User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Use of complimentary and alternative medicine common in diabetes patients
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
FROM THE EUROPEAN JOURNAL OF CLINICAL PHARMACOLOGY
The best exercises for BP control? European statement sorts it out
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
FROM THE EUROPEAN JOURNAL OF PREVENTIVE CARDIOLOGY
Long-haul COVID-19 brings welcome attention to POTS
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.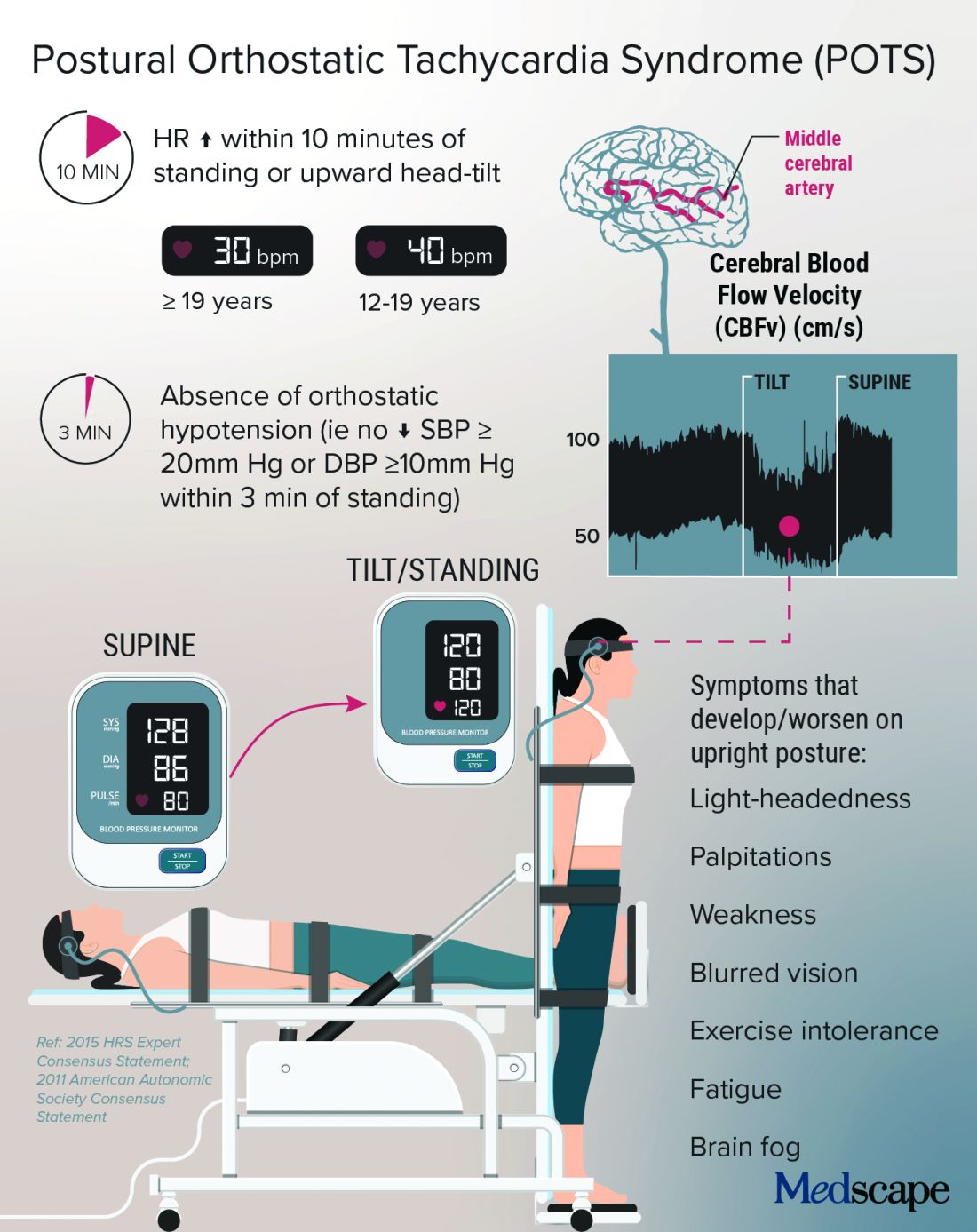
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.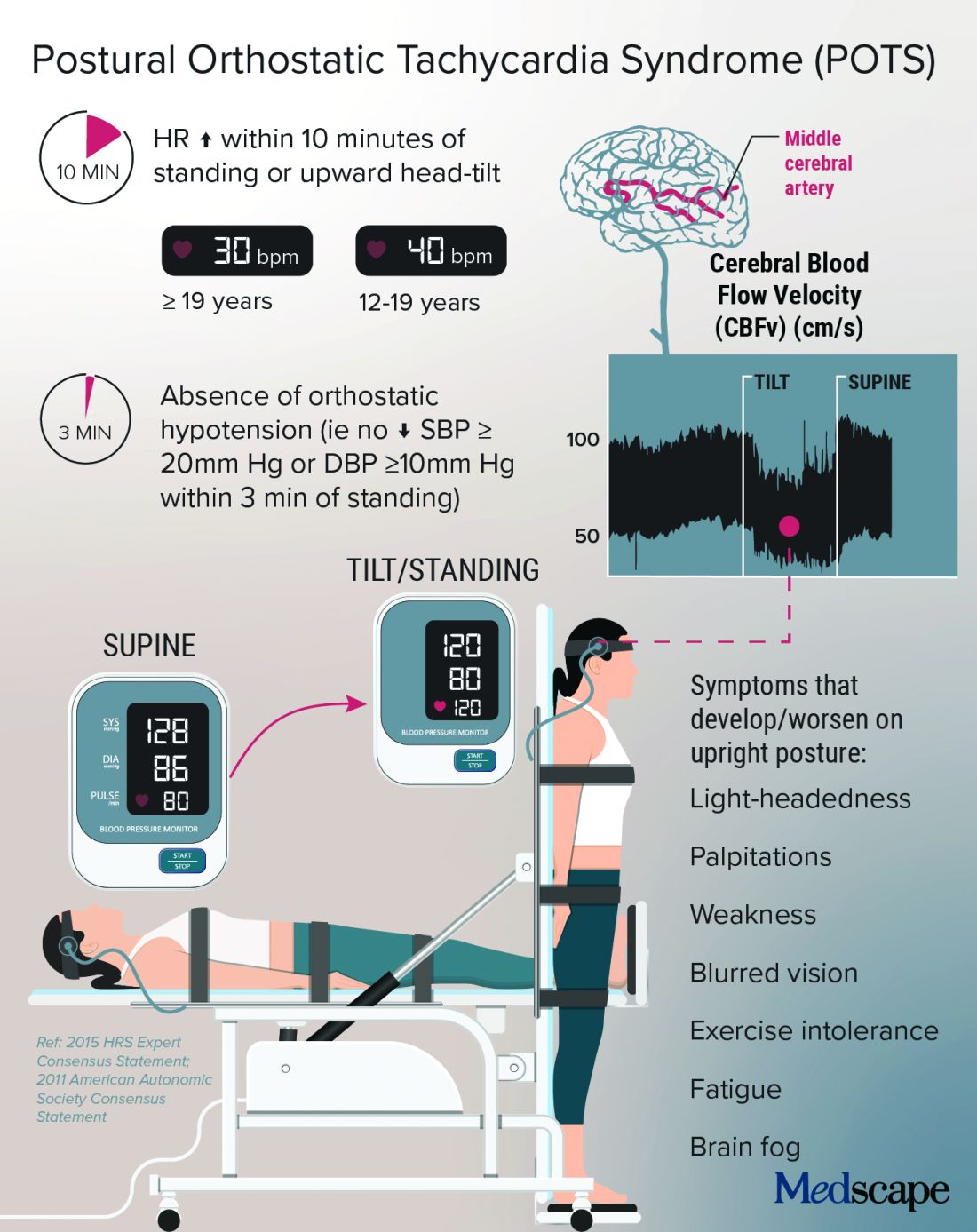
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.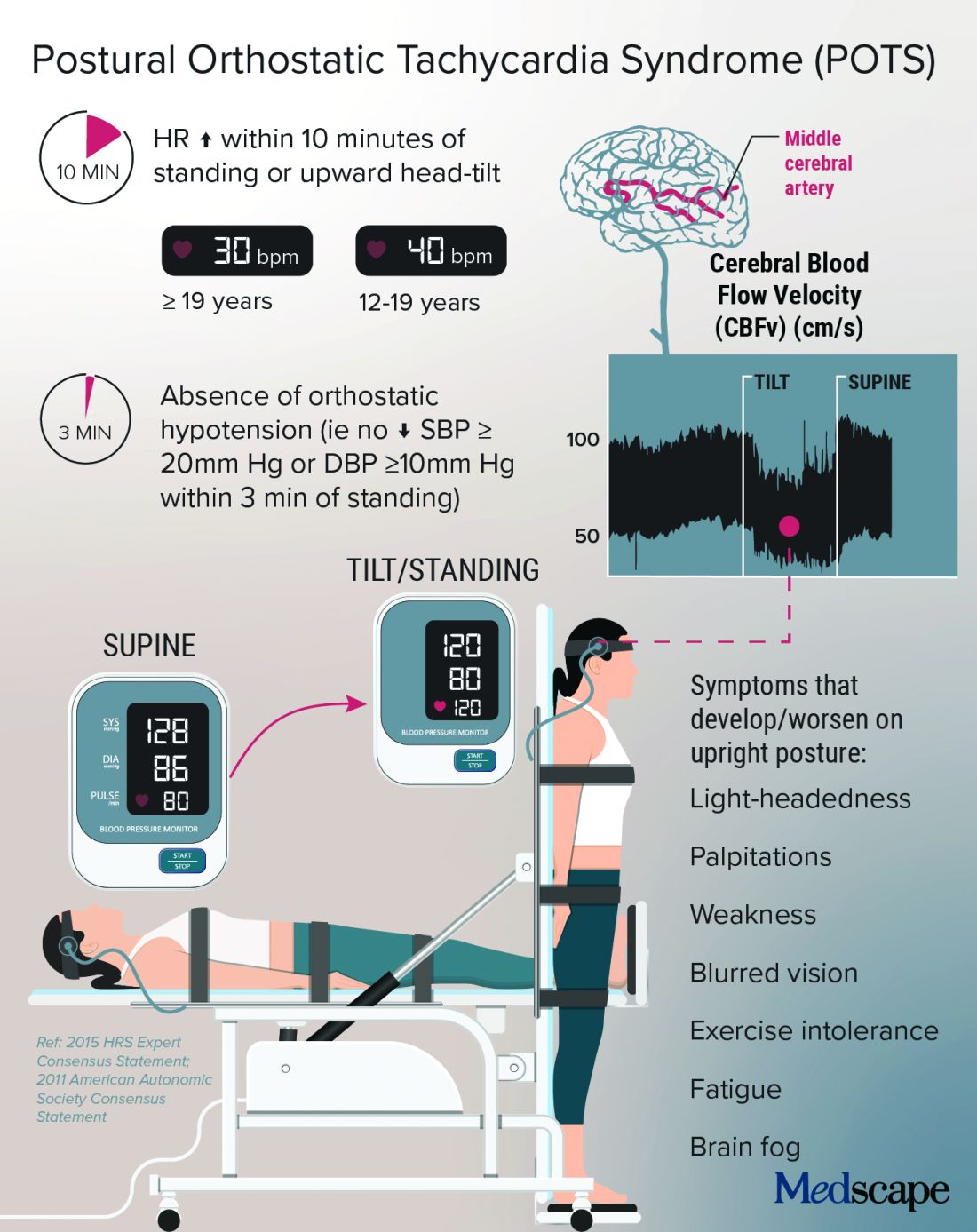
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Febuxostat, allopurinol real-world cardiovascular risk appears equal
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Cardiologist forks out $2M to resolve unnecessary testing claims
Michigan cardiologist Dinesh M. Shah, MD, has paid the United States $2 million to resolve claims he violated the False Claims Act by knowingly billing federal health care programs for diagnostic tests that were unnecessary or not performed, the Department of Justice announced.
The settlement resolves allegations that, from 2006 to 2017, Dr. Shah and his practice, Michigan Physicians Group (MPG), of which he is sole owner, billed Medicare, Medicaid, and TRICARE for unnecessary diagnostic tests, including ankle brachial index and toe brachial index tests that were routinely performed on patients without first being ordered by a physician and without regard to medical necessity.
The prosecutors also alleged that Dr. Shah was routinely ordering, and MPG was providing, unnecessary nuclear stress tests to some patients.
“Subjecting patients to unnecessary testing in order to fill one’s pockets with taxpayer funds will not be tolerated. Such practices are particularly concerning because overuse of some tests can be harmful to patients,” acting U.S. Attorney Saima Mohsin said in the news release. “With these lawsuits and the accompanying resolution, Dr. Shah and Michigan Physicians Group are being held to account for these exploitative and improper past practices.”
In addition to the settlement, Dr. Shah and MPG entered into an Integrity Agreement with the Office of Inspector General for the Department of Health & Human Services, which will provide oversight of Dr. Shah and MPG’s billing practices for a 3-year period.
There was “no determination of liability” with the settlement, according to the Department of Justice. Dr. Shah’s case was sparked by two whistleblower lawsuits filed by Arlene Klinke and Khrystyna Malva, both former MPG employees.
The settlement comes after a years-long investigation by the HHS acting on behalf of TRICARE, a health care program for active and retired military members. Allegations that William Beaumont Hospital in Royal Oak, Mich., paid eight physicians excessive compensation to increase patient referrals led to an $84.5 million settlement in 2018.
Dr. Shah was one of three private practice cardiologists who denied involvement in the scheme but were named in the settlement, according to Crain’s Detroit Business.
A version of this article first appeared on Medscape.com.
Michigan cardiologist Dinesh M. Shah, MD, has paid the United States $2 million to resolve claims he violated the False Claims Act by knowingly billing federal health care programs for diagnostic tests that were unnecessary or not performed, the Department of Justice announced.
The settlement resolves allegations that, from 2006 to 2017, Dr. Shah and his practice, Michigan Physicians Group (MPG), of which he is sole owner, billed Medicare, Medicaid, and TRICARE for unnecessary diagnostic tests, including ankle brachial index and toe brachial index tests that were routinely performed on patients without first being ordered by a physician and without regard to medical necessity.
The prosecutors also alleged that Dr. Shah was routinely ordering, and MPG was providing, unnecessary nuclear stress tests to some patients.
“Subjecting patients to unnecessary testing in order to fill one’s pockets with taxpayer funds will not be tolerated. Such practices are particularly concerning because overuse of some tests can be harmful to patients,” acting U.S. Attorney Saima Mohsin said in the news release. “With these lawsuits and the accompanying resolution, Dr. Shah and Michigan Physicians Group are being held to account for these exploitative and improper past practices.”
In addition to the settlement, Dr. Shah and MPG entered into an Integrity Agreement with the Office of Inspector General for the Department of Health & Human Services, which will provide oversight of Dr. Shah and MPG’s billing practices for a 3-year period.
There was “no determination of liability” with the settlement, according to the Department of Justice. Dr. Shah’s case was sparked by two whistleblower lawsuits filed by Arlene Klinke and Khrystyna Malva, both former MPG employees.
The settlement comes after a years-long investigation by the HHS acting on behalf of TRICARE, a health care program for active and retired military members. Allegations that William Beaumont Hospital in Royal Oak, Mich., paid eight physicians excessive compensation to increase patient referrals led to an $84.5 million settlement in 2018.
Dr. Shah was one of three private practice cardiologists who denied involvement in the scheme but were named in the settlement, according to Crain’s Detroit Business.
A version of this article first appeared on Medscape.com.
Michigan cardiologist Dinesh M. Shah, MD, has paid the United States $2 million to resolve claims he violated the False Claims Act by knowingly billing federal health care programs for diagnostic tests that were unnecessary or not performed, the Department of Justice announced.
The settlement resolves allegations that, from 2006 to 2017, Dr. Shah and his practice, Michigan Physicians Group (MPG), of which he is sole owner, billed Medicare, Medicaid, and TRICARE for unnecessary diagnostic tests, including ankle brachial index and toe brachial index tests that were routinely performed on patients without first being ordered by a physician and without regard to medical necessity.
The prosecutors also alleged that Dr. Shah was routinely ordering, and MPG was providing, unnecessary nuclear stress tests to some patients.
“Subjecting patients to unnecessary testing in order to fill one’s pockets with taxpayer funds will not be tolerated. Such practices are particularly concerning because overuse of some tests can be harmful to patients,” acting U.S. Attorney Saima Mohsin said in the news release. “With these lawsuits and the accompanying resolution, Dr. Shah and Michigan Physicians Group are being held to account for these exploitative and improper past practices.”
In addition to the settlement, Dr. Shah and MPG entered into an Integrity Agreement with the Office of Inspector General for the Department of Health & Human Services, which will provide oversight of Dr. Shah and MPG’s billing practices for a 3-year period.
There was “no determination of liability” with the settlement, according to the Department of Justice. Dr. Shah’s case was sparked by two whistleblower lawsuits filed by Arlene Klinke and Khrystyna Malva, both former MPG employees.
The settlement comes after a years-long investigation by the HHS acting on behalf of TRICARE, a health care program for active and retired military members. Allegations that William Beaumont Hospital in Royal Oak, Mich., paid eight physicians excessive compensation to increase patient referrals led to an $84.5 million settlement in 2018.
Dr. Shah was one of three private practice cardiologists who denied involvement in the scheme but were named in the settlement, according to Crain’s Detroit Business.
A version of this article first appeared on Medscape.com.
FDA okays transcatheter pulmonary valve for congenital heart disease
The Food and Drug Administration has approved Medtronic’s Harmony Transcatheter Pulmonary Valve (TPV) System to treat severe pulmonary regurgitation in pediatric and adult patients who have a native or surgically repaired right ventricular outflow tract (RVOT).
The Harmony TPV is the first nonsurgical heart valve to treat severe pulmonary valve regurgitation, which is common in patients with congenital heart disease, the agency said in a news release. Its use can delay the time before a patient needs open-heart surgery and potentially reduce the number of these surgeries required over a lifetime.
“The Harmony TPV provides a new treatment option for adult and pediatric patients with certain types of congenital heart disease,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the statement.
“It offers a less-invasive treatment alternative to open-heart surgery to patients with a leaky native or surgically repaired RVOT and may help patients improve their quality of life and return to their normal activities more quickly, thus fulfilling an unmet clinical need of many patients with congenital heart disease,” he said.
The Harmony valve, which was granted breakthrough device designation, is a 22-mm or 25-mm porcine pericardium valve, sewn to a nitinol frame. It is implanted with a 25-French delivery system using a coil-loading catheter.
The FDA approval was based on the 70-patient prospective, nonrandomized, multicenter Harmony TPV Clinical study, in which 100% of patients achieved the primary safety endpoint of no procedure or device-related deaths 30 days after implantation.
Among 65 patients with evaluable echocardiographic data, 89.2% met the primary effectiveness endpoint of no additional surgical or interventional device-related procedures and acceptable heart blood flow at 6 months.
Adverse events included irregular or abnormal heart rhythms in 23.9% of patients, including 14.1% ventricular tachycardia; leakage around the valve in 8.5%, including 1.4% major leakage; minor bleeding in 7.0%, narrowing of the pulmonary valve in 4.2%, and movement of the implant in 4.2%.
Follow-up was scheduled annually through 5 years and has been extended to 10 years as part of the postapproval study, the FDA noted.
The Harmony TPV device is contraindicated for patients with an infection in the heart or elsewhere, for patients who cannot tolerate blood-thinning medicines, and for those with a sensitivity to nitinol (titanium or nickel).
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved Medtronic’s Harmony Transcatheter Pulmonary Valve (TPV) System to treat severe pulmonary regurgitation in pediatric and adult patients who have a native or surgically repaired right ventricular outflow tract (RVOT).
The Harmony TPV is the first nonsurgical heart valve to treat severe pulmonary valve regurgitation, which is common in patients with congenital heart disease, the agency said in a news release. Its use can delay the time before a patient needs open-heart surgery and potentially reduce the number of these surgeries required over a lifetime.
“The Harmony TPV provides a new treatment option for adult and pediatric patients with certain types of congenital heart disease,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the statement.
“It offers a less-invasive treatment alternative to open-heart surgery to patients with a leaky native or surgically repaired RVOT and may help patients improve their quality of life and return to their normal activities more quickly, thus fulfilling an unmet clinical need of many patients with congenital heart disease,” he said.
The Harmony valve, which was granted breakthrough device designation, is a 22-mm or 25-mm porcine pericardium valve, sewn to a nitinol frame. It is implanted with a 25-French delivery system using a coil-loading catheter.
The FDA approval was based on the 70-patient prospective, nonrandomized, multicenter Harmony TPV Clinical study, in which 100% of patients achieved the primary safety endpoint of no procedure or device-related deaths 30 days after implantation.
Among 65 patients with evaluable echocardiographic data, 89.2% met the primary effectiveness endpoint of no additional surgical or interventional device-related procedures and acceptable heart blood flow at 6 months.
Adverse events included irregular or abnormal heart rhythms in 23.9% of patients, including 14.1% ventricular tachycardia; leakage around the valve in 8.5%, including 1.4% major leakage; minor bleeding in 7.0%, narrowing of the pulmonary valve in 4.2%, and movement of the implant in 4.2%.
Follow-up was scheduled annually through 5 years and has been extended to 10 years as part of the postapproval study, the FDA noted.
The Harmony TPV device is contraindicated for patients with an infection in the heart or elsewhere, for patients who cannot tolerate blood-thinning medicines, and for those with a sensitivity to nitinol (titanium or nickel).
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved Medtronic’s Harmony Transcatheter Pulmonary Valve (TPV) System to treat severe pulmonary regurgitation in pediatric and adult patients who have a native or surgically repaired right ventricular outflow tract (RVOT).
The Harmony TPV is the first nonsurgical heart valve to treat severe pulmonary valve regurgitation, which is common in patients with congenital heart disease, the agency said in a news release. Its use can delay the time before a patient needs open-heart surgery and potentially reduce the number of these surgeries required over a lifetime.
“The Harmony TPV provides a new treatment option for adult and pediatric patients with certain types of congenital heart disease,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the statement.
“It offers a less-invasive treatment alternative to open-heart surgery to patients with a leaky native or surgically repaired RVOT and may help patients improve their quality of life and return to their normal activities more quickly, thus fulfilling an unmet clinical need of many patients with congenital heart disease,” he said.
The Harmony valve, which was granted breakthrough device designation, is a 22-mm or 25-mm porcine pericardium valve, sewn to a nitinol frame. It is implanted with a 25-French delivery system using a coil-loading catheter.
The FDA approval was based on the 70-patient prospective, nonrandomized, multicenter Harmony TPV Clinical study, in which 100% of patients achieved the primary safety endpoint of no procedure or device-related deaths 30 days after implantation.
Among 65 patients with evaluable echocardiographic data, 89.2% met the primary effectiveness endpoint of no additional surgical or interventional device-related procedures and acceptable heart blood flow at 6 months.
Adverse events included irregular or abnormal heart rhythms in 23.9% of patients, including 14.1% ventricular tachycardia; leakage around the valve in 8.5%, including 1.4% major leakage; minor bleeding in 7.0%, narrowing of the pulmonary valve in 4.2%, and movement of the implant in 4.2%.
Follow-up was scheduled annually through 5 years and has been extended to 10 years as part of the postapproval study, the FDA noted.
The Harmony TPV device is contraindicated for patients with an infection in the heart or elsewhere, for patients who cannot tolerate blood-thinning medicines, and for those with a sensitivity to nitinol (titanium or nickel).
A version of this article first appeared on Medscape.com.
Step therapy: Inside the fight against insurance companies and fail-first medicine
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Encephalopathy common, often lethal in hospitalized patients with COVID-19
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.

Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.

Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.

Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROCRITICAL CARE
STEP 4: Ongoing semaglutide treatment extends weight loss
Weekly injections with the GLP-1 receptor agonist semaglutide helped people maintain, and even increase, their initial weight loss on the agent when they continued treatment beyond 20 weeks in results from an international, multicenter trial with 803 randomized subjects.
The study “reflects what we always see in practice, that when people lose weight their body then fights to regain it. The results underscore this” by showing what happens when people stop the drug, Domenica M. Rubino, MD, reported at the annual meeting of the Endocrine Society.
The STEP 4 study began with 902 obese or higher-risk people with an average body mass index of about 38 kg/m2 who underwent a 20-week, open-label, run-in phase of weekly subcutaneous injections of semaglutide (Ozempic), during which all subjects gradually up-titrated to the study’s maintenance dosage of 2.4 mg/week and allowing investigators to weed out intolerant, noncompliant, or nonresponsive people. After this phase excluded 99 subjects from continuing, and documented that the remaining 803 patients had already lost an average of 11% of their starting weight, the core of the study kicked in by randomizing them 2:1 to either maintain their weekly semaglutide injections for another 48 weeks or change to placebo injections.
After 48 more weeks, the 535 people who continued active semaglutide treatment lost on average an additional 8% of their weight. Meanwhile, the 268 who switched to placebo gained 7% of the weight they had reached at the 20-week point, for a significant between-group weight-loss difference of about 15% for the study’s primary endpoint. Those maintained on semaglutide for the full 68 weeks had a cumulative average weight loss of about 17%, compared with when they first began treatment, Dr. Rubino said. Concurrently with her report, the results also appeared in an article published online in JAMA.
“It’s reassuring that people who remain on this treatment can sustain weight losses of 15%, and in some cases 20% or more. That’s huge,” Dr. Rubino said in an interview. . After 68 weeks, 40% of the people who maintained their semaglutide treatment had lost at least 20% of their weight, compared with when they first started treatment.
“Preventing weight regain following initial weight loss is a well-known major challenge for people who lose weight,” commented John Clark III, MD, PhD, a weight management specialist at the University of Texas Southwestern Medical Center in Dallas who was not involved with the study. The findings from STEP 4 will be “helpful to have a discussion [with weight-loss patients] about the risks and benefits of continuing to take this medication longer than just a few months and if they want to continue taking the medication after they reach their goal weight,” Dr. Clark noted in an interview. “This new information reinforces that treatment continues to be effective after the short term.”
“This is obesity 101. If a treatment is provided that targets mechanisms of obesity, and then the treatment stops, we should not be surprised that weight regain occurs,” commented Ania M. Jastreboff, MD, PhD, codirector of the Yale Center for Weight Management in New Haven, Conn. “It’s tragic to see patients who, after successful weight loss, suffer regain because the treatment by which they lost weight stopped,” she said in an interview.
The STEP 4 study ran at 73 centers in 10 countries during 2018-2020. It enrolled adults without diabetes and with a BMI of at least 30, or at least 27 if they also had at least one weight-related comorbidity such as hypertension, dyslipidemia, or obstructive sleep apnea. Participants averaged about 47 years of age, almost 80% were women, and about 84% were White, including 8% of Hispanic or Latinx ethnicity.
The adverse-event profile was consistent with findings from trials where semaglutide treated hyperglycemia in patients with type 2 diabetes (semaglutide at a maximum once-weekly dosage of 1 mg has Food and Drug Administration approval for controlling hyperglycemia in patients with type 2 diabetes), as well results from other semaglutide studies and from studies of other agents in the GLP-1 receptor agonist class.
In STEP 4 9% of patients who received semaglutide during the randomized phase and 7% of those randomized to placebo had a serious adverse reaction, and about 2% of those in both treatment arms stopped treatment because of an adverse event. The most common adverse events on semaglutide were gastrointestinal, with diarrhea in 14%, nausea in 14%, constipation in 12%, and vomiting in 10%.
These GI effects are often mitigated by slower dose escalation, eating smaller amounts of food at a time, and not eating beyond the point of feeling full, noted Dr. Jastreboff.
The STEP 4 results follow prior reports from three other large trials – STEP 1, STEP 2, and STEP 3 – that studied the weight-loss effects of weekly semaglutide treatment in adults using varying enrollment criteria and treatment designs. “We’ve seen very consistent results [across all four studies] for efficacy and safety,” said Dr. Rubino, who owns and directs the Washington Center for Weight Management & Research in Arlington, Va.
NovoNordisk, the company that markets semaglutide, submitted data from all four studies to the FDA late last year in an application for a new label for a weight loss indication at the 2.4-mg/week dosage. The company has said it expects an agency decision by June 2021.
Dr. Rubino has been an adviser and consultant to and a speaker on behalf of Novo Nordisk, and she has also been an investigator for studies sponsored by AstraZeneca, Boehringer Ingelheim, and Novo Nordisk. Dr. Clark had no disclosures. Dr. Jastreboff is consultant for and has received research funding from NovoNordisk, and she has also been a consultant to and/or received research from Eli Lilly and Boehringer Ingelheim.
Weekly injections with the GLP-1 receptor agonist semaglutide helped people maintain, and even increase, their initial weight loss on the agent when they continued treatment beyond 20 weeks in results from an international, multicenter trial with 803 randomized subjects.
The study “reflects what we always see in practice, that when people lose weight their body then fights to regain it. The results underscore this” by showing what happens when people stop the drug, Domenica M. Rubino, MD, reported at the annual meeting of the Endocrine Society.
The STEP 4 study began with 902 obese or higher-risk people with an average body mass index of about 38 kg/m2 who underwent a 20-week, open-label, run-in phase of weekly subcutaneous injections of semaglutide (Ozempic), during which all subjects gradually up-titrated to the study’s maintenance dosage of 2.4 mg/week and allowing investigators to weed out intolerant, noncompliant, or nonresponsive people. After this phase excluded 99 subjects from continuing, and documented that the remaining 803 patients had already lost an average of 11% of their starting weight, the core of the study kicked in by randomizing them 2:1 to either maintain their weekly semaglutide injections for another 48 weeks or change to placebo injections.
After 48 more weeks, the 535 people who continued active semaglutide treatment lost on average an additional 8% of their weight. Meanwhile, the 268 who switched to placebo gained 7% of the weight they had reached at the 20-week point, for a significant between-group weight-loss difference of about 15% for the study’s primary endpoint. Those maintained on semaglutide for the full 68 weeks had a cumulative average weight loss of about 17%, compared with when they first began treatment, Dr. Rubino said. Concurrently with her report, the results also appeared in an article published online in JAMA.
“It’s reassuring that people who remain on this treatment can sustain weight losses of 15%, and in some cases 20% or more. That’s huge,” Dr. Rubino said in an interview. . After 68 weeks, 40% of the people who maintained their semaglutide treatment had lost at least 20% of their weight, compared with when they first started treatment.
“Preventing weight regain following initial weight loss is a well-known major challenge for people who lose weight,” commented John Clark III, MD, PhD, a weight management specialist at the University of Texas Southwestern Medical Center in Dallas who was not involved with the study. The findings from STEP 4 will be “helpful to have a discussion [with weight-loss patients] about the risks and benefits of continuing to take this medication longer than just a few months and if they want to continue taking the medication after they reach their goal weight,” Dr. Clark noted in an interview. “This new information reinforces that treatment continues to be effective after the short term.”
“This is obesity 101. If a treatment is provided that targets mechanisms of obesity, and then the treatment stops, we should not be surprised that weight regain occurs,” commented Ania M. Jastreboff, MD, PhD, codirector of the Yale Center for Weight Management in New Haven, Conn. “It’s tragic to see patients who, after successful weight loss, suffer regain because the treatment by which they lost weight stopped,” she said in an interview.
The STEP 4 study ran at 73 centers in 10 countries during 2018-2020. It enrolled adults without diabetes and with a BMI of at least 30, or at least 27 if they also had at least one weight-related comorbidity such as hypertension, dyslipidemia, or obstructive sleep apnea. Participants averaged about 47 years of age, almost 80% were women, and about 84% were White, including 8% of Hispanic or Latinx ethnicity.
The adverse-event profile was consistent with findings from trials where semaglutide treated hyperglycemia in patients with type 2 diabetes (semaglutide at a maximum once-weekly dosage of 1 mg has Food and Drug Administration approval for controlling hyperglycemia in patients with type 2 diabetes), as well results from other semaglutide studies and from studies of other agents in the GLP-1 receptor agonist class.
In STEP 4 9% of patients who received semaglutide during the randomized phase and 7% of those randomized to placebo had a serious adverse reaction, and about 2% of those in both treatment arms stopped treatment because of an adverse event. The most common adverse events on semaglutide were gastrointestinal, with diarrhea in 14%, nausea in 14%, constipation in 12%, and vomiting in 10%.
These GI effects are often mitigated by slower dose escalation, eating smaller amounts of food at a time, and not eating beyond the point of feeling full, noted Dr. Jastreboff.
The STEP 4 results follow prior reports from three other large trials – STEP 1, STEP 2, and STEP 3 – that studied the weight-loss effects of weekly semaglutide treatment in adults using varying enrollment criteria and treatment designs. “We’ve seen very consistent results [across all four studies] for efficacy and safety,” said Dr. Rubino, who owns and directs the Washington Center for Weight Management & Research in Arlington, Va.
NovoNordisk, the company that markets semaglutide, submitted data from all four studies to the FDA late last year in an application for a new label for a weight loss indication at the 2.4-mg/week dosage. The company has said it expects an agency decision by June 2021.
Dr. Rubino has been an adviser and consultant to and a speaker on behalf of Novo Nordisk, and she has also been an investigator for studies sponsored by AstraZeneca, Boehringer Ingelheim, and Novo Nordisk. Dr. Clark had no disclosures. Dr. Jastreboff is consultant for and has received research funding from NovoNordisk, and she has also been a consultant to and/or received research from Eli Lilly and Boehringer Ingelheim.
Weekly injections with the GLP-1 receptor agonist semaglutide helped people maintain, and even increase, their initial weight loss on the agent when they continued treatment beyond 20 weeks in results from an international, multicenter trial with 803 randomized subjects.
The study “reflects what we always see in practice, that when people lose weight their body then fights to regain it. The results underscore this” by showing what happens when people stop the drug, Domenica M. Rubino, MD, reported at the annual meeting of the Endocrine Society.
The STEP 4 study began with 902 obese or higher-risk people with an average body mass index of about 38 kg/m2 who underwent a 20-week, open-label, run-in phase of weekly subcutaneous injections of semaglutide (Ozempic), during which all subjects gradually up-titrated to the study’s maintenance dosage of 2.4 mg/week and allowing investigators to weed out intolerant, noncompliant, or nonresponsive people. After this phase excluded 99 subjects from continuing, and documented that the remaining 803 patients had already lost an average of 11% of their starting weight, the core of the study kicked in by randomizing them 2:1 to either maintain their weekly semaglutide injections for another 48 weeks or change to placebo injections.
After 48 more weeks, the 535 people who continued active semaglutide treatment lost on average an additional 8% of their weight. Meanwhile, the 268 who switched to placebo gained 7% of the weight they had reached at the 20-week point, for a significant between-group weight-loss difference of about 15% for the study’s primary endpoint. Those maintained on semaglutide for the full 68 weeks had a cumulative average weight loss of about 17%, compared with when they first began treatment, Dr. Rubino said. Concurrently with her report, the results also appeared in an article published online in JAMA.
“It’s reassuring that people who remain on this treatment can sustain weight losses of 15%, and in some cases 20% or more. That’s huge,” Dr. Rubino said in an interview. . After 68 weeks, 40% of the people who maintained their semaglutide treatment had lost at least 20% of their weight, compared with when they first started treatment.
“Preventing weight regain following initial weight loss is a well-known major challenge for people who lose weight,” commented John Clark III, MD, PhD, a weight management specialist at the University of Texas Southwestern Medical Center in Dallas who was not involved with the study. The findings from STEP 4 will be “helpful to have a discussion [with weight-loss patients] about the risks and benefits of continuing to take this medication longer than just a few months and if they want to continue taking the medication after they reach their goal weight,” Dr. Clark noted in an interview. “This new information reinforces that treatment continues to be effective after the short term.”
“This is obesity 101. If a treatment is provided that targets mechanisms of obesity, and then the treatment stops, we should not be surprised that weight regain occurs,” commented Ania M. Jastreboff, MD, PhD, codirector of the Yale Center for Weight Management in New Haven, Conn. “It’s tragic to see patients who, after successful weight loss, suffer regain because the treatment by which they lost weight stopped,” she said in an interview.
The STEP 4 study ran at 73 centers in 10 countries during 2018-2020. It enrolled adults without diabetes and with a BMI of at least 30, or at least 27 if they also had at least one weight-related comorbidity such as hypertension, dyslipidemia, or obstructive sleep apnea. Participants averaged about 47 years of age, almost 80% were women, and about 84% were White, including 8% of Hispanic or Latinx ethnicity.
The adverse-event profile was consistent with findings from trials where semaglutide treated hyperglycemia in patients with type 2 diabetes (semaglutide at a maximum once-weekly dosage of 1 mg has Food and Drug Administration approval for controlling hyperglycemia in patients with type 2 diabetes), as well results from other semaglutide studies and from studies of other agents in the GLP-1 receptor agonist class.
In STEP 4 9% of patients who received semaglutide during the randomized phase and 7% of those randomized to placebo had a serious adverse reaction, and about 2% of those in both treatment arms stopped treatment because of an adverse event. The most common adverse events on semaglutide were gastrointestinal, with diarrhea in 14%, nausea in 14%, constipation in 12%, and vomiting in 10%.
These GI effects are often mitigated by slower dose escalation, eating smaller amounts of food at a time, and not eating beyond the point of feeling full, noted Dr. Jastreboff.
The STEP 4 results follow prior reports from three other large trials – STEP 1, STEP 2, and STEP 3 – that studied the weight-loss effects of weekly semaglutide treatment in adults using varying enrollment criteria and treatment designs. “We’ve seen very consistent results [across all four studies] for efficacy and safety,” said Dr. Rubino, who owns and directs the Washington Center for Weight Management & Research in Arlington, Va.
NovoNordisk, the company that markets semaglutide, submitted data from all four studies to the FDA late last year in an application for a new label for a weight loss indication at the 2.4-mg/week dosage. The company has said it expects an agency decision by June 2021.
Dr. Rubino has been an adviser and consultant to and a speaker on behalf of Novo Nordisk, and she has also been an investigator for studies sponsored by AstraZeneca, Boehringer Ingelheim, and Novo Nordisk. Dr. Clark had no disclosures. Dr. Jastreboff is consultant for and has received research funding from NovoNordisk, and she has also been a consultant to and/or received research from Eli Lilly and Boehringer Ingelheim.
FROM ENDO 2021
Arcalyst gets FDA nod as first therapy for recurrent pericarditis
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.