User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Ghost Fat: The Unseen Consequences of Weight Loss
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Why Residents Are Joining Unions in Droves
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Tirzepatide Shortage Resolved? FDA Says Yes, Compounders No
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
Weight Loss After Anti-Obesity Medications Linked to Reduced Gout Risk
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Lifestyle Medicine: Not Just for the Wealthy
Primary care clinicians understand that addressing lifestyle-related chronic disease health disparities in minority and lower-income communities is a significant opportunity to alleviate unnecessary suffering. Disparate health outcomes associated with underlying comorbidities during the COVID pandemic exposed the urgency of this problem.
When it comes to delivering evidence-based therapeutic lifestyle behavior interventions to these populations, however, there is a misconception that lifestyle medicine is only for the wealthy. Such a misconception needlessly widens the gap in health disparities because the truth is that everyone deserves access to lifestyle medicine. Fortunately, there are numerous successful examples of delivering these services to underresourced patients. We can all contribute to narrowing health inequities by sourcing increasingly abundant lifestyle medicine resources.
All patients’ lived experiences are unique, and there is a wide range of potential challenges to achieving lifestyle behavior change. Ignoring these obstacles is a disservice to patients and almost certainly results in treatment failure. Requirements to document SDOH have been a tremendous initial step.
The next step is to have conversations with every patient about the powerful outcomes of even small lifestyle changes. All too often, clinicians forgo conversations on lifestyle change with patients affected by adverse SDOH and assume that social obstacles automatically mean that patients are neither willing nor able to attempt behavior modification. Instead, it is an opportunity for clinicians, particularly those certified in lifestyle medicine, to meet patients where they are, work with them to identify solutions, and provide referrals to community-based organizations with resources to help.
Small Steps to Big Changes
Not all lifestyle behavior interventions need to be programmatic or time intensive. Clinicians can guide patients toward simple but specific actions that can make a difference in health outcomes over time. Small steps, like eating one can of beans or two bags of frozen leafy greens each week, are a good start toward adjusted eating patterns. The American College of Lifestyle Medicine offers a whole-food, plant-predominant meal guide to share with patients.
Individuals can increase their physical activity in their living rooms by doing sit-to-stands or balancing on one leg. Deep breathing and establishing a sleep routine are other lifestyle behavior changes without a price tag.
It is true that early adopters of lifestyle medicine often had difficulty practicing in underresourced communities. Those practitioners were forced to operate on a cash-pay basis, making access to care cost-prohibitive for many patients. However, board certification has been available since 2017, and lifestyle medicine is being integrated into medical schools and residency programs. Many such board-certified clinicians now work in large health systems and bill under the usual methods. There are also frameworks, such as the community-engaged lifestyle medicine model, showing how to treat patients affected by adverse SDOH effectively.
For example, patients at risk for malnutrition because of illnesses like chronic kidney disease, cancer, and heart failure receive medically tailored meals and access to a registered dietitian through a partnership between UC San Diego Health and Mama’s Kitchen. In Pennsylvania’s Lehigh Valley, where 1 in 10 of the approximately 700,000 residents face food insecurity, the Kellyn Foundation delivers fresh food through the Eat Real Food Mobile Market and offers whole-food, plant-predominant cooking classes, interactive elementary school programs focused on healthy lifestyle choices, and therapeutic lifestyle-change programs in community locations. Three months after launching new mobile market sites in Allentown, 1200 households were utilizing $15 weekly food vouchers through the program. Lifestyle medicine clinicians serve inner-city and rural areas in independent practices, large health systems, and community-based practice activities.
To improve access to lifestyle medicine in underresourced communities, more clinicians trained and certified in lifestyle medicine are needed. The Health Equity Achieved through Lifestyle Medicine Initiative supports a diverse lifestyle medicine workforce by offering scholarships to clinicians underrepresented in medicine and is working to train and certify at least one physician within each of the 1400 federally qualified health centers where clinicians are on the front lines of delivering care to the most underserved populations.
A meaningful first step for clinicians to address health disparities is to screen patients for and document SDOH. The American Academy of Family Physicians offers useful tools to screen patients, identify community-based resources, and help patients create action plans to overcome health risks and improve outcomes. In a promising trend to better support addressing SDOH in clinical care, the 2024 Medicare Physician Fee Schedule final rule included new codes to support this effort.
Not every patient will be ready or willing to begin a lifestyle medicine treatment plan. Still, all of them will be grateful for the opportunity to decide for themselves. If we are invested in narrowing health inequities, lifestyle medicine and behavior change must be a topic in clinical encounters with all our patients.
Dr. Collings, director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Primary care clinicians understand that addressing lifestyle-related chronic disease health disparities in minority and lower-income communities is a significant opportunity to alleviate unnecessary suffering. Disparate health outcomes associated with underlying comorbidities during the COVID pandemic exposed the urgency of this problem.
When it comes to delivering evidence-based therapeutic lifestyle behavior interventions to these populations, however, there is a misconception that lifestyle medicine is only for the wealthy. Such a misconception needlessly widens the gap in health disparities because the truth is that everyone deserves access to lifestyle medicine. Fortunately, there are numerous successful examples of delivering these services to underresourced patients. We can all contribute to narrowing health inequities by sourcing increasingly abundant lifestyle medicine resources.
All patients’ lived experiences are unique, and there is a wide range of potential challenges to achieving lifestyle behavior change. Ignoring these obstacles is a disservice to patients and almost certainly results in treatment failure. Requirements to document SDOH have been a tremendous initial step.
The next step is to have conversations with every patient about the powerful outcomes of even small lifestyle changes. All too often, clinicians forgo conversations on lifestyle change with patients affected by adverse SDOH and assume that social obstacles automatically mean that patients are neither willing nor able to attempt behavior modification. Instead, it is an opportunity for clinicians, particularly those certified in lifestyle medicine, to meet patients where they are, work with them to identify solutions, and provide referrals to community-based organizations with resources to help.
Small Steps to Big Changes
Not all lifestyle behavior interventions need to be programmatic or time intensive. Clinicians can guide patients toward simple but specific actions that can make a difference in health outcomes over time. Small steps, like eating one can of beans or two bags of frozen leafy greens each week, are a good start toward adjusted eating patterns. The American College of Lifestyle Medicine offers a whole-food, plant-predominant meal guide to share with patients.
Individuals can increase their physical activity in their living rooms by doing sit-to-stands or balancing on one leg. Deep breathing and establishing a sleep routine are other lifestyle behavior changes without a price tag.
It is true that early adopters of lifestyle medicine often had difficulty practicing in underresourced communities. Those practitioners were forced to operate on a cash-pay basis, making access to care cost-prohibitive for many patients. However, board certification has been available since 2017, and lifestyle medicine is being integrated into medical schools and residency programs. Many such board-certified clinicians now work in large health systems and bill under the usual methods. There are also frameworks, such as the community-engaged lifestyle medicine model, showing how to treat patients affected by adverse SDOH effectively.
For example, patients at risk for malnutrition because of illnesses like chronic kidney disease, cancer, and heart failure receive medically tailored meals and access to a registered dietitian through a partnership between UC San Diego Health and Mama’s Kitchen. In Pennsylvania’s Lehigh Valley, where 1 in 10 of the approximately 700,000 residents face food insecurity, the Kellyn Foundation delivers fresh food through the Eat Real Food Mobile Market and offers whole-food, plant-predominant cooking classes, interactive elementary school programs focused on healthy lifestyle choices, and therapeutic lifestyle-change programs in community locations. Three months after launching new mobile market sites in Allentown, 1200 households were utilizing $15 weekly food vouchers through the program. Lifestyle medicine clinicians serve inner-city and rural areas in independent practices, large health systems, and community-based practice activities.
To improve access to lifestyle medicine in underresourced communities, more clinicians trained and certified in lifestyle medicine are needed. The Health Equity Achieved through Lifestyle Medicine Initiative supports a diverse lifestyle medicine workforce by offering scholarships to clinicians underrepresented in medicine and is working to train and certify at least one physician within each of the 1400 federally qualified health centers where clinicians are on the front lines of delivering care to the most underserved populations.
A meaningful first step for clinicians to address health disparities is to screen patients for and document SDOH. The American Academy of Family Physicians offers useful tools to screen patients, identify community-based resources, and help patients create action plans to overcome health risks and improve outcomes. In a promising trend to better support addressing SDOH in clinical care, the 2024 Medicare Physician Fee Schedule final rule included new codes to support this effort.
Not every patient will be ready or willing to begin a lifestyle medicine treatment plan. Still, all of them will be grateful for the opportunity to decide for themselves. If we are invested in narrowing health inequities, lifestyle medicine and behavior change must be a topic in clinical encounters with all our patients.
Dr. Collings, director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Primary care clinicians understand that addressing lifestyle-related chronic disease health disparities in minority and lower-income communities is a significant opportunity to alleviate unnecessary suffering. Disparate health outcomes associated with underlying comorbidities during the COVID pandemic exposed the urgency of this problem.
When it comes to delivering evidence-based therapeutic lifestyle behavior interventions to these populations, however, there is a misconception that lifestyle medicine is only for the wealthy. Such a misconception needlessly widens the gap in health disparities because the truth is that everyone deserves access to lifestyle medicine. Fortunately, there are numerous successful examples of delivering these services to underresourced patients. We can all contribute to narrowing health inequities by sourcing increasingly abundant lifestyle medicine resources.
All patients’ lived experiences are unique, and there is a wide range of potential challenges to achieving lifestyle behavior change. Ignoring these obstacles is a disservice to patients and almost certainly results in treatment failure. Requirements to document SDOH have been a tremendous initial step.
The next step is to have conversations with every patient about the powerful outcomes of even small lifestyle changes. All too often, clinicians forgo conversations on lifestyle change with patients affected by adverse SDOH and assume that social obstacles automatically mean that patients are neither willing nor able to attempt behavior modification. Instead, it is an opportunity for clinicians, particularly those certified in lifestyle medicine, to meet patients where they are, work with them to identify solutions, and provide referrals to community-based organizations with resources to help.
Small Steps to Big Changes
Not all lifestyle behavior interventions need to be programmatic or time intensive. Clinicians can guide patients toward simple but specific actions that can make a difference in health outcomes over time. Small steps, like eating one can of beans or two bags of frozen leafy greens each week, are a good start toward adjusted eating patterns. The American College of Lifestyle Medicine offers a whole-food, plant-predominant meal guide to share with patients.
Individuals can increase their physical activity in their living rooms by doing sit-to-stands or balancing on one leg. Deep breathing and establishing a sleep routine are other lifestyle behavior changes without a price tag.
It is true that early adopters of lifestyle medicine often had difficulty practicing in underresourced communities. Those practitioners were forced to operate on a cash-pay basis, making access to care cost-prohibitive for many patients. However, board certification has been available since 2017, and lifestyle medicine is being integrated into medical schools and residency programs. Many such board-certified clinicians now work in large health systems and bill under the usual methods. There are also frameworks, such as the community-engaged lifestyle medicine model, showing how to treat patients affected by adverse SDOH effectively.
For example, patients at risk for malnutrition because of illnesses like chronic kidney disease, cancer, and heart failure receive medically tailored meals and access to a registered dietitian through a partnership between UC San Diego Health and Mama’s Kitchen. In Pennsylvania’s Lehigh Valley, where 1 in 10 of the approximately 700,000 residents face food insecurity, the Kellyn Foundation delivers fresh food through the Eat Real Food Mobile Market and offers whole-food, plant-predominant cooking classes, interactive elementary school programs focused on healthy lifestyle choices, and therapeutic lifestyle-change programs in community locations. Three months after launching new mobile market sites in Allentown, 1200 households were utilizing $15 weekly food vouchers through the program. Lifestyle medicine clinicians serve inner-city and rural areas in independent practices, large health systems, and community-based practice activities.
To improve access to lifestyle medicine in underresourced communities, more clinicians trained and certified in lifestyle medicine are needed. The Health Equity Achieved through Lifestyle Medicine Initiative supports a diverse lifestyle medicine workforce by offering scholarships to clinicians underrepresented in medicine and is working to train and certify at least one physician within each of the 1400 federally qualified health centers where clinicians are on the front lines of delivering care to the most underserved populations.
A meaningful first step for clinicians to address health disparities is to screen patients for and document SDOH. The American Academy of Family Physicians offers useful tools to screen patients, identify community-based resources, and help patients create action plans to overcome health risks and improve outcomes. In a promising trend to better support addressing SDOH in clinical care, the 2024 Medicare Physician Fee Schedule final rule included new codes to support this effort.
Not every patient will be ready or willing to begin a lifestyle medicine treatment plan. Still, all of them will be grateful for the opportunity to decide for themselves. If we are invested in narrowing health inequities, lifestyle medicine and behavior change must be a topic in clinical encounters with all our patients.
Dr. Collings, director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Time-Restricted Eating Is Not a Metabolic Magic Bullet
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.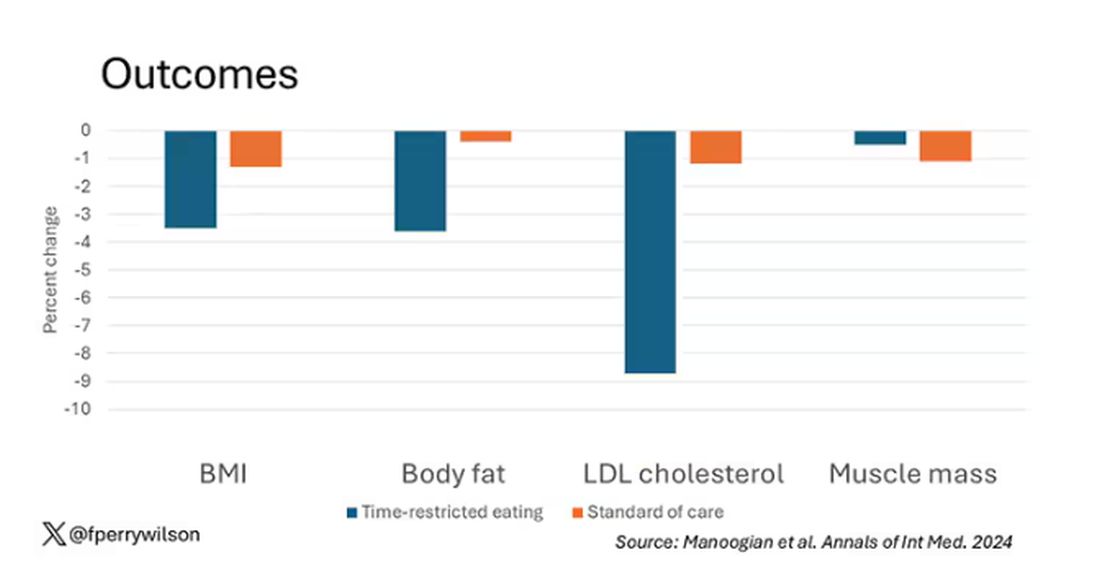
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.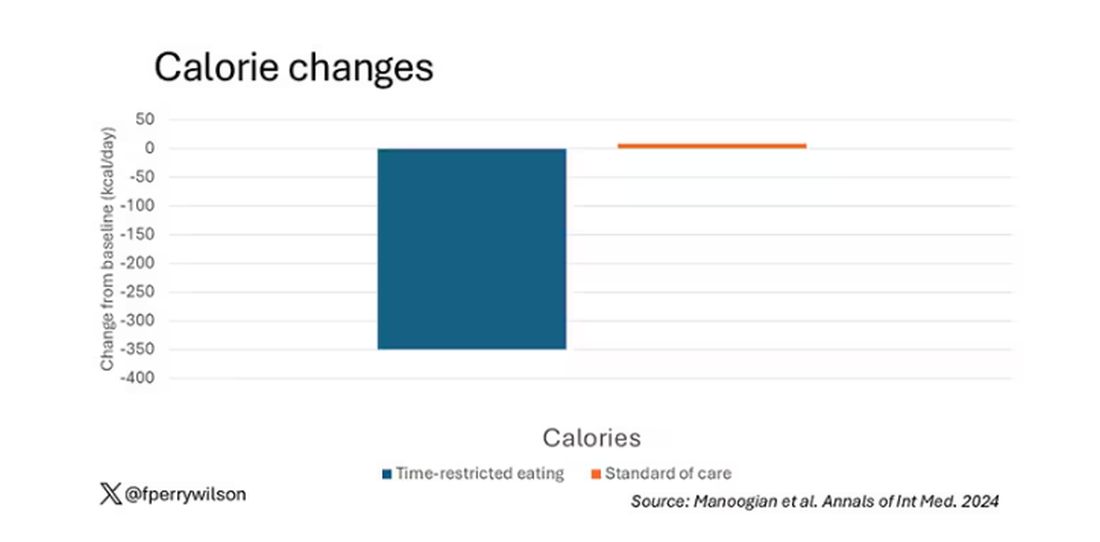
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 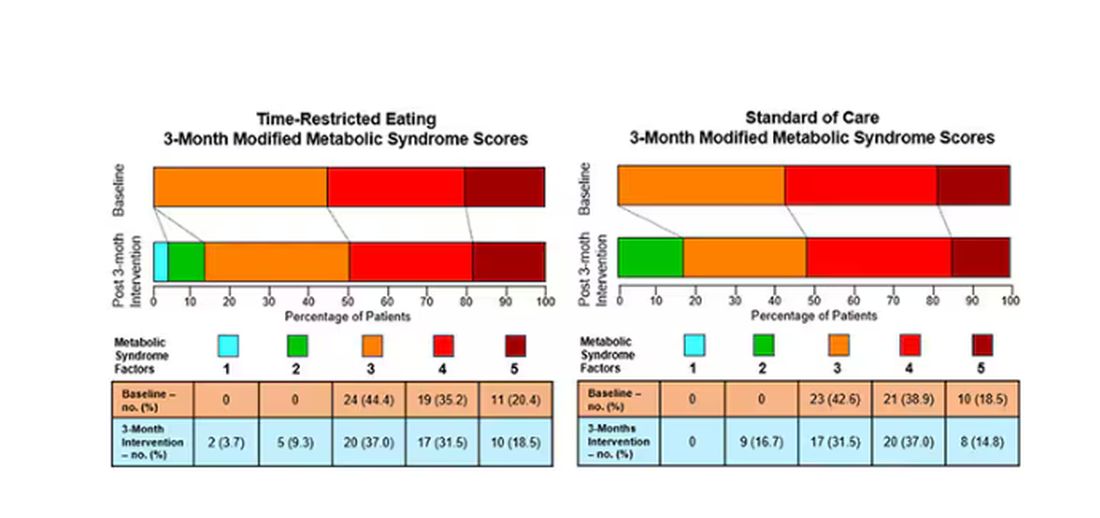
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.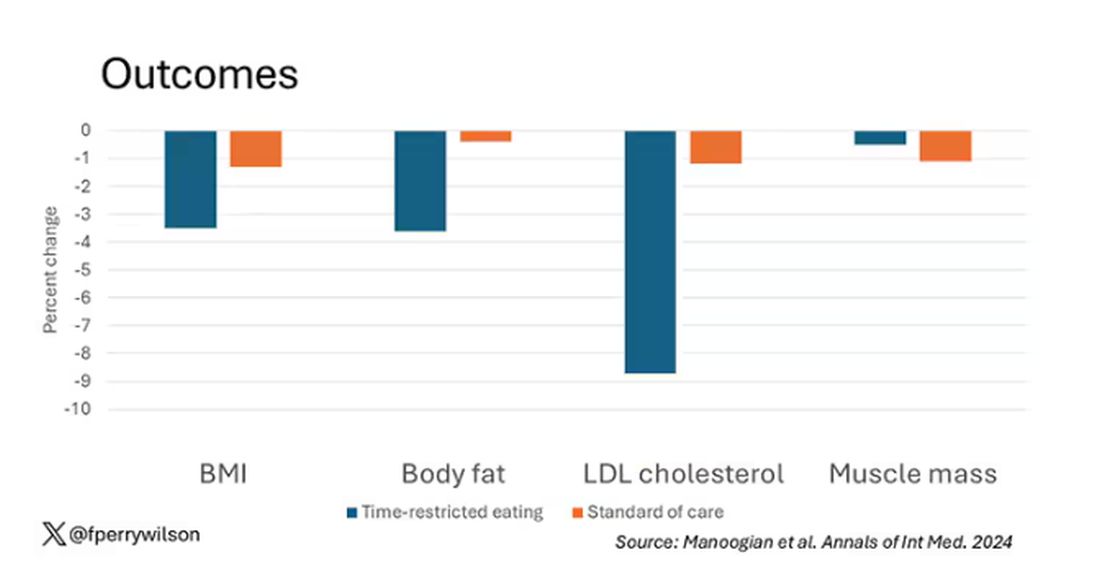
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.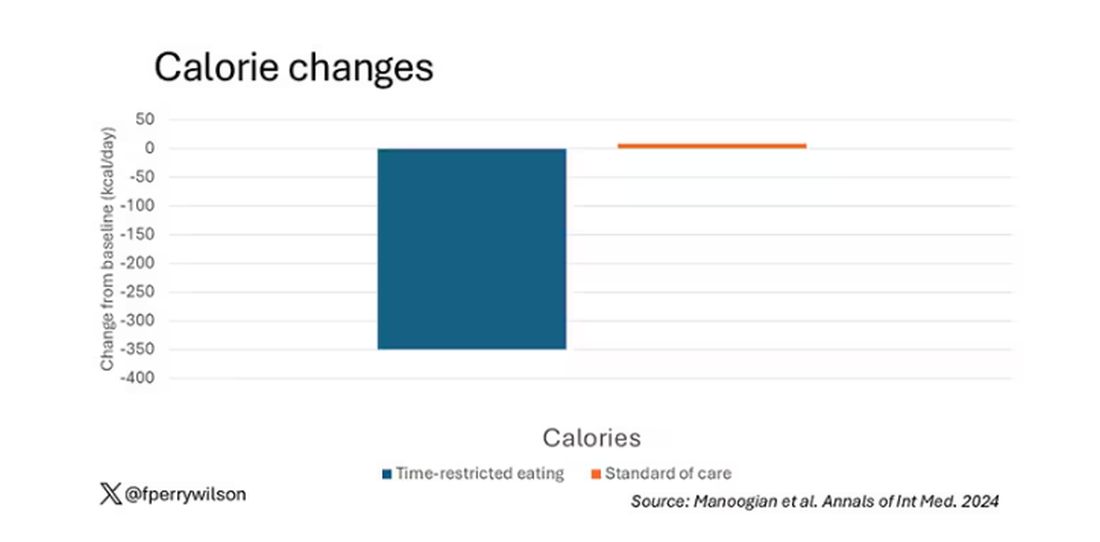
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 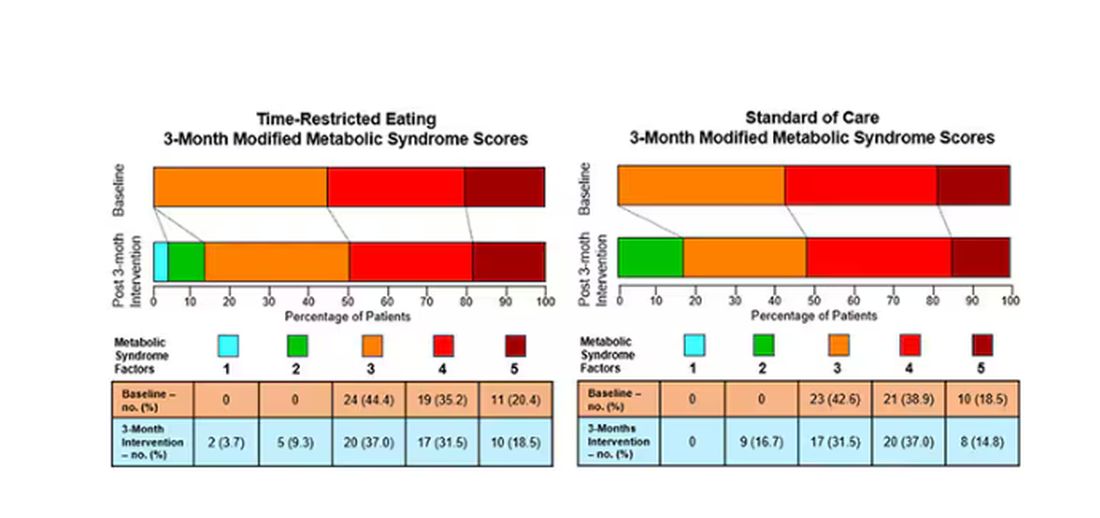
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.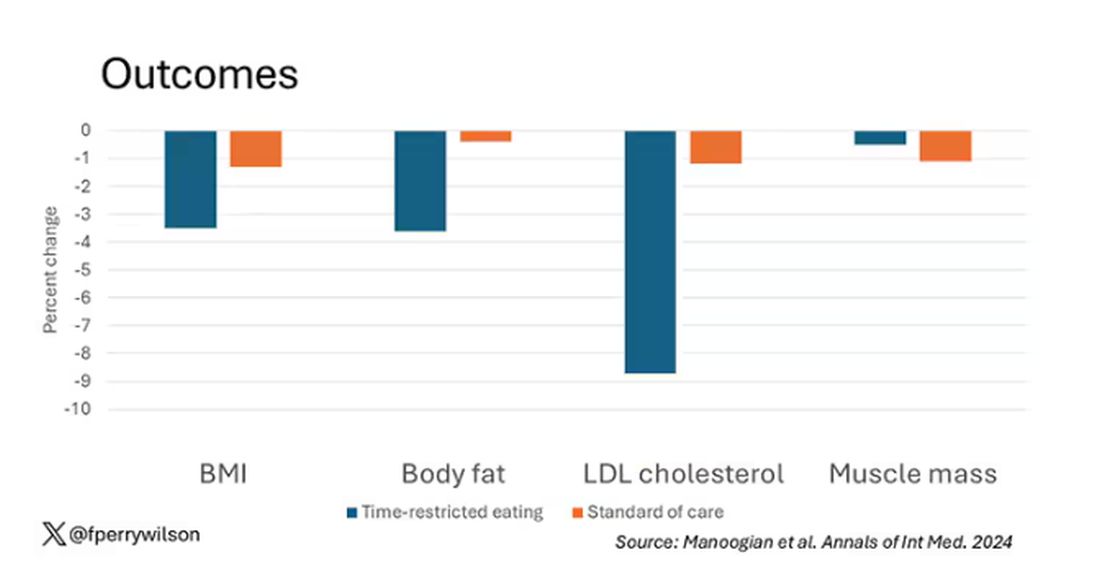
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.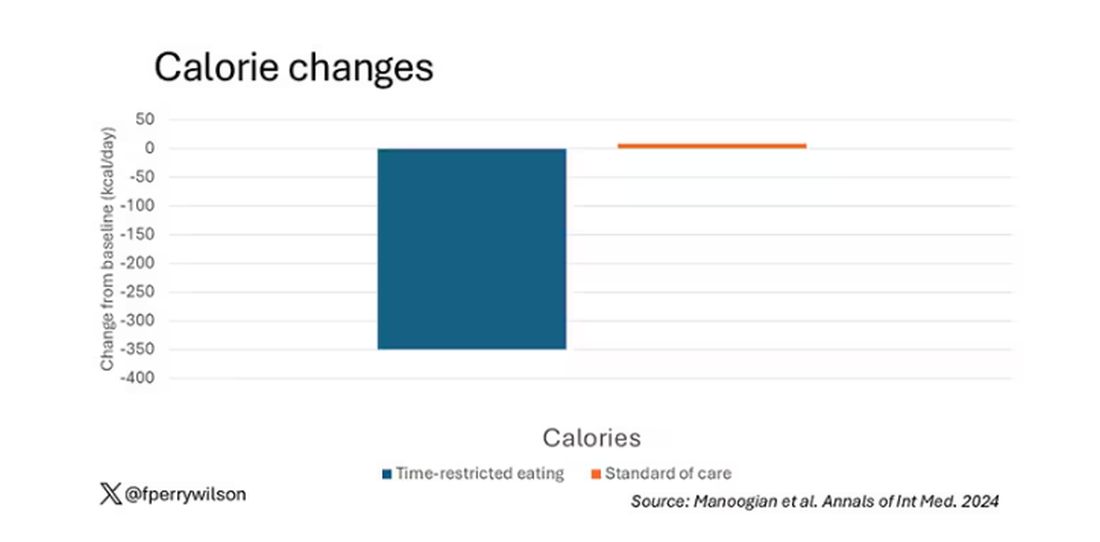
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 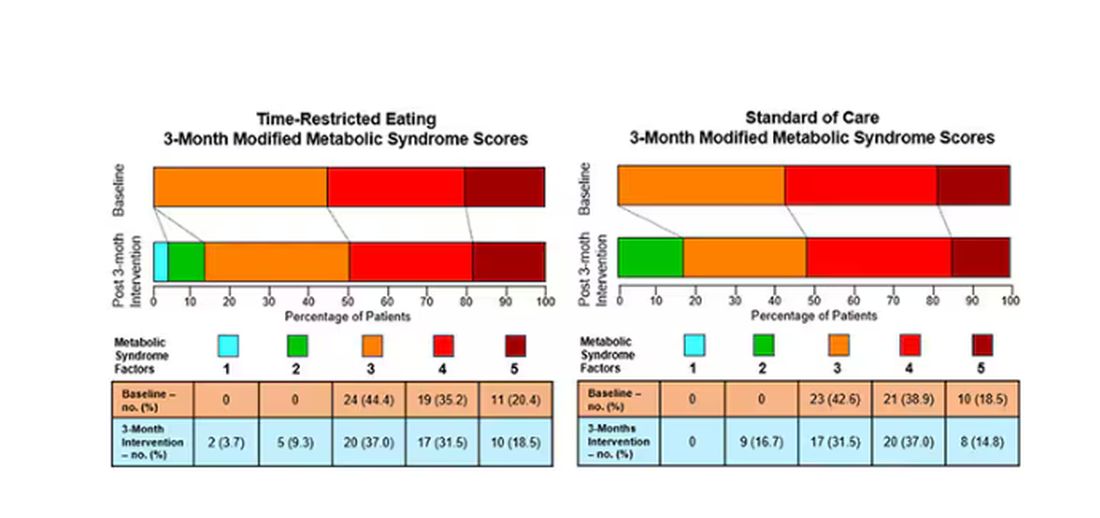
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Detecting Type 2 Diabetes Through Voice: How Does It Work?
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
An international study, Colive Voice, presented at the European Association for the Study of Diabetes (EASD) 2024 conference, shows that These results “open up possibilities for developing a first-line, noninvasive, and rapid screening tool for T2D, feasible with just a few seconds of voice recording on a smartphone or during consultations,” explained the study’s principal investigator Guy Fagherazzi, PhD, a diabetes epidemiologist at the Luxembourg Institute of Health, in an interview with this news organization.
How did the idea of detecting diabetes through voice come about?
During the COVID-19 pandemic, we began analyzing voice recordings from patients with chronic diseases. We wanted to find solutions to assess people’s health remotely, without physical contact. We quickly realized that this approach could be extended to other diseases. Because my main research focus has always been diabetes, I looked into how voice characteristics might correlate with diabetes. Previous studies had indicated that patients with diabetes have distinct voices compared with the general population, and this insight formed the starting point.
What mechanism could explain why patients with T2D have different voice characteristics?
It’s challenging to pinpoint a single factor that would explain why patients with T2D have different voices from those without diabetes. Several factors are involved.
Some biological mechanisms, especially those affecting the vascular system, influence symptoms in people with metabolic diseases such as diabetes. For example, people with T2D have more frequent cardiorespiratory fatigue. Obesity and overweight are also key factors, as these conditions can slightly alter vocal parameters compared with people of normal weight. Hypertension, common in patients with T2D, adds to the complexity.
Neurologic complications can affect the nerves and muscles involved in voice production, particularly the vocal cords.
Therefore, respiratory fatigue, neuropathies, and other conditions such as dehydration and gastric acid reflux, which are more common in patients with diabetes, can contribute to differences in voice.
These differences might not be noticeable to the human ear. That’s why we often don’t notice the link between voice and diabetes. However, technological advancements in signal processing and artificial intelligence allow us to extract a large amount of information from these subtle variations. By analyzing these small differences, we can detect diabetes with a reasonable degree of accuracy.
In your study, you mention that voice tone can indicate diabetic status. Could you elaborate?
Yes, voice tone can be affected, though it’s a complex, multidimensional phenomenon.
Patients who have had diabetes for 5-10 years, or longer, tend to have a rougher voice than those without diabetes of the same age and gender. In our study, we were able to extract many voice characteristics from the raw audio signal, which is why it’s difficult to isolate one specific factor that stands out.
Is there a difference in voice changes between patients with well-managed diabetes and those whose disease is uncontrolled?
The roughness of the voice tends to increase with the duration of diabetes. It’s more noticeable in people with poorly controlled diabetes. Our hypothesis, based on the results we presented at the EASD conference, is that fluctuations in blood sugar levels, both hypo- and hyperglycemia, may cause short-term changes in the voice. There are also many subtle, rapid changes that could potentially be detected, though we haven’t confirmed this yet. We’re currently conducting additional studies to explore this.
Why did you ask participants to read a passage from the Universal Declaration of Human Rights?
We used a highly standardized approach. Participants completed several recordings, including holding the sound “Aaaaaa” for as long as possible in one breath. They also read a passage, which helps us better distinguish between patients with and those without diabetes. This method works slightly better than other sounds typically used for analyzing diseases. We chose this particular text in the participant’s native language because it’s neutral and doesn’t trigger emotional fluctuations. Because Colive Voice is an international, multilingual study, we use official translations in various languages.
Your research focuses on T2D. Do you plan to study type 1 diabetes (T1D) as well?
We believe that individuals with T1D also exhibit voice changes over time. However, our current focus is on T2D because our goal is to develop large-scale screening methods. T1D, typically diagnosed in childhood, requires different screening approaches. For now, our research mainly involves adults.
Were there any gender differences in the accuracy of your voice analysis?
Yes, voice studies generally show that women have different vocal signatures from men, partly owing to hormonal fluctuations that affect pitch and tone. Detecting differences between healthy individuals and those with diabetes can sometimes be more challenging in women, depending on the condition. In our study, we achieved about 70% accuracy for women compared with 75% for men.
The EASD results focused on a US-based population. When can we expect data from France?
We started with the US because we could quickly gather a large number of patients. Now, we’re expanding to global and language-specific analyses. French data are certainly a priority, and we’re working on it. We encourage people to participate — it takes only 20 minutes and contributes to innovative research on noninvasive diabetes detection. Participants can sign up at www.colivevoice.org
Dr. Fagherazzi heads the Deep Digital Phenotyping laboratory and the Department of Precision Health at the Luxembourg Institute of Health. His research focuses on integrating new technologies and digital data into diabetes research. He has declared no relevant financial relationships.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
FROM EASD 2024
Cannabis Use Rising in Diabetes: What Do Endos Need to Know?
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
A recent US prevalence study estimated that 9% adults with diabetes used cannabis in the last month, a 33.7% increase between 2021 and 2022. Nearly half (48.9%) of users were younger than 50 years.
Cannabis use is also increasing sharply among those aged 65 years or older, many of whom have diabetes and other chronic conditions. In this demographic, the perceived risk surrounding regular cannabis use has dropped significantly, even as the data tell another story — that they are particularly at risk from emergency department visits for cannabis poisoning.
As legalization continues and cannabis products proliferate, endocrinologists will likely face more patients of all ages seeking advice about its use. Yet with few evidence-based resources to turn to, endocrinologists advising patients in this area are mostly left fending for themselves.
Evidence ‘Limited’
“The evidence on cannabis is limited mainly because of its scheduling in the United States,” Jay Shubrook, DO, a professor and diabetologist at College of Osteopathic Medicine, Touro University California, in Vallejo, California, told this news organization.
“It was declared to be a schedule I drug in the 1970s, which meant it was ‘dangerous’ and ‘had no medical benefit.’ This made it hard to access and study in human trials.”
That will likely change soon. On May 16, 2024, the US Department of Justice submitted a proposal to move marijuana from a schedule I to a schedule III drug under the Controlled Substances Act, emphasizing its accepted medical use. If approved, the door will open to more investigators seeking to study the effects of cannabis.
Yet, even in Canada, where recreational use has been legal since 2018 and cannabis is sold widely with government support, there are little hard data to guide practice. In 2019, Diabetes Canada issued a position statement on recreational cannabis use in people with type 1 diabetes (T1D) and type 2 diabetes (T2D). It sought to evaluate the effects of cannabis on metabolic factors and diabetes complications, as well as self-management behaviors in those aged 13 years or older.
The authors noted that five of the six studies upon which the statement was based did not consider or report the routes of cannabis administration, which have differing risks. In addition, their recommendations were based on grade D evidence and consensus.
What Patients Are Taking
Cannabis — also known as marijuana, weed, pot, or bud — refers to the dried flowers, leaves, stems, and seeds of the cannabis plant. The plant contains more than 100 compounds, including tetrahydrocannabinol (THC), which is responsible for the euphoric “high,” and other active compounds, including cannabidiol (CBD), which by itself is not mind-altering.
Cannabis can be ingested in several ways. It can be smoked (ie, joints, blunts, pipes, and water pipes), ingested in edible form (mixed or infused into foods), and inhaled using electronic vaporizing devices (ie, e-cigarettes or vape pens).
Compounds in cannabis can also be extracted to make oils and concentrates that can be vaped or inhaled. Smoking oils, concentrates, and extracts from the cannabis plant, known as “dabbing,” are on the rise in the United States.
There are no validated or standard dosage recommendations for cannabis strains and formulations, THC/CBD ratios, or modes of administration. Therefore, the Canadian Pharmacists Association prepared a guide for finding a safe and effective dose for medical purposes. GoodRx, a website with information on prescription drug prices, says that larger doses of THC pose greater risks, noting that the potency of cannabis has increased from 4% in 1995 to about 14% in 2019.
Potential Risks and Benefits: Canadian and US Perspectives
Health and safety risks vary with each of the different ways of using cannabis for individuals with and without diabetes, depending on a host of patient- and product-specific factors.
In a recent article proposing a “THC unit” for Canada’s legal cannabis market, researchers reported that consumers lack familiarity with THC levels, don’t know what constitutes a “low” or “high” THC amount, have trouble dosing, overconsume, and commonly experience adverse health events from cannabis use.
A recent study suggested that most clinicians are similarly uninformed, with “a lack of knowledge of beneficial effects, adverse effects, and of how to advise patients,” even for medical cannabis.
Diabetes Canada takes a stab at summarizing what’s known with respect to cannabis and diabetes, stating that:
“Research on recreational cannabis use suggests it may negatively impact diabetes metabolic factors and self-management behaviors. The safety of recreational cannabis use has not been demonstrated, whereas regular cannabis use is associated with worsening glycemic control, more diabetes-related complications, and poorer self-care behaviors, such as adequate glucose monitoring, adherence to medications, and compliance with dietary and physical activity recommendations for people living with both type 1 and type 2 diabetes.”
The American Diabetes Association’s information on cannabis consists of a patient-oriented article on CBD oil. The article stated:
“There’s a lot of hype surrounding CBD oil and diabetes. There is no noticeable effect on blood glucose (blood sugar) or insulin levels in people with type 2 diabetes. Researchers continue to study the effects of CBD on diabetes in animal studies.”
It concludes that:
“Although many claims continue to be made about CBD oil, there is little evidence of any benefit. It’s certainly not an alternative to traditional diabetes management. The safety of CBD is also unknown — it may have dangerous side effects that we won’t know about unless further research is done.”
A Roundup of Recent Studies
A smattering of recent studies have touched on various aspects of cannabis consumption and diabetes.
Angela Bryan, PhD, professor and co-director of CUChange at the University of Colorado Boulder, has been evaluating cannabis use in young adults (ages 21-40 years) in the SONIC study. Dr. Bryan reported at the American Diabetes Association (ADA) 84th Scientific Sessions that cannabis users were more likely to have a lower body mass index and less likely to develop T2D. Furthermore, chronic cannabis users were less likely to have measures of inflammation and no loss of insulin sensitivity.
Another study by Dr. Bryan’s group found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
Similarly positive results were found in a 15-week, double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD spray for neuropathic pain among treatment-resistant patients. The investigators reported that “clinically important improvements” were seen in pain, sleep quality, and subjective impressions of pain. Another small study of inhaled cannabis in treatment-refractory patients found a dose-dependent reduction in diabetic peripheral neuropathy pain.
Findings from a 9-year longitudinal study of approximately 18,000 Swedish men and women suggested no association between cannabis and subsequent T2D development after controlling for age, although these authors also called for longer follow-up and more detailed information about cannabis use to make “more robust” conclusions.
On the other side of the spectrum, a “rapid” review of recreational cannabis use in people with T1D and T2D found that recreational cannabis use may negatively impact diabetes metabolic factors and self-management behaviors and may increase risks for peripheral arterial occlusion, myocardial infarction, and renal disease. However, the authors cautioned that more robust research is needed to confirm the potential impact of cannabis on diabetes.
How to Advise Patients
When Dr. Shubrook was working with patients with diabetes in his family medicine practice in Ohio, cannabis wasn’t legal.
“’Don’t ask, don’t tell’ was the way we handled it then,” he said.
By contrast, in California, where he’s currently located, “it’s pretty well accepted and legal, and patients volunteer information about use, even if it’s recreational,” he said. “Realizing this was something we could talk about was really eye-opening to me.”
Talking to patients about cannabis use is a “20-minute conversation that details what they’re doing,” he said. He proceeds by asking questions: Are you using for recreational or medicinal purposes? What do you take? What do you take it for? Does it work?
“People will tell you,” Dr. Shubrook said. “They know exactly what it works or doesn’t work for and how it affects their glucose control, which in most cases is only minimally.”
He tells patients he would prefer they don’t inhale cannabis, given the risks posed to the lungs.
“Edibles may have a slower onset of effect, but depending on what they’re adding it to, glucose might be affected,” he noted. “And I have seen that chronic use can lead to hyperemesis syndrome.”
Overall, he said, “Take the time to talk to your patients about cannabis — it will allow them to be honest with you, and you can improve the specificity and safety of its use. If cannabis is legal in your state, encourage people to go to legal dispensaries, which will reduce the risk of it being laced with another drug that could increase the danger of use.”
A recent US prevalence study found that people with diabetes who use cannabis likely engage in other substance and psychoactive substance use, including tobacco use, binge drinking, and misuse of opioids and stimulants.
“Use of these additional substances could further exacerbate the health risks associated with diabetes and also emphasizes the importance of addressing polysubstance use among adults with diabetes,” the study’s author Benjamin H. Han, MD, Division of Geriatrics, Gerontology and Palliative Care, Department of Medicine, US San Diego School of Medicine in La Jolla, California, told this news organization.
“We were surprised at how strong the associations were, especially with use of substances that can increase cardiovascular risk,” Dr. Han added. “And given the strong association we found between cannabis use and use of other psychoactive substances in diabetes, clinicians must screen all their patients for psychoactive substance use.”
Diabetes Canada’s position paper states that despite the limited evidence, “there were sufficient data to begin developing recommendations for type 1 and type 2 diabetes about education, counseling, and management related to recreational cannabis use.”
Their recommendations include the following:
- Healthcare professionals should engage their patients in discussions about substance use on a regular basis, with a nonjudgmental approach.
- The use of recreational cannabis is not recommended for adolescents and adults with diabetes.
- People with T1D should avoid recreational cannabis use because of the increased risk for diabetic ketoacidosis.
- For adults with T1D or T2D who intend to use cannabis recreationally, individualized assessment and counseling should be offered to inform them of the general risks of cannabis, with a focus on harm reduction and reduction of the risk for potential adverse effects on diabetes management and complications.
- People with T1D or T2D should be offered education on and encouraged to read public information available through resources from various Canadian health authorities about the general risks of cannabis use to reduce the risk for nondiabetes-related adverse effects of cannabis consumption.
Of note, in 2018, the Canadian government produced an exhaustive compendium of information on cannabis for healthcare professionals that includes information relevant to managing patients with diabetes.
Dr. Shubrook and Dr. Han reported no competing interests.
A version of this article appeared on Medscape.com.
Hypothyroidism Treatment Does Not Affect Cognitive Decline in Menopausal Women
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Women with hypothyroidism treated with levothyroxine show no significant cognitive decline across the menopausal transition compared with those without thyroid disease.
METHODOLOGY:
- Levothyroxine, the primary treatment for hypothyroidism, has been linked to perceived cognitive deficits, yet it is unclear whether this is due to the underlying condition being inadequately treated or other factors.
- Using data collected from the Study of Women’s Health Across the Nation, which encompasses five ethnic/racial groups from seven centers across the United States, researchers compared cognitive function over time between women with hypothyroidism treated with levothyroxine and those without thyroid disease.
- Participants underwent cognitive testing across three domains — processing speed, working memory, and episodic memory — which were assessed over a mean follow-up of 13 years.
- Further analyses assessed the impact of abnormal levels of thyroid-stimulating hormone on cognitive outcomes.
TAKEAWAY:
- Of 2033 women included, 227 (mean age, 49.8 years) had levothyroxine-treated hypothyroidism and 1806 (mean age, 50.0 years) did not have thyroid disease; the proportion of women with premenopausal or early perimenopausal status at baseline was higher in the hypothyroidism group (54.2% vs 49.8%; P = .010).
- At baseline, levothyroxine-treated women had higher scores for processing speed (mean score, 56.5 vs 54.4; P = .006) and working memory (mean score, 6.8 vs 6.4; P = .018) than those without thyroid disease; however, no difference in episodic memory was observed between the groups.
- Over the study period, there was no significant difference in cognitive decline between the groups.
- There was no significant effect of levothyroxine-treated hypothyroidism on working memory or episodic memory, although an annual decline in processing speed was observed (P < .001).
- Sensitivity analyses determined that abnormal levels of thyroid-stimulating hormone did not affect cognitive outcomes in women with hypothyroidism.
IN PRACTICE:
When cognitive decline is observed in these patients, the authors advised that “clinicians should resist anchoring on inadequate treatment of hypothyroidism as the cause of these symptoms and may investigate other disease processes (eg, iron deficiency, B12 deficiency, sleep apnea, celiac disease).”
SOURCE:
The study, led by Matthew D. Ettleson, Section of Endocrinology, Diabetes, and Metabolism, University of Chicago, was published online in Thyroid.
LIMITATIONS:
The cognitive assessments in the study were not designed to provide a thorough evaluation of all aspects of cognitive function. The study may not have been adequately powered to detect small effects of levothyroxine-treated hypothyroidism on cognitive outcomes. The higher levels of education attained by the study population may have acted as a protective factor against cognitive decline, potentially biasing the results.
DISCLOSURES:
The Study of Women’s Health Across the Nation was supported by grants from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
First Patient-Derived Stem Cell Transplant a Success in T1D
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
The chemically induced pluripotent stem cell–derived islets came from the somatic cells of the patient, a 25-year-old woman who had lived for 11 years with unstable T1D with less than 50% time-in-target glucose range despite intensive insulin therapy. By 1 year following the transplantation of the cells into her abdomen, her glucose levels were nearly 100% in range, and her hemoglobin A1c had come down from 7.4%-8.0% to nondiabetic range (~5%).
Of note, she was already under immunosuppression for a prior liver transplant and remained on it throughout. There were no major safety concerns.
“We are very encouraged by the positive clinical findings seen in this first patient using this combination of technologies. These findings set a strong foundation for further development of stem cell–derived islet transplantation as a feasible treatment modality for diabetes,” study authors Soon Yi Liew, PhD, and Hongkui Deng, PhD, both of Peking University Health Science Center, Beijing, China, told this news organization in an email. Dr. Deng, the lead author, is the director of the university’s Institute of Stem Cell Research.
The findings were published in Cell.
What’s New With This Approach?
The use of the patient’s own cells is one of several ways in which this approach differs from other ongoing efforts in treating T1D with pluripotent stem cell–derived islets, such as those of the companies Vertex and Sernova, Dr. Liew and Dr. Deng explained.
Another difference is that “the patient-specific stem cell–derived islets used in this study were produced from induced pluripotent stem cells generated using chemical reprogramming, which is a nontransgenic approach to inducing pluripotent stem cells from somatic cells that uses only small molecules, different from the conventional method of viral transduction of transcription factors. ... Employing small molecules as reprogramming factors provides a greater degree of control — small molecules have defined structures easily manufactured and standardized, are not genome integrating, and are cost effective,” Dr. Liew and Dr. Deng said.
A third difference, they noted, is the placement of the stem cell–derived islets underneath the abdominal anterior rectus sheath of the patient, as opposed to the more commonly used hepatic portal vein. In addition to better ease of visualization, prior evidence suggested that this approach could lead to an improved engraftment and graft function and could circumvent graft loss from blood-mediated inflammatory responses associated with the liver site.
Moreover, they added, “to our knowledge, the rapidity with which insulin-independence was achieved post transplantation of stem cell–derived islets, 75 days post-transplantation, is also a first.”
Immunosuppression Remains a Challenge
Asked to comment, David M. Harlan, MD, the William and Doris Krupp professor of medicine and codirector of the Diabetes Center of Excellence at the University of Massachusetts Chan Medical School, Worcester, told this news organization, “on the one hand, it seems like a great breakthrough that you could take each individual cells and use those to make islets, but ... that process takes a long time, is very, very expensive, and then the T1D recipient still needs to be immunosuppressed. From a business point of view, I just don’t see it as getting any legs.”
Dr. Harlan, who had been involved in the islet transplantation field for several decades, pointed out that the additional autoimmunity of T1D poses a challenge beyond that of the body’s immune reaction to foreign tissue. “Because transplants have been around since the 1950s, we know a lot about how to prevent allogeneic rejection, from one person to another, but we know very little about how to prevent autoimmunity, so that’s still a very difficult nut to crack. I actually think the major effort should be focused on making the beta cells more hardy [via genetic modification] as opposed to focusing on the immune system. And there’s a lot of data to support that now, and that’s what we’re working on.”
Indeed, Dr. Liew and Dr. Deng said, “New immunomodulatory strategies to address graft longevity without immunosuppression remain to be established and tested. With reports of therapeutic efficacy of stem cell–derived islet transplantation such as with our study, stem cell–derived therapy without need for immunosuppression would be a meaningful next step in the treatment of this disease.”
The team has now performed the same procedure in two more patients and will report their data “in due course.”
Dr. Liew had no disclosures. Dr. Deng is a scientific adviser at Hangzhou Reprogenix Bioscience. Two coauthors are employees of Hangzhou Reprogenix Bioscience. Another is a former employee of Hangzhou Reprogenix Bioscience and is now affiliated with the Hangzhou Institute of Medicine, Chinese Academy of Sciences. Four coauthors have patent applications related to this work. Dr. Harlan is chief scientific officer and cofounder of Stability Health. He had no other disclosures.
A version of this article first appeared on Medscape.com.
FROM CELL