User login
New data underscore importance of biologic ‘sweet spot’
ORLANDO – To delay or prevent recurrence of Crohn’s disease in patients after they’ve undergone ileocolonic resectioning, the ultimate question is where the “sweet spot” is for timing biologic therapy.
“In 2016, symptoms will still guide treatment,” said Dr. Miguel D. Regueiro, professor of medicine at the University of Pittsburgh and clinical medical director of the University’s IBD Center, during the clinical track of this year’s annual Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s and Colitis Foundation of America. But when it comes to the exact timing of administering anti–tumor necrosis factor (TNF) agents, clinicians should look to risk factors for recurrence.
The notion that immediate treatment with a biologic after surgical resectioning is best is supported by phase III data from the international, multicenter PREVENT trial, for which Dr. Regueiro was principal investigator. It demonstrated that at week 79 and week 104, immediate treatment with the biologic infliximab 5 mg/kg every 8 weeks postsurgery in patients with high risk for recurrence (smokers, those with penetrating or fistulizing disease, or a history of resectioning) resulted in lower but not statistically significant rates of the composite endpoint of clinical recurrence and endoscopic scores greater than 2, when compared with placebo (P = .097 at 76 weeks and P = .098 at 104 weeks).
Dr. Regueiro noted in an interview that often, even though endoscopic recurrence scores might be high, following surgery, patients are in clinical remission and so do not report any symptoms. He noted that when only endoscopic outcomes prior to or at week 76 in the PREVENT trial were analyzed as the secondary endpoint, there was a statistically significant difference when compared with placebo: The 147 randomly assigned study arm participants had a recurrence rate of 22.4% vs. 51.3% in 150 controls (P less than .001). Further, Rutgeerts scores equal or greater than i-3 occurred in 83.1% of participants in the placebo group, compared with 28.4% in the infliximab group at week 76.
“The take-home message is that surgery induces a deep remission where patient’s ‘feel well’ and by using a clinical symptom score we do not detect recurrence, probably for years,” Dr. Regueiro said in the interview.
What about waiting to offer treatment?
Results from the POCER trial, also conducted internationally at a number of centers, support this approach.
In the trial, 174 postoperative patients at high risk for recurrence were randomly assigned in a 2:1 ratio to either standard care – colonoscopy at 18 months – or to receive a colonoscopy at 6 months, followed by medication if there was an endoscopic recurrence of i-2 or greater.
Both study arms were given metronidazole 400 mg twice a day for 3 months. If patients were intolerant, the dose was reduced to 200 mg twice daily or was stopped altogether. If they were high risk but medication naive, patients were given azathioprine 2 mg/kg or 6-mercaptopurine 1.5 mg/kg once daily, beginning within 1 month after surgery. Patients intolerant to this regime were administered adalimumab 160/80/40 mg accordingly, every other week.
At 18 months, those patients who’d been observed endoscopically at 6 months and given medication if necessary had a 49% rate of recurrence compared with 67% in the group given standard care, a statistically significant difference.
However, when Dr. Regueiro, who was not directly involved with the POCER trial, conducted an informal review of the data, he found that patients who’d been on thiopurines had an endoscopic recurrence rate at 6 months of 45% vs. the 21% rate in the adalimumab patients. “This means that waiting on anti-TNF and giving thiopurine meant nearly half the patients had recurrence in 6 months, compared with anti-TNF treated patients.”
So then, when should biologics enter the treatment picture?
Again, look to the risk profile, said Dr. Regueiro. Patients who are 30 years of age or younger, have ileocolonic disease, smoke, have penetrating disease, or have already had two or more surgeries or had a short duration between time of diagnosis and surgery are considered at high risk for return of the disease.
In his own practice, Dr. Regueiro said he puts all but the low-risk patients on some form of immediate postoperative medication. Patients at moderate risk, such as those who have had a resection within 10 years of diagnosis, receive 6-mercaptopurine or azathioprine plus metronidazole (if tolerated) and are given colonoscopy at 6-12 months postoperatively. If there is a recurrence at that point, then he will start the patient on an anti-TNF. If not, then he sees them again in 1-3 years for a colonoscopy. Dr. Regueiro treats patients at high risk for recurrence more frequently with combination therapies, immediately setting them on a regimen of anti-TNF plus immunosuppressive therapy followed by a 6-12 month postoperative colonoscopy after which he adjusts treatment if there is active disease, including increasing the dose of the biologic or switching to another one.
But just what length of time actually constitutes “immediately after surgery?” In the PREVENT trial, clinicians had up to 45 days to begin therapy, although Dr. Regueiro said he prefers to start between 2 and 4 weeks postsurgery, a number with which panel moderator Dr. David T. Rubin, codirector of the University of Chicago Digestive Diseases Center, agreed.
While these study results help pinpoint the range for when to use biologics, Dr. Regueiro said in the interview, “Future study is need to determine the ‘tipping point’ where postoperative Crohn’s disease recurrence results in significant bowel damage and renders medications ineffective. Finding the ‘biologic sweet spot’ of when to start aggressive therapy versus a ‘wait and watch’ approach remains the question.”
Dr. Regueiro disclosed he is a consultant for AbbVie, Janssen, UCB, Pfizer, and Takeda.
On Twitter @whitneymcknight
ORLANDO – To delay or prevent recurrence of Crohn’s disease in patients after they’ve undergone ileocolonic resectioning, the ultimate question is where the “sweet spot” is for timing biologic therapy.
“In 2016, symptoms will still guide treatment,” said Dr. Miguel D. Regueiro, professor of medicine at the University of Pittsburgh and clinical medical director of the University’s IBD Center, during the clinical track of this year’s annual Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s and Colitis Foundation of America. But when it comes to the exact timing of administering anti–tumor necrosis factor (TNF) agents, clinicians should look to risk factors for recurrence.
The notion that immediate treatment with a biologic after surgical resectioning is best is supported by phase III data from the international, multicenter PREVENT trial, for which Dr. Regueiro was principal investigator. It demonstrated that at week 79 and week 104, immediate treatment with the biologic infliximab 5 mg/kg every 8 weeks postsurgery in patients with high risk for recurrence (smokers, those with penetrating or fistulizing disease, or a history of resectioning) resulted in lower but not statistically significant rates of the composite endpoint of clinical recurrence and endoscopic scores greater than 2, when compared with placebo (P = .097 at 76 weeks and P = .098 at 104 weeks).
Dr. Regueiro noted in an interview that often, even though endoscopic recurrence scores might be high, following surgery, patients are in clinical remission and so do not report any symptoms. He noted that when only endoscopic outcomes prior to or at week 76 in the PREVENT trial were analyzed as the secondary endpoint, there was a statistically significant difference when compared with placebo: The 147 randomly assigned study arm participants had a recurrence rate of 22.4% vs. 51.3% in 150 controls (P less than .001). Further, Rutgeerts scores equal or greater than i-3 occurred in 83.1% of participants in the placebo group, compared with 28.4% in the infliximab group at week 76.
“The take-home message is that surgery induces a deep remission where patient’s ‘feel well’ and by using a clinical symptom score we do not detect recurrence, probably for years,” Dr. Regueiro said in the interview.
What about waiting to offer treatment?
Results from the POCER trial, also conducted internationally at a number of centers, support this approach.
In the trial, 174 postoperative patients at high risk for recurrence were randomly assigned in a 2:1 ratio to either standard care – colonoscopy at 18 months – or to receive a colonoscopy at 6 months, followed by medication if there was an endoscopic recurrence of i-2 or greater.
Both study arms were given metronidazole 400 mg twice a day for 3 months. If patients were intolerant, the dose was reduced to 200 mg twice daily or was stopped altogether. If they were high risk but medication naive, patients were given azathioprine 2 mg/kg or 6-mercaptopurine 1.5 mg/kg once daily, beginning within 1 month after surgery. Patients intolerant to this regime were administered adalimumab 160/80/40 mg accordingly, every other week.
At 18 months, those patients who’d been observed endoscopically at 6 months and given medication if necessary had a 49% rate of recurrence compared with 67% in the group given standard care, a statistically significant difference.
However, when Dr. Regueiro, who was not directly involved with the POCER trial, conducted an informal review of the data, he found that patients who’d been on thiopurines had an endoscopic recurrence rate at 6 months of 45% vs. the 21% rate in the adalimumab patients. “This means that waiting on anti-TNF and giving thiopurine meant nearly half the patients had recurrence in 6 months, compared with anti-TNF treated patients.”
So then, when should biologics enter the treatment picture?
Again, look to the risk profile, said Dr. Regueiro. Patients who are 30 years of age or younger, have ileocolonic disease, smoke, have penetrating disease, or have already had two or more surgeries or had a short duration between time of diagnosis and surgery are considered at high risk for return of the disease.
In his own practice, Dr. Regueiro said he puts all but the low-risk patients on some form of immediate postoperative medication. Patients at moderate risk, such as those who have had a resection within 10 years of diagnosis, receive 6-mercaptopurine or azathioprine plus metronidazole (if tolerated) and are given colonoscopy at 6-12 months postoperatively. If there is a recurrence at that point, then he will start the patient on an anti-TNF. If not, then he sees them again in 1-3 years for a colonoscopy. Dr. Regueiro treats patients at high risk for recurrence more frequently with combination therapies, immediately setting them on a regimen of anti-TNF plus immunosuppressive therapy followed by a 6-12 month postoperative colonoscopy after which he adjusts treatment if there is active disease, including increasing the dose of the biologic or switching to another one.
But just what length of time actually constitutes “immediately after surgery?” In the PREVENT trial, clinicians had up to 45 days to begin therapy, although Dr. Regueiro said he prefers to start between 2 and 4 weeks postsurgery, a number with which panel moderator Dr. David T. Rubin, codirector of the University of Chicago Digestive Diseases Center, agreed.
While these study results help pinpoint the range for when to use biologics, Dr. Regueiro said in the interview, “Future study is need to determine the ‘tipping point’ where postoperative Crohn’s disease recurrence results in significant bowel damage and renders medications ineffective. Finding the ‘biologic sweet spot’ of when to start aggressive therapy versus a ‘wait and watch’ approach remains the question.”
Dr. Regueiro disclosed he is a consultant for AbbVie, Janssen, UCB, Pfizer, and Takeda.
On Twitter @whitneymcknight
ORLANDO – To delay or prevent recurrence of Crohn’s disease in patients after they’ve undergone ileocolonic resectioning, the ultimate question is where the “sweet spot” is for timing biologic therapy.
“In 2016, symptoms will still guide treatment,” said Dr. Miguel D. Regueiro, professor of medicine at the University of Pittsburgh and clinical medical director of the University’s IBD Center, during the clinical track of this year’s annual Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s and Colitis Foundation of America. But when it comes to the exact timing of administering anti–tumor necrosis factor (TNF) agents, clinicians should look to risk factors for recurrence.
The notion that immediate treatment with a biologic after surgical resectioning is best is supported by phase III data from the international, multicenter PREVENT trial, for which Dr. Regueiro was principal investigator. It demonstrated that at week 79 and week 104, immediate treatment with the biologic infliximab 5 mg/kg every 8 weeks postsurgery in patients with high risk for recurrence (smokers, those with penetrating or fistulizing disease, or a history of resectioning) resulted in lower but not statistically significant rates of the composite endpoint of clinical recurrence and endoscopic scores greater than 2, when compared with placebo (P = .097 at 76 weeks and P = .098 at 104 weeks).
Dr. Regueiro noted in an interview that often, even though endoscopic recurrence scores might be high, following surgery, patients are in clinical remission and so do not report any symptoms. He noted that when only endoscopic outcomes prior to or at week 76 in the PREVENT trial were analyzed as the secondary endpoint, there was a statistically significant difference when compared with placebo: The 147 randomly assigned study arm participants had a recurrence rate of 22.4% vs. 51.3% in 150 controls (P less than .001). Further, Rutgeerts scores equal or greater than i-3 occurred in 83.1% of participants in the placebo group, compared with 28.4% in the infliximab group at week 76.
“The take-home message is that surgery induces a deep remission where patient’s ‘feel well’ and by using a clinical symptom score we do not detect recurrence, probably for years,” Dr. Regueiro said in the interview.
What about waiting to offer treatment?
Results from the POCER trial, also conducted internationally at a number of centers, support this approach.
In the trial, 174 postoperative patients at high risk for recurrence were randomly assigned in a 2:1 ratio to either standard care – colonoscopy at 18 months – or to receive a colonoscopy at 6 months, followed by medication if there was an endoscopic recurrence of i-2 or greater.
Both study arms were given metronidazole 400 mg twice a day for 3 months. If patients were intolerant, the dose was reduced to 200 mg twice daily or was stopped altogether. If they were high risk but medication naive, patients were given azathioprine 2 mg/kg or 6-mercaptopurine 1.5 mg/kg once daily, beginning within 1 month after surgery. Patients intolerant to this regime were administered adalimumab 160/80/40 mg accordingly, every other week.
At 18 months, those patients who’d been observed endoscopically at 6 months and given medication if necessary had a 49% rate of recurrence compared with 67% in the group given standard care, a statistically significant difference.
However, when Dr. Regueiro, who was not directly involved with the POCER trial, conducted an informal review of the data, he found that patients who’d been on thiopurines had an endoscopic recurrence rate at 6 months of 45% vs. the 21% rate in the adalimumab patients. “This means that waiting on anti-TNF and giving thiopurine meant nearly half the patients had recurrence in 6 months, compared with anti-TNF treated patients.”
So then, when should biologics enter the treatment picture?
Again, look to the risk profile, said Dr. Regueiro. Patients who are 30 years of age or younger, have ileocolonic disease, smoke, have penetrating disease, or have already had two or more surgeries or had a short duration between time of diagnosis and surgery are considered at high risk for return of the disease.
In his own practice, Dr. Regueiro said he puts all but the low-risk patients on some form of immediate postoperative medication. Patients at moderate risk, such as those who have had a resection within 10 years of diagnosis, receive 6-mercaptopurine or azathioprine plus metronidazole (if tolerated) and are given colonoscopy at 6-12 months postoperatively. If there is a recurrence at that point, then he will start the patient on an anti-TNF. If not, then he sees them again in 1-3 years for a colonoscopy. Dr. Regueiro treats patients at high risk for recurrence more frequently with combination therapies, immediately setting them on a regimen of anti-TNF plus immunosuppressive therapy followed by a 6-12 month postoperative colonoscopy after which he adjusts treatment if there is active disease, including increasing the dose of the biologic or switching to another one.
But just what length of time actually constitutes “immediately after surgery?” In the PREVENT trial, clinicians had up to 45 days to begin therapy, although Dr. Regueiro said he prefers to start between 2 and 4 weeks postsurgery, a number with which panel moderator Dr. David T. Rubin, codirector of the University of Chicago Digestive Diseases Center, agreed.
While these study results help pinpoint the range for when to use biologics, Dr. Regueiro said in the interview, “Future study is need to determine the ‘tipping point’ where postoperative Crohn’s disease recurrence results in significant bowel damage and renders medications ineffective. Finding the ‘biologic sweet spot’ of when to start aggressive therapy versus a ‘wait and watch’ approach remains the question.”
Dr. Regueiro disclosed he is a consultant for AbbVie, Janssen, UCB, Pfizer, and Takeda.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM 2015 ADVANCES IN IBD
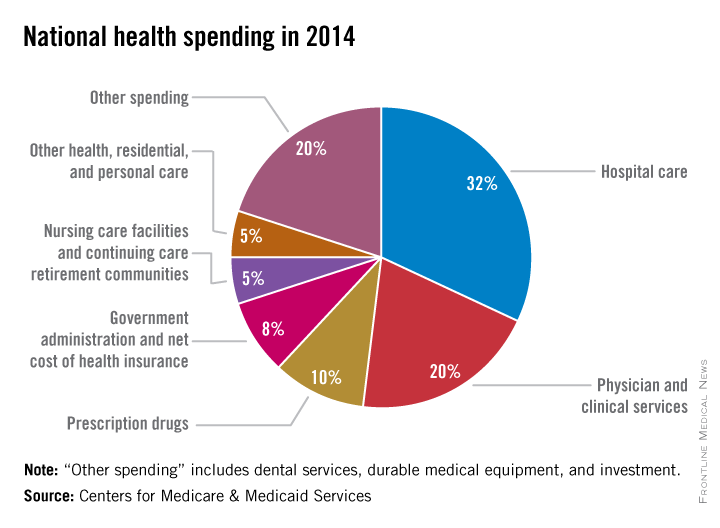
CMS finalizes ruling on prior authorization for some durable goods and equipment
The Centers for Medicare & Medicaid Services today issued its final rule on prior authorization for certain durable medical equipment, prosthetics, orthotics, and supplies.
The rule moves necessary documentation earlier in the approval process, requiring all relevant coverage, coding, and clinical documentation to be completed before certain goods are provided to a beneficiary and before the claim is submitted for payment, according to a CMS statement published Dec. 30 in the Federal Register.
Prior authorization is an effective way to reduce or prevent questionable billing practices and improper payments for durable medical equipment, prosthetics, orthotics, and supplies, according to the statement.
The rule includes review and approval timeframes and a provision for expedited claims in which delayed approval could adversely impact a beneficiary’s health.
Some of the items subject to “frequent unnecessary utilization” include certain powered air mattresses, continuous airway pressure devices, power wheelchairs, oxygen concentrators, and prosthetic limbs (especially for lower extremities).
On Twitter @whitneymcknight
The Centers for Medicare & Medicaid Services today issued its final rule on prior authorization for certain durable medical equipment, prosthetics, orthotics, and supplies.
The rule moves necessary documentation earlier in the approval process, requiring all relevant coverage, coding, and clinical documentation to be completed before certain goods are provided to a beneficiary and before the claim is submitted for payment, according to a CMS statement published Dec. 30 in the Federal Register.
Prior authorization is an effective way to reduce or prevent questionable billing practices and improper payments for durable medical equipment, prosthetics, orthotics, and supplies, according to the statement.
The rule includes review and approval timeframes and a provision for expedited claims in which delayed approval could adversely impact a beneficiary’s health.
Some of the items subject to “frequent unnecessary utilization” include certain powered air mattresses, continuous airway pressure devices, power wheelchairs, oxygen concentrators, and prosthetic limbs (especially for lower extremities).
On Twitter @whitneymcknight
The Centers for Medicare & Medicaid Services today issued its final rule on prior authorization for certain durable medical equipment, prosthetics, orthotics, and supplies.
The rule moves necessary documentation earlier in the approval process, requiring all relevant coverage, coding, and clinical documentation to be completed before certain goods are provided to a beneficiary and before the claim is submitted for payment, according to a CMS statement published Dec. 30 in the Federal Register.
Prior authorization is an effective way to reduce or prevent questionable billing practices and improper payments for durable medical equipment, prosthetics, orthotics, and supplies, according to the statement.
The rule includes review and approval timeframes and a provision for expedited claims in which delayed approval could adversely impact a beneficiary’s health.
Some of the items subject to “frequent unnecessary utilization” include certain powered air mattresses, continuous airway pressure devices, power wheelchairs, oxygen concentrators, and prosthetic limbs (especially for lower extremities).
On Twitter @whitneymcknight
Tricks for treating C. diff in IBD
ORLANDO – You can confidently treat mild to severe Clostridium difficile infection in persons with inflammatory bowel disease, without disrupting their immunosuppression or other treatments, according to an expert.
“If your patient with IBD needs a fecal transplant for C. diff., you should not be concerned about withholding it,” Dr. Alan C. Moss said during a basic science presentation at a conference on inflammatory bowel diseases (IBD), sponsored by the Crohn’s and Colitis Foundation of America. Dr. Moss is an associate professor of medicine and the director of translational research at Harvard Medical School, Boston.
The first step, after you’ve determined that your patient has a true C. diff. infection, as opposed to having only been colonized by the bacteria, is choosing the best antibiotic. “Unfortunately, almost all IBD patients are excluded from controlled trials of antibiotics in C. diff. infection, so all we really have to go on are retrospective cohort data,” said Dr. Moss.
One such study, uncontrolled for disease severity, showed that a third of 114 inpatients with IBD who had a co-occurring C. diff. infection had higher 30-day readmission rates when treated first with metronidazole, per current standards of care, compared with the remaining two-thirds of patients who were treated first with vancomycin. The metronidazole group also averaged double the length of stays of the vancomycin group (Antimicrob Agents Chemother. 2014 Sep;58:5054-9 [doi: 10.1128/AAC.02606-13]).
“This suggests that in IBD patients, especially for those who meet criteria for a severe C. diff. infection, vancomycin is the way to go,” Dr. Moss said, noting a trend of metronidazole for mild infections in this cohort having ever less efficacy.
Beyond mild infection, Dr. Moss said the first line of treatment should be vancomycin 125 mg four times daily, or 500 mg four times daily if it is complicated disease.
If your patient has recurrent C. diff. infection, Dr. Moss recommended a prolonged taper of vancomycin, but to be vigilant about it being truly an infection and not a flare-up of colonized bacteria.
“My bar for doing fecal transplant in these patients has dropped considerably in the last few years, because if you really want to squeeze out the niche that C. diff. occupies in the microbiome, fecal transplant is really the most effective way we have of doing that,” Dr. Moss said.
While there is a division in the field over whether to continue immunosuppression during antibiotic treatment, Dr. Moss cited a small study indicating that if a patient were on two or more immunosuppressants, they had a higher risk of death, megacolon, or shock during C. diff. treatment. “I think it’s hard to draw many conclusions from that,” Dr. Moss said. “It may just be a surrogate marker of severity of disease rather than infection, per se.”
The standard of care for recurrent and refractory C. diff. infection is now fecal transplant, according to Dr. Moss. A recent study of fecal transplantation showed an 89% cure rate of C. diff. infection after a single fecal transplant in IBD patients. Of the 36 IBD patients in the study, half of whom were on biologic and immunosuppressive therapies, four experienced disease flare-ups (Am J Gastroenterol. 2014 Jul;109:1065-71 [doi: 10.1038/ajg.2014.133]. N Engl J Med. 2013 Jan 31;368:474-5 [doi: 10.1056/NEJMe1214816]).
As for determining if there is an actual infection rather than colonization of C. diff., Dr. Moss said switching from using ELISA (enzyme-linked immunoassay) testing to PCR (polymerase chain reaction) testing instead was helpful in first-time infections because the latter is more sensitive for determining actual infection; however, if a patient has recurrent infection, the higher clinical specificity of PCR makes it harder to tell if a positive result is infection or simply colonization.
Some institutions have dropped ELISA testing altogether, Dr. Moss said, although he thinks the use of single molecule array testing is, with its exponential sensitivity, a “good half-way step” between ELISA and PCR, and is useful for determining who is colonized vs. who is actually producing the toxin, even at a very low level.
Dr. Moss disclosed he has consulted for Janssen, Theravance, and Seres, and has received research support from the National Institute for Diabetes, Digestive, and Kidney Disease, and Helmsley.
On Twitter @whitneymcknight
ORLANDO – You can confidently treat mild to severe Clostridium difficile infection in persons with inflammatory bowel disease, without disrupting their immunosuppression or other treatments, according to an expert.
“If your patient with IBD needs a fecal transplant for C. diff., you should not be concerned about withholding it,” Dr. Alan C. Moss said during a basic science presentation at a conference on inflammatory bowel diseases (IBD), sponsored by the Crohn’s and Colitis Foundation of America. Dr. Moss is an associate professor of medicine and the director of translational research at Harvard Medical School, Boston.
The first step, after you’ve determined that your patient has a true C. diff. infection, as opposed to having only been colonized by the bacteria, is choosing the best antibiotic. “Unfortunately, almost all IBD patients are excluded from controlled trials of antibiotics in C. diff. infection, so all we really have to go on are retrospective cohort data,” said Dr. Moss.
One such study, uncontrolled for disease severity, showed that a third of 114 inpatients with IBD who had a co-occurring C. diff. infection had higher 30-day readmission rates when treated first with metronidazole, per current standards of care, compared with the remaining two-thirds of patients who were treated first with vancomycin. The metronidazole group also averaged double the length of stays of the vancomycin group (Antimicrob Agents Chemother. 2014 Sep;58:5054-9 [doi: 10.1128/AAC.02606-13]).
“This suggests that in IBD patients, especially for those who meet criteria for a severe C. diff. infection, vancomycin is the way to go,” Dr. Moss said, noting a trend of metronidazole for mild infections in this cohort having ever less efficacy.
Beyond mild infection, Dr. Moss said the first line of treatment should be vancomycin 125 mg four times daily, or 500 mg four times daily if it is complicated disease.
If your patient has recurrent C. diff. infection, Dr. Moss recommended a prolonged taper of vancomycin, but to be vigilant about it being truly an infection and not a flare-up of colonized bacteria.
“My bar for doing fecal transplant in these patients has dropped considerably in the last few years, because if you really want to squeeze out the niche that C. diff. occupies in the microbiome, fecal transplant is really the most effective way we have of doing that,” Dr. Moss said.
While there is a division in the field over whether to continue immunosuppression during antibiotic treatment, Dr. Moss cited a small study indicating that if a patient were on two or more immunosuppressants, they had a higher risk of death, megacolon, or shock during C. diff. treatment. “I think it’s hard to draw many conclusions from that,” Dr. Moss said. “It may just be a surrogate marker of severity of disease rather than infection, per se.”
The standard of care for recurrent and refractory C. diff. infection is now fecal transplant, according to Dr. Moss. A recent study of fecal transplantation showed an 89% cure rate of C. diff. infection after a single fecal transplant in IBD patients. Of the 36 IBD patients in the study, half of whom were on biologic and immunosuppressive therapies, four experienced disease flare-ups (Am J Gastroenterol. 2014 Jul;109:1065-71 [doi: 10.1038/ajg.2014.133]. N Engl J Med. 2013 Jan 31;368:474-5 [doi: 10.1056/NEJMe1214816]).
As for determining if there is an actual infection rather than colonization of C. diff., Dr. Moss said switching from using ELISA (enzyme-linked immunoassay) testing to PCR (polymerase chain reaction) testing instead was helpful in first-time infections because the latter is more sensitive for determining actual infection; however, if a patient has recurrent infection, the higher clinical specificity of PCR makes it harder to tell if a positive result is infection or simply colonization.
Some institutions have dropped ELISA testing altogether, Dr. Moss said, although he thinks the use of single molecule array testing is, with its exponential sensitivity, a “good half-way step” between ELISA and PCR, and is useful for determining who is colonized vs. who is actually producing the toxin, even at a very low level.
Dr. Moss disclosed he has consulted for Janssen, Theravance, and Seres, and has received research support from the National Institute for Diabetes, Digestive, and Kidney Disease, and Helmsley.
On Twitter @whitneymcknight
ORLANDO – You can confidently treat mild to severe Clostridium difficile infection in persons with inflammatory bowel disease, without disrupting their immunosuppression or other treatments, according to an expert.
“If your patient with IBD needs a fecal transplant for C. diff., you should not be concerned about withholding it,” Dr. Alan C. Moss said during a basic science presentation at a conference on inflammatory bowel diseases (IBD), sponsored by the Crohn’s and Colitis Foundation of America. Dr. Moss is an associate professor of medicine and the director of translational research at Harvard Medical School, Boston.
The first step, after you’ve determined that your patient has a true C. diff. infection, as opposed to having only been colonized by the bacteria, is choosing the best antibiotic. “Unfortunately, almost all IBD patients are excluded from controlled trials of antibiotics in C. diff. infection, so all we really have to go on are retrospective cohort data,” said Dr. Moss.
One such study, uncontrolled for disease severity, showed that a third of 114 inpatients with IBD who had a co-occurring C. diff. infection had higher 30-day readmission rates when treated first with metronidazole, per current standards of care, compared with the remaining two-thirds of patients who were treated first with vancomycin. The metronidazole group also averaged double the length of stays of the vancomycin group (Antimicrob Agents Chemother. 2014 Sep;58:5054-9 [doi: 10.1128/AAC.02606-13]).
“This suggests that in IBD patients, especially for those who meet criteria for a severe C. diff. infection, vancomycin is the way to go,” Dr. Moss said, noting a trend of metronidazole for mild infections in this cohort having ever less efficacy.
Beyond mild infection, Dr. Moss said the first line of treatment should be vancomycin 125 mg four times daily, or 500 mg four times daily if it is complicated disease.
If your patient has recurrent C. diff. infection, Dr. Moss recommended a prolonged taper of vancomycin, but to be vigilant about it being truly an infection and not a flare-up of colonized bacteria.
“My bar for doing fecal transplant in these patients has dropped considerably in the last few years, because if you really want to squeeze out the niche that C. diff. occupies in the microbiome, fecal transplant is really the most effective way we have of doing that,” Dr. Moss said.
While there is a division in the field over whether to continue immunosuppression during antibiotic treatment, Dr. Moss cited a small study indicating that if a patient were on two or more immunosuppressants, they had a higher risk of death, megacolon, or shock during C. diff. treatment. “I think it’s hard to draw many conclusions from that,” Dr. Moss said. “It may just be a surrogate marker of severity of disease rather than infection, per se.”
The standard of care for recurrent and refractory C. diff. infection is now fecal transplant, according to Dr. Moss. A recent study of fecal transplantation showed an 89% cure rate of C. diff. infection after a single fecal transplant in IBD patients. Of the 36 IBD patients in the study, half of whom were on biologic and immunosuppressive therapies, four experienced disease flare-ups (Am J Gastroenterol. 2014 Jul;109:1065-71 [doi: 10.1038/ajg.2014.133]. N Engl J Med. 2013 Jan 31;368:474-5 [doi: 10.1056/NEJMe1214816]).
As for determining if there is an actual infection rather than colonization of C. diff., Dr. Moss said switching from using ELISA (enzyme-linked immunoassay) testing to PCR (polymerase chain reaction) testing instead was helpful in first-time infections because the latter is more sensitive for determining actual infection; however, if a patient has recurrent infection, the higher clinical specificity of PCR makes it harder to tell if a positive result is infection or simply colonization.
Some institutions have dropped ELISA testing altogether, Dr. Moss said, although he thinks the use of single molecule array testing is, with its exponential sensitivity, a “good half-way step” between ELISA and PCR, and is useful for determining who is colonized vs. who is actually producing the toxin, even at a very low level.
Dr. Moss disclosed he has consulted for Janssen, Theravance, and Seres, and has received research support from the National Institute for Diabetes, Digestive, and Kidney Disease, and Helmsley.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM 2015 ADVANCES IN IBD
Is metformin a future preeclampsia treatment?
Metformin decreased toxin levels implicated in preeclampsia, while also helping to heal injured omental blood vessels, researchers in Australia have reported.
Since the drug, a common treatment for type 2 diabetes, is already proven safe during pregnancy, the study’s lead author Dr. Fiona Brownfoot said clinical trials to test metformin’s efficacy in preventing and treating preeclampsia are “justified”. The findings were published online Dec. 22 in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2015.12.019).
Preeclampsia is characterized by elevated levels of soluble vascular endothelial growth factor receptor 1 and soluble endoglin, toxins produced by the placenta. When elevated, these toxins tend to damage endothelial cells, manifesting clinically as hypertension and multisystem organ injury. Preeclampsia occurs in 5%-8% of pregnancies, presenting after week 20 of gestation with new-onset hypertension and proteinuria. Since there have been no agents or drugs to decrease the production of these toxins in pregnancy, the only treatment options for preeclampsia are expectant management and delivery.
Dr. Brownfoot, a researcher in the Translational Obstetrics Group in the department of obstetrics and gynecology at the University of Melbourne and her associates found that when endothelial and placental cells taken from 23 women diagnosed with severe preterm proteinuric preeclampsia were incubated with metformin, there were improvements in endothelial dysfunction when compared with 25 gestationally matched controls. Metformin was also shown to improve whole blood vessel angiogenesis impaired by elevated toxin levels.
“Metformin appears to be the aspirin of the 21st century,” Dr. Roberto Romero, editor-in-chief of the American Journal of Obstetrics and Gynecology, said in a statement.
Noting metformin’s use in diabetes as well as in polycystic ovarian disease, and its recently discovered anticancer properties, Dr. Romero said the recent findings are “exciting and promising,” particularly since antiangiogenesis occurs not only in preeclampsia, but in other pregnancy complications such as fetal death, fetal growth restriction, and premature labor. He called for systematic reviews of previous randomized clinical trials of metformin in pregnant women, as well as new randomized studies to determine the effectiveness of metformin in preventing preeclampsia.
The work was funded by the National Health and Medical Research Council of Australia. The researchers reported having no conflicts of interest.
On Twitter @whitneymcknight
Metformin decreased toxin levels implicated in preeclampsia, while also helping to heal injured omental blood vessels, researchers in Australia have reported.
Since the drug, a common treatment for type 2 diabetes, is already proven safe during pregnancy, the study’s lead author Dr. Fiona Brownfoot said clinical trials to test metformin’s efficacy in preventing and treating preeclampsia are “justified”. The findings were published online Dec. 22 in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2015.12.019).
Preeclampsia is characterized by elevated levels of soluble vascular endothelial growth factor receptor 1 and soluble endoglin, toxins produced by the placenta. When elevated, these toxins tend to damage endothelial cells, manifesting clinically as hypertension and multisystem organ injury. Preeclampsia occurs in 5%-8% of pregnancies, presenting after week 20 of gestation with new-onset hypertension and proteinuria. Since there have been no agents or drugs to decrease the production of these toxins in pregnancy, the only treatment options for preeclampsia are expectant management and delivery.
Dr. Brownfoot, a researcher in the Translational Obstetrics Group in the department of obstetrics and gynecology at the University of Melbourne and her associates found that when endothelial and placental cells taken from 23 women diagnosed with severe preterm proteinuric preeclampsia were incubated with metformin, there were improvements in endothelial dysfunction when compared with 25 gestationally matched controls. Metformin was also shown to improve whole blood vessel angiogenesis impaired by elevated toxin levels.
“Metformin appears to be the aspirin of the 21st century,” Dr. Roberto Romero, editor-in-chief of the American Journal of Obstetrics and Gynecology, said in a statement.
Noting metformin’s use in diabetes as well as in polycystic ovarian disease, and its recently discovered anticancer properties, Dr. Romero said the recent findings are “exciting and promising,” particularly since antiangiogenesis occurs not only in preeclampsia, but in other pregnancy complications such as fetal death, fetal growth restriction, and premature labor. He called for systematic reviews of previous randomized clinical trials of metformin in pregnant women, as well as new randomized studies to determine the effectiveness of metformin in preventing preeclampsia.
The work was funded by the National Health and Medical Research Council of Australia. The researchers reported having no conflicts of interest.
On Twitter @whitneymcknight
Metformin decreased toxin levels implicated in preeclampsia, while also helping to heal injured omental blood vessels, researchers in Australia have reported.
Since the drug, a common treatment for type 2 diabetes, is already proven safe during pregnancy, the study’s lead author Dr. Fiona Brownfoot said clinical trials to test metformin’s efficacy in preventing and treating preeclampsia are “justified”. The findings were published online Dec. 22 in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2015.12.019).
Preeclampsia is characterized by elevated levels of soluble vascular endothelial growth factor receptor 1 and soluble endoglin, toxins produced by the placenta. When elevated, these toxins tend to damage endothelial cells, manifesting clinically as hypertension and multisystem organ injury. Preeclampsia occurs in 5%-8% of pregnancies, presenting after week 20 of gestation with new-onset hypertension and proteinuria. Since there have been no agents or drugs to decrease the production of these toxins in pregnancy, the only treatment options for preeclampsia are expectant management and delivery.
Dr. Brownfoot, a researcher in the Translational Obstetrics Group in the department of obstetrics and gynecology at the University of Melbourne and her associates found that when endothelial and placental cells taken from 23 women diagnosed with severe preterm proteinuric preeclampsia were incubated with metformin, there were improvements in endothelial dysfunction when compared with 25 gestationally matched controls. Metformin was also shown to improve whole blood vessel angiogenesis impaired by elevated toxin levels.
“Metformin appears to be the aspirin of the 21st century,” Dr. Roberto Romero, editor-in-chief of the American Journal of Obstetrics and Gynecology, said in a statement.
Noting metformin’s use in diabetes as well as in polycystic ovarian disease, and its recently discovered anticancer properties, Dr. Romero said the recent findings are “exciting and promising,” particularly since antiangiogenesis occurs not only in preeclampsia, but in other pregnancy complications such as fetal death, fetal growth restriction, and premature labor. He called for systematic reviews of previous randomized clinical trials of metformin in pregnant women, as well as new randomized studies to determine the effectiveness of metformin in preventing preeclampsia.
The work was funded by the National Health and Medical Research Council of Australia. The researchers reported having no conflicts of interest.
On Twitter @whitneymcknight
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Eighty percent of ED physicians say mental health crisis response needs overhaul
After a survey found that 80% of 1,500 U.S. emergency physicians think the system for treating persons in acute mental health crisis is broken, emergency medicine professionals teamed up with mental health workers and patient advocates nationwide to call for a new model of care.
The Coalition on Psychiatric Emergencies, or COPE, is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the American College of Emergency Physicians, the American Psychiatric Association, and the National Alliance on Mental Illness.
“It’s time we think about doing things differently,” Dr. Michael J. Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents in the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
COPE also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, said in an interview. “Establishing these new systems will likely require robust funding efforts.
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr. Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the U.S., there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1-31, 2015. The response rate was 6% and the margin of error of 2.5 percent.
On Twitter @whitneymcknight
After a survey found that 80% of 1,500 U.S. emergency physicians think the system for treating persons in acute mental health crisis is broken, emergency medicine professionals teamed up with mental health workers and patient advocates nationwide to call for a new model of care.
The Coalition on Psychiatric Emergencies, or COPE, is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the American College of Emergency Physicians, the American Psychiatric Association, and the National Alliance on Mental Illness.
“It’s time we think about doing things differently,” Dr. Michael J. Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents in the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
COPE also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, said in an interview. “Establishing these new systems will likely require robust funding efforts.
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr. Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the U.S., there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1-31, 2015. The response rate was 6% and the margin of error of 2.5 percent.
On Twitter @whitneymcknight
After a survey found that 80% of 1,500 U.S. emergency physicians think the system for treating persons in acute mental health crisis is broken, emergency medicine professionals teamed up with mental health workers and patient advocates nationwide to call for a new model of care.
The Coalition on Psychiatric Emergencies, or COPE, is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the American College of Emergency Physicians, the American Psychiatric Association, and the National Alliance on Mental Illness.
“It’s time we think about doing things differently,” Dr. Michael J. Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents in the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
COPE also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, said in an interview. “Establishing these new systems will likely require robust funding efforts.
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr. Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the U.S., there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1-31, 2015. The response rate was 6% and the margin of error of 2.5 percent.
On Twitter @whitneymcknight
Key clinical point: A new model of psychiatric ED care is being developed by the Coalition on Psychiatric Emergencies (COPE), to improve care, outcomes, and net costs.
Major finding: Eight in 10 emergency physicians believe a lack of training and resources keeps them from meeting a growing demand for emergency mental health services.
Data source: American College of Emergency Physicians survey of 1,500 physicians nationwide.
Disclosures: COPE is underwritten in part by Teva Pharmaceuticals.
Biosimilars primer: What you need to know now
ORLANDO – Regardless of what you think about using biosimilars, chances are you won’t be able to avoid using them if you already use biologics.
That’s according to Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago. “They’re coming and they will influence our practice, ” he told a clinical track audience at a conference on inflammatory bowel disease.
Before exploring how these medications may change how you treat patients, here’s a look at what they are and how they’re brought to market.
First, a little basic science review of small-molecule medications vs. biologic ones. Small-molecule agents are simple structures, which are stable enough to be replicated, do not tend to cause immunogenicity, and require very little in the way of testing for quality assurance.
By contrast, biologic medicines, including monoclonal antibodies, are complex structures – in some cases, highly complex – that are replicable, but often with a high degree of difficulty. Unlike small-molecule medicines, biologic drugs cannot be mass produced and require almost 250 sophisticated tests to ensure quality. They are less stable and can trigger an immunogenic response. The manufacturing process for biologics is so precise that the slightest disturbance in development can affect whether the medication is functional.
As a result, the typical development timeline for these medications is between 7 and 8 years, with costs running as high as $250 million each. Currently, there are more than 650 recombinant therapeutics in development worldwide, more than half of which are in the preclinical stage. The top original products being copied are adalimumab at 13, and infliximab with 9. Meanwhile, at least five as-of-yet unpublished studies are looking at how these potential adalimumab and infliximab biosimilars perform in inflammatory bowel disease (IBD), Dr. Rubin said. Biosimilars are used worldwide, primarily in Europe and Asia.
But when these biosimilars reach our shores, don’t call them generics. “I encourage you to not use that term, even when discussing them with patients,” Dr. Rubin said. Still, because the Food and Drug Administration says that a biosimilar should have no greater risk for adverse events or diminished efficacy compared with the original biologic just as with generics, pharmacists are within their rights to substitute biosimilars for original biologics without prescriber intervention.
That’s why, “There must be pharmacovigilance with biosimilars, just like with generics, after the drug is brought to market,” Dr. Rubin said.
Biosimilars are also not “biobetters,” medications that have modifications added to the original biologic product in order to improve their clinical performance. While biobetters can be patented, they do not have legal or regulatory status, however, because they are considered new drugs.
The FDA defines biosimilars as a biological product that is highly similar to the reference product, with no clinically meaningful safety, purity, or potency differences from the reference product.
Early in 2015, the biosimilar filgrastim-sndz (Zarxio TM, Sandoz-Novartis), which has been available in Europe since 2009, entered the U.S. market. With its biosimilarity to Filgrastim (Sandoz-Novartis), the medication’s primary indications are for various cancers and chronic neutropenia.
To help expedite bringing the medications to market, FDA guidance data requirements for biosimilars is abbreviated when compared with that for biologics. Rather than ask developers to conduct clinical trials, developers must provide at least one comparative study between the biosimilar and its original, according to the original drug’s indication. There also is what Dr. Rubin called a “weighted reliance” on analytical similarity to the original. In addition, no phase II dose-ranging studies are required. Indication extrapolation is also possible, meaning that safety and efficacy data leading to a biosimilar being approved for say, rheumatoid arthritis, could also be applied to Crohn’s disease.
So, what does all this mean for your patients? It depends upon in which state you practice: Even when a recombinant product meets the FDA criteria, whether or not a patient can be placed on a biosimilar comes down to state regulation. At present, 19 states have passed laws as to how and when biosimilars can be swapped out, most of them stipulating that a patient be notified when it occurs. Physicians maintain their rights to ask pharmacists to “dispense as written,” but since biosimilars are cheaper than their originals, you won’t necessarily get around mounting pressure from third-party payers to contain costs.
Dr. Rubin said this potential friction between insurers and physicians could result in delays with adverse effect on the patient. “If the insurance company says they prefer another agent over the one a patient is receiving, we all know about the unexpected delays that can occur when switching.”
Dr. Rubin predicted that the logistics of prescribing will be complicated by pharmaceutical marketing efforts. He noted the similar names of Remsima (Hospira) vs. Remicade (Janssen), Inflectra (Hospira) vs. infliximab generic. “It could be confusing for all of us.”
The question of how the drug will fare once inside the patient is still a matter of debate.
“The major issue is immunogenicity ... it’s impossible to predict in vitro,” said Dr. Brian Feagan, a copanelist with Dr. Rubin, and a professor of medicine at the University of Western Ontario in London, Canada. “Immunogenicity is determined by product-related factors, and a lot of clinical ones such as immunosuppression, coadministration, route of administration, disease-specific factors.”
The only way to truly determine the impact on immunogenicity of interchangeability, whether because of third-party payer stipulations or physician’s choice, is to do multiple switching trials, said Dr. Feagan.
But Dr. Stephen B. Hanauer, the Clifford Joseph Barborka Professor of Medicine in Gastroenterology and Hepatology at Northwestern University (Chicago), said that’s not likely to happen. “There’s no time for that as the FDA regulatory evaluation proceeds,” he said in an interview.
“The trial would take 2 years to accomplish, would need large numbers of patients in order to identify potential small differences, and would be too expensive.” All of which would defeat the purpose of the expedited approval process, Dr. Hanauer said, because the decision by Congress to give biosimilars the green light was to reduce cost.
On the other hand, said Dr. Feagan, the experiment on switching probably has already been done. That’s because despite what he referred to as efforts by pharmaceutical manufacturers to reassure physicians there is no drift from the original product, heterogeneity is inevitable.
These iterative qualities, according to Dr. Hanauer, essentially make the original products into biosimilars of themselves. Add to that, he said that depending upon the company used to perform the assays to determine immunogenicity, the range of results can vary widely, and you end up having to learn to live with a certain amount of uncertainty. “I’m not afraid of biosimilars,” Dr. Hanauer said while discussing biosimilars during an audience question time at the meeting.
“We are a little bit timid about biosimilars, but my sense is we will find our comfort level in the next few years, and we will start using them frequently,” Dr. Miguel Regueiro, medical director of the IBD Center at the University of Pittsburgh, said in an interview. “I think immunogenicity to biosimilars will be the same immunogenicity to the innovative biologics, but I don’t think we’re going to be comfortable with interchanging a biosimilar with a[n] original biologic because of the potential immunogenicity that can occur by switching between agents.”
Whether biosimilars can be used in place of their originals, said both Dr. Feagan and Dr. Hanauer, will come down to how extrapolated data is interpreted.
“I think the biggest debate the FDA is going to have [when indicating biosimilars for IBD] is overextrapolation,” Dr. Hanauer said in the interview. Since the FDA does not require clinical trials for biosimilars, but relies upon analytics instead, and because there are far less clinical data for biologics in IBD than there are for diseases such as rheumatoid or psoriatic arthritis, manufacturers will turn to those studies to demonstrate efficacy between originals and recombinants. “If 99.9% of the analytic assays and the clinical data in rheumatoid arthritis are virtually the same, I would assume that the data in inflammatory bowel disease is going to be virtually the same.”
However, at least in Canada, that was not the opinion of regulators who decided against approving the extrapolation of infliximab clinical data for indicating its biosimilar in IBD, but did allow extrapolation of the data for rheumatoid arthritis. “Health Canada decided that the antibody-dependent, cell-mediated cytotoxicity was different for IBD,” said Dr. Feagan.
Predicting the primacy of cost over keeping patients in remission, but at least for now, Dr. Rubin said the question of cost is “huge. Based on the European and Asian experience, the day one of these new products becomes available, the price of the existing therapies drops anywhere from 15% to 30%.”
Recent data places the cost of remission in the United States using infliximab at about $15,000.
Dr. Regueiro said these market forces are a good thing. “I don’t look at biosimilars in a negative context whatsoever. I think they are a necessary part of health care reform. Cost is definitely a driver, and that’s not bad.”
The meeting was sponsored by the Crohn’s & Colitis Foundation of America. Dr. Rubin has financial and consulting relationships with AbbVie, Janssen, Takeda, and numerous other pharmaceutical companies. Dr. Feagan has numerous relationships with pharmaceutical companies, including Abbott, Janssen, Teva, and others. Dr. Hanauer has served on the board of AbbVie and has financial relationships with numerous other pharmaceutical manufacturers. Dr. Regueiro did not have any disclosures relevant to this story.
On Twitter @whitneymcknight
This article was updated 1/6/16.
ORLANDO – Regardless of what you think about using biosimilars, chances are you won’t be able to avoid using them if you already use biologics.
That’s according to Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago. “They’re coming and they will influence our practice, ” he told a clinical track audience at a conference on inflammatory bowel disease.
Before exploring how these medications may change how you treat patients, here’s a look at what they are and how they’re brought to market.
First, a little basic science review of small-molecule medications vs. biologic ones. Small-molecule agents are simple structures, which are stable enough to be replicated, do not tend to cause immunogenicity, and require very little in the way of testing for quality assurance.
By contrast, biologic medicines, including monoclonal antibodies, are complex structures – in some cases, highly complex – that are replicable, but often with a high degree of difficulty. Unlike small-molecule medicines, biologic drugs cannot be mass produced and require almost 250 sophisticated tests to ensure quality. They are less stable and can trigger an immunogenic response. The manufacturing process for biologics is so precise that the slightest disturbance in development can affect whether the medication is functional.
As a result, the typical development timeline for these medications is between 7 and 8 years, with costs running as high as $250 million each. Currently, there are more than 650 recombinant therapeutics in development worldwide, more than half of which are in the preclinical stage. The top original products being copied are adalimumab at 13, and infliximab with 9. Meanwhile, at least five as-of-yet unpublished studies are looking at how these potential adalimumab and infliximab biosimilars perform in inflammatory bowel disease (IBD), Dr. Rubin said. Biosimilars are used worldwide, primarily in Europe and Asia.
But when these biosimilars reach our shores, don’t call them generics. “I encourage you to not use that term, even when discussing them with patients,” Dr. Rubin said. Still, because the Food and Drug Administration says that a biosimilar should have no greater risk for adverse events or diminished efficacy compared with the original biologic just as with generics, pharmacists are within their rights to substitute biosimilars for original biologics without prescriber intervention.
That’s why, “There must be pharmacovigilance with biosimilars, just like with generics, after the drug is brought to market,” Dr. Rubin said.
Biosimilars are also not “biobetters,” medications that have modifications added to the original biologic product in order to improve their clinical performance. While biobetters can be patented, they do not have legal or regulatory status, however, because they are considered new drugs.
The FDA defines biosimilars as a biological product that is highly similar to the reference product, with no clinically meaningful safety, purity, or potency differences from the reference product.
Early in 2015, the biosimilar filgrastim-sndz (Zarxio TM, Sandoz-Novartis), which has been available in Europe since 2009, entered the U.S. market. With its biosimilarity to Filgrastim (Sandoz-Novartis), the medication’s primary indications are for various cancers and chronic neutropenia.
To help expedite bringing the medications to market, FDA guidance data requirements for biosimilars is abbreviated when compared with that for biologics. Rather than ask developers to conduct clinical trials, developers must provide at least one comparative study between the biosimilar and its original, according to the original drug’s indication. There also is what Dr. Rubin called a “weighted reliance” on analytical similarity to the original. In addition, no phase II dose-ranging studies are required. Indication extrapolation is also possible, meaning that safety and efficacy data leading to a biosimilar being approved for say, rheumatoid arthritis, could also be applied to Crohn’s disease.
So, what does all this mean for your patients? It depends upon in which state you practice: Even when a recombinant product meets the FDA criteria, whether or not a patient can be placed on a biosimilar comes down to state regulation. At present, 19 states have passed laws as to how and when biosimilars can be swapped out, most of them stipulating that a patient be notified when it occurs. Physicians maintain their rights to ask pharmacists to “dispense as written,” but since biosimilars are cheaper than their originals, you won’t necessarily get around mounting pressure from third-party payers to contain costs.
Dr. Rubin said this potential friction between insurers and physicians could result in delays with adverse effect on the patient. “If the insurance company says they prefer another agent over the one a patient is receiving, we all know about the unexpected delays that can occur when switching.”
Dr. Rubin predicted that the logistics of prescribing will be complicated by pharmaceutical marketing efforts. He noted the similar names of Remsima (Hospira) vs. Remicade (Janssen), Inflectra (Hospira) vs. infliximab generic. “It could be confusing for all of us.”
The question of how the drug will fare once inside the patient is still a matter of debate.
“The major issue is immunogenicity ... it’s impossible to predict in vitro,” said Dr. Brian Feagan, a copanelist with Dr. Rubin, and a professor of medicine at the University of Western Ontario in London, Canada. “Immunogenicity is determined by product-related factors, and a lot of clinical ones such as immunosuppression, coadministration, route of administration, disease-specific factors.”
The only way to truly determine the impact on immunogenicity of interchangeability, whether because of third-party payer stipulations or physician’s choice, is to do multiple switching trials, said Dr. Feagan.
But Dr. Stephen B. Hanauer, the Clifford Joseph Barborka Professor of Medicine in Gastroenterology and Hepatology at Northwestern University (Chicago), said that’s not likely to happen. “There’s no time for that as the FDA regulatory evaluation proceeds,” he said in an interview.
“The trial would take 2 years to accomplish, would need large numbers of patients in order to identify potential small differences, and would be too expensive.” All of which would defeat the purpose of the expedited approval process, Dr. Hanauer said, because the decision by Congress to give biosimilars the green light was to reduce cost.
On the other hand, said Dr. Feagan, the experiment on switching probably has already been done. That’s because despite what he referred to as efforts by pharmaceutical manufacturers to reassure physicians there is no drift from the original product, heterogeneity is inevitable.
These iterative qualities, according to Dr. Hanauer, essentially make the original products into biosimilars of themselves. Add to that, he said that depending upon the company used to perform the assays to determine immunogenicity, the range of results can vary widely, and you end up having to learn to live with a certain amount of uncertainty. “I’m not afraid of biosimilars,” Dr. Hanauer said while discussing biosimilars during an audience question time at the meeting.
“We are a little bit timid about biosimilars, but my sense is we will find our comfort level in the next few years, and we will start using them frequently,” Dr. Miguel Regueiro, medical director of the IBD Center at the University of Pittsburgh, said in an interview. “I think immunogenicity to biosimilars will be the same immunogenicity to the innovative biologics, but I don’t think we’re going to be comfortable with interchanging a biosimilar with a[n] original biologic because of the potential immunogenicity that can occur by switching between agents.”
Whether biosimilars can be used in place of their originals, said both Dr. Feagan and Dr. Hanauer, will come down to how extrapolated data is interpreted.
“I think the biggest debate the FDA is going to have [when indicating biosimilars for IBD] is overextrapolation,” Dr. Hanauer said in the interview. Since the FDA does not require clinical trials for biosimilars, but relies upon analytics instead, and because there are far less clinical data for biologics in IBD than there are for diseases such as rheumatoid or psoriatic arthritis, manufacturers will turn to those studies to demonstrate efficacy between originals and recombinants. “If 99.9% of the analytic assays and the clinical data in rheumatoid arthritis are virtually the same, I would assume that the data in inflammatory bowel disease is going to be virtually the same.”
However, at least in Canada, that was not the opinion of regulators who decided against approving the extrapolation of infliximab clinical data for indicating its biosimilar in IBD, but did allow extrapolation of the data for rheumatoid arthritis. “Health Canada decided that the antibody-dependent, cell-mediated cytotoxicity was different for IBD,” said Dr. Feagan.
Predicting the primacy of cost over keeping patients in remission, but at least for now, Dr. Rubin said the question of cost is “huge. Based on the European and Asian experience, the day one of these new products becomes available, the price of the existing therapies drops anywhere from 15% to 30%.”
Recent data places the cost of remission in the United States using infliximab at about $15,000.
Dr. Regueiro said these market forces are a good thing. “I don’t look at biosimilars in a negative context whatsoever. I think they are a necessary part of health care reform. Cost is definitely a driver, and that’s not bad.”
The meeting was sponsored by the Crohn’s & Colitis Foundation of America. Dr. Rubin has financial and consulting relationships with AbbVie, Janssen, Takeda, and numerous other pharmaceutical companies. Dr. Feagan has numerous relationships with pharmaceutical companies, including Abbott, Janssen, Teva, and others. Dr. Hanauer has served on the board of AbbVie and has financial relationships with numerous other pharmaceutical manufacturers. Dr. Regueiro did not have any disclosures relevant to this story.
On Twitter @whitneymcknight
This article was updated 1/6/16.
ORLANDO – Regardless of what you think about using biosimilars, chances are you won’t be able to avoid using them if you already use biologics.
That’s according to Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago. “They’re coming and they will influence our practice, ” he told a clinical track audience at a conference on inflammatory bowel disease.
Before exploring how these medications may change how you treat patients, here’s a look at what they are and how they’re brought to market.
First, a little basic science review of small-molecule medications vs. biologic ones. Small-molecule agents are simple structures, which are stable enough to be replicated, do not tend to cause immunogenicity, and require very little in the way of testing for quality assurance.
By contrast, biologic medicines, including monoclonal antibodies, are complex structures – in some cases, highly complex – that are replicable, but often with a high degree of difficulty. Unlike small-molecule medicines, biologic drugs cannot be mass produced and require almost 250 sophisticated tests to ensure quality. They are less stable and can trigger an immunogenic response. The manufacturing process for biologics is so precise that the slightest disturbance in development can affect whether the medication is functional.
As a result, the typical development timeline for these medications is between 7 and 8 years, with costs running as high as $250 million each. Currently, there are more than 650 recombinant therapeutics in development worldwide, more than half of which are in the preclinical stage. The top original products being copied are adalimumab at 13, and infliximab with 9. Meanwhile, at least five as-of-yet unpublished studies are looking at how these potential adalimumab and infliximab biosimilars perform in inflammatory bowel disease (IBD), Dr. Rubin said. Biosimilars are used worldwide, primarily in Europe and Asia.
But when these biosimilars reach our shores, don’t call them generics. “I encourage you to not use that term, even when discussing them with patients,” Dr. Rubin said. Still, because the Food and Drug Administration says that a biosimilar should have no greater risk for adverse events or diminished efficacy compared with the original biologic just as with generics, pharmacists are within their rights to substitute biosimilars for original biologics without prescriber intervention.
That’s why, “There must be pharmacovigilance with biosimilars, just like with generics, after the drug is brought to market,” Dr. Rubin said.
Biosimilars are also not “biobetters,” medications that have modifications added to the original biologic product in order to improve their clinical performance. While biobetters can be patented, they do not have legal or regulatory status, however, because they are considered new drugs.
The FDA defines biosimilars as a biological product that is highly similar to the reference product, with no clinically meaningful safety, purity, or potency differences from the reference product.
Early in 2015, the biosimilar filgrastim-sndz (Zarxio TM, Sandoz-Novartis), which has been available in Europe since 2009, entered the U.S. market. With its biosimilarity to Filgrastim (Sandoz-Novartis), the medication’s primary indications are for various cancers and chronic neutropenia.
To help expedite bringing the medications to market, FDA guidance data requirements for biosimilars is abbreviated when compared with that for biologics. Rather than ask developers to conduct clinical trials, developers must provide at least one comparative study between the biosimilar and its original, according to the original drug’s indication. There also is what Dr. Rubin called a “weighted reliance” on analytical similarity to the original. In addition, no phase II dose-ranging studies are required. Indication extrapolation is also possible, meaning that safety and efficacy data leading to a biosimilar being approved for say, rheumatoid arthritis, could also be applied to Crohn’s disease.
So, what does all this mean for your patients? It depends upon in which state you practice: Even when a recombinant product meets the FDA criteria, whether or not a patient can be placed on a biosimilar comes down to state regulation. At present, 19 states have passed laws as to how and when biosimilars can be swapped out, most of them stipulating that a patient be notified when it occurs. Physicians maintain their rights to ask pharmacists to “dispense as written,” but since biosimilars are cheaper than their originals, you won’t necessarily get around mounting pressure from third-party payers to contain costs.
Dr. Rubin said this potential friction between insurers and physicians could result in delays with adverse effect on the patient. “If the insurance company says they prefer another agent over the one a patient is receiving, we all know about the unexpected delays that can occur when switching.”
Dr. Rubin predicted that the logistics of prescribing will be complicated by pharmaceutical marketing efforts. He noted the similar names of Remsima (Hospira) vs. Remicade (Janssen), Inflectra (Hospira) vs. infliximab generic. “It could be confusing for all of us.”
The question of how the drug will fare once inside the patient is still a matter of debate.
“The major issue is immunogenicity ... it’s impossible to predict in vitro,” said Dr. Brian Feagan, a copanelist with Dr. Rubin, and a professor of medicine at the University of Western Ontario in London, Canada. “Immunogenicity is determined by product-related factors, and a lot of clinical ones such as immunosuppression, coadministration, route of administration, disease-specific factors.”
The only way to truly determine the impact on immunogenicity of interchangeability, whether because of third-party payer stipulations or physician’s choice, is to do multiple switching trials, said Dr. Feagan.
But Dr. Stephen B. Hanauer, the Clifford Joseph Barborka Professor of Medicine in Gastroenterology and Hepatology at Northwestern University (Chicago), said that’s not likely to happen. “There’s no time for that as the FDA regulatory evaluation proceeds,” he said in an interview.
“The trial would take 2 years to accomplish, would need large numbers of patients in order to identify potential small differences, and would be too expensive.” All of which would defeat the purpose of the expedited approval process, Dr. Hanauer said, because the decision by Congress to give biosimilars the green light was to reduce cost.
On the other hand, said Dr. Feagan, the experiment on switching probably has already been done. That’s because despite what he referred to as efforts by pharmaceutical manufacturers to reassure physicians there is no drift from the original product, heterogeneity is inevitable.
These iterative qualities, according to Dr. Hanauer, essentially make the original products into biosimilars of themselves. Add to that, he said that depending upon the company used to perform the assays to determine immunogenicity, the range of results can vary widely, and you end up having to learn to live with a certain amount of uncertainty. “I’m not afraid of biosimilars,” Dr. Hanauer said while discussing biosimilars during an audience question time at the meeting.
“We are a little bit timid about biosimilars, but my sense is we will find our comfort level in the next few years, and we will start using them frequently,” Dr. Miguel Regueiro, medical director of the IBD Center at the University of Pittsburgh, said in an interview. “I think immunogenicity to biosimilars will be the same immunogenicity to the innovative biologics, but I don’t think we’re going to be comfortable with interchanging a biosimilar with a[n] original biologic because of the potential immunogenicity that can occur by switching between agents.”
Whether biosimilars can be used in place of their originals, said both Dr. Feagan and Dr. Hanauer, will come down to how extrapolated data is interpreted.
“I think the biggest debate the FDA is going to have [when indicating biosimilars for IBD] is overextrapolation,” Dr. Hanauer said in the interview. Since the FDA does not require clinical trials for biosimilars, but relies upon analytics instead, and because there are far less clinical data for biologics in IBD than there are for diseases such as rheumatoid or psoriatic arthritis, manufacturers will turn to those studies to demonstrate efficacy between originals and recombinants. “If 99.9% of the analytic assays and the clinical data in rheumatoid arthritis are virtually the same, I would assume that the data in inflammatory bowel disease is going to be virtually the same.”
However, at least in Canada, that was not the opinion of regulators who decided against approving the extrapolation of infliximab clinical data for indicating its biosimilar in IBD, but did allow extrapolation of the data for rheumatoid arthritis. “Health Canada decided that the antibody-dependent, cell-mediated cytotoxicity was different for IBD,” said Dr. Feagan.
Predicting the primacy of cost over keeping patients in remission, but at least for now, Dr. Rubin said the question of cost is “huge. Based on the European and Asian experience, the day one of these new products becomes available, the price of the existing therapies drops anywhere from 15% to 30%.”
Recent data places the cost of remission in the United States using infliximab at about $15,000.
Dr. Regueiro said these market forces are a good thing. “I don’t look at biosimilars in a negative context whatsoever. I think they are a necessary part of health care reform. Cost is definitely a driver, and that’s not bad.”
The meeting was sponsored by the Crohn’s & Colitis Foundation of America. Dr. Rubin has financial and consulting relationships with AbbVie, Janssen, Takeda, and numerous other pharmaceutical companies. Dr. Feagan has numerous relationships with pharmaceutical companies, including Abbott, Janssen, Teva, and others. Dr. Hanauer has served on the board of AbbVie and has financial relationships with numerous other pharmaceutical manufacturers. Dr. Regueiro did not have any disclosures relevant to this story.
On Twitter @whitneymcknight
This article was updated 1/6/16.
EXPERT ANALYSIS FROM 2015 ADVANCES IN IBD
AGA publishes microscopic colitis guideline
A microscopic colitis treatment guideline from the American Gastroenterological Association was published in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2015.11.008).
Microscopic colitis is most common in persons aged 60 years and over, typically presents as chronic watery diarrhea with nausea or abdominal pain caused by inflammation in the colon, and is diagnosed by colonic biopsy. It is more of a nuisance than life threatening, with no evidence that the persistent histologic inflammation predicts colorectal cancer or the need for surgical intervention.
The guideline strongly recommends, with moderate-quality evidence, treating symptomatic patients with budesonide rather than foregoing any treatment. The AGA also strongly recommends, with high-quality evidence, that budesonide be used over mesalamine to induce remission, unless such treatment is not feasible in a patient because of a drug reaction or its high price. In that case, the AGA recommends (with moderate-quality evidence) the use of mesalamine. Once induction therapy is discontinued, the AGA strongly recommends, with moderate-quality evidence, maintenance treatment using budesonide, if possible.
In patients for whom budesonide is not feasible, the AGA recommends that rather than forgo treatment, patients may be induced with bismuth subsalicylate (low-quality evidence) or prednisone (very-low-quality evidence).
Other recommendations made with low-quality evidence for treating symptomatic microscopic colitis include not using combination therapy with cholestyramine and mesalamine over mesalamine alone for induction therapy, nor Boswellia serrata to induce remission. The AGA also does not recommend (low-quality evidence) using probiotics over no treatment for the condition.
Because the meta-analysis of evidence conducted by the AGA only included data derived from clinical trials, the guideline does not include antidiarrheals, cholestyramine monotherapy, a variety of combination therapies, nor the medical treatment of steroid-refractory microscopic colitis, although the AGA did note in the guideline that very limited evidence from a series of cases suggests certain immunosuppressive therapies may benefit these patients.
On Twitter @whitneymcknight
A microscopic colitis treatment guideline from the American Gastroenterological Association was published in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2015.11.008).
Microscopic colitis is most common in persons aged 60 years and over, typically presents as chronic watery diarrhea with nausea or abdominal pain caused by inflammation in the colon, and is diagnosed by colonic biopsy. It is more of a nuisance than life threatening, with no evidence that the persistent histologic inflammation predicts colorectal cancer or the need for surgical intervention.
The guideline strongly recommends, with moderate-quality evidence, treating symptomatic patients with budesonide rather than foregoing any treatment. The AGA also strongly recommends, with high-quality evidence, that budesonide be used over mesalamine to induce remission, unless such treatment is not feasible in a patient because of a drug reaction or its high price. In that case, the AGA recommends (with moderate-quality evidence) the use of mesalamine. Once induction therapy is discontinued, the AGA strongly recommends, with moderate-quality evidence, maintenance treatment using budesonide, if possible.
In patients for whom budesonide is not feasible, the AGA recommends that rather than forgo treatment, patients may be induced with bismuth subsalicylate (low-quality evidence) or prednisone (very-low-quality evidence).
Other recommendations made with low-quality evidence for treating symptomatic microscopic colitis include not using combination therapy with cholestyramine and mesalamine over mesalamine alone for induction therapy, nor Boswellia serrata to induce remission. The AGA also does not recommend (low-quality evidence) using probiotics over no treatment for the condition.
Because the meta-analysis of evidence conducted by the AGA only included data derived from clinical trials, the guideline does not include antidiarrheals, cholestyramine monotherapy, a variety of combination therapies, nor the medical treatment of steroid-refractory microscopic colitis, although the AGA did note in the guideline that very limited evidence from a series of cases suggests certain immunosuppressive therapies may benefit these patients.
On Twitter @whitneymcknight
A microscopic colitis treatment guideline from the American Gastroenterological Association was published in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2015.11.008).
Microscopic colitis is most common in persons aged 60 years and over, typically presents as chronic watery diarrhea with nausea or abdominal pain caused by inflammation in the colon, and is diagnosed by colonic biopsy. It is more of a nuisance than life threatening, with no evidence that the persistent histologic inflammation predicts colorectal cancer or the need for surgical intervention.
The guideline strongly recommends, with moderate-quality evidence, treating symptomatic patients with budesonide rather than foregoing any treatment. The AGA also strongly recommends, with high-quality evidence, that budesonide be used over mesalamine to induce remission, unless such treatment is not feasible in a patient because of a drug reaction or its high price. In that case, the AGA recommends (with moderate-quality evidence) the use of mesalamine. Once induction therapy is discontinued, the AGA strongly recommends, with moderate-quality evidence, maintenance treatment using budesonide, if possible.
In patients for whom budesonide is not feasible, the AGA recommends that rather than forgo treatment, patients may be induced with bismuth subsalicylate (low-quality evidence) or prednisone (very-low-quality evidence).
Other recommendations made with low-quality evidence for treating symptomatic microscopic colitis include not using combination therapy with cholestyramine and mesalamine over mesalamine alone for induction therapy, nor Boswellia serrata to induce remission. The AGA also does not recommend (low-quality evidence) using probiotics over no treatment for the condition.
Because the meta-analysis of evidence conducted by the AGA only included data derived from clinical trials, the guideline does not include antidiarrheals, cholestyramine monotherapy, a variety of combination therapies, nor the medical treatment of steroid-refractory microscopic colitis, although the AGA did note in the guideline that very limited evidence from a series of cases suggests certain immunosuppressive therapies may benefit these patients.
On Twitter @whitneymcknight
FROM THE AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Health spending growth soars after years of low growth
Five years of low growth in national health spending expenditures reversed substantially in 2014, driven by new Affordable Care Act coverage mandates and higher prescription drug spending, largely for new hepatitis C treatments.
U.S. health spending climbed to $3 trillion and grew by 5.3%, as compared with 2013 when growth was 2.9%. Per capita spending in 2014 was up 4.5% to $9,523 from $9,115 in 2013, according to Centers for Medicare & Medicaid Services Office of the Actuary (Health Affairs. 2015 Dec 2 doi: 10.1377/hlthaff.2015.1194).
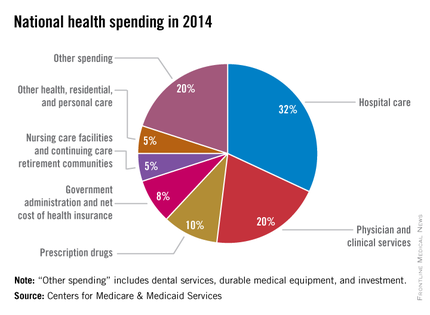
Anne B. Martin, an economist with actuary’s office, said the 2014 numbers reversed several years of historically low spending growth that tracked with the sluggish economy. She attributed the uptick in growth to the ACA’s access mandates as well as prescription drug purchases, namely those for HCV, which added $11.3 billion in new spending.
“We can’t necessarily say that the [low-growth] cycle has been broken, but this 2014 phenomenon is driven primarily by the ACA expansion and the one-time impact of bringing the new hepatitis C drug into the 2014 mix,” Ms. Martin said.
Between 2013 and 2014, 8.7 million additional patients were enrolled in public and private health insurance, bringing the total insured share of the population from 86% to 88.8%, the highest coverage rate since 1987, according to Ms. Martin and her colleagues.
The growth rate for private health insurance spending went from 1.6% in 2013 to 4.4% in 2014. The $991 billion spent reflected the addition of 2.2 million newly insured patients, and higher rates of spending on medications, clinical services, and inpatient care, compared with 2013.
Federal government spending grew the fastest in 2014 at 11.7%, an 8.2% faster growth rate than in 2013.
In 2014, 28% of all health care purchases were made by the federal government, up from 26% in 2013.
Medicaid-specific spending totaled $495.8 billion, an 11% growth rate in 2014, up from 5.9% in 2013, reflecting the addition of 7.7 million Medicaid enrollees, various increases in prescription drug rebates, and updated provider fees.
Medicare spending jumped to 5.5%, up from 3.0% in 2013, largely due to prescription drugs, although Micah Hartman, a statistician in the Office of the Actuary, said that the per-enrollee spending rate was 2.4% in 2014, up from –0.2% in 2013, which was due to physician and clinical services, higher administrative costs, as well as the net cost of insurance, including fees and administrative costs.
Mr. Hartman singled out Medicare Advantage as a key contributor, noting that the 9.7% increase in growth for that program was from ACA-stipulated fees.
Overall, pharmaceutical spending was $297.7 billion in 2014, according to the report, attributable to novel HCV drugs, other new treatments, fewer-than-normal patent expirations and, in some cases, a doubling of the costs for certain brand-name drugs. The overall 2014 pharmaceutical expenditure growth rate was 12.2%, compared with 2.4% in 2013, the largest differential since 2002.
Physician and clinical services in 2014 went from a growth rate of 2.5% to 4.6%, with total spending at $603.7 billion. Hospital spending last year was $971.8 billion, with a spending growth rate of 4.1%, compared with 3.5% in 2013.
On Twitter @whitneymcknight
Five years of low growth in national health spending expenditures reversed substantially in 2014, driven by new Affordable Care Act coverage mandates and higher prescription drug spending, largely for new hepatitis C treatments.
U.S. health spending climbed to $3 trillion and grew by 5.3%, as compared with 2013 when growth was 2.9%. Per capita spending in 2014 was up 4.5% to $9,523 from $9,115 in 2013, according to Centers for Medicare & Medicaid Services Office of the Actuary (Health Affairs. 2015 Dec 2 doi: 10.1377/hlthaff.2015.1194).
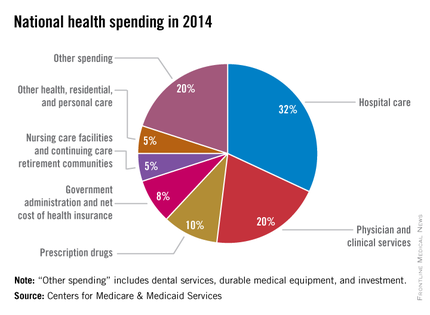
Anne B. Martin, an economist with actuary’s office, said the 2014 numbers reversed several years of historically low spending growth that tracked with the sluggish economy. She attributed the uptick in growth to the ACA’s access mandates as well as prescription drug purchases, namely those for HCV, which added $11.3 billion in new spending.
“We can’t necessarily say that the [low-growth] cycle has been broken, but this 2014 phenomenon is driven primarily by the ACA expansion and the one-time impact of bringing the new hepatitis C drug into the 2014 mix,” Ms. Martin said.
Between 2013 and 2014, 8.7 million additional patients were enrolled in public and private health insurance, bringing the total insured share of the population from 86% to 88.8%, the highest coverage rate since 1987, according to Ms. Martin and her colleagues.
The growth rate for private health insurance spending went from 1.6% in 2013 to 4.4% in 2014. The $991 billion spent reflected the addition of 2.2 million newly insured patients, and higher rates of spending on medications, clinical services, and inpatient care, compared with 2013.
Federal government spending grew the fastest in 2014 at 11.7%, an 8.2% faster growth rate than in 2013.
In 2014, 28% of all health care purchases were made by the federal government, up from 26% in 2013.
Medicaid-specific spending totaled $495.8 billion, an 11% growth rate in 2014, up from 5.9% in 2013, reflecting the addition of 7.7 million Medicaid enrollees, various increases in prescription drug rebates, and updated provider fees.
Medicare spending jumped to 5.5%, up from 3.0% in 2013, largely due to prescription drugs, although Micah Hartman, a statistician in the Office of the Actuary, said that the per-enrollee spending rate was 2.4% in 2014, up from –0.2% in 2013, which was due to physician and clinical services, higher administrative costs, as well as the net cost of insurance, including fees and administrative costs.
Mr. Hartman singled out Medicare Advantage as a key contributor, noting that the 9.7% increase in growth for that program was from ACA-stipulated fees.
Overall, pharmaceutical spending was $297.7 billion in 2014, according to the report, attributable to novel HCV drugs, other new treatments, fewer-than-normal patent expirations and, in some cases, a doubling of the costs for certain brand-name drugs. The overall 2014 pharmaceutical expenditure growth rate was 12.2%, compared with 2.4% in 2013, the largest differential since 2002.
Physician and clinical services in 2014 went from a growth rate of 2.5% to 4.6%, with total spending at $603.7 billion. Hospital spending last year was $971.8 billion, with a spending growth rate of 4.1%, compared with 3.5% in 2013.
On Twitter @whitneymcknight
Five years of low growth in national health spending expenditures reversed substantially in 2014, driven by new Affordable Care Act coverage mandates and higher prescription drug spending, largely for new hepatitis C treatments.
U.S. health spending climbed to $3 trillion and grew by 5.3%, as compared with 2013 when growth was 2.9%. Per capita spending in 2014 was up 4.5% to $9,523 from $9,115 in 2013, according to Centers for Medicare & Medicaid Services Office of the Actuary (Health Affairs. 2015 Dec 2 doi: 10.1377/hlthaff.2015.1194).
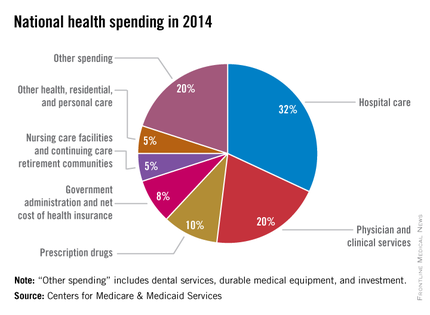
Anne B. Martin, an economist with actuary’s office, said the 2014 numbers reversed several years of historically low spending growth that tracked with the sluggish economy. She attributed the uptick in growth to the ACA’s access mandates as well as prescription drug purchases, namely those for HCV, which added $11.3 billion in new spending.
“We can’t necessarily say that the [low-growth] cycle has been broken, but this 2014 phenomenon is driven primarily by the ACA expansion and the one-time impact of bringing the new hepatitis C drug into the 2014 mix,” Ms. Martin said.
Between 2013 and 2014, 8.7 million additional patients were enrolled in public and private health insurance, bringing the total insured share of the population from 86% to 88.8%, the highest coverage rate since 1987, according to Ms. Martin and her colleagues.
The growth rate for private health insurance spending went from 1.6% in 2013 to 4.4% in 2014. The $991 billion spent reflected the addition of 2.2 million newly insured patients, and higher rates of spending on medications, clinical services, and inpatient care, compared with 2013.
Federal government spending grew the fastest in 2014 at 11.7%, an 8.2% faster growth rate than in 2013.
In 2014, 28% of all health care purchases were made by the federal government, up from 26% in 2013.
Medicaid-specific spending totaled $495.8 billion, an 11% growth rate in 2014, up from 5.9% in 2013, reflecting the addition of 7.7 million Medicaid enrollees, various increases in prescription drug rebates, and updated provider fees.
Medicare spending jumped to 5.5%, up from 3.0% in 2013, largely due to prescription drugs, although Micah Hartman, a statistician in the Office of the Actuary, said that the per-enrollee spending rate was 2.4% in 2014, up from –0.2% in 2013, which was due to physician and clinical services, higher administrative costs, as well as the net cost of insurance, including fees and administrative costs.
Mr. Hartman singled out Medicare Advantage as a key contributor, noting that the 9.7% increase in growth for that program was from ACA-stipulated fees.
Overall, pharmaceutical spending was $297.7 billion in 2014, according to the report, attributable to novel HCV drugs, other new treatments, fewer-than-normal patent expirations and, in some cases, a doubling of the costs for certain brand-name drugs. The overall 2014 pharmaceutical expenditure growth rate was 12.2%, compared with 2.4% in 2013, the largest differential since 2002.
Physician and clinical services in 2014 went from a growth rate of 2.5% to 4.6%, with total spending at $603.7 billion. Hospital spending last year was $971.8 billion, with a spending growth rate of 4.1%, compared with 3.5% in 2013.
On Twitter @whitneymcknight
FROM THE JOURNAL HEALTH AFFAIRS
FDA panel decides novel antidepressant does not have favorable risk benefit ratio
SILVER SPRING, MD. – An extended-release formulation of gepirone hydrochloride got a thumbs up for safety, but received a recommendation against approval for major depressive disorder from a Food and Drug Administration advisory panel.
At a Dec. 1 meeting, the FDA’s Psychopharmacologic Drugs Advisory Committee voted 11-2 in favor of gepirone’s safety profile, but concluded by a vote of 9-4 that the drug’s sponsor, Fabre-Kramer Pharmaceuticals, failed to demonstrate the drug’s efficacy.
The drug’s sponsor noted that data from 5 of 12 short-term, randomized, placebo-controlled studies of gepirone ER (extended release) were considered to be interpretable and should serve as the basis for assessment of efficacy. “Of the five interpretable studies, two clinical trials demonstrated statistically significant findings based on difference in adjusted mean change from baseline in Hamilton Depression Rating Scale-17 [HAMD-17] score at end of study,” according to a statement from the drug’s manufacturer. The effect size in those two studies was comparable to the effect size seen for many of the other approved antidepressants.
According to Fabre-Kramer, a meta-analysis of all five interpretable studies demonstrated statistically significant benefits of gepirone ER based on changes in adjusted mean HAMD-17 scores.
Adverse effects were reported by at least 5% of all subjects and included headache, dizziness, somnolence, nausea, dry mouth, diarrhea, constipation, insomnia, upper respiratory tract infection, nasopharyngitis, and fatigue. “In trials conducted to date, there is no evidence that treatment with gepirone ER causes certain side effects common to other approved serotonergic agents including withdrawal effects, high incidence of somnolence, weight gain, seizure risk, and sexual dysfunction,” the drug’s sponsor said in a statement.
The panel, however, concluded that the data from these studies were not substantial enough to warrant approval at this time. They noted that the study drug did not beat either placebo or the active control in three of the five trials that used an active control group. Further, the active control actually beat the study drug. “That is something we hardly ever see,” said Dr. Robert Temple, deputy director for clinical science at the FDA. “We’re not concluding that these studies prove [gepirone] doesn’t work, but it raises doubts about the available data and makes us believe there needs to be more data.”
The FDA previously had issued three nonapproval letters for gepirone since its development began in 1999, which is noted in the FDA’s analysis of the data.
Gepirone’s mechanism of action when formulated for extended release is as a partial agonist of the 5-HT autoreceptors and a full agonist at the postsynaptic 5-HT autoreceptors, allowing there to be fewer serotonin-related side affects, such as sexual dysfunction.
Dr. Dawn F. Ionescu of Massachusetts General Hospital and a member of the panel, summed up the panel’s observations of safety versus efficacy: “If this medication isn’t going to treat patients’ depression, what’s the point in giving them a medication that will also not cause as much sexual dysfunction?”
The FDA typically follows the advice of its advisory panels. None of the panelists involved in the vote had any relevant financial disclosures.
On Twitter @whitneymcknight
SILVER SPRING, MD. – An extended-release formulation of gepirone hydrochloride got a thumbs up for safety, but received a recommendation against approval for major depressive disorder from a Food and Drug Administration advisory panel.
At a Dec. 1 meeting, the FDA’s Psychopharmacologic Drugs Advisory Committee voted 11-2 in favor of gepirone’s safety profile, but concluded by a vote of 9-4 that the drug’s sponsor, Fabre-Kramer Pharmaceuticals, failed to demonstrate the drug’s efficacy.
The drug’s sponsor noted that data from 5 of 12 short-term, randomized, placebo-controlled studies of gepirone ER (extended release) were considered to be interpretable and should serve as the basis for assessment of efficacy. “Of the five interpretable studies, two clinical trials demonstrated statistically significant findings based on difference in adjusted mean change from baseline in Hamilton Depression Rating Scale-17 [HAMD-17] score at end of study,” according to a statement from the drug’s manufacturer. The effect size in those two studies was comparable to the effect size seen for many of the other approved antidepressants.
According to Fabre-Kramer, a meta-analysis of all five interpretable studies demonstrated statistically significant benefits of gepirone ER based on changes in adjusted mean HAMD-17 scores.
Adverse effects were reported by at least 5% of all subjects and included headache, dizziness, somnolence, nausea, dry mouth, diarrhea, constipation, insomnia, upper respiratory tract infection, nasopharyngitis, and fatigue. “In trials conducted to date, there is no evidence that treatment with gepirone ER causes certain side effects common to other approved serotonergic agents including withdrawal effects, high incidence of somnolence, weight gain, seizure risk, and sexual dysfunction,” the drug’s sponsor said in a statement.
The panel, however, concluded that the data from these studies were not substantial enough to warrant approval at this time. They noted that the study drug did not beat either placebo or the active control in three of the five trials that used an active control group. Further, the active control actually beat the study drug. “That is something we hardly ever see,” said Dr. Robert Temple, deputy director for clinical science at the FDA. “We’re not concluding that these studies prove [gepirone] doesn’t work, but it raises doubts about the available data and makes us believe there needs to be more data.”
The FDA previously had issued three nonapproval letters for gepirone since its development began in 1999, which is noted in the FDA’s analysis of the data.
Gepirone’s mechanism of action when formulated for extended release is as a partial agonist of the 5-HT autoreceptors and a full agonist at the postsynaptic 5-HT autoreceptors, allowing there to be fewer serotonin-related side affects, such as sexual dysfunction.
Dr. Dawn F. Ionescu of Massachusetts General Hospital and a member of the panel, summed up the panel’s observations of safety versus efficacy: “If this medication isn’t going to treat patients’ depression, what’s the point in giving them a medication that will also not cause as much sexual dysfunction?”
The FDA typically follows the advice of its advisory panels. None of the panelists involved in the vote had any relevant financial disclosures.
On Twitter @whitneymcknight
SILVER SPRING, MD. – An extended-release formulation of gepirone hydrochloride got a thumbs up for safety, but received a recommendation against approval for major depressive disorder from a Food and Drug Administration advisory panel.
At a Dec. 1 meeting, the FDA’s Psychopharmacologic Drugs Advisory Committee voted 11-2 in favor of gepirone’s safety profile, but concluded by a vote of 9-4 that the drug’s sponsor, Fabre-Kramer Pharmaceuticals, failed to demonstrate the drug’s efficacy.
The drug’s sponsor noted that data from 5 of 12 short-term, randomized, placebo-controlled studies of gepirone ER (extended release) were considered to be interpretable and should serve as the basis for assessment of efficacy. “Of the five interpretable studies, two clinical trials demonstrated statistically significant findings based on difference in adjusted mean change from baseline in Hamilton Depression Rating Scale-17 [HAMD-17] score at end of study,” according to a statement from the drug’s manufacturer. The effect size in those two studies was comparable to the effect size seen for many of the other approved antidepressants.
According to Fabre-Kramer, a meta-analysis of all five interpretable studies demonstrated statistically significant benefits of gepirone ER based on changes in adjusted mean HAMD-17 scores.
Adverse effects were reported by at least 5% of all subjects and included headache, dizziness, somnolence, nausea, dry mouth, diarrhea, constipation, insomnia, upper respiratory tract infection, nasopharyngitis, and fatigue. “In trials conducted to date, there is no evidence that treatment with gepirone ER causes certain side effects common to other approved serotonergic agents including withdrawal effects, high incidence of somnolence, weight gain, seizure risk, and sexual dysfunction,” the drug’s sponsor said in a statement.
The panel, however, concluded that the data from these studies were not substantial enough to warrant approval at this time. They noted that the study drug did not beat either placebo or the active control in three of the five trials that used an active control group. Further, the active control actually beat the study drug. “That is something we hardly ever see,” said Dr. Robert Temple, deputy director for clinical science at the FDA. “We’re not concluding that these studies prove [gepirone] doesn’t work, but it raises doubts about the available data and makes us believe there needs to be more data.”
The FDA previously had issued three nonapproval letters for gepirone since its development began in 1999, which is noted in the FDA’s analysis of the data.
Gepirone’s mechanism of action when formulated for extended release is as a partial agonist of the 5-HT autoreceptors and a full agonist at the postsynaptic 5-HT autoreceptors, allowing there to be fewer serotonin-related side affects, such as sexual dysfunction.
Dr. Dawn F. Ionescu of Massachusetts General Hospital and a member of the panel, summed up the panel’s observations of safety versus efficacy: “If this medication isn’t going to treat patients’ depression, what’s the point in giving them a medication that will also not cause as much sexual dysfunction?”
The FDA typically follows the advice of its advisory panels. None of the panelists involved in the vote had any relevant financial disclosures.
On Twitter @whitneymcknight
AT AN FDA ADVISORY COMMITTEE MEETING
Are you PrEPping your high HIV-risk patients?
One-third of U.S. primary care physicians are unaware that there is a daily prophylactic medication that can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%, according to the CDC.
In a Nov. 24 media briefing, Dr. Anne Schuchat, principal deputy director of the U.S. Centers for Disease Control and Prevention, said data from a recent national survey of primary care physicians indicated that 34% were unaware that a daily preexposure prophylactic (PrEP) medication was available for patients at highest risk for contracting the virus. “PrEP can only make a difference if all health care providers, not just infectious disease specialists, are aware of it and know who can most benefit from it, and if the people at greatest risk for HIV infection know PReP may be a viable treatment option.”
According to the CDC, 40,000 people are diagnosed as HIV positive annually in the United States. The CDC has identified the most at-risk groups to be 1 in 4 sexually active gay men, 1 in 5 injectable drug users, and 1 in 200 sexually active heterosexuals. The numbers are derived from an analysis of NHANES (National Health and Nutrition Examination Survey) data during 2007-2012. Dr. Schuchat told reporters that daily use of PrEP can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%.
Approved by the U.S. Food and Drug Administration in 2012, Truvada (manufactured by Gilead) is a combination of two antiretrovirals, tenofovir and emtricitabine, when taken daily has been shown to be highly effective in populations most at risk for contracting HIV. The most common acute side effect of the medication is nausea, although imperiled kidney function has been reported in a small but clinically significant population taking the medication. Dr. Schuchat recommended those who use PrEP have their kidneys evaluated every 3 months.
PrEP is part of the CDC’s “high-impact plan” for containing the HIV/AIDS epidemic nationally. Other strategies in the plan include antiretroviral treatment for people already living with HIV; the correct and consistent use of condoms; public health campaigns to keep people in care and reduce high-risk behaviors; increased access to drug treatment programs; and the availability of sterile injection equipment for people who inject drugs.
The cost of PrEP, according to Dr. Schuchat, is about $10,000 annually and is covered by Medicaid.
“PrEP has the potential to dramatically reduce new HIV infections in the nation,” Dr. Jonathan Mermin, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the briefing. “However, PrEP [works only] if patients know about it, have access to it, and take it as prescribed.”
On Twitter @whitneymcknight
One-third of U.S. primary care physicians are unaware that there is a daily prophylactic medication that can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%, according to the CDC.
In a Nov. 24 media briefing, Dr. Anne Schuchat, principal deputy director of the U.S. Centers for Disease Control and Prevention, said data from a recent national survey of primary care physicians indicated that 34% were unaware that a daily preexposure prophylactic (PrEP) medication was available for patients at highest risk for contracting the virus. “PrEP can only make a difference if all health care providers, not just infectious disease specialists, are aware of it and know who can most benefit from it, and if the people at greatest risk for HIV infection know PReP may be a viable treatment option.”
According to the CDC, 40,000 people are diagnosed as HIV positive annually in the United States. The CDC has identified the most at-risk groups to be 1 in 4 sexually active gay men, 1 in 5 injectable drug users, and 1 in 200 sexually active heterosexuals. The numbers are derived from an analysis of NHANES (National Health and Nutrition Examination Survey) data during 2007-2012. Dr. Schuchat told reporters that daily use of PrEP can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%.
Approved by the U.S. Food and Drug Administration in 2012, Truvada (manufactured by Gilead) is a combination of two antiretrovirals, tenofovir and emtricitabine, when taken daily has been shown to be highly effective in populations most at risk for contracting HIV. The most common acute side effect of the medication is nausea, although imperiled kidney function has been reported in a small but clinically significant population taking the medication. Dr. Schuchat recommended those who use PrEP have their kidneys evaluated every 3 months.
PrEP is part of the CDC’s “high-impact plan” for containing the HIV/AIDS epidemic nationally. Other strategies in the plan include antiretroviral treatment for people already living with HIV; the correct and consistent use of condoms; public health campaigns to keep people in care and reduce high-risk behaviors; increased access to drug treatment programs; and the availability of sterile injection equipment for people who inject drugs.
The cost of PrEP, according to Dr. Schuchat, is about $10,000 annually and is covered by Medicaid.
“PrEP has the potential to dramatically reduce new HIV infections in the nation,” Dr. Jonathan Mermin, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the briefing. “However, PrEP [works only] if patients know about it, have access to it, and take it as prescribed.”
On Twitter @whitneymcknight
One-third of U.S. primary care physicians are unaware that there is a daily prophylactic medication that can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%, according to the CDC.
In a Nov. 24 media briefing, Dr. Anne Schuchat, principal deputy director of the U.S. Centers for Disease Control and Prevention, said data from a recent national survey of primary care physicians indicated that 34% were unaware that a daily preexposure prophylactic (PrEP) medication was available for patients at highest risk for contracting the virus. “PrEP can only make a difference if all health care providers, not just infectious disease specialists, are aware of it and know who can most benefit from it, and if the people at greatest risk for HIV infection know PReP may be a viable treatment option.”
According to the CDC, 40,000 people are diagnosed as HIV positive annually in the United States. The CDC has identified the most at-risk groups to be 1 in 4 sexually active gay men, 1 in 5 injectable drug users, and 1 in 200 sexually active heterosexuals. The numbers are derived from an analysis of NHANES (National Health and Nutrition Examination Survey) data during 2007-2012. Dr. Schuchat told reporters that daily use of PrEP can reduce the risk of sexually transmitted HIV by 90% and drug needle transmission of the virus by 70%.
Approved by the U.S. Food and Drug Administration in 2012, Truvada (manufactured by Gilead) is a combination of two antiretrovirals, tenofovir and emtricitabine, when taken daily has been shown to be highly effective in populations most at risk for contracting HIV. The most common acute side effect of the medication is nausea, although imperiled kidney function has been reported in a small but clinically significant population taking the medication. Dr. Schuchat recommended those who use PrEP have their kidneys evaluated every 3 months.
PrEP is part of the CDC’s “high-impact plan” for containing the HIV/AIDS epidemic nationally. Other strategies in the plan include antiretroviral treatment for people already living with HIV; the correct and consistent use of condoms; public health campaigns to keep people in care and reduce high-risk behaviors; increased access to drug treatment programs; and the availability of sterile injection equipment for people who inject drugs.
The cost of PrEP, according to Dr. Schuchat, is about $10,000 annually and is covered by Medicaid.
“PrEP has the potential to dramatically reduce new HIV infections in the nation,” Dr. Jonathan Mermin, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the briefing. “However, PrEP [works only] if patients know about it, have access to it, and take it as prescribed.”
On Twitter @whitneymcknight
FROM A CDC MEDIA BRIEFING
Key clinical point: A third of physicians are unaware of prophylactic medication that can reduce HIV virus risk from sex by 90% and from injecting drugs by 70%.
Major finding: Transmission of HIV virus could be prevented in up to one-quarter of MSM, 70% of injectable drug users, and 1 in 200 sexually active heterosexuals.
Data source: Analysis of data from the 2007-2012 NHANES.
Disclosures: None.