User login
Tofacitinib an alternative treatment for refractory cutaneous dermatomyositis
Tofacitinib, an oral Janus kinase (JAK)-1/3 inhibitor approved for treating rheumatoid arthritis, was beneficial in treating cutaneous dermatomyositis in three patients who had failed traditional therapies, according to a report published in JAMA Dermatology.
Dr. Drew J.B. Kurtzman of the department of dermatology at Brigham and Women’s Hospital and Harvard University, Boston, and his associates evaluated the responses of three patients with multidrug-resistant cutaneous dermatomyositis to treatment with twice-daily oral tofacitinib (Xeljanz). Previous treatment included hydroxychloroquine, methotrexate, mycophenolate mofetil, and intravenous immunoglobulin. Two of the patients received tofacitinib as monotherapy, and one continued using hydroxychloroquine.
Response was measured with the validated Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) activity score. Secondary endpoints included tolerability, adverse events, and need for concurrent therapies. The results were published online in a research letter on April 27 (JAMA Dermatol. 2016. April 27. doi: 10.1001/jamadermatol.2016.0866).
They were treated for a mean of 9.6 months. Significant improvements were noted in all three patients, with clinical responses observed after only 4 weeks. CDASI activity scores decreased in all three patients. The mean improvement was 12 points, which exceeded the 4- to 5-point change reflective of a clinically significant response, the authors pointed out.
Because the two patients on tofacitinib monotherapy showed a decrease to an activity score of 14 or lower, they were considered to have improved from moderate to severe disease, to mild disease. Although the remaining patient experienced a lesser degree of improvement, the response to treatment was still deemed clinically significant.
In addition, all three patients reported less pruritus, and the two patients with classic dermatomyositis reported subjective improvements in strength and fatigue. No adverse events were reported for any of the patients. The greatest degree of improvement was seen in the one patient receiving the highest dose of tofacitinib, suggesting that the effect of tofacitinib on refractory cutaneous dermatomyositis may have been dose dependent, Dr. Kurtzman and his associates wrote.
Noting that larger studies on efficacy and long-term safety are needed to validate their findings, they added, “given the limited number of agents available for the management of recalcitrant skin disease, alternative options are needed. By mitigating the signaling cascades that are likely responsible for dermatomyositis, tofacitinib and other JAK inhibitors may represent a rational therapeutic approach.”
Tofacitinib was approved in 2012 for adults with moderately to severely active rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate.
No external funding source was disclosed. All but one of the seven authors declared no conflicts of interest. The remaining author’s disclosure included serving as a consultant for Biogen IDEC, Amgen, Janssen, AbbVie, Eli Lilly, and Momenta, and as speaker for AbbVie and Eli Lilly.
Tofacitinib, an oral Janus kinase (JAK)-1/3 inhibitor approved for treating rheumatoid arthritis, was beneficial in treating cutaneous dermatomyositis in three patients who had failed traditional therapies, according to a report published in JAMA Dermatology.
Dr. Drew J.B. Kurtzman of the department of dermatology at Brigham and Women’s Hospital and Harvard University, Boston, and his associates evaluated the responses of three patients with multidrug-resistant cutaneous dermatomyositis to treatment with twice-daily oral tofacitinib (Xeljanz). Previous treatment included hydroxychloroquine, methotrexate, mycophenolate mofetil, and intravenous immunoglobulin. Two of the patients received tofacitinib as monotherapy, and one continued using hydroxychloroquine.
Response was measured with the validated Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) activity score. Secondary endpoints included tolerability, adverse events, and need for concurrent therapies. The results were published online in a research letter on April 27 (JAMA Dermatol. 2016. April 27. doi: 10.1001/jamadermatol.2016.0866).
They were treated for a mean of 9.6 months. Significant improvements were noted in all three patients, with clinical responses observed after only 4 weeks. CDASI activity scores decreased in all three patients. The mean improvement was 12 points, which exceeded the 4- to 5-point change reflective of a clinically significant response, the authors pointed out.
Because the two patients on tofacitinib monotherapy showed a decrease to an activity score of 14 or lower, they were considered to have improved from moderate to severe disease, to mild disease. Although the remaining patient experienced a lesser degree of improvement, the response to treatment was still deemed clinically significant.
In addition, all three patients reported less pruritus, and the two patients with classic dermatomyositis reported subjective improvements in strength and fatigue. No adverse events were reported for any of the patients. The greatest degree of improvement was seen in the one patient receiving the highest dose of tofacitinib, suggesting that the effect of tofacitinib on refractory cutaneous dermatomyositis may have been dose dependent, Dr. Kurtzman and his associates wrote.
Noting that larger studies on efficacy and long-term safety are needed to validate their findings, they added, “given the limited number of agents available for the management of recalcitrant skin disease, alternative options are needed. By mitigating the signaling cascades that are likely responsible for dermatomyositis, tofacitinib and other JAK inhibitors may represent a rational therapeutic approach.”
Tofacitinib was approved in 2012 for adults with moderately to severely active rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate.
No external funding source was disclosed. All but one of the seven authors declared no conflicts of interest. The remaining author’s disclosure included serving as a consultant for Biogen IDEC, Amgen, Janssen, AbbVie, Eli Lilly, and Momenta, and as speaker for AbbVie and Eli Lilly.
Tofacitinib, an oral Janus kinase (JAK)-1/3 inhibitor approved for treating rheumatoid arthritis, was beneficial in treating cutaneous dermatomyositis in three patients who had failed traditional therapies, according to a report published in JAMA Dermatology.
Dr. Drew J.B. Kurtzman of the department of dermatology at Brigham and Women’s Hospital and Harvard University, Boston, and his associates evaluated the responses of three patients with multidrug-resistant cutaneous dermatomyositis to treatment with twice-daily oral tofacitinib (Xeljanz). Previous treatment included hydroxychloroquine, methotrexate, mycophenolate mofetil, and intravenous immunoglobulin. Two of the patients received tofacitinib as monotherapy, and one continued using hydroxychloroquine.
Response was measured with the validated Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) activity score. Secondary endpoints included tolerability, adverse events, and need for concurrent therapies. The results were published online in a research letter on April 27 (JAMA Dermatol. 2016. April 27. doi: 10.1001/jamadermatol.2016.0866).
They were treated for a mean of 9.6 months. Significant improvements were noted in all three patients, with clinical responses observed after only 4 weeks. CDASI activity scores decreased in all three patients. The mean improvement was 12 points, which exceeded the 4- to 5-point change reflective of a clinically significant response, the authors pointed out.
Because the two patients on tofacitinib monotherapy showed a decrease to an activity score of 14 or lower, they were considered to have improved from moderate to severe disease, to mild disease. Although the remaining patient experienced a lesser degree of improvement, the response to treatment was still deemed clinically significant.
In addition, all three patients reported less pruritus, and the two patients with classic dermatomyositis reported subjective improvements in strength and fatigue. No adverse events were reported for any of the patients. The greatest degree of improvement was seen in the one patient receiving the highest dose of tofacitinib, suggesting that the effect of tofacitinib on refractory cutaneous dermatomyositis may have been dose dependent, Dr. Kurtzman and his associates wrote.
Noting that larger studies on efficacy and long-term safety are needed to validate their findings, they added, “given the limited number of agents available for the management of recalcitrant skin disease, alternative options are needed. By mitigating the signaling cascades that are likely responsible for dermatomyositis, tofacitinib and other JAK inhibitors may represent a rational therapeutic approach.”
Tofacitinib was approved in 2012 for adults with moderately to severely active rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate.
No external funding source was disclosed. All but one of the seven authors declared no conflicts of interest. The remaining author’s disclosure included serving as a consultant for Biogen IDEC, Amgen, Janssen, AbbVie, Eli Lilly, and Momenta, and as speaker for AbbVie and Eli Lilly.
FROM JAMA DERMATOLOGY
Key clinical point: Tofacitinib could be an alternative treatment for refractory cutaneous dermatomyositis, and should be studied further.
Major finding: Three patients with refractory cutaneous dermatomyositis showed clinical responses to tofacitinib after 4 weeks.
Data sources: Three patients with refractory cutaneous dermatomyositis treated with tofacitinib over a mean of 9.6 months.
Disclosures: No external funding source was disclosed. All but one coauthor had no disclosures; the remaining author disclosed numerous ties to industry sources.
Acute viral bronchiolitis hospital stay not shortened by hypertonic saline
The results of two previously published meta-analyses supporting a shortening of hospital length of stay following the use of hypertonic saline in infants with acute viral bronchiolitis are unreliable, according to a study published in JAMA Pediatrics.
Hypertonic saline should not be expected to shorten the length of hospital stay for those with acute viral bronchiolitis in typical hospital settings in the United States, Dr. Corinne G. Brooks of the Leadership in Preventive Medicine and Pediatrics Residencies at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and her associates concluded.
The investigators reached this conclusion after reanalyzing data from the 18 randomized clinical trials using hypertonic saline in infants with bronchiolitis reporting hospital length of stay as an outcome measure in the two previously published meta-analyses, after finding no additional data sources through a literature search. The studies included 2,063 infants (63% male), with a mean age of 4.2 months and a mean length of stay of 3.6 days (JAMA Pediatr. 2016 Apr 18. doi: 10.1001/jamapediatrics.2016.0079).
Dr. Brooks explained the rationale behind the study by pointing out that the previously published analyses failed to address and account for the large amount of study heterogeneity in the assessed cohort of studies, necessitating a reanalysis of the full data set to investigate factors with the potential to introduce such heterogeneity.
The reanalysis produced two significant findings, which collectively accounted for all of the heterogeneity between the assessed studies. First, one of the study populations was determined to be a significant outlier with very different criteria for discharge and substantially longer expected hospital length of stay. Because the statistical significance of the weighted mean difference in hospital length of stay attributable to the use of hypertonic saline was sensitive to the removal of this study population, heterogeneity was found to resolve to moderate to acceptable levels. Second, an important baseline difference between the treatment arms in day of illness at study enrollment was found. Patients presenting later in their illness were more likely to be allocated to the hypertonic saline treatment arm in 6 of the 18 studies assessed, most of which were small positive studies. Therefore, this difference accounted for a systematic bias favoring treatment groups.
Based on their reanalysis of the available data, Dr. Brooks and her associates said that the appearance of a meaningful reduction in the length of hospital stay for infants with acute viral bronchiolitis was a direct result of the inappropriate combination of studies with clinically significant differences in outcome definitions, and the previously unnoticed systematic bias in treatment group allocation.
No external funding was provided. None of the authors reported any conflicts of interest.
When infants below 1 year of age experience viral bronchiolitis, usually from respiratory syncytial virus (RSV), they sometimes get admitted to hospital for supportive care. In hospital, the main goals are to reduce the work of breathing and tachypnea and increase oxygen saturation in the blood. In addition to supplemental oxygen, the use of hypertonic saline nebulizations has been proposed, studied, and endorsed by some investigators based on randomized trials.

|
Dr. Michael Pichichero |
In this paper from a group at Dartmouth Medical Center, we learn that a recent conclusion of benefit from hypertonic saline nebulizations on hospital length of stay likely was incorrect. The authors correctly point out that meta-analysis is a tricky business because it relies on a reasonable homogeneity among the populations included in the individual studies. If there is heterogeneity, this can complicate interpretation, although there are statistical maneuvers that can help determine if the heterogeneity that is inherent in meta-analyses has a major impact on conclusions, as appears to have occurred here.
When we must hospitalize an infant with bronchiolitis for hypoxemia, it creates a lot of stress for the family. As physicians, we seek to do anything that might help get the child home sooner – thus the 18 studies published on trying hypertonic saline, with varied results. I suspect that this paper from the Dartmouth group will not end the debate or deter future research into treatments that might help these babies.
Michael E. Pichichero, M.D., a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. Dr. Pichichero commented in an interview. He said he had no relevant financial disclosures.
When infants below 1 year of age experience viral bronchiolitis, usually from respiratory syncytial virus (RSV), they sometimes get admitted to hospital for supportive care. In hospital, the main goals are to reduce the work of breathing and tachypnea and increase oxygen saturation in the blood. In addition to supplemental oxygen, the use of hypertonic saline nebulizations has been proposed, studied, and endorsed by some investigators based on randomized trials.

|
Dr. Michael Pichichero |
In this paper from a group at Dartmouth Medical Center, we learn that a recent conclusion of benefit from hypertonic saline nebulizations on hospital length of stay likely was incorrect. The authors correctly point out that meta-analysis is a tricky business because it relies on a reasonable homogeneity among the populations included in the individual studies. If there is heterogeneity, this can complicate interpretation, although there are statistical maneuvers that can help determine if the heterogeneity that is inherent in meta-analyses has a major impact on conclusions, as appears to have occurred here.
When we must hospitalize an infant with bronchiolitis for hypoxemia, it creates a lot of stress for the family. As physicians, we seek to do anything that might help get the child home sooner – thus the 18 studies published on trying hypertonic saline, with varied results. I suspect that this paper from the Dartmouth group will not end the debate or deter future research into treatments that might help these babies.
Michael E. Pichichero, M.D., a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. Dr. Pichichero commented in an interview. He said he had no relevant financial disclosures.
When infants below 1 year of age experience viral bronchiolitis, usually from respiratory syncytial virus (RSV), they sometimes get admitted to hospital for supportive care. In hospital, the main goals are to reduce the work of breathing and tachypnea and increase oxygen saturation in the blood. In addition to supplemental oxygen, the use of hypertonic saline nebulizations has been proposed, studied, and endorsed by some investigators based on randomized trials.

|
Dr. Michael Pichichero |
In this paper from a group at Dartmouth Medical Center, we learn that a recent conclusion of benefit from hypertonic saline nebulizations on hospital length of stay likely was incorrect. The authors correctly point out that meta-analysis is a tricky business because it relies on a reasonable homogeneity among the populations included in the individual studies. If there is heterogeneity, this can complicate interpretation, although there are statistical maneuvers that can help determine if the heterogeneity that is inherent in meta-analyses has a major impact on conclusions, as appears to have occurred here.
When we must hospitalize an infant with bronchiolitis for hypoxemia, it creates a lot of stress for the family. As physicians, we seek to do anything that might help get the child home sooner – thus the 18 studies published on trying hypertonic saline, with varied results. I suspect that this paper from the Dartmouth group will not end the debate or deter future research into treatments that might help these babies.
Michael E. Pichichero, M.D., a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. Dr. Pichichero commented in an interview. He said he had no relevant financial disclosures.
The results of two previously published meta-analyses supporting a shortening of hospital length of stay following the use of hypertonic saline in infants with acute viral bronchiolitis are unreliable, according to a study published in JAMA Pediatrics.
Hypertonic saline should not be expected to shorten the length of hospital stay for those with acute viral bronchiolitis in typical hospital settings in the United States, Dr. Corinne G. Brooks of the Leadership in Preventive Medicine and Pediatrics Residencies at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and her associates concluded.
The investigators reached this conclusion after reanalyzing data from the 18 randomized clinical trials using hypertonic saline in infants with bronchiolitis reporting hospital length of stay as an outcome measure in the two previously published meta-analyses, after finding no additional data sources through a literature search. The studies included 2,063 infants (63% male), with a mean age of 4.2 months and a mean length of stay of 3.6 days (JAMA Pediatr. 2016 Apr 18. doi: 10.1001/jamapediatrics.2016.0079).
Dr. Brooks explained the rationale behind the study by pointing out that the previously published analyses failed to address and account for the large amount of study heterogeneity in the assessed cohort of studies, necessitating a reanalysis of the full data set to investigate factors with the potential to introduce such heterogeneity.
The reanalysis produced two significant findings, which collectively accounted for all of the heterogeneity between the assessed studies. First, one of the study populations was determined to be a significant outlier with very different criteria for discharge and substantially longer expected hospital length of stay. Because the statistical significance of the weighted mean difference in hospital length of stay attributable to the use of hypertonic saline was sensitive to the removal of this study population, heterogeneity was found to resolve to moderate to acceptable levels. Second, an important baseline difference between the treatment arms in day of illness at study enrollment was found. Patients presenting later in their illness were more likely to be allocated to the hypertonic saline treatment arm in 6 of the 18 studies assessed, most of which were small positive studies. Therefore, this difference accounted for a systematic bias favoring treatment groups.
Based on their reanalysis of the available data, Dr. Brooks and her associates said that the appearance of a meaningful reduction in the length of hospital stay for infants with acute viral bronchiolitis was a direct result of the inappropriate combination of studies with clinically significant differences in outcome definitions, and the previously unnoticed systematic bias in treatment group allocation.
No external funding was provided. None of the authors reported any conflicts of interest.
The results of two previously published meta-analyses supporting a shortening of hospital length of stay following the use of hypertonic saline in infants with acute viral bronchiolitis are unreliable, according to a study published in JAMA Pediatrics.
Hypertonic saline should not be expected to shorten the length of hospital stay for those with acute viral bronchiolitis in typical hospital settings in the United States, Dr. Corinne G. Brooks of the Leadership in Preventive Medicine and Pediatrics Residencies at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and her associates concluded.
The investigators reached this conclusion after reanalyzing data from the 18 randomized clinical trials using hypertonic saline in infants with bronchiolitis reporting hospital length of stay as an outcome measure in the two previously published meta-analyses, after finding no additional data sources through a literature search. The studies included 2,063 infants (63% male), with a mean age of 4.2 months and a mean length of stay of 3.6 days (JAMA Pediatr. 2016 Apr 18. doi: 10.1001/jamapediatrics.2016.0079).
Dr. Brooks explained the rationale behind the study by pointing out that the previously published analyses failed to address and account for the large amount of study heterogeneity in the assessed cohort of studies, necessitating a reanalysis of the full data set to investigate factors with the potential to introduce such heterogeneity.
The reanalysis produced two significant findings, which collectively accounted for all of the heterogeneity between the assessed studies. First, one of the study populations was determined to be a significant outlier with very different criteria for discharge and substantially longer expected hospital length of stay. Because the statistical significance of the weighted mean difference in hospital length of stay attributable to the use of hypertonic saline was sensitive to the removal of this study population, heterogeneity was found to resolve to moderate to acceptable levels. Second, an important baseline difference between the treatment arms in day of illness at study enrollment was found. Patients presenting later in their illness were more likely to be allocated to the hypertonic saline treatment arm in 6 of the 18 studies assessed, most of which were small positive studies. Therefore, this difference accounted for a systematic bias favoring treatment groups.
Based on their reanalysis of the available data, Dr. Brooks and her associates said that the appearance of a meaningful reduction in the length of hospital stay for infants with acute viral bronchiolitis was a direct result of the inappropriate combination of studies with clinically significant differences in outcome definitions, and the previously unnoticed systematic bias in treatment group allocation.
No external funding was provided. None of the authors reported any conflicts of interest.
FROM JAMA PEDIATRICS
Key clinical point: Physicians should not expect hypertonic saline to shorten hospital length of stay for those with acute viral bronchiolitis.
Major finding: Removal of heterogeneity from recent meta-analyses refutes the utility of hypertonic saline in reducing hospital length of stay for acute viral bronchiolitis.
Data sources: Two previously published meta-analyses pertaining to the use of hypertonic saline and hospital length of stay for acute viral bronchiolitis in infants.
Disclosures: No external funding was provided. None of the authors reported any conflicts of interest.
Seven procedures account for most emergency general surgery costs and deaths
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
A very low number of emergency general surgery procedures account for the majority of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide, according to a study published in JAMA Surgery.
“More than half a million patients undergo urgent or emergent general surgery operations annually in the United States, which accounts for more than $6 billion in annual costs. Only seven representative procedures account for approximately 80% of all admissions, deaths, complications, and inpatient costs attributable to operative emergency general surgery nationwide,” said Dr. John W. Scott from the Center for Surgery and Public Health, department of surgery at the Brigham & Women’s Hospital in Boston, and his associates.
The investigators sought to expand the current diagnosis-based definition of emergency general surgery in order to define a standardized, representative set of procedures that comprise the majority of the national clinical burden of emergency general surgery. To accomplish this goal, Dr. Scott and his colleagues examined data from the 2008 to 2011 Healthcare Cost and Utilization Project’s National Inpatient Sample, the largest publicly available all-payers claims database in the United States, from Nov. 15, 2015, to Feb. 16, 2016 (JAMA Surg. 2016 Apr 27. doi: 10.1001/jamasurg.2016.0480).
The results from this nationally representative observational study represented more than 2 million patient encounters, with a final analytic sample that included 137 unique four-digit ICD-9-CM procedure codes that mapped into 35 distinct three-digit procedure group codes. When ordered by burden rank, the cumulative attributable burden for total procedure count, total deaths, total complications, and total costs increased sharply through procedures ranked one to seven (partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy).
In addition, the procedure volumes were found to be highest for cholecystectomy and appendectomy, although the mortality and complication rates for these procedures were comparatively lower than for the other five identified procedures. For example, the frequency of procedures varied from 682,043 primary appendectomies to 9,418 primary laparotomies, but the mortality rate ranged from 0.08% for appendectomy to 23.76% for laparotomy. Similarly, the complication rate ranged from 7.27% for appendectomy to 46.94% for small-bowel resection. Study results also showed that mean inpatient costs ranged from $9,664.30 for appendectomy to $28,450.72 for small-bowel resection.
Based on their study data, Dr. Scott and his associates recommended national quality benchmarks and cost reduction efforts focused on the seven identified common, complicated, and costly emergency general surgery procedures.
No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
FROM JAMA SURGERY
Key clinical point: National quality benchmarks and cost reduction efforts should focus on the seven most common, complicated, and costly emergency general surgery procedures.
Major finding: The majority (80%) of all admissions, deaths, complications, and inpatient costs attributable to emergency general surgery procedures nationwide can be accounted for by seven representative procedures.
Data sources: The 2008-2011 Healthcare Cost and Utilization Project’s National Inpatient Sample claims database.
Disclosures: No external funding source was disclosed. Coauthor Dr. Adil H. Haider disclosed ties to industry sources. None of the other coauthors reported any conflicts of interest.
Outcomes for infants with necrotizing enterocolitis can be easily improved
Low cost, low-risk interventions can significantly lower the rate of necrotizing enterocolitis among very-low-birth-weight (VLBW) infants, according to a study published in Pediatrics.
Dr. Maria M. Talavera of the department of pediatrics at Ohio State University, Columbus, and her associates assessed the effects of a multipronged intervention on the rate of necrotizing enterocolitis (NEC) among VLBW infants admitted to the intensive care nurseries of Nationwide Children’s Hospital between January 2010 and December 2013. The intervention involved three initiatives: standardized early human milk feedings, standardized restrictive feedings during blood product transfusion and indomethacin therapy, and restrictive ranitidine use in infants of 1,500 g or less or aged 28 weeks or less (Pediatrics. 2016;137[5]:e20151119).
The study produced a collection of interesting findings, most of which suggested a high degree of success in reducing the rate of NEC among VLBW infants. In 2010, the baseline rate of necrotizing enterocolitis in this patient population was 8% of 335 infants. From November 2011 through December 2013, implementation of the interventional plan resulted in a rate of 3.1% of 606 infants.
Additionally, the percentage of discharged infants fed their mother’s own milk by day 3 of life showed a stepwise increase from 0% before September 2010 to 30% from October 2010 to September 2011, and increased to 50% by January 2012.
Perhaps most importantly, mortality among this population of infants attributable to NEC at Nationwide Children’s Hospital nurseries dropped from a baseline mean of 2.7% prior to the implementation of the interventional plan in 2010 to a sustained rate of 0.9% from 2011 to 2013.
Dr. Talavera and her associates cited the lack of a control nursery that did not implement these interventions as a major limitation of their study, but the study results would seem to make an excellent case for implementation of this simple, low-risk, low-cost interventional plan to reduce NEC among VLBW infants.
No external funding was provided. None of the authors reported any conflicts of interest.
Low cost, low-risk interventions can significantly lower the rate of necrotizing enterocolitis among very-low-birth-weight (VLBW) infants, according to a study published in Pediatrics.
Dr. Maria M. Talavera of the department of pediatrics at Ohio State University, Columbus, and her associates assessed the effects of a multipronged intervention on the rate of necrotizing enterocolitis (NEC) among VLBW infants admitted to the intensive care nurseries of Nationwide Children’s Hospital between January 2010 and December 2013. The intervention involved three initiatives: standardized early human milk feedings, standardized restrictive feedings during blood product transfusion and indomethacin therapy, and restrictive ranitidine use in infants of 1,500 g or less or aged 28 weeks or less (Pediatrics. 2016;137[5]:e20151119).
The study produced a collection of interesting findings, most of which suggested a high degree of success in reducing the rate of NEC among VLBW infants. In 2010, the baseline rate of necrotizing enterocolitis in this patient population was 8% of 335 infants. From November 2011 through December 2013, implementation of the interventional plan resulted in a rate of 3.1% of 606 infants.
Additionally, the percentage of discharged infants fed their mother’s own milk by day 3 of life showed a stepwise increase from 0% before September 2010 to 30% from October 2010 to September 2011, and increased to 50% by January 2012.
Perhaps most importantly, mortality among this population of infants attributable to NEC at Nationwide Children’s Hospital nurseries dropped from a baseline mean of 2.7% prior to the implementation of the interventional plan in 2010 to a sustained rate of 0.9% from 2011 to 2013.
Dr. Talavera and her associates cited the lack of a control nursery that did not implement these interventions as a major limitation of their study, but the study results would seem to make an excellent case for implementation of this simple, low-risk, low-cost interventional plan to reduce NEC among VLBW infants.
No external funding was provided. None of the authors reported any conflicts of interest.
Low cost, low-risk interventions can significantly lower the rate of necrotizing enterocolitis among very-low-birth-weight (VLBW) infants, according to a study published in Pediatrics.
Dr. Maria M. Talavera of the department of pediatrics at Ohio State University, Columbus, and her associates assessed the effects of a multipronged intervention on the rate of necrotizing enterocolitis (NEC) among VLBW infants admitted to the intensive care nurseries of Nationwide Children’s Hospital between January 2010 and December 2013. The intervention involved three initiatives: standardized early human milk feedings, standardized restrictive feedings during blood product transfusion and indomethacin therapy, and restrictive ranitidine use in infants of 1,500 g or less or aged 28 weeks or less (Pediatrics. 2016;137[5]:e20151119).
The study produced a collection of interesting findings, most of which suggested a high degree of success in reducing the rate of NEC among VLBW infants. In 2010, the baseline rate of necrotizing enterocolitis in this patient population was 8% of 335 infants. From November 2011 through December 2013, implementation of the interventional plan resulted in a rate of 3.1% of 606 infants.
Additionally, the percentage of discharged infants fed their mother’s own milk by day 3 of life showed a stepwise increase from 0% before September 2010 to 30% from October 2010 to September 2011, and increased to 50% by January 2012.
Perhaps most importantly, mortality among this population of infants attributable to NEC at Nationwide Children’s Hospital nurseries dropped from a baseline mean of 2.7% prior to the implementation of the interventional plan in 2010 to a sustained rate of 0.9% from 2011 to 2013.
Dr. Talavera and her associates cited the lack of a control nursery that did not implement these interventions as a major limitation of their study, but the study results would seem to make an excellent case for implementation of this simple, low-risk, low-cost interventional plan to reduce NEC among VLBW infants.
No external funding was provided. None of the authors reported any conflicts of interest.
FROM PEDIATRICS
Key clinical point: A simple three-part intervention can significantly lower the rate of necrotizing enterocolitis among very-low-birth-weight infants.
Major finding: In 2010, the baseline rate of necrotizing enterocolitis in this patient population was 8% of 335 infants. From November 2011 through December 2013, implementation of the interventional plan resulted in a rate of 3.1% of 606 infants.
Data source: VLBW infants admitted to eight intensive care nurseries from January 2010 to December 2013.
Disclosures: No external funding was provided. None of the authors reported any conflicts of interest.
Risk stratification for progression of primary biliary cholangitis at diagnosis
Risk stratification for those newly diagnosed with primary biliary cholangitis may be best accomplished through the use of the recently developed and validated UK-PBC scoring system, according to a short review published in Hepatology.
Dr. Bertus Eksteen of the Snyder Institute for Chronic Diseases at the University of Calgary (Alta.) described not only the importance of prompt risk assessment in order to prioritize who should receive therapy and be appropriately counseled, but also the difficulties presented by the current risk stratification scoring systems (Hepatology. 2016 Mar;63:697-9).
In his review, Dr. Eksteen asserts that the primary challenge for clinicians attempting to manage patients with primary biliary cholangitis is the selection of those at risk for disease progression. This assessment is of critical importance, as it informs clinical decision making regarding whether to initiate therapy or avoid it.
The review is partially focused on the advantages and disadvantages associated with the use of the multiple clinical and biochemical parameters that have been used to predict progression in primary biliary cholangitis to date. Additionally, the relative strengths and weaknesses of the UK-PBC scoring system are described.
According to Dr. Eksteen, the UK-PBC risk score represents the most complete tool for the assessment of risk of primary biliary cholangitis progression that can be used for clinical patient counseling. Furthermore, the UK-PBC is described as a scoring system with the potential to become a surrogate marker for primary biliary cholangitis progression and should be factored into the design of clinical trials for new agents in development.
The main limitation associated with the use of the UK-PBC risk score is that certain portions contributing to the overall score require at least 12 months of therapy with the only approved treatment for primary biliary cholangitis, ursodeoxycholic acid. This is problematic, as it does not provide the baseline thresholds necessary in order to prioritize patients for therapy, Dr. Eksteen said.
Despite its main limitation, Dr. Eksteen described this scoring system as extremely timely and valuable in the risk assessment of those with primary biliary cholangitis.
No external funding source was disclosed. Dr. Eksteen reported no conflicts of interest.
Risk stratification for those newly diagnosed with primary biliary cholangitis may be best accomplished through the use of the recently developed and validated UK-PBC scoring system, according to a short review published in Hepatology.
Dr. Bertus Eksteen of the Snyder Institute for Chronic Diseases at the University of Calgary (Alta.) described not only the importance of prompt risk assessment in order to prioritize who should receive therapy and be appropriately counseled, but also the difficulties presented by the current risk stratification scoring systems (Hepatology. 2016 Mar;63:697-9).
In his review, Dr. Eksteen asserts that the primary challenge for clinicians attempting to manage patients with primary biliary cholangitis is the selection of those at risk for disease progression. This assessment is of critical importance, as it informs clinical decision making regarding whether to initiate therapy or avoid it.
The review is partially focused on the advantages and disadvantages associated with the use of the multiple clinical and biochemical parameters that have been used to predict progression in primary biliary cholangitis to date. Additionally, the relative strengths and weaknesses of the UK-PBC scoring system are described.
According to Dr. Eksteen, the UK-PBC risk score represents the most complete tool for the assessment of risk of primary biliary cholangitis progression that can be used for clinical patient counseling. Furthermore, the UK-PBC is described as a scoring system with the potential to become a surrogate marker for primary biliary cholangitis progression and should be factored into the design of clinical trials for new agents in development.
The main limitation associated with the use of the UK-PBC risk score is that certain portions contributing to the overall score require at least 12 months of therapy with the only approved treatment for primary biliary cholangitis, ursodeoxycholic acid. This is problematic, as it does not provide the baseline thresholds necessary in order to prioritize patients for therapy, Dr. Eksteen said.
Despite its main limitation, Dr. Eksteen described this scoring system as extremely timely and valuable in the risk assessment of those with primary biliary cholangitis.
No external funding source was disclosed. Dr. Eksteen reported no conflicts of interest.
Risk stratification for those newly diagnosed with primary biliary cholangitis may be best accomplished through the use of the recently developed and validated UK-PBC scoring system, according to a short review published in Hepatology.
Dr. Bertus Eksteen of the Snyder Institute for Chronic Diseases at the University of Calgary (Alta.) described not only the importance of prompt risk assessment in order to prioritize who should receive therapy and be appropriately counseled, but also the difficulties presented by the current risk stratification scoring systems (Hepatology. 2016 Mar;63:697-9).
In his review, Dr. Eksteen asserts that the primary challenge for clinicians attempting to manage patients with primary biliary cholangitis is the selection of those at risk for disease progression. This assessment is of critical importance, as it informs clinical decision making regarding whether to initiate therapy or avoid it.
The review is partially focused on the advantages and disadvantages associated with the use of the multiple clinical and biochemical parameters that have been used to predict progression in primary biliary cholangitis to date. Additionally, the relative strengths and weaknesses of the UK-PBC scoring system are described.
According to Dr. Eksteen, the UK-PBC risk score represents the most complete tool for the assessment of risk of primary biliary cholangitis progression that can be used for clinical patient counseling. Furthermore, the UK-PBC is described as a scoring system with the potential to become a surrogate marker for primary biliary cholangitis progression and should be factored into the design of clinical trials for new agents in development.
The main limitation associated with the use of the UK-PBC risk score is that certain portions contributing to the overall score require at least 12 months of therapy with the only approved treatment for primary biliary cholangitis, ursodeoxycholic acid. This is problematic, as it does not provide the baseline thresholds necessary in order to prioritize patients for therapy, Dr. Eksteen said.
Despite its main limitation, Dr. Eksteen described this scoring system as extremely timely and valuable in the risk assessment of those with primary biliary cholangitis.
No external funding source was disclosed. Dr. Eksteen reported no conflicts of interest.
FROM HEPATOLOGY
Pathogen-reduced blood may cut transfusion-transmitted malaria
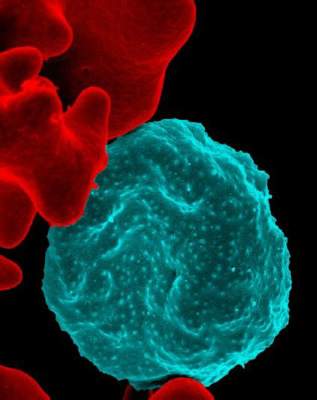
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
The results from the study by Dr. Allain and his associates should prompt efforts to introduce pathogen-reducing technologies for whole blood, red blood cells, or both.
Hope for this anticipated progress in pathogen reduction technology should be growing based on the two pathogen reduction technology systems in development, one of which was used in the study by Dr. Allain and his colleagues (Mirasol; Terumo BCT, Lakewood, Colo.). This method uses riboflavin (vitamin B2) and ultraviolet light to inactivate pathogens in whole blood. The other method (Intercept; Cerus, Concord, Calif.) uses a chemical compound, S-303, and glutathione in the red blood cell product.
The risk that blood recipients in Africa must accept, especially children, would be considered an intolerable risk in developed countries, and pathogen reduction technology that preserves the clinical benefits of transfusion could revolutionize transfusion safety where it is most needed.
Dr. Sheila O’Brien is director of National Epidemiology and Surveillance at Canadian Blood Services and adjunct faculty at the University of Ottawa. She reported having no conflicts of interest. These remarks are adapted from her editorial accompanying the article (Lancet. 2016 Apr 23;387:1701-3).
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
A method for reducing pathogens present in whole blood used for transfusions may reduce the incidence of malaria transmission, and also provide clinical support for patients with severe anemia or hemorrhage, according to the results of a prospective study published April 22 in the Lancet.
“This study is the first to show pathogen reduction treatment of whole blood for transfusion resulted in reduced transmission of a blood-borne infectious parasite in a region hyperendemic for malaria,” wrote Dr. Jean-Pierre Allain of the department of hematology at the University of Cambridge (England) and his coauthors.
The investigators examined the safety and efficacy of the Mirasol pathogen reduction technology system in the African Investigation of the Mirasol System (AIMS) trial. Between March 12, 2014, and November 7, 2014, 227 adults from Ghana with blood group O+ were admitted to the Komfo Anokye Teaching Hospital in Kumasi, and enrolled in this prospective, randomized, parallel-group, double-blind, controlled study of transfusion-transmission of malaria. The patients underwent up to two whole blood transfusions with either pathogen-reduced whole blood (treated), or whole blood prepared and transfused by standard local practice (untreated), within 3 days following randomization. (Lancet. 2016 Apr 23;387:1753-61).
Of the patients completing the study protocol and included in the subsequent primary endpoint analysis, 65 nonparasitemic patients were exposed to parasitemic whole blood (28 treated and 37 untreated) and compared with 99 nonparasitemic control patients who received nonparasitemic whole blood (55 treated and 44 untreated), reported Dr. Allain.
The investigators found that the incidence of transfusion-transmitted malaria was significantly lower for the nonparasitemic patients receiving parasitemic whole blood, than for the nonparasitemic control patients who received nonparasitemic whole blood. Of the 65 patients transfused with parasitemic whole blood, 1 of the 28 treated patients (4%) and 8 of the 37 untreated patients (22%) were found to have contracted transfusion-transmitted malaria. Additionally, the safety profiles of the patients receiving treated or untreated whole blood did not differ and no transfusion-related fatalities occurred.
In developing countries, blood supplies are often contaminated by infectious agents, and blood banking systems cannot afford the newest nucleic acid detection technologies for blood-borne pathogens, the investigators wrote. They suggested that technologies designed to reduce pathogens present in whole blood may be of clinical benefit to both individual patients and health care systems. The use of such methods could result not only in better patient outcomes, but also in greater stability in blood supplies, as well as an associated decrease in treatment costs attributable to reductions in preventable infections.
Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed financial ties to the funding source.
FROM THE LANCET
Key clinical point: The incidence of transfusion-transmitted malaria can be reduced by treating whole blood with a pathogen reduction system.
Major finding: Patients receiving pathogen-reduced whole blood had a lower incidence of transfusion-transmitted malaria (4%) than those who received standard treatment (22%).
Data source: Patients with anemia from a single center in Ghana being supported with whole blood transfusion.
Disclosures: Funding for this project was provided by Terumo BCT, which produces the Mirasol system. All but one of the coauthors disclosed ties to the funding source.
Excess mortality tied to alcohol use disorders disentangled
The substantially increased mortality associated with alcohol abuse disorders may be attributable to familial risk factors and the direct result of the disorders themselves, results of a study published online April 20 suggest.
“These results have clear implications for interventions that seek to reduce the substantially elevated rates of mortality in those with [alcohol use disorders],” Dr. Kenneth S. Kendler and his associates wrote.
The investigators examined the mechanisms underlying the association between alcohol abuse disorders and excess mortality using a large-scale, population-based prospective cohort study design. The pattern of mortality hazard ratios in nine age groups in unrelated members of the general population and in half-siblings, full-siblings, and monozygotic twins discordant for alcohol abuse disorders was assessed using a database including information for all people born in Sweden from 1940 to 1965 who had not died or migrated before1973 or the age of 15 years (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0360).
The total study population included 2,821,036 Swedish nationals, 6.17% of whom were registered for alcohol use disorders. Commensurate with findings from previous studies, those registered for alcohol use disorders had a substantially elevated mortality. After controlling for sex, educational status, and year of birth, the mortality hazard ratio for this population was estimated to be 5.83.
An additional analysis using a linear model showed that the mortality hazard ratio changed across the lifespan and declined rapidly with increasing age. In the youngest age group (15-24 years), the alcohol use disorders–related mortality hazard ratio was 5.04, and the ratio increased to a maximum of 8.19 at ages 30-39 years before showing a slow decline to 4.14 in those aged 65-70 years, reported Dr. Kendler of the Virginia Institute for Psychiatric and Behavioral Genetics at Virginia Commonwealth University in Richmond.
In additional analyses involving the general population and relative pairs discordant for exposure to alcohol use disorders, the findings suggested that the excess rate of death in people with alcohol use disorders was attributable to both predispositions in people who develop alcohol use disorders and the direct effect of the alcohol use disorders themselves.
Funding for this project was provided by grants from the U.S. National Institute of Alcohol Abuse and Alcoholism; the Swedish Research Council; the Swedish Research Council for Health, Working Life and Welfare; and Region Skåne. The authors disclosed no conflicts of interest.
The results from the study by Dr. Kendler and his associates should prompt efforts to better understand and treat alcohol use disorders, Dr. Andreas Heinz and associates wrote in an accompanying editorial.
For example, International Classification of Diseases codes for causes of death should be examined as part of a larger effort to elucidate the roles of alcohol-related aggression, comorbid drug consumption, and other environmental and social risk factors.
Also, sex differences in the prevalence and comorbidity of alcohol and drug use disorders are poorly understood, necessitating an examination of causes of death in different age groups according to sex and alcohol use disorders.
Finally, efforts to reduce harmful alcohol use in the aging population, as opposed to the traditionally targeted young adult population, should be increased to prevent or reduce alcohol use.
Dr. Heinz is affiliated with the department of psychiatry and psychotherapy at the Charité-Universitätsmedizin Berlin, Campus Mitte. The authors reported having no conflicts of interest (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0399).
The results from the study by Dr. Kendler and his associates should prompt efforts to better understand and treat alcohol use disorders, Dr. Andreas Heinz and associates wrote in an accompanying editorial.
For example, International Classification of Diseases codes for causes of death should be examined as part of a larger effort to elucidate the roles of alcohol-related aggression, comorbid drug consumption, and other environmental and social risk factors.
Also, sex differences in the prevalence and comorbidity of alcohol and drug use disorders are poorly understood, necessitating an examination of causes of death in different age groups according to sex and alcohol use disorders.
Finally, efforts to reduce harmful alcohol use in the aging population, as opposed to the traditionally targeted young adult population, should be increased to prevent or reduce alcohol use.
Dr. Heinz is affiliated with the department of psychiatry and psychotherapy at the Charité-Universitätsmedizin Berlin, Campus Mitte. The authors reported having no conflicts of interest (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0399).
The results from the study by Dr. Kendler and his associates should prompt efforts to better understand and treat alcohol use disorders, Dr. Andreas Heinz and associates wrote in an accompanying editorial.
For example, International Classification of Diseases codes for causes of death should be examined as part of a larger effort to elucidate the roles of alcohol-related aggression, comorbid drug consumption, and other environmental and social risk factors.
Also, sex differences in the prevalence and comorbidity of alcohol and drug use disorders are poorly understood, necessitating an examination of causes of death in different age groups according to sex and alcohol use disorders.
Finally, efforts to reduce harmful alcohol use in the aging population, as opposed to the traditionally targeted young adult population, should be increased to prevent or reduce alcohol use.
Dr. Heinz is affiliated with the department of psychiatry and psychotherapy at the Charité-Universitätsmedizin Berlin, Campus Mitte. The authors reported having no conflicts of interest (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0399).
The substantially increased mortality associated with alcohol abuse disorders may be attributable to familial risk factors and the direct result of the disorders themselves, results of a study published online April 20 suggest.
“These results have clear implications for interventions that seek to reduce the substantially elevated rates of mortality in those with [alcohol use disorders],” Dr. Kenneth S. Kendler and his associates wrote.
The investigators examined the mechanisms underlying the association between alcohol abuse disorders and excess mortality using a large-scale, population-based prospective cohort study design. The pattern of mortality hazard ratios in nine age groups in unrelated members of the general population and in half-siblings, full-siblings, and monozygotic twins discordant for alcohol abuse disorders was assessed using a database including information for all people born in Sweden from 1940 to 1965 who had not died or migrated before1973 or the age of 15 years (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0360).
The total study population included 2,821,036 Swedish nationals, 6.17% of whom were registered for alcohol use disorders. Commensurate with findings from previous studies, those registered for alcohol use disorders had a substantially elevated mortality. After controlling for sex, educational status, and year of birth, the mortality hazard ratio for this population was estimated to be 5.83.
An additional analysis using a linear model showed that the mortality hazard ratio changed across the lifespan and declined rapidly with increasing age. In the youngest age group (15-24 years), the alcohol use disorders–related mortality hazard ratio was 5.04, and the ratio increased to a maximum of 8.19 at ages 30-39 years before showing a slow decline to 4.14 in those aged 65-70 years, reported Dr. Kendler of the Virginia Institute for Psychiatric and Behavioral Genetics at Virginia Commonwealth University in Richmond.
In additional analyses involving the general population and relative pairs discordant for exposure to alcohol use disorders, the findings suggested that the excess rate of death in people with alcohol use disorders was attributable to both predispositions in people who develop alcohol use disorders and the direct effect of the alcohol use disorders themselves.
Funding for this project was provided by grants from the U.S. National Institute of Alcohol Abuse and Alcoholism; the Swedish Research Council; the Swedish Research Council for Health, Working Life and Welfare; and Region Skåne. The authors disclosed no conflicts of interest.
The substantially increased mortality associated with alcohol abuse disorders may be attributable to familial risk factors and the direct result of the disorders themselves, results of a study published online April 20 suggest.
“These results have clear implications for interventions that seek to reduce the substantially elevated rates of mortality in those with [alcohol use disorders],” Dr. Kenneth S. Kendler and his associates wrote.
The investigators examined the mechanisms underlying the association between alcohol abuse disorders and excess mortality using a large-scale, population-based prospective cohort study design. The pattern of mortality hazard ratios in nine age groups in unrelated members of the general population and in half-siblings, full-siblings, and monozygotic twins discordant for alcohol abuse disorders was assessed using a database including information for all people born in Sweden from 1940 to 1965 who had not died or migrated before1973 or the age of 15 years (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0360).
The total study population included 2,821,036 Swedish nationals, 6.17% of whom were registered for alcohol use disorders. Commensurate with findings from previous studies, those registered for alcohol use disorders had a substantially elevated mortality. After controlling for sex, educational status, and year of birth, the mortality hazard ratio for this population was estimated to be 5.83.
An additional analysis using a linear model showed that the mortality hazard ratio changed across the lifespan and declined rapidly with increasing age. In the youngest age group (15-24 years), the alcohol use disorders–related mortality hazard ratio was 5.04, and the ratio increased to a maximum of 8.19 at ages 30-39 years before showing a slow decline to 4.14 in those aged 65-70 years, reported Dr. Kendler of the Virginia Institute for Psychiatric and Behavioral Genetics at Virginia Commonwealth University in Richmond.
In additional analyses involving the general population and relative pairs discordant for exposure to alcohol use disorders, the findings suggested that the excess rate of death in people with alcohol use disorders was attributable to both predispositions in people who develop alcohol use disorders and the direct effect of the alcohol use disorders themselves.
Funding for this project was provided by grants from the U.S. National Institute of Alcohol Abuse and Alcoholism; the Swedish Research Council; the Swedish Research Council for Health, Working Life and Welfare; and Region Skåne. The authors disclosed no conflicts of interest.
FROM JAMA PSYCHIATRY
Key clinical point: Both men and women registered with alcohol use disorders showed substantial increases in mortality that differed across the lifespan.
Major finding: Controlling for sex, educational status, and year of birth, the mortality hazard ratio for those registered with alcohol use disorders was 5.83 and peaked at 8.19 in those aged 30-39 years.
Data source: A database of all 2,821,036 people born in Sweden from 1940 to 1965 who had neither died nor migrated prior to 1973 or 15 years of age.
Disclosures: Funding for this project was provided by grants from the U.S. National Institute of Alcohol Abuse and Alcoholism; the Swedish Research Council; the Swedish Research Council for Health, Working Life and Welfare; and Region Skåne. The authors disclosed no conflicts of interest.
Military sexual trauma tied to homelessness risk among veterans
A positive screen for military sexual trauma among recently discharged male and female veterans may be a predictive factor for homelessness. In addition, the association between military sexual trauma and homelessness is stronger among male veterans, results of a retrospective study published April 20 show.
Emily Brignone, Dr. Adi V. Gundlapalli, and their associates examined health care data from the Veterans Health Administration’s 2011 Operation Enduring Freedom and Operation Iraqi Freedom official roster of veterans. All of the veterans separated from the military between fiscal years 2001 and 2011, and used Veterans Health Administration (VHA) services between fiscal years 2004 and 2013 (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0101).
The total study population included 601,892, 590,989, and 262,589 U.S. veterans who screened positive for military sexual trauma at 30 days, 1 year, and 5 years, respectively, after their initial VHA visit, reported Ms. Brignone and Dr. Gundlapalli, both of whom are affiliated with the Informatics, Decision Enhancement, and Analytic Sciences Center at the VA Salt Lake City Health Care System.
They found that the incidence of homelessness in this population was 1.6%, 4.4%, and 9.6% within 30 days, 1 year, and 5 years, respectively. The rates for male veterans were higher than for their female counterparts, as evidenced by 30-day, 1-year, and 5-year homelessness rates of 2.3%, 6.2%, and 11.8%, respectively, compared with 1.3%, 3.9%, and 8.9%. About 25% of female veterans report experiencing sexual trauma during their military service, compared with 1% of male veterans, research shows (Am J Public Health. 2007;97[12]:2160-6).
Meanwhile, the rates of positive military sexual trauma screens among homeless veterans were almost twice as high, compared with the rates of veterans who were not homeless (0.7%, 1.8%, and 4.3%, respectively).
Logistic regression analysis models adjusted for mental health and substance use diagnoses showed that military sexual trauma screen status remained significantly associated with homelessness, such that veterans with a positive military sexual trauma screen were roughly 1.5-fold more likely to be homelessness than those with a negative screen. The adjusted models also showed that the interaction between military sexual trauma status and sex remained significant for the 30-day and 1-year cohorts.
Ms. Brignone, Dr. Gundlapalli, and their associates cited several limitations. For example, a positive screen for military sexual trauma is a self-reported marker rather than a diagnosis. “Because a positive screen for [military sexual trauma] is associated with increased service use, there may be more opportunities to detect homelessness among veterans with a positive screen,” they wrote.
The investigators said further research is needed to understand the temporal associations between sexual trauma, mental health diagnoses, and sex-dependent differences. Understanding those associations might be useful in attempts at prevention and intervention of postdeployment homelessness, they wrote.
A U.S. Department of Veterans Affairs grant funded this project. The authors disclosed no conflicts of interest.
The results of the study by Emily Brignone, Dr. Adi V. Gundlapalli, and their associates should promote zero tolerance for the perpetration of sexual trauma in the military, Natalie Mota, Ph.D., and her associates wrote in an accompanying editorial. “Education and awareness about the widespread deleterious effects of [military sexual trauma] on mental and physical health as well as military cohesion and productivity could help to advance this aim,” they wrote.
Ms. Brignone’s study also should prompt efforts to identify veterans with military sexual trauma in order to facilitate timely connections to evidence-based interventions such as Housing First approaches. Also, continued research focused on personalizing screening and outreach efforts specifically targeted to this population will be required to identify veterans at increased risk for postdeployment homelessness, they wrote.
Other possible solutions to reducing postdeployment homelessness are facilitated, supported, and encouraged reporting of military sexual trauma, sensitive and effective assessment of military sexual trauma, and facilitated access to evidence-based interventions for military sexual trauma–related mental health problems across health care systems.
Dr. Mota is affiliated with the department of clinical health psychology at the University of Manitoba in Winnipeg (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0136).
The results of the study by Emily Brignone, Dr. Adi V. Gundlapalli, and their associates should promote zero tolerance for the perpetration of sexual trauma in the military, Natalie Mota, Ph.D., and her associates wrote in an accompanying editorial. “Education and awareness about the widespread deleterious effects of [military sexual trauma] on mental and physical health as well as military cohesion and productivity could help to advance this aim,” they wrote.
Ms. Brignone’s study also should prompt efforts to identify veterans with military sexual trauma in order to facilitate timely connections to evidence-based interventions such as Housing First approaches. Also, continued research focused on personalizing screening and outreach efforts specifically targeted to this population will be required to identify veterans at increased risk for postdeployment homelessness, they wrote.
Other possible solutions to reducing postdeployment homelessness are facilitated, supported, and encouraged reporting of military sexual trauma, sensitive and effective assessment of military sexual trauma, and facilitated access to evidence-based interventions for military sexual trauma–related mental health problems across health care systems.
Dr. Mota is affiliated with the department of clinical health psychology at the University of Manitoba in Winnipeg (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0136).
The results of the study by Emily Brignone, Dr. Adi V. Gundlapalli, and their associates should promote zero tolerance for the perpetration of sexual trauma in the military, Natalie Mota, Ph.D., and her associates wrote in an accompanying editorial. “Education and awareness about the widespread deleterious effects of [military sexual trauma] on mental and physical health as well as military cohesion and productivity could help to advance this aim,” they wrote.
Ms. Brignone’s study also should prompt efforts to identify veterans with military sexual trauma in order to facilitate timely connections to evidence-based interventions such as Housing First approaches. Also, continued research focused on personalizing screening and outreach efforts specifically targeted to this population will be required to identify veterans at increased risk for postdeployment homelessness, they wrote.
Other possible solutions to reducing postdeployment homelessness are facilitated, supported, and encouraged reporting of military sexual trauma, sensitive and effective assessment of military sexual trauma, and facilitated access to evidence-based interventions for military sexual trauma–related mental health problems across health care systems.
Dr. Mota is affiliated with the department of clinical health psychology at the University of Manitoba in Winnipeg (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0136).
A positive screen for military sexual trauma among recently discharged male and female veterans may be a predictive factor for homelessness. In addition, the association between military sexual trauma and homelessness is stronger among male veterans, results of a retrospective study published April 20 show.
Emily Brignone, Dr. Adi V. Gundlapalli, and their associates examined health care data from the Veterans Health Administration’s 2011 Operation Enduring Freedom and Operation Iraqi Freedom official roster of veterans. All of the veterans separated from the military between fiscal years 2001 and 2011, and used Veterans Health Administration (VHA) services between fiscal years 2004 and 2013 (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0101).
The total study population included 601,892, 590,989, and 262,589 U.S. veterans who screened positive for military sexual trauma at 30 days, 1 year, and 5 years, respectively, after their initial VHA visit, reported Ms. Brignone and Dr. Gundlapalli, both of whom are affiliated with the Informatics, Decision Enhancement, and Analytic Sciences Center at the VA Salt Lake City Health Care System.
They found that the incidence of homelessness in this population was 1.6%, 4.4%, and 9.6% within 30 days, 1 year, and 5 years, respectively. The rates for male veterans were higher than for their female counterparts, as evidenced by 30-day, 1-year, and 5-year homelessness rates of 2.3%, 6.2%, and 11.8%, respectively, compared with 1.3%, 3.9%, and 8.9%. About 25% of female veterans report experiencing sexual trauma during their military service, compared with 1% of male veterans, research shows (Am J Public Health. 2007;97[12]:2160-6).
Meanwhile, the rates of positive military sexual trauma screens among homeless veterans were almost twice as high, compared with the rates of veterans who were not homeless (0.7%, 1.8%, and 4.3%, respectively).
Logistic regression analysis models adjusted for mental health and substance use diagnoses showed that military sexual trauma screen status remained significantly associated with homelessness, such that veterans with a positive military sexual trauma screen were roughly 1.5-fold more likely to be homelessness than those with a negative screen. The adjusted models also showed that the interaction between military sexual trauma status and sex remained significant for the 30-day and 1-year cohorts.
Ms. Brignone, Dr. Gundlapalli, and their associates cited several limitations. For example, a positive screen for military sexual trauma is a self-reported marker rather than a diagnosis. “Because a positive screen for [military sexual trauma] is associated with increased service use, there may be more opportunities to detect homelessness among veterans with a positive screen,” they wrote.
The investigators said further research is needed to understand the temporal associations between sexual trauma, mental health diagnoses, and sex-dependent differences. Understanding those associations might be useful in attempts at prevention and intervention of postdeployment homelessness, they wrote.
A U.S. Department of Veterans Affairs grant funded this project. The authors disclosed no conflicts of interest.
A positive screen for military sexual trauma among recently discharged male and female veterans may be a predictive factor for homelessness. In addition, the association between military sexual trauma and homelessness is stronger among male veterans, results of a retrospective study published April 20 show.
Emily Brignone, Dr. Adi V. Gundlapalli, and their associates examined health care data from the Veterans Health Administration’s 2011 Operation Enduring Freedom and Operation Iraqi Freedom official roster of veterans. All of the veterans separated from the military between fiscal years 2001 and 2011, and used Veterans Health Administration (VHA) services between fiscal years 2004 and 2013 (JAMA Psychiatry. 2016 Apr 20. doi: 10.1001/jamapsychiatry.2016.0101).
The total study population included 601,892, 590,989, and 262,589 U.S. veterans who screened positive for military sexual trauma at 30 days, 1 year, and 5 years, respectively, after their initial VHA visit, reported Ms. Brignone and Dr. Gundlapalli, both of whom are affiliated with the Informatics, Decision Enhancement, and Analytic Sciences Center at the VA Salt Lake City Health Care System.
They found that the incidence of homelessness in this population was 1.6%, 4.4%, and 9.6% within 30 days, 1 year, and 5 years, respectively. The rates for male veterans were higher than for their female counterparts, as evidenced by 30-day, 1-year, and 5-year homelessness rates of 2.3%, 6.2%, and 11.8%, respectively, compared with 1.3%, 3.9%, and 8.9%. About 25% of female veterans report experiencing sexual trauma during their military service, compared with 1% of male veterans, research shows (Am J Public Health. 2007;97[12]:2160-6).
Meanwhile, the rates of positive military sexual trauma screens among homeless veterans were almost twice as high, compared with the rates of veterans who were not homeless (0.7%, 1.8%, and 4.3%, respectively).
Logistic regression analysis models adjusted for mental health and substance use diagnoses showed that military sexual trauma screen status remained significantly associated with homelessness, such that veterans with a positive military sexual trauma screen were roughly 1.5-fold more likely to be homelessness than those with a negative screen. The adjusted models also showed that the interaction between military sexual trauma status and sex remained significant for the 30-day and 1-year cohorts.
Ms. Brignone, Dr. Gundlapalli, and their associates cited several limitations. For example, a positive screen for military sexual trauma is a self-reported marker rather than a diagnosis. “Because a positive screen for [military sexual trauma] is associated with increased service use, there may be more opportunities to detect homelessness among veterans with a positive screen,” they wrote.
The investigators said further research is needed to understand the temporal associations between sexual trauma, mental health diagnoses, and sex-dependent differences. Understanding those associations might be useful in attempts at prevention and intervention of postdeployment homelessness, they wrote.
A U.S. Department of Veterans Affairs grant funded this project. The authors disclosed no conflicts of interest.
FROM JAMA PSYCHIATRY
Key clinical point: Male and female U.S. veterans who screen positive for military sexual trauma have an increased risk of homelessness postdeployment.
Major finding: The primary outcome – the incidence of homelessness among veterans with a positive screen for military sexual trauma – was 1.6% within 30 days, 4.4% within 1 year, and 9.6% within 5 years.
Data source: Health care data on three cohorts (30 days, 1 year, and 5 years) of veterans who separated from the military between fiscal years 2001 and 2011 from the Veterans Health Administration’s 2011 Operation Enduring Freedom and Operation Iraqi Freedom official roster.
Disclosures: A U.S. Department of Veterans Affairs grant funded this project. The authors disclosed no conflicts of interest.
Standardized policies reduce health care utilization for neonatal abstinence syndrome
The standardization of hospital patient care policies was effective in decreasing health care utilization, such as length of pharmacotherapy and length of hospital stay, for infants with neonatal abstinence syndrome (NAS) according to a report published online April 15 in Pediatrics.
Assessment of the effects of a multicenter, multistate quality improvement collaborative focused on infants requiring pharmacologic treatment for NAS on patient outcomes, including length of pharmacotherapy (LOT), length of hospital stay (LOS), discharge on human milk, discharge with a parent, and discharge on a medication, was undertaken by Dr. Stephen W. Patrick of the departments of pediatrics, health policy, and the Mildred Stahlman Division of Neonatology and the Vanderbilt Center for Health Services Research, both in Nashville, and his colleagues.
In a prospective cohort study, four preplanned serial, cross-sectional quality audits of centers enrolled in the Vermont Oxford Network (VON) NAS Internet-Based Quality Improvement Collaborative were conducted in February 2013, August 2013, February 2014, and August 2014 (Pediatrics. 2016 Apr 15. doi: 10.1542/peds.2015-3835).
The study produced several findings indicative of improved hospital performance and patient outcomes based on the serial audit data from the 199 participating centers. Collectively, the centers examined the medical records of 3,458 infants with NAS, most of whom were born at term (78%) and treated with morphine (83%). Study data suggested that the participating centers effectively standardized their care, as evidenced by a significant increase in their mean number of policies from 3.7 to 5.1 of the 6 measured. Additionally, centers showed significant improvements in all measured policies, which included those focused on the following:
• Maternal substance screening.
• Evaluation and treatment of substance-exposed infants.
• Standardized NAS scoring.
• Inclusion of nonpharmacologic treatment strategies for NAS.
• Standardizing the pharmacologic treatment of NAS.
• The provision of human milk for substance-exposed infants.
As for patient outcomes, the median LOT and LOS decreased by 1 and 2 days, respectively (from 16 to 15 days for LOT [P = .02] and from 21 to 19 days for LOS [P = .002]). In an exploratory analysis, only policies to standardize NAS scoring were found to be significantly associated with improved patient outcomes: changes in LOT of –2.1 days and LOS of –3.1 days. Also, the proportion of infants discharged on a medication taper decreased from 39.7% to 26.5%, the investigators reported.
Dr. Patrick and his associates said that their findings support the American Academy of Pediatrics’ 2012 policy statement calling for standardization of NAS care by showing that such measures result in improved patient outcomes. Additionally, their model showed the ability to achieve rapid-cycle adoption of practice guidelines and that state governments and health agencies can collaborate to improve neonatal care and reduce costs through partnerships with structured systematic quality improvement collaboratives like VON.
This study was supported by the National Center for Advancing Translational Sciences and the National Institute on Drug Abuse, both part of the National Institutes of Health. Dr. Patrick and Dr. Schumacher are consultants to the VON and five other investigators are employees of VON; the other authors indicated no relevant financial relationships.
The standardization of hospital patient care policies was effective in decreasing health care utilization, such as length of pharmacotherapy and length of hospital stay, for infants with neonatal abstinence syndrome (NAS) according to a report published online April 15 in Pediatrics.
Assessment of the effects of a multicenter, multistate quality improvement collaborative focused on infants requiring pharmacologic treatment for NAS on patient outcomes, including length of pharmacotherapy (LOT), length of hospital stay (LOS), discharge on human milk, discharge with a parent, and discharge on a medication, was undertaken by Dr. Stephen W. Patrick of the departments of pediatrics, health policy, and the Mildred Stahlman Division of Neonatology and the Vanderbilt Center for Health Services Research, both in Nashville, and his colleagues.
In a prospective cohort study, four preplanned serial, cross-sectional quality audits of centers enrolled in the Vermont Oxford Network (VON) NAS Internet-Based Quality Improvement Collaborative were conducted in February 2013, August 2013, February 2014, and August 2014 (Pediatrics. 2016 Apr 15. doi: 10.1542/peds.2015-3835).
The study produced several findings indicative of improved hospital performance and patient outcomes based on the serial audit data from the 199 participating centers. Collectively, the centers examined the medical records of 3,458 infants with NAS, most of whom were born at term (78%) and treated with morphine (83%). Study data suggested that the participating centers effectively standardized their care, as evidenced by a significant increase in their mean number of policies from 3.7 to 5.1 of the 6 measured. Additionally, centers showed significant improvements in all measured policies, which included those focused on the following:
• Maternal substance screening.
• Evaluation and treatment of substance-exposed infants.
• Standardized NAS scoring.
• Inclusion of nonpharmacologic treatment strategies for NAS.
• Standardizing the pharmacologic treatment of NAS.
• The provision of human milk for substance-exposed infants.
As for patient outcomes, the median LOT and LOS decreased by 1 and 2 days, respectively (from 16 to 15 days for LOT [P = .02] and from 21 to 19 days for LOS [P = .002]). In an exploratory analysis, only policies to standardize NAS scoring were found to be significantly associated with improved patient outcomes: changes in LOT of –2.1 days and LOS of –3.1 days. Also, the proportion of infants discharged on a medication taper decreased from 39.7% to 26.5%, the investigators reported.
Dr. Patrick and his associates said that their findings support the American Academy of Pediatrics’ 2012 policy statement calling for standardization of NAS care by showing that such measures result in improved patient outcomes. Additionally, their model showed the ability to achieve rapid-cycle adoption of practice guidelines and that state governments and health agencies can collaborate to improve neonatal care and reduce costs through partnerships with structured systematic quality improvement collaboratives like VON.
This study was supported by the National Center for Advancing Translational Sciences and the National Institute on Drug Abuse, both part of the National Institutes of Health. Dr. Patrick and Dr. Schumacher are consultants to the VON and five other investigators are employees of VON; the other authors indicated no relevant financial relationships.
The standardization of hospital patient care policies was effective in decreasing health care utilization, such as length of pharmacotherapy and length of hospital stay, for infants with neonatal abstinence syndrome (NAS) according to a report published online April 15 in Pediatrics.
Assessment of the effects of a multicenter, multistate quality improvement collaborative focused on infants requiring pharmacologic treatment for NAS on patient outcomes, including length of pharmacotherapy (LOT), length of hospital stay (LOS), discharge on human milk, discharge with a parent, and discharge on a medication, was undertaken by Dr. Stephen W. Patrick of the departments of pediatrics, health policy, and the Mildred Stahlman Division of Neonatology and the Vanderbilt Center for Health Services Research, both in Nashville, and his colleagues.
In a prospective cohort study, four preplanned serial, cross-sectional quality audits of centers enrolled in the Vermont Oxford Network (VON) NAS Internet-Based Quality Improvement Collaborative were conducted in February 2013, August 2013, February 2014, and August 2014 (Pediatrics. 2016 Apr 15. doi: 10.1542/peds.2015-3835).
The study produced several findings indicative of improved hospital performance and patient outcomes based on the serial audit data from the 199 participating centers. Collectively, the centers examined the medical records of 3,458 infants with NAS, most of whom were born at term (78%) and treated with morphine (83%). Study data suggested that the participating centers effectively standardized their care, as evidenced by a significant increase in their mean number of policies from 3.7 to 5.1 of the 6 measured. Additionally, centers showed significant improvements in all measured policies, which included those focused on the following:
• Maternal substance screening.
• Evaluation and treatment of substance-exposed infants.
• Standardized NAS scoring.
• Inclusion of nonpharmacologic treatment strategies for NAS.
• Standardizing the pharmacologic treatment of NAS.
• The provision of human milk for substance-exposed infants.
As for patient outcomes, the median LOT and LOS decreased by 1 and 2 days, respectively (from 16 to 15 days for LOT [P = .02] and from 21 to 19 days for LOS [P = .002]). In an exploratory analysis, only policies to standardize NAS scoring were found to be significantly associated with improved patient outcomes: changes in LOT of –2.1 days and LOS of –3.1 days. Also, the proportion of infants discharged on a medication taper decreased from 39.7% to 26.5%, the investigators reported.
Dr. Patrick and his associates said that their findings support the American Academy of Pediatrics’ 2012 policy statement calling for standardization of NAS care by showing that such measures result in improved patient outcomes. Additionally, their model showed the ability to achieve rapid-cycle adoption of practice guidelines and that state governments and health agencies can collaborate to improve neonatal care and reduce costs through partnerships with structured systematic quality improvement collaboratives like VON.
This study was supported by the National Center for Advancing Translational Sciences and the National Institute on Drug Abuse, both part of the National Institutes of Health. Dr. Patrick and Dr. Schumacher are consultants to the VON and five other investigators are employees of VON; the other authors indicated no relevant financial relationships.
FROM PEDIATRICS
Key clinical point: The standardization of hospital patient care policies was effective in decreasing health care utilization for infants with NAS.
Major finding: The length of pharmacotherapy and hospital stay for infants with NAS were significantly reduced 1 and 2 days, respectively, by a program designed to standardize patient health care policies across participating hospitals.
Data sources: Prospective cohort study using serial cross-sectional audits of 3,458 infants with NAS in 199 centers enrolled in the VON NAS Internet-Based Quality Improvement Collaborative conducted in 2013-2014.
Disclosures: This study was supported by the National Center for Advancing Translational Sciences and the National Institute on Drug Abuse, both part of the National Institutes of Health. Dr. Patrick and Dr. Schumacher are consultants to the VON and five other investigators are employees of VON; the other authors indicated no relevant financial relationships.
New Analysis Bolsters Metformin as First Line in Type 2 Diabetes
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.