1 The 8 study sites were community treatment programs, and the participants were recruited during voluntary inpatient detoxification admissions. Some participants were randomized while on methadone or buprenorphine tapers and some after complete detoxification.
The intention-to-treat analysis included 283 patients in the XR-NTX group and 287 in the BUP-NX group. At 24 weeks, the number of participants who’d had a relapse event (self-reported use or positive urine drug test for nonstudy opioids or refusal to provide a urine sample) was 185 (65%) for XR-NTX compared with 163 (57%) for BUP-NX (odds ratio [OR] = 1.44, 95% confidence interval [CI], 1.02 to 2.01; P = .036).
The 12-week Norwegian noninferiority trial enrolled 159 participants.2 In contrast to the US study, all participants were required to complete inpatient detoxification before randomization and induction onto the study medication.
Patients on BUP-NX reported 3.6 more days of heroin use within the previous 28 days than patients in the XR-NTX group (95% CI, 1.2 to 6; P = .003). For other illicit opioids, self-reported use was 2.4 days greater in the BUP-NX group (95% CI, −0.1 to 4.9; P = .06). Retention with XR-NTX was noninferior to BUP-NX (mean days in therapy [standard deviation], 69.3 [25.9] and 63.7 [29.9]; P = .33).
Randomizing after complete detox reduces induction failures
Naltrexone, a full opioid antagonist, precipitates withdrawal when a full or partial opioid agonist is engaging the opioid receptor. For this reason, an opioid-free interval of 7 to 10 days is generally recommended before initiating naltrexone, raising the risk for relapse during the induction process.
Continue to: The Norwegian trial...
The Norwegian trial randomized participants after detoxification. The US trial, in which some participants were randomized before completing detoxification, reported 79 (28%) induction failures for XR-NTX and 17 (6%) for BUP-NX.1 As a result, a per protocol analysis was completed with the 204 patients on XR-NTX and 270 patients on BUP-NX who were successfully inducted onto a study medication. The 24-week relapse rate was 52% (106) for XR-NTX and 56% (150) for BUP-NX (OR = 0.87; 95% CI, 0.60 to 1.25; P = .44).
Cravings, adverse events, and cost considerations
Patients reported cravings using a visual analog scale. At 12 weeks in both studies, the XR-NTX groups reported fewer cravings than the BUP-NX groups, although by the end of the 24-week US trial, no statistically significant difference in cravings was found between the 2 groups.1,2
The Norwegian trial found a difference between the XR-NTX and the BUP-NX groups in the percentage of nonserious adverse events such as nausea or chills (60.6% in the XR-NTX group vs 30.6% in the BUP-NX group; P < .001), and the US trial found a difference in total number of overdoses (64% of the total overdoses were in the XR-NTX group). Neither trial, however, reported a statistically significant difference in serious adverse events or fatal overdoses between the 2 groups.1,2
The price for naltrexone is $1665.06 per monthly injection.3 The price for buprenorphine-naloxone varies depending on dose and formulation, with a general range of $527 to $600 per month at 16 mg/d.4
Editor’s takeaway
Two higher-quality RCTs show similar but imperfect effectiveness for both XR-NTX and daily sublingual BUP-NX. Injectable naltrexone’s higher cost may influence medication choice.
EVIDENCE SUMMARY
Two recent multicenter, open-label RCTs, 1 in the United States and 1 in Norway, compared monthly XR-NTX with daily BUP-NX.1,2 Both studies evaluated effectiveness (defined by either the number of people who relapsed or self-reported opioid use), cravings, and safety (defined as the absence of serious adverse events such as medically complex withdrawal or fatal overdose).
The participant populations were similar in both mean age and mean age of onset of opioid use. Duration of opioid use was reported differently (total duration or years of heavy heroin or other opioid use) and couldn’t be compared directly.
Naltrexone and buprenorphine-naloxone are similarly effective
The US study enrolled 570 opioid-dependent participants in a 24-week comparative effectiveness trial.1 The 8 study sites were community treatment programs, and the participants were recruited during voluntary inpatient detoxification admissions. Some participants were randomized while on methadone or buprenorphine tapers and some after complete detoxification.
The intention-to-treat analysis included 283 patients in the XR-NTX group and 287 in the BUP-NX group. At 24 weeks, the number of participants who’d had a relapse event (self-reported use or positive urine drug test for nonstudy opioids or refusal to provide a urine sample) was 185 (65%) for XR-NTX compared with 163 (57%) for BUP-NX (odds ratio [OR] = 1.44, 95% confidence interval [CI], 1.02 to 2.01; P = .036).
The 12-week Norwegian noninferiority trial enrolled 159 participants.2 In contrast to the US study, all participants were required to complete inpatient detoxification before randomization and induction onto the study medication.
Patients on BUP-NX reported 3.6 more days of heroin use within the previous 28 days than patients in the XR-NTX group (95% CI, 1.2 to 6; P = .003). For other illicit opioids, self-reported use was 2.4 days greater in the BUP-NX group (95% CI, −0.1 to 4.9; P = .06). Retention with XR-NTX was noninferior to BUP-NX (mean days in therapy [standard deviation], 69.3 [25.9] and 63.7 [29.9]; P = .33).
Randomizing after complete detox reduces induction failures
Naltrexone, a full opioid antagonist, precipitates withdrawal when a full or partial opioid agonist is engaging the opioid receptor. For this reason, an opioid-free interval of 7 to 10 days is generally recommended before initiating naltrexone, raising the risk for relapse during the induction process.
Continue to: The Norwegian trial...
The Norwegian trial randomized participants after detoxification. The US trial, in which some participants were randomized before completing detoxification, reported 79 (28%) induction failures for XR-NTX and 17 (6%) for BUP-NX.1 As a result, a per protocol analysis was completed with the 204 patients on XR-NTX and 270 patients on BUP-NX who were successfully inducted onto a study medication. The 24-week relapse rate was 52% (106) for XR-NTX and 56% (150) for BUP-NX (OR = 0.87; 95% CI, 0.60 to 1.25; P = .44).
Cravings, adverse events, and cost considerations
Patients reported cravings using a visual analog scale. At 12 weeks in both studies, the XR-NTX groups reported fewer cravings than the BUP-NX groups, although by the end of the 24-week US trial, no statistically significant difference in cravings was found between the 2 groups.1,2
The Norwegian trial found a difference between the XR-NTX and the BUP-NX groups in the percentage of nonserious adverse events such as nausea or chills (60.6% in the XR-NTX group vs 30.6% in the BUP-NX group; P < .001), and the US trial found a difference in total number of overdoses (64% of the total overdoses were in the XR-NTX group). Neither trial, however, reported a statistically significant difference in serious adverse events or fatal overdoses between the 2 groups.1,2
The price for naltrexone is $1665.06 per monthly injection.3 The price for buprenorphine-naloxone varies depending on dose and formulation, with a general range of $527 to $600 per month at 16 mg/d.4
Editor’s takeaway
Two higher-quality RCTs show similar but imperfect effectiveness for both XR-NTX and daily sublingual BUP-NX. Injectable naltrexone’s higher cost may influence medication choice.
1. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391:309-318.
2. Tanum L, Solli KK, Latif ZE, et al. Effectiveness of injectable extended-release naltrexone vs daily buprenorphine-naloxone for opioid dependence: a randomized clinical noninferiority trial. JAMA Psychiatry. 2017;74:1197-1205.
3. Naltrexone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
4. Buprenorphine and naloxone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
1. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391:309-318.
2. Tanum L, Solli KK, Latif ZE, et al. Effectiveness of injectable extended-release naltrexone vs daily buprenorphine-naloxone for opioid dependence: a randomized clinical noninferiority trial. JAMA Psychiatry. 2017;74:1197-1205.
3. Naltrexone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
4. Buprenorphine and naloxone: drug information. Lexi-Comp, Inc (Lexi-Drugs). Wolters Kluwer Health, Inc. Riverwoods, IL. http://online.lexi.com. Accessed November 20, 2020.
EVIDENCE-BASED ANSWER:
Yes. Monthly extended-release injectable naltrexone (XR-NTX) treats opioid use disorder as effectively as daily sublingual buprenorphine-naloxone (BUP-NX) without causing any increase in serious adverse events or fatal overdoses. (strength of recommendation: A, 2 good-quality RCTs).
Which oral nonopioid agents are most effective for OA pain?
EVIDENCE SUMMARY
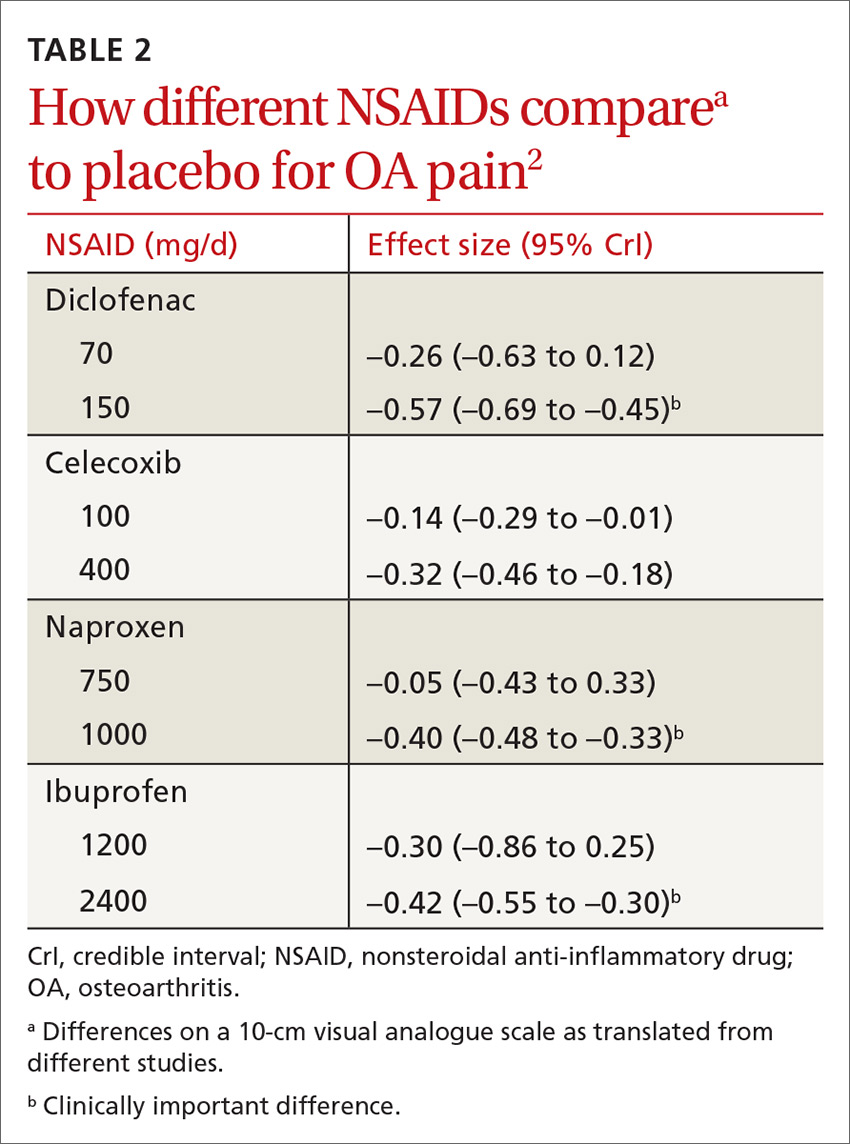
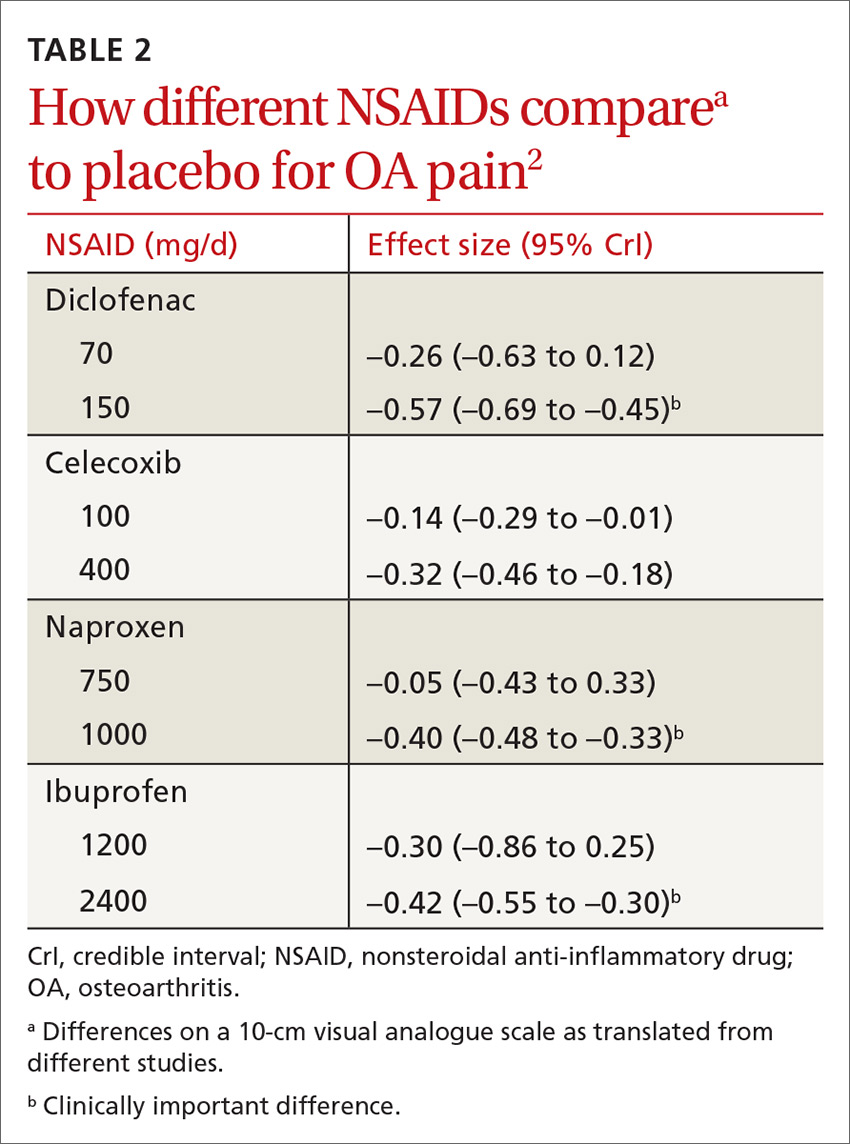
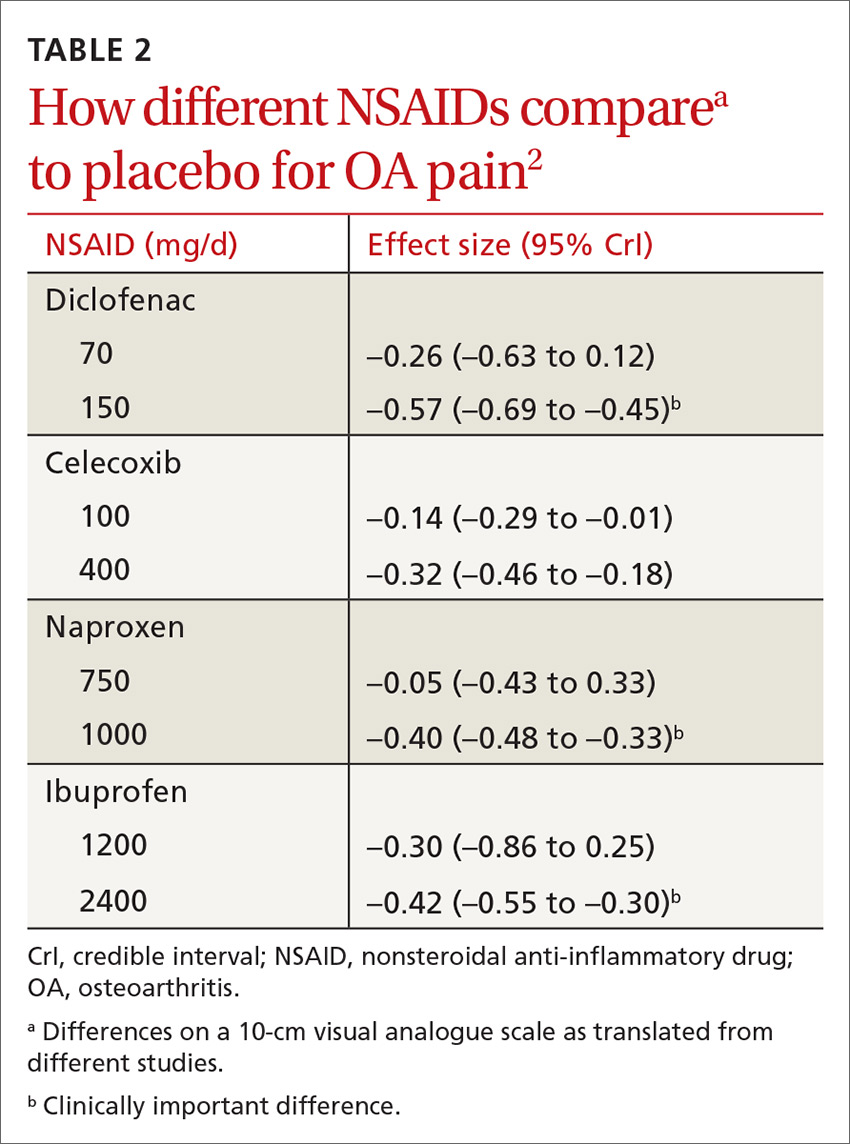
All NSAIDs at maximum clinical doses reduced large joint OA pain more effectively than placebo and acetaminophen based on data from a network meta-analysis of 129 RCTs with 32,129 patients (TABLE 1).1 When various doses of NSAIDs are ranked for efficacy based on their effect size compared to placebo, diclofenac 150 mg/d had the greatest treatment effect, followed by ibuprofen 2400 mg/d.2 Lower doses of NSAIDs—including diclofenac 70 mg/d, naproxen 750 mg/d, and ibuprofen 1200 mg/d—were not statistically superior to placebo (TABLE 2).2
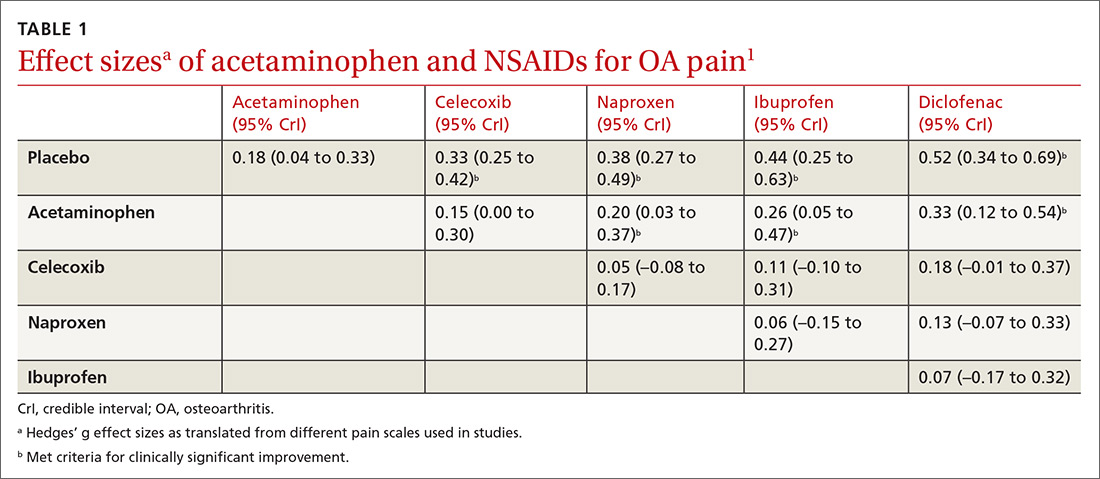
Selective vs nonselective. There was no statistical difference in pain relief between the selective COX-2 inhibitor celecoxib and the nonselective NSAIDs naproxen, diclofenac, and ibuprofen (TABLE 1).1
Meloxicam. A systematic review of 16 RCTs and 22,886 patients found that meloxicam reduced pain more effectively than placebo (10-point visual analogue scale [VAS] score pain difference of –6.8; 95% CI, –9.3 to –4.2) but was marginally less effective than other NSAIDs (VAS score pain difference of 1.7; 95% CI, 0.8 to 2.7).3
Acetaminophen. Data from 6 RCTs involving 2083 adults with knee OA indicate acetaminophen did not achieve clinical significance compared to placebo (TABLE 1).1 Another meta-analysis of 5 RCTs involving 1741 patients with hip or knee OA also demonstrated that acetaminophen failed to achieve a clinically significant effect on pain, defined as a reduction of 9 mm on a 0 to 100 mm VAS (–3.7; 95% CI, –5.5 to –1.9).4 Another network meta-analysis of 6 RCTs including 58,556 patients with knee or hip OA, with the primary outcome of pain (using a hierarchy of pain scores, with global pain score taking precedence) also found no clinically significant difference between acetaminophen at the highest dose (4000 mg/d) and placebo (–0.17; 95% credible interval [CrI], –0.27 to –0.6).2
RECOMMENDATIONS
In a systematic review of mixed evidence-based and expert opinion recommendations and guidelines on the management of OA, 10 of the 11 guidelines that included pharmacologic management recommended acetaminophen as a first-line agent, followed by topical NSAIDs, and then oral NSAIDs. The exception is the most recent American Academy of Orthopaedic Surgeons guideline, which continues to recommend NSAIDs but is now unable to recommend for or against acetaminophen.5
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet. 2017;390:e23-e33.
3. Chen YF, Jobanputra P, Barton P, et al. Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation. Health Technol Assess. 2008;12:1-278, iii.
4. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
5. Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43:701-712.
EVIDENCE SUMMARY
All NSAIDs at maximum clinical doses reduced large joint OA pain more effectively than placebo and acetaminophen based on data from a network meta-analysis of 129 RCTs with 32,129 patients (TABLE 1).1 When various doses of NSAIDs are ranked for efficacy based on their effect size compared to placebo, diclofenac 150 mg/d had the greatest treatment effect, followed by ibuprofen 2400 mg/d.2 Lower doses of NSAIDs—including diclofenac 70 mg/d, naproxen 750 mg/d, and ibuprofen 1200 mg/d—were not statistically superior to placebo (TABLE 2).2
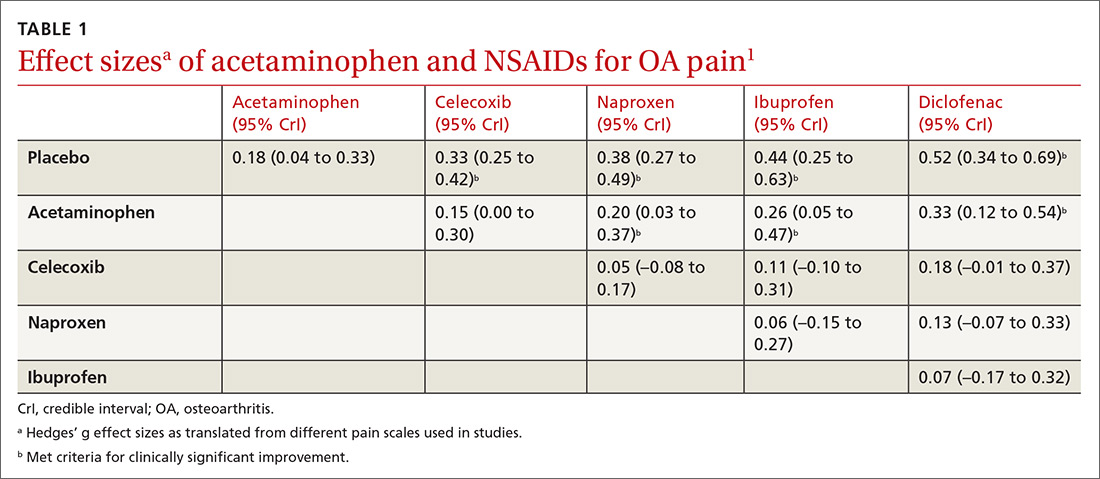
Selective vs nonselective. There was no statistical difference in pain relief between the selective COX-2 inhibitor celecoxib and the nonselective NSAIDs naproxen, diclofenac, and ibuprofen (TABLE 1).1
Meloxicam. A systematic review of 16 RCTs and 22,886 patients found that meloxicam reduced pain more effectively than placebo (10-point visual analogue scale [VAS] score pain difference of –6.8; 95% CI, –9.3 to –4.2) but was marginally less effective than other NSAIDs (VAS score pain difference of 1.7; 95% CI, 0.8 to 2.7).3
Acetaminophen. Data from 6 RCTs involving 2083 adults with knee OA indicate acetaminophen did not achieve clinical significance compared to placebo (TABLE 1).1 Another meta-analysis of 5 RCTs involving 1741 patients with hip or knee OA also demonstrated that acetaminophen failed to achieve a clinically significant effect on pain, defined as a reduction of 9 mm on a 0 to 100 mm VAS (–3.7; 95% CI, –5.5 to –1.9).4 Another network meta-analysis of 6 RCTs including 58,556 patients with knee or hip OA, with the primary outcome of pain (using a hierarchy of pain scores, with global pain score taking precedence) also found no clinically significant difference between acetaminophen at the highest dose (4000 mg/d) and placebo (–0.17; 95% credible interval [CrI], –0.27 to –0.6).2
RECOMMENDATIONS
In a systematic review of mixed evidence-based and expert opinion recommendations and guidelines on the management of OA, 10 of the 11 guidelines that included pharmacologic management recommended acetaminophen as a first-line agent, followed by topical NSAIDs, and then oral NSAIDs. The exception is the most recent American Academy of Orthopaedic Surgeons guideline, which continues to recommend NSAIDs but is now unable to recommend for or against acetaminophen.5
EVIDENCE SUMMARY
All NSAIDs at maximum clinical doses reduced large joint OA pain more effectively than placebo and acetaminophen based on data from a network meta-analysis of 129 RCTs with 32,129 patients (TABLE 1).1 When various doses of NSAIDs are ranked for efficacy based on their effect size compared to placebo, diclofenac 150 mg/d had the greatest treatment effect, followed by ibuprofen 2400 mg/d.2 Lower doses of NSAIDs—including diclofenac 70 mg/d, naproxen 750 mg/d, and ibuprofen 1200 mg/d—were not statistically superior to placebo (TABLE 2).2
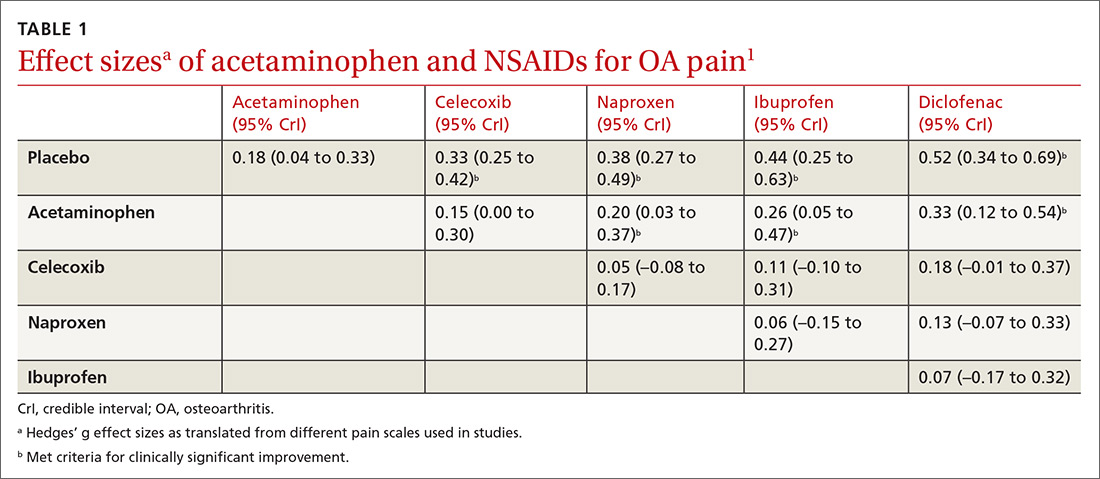
Selective vs nonselective. There was no statistical difference in pain relief between the selective COX-2 inhibitor celecoxib and the nonselective NSAIDs naproxen, diclofenac, and ibuprofen (TABLE 1).1
Meloxicam. A systematic review of 16 RCTs and 22,886 patients found that meloxicam reduced pain more effectively than placebo (10-point visual analogue scale [VAS] score pain difference of –6.8; 95% CI, –9.3 to –4.2) but was marginally less effective than other NSAIDs (VAS score pain difference of 1.7; 95% CI, 0.8 to 2.7).3
Acetaminophen. Data from 6 RCTs involving 2083 adults with knee OA indicate acetaminophen did not achieve clinical significance compared to placebo (TABLE 1).1 Another meta-analysis of 5 RCTs involving 1741 patients with hip or knee OA also demonstrated that acetaminophen failed to achieve a clinically significant effect on pain, defined as a reduction of 9 mm on a 0 to 100 mm VAS (–3.7; 95% CI, –5.5 to –1.9).4 Another network meta-analysis of 6 RCTs including 58,556 patients with knee or hip OA, with the primary outcome of pain (using a hierarchy of pain scores, with global pain score taking precedence) also found no clinically significant difference between acetaminophen at the highest dose (4000 mg/d) and placebo (–0.17; 95% credible interval [CrI], –0.27 to –0.6).2
RECOMMENDATIONS
In a systematic review of mixed evidence-based and expert opinion recommendations and guidelines on the management of OA, 10 of the 11 guidelines that included pharmacologic management recommended acetaminophen as a first-line agent, followed by topical NSAIDs, and then oral NSAIDs. The exception is the most recent American Academy of Orthopaedic Surgeons guideline, which continues to recommend NSAIDs but is now unable to recommend for or against acetaminophen.5
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet. 2017;390:e23-e33.
3. Chen YF, Jobanputra P, Barton P, et al. Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation. Health Technol Assess. 2008;12:1-278, iii.
4. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
5. Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43:701-712.
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet. 2017;390:e23-e33.
3. Chen YF, Jobanputra P, Barton P, et al. Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation. Health Technol Assess. 2008;12:1-278, iii.
4. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
5. Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43:701-712.
EVIDENCE-BASED ANSWER:
Nonsteroidal anti-inflammatory drugs (NSAIDs), when used at the maximum clinically effective dose, reduce osteoarthritis (OA) pain in large joints more effectively than either placebo or acetaminophen (strength of recommendation [SOR]: A, network meta-analysis of randomized controlled trials [RCTs]).
When ranked for efficacy, diclofenac 150 mg/d was the most effective (SOR: A, network meta-analysis of RCTs). The selective COX-2 inhibitors, such as celecoxib, are not more effective at reducing pain than the nonselective NSAIDs (SOR: A, meta-analysis of RCTs). Meloxicam is superior to placebo but marginally inferior to other NSAIDs (SOR: A, systematic review of RCTs).
Acetaminophen is no more effective than placebo (SOR: A, meta-analysis of RCTs).
How often does long-term PPI therapy cause clinically significant hypomagnesemia?
EVIDENCE SUMMARY
A systematic review and meta-analysis of observational studies examined the risk of hypomagnesemia, defined in various studies as serum magnesium levels of 1.6, 1.7, or 1.8 mg/dL.1 Two cohort studies, one case-control study, and 6 cross-sectional studies met inclusion criteria; 115,455 patients were enrolled. The studies were significantly heterogeneous (I2=89.1%), because of varying study designs, population sizes, and population characteristics.
PPI use increased the risk of hypomagnesemia (pooled odds ratio [OR]=1.5; 95% confidence interval [CI], 1.1-2.0) after adjustment for possible confounders such as use of diuretics.
Risk rises with long-term use, but severe hypomagnesemia is rare
Two more recent cohort studies produced conflicting results. Of 414 patients in a managed care cohort who received long-term PPIs, only 8 had mild hypomagnesemia (1.2-1.5 mg/dL) on nearly 14% of their combined 289 measurements. At final measurement, all patients had normal serum magnesium levels.2
A cross-sectional analysis of data from a retrospective cohort analysis of 9818 patients in the Netherlands found that any PPI use during the previous year was associated with an increased risk of hypomagnesemia (serum magnesium <1.73 mg/dL) compared with no use (adjusted OR=2; 95% CI, 1.4-2.9).3 The risk was greatest with use longer than 182 days (OR=3.0; 95% CI, 1.7-5.2). As with studies included in the meta-analysis, this study examined laboratory values exclusively. Only 3 of 724 PPI users had a serum magnesium level below 1.2 mg/dL, the point at which symptoms usually occur.
Case-control studies produce conflicting results
Two recent case-control studies also produced conflicting results. The first compared 154 outpatients who used PPIs for at least 6 months (mean, 27.5 months) with 84 nonusers.4 No association was found with hypomagnesemia (2.17 mg/dL vs 2.19 mg/dL), and none of the patients had a serum magnesium level below 1.7 mg/dL. The control group was poorly defined, however, and the study excluded patients taking diuretics.
Conversely, a study that compared 366 patients hospitalized with a primary or secondary diagnosis of hypomagnesemia (determined from an insurance claims database and defined as the presence of ICD-10 codes for hypomagnesemia or magnesium deficiency) with 1464 matched controls found that hospitalized patients with hypomagnesemia were more likely than controls to be current PPI users (adjusted OR=1.4; 95% CI, 1.1-1.9).5 Whether hypomagnesemia was the cause of the hospitalizations or an incidental finding wasn’t clear.
Concurrent use of diuretics and loop diuretics can increase risk
In a subgroup analysis of the second case-control study, PPI users who also used diuretics had an increased risk of hypomagnesemia (adjusted OR=1.7; 95% CI, 1.1-2.7) compared with patients who weren’t taking diuretics (adjusted OR=1.3; 95% CI, 0.8-1.9).5
Continue to: A comparison of the use of loop diuretics and...
A comparison of the use of loop diuretics and thiazides by patients taking PPIs found that concurrent use of loop diuretics increased serum magnesium reduction (−0.08 mg/dL; 95% CI, −0.14 to −0.02), but thiazides didn’t. Numbers were small: Of the 45 participants taking both a PPI and a loop diuretic, only 5 had hypomagnesemia (OR=7.2; 95% CI, 1.7-30.8).3
RECOMMENDATIONS
In 2011, the US Food and Drug Administration (FDA) warned of a possible increased risk of hypomagnesemia in patients taking PPIs long-term. The FDA advisory panel recommended evaluating serum magnesium before beginning long-term PPI therapy and in patients concurrently taking diuretics, digoxin, or other medications associated with hypomagnesemia.6
1. Park CH, Kim EH, Roh YH, et al. The association between the use of proton pump inhibitors and the risk of hypomagnesemia: a systematic review and meta-analysis. PLoS One. 2014;9:e112558.
2. Sharara AI, Chalhoub JM, Hammoud N, et al. Low prevalence of hypomagnesemia in long-term recipients of proton pump inhibitors in a managed care cohort. Clin Gastroenterol Hepatol. 2016;14:317-321.
3. Kieboom BC, Kiefte-de Jong JC, Eijgelsheim M, et al. Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study. Am J Kidney Dis. 2015;66:775-782.
4. Biyik M, Solak Y, Ucar R, et al. Hypomagnesemia among outpatient long-term proton pump inhibitor users. Am J Ther. 2014;24:e52-e55.
5. Zipursky J, Macdonald EM, Hollands S, et al. Proton pump inhibitors and hospitalization with hypomagnesemia: a population-based case-control study. PLoS Med. 2014;11:e1001736.
6. United States Food and Drug Administration. FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs). 03/02/2011. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm245011.htm. Accessed August 24, 2018.
EVIDENCE SUMMARY
A systematic review and meta-analysis of observational studies examined the risk of hypomagnesemia, defined in various studies as serum magnesium levels of 1.6, 1.7, or 1.8 mg/dL.1 Two cohort studies, one case-control study, and 6 cross-sectional studies met inclusion criteria; 115,455 patients were enrolled. The studies were significantly heterogeneous (I2=89.1%), because of varying study designs, population sizes, and population characteristics.
PPI use increased the risk of hypomagnesemia (pooled odds ratio [OR]=1.5; 95% confidence interval [CI], 1.1-2.0) after adjustment for possible confounders such as use of diuretics.
Risk rises with long-term use, but severe hypomagnesemia is rare
Two more recent cohort studies produced conflicting results. Of 414 patients in a managed care cohort who received long-term PPIs, only 8 had mild hypomagnesemia (1.2-1.5 mg/dL) on nearly 14% of their combined 289 measurements. At final measurement, all patients had normal serum magnesium levels.2
A cross-sectional analysis of data from a retrospective cohort analysis of 9818 patients in the Netherlands found that any PPI use during the previous year was associated with an increased risk of hypomagnesemia (serum magnesium <1.73 mg/dL) compared with no use (adjusted OR=2; 95% CI, 1.4-2.9).3 The risk was greatest with use longer than 182 days (OR=3.0; 95% CI, 1.7-5.2). As with studies included in the meta-analysis, this study examined laboratory values exclusively. Only 3 of 724 PPI users had a serum magnesium level below 1.2 mg/dL, the point at which symptoms usually occur.
Case-control studies produce conflicting results
Two recent case-control studies also produced conflicting results. The first compared 154 outpatients who used PPIs for at least 6 months (mean, 27.5 months) with 84 nonusers.4 No association was found with hypomagnesemia (2.17 mg/dL vs 2.19 mg/dL), and none of the patients had a serum magnesium level below 1.7 mg/dL. The control group was poorly defined, however, and the study excluded patients taking diuretics.
Conversely, a study that compared 366 patients hospitalized with a primary or secondary diagnosis of hypomagnesemia (determined from an insurance claims database and defined as the presence of ICD-10 codes for hypomagnesemia or magnesium deficiency) with 1464 matched controls found that hospitalized patients with hypomagnesemia were more likely than controls to be current PPI users (adjusted OR=1.4; 95% CI, 1.1-1.9).5 Whether hypomagnesemia was the cause of the hospitalizations or an incidental finding wasn’t clear.
Concurrent use of diuretics and loop diuretics can increase risk
In a subgroup analysis of the second case-control study, PPI users who also used diuretics had an increased risk of hypomagnesemia (adjusted OR=1.7; 95% CI, 1.1-2.7) compared with patients who weren’t taking diuretics (adjusted OR=1.3; 95% CI, 0.8-1.9).5
Continue to: A comparison of the use of loop diuretics and...
A comparison of the use of loop diuretics and thiazides by patients taking PPIs found that concurrent use of loop diuretics increased serum magnesium reduction (−0.08 mg/dL; 95% CI, −0.14 to −0.02), but thiazides didn’t. Numbers were small: Of the 45 participants taking both a PPI and a loop diuretic, only 5 had hypomagnesemia (OR=7.2; 95% CI, 1.7-30.8).3
RECOMMENDATIONS
In 2011, the US Food and Drug Administration (FDA) warned of a possible increased risk of hypomagnesemia in patients taking PPIs long-term. The FDA advisory panel recommended evaluating serum magnesium before beginning long-term PPI therapy and in patients concurrently taking diuretics, digoxin, or other medications associated with hypomagnesemia.6
EVIDENCE SUMMARY
A systematic review and meta-analysis of observational studies examined the risk of hypomagnesemia, defined in various studies as serum magnesium levels of 1.6, 1.7, or 1.8 mg/dL.1 Two cohort studies, one case-control study, and 6 cross-sectional studies met inclusion criteria; 115,455 patients were enrolled. The studies were significantly heterogeneous (I2=89.1%), because of varying study designs, population sizes, and population characteristics.
PPI use increased the risk of hypomagnesemia (pooled odds ratio [OR]=1.5; 95% confidence interval [CI], 1.1-2.0) after adjustment for possible confounders such as use of diuretics.
Risk rises with long-term use, but severe hypomagnesemia is rare
Two more recent cohort studies produced conflicting results. Of 414 patients in a managed care cohort who received long-term PPIs, only 8 had mild hypomagnesemia (1.2-1.5 mg/dL) on nearly 14% of their combined 289 measurements. At final measurement, all patients had normal serum magnesium levels.2
A cross-sectional analysis of data from a retrospective cohort analysis of 9818 patients in the Netherlands found that any PPI use during the previous year was associated with an increased risk of hypomagnesemia (serum magnesium <1.73 mg/dL) compared with no use (adjusted OR=2; 95% CI, 1.4-2.9).3 The risk was greatest with use longer than 182 days (OR=3.0; 95% CI, 1.7-5.2). As with studies included in the meta-analysis, this study examined laboratory values exclusively. Only 3 of 724 PPI users had a serum magnesium level below 1.2 mg/dL, the point at which symptoms usually occur.
Case-control studies produce conflicting results
Two recent case-control studies also produced conflicting results. The first compared 154 outpatients who used PPIs for at least 6 months (mean, 27.5 months) with 84 nonusers.4 No association was found with hypomagnesemia (2.17 mg/dL vs 2.19 mg/dL), and none of the patients had a serum magnesium level below 1.7 mg/dL. The control group was poorly defined, however, and the study excluded patients taking diuretics.
Conversely, a study that compared 366 patients hospitalized with a primary or secondary diagnosis of hypomagnesemia (determined from an insurance claims database and defined as the presence of ICD-10 codes for hypomagnesemia or magnesium deficiency) with 1464 matched controls found that hospitalized patients with hypomagnesemia were more likely than controls to be current PPI users (adjusted OR=1.4; 95% CI, 1.1-1.9).5 Whether hypomagnesemia was the cause of the hospitalizations or an incidental finding wasn’t clear.
Concurrent use of diuretics and loop diuretics can increase risk
In a subgroup analysis of the second case-control study, PPI users who also used diuretics had an increased risk of hypomagnesemia (adjusted OR=1.7; 95% CI, 1.1-2.7) compared with patients who weren’t taking diuretics (adjusted OR=1.3; 95% CI, 0.8-1.9).5
Continue to: A comparison of the use of loop diuretics and...
A comparison of the use of loop diuretics and thiazides by patients taking PPIs found that concurrent use of loop diuretics increased serum magnesium reduction (−0.08 mg/dL; 95% CI, −0.14 to −0.02), but thiazides didn’t. Numbers were small: Of the 45 participants taking both a PPI and a loop diuretic, only 5 had hypomagnesemia (OR=7.2; 95% CI, 1.7-30.8).3
RECOMMENDATIONS
In 2011, the US Food and Drug Administration (FDA) warned of a possible increased risk of hypomagnesemia in patients taking PPIs long-term. The FDA advisory panel recommended evaluating serum magnesium before beginning long-term PPI therapy and in patients concurrently taking diuretics, digoxin, or other medications associated with hypomagnesemia.6
1. Park CH, Kim EH, Roh YH, et al. The association between the use of proton pump inhibitors and the risk of hypomagnesemia: a systematic review and meta-analysis. PLoS One. 2014;9:e112558.
2. Sharara AI, Chalhoub JM, Hammoud N, et al. Low prevalence of hypomagnesemia in long-term recipients of proton pump inhibitors in a managed care cohort. Clin Gastroenterol Hepatol. 2016;14:317-321.
3. Kieboom BC, Kiefte-de Jong JC, Eijgelsheim M, et al. Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study. Am J Kidney Dis. 2015;66:775-782.
4. Biyik M, Solak Y, Ucar R, et al. Hypomagnesemia among outpatient long-term proton pump inhibitor users. Am J Ther. 2014;24:e52-e55.
5. Zipursky J, Macdonald EM, Hollands S, et al. Proton pump inhibitors and hospitalization with hypomagnesemia: a population-based case-control study. PLoS Med. 2014;11:e1001736.
6. United States Food and Drug Administration. FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs). 03/02/2011. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm245011.htm. Accessed August 24, 2018.
1. Park CH, Kim EH, Roh YH, et al. The association between the use of proton pump inhibitors and the risk of hypomagnesemia: a systematic review and meta-analysis. PLoS One. 2014;9:e112558.
2. Sharara AI, Chalhoub JM, Hammoud N, et al. Low prevalence of hypomagnesemia in long-term recipients of proton pump inhibitors in a managed care cohort. Clin Gastroenterol Hepatol. 2016;14:317-321.
3. Kieboom BC, Kiefte-de Jong JC, Eijgelsheim M, et al. Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study. Am J Kidney Dis. 2015;66:775-782.
4. Biyik M, Solak Y, Ucar R, et al. Hypomagnesemia among outpatient long-term proton pump inhibitor users. Am J Ther. 2014;24:e52-e55.
5. Zipursky J, Macdonald EM, Hollands S, et al. Proton pump inhibitors and hospitalization with hypomagnesemia: a population-based case-control study. PLoS Med. 2014;11:e1001736.
6. United States Food and Drug Administration. FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs). 03/02/2011. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm245011.htm. Accessed August 24, 2018.
EVIDENCE-BASED ANSWER:
Rarely. Proton pump inhibitors (PPIs) may be associated with decreases in serum magnesium laboratory values to below 1.6 to 1.8 mg/dL, especially when used concurrently with diuretics and loop diuretics (strength of recommendation [SOR]: C, disease-oriented outcomes based on cohort, case-control, and cross-sectional studies). Clinically significant or symptomatic hypomagnesemia (below 1.2 mg/dL) appears to be quite rare, however.
What are the benefits and risks of daily low-dose aspirin for primary prevention of CV events?
EVIDENCE SUMMARY
A 2013 systematic review of RCTs, systematic reviews, and meta-analyses examined the prophylactic use of low-dose aspirin for the primary prevention of cardiovascular disease (CVD) among adults 18 years and older.1 Twenty-seven papers met inclusion criteria; the total number of patients wasn’t reported.
A composite finding of nonfatal MI, nonfatal stroke, and CVD death indicated a number needed to treat (NNT) of 138 over 10 years of therapy (relative risk [RR]=0.90; 95% confidence interval [CI], 0.85-0.96). CVD death wasn’t disaggregated from this composite, but an analysis of all-cause mortality didn’t reach statistical significance (RR=0.94; 95% CI, 0.88-1.00). RR for nonfatal stroke alone also wasn’t disaggregated.
Risk of gastrointestinal (GI) bleeding was found to be a number needed to harm (NNH) of 108 over 10 years (RR=1.37; 95% CI, 1.15-1.62) whereas risk of hemorrhagic stroke didn’t reach statistical significance (RR=1.32; 95% CI, 1.00-1.74). This population-level review didn’t report disaggregated findings by age or baseline atherosclerotic cardiovascular disease (ASCVD) risk.
Another review finds benefit only for prevention of nonfatal MI
A 2016 systematic review included 2 good-quality and 9 fair-quality RCTs evaluating the benefits of low-dose aspirin compared with placebo or no treatment for primary prevention of CVD events in 118,445 patients ages 40 years and older.2 The review found benefit only for nonfatal MI, with an NNT of 126 over 10 years (RR=0.78; 95% CI, 0.71-0.87). There was no change in RR for nonfatal stroke (RR=0.95; 95% CI, 0.85-1.06); negligible impact on all-cause mortality (RR=0.95; 95% CI, 0.89-0.99); and no statistically significant benefit for CVD-specific mortality (RR=0.94; 95% CI, 0.86-1.03).
Aspirin carries risk of GI hemorrhage, but not hemorrhagic stroke
A companion 2016 systematic review of 16 RCTs, cohort studies, and meta-analyses evaluated the risk of serious bleeding in patients using low-dose aspirin for primary prevention of either CVD or cancer.3 The review (number of patients not reported) found that estimated excess bleeding events differed substantially depending on varying sources for baseline bleeding rates in aspirin nonusers.
The most conservative comparison yielded an NNH of 72 over 10 years of therapy (1.39 excess major GI bleeding events per 1000 person-years, 95% CI, 0.70-2.28). Comparison with other baseline bleeding rates in trial data yielded less risk of harm, with an NNH of 357 over 10 years (0.28 excess major GI bleeding events per 1000 person-years; 95% CI, 0.14-0.46). Excess risk for hemorrhagic stroke was not statistically significant (0.32 excess events per 1000 person-years; 95% CI, −0.05 to 0.82).
RECOMMENDATIONS
The US Preventive Services Task Force gives a Grade B recommendation (recommended, based on moderate to substantial benefit) to the use of aspirin to prevent CVD among adults ages 50 to 59 years with an ASCVD risk ≥10% who don’t have increased bleeding risk and are capable of 10 years of pharmacologic adherence with a similar expected longevity.4 The Task Force assigns a Grade C recommendation (individual and professional choice) to patients 60 to 69 years of age with the same constellation of risk factors and health status. Insufficient evidence was available to make recommendations for other age cohorts.
The American College of Chest Physicians recommends 75 to 100 mg of aspirin daily for adults 50 years or older who have moderate to high CV risk, defined as ≥10%.5
A working group of the European Society of Cardiology (ESC) released a statement in 2014 recommending aspirin for primary prevention in adults with a CV risk ≥20% and no risk factors for bleeding. For patients with a CVD risk between 10% and 20%, the ESC recommends deferring to patient preference.6
1. Sutcliffe P, Connock M, Gurung T, et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970.
2. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:804-813.
3. Whitlock EP, Burda BU, Williams SB, et al. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:826-835.
4. Bibbins-Domingo K, US Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836-845.
5. Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e637S-e668S.
6. Halvorsen S, Andreotti F, ten Berg JM, et al. Aspirin therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology Working Group on Thrombosis. J Am Coll Cardiol. 2014;64:319-327.
EVIDENCE SUMMARY
A 2013 systematic review of RCTs, systematic reviews, and meta-analyses examined the prophylactic use of low-dose aspirin for the primary prevention of cardiovascular disease (CVD) among adults 18 years and older.1 Twenty-seven papers met inclusion criteria; the total number of patients wasn’t reported.
A composite finding of nonfatal MI, nonfatal stroke, and CVD death indicated a number needed to treat (NNT) of 138 over 10 years of therapy (relative risk [RR]=0.90; 95% confidence interval [CI], 0.85-0.96). CVD death wasn’t disaggregated from this composite, but an analysis of all-cause mortality didn’t reach statistical significance (RR=0.94; 95% CI, 0.88-1.00). RR for nonfatal stroke alone also wasn’t disaggregated.
Risk of gastrointestinal (GI) bleeding was found to be a number needed to harm (NNH) of 108 over 10 years (RR=1.37; 95% CI, 1.15-1.62) whereas risk of hemorrhagic stroke didn’t reach statistical significance (RR=1.32; 95% CI, 1.00-1.74). This population-level review didn’t report disaggregated findings by age or baseline atherosclerotic cardiovascular disease (ASCVD) risk.
Another review finds benefit only for prevention of nonfatal MI
A 2016 systematic review included 2 good-quality and 9 fair-quality RCTs evaluating the benefits of low-dose aspirin compared with placebo or no treatment for primary prevention of CVD events in 118,445 patients ages 40 years and older.2 The review found benefit only for nonfatal MI, with an NNT of 126 over 10 years (RR=0.78; 95% CI, 0.71-0.87). There was no change in RR for nonfatal stroke (RR=0.95; 95% CI, 0.85-1.06); negligible impact on all-cause mortality (RR=0.95; 95% CI, 0.89-0.99); and no statistically significant benefit for CVD-specific mortality (RR=0.94; 95% CI, 0.86-1.03).
Aspirin carries risk of GI hemorrhage, but not hemorrhagic stroke
A companion 2016 systematic review of 16 RCTs, cohort studies, and meta-analyses evaluated the risk of serious bleeding in patients using low-dose aspirin for primary prevention of either CVD or cancer.3 The review (number of patients not reported) found that estimated excess bleeding events differed substantially depending on varying sources for baseline bleeding rates in aspirin nonusers.
The most conservative comparison yielded an NNH of 72 over 10 years of therapy (1.39 excess major GI bleeding events per 1000 person-years, 95% CI, 0.70-2.28). Comparison with other baseline bleeding rates in trial data yielded less risk of harm, with an NNH of 357 over 10 years (0.28 excess major GI bleeding events per 1000 person-years; 95% CI, 0.14-0.46). Excess risk for hemorrhagic stroke was not statistically significant (0.32 excess events per 1000 person-years; 95% CI, −0.05 to 0.82).
RECOMMENDATIONS
The US Preventive Services Task Force gives a Grade B recommendation (recommended, based on moderate to substantial benefit) to the use of aspirin to prevent CVD among adults ages 50 to 59 years with an ASCVD risk ≥10% who don’t have increased bleeding risk and are capable of 10 years of pharmacologic adherence with a similar expected longevity.4 The Task Force assigns a Grade C recommendation (individual and professional choice) to patients 60 to 69 years of age with the same constellation of risk factors and health status. Insufficient evidence was available to make recommendations for other age cohorts.
The American College of Chest Physicians recommends 75 to 100 mg of aspirin daily for adults 50 years or older who have moderate to high CV risk, defined as ≥10%.5
A working group of the European Society of Cardiology (ESC) released a statement in 2014 recommending aspirin for primary prevention in adults with a CV risk ≥20% and no risk factors for bleeding. For patients with a CVD risk between 10% and 20%, the ESC recommends deferring to patient preference.6
EVIDENCE SUMMARY
A 2013 systematic review of RCTs, systematic reviews, and meta-analyses examined the prophylactic use of low-dose aspirin for the primary prevention of cardiovascular disease (CVD) among adults 18 years and older.1 Twenty-seven papers met inclusion criteria; the total number of patients wasn’t reported.
A composite finding of nonfatal MI, nonfatal stroke, and CVD death indicated a number needed to treat (NNT) of 138 over 10 years of therapy (relative risk [RR]=0.90; 95% confidence interval [CI], 0.85-0.96). CVD death wasn’t disaggregated from this composite, but an analysis of all-cause mortality didn’t reach statistical significance (RR=0.94; 95% CI, 0.88-1.00). RR for nonfatal stroke alone also wasn’t disaggregated.
Risk of gastrointestinal (GI) bleeding was found to be a number needed to harm (NNH) of 108 over 10 years (RR=1.37; 95% CI, 1.15-1.62) whereas risk of hemorrhagic stroke didn’t reach statistical significance (RR=1.32; 95% CI, 1.00-1.74). This population-level review didn’t report disaggregated findings by age or baseline atherosclerotic cardiovascular disease (ASCVD) risk.
Another review finds benefit only for prevention of nonfatal MI
A 2016 systematic review included 2 good-quality and 9 fair-quality RCTs evaluating the benefits of low-dose aspirin compared with placebo or no treatment for primary prevention of CVD events in 118,445 patients ages 40 years and older.2 The review found benefit only for nonfatal MI, with an NNT of 126 over 10 years (RR=0.78; 95% CI, 0.71-0.87). There was no change in RR for nonfatal stroke (RR=0.95; 95% CI, 0.85-1.06); negligible impact on all-cause mortality (RR=0.95; 95% CI, 0.89-0.99); and no statistically significant benefit for CVD-specific mortality (RR=0.94; 95% CI, 0.86-1.03).
Aspirin carries risk of GI hemorrhage, but not hemorrhagic stroke
A companion 2016 systematic review of 16 RCTs, cohort studies, and meta-analyses evaluated the risk of serious bleeding in patients using low-dose aspirin for primary prevention of either CVD or cancer.3 The review (number of patients not reported) found that estimated excess bleeding events differed substantially depending on varying sources for baseline bleeding rates in aspirin nonusers.
The most conservative comparison yielded an NNH of 72 over 10 years of therapy (1.39 excess major GI bleeding events per 1000 person-years, 95% CI, 0.70-2.28). Comparison with other baseline bleeding rates in trial data yielded less risk of harm, with an NNH of 357 over 10 years (0.28 excess major GI bleeding events per 1000 person-years; 95% CI, 0.14-0.46). Excess risk for hemorrhagic stroke was not statistically significant (0.32 excess events per 1000 person-years; 95% CI, −0.05 to 0.82).
RECOMMENDATIONS
The US Preventive Services Task Force gives a Grade B recommendation (recommended, based on moderate to substantial benefit) to the use of aspirin to prevent CVD among adults ages 50 to 59 years with an ASCVD risk ≥10% who don’t have increased bleeding risk and are capable of 10 years of pharmacologic adherence with a similar expected longevity.4 The Task Force assigns a Grade C recommendation (individual and professional choice) to patients 60 to 69 years of age with the same constellation of risk factors and health status. Insufficient evidence was available to make recommendations for other age cohorts.
The American College of Chest Physicians recommends 75 to 100 mg of aspirin daily for adults 50 years or older who have moderate to high CV risk, defined as ≥10%.5
A working group of the European Society of Cardiology (ESC) released a statement in 2014 recommending aspirin for primary prevention in adults with a CV risk ≥20% and no risk factors for bleeding. For patients with a CVD risk between 10% and 20%, the ESC recommends deferring to patient preference.6
1. Sutcliffe P, Connock M, Gurung T, et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970.
2. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:804-813.
3. Whitlock EP, Burda BU, Williams SB, et al. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:826-835.
4. Bibbins-Domingo K, US Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836-845.
5. Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e637S-e668S.
6. Halvorsen S, Andreotti F, ten Berg JM, et al. Aspirin therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology Working Group on Thrombosis. J Am Coll Cardiol. 2014;64:319-327.
1. Sutcliffe P, Connock M, Gurung T, et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970.
2. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:804-813.
3. Whitlock EP, Burda BU, Williams SB, et al. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2016;164:826-835.
4. Bibbins-Domingo K, US Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836-845.
5. Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e637S-e668S.
6. Halvorsen S, Andreotti F, ten Berg JM, et al. Aspirin therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology Working Group on Thrombosis. J Am Coll Cardiol. 2014;64:319-327.
Evidence-based answers from the Family Physicians Inquiries Network
EVIDENCE BASED ANSWER:
One nonfatal myocardial infarction (MI) will be avoided for every 126 to 138 adults who take daily aspirin for 10 years (strength of recommendation [SOR]: A, systematic reviews and meta-analyses of multiple randomized controlled trials [RCTs]).
Taking low-dose aspirin for primary prevention shows no clear mortality benefit. A benefit for primary prevention of stroke is less certain. Although no evidence establishes increased risk of hemorrhagic stroke from daily low-dose aspirin, one gastrointestinal hemorrhage will occur for every 72 to 357 adults who take aspirin for longer than 10 years (SOR: A, systematic reviews and meta-analyses of multiple RCTs and cohort studies).
What is the best beta-blocker for systolic heart failure?
Three beta-blockers—carvedilol, metoprolol succinate, and bisoprolol—reduce mortality equally (by about 30% over one year) in patients with Class III or IV systolic heart failure. Insufficient evidence exists comparing equipotent doses of these medications head-to-head to recommend any one over the others (strength of recommendation [SOR]: A, systematic review/meta-analysis).
EVIDENCE SUMMARY
A 2013 network meta-analysis compared beta-blockers with placebo or standard treatment by analyzing 21 randomized trials with a total of 23,122 patients.1 Investigators found that beta-blockers as a class significantly reduced mortality after a median of 12 months (odds ratio=0.71, 95% confidence interval [CI], 0.64-0.80; number needed to treat [NNT]=23).
They also compared atenolol, bisoprolol, bucindolol, carvedilol, metoprolol, and nebivolol with each other and found no significant difference in risk of death, sudden cardiac death, death resulting from pump failure, or tolerability.
Three drugs are more effective and tolerable than others
A 2013 stratified subset meta-analysis used data from landmark randomized controlled trials (RCTs) that evaluated beta-blockers vs placebo in patients with systolic heart failure to compare metoprolol succinate (MERIT-HF) vs placebo with bisoprolol (CIBIS-II), carvedilol (COPERNICUS), and nebivolol (SENIORS-SHF) vs placebo (TABLE).2
Three of the drugs—bisoprolol, carvedilol, and metoprolol succinate—showed similar reductions relative to placebo in all-cause mortality, hospitalization for heart failure, and tolerability. Investigators concluded that the 3 drugs have comparable efficacy and tolerability, whereas nebivolol is less effective and tolerable.
Carvedilol vs beta-1-selective beta-blockers
Another 2013 meta-analysis of 8 RCTs with 4563 adult patients 18 years or older with systolic heart failure compared carvedilol with the beta-1-selective beta-blockers atenolol, bisoprolol, nebivolol, and metoprolol.3 Investigators found that carvedilol significantly reduced all-cause mortality (relative risk=0.85; 95% CI, 0.78-0.93; NNT=23) compared with beta-1-selective beta-blockers.
However, 4 trials (including COMET, N=3029) compared carvedilol with short-acting metoprolol tartrate, which may have skewed results in favor of carvedilol. Moreover, 2 trials comparing carvedilol with bisoprolol and 2 trials comparing carvedilol with nebivolol found no significant difference in all-cause mortality.3
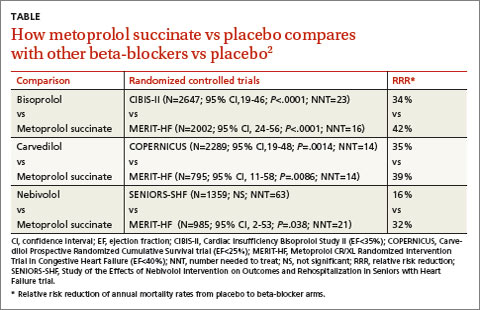
RECOMMENDATIONS
The 2010 Heart Failure Society of America Comprehensive Heart Failure Practice Guideline notes that the marked beneficial effects of beta blockade with carvedilol, bisoprolol, and controlled- or extended-release metoprolol have been well-demonstrated in large-scale clinical trials of symptomatic patients with Class II to IV heart failure and reduced left ventricular ejection fraction.4
The 2013 American College of Cardiology Foundation/American Heart Association heart failure guideline recommends the use of one of the 3 beta-blockers proven to reduce mortality (bisoprolol, carvedilol, or sustained-release metoprolol succinate) for all patients with current or previous symptoms of heart failure with reduced ejection fraction, unless contraindicated, to reduce morbidity and mortality.5
1. Chatterjee S, Biondi-Zoccai G, Abbate A, et al. Benefits of b blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ. 2013;346:f55.
2. Wikstrand J, Wedel H, Castagno D, et al. The large-scale placebo-controlled beta-blocker studies in systolic heart failure revisited: results from CIBIS-II, COPERNICUS and SENIORS-SHF compared with stratified subsets from MERIT-HF. J Intern Med. 2014;275:134-143.
3. DiNicolantonio JJ, Lavie CJ, Fares H, et al. Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol. 2013;111:765-769.
4. Heart Failure Society of America. Executive summary: HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Cardiac Failure. 2010;16:475-539.
5. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
Three beta-blockers—carvedilol, metoprolol succinate, and bisoprolol—reduce mortality equally (by about 30% over one year) in patients with Class III or IV systolic heart failure. Insufficient evidence exists comparing equipotent doses of these medications head-to-head to recommend any one over the others (strength of recommendation [SOR]: A, systematic review/meta-analysis).
EVIDENCE SUMMARY
A 2013 network meta-analysis compared beta-blockers with placebo or standard treatment by analyzing 21 randomized trials with a total of 23,122 patients.1 Investigators found that beta-blockers as a class significantly reduced mortality after a median of 12 months (odds ratio=0.71, 95% confidence interval [CI], 0.64-0.80; number needed to treat [NNT]=23).
They also compared atenolol, bisoprolol, bucindolol, carvedilol, metoprolol, and nebivolol with each other and found no significant difference in risk of death, sudden cardiac death, death resulting from pump failure, or tolerability.
Three drugs are more effective and tolerable than others
A 2013 stratified subset meta-analysis used data from landmark randomized controlled trials (RCTs) that evaluated beta-blockers vs placebo in patients with systolic heart failure to compare metoprolol succinate (MERIT-HF) vs placebo with bisoprolol (CIBIS-II), carvedilol (COPERNICUS), and nebivolol (SENIORS-SHF) vs placebo (TABLE).2
Three of the drugs—bisoprolol, carvedilol, and metoprolol succinate—showed similar reductions relative to placebo in all-cause mortality, hospitalization for heart failure, and tolerability. Investigators concluded that the 3 drugs have comparable efficacy and tolerability, whereas nebivolol is less effective and tolerable.
Carvedilol vs beta-1-selective beta-blockers
Another 2013 meta-analysis of 8 RCTs with 4563 adult patients 18 years or older with systolic heart failure compared carvedilol with the beta-1-selective beta-blockers atenolol, bisoprolol, nebivolol, and metoprolol.3 Investigators found that carvedilol significantly reduced all-cause mortality (relative risk=0.85; 95% CI, 0.78-0.93; NNT=23) compared with beta-1-selective beta-blockers.
However, 4 trials (including COMET, N=3029) compared carvedilol with short-acting metoprolol tartrate, which may have skewed results in favor of carvedilol. Moreover, 2 trials comparing carvedilol with bisoprolol and 2 trials comparing carvedilol with nebivolol found no significant difference in all-cause mortality.3
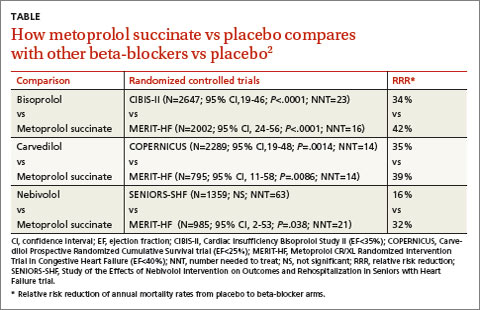
RECOMMENDATIONS
The 2010 Heart Failure Society of America Comprehensive Heart Failure Practice Guideline notes that the marked beneficial effects of beta blockade with carvedilol, bisoprolol, and controlled- or extended-release metoprolol have been well-demonstrated in large-scale clinical trials of symptomatic patients with Class II to IV heart failure and reduced left ventricular ejection fraction.4
The 2013 American College of Cardiology Foundation/American Heart Association heart failure guideline recommends the use of one of the 3 beta-blockers proven to reduce mortality (bisoprolol, carvedilol, or sustained-release metoprolol succinate) for all patients with current or previous symptoms of heart failure with reduced ejection fraction, unless contraindicated, to reduce morbidity and mortality.5
Three beta-blockers—carvedilol, metoprolol succinate, and bisoprolol—reduce mortality equally (by about 30% over one year) in patients with Class III or IV systolic heart failure. Insufficient evidence exists comparing equipotent doses of these medications head-to-head to recommend any one over the others (strength of recommendation [SOR]: A, systematic review/meta-analysis).
EVIDENCE SUMMARY
A 2013 network meta-analysis compared beta-blockers with placebo or standard treatment by analyzing 21 randomized trials with a total of 23,122 patients.1 Investigators found that beta-blockers as a class significantly reduced mortality after a median of 12 months (odds ratio=0.71, 95% confidence interval [CI], 0.64-0.80; number needed to treat [NNT]=23).
They also compared atenolol, bisoprolol, bucindolol, carvedilol, metoprolol, and nebivolol with each other and found no significant difference in risk of death, sudden cardiac death, death resulting from pump failure, or tolerability.
Three drugs are more effective and tolerable than others
A 2013 stratified subset meta-analysis used data from landmark randomized controlled trials (RCTs) that evaluated beta-blockers vs placebo in patients with systolic heart failure to compare metoprolol succinate (MERIT-HF) vs placebo with bisoprolol (CIBIS-II), carvedilol (COPERNICUS), and nebivolol (SENIORS-SHF) vs placebo (TABLE).2
Three of the drugs—bisoprolol, carvedilol, and metoprolol succinate—showed similar reductions relative to placebo in all-cause mortality, hospitalization for heart failure, and tolerability. Investigators concluded that the 3 drugs have comparable efficacy and tolerability, whereas nebivolol is less effective and tolerable.
Carvedilol vs beta-1-selective beta-blockers
Another 2013 meta-analysis of 8 RCTs with 4563 adult patients 18 years or older with systolic heart failure compared carvedilol with the beta-1-selective beta-blockers atenolol, bisoprolol, nebivolol, and metoprolol.3 Investigators found that carvedilol significantly reduced all-cause mortality (relative risk=0.85; 95% CI, 0.78-0.93; NNT=23) compared with beta-1-selective beta-blockers.
However, 4 trials (including COMET, N=3029) compared carvedilol with short-acting metoprolol tartrate, which may have skewed results in favor of carvedilol. Moreover, 2 trials comparing carvedilol with bisoprolol and 2 trials comparing carvedilol with nebivolol found no significant difference in all-cause mortality.3
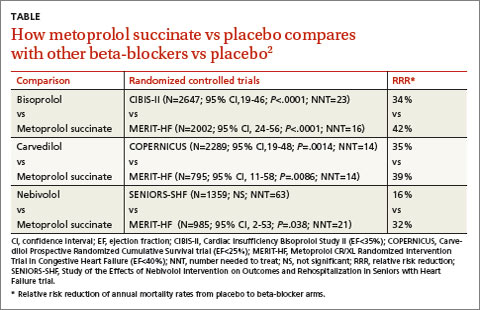
RECOMMENDATIONS
The 2010 Heart Failure Society of America Comprehensive Heart Failure Practice Guideline notes that the marked beneficial effects of beta blockade with carvedilol, bisoprolol, and controlled- or extended-release metoprolol have been well-demonstrated in large-scale clinical trials of symptomatic patients with Class II to IV heart failure and reduced left ventricular ejection fraction.4
The 2013 American College of Cardiology Foundation/American Heart Association heart failure guideline recommends the use of one of the 3 beta-blockers proven to reduce mortality (bisoprolol, carvedilol, or sustained-release metoprolol succinate) for all patients with current or previous symptoms of heart failure with reduced ejection fraction, unless contraindicated, to reduce morbidity and mortality.5
1. Chatterjee S, Biondi-Zoccai G, Abbate A, et al. Benefits of b blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ. 2013;346:f55.
2. Wikstrand J, Wedel H, Castagno D, et al. The large-scale placebo-controlled beta-blocker studies in systolic heart failure revisited: results from CIBIS-II, COPERNICUS and SENIORS-SHF compared with stratified subsets from MERIT-HF. J Intern Med. 2014;275:134-143.
3. DiNicolantonio JJ, Lavie CJ, Fares H, et al. Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol. 2013;111:765-769.
4. Heart Failure Society of America. Executive summary: HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Cardiac Failure. 2010;16:475-539.
5. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
1. Chatterjee S, Biondi-Zoccai G, Abbate A, et al. Benefits of b blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ. 2013;346:f55.
2. Wikstrand J, Wedel H, Castagno D, et al. The large-scale placebo-controlled beta-blocker studies in systolic heart failure revisited: results from CIBIS-II, COPERNICUS and SENIORS-SHF compared with stratified subsets from MERIT-HF. J Intern Med. 2014;275:134-143.
3. DiNicolantonio JJ, Lavie CJ, Fares H, et al. Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol. 2013;111:765-769.
4. Heart Failure Society of America. Executive summary: HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Cardiac Failure. 2010;16:475-539.
5. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
Evidence-based answers from the Family Physicians Inquiries Network
Can calcium supplements cause serious adverse effects in healthy people?
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
Yes, according to studies with some limitations. Calcium supplements with or without vitamin D increase the risk of myocardial infarction (MI), with numbers needed to harm (NNH) over 5 years of 69 to 240 (strength of recommendation [SOR]: B, meta-analyses of randomized controlled trials [RCTs] that evaluated a predominantly older female population and were limited by study designs).
Calcium supplements with or without vitamin D may increase the risk of stroke, with an NNH over 5 years of 283 (SOR: B, meta-analyses of RCTs).
Calcium supplementation, but not a diet rich in calcium, also increases the risk of renal calculi, with an NNH over 7 years of 272 (SOR: B, RCT and a cohort study, which also evaluated a predominantly older female population).
Evidence summary
A meta-analysis of 11 randomized, double-blinded placebo-controlled studies assessed the relationship between calcium supplements and the risk of cardiovascular events.1 A total of 20,071 predominantly female patients (83%) with a mean age of 72 years (range, 51-77 years) received ≥500 mg elemental calcium per day for at least 1 year. Median follow-up was 3.6 to 4 years. Five studies provided individual patient data and all 11 provided trial-level data.
In the 5 studies contributing patient data, women taking calcium supplements had an increased incidence of MI (hazard ratio [HR]=1.31; 95% confidence interval [CI], 1.02-1.67; P=.035) with an NNH of 69 over 5 years of calcium supplementation. The trial-level data, from 11 trials with 11,921 patients, also showed an increased incidence of MI in women taking calcium (relative risk [RR]=1.27; 95% CI, 1.01-1.59; P=.038). Neither the patient data nor the trial-level data demonstrated a significant increase in strokes.
Limitations of this meta-analysis include the fact that none of the trials was designed to address the risk of cardiovascular disease; in addition, some studies assessed outcomes by patient self-report, raising the possibility of information bias.
Some studies also show an increased stroke risk
The Women’s Health Initiative (WHI) study initially reported no increase in cardiovascular risk among women who received calcium and vitamin D supplements, but it didn’t take into account whether women were already taking calcium or vitamin D at the time of randomization.2 Re-analysis of the 16,718 women (mean age 62.9 years) randomized to calcium and vitamin D and not taking calcium supplements before the study found a statistically significant increase in the risk of MI or revascularization (HR=1.16; 95% CI, 1.01-1.34; P=.04).3
A meta-analysis of these findings and 2 additional RCTs (88% of subjects were female) comparing calcium and vitamin D supplementation with placebo found an increased risk of MI or stroke (RR=1.16; 95% CI, 1.02-1.32; P=.02).
Another meta-analysis that examined the WHI data and 5 placebo-controlled studies of calcium or calcium and vitamin D supplementation (82% of subjects were female) found an increased risk of MI, with NNHs over 5 years of 240 for MI (RR=1.26; 95% CI, 1.07-1.47; P=.005), 283 for stroke (RR=1.19; 95% CI, 1.02-1.39; P=.03), and 178 for the composite of MI or stroke (RR=1.17; 95% CI, 1.05-1.31; P=.005).3 The number needed to treat with calcium (with or without vitamin D) for 5 years to prevent one fracture was 302. The conclusions of this study were limited by post hoc and subgroup analyses.4
These studies did not address dietary sources rich in calcium. Dietary calcium results in lower peak serum levels than supplementary calcium, with less potential for adverse effects.3
Supplemental, but not dietary, calcium raises the risk of kidney stones
To assess the risk of renal calculi, the WHI randomized 36,282 postmenopausal women to calcium with vitamin D or placebo. Calcium and vitamin D increased the risk of renal calculi (HR=1.17; 95% CI, 1.02-1.34), with an NNH of 272 over 7 years.5
In a prospective cohort study of 91,731 women with 12-year follow-up, supplementary calcium was associated with an increased risk of kidney stone formation (RR=1.2; 95% CI, 1.02-1.41), whereas high dietary calcium was linked to a lower risk.6
Recommendations
The Institute of Medicine’s (IOM’s) recommended dietary allowance for calcium from diet plus supplements is 1000 mg a day for women until 50 years of age and no more than 1200 mg a day for women older than 50 years. The IOM advocates a maximum calcium intake of 2000 mg a day for women in both age groups because of the increased risk of kidney stones.7
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
1. Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.-
2. Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854.
3. Bolland M, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.-
4. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011;342:d2080.-
5. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669-683.
6. Curhan GC, Willett WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497-504.
7. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Report brief, November 2010. Washington, DC: Institute of Medicine; 2001. Available at: www.iom.edu/~/ media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20 Calcium%202010%20Report%20Brief.pdf. Access September 14, 2012.
Evidence-based answers from the Family Physicians Inquiries Network
Does surgery relieve the pain of a herniated disc?
YES, in the short term. Patients with an acute episode of low back pain, radicular symptoms, and evidence of a herniated disc on imaging may experience short-term pain relief from discectomy if their symptoms haven’t improved after initial conservative therapy (strength of recommendation [SOR]: A, multiple randomized, controlled trials [RCTs]).
Although surgery may enhance pain relief initially, no evidence supports a long-term benefit for surgery over conservative management (SOR: A, multiple RCTs).
Evidence summary
Disc herniation is defined as any protrusion of the disc nucleus, cartilage, or other associated tissues from the normal disc space. Lumbar disc herniations (LDHs) are most likely to occur in the L4 to L5 and L5 to S1 levels, causing low back pain and sciatica. Many LDHs occur without symptoms, however, so it’s important to correlate level and side of herniation before assuming causality. Expert opinion recommends early surgical intervention for patients with cauda equina syndrome or progressive neurologic deficits.1
Surgery provides short-term gains
A search identified 4 RCTs that compared surgical intervention with conservative management. The first, published in 1983, evaluated 126 patients with radicular pain and confirmed LDH who did not improve after 2 weeks of conservative therapy. The study assigned patients to either open discectomy or back school.2 Patients rated their results as good, fair, poor, or bad; a good or fair rating was considered a positive outcome.
At 1 year, significantly more patients in the surgery group reported positive results (P<.001), based on working capacity, neurological deficits, pain, and lumbar spine mobility. At 4 years, no significant difference was found between the groups.
The study showed significant crossover, with 26% of conservatively managed patients receiving surgery within the first year. Evaluators weren’t blinded, and outcome measurements weren’t based on standardized evaluation tools.
Crossover complicates comparison of relative treatment effects
The Spine Patient Outcomes Research Trial (SPORT), published in 2006, compared 501 patients with confirmed LDH and persistent symptoms after 6 weeks.3 Patients were randomized to open discectomy or nonoperative “usual care.” Both groups showed improvement in pain scores and no significant differences in standardized pain scales at 3 months, 1 year, or 2 years.
Crossover for the study was high: 40% of the surgical group didn’t have surgery, and 45% of the nonoperative group underwent surgery. Although the pattern of care in the SPORT study resembles common clinical situations,4 the high degree of crossover makes it difficult to draw inferences about relative treatment effects.5
Greater patient satisfaction with surgery
Another RCT followed 56 patients with confirmed LDH and symptoms for 6 to 12 weeks.6 Patients were randomized to receive microdiscectomy within 2 weeks of randomization or nonoperative care. Outcomes were based on standardized pain scales for leg and back pain. The surgical group had significantly better leg pain relief (P<.01) at the 6-week evaluation. At 12 weeks, neither back pain nor leg pain differed between the groups.
Although pain didn’t differ significantly, patients in the surgical group were more satisfied with their care, and physicians were more likely to believe that surgery would improve outcomes. Crossover from the nonoperative group was high, with 39% of that group undergoing surgery.
Surgery improves leg pain, not disability, more than conservative therapy
Another RCT also directly compared microdiscectomy to conservative treatment in 283 patients with confirmed LDH and symptoms lasting 6 to 12 weeks.7 The surgical group underwent microdiscectomy within 2 weeks of randomization. Pain and disability measurements, based on standardized scales, showed significant improvement in leg pain (P<.001) for the surgical group, but no significant difference in disability.
Patient perception of recovery on a Likert-type scale showed a median recovery time of 4 weeks for the surgical group and 12 weeks for the conservative therapy group. No significant differences in perceived degree of recovery were noted between the groups at 1 year; 95% of participants had a satisfactory recovery.
Again, significant crossover occurred: 11% of patients allocated to surgery recovered before surgery, and 39% of the conservative therapy group experienced worsening symptoms or intractable pain that led them to undergo microdiscectomy.
Open discectomy, microdiscectomy produce similar results
A Cochrane review of interventions for LDH included only the Weber2 and SPORT3 RCTs. The review also included 3 RCTs that compared open discectomy and microdiscectomy. These studies found no difference in pain relief or complications between the 2 interventions.8
Recommendations
The Institute for Clinical Systems Improvement guidelines for adult low back pain list cauda equina, progressive neurologic deficits, or uncontrolled pain as reasons for direct referral to a spine specialist.1 Patients can be treated conservatively for 6 weeks without imaging, unless other symptoms or concerns are present.
The guidelines recommend that patients with chronic sciatica (lasting >6 weeks) receive further imaging or referral to a specialist if the patient is a potential candidate for surgery.
1. Institute for Clinical Systems Improvement. Health Care Guideline: Adult Low Back Pain. 13th ed. Bloomington, Minn: Institute for Clinical Systems Improvement; 2008. Available at: www.icsi.org/low_back_pain/adult_low_back_pain__8.html. Accessed December 11, 2009.
2. Weber H. Lumbar disc herniation. a controlled, prospective study with 10 years of observation. Spine. 1983;8:131-140.
3. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450.
4. Angevine PD McCormick PC Inference and validity in the SPORT herniated lumbar disc randomized clinical trial. Spine J. 2007;7:387-391.
5. Mirza SK, Goodkin R. What patients know. Surg Neurol. 2008;70:5-7.
6. Osterman H, Seitsalo S, Karpinen J, et al. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine. 2006;21:2409-2414.
7. Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment in sciatica. N Engl J Med. 2007;356:2245-2256.
8. Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev. 2007;(2):CD001350.-
YES, in the short term. Patients with an acute episode of low back pain, radicular symptoms, and evidence of a herniated disc on imaging may experience short-term pain relief from discectomy if their symptoms haven’t improved after initial conservative therapy (strength of recommendation [SOR]: A, multiple randomized, controlled trials [RCTs]).
Although surgery may enhance pain relief initially, no evidence supports a long-term benefit for surgery over conservative management (SOR: A, multiple RCTs).
Evidence summary
Disc herniation is defined as any protrusion of the disc nucleus, cartilage, or other associated tissues from the normal disc space. Lumbar disc herniations (LDHs) are most likely to occur in the L4 to L5 and L5 to S1 levels, causing low back pain and sciatica. Many LDHs occur without symptoms, however, so it’s important to correlate level and side of herniation before assuming causality. Expert opinion recommends early surgical intervention for patients with cauda equina syndrome or progressive neurologic deficits.1
Surgery provides short-term gains
A search identified 4 RCTs that compared surgical intervention with conservative management. The first, published in 1983, evaluated 126 patients with radicular pain and confirmed LDH who did not improve after 2 weeks of conservative therapy. The study assigned patients to either open discectomy or back school.2 Patients rated their results as good, fair, poor, or bad; a good or fair rating was considered a positive outcome.
At 1 year, significantly more patients in the surgery group reported positive results (P<.001), based on working capacity, neurological deficits, pain, and lumbar spine mobility. At 4 years, no significant difference was found between the groups.
The study showed significant crossover, with 26% of conservatively managed patients receiving surgery within the first year. Evaluators weren’t blinded, and outcome measurements weren’t based on standardized evaluation tools.
Crossover complicates comparison of relative treatment effects
The Spine Patient Outcomes Research Trial (SPORT), published in 2006, compared 501 patients with confirmed LDH and persistent symptoms after 6 weeks.3 Patients were randomized to open discectomy or nonoperative “usual care.” Both groups showed improvement in pain scores and no significant differences in standardized pain scales at 3 months, 1 year, or 2 years.
Crossover for the study was high: 40% of the surgical group didn’t have surgery, and 45% of the nonoperative group underwent surgery. Although the pattern of care in the SPORT study resembles common clinical situations,4 the high degree of crossover makes it difficult to draw inferences about relative treatment effects.5
Greater patient satisfaction with surgery
Another RCT followed 56 patients with confirmed LDH and symptoms for 6 to 12 weeks.6 Patients were randomized to receive microdiscectomy within 2 weeks of randomization or nonoperative care. Outcomes were based on standardized pain scales for leg and back pain. The surgical group had significantly better leg pain relief (P<.01) at the 6-week evaluation. At 12 weeks, neither back pain nor leg pain differed between the groups.
Although pain didn’t differ significantly, patients in the surgical group were more satisfied with their care, and physicians were more likely to believe that surgery would improve outcomes. Crossover from the nonoperative group was high, with 39% of that group undergoing surgery.
Surgery improves leg pain, not disability, more than conservative therapy
Another RCT also directly compared microdiscectomy to conservative treatment in 283 patients with confirmed LDH and symptoms lasting 6 to 12 weeks.7 The surgical group underwent microdiscectomy within 2 weeks of randomization. Pain and disability measurements, based on standardized scales, showed significant improvement in leg pain (P<.001) for the surgical group, but no significant difference in disability.
Patient perception of recovery on a Likert-type scale showed a median recovery time of 4 weeks for the surgical group and 12 weeks for the conservative therapy group. No significant differences in perceived degree of recovery were noted between the groups at 1 year; 95% of participants had a satisfactory recovery.
Again, significant crossover occurred: 11% of patients allocated to surgery recovered before surgery, and 39% of the conservative therapy group experienced worsening symptoms or intractable pain that led them to undergo microdiscectomy.
Open discectomy, microdiscectomy produce similar results
A Cochrane review of interventions for LDH included only the Weber2 and SPORT3 RCTs. The review also included 3 RCTs that compared open discectomy and microdiscectomy. These studies found no difference in pain relief or complications between the 2 interventions.8
Recommendations
The Institute for Clinical Systems Improvement guidelines for adult low back pain list cauda equina, progressive neurologic deficits, or uncontrolled pain as reasons for direct referral to a spine specialist.1 Patients can be treated conservatively for 6 weeks without imaging, unless other symptoms or concerns are present.
The guidelines recommend that patients with chronic sciatica (lasting >6 weeks) receive further imaging or referral to a specialist if the patient is a potential candidate for surgery.
YES, in the short term. Patients with an acute episode of low back pain, radicular symptoms, and evidence of a herniated disc on imaging may experience short-term pain relief from discectomy if their symptoms haven’t improved after initial conservative therapy (strength of recommendation [SOR]: A, multiple randomized, controlled trials [RCTs]).
Although surgery may enhance pain relief initially, no evidence supports a long-term benefit for surgery over conservative management (SOR: A, multiple RCTs).
Evidence summary
Disc herniation is defined as any protrusion of the disc nucleus, cartilage, or other associated tissues from the normal disc space. Lumbar disc herniations (LDHs) are most likely to occur in the L4 to L5 and L5 to S1 levels, causing low back pain and sciatica. Many LDHs occur without symptoms, however, so it’s important to correlate level and side of herniation before assuming causality. Expert opinion recommends early surgical intervention for patients with cauda equina syndrome or progressive neurologic deficits.1
Surgery provides short-term gains
A search identified 4 RCTs that compared surgical intervention with conservative management. The first, published in 1983, evaluated 126 patients with radicular pain and confirmed LDH who did not improve after 2 weeks of conservative therapy. The study assigned patients to either open discectomy or back school.2 Patients rated their results as good, fair, poor, or bad; a good or fair rating was considered a positive outcome.
At 1 year, significantly more patients in the surgery group reported positive results (P<.001), based on working capacity, neurological deficits, pain, and lumbar spine mobility. At 4 years, no significant difference was found between the groups.
The study showed significant crossover, with 26% of conservatively managed patients receiving surgery within the first year. Evaluators weren’t blinded, and outcome measurements weren’t based on standardized evaluation tools.
Crossover complicates comparison of relative treatment effects
The Spine Patient Outcomes Research Trial (SPORT), published in 2006, compared 501 patients with confirmed LDH and persistent symptoms after 6 weeks.3 Patients were randomized to open discectomy or nonoperative “usual care.” Both groups showed improvement in pain scores and no significant differences in standardized pain scales at 3 months, 1 year, or 2 years.
Crossover for the study was high: 40% of the surgical group didn’t have surgery, and 45% of the nonoperative group underwent surgery. Although the pattern of care in the SPORT study resembles common clinical situations,4 the high degree of crossover makes it difficult to draw inferences about relative treatment effects.5
Greater patient satisfaction with surgery
Another RCT followed 56 patients with confirmed LDH and symptoms for 6 to 12 weeks.6 Patients were randomized to receive microdiscectomy within 2 weeks of randomization or nonoperative care. Outcomes were based on standardized pain scales for leg and back pain. The surgical group had significantly better leg pain relief (P<.01) at the 6-week evaluation. At 12 weeks, neither back pain nor leg pain differed between the groups.
Although pain didn’t differ significantly, patients in the surgical group were more satisfied with their care, and physicians were more likely to believe that surgery would improve outcomes. Crossover from the nonoperative group was high, with 39% of that group undergoing surgery.
Surgery improves leg pain, not disability, more than conservative therapy
Another RCT also directly compared microdiscectomy to conservative treatment in 283 patients with confirmed LDH and symptoms lasting 6 to 12 weeks.7 The surgical group underwent microdiscectomy within 2 weeks of randomization. Pain and disability measurements, based on standardized scales, showed significant improvement in leg pain (P<.001) for the surgical group, but no significant difference in disability.
Patient perception of recovery on a Likert-type scale showed a median recovery time of 4 weeks for the surgical group and 12 weeks for the conservative therapy group. No significant differences in perceived degree of recovery were noted between the groups at 1 year; 95% of participants had a satisfactory recovery.
Again, significant crossover occurred: 11% of patients allocated to surgery recovered before surgery, and 39% of the conservative therapy group experienced worsening symptoms or intractable pain that led them to undergo microdiscectomy.
Open discectomy, microdiscectomy produce similar results
A Cochrane review of interventions for LDH included only the Weber2 and SPORT3 RCTs. The review also included 3 RCTs that compared open discectomy and microdiscectomy. These studies found no difference in pain relief or complications between the 2 interventions.8
Recommendations
The Institute for Clinical Systems Improvement guidelines for adult low back pain list cauda equina, progressive neurologic deficits, or uncontrolled pain as reasons for direct referral to a spine specialist.1 Patients can be treated conservatively for 6 weeks without imaging, unless other symptoms or concerns are present.
The guidelines recommend that patients with chronic sciatica (lasting >6 weeks) receive further imaging or referral to a specialist if the patient is a potential candidate for surgery.
1. Institute for Clinical Systems Improvement. Health Care Guideline: Adult Low Back Pain. 13th ed. Bloomington, Minn: Institute for Clinical Systems Improvement; 2008. Available at: www.icsi.org/low_back_pain/adult_low_back_pain__8.html. Accessed December 11, 2009.
2. Weber H. Lumbar disc herniation. a controlled, prospective study with 10 years of observation. Spine. 1983;8:131-140.
3. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450.
4. Angevine PD McCormick PC Inference and validity in the SPORT herniated lumbar disc randomized clinical trial. Spine J. 2007;7:387-391.
5. Mirza SK, Goodkin R. What patients know. Surg Neurol. 2008;70:5-7.
6. Osterman H, Seitsalo S, Karpinen J, et al. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine. 2006;21:2409-2414.
7. Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment in sciatica. N Engl J Med. 2007;356:2245-2256.
8. Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev. 2007;(2):CD001350.-
1. Institute for Clinical Systems Improvement. Health Care Guideline: Adult Low Back Pain. 13th ed. Bloomington, Minn: Institute for Clinical Systems Improvement; 2008. Available at: www.icsi.org/low_back_pain/adult_low_back_pain__8.html. Accessed December 11, 2009.
2. Weber H. Lumbar disc herniation. a controlled, prospective study with 10 years of observation. Spine. 1983;8:131-140.
3. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450.
4. Angevine PD McCormick PC Inference and validity in the SPORT herniated lumbar disc randomized clinical trial. Spine J. 2007;7:387-391.
5. Mirza SK, Goodkin R. What patients know. Surg Neurol. 2008;70:5-7.
6. Osterman H, Seitsalo S, Karpinen J, et al. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine. 2006;21:2409-2414.
7. Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment in sciatica. N Engl J Med. 2007;356:2245-2256.
8. Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev. 2007;(2):CD001350.-
Evidence-based answers from the Family Physicians Inquiries Network
Should you evaluate for CAD in seniors with premature ventricular contractions?
Yes. Current guidelines suggest evaluating patients with premature ventricular contractions (PVCs) and associated risk factors for underlying coronary artery disease (strength of recommendation [SOR]: C, expert opinion).
Frequent PVCs are associated with acute myocardial infarction and sudden death in patients without known coronary artery disease (CAD). They are linked to increased mortality from all causes in elderly patients with a history of CAD, left ventricular dysfunction, hypertension, or valvular heart disease. Frequent PVCs during recovery from exercise stress testing are also associated with increased mortality.
There is strong evidence against suppressing PVCs with antiarrhythmics (SOR: A, randomized controlled trials [RCTs]).
Stress preventive measures
Jennifer Lochner, MD
Oregon Health and Sciences University, Portland
I find myself discussing PVCs most often with young women who don’t have known heart disease—rather than the elderly. I often discover PVCs on physical examination in the office or see them on a Holter monitor ordered to rule out other more worrisome arrhythmias.
This reminds me that I need to not only consider the issue of treatment aimed at suppressing PVCs (not helpful except when the patient has significant symptoms), but also to consider whether the patient has risk factors for CAD.
In future discussions with patients about PVCs, I plan to shift the focus to measures to prevent CAD—specifically tobacco cessation, weight management, daily physical activity, and a healthy diet.
Evidence summary
A consistent definition of frequent PVCs doesn’t exist in the literature. Some studies have found a significant risk of death or acute myocardial infarction associated with >30 PVCs per hour.1,2 The 2006 American College of Cardiology/American Heart Association/European Society of Cardiology guideline defines frequent PVCs as >10 per hour.3
Despite the association between frequent PVCs and increased risk of death and cardiac events, our review didn’t find studies that indicate the utility of evaluation strategies for higher-risk patients.
Frequent PVCs predict increased mortality
The Framingham study looked at the prognostic implications of frequent PVCs (>30 per hour) in a cohort of symptomatic patients examined over a 6-year period.1 Men, but not women, had a significant increase in all-cause mortality (relative risk [RR]=2.36; 95% confidence interval [CI], 1.65-3.2) and myocardial infarction or sudden death (RR=2.12; 95% CI, 1.33-3.38). The Copenhagen Holter study of a cohort of healthy patients demonstrated an increased risk of myocardial infarction or cardiovascular death in patients with >30 PVCs per hour (hazard ratio [HR]=2.85, 95% CI, 1.16-7.0).2
Frequent PVCs occurring during recovery from stress testing are also associated with increased mortality. A large prospective cohort study followed more than 29,000 patients with varying degrees of risk for 5 years. After adjusting for confounding variables, frequent PVCs (≥7 per minute or more complex ventricular ectopy) during recovery predicted an increased risk of death (HR=1.5; 95% CI, 1.1-1.9). Frequent PVCs arising during exercise stress testing were not associated with increased risk.4
Suppressing PVCs is a bad idea
Studies have evaluated whether suppressing PVCs with antiarrhythmic agents improves prognosis. Both Cardiac Arrhythmia Suppression Trials (CAST I: encainide and flecainide; CAST II: moricizine) showed that suppressing frequent PVCs significantly increased mortality in the treatment groups.5,6
Recommendations
In 2006, the American College of Cardiology, American Heart Association, and European Society of Cardiology published their Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death.3
The TABLE summarizes characteristics of patients with PVCs who were at higher risk of underlying cardiac disease and death. All patients with PVCs should have a history and physical examination, electrocardiogram, and electrolyte studies. Higher-risk patients should be considered for further evaluation, including stress testing, echocardiography, and ambulatory electrocardiogram (SOR: C, opinion).
TABLE
Characteristics of patients with PVCs who are at higher risk of cardiac disease/death
| PATIENT CHARACTERISTICS | LOWER RISK | HIGHER RISK |
|---|---|---|
| Morphology | Unifocal PVCs<10 PVCs per hour | Complex multifocal PVCs Ventricular tachycardia Ventricular fibrillation >10 PVCs per hour |
| Symptoms | Asymptomatic | Palpitations Presyncope Syncope |
| Preexisting conditions | None | Known history of CAD Structural heart disease Valvular heart disease Cardiomyopathy |
| CAD, coronary artery disease, PVCs, premature ventricular contractions. | ||
| Source: American College of Cardiology et al.3 | ||
1. Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham heart study. Ann Intern Med. 1992;117:990-996.
2. Sajadieh A, Nielsen OW, Rasmussen V, et al. Ventricular arrhythmias and risk of death and acute myocardial infarction in apparently healthy subjects of age 55 or older. Am J Cardiol. 2006;97:1351-1357.
3. American College of Cardiology, American Heart Association, European Society of Cardiology. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2006;48:e247-e346.
4. Frolkis JP, Pothier CE, Blackstone EH, et al. Frequent ventricular ectopy after exercise as a predictor of death. N Engl J Med. 2003;348:781-790.
5. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989;321:406-412.
6. The Cardiac Arrhythmia Suppression Trial II Investigators. Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. N Engl J Med. 1992;327:227-233.
Yes. Current guidelines suggest evaluating patients with premature ventricular contractions (PVCs) and associated risk factors for underlying coronary artery disease (strength of recommendation [SOR]: C, expert opinion).
Frequent PVCs are associated with acute myocardial infarction and sudden death in patients without known coronary artery disease (CAD). They are linked to increased mortality from all causes in elderly patients with a history of CAD, left ventricular dysfunction, hypertension, or valvular heart disease. Frequent PVCs during recovery from exercise stress testing are also associated with increased mortality.
There is strong evidence against suppressing PVCs with antiarrhythmics (SOR: A, randomized controlled trials [RCTs]).
Stress preventive measures
Jennifer Lochner, MD
Oregon Health and Sciences University, Portland
I find myself discussing PVCs most often with young women who don’t have known heart disease—rather than the elderly. I often discover PVCs on physical examination in the office or see them on a Holter monitor ordered to rule out other more worrisome arrhythmias.
This reminds me that I need to not only consider the issue of treatment aimed at suppressing PVCs (not helpful except when the patient has significant symptoms), but also to consider whether the patient has risk factors for CAD.
In future discussions with patients about PVCs, I plan to shift the focus to measures to prevent CAD—specifically tobacco cessation, weight management, daily physical activity, and a healthy diet.
Evidence summary
A consistent definition of frequent PVCs doesn’t exist in the literature. Some studies have found a significant risk of death or acute myocardial infarction associated with >30 PVCs per hour.1,2 The 2006 American College of Cardiology/American Heart Association/European Society of Cardiology guideline defines frequent PVCs as >10 per hour.3
Despite the association between frequent PVCs and increased risk of death and cardiac events, our review didn’t find studies that indicate the utility of evaluation strategies for higher-risk patients.
Frequent PVCs predict increased mortality
The Framingham study looked at the prognostic implications of frequent PVCs (>30 per hour) in a cohort of symptomatic patients examined over a 6-year period.1 Men, but not women, had a significant increase in all-cause mortality (relative risk [RR]=2.36; 95% confidence interval [CI], 1.65-3.2) and myocardial infarction or sudden death (RR=2.12; 95% CI, 1.33-3.38). The Copenhagen Holter study of a cohort of healthy patients demonstrated an increased risk of myocardial infarction or cardiovascular death in patients with >30 PVCs per hour (hazard ratio [HR]=2.85, 95% CI, 1.16-7.0).2
Frequent PVCs occurring during recovery from stress testing are also associated with increased mortality. A large prospective cohort study followed more than 29,000 patients with varying degrees of risk for 5 years. After adjusting for confounding variables, frequent PVCs (≥7 per minute or more complex ventricular ectopy) during recovery predicted an increased risk of death (HR=1.5; 95% CI, 1.1-1.9). Frequent PVCs arising during exercise stress testing were not associated with increased risk.4
Suppressing PVCs is a bad idea
Studies have evaluated whether suppressing PVCs with antiarrhythmic agents improves prognosis. Both Cardiac Arrhythmia Suppression Trials (CAST I: encainide and flecainide; CAST II: moricizine) showed that suppressing frequent PVCs significantly increased mortality in the treatment groups.5,6
Recommendations
In 2006, the American College of Cardiology, American Heart Association, and European Society of Cardiology published their Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death.3
The TABLE summarizes characteristics of patients with PVCs who were at higher risk of underlying cardiac disease and death. All patients with PVCs should have a history and physical examination, electrocardiogram, and electrolyte studies. Higher-risk patients should be considered for further evaluation, including stress testing, echocardiography, and ambulatory electrocardiogram (SOR: C, opinion).
TABLE
Characteristics of patients with PVCs who are at higher risk of cardiac disease/death
| PATIENT CHARACTERISTICS | LOWER RISK | HIGHER RISK |
|---|---|---|
| Morphology | Unifocal PVCs<10 PVCs per hour | Complex multifocal PVCs Ventricular tachycardia Ventricular fibrillation >10 PVCs per hour |
| Symptoms | Asymptomatic | Palpitations Presyncope Syncope |
| Preexisting conditions | None | Known history of CAD Structural heart disease Valvular heart disease Cardiomyopathy |
| CAD, coronary artery disease, PVCs, premature ventricular contractions. | ||
| Source: American College of Cardiology et al.3 | ||
Yes. Current guidelines suggest evaluating patients with premature ventricular contractions (PVCs) and associated risk factors for underlying coronary artery disease (strength of recommendation [SOR]: C, expert opinion).
Frequent PVCs are associated with acute myocardial infarction and sudden death in patients without known coronary artery disease (CAD). They are linked to increased mortality from all causes in elderly patients with a history of CAD, left ventricular dysfunction, hypertension, or valvular heart disease. Frequent PVCs during recovery from exercise stress testing are also associated with increased mortality.
There is strong evidence against suppressing PVCs with antiarrhythmics (SOR: A, randomized controlled trials [RCTs]).
Stress preventive measures
Jennifer Lochner, MD
Oregon Health and Sciences University, Portland
I find myself discussing PVCs most often with young women who don’t have known heart disease—rather than the elderly. I often discover PVCs on physical examination in the office or see them on a Holter monitor ordered to rule out other more worrisome arrhythmias.
This reminds me that I need to not only consider the issue of treatment aimed at suppressing PVCs (not helpful except when the patient has significant symptoms), but also to consider whether the patient has risk factors for CAD.
In future discussions with patients about PVCs, I plan to shift the focus to measures to prevent CAD—specifically tobacco cessation, weight management, daily physical activity, and a healthy diet.
Evidence summary
A consistent definition of frequent PVCs doesn’t exist in the literature. Some studies have found a significant risk of death or acute myocardial infarction associated with >30 PVCs per hour.1,2 The 2006 American College of Cardiology/American Heart Association/European Society of Cardiology guideline defines frequent PVCs as >10 per hour.3
Despite the association between frequent PVCs and increased risk of death and cardiac events, our review didn’t find studies that indicate the utility of evaluation strategies for higher-risk patients.
Frequent PVCs predict increased mortality
The Framingham study looked at the prognostic implications of frequent PVCs (>30 per hour) in a cohort of symptomatic patients examined over a 6-year period.1 Men, but not women, had a significant increase in all-cause mortality (relative risk [RR]=2.36; 95% confidence interval [CI], 1.65-3.2) and myocardial infarction or sudden death (RR=2.12; 95% CI, 1.33-3.38). The Copenhagen Holter study of a cohort of healthy patients demonstrated an increased risk of myocardial infarction or cardiovascular death in patients with >30 PVCs per hour (hazard ratio [HR]=2.85, 95% CI, 1.16-7.0).2
Frequent PVCs occurring during recovery from stress testing are also associated with increased mortality. A large prospective cohort study followed more than 29,000 patients with varying degrees of risk for 5 years. After adjusting for confounding variables, frequent PVCs (≥7 per minute or more complex ventricular ectopy) during recovery predicted an increased risk of death (HR=1.5; 95% CI, 1.1-1.9). Frequent PVCs arising during exercise stress testing were not associated with increased risk.4
Suppressing PVCs is a bad idea
Studies have evaluated whether suppressing PVCs with antiarrhythmic agents improves prognosis. Both Cardiac Arrhythmia Suppression Trials (CAST I: encainide and flecainide; CAST II: moricizine) showed that suppressing frequent PVCs significantly increased mortality in the treatment groups.5,6
Recommendations
In 2006, the American College of Cardiology, American Heart Association, and European Society of Cardiology published their Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death.3
The TABLE summarizes characteristics of patients with PVCs who were at higher risk of underlying cardiac disease and death. All patients with PVCs should have a history and physical examination, electrocardiogram, and electrolyte studies. Higher-risk patients should be considered for further evaluation, including stress testing, echocardiography, and ambulatory electrocardiogram (SOR: C, opinion).
TABLE
Characteristics of patients with PVCs who are at higher risk of cardiac disease/death
| PATIENT CHARACTERISTICS | LOWER RISK | HIGHER RISK |
|---|---|---|
| Morphology | Unifocal PVCs<10 PVCs per hour | Complex multifocal PVCs Ventricular tachycardia Ventricular fibrillation >10 PVCs per hour |
| Symptoms | Asymptomatic | Palpitations Presyncope Syncope |
| Preexisting conditions | None | Known history of CAD Structural heart disease Valvular heart disease Cardiomyopathy |
| CAD, coronary artery disease, PVCs, premature ventricular contractions. | ||
| Source: American College of Cardiology et al.3 | ||
1. Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham heart study. Ann Intern Med. 1992;117:990-996.
2. Sajadieh A, Nielsen OW, Rasmussen V, et al. Ventricular arrhythmias and risk of death and acute myocardial infarction in apparently healthy subjects of age 55 or older. Am J Cardiol. 2006;97:1351-1357.
3. American College of Cardiology, American Heart Association, European Society of Cardiology. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2006;48:e247-e346.
4. Frolkis JP, Pothier CE, Blackstone EH, et al. Frequent ventricular ectopy after exercise as a predictor of death. N Engl J Med. 2003;348:781-790.
5. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989;321:406-412.
6. The Cardiac Arrhythmia Suppression Trial II Investigators. Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. N Engl J Med. 1992;327:227-233.
1. Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham heart study. Ann Intern Med. 1992;117:990-996.
2. Sajadieh A, Nielsen OW, Rasmussen V, et al. Ventricular arrhythmias and risk of death and acute myocardial infarction in apparently healthy subjects of age 55 or older. Am J Cardiol. 2006;97:1351-1357.
3. American College of Cardiology, American Heart Association, European Society of Cardiology. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2006;48:e247-e346.
4. Frolkis JP, Pothier CE, Blackstone EH, et al. Frequent ventricular ectopy after exercise as a predictor of death. N Engl J Med. 2003;348:781-790.
5. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989;321:406-412.
6. The Cardiac Arrhythmia Suppression Trial II Investigators. Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. N Engl J Med. 1992;327:227-233.
Evidence-based answers from the Family Physicians Inquiries Network
Is the long-term use of proton pump inhibitors safe?
Long-term use of proton pump inhibitors (PPIs) appears safe, resulting in no clinically relevant adverse effects (strength of recommendation: B, based on nonsystematic reviews, cohort studies, or low-quality randomized controlled trials). No evidence clearly links PPIs to gastric cancer or carcinoid, enteric infections, or significant nutrient malabsorption.
Evidence summary
The long-term safety of PPIs is not completely known. There are 5 PPIs on the US market. Clinical experience with these medications ranges from 3 to 20 years. All of the identified studies addressing long-term use have follow-up of 10 years or less (Table). Studies of longer duration are warranted. We reviewed the possible adverse effects of these medications.
Gastric carcinoid. PPIs cause predictable and sustained hypergastrinemia in response to acid suppression. In rats, this causes enterochro-maffin-like cell (ECL) hyperplasia and carcinoid tumors, raising a safety concern in humans. In a nonsystematic review of 11 studies of 1800 patients who used PPIs from 6 months to 8 years, there were no neoplastic ECL changes or carcinoid tumors.1 Three other nonsystematic reviews support these findings.2-4 In a randomized controlled trial comparing efficacy and safety of rabeprazole with omeprazole for gastro-esophageal disease, 123 (51%) out of 243 patients completed 5 years of the study; no patients had neoplastic ECL changes.5
Atrophic gastritis and gastric cancer. Atrophic gastritis with intestinal metaplasia is associated with gastric adenocarcinoma. Because PPIs can theoretically cause atrophic gastritis, there is a concern that this could lead to gastric cancer. The evidence regarding atrophic gastritis is contradictory. A nonsystematic review identified 1 cohort study and 1 randomized controlled trial of patients taking omeprazole from 1 to 4 years, which showed no association between PPI use and atrophic gastritis.1 The same review reported that another cohort study of patients using omeprazole for 1 year showed an increase in atrophic gastritis. None of the studies reviewed showed an association between omeprazole use and intestinal metaplasia or its progression to gastric adenocarcinoma.1 Three other nonsystematic reviews support these findings.2,3,5 The available evidence indicates that PPI use is not clearly associated with atrophic gastritis, or with progression from gastritis to metaplasia or cancer.
Enteric infections. Because hypochlorhydria is associated with bacterial enteric infections, bacterial enteritis is a theoretical risk of long-term PPI use. A large case-control study of 54,461 patients using omeprazole for 1 year showed no association with such infections.6
Mineral malabsorption. Dietary calcium, phosphorus, magnesium, zinc, and iron depend on gastric acid for absorption. Two separate non-systematic reviews showed no problems with malabsorption of these micronutrients.1,3
B12 malabsorption. Two nonsystematic reviews showed a decrease in vitamin B12 absorption among patients on high-dose (up to 80 mg of omeprazole daily), long-term PPI therapy (eg, patients with Zollinger-Ellison syndrome).1,2 This has not been demonstrated for patients taking more typical doses of omeprazole. The clinical significance of this is unknown; however, the authors of these reviews suggested monitoring B12 levels of patients on long-term, high-dose PPI therapy.
TABLE
Potential proton pump inhibitor safety concerns
| Safety concern | PPI studied | Duration of studies | Evidence |
|---|---|---|---|
| Gastric carcinoids | Omeprazole, lansoprazole, pantoprazole, rabeprazole | 1–8 years | No increased risk1-5 |
| Gastric metaplasia/adenocarcinoma | Omeprazole | 1–5 years | No increased risk1-3,5 |
| Enteric infections | Omeprazole | 1 year | No increased risk6 |
| Mineral malabsorption | Omeprazole | 6 months–2 years | No increased risk1,3 |
| B12 malabsorption | Omeprazole | 10 years | Decreased B12 levels with high-dose therapy1,2 |
Recommendations from others
A Federal Drug Commission report indicates that labeling PPIs for cancer risk is not warranted.7 The American College of Gastroenterology and the University of Michigan Health System guidelines for treatment of gastroesophageal disease recommend long-term PPI therapy as an option without any warning against their use.8,9
No evidence of long-term adverse health effects from PPIs, but cost still a problem
Richard A. Guthmann, MD
Illinois Masonic Family Practice Residency, University of Illinois at Chicago
Proton pump inhibitors work. They effectively treat the symptoms and reduce the complication involved with peptic ulcer disease. The lack of evidence suggesting any long-term adverse health effects, even if not definitive, is very encouraging, but the cost of these medicines remains a problem. Both patients and third-party payers continue to object to their cost, and for this reason, as well as longer safety track records, less expensive medicines such as H2 blockers and over-the-counter antacids should be tried for longer-term treatment.
1. Laine L, Ahnen D, McClain C, Solcia E, Walsh JH. Review article: potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther 2000;14:651-668.
2. Garnett WR. Considerations for long-term use of protonpump inhibitors. Am J Health Syst Pharm 1998;55:2268-2279.
3. Freston JW. Long-term acid control and proton pump inhibitors: interactions and safety issues in perspective. Am J Gastroenterol 1997;92(4 Suppl):51S-57S.
4. Freston JW, Rose PA, Heller CA, Haber M, Jennings D. Safety profile of Lansoprazole: the US clinical trial experience. Drug Saf 1999;20:195-205.
5. Thjodleifsson B, Rindi G, Fiocca R, et al. A randomized double-blind trial of the efficacy and safety of 10 or 20 mg rabeprazole compared with 20 mg omeprazole in the maintenance of gastro-oesophageal reflux disease over 5 years. Aliment Pharmacol Ther 2003;17:343-351.
6. Garcia Rodriguez LA, Ruigomez A. Gastric acid, acid-sup-pressing drugs, and bacterial gastroenteritis: how much of a risk? Epidemiology 1997;8:571-574.
7. Proton pump inhibitor relabeling for cancer risk not warranted; long-term studies recommended. FDC Rep 1996;58(Nov 11)T&G:1-2.
8. Management of gastroesophageal reflux disease (GERD). Ann Arbor, Mich: University of Michigan Health System; last updated 2002 March. Available at: cme.med.umich.edu/iCME/gerd/default.asp. Accessed on March 16, 2004.
9. DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol 1999;94:1434-1442.
Long-term use of proton pump inhibitors (PPIs) appears safe, resulting in no clinically relevant adverse effects (strength of recommendation: B, based on nonsystematic reviews, cohort studies, or low-quality randomized controlled trials). No evidence clearly links PPIs to gastric cancer or carcinoid, enteric infections, or significant nutrient malabsorption.
Evidence summary
The long-term safety of PPIs is not completely known. There are 5 PPIs on the US market. Clinical experience with these medications ranges from 3 to 20 years. All of the identified studies addressing long-term use have follow-up of 10 years or less (Table). Studies of longer duration are warranted. We reviewed the possible adverse effects of these medications.
Gastric carcinoid. PPIs cause predictable and sustained hypergastrinemia in response to acid suppression. In rats, this causes enterochro-maffin-like cell (ECL) hyperplasia and carcinoid tumors, raising a safety concern in humans. In a nonsystematic review of 11 studies of 1800 patients who used PPIs from 6 months to 8 years, there were no neoplastic ECL changes or carcinoid tumors.1 Three other nonsystematic reviews support these findings.2-4 In a randomized controlled trial comparing efficacy and safety of rabeprazole with omeprazole for gastro-esophageal disease, 123 (51%) out of 243 patients completed 5 years of the study; no patients had neoplastic ECL changes.5
Atrophic gastritis and gastric cancer. Atrophic gastritis with intestinal metaplasia is associated with gastric adenocarcinoma. Because PPIs can theoretically cause atrophic gastritis, there is a concern that this could lead to gastric cancer. The evidence regarding atrophic gastritis is contradictory. A nonsystematic review identified 1 cohort study and 1 randomized controlled trial of patients taking omeprazole from 1 to 4 years, which showed no association between PPI use and atrophic gastritis.1 The same review reported that another cohort study of patients using omeprazole for 1 year showed an increase in atrophic gastritis. None of the studies reviewed showed an association between omeprazole use and intestinal metaplasia or its progression to gastric adenocarcinoma.1 Three other nonsystematic reviews support these findings.2,3,5 The available evidence indicates that PPI use is not clearly associated with atrophic gastritis, or with progression from gastritis to metaplasia or cancer.
Enteric infections. Because hypochlorhydria is associated with bacterial enteric infections, bacterial enteritis is a theoretical risk of long-term PPI use. A large case-control study of 54,461 patients using omeprazole for 1 year showed no association with such infections.6
Mineral malabsorption. Dietary calcium, phosphorus, magnesium, zinc, and iron depend on gastric acid for absorption. Two separate non-systematic reviews showed no problems with malabsorption of these micronutrients.1,3
B12 malabsorption. Two nonsystematic reviews showed a decrease in vitamin B12 absorption among patients on high-dose (up to 80 mg of omeprazole daily), long-term PPI therapy (eg, patients with Zollinger-Ellison syndrome).1,2 This has not been demonstrated for patients taking more typical doses of omeprazole. The clinical significance of this is unknown; however, the authors of these reviews suggested monitoring B12 levels of patients on long-term, high-dose PPI therapy.
TABLE
Potential proton pump inhibitor safety concerns
| Safety concern | PPI studied | Duration of studies | Evidence |
|---|---|---|---|
| Gastric carcinoids | Omeprazole, lansoprazole, pantoprazole, rabeprazole | 1–8 years | No increased risk1-5 |
| Gastric metaplasia/adenocarcinoma | Omeprazole | 1–5 years | No increased risk1-3,5 |
| Enteric infections | Omeprazole | 1 year | No increased risk6 |
| Mineral malabsorption | Omeprazole | 6 months–2 years | No increased risk1,3 |
| B12 malabsorption | Omeprazole | 10 years | Decreased B12 levels with high-dose therapy1,2 |
Recommendations from others
A Federal Drug Commission report indicates that labeling PPIs for cancer risk is not warranted.7 The American College of Gastroenterology and the University of Michigan Health System guidelines for treatment of gastroesophageal disease recommend long-term PPI therapy as an option without any warning against their use.8,9
No evidence of long-term adverse health effects from PPIs, but cost still a problem
Richard A. Guthmann, MD
Illinois Masonic Family Practice Residency, University of Illinois at Chicago
Proton pump inhibitors work. They effectively treat the symptoms and reduce the complication involved with peptic ulcer disease. The lack of evidence suggesting any long-term adverse health effects, even if not definitive, is very encouraging, but the cost of these medicines remains a problem. Both patients and third-party payers continue to object to their cost, and for this reason, as well as longer safety track records, less expensive medicines such as H2 blockers and over-the-counter antacids should be tried for longer-term treatment.
Long-term use of proton pump inhibitors (PPIs) appears safe, resulting in no clinically relevant adverse effects (strength of recommendation: B, based on nonsystematic reviews, cohort studies, or low-quality randomized controlled trials). No evidence clearly links PPIs to gastric cancer or carcinoid, enteric infections, or significant nutrient malabsorption.
Evidence summary
The long-term safety of PPIs is not completely known. There are 5 PPIs on the US market. Clinical experience with these medications ranges from 3 to 20 years. All of the identified studies addressing long-term use have follow-up of 10 years or less (Table). Studies of longer duration are warranted. We reviewed the possible adverse effects of these medications.
Gastric carcinoid. PPIs cause predictable and sustained hypergastrinemia in response to acid suppression. In rats, this causes enterochro-maffin-like cell (ECL) hyperplasia and carcinoid tumors, raising a safety concern in humans. In a nonsystematic review of 11 studies of 1800 patients who used PPIs from 6 months to 8 years, there were no neoplastic ECL changes or carcinoid tumors.1 Three other nonsystematic reviews support these findings.2-4 In a randomized controlled trial comparing efficacy and safety of rabeprazole with omeprazole for gastro-esophageal disease, 123 (51%) out of 243 patients completed 5 years of the study; no patients had neoplastic ECL changes.5
Atrophic gastritis and gastric cancer. Atrophic gastritis with intestinal metaplasia is associated with gastric adenocarcinoma. Because PPIs can theoretically cause atrophic gastritis, there is a concern that this could lead to gastric cancer. The evidence regarding atrophic gastritis is contradictory. A nonsystematic review identified 1 cohort study and 1 randomized controlled trial of patients taking omeprazole from 1 to 4 years, which showed no association between PPI use and atrophic gastritis.1 The same review reported that another cohort study of patients using omeprazole for 1 year showed an increase in atrophic gastritis. None of the studies reviewed showed an association between omeprazole use and intestinal metaplasia or its progression to gastric adenocarcinoma.1 Three other nonsystematic reviews support these findings.2,3,5 The available evidence indicates that PPI use is not clearly associated with atrophic gastritis, or with progression from gastritis to metaplasia or cancer.
Enteric infections. Because hypochlorhydria is associated with bacterial enteric infections, bacterial enteritis is a theoretical risk of long-term PPI use. A large case-control study of 54,461 patients using omeprazole for 1 year showed no association with such infections.6
Mineral malabsorption. Dietary calcium, phosphorus, magnesium, zinc, and iron depend on gastric acid for absorption. Two separate non-systematic reviews showed no problems with malabsorption of these micronutrients.1,3
B12 malabsorption. Two nonsystematic reviews showed a decrease in vitamin B12 absorption among patients on high-dose (up to 80 mg of omeprazole daily), long-term PPI therapy (eg, patients with Zollinger-Ellison syndrome).1,2 This has not been demonstrated for patients taking more typical doses of omeprazole. The clinical significance of this is unknown; however, the authors of these reviews suggested monitoring B12 levels of patients on long-term, high-dose PPI therapy.
TABLE
Potential proton pump inhibitor safety concerns
| Safety concern | PPI studied | Duration of studies | Evidence |
|---|---|---|---|
| Gastric carcinoids | Omeprazole, lansoprazole, pantoprazole, rabeprazole | 1–8 years | No increased risk1-5 |
| Gastric metaplasia/adenocarcinoma | Omeprazole | 1–5 years | No increased risk1-3,5 |
| Enteric infections | Omeprazole | 1 year | No increased risk6 |
| Mineral malabsorption | Omeprazole | 6 months–2 years | No increased risk1,3 |
| B12 malabsorption | Omeprazole | 10 years | Decreased B12 levels with high-dose therapy1,2 |
Recommendations from others
A Federal Drug Commission report indicates that labeling PPIs for cancer risk is not warranted.7 The American College of Gastroenterology and the University of Michigan Health System guidelines for treatment of gastroesophageal disease recommend long-term PPI therapy as an option without any warning against their use.8,9
No evidence of long-term adverse health effects from PPIs, but cost still a problem
Richard A. Guthmann, MD
Illinois Masonic Family Practice Residency, University of Illinois at Chicago
Proton pump inhibitors work. They effectively treat the symptoms and reduce the complication involved with peptic ulcer disease. The lack of evidence suggesting any long-term adverse health effects, even if not definitive, is very encouraging, but the cost of these medicines remains a problem. Both patients and third-party payers continue to object to their cost, and for this reason, as well as longer safety track records, less expensive medicines such as H2 blockers and over-the-counter antacids should be tried for longer-term treatment.
1. Laine L, Ahnen D, McClain C, Solcia E, Walsh JH. Review article: potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther 2000;14:651-668.
2. Garnett WR. Considerations for long-term use of protonpump inhibitors. Am J Health Syst Pharm 1998;55:2268-2279.
3. Freston JW. Long-term acid control and proton pump inhibitors: interactions and safety issues in perspective. Am J Gastroenterol 1997;92(4 Suppl):51S-57S.
4. Freston JW, Rose PA, Heller CA, Haber M, Jennings D. Safety profile of Lansoprazole: the US clinical trial experience. Drug Saf 1999;20:195-205.
5. Thjodleifsson B, Rindi G, Fiocca R, et al. A randomized double-blind trial of the efficacy and safety of 10 or 20 mg rabeprazole compared with 20 mg omeprazole in the maintenance of gastro-oesophageal reflux disease over 5 years. Aliment Pharmacol Ther 2003;17:343-351.
6. Garcia Rodriguez LA, Ruigomez A. Gastric acid, acid-sup-pressing drugs, and bacterial gastroenteritis: how much of a risk? Epidemiology 1997;8:571-574.
7. Proton pump inhibitor relabeling for cancer risk not warranted; long-term studies recommended. FDC Rep 1996;58(Nov 11)T&G:1-2.
8. Management of gastroesophageal reflux disease (GERD). Ann Arbor, Mich: University of Michigan Health System; last updated 2002 March. Available at: cme.med.umich.edu/iCME/gerd/default.asp. Accessed on March 16, 2004.
9. DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol 1999;94:1434-1442.
1. Laine L, Ahnen D, McClain C, Solcia E, Walsh JH. Review article: potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther 2000;14:651-668.
2. Garnett WR. Considerations for long-term use of protonpump inhibitors. Am J Health Syst Pharm 1998;55:2268-2279.
3. Freston JW. Long-term acid control and proton pump inhibitors: interactions and safety issues in perspective. Am J Gastroenterol 1997;92(4 Suppl):51S-57S.
4. Freston JW, Rose PA, Heller CA, Haber M, Jennings D. Safety profile of Lansoprazole: the US clinical trial experience. Drug Saf 1999;20:195-205.
5. Thjodleifsson B, Rindi G, Fiocca R, et al. A randomized double-blind trial of the efficacy and safety of 10 or 20 mg rabeprazole compared with 20 mg omeprazole in the maintenance of gastro-oesophageal reflux disease over 5 years. Aliment Pharmacol Ther 2003;17:343-351.
6. Garcia Rodriguez LA, Ruigomez A. Gastric acid, acid-sup-pressing drugs, and bacterial gastroenteritis: how much of a risk? Epidemiology 1997;8:571-574.
7. Proton pump inhibitor relabeling for cancer risk not warranted; long-term studies recommended. FDC Rep 1996;58(Nov 11)T&G:1-2.
8. Management of gastroesophageal reflux disease (GERD). Ann Arbor, Mich: University of Michigan Health System; last updated 2002 March. Available at: cme.med.umich.edu/iCME/gerd/default.asp. Accessed on March 16, 2004.
9. DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol 1999;94:1434-1442.
Evidence-based answers from the Family Physicians Inquiries Network